Slide 1 - Clinical Departments - Medical University of South Carolina

Keri T. Holmes-Maybank, MD
Medical University of South Carolina
June 18, 2013
Review the famous Groves article “Taking care of the hateful patient.”
Recognize physician characteristics that lead to a greater perception of a patient as
“difficult.”
Recognize patient characteristics and patterns of behavior classified as “difficult.”
Practice the collaboration, appropriate use of power, and empathy approach recommended for managing conflict by Elder.
Illness can alter the patient’s psyche leading to uncharacteristic behavior.
Acknowledge and accept emotional responses to patients.
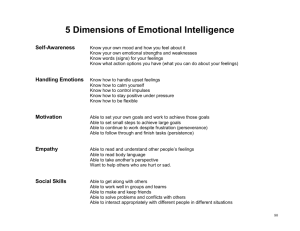
Physician awareness and acceptance of personal emotions may improve emotional intelligence and physician-patient relationships.
Most important is how the physician behaves toward the patient, not the emotion she is experiencing.
Empathy and collaboration are the keys to effective conflict management.
Dependent Clinger
Entitled Demander
Manipulative Help Rejecter
Self Destructive Denier
Appropriate need for reassurance
Escalates to unreasonable, BOTTOMLESS need for explanation, affection, and attention
Constant reassurance
Increasing dependency
See MD as inexhaustible resource
Warning signs:
Extreme gratitude
MD feels special
MD becomes exhausted, patient feels rejected, ramp up needy behavior with more desperate attempts at contact
Repugnance
Dislike
AVERSION
Empathy
Set limits early without feeling inhuman, without patient feeling deceived or disappointed
Difficult to refer to psychiatrist
Interpret as abandonment/rejection
Reassure you will still see them
Overtly hostile, superior
Intimidation, devaluation, induce guilt
Control by threatening punishments
◦ Withholding payment, demands for more tests/consults, or litigation
Lack of control
Compensation for MD power/knowledge
Ultimately fear abandonment
Entitlement = faith and hope in well-adjusted
Fear
Depression
Wish to counterattack
Do NOT debate or belittle
Acknowledge entitlement to have realistic good care
Very respectfully and non-confrontationally to explain how behavior may compromise health
Cooperative decision-making process
Rechannel energy into following the regimen
Smugly satisfied with failure
Do not want cure, want unending relationship with MD
No regimen will help
Pessimism increases with MD’s efforts and enthusiasm
Manipulation
Want MD close but keep them at significant distance - fear
Relationship will not end if they have symptoms
Deny assistance/advice while spiraling into poor health
Anxiety treatable illness being missed, then irritation, then depression and self-doubt
Guilty
Inadequate
Demoralized
Depression
Unproductive, time-consuming, exhausting
Don’t accuse of manipulation = doctor shopping
Share pessimism – say treatment may not be curative
Consistent, firm limitations – unrealistic expectations or demands
Regular follow-up
Patient’s fear of abandonment put to rest
Simple explanations
Hard to refer to psychiatrist
Make sure they have follow-up with MD
Empathy
Patient education
Encouragement and support
Unconscious self-murderous/injurious behaviors
Spiral of self-destruction while requesting assistance
Glory own destruction
Pleasure in defeating MD attempts to preserve life
Profoundly dependent
Self-hate, project hate through the MD
MD caught between ideal of saving patient and unwanted wish for patient to die
Malice
Objectivity challenged by hatred, or indifference (protects MD emotionally)
MD limited because patient will only allow so much care
All reasonable care for patient
Compassion – terminal illness
Do not abandon
Recognize without shame the feelings the patient provoke in MD
Cannot give perfect care
Physician develops positive or negative feelings toward patient based upon personal experiences in her life
Use it to gain knowledge about where patient is coming from
Patient feels threatened = behavioral regression
Projects these feelings onto MD
Patient feels relieved when these feelings are reflected by MD
Example: Patient feels helpless = complains incessantly = MD feels helpless
If MD recognizes can react supportively
Patient autonomy
Patients more educated
Boundaries are being crossed by email and info about physicians on internet
Defensive medicine
Productivity pressures
Changes in health care financing
Fragmentation of visits
Interrupted visits
Outside information sources challenge the physicians authority
Less trust in their physicians
Feel rushed or ignored may repeat themselves or prolong visit
18% of encounters classified as “difficult”
Greater perceived workload/overwork
Lower job satisfaction
Lack of training in communication/poor communication skills
Inexperience
Discomfort with uncertainty
Poor attitude
Professional identity
◦ I am unable to make better ***
◦ Conflicts with my professional standards
Personal qualities
◦ Feel taken advantage of
◦ Difficulty making relationship with patient
Time management
◦ Takes too much time
Comfort with patient autonomy
◦ Patient sets the agenda
Confidence in skills
◦ Too hard to solve
Trust in patient
◦ Lose trust in patient
Increased dissatisfaction with services
Become more demanding
Repeated visits without medical benefit
Seemingly endless complaints
Unmet expectations
Insatiable dependency
Report worsening symptoms
Do not seem to want to get well
Power struggles
Focus on issues seemingly unrelated to medical care
Worried every symptom represents a serious illness
Reported greater symptom severity
Chronic pain (+/- narcotics)
Psychiatric
◦ Axis II
◦ Depression
◦ Somatization (alcohol, borderline)
◦ Mood d/o (insist on physical cause)
◦ Anxiety (multi complaints, think cardiac, not enough being done)
Lower social class
Female
Thick clinical records
Older
More medical problems
Greater use of health care services
Poor functional status
Cluster A (odd or eccentric, fears social relations)
◦ Paranoid
◦ Schizoid
◦ Schizotypal
Cluster B (dramatic, emotional erratic disorders)
◦ Antisocial
◦ Borderline
◦ Histrionic
◦ Narcissistic
Cluster C (anxious or fearful disorder)
◦ Avoidant
◦ Dependent
◦ Obsessive-compulsive
Appendix B
◦ Depressive
◦ Passive-aggressive (negativistic)
Dissatisfaction
Physician's technical competence
Bedside manner
Time spent with clinician
Explanation of what was done
Higher number of visits
Difficult patients
9%
7%
13%
Notdifficult
1%
0.7%
3%
12%
4
3%
2
Jackson, JL, Kroenke K. Difficult Patient Encounters in the Ambulatory Clinic:
Clinical Predictors and Outcomes Arch Intern Med. 1999;159(10):1069-1075.
P <.001
P <.001
P =.002
P <.001
P =.004
Helpless
Inadequacy
Frustration
Anger
Guilt
Dislike
Leads to:
◦ Unconscious punishment of the patient
◦ Self-punishment by the doctor
◦ Inappropriate confrontation
◦ Desperate attempt to avoid patient
◦ Errors in diagnosis or treatment
◦ Decreased quality of care
◦ Work burdensome
◦ Burnout
Disproportionate emotional energy can be spent dealing with negative feelings
Strong negative emotional reaction is important clinical data about patient’s psychology (personality d/o)
Sensitivity to MD feelings
◦ Improved physician well being
◦ Less destructive patient behavior
◦ Lower risk of litigation
Collaboration
Appropriate use of MD power
Empathy
Priority setting
◦ Prioritize patient concerns
Diagnostic skills
◦ Thorough history, physical, and testing
Decision making
◦ Explain
◦ Be consistent and objective
◦ Be honest and fair
◦ Facilitate patient decision making
Team approach
◦ Use referrals (mental health, pain, etc.)
◦ Enlist/see family
◦ Provide quality care
Coaching
◦ Set small, achievable goals
◦ Short term symptom relief
Encourage patient to start taking responsibility
Think of their care as a team effort
Adjust expectations of what can be accomplished
Patient education
Collaboration has most impact on clinical interaction
Set clinical management rules
◦ Schedule patient frequently, longer visits
◦ Clinic time management
◦ Good documentation
Set boundaries and limits
◦ Set general limits
◦ Make explicit rules when necessary
◦ Limit number of patient concerns
◦ Limit time at each visit
Understand patients psyche
Focus on patient emotions
Compassionate and firm
Patient centered
Reinforce positives
Keep professional distance
Protects MD from developing negative responses to difficult and challenging behavior
Allows insight into patient issues and why patient has resorted to negative response patterns
◦ Illness can alter patients – uncharacteristic, childlike
Creates an environment conducive to more suitable health care delivery, a healthier lifestyle, better work satisfaction
Point person - may get conflicting info from consultants
Tactful assessment of patient’s distress/emotion
LISTEN
Interrupt less
Regular, brief summaries of patient’s concerns
Reconcile conflicting views of diagnosis/illness
Acknowledge problem
Both parties may contribute to difficulty
Use communication skills
You can discuss that have poor relationship:
“How do you feel about the care you are receiving from me?”
“It seems to me we sometimes don’t work together very well.”
Use “I” statements
◦ “I feel it’s difficult for me to listen to you when you use that kind of language.”
1. ***Does my patient prioritize health?***
◦ Not if patient works with MD to prevent and treat disease.
◦ Unpleasantness alone is not grounds.
2. Is confrontation of my patient ethically permissible?
◦ If patients self-corrosive decisions come with expectations of accommodation.
◦ If MD bearing majority of burden in failing treatment.
◦ If health deteriorating from patient action or inaction.
3. What if confronting my patient is emotionally gratifying?
◦ Recognize countertransference v. projective identification.
◦ Assess motives and emotions in real time and discuss with a peer.
Butler CC, Evans M. The “heartsink” patient revisited. Br J Gen Pract. 1999;49:230-
233.
Elder N, Ricer R, Tobias B. How respected family physicians manage difficult. J Am
Board Fam Med 2006;19:533– 541.
Feldman MD, Berkowitz SA. Role of behavioral medicine in primary care. Curr Opin
Psychiatry. 2012;25:121-127 .
Kontos N, et al. Fighting the good fight: Responsibility and rationale in the confrontation of patients. Mayo Clin Proc. 2012;87(1):63-66.
Fried TR, Bradley EH, O’Leary J. Prognosis communication in serious illness:
Perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc.
2003;51:1398-1403.
Groves JE. Taking care of the hateful patient. N Eng J Med 1978;298:883-887.
Haas LJ, Leiser JP, Magill MK, Sanyer ON. Management of the difficult patient.
American Family Physician. 2005;72(10)
Jackson, JL, Kroenke K. Difficult Patient Encounters in the Ambulatory Clinic:
Clinical Predictors and Outcomes Arch Intern Med. 1999;159(10):1069-1075 .
Mathers N, Jones N, Hannay D. Heartsink patients: A study of their general practitioners. Br J Gen Pract. 1995;45:293-296 .
O’Dowd TC. Five years of heartsink patients in general practice. BMJ
1988;297:528-530.
Strous RD, Ulman AM, Kotler M. The hateful patient revisited: Relevance for 21st century medicine. European Journal of Internal Medicine. 2006 (17)6;387-393.