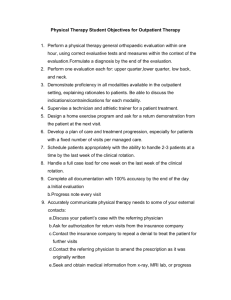
Average Annual Age-Sex Specific Re
advertisement

Average Annual Age-Sex Specific Re-visit Rates for FHT Physician Office Visits: Applying the Provincial Average to your Practice. Measuring and understanding demand is one of the fundamental principles of Advanced Access within the larger domain of Office Practice Re-design. In order to offer primary care patients an appointment without delay, capacity must exist or be created within the scheduling system. Alignment is needed between expected demand for office visits and the available supply of appointments. Annual demand can be measured as the number of patients in a practice or individual provider’s unique panel of patients X the expected number of visits per year per patient. To fully ensure that patient demand meets provider supply, the formula is: panel size X visits per patient per year (demand) = provider visits (# of appointments available) per week X provider weeks worked per year (supply). In the Ontario system however, it has proven to be quite challenging to capture this annual retrospective data to determine if a physician has the capacity to meet the demand of office visits requested by his/her patients. Re-visit rate is not easily individually derived from the various EMR’s or the OHIP billing system. To assist with this challenge, the Institute for Clinical Evaluative Sciences (ICES) has provided a spreadsheet (attached) of average annual FHT age-sex specific re-visit rates for physician office visits, courtesy of Dr. Rick Glazier. Characteristics of this data are: The data represents the average annual physician age-sex specific re-visit rate across FHT’s Collection period: From September 1, 2007 – August 31, 2008 for those patient who were enrolled with a FHT physician at any time during this period, who remained alive on August 21, 2008 Includes patient visits to all primary care physicians, i.e., not just visits to the physician with whom the patient is enrolled Includes walk-in clinics Excludes ER visits Does not include non-rostered patients When studying your annual patient re-visit profile, some important factors to be mindful of are: Your practice style may differ from the provincial average i.e. a physician may generate lower or higher re-visit rates, e.g., you may have higher revisit rates based on more internal demand (demand that you are generating for return visits). Teams are at different levels of interprofessional collaborative practice, potentially impacting re-visit rates; i.e., teams may be reducing physician visits as a result of enhancing scopes of practice of the team. The visit/appointment length; i.e., ‘same unit to same unit’ measurement may not apply when trying to match / compare the provincial FHT average age-specific demand with supply, i.e., appointment lengths may vary. Panel profile is not static. Panel composition varies and as such, so does demand. Determine your annual ‘look-back’ period. As close as possible to the present is likely the best reflection of your current panel. 1. Enter the number of your rostered patients in each age-sex cell of the spread sheet. The annual number of visits is calculated automatically. Populating this spread sheet with the number of your rostered patients provides you with an estimate of your annual demand for physician office visits based on FHT average age-sex specific annual visits rates for physician office visits. This is a more detailed analysis compared to an over-all average re-visit rate, but it is important to note that this may or may not be reflective of your practice. The tool allows you to examine your annual capacity using the provincial FHT average as a benchmark. 2. Adjust the total to include non-rostered patient visits during the same time frame. The number of non-rostered patients may vary significantly between FHT’s, and the re-visit pattern may also differ. 3. Calculate your annual supply within the identified time frame: available physician appointments per week X physician weeks worked per year. Ideally you are looking for alignment in your demand and supply. 1 + 2 = 3 Suggestions for how to use this spreadsheet: Moving forward: There are a number of considerations / strategies to employ if there is an imbalance in supply and demand. Starting points are: Capturing daily demand, supply and activity data, as this will provide more detailed information about the capacity and functioning of your practice / system / schedule. Analyzing your system and focusing on efficiency is a highly effective strategy to improve the functioning of the practice and increase capacity, integral to Advanced Access. If demand < supply: If in doing further studying annual and daily demand, you determine that you have more supply than demand, this suggests that you have unmet capacity in your practice and if you follow the principles of Advanced Access, you are likely in a position to enroll additional patients. If demand > supply: Should you find that demand is outweighing supply other strategies to re-shape / increase demand include: Maximizing the interprofessional team, shifting work to the most appropriate team member(s) Increasing the re-visit interval Max-packing visits Using the technology effectively, e.g., telephone follow-up where appropriate …………..all of which can reduce the number of physician visits that are required to meet the needs of your patient population. 2 Health Quality Ontario