File - Amanda McWhinney
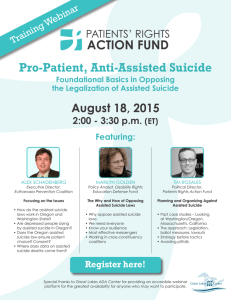
advertisement

Amanda McWhinney Research Paper Final Draft Friday, January 25, 2013 The legalization of physician assisted suicide has been an issue of controversy for several decades. Within the past few years, Oregon and Washington have legalized the practice, and other states are beginning to consider it as well. This paper is regarding whether or not physician assisted suicide should be legalized in all states. I believe physician assisted suicide is unethical, therefore, should not be legalized in all states. After doing much research, both in class as well as outside of class, I believe that there are three key reasons why it should remain illegal in all states— (1.) the term “terminally ill” is difficult to define and patients can outlive their prognosis, (2.) it is necessary to experience the entire process of dying, and (3.) physicians take the Hippocratic Oath to “cause no harm to patients.” “On October 27, 1997 Oregon enacted the Death with Dignity Act which allows terminally-ill Oregonians to end their lives through the voluntary self-administration of lethal medications, expressly prescribed by a physician for that purpose,” (Death with Dignity Act). The first reason why I do not believe physician assisted suicide should be legalized is because the phrase “terminally ill” is very difficult to define. According to the textbook Intervention and Reflection, author J. Gay Williams states, “Contemporary medicine has high standards of excellence and a proven record of accomplishment, but it does not possess perfect and complete knowledge. A mistaken diagnosis is possible, and so is a mistaken prognosis” (Munson 595). Terminally ill is defined as having no more than six months to live. There are numerous cases in which patients live much longer than their initial prognosis. In cases where the prognosis given to a patient is incorrect or inaccurate, and physician assisted suicide is legalized and therefore chosen by the patient, this can lead to the ending of life prematurely. 1 While conducting research on this particular aspect of the practice of physician assisted suicide, I found several videos and interviews with a woman, Tahni Morrell, whose husband was given just two months to live. Paul Morrell was diagnosed with colon cancer and after battling the disease for two years, his doctors gave him his prognosis with just a few months to live (Committee Against Physician Assisted Suicide). Paul surprised his doctors by outliving his prognosis by five and a half years. Tahni Morrell states, “It’s awful to think he [Paul] might have made a terrible decision based upon a doctor’s guess and cost us all that extra time together” (Committee Against Physician Assisted Suicide). Patients outlive their prognosis all the time and surprise themselves, their families, doctors and the rest of society. Physician assisted suicide should not be legalized in all states because when death becomes closer to a patient, it is necessary to experience the entire process of dying. As stated by Tahni Morrell, the time that her family was able to spend with Paul was the most precious gift they could have received from him. Based on the fact that they had no idea when Paul would pass away, they were able to make their time left with him count. When our class visited Hospice of Dubuque, Bonnie Hancock and Renee Frith, touched on this important aspect as well. If a patient was to end his/her life through physician assisted suicide, he/she would lose out on numerous opportunities. In the process of dying, patients are given the opportunities for family interaction, reconnection of old friends, forgiveness, helping others and the ability to let go and allow oneself to be helped and served (Hancock, and Frith). When a patient enters into Hospice, he/she is able to set individual goals that he/she would like to meet before he/she passes away. For example, if a patient would like to reunite with his/her distant son that he/she has not spoken to in decades, Hospice takes note of that and tries to meet these goals. If a patient ended his/her life with the practice of physician assisted suicide, he/she may not even consider reconnecting 2 with distant loved ones, due to the fact that he/she just wants to end his/her life and “get it over with.” Along with patients outliving their prognosis and experiencing the entire process of dying, I believe that physician assisted suicide should remain illegal in most states because physicians and doctors’ main purpose of their profession is to save lives. The practice of physician assisted suicide ultimately goes against this healing goal. One of the most common arguments is that patients should have the right to die if they would like to. In rebuttal, doctors and physicians should always provide the best health care to all of their patients, regardless of age or health. If this practice is legalized, J. Gay Williams states his belief: “It [physician assisted suicide] could have a corrupting influence so that in any case that is severe doctors and nurses might not try hard enough to save the patient. They might decide that the patient would simply be ‘better off dead’ and take the steps necessary to make that come about. This attitude could then carry over to their dealings with patients less seriously ill. The result would be an overall decline in the quality of medical care” (Munson 595). The role of the physician is that of a healer. However, the legalization of physician assisted suicide in Oregon and Washington have turned that role for some physicians into the role of a killer. Physicians are required to take the Hippocratic Oath, which states: “I will neither give a deadly drug to anybody who asked for it, nor will I make a suggestion to this effect” (Tyson). In the states of Oregon and Washington, physicians who have given the lethal drug to patients who asked for it have already broken this oath. Also, if physician assisted suicide became legal in all states, physicians would be able to legally suggest this, which again, is breaking the Oath. 3 If physician assisted suicide became legalized throughout all of the United States, patients who are terminally ill may feel obligated to commit suicide. When diagnosed, patients may feel as if they are a burden to the family members, and may consider ending their life much more of an option than if it remained illegal. Rather than continuing to provide the care and medications to the patient, physicians would most likely participate in the assisted suicide instead of trying to meet the needs of the patient. “The American Medical Association affirms that patients should not be abandoned simply because a cure may be impossible, as now happens too often… Patients near the end of life deserve to receive emotional support, comfort care, adequate pain control, respect for patient autonomy, and good communication” (Gloth III). Ultimately, the legalization of this practice and allowing physicians to participate in it would cause more harm than good to society. When arguing that physician assisted suicide is unethical and essentially wrong, it is necessary to apply ethical theories to the situation. The first theory that could be applied is Principalism. This theory states that all ethics can be reduced to four basic principles: autonomy, beneficence, nonmaleficence and justice. I believe that physician assisted suicide can be related to three of these principles, including, autonomy, beneficence and nonmaleficence. The principle of autonomy is the right to direct the course of one’s life (Class Notes). Autonomy can come into play with this topic because it is essentially the decision of the patient whether or not to end his/her life. The patient has the final control of remaining alive and dying naturally, or participating in physician assisted suicide. He/she is taking control and basically can choose the exact moment of his/her death. Beneficence can be defined as the duty to act in ways that promote the welfare of people and taking positive steps to help others (Class Notes). I believe that beneficence can be related to 4 physician assisted suicide because death can be looked at in a positive light if it is ending the suffering of the patient. When patients are terminally ill they usually suffer from several types of pain, whether it is physical, emotional or psychological, and oftentimes may feel more at peace if the suffering were to just end completely. When medications and treatments cannot stop the suffering, in some cases people may feel as if the positive step to help the patient is through physician assisted suicide. However, this may not always be factually correct. There is a way to promote the welfare of human beings who are suffering and dying through the use palliative care. This is the care that focuses on relieving and preventing the suffering of patients. This is a more positive way to view and treat the dying process. Nonmaleficence is the duty to act in ways that do not cause harm or injury to people (Class Notes). This practice of physician assisted suicide violates this principle due to the fact that it deliberately takes the life of a patient. Death is the ultimate harm that could be brought on someone. The Sixth Commandment states “Thou shall not kill” very clearly and I do not think there should be any exception to this. I believe the principle of nonmaleficence takes precedence over autonomy and beneficence in this case because there is no greater harm that could be done to someone than causing him/her to die. The second ethical theory that can be applied to the topic of physician assisted suicide is the theory of Utilitarianism, particularly Act Utilitarianism. This theory is about the “consequences of a particular action in a particular circumstance” (Class Notes). An action is considered right, according to Utilitarianism, when it promotes the greatest good for the greatest number of people. There are four steps to applying this theory; the first is to determine the course of action that can be taken in the situation (Class Notes). When relating this to the topic, the two 5 courses of action for the patient would be either to legalize physician assisted suicide or to allow only natural death. The second step of Utilitarianism is to determine the possible consequences for everyone affected for each course of action (Class Notes). For legalizing physician assisted suicide, some of the consequences for the patient would be the end of the suffering, as well as the termination of one’s life. For the family, some consequences would include the grief over the loss of the loved one, guilt for supporting the loved one end his/her life and the contentment of knowing that the loved one is not experiencing any more pain and suffering. For allowing only a natural death, some consequences for the patient would be the opportunities to interact with family and friends, find closure in the dying process, continue possible pain and suffering, reconnect with distant loved ones, grow in one’s spiritual life and have the chance to say a proper farewell to everyone. Some consequences for the family of the loved one would include helping the loved one in every step of the dying process, growing closer to him/her, being able to say a proper goodbye and find closure, and feeling content knowing that the loved one died in a natural, peaceful way. The third step of the Utilitarianism theory is to evaluate the consequences for each course of action and determine a value for that specific consequence (Class Notes). Regarding the ending of one’s life through physician assisted suicide, the consequences for the patient can be seen as both positive and negative. The consequences for the family can mostly be viewed at as being negative. On the other hand, the majority of the consequences of the patient dying a natural death tend to be more on the positive end. The family also experiences positive consequences as well. The fourth and final step of this theory is to determine the course of action that has the best consequences overall, or least bad consequences overall. In this case and by applying this theory 6 of Utilitarianism, I believe that allowing the patient to die naturally is the best course of action to take. One of the main reasons that people support physician assisted suicide is that it relieves the patient of his/her pain and suffering. Terminal illnesses generally come with harsh side effects and often causes the individual to “lose control” over his/her natural bodily functions and his/her life. Another argument in favor would be that patients often experience an inability to function in ways that make life meaningful. People with these terminal diseases do not want to live the rest of their lives in a way that is “not like them.” I acknowledge this argument and recognize where these opposing views are coming from. Janet Conn, President of the organization Compassion and Choices in Minnesota even offers this argument as well: “Most people don’t die in a very natural way, people tend to die in intensive care units where they are attached to machines…I think when death is swift and natural, that can be what you call peaceful and dignified” (Conn). In response to this strong argument in favor of legalized physician assisted suicide, one thing that people should consider is the practices of Hospice and palliative sedation. The goal of Hospice is to affirm life and try to improve patients’ comfort naturally (Hancock, and Frith). They provide a very natural process for patients, in which they go into their homes and keep them comfortable, peaceful, managed and allow them to spend time with their families. They provide medications for the patients’ symptoms, however on rare occasions that the symptoms are intractable; they do allow the patients and families to decide if they would like palliative sedation. Palliative sedation is essentially sedation to the point of unconsciousness, in which the patient will not wake up and will eventually die naturally when he/she is ready. It is for patients 7 in their final stage of terminal illness and an intervention of last resort to relieve pain (Class Notes). Unlike the practice of physician assisted suicide, in which the goal is to deliberately end the life of the patient, the goal of palliative sedation is to keep the patient comfortable. I believe that palliative care is a better, more ethical, option for end-of-life care due to the fact that no one is deliberately taking the life of a human being. Physician assisted suicide is a topic in which there are very strong arguments both in favor and against it. The most common argument supporting this practice is that people should be allowed the choice to be relieved of their pain and suffering. However, I believe that there are more, and stronger, arguments against this topic. The term “terminally ill” is difficult to define, and people oftentimes outlive their prognosis. There are also several opportunities that patients going through the dying process are allowed to experience if they choose to die in a natural state; opportunities that those who end their own lives miss out on. Physicians take the Hippocratic Oath and vow not to harm their patients, and this practice is the clearly violating that statement. The two ethical theories of Principalism and Utilitarianism argue against physician assisted suicide as well, and the alternatives of Hospice and palliative care offer a more natural and dignified death. Ultimately, I do not believe that physician assisted suicide is ethical by any means and I do not believe that is should be legalized. 8 Works Cited Class Notes Committee Against Physician Assisted Suicide, Question 2 Massachusetts. 2012. Video. Committee Against Physician Assisted SuicideWeb. 21 Jan 2013. <http://www.stopassistedsuicide.org/>. Conn, Janet. Personal Interview. 17 Jan 2013. "Death with Dignity Act." Oregon Health Authority. Oregon.gov. Web. 22 Jan 2013. <http://public.health.oregon.gov/ProviderPartnerResources/Evaluationresearch/deathwith dignityact/Pages/index.asp>. Gloth III., F. Michael. "Physician Assissted Suicide: The Wrong Approach to End of Life Care." United States Conference of Catholic Bishops. United States Conference of Catholic Bishops, n.d. Web. 21 Jan 2013. <1.http://www.usccb.org/issues-and-action/human-lifeand-dignity/assisted-suicide/to-live-each-day/physician-assisted-sucide-wrongapproach.cfm>. Hancock, Bonnie, and Renee Frith. Personal Interview. 18 Jan 2013 Munson, Ronald. Intervention and Reflection: Basic Issues in Bioethics. 9th. Boston: Wadsworth, 2012. 555-618. Tyson, Peter. "The Hippocratic Oath Today." NOVA. WGBH Website, 27 Mar 2001. Web. 21 Jan 2013. <1.http://www.pbs.org/wgbh/nova/body/hippocratic-oath-today.html >. 9