Who gets spinal cord injuries and how?
advertisement

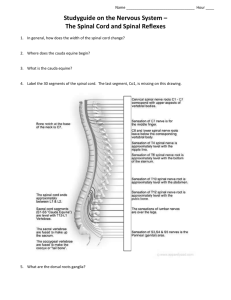
Spinal Cord Injury Too big a topic for 30 minutes…………….. • Goals: • Demographics • Mechanisms of Injury & Pathophysiology • Presentation & Diagnosis including common spinal cord syndromes Special Added Attraction: Neuroanatomy • Management • Little Fun • Won’t Cover • Bony spinal injuries • Imaging • SCIWORA Review! Who gets spinal cord injuries and how? What is the cost and frequency? Risk Factors • Young male most likely victim • Males 77-80% • Alcohol involved in at least 25% • Underlying spinal diseases • • • • Cervical spondylosis Atlantoaxial instability Osteoporosis Spinal arthropathies- ankylosis spondylitis or rheumatoid arthritis Spinal Cord Injury Facts • Direct medical expenses accrued over the lifetime of one patient- $500K- $2 million • Traumatic Spinal Cord Injury (TSCI) • Incidence 2010- 40 per million per year or approx. 12,400 annually • 2005- approx. 250,000 living survivors of TSCI in USA • Causes TSCI in US: • • • • • MVA 48% Falls 16% Violence (GSW, SW, etc) 12% Sports accidents 10% Other 14% Patients with spinal cord injuries are sick! What are the mechanisms of injury? Primary vs Secondary Injury? Pathophysiology • Most produced in association with injury to vertebral column • Fracture of one or more bony elements • Dislocation at one or more joints • Tearing of ligaments • Disruption and/or herniation of the intervertebral disc Pathophysiology: Primary vs Secondary Injury • Primary Injury- immediate effect of trauma • Forces of compression, contusion, shear injury to cord • Secondary Injury: • Begins within minutes & evolves over hours • Complex & incompletely understood • Mechanisms • • • • • • Ischemia Hypoxia Inflammation Edema Excitotoxicity Apoptosis • Clinically manifest by neurologic deterioration over first 8-12 hrs in patient who initially present with incomplete cord syndrome • Spinal cord edema develops within hours of injury • Maximal day 3-6 • Begins to recede after day 9 • Gradually by replaced hemorrhagic necrosis Clinical Presentation How do you assess the severity of spinal cord injury? Clinical Presentation • Typically pain at site of spinal fx • Patients with TSCI often have associated brain & systemic injuries that may limit patient’s ability to report localized pain • Approx 50% TSCI’s involve cervical cord and present with quadriparesis or quadriplegia • Severity of spinal cord syndromes classified using American Spinal Injury Association (ASIA) Scale • This is the “Stroke Scale” for Spinal Injury Terms • Sacral Sparing • Sensory sacral sparing includes sensation preservation (intact or impaired) at the anal mucocutaneous junction (S4-S5 dermatome) on one or both sides for light touch or pin prick or deep anal pressure (DAP) • Motor sacral sparing includes presence of voluntary contraction of external anal sphincter on digital rectal exam • Bulbocavernosus Reflex • Pull on foley or gently pinch penis or clitoris and monitor anal contraction • If reflex is intact, the anal sphincter will contract • Presence of the reflex indicates an incomplete lesion • Anal Wink (anocutaneous reflex) • Contraction of anal sphincter in response to pinprick stimulus of perineum • Deep Anal Pressure • Examiner’s finger inserted and gentle pressure applies to anorecal wall • Alternatively, pressure can be applied by using thumb to gently squeeze the anus against the inserted index finger. • Consistently perceived pressure should be graded as being present or absent (YES or NO) American Spinal Injury Association (ASIA) Complete Cord Injury (ASIA Grade A) • Rostral zone of spared sensory levels (C5 and higher dermatomes spared with C5-6 fx-dislocation), reduced sensation in the next caudal level, & no sensation in levels below, including NONE in sacral segments S4-S5 • Reduced muscle power in level immediately below injury followed by complete paralysis more caudally • Acute stage- reflexes absent, no response to plantar stimulation, muscle tone flaccid • Male w/ complete lesion may have priapism • Bulbocavernosus reflex usually absent • Urinary retention and bladder distention occur Incomplete Cord Injury (ASIA grades B-D) • Various degrees of motor function in muscles controlled by levels of spinal cord caudal to injury • Sensation partially preserved in dermatomes below area of injury’ • Sensation often preserved to a greater extent than motor function because sensory tracts are located in more peripheral, less vulnerable areas of the cord • Bulbocavernosus reflex and anal sensation often present • Incidence of incomplete vs complete has increased over last 50 yrs Neuroanatomy of the Spinal Cord Spinal Cord anatomy • Cross-sectional anatomy — The spinal cord contains the gray matter, the butterfly-shaped central region, and the surrounding white matter tracts. • The spinal cord gray matter, which contains the neuronal cell bodies, is made up of the dorsal and ventral horns, each divided into several laminae Spinal Cord Anatomy • Ventral Horn: • Contains motor nuclei of the spinal cord • Also contains interneurons mediating information from other descending tracts of the pyramidal and extrapyramidal motor systems. • Dorsal Horn: • Entry point of sensory information into the CNS. • Processes sensory information • Modulates pain transmission through spinal and supraspinal regulatory circuits. Efferent Motor Tracts • Pyramidal: • Originate in cerebral cortex • Carry motor fibers to spinal cord & brainstem • Corticospinal Tract (CST): voluntary control of muscles of body • To ipsilateral musculature • Anterior Corticospinal Tract (15-20%): ends in cervical & upper thoracic cord • Lateral Corticospinal Tract (80-85%): • Crosses in medulla & terminates in ventral horn. • From ventral horn goes to spinal nerve and muscles • Corticobulbar Tract: voluntary control of muscles of face • Extrapyramidal • • • • • Originate in brainstem & carry fibers to spinal cord Responsible for involuntary & automatic control of muscular function such as muscle to ne, balance, posture, & locomotion Tectospinal tract: mediates reflex postural movements of the head in response to visual and/or acoustic input Vestibulospinal: balance, posture, antigravity muscles Reticulospinal: • • • Medial Reticulospinal: increases tone & facilitates voluntary movements Lateral Reticulospinal: decrease tone & inhibits voluntary movements Rubrospinal: via red nucleus ?fine motor hand Afferent Sensory Tracts • Dorsal Column Medial Lemniscal (DCML)Pathway: • Ipsilateral fine touch (tactile sensation), vibration, & proprioception • In brainstem it is transmitted thru the medial lemniscus • Enter cord into dorsal horn and then go to ipsilateral Dorsal Columns • Dorsal Columns = Posterior Columns • Fasciculus cuneatus: cervical/thoracic- lateral localization/orientation • Fasciculus gracilis: lumbar/sacral- medially localization/orientation • Spinothalamic: • Enter cord and cross midline (anterior(aka ventral) commissure) then go to contralateral Anterior STT or Lateral STT • Anterior Spinothalamic: contralateral crude touch & pressure • Sensations not accurately localized (itch & tickle) • Lateral Spinothalamic: contralateral pain & temperature • Cervical medial localization/orientation • Sacral lateral localization/orientation • Spinocerebellar Tracts: The dorsal and ventral spinocerebellar tracts carry inputs mediating unconscious proprioception directly to the cerebellum • Spinoreticular tract carries deep pain input to the reticular formation of the brainstem Spinal Cord Blood supply • A single anterior and two posterior spinal arteries supply the spinal cord • Anterior spinal artery supplies anterior 2/3 of the cord • Posterior spinal arteries primarily supply the dorsal columns • Anterior & Posterior spinal arteries arise from vertebral arteries in neck • Various radicular arteries branch off the thoracic and abdominal aorta to provide addition blood supply to the spinal arteries • Artery of Adamkiewcz (aka Great Ventral Radicular Artery) • Largest & most consistent of radicular branches • Supplies the Anterior Spinal Artery • Enters spinal cord anywhere btn T5 &L1 (usually T9-T12) • Anterior Spinal Artery uninterrupted along the entire length of the spinal cord in most • In others, it is discontinuous, usually in midthoracic segment • These individuals more susceptible to vascular injury • The primary watershed area of the spinal cord in most people is in the midthoracic region Location of lesion in central cord syndrome Central Cord Syndrome • Characterized by loss of pain and temp sensation in the distribution of one or several adjacent dermatomes at the site of the spinal cord lesion • As a central lesion enlarges, encroachs on medial aspect of the corticospinal tracts or on the anterior horn gray matter, producing weakness in the analgesic areas. • There are usually no bladder symptoms. • Due to disruption of crossing spinothalamic fibers in the ventral commissure. • Dermatomes above & below the lesion have normal pain & temp sensation, creating the so-called “suspended sensory level” • Vibration & proprioception ( Dorsal Columns) are often spared. • Most frequently result of hyperextension injury in patients with long-standing cervical spondylosis. Get disproportionately greater motor impairment in upper compared with lower extremities, bladder dysfunction, and a variable degree of sensory loss below the level of injury Location of lesion in Brown-Sequard syndrome Brown-Sequard Syndrome • A lateral hemisection syndrome involves the dorsal column, corticospinal tract, and spinothalamic tract unilaterally. • Produces ipsilateral weakness, loss of vibration, & proprioception & contralateral loss of pain and temperature . The unilateral involvement of descending autonomic fibers does not produce bladder symptoms. • CAUSES: knife or bullet injuries & demyelination are most common causes. Rarer causes include spinal cord tumors, disc herniation, infarction & infections. Location of lesion in Anterior (Ventral) Cord Syndrome Anterior (ventral) cord syndrome • Relatively rare historically related to decreased blood supply • usually includes tracts in the anterior two-thirds of the spinal cord, • Corticospinal tracts, Spinothalamic tracts, and descending autonomic tracts to the sacral centers for bladder control • Corticospinal tracts injury produce weakness and reflex changes. Spinothalamic tract deficit produces bilateral loss of pain & temp sensation. • Tactile, position, & vibratory sensation as normal since controlled by DORSAL COLUMNS • Urinary incontinence is usually present • Causes: spinal cord infarction, intervertebral disc herniation, and radiation myelopathy. Location of lesion in posterior (dorsal) cord syndrome Dorsal (posterior) cord syndrome • Bilateral involvement of dorsal columns, corticospinal tracts, & descending autonomic tracts to bladder control centers in sacral cord • Dorsal column symptoms include gait ataxia and paresthesias • Corticospinal tract dysfunctions produces weakness • Acute: muscle flaccidity & hyporeflexia • Chronic: muscle hypertonia and hyperreflexia • Extensor plantar responses and urinary incontinence may also be present • CAUSES: MS,tabes dorsalis, Friedreich ataxia, subacute combined degeneration, vascular malformations, epidural and intradural extramedullary tumors, cervical spondylotic myelopathy, and atlantoaxial subluxation. Cauda Equina Syndrome • Involves lumbosacral nerve roots of cauda equine & may spare the cord itself • Injury to the nerve roots will classically produce flaccid paralysis of muscles of lower limbs (muscles affected depend on level of injury) and areflexic bowel & bladder. • Often asymmetric • All sensory modalities are similarly impaired & may be partial or complete loss of sensation • Sacral reflexes, bulbocavernosus & anal wink, will be absent • Causes: intervertebral disc herniation, epidural abscess, epidural tumor, intradural extramedullary tumor, lumbar spine spondylosis, and a number of inflammatory conditions including spinal arachnoiditis, chronic inflammatory demyelinating polyneuropathy, and sarcoidosis Conus medullaris syndrome • Similar to Cauda Equina but injury is more rostral in cord (L1 & L2 area) • Most commonly due to thoraco-lumbar bony injury • Depending on level of lesion, may manifest with mixed picture of upper motor neuron (due to conus injury) and lower motor neuron symptoms (due to nerve root injury). • Some cases difficult to clinically distinguish from cauda equina injury • Sacral segments may occasionally show preserved reflexes (ie bulbocavernosus & anal wink) with higher lesions of conus medullaris • There is early and prominent sphincter dysfunction with flaccid paralysis of the bladder and rectum, impotence, and saddle (S3-S5) anesthesia. • Leg muscle weakness may be mild if the lesion is very restricted and spares both the lumbar cord and the adjacent sacral and lumbar nerve roots. • Causes: disc herniation, spinal fracture, and tumors Transient Paralysis & Spinal Shock • Immediately after SCI, may be a physiological loss of all spinal cord function caudal to level of injury with flaccid paralysis, anesthesia, absent bowel & bladder control, loss of reflex activity • In males, especially those with cervical cord injury, priapism may develop. • May also be bradycardia & hypotension not due to causes other than the spinal cord injury. • May be secondary to loss of K from injured cells & accumulation in the extracellular space causing decreased axonal transmission Initial Evaluation & Management • ABCDE • Capnography • High cervical injuries may require intubation • Hypoxia in face of cord injury can adversely affect outcome • Hypotension- hypoperfusion can adversely affect outcome • Detailed neuro exam ASAP (ASIA format useful) Glucocorticoids for Rx of TSCI? • Still controversial? • Not recommended at HFH • “Steroids and Spinal Cord Injures: Steroids are NOT indicated for spinal cord injury” • HFH Trauma Practice Guidelines p.35 Prognosis for TSCI• Initial ASIA Grade A (Complete TSCI) • 10-15% improve • 3% improve to ASIA Grade D • <10% will be ambulatory at 1 year • Initial ASIA Grade B: • 54% recover to C or D • 40% regain some ambulatory ability • Initial ASIA Grade C: • 62% able to ambulate independently • Initial ASIA Grade D: • 97% able to ambulate independently • Most recovery for patients with incomplete TSCI takes place in first 6 months The Beer ? Who is this? Frank Netter MD “The Michelangelo of Medicine” 1906-1991