Occupational Health Risks for Healthcare Workers
advertisement

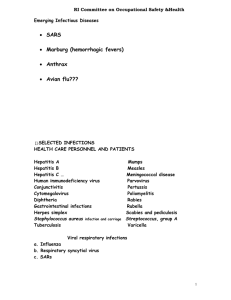
Occupational Health Risks for Healthcare Workers 1. Recognize infection health hazards for healthcare workers. 2. Explain the use of an occupational infection risk evaluation. 3. Outline methods of reducing occupational risk of infection for healthcare workers. December 1, 2013 Learning Objectives 2 • 40 minutes December 1, 2013 Time involved 3 • Biological hazard • Chemical hazard • Physical hazard • Ergonomic hazard • Psychosocial hazard December 1, 2013 Health Hazards in Healthcare Facilities 4 • If a separate department, size based on • Institution size • Number of staff • Services offered December 1, 2013 Occupational Health • Elements • • • • • Medical evaluations Education Immunisation program Management of illness/exposures Maintenance of records 5 • Conduct written risk assessment for staff hazards • • • • • Physical Chemical Biological Ergonomic psychosocial December 1, 2013 Prevention of Occupational Risk in Healthcare Facilities • Assess risk and estimate degree of risk annually 6 • 3 million healthcare workers exposed to bloodborne pathogens each year • > 90% of infections occur in developing countries • 95% of HIV seroconversions in HCWs caused by needlestick injuries December 1, 2013 Bloodborne Infection among Healthcare Workers 7 Risk group Description Examples 1 Biological agent unlikely to cause human disease Bacteria in yoghurt Yeast in beer 2 Biological agent that can cause human disease and might be a hazard to workers; it is unlikely to spread to the community; there is usually effective prophylaxis or treatment available Most bacteria Nearly all moulds Most viruses 3 Biological agent that can cause severe human disease and present a serious hazard to workers; it may present a risk of spreading to the community, but there is usually effective prophylaxis or treatment available Hepatitis B Hepatitis C Human immunodeficiency virus Tuberculosis 4 Biological agent that causes severe human disease and is a serious hazard to workers; it may present a high risk of spreading to the community; there is usually no effective prophylaxis or treatment available Lassa virus Severe acute respiratory syndrome? December 1, 2013 Biological Agents: Risk of Infection 8 Infection Cholera Conjunctivitis, viral (e.g., adenovirus) Cytomegalovirus (CMV) Diphtheria Haemorrhagic fever (Ebola, Marburg, Lassa virus) Hepatitis A Transmission in general Risk of transmission evaluation Risk classification of biological agents* Main risk Vaccine available Post-exposure prophylaxis (PEP) Staff to patient Rare Patient to staff Rare 2 Stool contact Yes High High 2 No No Rare Rare 2 Hand contact and touching eye Contact with body fluids, especially saliva, blood, and urine No No No data Rare 2 Close face to Yes face exposure, cough Bloodborne; some question of contact transmission Negligible Moderate 4 Blood splash on mucous membrane No Person-to-person by faecal-oral route; infected food handlers with poor personal hygiene can contaminate food Rare Rare 2 Stool contact Yes Faecal-oral, contaminated water Contact with eye secretions and contaminated objects Contact with urine, saliva, breast milk, cervical secretions, and semen from infected person who is actively shedding virus By droplets, also by contact December 1, 2013 Risk evaluation for infectious agents - 1 PEP with antibiotic should be discussed Antivirals should be discussed Immune globulin 9 Infection Transmission in general Risk of transmission evaluation Hepatitis B Via percutaneous, mucosal, and nonintact skin contact with blood, semen, vaginal secretions, and bloody fluids Via percutaneous, mucosal, and nonintact skin contact with blood, semen, vaginal secretions, and bloody fluids Contact with virus in saliva of carriers; contact with vesicle fluid Primarily via percutaneous contact with blood; mucosal or nonintact skin contact with blood; semen, vaginal secretions, and bloody body fluids less likely to transmit Low Moderate Low Hepatitis C Herpes simplex Human immunodeficiency virus (HIV) Risk Main risk classification of biological agents* 3 Needlestick injury Vaccine available Moderate 3 Needlestick injury No No Rare Low 2 Contact with infected site No No Rare Low 3 Needlestick injury Yes Postexposure prophylaxis (PEP) Hepatitis B immune globulin (HBIG) December 1, 2013 Risk evaluation for infectious agents - 2 Antivirals must be provided within hours! 10 Infection Transmission in general Risk of transmission evaluation Influenza Droplet spread; direct droplet transmission or droplet to contact transmission of respiratory secretions of infected patients Airborne; direct airborne transmission or airborne to contact transmission of respiratory secretions of infected person Droplet spread; direct droplet transmission or droplet to contact transmission of respiratory secretions of infected patients Droplet spread; direct droplet transmission or droplet to contact transmission of respiratory secretions of infected patients Direct and indirect contact Moderate Moderate Risk classification of biological agents* 2 High High 2 Rare Moderate Rare Measles Meningococcal infection Mumps Methicillinresistant S. aureus (MRSA) Main risk Vaccine available Post-exposure prophylaxis (PEP) Close contact with patient (Within 3 feet from coughing/ sneezing) Inhaling or contact with the patient’s respiratory secretions Yes Antivirals normally not recommended Yes Immune globulin 2 Close contact; face to face Yes (tetravalent A, C, W135, and Y) Antibiotic after close contact Moderate 2 Yes Rare 2 Close contact with patient (Within 3 feet from coughing/ sneezing) Skin contact December 1, 2013 Risk evaluation for infectious agents - 3 11 No No Infection Transmission in general Risk of transmission evaluation Norovirus Faecal-oral (direct or indirect contact with patient’s stool) Droplet spread; direct droplet transmission or droplet to contact transmission of respiratory secretions of infected patients Faecal-oral Animal bite Droplet contact or direct contact with respiratory secretions Person-to-person via faecal-oral route Droplet contact or direct contact with respiratory secretions; airborne transmission not demonstrated. High Pertussis Polio Rabies Respiratory syncytial virus (RSV) Rotavirus Rubella Vaccine available Post-exposure prophylaxis (PEP) High Risk Main risk classification of biological agents* 2 Stool contact No No Moderate Moderate 2 Cough Yes Macrolides Rare Rare Moderate Rare Rare Moderate 2 3 Bites Yes Yes Yes Moderate Moderate 2 Stool contact Moderate Moderate 2 December 1, 2013 Risk evaluation for infectious agents - 4 Yes 12 Infection Transmission in general Risk of transmission evaluation Salmonella or Shigella Person-to-person via faecal-oral route; via contaminated food or water; food handlers with poor personal hygiene can contaminate food Droplets, contact Low Severe acute respiratory syndrome (SARS) Scabies Streptococcus, Group A Syphilis Tetanus Postexposure prophylaxis (PEP) Low Risk Main risk Vaccine classification available of biological agents* 2 Stool contact Medium Medium 3 No Direct skin-to-skin contact with infested person Droplet contact or direct contact with oral secretions or drainage from infected wounds Direct contact with lesions of primary or secondary syphilis Low Low Rare No data 2 No data Rare 2 Bites, skin wounds No data No data Cough No December 1, 2013 Risk evaluation for infectious agents - 5 Skin contact 2 Direct contact with skin or mucous membrane lesions Antibiotics possible 13 Yes Immune globulin Infection Transmission in general Tuberculosis (TB) Airborne transmission Low to high from sources with active pulmonary or laryngeal tuberculosis; susceptible person must inhale airborne droplet nuclei to become infected Low to high Typhus Faecal-oral Low Low 3 Varicella, Chickenpox, disseminated zoster Contact with vesicles; droplet or airborne spread from respiratory tract of acute cases and perhaps from disseminated zoster High High 2 moderate moderate Negligible Rare Localised varicella-zoster (shingles) Yellow fever Contact with vesicles Mosquito bites Risk of transmission evaluation Risk Main risk classification of biological agents* 3 Cough Vaccine available BCG Bacille Calmette Guérin (Not given to healthcare workers) Stool contact Yes (IM, SC, oral) Yes Postexposure prophylaxis (PEP) Isoniazid (INH) for treatment of latent TB infection; 4 drug regimen for active TB December 1, 2013 Risk evaluation for infectious agents - 6 Varicellazoster immune globulin (VZIG) 14 Yes No • Eliminate the hazard Reduce the number of injections by providing oral medication Assign a central hospital for treating highly infectious patients December 1, 2013 Risk Reduction - 1 15 • Remove or isolate the hazard Use safety needles Single-use needles designed to retract or cover the sharp end immediately after use December 1, 2013 Risk Reduction - 2 Transport blood specimens in leak- and punctureresistant boxes Use puncture-resistant waste boxes for discarding sharp items and needles 16 • Organisational measures Limit number of staff members caring for a patient with certain illnesses Tuberculosis or MRSA Train staff regularly in safe work practices Establish an occupational safety committee Consider every patient to be potentially infected with hepatitis B or C or HIV Strict adherence to Standard Precautions/Routine Practices Audit compliance with prevention measures periodically December 1, 2013 Risk Reduction - 3 17 Evaluate use of personal protective equipment • Gloves • Discard and change between patients • Use only once or disinfect 2-3 times maximum December 1, 2013 Risk Reduction - 4 • Gowns • • • • Use if spills/splashes are possible Change between patients Single-use gowns preferred If used several times put on and remove it without touching the outer potentially contaminated side • e.g., during a shift time 18 Evaluate use of personal protective equipment • Eye goggles or face shields • Use if spills/splashes to the face possible • Disinfect regularly and if visibly soiled • Masks and respirators December 1, 2013 Risk Reduction - 5 • N95/FFP respirators with a tight face seal used if a risk of exposure to airborne pathogens • When not available, use surgical masks Develop written standard operating procedures For medium and high-risk activities Include staff protection and vaccination recommendations 19 • Provide a medical examination for all HCWs • Examination records and other health information should be kept confidential • Store in a secure place December 1, 2013 Risk Reduction - 6 • Repeat the examination periodically • All injuries documented in the respective staff member’s medical record 20 • Provide vaccinations for all non-immune HCWs Hepatitis B Influenza Mumps/Measles/Rubella/Varicella/Pertussis Poliovirus Tetanus, Diphtheria (as a routine adult vaccination) December 1, 2013 Risk Reduction - 7 21 • • • • Recapping of needles Unsafe handling of sharps waste Overuse of injections Lack of supplies December 1, 2013 Causes of Needle-stick Injury in Low Resource Countries • disposable syringes, safer needle devices, sharps-disposal containers • Failure to place needles in sharps containers immediately after injection • Passing instruments from hand to hand(e.g., in the OR) • Lack of awareness of the problem • Lack of training for staff 22 • The risk of transmission of bloodborne pathogen from an infected patient to a HCW by a needlestick injury: December 1, 2013 Risk of Blood-borne Pathogen Transmission • 30% for hepatitis B • 3% for hepatitis C • 0.3% for HIV 23 Post-exposure prophylaxis varies with immune status of HCW An unvaccinated HCW Receive both hepatitis B immune globulin (HBIG) and HBV vaccination Previously vaccinated and known antibody responder HCW No treatment Previously vaccinated, known non-responder HCW Both HBIG and HBV vaccination (a second vaccine series) or 2 doses of HBIG one month apart HCWs whose antibody response is unknown Test the HCW for antibody and administer HBIG + HBV vaccination if results are inadequate (<10mIU/ml) December 1, 2013 Hepatitis B Prevention: PEP 24 • Currently no recommended PEP for hepatitis C virus • Perform baseline and follow-up testing for antiHCV and alanine aminotransferase December 1, 2013 Prevention of Hepatitis C • Up to six months after exposure • Perform HCV RNA testing at 4-6 weeks • If an earlier diagnosis of HCV infection is desired • Staff members who develop hepatitis C should be treated after seroconversion 25 • Start as soon as possible, within 2-24 hours, not after 72 hours • Consider contraindications (e.g., pregnancy) • Medication taken for at least 4 weeks • Seek expert consultation if viral resistance is suspected • In case no PEP is available December 1, 2013 Prevention of HIV Infection: PEP • Perform HIV antibody testing for at least six months post exposure (e.g., at baseline, 6 weeks, 3 months, and 6 months) • Perform HIV antibody testing if an illness compatible with an acute retroviral syndrome occurs • Advise exposed persons to use precautions to prevent secondary transmission during the follow-up period 26 • Establish a tuberculosis control committee • Increase awareness about TB among HIV-positive patients • Place patients with suspected TB or with an abnormal chest radiograph in an isolation room December 1, 2013 Prevention of TB - 1 • With door closed and a special ventilation system (natural or artificial) • Place automatic closing devices on all TB isolation room doors • Continue isolation of TB patients until at least three negative acid-fast bacilli sputum smears obtained • Ensure that all HCWs entering a TB isolation room wear a N95/FFP mask • Restrict sputum induction procedures and aerosolised pentamidine treatments to TB isolation rooms 27 • Assign adequate number of trained staff to perform routine and urgent acid-fast bacilli smears on a daily basis • Initial anti-TB treatment regimens should include four drugs • TB patients should only be allowed to leave their rooms when medically necessary and must always wear a surgical mask when outside the room • Forbid immunocompromised staff from contact with, or caring for, TB patients • Perform routine tuberculin testing for tuberculin negative staff • Treat HCWs as soon as active TB is confirmed December 1, 2013 Prevention of TB - 2 28 • Healthcare workers are exposed to biological, chemical, physical, ergonomic, and psychosocial hazards • HBV, HCV, HIV and TB pose the greatest risk of infection • Infection with hepatitis B virus is preventable with immunisation December 1, 2013 Summary • All healthcare workers should be vaccinated against hepatitis B • Written standard procedures on how to manage needlestick injuries should be available and known to all staff 29 • Health worker occupational health. World Health Organization. 2010. http://www.who.int/occupational_health/topics/hcworkers /en/ • AIDE-MEMOIRE for a strategy to protect health workers from infection with bloodborne viruses. World Health Organization. 2011. http://www.who.int/injection_safety/toolbox/en/AM_HCW _Safety_EN.pdf • Simonsen L, Kane A, Lloyd J, Zaffran M, Kane M. Unsafe injections in the developing world and transmission of bloodborne pathogens: a review. Bull WHO 1999; 77: 789800. http://www.who.int/bulletin/archives/77(10)789.pdf December 1, 2013 References 30 1. Mucosal exposures cause 95% of HIV seroconversions in staff. T/F. 2. Prevention of tuberculosis includes a. b. c. d. Placing patient in an isolation room Patient wears mask when leaving the room Perform AFB lab tests daily All of the above December 1, 2013 Quiz 3. A risk assessment for staff hazards is useful to determine appropriate prevention strategies. T/F. 31 • IFIC’s mission is to facilitate international networking in order to improve the prevention and control of healthcare associated infections worldwide. It is an umbrella organisation of societies and associations of healthcare professionals in infection control and related fields across the globe . • The goal of IFIC is to minimise the risk of infection within healthcare settings through development of a network of infection control organisations for communication, consensus building, education and sharing expertise. • For more information go to http://theific.org/ December 1, 2013 International Federation of Infection Control 32