32byron-1 - ByronPsychology
advertisement
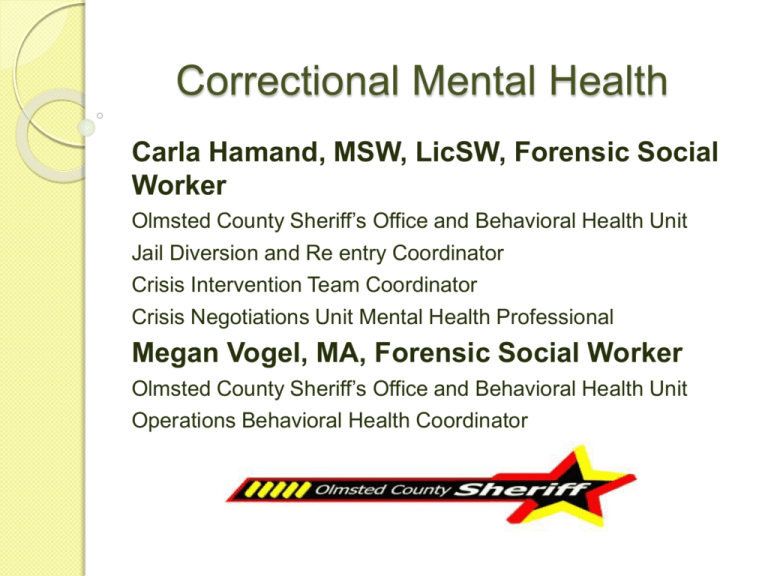
Correctional Mental Health Carla Hamand, MSW, LicSW, Forensic Social Worker Olmsted County Sheriff’s Office and Behavioral Health Unit Jail Diversion and Re entry Coordinator Crisis Intervention Team Coordinator Crisis Negotiations Unit Mental Health Professional Megan Vogel, MA, Forensic Social Worker Olmsted County Sheriff’s Office and Behavioral Health Unit Operations Behavioral Health Coordinator Objectives What are mental health professionals doing in the criminal justice system? What population do we serve? What mental health issues are most commonly seen in this population? Diagnostic assessment Open Discussion/Questions Working Within Criminal Justice System or in a Correctional Facility Balance the needs and interests: ◦ Individual in conflict with the law ◦ The mandate and of the various correctional agencies and organizations ◦ The perspective of victims ◦ Obligations to the community ◦ With an overriding emphasis on both public and personal safety A Social Worker’s Scope of Practice Within Corrections Highly dynamic Intense workloads Management of sensitive information Participation on interdisciplinary teams Building community partnerships Evidence-based best practices Olmsted County ADC Mental Health Team To provide those programs and services which are designed to evaluate, prevent, and treat mental health problems and which contribute to safe, humane corrections environments. Interdisciplinary Team: ◦ ◦ ◦ ◦ ◦ ◦ Operations Social Worker Forensic Social Worker Forensic Psychologist Psychiatrist Nursing Operations Staff Forensic Social Worker Jail Diversion-forensic assessment Re entry-Assess, Plan, Identify, Coordinate CIT CNU Court Commitments/Civil/Forensic Educator Supervise Interns Research Operations Social Worker Morning meeting Brief Jail Mental Health Screening Tool Prioritize day Assessment Treatment planning Educator Statistics Levels of Service 1-2-3 Mandated Services ◦ Suicide Risk and Assessment ◦ Screening for Mental Health Needs ◦ Crisis Intervention ◦ Medication Services offered to Specific Target Groups ◦ Substance Abuse/Dependence ◦ Anger Management ◦ Voluntary Programs ◦ Voluntary Psychiatric/Psychological Services ◦ Case Management Level Three ◦ Training for Correctional Staff ◦ Open Dialogue Between Correctional Staff and Correctional Mental Health Staff ◦ Assisting Administrators with Policy Define Mental Illness Most Commonly Seen in ADC Most Common Disorders Bio Psycho Social Environmental Cultural Issues Co-morbidity Substance Abuse/Dependence Adjustment Disorder Personality Disorders Mood Disorders Anxiety Disorders Psychotic Disorders Sexual Disorders Examine the Population Being Served 2.3 million housed in US prisons and jails 5 million on probation or parole 6% have a serious and persistent mental illness 20% have a serious mental illness 30-60% have substance abuse problems *US Census 311,915,120 Bio Psycho Social Environmental Cultural Factors ◦ Problems related to interaction with the legal system/crime ◦ Problems with primary support group ◦ Educational problems ◦ Occupational problems ◦ Housing problems ◦ Economic problems ◦ Problems with access to health care services ◦ Problems related to the social environment ◦ Other biopsychosocial and environmental problems Diagnosis Axis I Axis II Axis III Axis IV Axis V Axis I vs. Axis II Complicated Diagnostic Picture ◦ When the psychotic symptoms are controlled with medication, the underlying personality disorder becomes primary, resulting in behaviors that are difficult to treat and possibly unpleasant to work with. ◦ Misinterpretation of behavior. Dual Disorders, Co-morbidity or Co-occurring ◦ The presence of one or more disorders (or diseases) in addition to a primary disease or disorder. Substance Use Dependence Polysubstance Dependence Alcohol Dependence Amphetamine Dependence Opioid Dependence Personality Disorders Cluster A: • Avoidant • Dependent • ObsessiveCompulsive Cluster B: • • • • Antisocial* Borderline* Histrionic Narcissistic Cluster C: • Paranoid • Schizoid • Schizotypal Personality Disorders Distinctive set of traits, behavior styles and patterns that make up our character or individuality. How we perceive the world, our attitudes, thoughts, and feelings are all part of our personality. People with healthy personalities are able to cope with normal stresses and have no trouble forming relationships with family, friends, and coworkers. Those who struggle with a personality disorder have great difficulty dealing with other people. Personality Disorder Tend to be inflexible, rigid, and unable to respond to the changes and demands of life. Although they feel that their behavior patterns are “normal” or “right,” people with personality disorders tend to have a narrow view of the world and find it difficult to participate in social activities. A deeply ingrained, inflexible pattern of relating, perceiving, and thinking serious enough to cause distress or impaired functioning. Usually recognizable by adolescence or earlier, continue throughout adulthood, and become less obvious throughout middle age. Antisocial Personality Disorder Most commonly found in males. Very high percentage of prison/jail population. Characterized by: ◦ ◦ ◦ ◦ ◦ ◦ A pattern of disregard for others Involvement with law enforcement Fail to abide by social norms Aggressiveness Irritability Lack of concern for safety of self/others Actual Character, Ted Bundy Fictional Character, Hannibal Lector Random Character Borderline Personality Disorder Affects 2% of population Women tend to be most commonly diagnosed with BPD. Characterized by: ◦ Instability in relationships ◦ Impulsivity ◦ Low self-image ◦ Onset in early adulthood Social Chameleon Someone who changes the way they interact with people depending on who they're with. Anxiety Disorders PTSD: Common in veterans of war, victims/witnesses of violent crime, refugees, survivors of traumatic events. 10-20% incidence in law enforcement. Can occur at any age or time in life. Symptoms usually begin within 3 months of trauma but there may be a delay of months or years before symptoms appear. Symptoms may wax and wane throughout the disorder. Mood Disorders Depression ◦ 15% lifetime occurrence. ◦ Symptoms that interfere severely with the ability to work, sleep, eat, and the ability to enjoy pleasurable activities. ◦ Symptoms last longer than two weeks. Bipolar Disorder ◦ Also known as manicdepression ◦ Characterized by a wide swing in moods from high to low-each episode last about two weeks in a year-long period ◦ Others (10-30%) will develop rapid-cycling with four or more episodes in one year ◦ Type I and II ◦ “Low” and “high” symptoms ◦ “Low” symptoms the same as depression Psychotic/Thought Disorders Schizophrenia Schizophrenia Paranoid Type Schizoaffective Disorder Delusional Disorder Schizophrenia Schizophrenia is not “Split Personality” There is a common notion that schizophrenia is the same as "split personality” – a Dr. Jekyll-Mr. Hyde switch in character ◦ ◦ ◦ ◦ ◦ ◦ Affects 1% of the world’s population 2.7 million is the United States Treatment can result in 85% remission rates Onset is between 17-30 for women Onset is 20-40 for men Irrational thought processes Assessment Client Interview Collateral: Bio Psycho Social Environmental Cultural Psychometric Testing ◦ Gathering information from other sources can often help in the assessment. Family Friends Witnesses Providers Other resources (social services, detox) Assessment What brings them in? What is currently the matter? List all the symptoms that the client has experienced in their lifetime. List the current symptoms that the client is reporting. Inquire about additional symptoms. Have a discussion about the severity of symptoms. What level of impairment do the symptoms bring to their daily functioning? What substances have been used? Is there abuse or dependence? What are the symptoms? How do the symptoms interfere/affect symptoms of mental illness? Criminogenic Factors—Determining Risk WHY? Genetics Environment Bio Psycho Social Medical Brain Injury Drug Induced Other? In the diathesis–stress model, a biological or genetic vulnerability or predisposition (diathesis) interacts with the environment and life events (stressors) to trigger behaviors or psychological disorders. The greater the underlying vulnerability, the less stress is needed to trigger the behavior or disorder. Conversely, where there is a smaller genetic contribution greater life stress is required to produce the particular result. Even so, someone with a diathesis towards a disorder does not necessarily mean they will ever develop the disorder. Both the diathesis and the stress are required for this to happen. Websites http://www.co.olmsted.mn.us/sheriff/division s/lec/Pages/cit.aspx http://psychservices.psychiatryonline.org/cgi/ content/full/57/4/544/F1 http://gainscenter.samhsa.gov/pdfs/reentry/ap ic.pdf http://www.pbs.org/wgbh/pages/frontline/sho ws/asylums/ http://www.pbs.org/wgbh/pages/frontline/rele ased/view/ http://longgonefilm.net/