PALS Santa Rosa de Copan - Emory University Department of
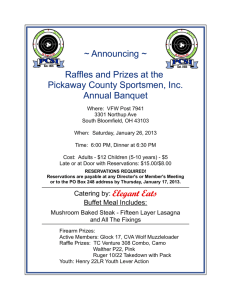
advertisement

PALS Santa Rosa de Copan Central American Medical Outreach CAMO Hospital Regional de Occidente February 25-28, 2008 PALS Objective – To teach Pediatric Advanced Life Support to a group of medical professionals in Santa Rosa de Copan Students came from many areas of Honduras including Tegucigalpa, Gracias, Santa Rosa de Copan, and Cesamo San Jose Copan Map of Honduras The Hospital Classrooms were housed in the Hospital Regional de Occidente Class list Group A Clara Lainez, MD Instituto Hondureno Seguro Social (IHSS) Thunia Fancinily, MD IHSS Alma Rodriguez, MD Hospital Regional Occidente ( HRO) Yadira Carcamo, MD Hospital Gracias Nelson Penman, MD HRO Jorge Madunado, MD HRO Hector Sandoval, MD HRO Class list Group B Jeanette Flores, MD Cesamo San Jose Copan Gloria Cacenes, MD Cesamo San Jose Copan Claudia Calix, MD Hospital Gracias Sonia Delattibodier, MD HRO Marisabel Rivera, MD HRO Marco Rodriguez, Paramedico, Santa Rosa de Copan Map of Honduras SRDC, Gracias, Tegucigalpa The Faculty Carlos Delgado, MD – Emory University, Atlanta, Georgia David Goo, MD - Emory University, Atlanta, Georgia Alex Rogers, MD - University of Michigan, Ann Arbor, Michigan Ricardo Jimenez, MD– All Children’s Hospital, St. Petersburg, Florida The Faculty Faculty The Course The PALS video was shown and translated into Spanish, pausing the video while discussion and translation occurred Skills station checklists were checked off and signed by the instructors Shock lecture was given in Spanish Dysrhythmia lecture was translated into Spanish Skills Stations Skills stations Skills Stations Skills stations BLS 1 person 30:2 2 Person 15:2 AED Airway Defibrillator Dysrhythmias Presenting the Video Intra-osseous Lecture Intra-osseous station Where to decompress a pneumothorax? Defibrillator Station Guest Lecturer Natalie (Anesthesiologist at Hospital Occidente) DOPE Pneumonic En Espangnol Desplazamiento Obstruccion Pneumotorax Equipo Shock Lecture Assess-Categorize-Decide-Act Testing Scenarios Las Drogas Teaching The Broselow Tape Working the Megacode Megacode Clinical Testing All participants passed the megacode. A few clinical deficiencies were identified and corrected. Thanks to the CAMO support staff Organization of participants Course Manuals Preparation of mannequins and all the many supplies for airway, BLS, AED, etc Copies of materials and tests Snacks, coffee, lunch Chicken legs for the intr-osseus skills station CAMO Organization of Equipment CAMO Support Staff Lunch and Snacks The Written Test Written Testing Pre-test and discussion were translated into Spanish Actual test was in Spanish 7 out of the 13 passed on the first try (Passing grade of 84) 2 missed just one extra question (80) Most were with in two questions (76) Remediation Remediation Tests were graded and key points were reviewed without answering the actual questions on the test. Participants were re-tested and all passed successfully Lunch post testing Graduation 13 Medical Professionals successfully finished the new PALS course Continued objectives will be to return and in time teach instructors and have a sustainable PALS class here in Santa Rosa de Copan Success! Faculty Organization Accomplishments Four pediatric emergency medicine attendings from 3 different hospitals around the US successfully put on a PALS course in Spanish The trip was self funded with the cooperation of CAMO a large non-profit group in Honduras Faculty preparation and teaching time as well as some equipment were donated to the course and hospital. In kind course donations Central American Medical Outreach About CAMO CAMO has been serving Central America since 1993. CAMO's founder, Kathryn Tschiegg, RN served as a Peace Corps volunteer in Honduras. Kathy returned to Honduras with a team of physicians and technicians from the United States in early 1992. In 1993 she founded CAMO to provide medical supplies, equipment and education to hospitals and clinics in Central America. CAMO At present, CAMO serves over 67,000 people a year in Central America Receives over $2million dollars in donated supplies, time and financial contributions. A distribution center was built in Honduras in 2003 and is now operated by CAMO’s Central American counterpart –Fundación CAMO. Fundación CAMO serves as CAMO USA’s local partner and conduit to the community. Equipment Each year has seen an increase in the size and the number of specialty teams and an increase in the amount of medical equipment integrated into the public health system. All equipment provided by CAMO is technically sound and in good working order. This equipment would be or has been discarded in the United States. Sustainability CAMO trains Honduran public health staff to use the donated equipment through the efforts of licensed medical professionals from the United States who donate their time and services to Central American hospitals and clinics. These medical teams travel with the sole purpose of integrating medical equipment and technology into the daily workings of these facilities and training the Central American staff to use their new skills after the U.S. teams leave. CAMO Programs Capital Improvements in Medical Facilities Dental Program Wheelchair Repair and Distribution Surgical Development: Orthopedics, Plastics, Eye, and Urology Prosthetic Lab MMERV Program Medical Education Technical School Research and Development Community Center/Gym Audiometry Multidisciplinary Breast Clinic Eye Clinic Day Care Center Medical Education Educational Programs Currently Running: • Respiratory care and equipment • Neonatal care & NALS • ACLS & CPR • OB/GYN • Laboratory and X-ray • Emergency medical services • Dentistry and orthodontics • Mammography & related areas Now PALS Accountability Where Does the Money Go? With the extensive network of volunteers and in-kind contributions CAMO is able to get $7 dollars worth of work and equipment out of very $1 donated – enabling CAMO to give the money to those who need it most. Volunteer Costs – Time and $$ It costs about $1,000 per team member for a week in Honduras Medical professionals donate their time with the understanding that they participate in an ongoing program which might require a commitment of 1 -2 weeks per year for five years. PALS will probably take three to four trips to accomplish the goal of a self-sustaining course Hospital Grounds Surgery and Women’s Surgery Emergency Room Ambulance Area Old Pediatric Area Outside Old Pediatric Ward Current Pediatric Ward Nursing Station Pharmacy Enfermera Preparing Meds Penicillin Test Dose Rounding with the Pediatricians Radiology and Chart Filing System in the Patients Bedspace (Chair) Reviewing X-rays Chest X Ray ? Pneumothorax Femoral Cutdown Femoral Cutdown Done at bedside Pediatrician on call, covers ER, Nursery, and Inpatient wards Used a 10 French feeding tube cut off at an acute angle and inserted into the femoral vein after nicking. Vessel then ligated and feeding tube tied in. Intubated in General Pediatric Ward Mother with Ventilated Child Hospital Occidente 18 month old female with a history of one week of eye swelling. No fever No history of trauma No pertinent past medical history Hospital Occidente ? Bot Fly Pathology Ophthalmomyiasis refers to the invasion of the lids, conjunctiva, cornea, and rarely the orbit or globe of the mammalian eye by fly larvae (order Diptera) .1 The human botfly (D hominis) is the most common cause of cutaneous myiasis in Central and South America, but few cases of external ophthalmomyiasis and no previous case to our knowledge of orbital invasion have been reported.2 1. Savino DF, Margo CE, McCoy ED, Friedl FE. Dermal myiasis of the eyelid. Ophthalmology. 1986;93:1225-1227. 2. Wilhelmus KR. Myiasis palpebrarum. Am J Ophthalmol. 1986;101:496-498. ambergriscaye.com/pages/town/botfly2.html The Bot Fly Scientific classification Kingdom: Animalia Phylum: Arthropoda Class: Insecta Order: Diptera Suborder: Brachycera Infraorder: Muscomorpha Section: Schizophora Subsection: Calyptratae Superfamily: Oestroidea Family: Oestridae http://en.wikipedia.org/wiki/Botfly The Human Bot Fly Bot Fly Pathology The female botfly glues her eggs onto the abdomen of a captured mosquito or other common fly. When the carrier insect lands on a human, the larva, or bot, hatches, burrows into the skin, and positions itself "head down" to feed, breathing through caudal respiratory spiracles. ambergriscaye.com/pages/town/botfly2.html Bot Fly Pathology The larva withdraws through a central punctum, falling to the ground and pupating before emerging as a mature botfly.3 Chloroform or lidocaine to anesthetize the bot may facilitate surgical removal as does occluding the breathing hole with ointment, beeswax, chewing gum, or pork fat.4 3. Lane RP, Lowell CR, Griffiths WA, Sonnex TS. Human cutaneous myiasis: a review and report of three cases due to Dermatobia hominis. Clin Exp Dermatol. 1987;12:40-45. 4. Elgart ML. Flies and myiasis. Dermatol Clin. 1990;8:237-244. ambergriscaye.com/pages/town/botfly2.html Human Bot Fly ambergriscaye.com/pages/town/botfly2.html Human Bot Fly ambergriscaye.com/pages/town/botfly2.html NICU Pediatric Interns in the NICU Premature Infant Hospital Occidente Macrosomia Edema Respiratory Failure Shock Breathing over ventilator NICU Flowsheet Dobutamine Albumin Furosemide Hydrocortisone Ciprofloxacin Clindamycin Fluconazole Midazolam Fentanyl Albuterol/Atrovent D10 NS Delayed Capillary Refill Time Post Bolus Improvement in CRT Delivery Room Resuscitation Equipment Delivery Room Delivery Area - Nursery ONLY Breast Feed! Breast Feeding Teaching Area Lecture to Pediatric Housestaff Benefits Cultural exchange Teaching Potential collaboration in the future Exposes us to the limitations of medical practice in other parts of the world Enlightens us about how our counterparts work internationally