NICE NG12 Suspected cancer - Croydon Health Services NHS Trust
advertisement

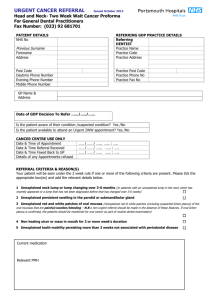
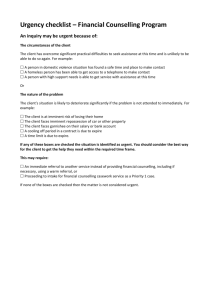
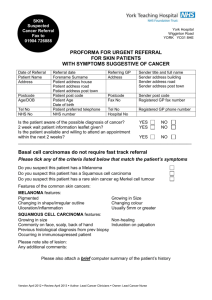
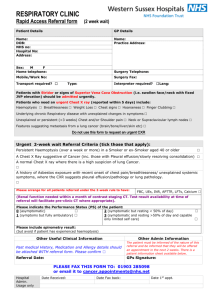
NICE NG12, 2015 Suspected cancer: recognition and referral The pan-London approach 11/11/2015 Dr Ishani Patel 1 Opening questions •How many patients were diagnosed via the 2ww route? •How many new diagnoses are made via A&E? •Which cancers are most likely to present in this way? •Why? •Have you read the new guidelines? •Your thoughts? UK outcomes lag behind 45 Colorectal cancer one year survival 90 AUS Lung Cancer one year survival SWE CAN 40 AUS SWE 85 CAN NOR 80 NOR 35 DEN DEN UK 75 UK 30 25 70 20 65 1995-99 AUS 100 2000-02 CAN SWE 1995-99 2005-07 NOR DEN UK 2000-02 AUS CAN Breast cancer one year survival SWE 2005-07 NOR DEN UK Ovarian cancer one year survival SWE 98 CAN NOR 80 CAN AUS 75 AUS 96 94 NOR 70 DEN 65 DEN UK UK 60 92 55 90 1995-99 AUS 2000-02 CAN SWE 2005-07 NOR DEN UK 50 1995-99 AUS 2000-02 CAN NOR 2005-07 DEN UK NG12, 2015 • Updated NICE guidelines for suspected cancer referrals was based on primary care data and is symptoms based • Reduced from 5-10% to a ≤3% PPV threshold • Suspected cancer pathway referrals and urgent direct access investigations • Transforming cancer services team are working with London Cancer Alliance and London Cancer • Pan-London routes/forms/pathways consistent with NICE, with a few exceptions and retention of past criteria • Educational support alongside the forms – due to be for formal use by March 2016 4 NG12, 2015 • There are 176 recommendations • Emphasis on Safety netting Child safeguarding Vulnerable adult safeguarding • Most importantly….. These recommendations are recommendations, not requirements, and they are not intended to override clinical judgement. 5 Pan-London Approach • Forms that integrate with all IT systems • Moving towards all electronic referrals (no more fax) • Check boxes for safeguarding concerns, mobility, sensory issues • Weblink to guidelines within the form • Autopopulate information from the record • Bloods • Imaging reports • Guidance/prompts within the form where needed • Patient information leaflets – translated into 11 languages 6 July 2015 edition MrsTT Mrs • • • • • • 65 year-old woman PMHx Type 2 Diabetes DHx Simvastatin, Metformin, Ramipril SHx Lives with partner and teaches in local school BMI 29 Last bloods on record are from 6 month ago • Describes a month of worsening mid back pain and some persisting left thigh pain for two months or so…. Brought on after a long walk in the Cotswolds • Self cared with OTC analgesia • Now beginning to affect her sleep • No weight loss in fact (to her dismay) in fact trying to lose weight as she hates taking so many pills for her long-term conditions! What would you do next? MrsTT Mrs Bloods FBC shows mild leucopenia Calcium on borderline ESR borderline for age Renal function normal Bone scan/ MRI Imaging Vertebral fracture at T10 Femur x-ray normal NICE Mrs T recommends Offer a FBC, CALCIUM, ESR for patients aged > 60 with 1. Back pain 2. Persistent bone pain (> 6 weeks) 3. Unexplained fracture Offer serum protein electrophoresis and Bence Jones Protein urine test within 48 hours to patients aged > 60 with 1. Raised ESR 2. Presentation consistent with possible MYELOMA Pan-London approach: Lowered age thresholds to > 40 years old Investigation Raised plasma viscosity or erythrocyte sedimentation rate and presentation consistent with myeloma Possible cancer Myeloma Recommendation Protein electrophoresis and Bence-Jones protein urine test < 48 hours Myeloma Refer using suspected cancer pathway Hypercalcaemia or leucopenia and presentation consistent with myeloma, age ≥60 years Protein electrophoresis or Bence-Jones protein urine results suggest Myeloma Haematological Leukaemia Myeloma Lymphoma Very urgent investigation: Refer children and young people for immediate specialist assessment for leukaemia if they have: • Unexplained petechiae OR • Hepatosplenomegaly. Offer a very urgent full blood count (within Urgent investigation: Offer a full blood count, blood tests for calcium and plasma viscosity or erythrocyte sedimentation rate (ESR) to patients aged: • 60 and over with: – Persistent bone pain (particularly OR back pain) – Unexplained fracture. Immediate Specialist Assessment: Consider very urgent referral (appointment within 48 hours) in children and young people with: • Unexplained lymphadenopathy OR • Splenomegaly. Take in to account associated symptoms, particularly: • Fever • Night sweats • Shortness of breath • Pruritus • Weight loss. Urgent referral: 48 hours) in children and young people with any of the following unexplained signs or symptoms: • Pallor • Persistent fatigue • Fever • Persistent infection • Generalised lymphadenopathy • Persistent or unexplained bone pain • Bruising • Bleeding. Consider a very urgent full blood count (within 48 hours) in adults with any of the following unexplained signs or symptoms: • Pallor • Persistent fatigue • Fever • Persistent or recurrent infection • Generalised lymphadenopathy • Bruising • Bleeding • Petechiae • Hepatosplenomegaly. Accompanying notes: Refer adults, children and young people with a blood count or blood film reported as acute leukaemia immediately. Offer a very urgent protein electrophoresis and a Bence-Jones protein urine test (within 48 hours) to patients aged: • 60 and over with: – Hypercalcaemia OR Leucopenia AND – A presentation that is consistent with possible myeloma. Consider a very urgent protein electrophoresis and Bence-Jones protein urine test (within 48 hours) if: • Raised plasma viscosity or ESR at levels consistent with myeloma AND • Presentation consistent with myeloma. Urgent referral: Urgently refer (appointment within two weeks) if the results of protein electrophoresis or Bence- Jones protein urine test suggest myeloma. Consider urgent referral (appointment within two weeks) in adults presenting with: • Unexplained lymphadenopathy OR • Splenomegaly. Take in to account associated symptoms, particularly: • Fever • Night sweats • Shortness of breath • Pruritus • Weight loss • Alcohol-induced lymph node pain. Haematology Recommendation Full blood count < 48 hours Full blood count < 48 hours Full blood count < 48 hours Features Possible Cancer Recommendation Features Possible Cancer Hepatosplenomegaly Splenomegaly (unexplained) taking into account any fever, night sweats, shortness of breath, pruritus, or weight loss Leukaemia Non-Hodgkin’s lymphoma Full blood count < 48 hours Consider suspected cancer pathway referral Fatigue (persistent) in adults Fever (unexplained) Leukaemia Infection (unexplained and persistent or recurrent) Leukaemia Bruising, bleeding, or petechiae (unexplained) Lymphadenopathy (generalised) Lymphadenopathy (unexplained) taking into account fever, night sweats, shortness of breath, pruritus, weight loss, or alcohol induced lymph node pain Leukaemia Lymphadenopathy or splenomegaly (unexplained) with fever, night sweats, or pruritus Lymphoma Consider suspected cancer pathway referral Pallor Leukaemia Lymphoma Shortness of breath with unexplained lymphadenopathy or splenomegaly Persistent back pain or bone pain or unexplained fracture age ≥60 years Lymphoma Consider suspected cancer pathway referral Weight loss with unexplained lymphadenopathy or splenomegaly Full blood count < 48 hours Consider suspected cancer pathway referral Myeloma Offer full blood count, blood tests for calcium, and either plasma viscosity or erythrocyte sedimentation rate Leukaemia Full blood count < 48 hours Leukaemia Full blood count < 48 hours Lymphoma Consider suspected cancer pathway referral Haematology Haematology Leukaemia in adults Consider a very urgent full blood count (within 48 hours) to assess for leukaemia in adults with any of the following: • • • • • • • • • pallor persistent fatigue unexplained fever unexplained persistent or recurrent infection generalised lymphadenopathy unexplained bruising unexplained bleeding unexplained petechiae hepatosplenomegaly. Leukaemia in children and young people Refer children and young people for immediate specialist assessment for leukaemia if they have unexplained petechiae or hepatosplenomegaly. Offer a very urgent full blood count (within 48 hours) to assess for leukaemia in children and young people with any of the following: • • • • • • • • pallor persistent fatigue unexplained fever unexplained persistent infection generalised lymphadenopathy persistent or unexplained bone pain unexplained bruising unexplained bleeding. 13 Haematology Non-Hodgkin's lymphoma in adults • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for non-Hodgkin's lymphoma in adults presenting with unexplained lymphadenopathy or splenomegaly. When considering referral, take into account any associated symptoms, particularly fever, night sweats, shortness of breath, pruritus or weight loss. Non-Hodgkin's lymphoma in children and young people • Consider same day specialist assessment for non-Hodgkin's lymphoma in children and young people presenting with unexplained lymphadenopathy or splenomegaly. When considering referral, take into account any associated symptoms, particularly fever, night sweats, shortness of breath, pruritus or weight loss. Hodgkin's lymphoma in adults • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for Hodgkin's lymphoma in adults presenting with unexplained lymphadenopathy. When considering referral, take into account any associated symptoms, particularly fever, night sweats, shortness of breath, pruritus, weight loss or alcohol-induced lymph node pain. Hodgkin's lymphoma in children and young people • Consider same day specialist assessment for Hodgkin's lymphoma in children and young people presenting with unexplained lymphadenopathy. When considering referral, take into account any associated symptoms, particularly fever, night sweats, shortness of breath, pruritus or weight loss. 14 Skin Malignant melanoma Squamous cell carcinoma Basal cell carcinoma Urgent referral Urgently refer (appointment within two weeks) if: • The patient presents with a suspicious pigmented skin lesion that has a weighted 7-point checklist score of 3 or more OR • Dermoscopy suggests malignant melanoma of the skin. Urgent referral: • Consider urgently referring (appointment within two weeks) if patient has a skin lesion that raises the suspicion of squamous cell carcinoma. Urgent referral: Only consider urgent referral (appointment within two weeks) for patients with: • A skin lesion that raises the suspicion of a basal cell carcinoma if there is concern that a delay may have an unfavourable impact, because of factors such as lesion site or size. Non-urgent referral: Consider routine referral for patients with: • A skin lesion that raises the suspicion of a basal cell carcinoma. Consider urgent referral (appointment within 2 weeks) for melanoma in patients with a pigmented or non-pigmented skin lesion that suggests nodular melanoma. Accompanying notes: The 7-point weighted checklist: Major features (scoring 2 points each) • Change in size • Irregular shape • Irregular colour Minor features (scoring 1 point each) • • • • Largest diameter of 7mm or more Inflammation Oozing Change in sensation Accompanying notes: Squamous cell carcinomas are usually raised lesions, a number of typical features have been described: often ulcerated keratinised or crusting lesions and growing typically on the head and neck or back of hand. They occur commonly and are higher risk in anyone who is immunocompromised or had a previous organ transplant. Refer all new skin lesions in this group urgently. Accompanying notes: Features suggestive of a basal cell carcinoma include: • An ulcer with raised, rolled edge, • Prominent fine blood vessels around the lesion, • Nodules, often waxy or pearly in appearance. Suspected basal cell carcinomas should only be excised in primary care in accordance with the NICE guidance on Improving outcomes for people with skin tumours including melanoma (May 2010). Specific sites of concern are sun-exposed areas such as the scalp, face, hands and arms, particularly in fairhaired patients. Skin Pan-London approach are asking to consider risk factors 1. 2. 3. 4. 5. Photo-damaged skin Immunosuppression Transplant H/x skin cancer FHx of skin cancer What does lesion site or size refer to when determining a routine referral or a 2ww for a BCC? Pan-London: rapidly growing lesions near the eyelid, lip margin or nose refer to local 2ww service as higher risk of it being an SCC as well as needing rapid plastics involvement 16 Brain and CNS Brain and CNS cancer Very urgent referral: Consider very urgent referral (appointment within 48 hours) in: • Children and young people with newly abnormal central neurological or cerebellar function. Urgent Direct Access: Consider urgent direct access MRI brain scan (appointment within 2 weeks) in: • Adults with progressive, sub-acute loss of central neurological function. Accompanying notes: • A ‘normal’ scan A normal investigation does not preclude the need for ongoing follow up, monitoring and further investigation. Furthermore, a seemingly ‘normal’ MRI scan may provide false reassurance in patients who have neurological pathology that MRI scanning is unable to detect. • Approximately 10% of patients may be unsuitable for, or unable to tolerate an MRI brain scan, e.g. patients with pacemakers in-situ or those with severe claustrophobia. In these patients a CT scan may be more appropriate, taking potential radiation exposure in to consideration. • Incidental findings A small percentage of MRI scans may yield abnormalities in otherwise healthy individuals. This may impact on these patients in a number of ways including further investigation and the potential impact on health insurance premiums. As incidental findings are not an infrequent result of MRI scanning, patients should have prior counselling and information to make them aware of the potential for such findings as a consequence of their investigation. • No definition of ‘progressive sub-acute loss of central neurological function’ has been provided for this update, but the 2005 NICE guidance for suspected cancer includes signs or symptoms that may cause concern, including: progressive neurological deficit, new-onset seizures, headaches, mental changes, cranial nerve palsy. • Headaches of recent onset accompanied by features suggestive of raised intracranial pressure, e.g. vomiting, drowsiness, posture-related headache, pulse-synchronous tinnitus, or other focal or non-focal neurological symptoms, such as blackout or change in personality or memory. • Consider urgent referral in patients with rapid progression of: sub-acute focal neurological deficit; unexplained cognitive impairment, behavioural disturbance or slowness, or a combination of these; personality changes confirmed by a witness and for which there is no reasonable explanation even in the absence of the other symptoms or signs of a brain tumour. Brain Skin and CNS Consider urgent (within 2 weeks) direct access MRI scan of the brain (or CT scan if MRI is contraindicated) in adults with • • • • • progressive, sub-acute loss of central neurological function new onset seizure history of a malignancy with symptoms personality change blackout • New onset headache with sinister features such as • Vomiting • Pulse-synchronous tinnitus • Worse on supine position • Awakens sleep • Behavioural slowness • Cognitive decline 18 Head and neck Laryngeal cancer Urgent referral: Consider urgent referral (appointment within two weeks) in patients: • Aged 45 and over with either: - Persistent unexplained hoarseness OR A dentist should consider urgent referral (appointment within two weeks) for patients with either of the following, which have been assessed by a dental surgeon and concluded to be consistent with oral cancer: • A lump on the lip or the oral cavity OR - An unexplained lump in the neck. Oral cancer Urgent referral: Consider urgent referral (appointment within two weeks) for patients with: • An unexplained ulceration in the oral cavity lasting for more than 3 weeks OR • A persistent and unexplained lump in the neck Consider urgent referral (appointment within two weeks) for assessment by a dentist in patients with either: • An unexplained lump on the lip or in the oral cavity OR • A red or red and white patch in the oral cavity consistent with erythroplakia or erythroleukoplakia. • A red or red and white patch in the oral cavity consistent with erythroplakia or erythroleukoplakia. Thyroid cancer Urgent referral: Consider urgent referral (appointment within two weeks) in patients with: • An unexplained thyroid lump. Head and neck • Pan-London age thresholds lowered to 40+ • Unexplained lump in the neck requires a concurrent chest x-ray to exclude lung cancer or lymphoma • Unexplained = solitary thyroid lump (not bulky or all thyroid lumps!) or with suspicious clinical features • Document risk factors • Alcohol • Tobacco • HPV • HIV/immuosuppresion • Area for dentists to refer • Unexplained tooth mobility without periodontal disease • Poor healing after dental extraction > 3/52 • • Pharyngeal cancers (23%) were omitted from the new guidance Retention of old criteria from CG27, 2005 and WHO oral cancer guidelines • • • Persistent sore throat Throat pain Hoarseness (concurrent CXR) 20 Mr A 61 year old male Office manager Never smoked You receive a OOH attendance note from local UCC New onset dysuria and one episode of haematuria – immediate attended UCC • Urinalysis abnormal: leuk, nits, prot and blood +++ • Urine CTG sent – normal • Urine culture sent - shows E.coli infection • Patient was treated for a UTI at the time and asked to review results with his GP 3 weeks later dysuria recurs but no visible haematuria • Urinalysis indicates blood but no infection parameters • Settles again after a second course of antibiotics What next….. Mr A What would you do next… • Abdomen ultrasound scan • KUB AXR • DRE, Full blood count and PSA • Glucose, HbA1c, bone profile • Routine referral to Urology • GUM clinic • Safety net and repeat urinalysis again even in the absence of symptoms NICE Recommends… What would you do next… • Abdomen ultrasound scan • KUB AXR • DRE, Full blood count and PSA • Glucose, HbA1c, bone profile • Routine referral to Urology • GUM clinic • Safety net and repeat urinalysis again even in the absence of symptoms NICE recommends 2ww BLADDER • Age 60+ • Unexplained non-visible haematuria with either • Dysuria • Raised WCC BLADDER/RENAL • Age 45+ • Unexplained visible haematuria without UTI • Persisting visible haematuria after successful Rx for UTI NICE recommends 2ww PROSTATE • SINGLE PSA above age-thresholds (BAUS) AUDIT across London to discuss whether TWO PSAs may be a referral criteria but at present aligning with NICE, NG12 Urological Prostate cancer Bladder cancer Urgent referral: Urgently refer men (appointment within two weeks) if either: • Their prostate feels malignant on digital rectal examination (DRE) OR • Their prostate specific antigen (PSA) levels are above the age-specific reference range. Urgent referral: Urgently refer patients (appointment within two weeks) if they are: • Aged 45 and over with either: – Unexplained visible haematuria without OR urinary tract infection Non-urgent investigation: Consider a PSA test AND DRE in men with any of the following: • Any lower urinary tract symptoms, such as nocturia, urinary frequency, hesitancy, urgency or retention • Erectile dysfunction • Visible haematuria. – Visible haematuria that persists or recurs after successful treatment of urinary tract infection. • Aged 60 and over with unexplained non-visible haematuria and either: – Dysuria OR – A raised white cell count on a blood test. • • • • Consider alternative contributing factors that may influence an individual’s PSA ranges. Urgent referral: Consider urgent referral (appointment within two weeks) in men with any of the following changes in the testis: • Non-painful enlargement • Change in shape • Change in texture. Direct access ultrasound: Consider a direct access ultrasound scan in men with unexplained or persistent testicular symptoms. Penile cancer Non-urgent referral: Consider referral in patients aged 60 and over with recurrent or persistent urinary tract infection that is unexplained. Renal cancer Accompanying notes: Prostate-specific antigen ranges: 40–49 years 0–2.5ng/L 50–59 years 0–3.5ng/L 60–69 years 0–4.5nh/L 70–79 years 0–6.5ng/L Testicular cancer Urgent referral: Urgently refer patients (appointment within two weeks) if they are: • Aged 45 years and over with either: – – Unexplained visible haematuria without urinary tract infection Visible haematuria that persists or recurs after successful treatment of urinary tract infection. Urgent referral: Consider urgent referral (appointment within two weeks) in men with any of the following, after exclusion of sexually transmitted infection as a cause or after treatment for a sexually transmitted infection has been completed: • A penile mass • An ulcerated lesion • Unexplained OR persistent symptoms affecting the foreskin or glans. Mr F 53 years old Ex – smoker on the record H/O pneumonia six months ago – had a post Rx CXR – normal Wife asked him to get 3 week cough checked out as keeping her up at night Not in fact an ex-smoker! Smokes hash in a pipe No haemoptysis fevers or weight loss Chest clear What do you do next….. 27 Mr F What would you do next….. • Chest x-ray • FBC • Spirometry • 2ww • Safety net and f/up in 3 weeks • Reassure • Smoking cessation advice 28 NICE recommends… What would you do next….. • Chest x-ray • FBC • Spirometry • 2ww • Safety net and f/up in 3 weeks • Reassure • Smoking cessation advice 29 NICE recommends…. Chest x-ray is normal FBC shows elevated platelets 2ww referral In symptomatic patients, the majority of chest X-rays will be abnormal, but a normal chest X-ray does not exclude diagnosis of lung cancer. This was shown in the 2006 BJGP study of normal and abnormal chest x-rays in lung cancer patients, 23% of lung cancer patients had a negative X-ray. Pan-London – retaining shoulder and chest pain as criteria 30 Lung Lung and pleural cancers Urgent referral: Urgently refer for lung cancer or mesothelioma (appointment within two weeks) in patients with: • Chest X-ray findings that suggest lung cancer or mesothelioma OR • Patients aged 40 and over with unexplained haemoptysis. Urgent investigations: Consider an urgent chest X-ray (to be performed within two weeks) for lung cancer or mesothelioma in patients aged 40 and over with any of the following: • Persistent or recurrent chest infection • Finger clubbing • Supraclavicular lymphadenopathy OR persistent cervical lymphadenopathy • Chest signs consistent with lung cancer or pleural disease • Thrombocytosis. Urgent investigation: Offer an urgent chest X-ray (to be performed within two weeks) to assess for lung cancer or mesothelioma in people: • Aged 40 and over if they have never smoked with 2 or more of the following unexplained OR signs or symptoms • Aged 40 and over and have previously smoked with 1 or more of the following unexplained signs or symptoms OR • Any age if they have ever been exposed to asbestos and have 1 or more of the following: – – – – – – Cough Fatigue Shortness of breath Chest pain Weight loss Appetite loss. Accompanying notes: In symptomatic patients, the majority of chest X-rays will be abnormal, but a normal chest X-ray does not exclude diagnosis of lung cancer. This was shown in the 2006 BJGP study of normal and abnormal chest x-rays in lung cancer patients, 23% of lung cancer patients had a negative X-ray. Lung Refer people using a suspected cancer pathway referral (for an appointment within 2 weeks) for lung cancer if they: • have chest X-ray findings that suggest lung cancer or • are aged 40 and over with unexplained haemoptysis. Offer a chest X-ray to assess for lung cancer in people aged 40 and over if they have 2 or more of the following unexplained symptoms, or if they have ever smoked and have 1 or more of the following unexplained symptoms: • cough • fatigue • shortness of breath • chest pain • weight loss • appetite loss. Consider an urgent chest X-ray (to be performed within 2 weeks) to assess for lung cancer in people aged 40 and over with any of the following: • persistent or recurrent chest infection • finger clubbing • supraclavicular lymphadenopathy or persistent cervical lymphadenopathy • chest signs consistent with lung cancer • thrombocytosis. 32 Lung Mesothelioma Refer people using a suspected cancer pathway referral (for an appointment within 2 weeks) for mesothelioma if they have chest X-ray findings that suggest mesothelioma. Offer a chest X-ray to assess for mesothelioma in people aged 40 and over, if: • they have 2 or more of the following unexplained symptoms, or • they have 1 or more of the following unexplained symptoms and have ever smoked, or • they have 1 or more of the following unexplained symptoms and have been exposed to asbestos: • cough • fatigue • shortness of breath • chest pain • weight loss • appetite loss. Consider an urgent chest X-ray (to be performed within 2 weeks) to assess for mesothelioma in people aged 40 and over with either: • finger clubbing or • chest signs compatible with pleural disease. 33 • 61 years old • Ex – smoker • New type 2 diabetes mellitus diagnosis on NHS health check • BMI 30 and no FHx • Lost a few kg in the past year • Vague upper abdominal pain and occasional heartburn • What do you do next….. 34 What do you do next…. • Abdomen US • Abdomen CT • Ca19/9 • FBC • Ferritin/ TIBC • Bone profile • ESR • Renal function • Liver function • Helicobacter pylori antigen test • Upper GI Endoscopy 35 What do you do next…. • Abdomen US • Abdomen CT • Ca19/9 • FBC (Hb and platelets) • Ferritin/ TIBC • Bone profile • ESR • Renal function • Liver function • Helicobacter pylori antigen test • URGENT Upper GI Endoscopy • ROUTINE Upper GI Endoscopy 36 Upper gastrointestinal • Raised platelet count with any of the following: Oesophageal and gastric cancer O - Oesophageal – – – – – – G - Gastric Urgent referral for endoscopy within two weeks: Urgently refer patients presenting with: • Dysphagia (at any age) (OG) OR • Aged 55 and over with weight loss AND Upper abdominal pain OR Dyspepsia (OG). Nausea Vomiting Reflux Weight loss Dyspepsia Upper abdominal pain (OG) OR • Nausea or vomiting with any of the following: – – – – Weight loss Reflux Dyspepsia Upper abdominal pain (OG). Pancreatic cancer Gall bladder Urgent direct access Consider an urgent direct access ultrasound scan (within two weeks) to assess for gall bladder cancer in people with an upper abdominal mass consistent with an enlarged gall bladder. Liver cancer Urgent direct access Consider an urgent direct access ultrasound scan (within two weeks) to assess for liver cancer in people with an upper abdominal mass consistent with an enlarged liver. OR Reflux Consider urgent referral (appointment within two weeks) for patients with an upper abdominal mass consistent with stomach cancer (G). Non-urgent direct access endoscopy: Consider non-urgent direct access endoscopy for patients presenting with: • Haematemesis (at any age) (OG) OR • Aged 55 and over with: – Treatment resistant dyspepsia (OG) OR – Upper abdominal pain and low haemoglobin (OG) Urgent referral: Urgently refer patients (appointment within two weeks) if aged 40 and over with jaundice. Urgent direct access CT scan or an urgent ultrasound scan if CT scan is not available: Consider urgent direct access CT scan (within two weeks) or ultrasound scan if CT scan is not available for patients: • Aged 60 and over, displaying weight loss AND any of the following: – – – – – – Diarrhoea Back pain Abdominal pain Nausea/vomiting Constipation New-onset diabetes. Accompanying notes: Consider that 10% of pancreatic cancers are missed by abdomen ultrasounds, whilst tumours smaller than 3cm will not be visible using an ultrasound. CT scans have the advantage of staging at the same time. Upper GI Oesophageal cancer Offer urgent direct access upper gastrointestinal endoscopy (to be performed within 2 weeks) to assess for oesophageal cancer in people: • with dysphagia or aged 55 and over with weight loss and any of the following: • upper abdominal pain • reflux • dyspepsia. Consider non-urgent direct access upper gastrointestinal endoscopy to assess for oesophageal cancer in people with haematemesis. Consider non-urgent direct access upper gastrointestinal endoscopy to assess for oesophageal cancer in people aged 55 or over with: • treatment-resistant dyspepsia or upper abdominal pain with low haemoglobin levels or raised platelet count with any of the following: • nausea • vomiting • weight loss • reflux • dyspepsia • upper abdominal pain, or • nausea or vomiting with any of the following: • weight loss • reflux • dyspepsia • upper abdominal pain. 38 Upper GI Stomach cancer Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for people with an upper abdominal mass consistent with stomach cancer. Offer urgent direct access upper gastrointestinal endoscopy (to be performed within 2 weeks) to assess for stomach cancer in people: • with dysphagia or aged 55 and over with weight loss and any of the following: • upper abdominal pain • reflux • dyspepsia. Consider non-urgent direct access upper gastrointestinal endoscopy to assess for stomach cancer in people with haematemesis. Consider non-urgent direct access upper gastrointestinal endoscopy to assess for stomach cancer in people aged 55 or over with: • treatment-resistant dyspepsia or upper abdominal pain with low haemoglobin levels or raised platelet count with any of the following: • nausea • vomiting • weight loss • reflux • dyspepsia • upper abdominal pain, or • nausea or vomiting with any of the following: • weight loss • reflux • dyspepsia • upper abdominal pain. 39 Upper GI Gall bladder cancer Consider an urgent direct access ultrasound scan (to be performed within 2 weeks) to assess for gall bladder cancer in people with an upper abdominal mass consistent with an enlarged gall bladder. Liver cancer Consider an urgent direct access ultrasound scan (to be performed within 2 weeks) to assess for liver cancer in people with an upper abdominal mass consistent with an enlarged liver. Pancreatic cancer Refer for same day assessment for pancreatic cancer if they are aged 40 and over and have jaundice. Consider an urgent direct access CT scan (to be performed within 2 weeks), or an urgent ultrasound scan if CT is not available, to assess for pancreatic cancer in people aged 60 and over with weight loss and any of the following: • diarrhoea • back pain • abdominal pain • nausea • vomiting • constipation • new-onset diabetes. 10% of pancreatic cancers are missed by abdomen ultrasounds, whilst tumours smaller than 3cm will not be visible using an ultrasound. CT scans have the advantage of staging at the same time New onset diabetes can appear two years before an US detected pancreatic tumour is possible CT is the gold standard! 40 Bone and sarcoma Bone sarcoma Soft tissue sarcoma Very urgent direct access: Consider a very urgent direct access X-ray (appointment within 48 hours) in any child or young person with unexplained: • Bone swelling OR • Bone pain. Very Urgent referral: Very urgent direct access: Consider very urgent direct access ultrasound scan (performed within 48 hours) for children and young people with: • An unexplained lump that is increasing in size. Urgent direct access: Consider very urgent referral in children and young people (appointment within 48 hours) with: • An X-ray that suggests the possibility of bone sarcoma. Urgent referral: Consider urgent referral (appointment within two weeks) in adults with: • An X-ray that suggests the possibility of bone sarcoma. Consider urgent direct access ultrasound scan (performed within two weeks) in adults with: • An unexplained lump that is increasing in size. Very urgent referral: Consider very urgent referral (within 48 hours) in children or young people with: • Ultrasound scan findings that are suggestive of soft-tissue sarcoma OR • Ultrasound scan findings that are uncertain and clinical concern persists. Urgent referral: Consider urgent referral (within two weeks) in adults with: • Ultrasound scan findings that are suggestive of soft-tissue sarcoma OR • Ultrasound scan findings that are uncertain and clinical concern persists. Sarcoma Bone sarcoma in adults Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for adults if an X-ray suggests the possibility of bone sarcoma. Bone sarcoma in children and young people Consider same day specialist assessment for children and young people if an X-ray suggests the possibility of bone sarcoma. Consider a very urgent direct access X-ray (to be performed within 48 hours) to assess for bone sarcoma in children and young people with unexplained bone swelling or pain. BONE PAIN includes night pain, pain not responding to simple analgesia, bony swelling and tenderness. Plain radiographs may be ‘normal’ in patients with early bone sarcoma and if there is bone pain and night pain not responding to simple analgesia consider urgent MRI scan or referral to a sarcoma centre 42 Sarcoma Soft tissue sarcoma in adults Consider a 2ww to a sarcoma centre to assess an unexplained lump that 4.3cm or larger (golf ball) DO NOT ARRANGE AN URGENT ULTRASOUND AS MRI IS THE GOLD STANDARD REFER TO SARCOMA CENTRE! Soft tissue sarcoma in children and young people Consider same day assessment for soft tissue sarcoma in children and young people with an unexplained lump that is increasing in size. Consider a same day assessment for children and young people if they have symptoms or imaging results suggestive of soft tissue sarcoma or if findings are uncertain and clinical concern persists. 43 Breast Breast cancer Urgent referral: Urgently refer patients (appointment within two weeks) if they are male or female: • Aged 30 and over with an unexplained breast lump (with or without pain) OR • Aged 50 and over with any unilateral nipple changes of concern including discharge or retraction. Consider urgent referral (appointment within two weeks) if: • There are skin changes suggestive of breast cancer OR • They are aged 30 and over with an unexplained lump in the axilla. Non-urgent referral: Consider non-urgent referral in patients under the age of 30 with an unexplained breast lump (with or without pain). Ms A 47 year-old Afro-Caribbean lady Known type 2 diabetes – diet controlled New onset unexplained vaginal discharge Not sexually active for 6 months Smears up to date Regular periods No IMB What next…. 45 NICE recommends… What would you do next…. • • • • • • • • Pelvic and abdomen exam Swabs/sexual health screen Cervical smear FBC Urgent US pelvis Non-urgent US pelvis Ca125 2ww 46 NICE recommends… What would you do next…. Pelvic and abdomen exam Swabs/sexual health screen Cervical smear FBC Urgent US pelvis Non-urgent US pelvis Ca125 2ww NICE Recommends…. 1. Full blood count Elevate platelets/Low Hb DIRECT ACCESS PELVIC US TO EXCLUDE ENDOMETRIAL CANCER 47 Gynaecology – Pan London Endometrial cancer • Refer women using a suspected cancer pathway referral (for an appointment within 2 weeks) for endometrial cancer if they are aged 45 and over with post-menopausal bleeding (unexplained vaginal bleeding more than 12 months after menstruation has stopped because of the menopause). • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for endometrial cancer in women aged under 55 with post-menopausal bleeding. • Consider a direct access ultrasound scan to assess for endometrial cancer in women aged 45 and over with: • unexplained symptoms of vaginal discharge who: • are presenting with these symptoms for the first time or have thrombocytosis or report haematuria, or visible haematuria • low haemoglobin levels or thrombocytosis or high blood glucose levels (diabetes) Cervical cancer • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for women if, on examination, the appearance of their cervix is consistent with cervical cancer. Vulval cancer • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for vulval cancer in women with an unexplained vulval lump, ulceration or bleeding. Vaginal cancer • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for vaginal cancer in women with an unexplained palpable mass in or at the entrance to the vagina. 48 Gynaecology – Pan London Ovarian cancer Refer the woman urgently if physical examination identifies ascites and/or a pelvic or abdominal mass (which is not obviously uterine fibroids) • Carry out tests in primary care if a woman (especially if 45 or over) reports having any of the following symptoms on a persistent or frequent basis – particularly more than 12 times per month: • persistent abdominal distension (women often refer to this as 'bloating') • feeling full (early satiety) and/or loss of appetite • pelvic or abdominal pain • increased urinary urgency and/or frequency. Consider carrying out tests in primary care if a woman reports unexplained weight loss, fatigue or changes in bowel habit. Advise any woman who is not suspected of having ovarian cancer to return to her GP if her symptoms become more frequent and/or persistent. Carry out appropriate tests for ovarian cancer in any woman of 45 or over who has experienced symptoms within the last 12 months that suggest irritable bowel syndrome (IBS), because IBS rarely presents for the first time in women of this age. • Measure serum CA125 in primary care and ultrasound scan of the abdomen and pelvis. • If the ultrasound suggests ovarian cancer, refer the woman urgently for further investigation. • For any woman who has 35 IU/ml or greater but a normal ultrasound refer 2ww 49 Gynaecological Endometrial Cancer Ovarian cancer Urgent referral: Urgently refer (appointment within two weeks) if physical examination identifies any of the following: • Ascites • Pelvic or abdominal mass (which is not obviously uterine fibroids). Urgent Investigation: Arrange CA125 and/or ultrasound tests in women (especially if 50 or over) with any of the following on a persistent or frequent basisparticularly more than 12 times per month: • • • • • Persistent abdominal distension (bloating) Early satiety and/or loss of appetite Pelvic or abdominal pain Increased urinary urgency and/or frequency New onset symptoms suggestive of IBS (as IBS rarely presents for the first time in women of this age). Consider CA125 and/or ultrasound tests if a woman reports any of the following: Urgent referral: Urgently refer women (appointment within two weeks) if they are: • Aged 55 and over with: – Post-menopausal bleeding (unexplained vaginal bleeding more than 12 months after menstruation has stopped due to the menopause). Consider urgent referral (appointment within two weeks) if they are: • Aged under 55 with: – Post-menopausal bleeding. Direct Access Ultrasound: Consider direct access ultrasound in women: • Aged 55 and over presenting with unexplained symptoms of vaginal discharge who: – Are presenting with these symptoms for the first time Report haematuria. OR Have thrombocytosis Consider direct access ultrasound in women: • Unexplained weight loss • Fatigue • Changes in bowel habit (though colorectal cancer is a more common malignant cause). • Aged 55 and over presenting with visible haematuria and any of the following: – – – Low haemoglobin Thrombocytosis High blood glucose level. Cervical cancer Urgent referral: Consider urgent referral (appointment within two weeks) if: • The appearance of the woman’s cervix is consistent with cervical cancer. Accompanying notes: A smear test is not required before referral, and a previous negative result should not delay referral. Vulval cancer Urgent referral: Consider urgently referring (appointment within two weeks) women with any of the following unexplained vulval signs or symptoms: • A vulval lump • Ulceration • Bleeding. Vaginal cancer Urgent referral: Consider urgent referral (appointment within two weeks) in women with an unexplained palpable mass in or at the entrance to the vagina. NG12: Colorectal Symptom Profile in primary care • • • • • • • • • • • • • • • Rectal bleeding PLUS diarrhoea for 6 weeks (>40) Rectal bleeding for 6 weeks (>60) CIBH for 6 weeks (>60) Mass (any age) Iron deficiency anaemia (Male Hb<11g/dl; female Hb<10g/dl) Loss of weight and abdominal pain (>40) Rectal bleeding (>50) Iron-deficiency anaemia (>60) CIBH (>60) Rectal bleeding, plus a second symptom (<50) Unexplained abdo pain or weight loss (<50) CIBH (<60) Iron-deficiency anaemia (<60) Non-iron deficiency anaemia (>60) Other symptoms Under 2005 Guidance Refer Under 2015 guidance Refer Approximate risk of cancer 5% or more 3-5% Refer Test for occult blood 1-3% Safety net 51 Lower gastrointestinal Colorectal cancer Urgent referral: Urgently refer (appointment within two weeks) for colorectal cancer in patients: • Aged 40 and over with: – Unexplained weight loss AND abdominal pain • Aged 50 and over with: – Unexplained rectal bleeding • Aged 60 and over with either: – Iron deficiency anaemia OR – Alteration in bowel habit • An unexplained positive Faecal Occult Blood Test (FOBT). Consider urgent referral (appointment within 2 weeks) for colorectal cancer in patients: • Any age with: – A rectal or abdominal mass • Aged under 50 with rectal bleeding AND any of the following unexplained signs or symptoms: – – – – Abdominal pain Altered bowel habit Weight loss Iron deficiency anaemia. Faecal Occult Blood Testing In the absence of rectal bleeding, offer FOBT to patients: • Aged 50 or over with unexplained: – Abdominal pain OR Weight loss – • Aged under 60 with either: – Changes in bowel habit OR Iron-deficiency anaemia – • Aged 60 and over with: – Anaemia even in the absence of iron deficiency. Anal cancer Urgent referral: Consider urgent referral (appointment within two weeks) in patients with either: • An unexplained anal mass OR • Unexplained anal ulceration. Colorectal – pan London LONDON IS NOT SUPPORTING USE OF FOBT! RECTAL BLEEDING • Aged 50 years or over with rectal bleeding • Aged Less than 50 years but MUST have one or more of the following Abdominal pain Change in bowel habit Weight loss Iron deficiency anaemia CHANGE IN BOWEL HABIT - aged 60 or over IRON DEFICIENCY ANAEMIA - aged 60 or over ABDOMINAL PAIN AND WEIGHT LOSS – aged 40 or over Abnormal physical examination • Abdominal mass thought to be large bowel cancer (any age) • Palpable rectal mass (any age) • Anal mass (unexplained and any age) • Anal ulceration (unexplained and any age) Anal cancer • Consider a suspected cancer pathway referral (for an appointment within 2 weeks) for anal cancer in people with an unexplained anal mass or unexplained anal ulceration. 53 Children and TYA Symptoms of concern in children and young people Take into account the insight and knowledge of parents and carers when considering making a referral for suspected cancer in a child or young person. Consider referral for children if their parent or carer has persistent concern or anxiety about the child's symptoms, even if the symptoms are most likely to have a benign cause. Leukaemia in children and young people Refer children and young people for immediate specialist assessment for leukaemia if they have unexplained petechiae or hepatosplenomegaly. [new 2015] Offer a very urgent full blood count (within 48 hours) to assess for leukaemia in children and young people with any of the following: • pallor • persistent fatigue • unexplained fever • unexplained persistent infection • generalised lymphadenopathy • persistent or unexplained bone pain • unexplained bruising • unexplained bleeding Hodgkin's lymphoma in children and young people Consider a very urgent referral (for an appointment within 48 hours) for specialist assessment for Hodgkin's lymphoma in children and young people presenting with unexplained lymphadenopathy. When considering referral, take into account any associated symptoms, particularly fever, night sweats, shortness of breath, pruritus or weight loss. Brain tumour/cancers Consider a very urgent referral (for an appointment within 48 hours) for suspected brain or central nervous system cancer in children and young people with newly abnormal cerebellar or other central neurological function. 54 Children and TYA Soft tissue sarcoma Consider a very urgent direct access ultrasound scan (to be performed within 48 hours) to assess for soft tissue sarcoma in children and young people with an unexplained lump that is increasing in size. Consider a very urgent referral (for an appointment within 48 hours) for children and young people if they have ultrasound scan findings that are suggestive of soft tissue sarcoma or if ultrasound findings are uncertain and clinical concern persists. Bone sarcoma Consider a very urgent referral (for an appointment within 48 hours) for specialist assessment for children and young people if an X-ray suggests the possibility of bone sarcoma. Consider a very urgent direct access X-ray (to be performed within 48 hours) to assess for bone sarcoma in children and young people with unexplained bone swelling or pain. Neuroblastoma Consider very urgent referral (for an appointment within 48 hours) for specialist assessment for neuroblastoma in children with a palpable abdominal mass or unexplained enlarged abdominal organ. Retinoblastoma Consider urgent referral (for an appointment within 2 weeks) for ophthalmological assessment for retinoblastoma in children with an absent red reflex. Wilms' tumour Consider very urgent referral (for an appointment within 48 hours) for specialist assessment for Wilms' tumour in children with any of the following: • a palpable abdominal mass • an unexplained enlarged abdominal organ • unexplained visible haematuria 55 Children and TYA Suspected cancer (part 1—children and young adults): visual overview of updated NICE guidance Hamilton et al, BMJ 2015; 350:h3036 56 You know more than most that cancer doesn’t just affect the people you support physically. It can affect everything – their relationships, finances and careers. We want to work with you to help you provide the best support possible for people affected by cancer and their families. So as well as offering resources to support you in your role, we can provide information to the people you support, so they know they’ll never have to face cancer alone. Together, we can help make sure people affected by cancer get the support they need to feel more in control – from the moment they’re diagnosed, through treatment and beyond. Our cancer support specialists, benefits advisers and cancer nurses are available to answer any questions your patients might have through our free Macmillan Support Line on 0808 808 00 00 (Monday to Friday, 9am – 8pm). To find out more about our work and services, visit macmillan.org.uk/professionals Macmillan Cancer Support, registered charity in England and Wales (261017), Scotland (SC039907) and the Isle of Man (604). MAC15454_DESKTOP PATIENT INFORMATIN LEAFLET http://londoncancer.org/media/48492/2wkreferral-patient-leaflet.pdf http://londoncancer.org/media/124336/patientinformation-for-urgent-referrals.pdf Final case…. 69 year old lady Acute swelling left calf consistent with a DVT NO triggers DVT Ax – Doppler confirms – Haematology initiates NOAC What next….. 58 Final case…. What next…… could be a sign of an underlying malignancy 1. 2. 3. 4. Urogenital Breast Colorectal Lung cancer Carry out an assessment for additional symptoms, signs or findings that may help to clarify which cancer is most likely and offer urgent investigation or a suspected cancer pathway referral (for an appointment within 2 weeks). 59 Cancer of unknown primary Some symptoms or symptom combinations may be features of several different cancers. For some of these symptoms, the risk for each individual cancer may be low but the total risk of cancer of any type may be higher. This section includes recommendations for these symptoms. Symptoms of concern in adults For people with unexplained weight loss, which is a symptom of several cancers including colorectal, gastro-oesophageal, lung, prostate, pancreatic and urological cancer: • Carry out an assessment for additional symptoms, signs or findings that may help to clarify which cancer is most likely and offer urgent investigation or a suspected cancer pathway referral (for an appointment within 2 weeks). For people with unexplained appetite loss, which is a symptom of several cancers including lung, oesophageal, stomach, colorectal, pancreatic, bladder and renal cancer: • Carry out an assessment for additional symptoms, signs or findings that may help to clarify which cancer is most likely and offer urgent investigation or a suspected cancer pathway referral (for an appointment within 2 weeks). For people with deep vein thrombosis, which is associated with several cancers including urogenital, breast, colorectal and lung cancer: • Carry out an assessment for additional symptoms, signs or findings that may help to clarify which cancer is most likely and consider urgent investigation or a suspected cancer pathway referral (for an appointment within 2 weeks). 60 Cancer of unknown primary • Unexplained weight loss colorectal, gastro-oesophageal, lung, prostate, pancreatic and urological cancer • Unexplained appetite loss lung, oesophageal, stomach, colorectal, pancreatic, bladder and renal cancer • Deep vein thrombosis urogenital, breast, colorectal and lung cancer Carry out an assessment for additional symptoms, signs or findings that may help to clarify which cancer is most likely and offer urgent investigation or a suspected cancer pathway referral (for an appointment within 2 weeks). 61 Non-specific features of cancer Suspected cancer (part 2—adults): visual overview of updated NICE guidance Hamilton et al, BMJ 2015; 350:h3044 62 Primary care investigations and results Suspected cancer (part 2—adults): visual overview of updated NICE guidance Hamilton et al, BMJ 2015; 350:h3044 63 Symptoms based infogram Assessing and referring adult cancers. Image from Suspect cancer (part 2- adults) BMJ 2015;350:h3044 Guidance Patient Support, Safety Netting and Diagnostic Access Guidance The following guidance is taken from pages 114–117 of the NICE 2015 guidance for suspected cancer referral, it includes recommendations on patient support, safety netting and the diagnostic process: • Explain to people who are being referred with suspected cancer that they are being referred to a cancer service. Reassure them, as appropriate, that most people referred will not have a diagnosis of cancer, and discuss alternative diagnoses with them. • When referring a person with suspected cancer to a specialist service, assess their need for continuing support while waiting for their referral appointment. If the person does have additional support needs because of their personal circumstances, inform the specialist (with the person’s agreement). • Advise those patients who may not meet immediate referral criteria to re-consult their GP if symptoms persist or progress. • If direct access for some tests is unavailable in your area, seek an alternative urgent referral pathway. • You will note that some symptoms from the 2005 NICE guidance for suspected cancer referral have been removed from the guidance update, although there may be no explicit recommendations, refer appropriately if clinical concern persists. • Give the person information on the possible diagnosis (both benign and malignant) in accordance with their wishes for information (see also the NICE guideline on patient experiences in adult NHS services). Macmillan has more than 500 free booklets available at be.macmillan.org.uk, covering different types of cancer, treatments and side effects. They also offer information and guidance on the day-to- day issues of living with cancer. • The information given to people with suspected cancer and their families and/or carers should cover, among other issues: – – How to obtain further information about the type of cancer suspected or help before the specialist appointment What type of tests may be carried out, and what will happen during diagnostic procedures. • Provide information that is culturally and linguistically appropriate as well as taking in to account the patient’s level of ability. Macmillan’s most commonly requested cancer information is available online to download in a selection of different languages. Macmillan’s Online Community is a network of people affected by cancer which anyone can join to get support from others going through a similar experience. Resources 1. National Institute for Health and Care Excellence. Suspected cancer: recognition and referral, 2015. www.nice.org.uk/guidance/NG12 http://www.nice.org.uk/guidance/ng12/evidence/full-guidance-65700685 2. NICE Suspected cancer: recognition and referral tumour site recommendations http://www.nice.org.uk/guidance/NG12/chapter/1-recommendations 3. BMJ Suspected cancer (part 1—children and young adults): visual overview of updated NICE guidance http://www.bmj.com/content/350/bmj.h3036 4. BMJ Suspected cancer (part 2—adults): reference tables from updated NICE guidance http://www.bmj.com/content/350/bmj.h3044 5. Macmillan Rapid Referral Guidelines http://www.macmillan.org.uk/Documents/AboutUs/Health_professionals/PCCL/Rapidreferralguidelin es.pdf 66 Transforming Cancer Services Team for London SECSU.tcstlondon@nhs.net Dr Ishani Patel ishanipatel@nhs.net Ishani.patel@btinternet.com 67