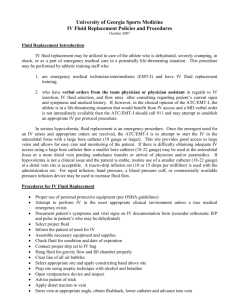
File
advertisement

PARAMEDIC PHARMACOLOGY: INTRAVENOUS FLUIDS & DRUG CALCULATIONS Amy Gutman MD EMS Medical Director prehospitalmd@gmail.com OVERVIEW Review of fluids & electrolytes Techniques of intravenous & intraosseous infusions Mathematical principles used in pharmacology & to calculate medication doses Medication administration routes DISCLAIMERS #1 I am a woman I am bad at math Do not extrapolate ALL women are bad at math #2 This is a boring lecture This is a necessary lecture Do not extrapolate ALL my lectures are boring MEDICATION ADMINISTRATION ROUTES Discussed Today Intravenous (IV) Intraosseous (IO) Other Routes Sublingual (SL) Subcutaneous (SQ) Parenteral (PO) Rectal (PR) Inhalation (IH) Endotracheal (ET) Transdermal (TD) Intramuscular (IM) Intranasal (IN) NATIONAL EMS EDUCATION STANDARD COMPETENCIES ~ PHARMACOLOGY Provider integrates pharmacology knowledge to formulate a treatment plan intended to mitigate emergencies & improve the overall health of patient Administer medications within scope of practice Understand “six rights” of medication administration Understand advantages, disadvantages & techniques for establishing venous access Review math concepts, including dose & rate calculations Describe role of medical direction MEDICAL DIRECTION Medication administration governed by local protocols & /or online medical direction Standing Orders: Off-line or indirect medical control of predefined procedures Online (Direct) Medical Control: Must contact physician prior to performing certain procedures When in doubt, contact medical control When an order is given: If unclear or inappropriate, ask physician to repeat the order Repeat back for confirmation the name, dose & route of delivery VASCULAR ACCESS In ill or injured patients, survival may depend on ability to obtain access for fluid & drug resuscitation Peripheral extremity Eternal jugular vein Intraosseous Harm can result from improper technique or insufficient pharmacology knowledge “RIGHTS” OF MED ADMINISTRATION Right patient Right drug Right dose Right route Right time Right documentation MEDICATION ADMINISTRATION Knowledge necessary prior to administration Mechanism of action Indications Contraindications Side effects Routes of administration Pediatric & adult doses Dose calculations Antidotes / reversal agents DOCUMENTATION Name of drug Dose of drug Time administered Administration route Name of person administering drug Patient’s response to drug DRUG CHECKS & LOGS At beginning of each shift, check drugs, supplies & equipment Not expired Not damaged Readily available in required quantities Paramedic responsible for documentation & security of all controlled substances State, regional & local distribution, security, exchanges & accountability policies Double lock system in each vehicle & at base storage Drug log must be kept for at least 3 years Medical director DEA number used to order narcotics UNIVERSAL PRECAUTIONS Treat all bodily fluids as infectious I don’t shake pt’s hands without gloves (especially kids) PPE, gloves & protective eyewear at all times Include full facial protection if possible splatter CDC states hand-washing most effective method to prevent the disease spread ASEPSIS Routine & thorough hand -washing Hand-sanitizer before & after every patient contact if no easy access to soap & water Keep equipment in clean conditions with disinfection between each patient & every shift Antiseptics prior to any invasive procedure Check linen, equipment & supplies prior to use for intactness, cleanliness CONTAMINATED MATERIALS CLEANING OR DISPOSAL After needle penetrates skin, it is contaminated After needle unsheathed, it is a weapon Immediately dispose of sharps in a puncture-proof sharps container Follow your agency protocol for disposal of infectious waste & cleaning of contaminated equipment BASIC PHARMACOLOGY KNOWLEDGE Specific protocol Specifics to that medication or IVF: Indications / Contraindications Therapeutic effects Side effects Appropriate dose & re-dosage Need (+/-) for medical control Allergies: Known by patient Obtain from reliable source if not from patient Check for medic-alert jewelry or tags. INTRAVENOUS FLUIDS CHOOSING APPROPRIATE IVF Based upon presenting & underlying illness or injury Even a small amount of the poorly chosen fluid may be harmful to a patient Most agencies have limited choices of each IVF class – easy to familiarize yourself with specifics of each BODY COMPARTMENTS CRYSTALLOIDS Commonly used prehospitally Normal saline, lactated ringers, dextrose & saline or water Made of water & electrolyte solutions that easily cross a semi permeable membrane Rapidly alter intravascular fluid levels Non-oxygen carrying Given as a constant rate or bolus Adult: 250cc Pediatric: 20cc/kg In trauma, consider permissive hypotension IV FLUIDS: HYPOTONIC 0.45% Normal Saline Dilutes serum by pulling water from vascular compartment into interstitial compartment Used for hyperosmolar conditions like severe dehydration Leads to hyponatremia if plasma sodium normal as has lower concentration of sodium than serum Cells swell & burst from increased osmotic pressure If rapidly infused causes cerebral edema & central pontine demyelinosis May cause sudden fluid shift from intravascular space to intracellular space leading to cardiovascular collapse Slower but deadly is third spacing ~ abnormal shift into serum if not enough protein to “hold” fluid in vascular space IV FLUIDS: HYPERTONIC 1 .8% - 10% saline, mannitol Osmolarity higher than serum as has more particles than serum Pulls fluid & electrolytes from the intracellular to intravascular (ECF) compartment Large volumes cause hypernatremia & severe dehydration Cells may collapse from increased extracellular osmotic pressure A little goes a long way to: Increase BP Reduce cerebral edema IV FLUIDS: ISOTONIC 0.9% Normal Saline Principal resuscitation fluid Contains sodium, potassium, chloride in almost same concentrations as “body water” or “plasma” Iso-osmolar compared to plasma so stays almost entirely in the extracellular space 3-1 replacement rule: 3cc isotonic solution needed to replace 1 mL of blood IV THERAPY: COLLOIDS Albumin, blood, dextran, hetastarch Contain particles which do not readily cross semi-permeable membranes Volume stays almost entirely within intravascular space for prolonged time compared to crystalloids Because of gelatinous properties cause platelet dysfunction interfering with fibrinolysis & coagulation factors (factor VIII) Can cause significant coagulopathy in large volumes OXYGEN-CARRYING SOLUTIONS Blood contains hemoglobin which carries oxygen to cells Impractical for prehospital unless specialized critical care transport Refrigeration & unique storage “Non-cross matched blood”, or “type O” expensive, rare, with potential complications Synthetic blood available, but rarely used outside trauma research institutions or the military PolyHeme, HemoPure (HBOC HemoglobinBased O2 Carrying Solutions) CHOOSING THE RIGHT SITE: ANATOMY & TECHNIQUES CHOOSING AN IV CATHETER Based on purpose of IV, patient age, location Over-the-needle catheters preferred in prehospital setting Readily secured Minimally cumbersome Allow for some patient movement Do not need to immobilize the entire limb Sized by diameter (gauge) Smaller gauge = larger diameter Choose largest-diameter catheter for chosen vein New needles retract after insertion EQUIPMENT NEEDED Gloves, PPE Tape & bio-occlusive dressing Tourniquet Alcohol, betadine, chlorhexadine Arm board Sharps container EQUIPMENT NEEDED IV solution Medical: NS Trauma: LR or NS* Medication drip: NS or D5W Administration set w/ extension tubing Macro drip (10-15 gtts/cc) for volume Micro drip (60 gtts/cc) for medications Catheter >12 yo + fluid resuscitation: 16-18g, IO <12 yo +/- fluid resuscitation: 20-24g, IO <6 yo: 20-24g, IO IV SOLUTION CONTAINERS Most packaged in clear plastic bags Labeling: Fluid type Expiration date Do not use after expiration date, appear cloudy, discolored, with visible particulate, or if packaging not intact INTRAVENOUS CANNULAS Over-The-Needle Hollow-Needle IV ADMINISTRATION SETS Macrodrip 10 gtts = 1 mL, for large amounts of fluid Microdrip 60 gtts = 1 mL, for restricted amounts of fluid Measured volume & secondary infusion sets Blood tubing Filter prevent clots from entering body BLOOD TRANSFUSIONS Blood type identified by obtaining blood type & cross-match “Blood-band” identifies blood type & blood product hung Blood must be checked against bracelet & verified by medic even if already checked by nursing Blood administered through specific tubing Assess vitals q15 mins & monitor for hemolytic reactions Tachycardia, hives, respiratory distress, CP PERIPHERAL ACCESS CHANGING INTRAVENOUS BAG OR BOTTLE Prepare new bag / bottle Occlude flow from depleted bag or bottle Remove spike from depleted & insert into new IV bag / bottle Open clamp to & titrate to appropriate flow rate FACTORS AFFECTING IV FLOW RATES Thick fluids (colloids) infuse slowly Cold fluids run slower than warm fluids Height of IV bag must overcome gravity if not a pressure bag The larger the diameter, the faster fluid can be delivered Check for constricting band, BP cuf f Evaluate for infiltration or trauma proximal to IV site GERIATRIC CONSIDERATIONS Puncturing vein may cause massive hematomas Tape may damage skin Use smaller catheters (20, 22, 24 g) Cardiovascularly sensitive to rapid fluid shifts Poor vein elasticity IV ACCESS COMPLICATIONS Pain Infection / Phlebitis Allergic reaction Catheter shear Arterial puncture Circulatory overload Air embolism Necrosis IV COMPLICATION ~ INFILTRATION Escape of fluid into surrounding tissue IV catheter passes through vein IV becomes dislodged Catheter inserted at too shallow an angle only entering fascia SSX: Edema at the catheter site Continued IV flow after proximal vein occlusion Tightness, burning, pain at IV site Treatment: Discontinue IV & reestablish in opposite extremity or more proximal location Apply direct pressure IV COMPLICATION ~ OCCLUSION Vein, catheter or tubing blockage 1 st sign is decreasing / no drip rate or blood in tubing Causes: Position of catheter within the vein BP overcoming flow Tourniquets! I nject 1-5 cc saline into IV to gently increase pressure to overcome obstruction & reestablish flow If occlusion does not dislodge, discontinue IV & re-establish in opposite extremity or proximal to current site IV COMPLICATIONS ~ HEMATOMA & ARTERIAL PUNCTURE Hematoma Accumulation of blood in tissues around IV Causes: vein perforation, improper catheter insertion or removal Stop IV, apply direct pressure Arterial puncture Bright red spurting blood Suspect if you have a great IV that does not flow, after checking for obstruction Withdraw catheter, apply direct pressure for 5 mins or bleeding stops Always check for a pulse prior to cannulation IV COMPLICATIONS ~ SYSTEMIC Anaphylaxis Sensitivity to IV fluid or medication Treat according to allergic / anaphylaxis protocol Pyrogenic reactions Pyrogens are foreign proteins capable of producing fever secondary to allergic reactions Characterized by abrupt fever with chills, backache, HA, N/V, weakness Stop infusion immediately Treat according to allergic / anaphylaxis protocol IV COMPLICATIONS ~ NECROSIS & INFECTION IV COMPLICATIONS ~ CIRCULATORY OVERLOAD Healthy adults can handle 2-3 extra liters of crystalloids Problems pts with cardiorespiratory or renal dysfunction who can’t tolerate hemodynamic stress from increased circulatory volume SSX: Dyspnea, JVD, HTN, rales, hypoxia, edema Treat by converting to saline lock, respiratory distress protocol IV THERAPY COMPLICATIONS ~ AIR EMBOLUS Flushing IV line & replacing empty IV bags limits likelihood of air embolism SSX: Respiratory distress, unequal BS, cyanosis Focal neurological symptoms Shock & cardiorespiratory arrest Treatment: LLR & Trendelenburg position 100% oxygen, treat specific symptoms according to pertinent protocol Rapid transport IV COMPLICATIONS ~ CATHETER SHEAR Part of catheter pinches against needle & slices through catheter creating a free-flowing segment SSX similar to air embolus Treatment Surgical removal of the tip LLR & Trendelenburg Do not rethread CHOOSING THE RIGHT SITE More than using a “BFN” Have a favorite site, favorite “Jelco” & favorite technique Have a back-up And a back-up to your back-up Practice, practice, practice ANTECUBITAL VEIN DORSAL “DIGITAL” VEINS EXTERNAL JUGULAR ACCESSING EXTERNAL JUGULAR VEIN INTRAOSSEOUS Technique of administering fluids, blood products & drugs into intraosseous space of tibia, humerus or sternum Long bones consist of a shaf t (diaphysis), the ends (epiphyses) & growth plate (epiphyseal plate ) IO space is spongy cancellous epiphyseal & diaphysis medullar y cavity. When in shock , peripheral veins collapse making IV access dif ficult IO space always patent to rapidly absorb fluids & drugs, similar to a central line GENERAL IO CONTRAINDICATIONS Cannot locate landmarks Fractures at / above site Amputations distal to site Previous surger y at site Infection at site Local vascular compromise Previous attempt in same site Osteogenesis imper fecta Occasionally dif ficult in combative & the obese IO INFUSION Identify landmarks & anatomy Have all equipment ready prior to starting Manufacturer-specific device & equipment IV tubing Medications SYYAMA J, ET AL. IO VS IV ACCESS WHILE WEARING PPE IN A HAZMAT SCENARIO. P E C 2 0 07 OBJECTIVE Determine time difference to obtain IO vs IV wearing HazMat PPE METHODS 22 EMT-Ps placed anterior tibial EZ-IOs & antecubital IVs Measured: time to skin access, vascular access & fluid infusion CONCLUSIONS With provider & mannequin in PPE, needle to skin time, vascular access time, & fluid infusion time all favored EZ-IO HUMERAL IO HUMERAL APPROACH Supine position, humerus adducted Palpate midshaft humerus proximally until reach humeral head At shoulder there is a protrusion (greater tubercle) which is the insertion site With opposite hand “pinch” anterior & inferior aspects of humeral head to confirm position of greater tubercle Stabilize arm, place IO at 90 degree angle to skin Humeral cortex less dense than tibia so minimal force required DISTAL TIBIA IO DISTAL TIBIAL APPROACH Landmarks are anterior distal tibia & medial malleolus (middle ankle bone protrusion) Medial insertion site, 2 finger widths proximal to medial malleolus “Big Toe = IO” PROXIMAL TIBIA IO PROXIMAL TIBIA APPROACH Tibial tuberosity is round protrusion distal to patella From tuberosity, move 1 inch medially to tibial plateau From tibial plateau, go proximally 0.5 inch towards patella This is thinnest portion of tibial bony cortex STERNAL IO STABILIZE THE IO STABILIZE THE BABY CENTRAL VENOUS ACCESS Large, deep veins that do not collapse until late shock Internal jugular, subclavian, femoral Though IO “peripheral”, it’s flow rate & placement in marrow makes it function essentially as central access CENTRAL ACCESS DEVICE Surgically implanted device permitting repeated access to central venous circulation Generally located on anterior chest near the 3 rd 4 th rib lateral to sternum Accessed with a special needle specific to the device Requires special training DIALYSIS FISTULA Dilated vein acts like an artery due to AV graft Do not access! Most common complication is bleeding Direct pressure +/proximal tourniquet MATHEMATICAL PHARMACOLOGY PRINCIPALS IV MEDICATION PACKAGING Vials Single or multi-dose Draw air into syringe, inject into vial & withdraw drug Ampules Tap neck area to drain fluid Using 4X4, snap neck of vial & withdraw drug Dispose of ampule pieces in sharps container Prefilled Syringes Remove caps & screw pieces together Dispel air & use as standard syringe Dry Powder meds Depress plunger in vial to mix with prepackaged saline Mix thoroughly until particulates completely absorbed METRICS Decimal system based on multiples of ten measuring length (meter), volume (liter), weight (gram) Prefixes indicate fraction of base being used Micro = 0.00001 Milli = 0.001 Centi = 0.01 Kilo = 1,000 Drugs packaged in dif fering units of weight & volume so conversion often required BASICS OF DOSE CALCULATION Necessary information: Desired dose (amount of drug) Drug concentration (total weight of drug contained in specific amount of volume) Volume on hand (volume of solution containing drug) PEDIATRIC DRUG DOSAGES Most pediatric drugs weight-based Length-based resuscitation tape Pediatric wheel charts EMS field guide / Smartphone app Once weight known, calculations same as for adults METRIC CONVERSIONS 1 gram (g) = 1000 milligrams (mg) 1 mg = 1000 micrograms (mcg) 1 liter (L) = 1000 milliliters (ml) If going from large to small value, move decimal point to right If going from small to large value, move decimal point to left 1 Kg = 1000 g 1Kg = 1,000,000 mg 1 Kg = 1,000,000,000 mcg POUNDS TO KILOGRAMS Kg x 2.2 = pounds (lbs) 1 Kg = 2.2 lbs 3 am: (lbs/2) – 10% = kg To convert kg to lbs: Kg x 2.2 = lbs (Kg x 2) + 10% = lbs CALCULATION EXAMPLE You want to give 5mg valium. Label states 10 mg in 2cc (10mg/2cc). How many cc’s will you give ? 5mg x 2cc = X cc 10 mg Therefore…1 cc of valium = 5mg of valium Phenergan ordered for 12.5 mg Supplied in 25 mg/ 2cc Therefore 12.5 mg / 1cc CALCULATING FLUID INFUSION RATES Adjust flow rate according to pt’s condition & per protocol You must know: Volume to be infused Period over which it is to be infused Properties of the administration Therefore, flow rate is: Volume to be infused x gtt/mL of administration set/total time of infusion in minutes = gtt/min WEIGHT-BASED CALCULATIONS Desired dose (D) x Patient’s kg Weight (W) = Volume to be Administered (X) Known dose on hand (H) CALCULATION EXAMPLE You are giving 0.5 mg/kg IVP to an 80kg patient. Drug prepackaged in 100mg/10cc To determine total dose: 0.5mg x 80kg = 40mg To determine total volume: 40 mg x 10cc = 4cc total volume 100 mg DRIP RATE CALCULATIONS Desired Dose x Volume of IV Bag x Administration Set gtt = gtt / min Amount of Drug Desired dose x Size of bag x gtt set = gtt/min Order is for 5 mg/min. You have 500cc NS, a 60 gtt/cc admin set & 2g of drug. How many gtt/min? 5mg/min x 500cc x 60gtt/ cc = 75gtt / min 2000mg SIMPLER DRIP RATE CALCULATION Volume x administration set / time (cc x gtt) / minutes You want to give a 500cc bolus using a 15 gtt set over 1 hour (500cc x 15gtt) / 60 mins = 125 gtts/min REFERENCES Caroline’s Emergency Care in the Streets 7 th Edition (Principles of Pharmacology, Medication Administration & Emergency Medications). Jones & Bar tlett. 2013 Pharmacology Drug Dosage Calculations. Shelby County EMS Training Division 2010 Linscott et al. Emergency Care. IV Access, Blood Sampling & IO Infusions. Brady 2009. Photo credits (IV inser tion, EJ cannulation) Scott Metcalf MD© SUMMARY P RE H OSP I TALMD@ G MAI L.C OM Find math formula or system that works for you Use Smartphone but remember that phones die! Back-up with paper, pen & brain IVF classes, pathophysiology & indications Dif ferent techniques, equipment & indications for vascular access “6 rights” of drug administration including basics of BLS & ALS medication utilization When in doubt contact medical control