Histology Ch 17 572-585 [4-20
advertisement
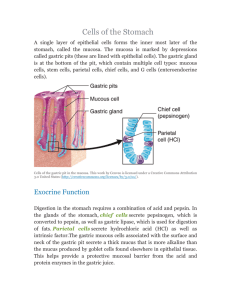
Histology Ch 17 572-585 Esophagus – fixed tube that delivers food and liquid from pharynx to stomach -attached to surrounding structures by connective tissue, but it is free in abdomen for 1-2cm -Length is ~25cm, and lumen is collapsed and has a branched appearance Mucosa – nonkeratinized stratified squamous epithelium with diffuse lymphatic tissue scattered throughout, and lymph nodules are present close to mucous glands -Muscularis mucosa is the deep layer of mucosa, composed of longitudinal smooth muscle and functions to aid in swallowing Submucosa – dense irregular connective tissue that contains large blood and lymphatic vessels, nerves, and ganglion cells (Meissner’s plexus). Glands and diffuse lymphatics also present. Muscularis Externa – two muscle layers: (1) inner circular layer and (2) outer longitudinal layer -upper 1/3rd is striated muscle and continuation of pharynx -middle 1/3rd is combination of striated and smooth muscle mixed together -Lower 1/3 is only smooth muscle, as is the rest of the digestive tract -A nerve plexus, called the myenteric plexus (Auerbach’s plexus) is between the two layers and innervates the muscularis externa to produce the peristaltic activity -Mucosal and submucosal glands of esophagus secrete mucus to lubricate and protect lumen Glands – two types present in wall of esophagus and both secrete mucus: 1. Esophageal Glands Proper – scattered in the submucosa of esophagus but concentrated near the top. They are small, compound tubuloalveolar glands and dilate during secretion. Mucus is acidic and viscous, sometimes forming transient cysts 2. Esophageal Cardiac Glands – found in the lamina propria of mucosa in the distal esophagus. Mucus is neutral pH. -Glands near the stomach protect esophagus from regurgitated contents, and excessive reflux is called pyrosis (heartburn), which can lead to Gastroesophageal Reflux Disease -The muscle of esophageal wall is innervated by both autonomic and somatic nervous systems -striated muscle in upper 1/3rd is innervated by vagus nerve (CN X) -smooth muscle in lower 1/3rd innervated by visceral motor neurons from vagus nerve Stomach – expanded part of digestive tube underneath the diaphragm that receives bolus from esophagus. Mixing of bolus and gastric secretions produce a fluid mix called chime -stomach is divided into three regions histologically, but FOUR regions anatomically: 1. Cardia surrounds esophageal orifice 2. Fundus lies above the level of horizontal line drawn through esophageal orifice 3. Body lies below the line of esophageal orifice 4. Pylorus is the distal, narrow sphincteric region between stomach and duodenum -Histologic divisions of stomach are based on the type of glands present in the mucosa: 1. Cardiac Region – contains cardiac glands 2. Pyloric Region – proximal part to pyloric sphincter containing pyloric glands 3. Fundic Region – largest part between cardia and pylorus containing gastric glands Gastric Mucosa – longitudinal submucosal folds, rugae, allow stomach to distend when filled -stomach is also composed of mucosa, submucosa, muscularis externa and serosa layers -rugae poorly developed in upper portion of stomach, but prominent in narrower regions -the rugae do not alter total surface area, but they accommodate expansion -Mamillated areas – small regions of mucosa are formed by grooves or shallow trenches that divide the stomach into bulging irregular areas -at higher magnification, openings can be seen called gastric pits or foveolae which receive contents from the gastric glands underneath them. -Surface mucus cells line the inner surface of the stomach and gastric pits -The epithelium that lines surface of gastric pits is simple columnar and are designated surface mucous cells. -each cell has an apical cup of mucinogen granules, creating a glandular sheet of cells. -mucus cup take up most of volume of cell, and stains with toluidine blue due to strong anionic groups in glycoprotein including bicarb -mucous secretion from surface mucus cells is called visible mucus because of its cloudy appearance, and forms a gel-like coat that adheres to epithelial surface and protects it against abrasions from chime -High HCO3 and K+ concentration of mucus protects epithelium from acidic content -Prostaglandins (PGE2) stimulates secretion of HCO3 and increase thickness of mucus layer with accompanied vasodilation in lamina propria to protect the tissue -stomach lining does not have absorptive capacity, but some H2O, salts, and lipid-soluble drugs may be absorbed -alcohol, NSAIDs, and aspirin enter lamina propria by damaging the surface epithelium Fundic Glands of Gastric Mucosa – also called gastric glands, they are present in entire gastric mucosa except for where cardiac and pyloric glands reside. -fundic gland produce gastric juice of the stomach, and are simple, branched, tubular glands that extend from the bottom of gastric pits to the muscularis mucosae. -the isthmus is a short segment located between gastric pit and the gland below housing the stem cells which self-renew and differentiates -cells destined to become surface mucus cells migrate up in gastric pits to surface, while other cells migrate downward maintaining population of fundic gland epithelium -several glands open into a single gastric pit, and each gland has a narrow, relatively long neck segment and a shorter wider base (fundic segment) -cells of the gastric glands produce 2L gastric juice per day, and contain 4 components: 1. Hydrochloric Acid (HCl) – concentrated at 155mmol/L and pH of <1 – 2, produced in parietal cells and initiates digestion of protein and converts pepsinogen to pepsin a. Most bacteria destroyed in stomach except for H. pylori, which contain urease which can create a protective ammonia cloud, allowing it to survive 2. Pepsin – potent proteolytic enzyme converted from pepsinogen produced by chief cells by HCl at pH lower than 5. It hydrolyzes peptide bonds. 3. Mucus – acid-protective coating for stomach secreted by mucus-producing cells. Mucus and bicarbs trapped in mucus layer maintain neutral pH and is called physiologic gastric mucosa barrier 4. Intrinsic Factor – glycoprotein secreted by parietal cells that binds to vitamin B12 and is essential for its absorption, lack of which causes pernicious anemia and B12 deficiency -Gastrin and other hormones are produced by enteroendocrine cells in the fundic glands and are secreted into lamina propria, where they enter circulation. -Fundic glands are composed of four functionally different cell types: (1) Mucus neck cells, (2) chief cells, (3) parietal cells, (4) enteroendocrine cells, (5) stem cells -Mucus neck cells are localized in the neck of the gland and are interspersed with parietal cells -located in the neck of fundic gland, mucus neck cells are interspersed with parietal cells -mucus neck cells are shorter than surface mucous cells and contain less mucinogen and do not exhibit a mucus cup -mucous neck cells secrete soluble mucus compared with the insoluble or cloudy mucus of surface mucous cell, and release of granules is induced by vagal stimulation -Chief cells are located in deeper part of fundic glands, and are typical protein-secreting cells with abundant rER with basophilic base, but eosinophilic apical cytoplasm due to secretory vesicles. Chief cells secrete pepsinogen and a weak lipase -Parietal cells secrete HCl and intrinsic factor – also called oxyntic cells, found in the neck of fundic glands and in deeper part of the gland -under electron microscope, parietal cells have a intracellular canalicular system that communicates with lumen of gland projecting numerous microvilli -microvilli project from surface of canaliculi and an elaborate tubulovesicular membrane system adjacent to canaliculi, which serve as a reservoir of plasma membrane containing proton pumps, which can be inserted into plasma membrane to increase acid production HCl is produced in the lumen of intracellular canaliculi – parietal cells have 3 receptors that activate HCl secretion: 1. gastrin receptor, (2) histamine H2 receptors, (3) acetylcholine M3 receptor -gastrin stimulation of the gastrin receptor is activates production of HCl: 1. Production of H+ Ions – occurs in parietal cell cytoplasm by carbonic anhydrase which hydrolyzes H2CO3 to H+ and HCO3-. CO2 diffuses across basement membrane into cell from blood capillaries 2. Transport of H+ ions – across the membrane to lumen of canaliculus occurs by the H+/K+ ATPase proton pump while K+ from canaliculus transported into cytoplasm 3. Transport of K+ and Cl- ions from cytoplasm into lumen of canaliculus through activation of K+ and Cl- channels in plasma membrane 4. Formation of HCl – from H+ and Cl- transported into the lumen of the canaliculus -Intrinsic Factor is secreted by parietal cells and is stimulated by same receptors as gastric acid secretion, and is used in absorption of vitamin B12 in ileum. Clinical Correlate: Pernicious Anemia and Peptid Ulcer Disease (PUD) -Achlorhydria is an autoimmune disease characterized by destruction of gastric mucosa, which can lead to absence of parietal cells and inhibition of intrinsic factor (IF) secretion, leading to pernicious anemia -Lack of intrinsic factor is MOST COMMON CAUSE of Vit. B12 deficiency -some bacteria bind B12-intrinsic factor complex to prevent absorption -total or partial gastrectomy causes loss of intrinsic factor = pernicious anemia -loss of gastric epithelium occurs in peptid ulcer disease (PUD), and even healed ulcers produce less intrinsic factor -H2 blockers such as ranitidine and cimetidine block attachment of histamine to suppress gastric acid and intrinsic factor production to treat peptic ulcers, but can cause B12 deficiency -Proton pump inhibitors such as omeprazole can inhibit H+/K+ ATPase without touching IF -Most peptic ulcers come as a result of H. pylori infection Clinical Correlation: Zollinger-Ellison Syndrome – excessive gastrin secretion from a tumor of gastrin-producing enteroendocrine cells in duodenum is called Zollinger-Ellison Syndrome or gastrinoma. -excessive secretion of HCl by parietal cells cause gastric/duodenal ulcers Functional Consideration: the GI Endocrine System: enteroendocrine cells account for 1% of epithelial cells in GI tract, but are largest endocrine organ in body -also found in pancreas, liver, and respiratory epithelium -Also called neuroendocrine cells (secrete similar hormones to those in CNS) -diffuse neuroendocrine system (DNES) – neuroendocrine cells distributed singly throughout GI system -In pancreas, enteroendocrine cells form accumulations called islets of Langerhans -Malignant DNES cells cause gastroenteropancreatic (GEP) neuroendocrine tumors -Carcinoid Syndrome – caused by release of variety of hormonally active substances by tumor cells -Amine precursor uptake and decarboxylation (APUD) cells – secrete variety of regulator substances in tissues or organs including respiratory epithelium, adrenal medulla, islets of Langerhans, thyroid gland, and pituitary gland. -Enteroendocrine cells also produce paracrine hormones such as somatostatin, which inhibits other GI and pancreatic islet endocrine cells -Neurotransmitters are also secreted by GI mucosa to stimulate smooth muscle. -Enteroendoctine cells secrete products into lamina propria or underlying blood vessels -there are 2 types of enteroendocrine cells: (1) Enteroendocrine “closed” cells which are small and do not touch lumen, and (2) enteroendocrine “open” cells, which touch the lumen and serve as primary chemoreceptors that sample contents of gland lumen and release hormones based on that information -secretion of closed cells is regulated by luminal content through neural and paracrine Cardiac Glands of the Gastric Mucosa – composed of mucus-secreting cells that surround the esophageal orifice and their secretions contribute to gastric juice and helps protect esophagus from gastric reflux. -glands are tubular, tortuous, and branched composed of mucus-secreting cells interspersed with enteroendocrine cells -short duct segment containing columnar cells interposed between secretory portion and shallow pits Pyloric Glands of Gastric Mucosa – similar to surface mucus cells + help protect pyloric mucosa -located near pyloric antrum and are branched, coiled, tubular glands, and empty into deep gastric pits that occupy half the thickness of mucosa Epithelial Cell Renewal in the Stomach – -surface mucous cells are renewed every 3-5 days through mitotic activity in isthmus -cells of fundic glands have a long life span (cells of ishmus migrate down glands to give rise to parietal cells, chief cells, mucus gland cells, and enteroendocrine cells) -parietal cells live 150-200 days; hypothesized that parietal cells originated from a bacterium called Neurospora crassa -chief and enteroendocrine cells live 60-90 cells -mucus neck cells live 6 days Lamina Propria and Muscularis Mucosa – in the stomach, it is restricted to the limited spaces surrounding gastric pits and glands – composed of reticular fibers with fibroblasts and smooth muscle cells -mucularis mucosa is composed of two relatively thin layers, inner circular and outer longitudinal layer Gastric Submucosa – composed of dense connective tissue with adipose and blood vessels as well as nerve fibers and ganglion cells that compose the submucosal (Meissner’s) plexus Gastric Muscularis Externa – consist of an outer longitudinal layer, a middle circular layer, and an inner oblique layer -arrangement of muscle is important as it relates to role in mixing chime -contains the myenteric (Auerbach’s) plexus that innervates the muscle layers