AirwayBasics - School of Medicine
advertisement

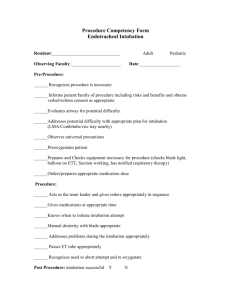
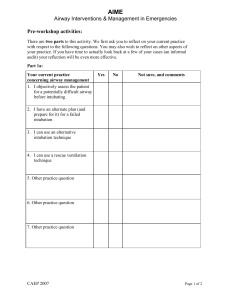
By: Parrish T. Eilers, MD LSU Emergency Medicine The Emergency Medicine Physician should be proficient in the assessment and management of all types of patient airways, regardless of age, gender, or level of difficulty. By the end of this lecture, students should able to: A) Properly assess a patient’s airway. B) Discuss techniques for properly ventilating a patient. C) Identify tools and proper technique needed for intubating a patient. D) Discuss RSI 1) Failure to oxygenate or ventilate 2) Unable to protect their airway 3) Expected Clinical Course The first step needed before intubating any patient, should be to assess their airway. Steps needed for airway assessment, should start with can I properly ventilate this patient Ventilation is the exchange of air between the lungs and the environment, including inhalation and exhalation. Endotracheal Intubation is the placement of an airway into the trachea for airway maintenance. Requirements for bag mask ventilation: Need to have an open airway Need to have a proper mask seal between the patient and your mask Evaluating for bag mask ventilation difficulty MOANS M: Mask Seal O: Obesity A: Age(>50 years) N: Neck Mobility S: Stiff(ie lung stiffness) Patients should ideally be supine in the “sniffing” position Mask should cover the nose and mouth of the patient Bring the patient’s face UP to the mask, by holding onto the mandible, not the soft tissue under the chin. Don’t push the mask down on a patient’s face. Can use oral or nasal pharyngeal airways to assist with bagging Two rescuer technique is best Evaluating for Difficult Intubation LEMON L: Look for any anatomy distortion E: Evaluate using 3-3-2 method M: Mallampati score O: Obstruction, any signs of N: Neck Mobility After assessing the airway, begin by looking down at the patient’s face from above the head. Then you gently scissor open the patient’s mouth, with your right hand. With the laryngoscopic blade in your left hand, insert it into the right side of your patient’s mouth and advance it along the tongue. If using a MAC blade, advance to the base of the tongue or the vallecula and sweep the tongue to the left. While doing this you’re also pulling your blade towards their feet. If using the Miller blade, then advance to the epiglottis and place the tip of your blade on the epiglottis. Then you sweep the tongue to the left and pull your blade towards your patient’s feet, lifting the epiglottis. Your Goal is just below the epiglottis. 1) Preparation 2) Preoxygenation 3) Pretreatment 4) Paralysis with Sedation 5) Protection of Airway(Sellick manuver) 6) Pass the Tube( with Confirmation) 7) Postintubation Management Preparation is key to intubating your patient and should begin before your patient even arrives at the hospital. Oxygen with Bag/Mask and NRB Suction Endotracheal tubes Oral and Nasal Airways Syringe Laryngoscope Blade with working Handle Bougie, LMA Mask with Face shield and Gloves Surgical airway Equipment All patient’s should be pre-oxygenated with 100% O2 by NRB or Bag/Mask for 2 minutes prior to intubation, even if they’re sats are 100% by NC O2. Because you want to blow off as much Nitrogen as possible and saturate your patient’s alveoli with oxygen. Give drugs to aid with the physiologic responses of intubation Lidocaine--------blunts bronchospasm and the reflex response Opioid(Fentanyl)---------blunts reflex response Atropine--------to avoid bradycardia in kids receiving Succinylcholine Depolarizing Agent----- to attempt to prevent fasciculations Give your RSI drugs, sedation first and then your paralytic. Usually pushed one right behind the other. Common Paralytics Succinylcholine Rocuronium Common Sedatives Etomidate Ketamine Ativan Versed The airway is usually protected by using the Sellick maneuver or cricoid pressure, during paralysis, intubation, and confirmation of tube placement. The cricoid ring is compressed with the assistant’s index finger and thumb. The tube is placed by direct visualization of the tube passing through the vocal cords. Inserted to a distance of about 3 times the tube size. Usually about 24cm in adult males and about 21 in adult females. Verify tube placement by watching the tube go through the cords, CO2 detector, auscultation of bilateral breath sounds, and CXR. Don’t forget long term sedation and vent settings. Also don’t forget to check your postintubation CXR.