Epidermal Growth Factor Receptor mutation testing for access to
advertisement

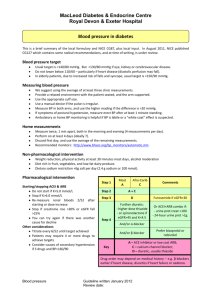
Epidermal Growth Factor Receptor mutation testing for access to gefitinib in first-line treatment for advanced Non-Small Cell Lung cancer May 2013 Introduction Lung cancer is the fourth most common cancer in New Zealand, but is the leading cause of cancer death (2009). Five-year survival is low, having remained largely unchanged between 1998 and 2009 – fluctuating between 8.9% and 10.2%. This is lower than in some other Western nations; for example, Australia and Canada have five-year survival of over 14%. Lung cancer is categorised by histology (the microscopic structure of tissue), and is broadly divided into small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). NSCLC represents 80-90% of cases. NSCLC is further divided based on the tissue of origin (histological classification or “histology” of the cancer). The most common subtypes are adenocarcinoma (50-60%) and squamous cell carcinoma (3040%), but there are a number of other less frequent subtypes (~10%). NSCLC presents with advanced disease (Stages IIIB-IV) in ~70% of cases, which is incurable and is treated with chemo or radiotherapy to improve quality of life and extend survival. Early-stage (Stages I-IIIA) represents only ~30% of cases, and is treated with surgery (or combined chemotherapy and radiotherapy if surgery is not possible) in an attempt to cure the disease. However, half of all patients who undergo “curative” treatment later relapse i.e. approximately 85% of all NSCLC patients’ progress to advanced disease. A subset of NSCLCs acquire activating mutations in the epidermal growth factor receptor (EGFR) gene which drives cancer cell growth. EGFR tyrosine kinase inhibitors (TKIs) block this signalling and produce a dramatic response in a small proportion of patients (10-12% in Europeans and 30-40% in Asians). The prevalence of EGFR mutations in the New Zealand lung cancer population is unknown, and may vary between ethnic groups. These mutations are found mainly in the adenocarcinoma histology, and at lower rates in other histologies. Erlotinib (an EGFR TKI) has been funded since 2010, initially for all patients who had previously had chemotherapy (i.e. as second-line treatment), regardless of EGFR mutation status. In August 2012, when PHARMAC approved gefitinib (an EGFR TKI) available before chemotherapy (first-line) only in those with a demonstrable EGFR mutation. EGFR TKIs produce response rates of 58 – 83% and median survival of ~ 23.3 months in people with EGFR mutations. Traditional chemotherapy has a 20 - 30% response rate and extends median survival from ~5 months to ~12 months. EGFR mutation testing and EGFR TKIs are an example of co-dependent technologies. The drug is only as effective as expected if the testing platform is reliable at identifying patients who are likely to respond to treatment, and therefore clinical outcomes are dependent on both the test and drug. All overseas jurisdictions have grappled with how to effectively introduce equitable EGFR testing for NSCLC, with guidelines published in Australia, Europe, Singapore and the United States. There is broad consensus amongst guidelines, but each adapts testing recommendations to the local environment. 1|P a g e Policy Question Should EGFR mutation testing be funded in New Zealand for access to first-line EGFR TKIs? What is the most clinically and cost-effective method of EGFR mutation testing in New Zealand? Rationale for Assessment Currently, two EGFR TKIs are funded in New Zealand, erlotinib (Roche) and gefitinib (Astra-Zeneca). Erlotinib was listed by PHARMAC in 2010 as a second or third-line treatment, regardless of EGFR mutation status. On 1 August 2012, PHARMAC listed gefitinib in the first-line only for patients with proven EGFR mutations, but did not define a testing strategy or elucidate a plan for funding testing. As PHARMAC restricted access to first-line EGFR TKI treatment to only those patients with non-squamous histologies and a proven EGFR mutation, the question of whether EGFR testing should be funded became primarily an equity and ethical issue. The decision was made to fund EGFR mutation testing on this basis, the National Health Committee, in cooperation with District Health Boards (DHBs) and the National Health Board, was set the task of developing recommendations for the most clinically sensible and cost-effective EGFR mutation testing in New Zealand. Technology Status & Commercial Considerations in New Zealand EGFR mutation testing falls under the broader category of molecular or genetic testing. This testing involves identifying and sequencing part of a person’s DNA in order to determine whether disease-causing mutations are present. There are a number of sequencing techniques, all of which have varying strengths and weaknesses, and all of which are used in clinical practice or research. Some genetic diseases require different diagnostic approaches (e.g. FISH, CISH or immunohistochemistry) depending on the type of genetic abnormality (e.g. HER2 testing for access to Herceptin®). The FDA has not specified a single technology for EGFR testing to be used in the United States, and most countries have chosen instead to specify the analytical performance of EGFR testing to which any technology must adhere. This has allowed the development of more than 10 potential testing platforms around the world. In New Zealand, three centres are currently performing EGFR mutation testing – two public (Auckland DHB and Canterbury DHB) and one private (PathLab, Bay of Plenty). All three use the Roche Diagnostics cobas® 4800 real-time PCR platform. This binds short strands of DNA (primers) that match known mutations and thereby identify mutations in a patient’s tumour. This is a “targeted” testing method which is only able to identify known mutations but is less time-consuming, can be performed on fewer tumour cells, and is more sensitive than direct DNA sequencing. The Roche platform is also able to test for two other gene mutations which have similar relevance in cancer treatment (KRAS for cetuximab in colorectal cancer and BRAF for vemurafinib in melanoma). Testing for these mutations is currently employed internationally. PHARMAC has received and is considering applications for both of these medications. 2|P a g e Methods The development of the recommendations for EGFR testing in New Zealand was completed in number of separate stages: 1. Preparation and publication of the NHC’s “Rapid Review on EGFR gene mutation testing in patients with advanced NSCLC for access to Gefitinib” in June 2012. 2. Convening an EGFR Working Group of sector leaders to develop clinical recommendations for EGFR testing, with development of final recommendations in April 2013. 3. Development of the final NHC recommendations regarding EGFR testing in New Zealand including implementation and funding strategy. 4. Interaction with the Health Innovation Partnership (HIP) to develop a research proposal to examine EGFR mutation nature and prevalence in the New Zealand population. The Rapid Review was prepared through a non-systematic narrative review of reports published by Health Technology Assessment (HTA) agencies, guidance documents issued by various professional organisations overseas and other papers identified through Google scholar. Information from these reports was synthesised under the Committee’s assessment domains to enable the evidence to be evaluated using the Committee’s 11 decision-making criteria. The EGFR Working Group was convened to develop sensible clinical recommendations for EGFR testing. It comprised seven individuals from across the country and met on two occasions. Draft recommendations were developed and distributed to relevant stakeholders for feedback prior to finalisation. The Working Group had sign off on the final version of the recommendations. On the basis of these clinical recommendations the NHC liaised with DHBs, the Ministry of Health and the NHB to develop a sensible approach to implementation and funding of the recommendations Summary of Findings Clinical Domain (includes safety & effectiveness of intervention) EGFR mutation testing’s clinical importance is derived from its ability to identify individuals most likely to benefit from EGFR TKIs. Its clinical effectiveness is therefore related directly to the benefit derived from the medication. As described earlier there is international consensus that EGFR TKIs should be offered as firstline treatment in EGFR mutant NSCLC. In unselected patients treated with EGFR TKIs response rates in early trials were 8 – 9% and median time to progression 2.2 to 3.0 months. In contrast, patients with activating EGFR mutations, EGFR TKIs produce improved response rates (58-83% vs. 20-30%); increased progression-free survival (9.4 – 13.1 months vs. 4.6 – 6.3 months); and increased overall survival compared to historical controls (23.3 months vs. 12 months), when compared to standard chemotherapy. In addition, treatment with EGFR TKIs results in fewer side effects. Treatment-related serious adverse events are 2 – 6% for EGFR TKIs compared to 14 – 20% with traditional chemotherapy. The NHC recommendations were developed by a clinical Working Group (WG) and aimed to produce recommendations both clinically sound and as cost-effective as possible. It provided guidance in six different areas. 3|P a g e The EGFR Working Group recommendations are listed below: EGFR Testing in New Zealand Rec 1: EGFR mutation testing should be provided by New Zealand laboratories in more than one centre. Eligibility for EGFR Mutation Testing Rec 2: EGFR mutation testing should be offered to patients with non-small cell lung cancer (NSCLC), with all histological diagnoses except confidently-diagnosed squamous cell carcinoma. EGFR Testing Pathway Rec 3: Eligible patients should have only a single EGFR mutation test during the course of their illness. Ideally, this should be undertaken on the first diagnostic biopsy, and should only be performed on the resection specimen if no previous EGFR mutation test has been undertaken. Rec 4: EGFR mutation testing should form part of the standard Pathology reporting process for eligible patients (who have not previously had an EGFR test). Rec 5: Current evidence does not support repeat biopsy or EGFR mutation testing at the time of relapse in patients who are able to or have had an EGFR test performed on their primary tumour. Rec 6: Accurate clinical information including disease stage, prior biopsy procedures and individual patient history (particularly in relapsed disease) should be included with any lung cancer pathology request to avoid test duplication. Sample Acquisition and Quality Rec 7: The largest amount of tissue, at the least risk to the patient, should be obtained at initial diagnosis. Rec 8: Endobronchial ultrasound (EBUS) guided biopsy is preferred to transbronchial needle aspiration (TBNA), and transthoracic core biopsy is preferred to fine needle aspirate (FNA) for sample acquisition wherever available and safe. Rec 9: Where biopsy material is inadequate for EGFR mutation testing this should be fed back to the diagnostic clinician, and the primary treating clinician should consider re-biopsy on a case-by-case basis. Pathology Processes for Testing Rec 10: A testing approach used must identify at least 90% of mutations known to predict for response to EGFR tyrosine kinase inhibitors (TKIs), and should be able to identify mutations when tumour cells comprise 10% of the sample (analytical sensitivity). Rec 11: Laboratories undertaking histopathological diagnosis (but not EGFR testing) should characterise samples as eligible, before sending them to the appropriate molecular testing laboratory. Rec 12: Any laboratory undertaking EGFR mutation testing must have molecular diagnostics accreditation from an appropriate laboratory accreditation organisation, and participate in an EGFR mutation testing quality assurance program. Rec 13: The turnaround time for the mutation test should be five working days from the arrival of the sample in the molecular diagnostics laboratory. Rec 14: The histopathological diagnostic report should not be delayed to await the EGFR test result, which can be issued as supplementary. Registering EGFR Mutations Rec 15: EGFR mutation status and the specific mutation identified should be recorded in the New Zealand Cancer Registry 4|P a g e Rationale for Recommendations: The group decided EGFR testing should be undertaken in New Zealand rather than Australia. This reflects the need to combine a cost-effective testing program, timely turnaround for results, and develop genetic testing capability for the future. EGFR testing costs in Australia range from NZ$400 - $492 with the additional courier cost of NZ$40 (3-5 days) – $300 (overnight). Thus, total costs could be NZ$440 - $792 per test, with a slower turnaround for results. Individual test costs are likely to be similar in New Zealand to those in Australia. Testing should be offered to all patients with NSCLC except those with confidently diagnosed squamous cell carcinoma. SCC represents 30 – 40% of all NSCLC but the rate of EGFR mutations is 0 – 1.1%. By excluding this subgroup, a negligible number of EGFR mutation positive cases would be missed whilst significantly reducing the number of cases tested. This is in keeping with PHARMAC’s Special Authority criteria for gefitinib funding and MSAC’s recommendation in Australia. The risk is also mitigated by the availability of erlotinib in the second-line, and when received second-line there was no statistically significant difference in overall survival. The WG’s recommendations regarding the EGFR testing pathway aimed to minimise unnecessary repeat testing, keep test arrangement as simple as possible (to reduce resource and time waste), whilst reinforcing the need to test as early as possible in a patient’s diagnostic pathway. It recommended that each eligible patient be funded for only one test during the course of their illness - on the first diagnostic specimen (if possible). Figure 2 shows the proposed testing algorithm. Testing was specifically approved regardless of disease stage, because of the extra resources wasted through a more complicated system testing only those with definite stage IIIB/IV disease (for whom gefitinib is available). The experience from the Royal Marsden Hospital in London showed in the first year of EGFR testing the turnaround for the test itself was 4.9 days, but the clinical turnaround was 17.8 days owing to “the time to request sample from referring hospital, sample identification and retrieval, section cutting, shipping and pathological review”. Additional benefits include: 1. Treatment of very unwell patients who may be unable to wait for delayed EGFR results; 2. Adherence to the cancer treatment targets; 3. Prevention of missed EGFR test requests through human error; 4. Improved test price per test through increased test batching; 5. Improved understanding of EGFR prevalence in New Zealand’s population 6. Analysis of factors which may affect the risk of relapse. The WG’s recommendations on sample acquisition and quality aimed to emphasise the importance of taking high-quality biopsies at the first attempt that are of sufficient volume and quality to allow genetic testing in order to reduce repeat biopsies for EGFR testing. This will have both a clinical and cost benefit. The WG’s recommendations regarding pathology processes for EGFR testing defined the minimum parameters to which any testing laboratory must adhere. It did not specify a particular testing technology, but rather outlined test characteristics that would be satisfactory, thereby allowing laboratories to adapt to improved testing techniques. The turnaround time (TAT) is the critical recommendation. Five days was felt to be clinically appropriate and would allow most, if not all, patients to have the EGFR mutation status available at the first treatment appointment. The current testing platform employed in New Zealand requires test batching, and in order to maintain an adequate turnaround time and costs low, fewer laboratories would be preferable. The WG felt it would be inappropriate to mandate a TAT for complete histopathological reporting, as this is well established in all centres. 5|P a g e The WG recommended that EGFR mutation status, and the specific mutation identified be recorded. The Executive have been working with Cancer Control New Zealand to include these fields in the updated New Zealand Cancer registry electronic platform. Figure 1: Proposed Testing Algorithm Diagnosed with Non-Squamous or NSCLC NOS EGFR mutation test at first biopsy or resection (Pathologist ordered) Re-biopsy (Clinician requested) Sufficient tissue Insufficient tissue EGFR status established Re-test Inconclusive result Stage IIIB/IV at diagnosis or progression to stage IIIB/IV No re-test EGFR Mutation positive EGFR Mutation negative or inconclusive Economic Domain The economic analysis explores the impact of the NHC’s involvement in this area. It does not explore the impact of PHARMAC’s funding decision by mandating EGFR testing for access to gefitinib as this was explored in the earlier Rapid Review. The argument for making testing available and testing every patient regardless of stage is both clinical and economic. It is important to note that 85% of NSCLC patients will be eligible for testing/EGFR TKIs during the course of their illness. A system which tests only Stage IIIB/IV patients will be more complicated and separate EGFR analysis from the standard pathology reporting. This more complicated system adds to health system cost through wasted resources. A simpler system (as recommended by the WG) makes testing part of the standard pathology process and provides timelier and more cost-effective results. 6|P a g e Figure 2: Resources wasted by implementing a complicated test request system in order restrict the number of tests undertaken. The lower diagonal lines represent the upper, mid and lower estimates of resources wasted for a given individual test price. For example, if the individual test price is $300, then the resources range from $19,440 – $76,050 (mid-point estimate $47,745). This shows that for all prices less than $400 per test it is more cost-effective from a systems viewpoint to test all patients. With the current platform, the number of laboratories undertaking testing affects both test cost and efficiency. The greater the number of laboratories, the fewer samples that will be processed by each. This increases the cost of each test and reduces the ability of each laboratory to meet to the 5-day turnaround time. As discussed in paragraph 15, three New Zealand laboratories perform testing use the Roche Diagnostics cobas® 4800 platform. Roche Diagnostics charges a list price for reagents at $220 per test, and a variable lease price for its PCR (polymerase-chain reaction) machine ($10,000-$20,000 per year, but it is waived if sufficient numbers of tests are performed on a machine). Tests are usually “batched” (on average 4-6 per batch, but up to 24 are possible), and with each batch a positive and negative control sample are also tested which are also charged $220. Therefore, the greater the number of samples in each batch and the more samples run through each machine, the less the total cost per test. Table 1 below shows how the number of laboratories affects the reagent-only cost of EGFR testing with the Roche platform. In order to maintain a 5-day TAT laboratories will have to batch samples at least once a week. This shows that funding two laboratories would save $47,000/year in reagent costs alone, compared to funding four laboratories. This analysis does not include laboratory overheads. Not included in this analysis is cost of leasing a machine as Roche did not disclose the number of tests required for Roche to forego this charge. However, if a greater number of laboratories undertake testing the lease price will increase total cost. 7|P a g e Table 1: The costs of EGFR test reagents based on the number of laboratories and the volume of tests undertaken by each laboratory. This shows that by decreasing batch sizes the cost of reagents per test increases affecting cost and laboratory efficiency. Number of Laboratories Yearly tests per laboratory Test per week Reagents cost per test (Roche list price) Total Annual Reagent Cost 1 2 3 4 1200 600 400 300 23 11.5 7.7 5.7 $239 $258 $277 $297 $286,800 $309,600 $332,400 $356,600 The impact of NHC involvement in developing a cost-effective approach to EGFR testing is difficult to quantify, but is estimated at $280,000 – 348,000. Much of the benefit relies on the implementation and uptake of the clinical recommendations regarding biopsy quality and sample processing. A direct benefit of NHC involvement has been in the rationalisation of testing to appropriate sub-groups and the recommendation against funding repeat testing (both on clinical grounds). An estimate of the annual financial benefit of NHC involvement is shown below. Table 2: The financial benefit of NHC involvement in the EGFR testing approach. This exploration compares the costs of an uncontrolled expansion to 4 laboratories compared to restricting testing to 2 laboratories. Assumptions below in footnote.1 Avoided Costs Description Machine lease cost Cost ($/year) 4 labs to 2 lab 20,000 – 40,000 Pathologist 1 hour/week 8,626 Scientist 3 hours/week 9,722 Additional test cost Increased reagent cost 47,000 Improved efficiency of system Avoided resource waste 29,745 Avoided EGFR tests: Repeat tests progression Assumptions: at 10% repeated at progression 10% repeated at relapse Repeat tests at relapse 48,000 24,000 – 72,000 Avoided repeat biopsies: Avoided complications Decrease repeat biopsies 15% to 10% (~$1539/box) Intercostal drainage avoided(0.375 - 1.125%) Total 1 Assumptions: 1. 2. 3. 4. 5. 6. 92,300 600 $280,000 – $348,000 Lab scientist salary –$65,000, hourly rate of $31.16/hr (based on 2086 hours/annum) Pathologist/Oncologist salary - $172,500 based on average 6 years’ experience, hourly rate of $82.69/hr Improved system efficiency – assumed test cost $400, additional resource use $99.75 Biopsy complications: 2 - 30% result in pneumothorax and 5 – 15% of these intercostal tube placement Cost of tube insertion is: tube + 1.2 days monitoring - $800 Biopsy prices (ADHB): Bronchoscopy and biopsy - $1698; CT-guided biopsy - $1380 8|P a g e Societal & Ethical Domain (including acceptability and equity) EGFR testing should be funded by the New Zealand public health sector, as there would be significant inequity if individual patients were required to fund their own testing. In advanced lung cancer, only 30-50% of patients who receive first-line treatment undergo second-line treatment. This lack of uptake is usually due to disease progression and perceived lack of benefit of further treatment. There is, therefore, widespread consensus in treatment guidelines that EGFR TKIs should be used in the first-line for patients with EGFR mutations. On the basis of these guidelines, and with the approval of gefitinib in the first-line in New Zealand, it would then be unethical to not fund EGFR testing, as this would unfairly disadvantage those who could not afford testing. Funding testing would also be widely acceptable to both clinicians and patients. It will add a cost burden to DHB laboratories. The decision to exclude patients with squamous cell carcinoma from testing is in line with PHARMAC’s criteria for access to gefitinib, which has a similar provision. This equity issue is mitigated by the availability of erlotinib in the second line regardless of mutation status. Equally, if an individual patient has clinical characteristics that suggest the presence of an EGFR mutation, despite having squamous cell carcinoma, testing could be negotiated at a local DHB level. Financial Domain (includes feasibility of adoption and budget impact) There will be approximately 1,020 – 1,175 tests performed per year (based on 85-98% uptake of testing in NSCLC with non-squamous histology) at a cost of approximately $300 - $500 per test. Across the whole sector this amounts to $357,000 - $587,500 per year. At a realistic cost of $400 per test the cost would be between $408,000 and $470,000. Figure 3: The estimated annual national cost of EGFR testing against the cost of an individual test, based on a range of 85% to 98% of eligible patients undergoing testing. Estimated Annual National Cost of EGFR Testing $1,000,000 Total Cost $800,000 $600,000 $400,000 $200,000 $0 $100 $200 $300 $400 $500 $600 $700 $800 Single Test Cost The impact can also be analysed by DHB. Figure 4 is based on lung cancer registrations in 2009 and gives an estimate of the number of patients who would have been eligible for testing and the associated cost (based on an individual test cost of $400). The error bars represent the costs based on a range of individual test costs from $300 to $500. In 2009, Canterbury would have spent $54,240 and West Coast $4,320. 9|P a g e Figure 4: The estimated annual volume and cost of EGFR testing by DHB. Estimates are based on lung cancer registrations in 2009. The error bars show the range in total costs based on an individual test price of $300 – $500. 175 150 125 100 75 50 25 0 Auckland Bay of Plenty Canterbury Capital & Coast Counties-Manukau Hawke's Bay Hutt Lakes MidCentral Nelson-Marlborough Northland South Canterbury Southern Tairawhiti Taranaki Waikato Wairarapa Waitemata West Coast Whanganui $70,000 $60,000 $50,000 $40,000 $30,000 $20,000 $10,000 $0 Number of patients Total cost Estimated Annual Cost of EGFR testing by DHB Testing is already undertaken in New Zealand, and the technology has no feasibility of adoption concerns. The NHC may choose to recommend fewer laboratories than are currently testing, but changing laboratory providers has been recently undertaken on a much larger scale, and this should not prove to be an obstacle to implementation. Societal and Economic Benefit The societal economic benefit has not been formally quantified for EGFR testing in patients as it cannot be assessed independently from EGFR TKIs. There are benefits from the laboratory industry viewpoint, by enhancing New Zealand’s capacity for genetic testing. The development of a workforce with these skills will allow New Zealand to more easily adapt to this rapidly changing area of diagnostics. The financial of impact of the NHC’s recommendations is limited by uncertainty surrounding the effective implementation of these recommendations. Limitations and Uncertainty Limitations can be divided into three categories: methodological, implementation and future relevance. From a methodological viewpoint non-systematic searches were employed in the development of all the documents. Important sources may have been missed, but the content of recent recommendations/guidelines in Australia and the United States of America, correlate well with the recommendations produced here. There is uncertainty about the level of fidelity with which the sector will interpret the recommendations. There is no clear blueprint for funding a national approach such as this, and there are many obstacles to this being successfully implemented across a broad range of stakeholders. The recommendations themselves are limited by the rapid evolution of technology in this area. There may be groups of patients currently covered in these recommendations who would not benefit from testing, or that a platform that is able to test for more than just one mutation supersedes the current technology. The 10 | P a g e recommendations should be reviewed in 18 – 24 months in the wider context of genetic/genomic testing across disease areas. Implementation Implementation of the EGFR recommendations has five parts (many of which will occur concurrently): 1. Endorsement of recommendations by the National Health Committee 2. Letter to Minister of Health 3. Engagement with National Health Board – discuss monitoring and review process 4. Distribution of EGFR WG final recommendations to relevant clinical and sector stakeholders 5. Delivery of Implementation Document to DHB CEs and GMs of planning and funding 6. Health Innovation Partnership (HIP) funding for EGFR research to determine prevalence of EGFR mutations, define the local mutation prevalence by ethnicity and examine the performance of the current testing approach. As there is no clear funding process for undertaking nationally co-ordinated testing at present funding could be approached in four different ways: 1. Nomination of a DHB and GM of Planning and Funding to lead negotiation of an RFP and nationally applied contract 2. Top-slicing from the laboratory budget with Ministry of Health-led procurement 3. DHBs contract individually with laboratories undertaking EGFR testing 4. PHARMAC could fund co-dependant technologies from the community schedule budget when mandating testing for access to a medication. The NHC Executive would favour Option 1: “Negotiation of a nationally consistent contract by a lead GM of Planning and Funding”. This avoids top-slicing but allows a consistent and equitable approach to testing across New Zealand. It prevents unnecessary diffusion of the technology but allows for a competitive tendering process. This should provide the best combination of economies of scale and a competitive marketplace. Options 2, 3 and 4 are not recommended. Option 1 adds complexity to DHB budgeting and adds central responsibility which does not exist now. Option 3 allows uncontrolled diffusion, without the ability to implement a nationally co-ordinated strategy. Option 4 is outside PHARMAC’s current practice and does not offer a long-term solution as genetic testing will become a more standard part of laboratories services in the future. The NHC may wish to provide guidance around the optimal number of laboratories to undertake EGFR testing. Three laboratories are testing at present in New Zealand. There are a number of potential contracting scenarios, but due to economies of scale, timeliness and loss of expertise the NHC executive would favour limiting the number of laboratories. Table 3 below explores the relative advantages and disadvantages of several scenarios. 11 | P a g e Table 3: Advantages and disadvantages with a varying number of laboratories performing testing Advantages Single laboratory Two laboratories Three laboratories Disadvantages Centre of excellence Consistent and equitable testing practices Greatest economies of scale Lowest cost for reagents Large batch size enabling rapid turnaround time Easiest audit and monitoring Single contract partner Concentration of resources allows for earlier adoption of new technologies Distribution of expertise Multiple centres of excellence Allows for growth in future demand Improved recruitment and retention at multiple centres Retains competitive contracting Greater flexibility for competing laboratories to innovate Still able to attain reasonable turnaround time Three established laboratories already testing Greater diffusion of expertise Greater competition for current and future contracts Improved geographical distribution More than three laboratories Widespread geographic distribution – reduced sample travel Regional adaptation Greatest competition Monopoly supplier Reduced competition leading to noncompetitive contracting Reduce national acquisition of testing skills No local provider in case of laboratory or machine malfunction Loss of expertise to accommodate growth in future genetic testing Lack of infrastructure for next-generation technologies Geographic dispersion creating unforeseen transport difficulties Reduced economies of scale Increased contractual complexity Reduction in number of laboratories currently testing Increased complexity of monitoring and audit Further reduction in economies of scale Increased costs and slower test turnaround Reduced national co-ordination of future innovation More complex contracting, monitoring and audit Competition for lowest single test cost may prevent early adoption of new or advanced technology Greatest cost and slowest turnaround of tests Reduced expertise due to low test volumes at each centre Less consistent testing practices Complex clinical audit and clinical information gathering Complex contracting, monitoring and audit Decreased ability to coordinate a national approach to testing and future genetics Competition for lowest single test cost may prevent early adoption of new or advanced technology 12 | P a g e The NHC support at least 2 laboratories undertaking EGFR mutation testing, but it does not seek to specify the optimal number of laboratories undertaking testing. A competitive RFP or EOI process is recommended with review in 3 years to ensure KPIs are being achieved and allowing adaption to new and emerging technologies, which should allow for an effective balance between cost and competition. There is a need in New Zealand to establish that EGFR mutation testing methods show appropriate analytic sensitivity and performance characteristics, if these assays are to be used to determine eligibility for access to tyrosine kinase inhibitors. Through a Request for Proposals (RFP) released in May 2013, the HRC and the NHC have sought to encourage New Zealand relevant research of high quality research that will determine the performance characteristics of EGFR gene mutation assays in non-small cell lung cancer in the New Zealand context. This will allow the NHC to learn from the implementation of national EGFR testing to help inform both future EGFR testing and broader genetic and genomic testing. Future Considerations Genetic testing volumes are likely to grow significantly in the next decade, as the clinical application of genetic information becomes more widespread. Figure 5 shows the growth in number of diseases for which genetic testing is available. Genetic testing volumes have grown by 280% in Australia between 2006 and 2011. It is likely that this trend will also be seen in New Zealand as the scope and clinical application of this testing increases. By applying a thoughtful national approach to testing at the outset in New Zealand, this uncontrolled growth in volumes and costs may be influenced. Figure 5: The growth in the number of disease for which genetic testing is available in both clinical and research settings Source: Hudson et al. Oversight of genetic testing laboratories. Nature Biotechnology 2006, 24(9):1083-90 13 | P a g e Prioritisation There are no competing technologies in NSCLC in New Zealand at present and therefore EGFR testing in this case must be prioritised across the total Laboratory Sector budget. As it is currently being funded it has effectively already been prioritised, and therefore implementation of the NHC recommendations should allow the most cost-effective strategy for testing in New Zealand. Performance Against Criteria Funding of EGFR mutation testing, if implemented in a cost-effective and thoughtful manner, fits the NHC decision making criteria well or very well across all domains. It does introduce an extra cost into the sector but this should be a relatively small cost to each individual DHB, but is offset by improved clinical outcomes. There was extensive engagement on the draft recommendations with feedback from many areas of the sector. Overall, there was widespread support for the content of the recommendations, with only minor changes needed to the drafts. Figure 6: Evaluation of EGFR mutation testing How well does the proposal fit the NHC's criteria? Criteria Not at all Clinical Safety and Effectiveness Health and Independence Gain Materiality Feasibility Policy Congruence Equity Acceptability Cost Effectiveness (Value for Money) Affordability Risk Other Criteria as the NHC thinks fit. Not very well Somewhat Well Very Well Explanation The tests have reasonable sensitivity and specificity, but do prodiuce some false positives and negatives EGFR TKIs are significantly more effective and better tolerated than chemotherapy in patients w ith EGFR-mutant NSCLC This affects 1,100-1,200 patients a year Infrastructure is in place and testing is currently underw ay NHC w ork serves to streamline testing and allow for adherence to cancer treatment targets. Funding the test affords equitable access to EGFR TKIs as PHARMAC requires a positive test for first-line access Recommendations deemed acceptable by stakeholders, improved treatment availability usually acceptable to patients but not formally tested. NHC w ork has attempted to inform the most cost-effective testing process, but success is unclear prior to implementation Will increase expenditure on diagnostic testing but w ill save money in the pharmaceutical budget Risk in funding strategies being addressed in implementation plan - risk in insufficient testing oversight N/A Criteria for Review Every recommendation made by the NHC is subject to review if the evidence upon which the assessment and recommendations are based changes. The recommendation to endorse EGFR testing for access to gefitinib in first-line treatment will be reviewed if the: The prevalence of EGFR mutations is either significantly higher or lower than international comparisons The availability of second-line EGFR treatment necessitates repeat EGFR testing Whole-genome or multi-locus sequencing becomes available at reasonable cost 14 | P a g e National Health Committee (NHC) and Executive The National Health Committee (NHC) is an independent statutory body which provides advice to the New Zealand Minister of Health. It was reformed in 2011 to establish evaluation systems that would provide the New Zealand people and health sector with greater value for the money invested in health. The NHC Executive is the secretariat that supports the Committee. The NHC Executive’s primary objective is to provide the Committee with sufficient information for them to prioritise interventions and make investment and disinvestment decisions. They do this through a variety of products including Prioritising Summaries, Technology Notes, EpiNotes, CostNotes, Rapid Reviews, and Health Technology Assessments which are chosen according to the nature of the decision required and time-frame within which decisions need to be made. Citation: National Health Committee 2013. Epidermal Growth Factor Receptor Mutation Testing Wellington: National Health Committee. Published in July 2013 by the National Health Committee PO Box 5013, Wellington, New Zealand This document is available on the National Health Committee’s website: http://www.nhc.health.govt.nz/ Disclaimer The information provided in this report is intended to provide general information to clinicians, health and disability service providers and the public, and is not intended to address specific circumstances of any particular individual or entity. All reasonable measures have been taken to ensure the quality and accuracy of the information provided. If you find any information that you believe may be inaccurate, please email to NHC_Info@nhc.govt.nz. The National Health Committee is an independent committee established by the Minister of Health. The information in this report is the work of the National Health Committee and does not necessarily represent the views of the Ministry of Health. The National Health Committee make no warranty, express or implied, nor assumes any legal liability or responsibility for the accuracy, correctness, completeness or use of any information provided. Nothing contained in this report shall be relied on as a promise or representation by the New Zealand government or the National Health Committee. The contents of this report should not be construed as legal or professional advice and specific advice from qualified professional people should be sought before undertaking any action following information in this report. Any reference to any specific commercial product, process, or service by trade name, trademark, manufacture, or otherwise does not constitute an endorsement or recommendation by the New Zealand government or the National Health Committee. 15 | P a g e