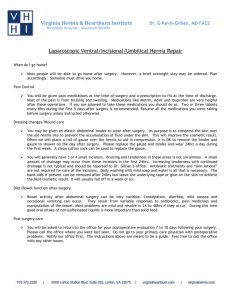
Admit Orders
advertisement

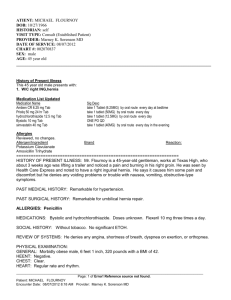
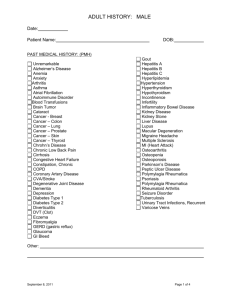
DOCUMENTATION IN YOUR 3RD YEAR AND BEYOND Summer Quarter 2010 Merrian Brooks and Amanda Kocoloski OVERVIEW General principles of documentation Types of Notes, the case of Ineda Surgery Admission Orders INTRODUCTION TO HOSPITAL CHARTING EVERYTHING must be written somewhere!!! H&P, progress notes, labs, orders Paper vs. EMR Example charts SAMPLE PATIENT: INEDA SURGERY Ineda is a 35 y/o f presenting to your office (outpatient) with a bulge in her groin. What do you want to know? Which aspects of the exam will you perform? What is your assessment? What is your plan? OUTPATIENT NOTE S: Pt is a 35 yo f presenting with a “bulge” in her groin x 2 months. It used to go away when she lays down but recently it remains even when supine. She denies discomfort. Last bowel movement yesterday. No nausea or vomiting. O: VS: T: 99.1 BP: 120/65 P: 90 R: 14 pain: 4/10 CV: S1 S2 no murmurs, no gallops Lungs: clear bilaterally, good excursion, good air movement Abdomen: flat, bowel sounds present, no rebound, no guarding, soft, irreducible mass in right groin below inguinal ligament appreciated, no erythema, no pain with palpation GU: no labial masses A/P: 35 yo f with femoral hernia. Plan:1. admit to hospital 2. consult surgery INEDA GOES TO THE HOSPITAL Ineda presents to the ER after her doctor calls ahead. You are sent to admit her to the floor. What do you need to know? What kind of exam will you do? What is your assessment? What is your plan? ADMISSION NOTE Full H&P related to CC Add a sentence (or 3) about the ER course Assessment Pt has an irreducible mass beneath inguinal ligament that is also evident on CT consistent with a femoral hernia. Plan While in the ER pt received 200mg of ibuprofen, and a pelvic CT scan that showed a femoral hernia of the right groin. Admission orders Other elements may include: informant and reliability, development/immunization (peds), problem list (complex pt) INEDA PREPS FOR THE OR Ineda is admitted. She is scheduled to have surgery the next day. What lab values do you need? What else needs to be documented before surgery? SURGERY PRE-OP NOTE Pre-op Dx: femoral hernia Procedure planned: Lotheissen-McVay femoral hernia repair Labs: CBC, Chem 7, PT/PTT, UA CXR: deferred EKG: normal 3 months ago Blood: type/screen, type/cross Orders: 1.NPO 2. skin prep Permission: Informed consent signed/on chart, INEDA IN THE OR Ineda goes into the OR and has a simple herniotomy. Luckily the small bowel that is trapped in the hernia is still healthy. Mesh is placed at the hernia site. What info should be documented? PROCEDURE/OP NOTES Procedure / Indication: Lotheissen McVay for femoral hernia Permission Physician / Assistants: Dr. Lotheissen DO, A. Kocoloski MSIV Estimated Blood Loss (EBL): 2mL Description I explained the risk/benefits and alternatives to the patient. The patient voiced understanding. Consent form signed placed on chart. Area prepped and draped in sterile fashion, Epidural anesthesia administered with Bupivicaine 0.5%. The abdominal wall was cut and the transversalis facia divided. The hernial sac was identified and small bowel was present in the canal. The bowel was healthy and removed from the hernial sac. Coopers ligament identified. Ethicon prolene mesh was placed over region. Sutures placed. Complications: none Disposition Pt a/o, resting, breathing quietly, extremities neurovascularly intact. Incision clean, dry, intact. In stable condition. SURGERY POST-OP NOTE Pre-op diagnosis: femoral hernia Post-op diagnosis: femoral hernia Procedure: Lotheissen McVay femoral hernia repair Surgeons: Dr. Lotheissen, A. Kocoloski MSIV Findings: femoral hernia at right groin region with healthy bowel in the hernial canal Fluids: 1000mL lactated ringers Anesthesia: epidural Estimated Blood Loss: 2 mL Drains:none Specimens: none Complications: none Condition/ Disposition: stable INEDA RECOVERS Ineda is now post op and resting. You arrive at 4 am to do your pre-rounds. What do you want to know? What exam do you want to do? How will your assessment be different? HOSPITAL PROGRESS NOTE Brief note concerning past 24 hours S: Pt did well overnight. Pain controlled with ibuprofen. Passed gas, no bowel movement. O: VS most recent; Exam: CV, Lungs, Abdomen, GU; Incision: clean, dry and intact. Osteopathic: bogginess at right thigh, increased tissue tension of right gluteal muscles. Recent labs. A/P: Pt is a 35 yo f pod#1 s/p right femoral hernia repair and right lower extremity somatic dysfunction. Will continue ibuprofen for pain management. Advance diet as tolerated. Continue to monitor I/O. Performed pedal pump and strain counter strain of both lower extremities, pt tolerated well. PRACTICE!!! Group 1. Hospital Progress Note A Group 2. Procedure Note: http://www.youtube.co m/watch?v=R2_0gOI8 uV0&feature=related Group 3. Hospital Progress Note B ADMISSION ORDERS: ADCA VAN DIMLS Admit to service of… Diagnosis Condition Allergies Vital Signs Activity Nursing Diet IV orders Medications Labs Special ADMIT Attending Physicians Name Unit/Floor: Medical Surgery Medical ICU Surgical ICU If the family physician is not the same as the attending, you can notify the family doctor as a courtesy. Admit: Dr. Duerfedlt, Medical Floor Notify: Dr. D.O. of patients admission DIAGNOSIS List both the diagnosis that caused the patient to be admitted (primary) and any other diagnosis(es) that the patient currently carries Diagnosis: Pneumonia Secondary Diagnoses: Hypertension, DM Type 2 CONDITION General condition of patient at time of admission Stable Guarded Critical Code Status Condition: Stable Code Status: Full Code ALLERGIES Medication, food or environmental allergies Be sure to state the reaction if known Allergies: Penicillin; anaphylaxis VITALS Frequency: How often do you want this patient’s vitals checked Is the patient’s condition one which you may expect a change over a short period of time? Parameters When should the doctor be called Vitals: q shift (every 8 hours) Notify H/O if BP<90/60, >160/110; Pulse >110 or <60; temp>101.5; UOP<35cc/h for>2hours; RR>30 *H/O = house officer ACTIVITY Restrictions on patients activity Bed rest Bedside commode Up Ad Lib Bathroom privileges Ambulation Up in chair Up with nurse assistance Fall precautions Seizure precautions Isolation Activity: Bathroom privileges, Fall Precautions NURSING Any special functions that the nurse must carry out and frequency if applicable I/O’s Oxygen (some docs put this other places too) Pulse oximeter Accu checks Drain and/or catheter instructions Incentive spirometry Wound care Stool guaiac Nursing: O2 2L via NC titrated to maintain sats at or above 95% Continuous pulse oximetry Accuchecks AC and HS Incentive spirometry q 2 hrs while awake DIET State any dietary restrictions NPO (nothing per oral) Ice chips only Clear fluid only Soft Full Thickened liquids 2200 calorie ADA Cardiac Low sodium Low residue Regular diet Diet: 1800 ADA diet IV *THIS SECTION IS RESERVED FOR IV FLUID ADMINISTRATION, NOT FOR IV MEDICATIONS* If ordering IV fluids, state Type of fluid (Normal Saline, Lactated ringer etc) Additives (KCL, MG) Rate in ml/hr at which fluid should be run Endpoint for infusion Maintenance fluids Rehydration Heplock KVO None IV: 0.9 NS KVO MEDICATION List medication specific to patients primary diagnosis List other meds that patient is currently taking that you want continued throughout admission List PRN medications (i.e. pain, fever) Include dose, mode of administration Can vary the dosage or the dosing interval, not both Be sure to include insulin orders here for patients getting Accuchecks EXAMPLE: MEDICATION Levaquin IV 650mg q day Tylenol 500 mg PO q 4-6 hr prn HA or fever greater than 101 Ambien 10 mg PO @ hs prn insomnia Sliding scale coverage of accuchecks using low-dose algorithm Duo-neb treatments q2hr prn SOB or wheeze Duo-neb tx q 6hours Mucinex 600mg PO Q 6hrs Lisinopril 10 mg PO Q day LABS List labs to be done and state when labs should take place Do you want the labs done now or in the morning? Remember admission orders are in place until the attending physician takes over patient care and changes orders. Think of what labs the attending will want to see when he or she evaluates the patient. Blood culture: now Sputum culture: now CBC, chem 7: in am SPECIAL Are there any special orders Ancillary services Radiology Consults Special preps Respiratory therapy to follow ADMISSION ORDERS Admit to: Dr. D on med-surg floor Dx: pneumonia Secondary Diagnoses: HTN, DM type 2 Condition: stable Allergies: Penicillin- anaphylaxis. Vitals: q shift (every 8 hours) If temp is greater than 102° call attending Activity: Bathroom privileges, fall precautions Nursing: O2 2L via NC titrated to maintain sats at or above 95%. Continuous pulse oximetry. Accuchecks AC and HS. Incentive spirometry q 2hrs while awake. ADMISSION ORDER Diet: 1800 ADA IV: 0.9 normal saline to KVO Labs Blood culture: now Sputum culture: now CBC, chem 7: in am Special: Respiratory therapy to follow Medications Levaquin IV 650mg qd Tylenol 500mg PO q 4-6 hr prn HA or fever greater than 101 Ambien 10 mg PO @ hs prn insomnia Sliding scale coverage of accuchecks using low-dose algorithm Duo-neb treatments q2hr prn SOB or wheeze Duo-neb tx q 6hours Mucinex 600mg PO Q 6hrs Lisinopril 10 mg PO Q day NOTE-WRITING RESOURCES Maxwell Quick Medical Reference A must-have!! Only $7.95!! DO or MDPocket is an alternative but is $25.00 How to be a truly EXCELLENT Junior Medical Student 250 Mistakes 3rd year medical students make Clinician’s Pocket Reference (Scut Monkey) www.medfools.com Medfools also has some sample personal statements