SUNYIT Teaching Day 2014 - Iris Gonzalo-Sowle BS, RN

*
Iris Gonzalo-Sowle, BS, RN-BC, ONC, FNP-S
Denise Richard, BSN, FNP-S
* Identify the prevalence of hypogonadism
* Identify the risk factors associated with hypogonadism
* Identify the signs and symptoms of hypogonadism
* Discuss the barriers that prevent men from seeking medical treatment for hypogonadism
* Identify treatment options available for medical management of hypogonadism
* Discuss risks and benefits of current treatment options
* Discuss contraindications of testosterone replacement therapy
* Review potential side effects of testosterone replacement therapy
* Discuss key teaching points to cover to ensure safe use of testosterone replacement therapy
* Implement safety strategies to prevent the misuse of testosterone replacement
*
No commercial support was received for this educational activity.
Primary
* Serum testosterone concentration and/or the sperm count are below normal and the serum
LH and/or FSH concentrations are above normal
Secondary
* Serum testosterone concentration and/or the sperm count are subnormal and the serum LH and/or FSH concentrations are normal or reduced
*
(Snyder, 2013)
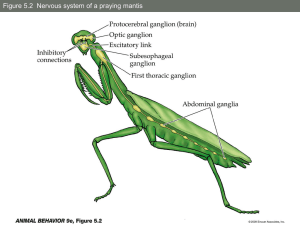
* Hypothalamus produces gonadotropin releasing hormone (GnRH) which stimulates pituitary to produce follicle stimulating hormone and luteinizing hormone.
* Luteinizing hormone stimulates the testes to produce testosterone.
* Primary hypogonadism (primary testicular failure) originates from problem in testes.
*
Secondary hypogonadism indicates problem in hypothalamus or pituitary gland which are what signals testicles to produce testosterone.
*
(Domino,2014)
PRIMARY
HYPOGONADISM
*
Klinefelter syndrome
*
Undescended testicles
*
Mumps orchitis
*
Hemochromatosis
*
Testicular injury
*
Cancer treatment
SECONDARY
HYPOGONADISM
*
Kallmann syndrome
*
Pituitary disorders
*
Inflammatory disease
* HIV
* Medications
* Obesity
* Normal aging
*
(Snyder, 2013)
*
2-4 million men are currently affected
*
12.3 cases per every 1,000 in the
United States
*
481,000 new cases annually in men between the ages of 40-69
*
(Domino, 2014)
* Obesity
* Type II Diabetes Mellitus
* COPD
*
Medications that affect testosterone production or metabolism
* Stress
* Trauma
* Infection
* Radiation therapy
*
Tumors (testes, pituitary, hypothalamus)
*
Chemotherapy
*
Inflammatory disease
* Exposure to environmental endocrine modulators
*
(Domino, 2014)
* Absence or regression of secondary characteristics
*
Anemia
*
Muscle wasting
*
Reduced bone mass or bone mineral density
(osteoporosis)
*
Abdominal adiposity
*
Gynecomastia
*
Sexual dysfunction
*
*
Reduced libido
* Reduced energy and stamina
* Depressed mood
*
Irritability
*
Difficulty concentrating
* Hot flushes
*
Decreased body hair
(McDermott, 2009)
* Puberty (sexual development)
*
Past or present major illnesses and nutritional deficiency
*
Treatment with medications that might affect testosterone levels, such as strong opiate pain medications (e.g. methadone) and strong steroid anti-inflammatory drugs (e.g. prednisone)
*
Sexual problems
* Any major life events that have occurred
*
Family history of similar problems
* Recent changes in body features and breasts
*
Damage to or shrinkage of the testicles
*
* Amount of body hair (underarm and pubic hair)
* Presence of breast enlargement or tenderness
* Size and softness of the testicles
* Penis size
*
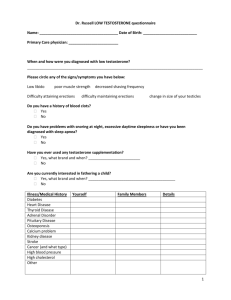
SERUM TESTOSTERONE CONCENTRATION
*
Most important single diagnostic test for male hypogonadism
* Normal range 300-800ng/dl
* Draw lab test at 8:00 am
* Illness, malnutrition, and certain medications can reduce testosterone temporarily, so testing may need to be postponed
*
Abnormal levels should be repeated to confirm true deficiency
*
(Snyder, 2013)
* Semen analysis
* Hormonal/Genetic testing
* MRI of Pituitary (to rule out adenoma)
* Testicular biopsy (rarely provides information that is useful)
*
TREATMENT: Depends on the cause and whether fertility is a concern.
*
Testicular failure: Hormone replacement restores sexual function, muscle strength, and prevents bone loss. Patients note an increase in energy, sexual drive, and feel better about themselves.
*
Pituitary problem: Pituitary hormones can be used to stimulate sperm production and restore fertility.
Testosterone replacement therapy can be used if fertility isn’t an issue.
*
Pituitary tumor: May require surgery, medication, or radiation.
*
(Bhasin et al., 2006)
* Restore sexual function, libido, well being, and behavior
* Produce and maintain virilization
*
Increase muscle strength
*
Optimize bone density and prevent osteoporosis
*
In elderly men, possibly normalize growth hormone levels
*
(Snyder, 2013)
* Injections-safe and effective. Given approximately every 1-2 weeks. Some physicians choose to only give the injection in the office (due to risk of misuse).
*
Patches- (Androderm) applied nightly. Important to rotate sites to prevent skin reactions. Do not apply to scrotom.
*
Gels-(AndroGel/Testim) rub into skin of lower abdomen, upper arm or shoulder. Less skin reactions than the patches.
Can’t shower or bathe for several hours after application.
Must avoid skin to skin contact or cover the area until gel is completely dry. Women and children should avoid contact with unwashed or unclothed area where gel has been applied. Gels are flammable and must be dry before going near an open flame.
*
(Snyder, 2013)
* Buccal tablet: Applied twice daily and adheres to a depression in the gum above the upper incisors. Releases testosterone across buccal mucosa into systemic circulation.
* Testosterone pellet: Three to six 75 mg testosterone pellets are implanted into subdermal fat of buttocks, lower abdominal wall, or thigh with a trocar under sterile conditions using local anesthesia every three to six months. Not routinely recommended.
*
(Snyder, 2013)
(Snyder, 2013)
* Misuse/abuse of testosterone amongst athletes, bodybuilders, weight lifters, and others to enhance athletic performance or physique
* Considered a controlled substance in NYS
(class II)
* Prescription cannot be sent electronically
* Paper script required
* No refills allowed
*
Testosterone therapy is contraindicated in:
*
Breast or prostate cancer
*
Enlarged prostate
*
Obstructive sleep apnea (if untreated)
*
Class III or IV heart failure
*
Smokers (erythrocytosis)
*
(Bhasin et al., 2006)
* Increased PSA
* Mood swings
* High blood pressure
* Skin irritation at site of application
*
Prostatic hyperplasia
* Prostate Cancer
* Erythrocytosis
* Decreased sperm count
* Lower extremity edema
*
Heart failure
*
Blood clots
*
(McDermott,2009)
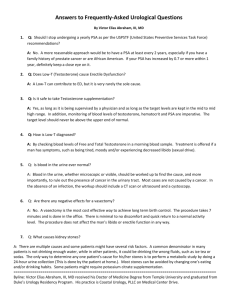
Digital rectal exam, PSA, CBC, done prior to initiation of testosterone therapy in:
* Any man over the age of 50
* Any man over the age of 40 with family history of Prostate cancer or is African
American
*
(Snyder, 2013)
*
Testosterone levels and CBC checked every 3 months for first year and then every 6 months if stable.
*
Annual digital rectal exam and PSA for as long as the patient remains on testosterone replacement therapy.
* For patients with a history of osteoporosis or past bone fractures, a bone mineral density testing
(DEXA scan) should be done every one to two years while receiving testosterone treatment.
*
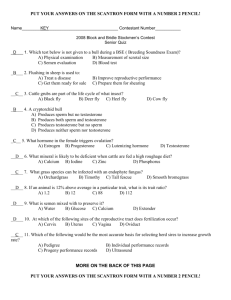
1. Risk factors for hypogonadism include all of the following except a) obesity b) age c) inflammatory disease d) enlarged prostate
2. Serum testosterone levels should be drawn at what time?
a) 5:00 pm b) any time c)
11:00 am d) 8:00 am
3. Testosterone therapy is contraindicated in: a) Class III or IV heart failure b) Enlarged prostate c)
Diabetes d) Hypertension
*
4. According to current clinical guidelines which tests should be performed prior to the initiation of testosterone therapy?
a)
CBC and PSA b)
CBC, COMP and PSA c) digital rectal exam, PSA and CBC d) digital rectal exam and PSA
5. Side effects of testosterone therapy include all of the following except: a) hypotension b) elevated PSA level c) localized skin irritation d) mood swings
6. Which teaching point is not indicated when providing education regarding testosterone gel application?
a)
Gels are flammable and should be allowed to dry completely before exposure to open flames.
b)
To reduce the risk of skin irritation gels should be applied to bilateral ankles.
c)
Exposure to skin areas where testosterone gel has been applied should be avoided in women and children.
d)
Gel should be applied after bathing or showering.
*
Bhasin, S., Cunningham, G. R., Hayes, F. J., Matsumoto, A. M., Snyder, P.
J.,Swerdloff, R. S., & Montori, V. M. (2006). Testosterone therapy in adult men with androgen deficiency syndromes: An endocrine society clinical practice guideline. The Journal of Clinical
Endocrinology & Metabolism, 91(6), 1995-2010
Domino, F. J. (2014). The 5 minute clinical consult. (2nd ed., pp. 1206-
1207). Philadelphia, PA: Lippincott Williams & Wilkins.
Endocrine Society. (2014). Testosterone therapy in men. Retrieved from http://www.hormone.org/patient-guides/2010/testosteronetherapy-in-men
Jackson, G. (2012). Late onset hypogonadism in males-think of it-act on it.
International Journal of Clinical Practice, 66(2), 115-116. doi:10.1111/j.1742-1241.2011.02865.x
*
McDermott, M. (2009). Endocrine secrets. (5th ed.).
Philadelphia, PA: Mosby Elsevier.
Snyder, P. J. (2013, February 11). Testosterone treatment of
male hypogonadism. Retrieved from www.uptodate.com.
Snyder, P. J. (2013, January 18). Clinical features and diagnosis
of male hypogonadism. Retrieved from www.uptodate.com
Vigen, R., O'Donnell, C. I., Baron, A. E., Grunwald, G. K.,
Maddox, T. M., Bradley, S. M., … Ho, P. M. (2013).
Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA, 310(17), 1829-
1836. doi: 10.1001/jama.2013.280386
*