Case caboxy
advertisement

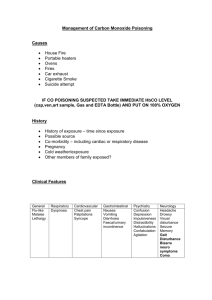
Deadly Air Case 23 yo F BIBEMS s/p suicide attempt. Patient was found unconscious in bathtub after making comments about suicidal ideation. She was foaming at the mouth, with empty bottles of Advil PM and Tylenol PM, and a charcoal grill lit nearby. Family members report recent EtOH use. EMS Report EMS reports patient is confused but able to move all extremities and follow commands. SpO2 measured in the field to be 90%. Carboxyhemoglobin level measured at 50%. Patient was given 100% O2 at 15 LPM by NRB and transported to Elmhurst hospital. Initial Hospital Workup Carboxyhemoglobin level measured at 1:30 am at Elmhurst hospital to be 44%. Measured again 45 mins later to be 11.7%. Patient was transferred to Jacobi Hospital by EMS, arrived at 4:30 am. History Patient did not remember events leading up to her arrival at Jacobi, and did not want to talk about what she did remember from earlier. Pt only c/o some mild SOB. Pt denied any chest pain, headache, body aches, dizziness or nausea. History PmHx: TMJ PsHx: none Meds: metformin (self-prescribed) All: NKDA FamHx: breast cancer, DM, Alzheimer’s SocHx: occ EtOH, pt denies smoking, drug use Vitals Temp: 98.3° F HR: 69 RR: 20 BP: 121/84 SpO2: 94% With an SpO2 of 94%, is she fine? Carbon monoxide diffuses rapidly across the pulmonary capillary membrane and binds to the iron component of hemoglobin with 240x the affinity of oxygen. The standard pulse oximeter cannot distinguish between carboxyhemoglobin and oxyhemoglobin, and will measure a falsely elevated level. Physical Exam Gen: Pt awake & alert in bed, slightly confused, NAD HEENT: NCAT, PERRL, EOMI, MMM, anicteric sclera, clear conjunctivae CV: RRR, normal S1/S2, no chest wall tenderness, no M/R/G LUNGS: slightly shallow breathing, CTA bilat, no wheezes/crackles, equal respiratory effort Physical Exam ABD: soft, NT/ND, +BS, no organomegaly EXT: 2+ pulses x4, no track marks, no edema Neuro: A&Ox3, but no memory of events leading up to incident, able to recall 3/3 words, CN IIXII grossly intact, no facial droop, EOMI, no gait abnormalities, reflexes 2+ in all extremities Labs 13.4 226 17.2 44 141 109 Calcium: 7.8 troponin I: 5.164 CK: 1133 91 57 EtOH level: < 10 ASA level: < 1 Tylenol level: < 10 51 PT: 9.8 PTT: 20.1 INR: 1.0 βhcG: neg 13 4.3 23.5 0.7 89 6.4 3.9 0.3 Complications of CO Poisoning Acute myocardial injury is common in cases of CO poisoning, and is associated with an increased long-term mortality. In a 2005 cohort study by Satran et al, 230 patients exposed to varying levels of carbon monoxide showed ischemic changes on EKGs in 30%, biomarkers diagnostic of myocardial injury in 35% and in-hospital mortality in 5% (12 patients, 8 from anoxic brain injury). Ten year follow-up in 2006 showed an overall mortality of 24% in these patients, with myocardial injury (as determined by elevated biomarkers or ischemic EKG changes) being a significant predictor of mortality (adjusted hazard ratio of 2.1). Complications of CO Poisoning Neurologic sequelae are the most frequent form of morbidity in CO poisoning, from hypoxic brain injury and white matter demyelination. Necrosis of the globus pallidus is the most common site of injury. Delayed neurologic sequelae have been seen weeks to months after apparent recovery, marked by cognitive deficits, personality changes, movement disorders and focal neurologic deficits. (Lo et al. 2007) Unenhanced CT scan about 16 hours after injury shows bilaterally symmetric low attenuation lesions in the cerebellum (blue arrows), globus pallidus (red arrows) and caudate nuclei (white arrows). The patient was in a house fire. (learningradiology.com) Now What? Initial Management of CO Poisoning: Prompt removal of patient from environment ABCs, consider intubation High-flow O2 Management of co-ingestion +/- Hyperbaric oxygen treatment Hyperbaric Oxygen Hyperbaric oxygen therapy exposes patients to 100% oxygen under supra-atmospheric pressure. This decreases the half-life of COHb from approx 90 mins on 100% O2 to 30 mins on hyperbaric O2. Indications for initiation of hyperbaric therapy: COHb level > 25% evidence of ongoing end-organ ischemia loss of consciousness pregnant women with COHb > 20% of evidence of fetal distress Greatest benefit is seen when treatment is given early, no benefit has been shown when patients are treated > 12hrs after exposure Hyperbaric Oxygen Weaver L, Hopkins R, Chan K, et al. Hyperbaric oxygen for acute carbon monoxide poisoning. New England Journal of Medicine 2002; 347(12): 1057. Single-center, double-blind trial that randomly assigned 152 patients symptomatic acute carbon monoxide poisoning to either three hyperbaric oxygen treatments or one normobaric oxygen treatment plus two sessions of normobaric room air. Neuropsychological tests were administered immediately after the sessions and 2 weeks, 6 weeks, 6 months and 1 year later. The primary outcome measured was cognitive sequelae 6 weeks after treatment. The trial was stopped early, with 76 patients in each group. Cognitive sequelae were less frequent in the hyperbaric oxygen treatment group (25.0% vs 46.1%). Hyperbaric Oxygen 5 ½ hours after exposure, the patient was given 2.8 ATM for 46 minutes, given in two dives of 23 minutes each. After the treatments, she reported improved breathing, with less difficulty taking deep breaths. Remaining Hospital Course Labs improved: repeat WBC at 6:30 am: 9.4 repeat cardiac enzymes: 5:30 pm: Troponin I: 4.200 CK: 428 2:15 am: Troponin I: 1.419 Pt was admitted to the burn unit at 8:00 am. Labs continued to trend down, and she was transferred to the psych unit two days later. Take-Home Points • Carbon monoxide diffuses rapidly across the pulmonary capillary membrane and binds to hemoglobin with very high affinity, decreasing its ability to transport oxygen. • Clinical findings of carbon monoxide poisoning are largely nonspecific but sequelae may include myocardial ischemia and delayed cognitive deficits. • Obtain a COHb level whenever CO poisoning is suspected, because SpO2 will give a falsely elevated level. • The most important interventions are airway control, prompt administration of O2 +/- hyperbaric oxygen treatment. References Clardy P, Manaker S, Perry H. Carbon monoxide poisoning. UpToDate, Traub S, UpToDate, 2013. Crawford Mechem C, Manaker S. Hyperbaric oxygen therapy. UpToDate, Traub S, UpToDate 2013. Henry S, Satran D, Lindgren B, et al. Myocardial injury and long-term mortality following moderate to severe carbon monoxide poisoning. JAMA 2006; 295(4): 398-402. Juurlink D, Buckley N, Stanbrook M, et al. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev 2005; :CD002041. Kwon OY, Chung SP, Ha YR, et al. Delayed postanoxic encephalopathy after carbon monoxide poisoning. Emerg Med J 2004; 21:250. Lo C, Chen S, Lee K, et al. Brain injury after acute carbon monoxide poisoning: early and late complications. Neuroradiology 2007; 189(4): W205-11. Satran D, Henry CR, Adkinson C, et al. Cardiovascular manifestations of moderate to severe carbon monoxide poisoning. J Am Coll Cardiology 2005. 45(9): 1513-6. Weaver L, Hopkins R, Chan K, et al. Hyperbaric oxygen for acute carbon monoxide poisoning. New England Journal of Medicine 2002; 347(12): 1057. Weaver L, Valentine K and Hopkins R. Carbon monoxide poisoning: risk factors for cognitive sequelae and the role of hyperbaric oxygen. American Journal of Respiratory and Critical Care Medicine 2007; 176(5):491-7.