Mycology - UAB School of Optometry
Mycology
Dental / Optometry Fundamentals II
Stephen A. Moser, Ph.D.
10/26/2011
1
Epidemiology
Geography
Endemic mycoses
Worldwide mycoses
Transmission of infection
Respiratory inhalation (systemic mycoses)
Cutaneous inoculation (sporotrichosis)
Systemic invasion by opportunistic normal flora
(candidiasis)
Contact with infected hosts (dermatophytoses)
2
Epidemiology (Cont.)
Risk factors and manifestations of disease
True pathogens versus opportunists
Environmental risk factors for systemic fungal disease
• Location and travel
• Occupation
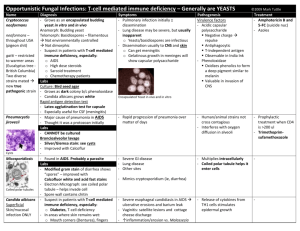
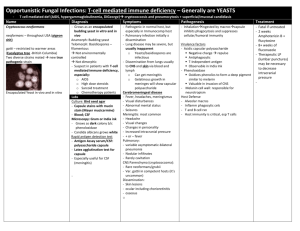
Host defenses and susceptibility to systemic fungal disease (CMI most important)
• Congenital and acquired T cell deficiencies (including
AIDS)
• Immunosuppression (transplants and malignancies)
• Diabetes mellitus
3
Endemic Distribution for Blastomycosis
4
General Characteristics
Aerobic - obligate or facultative
Eukaryotic : membrane bound nucleus and cytoplasmic organelles (may be multinucleate)
Achlorophyllous
Morphology (unicellular or multicellular)
Saprophytic (heterotrophic)
5
Characteristics of Fungal Cells
Cell wall : multilayered polysaccharide
Cellulose, glucans, mannans, chitin, polypeptides
Absence of teichoic acids, peptidoglycan, LPS
Cell membrane
Phospholipid bilayer
Ergosterol (relate to chemotherapy)
Cytoplasm - typical eukaryotic organelles
Nucleus - either uninucleate or multinucleate
6
Characteristics of Fungal Cells
Capsule
Present in some species (e.G. Cryptococcus neoformans )
Amorphous polysaccharide coating
Functions and activities
Antiphagocytic
Antigenic
7
Characteristics of Fungal Cells
Growth forms
Yeast - unicellular fungi which reproduce by budding ( Cryptococcus )
Mold - hyphae (mycelium)
Septate hyphae ( Aspergillus )
Non-septate, coenocytic hyphae ( Mucor )
Pseudohyphae ( Candida albicans )
Thermal dimorphism
8
Differences Between Bacteria and Fungi
PROPERTY FUNGI BACTERIA
Cell diameter
Nucleus
5-50 microns
Eukaryotic
1-5 microns prokaryotic absent Cytoplasmic organelles Present
Cell membrane sterols present (ergosterol)
Cell wall
Metabolism
Thermal dimorphism chitin, glucans, mannans, peptides
Mainly aerobes, facultative anaerobes
Common in many pathogenic species absent (except
Mycoplasma) teichoic acids, peptidoglycan, LPS obligate and facultative aerobes and anaerobes absent
9
Examples of Yeast &
Pseudohyphae
Blastoconidia
Pseudohypha
10
Blastomyces dermatitidis Thermal
Dimorphism
11
Example of True Septate Hyphae
12
Non-septate Hyphae
13
Asexual Reproduction
Conidia (spores) – asexual structures
Blastospores – formed by budding yeasts
( Blastomyces )
Chlamydospores – terminal or intercalary cells with thick walls ( Candida albicans )
Arthrospores – formed by fragmentation of hyphae ( Coccidioides immitis )
Sproangiospores – formed in sporangia by cleavage ( Rhizopus )
14
Classification Based on
Sexual Phase
Ascomycetes : Aspergillus, Histoplasma ,
Blastomyces , Dermatophytes
Basidiomycetes : Cryptococcus ,
Mushrooms
Zygomycetes : Order Mucorales Mucor ,
Rhizopus
Deuteromycetes (Fungi Imperfecti):
Sporothrix , Coccidioides, Candida
15
Clinical Types of Fungal
Infections
TYPE
1. Superficial
2. Cutaneous
DISEASE
Pityriasis versicolor
Ringworm (Tinea)
Candidiasis
ORGANISM
Malassezia furfur
Trichophyton species
Candida albicans and others
3. Subcutaneous
4. Systemic
Sporotrichosis
Pathogenic Fungi
Histoplasmosis
Blastomycosis
Coccidioidomycosis
Paracoccidioidomycosis
Opportunistic Fungi
Aspergillosis
Cryptococcosis
Candidiasis
Zygomycosis
Sporothrix schenckii
Histoplasma capsulatum
Blastomyces dermatitidis
Coccidioides immitis
Paracoccidioides brasiliensis
Aspergillus fumigatus and others
Cryptococcus neoformans
Candida albicans and others
Mucor and Rhizopus species
16
Routes of Infection
Inhalation of spores – major factor
Inoculation of spores into skin
Disease by normal flora in compromised host (Candida)
Hypersensitivity
Contact with infected host
(Dermatophytes)
Mycotoxins
17
Laboratory Diagnosis of Fungal
Infections
Microscopic Examination of tissues and body fluids
Gram stain
Giemsa
India Ink
Potassium hydroxide (KOH) wet prep
Hematoxylin and Eosin stain
Periodic-Acid Schiff stain (PAS)
Gomori-Methenamine Silver stain (GMS)
Mucicarmine or Alcian Blue stain
18
Budding Yeast - Gram Stain
Staphylococcus
Candida
19
Encapsulated Yeast - India Ink
20
KOH Prep - Broad-base Budding Yeast
21
H&E Stain - Budding Yeasts
22
GMS Stain - Septate Hyphae
23
Mucicarmine Stain C. neoformans
24
Histopathological Response to
Fungal Infection
Acute pyogenic abscess (Candida)
Chronic granuloma formation
(Histoplasma)
Chronic, localized dermal inflammation
(Dermatophytes)
Mixed pyogenic and granulomatous inflammation (Blastomyces)
Blood vessel invasion with thrombosis and infarction (Mucor, Aspergillus)
Hypersensitivity without tissue reaction
(allergic bronchopulmonary aspergillosis)
25
Fungal Cultures
Utilize Sabouraud agar with antibiotics
Identification criteria
Temperature of growth
Rate of growth
Colonial and microscopic morphology
Sporulation pattern
Biochemical reactions (yeast)
26
Fungal Serology
Generally poor and not as useful as in other pathogens such as viruses and bacteria, with some exceptions.
Cryptococcal antigen by latex agglutination: serum and CSF.
Coccidioides - early IgM response is useful for identification of acute primary disease -
CSF IgG prognostic value.
Skin tests for DTH - problems:
Cross-reactivity.
High positive rate in endemic areas.
27
Candidiasis
Clinical manifestations
Mucosal
• Vaginitis
• Esophagitis
• Oral thrush
Cutaneous
Chronic mucocutaneous
Systemic
• Fungemia
• Hepato-spleenic
• Endophthalmitis
• Renal
Urinary tract
28
Oral Candidiasis
29
Wet Mount - Candidiasis
30
Mucocutaneous
Candidiasis
31
Candida sp. Tissue GMS Stain
32
Aspergillosis
Clinical manifestations
Pneumonia
Aspergilloma
Allergic bronchopulmonary
Disseminated multiorgan involvement
33
Aspergilloma
34
Allergic Bronchopulmonary Aspergillosis
35
CNS Aspergillosis
36
Aspergillus sp – GMS Stain
37
Zygomycosis
Clinical manifestations
Sinusitis
Rhinocerebral
Pulmonary
Renal
38
Rhinocerebral
Mucormycosis in Diabetic
Ketoacidosis
39
Postmortem – Rhinocerebral Mucormycosis
40
Non-septate Branching Hyphae (PAS)
41
Histoplasmosis
Clinical manifestations
Most cases mild or sub-clinical pulmonary disease
• Dissemination appears to be common
Pneumonia
Chronic progressive pulmonary (cavitary)
Histoplasmoma
Disseminated
42
Histoplasmosis
– Calcified
Lesions
43
Histoplasmosis- GMS
44
Histoplasmosis – Bone Marrow
H. capsulatum
Histiocyte
45
Histoplasma capsulatum
In vitro In vivo
46
Presumed Ocular Histoplasmosis
Thought to be a late stage of primary histoplasmosis.
Causes abnormal blood vessels – scar tissue.
Organism has not been found in eye.
Treated with laser surgery.
47
Risk Factors for Endogenous
Endophthalmitis
Candidia species Central venous lines, neutropenia, abdominal surgery, intravenous drug abuse, broad-spectrum antibiotics
Aspergillus species Neutropenia, endocarditis, intravenous drug abuse, pulmonary disease being treated with high dose steroids, organ and stem cell transplant.
H. capsulatum
C. immitis
B. dermatitidis
C. neoformans
May accompany disseminated disease
Fusarium species Neutopenia, intravenous drug abuse
48
Fungal Keratitis
49
Chemotherapy
FDA approved
Polyenes (Amphotericin B, lipid encapsulated forms)
Azoles (fluconazole, itraconazole, ketoconazole, voriconazole)
Echinocandin (Caspofungin, Micafungin, Anidulafungin)
Nucleoside derivatives (5-flurocytosine)
Allyamines (Terbinafine)
Microtubule disruption (Griseofulvin)
Investigational
Nikkomycins (chitin synthase inhibitors)
Echinocandin/pnemocandin/lipopeptide class (inhibit glycan synthesis)
50
Antifungal Drugs for Systemic
Mycoses - Amphotericin B
Mode of Action
Binds to ergosterol, increases membrane permeability resulting in leakage of cytoplasmic components and cell death – Fungicidal
Spectrum of Activity
Candida, Crypto, Aspergillus, Histo, Blasto, Cocci, etc
Limitations
Nephrotoxicity
51
Antifungal Drugs for Systemic
Mycoses - Fluconazole
Mode of Action
Prevents ergosterol synthesis by inhibiting the C-14 demethylation step (cytochrome P-450 rx)
Fungistatic
Spectrum of Activity
Candida, Crypto, Trichsporonosis, dermatophytes
Limitations
Resistance in some Candida sp – krusei and glabrata
Not effective for non-dermatophyte moulds.
52
Antifungal Drugs for Systemic
Mycoses -Echinocandins
Mode of Action
Prevents synthesis of beta 1,3-glucan required for cell wall.
Fungistatic
Spectrum of activity
Aspergillus, Candida
NOT effective against Cryptococcus, zygomycetes.
53
Early Diagnosis of Invasive
Fungal Infections
•
•
•
•
Obstacles
Because of Immunosuppression typical signs and symptoms of infection are frequently absent
Few clinical features are uniquely specific for systemic fungal infection
Sputum and blood cultures are frequently negative
Invasive procedures
–
May be necessary for definitive diagnosis
–
Are often complicated in severely immunocompromised patient
54
Early Diagnosis of Invasive
Fungal Infections (Continued)
Benefits
Early diagnosis permits selection of a therapy of maximal effectiveness
Early intervention with antifungal therapy may help decrease the high mortality rate associated with serious systemic mycoses
55
Major Areas Covered
How fungi differ from bacteria
The major fungal infections
The epidemiology of fungal infections
Pathology of fungal infections
Mechanism of action of antifungal agents
56