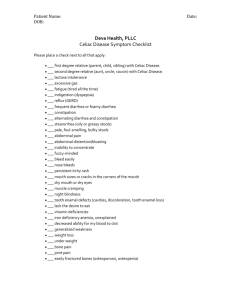
Celiac disease
advertisement

MALABSORPTİON SYNDROME Prof. Dr. Tufan KUTLU Malabsorption Malabsorption can be defined as subnormal intestinal absorption of dietary constituents, and thus excessive loss of nutrients in the stool; it may be due to a digestive defect, a mucosal abnormality, or lymphatic obstruction.” Characteres of stools in childhood 0-6 months Breast milk 1-12/day yellow to braun pH: 5 Formula 1-7/day yellow to braun pH: 7 6 months-1 year 2-3/day braun >1 year as adult 5-10g/kg/day Diarrhea Increase in the number of stools or a decrease in their consistency Constipation Decrease in the number of stools or an increase in their consistency Malabsorption syndrome Chronic diarrhea Protuberant abdomen Vomiting Weigth loss Short stature Anorexia.. Digestion of carbohydrates Carbohydrates Enzymes Starch 50 % Salivary amylase Sucrose 20-40 % Pancreatic amylase Lactose 20-40 % Disaccharidase Monosaccharides Glycose Galactose Fructose Sucrase-isomaltase Glucoamylase Lactase Carbohydrate malabsorption Sucrase-izomaltase deficiency Primary lactase deficiency Late onset lactase deficiency Glycose-galactose malabsorption Secondary disaccharidase deficiency Digestion of proteins Gastric asid Enterokinase Pancreatic proteases Protein malabsorption Kongenital enterokinase deficiency Pancreatic enzyme deficiency Aminoacid transport defects Digestion of lipids Gastric lipase Pancreatic Bile lipase acids Absorption Steatorrhea Pancreatic deficiency Congenital Cystic fibrosis Shwachman-Diamond syndrome Johanson-Blizzard syndrome Pearson’s syndrome Acquired Chronic pancreatitis Steatorrhea Bile acid deficiency Diminution of synthesis in the liver Bile duct atresia İncrease of bacterial deconjugation Diminution of ileal reabsorption (Crohn’s disease, ileal resection, short gut) Drugs (cholestyramine) Steatorrhea Abetalipoproteinemia Retinitis pigmentosa Neurologic symptoms Achantocytosis Cholesterol very low Treatment: no fat, MCT, vitamine ADEK supplementation Hypobetalipoproteinemia Steatorrhea Intestinal lymphangiectasia Hypoalbuminemia Lymphopenia Edema Mucosal absorption disorders Celiac disease Short gut Gastrointestinal diseases associated with maldigestion and malabsorption Intraluminal digestion Stomach Pernicious anemia Gastrointestinal diseases associated with maldigestion and malabsorption Intraluminal digestion Pankreas Cystic fibrosis Shwachman-Diamond syndrome Acute/chronic pancreatitis Tyripsinogen deficiency Lipase deficiency Amylase deficiency Gastrointestinal diseases associated with maldigestion and malabsorption Intraluminal digestion Liver İntestine Cholestasis syndromes Enterokinase deficiency Short bowel syndrome Gastrointestinal diseases associated with maldigestion and malabsorption Digestion at the enterocyte membrane Congenital disaccharidase deficiency Acquired/late-onset disaccharidase deficiency Lactase Sucrase-isomaltase Trehalase Lactase Sucrase-isomaltase Glucoamylase Gastrointestinal diseases associated with maldigestion and malabsorption Enterocyte absorption Glucose-galactose malabsorption Congenital chloride diarrhea Abetalipoproteinemia Hypobetalipoproteinemia Celiac disease Short bowel syndrome Milk/soy protein intolerance Whipple’s disease Inflamatory bowel disease Infections Acrodermatitis enteropathica Gastrointestinal diseases associated with maldigestion and malabsorption Uptake into blood and lymph Miscellaneus disorders Congestive heart failure Constrictive pericarditis Intestinal lymphangiectasia Intestinal lymphoma Carsinoid syndrome Immun deficiency syndromes Allergic gastroenteropathy Eosinophilic gastroenteropathy Drugs Presenting symptoms Chronic diarrhea Rectal bleeding Meteorismus Abdominal pain Weigth loss Failure to thrive Constipation Tenesmus Vomiting Anorexia Pallor Weakness Fever Geophagia Physical findings Weigth loss Short stature Protuberant abdomen Ascites Edema Hepatomegaly Splenomegaly Clubbing Pallor Gingival hipertrophy Aphthous mouth ulcers Arthritis Eritema nodosum Uveitis, episcleritis Diagnostic studies in the evaluation of maldigestion and malabsorption I Stool examination for blood, leukocytes, reducing substances, C. difficile toxin, ova and parasites and cultures for infectious bacterial pathogens Complete blood count, serum electrolytes, blood urea nitrogen, creatinine, calcium, phosphorus, albumin, total protein Urinalysis and culture Diagnostic studies in the evaluation of maldigestion and malabsorption II Sweat chloride test Breath analysis D-Xylose test Serum carotene, folate, B12, and iron levels Fecal alpha-1-antitrypsin level Fecal fat studies or coefficient of fat absorption studies Diagnostic studies in the evaluation of maldigestion and malabsorption III Fat-soluble vitamin levels: A, D, E, K Contrast radiographic studies: upper gastrointestinal series, or barium enema Gastroscopie/colonoscopie Small intestinal biopsy for histology, and mucosal enzyme determination Antibodies Anti-gliadin ab Anti-endomisium ab Anti-transglutaminase ab Autoantibody p-ANCA, ASCA Sweat test indications Failure to thrive Chronic diarrhea Rectal prolapsus Neonatal cholestasis Cirrhosis Pancreatitis Recurrent pulmonary infections Nasal polyps Meconium ileus Positive family history Disorders with sweat test positivity Cystic fibrosis Adrenal insufficiency Protein-calorie malnutrition Neonatal cholestasis G-6-PD deficiency Pancreatitis Glycogen storage diseases Hypoparathyroidism Hypothyroidism Nephrogenic diabetes insipidus Ectodermal dysplasia Causes of villous atrophy in infants and children Peptic duodenitis Celiac disease Acute gastroenteritis Cow’s milk and soy protein intolerance Eosinophilic gastroenteritis Immunodeficiency: congenital, acquired, AIDS Crohn’s disease Protein-calorie malnutrition Total parenteral nutrition Bacterial overgrowth or stasis Microvillus inclusion disease Autoimmune enteropathy Giardiasis Relative value of a small-bowel biopsy Diagnostic biopsy Celiac disease Congenital microvillous atrophy Immunodeficiency Eosinophilic gastroenteritis Crohn’s disease Abetalipoproteinemia Chylomicron retention disease Lymphangiectasia (mucosal type) Diagnostic or non diagnostic Autoimmun enteropathy Crohn’s disease Tropical sprue Isolated IgA deficiency Lymphangiectasia Giardiasis Nonspesific changes Milk or soy protein intolerance Intractable diarrhea AIDS Malnutrition Drug and radiation-induced lesions Contaminated small-bowel syndrome Graft-versus-host disease Specialized studies Schilling test Serum/urine bile acid determination Endoscopic retrograde pancreatography Provocative pancreatic secretion testing Causes of chronic diarrhea in neonates Cow’s or soy milk intolerance Glucose-galactose malabsorption Sucrase-isomaltase deficiency Congenital lactase deficiency Necrotizing enterocolitis Infections Cystic fibrosis Shwachman disease Abetalipoproteinemia Chylomicron retention disease Primary immunodeficiency Short bowel syndrome Intestinal lymphangiectasia Acrodermatitis enteropathica Microvillous inclusion disease Congenital chloride diarrhea Congenital bile salt malabsorption Congenital enterokinase deficiency CELİAC DİSEASE Celiac disease Celiac disease (CD), also called glutensensitive enteropathy, is a permanent intestinal intolerance to dietary wheat gliadin and related proteins that produces mucosal lesions in genetically susceptible individuals Historical background Gallen, 250 AD, described celiac disease Samuel Gee, 1888, first description of CD Dicke, 1950, role of wheat and rye flour in the pathogenesis of CD Paulley, 1954, first biopsy (surgical) Sakula ve Shiner, 1957, peroral intestinal biopsy ESPGHAN criteria, 1970, 1979, 1990, 2012 Genetics of celiac disease Prevalence of CD among first-degree relatives of CD patients is approximately 10 % 75 % of monozygotic twins have been found concordant with the disaese Association of CD (95 % in CD, 20-30 % in controls) with the HLA DQ α/β heterodimer encoded by the DQA1*0501 and the DQB1*0201 genes Epidemiology The reported prevalence of symptomatic CD is 1 in 1000 live births (1/250 – 1/4000) The prevalence of asymptomatic CD is 1/200 (1/100-1/300) Pathogenesis CD is an immunologically mediated small intestinal enteropathy. The mucosal lesions shows features suggesting both humoral- and cell-mediated immunologic overstimulation. All the evidence available suggests a glutendependent activation of mucosal immunity in CD. Pathology Partial to total villous atrophy Elongated crypts Increased mitotic index in the crypts Increased intraepitelial lymphocytes Infiltrations of plasma cells and lymphocytes as well as mast cells, eosinophils, and basophils in the lamina propria Clinical presentation Vomiting Anorexia Chronic diarrhea Weigth loss Irritability Failure to thrive Abdominal distention Muscle wasting Clinical presentation Short stature Delayed puberty Anemia Rickets-osteomalasia Joint complaints Cryptogenetic hepatitis Epilepsy Cerrahpaşa experience; Age at the time of diagnosis Age (year) n % <2 >4 >10 24 48 12 28.6 57.1 14.3 Symptoms Diarrhea: 85,5 % Abdominal distention: 41 % Weigth loss: 27,7 % Failure to thrive: 20,5 % Vomiting: 19,3 % Anorexia: 18,1 % Abdominal pain: 13,2 % Constipation: 3,6 % Physical findings Height < 3. p. : 60,7 % Weight < 3. p. : 66,7 % Hepatomegaly: 38,1 % Clubbing: 17,9 % Ascites: 8,3 % Edema: 4,8 % Laboratory findings Anemia: 50 % Trombocytosis: 64.7 % Low Fe: 60 % Low ferritin: 78,4 % Associated diseases Dermatitis herpetiformis Down syndrome Autoimmune diseases Thyroid diseases Addison’s disease Sarcoidosis Insulin-dependent diabetes mellitus Autoimmune hepatitis Alopecia… Down syndrome-celiac disease The prevalence of celiac diseae in Down syndrome: 1 - 18 % Insulin-dependent diabetes mellitusceliac disease The prevalence of celiac diseae in insulindependent diabetes mellitus: 1,5 - 8 % Laboratory findings Anemia Trombocytosis Folic acid deficiency B12 deficiency Hypoproteinemia Hypertransaminasemia Diagnosis Antigliadin antibodies Anti-endomysium antibodies Anti tissue transglutaminase antibodies Small intestinal biopsy Response to gluten-free diet Diagnosis ESPGHAN criteria Finding of villous atrophy with hyperplasia of the crypts and abnormal surface epithelium, while the patient eating adequate amounts of gluten. A full clinical remission after witdrawal of gluten from the diet. The finding of circulating antibodies to gliadin and endomysium at the time of diagnosis and their disappearence on a gluten-free diet, adds weight to the diagnosis. Diagnosis ESPGHAN criteria A control biopsy to verify the consequences on the mucosal architecture of the gluten-free diet is considered mandatory only in patients with equivocal clinical response to the diet and in patients asymptomatic at first presentation. Diagnosis Gluten challenge is not considered mandatory, except under unusual circumstances. These include situations where there is doupt about the initial diagnosis, for exemple when no initial biopsy was done, or when the biopsy specimen was inadequate or not typical of CD. The diagnostic challenge may be necessary to exclude other causes that could be responsible for the flat mucosa. Therapy Gluten-free diet; wheat, rye, barley and oats should be excluded Iron Folic acid Lactose-free diet Therapy Gluten-free diet Gluten-free bread Celiac disease-cancer It has been demonstrated that the risk of developing small intestinal lymphoma is increased in patients taking a reduced-gluten or a normal diet, whereas for patients who have taken a strict gluten-free diet for 5 years or more the risk of developing malignancies over all sites is not increased when compared with the general population. Celiac disease All the present evidence strongly supports the view that restriction of gliadin should be complete and for life for all patients.