Cystic Fibrosis Paper
advertisement

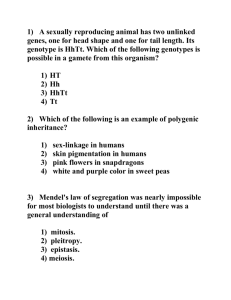
INTRODUCTION Cystic fibrosis (CF) is one of the most common life-shortening disorders in North America (1). It is relatively simple to diagnose. It is even simpler to understand, yet there is still no cure. Patients diagnosed with CF require daily therapy. The lungs are the most severely affected organ in CF patients, but this disease also affects the digestive system, liver, and reproductive organs (2). Medical treatments have greatly improved over the last two decades and as a result life quality and expectancy have increased accordingly. Nutritional therapy has made equally great strides in order to ensure the best quality of life for those diagnosed with CF (1). Even though it is a life-threatening disease, the medical innovations are making living with it easier every day. PREVELENCE AND ETIOLOGY Cystic Fibrosis is a chronic genetic disorder and occurs once in every 3,500 births. The disease is most prevalent in Caucasian populations (3). CF is passed down through both parents as a recessive gene. Since the defect must be passed on from both parents, there is a twenty-five percent chance that each child the couple has will develop cystic fibrosis. The defect is in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) protein. This then causes over 1,400 genetic mutations associated with the disease (4). The most common mutation resulting in the malfunction of the CFTR is the deletion of the codon for phenylalanine at position 508. This mutation is referred to as ΔF508 (4). COURSE OF DISEASE Cause 1 The mutation result in the cell’s inability to move chloride ions out of the cell. Water is then retained, and forms a thick, sticky mucus outside of the cell. Cystic Fibrosis leads to abnormal function of epithelial cells. Mostly, the exocrine glands within these epithelial tissues. Some organs that have exocrine glands include: pancreas, lungs, breasts, skin, cervix, testicles, intestines, stomach and the mouth. All of these organs can be affected by the thickened mucus (5). Lungs The majority of the problems will be concentrated in the lungs because of the excretion system of the mucus. There are many tiny cilia that move the mucus of the lungs up the esophagus and lets it fall into the stomach. Due to the thickened mucus, it is nearly impossible to clear the lungs, thus impairing lung function. This leads to difficulty breathing and to increased risk of infections (6). Digestive System The pancreas is also in great danger of being plugged. The pancreas produces: HCO3, CCK, trypsinogen, chymotrypsinogen, pancreatic lipase, carboxypeptidase, and amylase. All of which, aid in the digestion and absorption of the nutrients consumed. If these enzymes are absent from the digestive tract, there will be a great deal of malabsorption and maldigestion (6). Reproductive System Cystic Fibrosis could also lead to infertility, mostly in men. The seminal fluid will be much thicker and will not be likely to clear the vans deferens and ejaculation will not lead to pregnancy. Females have less difficulty with fertility, although it is still compromised. The 2 mucus around the cervix will be much thicker, and that makes it quite difficult for the sperm to penetrate to fertilize an egg (6). Other Affected Organs The liver is often damaged in CF patients. Liver disease is the third leading cause of death in CF patients. Damage generally begins when the pancreatic enzymes cannot clear the common bile duct and thus causes focal biliary fibrosis, which appears in most CF patients. A small percentage of CF patients will experience cirrhosis of the liver due to decreased function. In these cases, various forms of treatment are used to avoid liver transplants (7). DIAGNOSTIC TESTING Sweat tests are the most commonly used to diagnose CF. It is a non-invasive test. It consists of an electric pulse on the skin with medicine to induce sweating. The sodium content is then measured. This is one of the most cost effective tests for the disease (8). Genetic testing is also an option, even though it is vastly more expensive. Cells are harvested from the patient to determine genotype to compare to the known mutations of cystic fibrosis. Chest and Sinus x-rays are used to detect thick areas of mucus in these cavities (8). Lung function tests can also be employed. The FEV1 – Forced expiratory volume in 1 second measures the volume of air the can be forcefully exhaled in one second. This is usually decreased in CF patients. FEF – Forced expiratory flow measures the rate of air released during the middle of an expiration. This is also usually decreased in CF patients (8). MEDICAL THERAPIES Medications 3 Generally speaking, the medication, administered to CF patients, is used to treat common symptoms and problems associated with the disease. First of all, they are usually prescribed replacement pancreatic enzymes (PERT) to take with each meal. These are to make up for the lack of pancreatic enzyme released due to the pancreas being plugged with mucus. PERT is the first step to correct malabsorption and maldigestion (9). Pancreatic enzymes are encapsulated to be able to withstand the acidic environment of the stomach in order to be released in the duodenum. These enzymes help break down carbohydrates, fats, and protein. Dosage depends on: degree of pancreatic insufficiencies, the amount and content of food. PERT should help to control GI symptoms (steatorrhea) and promote growth. Fecal elastase, fecal fat, or nitrogen balance studies should also be performed to assess dosage. Fecal elastase is an enzyme secreted by the pancreas used to digest protein and is involved in hydrolysis of peptide bonds (10). Many times, they will also have several courses of antibiotics to fight against common infections. The thickened mucus on the lungs holds on to bacteria and easily lets them propagate. It is quite dangerous for CF patients to get an infection in the lungs because they are so hard to treat (1). It is very common for the tissues affected to become inflamed. It is then necessary for the afflicted individual to take anti-inflammatory drugs. These can either be ibuprofen or corticosteroids. Bronchodilators are often used to open the airway to allow easier breathing. These drugs are given inside a nebulizer to ensure efficacy. There are medications that can also help thin the mucus so it is easier to clear (4). It is quite possible for a CF patient to develop brittle bones due to malabsorption. It becomes necessary to give those individuals bisphosphonates to combat osteoporosis (11). Over 4 eighty percent diagnosed, develop CF related diabetes, thus insulin is in due course. The reduced pancreas efficacy makes this necessary (12). Some alternative and complementary therapies suggest the use of antioxidants will help. Research has concluded that it is unlikely. Next, it is suggested that a patient take probiotics to aid in digestion. It is unclear whether or not this supplement has any effect. Another treatment is acupuncture. This is supposed to help with chest wall pain and has been effective for many in pain management. One herbal supplement that is prevalent is Boswellia. It is supposed to have anti-inflammatory properties to aid in breathing (11). This claim has not been supported by research. It is also suggested that the supplementation of Omega-3 fatty acids could be helpful. The Cochrane review suggests research is not extensive enough to be sure that there is a correlated benefit (13). Physiotherapy In everyday physiotherapy, it is important to maintain a regular exercise routine. Aerobic and anaerobic have benefits. Aerobics clear airways and makes it easier to breathe, while anaerobic will strengthen the muscles in the chest wall. Good posture is also essential to airway clearance. Exercises to achieve good posture are recommended (14). Postural drainage is an important part of therapy. It entails lying in several choice positions while the back and chest are clapped to release the mucus. There are several devices available that achieve the same result so it is possible to accomplish therapy oneself. Another device is a high frequency chest wall oscillation (HFCWO) an electric air compressor connects to an inflatable jacket (vest) to vibrate your chest. It is also used to release the mucus from the 5 lungs. Once the mucus is released, it is possible to cough up. A CF patient is required to cough up a few cups of sputum a day (4). Breathing exercises are often implemented to aid in clearance. An active breathing cycle consists of breathing control for 30 seconds, three or four deep breaths, breathing control, three or four deep breaths, breathing control, huffing, and finally coughing. The cycle is repeated for the specified amount of time two or three times a day. If the individual is not receiving enough oxygen, they may need to start oxygen therapy (12). Surgical Options There are a few surgeries that CF may require. One is nasal polyp removal. CF often produces nasal polyps that can block the airways, thus necessitates their removal. Bowel surgery is also a possibility. If the digestive tract is particularly affected by blockages, they may become nonfunctional or die. This means bowel resections. If the CF is severe enough, a double lung transplant will lengthen the CF patient’s lifespan by a few years. The double lungs transplant is needed because the affected lung could corrupt the fresh one. This will not cure the CF, just lengthen life for a while. Over half of these recipients are dead after five years. The genes are still defective (7). PROGNOSIS AND QUALITY OF LIFE Patients need to visit their doctors for regular checkups about every three months. The doctors check for nasal polyps, lung function, nutrition, and compliance. Vitamin levels and liver function is checked as needed. Daily life of a CF patient consists of a couple hours of therapy a day. Added to that are regular exercise and strict compliance to diet and medications. 6 Furthermore, it is important to avoid illness and go for regular checkups. It is a very time consuming disease (12). Eventually, lung function will decrease so much, that the patient will need assistance breathing. Median survival age of those diagnosed is thirty-seven. This is a vast improvement to fifty years ago, when it was unlikely for the child to make it to adulthood (10). MEDICAL NUTRITIONAL THERAPY (MNT) The aim of MNT should be to control maldigestion and malabsorption that will cause deficiencies. It is important to provide adequate nutrients to promote growth and weight. Supporting pulmonary functions is very important as well. All MNT should be individualized for each patient to include medications, and other forms of treatment (6). It is essential to conduct a nutrition assessment frequently. The anthropometrics include: height, weight, head circumference, mid-arm circumference, and triceps skinfold. The biochemical component should measure: complete blood count, serum retinol, serum αtocopheral, albumin, electrolyte, and acid-base status. Dietary intake covers 3-day fat balance and feeding behaviors (3). Cystic fibrosis energy requirements are very individual, and change throughout life. Needs are based on gender, age, BMI, physical activity, respiratory infection, severity of lung disease, and severity of malabsorption. Higher energy expenditure is due to the increased effector of breathing. Energy consumption should be increased to fit the extra physical activity in the patient’s daily life. The ideal is to do indirect calorimetry, but it has been shown that the EER active equation best meets the needs of a CF patient when that is not possible (9). 7 Infants are best breastfed when possible. Otherwise it is important to make sure the formula meets all the requirements and possibly be supplemented with PERT. Pancreatic insufficiency give enzymes either mixed with food or directly into infant’s mouth formula fed: standard formula (20-27kcal/oz) with enzyme supplementation high calorie formula may be necessary (9). Children require high energy, moderate fat, and PERT (15). Adults need high energy to maintain weight. This includes 35-40% of total calories, or more as tolerated, including sources of EFAs. Monitor for EFA deficiency in regular blood lipid levels because the malabsorption of fat may lead to fat-soluble vitamins deficiency. Monitor fat intolerance in the stool. 15-20% of total calories should be from protein. Needs change as disease progresses. CF patients might become lactose intolerant due to the digestive insufficiency and should be aware of their tolerance. Adequate fluid intake can help thin out mucus in the lungs (9). Water-soluble vitamins are generally adequately absorbed. Low serum levels and high hepatic store of vitamin A are indicative of the failure of the liver to transport the vitamin. Vitamin D is a fat soluble vitamin of concern because the deficiency can cause decreased bone mineralization. Vitamin E deficiencies are associated with hemolytic anemia and abnormal neurological findings. Vitamin K absorption can be decreased due to antibiotic use and liver disease. Sodium will not likely need to be increased given the high sodium diet of the West. Supplementation of sodium is needed when: breastfeeding, fever, hot weather, and physical exertion. A sodium deficiency can be seen from lethargy, vomiting, and dehydration. Calcium deficiencies decrease bone mineralization. Zinc deficiencies affect growth and healing. Magnesium and iron are also nutrients of concern (9). Children and adults should be encouraged to have positive eating behaviors, enjoyable meal times, larger portions, and extra snacks. Nutrient dense food is recommended for adequate 8 calorie consumption. Adding supplements to food may be necessary. Enteral nutrition should be given if the patient is unable to meet needs orally (16). Elemental and nonelemental formulas can be used. Elemental is required if the patient is having trouble breaking down whole proteins. Parental nutrition is generally only used for short term after a gastrointestinal surgery (9). CONCLUSION CF is a chronic genetic disorder. It is very destructive. This disease is caused by a chloride ion imbalance that results in the formation of thick mucus on epithelial tissues. This thickened mucus affects the lungs, gastrointestinal system, liver, and reproductive organs of patients. Advancements in medical treatment allow patients to have better compliance to their prescribed treatments since they can do most of the therapy at home. Medical therapies such as PERT, manage the deficiencies that might otherwise occur. Life expectancy has risen to the forties. Medical advancements have made it possible for CF patients to enjoy a full and relatively normal life (1). 9 REFERENCES 1. Cystic Fibrosis Foundation. Frequently asked questions. Available at http://www.cff.org/AboutCF/Faqs/. Accessed February 25, 2014. 2. Mahan KL, Escott-Stump S. Krause’s Food and Nutrition Therapy. 12th ed. St. Louis, MO: Saunders Elsevier; 2008. 3. Group Health. Clinical Review Criteria. Available at http://www.ghc.org/allsites/clinical/criteria/pdf/hfcwo.pdf. Accessed February 25, 2014. 4. Cystic Fibrosis Foundation. Frequently asked questions. Available at http://www.cff.org/AboutCF/Faqs/. Accessed February 25, 2014. 5. Gibson RL, Burns JL, Ramsey BW. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respiratory Critical Care Med. 2003;168:918. 6. Hurt K, Bilton D. Cystic fibrosis. Med. 2012; 40:273-276. 7. Adler FR. Lung transplantation for cystic fibrosis. Proceedings Am Thoracic Soc. 2009; 6:619-633. 8. Braga SFF. Complementary therapies in cystic fibrosis: Nutritional supplements and herbal products. J Pharmacy Practice. 2013;26(1):14-17. 9. Trabulsi J, Ittenbac RF, Schall JI, et. al.Evaluation of formulas for calculating total energy requirements of preadolescent children with cystic fibrosis. Am J Clin Nutr 2007; 85(1): 144-151. 10. Fuster CO, Fuster GO, Galindo AD, Galo AP, Verdugo JM, Lozano FM. Analysis of energy expenditure in adults with cystic fibrosis: comparison of indirect calorimetry and prediction equations. Arch Bronconeumol. 2007;43(7):366-72. 11. American Lung Association. Cystic fibrosis. Available at http://www.lung.org/assets/documents/publications/lung-disease-data/ldd08chapters/LDD-08-CF.pdf American LungAssociationLungDiseaseData:2008. Accessed February 25, 2014. 12. Indiana University Health. Cystic Fibrosis. Available at http://iuhealth.org/riley/pulmonology/cystic-fibrosis/. Accessed February 25, 2014. 13. Oliver C, Watson H. Omega-3 fatty acids for cystic fibrosis. Cochrane Database of Systematic Reviews 2013, Issue 11. Art. No.: CD002201. DOI: 10.1002/14651858.CD002201.pub4. 10 14. Ikpa PT, Bijvelds MJ, de Jonge HR.Cystic Fibrosis: Towards personalized therapies.J Pediatr. [Epub ahead of print] 15. Haupt ME, Kwasny MJ, Schechter MS, McColley SA.Pancreatic enzyme replacement therapy dosing and nutritional outcomes in children with cystic fibrosis.Pathology. 2014;46 Suppl 1:S51. 16. Stanford Hospital's Adult Cystic Fibrosis Clinic - Molly Pam's Story. Available at http://www.youtube.com/watch?v=itQns51NKOo&feature=youtu.be. Accessed February 25, 2014. 11