PATHOPHYSIOLOGY OF DIGESTION AND ABSORPTION
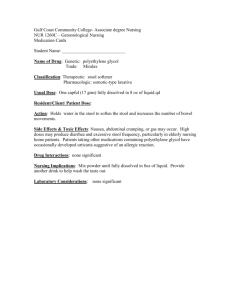
advertisement
M.H.Imanieh M.D. Pediatric Gastroenterology Department Shiraz University of Medical Sciences DEFINITION Subnormal intestinal absorption of dietary constituents and thus excessive loss of nutrients in the stool Stages of Intestinal Digestion and Absorption 1. Luminal hydrolysis and solubilization 2. Hydrolysis at the enterocyte membrane 3. Absorption across the enterocyte membrane and cellular processing 4. Uptake from the enterocyte into blood and lymph PATHOPHYSIOLOGIC MECHANISMS Digestion in the lumen Mouth : • Saliva is important for normal digestion • Parotid (20%), Submandibular (60%), Sublingual (20%) • Minor salivary glands in lips, palate,tongue and cheeks Stomach : • Acid (parietal cells), Pepsinogen, Lipase (chief cells), IF Pancreas : • Bicarbonate ions • Digestive Enzymes Liver : Solubilization of fat Small intestine : Enterokinase Malabsorption syndromes are characterized by chronic diarrhea (main symptom) , abdominal distention and FTT. PATHOPHYSIOLOGY OF DIGESTION AND ABSORPTION CARBOHYDRATES Starch (50–60%) Sucrose (30- 40%) Lactose ( from 0-20% in adults, 40-50% in infants) Salivary Amylase Pancreatic Amylase Sucrase- Isomaltase Lactase- Glucoamylase Glucose- Galactose pump Fructose Transport Lipase Lingual Fundus Pancreatic Colipase Bile salts F. acid Binding protein Apo protein Lipo protein Lymphatic system Gastric pepsinogen I, II Gastric pepsin I, II Trypsinogen enterokinase trypsin Proelastase trypsin elastase prochymotrypsinogen trypsin chymotrypsin Proendopeptidase trypsin endopeptidase Proexopeptidase trypsin exopeptidase Brush border peptidase Cytoplasmic peptidase Celiac disease Giardiasis Food allergy ( milk, soya, …) Alpha chain disease Hypogammaglobulinemia Dermatitis herpetiformis Bacterial overgrowth Eosinophilic enteritis cont Regional enteritis Post infectious enteritis Radiation enteritis Amyloidosis Seleroderma Tropical sprue Mastocytosis Cystic fibrosis Chronic pancreatitis Pancreatic hypoplasia Pancreatic resection Schwachman syndrome Postgastrectomy steatorrhea Gastrinoma (Zollinger-Ellison syndrome) Lipase or colipase def. Trypsinogen or enterokinase def. Cong. Sucrase – isomaltase def. Cong. Lactase def. Late onset lactase def. Cong. Trehalase def. Cong. Glocose- galactose malabsorption All causes of villous atrophy Parenchymal liver Dx. Cholestasis Blind loop syn. Stricture – fistula Hypomotility ( DM- Pseudo obst.) Ileal disease (TB, Crohn, resection) Neomycin- cholestyramin- ca carbonate Lymphangiectasia Whipple disease Lymphoma Constrictive pericarditis Mesenteric vascular insufficiency Vasculitis C.H.F Diabetes mellitus Hypoparathyroidism Hyperthyroidism Adrenal insufficiency Gastrinoma (Zollinger-Ellison syndrome) Carcinoid syndrome Abetal lipoproteinemia Lymphangiectasia Anderson’s disease Wolman disease Abdominal distention Pale, foul smelling bulky stool Muscle wasting Poor Wt. gain – Wt. loss Subcutaneus fat loss Sign- Symptome Malnutrition and Wt. loss Diarrhea Pathophysiology Malabsorption of fatcarbohydrate- protein Impaired absorption or increased secretion of water and electrolytes. unabsorbed dihydroxy bile acids and fatty acids. Flatus Bacterial fermentation of unabsorbed CHO Glossitis – cheilosis stomatitis Def . Of Iron- B 12 – Folate and … Bone pain Protein and calcium depletion Sign- Symptome Pathophysiology Osteoarthropathy Unknown Tetany – paresthesia Ca and mg depletion Weakness Anemia – hypokalemia Periph. Neuropathy Vit B12 and thiamine deficiency Eczema Unknown Dermatitis Def. of vit A – zinc- essential fatty acids Night blindness xerophthalmia Vit A deficiency Sign- Symptome Pathophysiology Nocturia Delayed reaborption of waterhypokalemia Azotemia- hypotension Fluid and electrolyte depletion Amenorrhea, ↓libido Protein and calori depletion 2° hypopituitarism Anemia Impaired absorption of Iron- B12 – folate Purpura ( bleeding tendency) Vit. K malabsorption DIAGNOSIS Hx. P/E Lab. Stool PH and reducing substance H2 breath test Oral tolerance test Stool osmolality Mucosal activity of disacharidases D- xylose test Stool alpha- 1 antitrypsin Chromium labeled albumin Serum albumin Stool chymotrypsin Stool fat (smear) 72 hrs stool fat Serum caroten D- Xylose test C14 triolein breath test WBC- OP- Cl.diff. toxin - PH Stool 72 hrs fat (75-100 grams/24 hrs) Blood CBC diff- ESR- Electrolytes - BUN Creatinine – T3, T4 – gastrin- VIP calcitonine - histamin plain film (pancreatic calcification)CTscan Radiology barium study ( upper GI- small, large bowel) biopsy and histology: celiac- GiardiaEndoscopy crohn’s- lymphoma- eosinophilic GEenzyme assay – A beta- wolmanlymphangiectasia MANAGEMENT Rx. of underlying dx. Nutritional support