Radiation Protection in Nuclear Medicine
advertisement

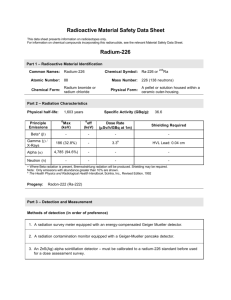
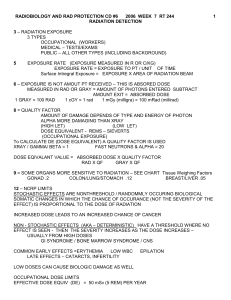
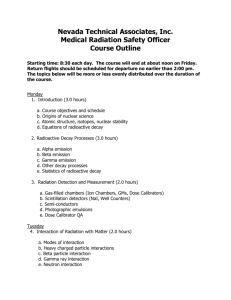
Nuclear Medicine Physics Radiation Protection in Nuclear Medicine Jerry Allison, Ph.D. Department of Radiology Medical College of Georgia A note of thanks to Z. J. Cao, Ph.D. Medical College of Georgia And Sameer Tipnis, Ph.D. G. Donald Frey, Ph.D. Medical University of South Carolina for Sharing nuclear medicine presentation content Federal Register/Vol. 80, No. 220/ November 16, 2015/Notices NUCLEAR REGULATORY COMMISSION [NRC–2015–0020] Sodium Iodide–131 Patient Release Information Collection AGENCY: Nuclear Regulatory Commission. ACTION: Request for information. SUMMARY: The U.S. Nuclear Regulatory Commission (NRC) is requesting information from the general public on a number of issues associated with medical treatment of patients with sodium iodide I–131 (hereafter referred to as I–131). Specifically, the NRC would like input on patient concerns about medical treatment involving the use of I–131, information that physicians use to make decisions on when it is safe to release I–131 patients based on radiation exposure concerns, radiation safety information used by I– 131 patients after their release, and the availability of a radiation safety informational guidance brochure for I– 131 patients that can be distributed nationwide. The information collected will be used to develop a Web site to provide patients with clear and consistent information about radioactive iodine treatments and to revise NRC patient release guidance. UCSD Imaging Research 4 UCSD Imaging Rersearch 5 Radiation exposure of the public 6 Sources of low-dose radiation 1982 data of NCRP: 4.6 mSv/person/yr • Natural background: 4 mSv/person/yr (88%) Radon at home: 2.57 mSv/person/yr (56%) Other sources: 1 mSv/person/yr (22%) e.g. U-238 and Th-232 in soil, cosmic rays from the sky, and internal radiation from 40K, 14C and 3H Fallout from nuclear power stations and consumer products: 0.46 mSv/person/yr (10%) 7 • Medical: 0.54 mSv/person/yr (12%) Sources of low-dose radiation 2006 data of NCRP: 6.7 mSv/person/yr • Natural background: 3.5 mSv/person/yr (52%) • Dramatic increase of medical dose from 0.54 to 3.2 mSv/person/yr (12% 48%) CT dose: ~ 1.6 mSv/person/yr (50% of medical) NM dose: ~ 0.8 mSv/person/yr (25% of medical) • Dramatic increase of NM and CT studies: 1984 2006 NM 6M 18 M (3% of all) CT 3M 67 M (12% of all) 8 Radiation dose effects 9 Stochastic and non-stochastic effects • Stochastic: The frequency of effects in a population depends on dose without threshold (e.g. cancer). • Non-stochastic: The severity of effects varies with dose above threshold (e.g. cataracts). • Aim of radiation protection: to prevent nonstochastic effects by limiting the radiation dose received as well as to reduce the probability of stochastic effects through ALARA practice. 10 Models of low-dose response • Lack of certainty for low dose effects (< 1 Sv/yr) • Linear no threshold (LNT) model: a line connecting the bottom end of high-dose response curve to the zero dose • Linear-quadric model: linear for the lowest dose and quadric for the remainder • Hormesis model: ‘J’ shape dangerous at high dose but beneficial at low dose, low dose sterilizing cancer cells and stimulating cell activities 11 Models of low-dose response damage linear+quadric 1 Sv/yr hormesis dose benefit 12 Internal dosimetry • Factors determining internal dose • Medical internal radiation dosimetry (MIRD) calculation schema 13 Factors determining internal dose • Administered activity • Initial activity in the source organ and the length of stay in the organ, depending on biodistribution and physical decay • Energy emitted per decay • Absorbed fraction by the target organ, depending on distance, attenuation, and target organ volume and composition 14 Factors determining internal dose • Source and target organs 15 MIRD calculation schema Mean absorbed dose D = ÃS orD/A0 = tS Where t = Ã /A0 • A0: administered activity. It is known. • Ã is activity accumulated in the source organ and t is the residence time. Ã or t depends on initial biodistribution, physical decay (lp), and biologic behavior (lb). It can be estimated by imaging at multiple times. 16 MIRD calculation schema • S: dose to the target organ from unit cumulated activity in the source organ • S has been tabulated for many organs and also for many radiopharmaceuticals. • S depends on radiation energy per decay and absorbed fraction by the target organ f. • 0 < f < 1, determined by photon energy and distance, attenuation, volume and composition of the target organ 17 Absorbed dose to individual organs F18FDG(10 mCi) Tc99mECD(30 mCi) Tl (3 mCi) brain 17 mSv 0.4 6.6 kidneys 7.8 5.8 51 heart 25 1.3 3 ovaries 4.1 5.8 11 testes 4.1 2.6 22 Spleen 5.6 1.5 2 bladder 27 54 5.7 ______________________________________________ EDE 8.6 mSv 8.4 mSv 18 mSv 18 Effective dose of NM procedures 19 ACOB/GYN’s statement and regulations • “Women should be counseled that x-ray exposure from a single diagnostic procedure does not result in harmful fetal effects. Specifically, exposure to less than 50 mGy has not been associated with an increase in fetal anomalies or pregnancy loss.” • Regulatory dose limit for the fetus of a declared pregnant worker is 5 mSv during the pregnancy. 20 Absorbed dose to fetus early 1st end of 1st trimester trimester _______________________________________ bone scan (20 mCi 99mTc-MDP) 5 mSv 4 mSv WB PET scan (15 mCi 18F-FDG) 15 mSv 10 mSv thyroid scan (0.2 mCi 123I) 0.2 mSv 0.1 mSv all dose << 50 mSv 21 Absorbed dose to fetus • Iodine can cross the placenta but fetal thyroid does not cumulate iodine before 12 wk of gestation. • Mental retardation from radiation occurs primarily at 8 to 15 weeks of gestational period. • A large portion of radiation comes from mother’s bladder so hydration and frequent voiding may reduce the radiation. 22 Radiation protection • U.S. Federal regulations (10CFR 19, 20, and 35) • ALARA: philosophy of radiation use whereby radiation dose is “as low as reasonably achievable” 23 Regulatory agencies • Nuclear Regulatory Commission (NRC) To regulate the nation's civilian use of byproduct, source, and special nuclear materials to ensure adequate protection of public health and safety, to promote the common defense and security, and to protect the environment. The NRC's regulatory mission covers three main areas: reactor safety, radioactive materials used in medicine, industry and research, and nuclear waste management • FDA To regulate radio-pharmaceuticals and NM devices 24 Regulatory agencies • EPA To regulate the radiation released to environment • DOT To regulate the transportation of radioactive material • Agreement States To enter an effective regulatory discontinuance agreement with the NRC to regulate most types of radioactive material in accordance with the compatibility requirements of the NRC 25 Agreement States 37 states have signed an agreement with the Nuclear Regulatory Commission stipulating that they will be the sole regulators, but will follow Federal guidelines. They may be more restrictive than these guidelines, but not less restrictive. In August, 2013, the NRC put the state of Georgia on probation due to multiple failures. The next review was set to be in January, 2014. The State passed the review. 26 Agreement States (2015) https://scp.nrc.gov/rulemaking.html 27 Advisory bodies • International Commission on Radiological Protection (ICRP) • U.S. National Council on Radiation Protection and Measurements (NCRP) • International Atomic Energy Agency (IAEA) • Conference of Radiation Control Program Directors (CRCPD) 28 “Radiation badges” • Anybody that may receive 1/10 of the annual occupational dose limit of 50 mSv needs to wear a radiation badge. • Minor likely to receive: Annual external dose (DDE) > 1 mSv LDE for eyes > 1.5 mSv SDE for skin > 5 mSv • If the waiting area for injected patients is close to the secretary, she/he should wear a radiation badge. How to wear a radiation badge? • For uniform radiation exposure, wear the badge on front of upper torso. • If particular body part is more exposed, wear the badge as close to this part as possible. • Wear the badge behind a lead apron (or at the collar outside the apron, GRU policy) • A person handling radionuclides must wear 30 both whole body and ring badges. How often are badges exchanged? • Every month @ GRU OSL = Optically Stimulated luminescent Dosimeter • Monitoring is only required for external exposure. There is NO requirement to monitor the internal exposure. Posting of badge reports Film badge readings are routinely posted on bulletin board on a monthly basis. Employer is responsible for informing each employee on an annual basis of his cumulative radiation dose. Occupational dose limits • Occupational dose limits: For an adult worker < 50 mSv/yr For an individual organ < 500 mSv/yr For the eye lens < 150 mSv/yr For fetus of a pregnant worker < 5 mSv/pregnancy General public limits: Dose < 1 mSv/yr Exposure rate < 2 mR in any given hour 33 Declared pregnant radiation workers • A declared pregnancy is when an employee voluntarily informs the radiation safety office in writing of her pregnancy and estimated date of conception. • It is entirely the choice of the worker. • NRC dose limit is 5 mSv (10% of the annual occupational dose limit) to the fetus for the entire pregnancy. • An additional dosimeter badge should be worn at the level of the fetus. • If a worker chooses not to declare her pregnancy, the pregnancy dose limit does not apply. Radiation dose to the hands • Typical dose received by hands without syringe shields is 5 to 10 mSv/hr/mCi when handling radionuclides. • For a radiation worker to reach the 500 mSv per year limit, she/he could spend 5-10 hours handling a 10 mCi syringe per year. • Syringe shields reduce the dose by a factor of 3. Radiation exposure rate around patient Typical exposure rate at 1 m from the patient soon after injection: • Most radiopharmaceuticals: 1 mR/hr (maximum dose to public 1 mSv/yr) • 18F-FDG: • 131I: 5 - 30 mR/hr 5 or 30 mR/hr for Graves or cancer dose respectively Surveys for contamination • Survey with a GM meter must be performed at the end of each day in all areas where radioactive materials are prepared or administered. • The GM meter must be able to detect an exposure rate as low as 0.1 mR/h. • Wipe tests must be performed once a week where radioactive materials are prepared, administered or stored. • A record of the results should be kept. Area surveys – daily • Using a GM meter, survey each room in which radioisotopes are used. • Record Model # & Serial # of the GM meter • Record actual reading; specify units (cpm or mR/hr) • Record background reading • Specify "action level" (criterion for immediate action if necessary) Area wipe tests – weekly • An accurate area map must be drawn and, on a weekly basis, a dry wipes (filter paper or swab) are taken in each area where radionuclides are used. • The wipes are counted in a well counter that uses open energy window. Also background counts are obtained. • Results of the counting procedure are correlated with the area map. If greater than 6600 dpm/cm2, notify the RSO Leak test of sealed sources All sealed sources with half-life longer than 30 days (dose calibrator standards, well counter calibration sources, spot markers, etc.) must be wipe-tested before initial use and then every 6 months. The results must be recorded in an appropriate logbook. The test must be sensitive to 0.005 µCi. Labeling and storage of radionuclides All containers, vials, syringes containing radioactive material should be • labeled properly With radiation symbols and words such as CAUTION (or DANGER), RADIOACTIVE MATERIALS Radionuclide Quantity of radioactivity and time/date measured • Stored and shielded in secure area • Constantly monitored when not secured Labeling and storage of radionuclides • A syringe shield needs to be labeled if it contains a syringe with radiopharmaceutical. • Alternatively, it may have a transparent portion to see the label. Acceptable methods of waste disposal Transfer to licensed person/company Decay in storage Release as effluents within authorized limits (generally unnecessary) Radioactive sharps disposal • Use separate containers (e.g. sharps) • Seal when full and label date and longest halflife • 3 S’s: Sealed, Shielded, Secure location • Before disposing, survey surfaces of container to make sure not higher than the background • Dispose of waste in appropriate containers (e.g. biohazard but no radiation symbol) Radioactive package receipt • Must be inspected within 3 hours of receiving or, if after hours, within 3 hours of start of the next day • Visually inspect the package for the DOT radioactive material label, breakage, and leakage DOT package labeling Surface exposure rate (mR/hr) Transportation index White I Yellow II Yellow III < 0.5 0.5-50 50-200 0 <1 1-10 Transportation index (TI) is the exposure rate (mR/hr) measured at 1 meter from package. DOT package labeling: Radioactive I 0 at 1 meter < 0.5 mR/h at surface DOT package labeling: Radioactive II < 1 mR/h at 1 meter < 50 mR/h at surface DOT package labeling: Radioactive III < 10 mR/h at 1 meter < 200 mR/h at surface DOT radioactive placard for the vehicle Vehicles carrying packages bearing Yellow III labels are required to post the placard shown below on the outside of the vehicle. 7 Radioactive package receipt • Measure exposure rates 1 meter from package and at the surface •If normal, proceed to wipe test 51 Exposure rate at 1 meter Exposure rate at surface Radioactive package receipt • Wipe test Wipe area is about 300 cm2 on all sides. The counts should be less than 6600/min (22 dpm/cm2). • If normal, remove the packing slip and open the package. • Complete entry in receipt log • Store package in appropriate shielded area 54 Retention of records 20.2102 - Licensee shall maintain records including: … ALARA Efforts to reduce the radiation dose so long as the expenditure does not overweigh the gain Decrease of exposure time for workers Increase of distance (inverse square) Shielding (e.g. lead pigs), signs and labels Personnel protection and monitoring ALARA levels at GRU • ALARA 1: 1.25 mSv in any given quarter • ALARA II: 3.75 mSv in any given quarter 56 Protection from external sources • Time around a radiation source • Distance from a radiation source • Shield for syringes, vials and dose calibrators, but usually not for walls 57 Photon intensity: inverse square law • Inverse square law used for unshielded source, particularly useful in PET I = I0/d2 • Exposure rate (R/hr) = GA/d2 G: exposure rate constant for a point source (Rcm2/(mCihr)) 58 10 mCi F-18 radiation dose rate Distance 0.5 m 1.0 m 1.5 m 2.0 m 2.5 m 3.0 m 3.5 m 4.0 m Dose rate w/o lead 22.6 mrad/hr 6.3 mrad/hr 3.0 mrad/hr 1.4 mrad/hr 0.93 mrad/hr 0.62 mrad/hr 0.48 mrad/hr 0.39 mrad/hr w 1/8” lead 13.6 mrad/hr 3.5 mrad/hr 1.6 mrad/hr 0.90 mrad/hr 0.54 mrad/hr 0.41 mrad/hr 0.29 mrad/hr 0.23 mrad/hr 30% increase in distance better than 1/8” lead shield 59 Photon intensity: exponential attenuation Exponential attenuation in a medium I = I0 exp(-md) • Reducing radiation using lead shield 60 Prevention against ingestion/absorption/inha lation of radioactivity • No eating, drinking and applying cosmetics in restricted areas • Wearing lab coats and gloves • Washing hands after handling radioactivity • Working with radioactive gases under a ventilated fume hood 61 What is wrong? No gloves, no syringe shield, no label, not on counter with lead glass and absorber What is wrong? No lab coat, no gloves, no ring badge, no syringe shield, no label, no absorber under 63 the injection spot, too happy perhaps? Reportable medical events • Diagnostic events resulting in a dose that is Greater than 50 mSv effective dose, or Greater than 500 mSv dose equivalent to any organ, or Greater than 500 mSv shallow dose equivalent to skin • Therapeutic events: administered dose exceeds 20% of prescribed dose Reportable medical events • Dose equivalent to an embryo/fetus is higher than 50 mSv, unless the dose is approved in advance by the AU. • Dose to a nursing child is higher than 50 mSv or permanent damage to an organ or physiologic system of the child. • Events of patient intervention (intentional or unintentional action, e.g. removing treatment device) in which the dose may cause permanent damage Reportable medical events • Must notify NRC/state, referring physician and patient in writing, giving pertinent details and plans for preventing recurrence • Mainly for radiotherapy not imaging Agent FDG (10 mCi) Tc-mibi (20 mCi) Tl (2 mCi) EDE 7.0 mSv 7.0 mSv 12 mSv Highest organ dose 59 mSv 29 mSv 46 mSv 66 Recordable but not reportable events Event resulting in a dose below the NRC limits. It may caused by • Administered dose falls 10% outside the prescribed dose range, or • Wrong patient, or • Wrong radiopharmaceutical, or • Wrong route of administration • Need to be recorded locally and kept 67 for 10 years Recordable but not reportable events • E.g. 10 mCi of In-111 octreotide is 66.7% more than the usually prescribed dose of 6 mCi. This is a recordable event for the hospital and nuclear medicine department but does not meet the NRC definition of medical event. What is major spill? • Activity released at location or on people 100 mCi Tc-99m or Tl-201 10 mCi Ga-67 or In-111 1 mCi I-131 • Radiation safety officer must be present. • Focus on containment, shielding, and decontaminating individuals What to do with a major spill? • Notify all persons in the area of spill • Prevent spread of contamination Cover spill with disposable, absorbable paper Remove contaminated clothing Shield radioactivity if possible Room sealed off Report incident to RSO immediately RSO directs further response. 70 What to do with a minor spill? • Notify all persons in the area of spill • Prevent spread of contamination Cover spill with disposable, absorbable paper Remove contaminated clothing • Clean up spill with disposable, absorbable paper • Survey the area until the exposure rate is lower than twice background level • Personnel monitored (hands, shoes, clothing) • Report incident to radiation safety officer What is wrong? No glove, no syringe shield, no label 72 What is wrong? The hot lab door is wide open.