H&P Exam I (OMS I Spring 2014).
advertisement

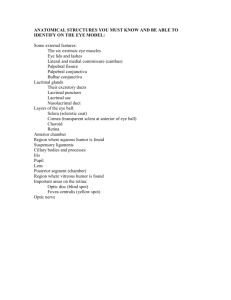
H&P Exam I Spring 2014 OMS I – Exam 1 Dermatology Primary lesions are the first to appear and are due to the disease or abnormal state. Flat lesions: <1cm (5mm) macule ; >1cm (5mm) patch Superficial raised (epidermal and/or superficial dermal location): <1cm (5mm) papule ; >1cm (5mm) plaque Deep raised (deep dermal and/or subcutaneous location): <1cm (5mm) nodule ; >1cm (5mm) tumor Serum filled: <1cm vesicle ; >1cm bulla Hemorrhagic: <3mm petechi ;>3mm purpura/ecchymosis Vascular: Telangiectasia Transient well defined erythema and edema: wheal/urticaria/hive Cyst – fluid or semisolid filled sac Comedone: plug of sebaceous & keratinous material in the opening of the hair follicle [open – black head, closed – white head] Dermatology Secondary lesions develop as a result of manipulation of the primary lesions, or they develop as part of the natural progression of primary lesions Epidermal accumulations: Discrete keratinocyte accumulation – scale Same as scale with RBCs,WBCs, serum – crust Epidermal thickening with accentuated skin lines- lichenification Shedding of sheets of keratinocytes - desquamation Skin Thickness changes: Decreased epidermal, dermal and/or subcutaneous thickness- atrophy Abnormally thick scar that stays within the boundary of the lesion – hypertrophic scar Abnormally thick scar that extends beyond the boundary of the lesion – keloid Linear atrophy with fragmented collagen/elastin fibers – stria Dermatology Break in Skin Surface: Linear break in skin – fissure Wider defect with partial epidermal loss – erosion Trauma induced by scratching or picking, either linear or papular - excoriation Wider defect with full thickness epidermal loss – ulcer Pus accumulations: Superficial – pustule ; deep – abscess Shape & Distribution Annular (ring) , nummular (circular or oval) Polycyclic or arcuate (curved like a bow) Linear or reticular Serpiginous (creeping) , targetoid (bulls-eye like) Grouped or scattered Dermatology Dematology Exam Be sure to offer full skin exam, need proper lighting, can incorporate into other parts of PE Hair inspection: quality, distribution palpation of hair & scalp Hair Pull Test: <10% telogen phase [not growing] Trichotilomania – pulling out hair Alopecia totalis – loss of nearly all hair Alopecia areata – localized nonscarring hair loss Hiruitism – excessive growth Loss of leg hair – peripheral vascular disease Skin inspection: head to toe, front to back; view sunexposed & hidden areas, exam under skin folds, color variation, texture/thickness, moisure/dryness, tempature, turgor Lesion decription: Asymmetry, Border, Color, Diameter, Location Nails inspection: color, texture (grooves, pitting), capillary refill [turn to pink in <3sec] Ophthalmology Start: 1. Check VISION : eye chart, finger counting, hand motion, light perception, no light perception 2. Shine light on PUPILS: red reflex (retinoblastoma), reactivity, size & shape Accomadation: CN III, Afferent defect: CN II Anisocoria = unequal pupils 3. Check ocular MOTILITY CN III: superior, inferior & medial rectus mm., inferior oblique m. pupils CN IV: superior oblique m. CN VI: lateral rectus m. Strabismus – improper alignment ; Hirschberg Test – corneal light reflex to check for alignment (if hits in the same location on both eyes, eyes are aligned) Ophthalmology Visual Fields: Extends further temporally 100-110 degrees, nasally and upward 60 degrees & downward 70 degrees Blind spot = optic nerve Unilateral visual loss = in front of chiasm, Bilateral visual loss = behind chiasm [strokes – typically behind] Optic Nerve: should see margins & vessels coming from center Optic cup: disc ratio usually 1:3 Ocular pressure: <21mmHg Fundus: posterior eye structures – retina, optic n, macula (yellow area, highest visual acuity) & fovea Myopia: nearsightedness (minus lens), longer eye Hyperopia: farsightedness (plus lens), shorter eye Presbiopia: loss of lens flexibility (need bifocals) Dilating eyes: (hx of glaucoma) Avoid neosynephrine if: pregnant, recent heart attack or stroke, shortness of breath Pilocarpine 1% if needed for reversing dilation Ophthalmology Diseases: Proptosis (forward projection of eye) – commonly w. Graves’ diseas, usually medial or lateral rectus muscle thickinging and usually bilateral Blepharitis (swelling/inflammation of eyelids) – can be bacterial, can lead to meibomian gland dysfunction (mucin deficient tears, corneal scarring, ocular surface irritation) Rx: steroids, antibiotics, baby shampoo Sty (inflammation around hair follicle) Chalazion (inflamed, clogged meibomian gland) Conjunctivitis (almost always go away alone) – allergic, bacterial [has mucous-type drainage & more red], viral [most common] Birth: given erythromyocin to prevent conjunctivitis & scarring from it, 6/1000 Ophthalmia neonatorum (Chlamydia) Episcleritis/Scleritis (CT inflammation between conjunctiva & sclera) 30% assoc. w. RA, Lupus, Sjogren, sarcoidosis, IBS, Wegners, TB Rx: steroid drops, wean off slowly Vitreous: “floaters” = liquefaction of vitreous Can be blood (diabetic), piece of retina (flashes of light) Cherry red spot – the macula, no arteries, sign of central artery occlusion (rest of retina appears white) Vein occlusion – back up of blood flow Hyperlipidemia – fatty deposits, arcus senilus (white ring around cornea) Papilledema – optic nerve edema seen as disc blurring Ophthalmology Unilateral PAINLESS Vision Loss: Artery or vein occlusion Retinal detachment Glaucoma (open angle) Cerebrovascular disease (occipital lobe) Macular degeneration (wet) Cataract Hollenhorst plaque (plaque from carotid artery lodged in optic artery) Unilateral PAINFUL Vision Loss: Angle closure glaucoma Optic neuritis (inflammed optic n., 50% develop MS [1st symptom], typically ♀ under 45y/o) Temporal Arteritis (Giant Cell - >50y/o, +/- Transient Ischemic Attacks or high Westergren Sed Rate, weight loss, jaw claudication, untreated total blindness, managed by rheumatologist w. steroids) Trauma Bilateral PAINLESS Vision Loss: Diabetic Retinopathy Macular Degeneration Genetic retinal diseases Cataract Occipital lobe stroke Brain mass (Papilledema) Drug toxicity (ethambutol) Uveitis (inflammation) Ophthalmology Normal Fundus Disc: clear outline, central cup is pale Retina: red/orange color, macula is dark, avascular area temportally Vessels: arterial 2: venous 3 ratio; arteries bright red, veins slight purplish HTN Retinopathy Disc: clear outline elevated, edematous w. blurred margins Retina: exudates (fluid collectins in retina from damaged vessels) & flame hemorrhages prominent flame hemorrhages surrounding vessels near disc Vessels: attenuated arterial reflex attenuated retinal arterioles Diabetic Retinopathy Disc: normal new vessels on disc surface partially obscured by fibrovascular proliferation Retina: numerous scattered exudates & hemorrhages obscured by proliferating tissue Vessels: mild dilation of retinal veins dilated veins abnormal new vessels in fibrous tissues (in vitreous) Papilledema Disc: elevated, edematous w. blurred margins & engorged vessels Retina: flame retinal hemorrhage close to disc Vessel: engorged tortuous veins Optic Atrophy Disc: marigins sharp & clear, pale white color Retina: normal Vessel: arteries attenuated, veins normal Ophthalmology Exam Be at same level as patient! 1. Vision [eye chart] – with glasses 2. Pupils – equal, round reactive Marcus Gun Pupil – flashing light back & forth, 1 constricts & other dilates upon light being shone into it 3. Motility – full, limited have them follow your finger 4. Visual fields – hands should be equidistant, cover same eye reflectively as patient [their L, your R] Have them stare at your eye move fingers in (both sides) & then up Ophthalmology Exam Ophthalmoscope Turn down the lights! Same eye level as your patient Your right eye, to THEIR right eye Get CLOSE To decrease corneal reflection: use smaller aperture reduces area of retina illuminated, direct light toward pupil’s edge instead of center or used a crossed linear polarizing filter Focus your instrument: Correct for you & your patient near-sighted correction=RED (object will get smaller, or moves with glasses movement) far-sighted correction=GREEN (object will get larger, or moves against glasses movement) Hold scope with pointer on side dial, middle finger under & rests on patient’s cheek Patient looks straight ahead, you angle in from the side ~15º & start focusing See vessel, follow vessel as it enlarges (heading toward nerve) Neck & Lymph Anatomy Review: Anterior Triangle: SCM laterally, Mandible superiorly, Neck midline medially Posterior Triangle: Trapezius laterally, Clavicle inferiorly, SCM medially Neck Inspection Proper exposure, symmetry, muscle mass, chin alignment, skin lesions, masses, trachea position, lymphadenopathy, thyromegaly Tracheal deviation – urgent if also in respiratory distress SAME side deviation – pneumothorax, OPPOSITE side deviation – tension pneumothorax ROM – flexion, extension, side bending, rotation Auscultation ALWAYS listen before feeling carotid a. Use BELL to detect low-pitched systolic bruits (don’t want to apply pressure if one is present, could dislodge thrombus or cut off flow) Carotid a. is beneath the SCM Have patient take breath in, let it out & hold it, then listen [don’t listen for too long – 5-6 heart beats - & let them breathe in between sides] Thyroid : increased blood flow causes bruit, sign of hyperthyroid ; follow same procedure as listening to carotid arteries Neck & Lymph Palpation [always use PADS of fingers] FRONT of patient : palpate posterior neck anatomy (cervical vertebrae, paraspinal m., occiput & posterio cervical chain lymph nodes) , tracheal deviation Lymph nodes: preauricular, postauricular, occipital, tonsilar, submandibular, submental, superficial cervical, deep cervical, posterior cervical, supraclavicular, infraclavicular BEHIND patient: **explain to patient what you’re doing, to feel structure – not strangling** Thyroid: Starting at chin moving down soft tissue thyroid cartilage cricothyroid membrane cricoid thyroid rings isthmus located over rings 2-4, move lateral from there for lateral lobes (can translate trachea to feel lateral lobes better) Can have patient swallow to feel smaller nodules [offer glass of water] Carotid A.: use pointer and middle finger, gentle traction on SCM, slowly depress carotid artery [not for expanded time & NEVER both at once] **absent bruit ≠ absent stenosis Neck & Lymph Lymphatics Major: cervical, axillary, epitrochlear (if arm dysfunction), inguinal Inspect then palpate Normal: <1cm, rubbery, mobile - should be able to roll them up/down & side to side Pathological : Localized & tender – infection w/in drainage area Generalized – HIV, TB, SLE, meds (phenytoin) Malignancy – nontender, firm, fixed nodes Using pads of fingers, massage in circular motion applying enough pressure to only engage skin Cervical : preauricular, postauricular, occipital, tonsilar, submandibular, submental, superficial cervical, deep cervical, supraclavicular, infraclavicular Axillary : [wear gloves] anterior fold, chest wall – medial, posterior fold, medial arm – lateral Epitrochlear : not normally palpable, if arm infected or axillary swollen; located above medial epicondyle [local or systemic infection if epitrochlear rather than breast malignancy ] Inguinal : lift garment, want to look to make sure you’re not going haywire but keep drape over patient, stand at hip level Neck & Lymph Special Testing – Meningitis Symptoms associated: Neck pain, stiff neck, headache, fever, photophobia, mental status change, nausea and vomiting Physical findings: Appears acutely ill, often in distress, confused or obtunded, febrile, tachycardia, tachypnea, occasional rash Palpate for Nuchal Rigidity With the patient in the supine position, palpate the nuchal cord (nuchal ligament) from occiput to C7 for nuchal rigidity The nuchal cord is firm and bandlike but softens with extension of the neck and is not typically tender Meningeal irritation can cause the patient to attempt to hold the head still, resulting in contraction of the neck muscles and rigidity of the nuchal cord that does not relax with extension of the neck Brudzinski’s Sign (passively flex patient’s neck): pain = positive, person may flex hips to relieve pain Kernig’s Sign (patient supine, flex their hip 90º then extend their lower leg): pain = positive ENT Ear History : hearing problems (unilateral, bilateral – sensory or conductive), assoc. problems (tinnitus, vertigo, otorrhea), duration, family Hx, noise exposure Vertigo CN VIII Presbycusis – progressive, bilateral sensory loss, high frequency Syphillis, Rubella, Meningitis, Gross Hearing Test: finger rub, whisper 2 syllable test tuning forks Weber [fork in middle of head or forehead]– lateralization, where they hear it louder = conductive loss side (or sensory hearing loss is louder in better ear) Rinne [start on mastoid (BC) until can’t here then move to in front of canal (AC)] – AC > BC = sensory hearing loss ; BC=/> AC = conductive hearing loss **louder in air is normal** ENT Ear Physical Exam External ear Auricle - cartilage covered by skin Meatus – entrance into the ear canal. Mastoid – temporal bone located behind the ear Ear canal – bony and cartilaginous portions, contains cerumen glands. The site of infection in otitis externa Adult: pull ear up and back to straighten the ear canal Child: pull ear down and back to straighten the ear canal “Tug test” – movement of auricle and tragus is painful in otitis externa, not in otitis media Middle ear Tympanic membrane – lateral limit of ME. Examine with the largest speculum possible Umbo – where malleus meets the TM Pars flaccida – above the short process of the malleus Pars tensa Ossicles (Malleus, Incus, Stapes) Eustachian tube Mobility tested with pneumatic otoscope Inner ear Cochlea, Semicircular Canals (balance, position/movement), CN VIII ENT Ear Tube Placement for recurrent otitis media : 5+ infections in a year, 3+ infections in 6 months, infection that does not respond to oral antibiotics, chronic middle ear fluid with conductive hearing loss, acute mastoiditis Placement: anterior inferior Tympanic membrane perforations may heal over time (central or marginal, water precautions) Cholesteatoma: epithelial doposition in middle ear, in pars flaccida, can be acquired or congenital Ball of skin keeps growing, can erode ossicles Etiologies congenital, chronic eustachian tube dysfunction with retraction or perforation Rx: surgical excision of cholesteatoma & all of the debris Ear Exam: L hand with L ear, R hand w. R ear Stand behind patient, your hand resting on their zygomatic arch Otoscope held upside down, pointy end facing patient How to tell which side of ear: MALLEUS at 2:oo = R ear, 10:00 = L ear ENT Nose Hx: rhinorrhea, congestion, epitaxis (U/L, B/L), trauma, duration, medications (chronic afrin), allergy, adenoid removal Anatomy: nasal turbinates humidify air & remove debris, nasal lacrimal duct drains into inferior meatus, Exam: Inspect the external nose, look for asymmetry or deformation Test for nasal obstruction by blocking one nostril at a time and asking the patient to breathe in Look inside the nose with either a large otoscope speculum or with a nasal speculum and headlight Touch nose edge, go in (can tilt head back slightly), then look around Nasal mucosal color, crusting, swelling, exudate Nasal septal deflection, perforation (cauterization, nose picking, nasal packing, afrin, granulomatous disease), crusting, polyps Normal: pink, dense [Polyps are clear, jelly-like] Sinuses Transillumination (one brighter than other) Percussion: maxilla & frontal, do L then R looking for symmetry, use tip of finger & hit at 90º movement only at the wrist ENT Mouth & Pharynx Anatomy: Lips – muscular folds, entrance to mouth Gingiva – mucosa, firmly attached to teeth and maxilla or mandible Labial frenulum – connects lips and gingiva Alveolar mucosa – mucosa adjacent to gingiva Labial mucosa – mucosa of the inner lip Tongue [CN XII paralysis – to same side] Uvula [CN X paralysis = to opposite side] Teeth (32 adult) Lingual frenulum Wharton’s ducts (submandibular) Palate – hard and soft Buccal mucosa – lines the cheeks Stenson’s ducts (parotid) Tongue Anatomy: Circumvallate papillae (Large, v-shaped pattern in posterior tongue, taste via CN IX to nucleus solitarius) Foliate papillae (Lateral tongue) Filiform papillae (No taste function) Fungiform papillae (Diffuse, taste via lingual nerve (V3) to chorda tympani and nucleus solitarius) ENT Mouth & Pharynx Exam Ask patients to remove dentures Look at the color of the lips, oral cavity Grasp the tip of the tongue with gauze to inspect the sides and posterior tongue Palpate the body and base of the tongue Ask patient to open the mouth, leave the tongue in and say “ah” (or with children, ask them to “pant like a puppy”) Use a tongue blade to press down the anterior half of the tongue ENT Tongue Disease: Fissured tongue – dry, cracked Geographic tongue Atrophic glottis – tongue more red, smooth, lack papilla Anemia, pellegra, Vit B/folate/Fe deficiencies, Celiac & Lichen planus Ankyloglossia – tongue tied, frenulum tethers tongue Mouth Disease: Oral thursh: white placks on mucus membrane (Candida albicans) Leukoplakia: white plaque (precancerous lesion, hyperkeratotic lesions), <10% carcinoma, from irritation Chancer sore: shallow ulcer, painful, tingling sensation from tissue injury, Celiac or Crohn’s disease Cold sore: outside on lips, Herpes simplex virus – exaberated by sun, stress, hormones Oral Pemphigus – autoimmune bollus disease Nikolsky sign: top layer of lesion can be rubbed off w. light pressure Tonsilitis: red swollen w. white spots Monotonsilitis – Epstein barr virus, both are covered in white, palate petechiae, hepatomegaly & jaundice Ludwig’s Angina : dental infection in floor of mouth, requires surgical drainage of abscess ENT Exam Head Symmetry, trauma, palpate for tenderness/lesions/deformity Facial expressions to test for CN VII (facial n.) – compare symmetry [UMN lesion(central) – contralateral lower portion of face; LMN lesion(peripheral) – ipsilateral half of face] Test orbicularis oculii m. – patient closes eyes and attempts to keep them closed as you pull up on their eyebrows Palpate face with tissue to test CN V (trigeminal n.) sensory portion, have patient clench their teeth to test CN V motor Patient’s eyes closed, look for symmetry between sides, don’t do angle of jaw [innerv. Great auricular n.) Sinuses: transillumination (dullness = sinusitis), palpation (apply firm pressure w. thumbs simultaneously for tenderness), percussion (tip of middle finger at 90º over frontal & maxillary sinuses; pain/discomfort = sinusitis ) ENT Exam Nose Check symmetry of breathing thru nose , ask to inhale (pain?) block one nostril at a time Hold speculum like a pencil, edge on tip of nose, look in then proceed into nose, move speculum around to visualize parts of nose Ear External ear inspection, behind ear – look for symmetry, piercings Adult: pull ear up & back, Child: pull ear down & back Hold speculum upside-down, your hand resting on their zygomatic arch, place speculum in until can’t see tip then look inside and proceed… visual canal & TM (superior inferior & anterior posterior) Malleus location: 2:00 – R ear, 10:00 L ear If whisper & finger rub tests okay, don’t need to go further Dysfunction: use 512Hz tuning fork for Weber (lateralization, conduction loss in louder ear, sensory hearing loss louder in better ear) & Rinne (sensory hearing loss AC > BC, conductive hearing loss BC=/> AC) ENT Exam Mouth/Throat Outside first Buccal area – anterior posterior Palpate for masses within the skin of cheek, floor of mouth Remember which finger you used so you don’t place that wet finger on patient’s face when switching sides !! Teeth – upper then lower Hard palate, soft palate Uvula CN X lesion – uvula deviates to OPPOSITE side of lesion Tonsils Pharynx Gag reflex : sensory stimluation via CN IX, motor response via CN X Tongue – top & under CN XII lesion – tongue deviates to SAME side as lesion Gums ** Always say please & thank you! ** Vitals Review BP: <120/<80 Shirt off, place cuff above antecubital fossa lined up with brachial artery (find via palpation – more medial side) Find radial pulse, pump quickly to 100 then increments of 10 until pulse is obliterated , deflate quickly Reinflate to that number + 20 Slowly deflate, 1st sound: systolic, 2nd sound: diastolic Sounds of Korotkoff: intial tapping, sounds increase intensity, hits max, sounds muffled then disappear Ausculatory gap: period of silence during ascultation where the first beat is heard, period of silence follwed with a return of audible pulse then second disappearance being diastolic RR: 12-20; depth, pattern Pulse: 60-100bpm, normal 2/4 strength, rhythm Temp: 98.6ºF BMI : healthy 18.5-24.9 (kg/m2) Dermatology Skin types 1: always burn easily, never tans, 2: burns easily, tans slightly 3: sometimes burn, tans gradually & mod. 4: burns minimally, always tans well 5: burns rarely, tans deeply 6: almost never burns, deeply pigmented Pallor = reduced oxyhemoglobin, Hypopigmentation – lack of sun exposure Brown – pituitary or adrenal disorder, hemochromatosis Skin mobile in certain directions – follow directions for best cosmetic results (O to T closing of subcutaneous sutures) Most common skin cancer – basal cell carcinoma [white n dome shaped] , second most squamous cell carcinoma [scaly red] ; melanoma [ABCDE] Nails Paronychia – infection Vertical split – damage to the matrix Onychomycosis – fungal infection Onycholysis – nail splitting Eye: Drusen: small collections found on the retina & optic n. often occuring w. macular degeneration & again Exudates: fluid collection sin the retina resulting from damaged blood vessels Retinopathy: non-inflammatory pathology of the retina Mouth Black hairy tongue – poor oral hygeine, thursh, antibiotic use Geographic tongue – normal variation Ear Insufflation: assessment of the mobility of the TM in the evaluation of fluid & middle ear pressures by forcing air against it through the use of an insufflation bulb attached to an otoscope