LPN-C - Faculty Sites
advertisement

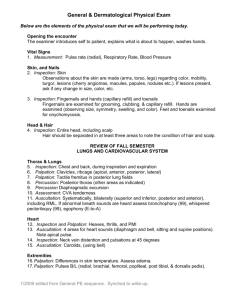
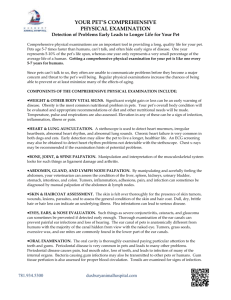
Head-to-Toe Assessment Unit One Head-to-toe assessment review Objective One Demonstrate head to toe assessment of the adult client Physical Examination Techniques Inspection = observation of the client (may at times include use of penlight, otoscope, and/or ophthalmoscope) Palpation = use of touch to assess client Use light pressure first to assess body surface Next use deep palpation to assess underlying structures Assess areas of pain/tenderness/discomfort last Percussion = tapping fingers on the client’s skin using short strokes to assess underlying structures to determine size/density/location Auscultation = use of hearing to assess client Types of Percussion and Auscultation Percussion - Direct percussion involves tapping lightly with the pads of the fingers directly on the client’s skin Indirect percussion involves use of both hands; strike the stationary finger like a hammer to produce the best sound Auscultation - Direct auscultation involves listening to the client without using an assistive instrument (i.e. wheezing, chest congestion) Indirect auscultation involves listening to the client with the use a stethoscope Assessment of 5 Percussion Notes Flatness = soft intensity, high pitch, short duration Heard over solid areas (muscle) Dullness = medium intensity, medium pitch, medium duration Heard over fluid-filled areas Resonance = loud intensity, low pitch, long duration Normal lung sound Hyper resonance = very loud intensity, lower pitch, longer duration Heard over hyperinflated areas (emphysema) Tympany = loud intensity, high pitch Heard over air-filled areas (gastric air bubble) General Survey *Begins at first contact with the client and continues throughout the exam *Provides an overall impression of the client/client system Appearance and behavior Appears stated age Speech/behavior appropriate to developmental stage Facial expressions Physical/emotional distress Skin color Vision and hearing Glasses, hearing aid, etc General Survey (cont’d) Speech Appropriate, logical Tone, speed, and clarity Vocabulary/grammar Body type and posture Body size/build Mobility, gait, and coordination Physical deformities Range of motion Dress, grooming, and hygiene Poor hygiene/unkempt Manner of dress appropriate for climate General Survey (cont’d) Mental status Level of consciousness Orientation Mood, affect Affect is the emotional state as it appears to others. Mood is the emotional state as described by the patient. Observe the patient's facial expression. No part of the body is as expressive as the face. Feelings of joy, sadness, fear, surprise, anger, and disgust are conveyed by facial expression. Facial expressions generally are not consciously controlled. Interaction Vital signs T/P/R and BP Pain assessment Allergies Height and weight Nutritional status Unexplained weight loss Skin Assessment Skin characteristics Temperature Compare upper and lower extremities, and bilaterally Excessive warmth may indicate fever, whereas excessive coolness may indicate poor circulation, shock, or hypothyroidism Moisture Should be warm and dry (but excessively dry skin may indicate dehydration) Color Varies per age, culture, ethnicity Mongolian spots = blue-black areas that are sometimes present on the lower back or buttocks of African American, Native American, and Asian babies Capillary hemangiomas (‘stork bites’) = small, irregular pink-red areas present around the face/neck of newborns Common Skin Color Variations Color Variation Description Significance Pallor Loss of pink/yellow tones or extreme paleness in light-skinned clients Loss of red tones in darkskinned clients Poor circulation, low hemoglobin level Assess via oral mucosa, conjunctiva, nail beds, soles of feet, palms of hands Cyanosis Blue-gray coloration of the skin; ashen Central cyanosis is R/T hypoxia May be seen in extremities after exposure to extreme cold Jaundice Yellow-orange cast to the skin Associated with liver disorders Assess via sclera, oral mucosa, palms and soles Flushing Widespread, diffuse area of redness Results from fever, excessive room temperature, sunburn, polycythemia, vigorous exercise Erythema A reddened area Associated with rashes, skin infections, prolonged pressure on the skin Ecchymosis Bruised (blue-green- Bruising may indicate physical abuse Petechiae Extravasation of blood into the skin May be associated with a disorder or medication yellow) area Tiny, pinpoint red or reddish-purple spots Skin Assessment (cont’d) Skin characteristics (cont’d) - Texture Should be smooth and soft May be affected by exposure, age, endocrine disorder, and impaired circulation Turgor Refers to the elasticity of the skin, and indicates hydration status Skin that takes 3 seconds or longer to return to its original position is termed ‘tenting’, and indicates dehydration Lesions Primary = result of disease or irritation Secondary = develops from primary lesions as a result of continued illness, exposure, injury, or infection Evaluate for size, shape, pattern, tenderness, pain, etc Skin Nodule--a solid mass extending into the dermis. (2) Tumor--a solid mass larger than a nodule. (3) Cyst--an encapsulated fluid-filled mass in the dermis or subcutaneous layer. (4) Wheal--a relatively reddened, flat, localized collection of fluid. An example is hives. (5) Vesicle--circumscribed elevation containing serous fluid or blood. An example is chickenpox. (6) Bulla-- large fluid-filled vesicle. An example is a second-degree burn. (7) Pustule--a vesicle or bulla filled with pus. An example is acne. Assessing Pitting Edema Trace Minimal depression noted when pressure applied +1 Application of pressure creates a depression of about 2 mm; no visible distortion; rapid return of skin to position +2 Application of pressure creates a depression up to 4 mm in depth that disappears in about 10-15 seconds +3 Application of pressure creates a depression of approximately 6 mm in depth that lasts about 1-2 minutes; area appears swollen +4 Application of pressure creates a depression up to 8 mm in depth that persists for about 2-3 minutes; area is grossly edematous Skin characteristics (cont’d) - Edema Excessive amount of fluid in the tissues Common in congestive heart failure, kidney disease, peripheral vascular disease, or low albumin levels Pitting edema is graded on a 0 to +4 scale Assessing the Hair Assess for color, texture, condition, and distribution Pediculosis = head lice infestation Nits (lice eggs) may be found on the hair shaft close to the scalp Alterations in hair distribution may be the sign of disease Alopecia = hair loss Chemotherapy Nutritional deficiencies Hirsutism = excess facial or trunk hair Endocrine disorders Steroid use Assess scalp (dandruff, dermatitis, psoriasis, etc) Assessing the Nails Condition of Nail/Nail Bed Indications or Concerns Pale or cyanotic beds Circulatory or respiratory disorders that result in anemia or hypoxia Half-and-half nails Appears as a distal band of reddish-pink that covers 20-60% of the nail; caused by low levels of albumin or renal disease Mee’s lines Appears as transverse white lines in the nail bed; results from severe illness Splinter hemorrhages Small hemorrhages under the nail bed that are associated with bacterial endocarditis or trauma Black nails Related to blood under the nail--occurs after a local trauma White spots Zinc deficiency Clubbing Refers to an angle of the nail bed that is 180° or more (normal is 160°); associated with hypoxic states (i.e. chronic lung disease) Spooning Iron deficiency Thickened nails Poor circulation or fungal infection Brittle nails Hyperthyroidism, malnutrition, calcium and iron deficiency Soft, boggy nails Poor oxygenation Vital Signs Body temperature Wait for 15-30 minutes after the client smokes or eats/drinks something hot/cold before taking an oral temperature Respirations Count unobtrusively for 30 seconds if respirations are regular, and for 60 seconds if they are irregular Observe rate, rhythm, and depth of respirations Blood pressure Client should be seated with both feet on the floor Client should be inactive for 5 minutes before measuring Use correct cuff size, and support the client’s arm at the level of his heart Vital Signs (cont’d) Assess apical pulse Palpate 5th intercostal space at the midclavicular line for stethoscope placement Count for 60 seconds Note pulse rate, rhythm, and quality, as well as the S 1 and S2 heart sounds Assess radial pulse Make sure client is resting while assessing the peripheral pulse Palpate appropriate site, counting for 30 seconds if the pulse is regular, and for 60 seconds if the pulse is irregular Compare pulses bilaterally Assessing the Head Observe symmetry of features, facial expressions Abnormal facial features may indicate genetic or chronic disorder (i.e. Graves’ disease, hypothyroidism/myxedema, Cushing’s syndrome) Assess jaw motion for clicking, pain, or crepitus, which may indicate temporomandibular joint syndrome (TMJ) Measure head circumference if indicated Acromegaly, a disorder of excessive growth hormone, may result in enlarged head in adolescents and adults Microcephaly is an abnormally small head size that may accompany mental retardation Hydrocephalus may present in infants and children, indicating an accumulation of excessive cerebrospinal fluid Assessing the Eyes External structures PERRLA (pupils equal, round, reactive to light and accommodation) Conjunctiva: smooth, glistening , and ‘peach’ in color Sclera: smooth, glistening, and blue-white in color Cornea: transparent, smooth, and moist Visual acuity Snellen chart measures distance vision Myopia = diminished distance vision Near vision measured by having client read newsprint from a distance of 14 inches Hyperopia = diminished near vision Presbyopia = decrease in near vision due to the aging process Assessing the Ears Otic structures External ear = collects and conveys sound waves; protects the middle ear from the external environment Otitis externa = infection of the outer ear that may result in a painful auricle or tragus Middle ear = consists of the tympanic membrane, eustachian tube, and the ossicles; conducts sound waves from the external ear to the inner ear Otitis media = middle ear infection that may present as tenderness behind the ear Inner ear = hearing and equilibrium Cerumen (ear wax) should be present, but should not occlude the ear canal May be black, dark red, gray, or brown in color Assessing the Nose Sinus areas should be nontender upon palpation Nasal passages should be pink and moist, and free from drainage or lesions Septum should be symmetrical Assess client’s ability to breathe freely through both sides of the nose Sense of smell is diminished in older adults due to atrophy of olfactory nerve fibers Assessing the Mouth and Neck Buccal mucosa should be smooth, moist, and pink: Common Buccal/Oral Variations Condition of Mouth/Oral Mucosa Indications or Concerns Paleness Anemia or inadequate oxygenation Canker sores Painful vesicles that erupt with allergies and stress Gingivitis Red, swollen or spongy, bleeding gingiva with receding gum lines; tenderness may be present; this is a sign of periodontal disease Parotitis Inflammation of the parotid salivary gland Stomatitis Inflammation of the oral mucosa Leukoplakia Thick, elevated white patches that do not scrape off; may be precancerous lesions Thrush White, curdy patches that scrape off and bleed caused by a fungal infection Aphthous ulcers Small, painful vesicles with a reddened periphery and white/pale yellow base; caused by viral infection, stress, or trauma Mouth and Neck Assessment (cont’d) Mouth/lips should be symmetrical Assess for swelling or drooping Assess for difficulty swallowing Assess teeth for dentures, obvious caries, loose teeth Tongue should be moist, symmetrical, slightly rough, smooth, pink, and freely movable Abnormal findings include deviation from midline; glossitis (inflammation of the tongue); limited mobility; dry, furry tongue related to dehydration; black, “hairy” tongue associated with fungal infections; swelling, nodules, or ulcers Palpate neck for tenderness/nodules, thyroid Inspect for swelling, ROM Lung Assessment Alterations in respiratory rate Bradypnea = slow respirations (<10 breaths/minute) Tachypnea = fast respirations (>24 breaths/minute) Alterations in respiratory effort Dyspnea = labored breathing Orthopnea = inability to breath in the horizontal position Abnormal breath sounds Wheezes = high-pitched, continuous musical sounds Usually heard on expiration Caused by narrowing of the airways Rhonchi = low-pitched, continuous sounds Caused by secretions in the large airways Often clears with coughing Lung Assessment (cont’d) Abnormal breath sounds (cont’d) - Crackles = discontinuous sounds that may be high-pitched, popping sounds (fine crackles), or low-pitched, bubbling sounds (course crackles) Usually heard on inspiration Stridor = piercing, high-pitched sound Primarily heard during inspiration Indicates respiratory distress Stertor = labored breathing that produces a snoring sound Retraction refers to the visible sinking of tissues around and between the ribs, sternum, or clavicles due to respiratory difficulty Note clubbing, coughing, and signs of hypoxia Cardiovascular Assessment Observe the precordium (area of the chest over the heart) for pulsations or heaves Abnormal anywhere except at the 5th ICS MCL (‘point of maximal impulse’, or PMI) Associated with an enlarged ventricle Palpate for ‘thrill’ (vibration or pulsation) over the chest May indicate abnormal blood flow and/or presence of a heart murmur Assess circulation Palpate peripheral pulses Check capillary refill Assess Homan’s sign or calf tenderness Assess extremities for peripheral edema Cardiovascular Assessment (cont’d) Blood pressure Cuff width should cover approximately 2/3 of the length of the upper arm for an adult, and the entire upper arm for a child Incorrect cuff size can result in measurement error of up to 30mmHg Using a cuff that is too large is better than using one that is too small Use the popliteal artery if brachial arteries unavailable Systolic pressure may be 20-30mmHG higher in the lower extremities, but diastolic pressure should be the same Auscultate apical rate and rhythm Listen to apical pulse for full minute Compare apical pulse to radial pulses Assessment of the Extremities Assess for musculoskeletal abnormalities, as major deformities may affect posture and gait Kyphosis = accentuated thoracic curve Scoliosis = lateral ‘S’ deviation of the spine Lordosis = accentuated lumbar curve Assess balance and movement by having client tandem walking, heel-and-toe walking, deep knee bends, and hopping in place Assess coordination via finger-thumb opposition and having client run the heel of one foot down the shin of the other Movements should be smooth and controlled Extremity Assessment (cont’d) Joints should be smooth, nontender, warm to the touch, and of similar color to surrounding tissue Color changes may indicate inflammation or infection Assess effect on joint function Active ROM Passive ROM Crepitus = clicking or grating at the joint Assess muscle strength by applying resistance while client is performing active range of motion exercises Should be strong and equal bilaterally Test ‘hand grasp’ strength and ‘foot push’ strength Both should be equal bilaterally Assessment of the Genitourinary System The GI system consists of the external genitalia, rectum, urethra, bladder, kidneys, ureters, and prostate in males Circumcision = excision of the foreskin of the penis No longer recommended as routine practice Parental preference remains widespread Hernia = protrusion of the intestine or other organ Typically found in the inguinal area in males May cause pain and distention Hemmorrhoids = dilated, painful anal vessels Commonly seen in pregnancy, childbirth, constipation Assess for problems or changes in voiding Objective Two Document findings by narrative charting Narrative Charting Tells the story of the patient’s experience in a chronological format Goal = track client’s changing health status and progress toward positive outcomes Especially useful in constructing a timeline of events (i.e. cardiac arrest, etc) Requires the writing out of the details of the patient’s care in sequence Be sure to organize your thoughts prior to beginning your documentation, as it can be easy to ramble in narrative charting Unit Two Physical assessment techniques for the lungs and abdomen Objective One Demonstrate the assessment technique of light palpation and percussion to abdomen Examination of the Abdomen Inspect and auscultate the abdomen first in order to avoid stimulating/altering bowel sounds through percussion/palpation; bladder should be emptied prior to examination Auscultate bowel sounds in all 4 quadrants of the abdomen Discontinue NG suction (or clamp tube) if indicated Absent bowel sounds = no sound auscultated after listening for 5 minutes Hypoactive bowel sounds = very soft and infrequent (i.e. 1 sound per minute) Hyperactive bowel sounds = loud, rushing sounds occurring every 2-3 seconds Examination of the Abdomen (cont’d) Palpation of abdomen Use light palpation (pads of fingertips) to evaluate for tenderness and guarding, superficial masses Involuntary rigidity of the abdominal muscles may indicate peritoneal inflammation Use deep palpation to assess organs (this is an advanced technique that is not usually performed by staff nurses) Liver border should be smooth and free of masses Should not be able to palpate the spleen Abdominal percussion should be primarily tympanic Liver should be dull over right MCL Stomach should be tympanic at left lower anterior ribcage Spleen should be dull near left 10 th rib posterior to MAL Objective Two Demonstrate the assessment technique of percussion of the thorax and abdomen Examination of the Thorax Thorax = formed by the ribs, sternum, and vertebrae; protects the heart, lungs, and great vessels Assess with client in sitting position Observe sternal angle Rib slope should be less than 90° Estimate chest diameter Anteroposterior diameter should be twice the size of transverse diameter ‘Barrel chest’ (equal diameters) often seen with COPD Osteoporosis may shorten length of spine, pushing ribs forward and downward Light palpation of the lungs (perform both anterior and posterior assessment) Assess symmetry of respiratory movement by having client inhale deeply while grasping the lateral ribcage with thumbs level to the 10th ribs Examination of the Thorax (cont’d) Palpation of the lungs (cont’d) -- Assess for tactile fremitus by having client repeat the words ‘99’ while using palm of hand to palpate chest and back Identify areas of increased or decreased fremitus Fremitus is decreased (or absent) if the bronchus is obstructed or there is fluid in the pleural space Fremitus is increased near large bronchi and over consolidated lung tissue (i.e. pneumonia) Percussion of the lungs Assess if underlying tissues are air-filled, fluid-filled, or solid Identify level of diaphragmatic dullness bilaterally during respiration per posterior percussive assessment Have client fold arm across chest and percuss across the top of each shoulder to identify lung apex Percuss symmetrical areas of lung while moving down client’s back Percuss areas along the sides beneath the scapulae and down the middle of client’s back Examination of the Thorax (cont’d) Percussion of the lungs (cont’d) -- Systematically move down the chest wall for anterior percussion assessment Should percuss dullness over the heart (left of the sternum from the 3rd to the 5th interspaces) Dullness replaces resonance when fluid or solid tissue replaces air Abnormally high dull sounds indicate pleural effusion or atelectasis Only a large amount of pleural effusion can be detected per anterior percussion because fluid displaces posteriorly when client is in the supine position Identify upper border of the liver by percussing dullness to the right of the thorax Identify tympanic gastric air bubble via percussion to the left of the thorax Unit Three Physical assessment techniques for the eye, ear, and nose Objective One Demonstrate the proper use of the ophthalmoscope Examination via Ophthalmoscope Perform examination in a darkened room Switch on ophthalmoscope light; turn lens disc to 0 Keep index finger on lens disc to facilitate refocusing during assessment; use right hand when examining client’s right eye, and left hand when examining client’s left eye Use large round beam (0) for large pupils Use small round beam for small pupils Use green/red beam to detect lesions May use thumb of opposite hand on client’s eyebrow to guide movement, and to gently ‘lift’ upper lid if needed Have the client look straight ahead at a specific point on the wall; hold scope firmly against your own face with your eye directly behind the sight hole Hold scope 15 inches away, and about 15˚ lateral to client’s line of vision; shine beam of light on the pupil Ophthalmoscopic Exam (cont’d) Identify optic disc Should be yellowish orange, oval or round Should note branching of vessels away from the optic disc, and progressive enlargement of vessel size as the vessels approach the disc Disc outline should be clear Lens should be transparent Assess for the ‘red reflex’ (orange glow) Absence may indicate cataract, detached retina, or artificial eye Keep light beam focused on the red reflex as you move ophthalmoscope closer to the pupil Identify arterioles and veins Arterioles are light red, smaller, with bright light reflex Veins are dark red, larger, with absent light reflex Ophthalmoscopic Exam (cont’d) Adjust lens disc Use clear glass lens for normal-sighted client Use lens with longer focus and rotate lens disc counterclockwise (minus diopters, or red numbers) for nearsighted client Rotate lens disc clockwise (plus diopters, or black numbers) for farsighted client Rotate progressively to +10 to +12 diopters to focus on the anterior structures of the eye Observe macular area (which is responsible for central vision) by having client look directly into the beam Identify retinal abnormalities Flame-shaped hemorrhages may indicate hypertension Large, horizontal line may indicate preretinal hemorrhage Tiny red spots are indicative of diabetic retinopathy Glaucoma Cataract Retinal Detachment Conjunctivitis Stye Diabetic Retinopathy Objective Two Demonstrate the proper use of the otoscope Otoscopic Examination Ear Assessment Perform examination in a darkened room Use the largest speculum the ear canal can accommodate Have the client tilt head toward the side not being examined Pull the helix up and back for adults, and down and back for children under the age of 5 May be painful in clients with acute otitis externa Insert speculum into outer 3rd of the ear canal; gently manipulate position to visualize the entire drum Observe for wax build-up, discharge, foreign body, redness or edema Assess for ‘cone of light’ and bony landmarks (i.e. the ‘handle’ and a portion of the malleus) Nasal Assessment Use short, wide nasal speculum Observe lower portions of the nose, then the upper portions Otoscopic Examination (cont’d) Assessing the Nose (cont’d) -- Use short, wide nasal speculum Observe lower portions of the nose, then the upper portions Assess the nasal mucosa Should be slightly more red than oral mucosa Observe for edema, exudates, or bleeding Inspect the nasal septum for bleeding or deviation (deviated septum is common in clients with chronic allergies, history of broken nose, etc) Observe the inferior and middle turbinates and middle meatus for edema, exudates, and polyps; note color http://www.brooksidepress.org/Products/Nursing_Fu ndamentals_II/lesson_6_Section_1A.htm Objective Three Assess the anatomical structures visible with the ophthalmoscope/otoscope (*Lab Practice)