Kathy Baule's - AANN Northern Illinois Chapter
advertisement
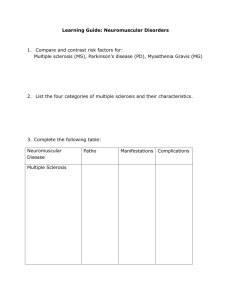
Infections of the Nervous System Kathy Baule RN, MSN, APN, CNSBC-CCRN, CNRN, RNFA Brain Abscess • Pathogenic– can happen in any individual • Opportunistic—can happen in individuals with a compromised immune system Abscesses--Incidence • • • • • Is 1-2% of SOL in brain (USA) Is 8% (INDIA) Antibiotic have helped change the incidence Lastly increased incidence because of opportunistic infection in immune compromised patient . http://www.medicalnewstoday.com/articles/185614.php Risk Factors • Congenital heart disease • Pulmonary AVM and AVFs as seen in hereditary hemorrhagic telangiectasia (HHT) • Bacterial Endocarditis (IV drug abuse) • Lung Infections Lung abscess Bronchiectasis Empyema • Dental Abscess • Systemic Sepsis Brain Abscess •Microorganism from remote site of infection •Multiple and deeply located •Mostly located in the frontal and parietal lobe •Primary include skin pustule, pulmonary infection, diverticulitis •Most common type of CHD •Brain abscess in CHD are generally solitary Penetrating trauma : Penetrating trauma are seen occur soon or after years from trauma. Contaminated bone fragments and debris provide a nidus for infection (A nidus is a breeding place where bacteria, parasites, and other agents of a disease lodge and develop) Sharp Stabbing Headache Penetrating Injury with Retained Object Penetrating Injury with Retained Object Brain Abscess Amyotrophic Lateral Sclerosis Disrupts the function of the motor neurons causing: • Rapid progression of weakness • Muscle atrophy • Muscle spasticity • Dysarthria (problems speaking) • Dysphasia (problems swallowing) • Dyspnea (problems breathing) Amyotrophic Lateral Sclerosis Pathology • Degeneration and death of motor nerves ▫ Upper Motor Neuron within brain/spinal cord ▫ Lower Motor Neurons leaves brain (stem)/spinal cord • Relatively spared ▫ Eye movements and bowel/bladder function Motor Neuron Disease Terminology Lower motor neuron Progressive Muscular Atrophy Upper motor neuron Amyotrophic Primary Lateral Lateral Sclerosis Sclerosis Amyotrophic Lateral Sclerosis Clinical Presentation • Asymmetric Weakness – most common • Onset single limb or bulbar • Local spread then regional spread ▫ Bulbar, cervical, thoracic, lumbosacral • Fasciculations Amyotrophic Lateral Sclerosis • Amyotrophic lateral sclerosis (ALS) is a rapidly progressive, invariably fatal neurological disease that attacks the nerve cells (neurons) • Responsible for controlling voluntary muscles (muscle action we are able to control, such as those in the arms, legs, and face). • The disease belongs to a group of disorders known as motor neuron diseases, which are characterized by the gradual degeneration and death of motor neurons. Amyotrophic Lateral Sclerosis Diagnosis • Two experienced Neurologists Laboratory Studies No study to prove or disprove Look for an alternate diagnosis Amyotrophic Lateral Sclerosis Prognosis • Variable – difficult to predict in an individual patient • 50% live 3-4 or more years • 20% live 5 or more years • 10% live 10 or more years • Occasional patients live 20 years Amyotrophic Lateral Sclerosis Treatment • Bulbar onset ▫ Prolonged survival ▫ Improved muscle strength • Entire population ▫ Prolonged survival ▫ No effect on effect on decline in muscle strength • Prolonged survival an average of 2-3 months AIDS • HIV is a virus spread through body fluids that affects specific cells of the immune system, called CD4 cells, or T cells. Over time, HIV can destroy so many of these cells that the body can’t fight off infections and disease. When this happens, HIV infection leads to AIDS. Anyone Can Get HIV • The Centers for Disease Control (CDC) estimates 1.1 million people age 13 and older are infected with HIV, and 50,000 people are newly infected each year. Anyone can be infected with HIV. • In 2010, men who have sex with men accounted for 63% of new infections, and women accounted for 20% of new infections. The incidence of HIV among African-Americans is about 8 times as high as in whites. • http://www.cdc.gov/hiv/library/factsheets/index.html You Can Have a Baby if You Are HIVPositive • Pregnant women who are HIV positive can pass the HIV virus to their babies. It can happen during pregnancy, during vaginal childbirth, or while breastfeeding. • However, if the mother receives treatment with antiretroviral drugs during pregnancy, has a Csection delivery, and avoids breastfeeding, she can greatly reduce the risk of passing the infection on to her baby. • http://www.cdc.gov/hiv/library/factsheets/index.html HIV-Infected patients • Dementia • Cerebral signs and symptoms are the most common • Global cerebral disease can present with altered mental status or generalized seizures • Whereas focal disease often produces hemiparesis, hemisensory loss, visual field cuts, or disturbances in language use. HIV-Infected Patients • Fungal, viral, and mycobacterial meningoencephalitides are the most common causes of global cerebral dysfunction, and progressive multifocal leukoencephalopathy (PML), primary CNS lymphoma, and toxoplasmosis account for the majority of focal presentations. • http://hivinsite.ucsf.edu/InSite?page=kb-04-01-02#S1.1X HIV • Availability of effective antiretroviral regimens has been associated with a dramatic decline in incidence and severity of opportunistic infections of the CNS. • Unfortunately, antiretroviral regimens have not demonstrably decreased the prevalence of PML, and the incidence among individuals with higher CD4 counts may be increasing. • The prognosis has improved dramatically, with long-term remissions now fairly common among patients receiving antiretroviral therapy. • http://hivinsite.ucsf.edu/InSite?page=kb-04-01-02#S1.1X Bell’s Palsy • WHAT IS BELL'S PALSY? Bells palsy is a condition that causes the facial muscles to weaken or become paralyzed. It's caused by trauma to the 7th cranial nerve, and is not permanent. • WHY IS IT CALLED BELL'S PALSY? The condition is named for Sir Charles Bell, a Scottish surgeon who studied the nerve and its innervation of the facial muscles 200 years ago. • HOW COMMON IS BELL'S PALSY? Bells palsy is not as uncommon as is generally believed. Worldwide statistics set the frequency at just over .02% of the population (with geographical variations). In human terms this is 1 of every 5000 people over the course of a lifetime and 40,000 Americans every year. • IS BELL'S PALSY ALWAYS ON THE SAME SIDE? The percentage of left or right side cases is approximately equal, and remains equal for recurrences. • IS THERE ANY DIFFERENCE BECAUSE OF GENDER OR RACE? The incidence of Bells palsy in males and females, as well as in the various races is also approximately equal. The chances of the condition being mild or severe, and the rate of recovery is also equal. Bell’s Palsy • Sudden weakness of half of the face • The smile is one-sided and the eye on the weak side resists closing. Bell’s Palsy’s Causes • Unknown Causes • Believed to be a result of swelling and inflammation of the nerves that control the muscles • Could be a reaction that occurs after a viral reaction Facial Nerve • Controls the muscles on one side of the face • Difficulty blinking, closing and facial expression such as smiling and frowning • Other symptoms include drooping of the eyelid and corner of the mouth, drooling, dryness of eye or mouth, impairment of taste and excessive tearing in one eye Bell’s Palsy Case Study • C.B., is a 19 year old female university student with complaints of dry left eye. She had taken out her contacts and supplemented the dryness with saline drops. As the time progressed over night he had noticed difficulty blinking with pain in the left ear. He had developed complete left facial paralysis. The symptoms began in August and with gradually recovery beginning two months post onset. She was seen by a Neurologist who confirmed the diagnosis of Bell’s palsy. • She was referred for facial neuromuscular retraining nine months post onset of symptoms. Initial evaluation revealed slightly increased resting tone, complete eye closure, slightly decreased smile with mild synkinesis noted. Attempted lip movements were accompanied by severe synkinesis of orbicularis oculi which resulted in almost complete eye closure (Figures 5, A-D). • The home program consisted of small selective movements practiced with inhibition of synkinesis. She attended clinic sessions once a month for the first six months and demonstrated a significant reduction in synkinesis during that time (Figures 5, E-H). Clinic visits decreased to once every three months with continued good compliance. The entire course of neuromuscular retraining lasted 18 months with improvements noted in volitional and spontaneous excursion of movement. The patient continued to demonstrate mild synkinesis of orbicularis oculi during broad, spontaneous laughter. She was extremely motivated and compliant with the home program, and was pleased with the treatment outcome. Photographic evaluation 12 months post left facial paralysis resulting Pre-treatment: Resting tone (A), smile (B), pucker (C), pout (D). Note normal resting tone, decreased excursion of left smile with mild synkinesis of left OCS/OCI and severe synkinesis of left OCS/OCI during lip movements. Reevaluation of same movements six months after beginning facial NMR (EH). Note improved excursion of smile and decreased synkinesis around eye with improved symmetry. Encephalitis • Most diagnosed cases of encephalitis in the United States are caused by enteroviruses, herpes simplex virus types 1 and 2, rabies virus (this can occur even without a known animal bite, such as for example due to exposure to bats), or arboviruses such as • West Nile virus, which are transmitted from infected animals to humans through the bite of an infected tick, mosquito, or other blood-sucking insect. • Lyme disease, a bacterial infection spread by tick bite, more typically causes meningitis, and rarely encephalitis. Encephalitis: Symptoms • Fever, headache, seizures, change in behavior or confusion and in extreme cases, brain damage, stroke or even death • Infection of the meninges, the membranes that surround the brain and spinal cord Infectious Causes • Bacteria, viruses, fungi and parasites • Many of these affect healthy people • For others, environmental and exposure history, recent travels or immunocompromised states (HIV, diabetes, steroids and chemotherapy) • Non-infectious causes: autoimmune causes and medication Treatment for mild cases • • • • Can be mistaken as the flu, mainly consists of: Bed rest Plenty of fluids Anti-inflammatory drugs— such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, others) — to relieve headaches and fever. • Antiviral drugs • Cases due to certain viruses usually require intravenous antiviral treatments. • Antiviral drugs commonly used to treat encephalitis include: ▫ Acyclovir (Zovirax) ▫ Ganciclovir (Cytovene) ▫ Foscarnet (Foscavir) Demyelinating Polyneuropathy Guillain-Barre • Guillain-Barre: is an acute inflammatory disease of the peripheral nerves. An autoimmune attack on the myelin (insulation around individual nerve fibers, called axons) results in demyelination. Loss of myelin can occur in sensory, motor or autonomic nerves. GB • After the first clinical manifestations of the disease, the symptoms can progress over the course of hours, days, or weeks. Most people reach the stage of greatest weakness within the first 2 weeks after symptoms appear, and by the third week of the illness 90 percent of all patients are at their weakest. • http://www.medicinenet.com/guillain-barre_syndrome/page2.htm GB • Approximately one third of patients require admission to an ICU, primarily because of respiratory failure. • After medical stabilization, patients can be treated on a general medical/neurologic floor, but continued vigilance remains important in preventing respiratory, cardiovascular, and other medical complications. • Patients with persistent functional impairments may need to be transferred to an inpatient rehabilitation unit. GB Treatment • Immunomodulatory treatment has been used to hasten recovery. Intravenous immunoglobulin (IVIG) and plasma exchange have proved equally effective. • Corticosteroids (oral and intravenous) have not been found to have a clinical benefit in GBS. • Consequently, this class of drugs is not currently employed in treatment of the syndrome. • http://emedicine.medscape.com/article/315632-treatment Demyelinating Polyneuropathy CIDP • Chronic Inflammatory Demyelinating Polyneuropathy(CIDP) is a neurological disorder characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder, which is sometimes called chronic relapsing polyneuropathy, is caused by damage to the myelin sheath (the fatty covering that wraps around and protects nerve fibers) of the peripheral nerves CIPD • Is common in young adults and is more prevalent in males • Presents with numbness and tingling beginning in the toes and the fingers, weakness in the arms and legs; loss of deep tendon reflexes; fatigue and abnormal sensations CIPD • 51-year-old female who has been treatment for GuillainBarre and CIDP. Her symptoms began on June 2001. She was having fatigue episodes with associated lower extremity weakness. The weakness was progressive in nature until she reached a point that she could not walk. She has chronic weakness in the bilateral lower extremities with associated numbness, tingling, and burning pain. • She is under the care at the Mayo Clinic. Her pain management regimen is currently controlling her discomfort at a level she can complete her activities of daily living with periods of rest. She denies any bowel or bladder incontinence, but has been treated for diverticulitis. CIPD • She received IVIG weakly and Cellcept • She has areas of numbness and tingling and chronic pain issues. She is stable on MSIR and Lyrica • She continues to have numbness, tingling and burning pain • She has an ataxic gait, but is able continue her activities of daily living and is currently baby sitting daily. Demyelinating Polyneuropathy ADEM • Is a rare inflammatory demyelinating disease of the central nervous system. ADEM is thought to be an autoimmune disorder in which the body’s immune system mistakenly attacks its own brain tissue, triggered by an environmental stimulus in genetically susceptible individuals. ADEM • The diagnosis of ADEM is based on clinical and radiologic characteristics. • There is no specific biologic marker or confirmatory test to specifically identify the disorder • There is no scientific, randomized, or controlled data on the diagnosis and treatment of ADEM. • Decisions about the diagnosis and treatment of this disorder are based primarily on the opinions of experts http://myelitis.org/symptoms-conditions/acute-disseminated-encephalomyelitis/diagnosis/ ADEM • Post-infectious In approximately 50-75 percent of ADEM cases, the inflammatory attack is preceded by a viral or bacterial infection. • There have been a large number of viruses associated with these infections, including but not limited to: measles, mumps, rubella, varicella zoster, Epstein-Barr, cytomegalovirus, herpes simplex, hepatitis A, influenza, and enterovirus infections. • A seasonal distribution has been observed showing that most ADEM cases occur in the winter and spring. The inflammatory attack and neurological symptoms often begin within a couple of weeks after the viral or bacterial illness. http://myelitis.org/symptoms-conditions/acute-disseminated-encephalomyelitis/ ADEM • Considered when individuals develop multifocal neurologic abnormalities with confusion, excessive irritability, or altered level of consciousness (encephalopathy) • Especially if the onset of symptoms occurs within 1 to 2 weeks after a viral/bacterial infection or a vaccination. • Must rule out that there is a direct infection of the central nervous system as opposed to an infection that subsequently triggered the immune system to cause the attack • Should a direct infection be suspected, one is often placed on an antibiotic and/or acyclovir (an antiviral drug) to fight the infection http://myelitis.org/symptoms-conditions/acute-disseminatedencephalomyelitis/diagnosis/ Lumbar Puncture/ ADEM • This test is useful because evidence of inflammation is common in cerebrospinal fluid (CSF), with pleocytosis (increased white blood cell count) and/or increased protein concentration. • While this is common, sometimes the CSF can be normal. Additionally, although oligoclonal bands are nonspecific and are more often associated with Multiple Sclerosis (MS), they are sometimes also present in ADEM. http://myelitis.org/symptomsconditions/acute-disseminated-encephalomyelitis/diagnosis/ etimes also present in ADEM. MRI of the Brain and Spine • Abnormalities are best defined by T2-weighted images, FLAIR sequences, and contrast-enhanced MRI with gadolinium. Abnormalities on MRI usually vary in location. • Lesions associated with ADEM tend to be bilateral, but can also be asymmetric and are typically poorly marginated. • Multiple lesions in the deep and subcortical white matter are common, which is characteristic of demyelination (gray matter lesions sometimes accompany white matter lesions, especially among children). • While the number varies, multiple brain lesions are usually present. ADEM lesions are typically large (though smaller ones have also been seen) with diameters ranging from <5 mm to 5 cm. Additionally, brainstem and spinal cord abnormalities on MRI are common in ADEM. • In the spinal cord, there are typically large confluent intramedullary lesions that extend over multiple segments of the cord. MRI • In a situation where nonspecific cerebrospinal fluid abnormalities and MRI evidence of white matter lesions are present, it is important that other inflammatory demyelinating disorders be considered. • These include: Multiple Sclerosis Multiple (MS), Optic Neuritis Optic (ON), Transverse Myelitis (TM), and Neuromyelitis Optica (NMO). Treatment • IV Corticosteroids are the most common treatment for ON. Or high dose tablets. While corticosteroids have been effective in improving short-term visual recovery, they do not seem to affect the long-term outcome. • Lack of long-term benefit and the risk of potential side effects (including: insomnia, weight gain, and mood alterations), the use of corticosteroids is usually not advised. • However, there are specific situation period of impairment and are usually considered when a more rapid recovery is required (such as patients with severe bilateral visual loss or those with occupations that require normal visual acuity). • Unfortunately, there are currently no acute treatments that can reverse vision loss caused by ON. http://myelitis.org/symptoms-conditions/opticneuritis/acute-treatments-on/ Meningitis • Meningitis is a disease caused by the inflammation of the protective membranes covering the brain and spinal cord known as the meninges. The inflammation is usually caused by an infection of the fluid surrounding the brain and spinal cord. Meningitis • Bacterial meningitis is usually severe. While most people with meningitis recover, it can cause serious complications, such as brain damage, hearing loss, or learning disabilities. • There are several pathogens (types of germs) that can cause bacterial meningitis. Some of the leading causes of bacterial meningitis in the United States include Haemophilus influenzae (most often caused by type b, Hib), Streptococcus pneumoniae, group B Streptococcus, Listeria monocytogenes, and Neisseria meningitidis. • In the United States, about 4,100 cases of bacterial meningitis, including 500 deaths, occurred each year between 2003–2007. Viral Meningitis • Meningitis is an inflammation of the tissue that covers the brain and spinal cord. • Viral meningitis is the most common type of meningitis • Often less severe than bacterial meningitis • People usually get better on their own • However, infants younger than 1 month and people with weakened immune systems are more likely to have severe illness Myasthenia Gravis • Myasthenia gravis is a disease of skeletal muscle acetylcholine receptors. The chemical transmitter, acetylcholine (ACh) is unable to bind to the receptors (AChR) on the postsynaptic membrane to transmit the nerve impulse to muscle fibers to produce a muscle contraction Myasthenia gravis is a disease of skeletal muscle acetylcholine receptors. The chemical transmitter,) is unable to bind to the receptors (on the postsynaptic membrane to transmit the nerve impulse to muscle fibers to produce a muscle contraction severe with marked bulbar involvement Myasthenia Gravis • 64 year old female developed sudden on-set of left eye double vision and weakness in BLE. She was seen by local Neurologist without a definitive diagnosis. • Tensilon test: The test helps: • Diagnose myasthenia gravis • Tell the difference between myasthenia gravis and other similar brain and nervous system conditions • Monitor treatment with oral anticholinesterase drugs MG • She has notable ptosis ("drooping") of both eyelids after repeated blinking exercises. When smiling, she appears to be snarling. • Electromyographic testing revealed progressive weakness and decreased amplitude of contraction of the distal arm muscles • Both her symptoms and electromyographic findings were reversed within 40 seconds of intravenous administration of edrophonium (Tensilon), an acetylcholinesterase inhibitor (i.e. an "anticholinesterase"). • Blood testing revealed high levels of an antiacetylcholine receptor antibody in her plasma, and a diagnosis of myasthenia gravis was made. Myasthenia Gravis • There is no known cure for MG, but there are effective treatments available. Common treatments include medications, thymectomy and plasmapheresis. Spontaneous improvement and even remission may occur without specific therapy. • She was treated with steroids, Imuran and Methotrexate • She is currently taking Rituxan (4 doses IV every two years); she is weaning her steroids. MG • She was treated with with pyridostigmine bromide, which is a long-acting anticholinesterase drug, and was also started on prednisone, which is a corticosteroid drug. • She also underwent occasional plasmapheresis when her symptoms became especially severe. • She was given a prescription of atropine as needed to reduce the nausea, abdominal cramps, diarrhea, and excessive salivation she experienced as side effects of the anticholinesterase drug. Multiple Sclerosis • Is a disease with unpredictable symptoms that can vary in intensity. While some people only have fatigue and numbness, severe cases can cause paralysis, vision loss, and diminished brain function. • MS affects about 2.5 million people worldwide and affects women twice as often as men (National MS Society, 2012). MS • In multiple sclerosis (MS), damage to the myelin coating around the nerve fibers in the central nervous system (CNS) and to the nerve fibers themselves interferes with the transmission of nerve signals between the brain, spinal cord and the rest of the body. • Disrupted nerve signals cause the symptoms of MS, which vary from one person to another and over time for any given individual, depending on where the damage occurs. MS • Types of MS. Four disease courses have been identified in multiple sclerosis: relapsingremitting MS (RRMS), • primary-progressive MS (PPMS), • secondary-progressive MS (SPMS), and • progressive-relapsing MS. • Each of these disease courses might be mild, moderate or severe. MS treatment • Treatments for signs and symptoms • Physical therapy. A physical or occupational therapist can teach you stretching and strengthening exercises, and show you how to use devices that can make it easier to perform daily tasks. • Muscle relaxants. You may experience painful or uncontrollable muscle stiffness or spasms, particularly in your legs. Muscle relaxants such as baclofen (Lioresal, Gablofen) and tizanidine (Zanaflex) may help. • Medications to reduce fatigue. • Other medications. Medications may also be prescribed for depression, pain, and bladder or bowel control problems that are associated with MS. • Prion Disease • Prion diseases or transmissible spongiform encephalopathies (TSEs) are a family of rare progressive neurodegenerative disorders that affect both humans and animals. They are distinguished by long incubation periods, characteristic spongiform changes associated with neuronal loss, and a failure to induce inflammatory response. • CJD Encephalopathy • Disease, damage, or malfunction of the brain. In general, encephalopathyis manifested by an altered mental state that is sometimes accompanied by physical changes. • Toxic • Metabolic • PRESS PRES Presentation • Patients present with headache, seizures, encephalopathy and/or visual disturbance. PRES • Most commonly there is vasogenic oedema within the occipital and parietal regions (~95% of cases), perhaps relating to the posterior cerebral artery supply. • The oedema is usually symmetrical. Despite being termed posterior, • PRES can be found in a non posterior distribution, mainly in watershed areas, including within the frontal, inferior temporal, cerebellar and brainstem regions • There are three main imaging patterns: • holohemispheric at watershed zones • superior frontal sulcus • parieto-occipital dominance http://radiopaedia.org/articles/posterior-reversibleencephalopathy-syndrome-1 PRES • PRES is reversible when treatment is instituted early, delayed diagnosis and treatment can result in chronic neurological sequelae. • Early recognition and controlled of blood pressure and seizure is the main stay of treatment. • Anesthesiologist, intensivists and other physicians involved in the evaluation of patients with markedly elevated blood pressure, eclampsia, renal failure etc should presumed PRES and must be aware of the clinical spectrum of the associated conditions, its diagnostic modalities, and treatment. Thank you!!