Pheochromocytoma - Healthcare Professionals
advertisement

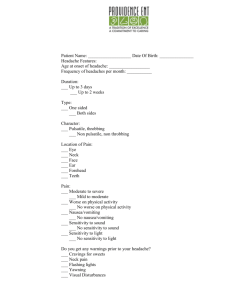
Endocrine CPC Tim Miller, MD 1/22/2008 Case CC: I have been having headaches HPI: Pt is a 33 year old Hispanic male seen for routine yearly follow up Reports headaches for 3 months Seen at walk-in clinic and diagnosed with migraines Midrin and Maxalt were not effective Case Headaches start behind both eyes and encompass his entire head Recently (past 2 weeks) headaches occur on a daily basis and are more severe Headaches mainly occur at night Seem to be worse with exertion Case Associated Signs/Symptoms Nausea Photophobia Phonophobia Roommate says he “looks pale” with attacks Sweats will accompany headaches, mainly at night Experiences “fluttering” in his chest and notes that his pulse is around 120 Case Pertinent Negatives No lacrimation No vision changes Location does not change Case PMHx: Seasonal allergies Eczema Positive PPD – currently on INH therapy NAFLD with elevated LFT’s (discovered prior to initiation of INH) Hypertriglyceridemia Case PSHx: None FH: Not given Meds: INH All: NKDA SocHx: Nonsmoker Occasional EtOH No drugs Entomology graduate student at Texas A&M Born in Cuba and moved to Texas to study Traveled to Peruvian rainforest for research within the last year Case Review of Systems: General: no weight loss HEENT: no vision/hearing changes, no odynophagia/dysphagia Pulmonary: no SOB, no cough Cardiovascular: no chest pain, (+) palpitations GI: no jaundice, no abd pain, no changes in bowel habits GU: no changes in bladder habits Case Physical Exam: BP 144/84 P 110 T 98.4 BMI 26 General: well nourished, healthy appearing male HEENT: NCAT, PERRLA, EOMI, no icterus, mm moist, conjunctiva pink Fundoscopic: no papilledema Neck: supple, no LAD, no bruits, no supraclavicular fat pad CV: tachycardic (110) and regular, no murmurs, gallops, or rubs Case Physical Exam cont: Resp: clear bilaterally, good resp effort Abd: mild TTP with deep palpation on the right, lateral to umbilicus, (+) BS, no HSM, no rebound/guarding Ext: no C/C/E Neuro: CN 2-12 intact, strength 5/5 x 4, no gait abnormalities Psych: normal mood and affect Skin: eczematous changes to palms and bilateral antecubital fossae Case Labs & Studies: CBC normal CMP normal other than ALT 131 Hepatitis Panel negative Ferritin normal Thyroid function tests normal 2-view CXR normal CT head w/wo contrast negative Problem List ACUTE Headache x 3 months Progressively worsening Looks pale with attacks Sweats with headaches Palpitations Hypertension Tachycardia Travel to Peruvian Rainforest CHRONIC Positive PPD INH Therapy Seasonal Allergies Eczema NAFLD Elevated LFT’s Hypertriglyceridemia Differential Diagnosis Chronic Headache Migraine Cluster Tension TB Meningitis CNS Neoplasm Hypertensive Headache Endocrine Headache Pheochromocytoma Cushing’s Disease Pituitary Adenoma Headache - Epidemiology Among the most common medical complaints Overall prevalence 12-16%; accounts for 1-2% of ER visits and up to 4% of outpatient office visits 90% of headaches fall into categories of migraine, cluster, and tension Headache - Classification Acute New onset or clearly different than previous headaches Often are a sign of serious illness Subarachnoid hemorrhage Meningitis Acute glaucoma Hypertensive encephalopathy Headache - Classification Subacute Occurs over a period of weeks to months May or may not be related to underlying systemic illness Recent subdural hematoma Subacute meningitis Primary or metastatic tumor Giant cell arteritis Optic Neuritis Headache - Classification Chronic Continues intermittently for years Usually has a benign cause Migraine Cluster Tension Sinusitis Dental Disease Headache – Approach to Diagnosis Age of onset Timing of pain Precipitating factors Characteristics of pain Location of pain Associated symptoms History of prior headaches and course of this type of headache Physical Exam Migraine Headache Unilateral and usually pulsatile Often associated with nausea, photo- and phonophobia Moderate to severe intensity 55% occur initially prior to age 20 Usually familial Auras occur in 10% of patients Most often occur in women Migraine Headache Clinical Presentation Classic Migraine (preceded by aura) Visual, noxious, or sensory alterations followed by intense unilateral throbbing headache Usually do not occur more frequently than weekly Last between 4 and 72 hours Common Migraine (lacks aura) Usually unilateral and throbbing Cluster Headache Clinical Presentation Brief, severe, constant, nonthrobbing headache Lasts 15-180 minutes without treatment Always unilateral Much more common in men Mean age of onset is 25 Episodes are separated by months or even years Cluster Headache Begins with sensation by the nose or behind the eye Ipsilateral lacrimation, conjuntival injection, or ptosis may occur Key to diagnosis is brevity of symptoms Tension Headache Clinical Presentation Lacks features of migraine or cluster Frequent (possibly daily), bilateral occipital, nonthrobbing Often a band distribution Rarely nausea, vomiting, or visual prodrome, although may occasionally have features of migraine Tension Headache? Women more common then men Secondary gain? Headache - Imaging Danger signs that indicate need for imaging Sudden onset of worst headache ever or headache that reaches full intensity in minutes Absence of similar terrible headaches in past Worsening pattern Focal neurologic signs or papilledema Fever Change in mental status or personality Rapid onset with strenuous exercise Presentation to any ER with headache Differential Diagnosis Chronic Headache Migraine Cluster Tension TB Meningitis CNS Neoplasm Hypertensive Headache Endocrine Headache Pheochromocytoma Cushing’s Disease Pituitary Adenoma CNS Tuberculosis 3 Categories TB Meningitis Intracranial Tuberculoma Spinal tuberculous arachnoiditis Account for 1% of all TB cases Quite rare in United States Fatal in 15-40% of cases, usually within 5-8 weeks Active TB outside the CNS is not necessary to make diagnosis Send CSF for acid fast smear, TB culture, and TB PCR Differential Diagnosis Chronic Headache Migraine TB Meningitis CNS Neoplasm Hypertensive Headache Endocrine Headache Pheochromocytoma Cushing’s Disease Pituitary Adenoma CNS Neoplasm Headache is a common symptom in patients with brain malignancies Worst symptom in half of patients Usually described as dull and constant, occasionally throbbing Typically tension-type (77%); can be migraine-type (9%), or other (14%)* Severe headaches are infrequent *Forsyth, PA, Posner, JB. Headaches in patients with brain tumors. Neurology 1993; 43:1678. CNS Neoplasm Other clues to malignant headaches 40% have nausea and vomiting Change in prior headache pattern Abnormal neurologic exam May worsen with maneuvers that increase the ICP (bending over, sneezing, coughing) Tend to be worse at night (vasodilatation from transient increase in PCO2) Typical location is bifrontal but may be generalized if ICP is increased Headache, nausea, papilledema ( ICP) Other signs of CNS malignancy include seizures, syncope, cognitive dysfunction, focal neurologic deficits Differential Diagnosis Chronic Headache Migraine CNS Neoplasm Hypertensive Headache Endocrine Headache Pheochromocytoma Cushing’s Disease Pituitary Adenoma Hypertensive Headache Routine essential hypertension has not been shown to directly cause headaches* Can lead to conditions that cause headaches Intracerebral or subarachnoid bleeding Sudden onset of severe headaches Hypertensive encephalopathy Insidious onset of headache, N/V, followed by restlessness and confusion, and eventually seizure and coma if not treated *Strovmer LJ, Vatten L, et al. Blood pressure and risk of headache. J Neurol Neurosurg Psychiatry 2002;72:463–6. Hypertensive Headache Law, et al studied whether blood pressure meds lowered headaches in a meta-analysis 94 randomized placebo-controlled trials using 4 major types of BP meds (thiazides, b-blockers, ACE-I, and ARB) Separated into treatment and placebo groups Average SBP fell by 9.4 and DBP fell by 5.5 in treatment groups 8% reported headaches in treatment groups and 12.4% reported headaches in placebo groups RRR 33% (P<.001) However, many observational studies do not support hypertension as a cause of headaches Law M, Morris JK, Jordan R, Wald N. Headaches and the treatment of blood pressure. Circulation. 2005; 112: 2301– 2306. Differential Diagnosis Chronic Headache Migraine Hypertensive Headache Endocrine Headache Pheochromocytoma Cushing’s Disease Pituitary Adenoma Cushing’s Disease Chronic excess of glucocorticoid Clinical features: Progressive obesity including moon facies, supraclavicular fat pad and buffalo hump Skin changes of easy bruisability and striae Osteoporosis Proximal muscle weakness Hypertension Headache in up to 47% of patients Pituitary Adenoma Microadenoma < 1 cm Macroadenoma > 1 cm Arise from anterior pituitary Secrete hormones depending on type of tumor (Prolactin, ACTH, GH) Clinical Presentation Visual defects are most common presenting symptom of nonfunctioning adenomas Bitemporal hemianopsia Headaches are common and nonspecific Pituitary apoplexy causes severe headache and diplopia and cranial nerve deficits Differential Diagnosis Chronic Headache Migraine Endocrine Headache Pheochromocytoma Cushing’s Disease Pituitary Adenoma Pheochromocytoma General Catecholamine secreting tumors of chromaffin cells arising from the adrenal medulla Epinephrine and norepinephinre; rarely dopamine Stimulate alpha and beta adrenergic receptors Approximately 0.2% of patients diagnosed with hypertension will have a pheochromocytoma Equal incidence in men and women Peak incidence between 3rd and 5th decade Catecholamines Epinephrine, Norepineprhine, and Dopamine secreted from the adrenal medulla Act on α1 (peripheral vasoconstriction) and α 2 receptors and β1 (heart rate and inotropy), β2 (muscle and liver vasodilatation) Effects of Catecholamines Increase force of cardiac contractility Increases heart rate (epi > norepi) Peripheral vasoconstriction Dilates bronchioles Glycogynolysis (mobilizing glucose) Increased metabolic rate Dilates pupils Inhibits non-essential processes such as GI motility Norepinephrine and epinephrine levels in human venous blood in various physiologic and pathologic states Cryer PE: Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system. N Engl J Med 1980;303:436. Pheochromocytoma Clinical Presentation Clinical Triad Episodic Headaches Sweating Tachycardia (or palpitations) Frequency ranges from multiple times per day to monthly Worsens with time and becomes more frequent Half will have paroxysmal hypertension and a third appear to have essential hypertension 5-15% present with normal blood pressure Pheochromocytoma – Clinical Presentation Headaches occur in 90% of symptomatic patients May be mild or severe and are variable in duration Sweating occurs in 60-70% of patients Other signs and symptoms Dyspnea Generalized Weakness Panic Attack Pheochromocytoma – Presentation May often be unmasked during routine procedure or drug administration Anesthesia induction Cold Medications Opiates Dopamine Antagonists Cocaine or TCA’s which inhibit catecholamine reuptake Childbirth Trauma Pheochromocytoma – Rule of 10’s 10% Bilateral 10% Malignant 10% Extra-adrenal 10% Calcify 10% Familial 10% Children Pheochromocytoma – Familial Conditions MEN 2a Pheochromocytoma Medullary Thyroid Cancers Parathyroid Tumors MEN 2b Pheochromocytoma Medullary Thyroid Cancers Neuromas Von Hippel-Lindau Cerebellar Hemangioblastomas Retinal Angiomas Renal Cell Carcinoma Pheochromocytoma Neurofibromatosis Café-au-lait spots Neurofibromas Pheochromocytoma Pheochromocytoma – Evaluation Which patients should be evaluated for pheochromocytoma? Patients with difficult to control hypertension Patients receiving more than 4 BP meds Patients with onset of htn before age 35 Patients with onset of htn after age 60 Patients with signs or symptoms of pheochromocytoma as mentioned before Patients with familial history of predisposing disorders Severe pressor response during anesthesia Pheochromocytoma – Lab Diagnosis Free plasma metanephrine level Screening Test for at risk patients 96% sensitive but 85% specific (better if drawn during an attack) Standard venipuncture test Pheochromocytoma – Lab Diagnosis Urinary catecholamines and metanephrines Confirmatory test 87% sensitive and up to 99% specific Must be collected in a 24-hour urine specimen Order metanephrines (best test), catecholamines, and vanillylmandelic acid (worst test) Ensure creatinine is measured to ensure adequacy Collect during or immediately after an attack if possible 2-3x increase in levels is diagnostic Pheochromocytoma – Lab Diagnosis Other diagnostic tests Clonidine Suppression Test Confirmatory test; 90% accurate Clonidine normally suppresses release of catecholamines centrally, but not from a pheo Administer Clonidine and measure plasma metanephrines before, and 3 hours after Levels will decrease in essential hypertension Levels remain increased in pheochromocytoma Chromogranin A level Increased in 80% of patients with pheochromocytoma Not specific for pheochromocytoma Pheochromocytoma – Imaging Imaging should only be obtained after biochemical diagnosis has been confirmed MRI has reported sensitivity of 100% for adrenal pheos Better than CT for picking up extra-adrenal tumors as well MRI can distinguish between incidentilomas on T2weighted images CT may miss tumors smaller than 1 cm Pheochromocytoma – Imaging MIBG Nuclear Medicine Scan is reserved for biochemically proven cases with negative MRI or CT MIBG structure resembles norepi and concentrates in adrenal or extra-adrenal pheos Used in familial syndromes, recurrent pheo, or malignant pheo Malignant Pheochromocytoma 10 % of pheochromocytomas are malignant Direct invasion into surrounding tissue Distant metastasis Clinical, biochemical, or histological features cannot predict malignancy Common metastatic sites include bone, liver, and lymph nodes Extra-adrenal Pheochromocytoma 90% of pheochromocytomas are located in the adrenal glands 98% located in the abdomen Extra-adrenal pheochromocytomas arise in paraganglion chromaffin tissue of the sympathetic CNS Anywhere from the base of the brain to the bladder Pheochromocytoma – After Diagnosis Rule out familial pheochromocytoma syndromes PTH level and Calcium level (MEN 2a) Ophtho consult to rule out retinal angiomas and MRI head to rule out cerebellar hemangioblastomas (VHL) CT pancreas and kidneys Consider genetic testing for family Pheochromocytoma – Treatment Block alpha receptors first with pure alpha blocker Phenoxybenzamine After alpha blockade is achieved, begin nonselective beta-blockers Administer last doses the morning of surgery Hydrate well and expand volume with isotonic saline Surgically resect tumor; give stress-dose steroids if bilateral adrenalectomy is planned Pheochromocytoma – Long term follow up Test plasma free metanephrines 2 weeks post-operatively, then every 5 years thereafter Ensure resolution of hypertension and associated complications Problem List ACUTE Headache x 3 months Progressively worsening Looks pale with attacks Sweats with headaches Palpitations Hypertension Tachycardia Travel to Peruvian Rainforest CHRONIC Positive PPD INH Therapy Seasonal Allergies Eczema NAFLD Elevated LFT’s Hypertriglyceridemia Differential Diagnosis Chronic Headache Migraine Endocrine Headache Pheochromocytoma Final Diagnosis: Pheochromocytoma Test of Choice: 24-hour urine catecholamines, metanephrines, and VMA References 1. 2. 3. 4. 5. 6. 7. Forsyth, PA, Posner, JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology 1993; 43:1678. Cryer PE: Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system. N Engl J Med 1980;303:436. Headache classification committee of international headache society. Classification and diagnostic criteria for headache disorders, cranial neuralgias, and facial pain. Cephalalgia 1988; 9 Suppl 7:1. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders. Cephalalgia 2004; 24:1. Strovmer LJ, Vatten L, et al. Blood pressure and risk of headache: a prospective study of 22 685 adults in Norway. J Neurol Neurosurg Psychiatry 2002;72:463– 6. Law M, Morris JK, Jordan R, Wald N. Headaches and the treatment of blood pressure: results from a meta-analysis of 94 randomized placebo-controlled trials with 24 000 participants. Circulation. 2005; 112: 2301–2306. www.uptodate.com