Scleroderma Presenting as Pulmonary Hypertension
advertisement

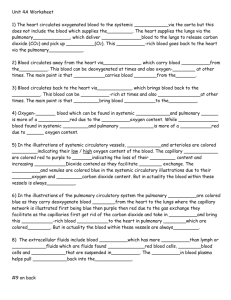
Scleroderma Presenting with Pulmonary Hypertension Cara Fininzio, D.O. Research Symposium June 9, 2010 Background • Scleroderma (systemic sclerosis) is rare multisystem disease, causing fibrosis of multiple organ systems • Skin, kidneys, lungs, GI tract, heart, and blood vessels can be affected • Two forms are identified but there can be some overlap Background • Diffuse cutaneous – Rapid development of symmetric skin thickening – Greater risk for other visceral disease early in course • Limited cutaneous – Symmetric thickening of skin on distal extremities/ face – Can have features of CREST Background • Diffuse: – Distal and proximal extremities, trunk, and face skin involvement – Raynaud’s phenomenon at onset or within 1 year of skin changes – Pulmonary involvement (fibrosis), renal, GI, cardiac – Antitopoisomerase I AB Background • Limited: – Distal extremity/ face skin involvement – Raynaud’s may precede by years – GI, PAH after 10-15 years of disease, biliary cirrhosis – Anticentromere AB Case Report History • A 69 year old Caucasian Female presented with worsening SOB and DOE for the past couple weeks • ROS: + orthopnea, SOB, DOE Past History • PMH- CHF/ Cardiomyopathy, HTN, Osteoporosis, Raynaud’s phenomenon, Pulmonary HTN, GERD, SAR, Lower Extremity Edema, Pruritis, Pneumonia September 2008 • PSH - Tonsillectomy as child • Allergies – None, NKDA Past History Medications: Lisinopril 5mg po daily Furosemide 20mg po daily Carvedilol 3.125mg po daily KCl 10meq po daily Omeprazole 20mg po daily Loratadine 10mg po daily Fosamax 70mg po q week Calcium + Vitamin D po daily FeSo4 325mg po BID Past History • Social- Married, retired, G4P3013, ~5 pack year tobacco history (quit 38 years ago), recovered alcoholic since 9/2008 (admits to a couple beers up to 2 pints of whiskey/ day in past) • Preventive – Colonoscopy 2007, Pap 2005, Mammogram 1/2009 all negative, Pneumonia Vaccine 2008, Influenza Vaccine, Measles and Varicella diseases ad child Past History • FxHx – Mother deceased in 80s (Breast CA at age 35), Father deceased age 67 with DM Previous Testing • Chest CT – Mild mediastinal lymphadenopathy 5-15mm nonpathologic, no hilar lympadenopathy, mild cardiomegaly • 2D echo – LVEF 30% (1/2009), pulmonary artery pressure of 40mmHg Previous Testing • PFT – FVC 2.87L 116% predicted, FEV1 2.08L 105% predicted, FEV1/FVC 73%, no bronchodilator response, Diffusion Capacity 49% predicted • CXR – Bilateral prominent interstitial markings chronic from 4/20/06 comparison, normal heart size Physical Exam • BP 131/74, P 69, RR 18, SaO2 100% on 2L NC, Afebrile • Gen: A& O x 3, well developed, NAD • HEENT: NC/AT, PERRLA, EOMI, MMM, trachea midline, no thyromegaly or lymphadenopathy • Neck: +JVD, no carotid bruits • Heart: Regular S1S2, no murmur, rubs, or gallops, soft heart sounds Physical Exam • Lungs: bibasilar crackles, no wheezing or rhonchi • Abdomen: soft, NT/ND, + bowel sounds, no organomegaly, no rebound or guarding • Ext: trace pitting edema BL lower extremities, +2/4 distal pulses, no clubbing or cyanosis • Skin: tightening/shiny skin of lower extremities and hands with mild erythema • Neuro: CN II-XII intact, strength 5/5 BL, cerebellar function intact Workup • Admitted with decompensated CHF – BNP 3360, mild bilateral pleural effusions and cardiomegaly on CXR, TnI 0.040.080.05 • Pulmonology consult- pHTN unclear etiology consider primary, ANA, RF, Lupus anticoagulant, complete PFT with DLCO, consider right heart catheterization and possible Revatio or Bosantan Workup • Renal consult for Stage IV renal failure • Recommended discontinue ACE inhibitor, lasix, avoid IV contrast and NSAIDS, testing ordered for autoimmune cause, consider mediastinal LN biopsy to rule out lymphoma/ sarcoidosis Workup • Normal Esophogram and Upper GI with small bowel follow through • Renal US unremarkable • Renal flow scan showed mild-moderate chronic parenchymal dysfunction bilaterally Workup • 2D Echo 2/21/2009 - LVEF 60%, moderate to severe PAH with RVSP 64mmHg, LVH, diastolic dysfunction • 2D Echo on 3/25/09 - LVEF 55%, severe PAH with RVSP 60-80mmHg, severely enlarged right atrium/ ventricle, impaired diastolic function Workup • Cardiology consult • Unable to normalize shortness of breath with diuretics, no obvious heart pathology, pulmonary HTN not generally associated with ETOH toxicity • Rheumatologic workup in process Workup • ANA Positive, SCL- 70 Ab 154, Negative cold agglutinins, ESR 1, C3 105, C4 11 (low), RF <20, Centromere Ab 12, Histone Abs 19, IgG <1, SSA Ro Ab 15, SSB La Ab 11, Smith Ab 7, Jo-1 Ab 27, DS DNA Ab 69 Summary Our patient: • Positive ANA and SCL-70 Ab • PAH with RVSP of 60-80mmHg on Echo • Raynaud’s phenomenon and thickened mildly erythematous skin changes Summary • Our patient was treated with supplemental oxygen and was referred to Hospice care due to rapid progression of her symptoms and decline in physical function • She died three months after the diagnosis of scleroderma was made Discussion Scleroderma • Mortality rate for systemic sclerosis has been a constant increasing trend for the past several decades [1] • Increased knowledge and understanding of scleroderma may be contributing to the increasing prevalence [1] • Apparent increased mortality of the disease seen from 1999-2002 [1] Scleroderma • A study by Mendoza showed age-adjusted mortality of systemic sclerosis was 3.2 times greater in women than men [1] • Mortality of this disease continues to trend upward due to the lack of a specifically targeted cure, but improvements in survival have been noted [1] • Most likely explained by decreased morbidity from better management of pulmonary hypertension and renal crisis than in the past [1] Pulmonary Hypertension • Commonly seen pathologic process and often the cause of death in multiple connective tissue disorders, including systemic sclerosis [2] • Up to 40% of patients with scleroderma have been reported to have pulmonary hypertension [2] • Those with the limited form seem to have an increased risk compared to those with diffuse skin disease [2] Pulmonary Hypertension • PAH is important in determining the prognosis in patients with systemic sclerosis [2] • Increased risk of developing pulmonary hypertension with positive U3RNP/ fibrillation and anticentromere antibodies [2] • Decrease with antitopoisomerase (Scl-70) antibodies [2] Raynaud’s and Scleroderma • Diffuse intimal proliferation causes occlusion of the lumen in blood vessels [3] • Leads to the narrowing and vasculopathy seen in pulmonary vascular disease as well as digital vessel pathology (i.e. Raynaud's) [3] • Raynaud's disease has been shown to be an associated risk factor for pulmonary hypertension in patients with systemic sclerosis [3] Raynaud’s and Scleroderma • Showed that patients with pulmonary hypertension had a longer duration of Raynaud's at the time of diagnosis compared to those without pulmonary hypertension and scleroderma [3] • In the patients with pulmonary hypertension the DLCO was very low at the time of diagnosis [3] • The pulmonary artery systolic pressures were found to be >70mm Hg [3] Raynaud’s and Scleroderma • Steen found their group of patients with long duration (greater than 10 years) of Raynaud's to have severe pulmonary hypertension with right heart changes • Determined that patients should be suspected to have pulmonary hypertension if they have had longstanding limited disease, ANA or anticentromere, PASP >40 mm Hg or DLCO <65% predicted [3] Testing Modalities • Echocardiogram, PFTs, exercise testing, and serum biomarkers are among the most common and effective screening modalities for pulmonary hypertension [4] • In symptomatic patients, echocardiography has a 90% sensitivity and 75% specificity for detecting moderate to severe pulmonary artery pressure elevations [4] Testing Modalities • Several studies have examined exercise echocardiography in patients with scleroderma and reported elevated pulmonary artery pressures [4] – They were not confirmed with right heart catheterization • DLCO in pulmonary function testing was found to show a linear decrease over 15 years in patients with systemic sclerosis who would eventually develop pulmonary hypertension [3] Testing Modalities • The 6MWD (6 minute walk distance) showed to be useful in assessment of severity of pulmonary hypertension [4] – Has not been used specifically to screen for it in patients with systemic sclerosis • BNP has been used as a marker of right ventricular dysfunction in patients with pulmonary hypertension due to systemic sclerosis [4] – It has not been validated to be a good screening tool alone Conclusion • This report demonstrates the effects of scleroderma on the lungs demonstrated by rapidly progressing symptoms from pulmonary artery hypertension in our patient • Our patient did complain of pruritis several months prior to her pulmonary symptoms – likely were due to skin changes and tightening secondary to underlying to scleroderma Conclusion • During her visits with a previous physician she was complaining of pruritis and treated symptomatically with PO antihistamines • Diagnosis of Raynaud’s phenomenon for several years before she presented with pulmonary symptoms • History of alcohol abuse and cardiomyopathy may also have contributed to delay in workup and diagnosis of scleroderma Conclusion • Although a small percentage of patients with Raynaud’s will end up developing scleroderma, it was an early sign of our patient’s disease • Recognition and complete evaluation would not necessarily have changed the disease course or outcome of our patient • Earlier recognition of the signs and symptoms of scleroderma may have led to an earlier diagnosis in our patient References • 1. Mendoza F, Derk CT. Systemic Sclerosis Mortality in the United States 1999-2002 Implications for Patient Care. J Clin Rheumatol. 2007;13(4):187-192. • 2. Goldberg A. Pulmonary Arterial Hypertension in Connective Tissue Diseases. Cardiology in Review. 2010;18(2):85-88. • 3. Steen VD. The Lung in Systemic Sclerosis. J Clin Rheumatol. 2005;11(1):40-46. • 4. Bull TM. Screening and therapy of pulmonary hypertension in systemic sclerosis. Curr Opin Rheumatol. 2007;19:598-603. References • 5. Coghlan JG, Pope J, Denton CP. Assessment of endpoints in pulmonary arterial hypertension associated with connective tissue disease. Curr Opin Pulm Med. 2010;16(suppl 1):S27-S34. • 6. Farmer RG, Gifford RW, Hines EA. Prognostic Significance of Raynaud’s Phenomenon and Other Clinical Characteristics of Systemic Scleroderma. A Study of 271 Cases. Circulation. 1960;XXI:1088-1095.