Colon Cancer
advertisement

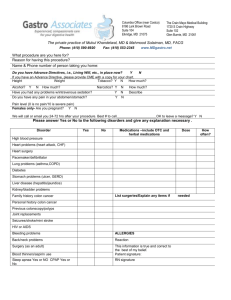
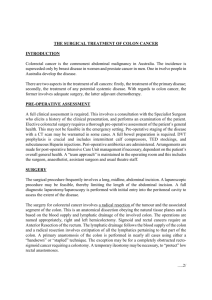
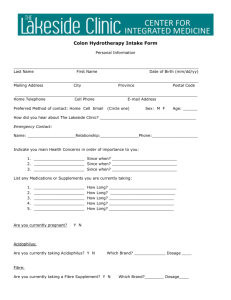
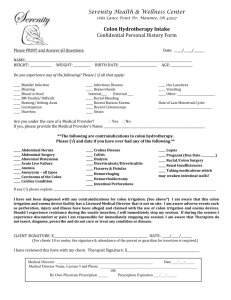
Drug Therapy by Design ……… Level II Learning Objectives After completing this case study, the reader should be able to: Identify common symptoms associated with colon cancer at presentation and with disease progression. Describe the treatment goals associated with early and advanced stages of colon cancer. Design an appropriate chemotherapy regimen for colon cancer based on patient-specific data. Formulate a monitoring plan for a patient receiving a prescribed chemotherapy regimen for colon cancer based on patient-specific information. Recommend alterations in a drug therapy plan for a patient with colon cancer based on patient-specific information. Use pharmacogenetic test results to design an appropriate drug therapy plan for a patient with colorectal cancer. Educate patients on the anticipated side effects of irinotecan, capecitabine, fluorouracil, oxaliplatin, bevacizumab, ziv-aflibercept, regorafenib, and epidermal growth factor receptor inhibitors. Patient Presentation Chief Complaint “The pain below my right ribs is getting worse. Also, I'm having more numbness, cramping, and burning sensations in my hands and feet, especially when I'm working a lot. I don't think I can tolerate it much longer.” HPI Peter Robinson is a 56-year-old man who presents with worsening pain in his hands and feet and increasing RUQ pain. He was diagnosed with stage IV colon cancer 11 months ago after presenting with abdominal pain, bloating and distention, a history of intermittent BRBPR, and no BM within the prior 4 days. He presented to the ED where a barium enema revealed an “apple core” lesion in his descending colon that was suggestive of malignancy (Fig. 150-1). An FDGPET/CT scan showed a complete bowel obstruction and several areas of focal intense uptake in the liver, consistent with metastases. His preoperative CEA was 5.6 ng/mL. He subsequently underwent a laparotomy with a left hemicolectomy and lymphadenectomy. The pathology revealed a moderately differentiated adenocarcinoma with extension through the bowel wall to the serosal surface. The tumor was KRAS gene wild-type. Ten of 13 lymph nodes were positive for tumor. Biopsy of a liver lesion confirmed hepatic metastases. A CT scan of the chest showed no evidence of lung metastases. Seven weeks later, chemotherapy was initiated with capecitabine, oxaliplatin (CapeOx), and bevacizumab. Except for occasional nausea, he generally tolerated the chemotherapy well. However, over the past 2 months he has been experiencing worsening redness and pain on the palms of his hands with numbness and tingling in his fingers and toes. Six days ago he received his 19th cycle of chemotherapy. UGT1A1 testing showed that he was homozygous for the UGT1A1*28 allele. FIGURE 150-1. Annular, constricting adenocarcinoma of the descending colon. This radiographic appearance is referred to as an “apple-core” lesion and is always highly suggestive of malignancy. (Reprinted with permission from Mayer RJ. Gastrointestinal tract cancer. In: Fauci AS, Kasper DL, Longo DL, et al., eds. Harrison's Principles of Internal Medicine, 17th ed. New York, McGraw-Hill, 2008:577.) PMH Type 2 diabetes mellitus × 9 years Hypertriglyceridemia × 5 years FH The patient is the oldest of three brothers; both siblings are alive and well. He has been married for 26 years and has one daughter who is 20 years old. Both his mother and father are in good health. His paternal grandfather died in his 60s from colon cancer, and his mother died in her 60s from ovarian cancer; he is aware of no other family history of malignancy. SH Self-employed as a graphic designer. He smoked cigarettes, one pack per day, since age 19 but quit 10 years ago. He does not drink alcohol and has never tried illicit drugs. Meds Morphine sustained-release 60 mg po twice daily Bisacodyl 5 mg po daily as needed Metformin 750 mg po once daily Fenofibrate 120 mg po once daily All NKDA ROS The patient reports diffuse abdominal pain that is continuous with a “grabbing, gnawing” sensation and painful redness and swelling on the palms of his hands. He rates the abdominal pain severity as 5–6 out of 10. The numbness, tingling, cramping, and burning sensations in his hands and feet have worsened in frequency and severity over the past 2 months and have not responded well to morphine. He rates the severity of the tingling and burning pain as 6/10. He denies fever, headaches, shortness of breath, cough, nausea, vomiting, or diarrhea. He reports no lesions in his mouth or difficulty swallowing. He has been having fewer bowel movements (about one every 3–4 days), but there is no pain or blood with passage of stool. He denies polyuria, polydipsia, and burning on urination. He has not noticed any bleeding or excessive bruising. Physical Examination Gen Patient is a slightly overweight Caucasian man who appears fatigued. VS BP 164/93 mm Hg, P 79 bpm, RR 22, T 35.6°C; Wt 87 kg, Ht 5′9″ Skin Redness and swelling of the palms of both hands and soles of feet HEENT PERRLA; EOMI; funduscopic exam without retinopathy; pale conjunctiva; no scleral icterus; moist mucous membranes; no lesions in oral cavity Neck/Lymph Nodes Supple neck; no lymphadenopathy Lungs/Thorax Symmetric chest expansion with respiratory effort; clear to A & P; regular breath sounds CV Normal heart sounds; regular rate and rhythm; no MRG Abd Well-healed scar on left upper abdomen; diffuse abdominal tenderness to palpation; no rebound tenderness; decreased bowel sounds Genit/Rect Prostate normal size; no masses palpated; stool heme negative MS/Ext Full ROM in all four extremities Neuro A & O × 3; cranial nerves II–XII grossly intact; reduced DTRs bilaterally; reduced feet sensitivity to light touch and pinprick bilaterally in stocking-glove distribution; vibration sensation reduced in distal legs Labs Na 137 mEq/L K 4.4 mEq/L Cl 98 mEq/L CO2 26 mEq/L BUN 17 mg/dL SCr 1.0 mg/dL Glu 117 mg/dL Hgb 9.6 g/dL Hct 29% Plt 252 × 103/mm3 MCV 87 μm3 MCHC 33 g/dL WBC 8.1 × 103/mm3 Neutros 40% Bands 3% Eos 4% Lymphs 45% Monos 8% AST 52 IU/L ALT 45 IU/L Alk phos 109 IU/L LDH 370 IU/L T. bili 1.2 mg/dL T. chol 199 mg/dL CEA 7.9 ng/mL Ca 8.7 mg/dL Phos 3.4 mg/dL Mg 2.3 mg/dL Urinalysis 1+ glucose, (−) ketones, 1+ protein, (−) leukocyte esterase and nitrites; (−) RBC; 2–3 WBC/hpf Abdominal CT Multiple liver metastases, increased approximately 30% in diameter compared to prior scan; multiple new lesions present in both lobes of the liver Chest CT No evidence of pulmonary metastases Assessment Unresectable stage IV colon cancer, with disease progression on CapeOx plus bevacizumab chemotherapy Clinical Pearl There is no available test, including presence of tumor tissue epidermal growth factor receptor expression, that predicts response to cetuximab or panitumumab. However, tumors can be tested for the presence of KRAS mutations that are predictive of lack of response to these agents. Patients with tumors that are KRAS mutant are not appropriate candidates for treatment regimens that contain cetuximab or panitumumab. Questions Problem Identification Identify all of the patient's drug therapy problems. What clinical, laboratory, and other information is consistent with colon cancer? Desired Outcome What are the goals of pharmacotherapy for this patient? Therapeutic Alternatives What chemotherapeutic options are appropriate for this patient? What treatment modifications are appropriate to address escalating oxaliplatin-induced neuropathy? Optimal Plan What drugs, dosage forms, treatment schedule, and duration of therapy are best for treating this patient's colon cancer? What additional drug treatment interventions should be considered for this patient? Outcome Evaluation How is the response to the treatment regimen for the colon cancer assessed? What acute adverse effects are anticipated with the chemotherapy regimen, and what parameters should be monitored? What pharmacologic measures can be instituted to prevent or manage the acute toxicities associated with the chemotherapy regimen? What are the potential late-onset toxicities of the chemotherapy regimen, and how can they be detected and prevented? Patient Education What information should you provide to the patient to enhance compliance, ensure successful therapy, and minimize adverse effects? Clinical Course His hypertension resolved after two cycles of the chemotherapy regimen you recommended, and his neuropathic symptoms diminished over time and with drug therapy. He received PRBC transfusions when his hemoglobin dropped below 9 g/dL. His sustained-release morphine dose was increased to 120 mg po every 12 hours, and oral immediate-release morphine sulfate 30 mg, every 4 hours as needed for pain was started. A scheduled regimen of docusate sodium 100 mg orally plus two senna tablets daily maintained a regular pattern of bowel movements. After seven more cycles of chemotherapy, he presented with worsening abdominal pain, fatigue, and new-onset dyspnea. An abdominal CT scan showed the liver lesions increased in size, and a chest CT showed multiple bilateral pulmonary nodules consistent with pulmonary metastases. His ALT and AST increased to five times the upper limit of normal. Follow-Up Question What treatment options would be appropriate to consider at this time? Additional Case Questions What is the role of UGT1A1 genotyping in the treatment of colon cancer? What is the role of KRAS tumor gene testing in the treatment of colon cancer? How should a patient who develops a thrombotic event during bevacizumab therapy be managed? Clinical Course The patient expressed interest in receiving further treatment for his colon cancer. After considering limited treatment options with his oncologist, he agreed to participate in a clinical trial. His analgesic therapy was modified, and his pain control was acceptable. His metastatic lesions remained stable (by clinical symptoms and CT scans) for 2 months. Self-Study Assignments 1. Develop an algorithm for treatment of colon cancer chemotherapy-induced diarrhea. 2. Develop patient-specific education materials regarding management of cutaneous toxicities of agents used in colon cancer treatment.