NAME: _______ DATE: ______ BLOCK: _____ BLOOD • The only
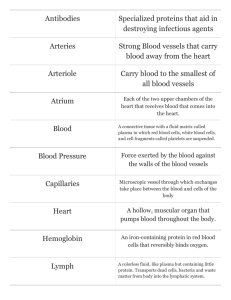
advertisement

NAME: ______________________________________ DATE: ___________ BLOCK: _____ BLOOD • • The only fluid tissue in the human body Classified as a connective tissue – Living cells = formed elements – Non-living matrix = plasma Physical Characteristics of Blood • Color range – Oxygen-rich blood is scarlet red – Oxygen-poor blood is dull red • pH must remain between 7.35–7.45 • Blood temperature is slightly higher than body temperature Blood Plasma • Composed of approximately 90 percent water • Includes many dissolved substances – Nutrients – Salts (metal ions) – Respiratory gases – Hormones – Proteins – _______________________ products Plasma Proteins • Albumin – regulates osmotic pressure • Clotting proteins – help to _____________ blood loss when a blood vessel is injured • Antibodies – help protect the body from antigens Formed Elements • Erythrocytes = ___________ blood cells • Leukocytes = _______________ blood cells • Platelets = cell fragments Erythrocytes (Red Blood Cells) • The main function is to _____________________________ • Contains hemoglobin • Anatomy of circulating erythrocytes – Biconcave disks – Essentially bags of hemoglobin – Anucleate (no nucleus) – Contain very few organelles • 4 - 6 million per mm3 of blood 1 Hemoglobin • ________________-containing protein • Binds strongly, but reversibly, to ______________________ • Each hemoglobin molecule has four oxygen binding sites • Each erythrocyte has 250 million hemoglobin molecules Homeostatic Imbalance • Anemia – _________________________ in oxygen-carrying ability of blood • May be caused by: – Low red blood cell count (RBC) – Abnormal or deficient hemoglobin – Lack of B12 or intrinsic factor – Lack of iron – Cancer • Sickle cell anemia – genetically defective hemoglobin • Polycythemia – abnormal increase in RBC – May be from bone marrow cancer or living at high altitudes – Causes increased viscosity of blood Leukocytes (White Blood Cells) • Crucial in the body’s _________________________ against disease • These are complete cells, with a nucleus and organelles • Able to move into and out of blood vessels (diapedesis) • Can move by ameboid motion • Can respond to chemicals released by damaged tissues Leukocyte Levels in the Blood • Normal levels are between 4,000 and 11,000 cells per mm 3 • Abnormal leukocyte levels – Leukocytosis • Above 11,000 leukocytes/ml • Generally indicates an infection • Could indicate _____________________ (WBC cancer) – Leukopenia • Abnormally low leukocyte level • Commonly caused by certain drugs Platelets • Derived from ruptured cells • Needed for the ___________________________ process • Normal platelet count is 250,000 - 500,000/mm3 Hematopoiesis • Blood ________ formation • Occurs in ________________________________________ • All blood cells are derived from a common stem cell (hemocytoblast) 2 • Hemocytoblast differentiation – Lymphoid stem cell produces lymphocytes – Myeloid stem cell produces other formed elements Fate of Erythrocytes • Unable to divide, grow, or synthesize proteins • Wear out in 100 to 120 days • When worn out, are eliminated by phagocytes in the _________________ or liver • Lost cells are replaced by division of hemocytoblasts Control of Erythrocyte Production • Rate is controlled by a hormone (_______________________________) • Kidneys produce most erythropoietin as a response to reduced oxygen levels in the blood • Homeostasis is maintained by negative feedback from blood oxygen levels Hemostasis • Stoppage of blood flow • Result of a break in a blood vessel • Hemostasis involves three phases – Platelet plug formation – Vascular spasms – Coagulation Platelet Plug Formation • Collagen fibers are exposed by a break in a blood vessel • Platelets become “__________________” and cling to fibers • Anchored platelets release chemicals to attract more platelets • Platelets pile up to form a platelet plug Vascular Spasms • Anchored platelets release serotonin • ________________________________ causes blood vessel muscles to spasm • Spasms narrow the blood vessel, decreasing blood loss Coagulation • Injured tissues release thromboplastin • PF3 (a phospholipid) interacts with thromboplastin, blood protein clotting factors, and calcium ions to trigger a clotting cascade • Prothrombin activator converts prothrombin to ______________________________ (an enzyme) • Thrombin joins fibrinogen proteins into hair-like fibrin • Fibrin forms a meshwork (the basis for a clot) Blood Clotting • Blood usually clots within 3 to 6 minutes 3 • • The clot remains as endothelium regenerates The clot is broken down after tissue repair Undesirable Clotting • _________________ – A clot in an unbroken blood vessel – Can be deadly in areas like the heart • _________________ – A thrombus that breaks away and floats freely in the bloodstream – Can later clog vessels in critical areas such as the brain Bleeding Disorders • Thrombocytopenia – Platelet deficiency – Even normal movements can cause bleeding from small blood vessels that require platelets for clotting • Hemophilia – Hereditary bleeding disorder – Normal clotting factors are missing Blood Groups and Transfusions • Large losses of blood have serious consequences – Loss of 15 to 30 percent causes weakness – Loss of over 30 percent causes shock, which can be fatal • Transfusions are the only way to replace blood quickly • Transfused blood must be of the same blood group Human Blood Groups • Blood contains genetically determined proteins • A foreign protein (antigen) may be attacked by the immune system • Blood is “typed” by using antibodies that will cause blood with certain proteins to clump (agglutination) • There are over 30 common red blood cell antigens • The most vigorous transfusion reactions are caused by ABO and Rh blood group antigens ABO Blood Groups • Based on the presence or absence of two antigens – Type ____ (only A antigen) – Type ____ (only B antigen) – Type AB (both A and B antigen) – Type O (neither A or B) Rh Blood Groups • Named because of the presence or absence of one of eight Rh antigens • Most Americans are ______________ 4 • Problems can occur in mixing Rh+ blood into a body with Rh– blood Rh Dangers During Pregnancy • Danger is only when the mother is Rh– and the father is Rh+, and the child inherits the Rh+ factor • The mismatch of an Rh– mother carrying an Rh+ baby can cause problems for the unborn child – The first pregnancy usually proceeds without problems – The immune system is sensitized after the first pregnancy – In a second pregnancy, the mother’s immune system produces antibodies to attack the Rh+ blood (hemolytic disease of the newborn) Developmental Aspects of Blood • Sites of blood cell formation – The fetal liver and spleen are early sites of blood cell formation – Bone marrow takes over hematopoiesis by the seventh month • Fetal hemoglobin differs from hemoglobin produced after birth CARDIOVASCULAR SYSTEM • • A closed system of the heart and blood vessels – The heart pumps blood – Blood vessels allow blood to circulate to all parts of the body The function of the cardiovascular system is to deliver ________________ and nutrients and to remove ___________________ and other waste products The Heart • Location – Thorax between the lungs – Pointed apex directed toward left hip • About the size of your fist The Heart: Coverings • ___________________________ – a double serous membrane – Visceral pericardium • Next to heart – Parietal pericardium • Outside layer • Serous fluid fills the space between the layers of pericardium • Pericarditis – inflammation of pericardium, which causes a decrease in serous fluid The Heart: Heart Wall • Three layers – Epicardium • Outside layer 5 • This layer is the parietal pericardium • Connective tissue layer – _______________________________ • Middle layer • Mostly cardiac muscle – Endocardium • Inner layer • Endothelium The Heart: Chambers • Right and left side act as separate pumps • Four chambers – _______________________ • Receiving chambers – Right atrium – Left atrium – _______________________ • Discharging chambers – Right ventricle – Left ventricle The Heart: Valves • Allow blood to flow in only one direction • Four valves – Atrioventricular valves – between atria and ventricles • ___________________ valve or _______________ (left) • ___________________ (right) – Semilunar valves between ventricle and artery • Pulmonary semilunar valve • Aortic semilunar valve • Valves open as blood is pumped through • Held in place by chordae tendineae (“heart strings”) • Close to prevent backflow The Heart: Associated Great Vessels • Aorta – Leaves left ventricle • Pulmonary arteries – Leave right ventricle • Vena cava – Enters right atrium • Pulmonary veins (four) – Enter left atrium Coronary Circulation • Blood in the heart chambers does not nourish the myocardium 6 • The heart has its own nourishing circulatory system – ___________________ arteries – Cardiac veins – Blood empties into the right atrium via the coronary sinus Homeostatic Imbalance • Valvular stenosis – valve flaps become stiff, often from endocarditis (bacterial infection of endocardium) • Faulty valves may be replaced by synthetic or pig valves • Angina pectoris – chest pain as a result of the myocardium being deprived of oxygen • _______________________________ (heart attack) – prolonged angina that kills heart cells The Heart: Conduction System • Intrinsic conduction system (nodal system) – Heart muscle cells contract, without nerve impulses, in a regular and continuous way • Special tissue sets the pace • ___________________ or pacemaker – In right atrium – Starts impulse • Atrioventricular node – At junction of right atrium and ventricle • Atrioventricular bundle – In interventricular septum • Bundle branches • ____________________________ – In wall of ventricles Homeostatic Imbalance • Heart block – damage to AV node causing ventricular contraction to beat at own rate (much slower) • Ischemia – lack of adequate blood supply to heart muscle • Fibrillation – rapid uncoordinated shuddering of heart muscle (caused by ischemia) • Tachycardia – rapid heart rate (over 100 bpm) • Brachycardia – much slower rate (under 60 bpm) The Heart: Cardiac Cycle • Atria contract simultaneously • Atria relax, then ventricles contract • ___________________ = contraction • ___________________ = relaxation • Cardiac cycle – events of one complete heart beat – Mid-to-late diastole – blood flows into ventricles 7 • • – Ventricular systole – blood pressure builds before ventricle contracts, pushing out blood – Early diastole – atria finish re-filling, ventricular pressure is low Heart sounds – __________ (closing AV valves) _______ (semilunar valves close) Heart murmur – abnormal or unusual heart sounds – From blood hitting thin walls – Valves not closing tightly – Narrowed valves The Heart: Cardiac Output – ___________________ Amount of blood pumped by each side of the heart in one minute – CO = (heart rate [HR]) x (stroke volume [SV]) • Stroke volume – Volume of blood pumped by each ventricle in one contraction The Heart: Regulation of Heart Rate • Stroke volume usually remains relatively constant – Starling’s law of the heart – the more that the cardiac muscle is stretched, the stronger the contraction • Changing heart rate is the most common way to change cardiac output • Increased heart rate – Sympathetic nervous system • Crisis • Low blood pressure – Hormones • Epinephrine • Thyroxine – Exercise – Decreased blood volume • Decreased heart rate – Parasympathetic nervous system – High blood pressure or blood volume – Dereased venous return Homeostatic Imbalance • Congestive heart failure – pumping efficiency of heart is diminished – Often from clogging of coronary arteries (atherosclerosis), persistent high blood pressure, and MI • _______________________________– left side of heart fails so blood not pumped out to body, but blood continues to move into lungs causing fluid to leak into lungs – Can lead to suffocation 8 Blood Vessels: The Vascular System • Taking blood to the tissues and back – ___________________ (away from heart) – Arterioles – Capillaries – Venules – ___________________ (toward heart) Differences Between Blood Vessel Types • Walls of arteries are the thickest • Lumens of veins are larger • Skeletal muscle “milks” blood in veins toward the heart • Walls of capillaries are only one cell layer thick to allow for exchanges between blood and tissue Movement of Blood Through Vessels • Most arterial blood is pumped by the heart • Veins use the milking action of muscles to help move blood • Capillary beds consist of two types of vessels – Vascular shunt – directly connects an arteriole to a venule • True capillaries – exchange vessels • Oxygen and nutrients cross to cells • Carbon dioxide and metabolic waste products cross into blood Homeostatic Imbalance • Varicose veins – pooling of blood in feet and legs and inefficient venous return resulting from inactivity or pressure on the veins; veins become twisted and dilated • Thrombophlebitis – inflammation of vein that results when clot forms in a vessel with poor circulation; if the clot moves to the lungs it causes a pulmonary embolism Pulse • ___________________ – pressure wave of blood • Monitored at “pressure points” where pulse is easily palpated Blood Pressure • Measurements by health professionals are made on the pressure in large arteries – ___________________ – pressure at the peak of ventricular contraction – ___________________ – pressure when ventricles relax • Pressure in blood vessels decreases as the distance away from the heart increases Blood Pressure: Effects of Factors • Neural factors – Autonomic nervous system adjustments (sympathetic division) • Renal factors – Regulation by altering blood volume – ___________________ – hormonal control 9 • • • Temperature – Heat has a vasodilation effect – Cold has a vasoconstricting effect Chemicals – Various substances can cause increases or decreases Diet Variations in Blood Pressure • Human normal range is variable – Normal • 140–110 mm Hg systolic • 80–75 mm Hg diastolic – Hypotension • Low systolic (below 110 mm HG) • Often associated with illness – ______________________________ • High systolic (above 140 mm HG) • Can be dangerous if it is chronic; weakens myocardium and causes atherosclerosis Capillary Exchange • Substances exchanged due to concentration gradients – Oxygen and nutrients leave the blood – Carbon dioxide and other wastes leave the cells Capillary Exchange: Mechanisms • Direct diffusion across plasma membranes • Endocytosis or exocytosis • Some capillaries have gaps (intercellular clefts) – Plasma membrane not joined by tight junctions • Fenestrations of some capillaries – Fenestrations = pores Developmental Aspects of the Cardiovascular System • A simple “tube heart” develops in the embryo and pumps by the fourth week • The heart becomes a four-chambered organ by the end of seven weeks • Few structural changes occur after the seventh week 10