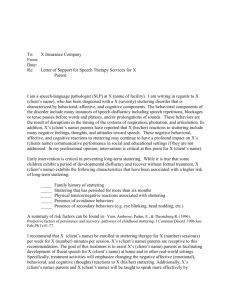
FTR- Final draft
advertisement

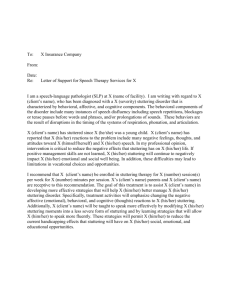
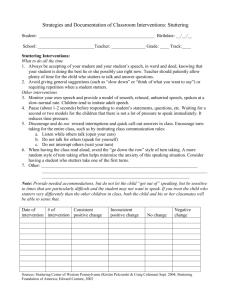
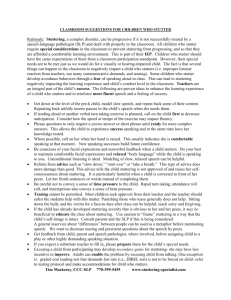
F-24: SPEECH/LANGUAGE THERAPY REPORT SPEECH/LANGUAGE THERAPY REPORT I. BACKGROUND INFORMATION T is a xx-year-old man who attended the Neurogenic Disorders clinic for the first time in the summer of 2012. In this clinic T received individual as well as group therapy for one hour each. Respiration support, breathing and anxiety management (due to his stuttering), and compensatory communication strategies were some of the goals addressed to improve T’s stuttering and dysarthria. T, originally from XX, was born two weeks premature and received growth hormones as infant. Based on past report, T’s mother did not see any issues until 5th grade where she noticed some repetitions in his speech and became “clumsy and kept falling and tripping”. T was misdiagnosed with cerebral palsy first, but later he was diagnosed with Cytochrome Oxidase Deficiency (COX). COX is a progressive disorder that deteriorates motor muscles (fine and gross) over time. Please refer to past assessment report for more information about COX. Based on the information gathered on his first evaluation in the spring of 2012, T tended to verbalize in short utterances, 1-3 word phrases and had difficulty articulating certain sounds due to his dysarthria and stuttering. Blocks and prolongations as well as secondary behaviors such as avoidance, and escape behaviors characterized his fluency. He talked with low loudness and monotone sound. Based on past report, T had signs of oral phase dysphasia and had learned compensatory strategies to clear residue. T’s hearing was affected by COX disorder also. He exhibits high frequency hearing loss. He received a hearing aid; however, he refuses to use it. He takes Fluoxetine (a generic form of Prozac) to control his depression. He attempted suicide on February 2012. Currently, T receives therapy from a psychologist once a month and sees a counselor every week. He mentioned during the initial interview that his hearing and vision still the same as last semester but felt that his speech has deteriorated. He stated that he feels frustrated when other people don’t understand him and has experienced mood swings due to that. T’s strategy to tolerate his frustration is by “just forgetting about it”. T’s first experience with speech therapy was during high school and then at the Arc Center in XX. He also received physical therapy. He currently attends the Arc Center three times a week. He stated that he is learning to become more independent. Recently, he started taking MUNI (SF public transportation) to come to clinic every Thursday. His hobbies are watching baseball and basketball games. He is a native English speaker, but has been exposed to Chinese. T got married in March 2012. Information and results for this report were determined through file review, interview, standardized and informal assessment measures and data collection. II. CURRENT SEMESTER’S ASSESSMENT A. Pre-test data The following assessment procedures were administered to compare any changes since his last formal evaluation: Interview- Client History Form Frenchay Dysarthria Assessment Stuttering Severity Inventory (SSI-4) F-24 Speech/Language Therapy Report Updated 06/06/04 06/21/12 06/21/12 & 06/28/12 06/28/12 Interview: The case history form was administered during the first meeting in order to gain information regarding any changes in T’s communication that occurred from his first assessment until 06/21/12. T stated that his speech has deteriorated since his last evaluation. He mentioned that it takes longer “to say the word out loud”. He also mentioned that his speech is better in the morning because he is more awake and uses more compensatory strategy such as gestures. T stated that in some opportunities he writes what he wants to say when people don’t understand him. Since he has hearing loss, he mentioned that is difficult to hear what other people say in a noisy environment and as a result, he feels frustrated. In the interview he also stated that his speech affects his social life and that he is aware of his speech errors. Frenchay Dysarthria Assessment: The purpose of this test was to compare and analyze any changes on T’s dysarthria since his first formal assessment until 06/21/12. Lips and Jaw: did not present any changes. Tongue: In first evaluation, T repeated “Ka La” 10 times in 5 seconds. It took 28 seconds to repeat “Ka La” 10 times on 06/21/12 assessment. Also his alternating movements were slow and took more than 10 seconds to complete it this time. The student clinician noticed that T had difficulty moving his tongue forward. Soft Palate: Student clinician did not observe any changes. Larynx: In first evaluation, T produced minimal pitch and volume changes. On last evaluation, T did not produce changes in those areas. Intelligibility: During a reading task (words and sentences), T’s speech was severely distorted receiving a grade of C based on the Frenchay Dysarthria Assessment. T interpreted 8 out of 22 words correctly. However, during conversation, T’s speech was more intelligible earning a B, meaning his speech was abnormal but intelligible and would occasionally repeat. Stuttering Severity Inventory (SSI-4): The SSI-4 was used in order to analyze T’s stuttering behaviors. T was asked to read a paragraph (adult level reading) that contained 228 syllables. He produced stuttering behaviors such as prolongations and blocks in 57 syllables. His longest disfluency was a prolongation that lasted 54 seconds. T produced unintelligible sentences when reading the paragraph. He also omitted words such as “is” and “that” and presented escape behaviors (said “yeah” several times during the reading) which made it difficult to assess. Facial grimacing, raising his left leg, and poor eye contact was also observed during the evaluation. Overall, T presented severe stuttering behaviors that affected his overall intelligibility. B. Post-test data Post-test data was gathered through observation and administration of the SSI-4 in order to measure progress. Due to client’s preference, the student clinician mainly focused on his fluency disorders; therefore, the Frenchay Dysarthria Assessment was not re-assessed. The data was collected on 08/02/12. Stuttering Severity Inventory (SSI-4): T was asked to read the same adult level reading paragraph he was asked in the beginning of the summer semester. He produced primary stuttering behaviors in 20 syllables (7 prolongations &13 blocks) total. Throughout the reading, he omitted one word “pump” and presented escape behaviors such as lifting his legs up and placing his left hand by his head. When reading the paragraph, T produced his main avoidance behaviors only twice: said “yeah” every time he stuttered. He used his strategies to reduce this behavior 6 times throughout the reading. During a conversation that lasted 5 minutes, T disfluency increased. He produced more avoidance behaviors as well as blocks. He mentioned that he feels more confident to use his strategies when reading than talking. After the administration of the test, T mentioned that the number of disfluency he presented was reduced because he felt more comfortable with the student clinician. It is recommended to re-test T with the SSI-4 and compare the results from the pre-test data with the following semester pre-test data. 2 III. INTERVENTION GOALS AND PROGRESS 1. Given minimum to moderate visual cues, T will increase his overall intelligibility by increasing his speech volume to become more comprehensible to an unfamiliar listener. a) T will modify position/ posture (seating upright) to enhance inspiration with minimum to moderate visual cues with 80% accuracy. b) T will respond to minimum to moderate visual/ verbal cues to “inhale more deeply” before beginning an utterance on phrases and or sentences with 80% accuracy. c) T will respond to verbal/ visual cues to use more force when exhaling to increase loudness/ maintain loudness levels on phrase/ sentence- level responses with 80% accuracy. Joe Duffy, Ph.D., BC-ANCDS, explains in detail the different speech strategies that patients with dysarthria can use to improve their overall intelligibility. In this presentation presented at the MAYO clinic, Duffy, Ph.D., BC-ANCDS provided different evidence- based practice strategies to increase volume throughout respiration and breath support exercises, http://www.docstoc.com/docs/78383942/DuffyTherapy-Techniques-Dysarthria Baseline: T’s speech was monotone and had low volume. Progress: Objective a: Goal met. On 08/02/12, T sat up straight independently during individual and group therapy. Objective b: Goal met. During a reading activity, T inhaled more deeply before reading an utterance when provided moderate verbal cues. Objective c: Goal partially met. Used more force when exhaling that increased his volume level 80% of the time. However, during a casual conversation, he did not use more force when exhaling to increase loudness. 2. T will reduce his fear about his stuttering when talking with an unfamiliar listener. a) T will identify his stuttering behaviors (core & secondary behaviors as well as his feelings and attitudes) when asked by the clinician with moderate to maximum cues with 80% accuracy. b) T will describe what he does when he stutters and when he avoids stuttering when asked by the clinician with moderate to maximum cues with 80% accuracy. The patient was the one who decided to work on his fluency. During the interview process, he communicated that his main concern was his fear when talking to unfamiliar individuals because he felt that he stutter more when meeting new people. It is important to prioritize the goals that are more meaningful for the client because this will increase his level of participation in therapy and increase the outcomes of therapy. An article discussing the importance of using client- centered goals can be found here http://div2perspectives.asha.org/content/22/1/28.abstract Baseline: T did not identify or described his stuttering behaviors and presented fear when talking to an unfamiliar listener. Progress: Objective a: Goal met. On 07/26/02, T identified his primary and secondary stuttering behaviors as well as his feelings and attitudes. The client was provided with a model and moderate to maximum verbal cues. Objective b: Goal met. T described his escape behaviors successfully with moderate to maximum verbal cues. 3. T will use fluency shaping exercises such as easy onset and block release exercises when talking with a familiar and unfamiliar listener with mild to moderate cues. . a) T will use easy onset and block release exercises when talking or reading with the clinician with maximum cues with 80% accuracy. b) T will use easy onset and block release exercises when talking with a familiar (group therapy partners) and unfamiliar listener with maximum to moderate cues with 80% accuracy. 3 An detailed explanations of the different fluency theories and therapy approaches were taken from chapter 6 & 14 in Stuttering an integrated approach to its nature and treatment by Barry Guitar http://books.google.com/books?id=NI57ybiwlg0C&printsec=frontcover&dq=stuttering+barry++guitar& hl=en&sa=X&ei=jMFgUYPVF6WJ2AWPqYGQBQ&ved=0CDoQ6AEwAA#v=onepage&q=stuttering% 20barry%20%20guitar&f=false Baseline: T did not use easy onset or block release exercises to control his stuttering. Progress: Objective a: Goal met. On 08/02/12, T used easy onset and block release exercises when reading and talking with the student clinician with maximum verbal cues and modeling. Objective b: Goal not met. On 08/02/12, T did not use easy onset and block release exercises during group therapy. 4. T will increase his intelligibility by minimizing his secondary behaviors during speech. o T will decrease his escape behavior (say “yeah” every time he stutters) when reading a small paragraph with maximum cues with 80% accuracy. o T will decrease his escape behavior (say “yeah” every time he stutters) when having a conversation with a familiar partner with maximum to moderate verbal cues with 80% accuracy. Baseline: T used secondary behaviors during speech numerous times. Progress: Objective a: Goal met. On 08/02/12, T decreased his escape behavior (said “yeah” every time he stutters) when reading a paragraph that contained 137 syllables to a familiar listener. He produced secondary behaviors twice and used his speech strategies 8 times throughout the reading. Objective b: Goal not met. On 08/02/12, Tdid not decrease his escape behavior when having a conversation. He produced 8 escape behaviors in a conversation with the student clinician that lasted 3 minutes. IV. IMPRESSIONS T was a positive and motivated client who was self-aware and concerned about his speech. He always arrived to therapy with a great attitude and was willing to work hard to improve his overall intelligibility. In the beginning of the semester he stated that his biggest concern and area he wanted to improve was his fluency. He was aware that his primary and secondary stuttering behaviors reduced his intelligibility. Also, he mentioned that when talking with unfamiliar partners he would get frustrated and anxious which made his stuttering behaviors increase. Talking more openly about his feelings and attitudes towards his fluency, and recognizing and analyzing his own primary stuttering behaviors has been very helpful for T. Also, working on diminishing his secondary and escape behaviors helped him feel that his speech was improving. During therapy he mentioned that the exercises towards these goals are hard, but he felt happy because he knows they are helping him to reach his goal. Working with appealing materials (readings and/or talking about the Giants, or basketball teams) made the therapy process more enjoyable for T. Moreover, practicing the new skills he was learning in therapy with unfamiliar partners was very beneficial. During the semester, T and the clinician went several times to the cafeteria and he ordered coffee using the skills learned in therapy. Based on observations, T made great progress. He stated that his anxiety level of when he speaks in group therapy has decreased. During group therapy he tries to carryover the skills learned during individual therapy. He sits straight when talking, and tries to reduce his avoidance and secondary stuttering behaviors by self correcting or taking a small break (lasting a few seconds) when he is stuck with a block or a prolongation. V. RECOMMENDATIONS Based on T’s progress on this semester’s therapy goals, he would benefit from continued speech therapy at the CD clinic to further increase his speech intelligibility. 4 o o o o Continue working on minimizing his primary and secondary fluency behaviors. Continue working on reducing the fear about his stuttering when talking with unfamiliar partners. Continue working on exercises that focused on increasing his respiration support, speech volume, and breath management during speech. T’s hearing should be evaluated periodically to determine any crucial changes as his medical condition progresses. REFERENCES Guitar, Barry. “Stuttering an integrated approach to its nature and treatment.” (2006). Philadelphia. Lippincott Willians & Wilkins. Swigert, Nancy. “The source of dysarthria”. (2004). East Moline, IL. Linguisystems. 5