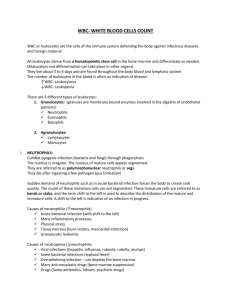
White Blood Cells:
advertisement

White Blood Cells 1 WHITE BLOOD CELLS: Morphology, Physiology & Benign Disorders White blood cells (WBC), also called “Leukocytes” are so named because of their appearance when separated from rest of the blood components by centrifuge. They, as a group, form one of the three cellular components of blood; the other two are red blood cells and platelets. White blood cells, however, are the least numerous cells, 500-1000 times less numerous than red blood cells and about 20-100 times less numerous than platelets. The normal WBC count is 4 - 11 x 109/L. In adults they are ultimately derived from bone marrow; in the fetal and neonatal period they are also formed in liver and spleen. The main function of WBCs, as group, is in the immune system & inflammation. The mature WBCs are of 3 main types, each with subtypes; the fourth type, mast cell, is derived from myelomonocytic stem cell and is tissue resident under normal conditions. Plasma cells are terminally differentiated B-cells that do not circulate normally in blood. 1. Granulocytes (a) Neutrophils (also called polymorphonuclear leukocytes, PMN) (b) Eosinophils (c) Basophils Neutrophil Eosinophil Basophil 2. Lymphocytes (a) T-lymphocytes (b) B-lymphocytes (c) NK-lymphocytes B or T Small lymphocyte Large granular lymphocyte of NK-cell type 3. Monocytes/Histiocytes (a) Circulating monocytes/tissue macrophages and histiocytes (b) Langerhans cells & (c) Dendritic cells (tissue residents) Monocyte The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 2 GRANULOCYTES: NEUTROPHILS: (1.8 – 7.7 x 109/L; 45% – 75% of all circulating leukocytes) Neutrophils are the most numerous of all granulocytes. A mature neutrophil is about 1216 m in size, contains abundant azurophilic (red-brown) granules and a nucleus with 3-5 lobes. The surface membrane of a neutrophil contains members of the integrin family of molecules such as CD11/CD18 and other molecules involved in cell-to-cell adhesion such as L-selectin and Sialyl-Lewis X protein. The neutrophils mature in bone marrow, circulate in blood, and finally emigrate to tissue at sites of inflammation. NEUTROPHIL GRANULES: They are of 3 types (1) Primary or Azurophilic granules (a) Myeloperoxidase (MPO) (b) Elastase (c) Proteinase 3 (d) -1 antitrypsin (e) Defensins (f) Lysozyme (g) Bactericidal permeability increasing protein (BPIP) (2) Secondary of Specific granules (a) Lactoferin (b) Lysozyme (c) Vitamin B-12 binding protein (d) Other proteins (3) Secretory vesicles (a) CD35 (b) Latent alkaline phosphatase NEUTROPHIL FUNCTION: Neutrophils are phagocytic cells that engulf and kill microorganisms (or, at least try to!). They respond to injury and emigrate to tissues in a sequence of events: (1) Adhesion and transmigration (2) Chemotaxis (3) Leukocyte activation (4) Phagocytosis The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 3 LEUKOCYTE ADHESION AND TRANSMIGRATION: This function is achieved through the binding of complementary molecules on the surface of leukocytes and endothelial cells. [These pictures are adapted from Robbins Pathologic Basis of Diseases, 6 th edition, W.B Saunders Co.] CHEMOTAXIS: After extravasation, leukocytes emigrate in tissues toward the site of injury, a process called, chemotaxis, defined simply as “locomotion oriented along a chemotactic agent”. Both endogenous and exogenous substances act as chemoattractants. The most common exogenous chemoattractants are bacterial products whereas the endogenous agenst include C5a, leukotriene B4, and interleukins (IL-8). ACTIVATION: This term refers to synthetic and secretory activities of leukocytes in preparation for their role in inflammation and microbial killing. Three parallel but distinct activities occur: (a) Production of arachidonic acid metabolites – from membrane phospholipids by the action of phospholipase A2 (b) Degranulation and secretion of lysozomal enzymes and activation of the oxidative burst – these two processes are induced by DAG-mediated activation of protein kinase (c) Modulation of leukocyte adhesion surface molecules The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 4 [This picture is adapted from Robbins Pathologic Basis of Diseases, 6th edition, W.B Saunders Co.] PHAGOCYTOSIS: This is the ultimate step of leukocyte function in the long process of (minutes to hours!) microbicidal attack. This can be divided into the following steps: (a) Recognition and attachment to the binding agent (b) Engulfment (c) Killing or degradation of the organism The leukocytes must first bind to microbial agents in order before they engulf and kill them. In almost all instances, microbial agents and other particulate materials to be engulfed are coated with specific protein molecules called “opsonins”, which bind to their receptors on leukocyte cell surface. Some of the opsonins & their receptors are (i) Fc fragment of IgG antibodies, which bind to the FcR leukocyte receptor (ii) C3b, generated after complement system activation, binds to complement receptors 1, 2 & 3 (CR1, 2, & 3) on leukocyte’s surface (iii)Carbohydrate-binding proteins of plasma called “collectins” bind to C1q receptor on leukocytes The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 5 The process of engulfment is simply extending psedopods around the particle and bringing it inside the cell. Actin and other proteins help in this process. Once the microorganism or other particulate material is inside the cell the process of degradation begins. Bacterial killing is accomplished largely by oxygen-dependent mechanisms in which phagocytosis stimulates a burst in oxygen consumption, glycogenolysis, increased glucose oxidation via the hexose-monophosphate shunt, and production of reactive oxygen metabolites and subsequently hydroxyl ions, OH. The generation of oxygen metabolites is due to the rapid activation of NADPH oxidase, which oxidizes NADPH, and in doing so, reduces O2 to superoxide ions, O2-. 2O2 + e NADPH oxidase 2 O2 + NADP + H Superoxide is then converted to into hydrogen peroxide, H2O2, mostly by spontaneous dismutation. 2O2 + H H2O2 + O2 The NADPH oxidase is a multiprotein enzyme complex consisting of several proteins components. In resting neutrophils, these NADPH oxidase protein components are separated into plasma membrane and cytosolic compartments. During assembly and activation of the oxidase, the cytosolic components (p67, p47, p40) translocate to the plasma membrane or phagosomal membrane, where they assemble with the membrane-bound components (gp91, p22, Rap1a) to form the functional enzyme complex as shown below. [This picture is adapted from The Molecular Basis of Blood Diseases, 3rd edition, W.B Saunders Co.] The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 6 The hydrogen peroxide formed as a result of the above reaction is insufficient for effective microbial killing. This is where myeloperoxidase comes into play. Myeloperoxidase in the presence of a halide ion such as Cl converts H2O2 into hypochlorous ion (HOCl), which is an effective killer of microbes by causing halogination or oxidation of proteins and lipids in microbes, which leads to inactivation of antiproteinases and activation of proteinases. Furthermore, HOCl forms chloramines complexes with amino-acids of proteins rendering them inactive. [This picture is adapted from Robbins Pathologic Basis of Diseases, 6th edition, W.B Saunders Co.] This H2O2-MPO-halide system is the most efficient bactericidal system in neutrophils. Most of the hydrogen peroxide is broken down by catalase into water and oxygen molecules. The overall oxidative burst mechanism is summarized below: [This picture is adapted from HEMATOLOGY, Basic Principles & Practice, 3rd edition, Churchill-Livingstone.] Bacterial killing can also occur through an oxygen-independent mechanism, whereby various constituents of neutrophilic granules such as BPIP, lysozyme, defensins and lactoferrin lead to the degradation of microbes through a variety of mechanisms. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 7 BENIGN DISORDERS OF NEUTROPHILS: The benign disorders of neutrophils can be categorized as (A) Quantitative disorders 1. Neutropenia (decrease) (a) Congenital (b) Acquired 2. Neutrophilia (increase) (a) Congenital (b) Acquired (B) Qualitative disorders (A) QUANTITATIVE NEUTROPHIL DISORDERS: Quantitative problems are much more common in clinical practice than qualitative disorders. 1. NEUTROPENIA (<1.8 x 109/L): The clinical manifestations of decreased number or function of neutrophils are principally the result of bacterial and fungal infection. The absolute neutrophil count (ANC) varies slightly in different ethnic groups and also varies with age. A fall in neutrophil count to about 1.0 x 109/L is usually not associated with an appreciable increase in the incidence of infections in otherwise healthy individuals. If the ANC drops further, the risk of infection increase such that below 0.5 x 109/L individuals are at risk of developing recurrent infections. Some of the causes are listed below: (a) Congenital (i) Congenital syndromes – Schwachman-Diamond syndrome, Kostmann syndrome Cohen syndrome, Barth syndrome, Dyskeratosis congenita, Facconi’s anemia, Familial benign neutropenia, Cyclic neutropenia, etc. (b) Acquired (i) Bone marrow suppression – by extensive involvement of the marrow by hematologic or other malignancies (ii) Bone marrow suppression/ablation – anticancer drugs (iii) Ineffective myelopoiesis – Myelodysplastic syndrome, vitamin B-12 deficiency (iv) Aplastic anemia – marrow toxicity by chemicals, drugs (v) Accelerated neutrophil destruction – sepsis (vi) Alloimmune neonatal neutropenia (vii) Autoimmune neutropenia – Idiopathic, Drug induced, Autoimmune disorders such as SLE (viii) Nutritional deficiencies (ix) Splenic sequestration – hypersplenism (x) Pure white cell aplasia The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 8 2. NEUTROPHLIA (> 7.7 X 109/L): An increase in the neutrophil count is perhaps more common than a decrease in the hospitalized patient. In most instances it is a mild to moderate elevation in the neutrophil count and in some cases no cause could be identified. Almost all cases of neutrophilia are acquired and only extremely rare congenital conditions exist. Infections are among the most common causes of acquire neutrophilia. Three basic mechanisms exist for a high neutrophil count: increased production in the marrow, increase release from the marrow, and increased demargination from the vessel walls into circulation. In most cases differentiation of a reactive increase in neutrophil count from chronic myelogenous leukemia (CML) is not a problem but in some extreme cases of reactive increase in neutrophil count called Leukemoid reaction (WBC > 50 x 109/L) a distinction may not be clear cut because immature myeloid cells including myeloblasts, promeylocytes and myelocytes may be seen in both leukemoid reaction and CML. However, a few findings may help in the differentiation such as the absence of an increase in basophil number, presence of Döhle bodies, toxic granules and cytoplasmic vacuoles in leukemoid reactions. Some of the causes are listed below: (a) Acquired (i) Acute infections – Bacterial, fungal, and some severe viral infections (ii) Acute inflammatory conditions – Acute gout, Kawasaki disease (iii) Chronic inflammation – Rheumatoid arthritis (iv) Stress neutrophilia – demargination by epinephrine & steroid hormones (v) Drug induced – Steroids, -agonists, Lithium, tetracyclines, marrow growth factors such as G-CSF (vi) Non-hematologic malignancies – lung cancer (vii) Exercise (viii) Heat stroke (ix) Cigarette smoking (x) Sweet’s syndrome (xi) Chronic idiopathic neutrophilia (b) Congenital (i) Hedreditary neutrophilia (ii) Familial cold urticaria and leukocytosis The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 9 (B) QUALITATIVE NEUTROPHIL DISORDERS: Any qualitative disorder affecting the normal functions of neutrophils will ultimately hamper the antimicrobial activity of these phagocytes and consequently leading to an increase risk of infections. Most of the manifestation result from recurrent bacterial and especially pyogenic (pus forming) infections. Some of these disorders can be categorized as follows: 1. ABNORMALITIES OF DEGRANULATION (a) Chediak-Higashi syndrome Fundamental defect in granule morphogenesis resulting in abnormally large granules with defective degranulation. The large granules are seen in numerous cells including granulocytes and their precursors, monocytes, granular lymphocytes, etc. (b) Specific granule deficiency 2. DEFECTS OF MICROBICIDAL ACTIVITY (a) Chronic granulomatous disease (CGD) X-linked & autosomal recessive types. Failure to express various functional components of the multiprotein complex. This results in failure to activate neutrophil respiratory burst leading to lack of killing of catalase-positive microbes. The diagnosis is made by a positive Nitroblue tetrazolium (NBT) test in which normal leukocytes generating reactive oxygen intermediates are capable of converting yellow NBT to blue but neutrophils with this deficiency can’t. (b) Glucose 6-phosphate dehydrogenase deficiency (c) Myeloperoxiadse deficiency (d) Deficiency of glutathione reductase & glutatione synthetase 3. ABNORMALITIES OF ADHESION (a) Leukocyte adhesion deficiency, type 1 & 2 (b) Neutrophil actin dysfunction The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 4. DEFECTS IN MOTILE RESPONSE (a) Hyper IgE syndrome (b) Defects in generation of chemotactic signals (c) Direct inhibition of motility by glucocorticoids & ethanol APPROACH TO PATIENTS WITH REPEATED INFECTIONS: [Adapted from Lehrer. Ann Intern Med 1988;109:127] The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. 10 White Blood Cells 11 EOSINOPHILS: (0.015 – 0.65 x 109/L; 0 – 7% of all circulating leukocytes) Eosinophils are non-dividing, end-stage cells that, like other leukocytes, differentiate from the hematopoietic stem cells in the marrow. Eosinophils migrate into the blood, where they circulate with a half-life of about 18 hours before entering into the tissues. Eosinophils are primarily tissue-dwelling cells with about 100 tissue eosinophils to 1 blood eosinophils. They are much less numerous than neutrophils but more numerous than basophils in the blood. In tissues they are more numerous than neutrophils as resident granulocytes. Normal adult marrow contains about 3% eosinophils. Normal eosinophils usually show a bilobed nucleus and multiple large granules. Eosinophils, like other granulocytes, can generate, proinflammatory mediators and are involved in specific inflammatory responses including but not limited to allergic reactions, responses to parasitic infections, responses to certain drugs and certain chronic inflammatory disorders. Eosinophil granules contain a number of proinflammatory mediators including (1) Major basic protein, (2) Eosinophil peroxidase, (3) Eosinophil cationic protein, and (4) Eosinophil-derived neurotoxin. Eosinophils are also capable of generating an array of lipid mediators. A number of cytokines are also produced by eosinophils as shown below. [This picture is adapted from The Molecular Basis of Blood Diseases, 3 rd edition, W.B Saunders Co.] BENIGN DISORDERS OF EOSINOPHILS: Most of the benign disorders in clinical practice are quantitative ones especially an increase in eosinophil count. A decrease in the eosinophil count is usually not a clinical problem and results from generalized bone marrow suppression either acquired, congenital or as a result of marrow replacement by malignancies. A much commoner problem is eosinophilia that at times can be quite enigmatic. Some of the causes of eosinophilia are given below: The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 12 A) COMMON CAUSES: 1. Parasitic infections (a) Ascariasis (b) Toxocara canis (c) Filiriasis (d) Othet 2. Allergic reactions (a) Allergic rhinitis (b) Atopic dermatitis (c) Urticaria/angioedema (d) Asthma B) UNCOMMON CAUSES: 1. Drug reactions – many drugs 2. Myeloid leukemias – AML-M2Eo, AML-M4Eo, CML 3. Lymphomas – T-cell lymphomas, Hodgkin lymphomas 4. Celiac disease 5. Solid tumors 6. Pulmonary eosinophilia 7. Cystic fibrosis 8. Bullous phemphigoid C) RARE CAUSES: 1. Mycobacterial infections 2. Bacterial infections 3. Fungal infections 4. Viral infections 5. Histiocytosis X 6. Hyper IgE syndrome 7. Idiopathic hypereosinophilic syndrome 8. Eosinophilic leukemia 9. IL-2 therapy 10. Rheumatoid arthritis BASOPHILS: (0.020 – 0.080 x 109/L; 0 – 2% of all circulating leukocytes) Basophils are the least numerous of all granulocytes in the peripheral blood. They have many similarities to tissue mast cells and some resemblance to monocyte lineage. Basophils circulate as mature cells in the blood and can be recruited to the tissues but they generally do not reside in the tissues. Both basophils and mast cells express highaffinity IgE receptor on their surface and have been regarded as important mediators in asthma, hay fever, and other allergic reactions. Basophils contain many proinflammatory mediators in their granules, can generate lipid metabolites, and secrete cytokines. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 13 BENIGN DISORDERS OF BASOPHILS: Most of the benign disorders in clinical practice are quantitative ones especially an increase in basophil count, which in itself is uncommon. A decrease in the basophil count is usually not a clinical problem and results from generalized bone marrow suppression either acquired, congenital or as a result of marrow replacement by malignancies. More commonly seen is basophilia that at times can be quite enigmatic. Some of the causes of basophilia are given below: A) BASOPHILIA: 1. Allergy or inflammation (a) Ulcerative colitis (b) Drug, food and inhalant hypersensitivity (c) Erythroderma (d) Juvenile rheumatoid arthritis 2. Endocrinopathy (a) Diabetes mellitus (b) Hypothyroidism (c) Estrogen administration 3. Infections (a) Chickenpox (b) Influenza (c) Smallpox (d) Tuberculosis 4. Iron deficiency 5. Neoplasia (a) Chronic myelogenous leukemia (b) Basophilic leukemia The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 14 LYMPHOCYTES: (1.0 – 4.8 x 109/L; 15%-45% of all circulating leukocytes) Lymphocytes as a group are the second most common white blood cells are essential to life. Functionally, there are three main groups of lymphocytes: (1) B-lymphocytes, (2) Tlymphocytes, and, (3) NK-lymphocytes. All the lymphocytes are derived from precursors in the bone marrow. They are the essential members of the immune and chronic inflammatory system and mediate a variety of functions as a group. [This picture is adapted from Immunology by Roitt et al, 5th edition. Mosby Press] B-LYMPHOCYTES: The B-lymphocytes (B-cells) comprise about 10%-20% of all circulating lymphocytes. They constitute more than 95% of the lymphocytes present in the lymphoid follicles seen in the lymph nodes, spleen, tonsils and adenoids, and, appendix. They are also found widely distributed in extralymphatic organs in regions known as mucosa-associatedlymphoid tissue (MALT) such as peribronchial epithelial lymphocytes and lymphocytes seen in the epithelia of gastrointestinal tract where B-cells secrete IgA for mucosal immune defense system. Small numbers of B-cells are also present in thymus. Lymphoid follicles and hence B-cells can also be seen in reactive conditions in various other organs where normal lymphoid follicles are not seen such as thymus, bone marrow, thyroid, cervix uteri, conjunctiva and other organs. The main function of B-cells is to produce immunoglobulins. Most of the secretory immunoglobulin is produced by plasma cells, which are terminally-differentiated B-cells. The B-cell recognizes antigens through their surface receptors, which is essentially a complex of surface immunoglobulin M (IgM) in complex with a heterodimer of transmembrane proteins Ig (CD79a) and Ig (CD79b). The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 15 [This picture is adapted from Immunology by Roitt et al, 5th edition. Mosby Press] The B-cell contains multiple cell surface markers that are involved in a variety of cell functions. Few of the B-cell “markers” include the following: 1. CD19 (earliest B-cell marker. Present on all B-cells) 2. CD79 (B-cell specific marker) 3. CD20 (present mostly on mature B-cells and not on TdT+ B-cell precursors) 4. CD10 (present on many TdT+ precursors and on germinal center B-cells only) 5. CD21 (EBV receptors) 6. CD40 (Activation marker) 7. Surface immunoglobulins (most specific for B-lineage cells) The B-cells do not contain any granules but may include cytoplasmic immunoglobulin inclusions in some reactive conditions. The terminally differentiated plasma cells contain a slightly different array of surface markers distinct from B-cells. In contrast to B-cells, plasma cells do not contain CD19, CD20, or surface immunoglobulins but contain CD30, CD38, and CD138 molecules. BENIGN DISORDERS OF B-LYMPHOCYTES: The reduction in the number of B-lymphocytes is mainly due to loss of B-progenitors by malignancy or marrow aplasia. A) PRIMARY/CONGENITAL 1. Agammaglobulinemia 2. Selective agammaglobulinemia 3. X-linked lymphoproliferative disease 4. Immunodeficiency with elevated IgM 5. Hyperimmunoglobulin A, D, or E syndrome B) ACQUIRED 1. Idiopathic Persistent polyclonal B-lymphocytosis 2. Polyclonal B-lymphocytosis associated with certain infections The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 16 T-LYMPHOCYTES: T-lymphocytes (T-cells) comprise about 60% - 70% of the circulating peripheral blood lymphocytes. T-cells are the main lymphocytes of the thymus where T-cell maturation and self-antigen recognition occurs. T-cells are also found in the interfollicular zone of lymph nodes, and, tonsils, and in the periarteriolar sheath of the spleen. They are also widely distributed in the extralymphatic organs mainly in the lamina propria and as intraepithelial lymphocytes of gastrointestinal tract, respiratory tract and other organs. Functionally, T-cells are of two main groups: T-helper cells (CD4+CD8-) and Tcytotoxic cells (CD8+CD4-). Two subsets of CD4+ T-cells are identified, TH-1, which synthesizes & secrete IL-2 & INF-, & TH2, which synthesizes and secrete IL-4, & IL-5. [This picture is adapted from Immunology by Roitt et al, 5th edition. Mosby Press] The T-cells contain a heterodimeric T-cell receptor in complex with CD3 molecule. [This picture is adapted from Robbins Pathologic Basis of Diseases, 6th edition, W.B Saunders Co.] The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 17 The T-cell contains two main, mutually exclusive types of T-cell receptors (TCR): type (as shown above) and -type. In the peripheral blood 95% of T-cell bear -type of TCR whereas other epithelia contain a slightly larger population of -type TCR. [This picture is adapted from Immunology by Roitt et al, 5th edition. Mosby Press] CD4+ T-cells recognize antigens in association with class II major histocompatibility molecule (MHC) whereas class I MHC molecules present antigens to CD8+ T-cells. [These pictures are adapted from Robbins Pathologic Basis of Diseases, 6th edition, W.B Saunders Co.] The main function of T-helper cells is to secrete cytokines that influence the functions of almost all other cells of the immune system such as activation of macrophages and also help B-cells in maturation. That is why we always seen a few CD4+ T-cell within germinal centers of lymphoid follicles where T-helper cells are involved in B-cell maturation and differentiation. The CD8+ T-cells are directly cytotoxic to viruses and may be other cells and also produce some cytokines. A subset of T-cells, especially CD8+ cytotoxic T-cells contain granules that are morphologically recognized as large granular lymphocytes (CD3+ LGL). The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 18 The T-cells exhibit a variety of surface receptors including but not limited to the following: 1. CD3 (most T-cell specific) 2. CD4+ (T-helper cells; also expressed by monocytes) 3. CD8+ (T-cytotoxic cells; also expressed by NK-cells) 4. CD2 (also expressed by monocytes) 5. CD1 (Cortical thymocytes only) 6. CD5 (also expressed normally by a subset of mantle zone B-cells of follicles) 7. CD7 (earliest T-cell marker) 8. T-cell receptor (T-cell specific) 9. CD45R0 10. CD43 BENIGN DISORDERS OF T-LYMPHOCYTES: The term lymphopenia and peripheral lymphocytosis in clinical practice almost always refer to T-cell disorders rather than B-cells. Some of the disorders are listed below: A) T-LYMPHOCYTE DEFICIENCY OR DYSFUNCTION: 1. Thymic aplasia (DiGeorge syndrome) 2. Thymic dysplasia (Nezlelof syndrome) 3. Wiskott-Aldrich syndrome 4. LFA-1 deficiency 5. Cartilage-Nail hypoplasia 6. AIDS, CD4+ T-cell deficiency 7. Combined T-cell and B-cell deficiency states 8. Viral infections – Hepatitis, Influenza, Herpes virus 8 infections 9. Iatrogenic 10. Marrow aplasia or hypoplasia B) T-LYMPHOCYTOSIS 1. EBV mononucleosis 2. CMV mononucleosis 3. Other mononucleosis syndromes 4. Certain viral infections – Rubella virus, Herpes simplex type II, adenovirus 5. Autoimmune disorders 6. Sarcoidosis 7. Chronic inflammatory conditions 8. Thymoma 9. Post-splenectomy 10. Cigarette smoking 11. Bordetella pertussis lymphocytosis 12. Stress lymphocytosis The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 19 NATURAL KILLER LYMPHOCYTES (NK-CELLS): NK-cells constitute about 10-15% of the peripheral blood lymphocytes and do not contain cell surface T-cell receptors or immunoglobulins and hence these cells do not rearrange either T-cell receptor of immunoglobulin genes. They are called natural killer cells because they can cause cytotoxicity without prior sensitization by antigens. This innate ability to kill virus-infected cells and some tumor cells is the first-line defense of the body’s immune system. Morphologically, these cells are larger than small B-cells or T-cells and contain azurophilic granules and are also called large granular lymphocytes (LGL). It should be remembered, however, that a fraction of CD8+ T-cells also contains granules and also constitute the LGLs. Thus LGLs are of two types: CD3 NK-cells, and, CD3+CD8+ T-cells. NK-cells do not contain surface CD3 molecules but contain CD16, CD56, and also CD8 molecules. NK-cells also secrete some cytokines including IFN-, TNF- and, GM-CSF. The mechanism of NK-cell mediated cytotoxicity is shown below: [These pictures are adapted from Robbins Pathologic Basis of Diseases, 6th edition, W.B Saunders Co.] NK-cells are increased in viral infections, autoimmune disorders, some chronic inflammatory conditions, and in malignancies. The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 20 MONOCYTES/MACROPHAGES: (0.2 – 0.8 x 109/L; 2%-10% of all circulating leukocytes) Circulating monocytes and tissue macrophage and related antigen presenting cells form a widely distributed system of mononuclear phagocytes (MNP). [These pictures are adapted from Immunology by Roitt et al, 5th edition. Mosby Press] The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 21 Macrophages are the antigen presenting cells to T-cells in association with MHC class II molecules. Circulating monocyte is a large cell, about 12-15 m in diameter, contains a unilobed round to irregular nucleus and very small azurophilic granules. During an inflammatory response, these monocytes migrate to tissue and become tissue macrophages/histiocytes. These tissue macrophages and other related antigen-presenting cells including follicular dendritic cells and interdigitating reticulm cells of the node and Langerhans cells of the skin process antigens and present them to CD4+ T-cells. They exhibit a distinct surface marker profile that includes expression of CD2, CD4, CD11, CD14, CD33, CD64, and CD68. Macrophages secrete a variety of cytokines and perform myriad of functions in inflammation as shown below: [These pictures are adapted from Robbins Pathologic Basis of Diseases, 6th edition, W.B Saunders Co.] In addition to class II MHC molecules, monocytes/macrophages contain numerous surface receptors; some of which are listed below: 1. Fc receptors for IgG, IgE, IgA 2. Complement receptors – C3b, C3bi, C5a, C1q 3. Cytokine receptors – for IL-1, Il-2, IL-3, IL-4, INF-, INF-, INF-, GM-CSF 4. Chemokine receptors – for CCR1, CCR2, CCR3, CXCR4, CCR5 5. Receptors for small peptides – for histamine, vitamin D, serotonin, endorphins 6. Hormone receptors – insulin, glucocorticoids, angiotensin 7. Fibronectin and Laminin receptors The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended. White Blood Cells 22 BENIGN DISORDERS OF MONOCYTES/MACROPHAGES: Monocytosis and tissue histiocytosis is a much commoner problem in clinical practice than monocytopenia. A variety of conditions are associated with an increase in monocytes and/or tissue macrophages. Some of the benign disorders are shown below: (A) MONOCYTOPENIA: 1. Aplastic anemia 2. Hairy cell leukemia 3. Glucocorticoid therapy (B) BENIGN MONOCYTOSIS/HISTIOCYTOSIS: 1. Reactive infection-associated monocytosis 2. Primary hemophagocytosis 3. Infection-associated hemophagocytosis 4. Drug-associated hemophagocytosis 5. Rosai-Dorfman disease 6. Gaucher disease 7. Niemann-Pick disease 8. Gangliosidosis 9. Reactive Langerhans cell histiocytosis (C) MONOCYTE/MACROPHAGE DYSFUNCTION: 1. Alpha-1 proteinase inhibitor deficiency 2. Chediak-Higashi syndrome 3. Chronic granulomatous disease 4. Glucocorticoid therapy 5. Kawasaki disease 6. Solid tumors 7. Tobacco smoking The contents & pictures in this handout are derived from various sources including books, journal articles and patient material for teaching purposes only. No commercial incentives are sought or intended.