Chapter 24 - Las Positas College
advertisement

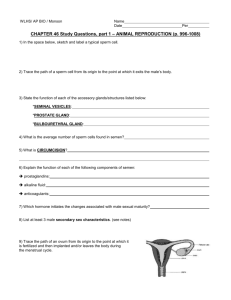
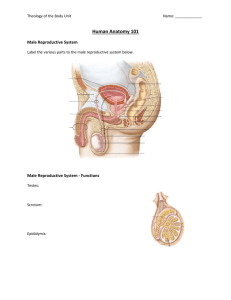
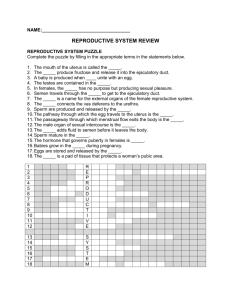
Chapter 24 The Reproductive System I. The Male Reproductive System (pp. 712–722, Figs. 24.1–24.10) A. The function of the male and the female reproductive systems is to produce offspring; the primary sex organs, the gonads, produce gametes: the sperm in males, and the egg in females. (p. 712, Fig. 24.1) B. All other genitalia in both sexes are accessory sex organs. (p. 712) C. The scrotum is an external sac of skin that contains the testes. (pp. 712–713, Figs. 24.1–24.2) D. The testes are the male primary sex organs, or gonads, and are the site of sperm production. (pp. 713–714, Fig. 24.3) 1. Gross anatomical examination of a testis reveals the size is about 2.5 cm (1 inch) in width and 4 cm in length; the tunica vaginalis partially encloses each testis. (pp. 713–714, Fig. 24.3) 2. Seminiferous tubules are the sperm-forming tubules; spermatogenesis is the process of forming sperm cells. (pp. 714–717, Figs. 24.3–24.5) i. Spermatogenic cells are spermatogonia, primary and secondary spermatocytes, and spermatids. (p. 715, Fig. 24.4) ii. Successive stages of spermatogenesis are (1) formation of spermatocytes, (2) meiosis, and (3) spermiogenesis. (p. 715, Figs. 24.4–24.5) iii. Sustentacular cells surround spermatogenic cells and form the blood-testis barrier. (pp. 715–716) iv. Myoid cells surround seminiferous tubules and help squeeze sperm through the tubules. (p. 717, Fig. 24.3b) v. Interstitial cells secrete androgens, primarily testosterone. (p. 717, Fig. 24.3b) E. The reproductive duct system in males traces the pathway sperm cells follow beginning with the seminiferous tubules and ending with the urethra. (pp. 717–720, Figs. 24.5–24.7) 1. The epididymis is the site where sperm mature. (pp. 718–719, Fig. 24.6) 2. The ductus deferens stores and transports sperm during ejaculation. (pp. 718–719, Figs. 24.1 and 24.6) 3. The spermatic cord contains the ductus deferens, blood vessels, and nerves; the inferior part lies in the scrotum and the superior part runs through the inguinal canal. (p. 719, Fig. 24.7) 4. The urethra carries sperm from the ejaculatory duct to outside the body. (p. 720, Fig. 24.8) F. Accessory glands in males include the seminal vesicles, the prostate gland, and the bulbourethral glands; accessory glands produce secretions that contribute to semen formation. (pp. 720–722, Figs. 24.1 and 24.8– 24.9) 1. The paired seminal vesicles secrete a sugar-rich fluid that forms 60% of the ejaculate. (pp. 720–721, Figs. 24.1 and 24.8) 2. The prostate gland surrounds the prostatic urethra; its secretions constitute about one-third of the volume of semen and function to clot and liquefy ejaculated semen. (pp. 721–722, Figs. 24.8–24.9) 3. The bulbourethral glands produce mucus that lubricates the urethra for sperm passage. (pp. 721–722, Figs. 24.1 and 24.8) G. The penis is the male organ of intercourse and delivers sperm into the female reproductive tract. (p. 722, Figs. 24.1–24.8) H. The male perineum contains the scrotum, the root of the penis, and the anus; the bony landmarks are the coccyx, the ischial tuberosities, and the pubic symphysis. (p. 722, Fig. 24.10) II. The Female Reproductive System (pp. 723–736, Figs. 24.11–24.22) A. The female reproductive system differs from the male system in several important ways; the gametes are eggs, female organs prepare to support developing offspring, and female organs undergo changes according to the reproductive cycle called the menstrual cycle. (p. 723, Figs. 24.11 and 24.19) B. The ovaries are the female primary sex organs and the site of egg cell production. (pp. 723–727, Figs. 24.11– 24.13) 1. The ovarian cycle is the monthly menstrual cycle as it relates to the ovary; the ovarian cycle has three phases: (1) the follicular phase, (2) ovulation, and (3) the luteal phase. (pp. 724–727, Figs. 24.13–24.14) i. During the follicular phase (first half of the ovarian cycle, days 1–14), 6–12 primordial follicles start to grow. (pp. 724–726, Fig. 24.13) ii. Ovulation is the midpoint of the ovarian cycle; an oocyte is released from a follicle at the surface of the ovary. (p. 726, Fig. 24.14) iii. In the luteal phase (second half of the ovarian cycle, days 15–28), the ruptured follicle becomes the corpus luteum. (p. 726, Fig. 24.13) 2. Oogenesis, the production of female gametes, starts before birth and takes decades to complete. (pp. 726– 727, Fig. 24.15) C. The uterine tubes (also called fallopian tubes or oviducts) receive the ovulated oocyte and provide a site for fertilization. (pp. 727–728, Figs. 24.11–24.12 and 24.16–24.17) D. The uterus (womb) is a hollow, thick-walled organ whose functions are to receive, retain, and nourish a fertilized egg throughout pregnancy. (pp. 728–734, Figs. 24.11–24.12 and 24.17–24.19) 1. Supports of the uterus are several ligaments, mesenteries, and muscles of the pelvic floor. (p. 729, Figs. 24.11–24.12 and 24.17) 2. The uterine wall is composed of three basic layers: an outer perimetrium, a middle myometrium, and an inner endometrium. (pp. 729–730, Figs. 24.12 and 24.18) 3. The uterine cycle is the menstrual cycle as it involves the endometrium. (pp. 730–731 and 734, Fig. 24.19) E. The vagina is the distensible, muscular tube that connects the uterus to the body’s exterior; it receives the penis and semen during intercourse and acts as the birth canal. (p. 734, Figs. 24.11–24.12) F. The external genitalia, also called the vulva, are the female reproductive structures that lie external to the vagina in the diamond-shaped perineum. (pp. 734–735, Fig. 24.20) G. The mammary glands are modified sweat glands that are present in both sexes but function only in lactating females. (pp. 735–736, Fig. 24.21) III. Pregnancy and Childbirth (pp. 736–742, Figs. 24.22–24.25) A. Pregnancy begins with a fertilized oocyte and ends with production of offspring nine months later. (p. 736) 1. Events leading to fertilization are the acrosomal and cortical reactions that accomplish the sperm penetration of an oocyte. (pp. 736–738, Fig. 24.22) 2. Implantation occurs in the uterus about six days after fertilization. (p. 738, Figs. 24.23–24.24) 3. Formation of the placenta involves both embryonic (trophoblastic) and maternal (endometrial) tissues. (pp. 738–740, Fig. 24.24) 4. Anatomy of the placenta ensures no mixing of maternal and fetal blood occurs; the placenta is an organ of transport between the mother and fetus. (pp. 740–741, Fig. 24.24) B. Childbirth or parturition, the act of giving birth, occurs an average of 266 days after fertilization and 280 days after the last menstrual period; the stages of labor include dilation, expulsion, and the placental stage. (pp. 741– 742, Fig. 24.25) IV. Disorders of the Reproductive System (pp. 742–743) A. Cancers are the primary cause of disorders of the male and female reproductive systems. (p. 742) B. Reproductive system cancers in males include testicular cancer and prostate cancer. (p. 742) 1. Testicular cancer affects approximately 1 of 50,000 males most often in the age bracket of 15–35 years; this cancer is cured in 95% of all cases. 2. Prostate cancer is a slow-growing cancer that is the second most common cause of cancer death in men; lung cancer is first. C. Reproductive cancers in females include ovarian cancer, endometrial cancer, cervical cancer, and breast cancer. (pp. 742–743) 1. Ovarian cancer affects 1.4% of women and is the fifth most common cause of cancer death in women. 2. Endometrial cancer affects 2% of women and is the fourth most common cause of death in women (after lung, breast, and colorectal cancers). 3. Cervical cancer occurs in 1% of women between ages 30–50 years; survival rates improve with early detection. 4. Breast cancer, the second most common cause of cancer deaths in women, kills 3% of the women in the United States. V. The Reproductive System Throughout Life (pp. 743–747, Figs. 24.26–24.28) A. Embryonic development of the sex organs of both males and females begin development during week 5. (pp. 743–745, Figs. 24.26–24.27) B. Descent of the gonads occurs in both sexes after forming in the dorsal abdomen; testes descend into the scrotum and ovaries descend into the pelvis. (pp. 746–747, Fig. 24.28) C. Puberty generally occurs between ages 10 and 15 when reproductive organs mature and reproduction is possible. (p. 747) D. Menopause in women occurs normally between ages 46 and 54 and marks the end of ovulation and menstruation. (p. 747) SUPPLEMENTAL STUDENT MATERIALS to Human Anatomy, Fifth Edition Chapter 24: The Reproductive System To the Student Up to this point, along with the structure and function, you have studied the embryology, growth, and development of all the systems that make you unique from other organisms. Your study of male and female reproductive systems provides the information you need to understand how you, as a species, physically survive from one generation to the next. In terms of the human life cycle, this is the last topic to explore. The reproductive system includes the study of the phenomenal mechanisms that result in the production of gametes by the testes and ovaries, and the supporting roles of the many male and female organs that ultimately accomplish the overall reproductive goal, production of offspring. The amount of information is vast and decidedly complicated because of the vital roles played by hormones in processes such as the menstrual cycle and pregnancy. Step 1: Describe the structure and function of the organs of the male reproductive system. - Define sexual reproduction. - Identify the primary sex organs or gonads of the male and comment on their delayed development compared to other organ systems of the human. - Describe the scrotum, and explain the associated structures that aid in regulation of temperature for the testes. - Define testis, identifying its primary functions and structural features, and explain the origin of the word. - Explain completely the details of spermatogenesis, using diagrams and time lines, including the formation of spermatocytes, meiosis, and spermiogensis. - Explain how meiosis differs from mitosis, and indicate how many functional sperm result from one diploid cell. - Distinguish clearly between examples, structure, and function of spermatogenic cells, sustentacular cells, myoid cells, and interstitial cells and identify whether each type of cell identified is haploid or diploid. Step 2: Describe the reproductive duct system in males. - List the individual parts of the system of ducts through which sperm travel from their point of origin in the testis to the external urethral orifice, explaining the location of each part. - Explain the location, histology, and functions of the epididymis. (Hint: Remember sperm are stored here for weeks.) - Explain how sperm move through the ductus (vas) deferens. - Describe the anatomical path of the ductus deferens through the pelvic cavity. - Describe the location of the spermatic cord, including its components, and clearly distinguish between it and the ductus deferens. - Describe the descent of the testes, an embryological event covered near the end of the chapter, explaining how the tunica vaginalis is a peritoneal structure. - Identify the location, structure, and function of the male urethra, relating to its three parts. Step 3: Describe the accessory glands associated with the male reproductive system. - Describe the location, structure, and function of the seminal vesicles, including details of the secretion produced. - Describe the location, structure, and function of the prostate, including details of the secretion produced. - Describe the location, structure, and function of the bulbourethral glands, including details of the secretion produced. Step 4: Describe the penis and male perineum. - Describe the gross anatomy of the penis, explaining its function. - Identify the types of erectile tissues, explaining the mechanism of erection and why the erect penis does not buckle or kink during intercourse. - Distinguish between erection and ejaculation. - Draw the diamond-shaped region of the male perineum, and label the bony landmarks, structures, and openings contained there. Step 5: Describe the structure and function of the female gonads, including ovum production and associated hormonal events. - Identify the primary sex organs or gonads of the female and comment on their delayed development compared to other organ systems of the human. - Describe the location, structure, and function of the ovaries, including their supporting mesenteries and ligaments. - Define and describe the menstrual cycle, summarizing structural and hormonal changes occurring to the ovary. - Define and describe the follicular phase, ovulation, and the luteal phase of the ovarian cycle, including the names of hormones and hormonal functions. - Distinguish clearly between FSH and LH, listing functions associated with the menstrual cycle. (Hint: Do not forget that although these hormones are named for female structures, they also have male functions.) - Explain how the corpus luteum functions as an endocrine gland. - Explain completely the details of oogenesis, using flowchart diagrams and time lines, including the formation of oogonia, meiosis, and ova. - Identify which cells in the oogenesis flowchart are haploid and which are diploid. - Explain how many functional ova result from one diploid cell. - Identify the structure from which an oocyte ovulates and the precise space into which it is released. - Define fertilization. Step 6: Describe the accessory ducts and organs associated with the female reproductive system. - Describe the location, structure, and function of the uterine tubes, including specific regions and the histology of the tubular wall. - Explain how the ovulated oocyte is propelled into the infundibulum from the peritoneal cavity of the pelvis. - Note the characteristics of the uterine tube that aid movement and help sustain the oocyte or possible embryo on its journey to the uterus. - Describe the location, structure, and function of the uterus, including its gross anatomical features and the function of cervical mucus. - Name and describe the uterine supporting ligaments and mesenteries. - Name the tunics of the uterine wall, explaining their functions. - Describe the uterine structural and hormonal changes associated with the menstrual cycle, identifying three phases. - Explain what happens if fertilization and implantation occur, as well as what happens physically if those events do not occur. - Relate and explain the structure of the vagina to its function, including the layers of the vaginal wall. - Distinguish between the fornix of the vagina and the cervix of the uterus. Step 7: Describe the vulva and female perineum. - List, locate, and describe the structures of the female external genitalia. - Define the term homologue, and identify four male and female homologous structures. - Diagram the female perineum as a diamond-shaped region, and label its bony landmarks, openings, and associated structures. - Describe the structure and function of the mammary glands, distinguishing between mammary glands and breasts. Step 8: Describe the events that occur in the female reproductive tract during pregnancy and childbirth. - Review stages of basic embryology in Chapter 3. - Define fertilization and discuss events leading to sperm penetration of an oocyte. - Describe the process of implantation. - Explain the formation of the placenta, including its structure and function. - Explain the three successive stages of labor involved in childbirth. Step 9: Explore the disorders of the reproductive system and changes that occur with aging. - Read about reproductive system cancers in males: testicular cancer and prostate cancer, and focus on specific details as instructed by your professor. - Read about reproductive cancers in females: ovarian cancer, endometrial cancer, cervical cancer, and breast cancer, and focus on specific details as instructed by your professor. - Describe the embryonic development of the sex organs, and explain why the male ducts and female ducts are not homologous. - Describe the descent of the gonads, naming termination points. - Note the anatomical changes that occur during puberty and menopause.