to study from
advertisement

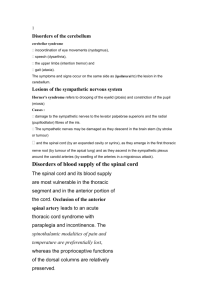
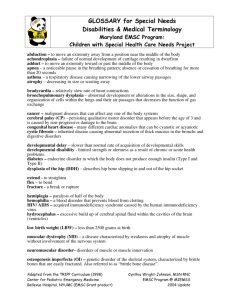
MUSCULOSKELETAL SYSTEM I. Anatomy and Physiology of the Musculoskeletal System biggest problem is interference with daily living (ADL activities of daily living like opening milk carton) worry about elderly in surgery due to clots, infection and respiratory complications A. Bones B. Muscles skeletal cardiac smooth C. Tendons muscles attach to bone D. Bursae muscles glide over bone, can be inflamed = pain so ADL limited E. Joints bone and ligaments joined F. Ligaments G. Synovial membrane Rheumatoid arthritis= swelling solidification of joints II. Common Descriptive Terms for Joint Range of Motion(ROM) and Movements of Skeletal Muscles do range of motion – must know these terms so physician can tell you how to position patient A. Flexion: decrease in joint angle, bending of the extremity at the joint. B. Extension: increase in joint angle, straightening of the extremity at the joint. C. Abduction: to move away from the midline of the body. D. Adduction: to move toward the midline of the body. E. Inversion: to rotate inward refers to sole of foot. F. Eversion: to rotate outward. Sole of foot only G. Pronation: to turn or face body or body part downward. H. Supination: to turn or face body or body upward.palm up carry soup in hand I. Internal rotation: to turn toward the midline of the body. We turn person toward midline – if broken hip pillows whole leg turned inwards J. External rotation: to turn away from the midline of the body. Turn away from body Need to know for traction = internal and external rotation III. Developmental Considerations old persons= bone density decr dt osteoporosis. Women worse after menopause. Incr kyphosis so shrink, vertebral column starts to collapse since weight bearing, so shrink muscles shrink in size, articular cartilages deteriorates so bones not cushioned so develop degenerative joint disease – do joint replacement which lasts 10-15 years Know about safety in home for adults and kids throw rugs are risk factors, side rails on beds can only use one or 2 more than than and need a MD order to put restraints or 3-4 rails are restraints so outlawed some beds on floor IV. Examination Technique: Musculoskeletal System (in check off only need to assess upper extremities and shoulders for range of movement) Pain most common problem and it limits ADL A. Overall Appearance 1. Abnormal findings B. C. D. a. dwarfism decr growth hormone prior to puberty, if adult it is a disproportion growth. If give growth hormone, causes diabetes, secondary heart and kidney disease due to diabetes, can develop hypertension at age 19. organs will be small in size a. Acromegaly look at hands and feet, thyroid enlarge so voice husky, look for cardio and renal probls b. Osteoporosis frail easy fractures low density give calcium c. Missing limbs need to note if trying to feed or elevate. If artificial – take it home so not stolen d. Polydactyl extra fingers e. Syndactyl fingers fused Posture 1. Abnormal findings a. thoracic kyphosis a. poor posture – largest cause is back pain Gait and Mobility 1. Abnormal findings a. spastic hemiparesis upper motor neuron lesion stroke or brain bleed if lower extremity have to swing leg to move it so spastic beware of stair climbing if in apartment b. cerebellar ataxia multiple sclerosis or if on alcohol c. *****festinating gait hesitate then shuffle parkinsons impt shuffling gait, hesitate to start moving, posture stooped, lose arm hand swing to give balance, so fall, walk into walls . Normal intellect though d. steppage or footdrop stroke or spinal cord injury slap foot to floor, if in bed, foot will drop so wear boot to keep foor dorsoflexed. Again a problem with stair climbing. Put plastic brace to help with steps e. gait of older adult old people move slow. Don’t like to rise early and have problem opening things like butter, milk cartons, salt packets. f. scissors gait walk with ballon between thighs multiple sclerosis only lower legs really move PT and OT will get patients home – will assess home Inspection of Muscle Size and Shape 1. Abnormal findings a. Hypertrophy weight lifting, pathologic or physiologic b. Atrophy of disuse – in cast 6-8 weeks, spinal cord injury c. limited ROM - inflammation and pain, try to move – don’t want joints to solidify d. ***involuntary movements – resting and intention tremors e. resting tremors parkinsons, lack dopamine, constant movement look for pill rolling in fingers, at rest if working on purposeful movements the tremor will subside f. g. h. i. j. E. intention tremors multiple sclerosis – tremor when trying to stimulate muscles to do something. Opposite of resting tremor. Demylination – releasing sparks fasciculations twitching of muscle group tics same as fasciculations chorea random movement of muscle groups Huntingtons need side rails, yell, exaggerate movement if stimulated like need to poop . need extended care athetosis cerebral palsy trunk stable withering movement that goes away when sleep. CP due to lack of oxygen Joints 1. Abnormal findings a. rheumatoid changes swollen hot bilateral, in pleura, kidney, b. dislocation will put pressure on nerves be careful c. tophi nodules of uric acid in elbows and ears, kidney disease, gout d. inflammation F. Muscle Tone should feel resistance when testing strength 1. Abnormal findings a. Flaccidity (hypotonicity) spinal cord injury below the level of injury limb will drop to bed b. Spasticity opposite to flaccidity. Contraction – stroke and end stage of parkinsons- resistant muscles c. Crepitus knees cracking, bone fragments rubbing G. Muscle Strength 1. Abnormal findings check if bilateral – test simultaneously hands, feet, legs a. diffuse reduction in muscle strength fatigue or pain if not a chronic disease. Flu, multiple sclerosis b. hemiparesis (hemiplegia) stroke H. Spine 1. Abnormal findings a. Scoliosis butt facing you bend down and run finger up verterbral column. Can treat if adolescent, one leg will become shorter so will need one higher shoe. b. kyphosis c. lordosis concave lumbar spine, pregnancy or obesity push belly out I. Assessing Musculoskeletal Pain and weakness medicate to get out of bed to avoid hospital complications and to get home. MENTAL STATUS AND NEUROLOGICAL EXAM I. Anatomy and Physiology of the Nervous System - Assessment includes not tested on the anatomy part must know it controls all body function Macro structure: Brain CSF and Blood in under skull if any one incr in volume you get incr ICP. Heart can’t fix so will not get blood to brain, head will die. Give steroids to decr edema **** not for change in level of consciousness - orientation evaluation of motor, sensory, autonomic, cognitive and behavioral elements. A. Protective Membranes 1. Macrostructure skull covers brain, blood CSF 2. Meninges sheaths neuro system B. Division of the Nervous System 1. CNS (brain and spinal cord) 2. Peripheral Nervous System (outside the CNS) 3. Autonomic Nervous System a. Sympathetic fight or flight, compensatory for cardio renal insufficiency b. Parasympathetic compensates sympathetic C. The Brain (Major units: Cerebrum, cerebellum and brain stem) 1. Cerebrum a. cerebral cortex (gray matter) b. lobes 2. Cerebellum – coordination/equilibrium Parkinsons 3. Brain stem – cranial nerves arise *** CONTROL MUSCLE MOVEMENT FROM NECK ABOVE outside vagus which also controls diaphragm, heart and lungs. If swelling, incr ICP.and will cut off breathing- big problem D. ***Cranial Nerves (12 pairs) PGE 667 1 Olfactory II optic III oculomotor trochlear ascending track is sensory pathway descending motor track (tells muscles what to do) some affect one or the other or both E. F. G. H. Spinal Cord – Ascending/Descending Tracts Major Sensory Pathways (ascending tracts) 1. Posterior (dorsal Column) 2. Spinothalamic tract Major Motor Pathways (descending tract) 1. Pyramidal tract 2. Extrapyramidal tract 3. Cerebellar system Spinal Nerves – 31 pairs – ***Dermatome symmetral bands of skin innervated by sensory routes from spinal cord- touch pain test for peripheral neuropathy glove and boot effect. I. II. Reflex Arc – Defense Mechanism of the Nervous System ***specific response to an adequate stimulus solicited when unconscious. – DTR deep tendon reflex need stimulus to spinal cord synapse. If spinal cord injury below level of reflex, no synapse, no response to hammer. But if a stroke person the reflexes are HYPER reflexive compared to other limb. Sometimes only way to tell if a stroke is to see this hyperreflex. Must distract the patient so they don’t try to modify it. Do relaxation techniques Assessment of the Neurological System A. Developmental considerations 1. Infancy cephalocaudal develops head to toe not completely at birth head first, walking last 2. Older adult at risk for injury to nervous system and susceptible to decr oxygen to brain due to plaque, atherosclerosis arteries giving blood to brain really thin so a problem esp to back of brain. Give blood thinners can’t scrape arteries narrower than 2 cm. Myelin sheath degenerates so nerve conduction and movement is slower. Age 50 brain cells decr 1% per year. Sensory changes = visual and auditory acuity decreases. Can’t feel hot and cold, problems with balance, and some cognitive changes – short term memory lost quicker. B. C. D. Mental status 1. Method of Examination a. LOC alert lethargic semicomatose comatose best to actually chart what you see. “can not shake and yell to arouse” “no response to pain” “can stimulate oral reflex to eat” “eat without gagging” b. language c. mood and affect d. orientation e. attention repeat memorized words, illusions hallucinations “do you ever hear you name when you are alone? f. memory (recent/remote) infection trauma stress besides “do you ever lose your car when you park it” dementia can cause it g. perception h. abstract meaning i. thought processes j. though content k. calculation 2. Abnormal findings a. consciousness b. orientation c. attention d. perception e. memory Communication 1. Method of Examination 2. Abnormal findings a. aphasia worry about swallowing concern get a speech therapist (motor(lose muscle ability to modulate words), sensory aphasia is a general category (lose some sort of comprehension – picture of water bottle, can’t piece together a picture of bedpan and ability to pee), nominally (stroke, lose name of certain item, substitutes name but rest ok. Will have to figure it out. Thinks a cat is the word for dog) syntactical (problems putting sentences together) b. dysarthria too much alcohol c. dyslexia written problems esp if boys and left handers Sensory Assessment look at check off – light touch etc items 58-62 do distally dermatome regions, temperatures (tubes of acetone – see if person can tell) vibrations (sign of peripheral neuropathy – tuning fork Weber and Rinne test) ****position and proprioception on digit – wiggle finger with persons eyes shut – tell if digit up or down. – sensory inervations probs and peripheral neuropathy Write a letter on person’s hand .. 1. Method of Examination 2. Abnormal findings a. Pain *** -hypoalgesia ** decr pain sensation – spinal cord injury -analgesia ** reduce pain give analgesics not to erase it -hyperalgesia ** incr sense to pain often assoc if person has a high fever b. Touch lesions of brain or spinal cord -hypoesthesia decr sense of touch -anesthesia decr sense of touch -hyperesthesia incr sense of touch -paresthesia numbness and tingling, different sensation of pain, ants going up legs, legs prickling renal disease, multiple sclersis -dysesthesia abnormal sense of pain c. Position proprioceptor test of fingers -abnormal findings peripheral neuropathy or spinal cord injury, or treatments with lots of chemo, or lots of RA treatments. d. Vibration spinal cord injury or neuropathy -abnormal findings e. stereognosis -abnormal findings -astereognosis cant recognize the object. Don’t know quarter is a coin. Or what keys are f. graphesthesia cant recognize a number or letter -abnormal findings -graphanesthesia E. Cranial Nerves 1. Method of Examination *** every test do if inhale in – not exhale or get snot. 2. Abnormal findings a. cranial nerve I – anosmia cant detect odor. If bilateral or unilateral. Polyps or if snort dope. But other than that can be cranial nerve problem. In elderly nose, occlude nares and can inhale deeply coffee, cinnamon ***scent under nares and inhale deeply up. b. cranial nerve II – visual acuity distant vision – Snellen chart abnormal findings distant vision stand on making tape on floor – cover right eye – tell color, then read 20/20 line 20/40 pretty good. Then cover left eye and read line backwards – Myopia (nearsightedness) only if do over age 40 hold paper and see how far away they hold it – Hyperopia (farsightedness) – Decreased color vision – Confrontation test – see book wiggle fingers for peripheral vision F. Pupil size gauge with penlight and ruler should constrict in unison. Pupil accommodation should be equal – right and left should both get larger as move pen towards eye test 6 cardinal fields of vision draw and H and an I with finger and look for nystagmus little oscillating movement , cover test. c. cranial nerve III, IV and VI nystagmus – on test. Fine oscillating movement. (myopia, hyperopia) ***dilate from near to distant, ***constrict when shine a light if brain injury may be unilateral d. cranial nerve V trigeminal blunt vs sharp on cheek clench teeth decr sense of pain when clench teeth will have probs chewing, multiple sclerosis e. cranial nerve VII (Bell’s Palsy) facial nerve on one side of face can’t even raise eyebrow.. whole side paralysed f. ****cranial nerve VIII acoustic – crude hearing voice test Weber and Rinne *** air conduction is greater than bone conduction … must to both tests midline feel vibration equal from side to side. (tuning fork on center forehead bone – feel sound on left side ) If a conduction block of air conduction… sound will be greater on that side. If sensory or neuro loss on right sound won’t be in right ear. If tuning fork on ear and block in left ear, can’t feel or hear sound on left ear. Both parts of test weber on forehead. Sound greater on right = block on right or sensoneuro loss on left - do rinne (air conduction and vibration on bone) on mastoid process . and loss is neuro loss (can be ear wax) g. cranial nerves IX and X glosspharyngeal and vagus ah so can see uvula and palate h. cranial nerve XI i. cranial nerve XII tongue location, say light tight dynamite worry about swallowing. Reflexes only do sitting distract partner clench teeth for upper reflexes pull arms for lower reflexes. Bicepts tricepts (large part of hammer – back of arm hit directly) brachioradialis (inside wrist and wrist needs to flex up) knee (dangle off bed foot will extend) achilles (hit back ) planter (metal part of hammer and toes will planter flex curl under up until age 2 ½ will have abnormal planter reflex, and may spread other toes and only dorsoflex big toe) must know exactly what happens when hit. PLUS++ is normal if Arrow points down, normal Babinski 1. Method of Examination 2. Abnormal findings a. Hyperreflexia exaggerated reflex > ++ stroke, can’t decipher stimulus, so more vigorous intense response b. G. H. Hyporeflexia below level of reflex, have no response spinal injury c. clonus stroke with some paralysis and dorsoflex will see a spasm d. ****positive Babinski/plantar great toes dorsoflex and others fan out. Normally they curve down after age 2 1/2 e. Kernigs meningitis flex at knee and then straighten – see pain in back if inflamed meninges f. Brudzinski’s meningitis nuchl rigidity will have stiff neck Cerebellar Function 1. Method of Examination 2. Abnormal findings a. Romberg (hands at side feet apart, close eyes, if upper motor neuron lesions, will fall to side within 20 sec. cerebellum multiple sclerosis, alcohol stroke persons will start to sway) b. Dyssynergy lack of coordination c. Dysmetria cant tell force of speed or distance – parkinsons alzheimers, d. Dysdidochokinesia clumsy Abnormal Postures a. decerebrate rigidity base of brain rigid extremities, cant bend limbs. Can see with MS, worry about bedsores b. decorticate rigidity rigid flexion spinal injuries especially upper extremities. Worry about bedsores Coordination of upper and lower extremities , gait Reading/Learning Activities Jarvis Text: Ch. 7 and 23 THE COMPLETE PHYSICAL ASSESSMENT III. Limit the number of position changes Invasive procedures last Cephalocaudal General Approach A. How complete should the exam be? B. Sequence C. Equipment D. Preparing and approaching the client E. Preparation of the Physical Setting F. Examiner position G. Helpful hints: 1. Be organized 2. Develop a routine to keep the exam consistent 3. Before you begin, think about what you plan to do and how you plan to complete the exam. 4. Practice the techniques to build your self confidence as well as accuracy. H. Legal Considerations I. Ethical Considerations J. Steps for PE – Refer to Validation Skills Guide K. Documentation Reading/Learning Activities Jarvis Text Ch. 28