4- News Clippings July - December 2007
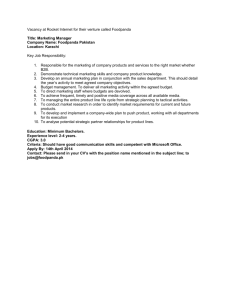
advertisement

Billions for hospitals, roads KARACHI: The City District Government Karachi (CDGK) will start 50 new major development schemes in the next fiscal year 2007-08, according to budget documents, to use up Rs 45.6 billion. The Tameer-e-Karachi Programme has been allocated Rs 5.3 billion for goth development, roads, bridges, flyovers, drains, crisis centres, solid waste, and the water supply master plan. The CDGK is going to contribute Rs 320 million to the Citizens Community Boards and Rs 100 million to the Gutter Baghicha Park project, besides initiating the construction of Jheel Park (Rs 100 million) and Kite Park (Rs 100 million). For other CDGK parks, Rs 131.62 million has been set aside. In the health sector Rs 95 million has been allotted for new wards in Abbasi Shaheed Hospital, while Rs 176 million and Rs 137.5 million have been allocated to the Karachi Medical and Dental College (KMDC) and the Karachi Institute of Heart Diseases (KIDH) respectively. Furthermore, Rs 75 million is to go towards developing a health management information system for the KIHD. Other major development projects include Karachi Elevated Expressway (Rs 1.35 billion), development in all union councils (Rs 1.6 billion), development of inter-city, town and union council roads and intersections (Rs 155 million). (Daily Times-B1, 01/07/2007) ‘Voices told me to castrate myself’ KARACHI: A 30-year-old man has landed in hospital after cutting off his own genitals with a blade which he claimed he did after he heard voices in his head telling him he was a “eunuch”. Zahoor, a resident of Saeedabad who appeared educated, told Daily Times from his hospital bed Saturday that the voices he heard in his head had been disturbing him a lot. As soon as he castrated himself, neighbours rescued him and took him to the Edhi centre at Mereweather Tower from where he was rushed to Civil Hospital. Emergency ward chief Dr Tariq Ayubi, who treated Zahoor himself, said that he had seen up to 30 such cases in his career. Ayubi said that the bleeding stopped after a while. Zahoor’s urination will not be affected. He will require constant dressings for the next few days and plastic surgery may be required. Zahoor told doctors that he abused a certain medication and that he had cut his penis off and thrown it near Mereweather Tower. He said he did not feel that much pain and would just need a slight painkiller. He has been admitted to the urology department. According to Ayubi, three broad categories of people do this: The first are the psychiatrically ill, the second are victims of family conflict and the third are those men who are apparently frustrated by their wife’s accusations. Last year, a government official in the Punjab castrated himself due to a misunderstanding with his wife, according to sources at Civil Hospital. (Daily Times-B1, 01/07/2007) Illegal kidney sales POLICE in Lahore have detected at least 10 hospitals, in addition to three others charged with illegal organ trade, engaged in kidney transactions. The task of eliminating the sale and purchase of organs is proving difficult in the absence of a proper law regulating organ donation. As long as our legislators dawdle over the passage of a draft ordinance seeking to curb the organ racket, the scourge of kidney sales will continue. Such transactions are no longer confined to the poor selling a kidney in order to escape their ever-mounting debts. Kidneys are now being extracted from unsuspecting individuals who are kidnapped for this purpose. There have also been cases where people admitted to hospital for surgery have been deprived of a kidney on the operating table. This trend is bound to continue as the absence of legislation is encouraging unethical doctors and middlemen to join forces and make a killing in the process. While the endless wait for a transplant law continues, concerned doctors, the media and civil society members can do much to promote the idea of cadaver donation among the public. Inhibitions based on religious beliefs can be overcome by pointing out that a number of Muslim countries approve of cadaver donation. Health fears, too, can be tackled by pointing out to close relatives of renal patients that it is possible to lead a full life on one kidney. Creating such awareness is important in a country where thousands of kidney patients require transplants. Such public knowledge will also deter hospitals from indulging in unethical practices. However, much depends on when — and with what changes to the existing draft — the law is enacted. The police need a legal instrument for swooping down on errant hospital administrations and individuals, and without this, the organ trade will not be brought to an end. (Dawn-7, 04/07/2007) Gastroenteritis isn’t a rich man’s disease, doctors say KARACHI: The Abbasi Shaheed Hospital has been registering an average of 15 to 20 gastroenteritis patients from poor localities a day since last week’s monsoons in the city, the hospital’s casualty coordinator Zulfiqar Ali told Daily Times Tuesday. Prior to the current outbreak, the hospital registered one to two gastroenteritis patients daily, “and then too, it was mostly the patient’s own fault. Dirty water tanks, etc, were major reasons for the disease,” Ali said. The patients coming in right now are divided into two categories. Those with chronic gastroenteritis are admitted to the hospital, while the rest are discharged by the casualty department. Children below the age of 12 are sent to the paediatrics department, Abbasi Shaheed Hospital AMS Dr Syed Javed Akhtar said. The hospital’s paediatric department received 31 patients on July 1 and 32 patients on July 2, all of who were admitted for observation. The casualty department (for patients above the age of 12 years), on the other hand, admitted four patients on July 2. The casualty department has been divided into three on-call teams to deal with the current outbreak of gastroenteritis. The medicine unit-1 is on call Mondays and Thursday, the medicine unit-2 is on call Tuesdays and Fridays, and the medicine unit-3 is on call Wednesdays and Saturdays. The teams rotate on Sundays, Dr Akhtar said. 1 Most of the patients come in from lower-income areas, the AMS said, adding that a majority of the gastroenteritis patients admitted at the hospital on July 2 came from Orangi Town, Liaquatabad, and New Karachi. “Sewerage seeps into pipes that carry drinking water, and that is a major cause for the disease,” Dr Akhtar said. “We hardly ever get any gastroenteritis patients from ‘affluent’ suburbs.” During the rainy reason, the Rota virus transmits this disease in children, he said. “A different set of virii are responsible for gastroenteritis in adults. The symptoms, however, are the same in all patients: vomiting, ‘loose motions,’ and high fever. The intensity of the fever depends on the amount of dehydration caused by the excessive defecation. The more the dehydration, the higher the fever will be,” Dr Akhtar said. “We have not had any casualties at the hospital yet, however.” Precautionary measures against gastroenteritis include using either boiled water or mineral water, the AMS said. In addition to this, fruits and vegetables should be washed with warm water, food from outside should be avoided, and feeders for babies should be sterilised. “We encourage breastfeeding, though, and the stupid habit of giving pacifiers to children should be ended. They’re unhygienic, and are major causes for stomach diseases in children,” he said. A mother suffering from gastroenteritis will not transmit the disease to her child through breastfeeding, Dr Akhtar maintained. Doctors on duty at the Liaquat National Hospital (LNH), on the other hand, maintained that they have received very few gastroenteritis patients “if at all” during the current outbreak. “Gastroenteritis is not a disease of the affluent,” they maintained. “People who generally get it cannot afford to come to LNH. They will go to government hospitals.” The head of the gastroenteritis department, Dr Pervez Ashraf, was not available for comment. No one was available to answer gastroenteritis-related questions at Jinnah Postgraduate Medical Centre (JPMC) either. Moreover, the hospital has not been reporting gastroenteritis statistics to the Sindh government’s monitoring cell, Sindh Deputy Health Secretary Dr Shakeel Malik said. (Daily Times-B1, 04/07/2007) Little stress on women’s health By Zubeida Mustafa MORE appalling than the state of the reproductive health of women in Pakistan is the ignorance shown by our policymakers and leaders of opinion about the silent suffering of women. Dr Shershah Syed, the president of the Society of Obstetricians and Gynaecologists of Pakistan, who is one of the most outspoken critics of the government’s health policy, recalled the other day his encounter with political leaders before the 2002 elections. The PMA had arranged a meeting with party representatives to brief them about women’s health. Thus the doctors hoped to enlist the cooperation of the prospective parliamentarians in health matters after the election. He was shocked when most leaders refused to believe the statistics he gave about maternal mortality. They rejected promptly the grim picture he painted as a lie. They alleged that he was exaggerating when he told them how women were suffering due to the inadequate facilities available for maternal and neonatal health. The fact is that reproductive health has been a subject that has been shoved under the carpet. Until recently it was not even discussed openly – thanks to the prudishness and hypocrisy of our society – and there was little public awareness about it. The situation changed somewhat when Benazir Bhutto in her second term as prime minister set up the National Committee on Maternal and Neonatal Health (NCMNH) in 1994 with Dr Sadiqa Jafarey as the president. It was mandated to “analyse the problem of high maternal mortality and morbidity in the country and develop and demonstrate workable approaches with the objective of lowering the high rate of maternal deaths.” This proved to be an uphill task. Dr Sadiqua Jafarey, the president of NCMNH and one of the most senior gynaecologists in the country who has devoted her entire working life to the cause of women’s health, says it is difficult to say whether the committee has made any impact on the maternal mortality rate (MMR) because there is no benchmark for it to follow. The National Institute of Population Study, Islamabad, has now conducted a survey the results of which are awaited. “Our experience has been that the MMR in all major tertiary care hospitals has remained unchanged. But that could be due to growing awareness and more women with complications being brought to hospitals which neutralises any drop that might have occurred.” Dr Jafarey feels that the NCMNH’s greatest achievement has been to create public awareness of the importance of women’s reproductive health in Pakistan. At least the issue is now being discussed and last week her committee focused its consultation on unsafe abortions, which are one of the major causes of maternal mortality after haemorrhage, sepsis, eclampsia and obstructed labour. The NCMNH has shown the courage and foresight to bring the problem of unsafe abortions into the open since nearly a tenth of maternal deaths in the country take place as a result of the complications caused by the dangerous termination of pregnancies by unskilled dais. Thanks to the NCMNH’s efforts the government announced in April 2005 the National Maternal and Child Health Policy and Strategic Framework (2005-2015) and an implementation programme last year. This document focuses on the health interventions which are essential to save the lives of expectant mothers. Recognising the fact that most babies in Pakistan are born at home without any skilled supervision, the government seeks to train midwives, birth attendants and lady health visitors who work in the community. It has also been realised that inadequate emergency obstetric and neonatal care facilities in hospitals is also responsible for a high MMR – estimated to be 500 per 100,000 live births in Pakistan by the UNFPA’s State of the World Population, 2007. The government has earmarked Rs31.5 billion to be spent in five years on this programme. Will this amount be forthcoming? The policy acknowledges that Pakistan spends too little on health – only 0.65 per cent of GDP. The internationally recommended figure is two per cent of GDP. 2 Another important factor that has been recognised but has not been addressed is the socio-cultural and economic causes of maternal mortality. The poor reproductive health of women in Pakistan reflects their abysmal status. When resources are scarce – be it in the national exchequer or in the family budget – it is taken for granted that the cuts will be exercised on the spending on women, be it their healthcare or education. Closely linked to maternal health is the performance of the population programme. It may be designed primarily to prevent births and thus reduce the population growth rate, but the population programme has a direct bearing on maternal health by regulating the family size and the spacing of children. For it is now known that a woman’s reproductive health is determined to a large extent by the number of pregnancies she has had and the gaps between them. These are in turn influenced by the availability of contraceptives. The contraceptive prevalence rate in Pakistan is dismally low (a paltry 20 per cent) and as a result there is a high unmet need. In other words, there are far too many women who are burdened with unwanted pregnancies because they have no access to birth control measures. It is a myth that people’s religious beliefs come in the way of planned parenthood. Denying them contraceptive choices and facilities is at the root of our failed population programme which should be integrated closely with the maternal healthcare strategy – as Dr Nafis Sadik, the previous executive director of the UNFPA, never tired of recommending. All these interrelated factors play on each other and multiply the impact of every factor. The need is to break the vicious cycle. This would explain why countries which show a low MMR also have a high contraceptive prevalence rate and a high literacy rate among women. Will our policymakers respond to the challenge they face? They will have to show their commitment to women’s rights by translating it into better maternal and child health as laid down by the millennium development goals. (By Zubeida Mustafa, Dawn-7, 04/07/2007) Children suffer at NICH Gastro Ward Gastro Ward at the National Institute of Child Health (NICH) is chock-full. There are around 20 beds in this ward, but there are at least two children sleeping on one; their mothers sitting, fanning themselves, head resting on their hands, silently worrying about the fate of their children. From time to time, they glance at their sleeping infants, and strike the cheeks or hair, or slip their large adult fingers in the small, delicate baby fist. Naima, a two-year-old child sleeps soundly as her mother, Yasmin, sits next to her on the bed. “It has been one week since my child has been ill,” says Yasmin. “It started with vomiting and then led to diarrhea and since then I have not seen her getting any better even though the doctors say she is improving.” Yasmin says the water they use in the house is bought at Rs 3 per canister (30 liters), which is what they use for drinking, but she is not clear where the water comes from, and whether it is safe or not. Though Naima’s case is bad, there are worse cases in the hospital. One-year-old Ammad has been constantly shifted from one hospital to another. Now he lies at NICH, sharing a bed with another baby, faint with weakness and dehydration. His mother says that he fell ill three or four days ago, but at six in the morning of July 3, she says, he started vomiting violently, and releasing nothing but water in his faeces. Ammad’s mother, Amna, says they live in E-Market, an area near Nursery (Sharea Faisal), and ever since the rains, the family has been receiving water with a strange chemical taste. “I don’t know why, but it tasted like DettolÆ,” she says making a face. “I wasn’t there at the time another child in the house gave my son tap water. We always boil the water before drinking it, but the kids didn’t know,” she says. Amna has already faced a tragedy once before when two years ago her daughter died of the same disease. Her eyes show no emotion as she speaks but it is not because she is not sad. It is because she has almost accepted the fact that she has to be prepared to maybe lose another child. She opines because she does not have contacts that makes it more difficult for her to receive any good treatment for her child. “The last time my daughter Aiman was here, my husband knew a man Imran who worked here. Although she could not be saved, Imran did the best he could for us. Now no one is very cooperative in this place. The last time the doctor came was at 9:00 am to attach a drip to my son’s arm. It’s been six hours now and not a single person has come to check up on him.” A slight note of anger tinges her voice as she talks about it. Amna explains that the attendants, who were sent to attach the drip to her son, were violently prodding him on his arms and feet and seemed absolutely incapable of doing their job. “At least they should realize they are handling a child,” she says as annoyance marks her quiet voice, “They just tried to poke him almost anywhere they could find with the needle,” she points almost hatefully to a bottle of Ringolact (Lactated Ringer’s) hanging on the drip stand, with the needle at its other end piercing Ammad’s delicate skin. It is not a coincidence that the Gastro Ward is filled with only children aging one to two years. Gastroenteritis is one of the most deadly diseases that usually occurs among infants, especially in developing countries. This mainly depends upon the feeding and living conditions of the infant and also upon whether the water consumed is contaminated or not. In Karachi, almost all areas, especially the poorer localities are the worst hit by this disease. Children are often seen splashing around in the water accumulated on the roads, most of which is stagnant water, serving as a breeding ground of mosquitoes, flies and disease-carrying pathogens. Some are even seen playing in the water running through the waterways in the city, which is clearly mixed with sewage water. With lack of education, parents do not realize that this is an invitation to death. But besides this, the unfortunate fact is that even the water running through the pipe lines, meant for consumption, is more than often contaminated, mixed with sewage water and noxious chemicals, and this water is not only used for bathing but even for drinking. There are very few people who boil water for drinking purposes. 3 Dr Ejaz Tunio, who works at the NICH, says that the gastro cases have increased immensely after the heavy rains in Karachi as they do every year. “If we got 100 cases in the Emergency OPD before the rains, we are getting around 200 more now. But there have been other rain-related problems with children, including head injuries and fractures through slipping. But for those we have taken CT scans and X-rays and have forwarded the cases to JPMC. We haven’t had mortalities in NICH at least, but it is true that some cases of injuries have been serious.” Rizwana, who lives in Sachchal Goth, says her child has been ill since Thursday last week, and although she has been boiling water, the water running through the pipe lines in her house must be so dangerous that even boiling it did not help. Belonging to a poor family that lives in Ibrahim Hyderi, she says it is a relief that NICH is not charging her for doctors’ fee or anything else, except the medicines and the injections that she has to buy from outside. But she does complain about the lack of help from any kind of organization or the government to help the poor protect their children. She says it costs at least Rs 350 per drip, and it is almost insane, she says, how she and her husband are managing to spend on the medicines, the drips, the vaccines and the pampers, besides the money needed for food and other domestic expenditures. But this is a woman who still works as a sweeper in a house. Rubina does not work, because she has seven children, and she shows her light brown eyes, patched dark like a raccoon’s from crying and staying awake all night. “I don’t know what to do in order to tell the authorities that I don’t even have enough money to save my child’s life. I lost my son two months ago to the same disease. Now my other son is losing his life, lying there in high fever and I’m just borrowing from people to pay for my medicines. How do I say to those on topÖI want to tear my heart out in front of them and tell them what I’m feeling, but no one will listen. Can’t they just stop building bridges and just give us free medicines instead?” Statistics Total cases in Karachi: 887 (99 percent gastro; others include skin diseases, etc) Admitted in hospitals: 52 (in OPDs) Rest of Sindh -Cases recorded: 923 (268 admitted in OPDs) Number of deaths: 1 (dengue fever) (Statistics are recorded every 24 hours) (By Xari Jalil, The News-14, 04/07/2007) ASH gets lithotripsy machine KARACHI, July 4: The city government has installed a lithotripsy machine worth Rs28.6 million at the Abbasi Shaheed Hospital with the help of two German engineers. The machines are also available at the Jinnah Postgraduate Medical Centre and Civil Hospital Karachi. However, ASH is the first hospital being run by the city government where such a machine has been installed. The German engineers, Davide Vinzi and Jorg Kaiser, were providing technical training to the hospital staff about the functioning of the machine. The lithotripsy machine is used to fragment and disintegrate kidney stones through high-energy shock waves. (Dawn-18, 05/07/2007) Dengue fever once again IT appears that Karachi will once again have to brace itself for a possible outbreak of dengue fever. Viral haemorrhagic fever, a more lethal form of the disease, has already claimed two lives in the last three weeks. As hospitals start taking in patients suffering from suspected dengue fever, there are fears of a repeat of the situation last year when the disease claimed 50 lives while hundreds tested positive for the virus. With the onset of the rainy season, pools of stagnant water — the ideal breeding ground for mosquitoes — are once again visible in several areas of the city, with no signs of their being drained. It is also not clear how prepared hospitals in the city are to cope with another outbreak of the disease, especially as many lack the required diagnostic and treatment facilities. Dengue fever may be self-limiting in most patients, but complications can prove fatal if hospitals are not equipped to handle cases where blood transfusion is needed. Going by last year’s poor disease management by the authorities, there is every reason to be skeptical of the government’s level of preparedness this year. However, the people, too, must be faulted for not adapting basic measures to protect themselves from mosquito bites. Apart from applying insect repellent and wearing long-sleeved clothing, people should be wary of exposed standing water in and around their homes, in potted plants and uncovered containers. Such safeguards should be promoted through the media and regular government campaigns. Not only will this prevent the spread of dengue fever, other vector-borne diseases like malaria, too, can be warded off. Precautionary measures at the government and community levels must be taken now before hospitals are flooded with dengue cases. (Dawn-7, 06/07/2007) Doctors raise alarm over dengue fever outbreak KARACHI, July 5: Fearing the spread of dengue fever – also known as viral haemorrhagic fever in technical parlance – in the city in the coming weeks, the Karachi chapter of the Pakistan Medical Association (PMA) has urged the government to intensify its efforts against the much-dreaded disease at all levels. The appeal came after cases of suspected dengue fever started arriving at different hospitals following the recent rains and at least two confirmed dengue patients died at a private hospital in the last three weeks or so. 4 A senior doctor at the Liaquat National Hospital told Dawn on Thursday that about 30 people with suspected VHF were brought to the hospital in June and nine of them were tested positive. One of the nine patients had expired at the hospital only last week, the doctor added. Health officials said that some more suspected VHF cases were reported at a few hospitals and clinics in the city last month.The PMA suggested launching of concerted efforts by all civic agencies and cantonment boards at the levels the federal, provincial and district governments without any delay to eliminate the species of the mosquito responsible for VHF, from all parts of Karachi. It also laid emphasis on the need for a massive awareness campaign to be run on a regular basis, besides effective fumigation to be carried out at regular intervals. It identified the places requiring fumigation, pointing out that puddles of stagnant water on roads and streets – especially those around hospitals, schools, offices, nurseries, parks – become a breeding ground for mosquitoes. In a statement, PMA General-Secretary Dr S.M. Qaiser Sajjad said that the association had already sounded an alert following an increase in the number of dengue cases after the rains in the city. He recalled that dengue fever had claimed 52 lives in Karachi while more than 7,000 people had reported having contracted the virus across the country last year. The PMA also urged the government to set up quality laboratories at major public sector hospitals in Karachi where poor people could avail themselves of the facility of diagnosis of various viruses. (Dawn-17, 06/07/2007) Rise in Hepatitis C THE results of an informal survey conducted by the Prime Minister’s National Programme for Prevention and control of Hepatitis and the Punjab health department are disturbing. Out of 34 districts in the province, including Lahore, 30 face a serious threat of Hepatitis C. This is not good news for the programme that was launched two years ago and, despite many promises about providing medicines and screening tests, does not have much to show for its success. An increase in Hepatitis B cases has been found in D. G. Khan, Muzaffargarh, Multan and Bahawalnagar which too calls for speedy preventive and curative measures. These are life-threatening diseases and for Hepatitis C, no real cure has been found so far. There has been some breakthrough in treatments abroad but these must be very expensive. The government must explore ways in which patients afflicted with the disease can best be treated for it is ultimately its responsibility to care for its people. It must also ensure that blood screening tests, vaccinations and treatment is provided, particularly in the rural areas where healthcare is lacking. This is not an illness that can be “treated” by quacks so the health department has to dispatch doctors to remote areas so that they can treat the poor. There are however many steps that can, and should, be taken by the health authorities. For starters, awareness on the blood-borne diseases must be raised. A lack of it is largely responsible for the large number of hepatitis B and C patients, once estimated to be ten million by the World Health Organisation. A big contributing factor is medical malpractice like the reuse of syringes, which also spreads Aids. People must know the dangers of this and their safe disposal must be strictly monitored at hospitals. The government cannot afford to be complacent on this score. (Dawn-7, 12/07/2007) PMDC earns doctors’ ire over ‘violation of rules’ KARACHI, July 11: The Pakistan Medical Association (PMA), Karachi chapter, on Wednesday strongly condemned the Pakistan Medical and Dental Council (PMDC) for ignoring its own rules and regulations. The PMDC, in its 108th session, which was dominated by private institutions, made decisions in favour of those institutions that had been found deficient by the inspection team. The reports of the inspection team for 40 institutions were not presented in the council meeting. Even then the council recommended their recognition, a PMA release said. The presentation report of the inspection team for every institution is mandatory under the PMDC rules and regulations. This is the second time that the council has taken an illegal decision in the absence of a large number of representatives from major medical institution like the College of Physicians and Surgeons of Pakistan, Jinnah Post-Graduate Medical Centre, National Institute of Cardiovascular Diseases, National Institute of Child Health, Army Medical College, PostGraduate Medical Institute Lahore, Post-Graduate Medical Institute Peshawar, Ayub Medical College, Balochistan University, Peshawar University, Punjab University, Shaikh Zayed Medical College and others. In fact they were not even invited for this meeting to avoid any objection, the statement added. The PMA Karachi appreciated the reaction shown by the PMA Punjab and said it would support its actions against the PMDC irregularities. It also believed that all the council members of the PMDC from different medical institutions of the country who were not invited nor consented for the PMDC meeting should raise there voices and protest against the illegal decision. “If these types of illegal decisions continued unabated, then very soon qualified quacks would be seen playing with the health of the citizens all over Pakistan,” it said, adding that already approximately 650,000 quacks were playing with the lives of innocent people across the country. The PMDC should be a strong autonomous body for the betterment of the medical institutions to produce good quality, trained and patient-friendly doctors, who can benefit ailing people, the release concluded. (Dawn-17, 12/07/2007) 5 Men’s role in women’s health IN a patriarchal society such as ours, little progress can be made on maternal health without the support of male family members. Appropriately then, the theme for this year’s World Population Day, observed on Wednesday, was “Men as partners in maternal health”. But such a slogan rings hollow in societies where decision-making by women is circumscribed to an extent where they are not even allowed a say in the number of children they want to bear. With an average fertility rate of 4.3 — greater in the rural areas — the number of children per woman is among the highest in the region. Early marriages, gender discrimination and poor accessibility to health and contraceptive services have complicated the issue for women whose destiny is decided by husbands, fathers, brothers and male community and religious leaders who formulate public opinion. Maternal mortality in the country is in the vicinity of 350 to 500 per 100,000 live births, indicating that reproductive health needs are largely ignored. Under such circumstances, it is essential to create an environment where women are encouraged to take decisions about the size of their families and men are urged to support them in their role as heads of families, breadwinners and managers of community resources. How this can be achieved is another story. The task will be gargantuan no doubt, given the prevailing anachronistic notions on birth control and the perception of women as inferior beings. It will call for a total change in outlook, and the government will have to do all it can to lessen gender disparities and give women a more prominent role in decision-making. Religious and community leaders, too, can play their part as moulders of public opinion, and the relevant authorities should induct them in any campaign aimed at disseminating information about reproductive health. (Dawn-7, 13/07/2007) New morgues, funding for health care units soon KARACHI, July 12: Just 13 of the 36 maternity homes run by the City District Government Karachi (CDGK) are functional, while 61 healthcare facilities remain inoperative because of financial and administrative difficulties. This was announced by the executive district officer (health) of the CDGK, Dr A.D. Sajnani, at the Sindh Government Children Hospital on Thursday. He said that the non-functional maternity homes lacked staff and equipment while the healthcare units suffered because of a ban on the appointment of doctors and paramedical staff, as well as the lack of funding. However, he added that the provincial government has allocated Rs20 million for this purpose in its new budget. Mr Sajnani said that work on five morgues had been initiated and the tenders would shortly be finalised. These will be established on the premises of the New Karachi, Abbasi Shaheed and Ibrahim Hyderi hospitals, Landhi Medical Complex and one additional location that is yet to be decided, and will provide free-of-cost cold-storage facilities to 100 bodies each. He added that there is currently no such facility in the government sector, and the Edhi Foundation’s morgue is often overloaded. Confirming the his department has stopped issuing new licenses to medical stores for the sale of drugs, Mr Sajnani said that the special secretary (public health) of the Sindh Health Department has verbally requested this. “There is tremendous pressure from applicants but we are not in a position to issue new licenses, in line with a decision taken at the Sindh Governor’s House a couple of months ago,” he said. On March 24, the governor of Sindh, Dr Ishrat-ul-Ibad, ordered a province-wide ban on new licenses for medical stores or chemists until a strategy is evolved to enforce the Federal Drug Act. Taking note of the reported sale of fake drugs, Dr Ibad had asked the relevant quarters to prepare a strategy in a week’s time. Asked about this, Dr Sajnani said that he had been told that a draft policy had been prepared by the provincial health department and had been passed on to the law department for vetting. (Dawn-19, 13/07/2007) 250 ambulances for 15m people In a city of almost 15 million, there are only 250 ambulances. That makes it almost 60,000 people to one ambulance. What is worse is that most of these are private ambulances run by social welfare organizations. For all practical purposes, the government has abdicated from its role to provide this essential service in Karachi. What makes it worse is that many of these ambulances are in poor condition without basic facilities like oxygen cylinders or first aid apparatus. This puts the lives at risk every day while the government looks the other way. A survey conducted by The News revealed that about five percent ambulances in Karachi are equipped with that necessary items which are generally considered an essential part of any ambulance in the modern world. It may be added that in Karachi, an average of 10 people are victims of road accidents daily and are brought dead to different public sector hospitals. In addition, 20 to 30 injured persons are brought to hospitals daily. Most of these are brought on ambulances run by the social welfare organisations. These organisations run their affairs with the cooperation of philanthropists. Their donations help these organizations to provide ambulance services and numerous other facilities to the public. The Edhi Welfare Trust, which has the largest ambulance network service in the country, has 100 small and 50 big ambulances in Karachi alone. In addition, the Chippa Welfare Organization has 25 ambulances operating in Karachi. The Red Crescent (Hilal-e-Ahmar) has 12 ambulances which operate throughout the Sindh Province. The ambulances of the Red Crescent organization seem to be the best equipped in the city but are not pressed into service as often as others. Most of the ambulances are four-wheel drive vehicles. In addition, the Hilal-e-Ahmar has the only functional cardiac ambulance in the city. This ambulance is equipped with ECG, BP apparatus and oxygen cylinders. 6 Properly equipped ambulances are rare in the city. The majority of Edhi and Chippa ambulances are Suzuki Hi-Roof vans which are poorly equipped. They are also rashly driven by poorly paid and overworked drivers. However, these smaller ambulances are considered as the best choice for the heavy traffic of Karachi to transport the patients to hospitals from the different parts of the city. In addition, two private organizations - Qadir Khan Mandukhail has two ambulances and Al-Azam Welfare Trust has eight. But these are used to carry patients out of Karachi in most instances. The irony is that the major public sector hospitals of the city barely have a couple of ambulances each. Most of these ambulances are in a poor state of maintenance and are rarely used for the public. Lyari General Hospital, Sindh Government Hospital New Karachi, Sindh Services Hospital, NICH, Cardio Hospital and Abbasi Shaheed have their own ambulances. But most are in poor working order. The Jinnah Post Postgraduate and Medical Centre has 12 ambulances but these are used to transfer patients to different wards within JPMC. One of JPMC ambulances is equipped with life saving equipment and two are equipped with necessary items which are needed to handle emergency. The rest of the ambulances have only stretchers. These ambulances are also used to transport patients to other laboratories outside the hospital for conducting certain tests not done at JPMC. In addition, many private hospitals also have their ambulances but these are not used for city emergencies. The city’s already scarce ambulances are also pressed into work for other purposes. During bomb hoax calls, ambulances are also called on the spot and made to stand by at great cost to the general public. While charges for the private ambulances are reasonable, there are numerous complaints on service. Edhi ambulances charge Rs50 for every 10 kilometer. Chippa Welfare Organization charges Rs100 for each 10 kilometers. Chippa has 75 ambulance drivers who work round the clock. Chairman, Chippa Welfare Organization, Muhammad Ramazan Chippa estimates that his organization needs 175 more ambulances to deal with accidents and emergency like situations in the city. Many people who availed the services of these ambulances claim with bitterness that they were literally blackmailed at the hands of ambulance drivers. They said besides the transportation charges of patients, they are also asked to pay “lifting charges” of patients as well. But there are some organizations that say they take public complaints seriously. Transport Officer of Red Crescent, Abdul Jabbar Qabulio, said that his organization has transparent system of charging. He said Rs18 per kilometer are charged for a Pajero ambulance, Rs12 for Toyota Hiace and Rs25 per kilometer for the cardio ambulance. He said any driver who receives more charges from the public could be suspended. What is sad is that both the Sindh government and the CDGK do not have a fleet of emergency ambulances for the city. There is also no system in place to coordinate ambulance activity, which is done in other cities around the world. At a time when the Punjab government has set up an emergency response system with a fleet of state of the art ambulances, the absence of such a service in Karachi leaves a gaping hole in the work of the government. Many people ask where government funds are going if there is nothing for such essential services of the city. (By Qadeer Tanoli, The News-13, 17/07/2007) Poor care at JPMC Due to uncooperative attitude of doctors at the Jinnah Postgraduate Medical Centre (JPMC), relatives of blast victims brought here had to suffer needlessly after being processed in the emergency ward. The post-emergency ward care was almost non-existant said many. Many had to look for doctors and nurses for care after being treated and shifted to other wards of the hospital. In one instance, Muhammad Naeem, hailing from Pishin, a pushcart vendor at Hub Chowki, was injured in different parts of his body owing to shrapnel. He was brought to JPMC after the blast where he was provided first aid at the emergency ward. After this, he was shifted to Ward 14. One of his legs was badly injured and he had several injuries in his chest. He was also injured in one eye. When this scribe visited the patient at the hospital, he was completely unconscious. Relatives of the victim said that after the admission of the victim at Ward 14, they attempted lot to get some doctor for him but in vain. They said that whenever the victim talked, he complained about some movement in his chest. This reporter found no doctor at the ward to attend to this seriously injured person. Only a nurse was looking after all the matters of the whole ward. The nurse told the relatives of the victim to approach the emergency ward, as the orthopedic doctors would be available there and would provide all information. The relatives of the victim along with this reporter visited the orthopedic section of emergency ward. The doctors deputed there were not able to tell them who would be responsible to look at their patient. The duty person there asked the bewildered relatives to approach the Causality Medical Officer (CMO) for “further information.” It was their bad luck that the CMO was not present at the emergency ward at that time. The relatives were also told to wait for the doctor to come and that it was “not their problem” as the patient had already been shifted out of the emergency ward. (By Qadeer Tanoli, The News-13, 20/07/2007) 7 Waterborne diseases claim 1.2m lives KARACHI, July 22: Around 1.2 million people, including 250,000 children below five years of age, die of waterborne diseases every year in the country. This was observed by doctors at a programme on waterborne diseases organized by the scientific sub-committee of the Pakistan Medical Association on Saturday. According to them, three million people suffer from waterborne diseases annually and the loss of precious lives and its consequent socio-economic cost can be avoided only if supply of clean water is ensured and simple hygiene practice is adopted by people. The doctors said that waterborne diseases like cholera, typhoid, gastroenteritis, hepatitis A and E had become a major problem in the country as water supply and distribution system had become obsolete and the quality of the so-called mineral water of 118 brands available in the market had been found below the standard. However, what perturbed one of the participating family physicians, Dr Ross Masood Ahmed, more was the lack of awareness among general public about basic hygiene. He said, “Besides the government indifference towards the issue, lack of concern about hygiene among people particularly among the lower economic strata of society was worrying,” he added. Dr Ahmed warned against use of ground water that contained certain chemicals, which could cause skin infections and hair loss. “The ground water in the old city areas is extremely dangerous while it is slightly better in Malir, Landhi and other suburbs,” he said, observing that the ground water even after being boiled is not purified completely. He said tap water should be boiled in a stainless steel container, which was the most effective method to disinfect water. “The widely-used water filters kill bacteria but not viruses,” he remarked. He also underlined the need for creating awareness about the hazards of junk food. Starting off her presentation with the world statistics about waterborne diseases, Dr Afia Zafar of Aga Khan University’s pathology department said about four billion episodes of diarrhoea resulted in an estimated two million deaths, mostly among children, every year. Waterborne bacterial infections may account for as many as half of these episodes and deaths, she added.Many deaths, she said, among infants and young children were due to dehydration, malnutrition, or other complications of waterborne bacterial infections. “Infection does not transmit only from consumption of contaminated water but also from exposure to contaminated water. Person-to-person transmission can take place if there is poor sanitation,” she said. She also advised people to avoid drinking the water and beverages with ice of unknown purity and uncooked/unpeeled vegetables or fruits. PMA General-Secretary Dr Qaiser Sajjar said the high mortality and morbidity owing to waterborne diseases reflected the apathy of civic agencies. The government must fulfill its basic duty and ensure provision of safe drinking water to everyone, he said. Journalist Zubeida Mustafa stressed the need for health education and better ties between the media and medical fraternity to address the issue. (Dawn-13, 23/07/2007) Antibiotics remain best selling drugs Imran, the owner of Naveed Medicos, says antibiotics are the most commonly sold medicines, according to his shop’s records. Other chemist shop owners and salesmen agree with this observation. It has also been observed that besides antibiotics, a close follower in the sale of medicines is sleeping pills, relaxants and anti-depressants along with salts and multi-vitamins. “Augmentin is one of the antibiotics which have the highest sales but there are others, too, including salts which are injectable, such as Decolphanex Sodium, which is an analgesic (painkiller),” he explains. According to Imran, sleeping pills are sold over the counter very easily all over the city, even though it is banned. He explains that these medicines are not only easily available, but they are also not very expensive so a regular user or an addict has easy access to them. A strip of Ativan (Lorazepam) is available for Rs10 to Rs15 depending on the dosage, while Valium (Diazepam) is available for Rs10. Similarly, Zulfiqar, another shopkeeper, says that antibiotics are available in the form of pills, capsules and suspensions. He adds that they are sold the most not counting the sale of “normal” medicines, the sales of which are an everyday affair, such Panadol, Ponstan, Paracetomol, Strepsils and cough syrups (analgesics). “These are sold the most, because they are the lightest ones,” says Zulfiqar. “Since people suffer from minor aches and pains, or sore throats and cough and cold occasionally, these medicines are usually bought and sold without prescription.” He, however, denies the increasing sale of strong and potent medication, especially drugs for psychiatric treatment, without a prescription. “I can tell from the person’s face whether he genuinely needs medicine or is an addict. I refuse to give these medicines without a prescription.” Inside Abbasi Shaheed Hospital, that falls under the City District Government Karachi (CDGK), there is a pharmacy that is near the Emergency section. Ibrahim, the man who sits at the counter during the day shift, says that antibiotics are sold the most including Valosef, Cyprphloxasim and Hycortisum. He says these are also available in injections. But this pharmacy does not keep any kind of psychiatric drug or tranquilizer. The medico legal officer (MLO) of the Hospital, Dr Mazhar, says that the long-term use of antibiotics can result in immunity and decrease the effectiveness of the drug. He says that there are two kinds of infections: viral and non viral. Since viruses cannot be seen under the microscope, there is no known cure for them. That is why viral infections either come to an end on their own, or a broad spectrum antibiotic is used to terminate the illness. A broad spectrum antibiotic, as compared to a narrow spectrum one, kills germs on a large scale, whereas the latter aims to kills only a certain type of germ. In viral infections, therefore, only the symptoms are treated, because there is no cure for the virus. 8 “The over-use of antibiotics is not correct, that is why it is inadvisable for children to take antibiotics for every minor illness. Instead, these medicines should be given only when there is no other way out. Non-viral infections for example, have to be treated with antibiotics. But the correct procedure to administer antibiotics to a patient requires careful monitoring, along with indications, and a time limit for the medication. Without this, adverse effects may be seen in the long term.” For antibiotics, a Culture and Sensitivity (CS) reading is taken. Culture means there are tests taken to determine the type of germs present, whereas Sensitivity refers to the ideal drug for killing germs. On the other hand, he says that Valium (Diazepam) is a not a drug that anyone can be addicted to, except psychologically. These drugs are basically used when a person has trouble sleeping. Ativan (Lorazepam) on the other hand is used in the treatment of anxiety disorders and for short-term (up to four months) relief of symptoms of anxiety. It belongs to a class of drugs known as benzodiazepines. Ativan is a drug which is stronger than Valium and, although it is used to put one to sleep, it has a tendency to be abused by those who know its effects. Generally, doctors discourage the use of sleeping pills, because they say that when usage is discontinued abruptly, it can lead to withdrawal symptoms in the patient. Only in cases where there is no way out or if the patient is being monitored, are these medications given. With Ativan, these symptoms are bound to occur for anyone who has not taken the medicine in either a long time or someone who is taking it for the first time. Side effects include dizziness, memory problems, sedation, transient amnesia, unsteadiness and weakness. Side effects due to a decrease in dose or abrupt withdrawal from Ativan include abdominal and muscle cramps, convulsions, depression, inability to fall asleep, sweating, tremors and vomiting. Dr Affan Tariq, who is a physician and has his own clinic says that if a patient is sensitive to or has ever had an allergic reaction to Ativan or similar drugs such as Valium, s/he should not take this medicine. It should also be avoided if the patient has an eye disease, or acute narrow-angle glaucoma. “Anxiety or tension related to everyday stress usually does not require treatment with Ativan. This is a very strong medicine and should not be taken every day. Also, if you are driving or doing something else which requires your full attention, Ativan may cause you to become drowsy or less alert. If you are severely depressed or have suffered from severe depression, consult your doctor before taking this.” Dr Shifa, who works in a government hospital, says that drugs such as these should never be combined with the use of alcohol. Other dangerous tranquilizers which are available in the market include Restoral, Noctamid, Sosegon and Buprone, along with Lexotanil which is basically a relaxant but many people buy it without a prescription. Anti-depressants are however not abused as such because they do not tend to give a ‘high’. Dr Mazhar says there are cases where people try to kill themselves with sleeping pills and an overdose could definitely lead to respiratory failure or cardiac arrest. However, there are antidotes. The best way is to wash the patient’s stomach out with water, so that the effects of the pills are minimised. Antibiotics such as Augmentin do not have major side effects apart from the fact that their effectiveness decreases when taken over an extended period of time. Less than three per cent people suffer from an allergic reaction such as skin rashes, diarrhea, stomatitis, etc, but these are very rare and should not be a regular source of danger to patients. (By Xari Jalil, The News-20, 23/07/2007) Disagreement over site delays trauma centre project KARACHI, July 23: The fate an ambitious trauma centre project, approved by the prime minister a year and a half ago, is hanging in the balance since officials of the provincial health department and the Civil Hospital Karachi (CHK) management have been unable to agree upon a site. The Rs237.5 million so far allotted to the project lie unused while sources blame the delay on poor homework on part of the health department and the CHK management, which failed to take stakeholders’ concerns into account. “Inconclusive meetings” “Meetings held over the past four months have proved inconclusive,” the source informed Dawn. “Options that were initially considered favourable, such as locating the centre outside the city near the Ojha Institute of Chest Diseases or in the administration block of the Services Hospital, were rejected in subsequent meetings. Another meeting at is due on Wednesday and will be presided over by the health minister.” Other invitees include the health secretary, the chairman of the CHK board of governors, the CHK medical superintendent (MS), the MS Services Hospital and the police surgeon. The in-charges in the HIV/AIDS lab, the blood transfusion cell and the CHK chemical examiner have also been invited, though they are not apparently concerned with the debate over the trauma centre. “Perhaps they have been called to discuss some other issues,” commented the source. Wrangling over site The meeting’s participants are to discuss the possibility of shifting the CHK neurosurgery and ophthalmology departments to make room for the trauma centre. This option was earlier floated in February this year but was “temporarily” rejected when strong opposition was voiced by Dr Junaid Ashraf, who heads the neurosurgery department, and Dr Ziauddin Ahmed Shaikh and Dr Adrees Adhi, in charge of the ophthalmology departments Units 1 and 2 respectively. The doctors argued that the CHK does not have the space to shift the wards of these departments and that such a move, even for a short period, would endanger patients’ lives. Furthermore, they pointed out, the College of Physicians and Surgeons of Pakistan would no longer recognise these departments as postgraduate training centres since a shift would force the closure of services, facilities and academic activities. 9 The brainchild of former CHK medical superintendent Prof M. Saeed Quraishy, the trauma centre was approved by the Executive Committee of the National Economic Council a year and a half ago. The three-year project hit the headlines when it was reported that Services Hospital would be razed to establish the trauma centre. After facing stiff opposition from all quarters, the officials concerned reverted to the original plan of building the centre on Chand Bibi Road, where the 7,222 square yards earmarked for the project include the current eye and neurosurgery departments of the CHK, and quarters that house city government employees and the hospital’ paramedical staff. Health department officials claim that no detailed study report was carried out for the Rs1.4 billion project which is to be completed on a 50:50 cost sharing basis between the federal and provincial governments. The former allocated Rs50 million in 2006 and Rs37.5 million this year in this regard, while the government of Sindh allocated Rs150 million this year. (By Faiza Ilyas, Dawn-18, 24/07/2007) Construction plan finalised for CHK’s trauma centre KARACHI, July 25: Sindh Health Minister Syed Sardar Ahmad on Wednesday approved the relocation of the ophthalmology and neurology departments of the Civil Hospital Karachi to make way for a 14-storey trauma centre. Addressing a meeting called to finalise the details of the proposed trauma centre, Syed Sardar Ahmad directed the CHK Board of Governors to prepare a new PC-1 at the earliest. Earlier, an 11-storey building was planned in the hospital’s vicinity for the establishment of a well-equipped trauma centre in the city. Under the plan, the first four floors would be reserved for car parking. The project, approved by the Executive Committee of the National Economic Council about 18 months back, could not be initiated because the Sindh government reportedly failed to make up its mind about the site. The cost of the project, which is likely to be completed in three years, will be shared equally by the federal and provincial governments. According to the decisions taken at the CHK meeting, now the trauma centre will be constructed on an area of 317,000 square feet while the eye and neurology departments will be shifted to the Sindh Services Hospital premises off M.A. Jinnah Road. The offices of the Sindh Blood Transfusion Authority, chemical examiner and two other health-care facilities existing at present on the premises of Services Hospital will also be shifted. The minister asked the Sindh HIV/AIDS Control Programme manager to identify possible sites at any of the provincial government health-care facilities or hire an appropriate building close to any of the major hospitals of the city for shifting the laboratory and treatment centre from the Services hospital at the earliest. The meeting was told that the Sindh Blood Transfusion Authority and all its services would be relocated to the City District Government Dispensary Mehmoodabad. Board of Governors Chairman Abu Shamim Arif, Medical Superintendent Dr Kaleem Butt and others attended the meeting. On the occasion, the minister in principle agreed on a proposal for the establishment of an operation theatre of the gynaecology department and asked the civil hospital to fulfil all formalities for an approval. (By Mukhtar Alam, Dawn-17, 26/07/2007) An effective TB control strategy IF the government wants to win the war on tuberculosis, it must do more to make people aware of the disease. According to a recent report, TB kills 9,000 people in the NWFP every year. The number is likely to be higher given that it is difficult to register patients, especially in the rural and tribal areas where there are very few healthcare centres. Nonetheless, it is a high enough figure for a disease that can be contained if diagnosed early and treatment is sought on time. Sadly, many people are still unaware of the symptoms of the disease or the free treatment centres that are there in the province. The most effective way of dealing with TB is by implementing the strategy of DOTS (directly observed treatment, short course) but results have not been very promising. Pakistan will have to rethink its strategy if it wants to meet the targets set out by the World Health Organisation which is to reduce the number of TB patients by 10 per cent by 2010. Early this year authorities said that they planned to get more health workers and even religious leaders involved in shedding social stigma often associated with TB. This must be done more forcefully so that the message is conveyed effectively. These efforts will prove futile if TB control centres are not fully equipped to deal with patients seeking treatment. Despite a TB control programme in Kohat district, 200 people are said to be afflicted by TB every year. Why is this happening? Most people cannot afford private treatment which can cost up to Rs200,000. How many in this poor country can afford that? The health ministry must look into this matter and ensure that all centres are amply stocked with preventative and curative medications. Pakistan ranks sixth on the list of TB-stricken countries and it must commit itself to eradicating the disease in a few years. (Dawn-7, 27/07/2007) Organ transplantation SIUT identifies loopholes in draft law KARACHI, July 27: Based on information available with them, senior urologists and transplant surgeons have expressed the view that the government was heading for a “bad law” in the shape of a presidential ordinance on human organ transplantation. Speaking at a press conference at the Sindh Institute of Urology and Transplantation (SIUT) on Friday, they said it was due to their long struggle and the concerns of civil society members that the federal government had revised the draft of the ordinance in question once again. 10 But a majority of the speakers maintained that there were still certain loopholes in the proposed ordinance, which would “pave the way for naked commercialisation of human organs, including kidneys, in the country.” According to reports, a revision of the draft of the Transplantation of Human Organ and Tissue Ordinance, 2007, apparently aimed at regulating the removal, storage, sale and transplantation of organs and tissue, is being considered so that it could be placed before the president for an early promulgation. The lead speaker at the briefing, president-elect of the Transplant Society of Pakistan (TSP) and Director of the SIUT, Prof Adibul Hassan Rizvi, said that it was heartening that the government had now started realising the problems of organ transplantation. ‘Transplant tourism’ Dr Rizvi said that transplant activity in the country started in the early 1980s when India was the main centre for the organ trade. After imposition of the ban on unrelated transplants in that country the whole trade shifted to Pakistan, which has now become important in the transplant tourism industry. “Commercialism is at the maximum in our country. The poorest of the poor are being exploited and their organs are made available to the rich at cheap rates,” Dr Rizvi added, saying that people in many cases had been forced by unscrupulous elements to surrender their kidneys. He said that the government should ensure complete elimination of transplants from unrelated donors, otherwise considerable health complications for both the kidney recipient and donor could arise. He suggested that the proposed set of laws should be reconsidered and amended further with the consultation of his group of consultants as well in order to make the document meet the norms and protocols of international agencies, including the WHO. According to the ordinance’s draft, part of which was made available to newsmen during the press briefing, section 3, subsection 2 states as follows: “In case of non-availability of a donor as explained under subsection (1) and there is a threat to life of an end stage renal disease failure patient, liver, heart, or lungs patients, the evaluation committee may allow donation by a non-blood relative or relative or non-relative, after satisfying itself that such donation is voluntary.” “The donor under this sub-section shall be compensated as may be prescribed.” Fears of commercialism Commenting on the clause, Dr Rizvi said that it should be omitted entirely as it would open the floodgates for commercialism. “In a life threatening situation end stage kidney failure patients can be successfully treated by dialysis. As for patients with liver, heart or lung failure, living donors cannot provide organs in most cases because of very high risks to the donor,” he added, saying that one could not donate a heart as one would die instantaneously. The SIUT director further said that the rate of “unrelated kidney transplants,” which was around 25 per cent in 1999, had increased to 85 per cent in the country, which was likely to shoot up further, that too in an organised way through the law under study. “No law is better than a bad law,” he remarked. At present, in addition to local exploitation, patients from abroad, including those from some Middle Eastern countries, the US and other developed countries manage to lure the economically-deprived donors. In fact, pools of kidney vendors have formed in different parts of the country, particularly in Punjab. The SIUT has long been advocating for “cadaver laws.” Answering a question, Dr Rizvi said that there was now a ray of hope as the Supreme Court of Pakistan had also called for the enforcement of a human organ law in the country and that was why his society, which enjoyed the support of the Pakistan Society for Nephrology and the Pakistan Association of Urological Surgeons, had also sent a draft on kidney transplant and donation laws, which was proposed originally in the 1990s. Wrong signals Stressing the need for the rectification in the reported fresh draft, another senior doctor, Anwar Naqvi, who is also the secretary-general of the TSP, said that certain sections of the proposed ordinance suggested donation of organs against payment, which was going to have a bad connotation. He gave an overview of the proposed legislation and suggested the deletion or amendment of some sections or subsections of the proposed legislation, including section 3 and its subsection 1, section 4 and its subsection 1, section 5 and subsections 1 and 2 section 8 and subsections 1, 5 and 6. He also demanded provisions in regard to post-transplant care and medicine for the organ donors. He said that rules should be framed to establish a transplant registry to document all transplantations. Dr Sajjad Husain, President PAUS, said that the proposed laws would cause exploitation by few at the cost of many. Dr Farhat Moazzam, Chairperson of the Centre for Biomedical Ethics and Culture, said that giving monetary value to any organ transplantation was unethical. Devising a law that prohibits buying and selling of organs is the only way to be fair to all stakeholders, she added, and referred to some international protocols which, according to her, compared the organ trade with human trafficking. (Dawn-17, 28/07/2007) Over 1,800 Aids cases in Sindh KARACHI, July 27: The total number of officially confirmed HIV/Aids cases in Sindh has gone up to 1,841 and the number of such cases reported from across the country stands at 3,364, according to the data compiled in March this year. This was stated by Manager for Enhanced HIV/Aids Control Programme Dr Arshad Mehmood Khan while speaking at a meeting organised by UNAIDS here on Friday. He said that 108 cases were full-blown Aids. At the national level, the number of HIV-positive cases has been put at 3,099 and that of full-blown Aids 265. 11 The meeting was told that 122 HIV-positive cases were registered with the HIV and Aids Treatment Centre in Karachi and 51 of them (35 men and 16 women) were currently on ARV medicines. The programme is aimed at maintaining HIV prevalence at less than five per cent. “We are also strongly committed to preventing a spread of HIV infection among the general population and to maintaining it below one per cent,” said Dr Khan. (Dawn-17, 28/07/2007) Removal of lacunas in human organ law urged Director Sindh Institute of Urology and Transplantation (SIUT) and President-elect of Transplant Society of Pakistan Prof Adib-ul-Hassan Rizvi has called for first removing certain lacunas in the Human Organ and Tissue Ordinance 2007 before its implementation. He was speaking at a press conference regarding the proposed legislation on organ transplantation in Pakistan on Friday. Director Centre for Biomedic and Medical Ethics Dr Farhat Moazzam, Prof Anwer Naqvi and Dr Aasim Ahmed were also present. Rizvi was of the opinion that, without the removal of these lacunas, the ordinance will not benefit the people and instead would harm the donor and promote organ trade in the country. He said that the Cadaver Law was lying with parliament for approval since 1993. “The government has started some activity for passing this bill into a legislation which is a positive change. However, they have introduced few clauses which, in our view, will encourage organ trade in the country,” he said. “Section 3, sub-section 2, of the ordinance can be cited as one of the examples in this regard,” he said. This clause reads as, “In case of non-availability of donor and there is a threat to life of an end stage kidney failure patient, liver, heart or lungs patient, the evaluation committee may allow donation by a non-blood relative or relative after satisfying itself that such donation is voluntary. Donor in this sub section shall be compensated.” Rizvi that said in a life threatening situation end stage kidney failure patients can be successfully treated by dialysis. As for patients with liver heart or lung failure, living donors cannot provide organs in most cases because of a very high risk to the donor. Similarly, one cannot donate a heart as one would die instantaneously, he added. He said that if this compensation is allowed to donors, it will encourage organ trade. He said that transplant activity was started in the early 80s in Pakistan. In those days, India was the main centre for organ trade. But India implemented a law and banned unrelated transplant and the entire trade shifted to Pakistan, he maintained. He said this has given a bad name to the country. (The News-13, 28/07/2007) 42 years later: Landhi slaughterhouse to become operational KARACHI: The City District Government Karachi (CDGK) has signed an agreement with the Multix International Corporation to bring the Landhi slaughterhouse back into function within eight months. The Karachi Municipal Corporation (KMC) had set up this slaughterhouse in 1965 on 101 acres of land in Landhi to utilize a Yugoslavian grant of Rs 16.5 million. Construction was completed with an estimated cost of Rs 35 million for the mechanical slaughtering system and 14 different sections could provide hygienic meat to the citizens. However, the slaughterhouse remained non-functional for a single day and has been closed for 42 years. The agreement was signed Saturday between the CDGK’s Enterprise and Investment Promotion Department (E&IP) EDO Hassan Naqvi and representatives of the Multix International Corporation. City Nazim Mustafa Kamal was also present on the occasion. “The agreement was signed under the public/private partnership and will provide hygienic meat to the citizens and also generate revenue of Rs 9 million yearly for the city government,” he said. He also added that the firm would start work within a week to make this abattoir functional. It will provide the facility of slaughtering animals within its premises in the first four months while in the next four months, the mechanical system of slaughtering animals would also begin functioning. Kamal had taken notice of this closure on his visit to Landhi Town June 11 and directed officials concerned to take measures for its stimulation. Consequently, The E&IP department had invited local and international firms to take control of the abattoir after which the Multix International Corporation was chosen. This private firm has to operate the abattoir for 15 years and renovate it with the estimated cost of Rs 112 million. From its first year, the firm will give a share of 40 percent of its total income to CDGK and will increase it by 80 percent in the last year of the agreement. Fumigation drive in Shah Faisal Town: Shah Faisal Town Nazim Muhammad Imran inaugurated the new phase of the insecticide spray drive on Saturday. In this phase, 50 vehicles mounted with fogging machines will spray insecticide in every nook and corner of the town, including all the shopping centers, markets, schools, colleges, worship places, and residential areas. Imran said that the drive is being launched on the directives of City Nazim Syed Mustafa Kamal to eliminate mosquitoes and other insects from residential areas, and to provide a healthy environment for the citizens. He further asked all the union council (UC) nazims, naib nazims, and councilors to supervise the spray drive in their respective areas, and make sure that all places were properly sprayed. 12 Site Town Nazim Izharuddin Ahmed opened a one-day free medical camp in UC 2 to provide quality healthcare facilities for the residents. The camp was organized by the town administration in collaboration with the Khidmat-e-Khalq. Ahmed applauded the efforts of the doctors and paramedical staff for establishing such a free medical camp, and vowed to continue this practice in the future. Jamshed Town Nazim Javed Ahmed issued orders to put all the departments on high alert to deal with the consequences of unexpected rains. He, along with other town officials, visited different UCs to review the task of cleaning storm and sewerage drains, and asked the concerned officials to complete the tasks as soon as possible. (Daily Times-B1, 29/07/2007) Maternity home fails to use OT in 20 years KARACHI, July 29: Dust covers the tiled floor, surgical operation table and the lights around it, trolleys, cupboards and medical equipment in the operation theatre (OT) of the Lyari Maternity Home. The OT is lying locked for almost two decades. A facility that couldn’t function even for a single day, the OT symbolises the countless government projects which are initiated with a huge chunk of public money and with a lot of pomp in the name of public good but abandoned without a decision on their fate. The initiative to provide an OT at the Lyari Maternity Home was unique as none of the 30 government maternity homes in the city has an OT. “It could prove to be of great benefit to poor patients who cannot afford the expensive surgery and even traveling to some other health facility for the same. Unfortunately, the OT couldn’t open for want of an obstetrician and the relevant staff,” regrets Dr Khurtoom Fatima, in-charge of the maternity home located in UC-11, Gharib Shah, Lyari. While the maternity home, one of the oldest in the city, refuses to take complicated cases that may require a surgery, it’s open for a four-hour OPD in the morning and 24-hour for normal delivery cases. There has been a significant drop in the number of patients coming to the hospital over the past three years, though mainly due to the deteriorating law and order situation in this part of the town. “Working in such conditions where you fear for your own the patients’ life, is difficult. Often we have to shut down the facility to escape being caught in cross fire. Apprehending that shooting may start anytime, the staff leaves as soon as their duty ends. I opted to work here only because it is close to my residence, says another doctor, Dr Tasneem Memon. The average number of delivery cases handled every month at the hospital in 2004 was around 150 which has dropped to 60-90 this year. The cases handled at the OPD have also come down by almost 50 per cent. Staff and performance It’s surprising to note that despite security concerns and a sharp decline in the number of patients, the maternity home has 47 staff members – 22 for the OPD and 27 for the delivery section. The double-storey facility also serves as a vaccination centre. The staff includes three doctors, one staff nurse, five midwives, four lady health visitors, three vaccinators and four ward-boys. Dr Khurtoom has been serving as an RMO (resident medical officer) for seven years. The unhygienic conditions prevailing in the labour room makes one assume that no patient has been admitted to the 10bed ward for long. This is in spite of the fact that there are seven sweepers and nine midwives among the staff. One can safely assume that the staff supposed to ensure cleanliness and hygienic conditions are not efficient or not attending to their duties properly. “The condition of this maternity home was much worse until a few weeks back. It has improved to some extent because of the renovation work, which is still under way,” Dr Tasneem said. According to a town administration official, the renovation is being carried out at a cost of Rs1.8 million. No deadline for the completion of the work has been set, he says. No tangible facilities Dr Khurtoom revealed that before the inception of the incumbent city government, food used to be served to the patients admitted here. The hospital management had also been receiving Rs1,000 under the head of maintenance on request. “Both these facilities have since been withdrawn and the management is currently without any financial support from the authorities,” she stated. She also complained of an acute shortage of medicines. “The medicines we ask for are always in short supply while those which we don’t need are supplied to us regularly,” she wondered. She pointed out that patients are charged only Rs3 for an OPD slip and Rs25 for an admission case. However, she added, people felt that the services offered at the hospital were poor because patients had to get all relevant tests done from some other institution and purchase medicines, injections, drips and other things used in delivery cases on their own. The maternity home does not offer diagnostic facilities. There is an ultrasound machine at the disposal of the management but it has been lying out of order for quite some time and dumped in the storeroom. The x-ray machine provided to the hospital few years ago is currently being used in a government hospital located in Saddar Town. (By Faiza Ilyas, Daily Dawn, 30/07/2007) 13 AUGUST Medical stores barred from selling 145 vital drugs LAHORE, July 31: The new drugs rules have barred medical stores in Punjab, whose number is in thousands, from selling 145 life-saving and other vital medicines in order to promote ‘pharmacy culture’. The Punjab governor has notified the Punjab Drugs Rules 2007 under section 44 of the Drugs Act 1976. The rules have been revised after a gap of 19 years. The Wholesale Chemists and Druggists Association’s Lahore chapter president, Nisar Chaudry, told Dawn that no stakeholder had been taken into confidence in the ‘very important’ process which he claimed was aimed at benefiting multinationals and promoting pharmacy culture in the province. Under the new rules, the period of renewal of drug sale license has been reduced from two to one year. The licensing authority shall not renew a license without considering an inspection report submitted by an inspector. The rule 20 (1) (e) says: “A licensee of a medical store shall not sell or store a drug mentioned in the schedule G”. The drugs included in this schedule are; for anti-leprosy - Rifampicin Injection, Dapsone, Clofamazine, Ethionamide and Prothionemide —, for immunological products, vaccines, sera\ant-sera - Vaccines of Anthrax, BCG, Botulisms Antitoxin, Cholera, Influenza, Measles, MMR, Rubella, Pneumococcal, Poliomyelitis, Smallpox, Typhoid, Rabiies and Homophiles Influenza Type B, and Immunoglobulins —, for products related with malignant diseases and immunosupression - Folinic Acid, Doxorubicin HCI, Mercaptopurine, Thioguanine, Vincristine, Cisplastin, Busulphan, Carmustine, Lomustine, Cyclophosphamide, Melphalan, Fluorouracil, Mitozantrone, Methottrexate, Vinblastine, Carboplatin, Bleoimycin, Chlorambucil, Dacarbazine, Amasascrine, Azathioprine and Cyclosporin - for anesthesia and inhalation anesthetics Propofol, Enfluran, Isofluran, Halotha ne, Bupivacain, Thiopentone, Benzodiazepine, Mitazolam, Naloxone Hcl, Vancuronium, Pancuronium, Tubocuraine, Suxamethonium and Neostigmine - for antibiotics - Spectinomycin, Teicoplanon, Sodium Fusidate, Vancomycin, Colistin and Impenem - for inotropics - Primacor, Enoximone and Milrinone - for injection prostaglandins - Dinoprotone, Gemeprost AND Carboprost - for alpha blocker - Prazosin Hcl, Daxazosing, Indramine and Alfuzosin - for biotechnological products - Interferon and Erythropoetin - for narcotics, psychotropic and tri cyclic antdepressant - Morphine, Buprenorphine, Nalbuphine, Fantanil, Pethidine, Lorazepam, Temazepam, Chlorpromazine, Melprobamate, Chlordiazepoxide, Alprozolam, Clonazepam, Flurazepam, Loprazolam, Oxazepam, Amoxapine, Iprine Dole Codine, Pentazocine, Lithium, Dextropropoxyphene, Clomipramine, Mianserin, Maprotiline, Dothiepin, Doxepin, Nortriptyline, Trimiprammine, Tranycypromine, Flupenthixol, Tryptophan, Imipramine and Amipriptyline - for anti-viral Acyclovir, Amantadine Hcl, Famciclovir, Inosine Pranolsex, Zidovudine, Ganciclovir, Idoxuridine, Riavirin, Vidarabrin, Trifluridine and Methisozone - for thrombolytic enzymes - Alteplase, Streptokinase, Anislreplase and Urokinase - for dialysis - Peritoneal, Haemodialysis, Hyper tonic solution, Lysine solution and Isotonic solution - for creams and aerosols steroidal preparations — Methylprednislone, Dexamethasone, Hydrocortisone, Prednisolone, Tramcionolone and Beclomethasone for hormones - Vasopressin, Desmopressin, Stanozolol, Nandrolone, Mesterlolone, Finasteride, Finasteriode, Somatropin, Testosterone and Progestrogens. “Non-availability of such a large of number of drugs from about 50,000 medical stores in Punjab means creating a lot of trouble for patients as there are only few hundred pharmacies in the province, Nisar Chaudhry said. The role of wholesalers and distributors had also not been explained in the rules as well. Besides this, the rules say the licensing authority shall not issue a license unless the premises of a pharmacy or medical store is clean and hygienic, has adequate facility for storage of drugs and for their protection from direct sunlight and dust. Under the rules, an aggrieved party may file an appeal to the provincial appellate authority within 30 days of the date of the order issued by the licensing authority. A nine-member provincial quality control board, headed by the provincial health secretary, has been constituted. The board may constitute a committee in a district to be known as the district quality control board. Both boards may meet at least once a month to review the situation of drugs’ quality control. Before referring a case to a drug court, the provincial or district board shall ascertain the name of the director, partner, and employee of the company who is prima facie responsible for the commission of the offence under the Act or rules and may allow an inspector to institute prosecution against such person. According to the rules, no person shall be appointed as an inspector unless he holds a degree in pharmacy from a university or an institution recognised by the Pharmacy Council of Pakistan and has at least one-year experience in manufacture, sale, testing and analysis of drugs. (By Zulqernain Tahir, Dawn-12, 01/08/2007) Billions for hospitals, roads KARACHI: The City District Government Karachi (CDGK) will start 50 new major development schemes in the next fiscal year 2007-08, according to budget documents, to use up Rs 45.6 billion. The Tameer-e-Karachi Programme has been allocated Rs 5.3 billion for goth development, roads, bridges, flyovers, drains, crisis centres, solid waste, and the water supply master plan. The CDGK is going to contribute Rs 320 million to the Citizens Community Boards and Rs 100 million to the Gutter Baghicha Park project, besides initiating the construction of Jheel Park (Rs 100 million) and Kite Park (Rs 100 million). For other CDGK parks, Rs 131.62 million has been set aside. In the health sector Rs 95 million has been allotted for new wards in Abbasi Shaheed Hospital, while Rs 176 million and Rs 137.5 million have been allocated to the Karachi Medical and Dental College (KMDC) and the Karachi Institute of Heart 14 Diseases (KIDH) respectively. Furthermore, Rs 75 million is to go towards developing a health management information system for the KIHD. Other major development projects include Karachi Elevated Expressway (Rs 1.35 billion), development in all union councils (Rs 1.6 billion), development of inter-city, town and union council roads and intersections (Rs 155 million). (Daily Times-B1, 01/07/2007) Cabinet approves organs law ISLAMABAD, Aug 1: The federal cabinet on Wednesday approved the Transplantation of Human Organs and Tissues Ordinance 2007 after taking out the controversial clause regarding compensation for the donors. The cabinet also appointed an inter-ministerial committee comprising Health Minister Nasir Khan, Law Minister Wasi Zafar, Advisor to Prime Minister Sharifuddin Pirzada, Minister for Ports and Shipping and Housing Babar Ghouri and Federal Health Secretary Khushnood Lashari to fine tune the text of the draft law. The committee has been given eight days to finalise the draft ordinance. Prime Minister Shaukat Aziz would then advise President Musharraf to promulgate the ordinance when the ongoing session of the National Assembly is over. The National Assembly is likely to remain in session till August 17. The ordinance was approved after intense debate in the cabinet that lasted for almost two hours with some of the ministers and key government functionaries advocating non-related donations and compensation for the donors. The draft that had been presented before the cabinet included certain controversial clauses including the provision for compensated donations in case of non-related donors, which was being implied as an attempt to give legal cover to trade of kidneys. However, in view of the public pressure it was decided that this controversial clause should be removed thus closing possible avenues for commercialism in transplant affairs. (By Baqir Sajjad Syed, Dawn-1, 02/08/2007) City govt to establish ambulance network KARACHI, Aug 1: The city government has decided to establish a state-of-the-art ambulance network which will be linked with all major hospitals and the fire brigade department. This was stated by City Nazim Mustafa Kamal while talking to newsmen on the occasion of handing over 10 newlyprocured ambulances to the health department at the Civic Centre on Wednesday. The ambulances were given to hospitals and maternity homes in Keamari, Bin Qasim, Landhi, Soldier Bazaar, Karachi Institute of Heart Diseases, Leprosy Hospital, Manghopir, KDA Employees Clinic and others. The nazim said that the network of ambulances would be established as part of the city government’s efforts to provide immediate rescue and health facilities to trauma patients. In the next phase, he said, 10 new ambulances having mini-operation theatre would be procured which would also serve as mini-mobile hospitals. The ambulances, he said, would be equipped with a wireless system connected with hospitals. He said the city government had planned to introduce a new toll-free number for the ambulance service and three centres would be established with medical staff at their disposal. Mr Kamal said medical experts were consulted before giving final approval to the project. According to them, the initial 20 to 25 minutes were very crucial for a trauma patient and his life can be saved by providing first aid immediately. Dr Vaqar Kazmi, Dr Nasir Javed, EDO Health and other officials were also present. Meanwhile, City Nazim Syed Mustafa Kamal along with Gulshan-i-Iqbal Town Nazim Muhammad Wasay Jalil inaugurated a newly purchased loader for the sanitation department, PPI adds. The loader has been purchased to enhance performance of the sanitation department. It will help the shifting of debris to landfill sites. Town Naib Nazim Shoaib Akhtar, TMO Shafiqur Rehman, DTO Solid Waste Nafees Khan, DTO M&R Nisar Soomro were also present. Night sweeping All major roads, vegetable, meat markets and shopping centres in Shah Faisal Town will be cleaned during night sweeping that will start from Aug 15. This was stated by Town Nazim Muhammad Imran while inspecting cleanliness work in union councils 3 and 4. He said 100 sanitary workers would be recruited on a contract basis to enhance the performance of the solid waste department. The town nazim also distributed more than 50 hand trolleys and 100 brooms among the sanitary staff and directed them to discharge their duties with responsibility. TO Infrastructure Wakeel Ahmed, DTO Solid Waste Aslam Pervez, UC-3 Nazim Abdul Jalil, Naib Nazim Muhammad Ainul Haq, UC-4 Nazim Muhammad Shamim Khan and Naib Nazim Karimuddin were also present. (Dawn-18, 02/08/2007) Govt hospitals turn to private security firms KARACHI: Government hospitals in the city, including those run by the City District Government Karachi (CDGK), the provincial government, and the federal government, are guarded by personnel from private security agencies rather than members of the State’s law-enforcement agencies, Daily Times has learnt. 15 The Abbasi Shaheed Hospital (ASH), which falls under the jurisdiction of the CDGK, has invited tenders from private security companies. ASH Deputy Medical Superintendent (DMS) Dr Nadeem Rajput said that the personnel would be used for the entire hospital. “This is a routine procedure and we have had a contract with private security companies for the past year-and-a-half,” he added. Other sources within the hospital, however, had a different story to tell. “Personnel from private security companies will be used solely for the new trauma centre,” they said. “The maintenance of law and order generally becomes a problem at this unit.” Dr Rajput maintained, however, that the private security personnel hired in the past had been used for the entire hospital. He was not aware of how many people would be hired this time around. “We’ve just advertised the tenders. Companies will come in with their presentations now and will advise us on the brawn required, armed or unarmed. The final decision will be taken after this process,” he said. “Currently, we employ 93 armed and unarmed people from these private security companies.” Dr Rajput also said there was no special reason for requesting private protection instead of using personnel from the CDGK’s security wing. “I think every organisation has the right to decide the kind of protection suits it best. We opted for private security companies more than a year ago to guard the entire hospital,” he said. CDGK EDO Health Dr AD Sajnani told Daily Times that this wasn’t something new and all government hospitals, including the Civil Hospital Karachi (CHK) and the Jinnah Postgraduate Medical Centre (JPMC), used private security companies. “The ASH has been using them for the past two years. Tenders have been advertised recently because it is time to renew the old contracts,” he said. When asked why there was a need for private security companies in the presence of State-run security agencies, the EDO said, “People tend to get really rowdy, and the need for increased security comes in hence the decision to opt for private security companies.” He did not say why the city’s police force, Rangers etc were not sufficient for these purposes. Sources in the Sindh Home Department told Daily Times that the number of available police personnel is insufficient. “If we start using them to guard places, we won’t have any left to manage the everyday law and order situation here,” they said. “A number of personnel were pulled back from ‘guard duties’ a while ago. This is probably why the need for private security agencies arose.” No efforts have been made to hire more police officers at the moment, however, and the allocations in the Sindh budget 2007-08 for police forces in nine out of 18 towns of Karachi were considerably reduced as compared to last year’s budget. While the Capital City Police Office did see a substantial increase in budget allocations, most of the amount was earmarked for “operating expenses,” such as the purchase of transport for the CCPO’s staff and office, as well as the purchase of fixtures and fittings, and for miscellaneous loans and grants. (By Urooj Zia, Daily Times-B1, 03/08/2007) Doctors hail proposed organ transplant ordinance For over 14 years now, doctors in Pakistan have been struggling against the proliferating organ trade in the country. This week, however, a light at the end of the tunnel appeared when the federal cabinet approved the Transplantation of Human Organs and Tissues Ordinance 2007, giving rise to the hope that the increasing sale of kidneys will be curbed, which has given a bad name to the country. The Sindh Institute of Urology Transplantation (SIUT), initiator of the legal move on the issue, welcomed the proposed ordinance after the reported removal of a controversial clause pertaining to compensation for the donors. This was allegedly inserted in the original draft of the SIUT in 1993 by the supposed kidney mafia believed to be earning one billion rupees per year. The Pakistan Medical Association (PMA), while appreciating the proposed ordinance, expressed its reservations over the exclusion of the representative of stakeholders (doctors’ organisations) in the committee, who could have ‘fine tuned’ the ordinance within eight days. Also, the PMA disapproved of the government’s increasing tendency to promulgate the ordinance, instead of bringing the legislation after being debated upon by the parliament. “We hail the ordinance because our core issue relating to compensation for donors has been addressed,” Dr Bakhsh Ali of the SIUT told The News. He said another issue regarding cadaver donor law, has also been reportedly addressed. He said this is more important in the sense that a patient suffering from renal failure can survive on dialysis if there is no donor but in case of the heart and lung, a cadaver donor is the only hope for treatment. Dr Ali said it would have been advisable if representatives of different doctors’ organisations, which had launched a sustained struggle since 1993, had been included in the committee. However, he pointed out that Dr Adibul Hasan Rizvi, the head of SIUT, who was in Islamabad was a part of the deliberations on the proposed ordinance. Dr Ali hoped the ordinance will go a long way to help control kidney trade, as Pakistan has turned in an ‘organ bazaar’ where patients from the Middle East, Europe, etc., buy kidneys, especially the poverty-stricken regions of Punjab. According to him, there are powerful elements involved in this trade who had allegedly included a controversial clause in SIUT’s original draft. The PMA secretary general, Dr Kaiser Sajjad, hailed the ordinance against kidney sale, which has been rampant in the country since the last 20 years. Around 2,000 kidney transplants take place in Pakistan each year. Dr Sajjad claimed that hospitals have been set up, especially in Lahore and Rawalpindi, where poor people are brought to sell their kidneys in exchange for a meagre sum of money. He said the mafia involved in this trade tends to rake two million rupees from rich and wealthy patients but they give only Rs60,000 to 1,50,000 to the donors, who are discharged without proper treatment. He said kidney donations must be restricted to family members only and no room be left for monetary incentives. 16 Dr Sajjad wondered why the government is reluctant to bring the legislation forward in the Parliament instead of promulgating the ordinance, which would lapse after 90 days. He said that the doctors’ organisations should be given proper representation in the committee. Pakistan has been in the news, as the country — in words of the reinstated chief justice Iftikhar Mohammed Chaudhry — has become a “safe haven for the traders of human organs.” The judiciary’s recent suo moto notice apparently prompted the government to take the perceived concerted efforts for enforcing a law against kidney sale. It may be mentioned here that the United Nations passed a resolution against the sale of human organs for monetary consideration in 2003 while the World Health Organisation has termed monetary incentives in exchange for organs as exploitation. (The News-19, 04/08/2007) City Council endorses allotment of land to SIUT KARACHI, Aug 4: The City Council on Saturday endorsed the city government’s decision to allot a 989-square-yard plot to the Sindh Institute of Urology and Transplantation for establishing a hospital. The city government has already made it clear that it will retain the ownership of the plot, carved out from a piece of land measuring 17,372 square yards on Chand Bibi Road, maintaining that the decision to accommodate an SIUT hospital in the vicinity had been taken in the greater interest of the public. It has further stated that the possession and use of the allotted plot will be limited to the sole purpose of constructing and operating the hospital. A resolution endorsing the CDGK’s decision was moved jointly by the treasury and opposition benches who acknowledged the internationally recognised services to the nation, especially the ailing humanity and the medical profession, being rendered by SIUT chief Dr Adibul Hassan Rizvi. Convenor of the house Nasreen Jalil put the resolution to members for a debate, which was initiated by Asif Siddiqi, leader of the Haq Parast Group. He hailed the city government’s decision, and noted that it would help the SIUT to extend the network of its services. He assured the house that there would be not injustice with the occupants of some residential quarters who would have to be evicted from the project site. Another treasury member, Masood Mehmood, maintained that the debate on the resolution should not prolong as the allotment of land to the SIUT was not a political issue but a public welfare move. Opposition leaders Rafique Ahmed of the Al-Khidmat Group agreed to his suggestion following which the house unanimously adopted the resolution. Tom Tancredo’s remarks Earlier, when the house resumed the session, Mr Rafique Ahmed sought the chair’s permission to move a resolution condemning the remarks by the US Republican candidate Tom Tancredo, who had suggested using threat to attack the holiest Muslim sites to deter a terrorist attack against the US. The treasury side maintained that though the remarks were condemnable in the strongest possible words, the City Council was not an appropriate forum to take up the issue. The chair quoted the relevant SLGO rules, and ruled that the house could not discuss such issues. (By Latif Baloch, Dawn-17, 05/08/2007) 20 per cent pregnancies end in miscarriages KARACHI, Aug 4: Twenty per cent pregnancies end prematurely because of chromosomal abnormalities in the foetus while introduction of laparoscopic surgery to end ectopic pregnancy marks a major leap ahead from the extended recovery period required after common surgery. Addressing a public health awareness programme at the Aga Khan University Hospital on Saturday, doctors discussed the issues surrounding early loss of pregnancy and highlighted the recent advancements in the field of obstetrics. “Miscarriage is pregnancy loss prior to 24 weeks gestation. It occurs in 10 to 20 per cent of all pregnancies and may be associated with significant psychological sequel,” said Dr Rozina Sikandar, consultant obstetrician and gynaecologist at Aga Khan University Hospital, in her presentation on Early Pregnancy Loss and Recurrent Miscarriage.Foetal chromosomal abnormality (error in development of baby in utero) is the commonest cause of early miscarriage (i.e. pregnancy loss before 12 weeks) while late pregnancy loss (between 12 and 24 weeks) occurs less frequently and constitutes less than three per cent of all pregnancy outcomes. She said all couples with a history of recurrent miscarriage should be evaluated for a possible cause although a significant proportion of cases remain unexplained despite detailed investigation. While this is frustrating both for the patient and the doctor, it is reassuring that the prognosis in these women for a successful future pregnancy with supportive care is 65 to 75 per cent. Dr Nadeem Faiyaz Zuberi discussed the ectopic pregnancy and its laparoscopic treatment. In ectopic pregnancy, he said, the baby grew outside the uterus, most commonly in the uterine tube. Pre-existing uterine tubes damage was a significant risk factor for ectopic pregnancy and about 50 per cent of ectopic pregnancies were associated with some degree of tubal disease due to pelvic infection, endometriosis, appendicitis, previous pelvic surgery, reversal of a tubal ligation or fertility treatment, he said. 17 At times there is no obvious explanation for why an ectopic pregnancy has occurred. However, once a woman has had an ectopic pregnancy, she has a higher likelihood of having another one and should be monitored carefully if another pregnancy is attempted or suspected. According to him, surgical treatment of ectopic pregnancy historically requires a laparotomy using a skin incision. However, with advancements in laparoscopic surgery, the foetus can now be removed using two to three small button-hole incisions. Following operative laparoscopy, patients are generally able to go home within 24-hours of surgery and return to normal in three to seven days at home. (Dawn-18, 05/08/2007) Doctors stage sit-in on Sharea Faisal The dismissed doctors of Jinnah Postgraduate Medical Centre (JPMC), on Saturday staged a sit-in on Sharea Faisal, pleading the federal govt to review its decision regarding termination of their services. The doctors, numbering around 53 including 15 lady medical officers whose services were terminated on Monday, took out a rally from the JPMC. Chanting slogans and carrying banners, inscribed with slogans like ‘save the future of doctors’ they protested on the main thoroughfare for half an hour, causing gridlock on the city’s one of the busiest arteries. Contingents of police rushed to the troubled site and cops warned the medical officers to call off their protest. The doctors, realising the gravity of the situation, proceeded towards the Karachi Press Club (KPC) to register their protest. Talking to The News, Dr Naeem, Dr Shazia, Dr Ajeet and other doctors of the newly created Doctors’ Action Committee said the JPMC administration had ‘verbally’ promised them that they would be accommodated. Referring the reported telephonic contact between the Executive Director JPMC, Dr Rashid Jooma and the federal health secretary, the protesting doctors said that no written letter has been issued so far. (The News-13, 05/08/2007) Corruption and health Transparency International's World Corruption Report of 2007 with its focus on corruption in the judicial system is especially relevant to Pakistan with respect to the spotlight on the judiciary. However, its findings have also opened a debate in several sectors in the country owing to its inclusion of Pakistan amongst the 37 countries studied and the sectoral comparative rankings. The interest in the area has also been further exacerbated by reports of two recently conducted surveys in Pakistan. According to the first, a perception survey of civil servants conducted by PIDE, 93 per cent of the respondents think that performance of the civil services has deteriorated over the years. According to the second survey, conducted by Gallup, 43 per cent of the urbanites believe corruption is prevalent in the country. Discussions relating to the health sector are never complete without references to malpractices which fall within the purview of fiscal and ethical corruption; even if half of this anecdotal evidence is grounded in reality, the fiscal costs incurred to the state and the cost of accessing care -- which remain undocumented -- appear to be significant. In recent years public sector allocations for financing health have significantly increased; however, corruption stands as a key impediment to the impact of well-intentioned spending on health. Without addressing this issue, the commitment to meet goals articulated in the Millennium Declaration as well as others embodied within indigenous policy instruments such as the MTDF simply cannot be met. It is for this reason that the government should accord high priority to the issue because of the potential it has to compromise public investments in a highly constrained environment. What should therefore be done in this regard? As a starting point, there is a need to understand and prioritise corruption risks by corruption mapping and analysing incentives and disincentives. This must be done at several domains. The anecdotal reports of corruption in the pharmaceutical sector must receive careful and objective analysis. Corruption in this domain has a direct bearing on the performance of the health system. This practice can involve both the regulators and the private sector and may involve any step along the drug supply chain, starting from registration, licensing and accreditation to the setting of prices, marketing of drugs and sale and procurements. Corruption in this sector has its roots in the commercial interests of the non-bonafide pharmaceutical companies, who find compliance with regulations costly and try to bypass procedures to get their product registered, speed up the approval process, get favourable prices or to have their drugs included on the essential drug list in order to increase their market share. The contracting process for the purchase of drugs offers a lucrative source of returns for corrupt officials and suppliers through kickbacks, over-invoicing, and outright graft. There is anecdotal evidence for the same in Pakistan from several public hospitals; however this needs to be assessed carefully and its magnitude quantified. In the procurement process, common corrupt practices include collusion among bidders, kickbacks from suppliers and contractors to reduce competition and to influence the selection process, and bribes to public officials monitoring the winning contractor's performance. Corrupt procurement officers can also purchase sub-standard drugs in place of quality medicines and pocket the difference in price. It is also reported that varying quantities of drugs and medical supplies are stolen/pilfered from central stores of hospitals and individual facilities and are diverted for resale. This result -- it could be speculated -- is due to institutionalised corruption, which involves a variety of practices such as record falsification, dispensing drugs to 'ghost patients', graft and padding of bills, clever book keeping, overpayment for supplies, over-invoicing or simply pocketing the patient's payment. Other forms of abuse, fraud and mismanagement can occur due to insufficient management and monitoring capacity; e.g. supplies do not meet expected standards, or they are only partially delivered or not delivered at all, or selling low quality, expired, counterfeit and harmful drugs at cheaper prices. 18 The process of licensing pharmacies or chemists' shops can also be corrupted. However, most important in the pharmaceuticals domain is the issue of aggressive drug marketing strategies, which can lead to the unethical promotion of medicines or to conflict of interest that influence physician's judgments. Instances where physicians actually have financial/material incentives to prescribe certain drugs are also well described anecdotally. In Pakistan, more than 450 pharmaceutical companies manufacture almost 45,000 registered drugs. Such competition coupled with hospitality-based incentive-intense marketing can lead to unethical marketing practices, which have the potential to affect medical practice and treatment decisions of physicians. The ultimate outcome of all these practices are either higher price for purchased medicine and/or compromised quality. Patients are the directly affectees in this process as they are forced to supply their own medications. The second area which should be carefully analysed is staff absenteeism and dual job holding; this undermines service delivery and leads to closed/under utilised public health facilities; this in turn, conflicts with the equity and health objectives of publicly financed health care. In a minority of cases, absenteeism is unavoidable; for example, rural health workers often need to travel to larger towns to receive their payments, fetch supplies or drugs and are sometimes delayed by poor infrastructure. However, in most cases absences are frequently motivated by responsibilities at a second job. Other than absenteeism there are also other staffing issues that can undermine productivity at public health facilities through shaving off hours, late arrival and early departure, and frequent and long breaks. Absenteeism is symptomatic of ineffective management and it also compromises the quality of health care across the board by relying on ill-trained providers or quacks for care. The third area of assessment falls under the current restructuring arrangements at the primary health care level, where the administration of Basic Health Units (BHUs) and Rural Health Centers (RHCs) is being handed over to the private sector. Though a step in the right direction, an important caveat here is that this may open a potential avenue for lack of transparency in contracting arrangements, which flags a clear imperative for ensuring procedural clarity and transparency. Corruption can also be ingrained at a regulatory level in the healthcare domain. Several regulatory institutions can form settings for such practices. Pakistan does not have an institutional mechanism for quality control, hospital accreditation or provider credentialing except for the Pakistan Medical and Dental Council, which serves the role of provider registration only. Pakistan is, however currently underway to establishing the National Drug Regulatory Authority. Experience from many developing countries suggest that if such regulatory institutions are created without awarding the right incentives to regulators and institutionalising the right checks and balances, then paradoxically they compromise the health system rather than strengthen it. Furthermore, corruption also needs to be quantified at the governance level particularly with reference to the losses incurred through the anecdotally reported kick-backs, pilferage, and embezzlement -- a manifestation of a poor fiscal control over public funds. Other forms of intellectual and ethical corruption such as deliberate lack of over-sight, unfair hiring practices, in attention to staff accountability for misconduct and preferential treatment with connected individuals and basing priorities on political expediency and benefaction rather than evidence have also been reported. The magnitude and determinants of these needs to be quantified. The assessment should guide strengthening of anti-corruption measures which leads to the practical level. Corruption necessitates a mutually re-enforcing anti-corruption agenda; this is where the National Accountability Bureau can play strategic role - both in the investigative and preventive domains in light of section 33-B of the NA Ordinance of 1999. A number of next steps should logically follow. First is to ensure that laws are in place to deter corruption. A number of legal instruments in Pakistan make corruption a punishable offence. However, new statutes representing a stronger commitment to eradicating corruption are also needed. It is true that laws have limitations owing to the limited capacity of enforcing agencies and true that anti-corruption work cannot be complete without enhancing institutional capacity. Notwithstanding, statues must still be the first step; ensuring that they are not open to interpretation and are not exploitable. This, in the long run, will aid their implementation. In addition, other laws such as freedom of information laws also need to be reformed. Secondly, there is a need to review procurement and financial management policies in the health sector. A number of new regulatory institutions have been created to streamline public procurement such as PIPRA and a range of reforms have been institutionalised to streamline financial management and accounting systems. Their guidance to the health sector should be reviewed and leveraged. Policies should also be able to mitigate collusion in the procurement process. Thirdly, the use of technology is being increasingly promoted in the health sector. Particularly its effective use in the area of establishing systems can enable and promote greater transparency. For example, electronic national health accounts promote greater transparency in health systems; electronic public expenditure tracking procedures and electronic equipment and supply inventories can track leakages from the system. Also, a nation-wide database for matching staff and wage payments can maintain up-to-date personal records and, therefore, can assist in eliminating abuses such as paying 'ghost workers'. In addition, drug procurement reforms centered on electronic bidding can promote greater transparency in the process of drug registration and pricing. In the fourth place, local regulations will have to be strengthened in line with the international code of marketing practises and should be strictly enforced as minimum requirements for the pharmaceutical industry and the medical community to comply with. Other measures should be promoted to check mushrooming of spurious drugs which was significantly in the limelight a year ago with the suo moto action by the Chief Justice. Strict penalties should be implemented for violations of the laws that check spurious drugs to gain access to the market. Moreover, fake licenses to sell, duplicate documents, absence of warranty of purchase of all products, gaps in the sale purchase record of all products, inadequate storage practices at outlets, and the absence of unqualified personnel at outlets should also be checked. In the fifth place, at a service delivery level, corruption can be countered by mainstreaming alternative modes of service delivery and financing. In autonomous hospitals this can be done by strengthening governance and bringing efficient management with administrative and fiscal controls. Service delivery reforms at the basic health care level can increase accountability through management devolution/contracting out and by giving greater fiscal and administrative autonomy. In such arrangements institutional incentives- such as the ability to hire and fire the staff and authority to reward performance and discipline, transfer and terminate employees who engage in abuses and the ability to audit -can also help counter 19 corruption. With reference to quackery, coercive regulation is unlikely to be effective. Therefore, decisions to curb these practices have to be pragmatic and feasible such as by developing approaches to mainstream their role into the delivery of care. This can be done by accrediting them to provide some services. However, an anti-corruption agenda at a health systems level is complex and warrants health system reconfiguration. This goes beyond incentives and has to do with health systems' reforms in a broader sense. A comprehensive anti-corruption agenda in the health sector also has to scope much further than what has been stated. It has to take into account other overarching issues such as remuneration of public servants through civil and public service reforms - which is the mandate of the national Commission on Government Reform. In addition there is also the need to create operational linkages of the National Accountability Bureau with the health sector. In a nutshell, healthcare provision depends on a system which efficiently combines financial and human resources and supplies to deliver services. However, both poor governance and corruption in the health system are manifestations of a broader systems phenomenon in a country. Addressing these issues requires mandates and prerogatives both within and without the health sector. That is why ideally, an anti-corruption drive in health must ride a much larger wave. (By Sania Nishtar, The News-Policy II, 05/08/2007) Hepatitis in expecting mothers on the rise KARACHI, Aug 5: “Hepatitis has become increasingly common in villages and we have been receiving more and more cases of Hepatitis B and C,” said Medical Superintendent of a maternity home, located in Old Thana, Gadap Town, Dr Noor Qureshi, who said many cases were referred to the hospitals where better treatment facilities were available. He said there were 11 hepatitis patients registered with the maternity home for antenatal check-ups. “Sadly, they cannot avail delivery service here because these cases need special handling which we cannot provide,” he stated when asked about the major difficulty being faced by women at the facility where a large number of maternity cases coming from the villages of Gadap Town and its outskirts, as well as Sindh interior, are handled. More than 30 women visit the facility every day and 60-65 deliveries are performed every month. Dr Qureshi, a recent appointee, said patients with a history of hepatitis were referred to government tertiary care hospitals in the city. “In such cases, not only the life of mother and baby is at risk, but the medical staff handling them may also be exposed to the highly infectious disease,” he argued to justify the practice. He was of the view that if there was a registered hepatitis patient, it was better to inform her about the risks involved prior to her delivery time and refer the case to a hospital having better and appropriate treatment facilities. Dr Qureshi noted with regret that there was no government-run health care unit in Gadap Town where patients could avail diagnostic facility for hepatitis. “People, men or women, have to be referred to some other government hospital for the purpose as villagers cannot afford expensive treatment at private hospitals,” he said, suggesting that the best way to check the disease was effective prevention. Emergency treatment Dr Zainab Shah, in-charge of the maternity home, in reply to a question about unregistered hepatitis patients turning up for delivery in an emergency, said emergency treatment was not refused to anybody. As a routine, utmost care in handling all cases was taken and all equipment sterilised, she said, adding that extra caution was being ensured these days before admitting a case in view of the growing number of hepatitis and other high risk cases. In this context, she also pointed out that the hospital’s ambulance service had been dysfunctional for more than seven months. Dr Shah said that high risk cases included those of acute anaemia and diabetes. “Such cases are also referred to some other government hospitals,” she said, observing that acute anaemia happened to be more common among expecting mothers. Besides poverty and lack of awareness, she noted, multiple pregnancies is a major cause. “It’s ordinary to find women having undergone eight to 10 pregnancies but left with only three to six surviving babies,” she claimed. According to Dr Shah, anaemia exposes women to a greater risk of having postpartum hemorrhage. We do provide women with contraceptives and motivate them to use the same but we don’t have the provision for tubal ligation. She, however, observes that over the years, women’s response to family planning services was better. As many as 30 women received treatment for tubal ligation at a camp organised by an NGO last year, Not ideal for professionals The maternity home has undergone a complete renovation a few months back. With rooms whitewashed and floors tiled, it comprises a labour room and a six-bed ward offering 24-hour service for normal delivery. However, the facility is without a doctor for night shift. “Since it’s a far off place, doctors do not prefer being posted here. Those who are posted here get themselves transferred to some other place,” said Dr Shah. Besides three dais, two lady health visitors and a senior staff nurse and two midwives working here under a Unicef project, “Women’s Right to Life and Health, according to Dr Qureshi, who stated that Unicef had also provided stretchers, a delivery table and equipment to the health facility. With a new block, comprising an operation theatre and a children’s nursery, currently under construction and diagnostic facilities planned, the Rs19 million project is expected to be completed by June next year. (By Faiza Ilyas, Dawn-13, 06/08/2007) Attack on polio team AS we had feared, the nationwide polio vaccination campaign hit its first snag on Tuesday in the tribal areas when a health team was beaten up by armed men in Bajaur. As a result of this incident, the polio campaign has been suspended in the agency until further notice. This is exactly what those opposed to the polio vaccine want but authorities must not cave in. Campaigns against the polio vaccine in the past few years have caused a lot of damage in the NWFP and tribal areas 20 where a rise in polio cases has been reported and tens of thousands of parents have refused to have their children inoculated. Opponents have used illegally set up radio stations and mosque loudspeakers to convince people that the vaccine is a western conspiracy aimed at reducing the Muslim population. Unfortunately the government’s awareness campaign has not turned people against the vitriol being spewed by illiterate clerics. It needs to reach out to the people and make them aware of the fatwas, signed by prominent religious scholars including Maulana Fazlur Rahman, who say that the vaccine is not un-Islamic. The government also needs to arrest irresponsible elements who threaten people’s lives with their blind prejudice. It is understandable that the campaign had to be suspended for security reasons but they did this last month and cannot keep suspending campaigns, especially if cases of polio are being reported. Security threats are real — a doctor was killed in February while on his way to Bajaur to raise awareness on the polio vaccine — but need to be countered. It is important that those involved in this campaign are given protection but on no account should the campaign be called off. Doing so will be seen as a sign of weakness on the part of the government. (Dawn-7, 09/08/2007) Doctor indicted for stealing patient’s kidney KARACHI, Aug 8: Senior civil judge, Central, Qazi Naeem, indicted on Wednesday a doctor accused of stealing a patient’s kidney. Dr Kashif Mateen, son of Syed Mateen Zaidi, faces charges of having stolen a kidney from Mohammed Kashif, son of Zamir Hussain Siddiqui, while the patient was undergoing surgery on May 7, 2006. The defendant pleaded not guilty to the charges and the court fixed Aug 25, 2007, as the date for recording the statements of the prosecution witnesses. According to the prosecution, the plaintiff went to North Nazimabad’s Medi Complex Hospital complaining of severe abdominal pain. The clinic, which is run by the defendant, told Mr Kashif that he would have to undergo surgery to remove stones from his gall bladder. The patient was given medication and operated upon, but the doctor did not tell him that one of his kidneys had been removed. When Mr Kashif continued suffering pain in the same area, he consulted a doctor in Papush Nagar. After conducting various tests, including an ultrasound, the doctor told Mr Kashif that he had merely one kidney and that the other one had been removed. Mr Kashif registered a case under Sections 334 and 404 of the Pakistan Penal Code with the Taimoria police station (FIR No 280/06) against Dr Mateen, who was subsequently arrested on July 8, 2006. The court framed charges against the defendant and directed the district attorney to produce prosecution witnesses. (Dawn-17, 09/08/2007) 10,000 epidemic cases reported after rains Around 10,000 diarrhoea and gastroenteritis cases have been reported in Sindh since the heavy rains lashed the province and health officials have feared more epidemics if unhygienic conditions persisted. “We have received 10,000 diarrhoea cases across the province since 8th of August,” said Deputy Secretary Health, Sindh, Dr Shakil Mullick on Saturday. He pointed out that 3,700 cases were alone reported in the metropolis during the last five days and added that about 100 respiratory infection cases were reported in the interior Sindh after the rains. “Definitely, there was great danger of breaking out of epidemics (mainly diarrhoea) if unhygienic conditions continued,” he said. “Usually, cases of infections, gastroenteritis and malaria get increase after rains because of filthy atmosphere and lack of potable drinking water,” said Dr Seemi Jamali, Deputy Director of the Jinnah Postgraduate Medical Centre (JPMC). She suggested that concerted efforts should be made to drain out the stagnant water and proper spray should be carried out in order to prevent spread of malaria. “The hospitals tend to receive cases of gastroenteritis, eye infection, skin diseases and malaria etc after rains because of filth and stagnant water which provide breeding grounds for flies and mosquitoes and owing to mixture of sewage with drinking water,” said Dr Kaleem Butt, medical superintendent of the Civil Hospital Karachi. He however said that they have so far received no cases of epidemics after the rains. “Nursing hostel and the administration block of the Civil Hospital were still flooded,” Dr Butt said. Dr Habib Rehman Soomro, central Secretary General of the Pakistan Medical Association (PMA) claimed that cases of epidemics after the rains have already been reported at government-run hospitals and added that the hospitals high ups were not disclosing exact figure in order to save the rulers from possible embarrassment. Dr Seemi Jamali said the JPMC administration deployed its two sucking machines to drain out the rainwater accumulated in its emergency ward after finding no positive response from the Cantonment Board. She said the emergency ward was still flooded and the doctors were treating patients at a make-shift arrangement at another department. “We have been moved to another venue in view of accumulation of rainwater in the emergency ward and so far nothing has been done by the Cantonment Board,” she said. She said the hospital has received nine bodies since Thursday. Nursing hostel and the administration block of the Civil Hospital were still flooded, said Dr Kaleem Butt. (By Imtiaz Ali, The News-13, 12/08/2007) Maternity home without health-care facility KARACHI, Aug 12: With an unfinished structure erected to make staff residential quarters, rooms meant for doctors and private patients being used as store rooms and an operation theatre that has been closed for almost two years, the Shah Faisal Maternity Home and Child Healthcare Centre is one of the many public healthcare facilities which paints a dismal and gloomy picture of the situation of health sector in Pakistan. 21 Inaugurated thrice Interestingly, this health facility located in Shah Faisal Colony No.1, has been inaugurated thrice by different government officials during the past 14 years pointing towards the psyche of our officials who use such projects just to boost their public image. Commenting on its multiple inaugurations, Dr Waseem Iqbal said that last time the facility was inaugurated in October 2004. “Every time the old plaque is removed and a new one is installed bearing the name of the dignitary. The truth is that nobody really owns this maternity home as it is being run on an ad hoc basis. There is no budget for it nor there are any regular employees,” she added. Dr Waseem joined the health facility in 1995-a year after its construction-as in-charge gynaecologist. Security concerns Recalling those days, she said that the law and order situation of the locality was poor and armed activists of an ethnic political party used to take control of the hospital building at night since the building was without a boundary wall. She said that this maternity home was a result of community contributions and as soon as it was completed, every political and religious party made attempts to get hold of this place to use it for its activities. At last, it was decided to be used as a maternity home. Following its opening, a large number of staff was appointed here comprising 11 doctors and four lady health visitors. However, all left one by one due to security reasons and also because there wasn’t much work, she said. ‘No govt support’ When efforts to seek government support in raising a boundary wall failed, a trust came to our rescue, Dr Waseem said. She said that the trust not only helped in erecting the boundary wall and iron fences etc, it also donated trees which you could still be seen flourishing. The same trust built an operation theatre in 1999. With an operation table and lights donated by the trust and instruments handed over by the defunct KMC administration, the operation theatre started functioning till it had to be closed down in 2005 due to shortage of staff. Dr Waseem said that the main hindrance in the smooth functioning of the facility was the absence of regular staff as all of them were on deputation. “Though the maternity home is under the city government, there are some employees who have come from the Sindh government. They leave as their period is over or get themselves transferred. The construction which had started in ’95 for residence quarters is still incomplete,” she deplored. According to Dr Waseem, this is the only maternity home without residential facilities in the East zone. Despite presence of ample staff comprising three doctors, five nurses, a midwife and three ayas, on average five deliveries are carried out in a month. Two doctors only attend to the patients of general out-patient department and leave by 2pm. “Women do come regularly for antenatal checkups but avoid deliveries here. One reason is the misconception that only a doctor is capable of handling deliveries and services are not good at government setups”, adds Dr Waseem. A staff at the maternity home, however, revealed that the doctors encouraged women to come to their private clinics for deliveries. According to a staff nurse, Parveen Wilson, apart from high risk cases, first delivery cases are also not attended as the chances of developing complications are high in such cases. Complicated cases are referred to Civil and Jinnah hospitals. ‘Abortion cases high’ There are no diagnostic facilities though an X-ray room exists. Also, there are many rooms in the facility which are either empty, locked or being used as store rooms. There is no ambulance, but a post of driver exists who works as a watchman and at times replaced by naib qasid. Along with a separate facility for childcare, there is also a section for family planning service. According to Dr Wasim, the number of women seeking abortion is high. “Three to four women come to us everyday for abortion. We do encourage child spacing but advice women not to go for abortion as it can be harmful to their health,” she said. (By Faiza Ilyas, Dawn-17, 13/08/2007) Pakistan needs 74,000 more pharmacists HYDERABAD: Scholars, educationists, pharmacists and other medical experts have underlined the need for increasing the number of pharmacists, particularly in hospitals, for provision of proper health care. Speaking at a seminar on “New trends in the practice of pharmacy”, organised by the Faculty of Pharmacy, University of Sindh, here, the speakers pointed out that there is a need for 80,000 pharmacists in the country, but only 6,000 pharmacists were working presently. They also emphasised the need for special efforts to boost pharmacy education and research because, they added, the services of pharmacists were essential to measure the quality of medicines, create awareness among patients about medicine use and proper sale of medicines at medical stores. Due to the shortage of pharmacists in hospitals, unprofessional people are running pharmacist shops, they said and emphasised the need for proper training of pharmacists and recognition of their profession. Vice-Chancellor, University of Sindh, Mazharul Haq Siddiqui, presided over the seminar. He said though there were weaknesses among doctors but the majority of them were delivering service in the best way. He said Sindh University, realising the importance of pharmacy education, had upgraded its institute up to a faculty with four departments. The VC added that a project of Rs 100 million had been launched, which was near completion. 22 He said that under the project, equipment had been provided at a cost of Rs 16 million and glassware and books at a cost of Rs 10 million. The VC called upon the provincial health department to provide internships to students of the university’s Pharmacy Faculty for training to enable them to do community service. Director-General Health Services Dr Hadi Bux Jatoi, who was the guest of honour at the seminar, said the society had been facing multiple problems, including lack of proper healthcare. He said that due to lack of accountability, nobody was performing duty in a proper manner and nobody was willing to ask them to do so. (The News-3, 13/08/2007) Rains leave hospitals flooded with gastroenteritis cases KARACHI, Aug 13: After the recent heavy showers that collapsed civic infrastructure in the city, increasing number of gastroenteritis cases are being reported at government hospitals. At the National Institute of Child Health, more than 50 children were being brought daily at the emergency ward with symptoms of mild to severe dehydration since the advent of rains, Dr Shamsher Ali told Dawn on Monday afternoon. “Today, we have received 31 patients so far. Of them, 10 children have been admitted. But, their number will increase as the day progresses,” he said. He pointed out that majority of the children, who had been brought to the healthcare centre so far, aged between four and nine years while 75 per cent of them were on bottle feeding. “This is the major reason for children becoming vulnerable to infection. Parents are repeatedly told to stop bottle feeding, use boiled water, properly clean utensils and give an easy digestible diet to children,” he said, adding that most of the patients were coming from low-income areas where proper sewerage system did not exist. About 80 cases were reported at Jinnah Postgraduate Medical Centre on Monday which was much higher than the daily average of around 40 to 50 gastroenteritis cases reported at the hospital, said Dr Seemin Jamali, in charge of JPMC’s emergency section. She advised public to fumigate homes, eat well-cooked food and prevent children from consuming ice candies and junk food. There was an imminent danger of dengue epidemic after rains so every precaution should be taken to avoid the repeat of last year’s episode, she said. The Medical Superintendent of Civil Hospital Karachi, Dr Kaleem Butt, said there had not been a sudden surge in gastroenteritis cases at the hospital yet. However, he said, the possibility could not be ruled out in the coming days. Swift action required The Pakistan Medical Association has urged civic agencies to take swift action for disposal of rainwater accumulated in almost every locality before it becomes a breeding ground for mosquitoes and flies, which could result in spread of malaria and other infections. Chlorination stops At a time when the incidence of diarrhoea, gastroenteritis and other water-borne diseases are already on the rise, the process of chlorination and putting alum has come to a halt at all the seven filtration plants of the KWSB, resulting in supply of unclean water to the city. Confirming that almost the entire city was being supplied muddy water nowadays, sources in the KWSB said the process of chlorination and alum mixing had been suspended temporarily. They said the water supplied to the city, from both the Indus and Hub sources, was carrying enormous quantity of mud and as such mixing even a high quantity of chlorine and alum would not give desirable results. (Dawn-19, 14/08/2007) Hundreds suffer as JPMC clinics forcibly closed KARACHI, Aug 16: Hundreds of patients were forced to return home without getting medical treatment from the Jinnah Postgraduate Medical Centre here on Thursday as different outpatient clinics (OPDs) could not be held following Wednesday’s killing of a student at the Sindh Medical College in a clash between two student groups. Members of a student group ensured that things could not function as normal on Thursday by using different pressure tactics to register their protest against the killing. OPDs of the departments of medicine, surgery, gynaecology, orthopaedics, chest, urology, psychiatry and others could not be held while the functioning of the emergency ward was also affected for a brief period in the morning, but functioned normally later on in the day. Offices of the Punjabi Students’ Association (PSA) ‘Punjab House,’ located in Bazzatta Lane, was also set on fire on Thursday. “The premises were in possession of the members of the PSA, which were set on fire gutting furniture and different fixtures. No casualty was reported in the incident,” SPO Saddar DSP Kamran Rasheed said. Similarly, two rooms of the Shah Latif Hostel, said to be in the possession of PSA students, were also set alight gutting furniture and different fixtures. Tension spread to different colleges and universities across the city where extra security was deployed by the police and Rangers to avert any possible spill over. 23 Police have registered two cases in connection with Wednesday’s incidents at the JPMC, one pertaining to creating a law and order situation in which five students of the PSA were arrested from the spot. The second FIR was registered in connection with the murder of Hafiz Abdul Rehman, a final year student and member of the Islami Jamiat-i-Talaba. Rangers take over security A unit of the Pakistan Rangers (Sindh) on Thursday took control of security at two major medical colleges of the city to avoid any “repercussions” in the aftermath of Wednesday’s violence, officials said. According to a Rangers’ spokesman, a unit comprising “a few” hundred paramilitary personnel reached the premises of the Sindh Medical College and the Dow Medical College and assumed security duties at the campuses. The Dow University of Health Sciences (DUHS), to which these colleges are affiliated, had already suspended teaching activities there and the newly established Ishratul Ibad Dental College for three days to ensure there was no bloody sequel to Wednesday’s incident.The officials of the two colleges said they had issued notices to over 200 students residing in the boys’ hostels to vacate them by Friday. “We have issued notices to the residents of the boys’ hostels and would get the spaces vacated by Friday (today),” Dr Tariq Sharafatullah, Principal of the SMC, told Dawn. Around 120 students are housed in the SMC’s boys’ hostels. Prof Salahuddin Afsar, Principal of the DMC, said the college administration had issued similar notices to some 100 residents of its boys’ hostel. The two top officials said no untoward incident was reported in their premises due to beefed-up security and suspension of teaching activities. They gave no deadline when the students would be allowed to re-occupy their rooms in the hostels. “We’ll decide as soon as the situation normalises,” Prof Afsar said. Prof Masood Hameed Khan, Vice-Chancellor of DUHS, had earlier said rooms at the SMC’s hostels would be re-allotted after strict scrutiny of the students. The DMC management had already re-allotted hostel rooms lately. (Dawn-17, 17/08/2007) Drive to check maternal deaths stressed KARACHI, Aug 16: The only way to check the high maternal mortality ratio (MMR) in Pakistan is to initiate a massive, longterm and efficient midwifery training programme. This was suggested in a report titled ‘Health of Women in Pakistan: Annual Report 2007’, released by the Society of Obstetricians and Gynaecologists of Pakistan (SOGP) at the PMA House on Thursday. This first ever report prepared by the SOGP on women’s health was presented by its president Dr Shershah Syed, Secretary Ayesha Nasir and Finance Secretary Dr Nighat Shah. The report contains data on women’s health, status of girl child and menopausal women and also highlights the issue of domestic violence and other problems being faced by women and identifies the flaws in obstetrics and gynaecology training. Speaking at a press briefing, Dr Shershah said that the basic aim to prepare this document prior to general elections was to make political parties include these important issues in their manifestoes. “A country has no future with a huge population of uneducated, unhealthy and battered women. All political parties need to resolve that these issues concerning women would be addressed on priority if they come into power,” he said. The SOGP was ready to help the government uplift the status of women’s health, provided it showed sincerity and a political will in resolving the problems at hand, he remarked. Underlining the role of midwifery, Dr Syed observed that competent midwives could play a crucial role in the reduction of the maternal mortality rate. The role of midwives, as a catalyst to social change, had long been neglected and their profession had not received the respect and status it deserved, he said. According to the report, Pakistan loses three women per hour owing to pregnancy-related complications and the MMR stands at 340-500/100,000 pregnancies. Haemorrhage, hypertension and infection are the three major causes of maternal death. Delay in making a decision to consult a doctor or in acquiring transportation and emergency care also contributes to MMR. Under-five mortality rate is 103/100,000. Over 80 per cent of deliveries take place in the presence of unskilled birth attendants, therefore, a large number of women, around 375,000 women annually, suffer from vaginal fistula, recto-vaginal fistula, depression and chronic pelvic complications after delivery, which are preventable. About the health facilities and health budget, the report says that the government spends a meager 0.6 per cent of the GDP on health and around 2,400 basic health units, rural health centers and taluka hospitals are non-functional. There is one specialist and one doctor for 14,500 and 2,300 people respectively. There is no national screening programme for breast, cervical and prostate cancers, some of the leading causes of women’s death in Pakistan. It said that the state of postgraduate education in obstetrics and gynaecology was poor. “There is a need to make sure that all medical students know about maternal death, morbidity and emergency obstetric care,” the report states. It also calls for the need to change social attitudes towards women and mass education for girls on a priority basis. The SOGP’s demands included provision of free emergency obstetric care in all public sector hospitals and maternity 24 homes round-the-clock; training programme to produce an army of skilled midwives; autonomous status to National Committee on Maternal and Newborn Health to monitor emergency obstetric care in country and consultation with SOGP and Pakistan Medical Association on women’s health. The report is based on UNDP Human Development Report 2006, Pakistan Millennium Development Goal Report 2005, Human Development in South Asia 2004, Health Situation in South East Asia Region and World Development Report 2003-04. (By Faiza Ilyas, Dawn-19, 17/08/2007) Three expectant mothers die every hour, says report Three women die per hour in Pakistan because of pregnancy-related complications, disclosed the annual report of Society of Obstetricians and Gynaecologists of Pakistan, issued at a press conference at PMA House here on Thursday. Dr Sher Shah Syed, President of the society, while presenting the annual report of the year 2007, “Health of Women in Pakistan”, said that around 400,000 women suffered every year from pregnancy-related complications as more than 80 per cent of the women delivered at home in the presence of unskilled birth attendants. He said that as against one male baby death during delivery, six female babies died at the time of delivery. He criticised growing violence against women and revealed that 90-92 per cent babies left in cradles outside Edhi Centres through out the country were girls. He said that about 30,000 midwives are urgently needed to overcome the current situation and the government should have a proper plan to achieve this goal. He said the purpose of presenting the report at this particular juncture was to highlight the issue in the upcoming election campaigns, so that the political parties could focus on the problems of women in their manifesto. He said that his society was planning to hold a seminar on the issue for the politicians and policy makers of the country, so that they could realise the actual dismal scenario regarding women’s health in the country. He announced the release of the report on an annual basis. Dr Ayesha Nasir, general secretary of the society, said that the government was getting huge grants and loans from donor agencies to improve women’s healthcare in Pakistan but it failed in proper utilisation of these funds because of the lack of political will and ignorance about the existing healthcare system in the country. She said that cancer, especially breast cancer, was a major cause of death among women in Pakistan but screening facilities for these diseases were not yet there. She said that the private sector was just focusing on the elite. Consequently, the poor masses were facing the worst situation regarding health. Dr Nighat Shah, treasurer of SOGP, criticised the government for its neglect of the health sector. She said that the government hospitals were providing health facilities to just 20-22 per cent of the population. She said that in Japan and Sweden, one death in 100,000 cases of delivery was reported while this ratio was 400-600 in Pakistan. She said that even many Third World countries were focusing on the health sector but the government of Pakistan was not performing its duties. She reminded the participants that provision of healthcare facilities to people was the exclusive responsibility of the state. She said that as the wives of our rulers and politicians gave birth to their babies abroad, the rulers were just not aware of the poor status of health services in public sector hospitals. She said that government had money for BMW cars for ministers but not for provision of better health facilities to common people. She said that the matter was not of money but of priority. The SOGP office-bearers said doctors are worried about the health education provided in our medical institutions and increasing number of private clinics run by unskilled people without any checks and balances. They termed it the result of the government’s negligence. They condemned the termination of pregnancy after diagnosis of female conception, fewer opportunities for the girl child for education, discriminatory behaviour towards women in every field, sale and barter of girls, and honour killing and demanded immediate action to improve the situation. Doctors also demanded provision of better care and attention in hospitals, especially gynaecology cases. They demanded free Emergency Obstetrics Care (EmOC) in government hospitals on a 24-hour basis and stressed the need to consult with SOGP and PMA in order to improve women’s health in the country. They criticised appointments on political basis in the health department and demanded complete transparency in government projects regarding health. They urged initiating mass education programmes for girls along with structured a post-graduate training programme for doctors to produce skilled gynecologists in the country. They appealed to people to not vote for those parties and candidates in next election who did not prioritise the women health issue in their manifesto. (The News-14, 17/08/2007) Organs trade gets new lease of life ISLAMABAD, Aug 17: The commercial dealings in organs got yet another lease of life when the government decided not to promulgate the Transplantation of Human Organs and Tissues Ordinance 2007, already approved by the cabinet, and instead introduce a bill in the National Assembly on the last day of the current session of the lower house of parliament, ostensibly under pressure from the lobby patronising organs trade in the country. There is little possibility that the present National Assembly, nearing the end of its life, would be able to take up the bill. Sources claim the last-minute change in strategy, which appears to be no more than an attempt to further delay the promulgation of the law, was done on the instructions of Prime Minister Shaukat Aziz who had earlier in January turned down a health ministry’s proposal not to refer it to the cabinet and instead advise President Musharraf to promulgate the ordinance -- a move that delayed the process by at least eight months. 25 Government’s haste was evident from the absence of federal health minister, minister of state for health and parliamentary secretary for health from the house at the time of introduction of the bill. The Supreme Court had earlier given one month to the government to legislate on transplantation of organs. The deadline expires in the first week of September and the court would resume hearing of the case on September 3. Federal Secretary Health Khushnood Lashari gave a very simplistic explanation of introducing the bill on the last day of the session saying: “We (the government) were not aware that the National Assembly was going to be prorogued. President of Transplant Society Dr Adib-ul-Hassan Rizvi said he was utterly disappointed by the government move. The bill has now been placed before the parliament for the fifth time during the past decade and a half, but on each occasion it failed to get through because of intense opposition from the lobby opposing the law. During all this delay the kidney trade thrived and the business in the country is today valued at almost Rs one billion a year. Prior to this latest move by the government, certain controversial clauses, like payment of compensation to unrelated donors, were inserted in the draft of the ordinance that was placed before the cabinet at its August 1 meeting. However, the government under pressure from civil society and doctors’ associations removed the controversial clauses and the ordinance looked imminent. Annually 2000 kidney transplantations are carried out in the country. Of these 500 are performed in government hospitals from living related donors. The rest 1,500 are from unrelated kidney sellers and these transplants are performed in private hospitals. About 900-1,000 of these are for foreigners who come from more than 20 countries of the Middle East, North America, Europe and South Asia and paying hefty amounts. The rest are locals. Those who are non-affording and have no family donors rely on donations from family, friends and social welfare organisations to pay for huge costs of transplantation at private hospitals. Once transplanted they find payment for followup medicines particularly immunosuppressive drugs difficult which can cost between 10,000 to15,000 rupees per month. Ultimately they stop medication and lose their transplanted kidneys. So the unrelated commercial transplant seldom helps them in the long term as the poor recipients hardly bear subsequent costs. Commercial dealings of kidneys are centred in Lahore and Rawalpindi and majority of the kidney sellers are from rural Punjab, almost 70 per cent of them are bonded labourers. These desperate people sell their kidneys for Rs70,000 to 120,000 mainly to pay off their debts. Recent surveys have shown that 95 per cent of the sellers do not achieve their objectives and remain desperately poor and in debt. Selling their kidneys brings no financial benefit and many complain of their payment being siphoned by middleman and hospital for travel and operation expenses. Moreover, most have feeling of guilt and they are depressed and often unable to keep their livelihood. (By Baqir Sajjad Syed, Dawn-1, 18/08/2007) Patient dies in traffic jam after 5 ANP men held KARACHI: Rioting broke out in Malir after the police took five Awami National Party (ANP) activists into custody Friday. Men wearing masks roamed the streets openly brandishing weapons. Supporters blocked the roads from Quaidabad to Kala Board, including the National and Super highways, and pelted passing vehicles with stones. The chaos caused a huge traffic jam that forced families to abandon their vehicles and make it on foot. A journalist who also got stuck in the jam said that he had to get off and after two hours in his vehicle and walk because traffic was not moving an inch. He said that he saw three ambulances stuck as well. Later there were reports that one patient had died inside a car. TPO Bin Qasim Abdul Aleem Jaffery told Daily Times that the police was on snap-checking when a suspicious car (JL-1000) was stopped. The TPO said they recovered two baby Kalashnikov, a repeater gun, a triple two rifle, a TT pistol and a Kalashnikov from the possession of five men identified as Khanzada, Bashir, Nadeem, Imtiaz and Zubair. ANP President Shahi Syed that the men who were arrested by the police were guards who were passing through Malir 15 after a party rally in Saddar. “They were licensed weapons,” Shahi Syed said. “The police beat the men up also.” (DailyTimes-B1, 18/08/2007) Experts demand ordinance on organs trade KARACHI, Aug 18: The director of the Sindh Institute of Urology and Transplantation (SIUT) and president-elect of the Transplant Society of Pakistan (TSP), Professor Adibul Hassan Rizvi, has appealed to President Gen Pervez Musharrraf to immediately promulgate the Transplantation of Human Organs and Tissues Ordinance 2007 and save Pakistan from the ignominy of being referred to as an “organ bazaar”. Speaking at a press conference jointly organised by the Pakistan Society of Nephrology (PSN), Pakistan Association of Urological Surgeons (PAUS) and TSP at Dewan Farooq Medical Complex of SIUT on Saturday, he expressed disappointment over the government’s move of introducing the bill, already approved by the cabinet, in the National Assembly just a few hours before it prorogued after a 19-day session. He feared that the passage of the law from the lower house of parliament would take years. “For how long we will see the worst form of human exploitation?” he wondered and appealed to the president to promulgate the ordinance without further delay. Once the ordinance was in place, it would be easier for the National Assembly to pass it later as a law, he argued. The struggle against organ-trafficking, he said, was decades old when the first bill was prepared by Syed Iqbal Haider in 1992. Since then, the bill has been vetted by different committees of the Senate and the National Assembly but, unfortunately, has failed to see the light of day. “Over the years, Pakistan has earned the epithet of an ‘organ bazaar’ where people from all over the world come to buy cheap kidneys for $15,000 to $20,000. The organ trade is flourishing in Pakistan because there is no law, thanks to the government and people who are powerful enough to influence the government,” he said. 26 The situation, he recalled, was completely different 12 years ago when 75 per cent of the transplants concerned living and related donors. Today, 80 per cent of organ transplantation was done on a commercial basis in the country due to a lack of legislation. India was an example in this case where a law had been introduced and many doctors sent to jail for their involvement in kidney trade, he said. Dr Farhat Moazzam, the chairperson of the Centre of Biomedical Ethics and Culture, SIUT, said that in the absence of any legislation organ-trafficking was being treated as a case of theft and doctors earlier caught for this crime had been released. Public awareness, she said, was a long-term solution to the problem as it also had social dimensions. “Almost all the victims are illiterate people who live in abject poverty and many of them are forced to sell their kidneys to repay debts,” she said. Answering a question regarding any loophole in the proposed ordinance, Dr Anwar Naqvi said that it was in a better shape as most of the objectionable clauses had been removed. About the future course of action, he said Dr Rizvi would meet the president in this regard. Dr Sajjad Hussain and Dr Iffat Yazdani also spoke. (By Faiza Ilyas, Dawn-17, 19/08/2007) Maternity home fails to provide 24-hour emergency service KARACHI, Aug 19: The recently released report titled Women’s Health in Pakistan by Society of Obstetricians and Gynaecologists of Pakistan (SOGP) blames the unavailability of 24-hour emergency obstetric care at government hospitals and maternity homes for the country’s persistently high maternal mortality ratio (MMR). There is little doubt about the veracity of this assertion as none of the 30 maternity homes functioning under the city district government provides roundthe-clock emergency obstetric care. A case in point is Seth Seoomal Murchand Khilnani Maternity Home. Opened by the then Mayor M.H. Gazdar in 1942, the maternity home is ranked among the few well-managed public sector health facilities for women. But, surprisingly, despite having a team of competent doctors, a fully equipped operation theatre and labour room, the facility fails to function for 24 hours on a daily basis. Sources say that the operation theatre has been closed since February when its lights malfunctioned and rainwater seeped into wires. The problem may be rectified but nobody is really interested in making the OT functional which would mean extra work. Even when the OT was functioning, few operations were performed, and that too during daytime, the sources recall. Partially acknowledging the problem, medical officer Dr Bushra Israr, however, maintains that the OT is still being used for ‘minor operations’ but more staff is required to run the service on a regular basis. “We need separate staff to deal with emergency and OT requirements. There is no anaesthetist and we have to call one when the need arises,” she said, adding that the 30-bed facility needed an RMO (resident medical officer) to be able to run for 24 hours daily. Another major handicap in pursuing this goal is also that public sector health facilities, by and large, operate on an ad-hoc basis and there is no constant provision of funds. In case of maternity homes, the only government help that they receive is for repairs or medicines. As for this healthcare facility, proper renovation is badly needed as, according to the staff, most of its ceilings leak and the roof has fallen apart in some places. At present, 35-member staff, including seven doctors, four nurses, two midwives and two lady health visitors, work here in shifts. While this seems to be enough manpower to properly run the facility, there is no system in place to identify patients needing immediate help. Consequently, such patients suffer as they have to wait for long periods for their turn. “The doctors come late and the patients have to wait for hours for their turn. I am having constant pains but I have to wait for my turn till all other patients who have come before me are examined,” complained a woman. However, despite these lapses in service, the facility is a preferred choice and women from all over Karachi come here for antenatal checkups and normal delivery. Around 200 patients daily visit the OPD while over 70 deliveries are performed here every month. “This is mainly because of the good performance of some staff who have been working here for a long time. People know us and there are families who have been visiting us for generations. We have never had a death at our facility,” proudly asserts Marsi Khurshid, the sister-in-charge who has been working here for 18 years. According to her, the number of patients frequenting the facility was much higher a decade ago when free food was provided to patients. As more and more private health-care facilities sprang up, their number decreased. Still, some aspects are unique to the facility. Apart from being one of the oldest health-care facilities, it’s the only public sector maternity home in the city which has a midwifery school and is among the few where ultrasound and lab facilities for simple blood and urine tests are available at nominal charges. There are also separate sections for pediatrics and family planning. Shedding light on social attitudes towards birth control methods, Surriya Asim, who heads the family planning section, says that a major change is men’s willingness to undergo vasectomy if they are told that the use of contraceptives can harm a woman’s health. “It all has come through awareness. We discourage abortion, but motivate women about child-spacing,” she said. The midwifery school, named after the late Professor Karar Hussain’s wife, Sartaj Bano, opened in 2004. Narrating the story behind its establishment, Dr Shershah Syed, former secretary-general of the Pakistan Medical Association, said that this old building was earlier being used as a clinic for KMC employees. After the second local government elections, some political activists took control of it, but on the immediate intervention of City Nazim Mustafa Kamal the building was vacated. 27 “This shows that any difficulty can be overcome with a political will. It’s sad that millions of rupees were spent on a fancy fountain while pregnancy-related complications claim lives of thousands of expectant mothers every year only because successive governments have failed to make health facilities operate round the clock,” he regretted. (By Faiza Ilyas, Dawn-13, 20/08/2007) Filthy water puts KU students at risk KARACHI: Probably S.T. Coleridge had foreseen the water problem of Karachi University when he wrote the Rhyme of the Ancient Mariner. The water supply system of the University of Karachi is as messed up as that of the entire city. Apart from the university’s algae-infested water tank, which has not been cleaned for years, the deteriorated condition of water pipes speaks volumes of the official carelessness. The supply of contaminated water put the health of around 24,000 enrolled students and 600 to 700 university teachers at risk. The main line that supplies water to the university has been dug up at many places near Maskan, PCSIR labs and Sheraton Flats to let the air pass through it though it also allows foreign elements which causes contamination. The university laboratory had recently tested the water and submitted its report to the administration. Though KU administration paints a rosy picture of it, lab sources disclosed that the water samples were found hazardous for health. “It is as bad as that of the rest of the city. Though I can’t reveal much as the report is confidential, I can tell you that it shouldn’t be consumed without being filtered and boiled,” an official said on condition of anonymity. The water tank seemed to be haven for insects and animals while the pipes were all covered with rust and wild shrubs grew crazily about the place when the scribe inspected them. The head of the pumping system, Rasheed Alam, puts all the blame on Karachi Water and Sewerage Board. He said: “We supply water the way we get it from the KWSB. The tank from which they supply water has at times dead animals in it as well”. He said the tank hadn’t been cleaned for the last three years. Besides, he said the badly corroded pipes were one of the main reasons for water contamination. “The six-inch-diameter pipe has so much of rust that it only allows water that a twoinch-diameter pipe can supply,” he added. He simply denied if there was any filth except for the insects in the tank but said that there had been a few instances when they had actually found polythene bags in the pipelines. The university engineer, who looks after the maintenance of the waterlines, never replied to the phone calls made to have a better insight into the situation. Though filters have been installed at some of the departments, teachers prefer not to drink water from it and bring boiled water from their homes. “We know the condition of the tank and we can’t risk our lives just to experiment whether we survive after drinking water from here,” says one of the teachers. However, those residing on the campus complain about the negligence of the staff and indifferent attitude of the administration. Mostly students are unaware of the whole scenario as they merrily take a dose of the bacteria and germs to quench their thirst. (By Meera Jamal, Dawn-15, 20/08/2007) Water-borne diseases hit residents of Bin Qasim The post-rain situation in Bin Qasim Town may lead to an outbreak of infections such as diarrhoea vomiting, allergy and eye-ailments, as the City District Government Karachi (CDGK) is not cooperating with the town management. Town Naib Nazim Yousuf Shah told The News on Saturday that the town had no proper equipment and machinery to remove stagnant rainwater from the area. “We have limited resources and despite the fact that we are using them properly, we are unable to clear all areas,” he said, while accusing the CDGK of not assisting the town. “It is the CDGK’s responsibility to spray each town every week to avert an outbreak of disease after the rain but unfortunately, it has failed to take any initiative in this regard,” Shah said. Moreover, if this continues in the fishermen colonies, the results can be disastrous. “We cannot spend a single penny on health and education from the town budget as it can be termed a violation of the Local Government Ordinance (LGO),” Shah added. Activists claim that due to the stagnant rainwater in many fishermen-dominated localities, there are chances of outbreak of disease. The town administration has not taken any measures to remove the garbage polluting the area, they added. All the roads are still in a dilapidated condition, disconnecting the nearby localities. For instance, the main road connecting Ibrahim Hyderi, Rehri, Chashma and Dabla goths is damaged and the worst affected people are patients, whose families face problems in bringing them to nearby hospitals on time. Moreover, there is only a 50-bed Sindh government hospital in Ibrahim Hyderi for all neighbouring localities. The hospital is receiving more than 20 patients daily, suffering from diarrhoea and allergies, most of them children and women. Several cases have been referred to thje Jinnah Postgraduate Medical Centre (JPMC), due to unhygienic conditions in the hospital. However, those who are relatively well-off prefer to take patients to private hospitals. People in Dabla Goth are still residing in their make-shift homes, because not only rainwater but seasonal high tides have also played havoc with them. They received no relief and help from any government and non-government organisation except false promises by the high-ups on their visits to the flooded locality. Shah said that they designed a proposal and presented it to the CDGK for Dabla Goth as the people here are the main victims of high tides and rains living in a low-lying locality. (By Jan Khaskheli, The News-14, 20/08/2007) 28 Eight million diabetic patients in Pakistan Around eight million people are suffering from diabeties in the country and their number was constantly increasing, said Dr Obaid Ahmed Hashmi on Sunday. “Thousands of affected diabetic patients could not realise it due to lack of awareness,” he said. He was speaking at a seminar at Al-Mustafa Medical Centre. He said Pakistan stood at number eight in this regard. “This disease adversely affects the heart, mind, kidney, eyes and other body parts,” he said. He said that in case of wounds, body parts of two to three diabetic patients are cut each month at the centre. Dr Farhan said that heart problem was increasing mainly because of cholesterol and blood pressure. He said that bringing changes in life styles, such as starting to exercise, could help overcome heart and diabetic complications. Meanwhile, Dr Prof Sharif Hashmani said that those wearing goggles could get rid of the safety glasses through a surgery with the help of modern techniques. He was speaking at a seminar organised by the Memon Professional Forum on Sunday. (The News-19, 20/08/2007) First report of Karachi’s largest Dengue epidemic published by AKU KARACHI: In the first report of the largest epidemic of dengue hemorrhagic fever (DHF) virus infection from Karachi, experts from the Aga Khan University Hospital found that adults were also susceptible and not just children as was previously believed. These findings were presented in a study ‘Dengue outbreak in Karachi, Pakistan, 2006: experience at a tertiary care center’ by E. Khan, J. Siddiqui, S. Shakoor, V. Mehraj, B. Jamil and R. Hasan and was published online in the journal Transactions of the Royal Society of Tropical Medicine and Hygiene on Aug 13. Medical records of 172 IgM-positive patients were reviewed. Patients were categorized into dengue fever (DF) and DHF. The mean age of the patients was 25.9 years, 55.8% were males. Five cases (2.9%) had a fatal outcome. Three were from a pediatric group (<15 years). In Asia, dengue has made its route geographically from Southeast Asian countries. In India the first epidemic of dengue was reported in 1963–1964. Since then, multiple outbreaks have been reported from different regions of India. New Delhi has a record of seven outbreaks since 1967. The last major outbreak reported in Delhi was in 2003. In Pakistan the first confirmed outbreak of DHF was reported in 1994 by the AKUH; the serotype reported was DENV-2. Thereafter, sporadic cases of DHF continued to be documented from different parts of the country. Antibodies specific to DENV-1 and DENV-2 were found in sera of children presenting with undifferentiated fever in Karachi, indicating that these two dengue serotypes predominated/prevailed in the 1990s. During 2005–2006, however, there was an unprecedented increase in epidemic DHF activity in the country, with a large number of cases being reported from Karachi. More than 3,640 patients with signs and symptoms suggestive of DF were admitted to several referral hospitals in the country, including the AKUH. There were 40 deaths, of which 37 were from the province of Sindh, making it the largest and most severe outbreak of DF in the country. Between May and November 2006 a total of 3,075 serum samples were received for detection of anti-dengue IgM. Of these, 482 were from patients admitted with a clinical suspicion of DF or DHF, and 172 were found to be anti-dengue IgMpositive. The medical records of these 172 patients with confirmed laboratory diagnosis for dengue virus infection were reviewed retrospectively for demographic, clinical and laboratory data. Most of the cases were from the east, center and north of Karachi. Two patients (1.2%) were referred from other parts of the Sindh province, while two patients were from Punjab. In 2006, the first case of DHF was admitted in the month of May. Thereafter, the numbers of cases steadily increased over the next 5 months. The largest number of cases was admitted from August to October, and the number of patients decreased during the month of November. Unprecedented population growth and unplanned urbanization are the two main factors that have led to the emergence of dengue virus infection in tropical developing countries. Karachi is also facing a similar crisis. Karachi experienced the first major outbreak of DHF in 1994, and since then DF has been recognized as one of the causes of fever in the area with few cases of DHF and very few deaths directly attributable to DHF/DSS. This is the first report of the largest epidemic of DHF with IgM-confirmed cases from Karachi, Pakistan. Analysis of monthly dengue cases showed peak incidence from August to October 2006. DHF is considered primarily to be a disease of children under the age of 15 years and is a leading cause of hospitalization of young children in Southeast Asia. In the study, 83.6% of adult patients presented to the hospital with signs and symptoms compatible with DHF. A similar age distribution was also noted during the 1994–1995 outbreak in Karachi. This observation is consistent with reports from other endemic countries. A 3-year study from India showed a maximum number of cases between the ages of 21 and 30 years. Hyperendemicity (co-circulation of more than one serotype) and/or introduction of a new virulent serotype in the community perhaps render the adult population more susceptible to a severe form of the disease. The population of Karachi has had a prior encounter with DENV-1 and 2. Serum samples from the patients with suspected DHF/DSS in the early part of this epidemic (autumn of 2005) revealed DENV-3 as the cause of the DHF. The shift in the age distribution of DHF in the study population is consistent with observations in other studies conducted in other endemic regions and is perhaps due to the introduction of a new serotype of dengue (DENV-3) in Karachi. The primary pathophysiologic abnormality seen in DHF and DSS is an acute increase in vascular permeability that leads to leakage of plasma into the extravascular compartments, resulting in hemoconcentration and decreased blood pressure. 29 Plasma volume studies have shown a reduction of more than 20% in severe cases. In the study, hemoconcentration by definition was documented in a few patients only. This is a very important finding, as raised hematocrit is one of the defining characteristics of DHF, based on WHO criteria, and an elevated hematocrit value is used for case definition in field studies during outbreak situations. Iron deficiency anemia and hemoglobinopathies are major problems in Pakistan. About 5% of the Pakistani population carries the ?-thalassemia trait. The patients may have had a low baseline hematocrit, leading to relative hemoconcentration. The role of these factors leading to low hematocrit levels in the presence of DHF without overt hemorrhage in the study population needs further studies. The experts observed a significant independent association of male gender and vomiting with DHF. It is their opinion that the uneven male-to-female ratio in the patient population is a reflection of the social bias of male gender in society. Failure to seek medical attention for females in the family (adults as well as children) in a timely manner may have led to high mortality in females. (DailyTimes-B1, 20/08/2007) JPMC set to outsource security set-up KARACHI, Aug 20: The Jinnah Postgraduate Medical Centre (JPMC) will outsource its security set-up in order to make it more effective. This was stated by Prof Rashid Jooma, the executive director of the prime federal government-run hospital in the city, on Monday. Talking to Dawn, Prof Jooma said that a proposal to enhance the security arrangements and improve the related affairs at the hospital was placed before a meeting chaired by Federal Health Secretary Khushnood Akhtar Lashari. The meeting was specially convened to review the situation after the killing of a student of the School of Physiotherapy, JPMC, on Aug 15. The JPMC executive director said that the proposal had in principle been approved by the health secretary and now the hospital would forward the relevant project paper to the federal ministry for funding and other relevant action. Estimating that the security augmentation project would cost around Rs65 million and would be completed over a period of two years, Prof Jooma said that the hospital would have a security system manned by over 200 persons, equipped with a closed-circuit television system, communication system for the personnel and weapons and vehicles including four wheelers and motorbikes. (Dawn-19, 21/08/2007) Villagers suffering from skin diseases According to reports, people, particularly children, living close to the oil and gas exploration and production fields in Sindh have been affected by skin diseases caused by the toxic material disposed in the open fields here. The oil and gas exploration carried out by multinational companies, in Taluka Johi and districts Dadu, Thatta and Badin, use toxic materials during their drilling and exploration process. The disease caused by contamination manifests itself in the form of marks on the feet, fingers, palms, throats and legs. According to the parents of the afflicted children, the disease has been termed “incurable” by the local doctors. Toxic waste can be seen in the fields near the village settlements close to the main Dadu-Johi road. According to the international environmental standards, toxic material should be discarded properly, away from any human settlements. Furthermore, locals say that following the company’s operation, the drinking water sources of nearby villages has also been contaminated with oil. This has forced the women of these communities to travel miles in search of water. According to a survey by the Participatory Development Initiative (PDI), the villages of Dhani Dino and Mohammed Buksh Panhwar in Johi and Dadu districts are the most affected. Similar symptoms can be seen in other gas exploration areas of Taluka Jati, Thatta district. A PDI spokesman told The News that the oil and gas company in question has established two health dispensaries in the area. However, they serve no purpose because of unqualified doctors as well as the unavailability of medicines. The local people point out that, while these multinational companies are making millions of dollars, they should provide health and other facilities to the communities adopted by them for exploitation — as pointed out by the standards of international Corporate Social Responsibility — instead of polluting the environment and spreading incurable diseases. (By Jan Khaskheli, The News-20, 22/08/2007) Substandard mineral water factory sealed The staff of Malir town administration and the food inspectors of the City District Government Karachi (CDGK) raided a factory which was producing substandard mineral water and drinks. Town Nazim, Ansar Ahmed Sheikh received information about the factory in Moinabad Phase 3 and sent a team led by the TO Municipal Regulation Muhammad Asif. According to reports, the team sealed the factory, seized drinks and mineral water worth millions of rupees. However no arrests were made. Gadap Town: Town Nazim, Ghulam Murtaza Baloch on Wednesday visited different areas and inspected the overall situation after heavy rains. He called for the immediate draining out of accumulated rainwater, especially around mosques and added that dewatering pumps have already been distributed among various Union Councils (UC) of the town. Baloch asked citizens to register their complaints at the town emergency control room on the phone numbers 4561228 and 4561287. 30 Liaqatabad Town: Town Nazim, Osama Qadri, after heavy rains on Wednesday visited the Sanitary Market Gulbahar, Lasbella Bridge, Nazimabad, Liaqatabad and Gharibabad underpasses, and areas around Abbasi Shaheed Hospital while paying particular attention to the Gujjar Nullah. The nazim advised citizens residing near Gujjar Drain to vacate their homes. Landhi Town: Town Nazim, Asif Hasnain declared a rain emergency on Tuesday night. Hasnain asked citizens to lodge their complaints on 5035729. Korangi Town: Town Nazim, Mohammad Arif Khan Advocate on Wednesday visited the low-laying areas of his district and inspected the draining of rainwater. (The News-20, 23/08/2007) 1,960 women to be trained as midwives KARACHI, Aug 25: The Sindh health department with the assistance of the federal government is all set to initiate the training of 1,960 women as qualified midwives to serve across the province. This was stated by the project director of the National Maternal, Neonatal, and Child Health programme (Sindh chapter), Dr Shahab Jan, during a meeting of the programme’s provincial steering committee here on Saturday. Sindh Health Minister Syed Sardar Ahmed chaired the meeting and assured all-out support to streamline the programme. He said that through this programme the government would ensure presence of qualified and well-trained midwives in all the 22 districts of the province.The minister said that the government was committed to improve the health status of the womenfolk and children.The programme’s project director said that as many as 1,960 women would be trained during the 18 month course and the trainees would also receive a monthly stipend of Rs3,500. He said that the federal government would release Rs77 million this year, as the first tranche of financial support, for the five-year programme. The cost of the entire project is said to be Rs3,246.74 million with Rs247.743 million allocated for training component, Rs131.119 million for public awareness and media campaign, Rs128.30 million for civil work and Rs627.490 million for procurement of required equipment and the project will also receive additional funds of Rs2 billion from the government of Norway during the five years. The project director said that under the programme in question all the 108 rural health centres in Sindh would be provided with lady doctors, lady health visitors and drivers to enhance public accessibility to family planning and other relevant services, besides 90 ambulances for different taluka and district hospitals where services of master trainers might also be acquired to refresh professional skills of the already serving lady doctors and gynaecologists. The provincial health minister stressed the need for a transparent and foolproof procurement plan for the project. He also sought relevant details from the nursing council about the training programme so as to assess the relevance of the course. The minister underscored the need for an early establishment of midwives training centres across the province and directed Special Health Secretary Dr Abdul Majid to convene a meeting of the Director Nursing and the Pakistan Nursing Council. (Dawn-18, 26/08/2007) Murder of second medical student in 10 days Fear looms at JPMC A second medical student was murdered on the premises of the Jinnah Post-Graduate Medical Centre (JPMC) on Saturday morning despite the beefed up security presence after the killing of a student on 15 August. The incident on Saturday once again triggered violence, causing immense inconveniences for patients and doctors, witnesses and the hospital administration said. Some students also sustained injuries in ‘fresh fighting’ between the supposed rival student groups, forcing the Dow University of Health Sciences (DUHS) to announce the closure of the Sindh Medical College (SMC) for three more days till 30 August. The incident occurred at a time when some semblance of normalcy was returning to the JPMC after closure of its OPDs and emergency wards for five consecutive days following the killing of a third-year student of the School of Physiotherapy ten days ago. On Saturday, a first-year student of the same school was reportedly shot dead in ‘clashes’ after the previously-announced collective “arrival” of activist students of the group at around 10 a.m. Almost all out-patients departments (OPDs) of the city’s biggest hospital looked deserted as the charged atmosphere prompted doctors to stay away from their duty, said an official. Contingents of police and Rangers were deployed after scuffles broke out between the mob and security men. “We were attacked in the presence of eleven mobiles of police and Rangers,” said injured Sardar Wajid The scuffle between the policemen and activists also broke out at the Surgical ICU when a senior police officer arrived there. Rangers rushed to the spot and managed to ‘save’ the officer from manhandling. Hundreds of activists were seen chanting slogans against the law-enforcement agencies. MNA Mohammed Hussain Mahenti, MPA Nasrullah Shajji and Dr Merajul Huda Siddiqi arrived and tried to pacify the situation after holding talks with the LEA officials. 31 After a reported verbal understanding, the LEAs left the JPMC. But a scuffle again broke out when a policeman arrived at the premises in the evening - ostensibly to conduct legal proceedings. The mob attacked him outside the Accident & Emergency ward, forcing him to flee. He fell down in accumulated rainwater after being hit by heavy stone. The LEAs conducted aerial firing to disperse the mob. Contingents of police and Rangers immediately reached the spot. A senior Rangers official, Mr Kayani held talks with the legislator Nasrullah Shajji there. The legislator informed him that two of their men were murdered at this place but they observed patience. But the security men reacted sharply when a stone hit one of them. The Rangers official reminded him of the ‘verbal understanding’ and said that the lady doctors called him on the phone to express fears about their security. He demanded arrest of ‘nominated persons.’ The TPO Saddar also joined the talks and asked the legislator to send someone to lodge a FIR. In rebuttle, the legislator alleged that the police often pick up people without any FIRs. MNA Mohammed Hussain Mahenti said he contacted the CCPO before the previously-announced collective “arrival” of the rival group’s activists on Saturday morning, who then informed him that the TPO was present there to control the situation. (By Imtiaz Ali, The News-13, 26/08/2007) The repercussions The road leading to the JPMC was closed for traffic and the LEAs only allowed those who were carrying identity cards of the hospital to enter. The National Institute of Cardio-vascular Diseases (NICVD), National Institute of Child-Health (NICH) and the Kidney Centre are also located in the area. The closure of the OPDs, the emergency ward and the road itself, caused sufferings for the patients. A man told The News that his brother, Mohammed Akram, was injured in a road accident in Site and sustained head injuries. He said he had come from Hyderabad to inquire about health of his brother whose whereabouts were not known. A young man who returned from the emergency without getting treatment for a frail woman he was accompanying said that he would now go to private hospital. A young woman who had brought her ailing mother for treatment said that they had come from a far way place and asked why the emergency was closed. “The doctors and paramedical staff were present but they were reluctant to treat the patients out of fear,” said deputy director Dr Seemin Jamali. (The News-13, 26/08/2007) 4 major hospitals ‘cordoned off’ after another 1st-yr med student shot dead KARACHI: Hundreds of patients were denied access to the four major hospitals on Rafiqui Shaheed Road that was cordoned off from both ends by the Rangers and police after a first-year medical student was shot dead Saturday morning. Five other students were injured in clashes between the Punjabi Students Association (PSA) and Islami Jamiat Tulaba (IJT), two rival student organisations. Just ten days earlier another student was beaten to death in a similar outburst at the hospital. The shooting took place at about 10:00 a.m. and according to the hospital administration, IJT activist Farhan Butt was shot in the chest. He hailed from Jhelum, Punjab, and was a School of Physiotherapy student. Five other medical students - Sardar Wajid, Javed Iqbal, Fayaz Alam, Ahmed Ali and Faisal Azeem – were injured badly when the two groups attacked each other with stones and iron rods. Three of them are said to be in critical condition. Heavy contingents of Rangers and police forced the JPMC administration to close down the emergency ward and OPD. Patients had to be moved into the wards as tear gas shelling and baton charge were used outside to disperse the angry crowds of students. The IJT blamed the PSA. Not a single person was arrested nor was a case filed by the time this report was filed. “It will take little bit time to lodge the FIR, as the relatives and party workers are busy with the funeral,” TPO Saddar Capt. (retd) Tahir Naveed told Daily Times. “They have not been identified and as it was a clash between two rival groups and everyone claims to be right, any arrests will lead to more tension,” he argued. He rejected allegations that the police had forced the JPMC administration to shut down the emergency, OPD and the main road. “At the time of the incident there was firing, so we just blocked the road for 10 to 15 minutes and after that we opened it for the general public,” he maintained. There are four major hospitals on that road - Jinnah Postgraduate Medical Center (JPMC), the largest state-run hospital of the province, the National Institute of Child Health (NICH), the National Institute of Cardio-Vascular Diseases (NICVD) and the Kidney Center. Till late afternoon, the Rangers did not allow vehicles through and patients were forced to walk from Shahra-e-Faisal. Several attendants were seen carrying elderly patients on their shoulders and walking to the hospital. Due to the violence, several operations at JPMC and NICH were canceled, as a large number of doctors and paramedics were unable to reach work. The number of admissions to these hospitals fell. Jinnah hospital’s 26 OPD clinics were forced to close and hundreds of patients had to return home without being seen. The duty officer at the emergency ward at the 32 children’s hospital told Daily Times that only 52 patients made it to their emergency ward but usually the number touches 300 on an average day. The doctor in charge at the NICVD said that they had only admitted 63 patients by 4:00 pm but usually received more than 150. The presence of the Rangers jawans and police caused panic in the area as well. Drug stores and grocery shops were closed as well. Slogan-shouting IJT activists gathered at the JPMC causality to receive the body of their colleague. MMA Deputy Parliamentary Leader in the Sindh Assembly Nasarullah Shajji also turned up. “The teargas entered the wards and disturbed the patients seriously,” a JPMC PRO told Daily Times. Many of the patients in serious condition had to leave. “The Rangers and police also opened aerial firing that caused panic among the patients and hospital staff.” The doctors, who were stuck inside the hospital during the entire escapade only managed to return home late, exhausted and with some of them suffering from asthmatic reactions to the tear gas. The angry students entered the casualty where they damaged machinery. JPMC moved 16 critical patients. In the evening, Jinnah hospital director Rasheed Jooma met the governor. He declined to issue a statement, however. “The federal government has directed me not to talk to the press,” he told Daily Times before turning his cell phone off. (DailyTimes-B1, 26/08/2007) Pharmacists’ role in healthcare system PHARMACISTS’ role in the healthcare system is rising with the development of new drugs, emergence of new resistant microbes, and the changes in healthcare delivery systems. Pharmacists are the third largest healthcare professional group in the world but they still have a long way to contribute a significant role in the healthcare milieu of Pakistan. Building new pharmacy institutes is the need of the hour; however, they face the serious challenges posed by the country's infrastructure and a shortage of trained staff, but above all they suffer from the lack of a comprehensive pharmaceutical education policy and clear objectives to aim for. While producing more pharmacists is equally important, it is also imperative that, with the increasing number, one expects a change in the medicine use situation in the country. There must be some improvements in how drugs are manufactured, distributed, sold, and used. The weakness in pharmacy education has marginalized the pharmacy profession and hindered pharmacists from consolidating their role. As a result, pharmacy practice has been affected and subsequently poses adverse effects on the country's healthcare sector. There are no independent drug information services at public hospitals and this provides opportunities for drug detailers and medical representatives to disseminate biased drug information to doctors. Medication errors and adverse drug reactions go unreported because of the lack of pharmacy support services. Hence, this is the time for the Ministry of Health (MoH), along with the Pakistan Pharmacist Association (PPA) and Pharmacy Council Pakistan (PCP), to commission a working group that can work on pharmaceutical education, research, clinical practice and policy reforms. Job opportunities for pharmacists should be expanded in all areas of pharmacy practice such as clinical, community, hospital, pharmaceutical management and industry Appointments should be made available for pharmacists in Drug enforcement administration, Department of justice, and in the National Institute of Health. Pharmacists may serve as noncommissioned or commissioned officers in the Army, Navy, Air Force and Coast Guard. ARIF ALI ARAIN, Karachi (Dawn-6, 27/08/2007) Maternity home short of staff and adequate amenities KARACHI, Aug 26: Staff shortages, water availability and disrupted electricity have greatly affected the services of the Korangi Maternity Home, the only government-run health facility in the town. The centre, which also hosts the town’s tuberculosis diagnosis and treatment service, is daily visited by a large number of patients but constant power outages and the unavailability of drinking water add to their woes as they stand in a long, dark corridor awaiting their turn. “The weather is pleasant today otherwise we would not have been able to stand here for so long,” complained one of the women in the queue. “There is no water or electricity at the moment. Not that electricity would have made much of a difference since there is no ceiling fan either.” According to Deputy Town Health Officer Dr Zafar Ali, the electricity problem is critical, particularly during deliveries when the procedure takes place in the light of torches and candles. “These tense episodes could end if we were provided a generator,” he commented. Patients also complained about the facility’s filthy condition and one of them claimed that after a long time, it had just been cleaned before Dawn’s visit. “The place was littered with empty drip bottles, plastic bags, disposable injections and other garbage,” she claimed. One proof of this statement was a small room inside the ward which was full of stained bed sheets and empty drip bottles, giving the impression that these items had been hurriedly dumped there. Dr Ali conceded that the administration failed to ensure cleanliness but pointed out that little can be done to improve the situation since only one sweeper has been sanctioned for the facility. 33 Raising other problems, he told Dawn that the facility is desperately in need of another female doctor. Before the appointment of the doctor who works there currently, the maternity home made do with just a lady health visitor and a staff nurse for two years, he said. Not that there’s a shortage of doctors appointed to the facility, he added. “On paper, there are 12 to 15 staff members including doctors, a pathologist, a radiologist and a dispenser who have been on the payroll for a long time,” he complained. “But they are actually working at other healthcare facilities.” “This problem is not restricted to our facility. There are many health setups in rural and semi-urban areas where the appointed staff is actually employed elsewhere. Transport problems and the fear of poor conditions prevent doctors from working in far flung areas and at times, appointments are soon followed by transfers,” added Dr Munawwar Ali, who has recently taken charge as the facility’s medical superintendent and looks after the Directly Observed Treatment Strategy (Dots) programme. Located in Korangi 2½, the 15-bed maternity home was inaugurated by the then mayor of Karachi, Abdus Sattar Afghani, over two decades ago. It also houses the town health offices on its second floor. Deputy THO Dr Ali explained that the city district government has not provided them with office space yet and they intend to shift as soon as possible since the floor is was originally meant to house an operation theatre. “We need an operation theatre and more female doctors,” he said. “A request in this regard has been sent many times to the high-ups, but to no avail.” Currently, the over 70 normal deliveries performed every month are managed by two staff nurses, three lady health visitors and four midwives working in shifts. Dr Sadia Khayyam, the only lady doctor, leaves by 2pm. “I am not on call and only attend to patients in the morning,” she asserted. “The staff here is extremely competent, more experienced than many doctors.” She added that there is no problem in referrals and that a Sindh government hospital is located nearby while high-risk cases, including first pregnancies, are sent to either JPMC or Civil Hospital Karachi since there is no operation theatre, incubator, ventilator, nursery or paediatrics section here. She pointed out the poverty, the lack of education and awareness about family planning are major impediments to improving women’s health. She referred to a 40-year-old woman who was undergoing an examination for her 10th pregnancy and said that multiple pregnancies are common despite the influx of so much relevant information on the media. “Pregnancy at an older age risks both the woman and the baby’s life,” she commented, “but we can’t lecture this woman now lest she goes to an unskilled midwife.” Though the administration claims that TB is more common among women in the reproductive age bracket, they have nevertheless kept no records of expectant mothers with TB. “I can’t give you the exact figures but I can say that four to five pregnant women afflicted with TB come every three months for delivery,” said Dr Zafar. “Special precautions are needed for such cases since TB is an air-borne infection. We provide free treatment and all babies are vaccinated against TB when they are born.” Women are considered more vulnerable to the disease because of malnutrition, poor sanitation and over-crowded living environments. In view of the increasing numbers of hepatitis and TB patients, Dr Zafar feels that the government must introduce screening for TB, hepatitis and HIV/AIDS at all health facilities. The maternity home is also badly in need of renovation. Though charges for antenatal checkups, vaccination and ultrasounds are nominal, many patients claimed that their relatives paid Rs600 instead of the Rs100 official charges for a delivery. About this malpractice, the administration maintained that patients don’t lodge an official complaint and are often found admitting that they gave extra money to the nurse of their own free will. For equipment sterilisation, Dr Zafar claimed that there is an autoclave which they said is locked up. When this scribe insisted on seeing the machine, a staff member confessed that actually, a boiler is used for this purpose. While the city government plans to spend a huge amount of money on various health projects in the city, one feels that a wiser step should be to pay attention to the existing facilities that are failing to meet their objectives. (By Faiza Ilyas, Dawn-13, 27/08/2007) One dies due to situation at JPMC A thin attendance of doctors and other staff was witnessed at the Jinnah Postgraduate Medical Centre (JPMC) on Sunday following the murder of a medical student and the subsequent violence on Saturday. Patients visiting the JPMC on Sunday were advised to go to the Civil Hospital for treatment where an emergency had been declared to entertain patients with severe complications, the hospital sources said. Sources said that a patient with serious complications was brought to the hospital from the DHA and the hospital attendants advised them to take him to the Civil Hospital for proper treatment. However, he died before be could be taken to the Civil Hospital as he was unable to get oxygen. A doctor at the Emergency Ward of the Civil Hospital told The News that they received some patients who had been referred there by the JPMC. Dr Seemin Jamali, in-charge of Accident and Emergency Ward of the JPMC, said the mob damaged sensitive equipments (ACG machine, BP operator, screen operation etc) of the Emergency Ward in Saturday’s violence. The equipment had been bought with the assistance of philanthropists. She said the Emergency Ward of the hospital is under construction through public-private partnership and wondered if such destruction on the part of the miscreants continued how the philanthropists would extend their help. She refuted the reports that the doctors have been verbally asked not to turn up on duty because of the tense atmosphere in the hospital. One doctor said as fear looms large at the JPMC, many doctors were reluctant to perform their duty. Dr Kaleem Butt, Medical Superintendent of the Civil Hospital said they have declared the emergency at the hospital and extra staffs have been deputed at the casualty and other departments to meet any eventuality. Extraordinary security was seen at the JPMC on Sunday. (The News-13, 27/08/2007) 34 ‘Ambulances can get only 550 out of 750 patients through’ KARACHI: Only 550 out of 750 calls could be answered by ambulances because of the massive traffic gridlocks according to data from two months ago, Faisal Edhi of the Edhi Foundation told Daily Times Sunday. The four hospitals on Rafiqui Shaheed Road – NICVD, the Kidney Centre, NICH and JPMC – become inaccessible for ambulances in particular. Edhi explained that old city areas as well as the intersection at Regent Plaza on Shahrah-e-Faisal leading to the four hospitals are where dozens of ambulances face problems each day. It gets worse during rush hour, he added. “If the traffic police paid attention to their duty, the problems would go down,” he said, putting the number of patients dying on the way to hospital in the hundreds each month. Edhi suggested that the traffic police introduce the Junction Box system as is used all over the UK and the US. “This system should be implemented at every roundabout in the city,” he said, adding that the traffic police should quadruple ‘token money’ but give concessions to motorcycle riders. The previous city government had proposed an underpass at the intersection of Regent Plaza on Shahrah-e-Faisal. “If the present city government adopted the idea of an underpass at this intersection, the traffic flow at Shahrah-e-Faisal will smoothen out,” a city government official suggested but on the condition of anonymity. There is also a perception that these problems will persist unless the city government or any other stakeholder, including the Karachi Cantonment Board and Pakistan Navy do not come forward to help. The government is cognizant of the fact that the four hospitals in a row on Rafiqui Shaheed Road suffer. Last year, the governor had announced that they would revive the route passing through Bizerta Lines behind Ayesha Bawany School to JPMC. (DailyTimes-B1, 27/08/2007) What happened that day at Jinnah hospital was really ‘sick’ KARACHI: It felt as if someone had set chilies on fire and the vapour had filled the air, recalled 65-year-old Sher Mohammad, an Edhi ambulance driver for 17 years, who has yet to recover from the tear gas shelling. From behind the grille of the Edhi office at Jinnah hospital, Sher and the other drivers watched the Rangers and police shake down the protesting students Saturday. “All of a sudden the tear gas filled the air. I can’t see now, therefore I haven’t been able to drive the ambulance for two days,” he said. Sher Mohammad was not the only person to suffer on Saturday when another first-year medical student was killed in violence that broke out between two student groups outside the Jinnah hospital casualty. Haleema Khatoon Kumbhar, a resident of a small village near Kot Ghulam Muhammad (old Jamesabad), lost her sevenyear-old daughter for more than eight hours during the mayhem. “From the morning there had been rumors that a very big fight had started between two political parties inside the ward,” she told Daily Times. “There were no doctors and even the chowkidar was absent.” Haleema had been looking for the channa seller around the main building when the violence broke out. Her daughter Maria had been hungry and wanted something to eat. “All of sudden, a herd of people entered inside the only open gate of the main entrance, as there was fire outside,” she recalled. Haleema and Maria also started running but somewhere along the way Maria slipped away from her mother. “I was unable to stop and look at what happened because people were running all around the place.” It was only the evening that Haleema found Maria with another attendant in the main waiting hall. The law enforcement personnel were disgusted with what they saw. “They are meant to be students and doctors of the future but they fight and create problems for us,” a policeman told Daily Times. That day he and the other police couldn’t find anything to eat the whole day as they were on duty. “I wish I could have opened fire when a group of students started screaming ‘Wardi behind terrorism’ in front of us, but I couldn’t,” said a Rangers jawan, who has been posted there for the last three days. JPMC is still heavily guarded. “Contingents from different police stations - Preedy, Mithadar, Kharadar, Saddar, Jackson, Dockyard and Defence – have been deployed here for the last two days, disturbing the routine work of all these stations,” a police official from Mithadar, Liaquat Ali Jat, told Daily Times. (By Amar Guriro, DailyTimes-B1, 28/08/2007) Plan for govt doctors shelved ISLAMABAD, Aug 28: The federal cabinet has shelved a plan for institution-based private practice of doctors in government hospitals owing to an expected adverse reaction from the country’s doctors’ community ahead of elections, it is learnt. Informed sources told Dawn on Tuesday that a recent meeting of the federal cabinet considered a proposal of the ministry of health for institution-based practice of doctors in public sector hospitals that were prepared on the directives of the Supreme Court of Pakistan. A two-member Supreme Court bench comprising Chief Justice Iftikhar Muhammad Chaudhry and Justice M Javed Buttar had taken a suo motu notice of the private practice among doctors of public hospitals. On August 6, the attorney general had informed the Supreme Court that a summary seeking gradual improvement in medical practice had been submitted to the cabinet for approval. He, however, did not inform the court that the federal cabinet had already shelved the summary in its meeting of August 1, 2007. A cabinet member said the meeting discussed the proposal in detail but deferred a decision when some ministers pointed 35 out that lawyers’ community was already up in arms against the government and joining of another influential community like doctors would not be affordable given the fact that election activities were speeding up. He said the ministry concerned apprised the cabinet that the doctors’ community had been consulted on the initiative but some political ministers were too sensitive about the timing. The ministry of health even assured to introduce institutionbased practice as a voluntary scheme but of no avail. The health ministry also stated that the scheme had been designed on the pattern of army hospitals and would be beneficial for the general public and also for the medical professionals and hospitals. The converse view was that almost all hospitals are facing the problem of shortage of beds and there are capacity constraints. The cabinet was informed that this practice was earlier tried in the NWFP but failed when most of the A-grade doctors left their government jobs. Some of the members said the proposal had several implications and timing was not right to introduce it.After detailed discussion it was agreed that the timing for the implementation of these proposals was not conducive. Informed sources said the doctors’ community and the ministry of health had agreed to introduce the scheme for regulating the private practice of public sector doctors and offer wide-ranging facilities and diverse services under one roof to the general public. The health ministry claimed that revenue generation through institution-based practice could be used for improving health facilities at hospitals, enhancing the income of doctors and re-gaining the public trust in government hospitals. They had also agreed to introduce the scheme in a gradual, phased and voluntary basis, starting with Pakistan Institute of Medical Sciences (PIMS) at the federal level and one each tertiary hospital in all the provinces. Under the scheme, the entire revenue was to be shared by the doctors and hospitals on 50:50 basis. In Punjab, institution-based practice is already in vogue in two hospitals -- Sheikh Zayed Hospital, Rahimyar Khan and Punjab Institute of Cardiology, Lahore. A rule that barred the government hospitals from directly utilizing this revenue was, however, seen as a legal hitch and the ministry of finance was not ready to given away its authority of controlling revenues. During the hearing the CJ observed that except Pakistan almost every country including India had legislation on institution based private practice and referred to institutions like the Aga Khan University Hospital and Combined Military Hospital (CMH) and the Military Hospital (MH) which have allowed such practice. Earlier a committee under the Inspector General (Hospitals) Ministry of Health after consultations with the provincial health secretaries, the Pakistan Medical and Dental Council (PMDC) and the Pakistan Medical Association (PMA) had recommended a phased institutional-based private practice after normal hospital hours. They had agreed that utilities should also be made up from the hospital share and the utilisation of revenue/income should be monitored in each hospital by a vigilance committee. (By Khaleeq Kiani, Dawn-1, 29/08/2007) Report highlights sorry state of women’s health in Sindh The state of women’s health is dismal as compared to their counterparts because of the negligence in this regard based on the notion that men are the primary bread earners. Besides this, healthcare is either expensive or not easily accessible, especially in the rural areas. The gloomy situation was pointed out in a report prepared by the Sindh government about women’s health and working conditions. Inadequate and out-of-reach primary and reproductive health care services, poor family planning, nutrition and education, etc, are major factors behind the sorry state of women’s health and healthcare according to the report. Marriages girls who are minors, resulting in early child birth, means that they face extraordinary sexual and reproductive health issues, said the report, adding that infant mortality rate is high in Sindh. Untrained midwives deal with the labour process in the rural areas and a shortage of health facilities prompts people to go to Attai Doctors (quacks), Aamils (spiritual healers) and Dargahs (mausoleums of saints) for the treatment of their ailments. Mental illness remains a seriously neglected area and women suffering from emotional disturbances are taken to persons who deal in exorcism. Highlighting the role of women in Sindh’s economy, the report revealed that women have been playing a vital role in the economy as farmers, workers in the informal sector, employees in manufacturing, industries, the service sector and as home-based women workers. “They comprise the invisible workforce,” the report said. It added that since women’s efforts are not recognised formally and hence cannot be quantified, they are thus in a disadvantaged position as their rights are also not formally recognised. They are not given any representation in economic decision-making forums and their access to credit, formal labour markets and land ownership is also limited by social constraints. These factors, pertaining to mobility and social attitudes, hamper their development. The report expressed concern over the virtually nom-existent allocation of funds for mother and child health in Sindh stating that the federal government has allocated Rs2 million, Punjab Rs40 million and the NWFP spends Rs13 million, for the same. Balochistan is the only province that made some relatively reasonable expenditure of Rs100 million for the mother and child. The report also criticise the uneven distribution of hospitals and health facilities. In Karachi alone, the four largest hospitals are concentrated in a particular area. It added that the status of a woman is linked to her marital role and her nuclear family, hence protecting the virginity of adolescent girls is considered of the greatest concern to her family, leading to increased restricted mobility and segregation. (By Imtiaz Ali, The News-13, 29/08/2007) 36 Gulistan-e-Jauhar in need of rescue against water-borne diseases Water-borne diseases, in particular gastroenteritis, has been reported from various parts of Gulistan-e-Jauhar where overflowing sewerage has entered many apartment buildings. The sewerage has been seeping into the courtyards, as well as into the underground water tanks, residents complained. Parents were worried about their children’s and their own health, as the water supply, too, is highly contaminated. Many children have been treated for stomach-aches and skin rashes. The worst-hit residential complexes are parts of Haroon Royal City, Noman Grand City, Arif Pride, Rufi Heights, Shumial Arcade, and Ahmad Comforts in Block-17 of Gulistan-i-Jauhar. The stagnant sewerage water has also provided a breeding ground for mosquitoes, carriers of malaria, and other diseases. Some GPs of the area warned residents not to use the water stored in their underground tanks and instead purchase the purified water in containers. It has been more than a month since the city government hurriedly dug up the place for laying another sewerage line. However, after fabricating the structure of the manholes, the work force has disappeared and does not seem to bother about the filth that has accumulated all over due to lack of outlet connections for sewers from different apartment buildings. Residents say they tried to seek a remedy from the city government and the Faisal Cantonment, since parts of Gulistan-eJauhar is under this Cantonment, but no one seems to be ready to come to their rescue. Both the agencies were holding the other responsible for the plight of the people. Because of the contaminated water many residents have shifted to their relatives’ or friends’ homes but those without this option are left languishing there. The other problem the residents are facing, for almost eight or nine months now, is the presence of excessive dust in the atmosphere, which is causing respiratory problems. The problem as also affected the school-going children who have to wade through the clouds of dust to board the school van every morning. On the pretext of development work, Gulistan-eJauhar has been turned into something worse than a slum where utility services infrastructure have just crumbled. (The News-14, 29/08/2007) 3 brothers and buddy burnt by firecrackers KARACHI: Four children, three of them brothers, were burnt Tuesday night within the limits of the Liaquatabad police station while playing with firecrackers. The three brothers, Yasin, Hamza and Usama, and a friend named Asif, all between the ages of seven and nine, were rushed to Abbasi Shaheed Hospital from where they were referred to the National Institute of Child Health (NICH). They were admitted there in critical condition. Millions of rupees were spent on firecrackers for Shab-e-Barat. Burfi, kalashan patti, China bomb, rani bomb, citi bomb, flier bomb, aao pyar karain are the best sellers. “I’ve been doing this work for the last ten years,” said Shahrukh. “Shab-e-Barat is my big payday.” He did admit that it was wrong but explained that “a job is a job” and other people are also doing it. “If we don’t cooperate with the police then how can we run our businesses? The police know everything that is going on around them. Money is a big thing and that’s why business continues as usual.” Police from different stations have arrested around 20 people and have recovered over 10 million rupees worth of fireworks and firecrackers during the last ten days. Chief of Police Azhar Ali Farooqui said that the police just decreased the activity; they didn’t eradicate it because they have a lot of other matters to attend to. “It is not a major issue for the police,” he said. To a question, he said that it cannot be outright denied that police officials are not involved. A policeman of Gulberg Town told Daily Times, “The people that don’t have any sense do it. Our police took some people, including children, into custody. We have to release the children because something like this can affect their careers. Sure if it was a professional criminal we would hold him but children are children. How can we arrest them?” Khodi Garden, Joria Bazaar is the biggest wholesale market of fireworks and firecrackers. (By Faraz Khan, DailyTimes-B1, 29/08/2007) Doctors worried about possible cut in ties between JPMC & SMC KARACHI, Aug 30: The Sindh government must look into the threat of a possible disaffiliation of the Sindh Medical College (SMC) from the Jinnah Postgraduate Medical Centre (JPMC) and order steps for the creation of a peaceful environment at the public sector medical colleges in the city. These demands were put forward by senior office-bearers of the Pakistan Medical Association (PMA) during a press conference at the PMA house here on Thursday. The General-Secretary of the PMA Karachi chapter, Dr S.M. Qaiser Sajjad, said that the recent spate of violent events at health care facilities, which largely involved students of medicine and other relevant fields, revealed flaws in the teaching and training methods and relevant administrative affairs, which should be taken care of on an emergency basis. Assisted by the PMA’s central general-secretary, Dr Habibur Rahman Soomro, and Dr Aziz Tank of the College of Family Medicine, Dr Sajjad discussed in detail the academic and administrative affairs of the Dow University of Health Sciences’ 37 (DUHS) affiliated institutions and expressed fear that students of the SMC would suffer, if appropriate steps were not taken on time. They were of the view that it was high time the DUHS reviewed the long prevailing relation between the two institutions ie the JPMC and the SMC. The PMA office-bearers said that since the inception of the SMC, its students had been acquiring their clinical education and training at the JPMC. But for quite some time it seemed that the JPMC faculty was reluctant to own these students and was now reported to be considering disaffiliating the college on the pretext of ‘law and order and politicisation of the patient care complex’ due to frequent visits by the SMC students, they said. Dr Sajjad said that the DUHS administration should have properly planned the facilities for the SMC students and interaction between the faculty members of both the JPMC and SMC right at the time of the establishment of the university. As a solution to any possible cut in the relations between the federal government hospital and DUHS, Dr Sajjad suggested that Sindh government-run hospitals located in New Karachi, Liaquatabad, Korangi and Saudabad should be affiliated with the SMC and faculty position be awarded to all those postgraduate doctors working in the hospitals. He said that these four hospitals had already been notified by the government as teaching hospitals and an organised clinical teaching programme could be initiated at these institutes so as not only to help overcome training problems of the medical students but also to provide up to the mark health care facilities to the local population. Criticising the DUHS administration, Dr Sajjad called for the restoration of boarding facilities for students and doctors. Instead of dislodging anti-social elements from the hostels, the varsity administration had deprived all the deserving people of this facility, he said. The PMA general-secretary, also an SMC alumnus, alleged that it was due to the negligence of the university that the SMC students had been isolated in an environment not conducive to learning. He was of the view that the transfer of the faculty in the basic medical sciences at the Sindh and Dow medical colleges to the newly established Dow International Medical College had added to the sufferings of the students of both the institutions. Dr Sajjad said that that instead of planning for further expansion and establishment of new features, the DUHS at the moment should focus on serious issues confronting both the colleges. In reply to questions, the PMA office-bearers said that they understood that the medical institutions and hospitals of the Sindh government were well in a position to absorb the house-job officers of the SMC, posted at the JPMC every year, and also to give standard faculty and facilities to students likely to be dislodged from the JPMC. (Dawn-17, 31/08/2007) SEPTEMBER Govt urged to take steps against rabies KARACHI, Aug 31: Expressing concern over a surge in dog mauling cases in the country as well as in Karachi, experts have urged the government to gear up it efforts for the prevention of rabies. According to health practitioners and environmentalists, around 1.5 million dog mauling cases and 2,000-5,000 deaths from rabies are reported annually in Pakistan. In many cases, people bitten by dogs receive improper treatment either due to a lack of awareness or insignificant response from the government. These observations were made at a press conference organised at the Karachi Press Club on Friday to highlight the issue of rabies-related deaths and World Rabies Day in the city on Sept 8. A number of doctors, veterinaries and chief of an NGO on environment and public health issues expressed their views on the increase in the number of stray dogs, diagnosis and treatment modalities, quality of anti-rabies vaccines, role of municipalities in controlling the population of stray dogs, etc. Leading the conference, president of Rabies in Asia (Pakistan) and a senior infectious disease consultant, Dr Naseem Salahuddin, said that rabies was prevalent in both the urban and rural areas across the country and children were the worst sufferers who were usually bitten on the face, head or neck and often mangled beyond recognition. She said that rabies infection once developed in human bodies ended only with the death of the infected person. Dr Salahuddin also pointed towards the inefficacy of the anti-rabies vaccines produced and distributed by the National Institute of Health, which were largely administered to dog bitten people at government health facilities despite being known for causing severe reactions as well. Stressing the need for cell culture vaccines, she said that the government should make arrangements for the import of those modern vaccines on a large scale as those had also been recommended by the World Health Organisation (WHO). She said that the cell vaccines were highly effective but beyond the reach of the common man due to their high cost. However, the rabies centres established at the JPMC and Civil Hospital were administering these vaccines to patients through some donations. She advised the people that in case they experience or witness a dog bite they should wash the wound with water and soap for at least ten minutes to get the spot cleaned of infection, without wasting any time, and then report to some competent doctor or hospital for vaccination. Dr Qaiser Sajjad, general-secretary of the Pakistan Medical Association, Karachi, said that on an average the major public sector hospitals in the city received 10-12 cases daily. He said that relevant treatment should be made available at all the public sector hospitals round the clock. 38 Shahida Kauser Farooq, the chairperson of Subh-e-Nau, an environment and public health concern, said that rate of increase in dog population was alarming and needed to be addressed by the city government as well. One of the speakers said that the Infectious Disease Society of Pakistan, Subh-e-Nau, and Rabies in Asia (Pakistan chapter) Foundation would be joining countries across the world on World Rabies Day on Sept 8. A walk, to be led by Sindh health minister, will be organised at 9am from Mazar-i-Quaid to Old Numaish and the PMA will hold a seminar at PMA House at 3pm. (Dawn-18, 01/09/2007) Kidney sale THIS is in response to Tanweer Ahmed’s letter, ‘Organ sale’ (Sept 1), advocating ‘legalising’ the trade by providing a health insurance cover to the donors as well as instituting a strict monitoring system. He also suggests that payments should be made to the donor’s bank accounts, perhaps to eliminate the menace of middlemen. There are certain facts that need to be pointed out. First, the term ‘donor’ is incorrectly used in this context because what we are talking about are ‘vendors’, forced to sell parts of their body driven by sheer poverty and not donors who give out of free will without coercive influences. A state-run money-for-kidney programme has been in place for some time in Iran and has now been shown to have major concerns, with an obvious one being that it is the poor who seem to be the only ones losing their kidneys while rich seem to be the only ones benefiting from this arrangement. Mr Ahmed proposes what seems to be robust insurance system for the kidney vendors to take care of them for the rest of their lives. In a country where there is hardly any health insurance system worth mentioning except for the wealthy, to create such a system for the most downtrodden of this country seems a utopian idea. As far as the suggestion for directly depositing the promised amount into the vendor’s bank accounts, many of these unfortunate souls possess what they can wear and carry around. Some have ‘salaried’ jobs which pay a paltry Rs800 a month on which they support not only themselves but their families. Others are not so lucky and are in bonded labour. To think that these people would be managing bank accounts seems rather ludicrous. Money for body parts is an abhorrent concept, call it compensation, appreciation or gift. Paying it in cash or cheque makes it no less repulsive. Various methods of making it kosher have been tried elsewhere and have failed. It is time we stopped trying to legalise organ trade and instead strengthened the hands of those who are trying to fight this menace. DR AAMIR JAFAREY Centre of Biomedical Ethics and Culture, SIUT, Karachi (Dawn-6, Letter to the Editor, 04/09/2007) New victim takes polio cases tally to five KARACHI, Sept 6: With the detection of a polio case in Baldia Town, the tally of confirmed polio cases in Sindh for the current year has reached five, said Dr Salma Kouser Ali, project director of Expanded Programme on Immunisation (EPI), Sindh, on Thursday.She was briefing a group of Unicef and the World Health Organisation (WHO) officials from Geneva and Islamabad led by Dr Rafah S. Aziz, senior adviser to Unicef on global polio eradication initiative, at her office. As many as 12 polio cases have so far been confirmed throughout the country during the year. According to Dr Ali, like four cases which have been reported in Sindh and confirmed by the relevant authorities, the latest case was also imported from outside the province. The case was reported in the mid of August and now has been confirmed by NIH and Geneva lab of the WHO as well, she informed the participants of the meeting. Earlier, one confirmed polio case had been reported from Baldia Town (Karachi), two from Khairpur and one from Jacobabad. According to Dr Ali, the latest victim, four-year-old Akramullah, son of Mairaj, had moved to Karachi from Swat in August. She highlighted the achievements of EPI Sindh in regard to the elimination of the polio virus in the province and also referred to some of the challenges. She also stressed the need for reviewing the current communication strategy and development of province/district specific plans with the involvement of local partners. She added that a lack of trust or misconceptions regarding vaccines among people also needed to be addressed with the support of the media and religious leaders. Dr Ali said that Sindh was all poised to eradicate the polio virus circulation during the year, while all measures had been taken to check the infiltration of the virus. Almost all the cases confirmed so far in the province pertained to children of travellers and migrants, she said. Others who were present during the briefing included Liliane Boualam, a WHO technical officer, Melissa Corkum, Unicef’s programme communication officer at Islamabad, Dr Asif Aslam of the Unicef Karachi, and Dr Laila Rizvi. Later the group visited some nomadic populations in Gulshan Town, where mop-up polio vaccination campaign concluded on Thursday. In the meantime, the Sindh health officials have detected a case suspected of carrying polio virus. According to a source in EPI Sindh, the stool sample of an under-five male child from Thatta have been sent to the authorised laboratory for confirmation of the polio virus. The boy has developed symptoms similar to those affected by the polio virus, but any official version about the status of the case would come only after receiving reports from the National Institute of Health, Islamabad, added the source. (By Mukhtar Alam, Dawn-17, 07/09/2007) 39 Poor hygiene at Korangi hospital KARACHI, Sept 7: While infection control at health facilities is an important concern in the developed world, most medical centres in Pakistan have little or no preventative measures in place. The gravity of the situation can be gauged from the fact that in the US, where the standards of hygiene are generally high, hospital infections affect two million people a year, cost 100,000 lives and add $30.5 billion to the country’s healthcare tab, estimates the Committee to Reduce Infection Deaths. The situation in many of the city’s hospitals is critical. A case in point is the gynaecology and obstetrics department of the Sindh Government Hospital, Korangi No 5. The only government-run hospital in the area, this dispensary-turned-tertiary care health facility is visited every day by a large number of patients, particularly women seeking antenatal checkups, treatment for menstrual irregularities or postpregnancy complications. The gynaecology department is crowded until the afternoon and patients often have to leave without having had a medical examination since the out-patient department closes at 2pm. While this is inconvenient, the patients’ major complaint is the lack of hygiene. “The labour room is filthy,” complained the mother of a woman admitted into the facility for delivery. “There is no dustbin in the ward and there were no sheets and pillows on the bed when my daughter was admitted. They were only provided when we complained. Similarly, the washrooms are very dirty, there are no utensils and most of the taps have been stolen.” An inspection of the delivery room proved her contentions. The floor was stained with blood and a bucket serving as a waste-bin was full of used cotton swabs. There is no water supply and a small container is used instead as a temporary arrangement. Furthermore, the room lacks a baby warmer, which is essential to help newborns adjust to the temperature change. In defence of the pathetic state of the delivery room and the ward, the facility staff said merely that the building was being renovated and an additional block equipped with better facilities has been constructed, to which the gynaecology ward will be shifted within a month. However, they complained, the functioning of the department is seriously hampered by theft. “Taps, fans, stethoscopes, a blood pressure examination machine and even delivery sets have been stolen. At the moment, we have just one set with which we carry out over a dozen deliveries a day,” said a nurse. According to another source, the hospital uses the household antiseptic Dettol for sterilisation purposes. “An auto-clave is the best way to sterilise equipment but if that is unaffordable, a boiler or even a chlorine solution can be options,” said the source. “A household antiseptic cannot possibly serve the purpose.” Frequent power outages are a major impediment in the functioning of the operation theatre, which is opened only for planned surgeries. The rented generator often malfunctions and causes delays during surgeries, with the result that the facility refers complicated cases to the Jinnah Postgraduate Medical Complex or the Civil Hospital Karachi. The electricity breakdowns also mean that patients are sent elsewhere for ultrasound scans and other tests. “This becomes quite costly but since the doctors give us a patient hearing and we feel comfortable, we tend to ignore such lapses in service,” agreed most of the patients. However, they pointed out, the nursing staff at the Sindh Government Hospital demand money for services that are part of their duty, which is unacceptable. The healthcare facility employs 34 staff members, including 10 doctors, some of whom are on call for emergency duty. However, such situations rarely occur since only normal, registered cases are attended to at night. One source claimed that most of the doctors run private clinics in the evenings and are unwilling to work night shifts. The doctors, however, feel that they are doing their best within the limited resources available and express the hope that most of their problems will be solved once they shift to the new block, which awaits an electricity connection. “The hospital is big enough to be a teaching hospital. Over 150 patients visit the out-patient department every day and about 200 deliveries are performed every month,” said Dr Ayesha Sameen and Dr Tahira. “But such a large number of patients can only be treated well if the staff is increased and a better management system is put in place.” (By Faiza Ilyas, Dawn-17, 08/09/2007) Shiraz gets new limbs, courtesy Indian doctor Shiraz, 10, a victim of the criminal negligence of a factory owner in the Sindh Industrial Trading Estate (SITE), has been provided artificial limbs by a team of Indian doctors and now he is able to stand on his feet. Earlier, Shiraz had been fitted limbs that contained steel rods, which made life difficult for him. His new limbs have made him a lot more comfortable. He owes his treatment to Dr Prakash, an Indian, who along with other doctors was invited to Pakistan by Dr Feroz of the National Institute of Child Health (NICH) where Shiraz, Iftikhar and Naveed were rushed after a grave tragedy on Feb 12, 2006. Shiraz suffered severe deep burns in both feet, legs and hands when he along with his friends Iftikhar, nine, and Naveed, eight, strayed into an industrial plot in Abidabad, Baldia Town, Karachi on February 12, 2006, where an unscrupulous industrialist had dumped deadly chemicals. Iftikhar died of severe burns while Shiraz suffered from what doctors call “auto amputatation.” “I went to Farooq-e-Azam Madresah where I studied along with my friends but my teacher was offering prayers. So we went to the ground where we played cricket. We were severely burnt. I screamed and an Afghan rag picker took me out of the dump,” he tells The News. “Now I have artificial legs but I still feel pain. However, I will join my school again and become a doctor,” he says shyly. 40 Shiraz’s father was a driver by profession and has three brothers and three sisters. His eldest brother, Shahzad, 15, has passed the matriculation examination and is determined to continue with his studies. The gross negligence of the culprit would have gone unnoticed had there not been a furore in the print and electronic media that forced the honourable court to take notice of the gruesome incident. The impoverished people of the shanty town Abidabad formed an “action committee” under the leadership of two young men, namely Nawab Ali and Noor-ur-Rehman and filed a petition in the Sindh High Court to seek justice. The case is being pursued by a young lawyer Faisal Siddiqi, pro bono. The respondents include Farooq Gharib, chief executive, Gharibsons (Pvt) Limited who owns Plot F-620 and F-621, SITE Town, Karachi, where the chemical waste was dumped, as well as the managing director, SITE. Farooq Gharib, a chipboard manufacturer is the main accused but he is on bail. Shiraz’s family has been completely devastated by the tragedy. His father, Ali Sarwar, has lost his job and now works as a daily wage earner at Ghani Chowrangi, Shershah. “I have been told that Shiraz will not be able to walk for 15 years but I will make sure that he continues his studies. The education of my other children has also been affected due to Shiraz because his elder brother had to continuously stay with him at the hospital,” says Sarwar. “I owned a small house that has been sold. I am an affectee of the Tarbela Dam and also had a piece of land in my village but that too has been sold for Rs120,000 to bear the expenses of Shiraz’s treatment. Sometimes Shiraz needs two injections daily that would cost Rs10,000. Now I am bankrupt and live in a rented house,” he says. “SITE Limited gave us Rs150,000 as compensation but that too has been spent on Shiraz’s treatment,” he says. Mercifully, the court of law has been kind towards Shiraz. A three-member bench of the Supreme Court headed by Justice Nawaz Abbasi and comprising Justice Hamid Ali Mirza and Justice Ghulam Rabbani recently dismissed two appeals by Farooq Gharib, owner of Gharibsons(Pvt) Limited as not pressed. The accused went into two appeals in the Supreme Court after it directed the investigative officer to proceed against him in accordance with the law. Munir A. Malik, president, Supreme Court Bar Association appeared for Shiraz and arguments were heard and both appeals were dismissed as ‘not pressed.’ Malik fought the case of the victim pro bono. (By Shahid Husain, The News-14, 09/09/2007) Manghopir maternity home victim of neglect KARACHI, Sept 11: While the lack of facilities is a major reason why so many government healthcare units fail to operate round the clock, there are instances where administrative compulsions, bureaucratic hurdles and lack of interest on part of the officials concerned impede the provision of health services. The Manghopir Maternity Home, situated in Site Town, is one such case. Built more than two decades ago, the maternity home has recently been renovated at a cost of Rs7.5 million through an MPA’s funds. The Unicef, too, has extended its support and under its project, the Women’s Right to Life and Health, provided two midwives and assisted in establishing a well-equipped labour room and a midwifery school. But, despite having these facilities, the maternity home has failed to function properly. Few women visit the facility and fewer still opt for delivery. “This is because the maternity home has remained temporarily dysfunctional many times in the past. Though at present two doctors are working here in the morning, there were times when this facility was without any doctor and those appointed were quite irregular. The officials concerned are not serious about making this health facility fully functional, which is evident from the fact that they have stopped two midwives, appointed under the Unicef project, from working,” says an official requesting not to be named. Under the Unicef project, the maternity home has been provided with labour tables, trolleys, a baby warmer and surgical equipment. Expensive machines such as an incubator, an autoclave and X-ray and ultrasound machines bought with MPA Fareeda Baloch’s funds are all lying covered in a room. The situation is deplorable considering the fact that there is no government hospital in Site Town, having a population of more than 0.7 million. The government health facilities in the town comprise only two maternity homes; the other being closed for renovation. This pathetic situation does require immediate corrective measures by the government, but more appalling is what the girl students are facing at the so-called midwifery school opened here three years ago. The midwifery school “What we have got in the name of a midwifery school is a classroom, a book and an administrator-cum-teacher. At times, we are thrown out of the classroom when a workshop is to be held here. For clinical training, students are sent to the Sobhraj government hospital, and for passing exams they have to take notes from girls studying in other schools,” a student complains. The students have a host of other requests to make, including the installation of a water filter, payment of stipend and provision of proper furniture for the classroom. What is strange, however, is the fact that the 14 students who have been enrolled here for over eight months have never been given an opportunity to observe a delivery at the maternity home. 41 Explaining the reason for it, Town Health Officer Dr Moosa Memon, who looks after the maternity home, says efforts are under way to make the maternity home fully functional and till that time students have more opportunities to learn at hospitals such as the Sobhraj, Qatar and New Karachi hospitals, where a large number of deliveries are performed daily. “Erecting a concrete structure is not the end and we do realise that the health facility needs to be fully functional. The renovation is near completion and soon we will embark on a plan to hire more staff,” Dr Moosa Memon says, adding that he is also aware of the problems students are facing and something will be done about them soon. For the executers of the Unicef project, the Manghopir Maternity Home experience has been a huge disappointment. The project initiated in 2002 has failed to bring about any improvement in the health status of women in the locality, according to Dr Shershah Syed, who heads the WRLH project in Sindh. “There is nothing to boast of. The government is non-cooperative which is why we failed to bring about a change for the better. The midwifery school is in miserable shape since there is no teacher there. “We want to continue our support, but if the conditions persist, we will prefer to invest our energies in an institution where people are willing to work,” Dr Syed says. (By Faiza Ilyas, Dawn-18, 12/09/2007) Smoking on the rise among future medics KARACHI, Sept 11: A study conducted at three of the country’s medical colleges has shown the high incidence of tobacco use among future medics, despite their having adequate knowledge about the health hazards involved. Published in the August issue of The International Journal of TB and Lung Disease 2007, ‘Smoking habits and beliefs of future physicians of Pakistan’ was conducted between March 2004 and July 2005 by a group of Aga Khan University (AKU) students. A total of 1,029 students from AKU, the Dow Medical University and the Khyber Medical College (Peshawar) participated in the survey. The study concludes that the overall incidence of smoking lies at 11.2 per cent; 22.4 per cent of the male respondents are smokers against 2.1 per cent of the female. Smoking was found to be more prevalent among men, hostel residents and first year medical students. The mean age at which respondents started using tobacco was found to be 17, ie before they started medical school, and the average number of cigarettes smoked per day was 7.5. Of the total respondents, 22.4 per cent reported having used tobacco at some point and almost half had tried to quit. Most of them smoked filtered cigarettes. The study states that research over the years shows that tobacco use among medical students has increased in Pakistan; by contrast, studies from the US and Australia show decreasing rates. Most students – 80 per cent – agreed that smoking increases the risk of lung cancer and is implicated in coronary artery disease. Having a good personal health emerged as the major reason for not smoking. The majority believed that passive smoking was harmful and were generally supportive of legislative measures to reduce tobacco use, such as restricting smoking in public places and the curbs of the sale of tobacco to children. A lesser but nonetheless significant number thought that there should be a complete ban on tobacco advertisements and that the prices of tobacco products be increased. Interestingly, most smokers proved quite confident about their ability to quit, with about 36 per cent believing that a family member or friend could help them in this regard. A much lower number responded in favour of the influence of a health professional or religious leader. The study found that though smoking was less common among final year students than first year students, the imminent graduates smoked an average of 11.5 cigarettes a day against the 5.60 among first year students. Doctors, the study notes, have so far been unable to act as role models for the general public to quit smoking and in fact, a 32 per cent smoking prevalence was reported in a study on house-officers. It suggests courses on tobacco awareness to help prevent medical students from starting smoking. The study also states that smoking is on the rise in developing countries, including Pakistan. A recent National Health Survey of Pakistan puts the overall prevalence of smoking at 15.2 per cent, 28.6 per cent in adult men and 3.3 per cent amongst women. Disturbingly, a smoking rate of 55 per cent was reported among adult men in a recent study conducted in rural Sindh. ‘Smoking habits and beliefs of future physicians of Pakistan’ was conducted by Haq Nawaz, Sardar Zakria Imam, Ali Bin Sarwar Zubairi, Aqil Hussain, Yasir Jamal Sepah and Mohammed Islam under the supervision of Dr Javaid Ahmed Khan, section head of Pulmonary and Critical Care Medicine, AKU. (Dawn-17, 12/09/2007) Steroid injections for cows endanger human lives The milk from cows injected with steroids may cause low immunity level in humans, leading to several diseases. Such animals are given steroids so that they can produce more milk. Also, steroid injections are known to speed up the process of fowl or calf birth in animals. Several cattle pen owners use this unnatural method to increase their profits. Sadly, this also leads to low infertility among cows and buffaloes. Generally, the owners of cattle pens inject 2cc of steroids in buffaloes twice a day. This injection is available in markets for Rs10-12. It increases the body temperature of buffaloes, as a result of which the milk discharge is quicker. However, the animals stop giving milk when the effect of the injection wears off. Moreover, this is practiced on those cows whose newly-born calves are separated from them so that the milk production is high. The calves are sold in Kutta Market situated in Buffalo Colony (Bhains Colony), which are then slaughtered and sold to restaurants. Their skin is sold at high prices. 42 The Secretary General of the Pakistan Medical Association (PMA), Karachi, Dr Qaisar Sajjad, says that these injections affect humans also when they drink this milk. For one thing, the immunity level decreases when the steroid-treated milk is consumed consistently. Ailments such as flu, hair loss, obesity, high cholesterol level and sometimes kidney failure are the most common result of this. Furthermore, Sajjad said that “there may be problems in deliveries as well and that this practice is slow poisoning for consumers. He added that such milk may also cause early maturity in children. The veterinary surgeon, Dr Isma Gheewala, presents a different side to this issue. According to her, cows are unable to produce naturally because when their calves aren’t present, their bodies are unable to produce the hormone which stimulates the milk-producing glands. Therefore, injections of the hormone oxypocin are used to stimulate their pituitary glands. She said that, generally the effects of the injection last for only two hours. The procedure is not used unnecessarily because it is not how one can get more milk. She maintains that the injections have no side effects on animals. (By Qadeer Tanoli, The News-20, 12/09/2007) ‘NED couple died from poisoning’ KARACHI, Sept 13: A newly-married couple, found dead in mysterious circumstances the morning after their wedding, was poisoned, the results of chemical reports established on Thursday. Traces of poison were found from the viscera of Mohammad Azeem and Beenish, both graduates of NED University, sources close to the chemical lab told Dawn. A senior police official requesting anonymity said that “from the beginning of this case we were of the opinion that it’s an inside job. Now the results of the chemical report suggest that either some family member or a friend could have been behind the poisoning.” “Police will now act in accordance with the results of the chemical report and the arrests of some family members or friends of the slain couple could not be ruled out in a day or two,” a senior police official remarked. Mohammad Azeem and Beenish were found dead the morning after their wedding night in their apartment in North Nazimabad on August 11. As the investigation picked up pace following the incident, DIG Zone West Falak Khursheed had remarked that “it is no outside job, but seems to be someone close to the couple who could be behind the murder.” Earlier police were considering another possible scenario which suggested that for some reason the groom could have killed the bride and later on consumed poison. Hospital sources who had examined the bodies said that Beenish died at approximately 6am while Azeem passed away at around 10.30am. He was rushed to the Imam Clinic by his friend Ghayur along with Azeem’s aunts, where he was pronounced dead. They then took him to Aga Khan Hospital from where his body was shifted to Abbasi Shaheed Hospital for a post-mortem examination. Sharing some findings a police official preferring anonymity said that spectacles were found from the bedside table of the couple’s bedroom. It remained a mystery as to whom the glasses belonged and throughout the questioning of different family members no one claimed ownership of the glasses. Finally Beenish’s paternal uncle Razzak admitted that the spectacles belonged to him and he had earlier preferred to stay quiet. Furthermore, an eyewitness named Babar, a neighbour of the groom’s parents who helped the family shift the bodies, told police that he saw two glasses half-filled with ‘Energile,’ an energy drink, placed at the couple’s bedside table, the police official added. For the last two years Azeem was working at Siemens along with Ghayur, while Beenish and Zainab were the only two females in his batch of 40 students at NED University. Mohammad Azeem has three sisters and eight paternal aunts who, according to the family, practically raised him. Beenish, on the other hand, has two paternal uncles, Razzak, an employee in a local bank, and Imran, an engineer based in Islamabad. Background interviews further suggest that an altercation occurred during the photo session at the marriage ceremony and Azeem’s aunts boycotted the session, but a patch-up was made in the early morning. (By S. Raza Hassan, Dawn-17, 14/09/2007) People, encroachers also block ambulance movement KARACHI: While traffic jams have been plaguing the city, people who deal with patients and ambulances have complained that people in general, the citizens of Karachi, are part of the problem. There are encroachments around the entrances to hospitals such as Civil Hospital and drivers don’t always give way even if an ambulance’s siren is screaming behind them. Ambulances transport about 500 to 700 patients every day. “Citizens don’t pay any attention to the ambulances in this city. And the police also helps people create difficulties for us,” Edhi ambulance driver Muhammad Aslam complained. To reduce the loads on these hospitals, chief volunteer of the Edhi Foundation Faisal Edhi has suggested the government establish fully equipped trauma centres and emergency wards on the Super Highway, National Highway and the RCD Highway. Faisal told Daily Times that it takes Edhi ambulances 1.5 hours to get to Civil hospital from Liaqutabad - it used to take about 30 minutes. The delay in opening I. I. Chundrigar Road, the three lanes of parking on Bundar Road and the massive traffic jams in Saddar, Lyari and Keamari are creating a lot of problems for Edhi ambulances. 43 He disclosed that recently the government has planned to establish a major hospital near Ojha Hospital on University Road. “If the government is serious about it then that would be really good and would reduce the load on the major public sector hospitals,” he said. Karachi is a cosmopolitan city and the few major public sector hospitals are not enough for the citizens, he said. “The city needs more than 120 trauma centres in different places so volunteers can get patients there immediately,” he said. Civil Hospital Karachi is the second largest public sector hospital of the province after JPMC with 1,780 beds. “Most of the patients who come to the casualty department are in critical condition because they’re late,” a doctor at the causality ward of Civil hospital told Daily Times. He said that in 24 hours, 500 to 700 patients involved in road accidents, firing incidents and others are brought in but most of them are in critical condition. Furthermore, when ambulances turn in to Civil hospital’s casualty, they face even more difficulty because the road is full of illegal encroachments in the form of pushcarts, taxis and rickshaws. “I left my Tower office to go to Civil hospital for a meeting with doctors at 1:00 p.m. and I got there at 2:15 p.m. You can imagine just what kind of condition the road is in to be able to increase a 10 minute trip to over an hour,” Anwar Kazmi, personal secretary to Abdul Sattar Edhi, told Daily Times. “As soon as you go inside Civil hospital you’ll find hundreds of motorcycles parked at the main entrance of the casualty department. These bikes belong mostly to hospital staff,” Kazmi said. There are two main entrances to the casualty department of CHK, one from Bundar Road and the other from Chand Bibi Road. The Bundar Road entrance has encroachments and on Chand Bibi Road, the CHK administration has closed the main gate. So no matter which side is used ambulances face difficulties. “On the day of the Hub blast, I really got upset because there were more than fifty ambulances and the illegal encroachers were not allowing anyone to move,” recalled Muhammad Aslam, an Edhi driver at the Edhi centre outside CHK. He said that after the blast the hospital administration had removed all these encroachers but now they’re back. When Daily Times tried to get an official statement from the Civil hospital administration, Dr Hamid, the additional medical superintendent, said, “The medical superintendent is on vacation and I am not authorized to issue any statement. When the MS comes back he will issue an official statement.” (By Amar Guriro, DailyTimes-B1, 15/09/2007) Unhygienic practices put public health at risk KARACHI, Sept 15: The city has a number of roadside eateries besides fruit, vegetable and meat markets in every other locality though hardly any of these take care of hygiene and food inspectors seem least bothered about checking the unhygienic practices. With garbage and rubbish all around, the city not only gives an ugly look but also sees an outbreak of viral infections and other diseases every now and then. The recent spread of conjunctivitis, an eye ailment, is also attributed to the prevailing unhygienic conditions by ophthalmologists. However, the city administration seems comfortable without doing anything about the removal of filth. A visit to the food corners located on Burnes Road (now Mohammad Bin Qasim Road), Shahrah-i-Iraq, Empress Market, Bohri Bazaar, Tariq Road and Hassan Square area shows that several restaurants have encroached upon footpaths, service lanes and pavements by placing chairs and tables on them. The customers are served food there despite the fact that sewage, which continues to gush out from choked gutters, often remains accumulated along the footpaths. Etiquettes and other matters take secondary importance when the food is available at cheap rate to customers. Hence, both the waiters and the customers throw the leftovers on pavements and lanes with ease in total disregard for the environmental concerns. The whole area around such outlets turns virtually into a landfill site littered with leftovers and garbage. Referring to the menace of overflowing gutters in the vicinity of eateries and local restaurants, sources in the Karachi Water and Sewerage Board said that the sewers at such places often got choked because the leftover food along with the discarded crockery were thrown into manholes. They said the manholes near the food outlets were generally uncovered for the very purpose. Unhygienic practices are not restricted to food outlets alone, as meat sellers and fruit vendors too openly flout the mandatory rules of placing nets on the commodities, thus exposing the citizens to serious health hazards. Meat sellers are doing a roaring business in Lea Market, Guru Mandir’s KBN Market, Tariq Road’s commercial area, Federal B’ Area, Liaquatabad Market, Nazimabad’s Gole Market, Karimabad, Burnes Road and at roadside stalls set up in different localities. In Saddar, a large number of pushcarts selling fruits and other eatables have occupied two lanes of Mir Karam Ali Talpur Road, submerged by sewage. (Dawn-18, 16/09/2007) An unholy alliance The debate about unethical practices being adopted by pharmaceutical companies to boost their sales is gaining momentum day by day. Though there is no major objection from any quarter to the promotional schemes of these companies, many view the close relationship between the medical profession and the pharmaceutical industry with scepticism. 44 Pharmaceutical companies are being increasingly blamed for corrupting the medical profession and making lucrative offers to doctors prescribing their products to the patients. The favours that are normally doled out to medical practitioners by pharmaceutical companies include foreign trips with family; costly gifts like watches, mobile phones and cars; furnishing of clinics; and share in the proceeds from sale. There are also reports that many doctors have set up their own pharmaceutical companies, or have bought shares in the existing ones, and are prescribing only their products to patients. Muhammad Ashiq, a medical representative, told TNS that some doctors even ask for a 'share' in the total sales made to their patients. "The staff at medical stores maintains record of these sales as well as of the doctors recommending the medicines. At the end of the week or the month, representatives of pharmaceutical companies consolidate the records collected from all the medical stores selling their products to find out which doctor has helped them how much. The pre-decided 'share' in the total sales is then disbursed to the doctors according to their 'contribution'," he informs. The major reason for the prevalence of such unethical practices is that there is a big difference in the prices of same medicines being sold under different brand names (the Ministry of Health registers and approves the price of each brand of a medicine). Patients and their attendants are normally not aware of this fact, and religiously follow the advice of their doctor. The logic behind the big difference in the prices of same medicines is that some pharmaceutical companies have invested more in research and development, thus their products are priced higher than those of others. A common perception among patients is that most doctors prescribe medicines by only those pharmaceutical companies that offer them incentives, says a Lahore-based physician who did not want to be named. "The nexus between the medical profession and the pharmaceutical industry is getting stronger day by day, as the people concerned have no fear owing to the fact that no one can challenge a qualified doctor's advice. If a doctor says a particular brand of a medicine suits a patient the most, no one can argue with him or her. Similarly, if patients do not buy the prescribed brand of a medicine, they risk estranging their doctor," he comments. According to a study conducted by The Network for Consumer Rights, an Islamabad-based non-governmental organisation (NGO), the cheapest brand of tablet Ciprofloxacin 500 mg is priced at Rs 5.50, while the most expensive brand of the same medicine at Rs 50.40. In some cases, the difference in the price of the cheapest and the most expensive brand of a medicine is as high as 1,000 per cent, the study reveals. The table -- prepared by The Network for Consumer Rights -- lists 12 drugs; the number of brands of each registered with the Ministry of Health; the minimum price and the maximum price of these drugs; and the maximum price as a percentage of the minimum price, showing how high is the maximum price compared with the minimum price in percentage terms. When contacted for comments, Pakistan Medical and Dental Council (PMDC) sources told TNS that they are aware of the big difference in the prices of same medicines being sold under different brand names and are also working on a plan to address this issue. In this respect, they cite the relevant sections and sub-sections of the PMDC code of conduct that state: i) The practitioner must act in patient's best interests when making referrals and providing or arranging treatment or care. No inducement, gift or hospitality that may affect or be seen to affect judgment may be accepted. Neither will a practitioner offer such inducements to colleagues; ii) Financial or commercial interests in organisations providing health care, or in pharmaceutical or other biomedical companies, must not affect the way that patients are prescribed, treated or referred; iii) Financial or commercial interest in an organisation to which a patient is to be referred for treatment or investigation must be declared to the patient; and iv) Before taking part in discussions about buying goods or services, any relevant financial or commercial interest that the practitioner or the practitioner's family might have in the purchases must be declared. The PMDC code of conduct also discourages doctors from "entering into business or other arrangements that include financial incentives; sharing of fees, including refund based on successful outcomes; and payments for referral of patients for laboratory investigations or other procedures except when a partnership is publicly known to exist." A suggestion that seems to carry weight is that the speakers in medical conferences should be allowed to use only scientific generic names of drugs in their presentations. Another valid suggestion is that doctors should hold their conferences at lecture halls and auditoriums of medical institutions rather than the banquet halls of five-star hotels. Dr Talib Lashari, executive coordinator of The Network for Consumer Rights, suggests that scientific data in the public domain should be made available, on request, to prescribers and any other person entitled to receive it. He says financial or material benefits should not be offered to or sought by health care practitioners, as it influences their prescription of drugs. Dr Lashari opines that though the government may adopt legislation or other measures in this regard, different groups will have to adopt self-regulatory measures to curb these unethical practices. These groups should monitor and enforce the standards themselves, he stresses. Commenting on the role of medical representatives, Dr Lashari says they should make available to prescribers and dispensers complete and unbiased information about each product. In case of any wrongdoings by them, owners of pharmaceutical companies should be held accountable, he suggests. (By Shahzada Irfan Ahmed, The News-45 Political Economy, 16/09/2007) 45 Better late than never The government of Pakistan has finally put a law in place to regulate transplantation of human organs and put an end to their illegal trade. Titled Transplantation of Human Organs and Tissues Ordinance 2007, and promulgated by the president of Pakistan on September 3, 2007, the law aims at stopping the heinous practice of trading in human organs, mainly the kidney trade, and bringing 'kidney mafia' to the book. It may look strange but the fact is that it has taken around 15 years for the government to finalise this law. Efforts in this regard were made in the early 1990s when the Sindh Institute of Urology Transplantation (SIUT) proposed putting in place a regulatory mechanism to monitor human organ transplants. SIUT's proposal had the support of different bodies including those of transplant surgeons, nephrologists, NGOs, social workers and so on. The institute has always opposed the provision of compensation to donors as, according to it, this would lead to further proliferation of this trade and exploitation of the poor. The need to come out with this law was felt the most by the government when the Chief Justice of Pakistan, Iftikhar Muhammad Chaudhry took notice of the hopeless situation early this year and asked the government to clarify why it had failed to legislate on such an important matter. Soon afterwards, a draft law was prepared hurriedly but it invited severe criticism from different quarters. The main objection was against the sub-clause that recommended payment of compensation to non-relative donors. It said: "In case of non-availability of a donor as explained under subsection (1) and there is a threat to life of an end stage renal disease failure patient, liver, heart, or lungs patients, the evaluation committee may allow donation by a non-blood relative or relative or non-relative, after satisfying itself that such donation is voluntary." "The donor under this sub-section shall be compensated as may be prescribed," it further stated. The law in its final shape prescribes severe punishments for those guilty of commercial dealing in human organs. Dr Adibul-Hassan Rizvi, Director SUIT, terms the promulgation of the ordinance a great success of those lobbying for it for decades. Talking to TNS, Dr Adib says Pakistan became hub of this illegal activity in early 1980s when India was the main centre for organ trade. After the imposition of the ban on unrelated transplants, the whole trade shifted to Pakistan. He says the rate of unrelated kidney transplants has increased at an alarming pace in the last decade; from around 25 per cent in 1999 to 85 per cent in 2007. The best part of the story is that the ordinance allows cadaver transplants under which a donor's organs can be removed once he is declared clinically or brain dead. This provision even makes transplant of heart and lung possible as no living person can donate these organs in his lifetime. Such a person's relatives will have to be contacted for approval before operating on his body. In case of unclaimed brain-dead hospitalised patients, the law says that their case shall be presented to an evaluation committee for transplantation after an intense search for their relatives within 24 hours. A transplant surgeon tells TNS on conditions of anonymity that around 2,000 kidney transplants take place in Pakistan each year. Most of these transplants are done in Lahore and Rawalpindi where rackets comprising surgeons, agents, hospital owners etc make poor people sell their kidneys in exchange for a small sum of money. On the other hand, he says, the kidney mafia makes millions from this trade especially when they sell kidneys to foreign patients. He says it was due to involvement of these millions and billions that all measures to check this trade had gone futile in the past. The surgeon says once there will be a ban on non-related kidney transplants and availability of dead persons' organs, this trade will die a natural death. People themselves prefer to buy a stranger's kidney rather than making any of their near and dear ones part with such a vital organ. Once other options are exhausted, they will definitely opt for organs donated by their close relatives. Prof Dr Nawaz Chughtai, Professor of Urology at King Edward Medical University (KEMU) tells TNS that the evaluation and monitoring committees provided for in the law will go a long way in curbing malpractices in this respect. He says that under special circumstances the evaluation committee may allow donation by a non-'close blood relative,' but only after satisfying itself that such donation is voluntary. The evaluation committee under the ordinance shall consist of a surgical specialist, a medical specialist, a transplant specialist, a nephrologist, a neurophysician and an intensivist where available and two local notables having a good record of social service. The evaluation committee shall be established for every recognised medical institution and hospital where at least 25 transplants are being carried out annually. This committee will ensure that the law is followed in its true spirit. Kidney transplants will be carried out only after they have given approval and ensured that the donor is fit enough to part with one of his/her kidneys. Similarly, the law provides for a monitoring committee to be headed by the Federal Minister for Health, and comprising Secretary Ministry of Health, Surgeon General of Pakistan Army, President Transplantation Society of Pakistan, Executive Director Pakistan Medical Research Council, President Ophthalmological Society of Pakistan, President, Pakistan Medical Association of Pakistan, President Pakistan Society of Gastroenterology, and a Surgical Transplant Specialist, as its members. This monitoring committee will inspect hospitals; centres etc where transplants are being carried out and also ensure the quality of medical service. Dr Chughtai says that the ordinance disallows kidney transplant of foreign patients in Pakistan so that chapter is closed. He hopes the pool of voluntary donors and registry of potential recipients will also be established, as envisaged under the law, and regulated as may be prescribed. He tells TNS that in countries like USA, Canada and Saudi Arabia the government is compensating voluntary donors and even taking responsibility of their medical needs for the rest of their lives. "We can hope our government also sets up a similar fund in the near future." He is of the opinion that everybody, except the unscrupulous elements hurt by it, would respect the law. For those who don't, there's severe punishment under the ordinance. He says punishment for unauthorised removal of human organs or tissues or commercial dealings in human organs is imprisonment for a term which may extend to 10 years or with fine which may extend to one million rupees or with both. Similarly, those violating other provisions of the law for which there are no clear-cut instructions shall be punished with imprisonment for a term which may extend to three years or with fine which may extend to three hundred thousand rupees or with both. 46 He says there is dire need to create awareness among masses about cadaver transplants. Many people think that operating on a deceased person's body is tantamount to dis-respecting it. Whereas, he says, there are others also who believe that a dead body should be buried intact. Their point is that every organ of the body will give testimony on the Day of Judgement. These people will have to be told that saving life of a fellow human being is the noblest of all acts, he says.. (By Shahzada Irfan Ahmed, The News-27, 16/09/2007) PMA report depicts gloomy health situation Health indicators of Pakistan are considered among the worst in the world as one child dies every minute from diarrhea, acute respiratory infection and EPI disease. Around 400,000 infants die in the first year of life every year, said a report prepared by Pakistan Medical Association (PMA), entitled: Health of the Nation. About 30,000 women die from pregnancy-related causes as 80 per cent of births take place at home with no or unskilled birth attendants. Communicable diseases such as tuberculosis remain a serious concern, while about 500,000 new malaria cases are reported every year. According to the report, around 25 million smokers consume 36 billion cigarettes while incidents of cancer, kidney diseases and Hepatitis B & C are on the rise. The rulers claimed spending more money on health as compared to the past but the fact remains that the majority of the population has no access to primary healthcare, emergency obstetrical care or emergency healthcare, said the report. A big proportion of the population is deprived of clean drinking water, causing several diseases and putting heavy burden on the health sector. Hepatitis B vaccination is not available, hence its patients are increasing, the report claimed. More than 80,000 people are HIV positive and there is no organised plan to fight this. The PMA report noted with concern that the rulers have not shown any commitment or political will to address the real health issues of the country. “The health of the nation has become a matter of cheap slogans and corruption, more so with increased donor funding,” it said, adding that the government has failed to implement a devolution plan in the health sector properly. “The district governments are not able to provide relief to the patients because of the tussle between the federal, provincial and district governments,” the report noted. It pointed out that there was only one nurse against eight doctors and only one doctor per 2,300 people as the government has no plan to produce adequate number of nurses and paramedical staff, which is badly needed to run the health facilities in rural and urban areas. The report criticised the government’s plan of producing “community midwives” through one year training, which is insufficient and would likely become another waste of resources like the “Dai” training programme of the past. “The government and donor agencies have failed to understand that a shortcut to reduce maternal deaths doesn’t exist,” the report said. It expressed serious concern over joblessness of around 6,000 doctors in Punjab, 3,500 in Sindh and 2,000 in NWFP, adding that the government has no policy to utilise these doctors. On the other hand, the provincial governments have increasingly shown a tendency to recruit doctors on contract basis, bypassing the Public Service Commission, resulting in “politicisation” of the health department. Talking about the private hospitals, the report alleged that majority of such hospitals are not providing standard healthcare. They are also exploiting young doctors by paying them minimal salaries and forcing them to work in an “unhealthy environment”. About quackery, the report said more than 600,000 quacks are playing with the lives of poor people while the government is “criminally” allowing them to continue their business. The report also lamented that the government has failed to produce a drug policy to control the use of “magic drugs” for the treatment of cancer or sexual ailment. “Essential drugs are not available while the market is full of spurious and substandard drugs,” the PMA claimed. It suggested that the government should create a system wherein essential drugs should be made available “economically” and the rulers should not be working for the vested interests of the pharmaceutical industry. The report contains several suggestions to improve the overall health situation. It has described health expenditure of 0.5 per cent of GDP in public sector as “extremely low”. It believes that the effectiveness of foreign-funded projects depend on “good progress in other sectors of life”. The PMA was of the considered opinion that political stability, economic growth and total eradication of corruption was required for establishing a modern healthcare system. It demanded that the government should spend at least 6 per cent of GDP in public healthcare system to make it effective. Suggesting decentralisation of the healthcare system, local accountability and audit, the report said without depoliticising health institutions and introducing meritocracy, the nation will continue to suffer in terms of health. (By Imtiaz Ali, The News-14, 17/09/2007) Baby born in ambulance KARACHI: A baby was born inside a Chhipa ambulance on the way to hospital Sunday. “We received a call from Mahmood Ahmed, an official of the Navy Dockyard and resident of Surjani town Sector 4-A, to take his wife Samreen Sultana to PNS Rahat at Karsaz,” Kaleem, the on-duty officer at the Chhipa control room told Daily Times. He said that at 11:30 p.m., when she was on the way to hospital she given birth to a son. “Our driver was quite clever. Rather then taking her to PNS Rahat, he took her to Osaaf clinic, a private hospital near Karsaz, and both are alright,” Kaleem added. (By Amar Guriro, DailyTimes-B1, 17/09/2007) 47 Recycling hospital waste AS the number of healthcare facilities increases in the country, so does the waste they produce. But the mechanisms to deal with this waste have been evolving at a much slower pace. This sluggishness was highlighted in Lahore when the authorities raided an illegally run plant recycling highly toxic hospital waste. The man running the plant was receiving his extremely dangerous raw material through the connivance of sanitary inspectors of three big public-sector hospitals in the city. The plant has now been sealed. The raid is the first of its kind in the provincial capital but it seems that the illegal practice of recycling hospital waste must have been going on for quite a while. In fact, another recent news report says the Punjab government has issued orders against 70 hospitals across the province for failing to abide by the Hospital Waste Management Rules issued in 2005 under the Environmental Protection Act of 1997. This failure to stick to the rules is turning healthcare facilities into disease-spreading agents. Punjab’s 250 hospitals with a total capacity of 41,000 beds produce 15 tonnes of hospital waste daily. If more than 25 per cent of them are not treating their waste properly and some others are allowing the waste to be recycled illegally, then the provincial authorities should brace themselves for a medical disaster just waiting to happen. Thursday’s raid aside, the official response to the problem has been marked by bureaucratic inertia and an unwillingness to enforce laws. The federal government took eight years to issue waste management rules after the environment law was promulgated and that too without laying down stringent mechanisms for their implementation. With healthcare providers left to themselves to manage the waste they produce without any outside monitoring, it should be surprising if even the big public-sector hospitals are implementing the rules. Given this indifference, the Lahore raid signals that the authorities are finally waking up to the danger their inaction may cause. But a solitary raid, no matter how successful, remains what it is: a one-off attempt at resolving a problem that requires comprehensive solution. (Dawn-7, 18/09/2007) Baby born in ambulance on Sept 11 never stood a chance KARACHI: A baby, who was born in an ambulance outside the gates of Jinnah hospital Tuesday, died two days later amid speculation that a delay in reaching hospital could have contributed to the tragedy. “Someone told me that if we named him Armaan (desire) he would be fine,” his 29-year-old mother Sehar told Daily Times, at her house in sector 11-C/1, North Karachi. This would have been her second child. Her first son, Mohammad Ahsan, was born two years after she married a baker, Muhammad Anwer, in 1988. After Ahsan was born she became pregnant twice but miscarried. “This time, my husband and I were careful and long before the delivery we went through all the required medical investigations at a North Karachi center. The doctors said that the case might be caesarian and that the baby was two months premature but normal.” At 8:00 p.m. Tuesday (Sept 11) Sehar felt labour pains and informed her husband on the phone before leaving in a Khidmat-e-Khalq ambulance with her mother, an aunt and a friend. Muhammad Anwer left his shop immediately on his motorcycle but got stuck in traffic somewhere in Hyderi, according to Sehar. “We reached Lady Dufferin Hospital after an hour at about 9:00 p.m. after being stuck in traffic jams at many places,” she said. They took an hour for what Sehar referred to as a 30-minute journey as one route was reportedly blocked. Sehar claims that the Lady Dufferin staff did not agree to deliver her baby as she had not registered with them earlier. However, Lady Dufferin MS Dr Faridon Setna rejected these claims and said that if a patient was brought in an emergency, they were admitted and if they could not afford treatment there was a charity fund for such cases. The problem with Sehar’s case was, however, that she was asked to sign a consent form, taking responsibility for whatever happened as there was risk involved as the baby was premature and she had arrived late, according to Dr Setna. The hospital said that Sehar refused to sign the forms. When questioned why, Sehar told Daily Times that she and her mother got frightened when the hospital told them that there was a risk in the delivery and reportedly said that she and the baby could both die. “There was no man with us and so we couldn’t decide what to do,” she said. After two hours, Sehar and her family decided to go to Jinnah hospital in another ambulance, this time a Chhipa one. The baby was born right at the JPMC gate inside the vehicle. “My baby was perfectly alright but the doctors said that as he was born inside the ambulance, the cold air had affected him and he was suffering from chest congestion,” Sehar claimed. The baby was taken to NICH next door but died the next afternoon. Sehar believes that her baby died because of the delays – the delays caused by the traffic jams to Lady Dufferin Hospital, the wait there, and then the journey to JPMC. When Daily Times asked Dr Setna to comment on the matter, he said that even if Sehar had left Lady Dufferin, she should have gone to Civil hospital, which was far closer than JPMC. “If we did not admit her why did she not go to Civil hospital that is just next to Lady Dufferin,” he asked. “She could have reached there within two minutes. She should explain why she rushed to JPMC.” When Daily Times questioned Sehar about her decision to undertake a longer journey to JPMC instead of going to Civil hospital, she answered that the Chhipa ambulance driver had suggested it. Daily Times contacted the Chhipa service control (111-111-134) Sunday and repeatedly again till the filing of this report Monday night in a bid to contact driver Zahir Khan. Chhipa had earlier identified him as the ambulance driver in Sehar’s case. But then Zahir Khan could not be contacted to be questioned on his alleged suggestion to take Sehar to JPMC even though Civil hospital was closer. Daily Times went through four Chhipa officers, Kaleem, Anees, Rizwan Hyder and Mohammad Tahir, at different times and all of them said that Zahir could not be contacted. Hyder said that he would not comment on the matter. Officer Kaleem disclosed during one phone call to trace Zahir that there was a “garam case” (hot new case) of another baby born in a Chhipa ambulance Sunday night. (The matter was reported in Monday’s Sept 17 edition.) Kaleem said that driver Zahir could be found at the Chhipa center located at the main emergency gate of Civil hospital but when Daily Times visited Monday he was nowhere to be found despite repeated requests to Chhipa to trace him. Chhipa said then and later that they did not have his home number and he did not have a cell phone. 48 Officer Mohammad Tahir told Daily Times that Chhipa has a total of 24 ambulances in Karachi city and within the last 15 days two babies were born in them. Anwer Kazmi, personal secretary to Abdul Sattar Edhi told Daily Times that the Edhi Foundation has 150 ambulances. Daily Times reported on Aug 12 that a baby was born in an Edhi ambulance near JPMC due to a traffic jam. (By Amar Guriro, DailyTimes-B1, 18/09/2007) Proposed Rs1.5 bn Trauma Centre hits snags The proposed trauma centre at the Civil Hospital has hit snags as funds amounting to Rs1.5 billion have already lapsed last year over ‘trivial issues’, sources at the hospital told The News on Tuesday. There were strong apprehensions that the funds were also likely to lapse this year as the place decided for it has not been vacated so far. The sources said the trauma centre would be established at the current place of the Neurosurgery ward and eye department of the Civil Hospital. Some residential areas would also be vacated for this purpose. The concerned officials had already requested the City District Government Karachi in this regard. The 14-storeyed building of the centre would be established with ‘all modern facilities’ and a helipad to meet any eventuality in the mega-city. It would be first such facility in the provincial metropolis, which is being set up with financial assistance of the federal government which will bear 50 per cent cost of the project. The Sindh government will provide the remaining funds for this ‘state-of-the-art facility’. As the neurosurgery and eye wards could not be closed, it was decided at a high-level meeting that both departments would be shifted to offices of ‘Chemical Examiner’ adjacent to Services Hospital from where Sindh Aids Control programme would be shifted to another place. Offices of Chemical Examiner would replace it. However, sources said the Aids programme officials were delaying their shifting since the last two years on ‘insufficient grounds’ despite ‘firm decision’ of the Sindh Minister for Health, Syed Sardar Ahmed. The sources said several meetings have been held in this regard but the place was not being vacated. They pointed out that last such meeting was held on June 25, under the chairmanship of the provincial health minister, which took ‘strong exception’ to the situation. The minister ordered immediate shifting of offices of the Aids programme but so far it has not been implemented, the sources said. They added that around 15 days ago, office of the Sindh Blood Transfusion Authority (SBTA) at Services Hospital was shifted to another official building near Kala Pul. The trauma centre was supposed to be completed within three years but almost two years have gone by in sorting out ‘small issues,’ the sources said. The proposed trauma centre spread over 6,000 yards is among 22,00 major health and education related projects in the country, the sources said. They said tenders had already been invited and construction work would soon start provided the place was vacated. Medical Superintendent of Services Hospital said that both Sindh Aids Control and Chemical Examiner were independent institutes and had nothing to do with the hospital. He said a space was provided to the Aids programme on instructions of then health minister and health secretary; hence they were entitled to ask them to vacate the place. Dr Azra Abro, head of the Aids control programme told The News that so far, she has not received a written order for shifting the office to another place. (By Imtiaz Ali, The News-13, 19/09/2007) Rangers to be deployed at Lyari General Hospital The Sindh Government has decided to deploy Rangers at the Lyari General Hospital (LGH) in the wake of continued violence, triggering fear and anxiety among doctors and other staff, official sources told The News on Wednesday. The sources said that the incoming Health Secretary, Malik Israr, held a meeting with the administration of the LGH, where the security situation was assessed. This meeting was followed by a visit of Sindh Health Minister Syed Sardar Ahmed to the hospital few days ago. A senior doctor of the LGH told The News that they were expecting redeployment of Rangers within the next few days. He said lack of security, along with a shortage of water, were main problems there. The sources said that the Rangers had restored some sense of security when they were deployed at the hospital some months ago. However, around two-three months ago, the Rangers were withdrawn from the hospital because of law and order problem in the rest of the city following the May 12 mayhem. The volatile security situation in Lyari Town has adversely affected functioning of Lyari General Hospital, sources said. Continued violence has prompted several ‘non-local’ doctors to avoid performing their duties, especially in the evening shift. Acute sense of insecurity prevailed at LGH as some doctors have been subjected to strong-arm tactics by rogue elements of the area, the sources said. They said that, some days ago, an orthopaedic surgeon went to meet his friend, an ENT surgeon, in the hospital. In the meantime, some youths arrived there and “ordered” the doctor to treat a patient brought by them. The orthopaedic surgeon told them that it would be advisable for them to consult the concerned doctor. This innocuous suggestion infuriated the people who started beating him severely, the sources said. 49 When the news of the beating rapidly spread to other wards, the doctors boycotted their duty temporary. However, soon after that, they abandoned their protest, the sources added. Following this incident, several specialists were reluctant to join duty. Lyari General Hospital is considered one of the major hospitals in the city where MBBS students of Dow Medical College also do their house job. But after some robbery incidents, they have also shown their reluctance to go there, the sources said. Less than normal attendance of other specialists has caused immense inconvenience to patients who now to go to Civil Hospital or Jinnah Post-Graduate Medical Centre (JPMC) instead. A senior citizen of Lyari said they also avoid venturing out after sunset as around 15-20 armed teenagers roam freely in the area terrorizing the people. (The News-13, 20/09/2007) 18 die in toxic liquor tragedy KARACHI, Sept 20: At least 18 people died after drinking toxic liquor in different localities of the city on Thursday. Over 30 other affected people were hospitalised, some of them in a serious condition. Sindh Health Minister Sardar Ahmed told Dawn that the victims belonged to the Muslim, Christian and Hindu communities and they had consumed the poisonous liquor on Wednesday night. “Twenty-two affected people were brought from Railway Colony, Mithadar, to the Civil Hospital Karachi, where six of them died and four others were in a critical condition,” he said. The minister said ten people died at the Jinnah Postgraduate Medical Centre. “They were brought to the facility from different localities.” Mr Ahmed said the victims had drunk illegally made liquor, adding that at least five affected people were still hospitalised at the JPMC. “The source of the contaminated liquor is apparently the same,” he said. DIG South Javed Ali Shah Bukhari told Dawn that the victims had bought the toxic liquor somewhere in the Mehmoodabad police limits. “The area SHO has been suspended and an investigation is under way,” he said. The deputy director of the JPMC’s emergency centre, Dr Seemin Jamali, said the victims started arriving at the facility in the early hours of Thursday. “They were brought in at different times and from different localities in a highly critical condition,” she added. She said eight of the nine victims brought to the facility died, while one affected person was still unconscious. Those who died at the Civil Hospital were identified as Akhlaq, Krishan, Arshad, Boota Masih, Khalid and Shafqat. The victims’ ages ranged between 25 and 45. JPMC sources said Suresh was from Masoom Shah Colony, Shaukat from Kashmir Colony, Dost Mohammed and Raees Uddin from Hazara Colony, Parkarsh from Jutland Lines and Mohammed Ashraf and Gopal from the Frere area, Ibadat, Mohammad Ali and Zaigham. Civil Hospital sources said the bodies of two victims were taken away by their families without allowing legal formalities to be carried out. They identified the victims as Rashid Munawwar and Javed, residents of Railway Colony. A relative of one of the victims, who wished to remain unidentified, told Dawn that the toxic liquor was bought at a den in Chenesar Goth in the Mehmoodabad police limits. “They bought the Kuppi (illegally made liquor) yesterday and their condition started deteriorating shortly after they consumed it,” he added. Police said the victims, including sanitary workers, belonged to low-income families. Saddar SP Tahir Naveed said the preliminary investigation had revealed that the victims had bought the contaminated liquor in Chenesar Goth. “We have formed an inquiry team to investigate the matter,” he added. The SP said it appeared that the business of illegally made liquor thrived due to the closure of licensed liquor shops during Ramazan. “Addicted drinkers buy such stuff from dubious establishments and such incidents take place every year,” he said. Meanwhile, sources said the sale of Kuppi and Tharra – two types of illegally made liquor – was rampant in certain parts of the city such as Chenesar Goth, Kala Pull, Lyari, Machchar Colony, Sohrab Goth, Malir Mander and Chakiwara. They said the users sometime mixed the red-coloured Kuppi with transparent Tharra to intensify the effect of the stuff, but the mixture often became toxic. (By Tahir Siddiqui, Dawn-17, 21/09/2007) Qadri’s family to sue hospital The family of Advocate, Ateeq Qadri has decided to sue the Agha Khan University Hospital (AKUH) on charges of negligence because of which Qadri died, Salim Noori told The News. Qadri who was attacked by unknown assailants last Thursday expired on Saturday at the AKUH. According to his family members Ateeq Qadri was in stable condition when he was admitted but after a four hour long operation on Friday his condition worsened at which point he was put on ventilation. On Saturday he was pronounced dead. A panel of lawyers were contacted for the format of petition who have told Noori that within couple of days a petition will be filed in the court of law. The family consulted senior doctors at the Jinnah Postgraduate Medical Centre (JPMC). Later they were informed by Dr Anwer Tanoli a neurosurgeon at JPMC said that, had the case been handled by a senior doctor Qadri would have lived. 50 When officials of AKUH were contacted, they said that Qadri was brought to the Emergency Room of the AKUH on September 14, 2007 following multiple guns shot injuries. The family gave a history of multiple gun shot injuries from a close range at home. He was initially treated at Jinnah Post Graduate Medical Centre where a chest tube was inserted in his left chest. He was a known case of diabetes mellitus. AKUH says that the patient was immediately rushed to the operating room without any formalities of admission. At the Operation Room the patient was further assessed by the orthopedic and cardiothoracic teams. At the time of surgery the surgeons found almost a liter of blood in the abdominal cavity, multiple perforations of the intestines, a total of 13 perforations were identified. His liver, stomach and spleen were normal. Subsequent to this surgery, the surgeon met and explained the patient’s condition to his brother and couple of family members. Critical nature of injuries was explained and the patient was transferred into the Intensive Care Unit. He was further evaluated on September 15 and once again the severity of illness was explained to the family. In the morning of September 15, 2007 one of the brothers of the patient asked the surgeon to withdraw all treatments. At that time the surgeon explained him the consequences, nature of injuries and the 20% possibility of survival and advised him not to suggest for a withdrawal at that point in time. Subsequently the patient was seen by a cardiothoracic surgeon as well. The family once again approached the on-call Resident Surgeon requesting withdrawal of the treatment. The Resident Surgeon explained all the pros and cons for withdrawing of such support but on family’s persistence, a written request from the family was documented, support was withdrawn and patient subsequently died. Atiq Ahmed Qadri was a senior member of the Karachi Bar Association. He has left behind 4 sons and 2 daughters eldest being 15 and youngest 8 years old. He was the second lawyer, targeted within one week. However, family members say they will file a case against AKUH in the court of law. He said that an FIR has been registered already as police officials came to the hospital and took the signature and version of the relatives. (By Shamim Bano, The News-13, 21/09/2007) Most child cancer patients from low income group KARACHI: Parents of cancer patients treated at the Oncology Unit of the National Institute of Child Health (NICH) mainly pertain to the low socio-economic class and belong to big families. This was revealed in a study conducted to assess the socio-economic status of parents of children under treatment for cancer at the NICH’s Oncology Unit, supported by Child Aid Association led by senior pediatrician Dr Nizam-ul-Hasan. An elaborate survey, conducted by local students for this study, found that 60 percent of these children are from Karachi while the rest come from other cities and villages from across the country. Seventy-two percent of these patients are boys while only 28 percent are girls. Most of those living outside Karachi are either unemployed or living on minimum wages as labourers for big landlords. Most have no means to bear medical expenses and 78 percent of them earn Rs 1,000 to 6,000 monthly. The study also found that 65 percent of these children have three to six people in their immediate family while 35 percent had more than seven people. In most of the cases, a single family member supports the rest of the family with no other source of income. Many were found to be living as tenants or with many families sharing one house. Seventy percent of them live with their parents in houses with only one or two rooms and 70 percent of them do not own any means of transport, with only about 30 percent having bicycles or motorcycles. (DailyTimes-B1, 21/09/2007) Newborn babies undergo open-heart surgery KARACHI, Sept 21: Two newborn babies recently underwent successful life-saving open heart surgeries in a Karachi hospital. These operations – the first of their kind in the city -- were performed by a Pakistani team of doctors. Both babies have recovered well; one of them has already been discharged while the other will be released from hospital in a day or so. Three-week-old Abdul Khaliq Moosani and 11-day-old Aman Humayun were reported with Transposition of the Great Arteries (TGA), a congenital heart defect at the Aga Khan University and Hospital (AKUH) in August. Initially, both of them underwent balloon arterial septostomy, a perquisite for the arterial switch operation, which was performed later. “Until now many parents, especially of children with this particular congenital heart disease, were forced to travel outside Pakistan for corrective surgery. But now, all types of congenital paediatric cardiac surgeries can be (performed) in the city,” said Dr Muneer Amanullah, congenital and paediatric cardiac surgeon and assistant professor who headed the fivemember team that included Dr Mehnaz Atiq, Dr Mohammad Hameed, Dr Mansoor Khan and Dr Anwar-ul-Haq. Earlier, he said, infant and neonatal open heart surgeries had been performed at the Lahore Children’s Hospital and the Armed Forces Institute of Cardiology (AFIC), Rawalpindi. The reason for having such few surgeries was a lack of expertise as the number of trained paediatric cardiac surgeons in Pakistan was limited. “Each year, 120,000 children are born with congenital heart disease in Pakistan. Almost 90 per cent of these children either die or are diagnosed so late that even surgery is ineffectual,” Dr Muneer said, adding that TGA comprised 10 per cent of the congenital heart disease cases and had a very high mortality rate, within a month of the baby’s birth. 51 The reasons of having TGA were still unknown and the condition could affect anybody. However, it was comparatively common in boys. Explaining TGA, commonly known as ‘blue baby syndrome,’ Dr Muneer said this was an abnormal development of the foetal heart during the first eight weeks of pregnancy in which the main arteries came from the wrong side of the heart. As a result the blue blood, which had not taken up oxygen, was pumped round the body while the oxygenated blood went back into the lungs. “The symptoms appear very early in life, usually in the first few days. The baby is blue and breathless and unable to feed. Immediate medical intervention is necessary as the birth defect can endanger life. ‘‘The surgery has no adverse effect on the child’s normal growth and he or she doesn’t require any further surgical procedures or special precaution later in life. ‘‘After initial regular check-ups, follow-ups are needed once a year,” he observed, while stressing the need for educating parents as well as general paediatricians about TGA. (By Faiza Ilyas, Dawn-18, 22/09/2007) Toxic alcohol death toll rises to 39 KARACHI, Sept 21: The death toll from toxic bootleg liquor consumption rose to 39 as 21 more people died at hospitals on Friday. The condition of 18 more people said to have drunk the poisoned brew was reported to be critical. Hospital sources said the affected people, who had symptoms of nausea, severe cramps, shaking and blurred eyesight coupled with unconsciousness, had a faint chance of survival. A ward boy at the Jinnah Postgraduate Medical Centre said he saw such patients being brought to the hospital and bodies being taken away throughout the day. The Deputy Director of the JPMC’s Accident and Emergency Department, Dr Samin Jamali, told Dawn that 23 affected people and three dead victims of the toxic liquor were brought to the facility on Friday. “Eleven of them died at the hospital and the remaining 14 are still admitted to Ward 5,” she said. The doctor said the sick people were in a highly critical condition. “The have minimum chances of survival,” she said, adding that the toll was bound to rise with each passing hour. Dr Jamali said the affected people were still being brought to the JPMC from different parts of the city. “We don’t know how many others are still on their way to hospital,” she said. The illegally made liquor, known as Kuppi and Tharra in the local parlance, contained methyl alcohol, which is intended for industrial use and is fatal to drink in large quantities. Doctors said the victims died of respiratory paralyses. They said a depression in the respiratory centre of the brain occurred once the victim’s liver stopped absorbing toxicity. Meanwhile, police arrested six people suspected of blending the industrial alcohol and selling the contaminated mixture to unsuspecting alcohol users. Capital City Police Officer Azhar Farooqui told Dawn that the suspects, including the main supplier and the main manufacture of the toxic brew, were arrested and their hideaways raided. He said methyl alcohol, also known as methanol, was used in the manufacture of the brew at a smaller level in different parts of the city. “We are co-ordinating with other agencies to keep a check on the sale of chemicals for industrial use,” he added. As many as 18 people died and many others fell ill on Thursday after they consumed toxic liquor in different localities. Of them, 10 affected people died at the Civil Hospital Karachi and six others died at the JPMC. Two bodies were taken away from Civil Hospital without medico-legal formalities. JPMC sources said those who died on Friday included Mukhtar, 40, from Drigh Colony, Raja Saeed Ghulam, 60, from Bizerta Line, Raja Sohail, 22, and Bashir Masih, 50, from Railway Colony, Sabir, 36, from Mehmoodabad, Mohammad Ali, 26, from Lines Area, Lal Ji, 50, and Johnson, 19, from Frere and Ashiq Ali, 46, from Korangi. (By Tahir Siddiqui, Dawn-17, 22/09/2007) A fine line between bliss and blight Lack of scientific knowledge, distillation facilities and equipment available to bootleggers, who brew homemade liquor at illicit breweries or distilleries, sometimes result in the production of toxic “methanol or methyl alcohol” that is highly fatal for humans, experts said on Saturday. As many as 43 persons died in Karachi over the last two days after consuming poisonous liquor, without knowing what went wrong, as, normally, they used to consume same type of raw liquor, which is very popular among the people of lowincome groups in remote localities of the city. Several experts including chemists, biochemists, doctors and police officials were of the opinion that inexperienced winemakers sometimes produced toxic liquor containing “methanol or methyl alcohol” and owing to lack of any scientific equipment and knowledge, they market it, which results in the deaths of the consumers. As far as production of cheap liquor is concerned, it is carried out through fermentation of rotten fruits, mainly grapes and apples. Yeast is added to the mash of rotten fruits for its fermentation, the process which converts sugars into alcohol, and which produces carbon dioxide as a byproduct. 52 “Rotten fruits are packed in a metallic or plastic container with yeast for fermentation. The yeast converts the sugars available in rotten fruit juice into ethyl alcohol. However, sometimes, instead of ethyl alcohol, methanol is formed, which is a highly toxic substance” Dr Aamir Jamil, a biochemist serving at the University of Agriculture, Faisalabad said. According to him, there are different forms of alcohols and they are divided into three categories: primary, secondary and tertiary. Most of the alcohols are considered as deadly poisons and the only form of alcohol that can be safely ingested by humans is “ethyl alcohol or ethanol”. However, owing to their lack of knowledge of chemistry and unavailability of the equipment to test, the bootleggers cannot distinguish between the desired product (ethyl alcohol or ethanol) and toxic “methanol.” They sell it to consumers in any case. Some persons aware of the process of illegal bootlegging claimed that the only test carried out by the illegal wine-makers is tasting their product. If it is sweet, they consider it safe for human consumption and if it is sour, they term it “poison”. However, as bootleggers make investment in winemaking on purchase of fruits, yeast and sometimes chemicals like tincture and medicines, they don’t discard the poisonous liquor containing “methanol” and sell it to consumers in plastic bags, whose price varies from Rs 30 to 60 or 70. In order to make the poisonous liquor taste sweet, the bootleggers add some sugar in addition to sedatives including medicines like dizapam tablets, tincture and spirit to make it strong as well as sweet to satisfy their customers, an expert said. But the consumers of home-made wine, which is commonly known as Kuppi, Tharra, (also Thelly in interior of Sindh) and Katchi Sharab, first taste the wine and if it is found sour in taste, they normally don’t use it and complain to seller or the one who prepares it. Biochemists and doctors believe that although normal ethyl alcohol is also dangerous for human consumption as it affects central nervous system of the consumer, the toxic methanol can result in death of the consumer as even 50 to 100 ml of its ingestion can cause death of a human being. According to Dr Shahid Ahmed Abbasi of Aga Khan University Hospital, symptoms of methanol poisoning include bizarre behaviour, falling into a coma, extreme dizziness, severe headaches and seizures. “Methanol poisoning can render a person temporarily blind, the digestive system starts to immediately reject methanol and symptoms may include severe stomach pain, nausea, and diarrhea. Methanol also disrupts liver and pancreatic function. Even with treatment, methanol poisoning can cause permanent liver damage and death”, he added. He said that other symptoms in methanol poisoning are difficulty in breathing, signs of low oxygen levels through blue fingernails and lips, complete fatigue and cramps in the legs. (By M Waqar Bhatti, The News-13, 23/09/2007) Urban lifestyle causing increase in neck pains As the life of urban individuals becomes more and more stress full and hectic, a considerable number of people are developing neck pain every year. This can be caused by the unhealthy lifestyles of individuals which focus more on luxury and office work then diet and exercise. Doctors tell us that the neck has a hard job to do— that of holding the head up, leaning, bending, twisting—and by staying in one position for a long period of time makes this job even more difficult. Apart from the neck aches that are caused by modern lifestyle, the functioning of the spine may be altered by aging, disease or injury. This makes neck pain or stiffness a common discomfort for elderly people. Sometimes ligament and muscle strains cause neck pains that are generally known as wry or sore neck. However, generally speaking, everyday activities are to blame as cause of the rise in neck pain, said Dr Ehsan Bari, assistant professor of surgery department at the Aga Khan University Hospital. “These activities include bending over a desk for hours, having poor posture while watching TV or reading, placing a computer monitor too high or too low, sleeping in an uncomfortable position, or twisting or turning the neck in a jarring manner while exercising etc,” Dr Bari explained while talking to The News on Tuesday. In this condition the pain and stiffness is generally localised to the region of the neck. The muscle stiffness and spasm at times can give rise to abnormal neck postures in which the head is forced to turn on one side (torticolis). He added that this kind of pain responds well to simple measures such as, gentle massages with analgesic balms or olive oil which helps relax sore muscles. The application of ice is also beneficial as it decreases inflammation. Also, alternate application of ice and heat for 15-20 minutes, with an hour’s rest between each, is beneficial, he suggested. Pain killers which are non-steroidal and anti-inflammatory can also relieve pain and reduce swelling. A soft collar to support the neck especially during the acute pain period is helpful. However, it should be only taken during the acute phase, he said. This combined with a physiotherapy program of appropriate stretching and muscle strengthening exercises will likely provide relief against the neck pain. In resistant or refractory cases, stronger analgesics, cervical traction, transcutaneous electric stimulation (TENS) of neck areas helps in relieving pain. Talking about other causes apart from general activities, Dr Ehsan said that neck pain can also be caused by the injuries like whip lash and vertebral fractures, infection or inflammation of the neck joints or soft tissue and degenerative diseases such as spinal stenosis (narrowing of the spinal canal) or prolapsed intervertebral disc (slip disc). The neck pains arising due to the slip disc may radiate to the shoulder, chest and upper extremities. This pain is often associated with numbness and weakness in the arm, he said. Contrary to the general belief it is not a very common cause of neck pain. Less than 1% of the neck pain is caused by disc herniation. Another cause of the neck pain is the compression of the spinal cord. This causes damage at an involved level resulting in the impaired coordination of the hands, gait disturbances (difficulty walking) with weakness in the lower limbs, spasticity 53 (stiffness) and poor urinary control. If left untreated this condition can aggravate and lead to irreparable damage, he warned. Disc prolapse and early compression should be treated conservatively. In most cases they respond well to the above mentioned therapies. However if the condition persists or there is deterioration in symptoms, an MRI scan of the neck is needed. The disc prolapse or cord compression is always visble on a quality scan. Decision of the surgery is based on the result of the MRI scan in combination with deteriorating symptomotolgy of the patient. In properly selected patients surgery is safe and rewarding, he believed. Dr Ehsan Bari said that one can prevent neck pain or its recurrence by adopting some simple measures. Good posture is essential. “If your work entails prolonged sitting hours you need appropriate back support”, he said. While working on the computer adjust the monitor at eye level. “If your profession involves bending of the neck, take regular breaks to stretch your neck”, he recommends. When sleeping make sure your mattress is firm and your pillow is properly and comfortably supporting your neck. Stress aggravates neck pain. Regular exercises that involve stretching of the neck and upper body can also relieve unwanted stress and tension, he said. (By Imtiaz Ali, The News-19, 23/09/2007) Toll rises to 41 as ‘blind’ drunk patients unlikely to recover KARACHI: There are very slim chances that the people brought blind to hospitals in the poisonous liquor kuppi case over the last few days, will recover, doctors have said. Three more people were admitted to poison control ward No. 5 of Jinnah Postgraduate Medical Center Saturday morning bringing the total to 29, said Deputy Director Dr Seemin Jamali, who is also in charge of the Accident and Emergency Department. Their names are Pervez Masih, 34, of Sultanabad, Sohail Chaudry, 27, of Clifton and Murad Khan, 50, of Clifton. The Methanol poisoning was so high in the patients who went blind that there are hardly any chances they will recover. When asked how come patients are still trickling in three days after the incident, Jamali said that they could have drunk liquor from the same stock. Anyone who has more than 30ml of absolute methanol has low chances of survival, she added. According to the police, the man arrested in the case so far, Sabz Ali and his brother Farooque alias Farooqa, have been involved in a number of criminal and narcotics cases and have been proclaimed offenders. Farooque is still at large. Sabz Ali has four brothers and two sisters. His family hails from a village named Toro in district Mardan. Sabz Ali, Farooque and two other brothers were once police constables with long postings at the police headquarters naval in Saeedabad. Sabz Ali was recruited in 1995. He and his brothers were allegedly involved in the murder of Raja Sabir, the brother of Sub Inspector Raja Khalil in a drugs case. FIR No. 159/99 was lodged against Sabz Ali and his brothers Farooque and Maroof. Sabz Ali, Farooque and Farooque’s son Irfan are among the main accused in the current kuppi case. These brothers have reportedly hired the services up to eight lawyers and are on bail before arrest in several cases. The Mehmoodabad police have recovered two drums of premature and one dozen ready-to-use kuppi. Meanwhile, the Mithadar police have arrested two accused, Naeem and Obaid. Police claimed that both were arrested from their houses but Naeem claimed that he had gone to the police station himself. “I am a kuppi user and am not linked to the business,” Naeem told Daily Times Friday night. “I used to purchase kuppi from police constable Akhlaque and bought 5 bottles from him on Thursday. Akhlaque made a profit margin of Rs 50 on each bottle. I helped the police arrest Obaid from his house. Obaid runs a medical store in Jackson Market near Keamari.” The police recovered hundreds of empty bottles and two 34-litre drums from Obaid’s house. Mithadar police sources said that when they raided the place, he took 30 minutes to open the door and in the meanwhile was draining the alcohol. Also, a special investigations team has arrested two more accused, including Ashraf who is an assistant sub inspector (ASI) with the KESC police. (DailyTimes-B1, 23/09/2007) Families of alcohol victims tell their side of the tale Railway Colony sprawls over a large area, where most of the residents are employees of the lowest grade in Pakistan Railways, and have lived here for a long time. The crux of the population is from Punjab, but residents are fairly homogenized in terms of religion as they include Muslims, Christians and Hindus. Arif Rafique, lives here with his aunt, in a small two-room ‘apartment’, that smells strongly of sewage and wet clothes. The family has 11 members, including children, and it seems impossible for them to fit in this place. Rafique’s immediate family does not account for this large number. His daughters have all been married off, his wife was killed in an accident three years ago, and both his sons have succumbed to heroin abuse. The old woman who is Arif’s aunt speaks in a combination of Punjabi and Urdu. She claims he started drinking right after his wife died. “One of his sons was found dead by a heroin overdose near the railways tracks,” she said, “and the other…” They all exchange looks but Arif’s younger sister intervenes and boldly completes the sentence, “We don’t know where he is anymore. He’s a junkie too. He doesn’t even come home anymore.” Fifty-year-old Arif was apparently very depressed, after he lost his wife and became even more unable to handle personal problems after he lost both his sons. He started drinking but unfortunately as a person of his income group cannot afford pure, distilled alcohol, he had to resort to ‘kuppi’ and ‘tharra’, or home-distilled spirits. 54 Internationally known as moonshine, ‘tharra’ and ‘kuppi’ are more or less the same, a mixture of spirit (ethanol) sometimes adulterated further with pills to cause greater intoxication. These are made by fermenting the mash of sugar cane pulp in large spherical containers made from waterproof material with up to 100 per cent alcohol. It is a dangerous drink, mainly because of the risk of alcohol or copper formaldehyde poisoning. Rafique is now admitted in the Civil Hospital. His stomach has been washed but his family is still tense and disillusioned. “How do we know he will not start again when he returns?” questions his sister Shamim, “And how will we know who the dealers were? Most have fled to their villages in Punjab, and will never be caught. Something should be done about this illegal business.” In Railway Colony a total of nine people have been killed by alcohol poisoning of the 18 in Karachi. It is more than obvious that the spirit was made by one manufacturer but none of the families have any idea who the dealers are. “We didn’t even know that they drank,” said the mother of another victim, who is now also admitted in the CHK. “All I know is Liaquat said he would be going out to work, (he was an electrician), and went out. How did I know he would be drinking with his friends?” Moreover, Mukhtiari is worried but relieved that her son has been saved. Unlike Rafique’s case, where the doctor has given a time line of 15 days and has told the family that if he survives during this period he will live, Liaquat is now visibly better. “That night when he came home, he just went to sleep and slept soundly the entire night and wouldn’t even wake up the next morning,” says Mukhtiari. “Eventually we grew a bit suspicious when so many bodies had been found dead in our colony the next morning. When we asked him if he had drunk anything he refused. But his eyes were red and told us otherwise.” Eighteen-year-old Liaquat who belongs to a Christian family, never took anything other than ‘gutka’, says his sister. “We are poor, where could he drink regularly from?” But in Lakshmi’s house, there is a heavy silence, following the death of her father-in-law. In the main room a small group of sari-clad women sit talking in undertones, but their faces reveal the tension of the upcoming days. Lakshmi’s brother Santosh says that Krishan, 55, came home complaining of not being able to see anything and he was vomiting continuously. They took him to Civil Hospital where the doctor gave him ‘an injection’, and diagnosed him with ‘indigestion’. Later he fell ill again, and this time when he was taken to the hospital, he expired. “I don’t know what to do,” she laments, “He earned 3000 rupees working as a sweeper in an office, now who will earn that extra bit of money.” Rajesh, her cousin says that moonshine also comprises Mandrax, which is a synthetic drug that is compiled by means of the mixing chemicals whereby a tablet is produced. The active ingredient in Mandrax is Methaqualone. Most of the ingredients are bought from medical stores and even suppliers of medication in hospitals are thought to be part of the mafia which smuggles these banned or exclusive drugs to make moonshine. Mandrax mixed with spirit can be fatal, but its usual effects include relaxation, euphoria, and drowsiness, also reducing heart rate and respiration, whereas an overdose can cause delirium, convulsions, vomiting, renal insufficiency, coma, and death through cardiac or respiratory arrest. It resembles barbiturate poisoning but with increased motor difficulties and a lower incidence of cardiac or respiratory depression. (By Xari Jalil, The News-20, 24/09/2007) In vino veritas, but survivors swear absolut abstinence KARACHI: Regret, concern for their families, and appreciation for divine intervention was how the survivors of the Kuppi fiasco said they felt while talking to Daily Times Sunday. At least 41 people were reported dead from Methanol poisoning across the city after they bought adulterated moonshine because regularized wine shops close in Ramadan. Four patients, Khalid, 35, Sohail, 24, Saleem, 30 and Pervez, 27, were admitted to JPMC and three others, Mehmood Baig, 45, Arif Maseeh and Liaquat Maseeh, 22, were admitted to Civil hospital. “What would’ve happened to my family if I had died?” asked Khalid, who is a sweeper and father of one girl and three boys. He was admitted Friday night to JPMC. Sohail, a scrap vendor who is married and lives near Teen Talwar, Clifton, said that he bought the liquor along with one Murad from Kala Pul. Murad drank a lot more than and didn’t survive. “I thank God for saving me from being one of the victims,” he said. Saleem, the youngest of two brothers and four sisters and a resident of Jacob Lines, is in the poultry farm business and was admitted Thursday night. He said that he was thankful to God for being alive. He said that he felt guilty of committing a sin in this holy month and that he has learnt an unforgettable lesson. Pervez, a resident of Hijrat Colony who recently lost his job, was also admitted Thursday night. “There was no other way to overcome the anxiety but to drink,” he said but adds that he now regrets what he did. According to Mehmood Baig, a resident of Railway Colony, he consumed the poisonous liquor along with Khalid and Akhlaq, who didn’t make it. He told Daily Times that Khalid bought two bottles of kuppi from Kala Pul. “I was fasting regularly but on the fifth day of Ramadan I fell ill. On the insistence of Khalid and Akhlaq I drank the liquor.” He said that it was a punishment from God and that he was thankful to God for saving his life. Arif Maseeh, a sweeper, a resident of Railway Colony and father of five daughters and one son, said, “What would’ve happened to my kids if I died? Who would look after them?” He said that he bought the kuppi from Naeem and consumed it at his friend Yasir’s house. Liaquat Maseeh is a mechanic from Railway Colony who consumed the liquor Friday night with his friend Zeeshan (who 55 died earlier). Liaquat said that since he was persuaded to drink by his friends he didn’t have too much. “I will never indulge in such an act again.” The names of the 29 patients who, at the time this report was filed, are alive and still being treated at the JPMC are: Mohammed Saleem, 35, resident of Jacob Line; Jaffer Sohail, 23, resident of Railway Colony; Aslam, 40, resident of Bizerta Line; Mohammed Faisal, 22, resident of Lines Area; Mohammed Akber, 30, resident of Jet Line; Rafiq Ahmed, 38, resident of Quaidabad; Pervez, 29, resident of Lines Area; Chandan, 20, resident of Lines Area; Asif, 19, resident of Lines Area; Pardeep, 18, resident of Chanesar Goth; Rashid, 18, resident of Railway Colony; Shahid Ali, 40, resident of Nasir Colony; Johnson, 19, resident of Bizerta Colony; Harrison, 26, resident of Akhtar Colony; Kishan, 26, resident of Punjab Colony; Javed, 30, resident of Kala Pull; Heera Lal, 40, resident of Clifton; Khalid, 27, resident of Korangi No. 2 ½; Shahzad, 25, resident of Korangi No. 2 ½; Pala, 35, resident of Orangi; James, 42, resident of Army Workshop; Gulzar, 28, resident of Army Public School Area; Mohammed Ashraf, 22, resident of Korangi; Rafiq Maseeh, 50, resident of Jet Line; Younus, 55, resident of Cantt. Railway Station Area; Pervez, 34, resident of Sultanabad; Sohail Chaudhry, 27, resident of Clifton; Murad Khan, 50, resident of Clifton. (DailyTimes-B1, 24/09/2007) Rabies claims at least 2,000 lives annually Islamabad: Rabies — the poor man’s disease — claims 2,000 to 5,000 lives annually, according to data prepared on the basis of reported cases at the Health Management Information System (HMIS). According to the available data, though unofficial, more than 150,000 cases of rabies, mostly due to dog-bite, are reported from across the country annually. The HMIS also confirmed more than 100,000 rabies cases every year. The disease, which has caused more than 25,000 deaths during last six years, has not been given proper attention by concerned authorities. According to the HMIS, the reporting of the viral disease is extremely low in the country. The National Institute of Health has contributed a little to improve reporting and recording system of cases and on the subject of rabies treatment. “It shows how badly the disease is being ignored even when the number of deaths caused by it annually is hundreds of times greater than that of caused by AIDS,” said a health official working at the NIH on condition of anonymity. Almost all healthcare facilities across Pakistan providing treatment to victims of rabies has been declared obsolete by the World Health Organisation in 1992. Rabies is a severe viral disease caused by Rabdo Virus carried in the saliva of infected animals. It is transmitted to human beings through bites, scratches or licks even. It is fatal if not treated properly. It affects the central nervous system of most warm-blooded animals and victims of such animal bites have to be immediately vaccinated. After being exposed to the disease, the survival of the victim is almost impossible. In rabid animal bite cases, the virus spreads from the injured part to the nerves and onto the spinal cord damaging victim’s brain ultimately resulting in death. It causes convulsions, inability to move and strange behaviour developing hydrophobia (an extremely intense aversion to water, especially the fear of drinking water or other liquids) in the victim exposed to the disease. “Keeping in view the prevailing situation regarding rabies and animal bites (mostly dog bites), the Ministry of Health, WHO and the NIH started Rabies Prevention and Control Programme in 2000,” said National Coordinator of Rabies Prevention Programme Dr Shahab Akhtar Kazi, while talking to The News. The programme, however, has not yielded much so far and achieved a little only. When asked, D Kazi said, “For ideal treatment of rabies, availability of tissue culture (anti-rabies) vaccine and anti-rabies serum — Rabies Immune Globulin (RIG) — is a must. At present, the NIH is not providing tissue culture vaccine to healthcare facilities in Pakistan.” Throughout the country, healthcare facilities provide first aid to victims of rabies and follow the fourteen-injection sheep brain (sample type) anti-rabies vaccine course for their treatment. Injections are administered for 14 days on daily basis. In case of gap, the treatment gets started afresh. The administration of anti-rabies vaccine injections without any dose of rabies immune globulin makes the treatment almost ineffective and is medically known as ‘unethical treatment.’ The exact treatment process requires one dose of passive immunisation with RIG along with active immunisation with five doses of TCV over a 28-day period, an official at the NIH pleading anonymity told ‘The News.’ Joint Director and Chief Biological Production Division at the NIH Shahid Akhtar had earlier told ‘The News’ that the National Institute of Health can only provide sheep brain (sample type) ARV to hospitals and not the RIG. The NIH is preparing Equine Rabies Immune Globulin (ERIG) but only in little quantities, while no initiative has so far been taken by the NIH for preparation of Human Rabies Immune Globulin (HRIG). ERIG is processed in the body of horse, while HRIG in human body. HRIG is prepared nowhere in Pakistan. The joint director has also stated that in severe biting cases of suspect animal, RIG must be administered along with ARV and people should buy it from the market. The NIH prepares Anti-Rabies Vaccine (ARV) — sheep brain (sample type) vaccine only — for the treatment of rabid animal bite victims. As per 1980 Presidential Ordinance, the NIH is supposed to be the sole producer of vaccines and sera for prophylactic and therapeutic use and is responsible for meeting their requirement countrywide. Responding to a query, Dr. Shahab Akhtar Kazi said that in category-III of dog bite cases, in which blood oozes out of the wound, RIG must be administered to a victim. Category-III means single or multiple transferral bites or scratches that are contamination of mucous membrane with animal’s saliva, licks. 56 He stated that in rabid-dog bite case, an adult patient requires one vial of 10 ml HRIG that costs around Rs35,000 in the open market. Two vials of ERIG (20 ml) can also be administered in place of HRIG in case of an adult victim, however, the ideal treatment is administration of HRIG along with five doses of TCV. Two vials of 10 ml ERIG cost around Rs5,000 in the market. Incubation period of rabies varies widely, from four days to several years but general medical practitioners do not take this fact into consideration. Also the dog-bite cases, undoubtedly mostly from the poor section of society, cannot afford to have the ideal treatment that normally cost more than Rs35,000. “Health experts around the globe say that patients from many other diseases might not die, but a victim of rabies, if left untreated, would lead to death,” said Kazi in reply to a question. Health experts are of the view that the NIH may resolve the issue by preparing TCV and RIG in sufficient quantities and providing them to healthcare facilities, including rural health centres and hospitals, at affordable prices. They are also of the view that rabies is being ignored because the foreign funding for it is very small as compared to AIDS and other programmes like EPI. NIH Executive Director Maj-Gen (retd) Masood Anwar, when contacted by The News, said that the NIH is preparing ARV — sheep brain (sample type) vaccine. He claimed that the NIH is preparing ERIG too but in a little quantity due to small number of horses for the purpose. He was of the view that rabies can only be controlled by killing stray dogs and not by vaccination. Responding to a query, he said, the NIH is working on signing an agreement with a company on phased-manufacturing of TCV. There are some technical problems relating to terms and conditions of the agreement. “If the agreement is signed, in the first phase, we will import manufactured vials of TCV from abroad. In the second phase, we will import concentrate for the vaccine and prepare TCV here,” he explained. He added that after three years, the NIH will be able to prepare both the concentrate and TCV indigenously. When asked if the NIH fails in signing agreement with the company, how much more time it would take for the preparation of TCV, he said, the project would most probably take more than three years. “I am unable to say what would be the fate of the project then but I hope the agreement would be signed in a few days,” he said. (By Muhammad Qasim, The News-3, 25/09/2007) Protecting against dengue fever WHILE the adage “prevention is better than cure” can be applied to a number of illnesses anywhere in the world, it must be particularly true in Karachi’s case where dengue fever is once again on the march. In keeping with their past record, the city authorities have failed to respond to a threatening situation and have so far shown little inclination to eliminate its source — the mosquitoes. In many areas, overflowing drains and stagnant pools of leftover rainwater have provided an ideal breeding ground for these harbingers of disease. Considering that viral haemorrhagic fever, a more deadly manifestation of dengue, killed some 50 people in the city last year, besides causing severe health complications in hundreds of others, it is no surprise that the government has decided to reactivate the health department’s dengue monitoring cell. Hopefully, the data that the cell will collect will form part of a long-term strategy to control a disease that could become a regular feature after the annual rainy season in Karachi. In fact, it is feared that this year too, in the absence of proper facilities, the hospitals will have a difficult time handling the number of dengue fever cases coming in, leading to several fatalities. It is for this reason that general guidelines must be issued on a regular basis to inform the public of precautionary measures that can ward off mosquito bites. The use of long-sleeved clothing and insect repellent and sleeping under mosquito netting are some known precautionary steps to guard against mosquito bites. While individual efforts are important, one cannot over-emphasise the civic authorities’ responsibility of eliminating the dengue virus-carrying mosquito. This calls for a cleaning-up campaign in the city to drain off stagnant water collected in low-lying areas and empty plots. Such precautions will have the added advantage of protecting against the malarial parasite, again borne by mosquitoes. (Dawn-7, 26/09/2007) Govt instructing hospitals to hide Dengue cases The Sindh Government, ostensibly fearing the possible political implications of resurfacing of Dengue cases, has not only preferred to ignore the resurfacing of the deadly disease almost completely, but has reportedly instructed the city hospitals to hide cases Dengue, sources knowledgeable about this told The News on Tuesday. “The officials are preventing us from disclosing the exact figures,” one official of a hospital said on condition of anonymity. He said that the officials’ tone was not threatening but in a ‘polite way’ they requested us to hide the facts. He said ‘they (the officials) are not interested in listening to facts instead they were more interested in hiding the facts.’ He was of the opinion that the officials were probably reluctant to face reality because they had not taken any concrete effort this year to prevent the breakout of dengue cases. Contrary to claims of the officials that the number of patients was very low, the doctors said Dengue patients were increasing. A senior official of Civil Hospital, Karachi, said that over the last one week they were receiving suspected cases of Dengue 1-2 with high-grade fever almost on a daily basis. He said that one suspected dengue patient was also admitted in the hospital on Tuesday. Meanwhile, an official of AKUH said that from September 1 to 24, they had received total 36 patients, whose ages were from six years to 82 years. Out of them 28 were discharged and one patient died. The official said that in the last four days, the AKUH received 10 dengue positive patients but five of them were discharged after treatment. The doctors said if dengue virus bit the same patient, chances of his bleeding would be increased. They said there are three types of ‘strain’ and if same strain hits last year’s patient, his/her health complications would be increased. (The News-13, 26/09/2007) 57 Pollution can cause blood clots Prolonged exposure to air pollution can increase the risk of cardiovascular disease. Tiny particles in the air can not only impair functioning of lungs but also trigger clotting in the blood putting one at an increased risk for heart attacks and strokes. Lungs inflamed by pollution promote secretion of interleukin-6 (IL-6) by the immune cells and lead to inflammation. IL-6 has been shown to make blood more likely to clot. Such inflammation in the lungs caused by exposure to particulate matter can also lead to death from cardiovascular disease. To assess the impact of air pollution on cardiovascular diseases, researchers at the Northwestern University in Chicago, US studied the effects of air pollution in mice. This involved exposing mice to particles of air pollution collected by the US Environmental Protection Agency (EPA). Mice treated with a dose of well-characterised particulate matter of less than 10µM in diameter exhibited a shortened bleeding time, decreased plasma clotting times, increased levels of fibrinogen and increased activity of factor II, VIII and X. This clotting tendency was associated with an increase in the lung concentration of IL-6. The results highlighted the way in which exposure to air pollution could lead to the formation of blood clots. Mice exposed to pollution showed a 15-fold increase in IL-6 just 24 hours later. The time frame is important because some studies have shown that a spike in air pollution can boost heart attacks within 24 hours. Thus, besides lung disease, patients with coronary heart disease also need to avoid high levels of air pollution. The study appeared in the latest Journal of Clinical Investigation. (The News-20, 26/09/2007) Doctors demand drive against mosquito-borne diseases KARACHI, Sept 26: Expressing concern over the resurfacing of mosquito-borne diseases, including dengue fever in the city, the Pakistan Medical Association, Karachi, says heavy responsibilities lie on the government for eliminating mosquitoes. In a statement on Wednesday, the PMA said the outbreak of dengue fever/hemorrhagic fever was all expected, particularly after the rains, and as such government agencies should have gone for the eradication of mosquitoes on an emergency basis. “We have already indicated about the increase in the number of cases of dengue fever/ hemorrhagic fever in Karachi after the rain. Last year approximately 60 people had died (52 in Karachi) and more than 7,000 people suffered all over Pakistan,” said the statement issued by the general secretary of the PMA Karachi, Dr S. M. Qaiser Sajjad. It said the government should make arrangements at its hospitals for the diagnosis of dengue fever and also educate the public through the electronic and print media about the disease. The government should also provide platelets to all needy patients free through registered healthy donors. Private hospitals should also be told to give special concession on laboratory tests to diagnose dengue fever as custom duties had already been abolished by the government, it was added. Coming to the aspects of awareness about the dengue epidemic, the PMA said it had been providing awareness about preventive measures against dengue fever as there was no specific treatment for the disease. “This is a viral disease caused by a mosquito called Aedes Aegypti. It is interesting to note that it breeds only on the surface of clean water and bites humans in daylight, preferably just after and before sunrise and sunset. There is no transmission of the disease from human to human. “Its only occurs when infected (virus) mosquito (Aedes Aegypti) bites any healthy person. As this is not a contagious disease, there is no need to isolate the patient. Any healthy mosquito (Aedes Aegypti) can become infected when it bites an infected dengue patient. During his illness (till the fever subsides), the patient complains of fever, headache, pain inside the eyes, joint pain, body ache, rashes all over the body, bleeding from the nose, mouth, etc.” The PMA also stressed the need for making the public sector hospital laboratories more functional, efficient, and competitive. It also demanded the establishment of a diagnostic centre for all types of viral diseases. “There are a lot of cases of fever of unknown origin in Karachi which may be caused by different viruses,” it concluded. (Dawn-19, 27/09/2007) Steps urged to prevent dengue outbreak KARACHI, Sept 26: Viral haemorrhagic fever and dengue are spreading in almost all the localities of the city, and, as such, there is a need for both the community and civic agencies to initiate extra measures to overcome the situation, said doctors. A survey conducted by Dawn showed that the arrival of patients affected with haemorrhagic fever and dengue at various health-care units in the city was continuing. Patients ranging from six to 80 years of age are reporting from both the posh and less-privileged areas of the city, said sources from a couple of hospitals on Wednesday. Sindh Deputy Health Secretary Dr Shakil Malik told Dawn that 23 patients had been admitted to six government and private hospitals over the past 24 hours ending around 3pm on Wednesday. As many as 20 patients had been tested positive for dengue fever, he added. 58 The hospitals where dengue patients were admitted are Civil Hospital Karachi, Aga Khan University Hospital, Liaquat National Hospital, Ziauddin Hospital, Bismillah Taqee Hospital and Zainab Panjwani Hospital. The AKU received eight patients in its out-patient department on Wednesday. They all tested positive for dengue. A local laboratory has tested 24 OPD patients -- from August till date – out of which 12 are said to be positive and the rest negative. Dr Zaki Hasan, a consultant physician from Darul Sehat in Gulistan-i-Jauhar, said that his hospital had received about 15 dengue-positive patients, in addition to attending to a similar number of patients suspected of suffering from mosquitoborne diseases and viral hemorrhagic fever in the OPD, in recent weeks. All were residents of Gulistan-i-Jauhar, he said. According to a source, Gulistan-i-Jauhar faced problems of water accumulation due to rains or water line leakages. Patients reporting to other hospitals for dengue treatment belonged to Saddar, DHA, Gulshan-i-Iqbal, Model Colony, PIB Colony, Kharadar, North Nazimabad, F.B. Area, Faran Housing Society, Fatima Jinnah Colony, New Karachi, Nazimabad, Clifton, Korangi, Garden West and PECHS. Monitoring cell In the meantime, a health department official said that a monitoring cell pertaining to dengue fever cases had been reactivated, but preparation of any consolidated report based on information received from various hospitals would take at least another couple of days. “We are reminding the hospitals to take the issue of dengue-relevant data as a serious matter and keep updating the health department as a priority,” added the official. Dr Rafiq Khanani of the Infection Control Society of Pakistan feared that there were chances of an increase in cases of dengue fever just as in previous years in October due to hot weather conditions. “Civic agencies should carry out extra fumigation and cleanliness drives, particularly in areas from where dengue cases are being reported,” he added. Shedding light on the prevention of dengue-related diseases, he said that apart from mosquito control by standard methods both indoors and outdoors, the most important measures included prevention of mosquito bites by covering the body as much as possible and using mosquito repellents on exposed parts, especially taking care of children and the elderly. He maintained that proper management guidelines must be known to all doctors, including general practitioners, saying that plenty of oral fluids, especially fruit juices and ORS, should be given to patients, while antibiotics and anti-malarials should be avoided as these complicate the cases and decrease the platelet and white cell counts further and increase the chances of bleeding and delay the recovery of the patient. He said that all suspected, probable and confirmed cases of dengue and haemorrhagic fever should be reported to the relevant health authorities at the earliest. He also called for mandatory spraying of all long route transport vehicles to prevent other areas from getting infected mosquitoes. An expert in blood transfusion said that the government should also designate reputable diagnostic centres for confirmation of dengue virus in blood samples either free of cost or on subsidised rates so that the poor and the needy could move suspected cases for treatment at the earliest. (By Mubarak Alam, Dawn-17, 27/09/2007) Expiry dates need attention Expiry dates on products are taken seriously by consumers these days. Throughout the world when something is bought, the expiry date is always checked. If it’s past its date, the product is trashed without a second thought. Locally, however, many consumers are still trying to understand what expiry dates mean. It is only a certain segment that actually deems it important. The absence of expiry dates and the lack of awareness on the part of the consumers is a problem that requires attention on part of the government, and the authorities that deal with this issue. The Pakistan Standards and Quality Control Authority (PSQCA) is one such department that deals with the quality control issues. However, their performance is less than satisfactory. Even now in the market, several products are sold that do not have an expiration date. In fact some do not even have a manufacturing date so the consumer cannot even second-guess when the product will expire. Even though blind faith in expiry dates is hardly the solution, the fact that there is a complete lack of awareness about the issue makes the situation all the more worse. Consumers who usually visit government-run utility stores, for instance, do not know anything about product expiration. “I don’t care about expiration dates. I consider it a blessing if I actually get my turn in this long line of customers here,” said Hamid, a customer waiting his turn in a line of over 50 people. “I know that a commodity can rot after a certain period of time. For example, rice can get spoilt if it’s kept for too long, but I didn’t know that medicines and things like mosquito coils could also have expiry dates,” said another customer. The problem is not only confined to edible items but also to other products such as cosmetics. Dr Manzoor Qureishy, a physician, says that “cosmetics should not be sold after their expiry dates but they are. In fact, cheap copies are openly sold too. These can be tainted by oxidisation, heat or bacteria and can cause allergies or even infections.” In this regard, the packaging should also give directions on how to use the product after opening as well, because contact with air or light can change some products, rendering the original expiry date irrelevant. This means that the dates only tell consumers how long they can keep the product without opening it. However, besides some medicines such as eye drops, not many give the time within which the product can be used. Unfortunately, the manufacturers are let off easily. No one bothers to check up on the status of the products in the market. 59 There are no magistrates, watchdogs or product standard and quality monitors who decide that a certain product is not up to the standard and should, therefore, not be on the shelf. Thus, the consumers should form a platform or a watchdog association which can be responsible for surprise checks in the market. Even now, there are several brands of chips, and biscuits which are sold in large numbers but have no date on them. The culprits should be required to pay hefty fines and this should include shopkeepers who keep such goods on their shelves. In fact consumers should be told to check on other things required on food labels, such as the ingredient listings, net weight, country of origin and the name of the local manufacturer or importer. This can only be possible if the consumer platforms of Pakistan work on such issues with more fervour. Unfortunately with only three such organisations in the entire country and merely 18 courts — all in one province — fighting for consumer rights will always seem impossible. The bad news is that drug and product manufactures are not expected to change their standards too soon. For this, consumers should be aware of certain things. Signs of change should be noted, such as the change in colour after opening a product. As far as medicines are concerned, unless the instructions stipulate otherwise, a drug should not be kept for more than two months after opening it. Food companies generally adhere to directives about marking expiry dates but the consumer is left in ignorance when buying food sold in bulk — say a kilogram of rice from a large sack at the wholesale market. (By Xari Jalil, The News-19, 27/09/2007) PMA expresses concern over resurfacing of Dengue fever The Pakistan Medical Association (PMA) has expressed concern over the resurfacing of a mosquito-born disease known as Dengue fever in the city. The PMA said in a press release on Wednesday that the body had already warned about the possible resurfacing of the Hemorrhagic fever in Karachi after the last rains. The PMA has urged the people to take preventive measures against the viral disease. “The disease spreads when a mosquito called Aedes Aegypti bites human being, which breeds only on the surface of clean water,” it said and added that the disease doesn’t transmit from one person to another rather it only occurs when the infected mosquito (Aedes Aegypti) bites any healthy person. “Any healthy mosquito (Aedes Aegypti) can become infected when it bites an infected Dengue patient,” it said and added that fever, headache, pain inside eyes, joint pain, body ache, rashes all over the body and bleeding from nose and mouth are the symptoms of the disease. “The government should make arrangements at hospitals for diagnosing dengue fever besides informing the general public about the disease through electronic and print media,” it said. The government should also ask private hospitals to offer special concession on laboratory tests of the disease. PMA Karachi believes that every individual should aware about the cause, sign and symptoms, prevention and treatment of dengue hemorrhagic fever. The important point is to complete eradication of mosquitoes from Karachi by taking correct preventive measure through all government agencies and every individual, he advised. PMA condolence: The Pakistan Medical Association (PMA), Karachi has condoled the death of Dr Shoiab Tauheed, Prof of Physiology at Dow Medical College Karachi. The diseased was the life member of PMA Karachi and a regular contributor to Journal of Pakistan Medical Association. “He was an excellent teacher who had passion to teach younger and senior medical students and always worked to inculcate scientific thinking in medical students,” said a press release issued by PMA on Wednesday. (The News-14, 27/09/2007) Who killed the JPMC doctor? All out-patients departments (OPDs), except the emergency of Jinnah Post-Graduate Medical Centre (JPMC), remained closed on Thursday to mourn the death of a professor of clinical pathology and head of the College of Medical Technology (CMT) Dr Mubashir Sheikh who was gunned down near his clinic in Manzoor Colony on Wednesday night. The Ghaibana-e-Namaz Janaza (funeral prayer) was held at premises of the JPMC. Doctors held a condolence meeting where Dr Rasheed Jooma, executive director of the JPMC, and others expressed their sorrows. He termed the death of Mubashir Sheikh as ‘an irreparable loss’ for the hospital. The Doctors also formed an ‘action committee’ to assess security for the doctors and paramedical staff. They would also assess the security measures being taken by law-enforcement agencies. Senior doctors were seen wearing black armbands in protest against the prevalent lawlessness. They vowed to continue to boycott all OPDs for one hour from 9 to 10 a.m. daily till the arrest of the culprits. They announced to hold an important meeting of all doctors on Saturday to chalk out a future line of action, which is likely to be attended by the federal health secretary, said Dr Seemin Jamali, deputy director JPMC. Dr Rasheed Jooma, talking to The News at his office, said that the reasons behind the murder of the senior doctor were not understandable. Though it could not be said that Sheikh had expressed concerns about his security but instead he had suggested that we should become ‘cautious’ as certain students were ‘very different,’ Jooma said. Jooma also said that he didn’t think that the students could commit such a heinous act. He hinted that Sheikh might have been targeted by ‘locals’ (implying residents of the area where the incident occurred). However, Jooma hastened to add that it was for the investigators to determine the possible motive behind the gruesome incident. 60 The JPMC head said that he sent a reminder to both Rangers and the police authorities to make security arrangements for doctors and paramedical staff. A senior doctor, and a colleague of the late Dr Sheikh, told The News that the head of the CMT had expressed his reservations about security as, according to him, certain students were behaving in ‘rough manner.’ He said that these students had also subjected him to undesirable attitude at his office. The CMT, built around 3-4 years ago, has remained closed after the bloody clashes between two supposed rival student groups on 15 and 25 August respectively, which claimed lives of three students. Dr Shahid Iqbal Danish, deputy-director of JPMC, said that the deceased students belonged to the college of physiotherapy not the CMT. Shahid Sheikh, elder brother of Dr Sheikh, talking to The News at the late doctor’s residence in Defence, also said that his brother was concerned about his (own) security but he did not mention a specific threat. Talking about his brother, he said that Dr Sheikh was born in Karachi and became associated with the JPMC after graduating from the Sindh Medical College more than 20 years ago. “I raised him like my own son,” the elder brother Shahid said, adding that he was very saddened and that the four children of the family, including the one son of the deceased, were ‘gravely concerned.’ Meanwhile, Dr Mubashir Sheikh was laid to rest in a local graveyard in Steel Town. (By Imtiaz Ali, The News-13, 28/09/2007) Small groups of HIV+ people spreading disease in rest of population: study KARACHI: Karachi experienced an explosive HIV epidemic in intravenous drug users (IDU) in late 2003 and early 2004, which has spilled over into the male commercial sex networks, recent research has said. The ultimate size and impact of the HIV epidemic in Pakistan will depend on the effectiveness of prevention activities in these risk groups. This and other observations appeared in a study, ‘HIV risk in Karachi and Lahore, Pakistan: an emerging epidemic in injecting and commercial sex networks’ by A Bokhari et al. that was published in the International Journal of STD and AIDS in July. The groups sampled in Lahore and Karachi were (i) male IDUs: men who have injected drugs at least once in the past six months, (ii) female sex workers (FSWs): women who have engaged in selling sex at least once in the past three months, (iii) male sex workers: males who have sold sex at least once in the past one year, (iv) Hijras: individuals who were born biologic males or transgenders, and have adopted a predominantly female sexual persona and dress as women and (v) truckers and assistants: men driving trucks or assisting drivers along inter-state transport routes. A study of IDUs in Karachi in December 2003 identified that injecting drug users clearly had the highest HIV seroprevalence at 23%, followed by males (4%) and Hijras (2%). In total, 18% of IDUs in each city stated that they used a needle previously used by someone else at their last injection, and 24% in each city stated that they passed the needle they had just used to someone else. A total of 42% of Karachi IDUs and 62% of Lahore IDUs reported any sex with a woman in the previous year. Male-to-male sex behaviour was also commonly reported by IDUs in both cities, and 14% of all IDUs reported unprotected non-vaginal sex with a male partner in the past month. Condom use by IDUs was below 50% in all reports for male and female partner types. In total, 24% of MSWs in Lahore and 9% in Karachi had sex with a non-paying female partner in the past month, and 17% of those sex acts were covered by a condom. Hijras reported a median duration of commercial sex experience of six years in Lahore and 10 years in Karachi; 96% had sold non-vaginal sex to men in the past month, with a median of four partners in the past week (range 1–21). Forty percent (40%) had non-paying male non-vaginal sex partners in the past month, and they used a condom during 8% of last sex acts with these partners. Eleven percent (11%) had sex with a woman in the last year, and 25% of last female sex acts were covered by a condom. In addition to the male and female commercial sex partners, 15% of truckers reported sex with other non-paying female partners, with whom 6% used a condom at last sex. In this nominally heterosexual male risk-group, 22% of Karachi male truckers reportedly buying sex from a male or Hijra in the past year, compared with 7% in Lahore. Condom use at last male commercial sex act was under 1% overall for truckers, and under 15% stated that they could access a condom any time they needed one. Intervention contact in the past year was below 2% for MSWs, Hijras and truckers, under 6% for FSWs and 24% for IDUs in Karachi and 62% for IDUs in Lahore. The study in Karachi, which found one in 160 IDUs infected with HIV in late 2003, was carried out in the same population and geographic area as these studies in mid-2004. The dramatic rise to 23% HIV prevalence in Karachi IDUs in those few short months reflects the pattern of exponential growth possible in IDUs where needle sharing is common. It is not unusual for prevalence levels to reach 50% within the first two years of an IDU epidemic. Also, in contexts where needle sharing is common, the timing and pattern of take-off of an IDU epidemic depends more on networking characteristics rather than solely on individual risk indicators. The fact that the strongest statistical association with HIV infection was for needle exchange attendance in the past month, informs us that at least one of the highest risk networks has been successfully accessed. It should also be noted that twothirds of HIV infected IDUs sampled did not attend needle exchange in the past month. It is likely that sexual and nonmedical injection transmission will also be the predominant modes of HIV transmission in these drug injecting and sexual high-risk groups in Pakistan. It is noted that the injecting and sexual risk indicators in Lahore are at least as great as those in Karachi. Also, the identification of two HIV-infected IDUs in Lahore places that city in much the same position as Karachi in late 2003. 61 A WHO team estimated that unsafe medical injections may account for up to 7% of all new HIV infections in the region in which Pakistan is situated between 2000 and 2030. (DailyTimes-B1, 28/09/2007) Two govt hospitals reserved for patients 19 more dengue victims turn up KARACHI, Sept 28: As many as 19 fresh cases suspected of having contracted the deadly dengue fever have been reported from four different health facilities of the city during the last 24 hours ending at 3pm. According to sources in the monitoring cell of the Sindh health department, most of the prominent hospitals in the private sector are not cooperating with the relevant authorities in the compilation of dengue-related data. As many as seven cases have been tested positive for dengue at the Jinnah Postgraduate Medical Centre, one at the Civil Hospital Karachi, eight at Darul Sehat, two at the Aga Khan University Hospital and one at Bismillah Taqee. Meanwhile, the city government on Friday notified Abbasi Shaheed Hospital and Government Hospital New Karachi as the focal points for diagnosis and management of cases related to mosquito-borne diseases. CDGK sources said that these two major hospitals had been equipped with all the facilities required for the treatment and diagnosis of dengue fever. Besides, the city government had also provided diagnostic kits to all of its main hospitals so that patients could avail themselves of the necessary medical attention absolutely free of cost, the sources added. Free tests and treatment of dengue fever has also been arranged at the Civil Hospital Karachi and the Jinnah Postgraduate Medical Centre. All the private hospitals have been asked to refer cases of dengue and haemorrhagic fever to the Abbasi Shaheed Hospital or Government Hospital New Karachi to provide them timely and better treatment under intensive care. The health department has also chalked out a comprehensive programme to create public awareness about the causes and treatment of dengue and haemorrhagic fever. People have been advised to take necessary measures including installation of protective nets on doors and windows and carrying out fumigation inside their homes. Dengue fever is caused by a specific type of mosquito that bites only during daytime, especially around the time of sunrise and sunset. The breading of such mosquitoes takes place only in clean water containers, like drums, buckets, etc.There is no specific treatment for dengue fever. However, careful clinical management by experienced physicians and nurses frequently saves the lives of the DHF patients. With appropriate intensive supportive therapy, mortality may be reduced to less than one per cent. Maintenance of the circulating fluid volume is the central feature of the DHF case management. Fumigation drive from Oct 3 The city government plans to embark on a large-scale fumigation campaign in the city from Oct 3. The ongoing spray campaign of health department of the city government scheduled to end on Oct 2 will be continued with a fresh and more aggressive exercise from Oct 3 in all the 18 towns of the city. (Dawn-17, 29/09/2007) Middle class youth latest victims of HIV/Aids Raza Mohammad Baloch, 45, a resident of a low-income area in North Karachi was devastated when he was diagnosed with HIV positive six years ago. He had spent 15 years in Dubai as a driver and was making good money. He blamed his ‘careless attitude’ for contracting the virus. He was diagnosed with this disease in 2001 when he intended to get a mandatory visa extension. “Initially, I was terrified,” he told The News on Friday. People told him that treatment was expensive — Rs60,000 each month — and the disease was incurable. “I was extremely disturbed when my family members came to know about this disease and they started dissociating themselves from me,” Baloch recalled. “They (the family members) separated my things and even marked utensils ‘mistakenly’ so they would not get infected. Relatives also behaved the same way.” He said that, initially, he got treatment from hakims for more than one year and spent Rs200,000 on it but his condition did not improve. Raza Baloch said he came to know about the treatment when he came to the Civil Hospital. He said he also brought his family members to the facility where doctors informed them of the ways in which one contracts HIV. Raza, the father of five children, said now his health is improving and he is very careful. He said that since June 2006, the Sindh Aids Control Programme (SACP) was also providing him medicines free of cost. In April 2007, Baloch got job in a project being run by the Global Fund. Baloch is among the 200 registered HIV-positive patients at the Aids Control Centre in the Services Hospital. Other patients included a three-month-old child presumably infected by parents, a one-year-old baby and others. Dr Azra Abro, head of the Aids Control Centre said that the number of HIV positive patients was increasing. She said that now, mostly young men below 30 or above 30 years, belonging to the middle class are being infected with HIV positive as compared to when mostly old men were victims. She said that in the past, the patients came when their disease had reached at its fourth stage but now people are approaching the medical facility at an early stage of disease presumably owing to the influence of media. 62 She said that patients even belonging to Balochistan visit this medical centre for treatment even though this centre has liaisons with three other such facilities in Sindh including the Chandka Medical College, Larkana. She pointed out that the SACP is providing medicines to the patients free of cost since May 2006. Now, a test worth Rs12,000 is also being provided free of cost. To a question, she said that there were apprehensions that financial help to this medical facility might be reduced in future partly because of increasing number of patients and western countries gradual loss of interest in these disease, as the donors are focused on emerging health challenges. (The News-19, 29/09/2007) Murder of three students at medical college PCOs racket belived behind JPMC deaths The murder of three medical students in August has been linked to the operation of unauthorized PCOs within the premises of the Jinnah Postgraduate Medical Centre, hospital officials and investigators said on Monday. The deaths resulted from a series of scuffles which initially erupted on an argument over rates charged at a public call office (PCO) within JPMC premises. This led to the death of students, some of whom were deliberately targeted by activists of rival political groups. Officials alleged that some of the PCOs were owned and run by certain activist students. It was their operation and scuffles over their operation that ultimately led to the murder of three medical students and injuries to several others on August 15 and 25 respectively. “Though there could be many reasons behind the murders, we believe that bone of contention was the thriving business of phone booths and issues associated with this,” one of the top officials of the city’s biggest hospital told The News. He said one student organisation was allegedly running phone booths for some years, even before the ready availability of mobile phones. It was at one of these booths that a scuffle broke out between the activists of the supposedly rival student groups. As a first step, the JPMC administration has removed around 11-12 PCOs, which they claimed were being run illegally for the past several years. The JPMC administration took this step following the student clashes. Another senior official claimed that there were reports that certain student activists used to take protection money from unauthorized businesses on the premises of the hospital. The official said that removal of encroachments was a step at breaking this monopoly. Earlier, the administration had vacated the old hostel of what it called ‘undesirable elements’ that were residing there for many years. The official said that certain persons had also encroached on land of the JPMC and the administration had decided to pursue the same before judicial forums. Qamar Zaman, then SIO (Station Investigation Officer) of Saddar Town confirmed that a scuffle had erupted at the PCO inside the JPMC over charges of phone use, in which sticks were used, leading to the death of one young man. He claimed that it was a minor issue which led to the tragic death of three students one after the other. One medical student was killed on August 15 inside the premises of the JPMC, triggering widespread violence. All outpatient departments and the emergency ward remained closed for several days as an uneasy calm prevailed at the hospital. When the situation was returning to normalcy, another bloody clash took place at the hospital premises that led to the death of another student and injuries to several others; one of them later succumbed to his injuries. It also enhanced the sense of insecurity and anxiety among the doctors and other hospital staff. Consequently, both the Dow Medical College and Sindh Medical College were also closed for several days. The boys’ hostels were vacated from students and ‘outsiders’, causing inconvenience to genuine students, especially foreigners. Subsequently, extra-ordinary security arrangements were made to provide security to the doctors and other staff, who were reluctant to rejoin their duties. Since then, an APC (armoured personnel carrier) of Rangers had been deployed at the JPMC and Rangers also remain alert at the main gate of the newly-built emergency and accident ward of the JPMC to meet any eventuality. However, the death earlier this week of a senior doctor (box) has once again raised fears about the safety of staff and patients at the JPMC. (By Imtiaz Ali, The News-13, 29/09/2007) Manzoor Colony residents miss the ‘good’ doctor KARACHI: Dr Mubashir Shaikh, a senior pathologist at JPMC who was killed two days ago, is being missed at Manzoor Colony where he ran his clinic. “Whenever we had any kind of medical problems or needed surgery, Shaikh was always there to help us and got us treated from Jinnah hospital,” said one shopkeeper. Fayyaz, whose shop is located right opposite Shaikh’s private clinic, said they still couldn’t believe that he was killed. When Fayyaz heard the gunshots, Wednesday, he thought it was the noise of firecrackers from children playing outside. However, soon after the shots were fired, people shouted that Shaikh had been killed. Another shopkeeper said that most people had gone for prayers at the time. Shaikh not only looked after the residents of the area, but also helped the poor, they said. Shaikh’s elder brother, Dr Shahid, is the owner of the shops located on the same street. According to residents, Shaikh had opened his clinic in one of these shops before moving into the present one. 63 He did not have any enemies in the eighteen years he spent in this area, one of the residents remarked. The patients and people of this area mourn his death along with his family members and demanded the authorities to catch the culprits behind the murder. APP adds: Doctors and other medical staff of the Jinnah Postgraduate Medical Centre (JPMC) registered their one-hour token protest from 9 a.m. to 10 a.m. on Friday against Shaikh’s murder. They did not attend to any patient of the hospital. However, emergency and accident cases were treated. JPMC will hold a condolence today at 10:00 a.m. (By Shahzad Shah, DailyTimes-B1, 29/09/2007) Three Dengue fever deaths in as many days Provincial Minster for Health Syed Sardar Ahmad on Saturday confirmed that Dengue fever had so far claimed three lives within as many days in Sindh. Addressing a press conference on Saturday, he said that the federal government had been asked to allow duty-free import of kits that identify Dengue fever in a patient so that diagnosis could be cheaper. “So far three casualties have been confirmed and 10-20 patients are daily visiting public and private hospitals, 50 per cent of whom are Dengue-positive,” he said, and regretted that Dengue fever data was not available from small clinics. Were this data collected, the number of cases could rise, he admitted. Sardar Ahmad said that private clinic operators had been called to hold a meeting with him on Monday in which they would be asked to keep providing daily feedback about the Dengue cases in their areas so that targeted action could be taken. Regarding the government’s performance so far to control the outbreak of the disease, he said that all Executive District Officers (Health) had been directed to initiate fumigation campaigns in their relevant districts while the EDO, Health, Karachi, had already provided 20 spray machines to carry out the fumigation in town. Prevention is more important in this regard as mosquitoes carrying dengue virus usually breed in less polluted stagnant water, he added. The Dengue fever Monitoring Cell on Saturday reported 15 new cases of Dengue fever, bringing the total number of hospitalised patients to 49 in Karachi. The Coordinator of the Cell and Additional Health Secretary, Dr Shakil Malik, giving details of the situation, said that the Jinnah Post-Graduate Medical Centre received four new cases followed by two each in Liaquat National Hospital, Bismillah Taqee Hospital, and Zainab Panjwani Hospital, on Saturday. As many as 11 Dengue-positive patients were said to be under treatment at Liaquat National Hospital, 16 each at Ziauddin Hospital and Jinnah Post-Graduate Medical Centre and five at Bismillah Taqee Hospital. (The News-14, 30/09/2007) OCTOBER Bin Qasim maternity home handled no case in 20 years KARACHI, Sept 30: No delivery has ever taken place in the sole government-run maternity home in Bin Qasim Town since its inauguration two decades ago. With a population of 315,684 people, the town has no government hospital either and people have to travel long distances to reach public health facilities in the city. This arduous journey at times risks their life. The town’s only public sector maternity home being run in Union Council Ghaggar has been without water, electricity and gas for years. The poor expecting mothers have to rely on unskilled dais (traditional birth attendants) at the time of delivery. In case of complications, they have to rush to government hospitals in the city. “There have been incidents in the past when women died on their way to a hospital. Besides, a pickup charges Rs1,200 for a trip to the city which poor people simply can’t afford. This health facility never worked like a maternity home and no delivery has ever taken place here. The issue has been brought to the notice of government officials many times but to no avail,” said Mohammad Khan Kalmati, a social worker of the area. According to him, Union Council Ghaggar where the maternity home is located has 70 small villages with a total population of around 40,000 Baloch and Sindhi people. Majority of the people have been living here for ages while others are nomads. The predominant profession is factory labour. Sharing his views, the maternity home’s in charge, Dr Shaheen K. Shaikh, says: “Without electricity and water, it’s no wonder that no delivery ever took place here. We feel bad about not serving the basic purpose of this facility which is supposed to run 24/7,” she says. She recalls that the maternity home has functioned without any doctor many times in the past while there were times when she sat alone in the maternity home without anyone for her assistance. Now the staff comprises a doctor, midwife and lady health visitor though they all leave by 2pm. Daily visited by 50 women, the health facility has no water connection. A water tank that exists on its premises has not been cleaned for long and visitors avoid drinking that water. Women generally visit the facility for common complaints like gastric problems, flu and iron deficiencies, for which they are given medicines free of cost. 64 “There is no emergency aid available there nor any facility to deal with neonatal and post natal complications. The health set-up does not serve any purpose other than a dispensary. With low literacy level and lack of awareness, women look at pregnancy as a routine matter and do not seek medical advice for the purpose even if they are told to do so,” she observes. She cites abject poverty and lack of husbands’ support as the two major factors for the delay in seeking medical help which often lead to complications. For investigation, women are referred to Gharo Rural Health Centre or Makli District Hospital. Tuberculosis, according to her, is quite common especially among the residents of Mayyo village where two to four people in a family are suffering from the disease on an average. Skin infection is also common due to exposure to chemicals and toxic fumes in factories, she adds. Regarding the socio-economic conditions of area people, midwife Razia Begum says the drug menace has deteriorated their financial and health status further. “Now even small children have taken to drugs. Women do embroidery and sell eggs to meet their daily expenses. Acute economic stress has a direct bearing on the children’s development and they don’t seem like growing with age,” she adds. Area residents complain that the absence of any fully-fledged hospital in the town has given impetus to the business of quacks and faith healers. “Quacks take rounds of villages on bikes and sell cheap medicines and injections for quick relief. There is no check on their activities,” they disclose. They also criticize the staff posted at the nearby basic health unit where they take their children for immunization. Patients generally don’t get proper medicines and at times there is no doctor, they claim while citing the reasons for lesser number of visits. When asked about the improvement plans for existing health facilities, Town Health Officer Irshad Khan said he had written letters to the Executive District Officer Health and Karachi Nazim about the matter, but unfortunately no action had been taken so far. “We are aware of the inconvenience being caused to the people and that’s the reason a new maternity home has been constructed in Razzakabad that will be made functional in a month or so. It will be equipped to carry out normal deliveries as well as operations in complicated cases. The feasibility of a 100-bed hospital on the National Highway has also been approved,” he said. There were 40 health facilities, including 27 district council dispensaries, 13 BHUs and 12 Sindh government dispensaries in Bin Qasim, he said, admitting that there was no hospital in the town. “These infrastructures have fallen victim to official neglect and the system of up-gradation is slow. As a temporary arrangement for the maternity home in Ghaggar UC, we had taken power lines from the neighbouring areas, but the cables were either cut or stolen,” he regretted. (By Faiza Ilyas, Dawn-13, 01/10/2007) Drug prices in Pakistan lower than in India: PPMA The Pakistan Pharmaceutical and Manufacturers Association (PPMA) on Sunday claimed that a majority of the drug prices in Pakistan are 20-70pc lower than in India. It said that out of the top 100 products 75pc of them are priced at 20-70pc lower than in India such as Augmentin (a popular antibiotic) and Insulin etc. PPMA said nearly 20pc of the products are smuggled and not exported to other countries like India, Bangladesh, Africa, Far East etc. “This is because the prices of majority of the pharmaceuticals are very low in Pakistan,” it said. In neighbouring India and Bangladesh, the prices of only 78 products are controlled and the remaining decontrolled. This system has seen the prices being reduced downward due to the free market economy mechanisms, PPMA believed. The input costs for production and manufacturing in Pakistan are one of the highest in the world. Nearly 90pc of the raw materials are imported which are subject to customs duties and high logistics, transportation and insurance costs. The cost of power and water in Pakistan (which remains highly unreliable) is twice as much as it is in China and is about 20pc higher than in India, the PPMA said. And pharma production is highly power intensive due to the air and water filtration requirements and heavy machinery. Even steel and cement in Pakistan are more expensive than the USA, it added. The interest rates for factories to invest in capital as well as to fund its working capital are one of the highest in the region and the world, the pharma industry claimed. “In spite of these high costs of inputs and rampant inflation, not a single price increase has been granted to Pakistani Pharma Industry since December 2001,” said the PPMA. It added that the drug prices have remained the same due to free market mechanisms and competition, while the price of every commodity has increased in Pakistan in the past several years. But the PPMA admitted that certain medicines such as Zantac and Losec and a few others are indeed highly priced. (The News-14, 01/10/2007) Villagers suffer as malaria kills five KARACHI, Oct 1: A large number of the inhabitants of coastal villages are desperately awaiting government help against malaria, which has claimed five lives over the past 15 days. Worst-hit is Deh Allah Bano in the Gabo Pat union council, Keamari Town. The epidemic has crippled livelihood activities in the affected areas and dozens of families are battling disease and hunger. 65 “Every second person is ill with mild to high-grade fever, headache, dizziness and nausea,” said Gul Khan, a primary school teacher in Haji Noor Mohammed village, who is ill himself. “Five people, including three children, have died but no government aid is in sight.” Referred to as the ‘Thar of Karachi’, UC Gabo Pat has a population of around 250,000 people but enjoys no basic facilities or civic infrastructure. The people live in small huts close to their cattle and survival depends on fishing and scanty cultivation. Village ponds filled by the annual rains constitute the only source of drinking water, which puts villagers at great risk of water-borne diseases such as diarrhoea and gastroenteritis. Malaria-related deaths have occurred in Ali Baksh, Moosa Daulat Faqir, Hussaini Sahib Khan, Haji Mohammed and Noor Mohammed villages, all located in Deh Allah Bano which has a total of 18 villages. Each village has a population of over a thousand people. No medical aid at hand While the residents this writer spoke to did not know the name of the illness resulting in the deaths, they said that mosquitoes had invaded heir homes and the victims suffered fits and severe fever. They had been taken to a doctor once but abject poverty did not allow further treatment. When this correspondent visited the villages, dozens of families had left to seek treatment in Mauripur since all the government-run dispensaries in UC Gabo Pat have been closed for a long time. “Mauripur is a 45-minute drive from here,” said 50-year-old Rehmatullah. “Finding transport is a major problem and delays treatment. The local bus leaves at 7am and returns at 4pm. In case of an emergency, we have to arrange private transport which can cost between Rs600 and Rs800 a trip,” he said, adding that the disease had deprived the villagers of what little they earned. “The men are unable to fish while the women have abandoned cultivation,” said Hasina, who has five children and lost her husband after last year’s rains. “Although every monsoon is followed by disease in our villages, this season is proving much tougher in terms of sickness and fatalities.” That the illness threatening the lives of these citizens is malaria was confirmed by Dr Kishor Kumar, who runs a private clinic in Mauripur. “Over the past fortnight, I have treated over a thousand malaria patients, mainly from the coastal villages. These poverty-stricken people are vulnerable to disease since most of them suffer from malnutrition and anaemia. It is common for children to show stunted growth and low-weight birth,” he said. According to a member of the Pakistan Fisherfolk Forum, Surriaya Talpur, the town health officer was informed of the situation and he promised a free medical camp as well as a fumigation drive in the area. “But so far, there has been no government action,” she complained. “The situation demands immediate attention since delays can cost more lives. Furthermore, the people should be provided alternative income resources until they are able to resume their jobs.” (By Faiza Ilyas, Dawn-17, 02/10/2007) Dengue death toll rises to six KARACHI, Oct 3: Another patient, who was tested positive for dengue fever, died at a hospital here on Wednesday, when the number of in-house viral hemorrhagic fever cases touched the mark of 113 in 12 city hospitals. According to an official of the provincial health department, the victim was a 26-year-old woman from Kharadar. She was rushed to the Aga Khan University Hospital, besides six other dengue-positive patients from different localities during the last 24 hours ending at 3pm, on Wednesday. A 25-year-old woman, resident of the Defence Housing Authority, had died of dengue fever at the AKU about two weeks ago. Health experts fear that the situation might spin out of control and the hospitals may see a surge in the number of dengue patients this year. Patients, both male and female, with ages ranging from 6 to 82 years, are coming from across the city, which indicates the prevalence of poor hygienic conditions, particularly after the monsoon rains, and poor disposal of garbage and below the mark fumigation in the city. The health department’s data about dengue fever cases shows that the number of cases reported to hospitals is notably high. Against a figure of 250 or so of VHF or DF patients recorded in August and September of 2006 in the province, now hospitals have registered as many as 502 cases in Karachi, of which 231 have been tested positive for dengue fever. Four deaths occurred in September this year in the city. Reports from hospitals suggest that the VHF/dengue epidemic has made inroads almost in all localities. Patients, including children continued to be taken to hospitals from the DHA, Gulshan-i-Iqbal, Garden East, Kharadar, PECHS, North Karachi, Malir, Clifton, F. B Area, Gulistan-i-Jauhar, University Road, Landhi, New Karachi, Akhtar Colony, Gilgit Colony, Shah Faisal Colony, Korangi-4, Jacobline, Korangi 100 Quarters, Jauhar Complex, Sherpao Colony, Korangi Industrial Area, Sherabad in Landhi, Qayyumabad, Tariq Road, Ghausia Market in Malir, Keamari, Chanesar Goth, Karsaz, Saddar, Model Colony, PIB Colony, North Nazimabad, Faran Housing Society and Garden West. According to the health department, with the latest fatality caused by the mosquito-borne disease, dengue fever and dengue fever syndrome, the number of deaths reported to it reached five. The reporting cell on dengue has also approached a hospital for the confirmation of the death of the woman from the DHA, which has already been reported in a section of the press, said an official. The breakdown of dengue patients admitted at different hospitals, as reported to the Sindh health department’s dengue fever reporting cell, was as follows on Wednesday: Aga Khan Hospital -- 7, Liaquat National Hospital -- 15, Civil Hospital -- 6, Ziauddin Hospital -- 16, JPMC -- 41, Bismillah Taqee Hospital -- 10, National Institute of Child Health -- 2, Baqai Hospital -- 2, Patel General Hospital -- 5, OMI Hosptal -- 66 3 and Usman Memorial Hosptal -- 2. Health experts said there had been an increase in the number of patients affected by dengue fever virus in F. B Area, particularly in Gulberg Town, in the recent days. They say that the only way to prevent dengue infection was to eliminate mosquitoes. The world health body and the federal health ministry should also probe the problem of viral infections in the city, which mostly has hit youngsters. They say the authorities, including the international bodies, should look into the matter seriously and ensure inspection of residential places and surrounding areas as well to assess the root-cause of the cases. The locality of patients and their living and working conditions, income, health facilities available to them and the overall environment and hygienic conditions around their houses and schools, needed to be known, said a senior doctor. In the meantime, Karachi DCO Javed Hanif Khan presided over a meeting on Wednesday to review the measures taken by the CDGK against the spread of dengue. The meeting decided that in addition to the Abbasi Shaheed Hospital, the Sindh Government Hospital in New Karachi and some other major hospitals of the city government should provide the citizens with free facilities for blood tests for detection of dengue virus. The meeting also agreed that the fogging and insecticide spray exercise would be expedited in all parts of the city, including suburbs and rural sections, particularly where puddles, nullahs and rivers existed and sewerage manholes lay open. (Dawn-17, 04/10/2007) Gynae services at CHK still suspended KARACHI, Oct 3: Women requiring urgent medical attention during pregnancy and labour are being turned away by the Civil Hospital Karachi (CHK) because the elective operation theatre suspended services three weeks ago owing to conditions rendering surgical procedures dangerous, such as sewage dripping on to the operation table, non-functional lights and falling plaster. Furthermore, all gynaecological, obstetrical and emergency labour services have remained suspended since September 24 because doctors refuse to work in the emergency operation theatre or the labour room until their concerns are addressed. The out-patient department alone remains functional but the hospital is taking no admissions. The CHK Gynaecology and Obstetric Department is one of the few places where emergency departments operate round the clock, but doctors have stopped working in protest against what they call the administration’s “persistent apathy towards the dangerous conditions prevailing in the elective OT.” Meanwhile, over 30 patients a day, including emergency cases, are being referred to other hospitals at the time of delivery. As a doctor pointed out, “in the struggle between the doctors and the administration, the direct victims are the patients.” Patients visiting the facility have urged the authorities to provide a 24-hour emergency service until the dispute is settled. Dangerous conditions Nevertheless, the complaints appear justified. Giving journalists a tour of the elective OT for both major and minor surgeries, Professor Dr Ghufrana Umar Memon pointed out the sewage from upper storey bathrooms leaking into the theatre and dripping on to the lights and the operation table. “This dirty water and plaster has fallen on patients and surgeons in an environment that is supposed to be sterile,” she informed. “It causes a very high incidence of infection and increased morbidity in all the post-operative patients but the administration, which has been aware of the issue since 2004, has shown no concern.” Dr Memon said that one of the overhead lights malfunctions frequently, forcing the postponement of major surgeries. In the minor operation theatre, the operating tables and lights do not function properly and there is only one anaesthesia machine. “The autoclave in the theatre is small and rusted, so we cannot sterilise all the equipment,” she stated. “We boil the rest but that doesn’t kill all the germs. The power supply is erratic and the theatre does not even have a supply of water.” She also complained that all surgical specialities had been shifted to the new OT complex except those of the gynaecology/obstetric department. Doctors say that they have repeatedly informed the management about the elective OT’s deplorable state and other issues such as staff shortages and inadequate emergency services, but have received no positive response. As a last resort, they discontinued all gynaecological, obstetrical and emergency labour services. Injustice to the poor Although Dr Memon claimed that only cases requiring surgery were sent to the Jinnah Postgraduate Medical Complex and Sobhraj Hospital, other doctors at the department said that no case had been attended to since September 24. “All three departmental units are closed,” said one of the doctors. “Yesterday, a woman arrived with a ruptured uterus but was referred elsewhere. Yes, the elective OT is in shambles but the emergency operation theatre and the labour room are state-of-the-art. Doctors have been very insensitive in stopping these services as well.” Her views are endorsed by the patients, one of whom termed it “a grave injustice to the poor.” Upon being contacted by Dawn, the chairman of the Board of Governors of the CHK and the Lyari General Hospital, retired bureaucrat Abu Shamim Arif promised that repairs had been initiated at the elective OT and the matter will be resolved by the end of the week. “However, the protesting doctors should realise that having a project approved by the government requires time,” he said. “In the June to September quarter, the hospital has not received a single penny from the government for repairs.” In terms of shifting the elective OT to the new OT complex, Mr Arif said that there was no vacancy in which the ward could be transferred. He added that doctors should remember that the new complex was funded not by the CHK but by the Dowites, an association of former Dow Medical College students. (By Faiza Ilyas, Dawn-17, 04/10/2007) 67 Dengue death toll climbs Another dengue fever patient died in the city on Wednesday, bringing total number of deaths to five since August 2007, according to the Deputy-Secretary, Health, Dr. Shakil Mullick. The number of cases of dengue has been rising consistenly over the past couple of months with the government unable to come up with a concerted strategy to deal with the problem. A 26-year old woman, hailing from Kharadar, was admitted to the Aga Khan hospital on Tuesday night where she died on Wednesday. Both the hospital administration and the health official said her name was withheld on the insistence of her family. The official said around 32 more dengue-affected patients were admitted in different hospitals in the metropolis on Wednesday, bringing the total number to 502 so far since August. However, this high death toll has neither woken authorities in the provincial capital nor in Islamabad. Most officials consider this as routine and have not come up with a plan to fight the problem in an effective manner. Private hospitals are now receiving a rising number of patients. An official of the Aga Khan University Hospital (AKUH) said they received seven more dengue-positive patients on Tuesday night. Of these, one (woman) expired. One got discharged and five dengue-positive patients are still admitted at the AKUH. The official said they had received a total 57 dengue-positive patients between September 1 and October 3, ranging in age from 6 to 82 years. Two of them died. Around 46 patients were discharged while nine are still admitted. An official of another private hospital said they were receiving two to three patients daily from various localities. APP adds: Dr. Shakil Mullick said on Wednesday that 224 patients were found to be dengue-positive, 195 negative and results for 76 were awaited. This figure differs slightly from those collected independently but at the same time confirms the seriousness of the issue. “Four of these patients were those who died of the ailment including three women and one men - all below 40,” he said. As for the fresh cases reported at 12 different hospitals of the city, Dr. Malik said 25 new cases were referred to these hospitals and 109 were either admitted the same day or hospitalised for a couple of days. Those hospitalised include people reporting for persistent high fever and extremely low blood platelet count or registered with profuse bleeding besides severe dehydration. Dr Shakil said an increasing number of patients were being reported from Federal B Area, Defence, and Clifton, followed by other areas. It is believed that the patients that are coming from Defence and Clifton may be due to the large number of ponds that have been left by the Cantonment Board Clifton and the CDGK in open plots of these areas. These are ideal breeding grounds for the killer mosquitoes. Giving a detail of cases received at different public and private sector hospitals of the city, he said six new cases were reported on Wednesday at the Civil Hospital, Karachi, which already has six victims admitted. Two new admissions were reported at National Institute of Child Health (NICH) while two new cases were brought to Liaquat National Hospital with 15 already admitted. Forty-one were said to be hospitalized at the Jinnah Post-Graduate Medical Centre for the past few days with eight new cases brought on Wednesday. Ziauddin Hospital reported 16 admitted and a fresh case, Bismillah Taqee three new cases and 10 already admitted, Patel Hospital one new case and five already admitted, OMI Hospital three admissions and no new case, Usman Memorial Hospital three already hospitalised and no fresh case and Darul Shifa two fresh cases. Answering a question regarding dengue fever among children Dr Shakil said the cases often go unchecked as children as a routine report with high fever, cold and cough and are put on proper medication - with due care to address dehydration. Doctors tend to be cautious not to resort to antibiotics or Anti-malarials, he said, mentioning that in specialised facilities where chances for wide range of tests are available such patients can be easily diagnosed. (The News-13, 04/10/2007) Faulty drug-buying law changed but not implemented yet KARACHI: The Public Procurement Regulatory Authority (PPRA) Rules of 2003 were recently amended after loopholes in the laws created problems for Sindh and city government hospitals. The PPRA rules did not specify how much hospitals could spend on direct procurement (emergency local purchases at minimal rates) as opposed to procurement via rate contracts (long-term agreements for day-to-day medical supplies). “Due to this loophole, objections were raised when hospital receipts were sent to the AG Sindh for auditing. They said that payments could not be made because the law did not specify how much of its budget a hospital could spend on local purchases. Hospital medical superintendents came to us and asked us to rectify this loophole because delayed payments meant problems in procuring required medication and equipment. Amendments were therefore made and now hospitals can only spend 25 percent of their budgets on local purchases, and 75 percent on purchases via the rate contract system,” Sindh health department deputy secretary (procurement), Dr Abdul Jabbar Memon, told Daily Times. Local purchases are used for buying drugs and other items from chemists around hospitals in case of emergencies while the rate contract system is used for the purchase of medicines and related items required for the day-to-day running of the hospital. Both systems require companies to bid for tenders. 68 For local purchases, pharmacists and chemists around specific hospitals bid for the appropriate tender, and the selected bidder agrees to provide the required medicines at the lowest possible costs in cases of emergencies, such as natural disasters. In case of a rate contract, pharmaceutical companies have to fill out a detailed three-page form at the time of bidding. The forms judge them according to the capabilities of their personnel, facilities, financial position, managerial criteria, relevant experience and past performance. In the past, the Sindh health department’s procurement division would make a list of pharmaceutical companies that fulfilled the required criteria. These companies then provided the required medication and equipment to hospitals on the rates agreed upon in the contract. “Since last year, however, hospitals have been issuing tenders and checking bids themselves. They decide what they want and where they will get it from. The only thing that the procurement department is required to do is monitor the process to make sure that the hospitals are following the criteria mentioned in the PPRA rulebook,” Dr Memon said. According to the old Sindh purchase manual (issued in 1991), all Sindh government hospitals used the ‘25/75’ rule for purchases, Dr Memon said. “This brought in some discrepancies, however,” sources in the Sindh health department said, without elaborating on what the discrepancies were. The PPRA rules, which overrode all previous policies, were then implemented in 2003. “While these rules removed the discrepancies which had been the result of the older rules, they did not clarify how much of a hospital’s budget could be used for local purchases, and how much was to be allotted for the rate contract system,” sources said. “Every hospital used its own discretion in this matter.” The Abbasi Shaheed Hospital (ASH), for instance, currently allots 20 percent of its budget for local purchases, and 80 percent for rate contract, ASH Deputy MS Dr Nadeem Rajput told Daily Times. “The new rule will not have an effect on our budget, because we’ll just reallocate the amount – the budget is fixed,” Dr Rajput said. “We’ll implement the new quotas as soon as we receive an official notification about the changes. We have not been notified yet.” The new rule will, however, remove issues that hospitals had with the AG Sindh audits because of the loophole in the preamended PPRA rules, and money will now be available on time, a medical superintendent at a Sindh government hospital said, on condition of anonymity. According to the last report received Wednesday, however, changes in the PPRA laws have yet to be implemented. “As far as I know, the laws have not been implemented completely. That portion is still in the works,” Deputy AG Sindh, Khalid, told Daily Times. (By Urooj Zia, DailyTimes-B1, 05/10/2007) Rabid dog bites 10 people in Korangi KARACHI, Oct 6: As many as 10 persons bitten by the same rabid dog in Korangi were brought to the Jinnah Postgraduate Medical Centre for anti-rabies treatment on Saturday. Dr Seemin Jamali, In-charge of the JPMC’s emergency section and anti-rabies cell, said that victims, aged from four to 40 years, kept reporting to the hospital till the afternoon. The majority of the patients were children. She said that the patients were given vaccines and immune globulin free of cost and discharged later on, with the instruction that they should complete the treatment comprising anti-rabies vaccines in the next 90 days at the hospital. She mentioned that the JPMC received dog-bite cases from time to time and warned parents to pay special attention to their children, as they constituted a large number of dog-bite victims. “About six weeks back, we received 11 people, including children, who were bitten by a dog in Landhi,” she recalled. (Dawn-17, 07/10/2007) Maternity services in Baldia fail to take off despite Unicef help KARACHI, Oct 7: For the executers of the Women’s Right to Life and Health – a Unicef project being run in the city – Baldia Rural Health Centre’s experience was a sheer disappointment. Despite their best efforts and support with provision of all required facilities for basic obstetric care last year, the health unit has failed to launch maternity services. Located in UC-7 of Baldia Town, the health centre was founded in 1980s as a dispensary. Since there was no maternity home or government hospital in the town, the health centre was envisaged to deliver maternity services. Though rooms for doctors, nurses and patients were built on the first floor of the building in later years, the project owing to official neglect could not be completed. Last year, Unicef extended its support to the health centre under its project, Women’s Right to Life and Health (WRLH), which was aimed at improving the status of maternal and newborn health by helping the existing government health units remove lacunas and ensure maternity services available to local population round the clock. Under the project, being run in 12 hospitals and maternity homes, support was provided in all problematic areas that had remained an obstacle in the provision of maternity services. That included a labour room equipped with all necessary paraphernalia, for instance, delivery tables, oxygen cylinders, surgical equipment, trolleys, a baby warmer, a suction machine, bedside screen as well as a stretcher and a wheel chair. To solve the chronic problem of water shortage at the health unit, a fiber water tank was installed. The international donor agency also provided support in renovation of the building, setting up a private ward, deputing two midwives and arranging monthly visit of a gynaecologist who could motivate and guide the staff properly. Despite the donor agency’s heavy investment of financial and human resources, Baldia Rural Health Centre failed to have a single delivery and made little progress. 69 Former project manager Mumtaz Ahmed said: “For us, Baldia RHC experience is an utter failure. We tried to fulfill all their needs, but the result was naught. There is a need to ponder why an adjacent private hospital successfully runs maternity services while this health unit has failed to have a single delivery despite having a strong government-foreign donor’s assistance for a complete year,” he observed. Reasons of failure Elaborating upon the reasons why the project couldn’t take off, WRLH Project Director Dr Shershah Syed said the government didn’t provide them with the skeleton staff needed to run the maternity home, a problem common at all maternity homes of the city. “We are failing to run maternity homes in Sindh because of government’s lack of political will. The government is too busy in mega projects and seems to have no interest in improving the health status of the poor women,” he said. Support withdrawn Upon seeing no progress, the WRLH eventually withdrew its support some months ago. One midwife has already left the place on finding a better job since her expertise were not being utilised here. Today, the two-floor building of health centre with a plenty of locked rooms stands as an evidence of wasted resources. One can still see the plaque placed on the first floor announcing the inauguration of maternity services by former health minister Shabbir Ahmed Qaimkhani. With an average of 45 patients at the OPD daily, the health centre offers little to the poor who have to spend a lot of money on diagnosis and treatment at private concerns. Shouldering burden When asked about the state of affairs, Baldia Town Health Officer Dr Arif Niaz admitted that shortage of staff was the real problem. However, he said, the RHC was the only dispensary in the entire town whose SNE (Schedule for New Expenditure) had been approved. The SNEs for four other government health units in the town still await approval. Thus, the budget allocated and doctors and staff deputed for this health centre were distributed among all the rest. “I have been trying for years to get the SNE of other government health units approved, but to no avail,” he regretted. The health officer said though a hospital structure was constructed in the area he was not sure when the project would complete and the hospital would be functional. Demanding immediate approval of SNEs and timely delivery of medicine stocks, he said, “We appeal to the government to get the four health units, under the occupation of Rangers and some nazims, vacated so that public could get relief as the town having about 800,000 population had no other government hospital and maternity home.” (By Faiza Ilyas, Dawn-13, 08/10/2007) Toll from toxic liquor tragedy tops 50 As many as 50 people who consumed toxic liquor on Sept 19 have expired so far, a police official told The News. Amongst them 10 deaths took place in the jurisdiction of Mithadar police station alone. Strangely enough deaths due to toxic liquor hve become almost a routine during the month of Ramazan when wine shops are closed and the low-income population in the metropolis as well as other parts of the country take the liberty of consuming what is locally called “kuppi” and “tharra,” manufactured by unscrupulous elements in connivance with police. “I can confirm that the illicit business is conducted in connivance of police,” a senior police official told The News, requesting anonymity. The sources said that a person known as Obaid runs the business of manufacturing “kuppi” and “tharra” in Keamari under the garb of a medical store. “Obaid is under arrest and has more than 15 cases registered against him in Dockyard police station for running the business of illicit liquor. “His brother Pervez has also been arrested while another brother Javed is absconding. A total of six people have been arrested including assistant sub-inspector (ASI) Sharif,” the source said. Yet another culprit Naeem fled from the Civil Hospital Karachi when he saw police but was later arrested from Korangi. Naeem took ‘kuppi’ and ‘tharra’ from Keamari and sold it at Railway Colony and other spots in the city. The price of a ‘kuppi’ ranges between 100-150 rupees. The liquor becomes toxic because its manufacturer was not able to gauge its alcohol content. “Obaid’s father was also involved in the same business,” said a source. The victims of September’s toxic liquor tragedy included Muslims, Hindus and Christians and were brought to Civil Hospital and Jinnah Postgraduate Medical Centre (JPMC) from different parts of the city. DIG South Javed Ali Shah Bukhari told journalists after the incident on Sept 19 that the victims had purchased poisonous liquor in Mehmoodabad police limits. The Station House Officer (SHO) of the area was suspended. The Sindh government also suspended three excise inspectors after the tragedy and constituted a committee to ascertain the causes of death of so many people. Not surprisingly, the victims were poor people, including some sanitary workers who usually indulge in drinking after completing their tedious job. Most of the localities where the business of illicit liquor is thriving have pockets of minorities, including Christians and Hindus whose religion does not prohibit drinking but who become victim of cheap varieties due to their weak economic background. It has been reported that the ‘kuppi’ and ‘tharra’ business has flourishing in poor localities including Chenesar Goth, Kala Pull, Lyari, Sohrab Goth, Maachar Colony, Malir Mander and Chakiwara. The users sometimes mix the red colour ‘kuppi’ with colourless ‘tharra’ to get a bigger kick. “Blindness is one of the symptoms in people who have a history of drinking low grade liquor and nobody knows to what 70 extent the process of distillation has taken place in manufacturing of kuppi and tharra,” said Dr. Abdul Razzak, medico-legal officer of JPMC. The toxic liquor marketed blatantly in various parts of Pakistan is made of methyl alcohol that heavily affects the nervous system, particularly the optic nerve. Once absorbed in the body, it is very slowly eliminated. Symptoms of overexposure may include headache, drowsiness, nausea, vomiting, blurred vision, blindness, coma, and death. In contrast, the licit liquor is made up of ethyl alcohol that is not fatal. So far, despite the high death toll, the government is grappling for leads and culprits who were responsible for the tragedy. (By Shahid Husain, The News-13, 08/10/2007) Management of platelets needed to cope with Dengue There is an urgent need for the management of platelets that need to be transfused in Dengue fever, but the 15-million strong metropolis Karachi has hardly five facilities where cell separators were available, Dr Syed Abdul Mujeeb, In-charge, Blood Bank, Jinnah Postgraduate Medical Centre (JPMC), told The News. He said there were two options to transfuse blood. One: In ‘mega units,’ donors were attached with a machine called a cell separator, which takes out six to seven units of platelets in one hour. The second procedure requires a refrigerated centrifuge machine and envisages taking out one unit of platelets from a single donor. In this case, six donors were needed to meet the platelet requirements of a single patient. He said Rs7,500-8,000 was spent if cell separators (the first ‘mega unit’ option) were utilised while the second procedure was cost effective but cumbersome because, as mentioned earlier, as many as six donors were needed. “There must be guidelines for rational and appropriate transfusion of platelets in order to ensure maximum benefit to Dengue patients,” he said. “Physicians need to be appropriately trained to manage Dengue patients regarding transfusion of platelet concentrate,” he added. “The transfusion dosage is one unit platelet concentrate per 10kg body weight. Hence, for patients with less than 60kg body weight, it may be more appropriate to transfuse a single unit platelet concentrate instead of opting for mega unit,” he said. “This will reduce the demand for mega units and also reduce the cost of management,” he explained. There are 83 registered blood banks operating in Sindh, including 47 that are functioning in Karachi. As many as 106 blood banks in the province have been sealed because they failed to fulfil the requisite standardisation, Dr Zahid Ansari, Manager, Sindh Blood Transfusion Authority, told The News. However, 36 blood banks in the province have applied for registration and their cases were in the pipeline, he hastened to add. He denied that there was a shortage of platelets in the province and said that Dengue patients needed platelets and not the whole blood, as was the general impression. Dr Afia Zafar, consultant microbiologist Aga Khan University Hospital (AKUH) said it was true that amongst most of the Dengue patients the number of platelets fall but not to the extent that they need transfusion. “But if they remain sick for more than five days they should visit their family physician and the latter must check their platelet level to keep an eye on the rate of fall of platelets. Patients usually do not need blood transfusion if the platelets level is 20,000-30,000. However, they may require transfusion if the level is below that and the decision is taken by the physician on the basis of the patient’s clinical condition and platelets levels,” she explained. However, Dr Mujeeb warned that contaminated blood could result in septicemia shock and deadly diseases such as HIV/AIDS, and hepatitis B and C besides malaria. He affirmed that illegal blood banks could exploit the situation since platelets were a requirement in the treatment of Dengue. “The Blood Transfusion Act is likely to be re-drafted soon because the government feels that it is not in accordance with the international standards of blood transfusion,” he disclosed. “The previous Act was punishment-oriented and the government wants to enforce a balanced and more rational Act,” he said. He said two German organisations have extended their help in re-structuring and re-organising blood transfusion services in Pakistan. “A situational analysis has already been done and a five-year strategic plan is almost complete. There is a consensus among provinces regarding draft proposal of safe blood transfusion,” he said. He said that the two German organisations have already made commitments for necessary funding. He said regional blood transfusion centres would be established in all provinces to cater to their needs. (By Shahid Husain, The News-13, 09/10/2007) All this digging is causing Dengue, say experts KARACHI: The on-going construction work in the city is one of the major reasons for the dengue outbreak in Karachi, said speakers at a seminar on Tuesday. The seminar, organized by the Institute of Infectious Diseases, Dow University of Health Sciences (DUHS), was addressed by Prof. Salahuddin Afsar, Dow Medical College (DMC) principal, Dr Kaleem Butt, medical superintendent at CHK, Prof. Rafiq Khanani, Prof. Rafiq Ahmed, Dr Tahir Shamsi of the Bismillah Taqee Institute of Blood Diseases, and Dr Farheen Ali of AKUH. Prof. Afsar said that prevention and elimination of breeding areas was the key to controlling dengue as no definitive treatment was available. 71 Dr Butt mentioned that dengue cases were reported even from rural areas such as Thatta and Mirpur Sakro last year, and he urged planners to focus on this aspect of the issue as well. Dr Ali, in her presentation on “Clinical manifestation and management of dengue” observed that general physicians were instrumental in promoting prevention techniques. Dr Khanani, discussing “Dengue – a diagnostic challenge”, said that for the last three years, experts had been warning that the scenario was worsening and regretted that there was not data sharing between institutions, because of which guidelines promulgated for diagnosis and intervention were not widely available. Dr Iftikhar said that construction companies and builders must be required by law to ensure that dug-up water reservoirs were properly covered and loop holes plugged. He said that dripping of water from air conditioners and moving water tankers, poor care towards stored water and water in vases were also identified were also breeding points. He suggested that opinion leaders such as khateebs could be involved in motivating people to ensure prevention at collective and individual levels. ‘2005 earthquake caused dengue outbreak’: The massive population influx in Karachi after the October 8, 2005 earthquake caused the outbreak of Viral Hemorrhagic Fever in this area as Congo Fever, VHF and associated viral infections have previously been registered mainly in the mountainous parts of the country, Dr Aslam Parvez, CDGK focal person for infectious diseases. Dr Parvez said that it was possible that VHF might be transmitted to other parts of the country where people from Karachi visit, which was why a comprehensive approach was required to eliminate the infection at all levels. Staff Report adds: Platelet bags would now be available for Rs 7,000 instead of Rs 10,000 as the Central Board of Revenue has waived the import duty, coordinator Dengue Fever Monitoring Cell Dr Shakeel Malik told Daily Times. Dr Malik said that no cases were reported on Tuesday, while the number of fresh cases on Monday was 38. So far, he said, seven dengue deaths had been reported, 328 patients had been tested dengue positive and 214 had been tested negative. He said these cases were mainly reported from private medical institutions and the number of suspected dengue patients since August had risen to 686. (DailyTimes-B1, 10/10/2007) With or without (gutka) Nadeem Ansari is a computer technician at one of the computer centres in the city. His working hours are divided into two shifts: morning and afternoon. He is required to come in for the morning shift on alternate days. In Ramazan, however, he changed all his morning shifts to evening because “during the day I fast, so I cannot eat gutka and tobacco, without which I cannot survive. Therefore, I have it after Iftar till late night, which makes it difficult for me to get up for work in the morning.” Then, there is Qasim Shah is a driver who cannot fast because of his severe addiction to gutka. Initially, he started chewing on gutka when he had to work overtime because he needed something strong enough to keep him awake through out the night. When a friend suggested that he use tobacco, he also started eating gutka. “The ffirst time when I had to fast after being hooked onto gutka, I felt very dizzy in the morning and extremely sleepy. It was affecting my work and my health. After spending 10 rozas like this, I decided that I cannot fast anymore,” he said. Since then, Qasim has not fasted because of his addiction to gutka. These are just a few examples. There are countless stories of such people who cannot fast, or cannot function for that matter, if they do not chew on gutka and tobacco. Due to the high demand for these products, the supply continues unabated through out the year. Gutka and tobacco are sold at small paan cabins through out the city. On an average, there are at least two cabins in any given area. During a visit to a few such places, The News learnt that some of these cabins remain open during the day in Ramazan also, because the demand for gutka remains the same. For example, Khadim Hussain’s cabin in PECHS, Block 5, does roaring business. In fact, he makes quite a bit of money before Iftar also. When asked about his business he said that “there are a number of people who come and ask for gutka, tobacco paan and cigarettes,” he said. Another such cabin owner, Junaid in Bahadrabad, said that though he has a lot of customers who come to him during the day, still he has his shutters pulled down so that people don’t quiz him too much. Junaid said that while he does feel pangs of guilt for keeping his shop open during the day in Ramazan, he pointed out that he wants to make also. Some cabin owners, however, said that the turn-out of customers during the day is not that high as most people prefer to come after Iftar. In fact, according to them, business picks up after Iftar, but additional business during the day in Ramazan is an added bonus. Some times the addiction is so bad that it causes health problems if a gutka consumer cut down on it for whatever reason (such as Ramazan). For example, Zubair, a regular gutka user says that there is no way he can think of getting off gutka because he has already tried and all he got was headaches and sleeping disorders. He argues that since giving up gutka is so problematic, he can give up on other things, such as fasting, because the lack of gutka can become a health issue for him. Sadly, there has never been proper legislation for banning these addictive items. According to Captain Majid, special secretary of the public health sector, the ban on gutka was forwarded by the home department to the assembly. “It was moved to the assembly after continuous appeals by concerned doctors and medical bodies to be formulated in the form of a bill, but it was never taken up” he said. However, locally, the City District Government Karachi (CDGK) has tried to impose a temporary ban in the city on the manufacturing of gutka and has said it will take to task any such person who is involved in its production or sale. The Secretary General of the Pakistan Medical Association (PMA), Dr Qaisar Sajjad, while talking to The News said that “Such a ban is always going to be taken lightly because there will be no arrests made. But if there were a law, it would be followed by punishments for those not adhering to the rules.” (By Sidra Rafique, The News-19, 11/10/2007) 72 34 more Dengue cases reported Around 34 more new dengue fever cases were reported from different hospitals on Thursday, bringing the total number to 855 so far since August, said a provincial health official. He said 151 water-borne dengue virus patients were still admitted in various hospitals of the city. The official said test of 392 patients proved positive while test of 220 was negative. He said seven deaths caused by the virus have been reported in the metropolis so far this year. Dr Rafiq Khanani, Director Dow Diagnostic Lab told The News that combination of malaria and typhoid with dengue fever was complicating the situation. He said normally the health of the dengue fever patients could be stabilised within 3-4 days and around 95pc such patients do not need proper treatment if they take adequate sleep. He said only 4-5pc Dengue patients needed treatment in case of reduction of platelets. He said malaria was found in test of around five percent who tested positive The ratio of typhoid in dengue patients was two percent. He said complications of those patients have increased who were also affected with malaria and typhoid simultaneously. He said a number of Dengue fever patients was constantly increasing and it was much higher than what the officials claimed. Dr Rafiq Khanani said the doctors for their study purposes have approached five doctors in different areas of the city. Two doctors belong to Nazimabad, and one each from New Karachi, Federal B. Area and Lyari Town. These doctors gave a report that they have treated around 48 dengue fever patients in the last week only. Dr Khanani said one doctor in the city treats around 8-10 Dengue suspected patients each day and on basis of it, he could say that the number of dengue patients was in thousands in the metropolis. (The News-13, 12/10/2007) Lack of sports facilities deters youth The government’s lack of interest in promoting sports has hit the ‘nurseries’ of sportsmen in Lyari, Mauripur and Malir. All schools here were sports nurseries that produced several famous sportsmen, especially Lyari and Mauripur. “There is no place left for children interested in playing cricket and football.” A few years back, leading sportsmen visited different schools voluntarily every weekend to guide young players at their school grounds and selected a few of them for major teams. However, now neither sportsmen visit these schools nor do school managements feel the need for such activities. Though, government has built international-level stadiums at different places, but they are either closed for newcomers or are occupied by law-enforcing agencies. All covered stadiums are banned for teenagers. For example, earlier the Peoples’ Ground (also known as Peoples’ Stadium) attracted hundreds of people daily, who would indulge in sports and exercise over there. There weren’t just football and cricket lovers over there. In fact, some people organised traditional games such as kabaddi and malakhra to attract people from different areas. However, now the Pakistan Rangers have occupied this stadium since its completion and the Football House, situated at Chakiwara, Lyari, is also under its control. Moreover, the two floors of Keamari Government Degree College are also being used by the Rangers. It is has been found that when the college principal asked the Rangers to vacate the place, their spokesman said that they will move after the completion of the Lyari Stadium. The Chairman, Mauripur Baloch Football Club, Kamal Durra, said that previously, there was a sports fund for primary schools before Partition to encourage teenagers. Sports children got milk as a reward for maintaining their health and keeping physically fit. The Mauripur Football Club has been working since 1932 and has played a key role in promoting sports activities, producing several world-famous footballers. It was announced that each town will have a modern football club but the dream is yet to be fulfilled, Durra added. “We have a single-point plan, which is to save the future of our youth, as drug peddlers are running their business everywhere,” said the General Secretary Mauripur Football Club, Abdul Kausar. Saner elements of Lyari believe that these drug peddlers have forced the youth to join criminal activities in the neighbourhood so that they can continue their business. They are using the youth for their under-handed designs. There are eight football clubs in Mauripur running on a self-help basis by senior sportsmen. They have never received donations from the city government, Keamari Town or union council (UC) Mauripur. Now, young boys and teenagers go to the playgrounds in Mauripur, which are open for all. A local coach, along with one internationally-acclaimed player, trains these children free of cost. Furthermore, a team requires Rs5,000 for purchasing a kit, which in the past was provided by the government and the Lyari Labour Welfare Centre. Moreover, the defunct Karachi Metropolitan Corporation fixed Rs5,000 for each club but now the City District Government Karachi (CDGK) does not pay a single rupee to these clubs. When there is no drinking water and furniture for children in schools, how can one be expected to have library and sports activities in schools,” lamented Kausar. Now, getting a job in any government, semi government and/or private firms is the only attraction for them. Kausar said that the fall of East Pakistan affected the sports of the country immensely. Earlier, each player received Rs10,000 in a single trip for playing a match, which was a sufficient amount in those days. Abdul Sattar, a football admirer from Lyari said: “Now, sport has commercialised to a great extent. Those world famous sportsmen, who volunteered to coach in schools, are now hesitant to waste their time. The spirit has disappeared.” There is no shortage of funds with the Pakistan Football Federation (PFF), but distribution system is not fair and transparent,” Sattar said. Earlier, the Abdullah Haroon Government School, Sindh Madressatul Islam and NJV High School were among the winners in each inter-school tournament in the city. The seniors selected best players for the national team but now these institutions are hardly playing their part when it comes to promoting sports. (By Jan Khaskheli, The News-20, 12/10/2007) 73 Isolation ward for Dengue patients at ASH An isolation ward for the treatment of Dengue fever patients has been set up at Abbasi Shaheed Hospital (ASH), said City Nazim Syed Mustafa Kamal on Saturday. During his visit to the trauma centre and newly-set up ward at Abbasi Shaheed Hospital, he listened to complaints of patients’ attendants and issued necessary instructions to the relevant authorities to redress the same. Mustafa Kamal said that ASH was the first hospital to have such a ward, adding that that the city government was bearing all treatment expenses of the affected people, including blood transfusion. The platelets costing Rs7,000 to Rs 12,500 would be purchased from Bismillah Taqi and Hussaini blood banks and the city government would pay for it, he added. He said that experienced doctors and paramedical staff have been deployed at the new ward. “Special chemical coated nets have been installed around the beds of patients,” he said, adding that the nets have a life of three years. The Nazim claimed that adequate funds have been allocated for the treatment and proper care of the patients in the Dengue isolation ward. As for the situation in the city, He said that, as a part of preventive steps, germicides were being sprayed in different parts of the metropolis through 80 spray machines. He claimed that modern machinery was available at the Abbasi Shaheed Hospital, where more facilities were being provided as compared to even private sector hospitals. He further said that the hospital has a 30-bed emergency ward with advanced facilities, which happens to be largest in the city. The Nazim also announced that another lab would be opened at ASH just after Eidul Fitr. For this purpose, new machinery and instruments have been imported, he said, adding that anti-rabies vaccination had been provided in adequate quantity and provided to patients free of cost. (The News-13, 14/10/2007) Key CHK issues still unresolved KARACHI, Oct 16: A rift has developed between the administration of the Civil Hospital Karachi (CHK) and senior doctors over the resumption of work at the hospital’s Gynaecology & Obstetrics Department where services have been suspended for nearly a month in protest against its poor facilities. Despite an official announcement that repairs have been completed and all gynaecological, obstetric and emergency labour services will resume on Wednesday (October 17), doctors say that their basic concerns have not yet been met and that they are unwilling to start work. The chairman of the board of governors of the CHK and the Lyari General Hospital, Abu Shamim Arif, claimed in this regard that all repairs had been completed and there was no reason for doctors to continue their protest. “We have solved their immediate problems to the best of our ability and there is no reason to continue to deprive patients of the department’s services,” he told Dawn. Asked about any official notification in this regard, Mr Arif said that the department had not been closed on his orders in the first place. He added that the doctors’ other concerns were “operational” and said that these could be attended to at a later stage, after discussions. ‘Repairs merely cosmetic’ However, the head of the Gynaecology & Obstetrics Department, Dr Ghufrana Umar Memon, said that if the doctors resumed services, the administration would simply ignore their concerns as it had done for the past four years. “The repairs are merely cosmetic and the real problems remain unresolved,” she told Dawn. “We want the administration to address the issues that have affected the quality of service for many years.” Dr Memon pointed out that considering the increasing number of patients, there is a desperate need to extend the gynaecology services. The rush of patients under normal circumstances can be estimated given that the day after Eid, the hospital received over 40 patients although all gynaecological and obstetric services have been suspended for nearly a month. “Of these, five women needing immediate medical intervention were admitted into the hospital, 10 were sent home after being given medical advice while 28 were referred to other hospitals,” she said. The long-term issues the protesting doctors referred to include that fact that there is only one operating table in the emergency room. According to Dr Memon, arguments have broken out between doctors and patients since only one case may be operated upon at a time. The elective operation theatre facilities are inadequate and in poor shape, and doctors want the immediate provision of alternative arrangements in the new OT complex. They also claim that the elective surgery theatre needs complete renovation and be equipped with modern facilities. “In order to extend the gynaecological services, the OTs being shifted from the first floor housing the gynaecological department to the new OT complex should be handed over to the gynaecological department,” said Dr Memon. Expressing the hope that an October 18 meeting with the health minister and the vice-chancellor of the Dow University of Health Sciences would bring positive results, Dr Memon pointed out that “the administration should realise that the beneficiaries of our demands for more space, trained OT staff and better facilities will be the patients, not us.” (By Faiza Ilyas, Dawn-15, 17/10/2007) Sepsis, delays leading causes of casualty death at hospital: AKU study KARACHI: Sepsis or the body’s response to bacteria is the leading cause of death in patients of all age groups in the emergency department of the Aga Khan University Hospital, its researchers have found. Also, their study highlighted the deficiency of the city’s healthcare system as the patients who died had been in contact with another healthcare facility for their illness. Furthermore, the patients died within 3.5 hours of arrival, suggesting that they must have been sick for several days and if they had been given a better primary care, many of them might not have deteriorated to such an extent. These findings, ‘Emergency department deaths despite active management: Experience from a tertiary care centre in a 74 low-income country’ by AKU’s Dr Nadeem Ullah Khan of Emergency Medicine, Department of Medicine, Dr Junaid Abdul Razzak, Syed Muhammad Hammad Alam and Humaid Ahmad were published in the international journal ‘Emergency Medicine Australasia’ in June. This was a retrospective case series of all deaths pronounced in the emergency department (ED) of Aga Khan University Hospital (AKUH) during the 2 year period (1 Jan 2001–31 Dec 2002). The AKUH is a 450-bedded private, fee-for-service, urban tertiary care teaching hospital located in Karachi, a city of 14 million people. The ED at AKUH has an annual census of approximately 40,000 patients including both adults and paediatrics. The hospital is not a designated government trauma centre and therefore it is usually not the first hospital to receive trauma patients. Most people present to the ED through private transport because of lack of established prehospital care infrastructure. Of the 78 418 patient visits, 601 patients (0.7%) were pronounced dead. Of these, 577 patients had complete records. Seventy per cent of these were dead-on-arrival, 1% had do-not-resuscitate orders and 29% or 166) died despite active management. Initial vital signs were found to be abnormal in almost all cases (98%). The leading causes of death were sepsis (23%), myocardial infarction (19.7%), cerebrovascular accident (10.7%) and pneumonia (8.2%) among adults and sepsis (36.4%), myocarditis (15.9%) and pneumonia (9.1%) among children. Deaths in the ED are a common occurrence with a reported frequency as high as 0.4%. Multiple factors are believed to affect the outcome of a patient during an emergency including timely access to care, availability and quality of prehospital and hospital care, overcrowding in the ED, acuity of illness, age distribution of the population being served, comorbidities and the length of stay in the ED. Information regarding deaths in an emergency care setting is not readily available from low-income countries. Given a significantly different disease burden in these countries and a marked variability in the access and quality of health care the causes and presentations are likely to be different. The AKUH study aimed to determine the frequency, the causes and the features common to patients who died in the ED despite active management in a tertiary care hospital in Pakistan. Adult patients constituted about 73% or 122 of these ED deaths. The mean age was59 years with men outnumbering women by 2:1. More than half of all the patients were less than 65 years of age (55%). Two-thirds of patients dying in the ED had one of these three complaints: dyspnoea or shortness of breath (40%), altered mental status (25%) and chest pain (11%). The mean duration of presenting symptom was 22 h. Approximately 90% of patients had one or more chronic comorbid condition. One-fourth of these patients had already received some care prior to presentation and most of them had received it at another hospital. Five (3%) of these patients were seen in the same hospital within the past 48 h; four were discharged from the ED and one was admitted and discharged from the hospital. Based on the initial triage assessment, 95% of these patients were triaged to the critical care or resuscitation area of the ED. The patients had an average ED length of stay of about 3 h 20 min and their final ED diagnoses were: septicaemia (23%), myocardial infarction (19.7%), cerebrovascular accident (10.7%) and pneumonia (8.2%). Trauma caused a total of four deaths in this age group, all were men and all had traumatic brain injury as a cause of death (Table 1). Of all the paediatric patients, 44 or 18% were neonates, 25% were infants and 57% were between 1 and 14 years of age. Unlike adults, female children died more frequently in the ED (male : female 1:1.5). The most common presenting complaints in paediatrics were: dyspnoea (43%), altered mental status (26%) and seizures (7%). About one-third (39%) of these patients received medical care prior to presentation to the ED with more than half being at another hospital in the city. None of the patients was seen within 48 hours of their presentation to the ED. The study shows that infections (sepsis, myocarditis and pneumonia) and atherosclerotic vascular diseases (myocardial infarctions and strokes) were the leading cause of ED death, despite active management, in the population. Vital signs were abnormal in almost all cases and dyspnoea and altered level of consciousness were presenting complaints in the majority of those who died in the ED. These findings are similar to the findings of another study from Pakistan where severe sepsis and septic shock were found to be the major reasons for hospital and ICU admissions. AKUH is not a designated trauma centre and thus does not receive a large number of trauma patients. However, even with the relatively lower number of trauma patients in the study, they found that all had died because of head injuries. The study exposes significant differences in the cause of ED mortality between high- and low-income countries. Two studies from the USA, for example, show that cardiac, cerebrovascular, trauma and pulmonary embolism are the major causes of ED deaths unlike sepsis and pneumonia found in the AKUH study. Recent advances in the care of sepsis patients, through ‘early goal directed therapy’ have shown significant benefits with a mortality reduction of up to 16%. Sepsis is the leading cause of death in all age groups in the setting. Improved infection prevention, proper early treatment and better emergency care including early goal-directed therapy could potentially save a large number of lives. (DailyTimes-B1, 17/10/2007) Organ donation for transplant surgery I HAVE been following up the debate and news on organ donation for transplant surgery in your newspaper and on TV channels. This debate, by and large, involved two groups, both pleading to protect their own interests. It is ironic that the main party involved in this serious matter, i.e. the patients who are left to live a miserable life unless they receive a transplant, has no part to play in this whole discussion. Only those who have such patients in their families can appreciate the apathy and misery of these patients. 75 As a transplant surgeon, I have been involved in this intricate life-changing surgery for the last 17 years and have worked in Pakistan and the UK. My main concerns regarding my own experience in Pakistan have been the gender of live, related donors and non-compliance on the part of the recipients. Most of the donors in my practice were women: sisters, mothers, daughters, cousins or from one of the many wives, who have no say in matters concerning their lives, raising concerns of coercion. My other concern was the financial burden on the recipients, most of whom stopped their immuno-suppression after one year due to high cost. It is impossible to implement a uniform programme for organ donation for all countries due to deep differences: economical, social, religious and cultural. However, it is universally accepted that transplant tourism and commercial transplantation are certainly immoral, and have given Pakistan a very bad name but, more importantly, it is dangerous for patients. Pakistan is hugely underdeveloped with the exception of a few big cities. Before implementing a transplantation programme or any other super surgery requiring huge finances, there are other pressing issues which require urgent attention. The government needs to make serious efforts to save mothers, neonates and infants who die due to lack of basic facilities, and control simple diseases like diarrhoea, tuberculosis, typhoid, poliomyelitis and malaria, which still claim too many lives in Pakistan. More attention should be given to prevent and control diseases which lead to kidney failure. As the quality of dialysis in Pakistan is substandard, the government should provide funds for this purpose so that these patients can be dialysed in proper setup free of cost. As regards cadaver donation, in a society where relatives do not give permission for post-mortem, considering it mutilation and insult to the departed soul, just mentioning cadaver donation is frowned upon. Allowing cadaver donations in such a society will encourage body mafias to emerge. In order to get organs, people who are weak, underprivileged, homeless and unfit to survive will fall prey to middlemen and will be killed to supply organs to rich recipients by ruthless surgeons looking to fulfil their ambitions and greed. As regards live donation in Pakistan, in my opinion one has to be a little rationale in deciding the fate of renal failure patients. We should take the middle-of-the-road approach. The live, related donation programme must be encouraged and, at the same time, unrelated donations should not be stopped or discouraged, but be regulated and controlled. In this regard a joint government- and private sector-controlled live donation programme should be set up where every donor, whether related or unrelated, should be adequately compensated. This shall avoid the exploitation of unrelated donors and save several related donors from donation against their will. PROF MAQSOOD ANWAR NOORANI Consultant-General and Transplant Surgeon, London (Dawn-6, Letter to the Editor, 18/10/2007) Viral infection claims another life in Keamari KARACHI, Oct 20: A pregnant woman died of viral disease in Deh Allah Bano, located in Union Council Gabopat of Keamari Town, raising the death toll from the infection to eight in the area. Earlier, two women – one of them pregnant – had died in Ali Baksh Goth, while four children and a man had died in different villages falling in the same jurisdiction. The area, under the grip of a viral disease for a month, has failed to receive any effective government intervention so far. According to Pakistan Fisherfolk Forum representative Surriya Talpur, the deceased, 27-year-old Zubaida Younus residing in Haji Ibrahim Goth, was eight months pregnant with her first baby. Though she had been ill throughout Ramazan, her condition deteriorated on Saturday and she was taken to a Mauripur clinic. “She complained of high fever and severe joint pain and was discharged when her condition improved a bit after being administered injections and drips. Later, we are told that she died within three hours of her arrival in the village,” she said, adding that this was the second death of an expectant mother by viral infection in Deh Allah Bano. Earlier, 23-year-old Maluka, also pregnant with her first child, died with similar symptoms in Ali Baksh Goth a day before Eid. On Eid day, 50-year-old Kulsoom died in Haji Noor Mohammad Goth. “Successive deaths in the area, that too on Eid, overwhelmed the poor villagers with grief. They desperately need economic support in terms of food and medical aid as the sickness is consuming all their resources,” Ms Talpur lamented. According to her, the disease has affected almost all the 18 villages of Deh Allah Bano. Recently, 12 people of Haji Noor Mohammad Goth were treated at different Mauripur clinics. Two of them are in critical condition, admitted to the ICU of the Civil Hospital. They are identified as Lal Mohammad and Karim Bux. “The dangerous part is that none of the patients that have been ‘treated’ so far could develop immunity against the disease as they fall ill again after receiving treatment. There is no sign of a fumigation drive in the villages which have literally been invaded by mosquitoes,” she said while criticising the town health administration which, she said, had failed to contain the disease. When asked about the testing of the blood samples collected for identification of the virus, Keamari Town Health Officer Dr Nazeer Ahmed Kolachi said that of the 50 blood samples that had been tested at the Civil Hospital’s laboratory, a few of them were malaria-positive. “We don’t know what virus was present in other samples since the tests were carried out only to examine the presence of malaria,” he maintained while dispelling the impression that it could be dengue as none of the patients, according to him, had dengue symptoms. 76 “In the absence of any government virology laboratory in the city, it’s difficult to say anything with certainty about the rest of the samples. However, every viral infection ends after a limited period, so we are giving symptomatic treatment to patients,” he said. The last time the town administration’s medical team had visited the affected villages was on Oct 11, he said, while adding that a medical camp would be established in the area on Monday in which routine vaccinations would be carried out along with free distribution of malaria medicines. (Dawn-19, 21/10/2007) Burn victims suffer in silence KARACHI, Oct 21: Domestic violence is a phenomenon not new to any society. In its most extreme form victims are killed either by stabbing, strangulation, burning or other grisly methods. Particularly disturbing is the number of burn cases reported by women in Pakistan, which shows no sign of decreasing. Data collected by the Madadgar Helpline for Children and Women states that 162 women were set on fire in Sindh in 2001, 75 in 2002, 123 in 2003, 168 in 2004, more than 100 each in 2005 and 2006, and 82 in 2007 from January to August. However, the overall data collected from Jan to Aug 2007 of women burn victims throughout Pakistan goes way above 1,779. Though the Human Rights Commission of Pakistan’s report for 2006, published on its website, claims that 113 women in Punjab had been burnt that year, out of which only seven were unmarried, the report does not include the cases of women who are supposedly burnt because of their own “mistakes.” The stove blew up or a match was lit while gas was leaking are some of the common explanations given for women burn victims. But many people argue that why is it mostly daughters-in-law or wives that get burnt and not any other members of the family? Rukhsana (30) was tortured on the issue of dowry by her husband Pervaiz Ahmed, his first wife and his other family members three years ago. However the ordeal did not end there as they went on to douse her with kerosene and then set her on fire. A similar incident happened to 18-year-old Amina. She was burnt by her husband Asif and his family a year ago. Neither Amina nor Rukhsana managed to survive. Social stigma None of the accused were brought to trial despite the fact that FIRs were registered in both cases. None of the women had informed their families about any domestic discord between them and their in-laws. Since it is a common feature of society for women not to reveal their family problems to anyone, they end up suffering in silence for the rest of their lives or worse, are killed. Surprisingly, almost all the 20 women patients admitted to the Civil Hospital Karachi’s Burns Centre said that either they had been burnt as a result of a cooking accident or that they were suffering from epilepsy and had fits while cooking. There was only one woman who said that a boy threw acid on her and her mother when she refused his advances. “Epilepsy is an excuse,” said Executive Director of the Burns Ward, Dabir-ur-Rehman, “that most female patients burnt by family or husbands, find convenient.” “I have come across a woman who was allegedly burnt while cooking and her husband also burnt his arms while reportedly trying to save her. But when I asked her in confidence on the promise of not disclosing the details to anyone, she told me that her husband had burnt her and held her shoulders, burning his arms in the process in order to assure that she burns to death,” he said. The man got off the hook while the woman died in a few days’ time. Dabir-ur-Rehman disclosed that female patients do not admit the truth for the fear that if they do, they will not find justice nor will their family accept them. Dr Wasif Ali, a psychiatrist, said that Pakistan does not have a very high ratio of epilepsy in females and the statements made by the majority of female patients in the burns ward seemed far removed from reality. “The real picture can easily be found if the EEG of the patient is taken soon after they are admitted,” he said. “What happens is that the medico-legal officers take money from the abuser’s family and convince the patient’s relatives to opt for this easy way out as it is too much of a hassle if they tell the real story to the police, who are not going to help them in any way” he added. Describing the history of violence and aggression, Dr Ali said that it is human instinct to use brutality in order to assert authority as it gives a sense of gratification. Vicious circle “Our society in particular is such that it regards females as paon ki jooti. They can be treated in whatever way and humiliated any time,” he pointed out. He shared the findings of a study carried out a few years ago that says 55 to 60 per cent of the men who batter their wives have seen domestic violence going on in their family during their childhood. He also told this reporter that one out of every four women, belonging to all socio-economic backgrounds, are subjected to domestic violence. “Interestingly, you will hardly come across men in such great numbers who are burnt while cooking. Are there not men who cook at home or in street-side restaurants?” he asked. Supreme Court advocate and human rights activist Zia Ahmed Awan blamed society and its stereotypes for domestic violence against women. “Women are not aware of their rights and blindly follow what society dictates,” he claimed. Legal loopholes Another fact contributing to it is the lack of any clear law in the Pakistan Penal Code on domestic violence. The advocate said that the system is such that if a woman musters enough courage to report a case against her husband, the police will not register the case and if they do, it will be nothing more than a non-cognizant report. “What should be done is that the 77 police should take the patient’s statement as soon as she arrives in the hospital. What happens is that after a few days the family strikes a deal with the offender and the whole issue is settled,” he said. “Women should not give up easily and should fight back. It is the government’s responsibility to provide protection to its citizen -- men and women -- be it inside the home or outside,” he added. Though there have been very few cases in which those who burnt their wives or women of the family were bought to justice, it is much more disappointing to see victims give up their rights and put up with torture and not raise their voices against it. (By Meera Jamal, Dawn-13, 22/10/2007) Dengue patients’ number rises to 1,527 The Dengue fever patients’ number in the city has risen to 1,527 since August, a provincial health official said on Tuesday. Around 48 new cases were reported from different areas on Tuesday. The official said that two hospitals, which were earlier reluctant to share information about Dengue fever patients, started giving reports about those admitted there. The number of patients, according to this information, appear to have increased. As many as 110 patients tested positive for Dengue were still admitted in the hospitals. The official said a total 534 cases tested positive and 11 of these had died. Doctors said that there were several issues associated with Dengue fever. The concerned authorities, they allege, are not aware of ways to deal with it. Doctors were also not trained on how to diagnose and manage Dengue cases properly. Without proper management, Dengue hemorrhagic fever cases fatality rates that can exceed 20 per cent. However, given the modern intensive supportive therapy, these rates can be reduced to less than 1 per cent. Dengue fever is caused by four types of Dengue viruses known as Dengue 1, 2, 3, and 4. If an individual is infected with type 3, the person develops antibodies against Dengue 3 virus. This infection is known as Primary Dengue infection (First time infection). If this person is later infected with the same Dengue 3, there will be no relapse as the person will have become immune. However, if this person is infected with a dengue virus other than type 3, there will be severe infection (known as secondary infection - second time, third time, and so on). Dr Rafiq Khanani, Associate Professor and Senior Pathologist at the SMC and DUHS said on Tuesday that many doctors not knowing this fact discarded the diagnosis of Dengue fever if Dengue IgG is present. Several laboratories are offering only IgM antibody test and are missing this important group of patients by giving a Dengue IgM Negative report to infected individuals, he added. Another problem is that Dengue Test Kits are from different manufacturers and a large number of kits detect Dengue Type 2 only -resulting in a large number of negative reports, Khanani believed. He suggests that authorities ensure that kits available are up to standards, tests are done properly by qualified personnel/laboratories and doctors be trained to interpret reports. Another important aspect of Dengue, which is not recognised commonly, is that a majority of persons infected do not have any symptoms and infection can only be detected if a Dengue antibody test is performed. He pointed out that the World Health Organisation had a programme known as DEWS. It requires a system for early reporting of infectious diseases so that appropriate control measures are instituted in timely manner. However, implementation strategy is poorly understood and, therefore, these diseases assume epidemic proportions. If this system is not implemented, “we may experience epidemic of other diseases such as yellow fever and west Nile Encephalitis”, Dr Khanani feared. (By Imtiaz Ali, The News-13, 24/10/2007) Leaking pipes, poor sanitation spreading dengue KARACHI: A large number of leaking water pipes in the city has provided ideal breeding ground for dengue fever as the number of infected patients has reached 1,573 along with 11 casualties according to official figures. Sindh Health Department’s monitoring cell for dengue fever on Wednesday confirmed that 1,032 cases of clinically positive and another 521 serologically positive were reported since August 1. No part of the city can be declared ‘severely affected’ or ‘dengue-free’ as the whole city is facing water leakage and solid waste problems, said Additional Health Secretary Dr Shakil Malik. Water accumulation was the major cause of dengue in the city. “Around 43 patients were reported in the last 24 hours and we have an unconfirmed report of a casualty,” he said. The cause of one death on Wednesday could not be confirmed, while so far 115 confirmed dengue patients were admitted to different government hospitals. Provincial government officials said that 23 patients were admitted to Ziauddin Hospital, seven at the Jinnah Postgraduate Medical Centre (JPMC), four each in Civil Hospital Karachi (CHK) and Aga Khan University Hospital (AKUH). (DailyTimes-B1, 25/10/2007) Permission to carry out organ transplants Hospitals get go-ahead without inspection KARACHI, Oct 25: The Human Organ Transplant Authority (HOTA) has allowed as many as 19 hospitals and institutions in Karachi, Lahore and Rawalpindi to carry out transplant activities on a temporary basis, without undertaking any physical inquiry of the manpower, equipment, specialised services and other relevant facilities. 78 This was disclosed by HOTA administrator Maj-Gen (retd) Abdul Qadir Usmani while speaking at a press conference at the Sindh Institute of Urology and Transplantation on Thursday. He said the authority had received in all 19 applications from institutions, providing details about human resources, facilities and support facilities available with them, and granted interim registration to all of them. According to Mr Usmani, HOTA, set up about a month back, had sent a pro-forma to 31 hospitals and institutions to fill in to get themselves registered in line with the provisions of the Transplantation of Human Organs and Tissues Ordinance 2007. However, besides the HOTA selected institutions some other health-care centres also downloaded the pro-forma from the health ministry’s website and submitted it for registration, it was added. “Since HOTA is still in its infancy and is waiting for necessary finances and manpower for its working, it was deemed fit to defer the physical inquiry of the health premises in question and to issue interim certificates of recognition to all applicants, enabling them to practise operative surgery in transplantation of human organs or tissues,” the administrator said, adding that HOTA might begin the inspection visits in the next six or so weeks. Referring to the apprehensions expressed during the conference that HOTA acting in a haste had also enlisted a few institutions which had earned a bad name in the past for their alleged corrupt or unethical practices in the name of kidney transplantation, Gen Usmani said there might be some weight in the apprehensions, but the authority’s problem was that it could not effect a law or impose any penalty retrospectively. He said HOTA was required to entertain all cases and judge the performance of the transplant institutions under the organ transplant ordinance only. The accordance of registrations to 19 health institutions, including 12 from the private sector, was not a final decision and the list would be updated periodically by excluding or including institutions. The administrator said that HOTA was also considering establishing three evaluation committees on a regional basis in Karachi, Lahore and Islamabad initially to ensure that no organ or tissue was retrieved from non-related living donors without its prior approval. These committees, whose number could be increased in future, will also determine brain death of a person and examine the fitness or otherwise for transplantation of a human organ into another body. Answering a question, he said a draft act on organ transplantation had already been sent to the national assembly for its consideration and enactment at the earliest; otherwise the prevailing transplant ordinance could also be revalidated by the president for a further period. Those who also spoke at the press conference included Prof Farrukh A. Khan, president of the Transplantation Society of Pakistan, who said that those who could not afford the cost of any organ for transplantation would be helped through an exclusive fund. In reply to a question about the chances of exploitation of patients by private hospitals, SIUT director Prof Adibul Hasan Rizvi said that the life of private organ transplant and dialysis centres depended on the performance of the government sector health facilities. “We should improve the standard of the public sector health institutions and also ensure a national registry of transplants on a priority basis, which could help check many of the human organ transplant-related problems in the country,” he added. Earlier during the day, a seminar on “Curbing commercialism and increasing transplant activity” was organised by the SIUT, which was also attended by senior doctors and members of the judiciary. Prof Francis Delmonico of the International Transplant Society, USA, spoke about the success of ethical transplantation in the United States and held that the practice helped in increasing the availability of donor organs. Prof Mehmet Haberal from Turkey spoke on the success of cadaver organ transplantation in his country, which has the law and infrastructure for retrieving organs. Prof Faisal Shaheen, president of the Saudi Committee of Organ Transplantation, said that cadaver organ donation had been practised in Saudi Arabia for many years. Donation by deceased was allowed in Islam and it had been approved by almost all Muslim countries, he added.The other speakers, including federal health secretary Khushnood Lashari, lauded the role of the SIUT in what they termed a long battle in getting a set of laws on cadaver donations for the benefit of the people of the land. In the meantime, about 750 individuals from Karachi and other parts of the country, including medical professionals, members of civil society and the judiciary as well as SIUT employees, filled out a SIUT-prepared card at a ceremony on Thursday and committed themselves to donating their organs, said a spokesman for the SIUT. (By Mukhtar Alam, Dawn-17, 26/10/2007) Organ transplantation Controversy erupts as 19 hospitals given green light An evaluation committee, led by a retired Army general, set up after the promulgation of the Organs Transplantation Ordinance, has given permission to 19 hospitals, including 12 private institutions, to carry out organ transplantation. This was stated during a press conference at the Sindh Institute of Urology Transplantation (SIUT) here on Thursday. “Around 31 hospitals in Sindh and Punjab applied for conducting organ transplantation but we gave ‘interim recognition’ to 19 hospitals,” said Maj Gen (retd) A.Q Usmani, chairman of the committee. Flanked by Dr Adeeb Rizvi, Director, SIUT, Sajjad Hussain, President, Pakistan Association of Urological Surgeons, Farakh Khan, President, Transplantation Society of Pakistan (TSP), Muhammad Tufail, President, Pakistan Society of Nephrologists, and Saeed Akhter, General-Secretary, TSP, the chairman admitted that many of the hospitals were allegedly involved in commercial exploitation of the poor. This disclosure raised eyebrows during the press conference. 79 “I am shocked to learn that most of the hospitals allowed to carry out transplantation were involved in exploitation of the poor kidney donors in the recent past,” Dr Adeeb said. He urged the general to reconsider this decision. Another speaker smilingly said that this recognition was equal to the ‘national reconciliation ordinance’, which washed away the sins of the rulers and officials. The chairman defended his decision by saying that, ‘the law cannot be applied in retrospect.’ Dr Adeeb maintained that, ‘we have to protect the ordinance as sustained struggle of doctors, civil society and media is not over.’ He was apprehensive that certain legislators might block the legislation against commercialisation of human organs or that the ordinance might be made powerless. Saeed Akhter lamented that transplantation did not exist as science or art in the country. Sajjad Hussain said there was need to create awareness for culture of donation. He said that organs donation occurred in the country for the first time in the 1980s but, regrettably, later organs tourism started based on exploitation of the poor. Referring to the ‘donor card’ initiated by the SIUT, he claimed hundreds of people have shown their willingness to donate their organs. Farakh Khan said it was good to see that the government would set up a fund as treatment after transplantation was very expensive. Dr Bakhsh Ali, spokesman for SIUT, said that around 800 people have applied for a ‘donor card, a gift of life’ to donate their organs after death. (The News-13, 26/10/2007) Transplanting life THE newly promulgated Transplantation of Human Organs and Tissues Ordinance 2007 is being hailed by doctors and the civil society as a promising step to give hope of life to end-stage kidney-failure patients. It is also expected to curb the exploitative organ trade that has brought such a bad name to the country and the medical profession. This ordinance may be a result of an arduous 15-year battle but victory is still far from absolute. The most difficult task ahead is to ensure that it gets a permanent status by being adopted as an Act and is implemented fully, which is still in doubt. It prescribes severe penalties for violators and can put out the transplant tourism mafia significantly by making evaluation committees responsible for monitoring transplantation cases and ensuring that no commercialism is taking place. However, there are fears — and not unfounded — that the first violation may have already occurred as 19 hospitals in Karachi, Lahore and Islamabad have been temporarily permitted by the Human Organ Transplant Authority (HOTA) to conduct operations without prior inspection. Apprehensions abound that in doing so, the authority may have also included institutions of dubious repute. These oversights can not only delay the ordinance from becoming a law but also keep it from putting an end to unethical practices. Regional monitoring committees are the most important aspect of the edict to prevent unscrupulous elements from bypassing laws and ensuring that no organ is procured from non-related living donors. The ordinance also lends official recognition to the fact that some among us are vulnerable to the point of being constrained to sell their organs and sacrifice their physical integrity and well-being. That is because there is a severe shortage of organs and the Sindh Institute of Urology and Transplantation (SIUT) must be lauded for its donor card campaign to combat commercialism and exploitation and to increase the availability of organs from deceased donors. The campaign will create awareness and encourage people to will their organs in case of brain death, which is allowed in Islam and is currently being practised in many Muslim countries. An evaluation mechanism is also required to ascertain brain death, tissue suitability and fitness levels to facilitate the transplantation procedure. The sooner this is set up the easier it will be to implement the ordinance. (Dawn-7, 27/10/2007) Child cancer up 50% at NICH KARACHI: The rate of child patients treated for cancer at National Institute of Child Health (NICH) went up by 49 percent during October 2006 to September 2007. The Child Aid Association (CAA), supporting the Oncology Unit at NICH, has mentioned in its annual report 2007 issued on Friday that a total of 324 new patients were registered and treated at the unit. During 2007, the CAA also established Cytogenetic Laboratory, which was country’s second in public sector institution while first of its type in any children hospital. The facility available at NICH since July 2007 is essential in diagnosis of different genetic disorders besides blood diseases. In addition to its support for children suffering from cancers, CAA provided either totally free or a 50 percent free special investigations and medicines not available at NICH to 896 patients from other units of NICH. (DailyTimes-B1, 27/10/2007) The lady doctors of Larkana Last week I visited a government hospital for women in Larkana. Established in the 1970s, the hospital offers a gynecology ward, a general health ward, a menopause and infertility clinic and a quaint but small women's mosque on their premises. The hospital's gynecology unit treats approximately 150 out patients every day, delivers up to 20 children by cesarean section and another 15 by natural birth per day, and cares for up to 50 expectant mothers. Somewhat miraculously, all this pre and postnatal care comes at the hands of only thirty doctors. Thirty women, that is. These thirty women doctors work around the clock, understaffed and ill equipped, to uphold the Hippocratic oath they swore to when they first became physicians. The oath -- first, do no harm -- is not one these phenomenal doctors take lightly. 80 There are only five beds in the natural delivery ward, sometimes they are all occupied and the women must give birth in unison with no luxury such as privacy awarded to them. Waste management in the natural delivery room consists of a black trashcan placed at the edge of the bed where afterbirth, blood, and fluids are disposed of. Rubber sheets, which are quickly washed down after each delivery, cover the beds. The hospital cannot afford to buy and clean cotton sheets for the patients. Similarly, there are no hospital gowns for the women to wear; they deliver in the clothes they came in. There are a sparing amount of beds available and no unit for the newborn infants, they are handed to their mothers after birth and sleep with them on their narrow, steel-rimmed beds. Though lacking in sufficient equipment and medication, the hospital, a government run one, equitably treats women from Larkana and the rural areas surrounding upper Sindh. They charge Rs. 800 for cesarean deliveries -- with free post-operative medical care -- and approximately Rs. 350 for natural deliveries. The lady doctors of Larkana are true heroes. They work for meager salaries, between Rs. 6,000 to 17,000 -- a pittance for their superior skills. They work day and night, weekends, and holidays and though exhausted, their bedside manner is impeccable (they were very gracious when I fainted in the middle of a cesarean section, from the halothane mind you. Not because I was frightened or anything, no sir). The problem here is not the doctors or the health care provided in the interior of Sindh, the problem is, as usual, the state and their fundamental incompetence in caring for the most basic needs of the people. The government has not offered the prerequisite test that determines positions in their hospitals since 2005. The last time the government held the test they awarded 110 doctors, out of a possible 30,000 qualified candidates, commissions in government hospitals. Why? When so many people are denied access to health care why would the government scale back the number of doctors in its hospitals? The answer, the explanation to why government hospitals in Sindh are finding it increasingly difficult to provide adequate care for women, especially expectant mothers and infants, is wholly inadequate, especially given Pakistan's dismal health statistics. According to the Red Crescent, Pakistan ranks far behind other developing countries in the reproductive health risk index. We have one of the lowest records of female health and education, combined with the poverty and low social status that affects most Pakistani women, these factors ultimately result in women being systemically disadvantaged when it comes to asserting their rights to health care. As it stands, according to the United Nations Population Fund (UNFP) Pakistan boasts one of the highest rates of maternal mortality in the world. Five to six women die every hour during childbirth due to completely preventable causes. During the nine months of pregnancy one in 38 Pakistani women dies from not receiving any prenatal care whatsoever, compared to one in 230 women in our neighbouring state Sri Lanka. Almost half of the total number of pregnant women in Pakistan are anemic throughout their pregnancies due to improper nutrition and in time they give birth to disproportionately malnourished children. Our infant mortality rate -- 82 infant deaths for every 1,000 -- is also a record holder. These deaths are seen as inevitable due to the fact that out of the approximate six million women that bear children in Pakistan every year, two thirds of them receive absolutely no prenatal care, factor that in with the reality that 80% of infants are delivered at home without the aid of a trained physician. With statistics as grim as these, why the rollback on doctors in government hospitals? The immediate concern is money, it's always money. Government hospitals pay their staff salaries that private hospitals in the interior of Sindh, comfortably relaxed in the glory of privatization, would never dish out. On average, a doctor working in a government hospital in Sindh receives a stipend of Rs. 12,000. An equally qualified doctor working in a private hospital in the interior has to make do with Rs. 3,000 a month. With salaries so low, it's financially no different to work as a traveling midwife than it is to hold a private position. One might also argue that it's not exactly worthwhile for government hospitals to be handing out so much money from their annual budget to their employees, especially not since corruption is such a celebrated (and now safe, thanks to the NRO) component of the Pakistani work ethic. The second reason, as far as I can tell, is that the National Program for Family Planning and Primary Health Care is prioritizing a new initiative. They are training, paying, and supervising Lady Health Workers (LHWs) from regional communities -- who are not qualified physicians, only trained in first aid-- to deal with local health issues and provide basic care. While the idea of LHWs is theoretically commendable, it is certainly curious that the government would undertake such a program for largely superficial medical ailments when there are thousands of women and infants dying from severe and complicated health factors. Maternal mortality is a serious killer in Pakistan. The fact that the government pays the LHWs a salary of Rs. 2,600 a month, far less than they would have to pay government hospital staff, is also telling. The UNFPA wrote in a 2003 report that 'there is no evidence that the training programs in Pakistan have worked to reduce maternal mortality' further concluding that at most it had improved the performance of local midwives. Most, if not all, of these women's and infants deaths could be avoided and easily so. With access to trained physicians, medical care and prenatal treatment Pakistan's women would survive their pregnancies. We are not talking of life threatening illnesses, not of AIDS or Cancer; we are talking of a nation with an appalling low maternal health index that is cutting back on the number of positions in their more affordable hospitals. The Sindh Health Department's website, (navigating it is an exercise in futility, I don't advise it) is crammed full of data, and yet it doesn't address the most serious problem facing Pakistan's government hospitals -- the fact that there are no doctors in them. (By Fatima Bhutto, The News-6, 28/10/2007) CHK trauma centre row refuses to go KARACHI, Oct 28: Civil Hospital Karachi’s administration took a step towards its much awaited trauma centre project after it recently floated a tender for making major structural changes in the building of the director laboratories and chemical examiner to house the neurosurgery and eye departments, the two units of the hospital which need to be demolished to make way for the trauma centre. The centre has already been delayed for two years due to the controversy over the project site. Though the health department officials ignored the objections against the project site and are moving ahead for its construction, the controversy is very much alive and many doctors associated with the project in different capacities still question the rationale behind building a trauma centre at a location that restricts accessibility. Due to this very reason, they believe that the huge amount of money -- Rs1.4 billion -- to be spent on this project would go to waste while criticising the displacement of an institution, a health setup and two important departments of CHK. 81 At the moment, the Aids control set-up at the Services Hospital, where the laboratories would be shifted, has already moved to the CHK’s infectious diseases department, while the neurosurgery and eye units are waiting to initiate the process once the building housing the laboratories, located on the premises of Services Hospital, is vacant and the required structural changes are made. “The laboratories, the sole facility serving the forensic needs of Sindh and Balochistan, are being moved from a ground plus-two building spread over an area of around 24,000-square-feet to a much smaller place at the Services Hospital to accommodate the neurosurgery and eye units. Structural changes will delay the project more. Besides, there is no point in building a trauma centre in a tertiary care hospital anyway,” a doctor said, while raising doubts about the capability of the CHK administration and the health department’s expertise in building and managing a state-of-the-art trauma centre when they have been unable to resolve the hospital’s very basic long-standing problems of water, electricity and sewerage. Doctors not consulted This project, he claimed, was made at the “higher level” by quarters having vested interests and imposed on the doctors concerned as none of them were ever invited to any of the meetings on the trauma centre. “Nobody can question the importance of a trauma centre, but specialised projects need to be handled by experts and in this case it should be those doctors who have international and local experience in trauma care. The government should make the name of the experts involved public. Who will benefit from this Rs1.4bn project, which will be under the CHK’s administration, which has a poor management record?” asked another doctor. “With this amount of money, five 100-bed trauma centres can easily be established at different hospitals,” he claimed. The doctors also asserted that the academic council of the Dow University of Health Sciences had opposed the shifting of the neurosurgery and eye units as it would particularly affect their services. When asked for comment over the controversy, Pakistan Medical Association President Dr Qaiser Sajjad said that he didn’t have enough knowledge about the problems involved at the project site. However, he felt that the populous city needs not one but many trauma centres, besides having a disaster management programme. “The government should make emergency sections of all government hospitals functional round-the-clock and set up many trauma centres keeping in view the growing population. At the same time, we need to have a disaster management programme in place under which we can train staff for specialised care to better cope with all sorts of mishaps,” he said. The 7,222-square-yards earmarked for the project on Chand Bibi Road includes the present eye and neurosurgery departments, the quarters housing city government employees and paramedical staff of the hospital. The trauma centre project, which has no detailed study report, according to health department officials, would be completed on a fifty-fifty cost sharing basis between the federal and provincial governments. The federal government allocated Rs50 million last year and Rs37.5 million this year while the provincial government has allocated Rs150 million this year. (Dawn-14, 29/10/2007) Healthcare for all THE health of the nation may be dismal but the health of around 18 parliamentarians and government officials is stable thanks to the prime minister using his discretionary powers and lifting the ban on certain public officials’ medical treatment abroad. As a result of this, the government spent Rs65m on treating 18 ‘bigwigs’ in foreign medical institutions. Granted some of the procedures are unavailable in the public sector hospitals in the country but most of the medical treatment could have taken place in private hospitals in Pakistan. That this was not good enough speaks volumes about the officials’ faith in the health sector here. One minister’s heart surgery in the UK was approved for 25,000 pounds while another minister was allocated a whopping 100,000 pounds for one-year treatment in Britain. A parliamentary secretary’s son’s treatment was allocated 50,000 pounds while three children of a deceased secretary of the privatisation commission are being treated in Saudi Arabia for multiple injuries caused in a road accident, for whatever costs. Meanwhile the public per capita health expenditure is a paltry Rs360. Something is terribly wrong with this picture. How can the prime minister approve huge sums to treat a few individuals when hundreds of millions of people do not have access to the most basic of healthcare in the country? It is said that the sum of Rs65m could have run a tertiary care hospital for one year. Statistics on maternal and child mortality are grim; children should not be dying of diarrhoeal diseases that can be prevented if there is access to clean drinking water. Basic health care units in the rural centres are barely equipped to deal with emergencies, let alone treat anyone for complicated ailments. The ban was a good thing and should stay, exceptions being rare rather than the norm. To do so otherwise would be criminal. The government should be increasing its budgetary allocation to health, not curing a few individuals. (Dawn-7, 29/10/2007) Myriad problems afflict Lyari general hospital KARACHI, Oct 28: Established in the 1970s as a major public health facility, the Lyari General Hospital was later turned into a tertiary-care hospital and made part of the Dow University of Health Sciences. However, owing to numerous problems, its performance has remained far from satisfactory. One of the major objections patients have is related to its emergency services. The health facility, visited by over 1,500 people daily, is almost deserted by 1pm as the majority of the staff, which includes doctors, paramedics as well as sweepers, leave for home by then. The location of the hospital also restricts accessibility as no buses or coaches can approach the facility and patients and their attendants have to reach there by rickshaws and tongas. There is no check on patients’ movements either and it’s a common practice that they leave their beds against medical advice, rest at home and return later in the day or the next morning. Though a casualty section exists that runs 24 hours, patients complain that all major emergency cases, except that of labour, are referred to the Jinnah Postgraduate Medical Centre and Civil Hospital Karachi. 82 “Over 400 patients report daily to the casualty section. Of them, we admit non-surgical emergencies and attend to patients for referrals or medical advice and prescription. This is because all the staff leaves by 1pm. Besides, the section, too, is not properly equipped to deal with critical emergencies,” said a doctor at the department. ‘Ghost town’ About the hospital’s working in late evening hours, a patient said: “After 1pm, the hospital looks like a ghost town. Only maternity and paediatric cases are attended to and that’s the reason people don’t come here for other emergencies and go to CHK or the JPMC straightaway.” His assertion was found to be quite true when this reporter visited the hospital the next afternoon. Excluding the gynaecology operation theatres, all OTs, including the emergency OT, surgical ICU, coronary care unit as well as all diagnostic facilities, were shut. It was also found that doctors keep the majority of surgeries booked for the morning. Due to this at times patients have to wait months for their turn. A few doctors were on duty in different wards but surprisingly, there were almost no paramedics to be found. Only one nurse was spotted in the paediatrics department. Explaining the situation, a doctor claimed that the union of paramedics was too strong and almost half of them only come in the morning to mark their attendance. “They do other jobs in the morning and then show up at closing time. The medical superintendent is powerless while they don’t pay any heed to what the doctors say. If someone sticks to a point, the entire staff unites against that doctor and forces him to withdraw the objection,” he said. He also pointed out that security concerns were one of the major reasons why the hospital had failed to function at its optimum level. Angry attendants “An unstable law and order situation in the locality and security concerns about the hospital’s premises are the major reasons that have acutely affected the working of the hospital staff,” he said, while adding that the hospital catered to the needs of Lyariites, most of whom had little understanding of medical complexities. “They can become aggressive about almost anything. There have been instances when doctors were beaten up by attendants,” he said. Recalling a recent incident, he said that a doctor in the orthopaedics department was beaten up simply because he had asked an attendant not to spit pan on the floor. He also complained about the shortage of staff and maintained the hospital had expanded its operations over the years, but the number of the staff was the same. Besides security concerns, water shortages, frequent power outages and a lack of building maintenance and hygiene are some of the major areas that need immediate attention. A case in point is the paediatrics OPD. The section, visited by over 200 patients daily, was littered with garbage and there was dust all over the place when this reporter visited. It seemed that the section had not been cleaned for ages. There was no water supply in the section, housed in a separate, dilapidated building. An incomplete structure of a washroom stood there as one of the patients complained that its door had not been fixed in four years. He claimed that the earlier washroom was demolished for no reason and this one was left incomplete. The internal telephone exchange has not been working for one-and-a-half years. The same is the case with the lifts. Out of the eight dialysis machines, only one works properly. Though there is seepage in almost all departments, the ceilings of all the operation theatres on the third floor leak while sewerage and drainage problems are a permanent feature. Most of the departments are supplied with saline water and the little tap water that is available is saved for operations. Despite all these problems the hospital, a staffer claimed, maintained a good system of equipment sterilisation. Patients are charged Rs50 for X-rays, Rs25 for ultrasounds and Rs150 for a complete blood count. However, these services are free for in-house patients. A doctor demanded that these services should be free for all as was being done at the CHK, since both hospitals were under the same board of governors. When asked to comment on the situation, Medical Superintendent Dr Mukhtar Khwaja maintained that there was no problem at the hospital and all doctors performed their duties as required and there was no shortage of staff either. About any surgical emergency, he said that resident medical officers took care of that and called any doctor required to deal with the emergency. He also described the paramedics’ union as a helping hand and said a hospital couldn’t run without their support. He commended the gynaecology department’s doctors whose workload, he said, had increased after the closure of the CHK’s unit. “The only problem the hospital has is in maintenance and repairs, which are under the works and services department,” he pointed out, adding that there was a lack of coordination between the hospital and the said department. (By Faiza Ilyas, Dawn-13, 29/10/2007) Two more deaths take dengue toll to 13 KARACHI, Oct 29: Two deaths due to dengue fever were on Monday reported to the provincial monitoring cell by two private hospitals, bringing the official death toll to 13 while the number of suspected cases stood at 1,735 by October 23. However, the monitoring cell is yet to confirm a recent suspected dengue death at PNS Shifa and two additional dengue fatalities reported by private hospitals during the last couple of months. Furthermore, the nearly two thousand suspected cases of dengue fever do not include the 171 patients received under suspicion of the illness and treated at PNS Shifa up to the end of last week. 83 According to the monitoring cell’s data, nine of the people confirmed to have died of the hemorrhagic fever were women aged between 20 and 70 years. Dr Shakeel Mullick, deputy secretary of the Sindh Health Department and in charge of the provincial dengue monitoring cell, told Dawn that one of the reported fatalities was that of a 38-year-old woman from PECHS who expired at the Liaquat National Hospital during the 24 hours ending at 3pm on Monday. The other confirmed dengue death was reported by Baqai Hospital, where a 20-year-old woman died on October 23. Dr Mullick added that his cell had also been informed about the admission of a suspected dengue case at the Liaquat University Hospital Hyderabad-Jamshoro. This is the first case to have been reported from the interior of Sindh during the current spell of the mosquito-borne virus. Meanwhile, 38 new patients suspected to be suffering from dengue fever were admitted to seven government and private hospitals in Karachi. Dr Ziauddin Hospital alone received 20 cases recently, bringing the number of suspected cases brought there to 658 during the current spell. Bismillah Taqi Hospital has so far received 291 patients while the Jinnah Postgraduate Medical Centre and the Aga Khan University Hospital have received 244 and 186 patients respectively. Of the officially confirmed deaths, the first fatality took place on September 2 when a 21-year-old housewife, a resident of Malir who had tested positive for dengue fever, expired at the Liaquat National Hospital. By October 28, this hospital had reported seven dengue-related deaths, four men and three women. Over a span of 20 days, the Aga Khan University Hospital reported two deaths, women in their mid-twenties who lived in the DHA and Kharadar respectively. The JPMC reported the deaths of two women on October 8, while the Civil Hospital Karachi reported the death of a 60-year-old woman who arrived from Balochistan for treatment on October 16. PNS Shifa confirmed the death of a dengue patient on October 23. The last confirmed dengue death was reported from AKU Hospital on October 3. Of the 1,735 cases reported up to October 23, 598 patients tested positive to dengue fever. The monitoring cell informed Dawn that 104 patients were undergoing in-house treatment at eight hospitals. (By Mukhtar Alam, Dawn-17, 30/10/2007) 50% AIDS cases of Pak reported from Sindh KARACHI: Official estimates put the number of positive HIV/AIDS cases at 100,000 in Pakistan and around 50 percent of them are in Sindh alone, informed Dr Arshad Mehmood, programme manager of the Sindh AIDS Control Programme (SACP). He said this during a seminar organized Tuesday under the banner of SCAP and UNAIDS at a local hotel. The main objective of the seminar was to encourage the media to play their equal role in preventing the spread of this deadly disease. UNAIDS supports the government and the civil society in tackling the AIDS epidemic in Pakistan, said Mr. Arkadiusz Majszyk, the country coordinator of UNAIDS. He said, “This effort is a step towards developing a group of media leaders who can advocate and highlight the cause in Pakistan and also at a global level.” The people who are HIV positive because of their high-risk behaviour, such as those indulging in commercial sex activities and drug injections, are not aware of their HIV status and can pass on the infection to their families and loved ones. The media can help educate the masses and protect them from AIDS. In Pakistan, according to a careful estimate, there are above 3,800 recent positive HIV cases, out which 1,900 are from Sindh. This includes men, women and children. One of the main reasons for the number of cases being high in Sindh is that Karachi is like a mini-Pakistan with 20 million people and people come from all over to this city for employment opportunities. This influx has made it easier for this disease to spread in Karachi and other parts of Sindh. According to Dr Syed Qamar Abbas, deputy programme manager of SACP, the media can help in developing an HIV/AIDS prevention programme with a focus on stigma and discrimination. It can also help in bringing out the large number of hidden cases. Dr Abbas admitted that the number of cases is actually double than what is usually reported. “Five years ago, India went through the same denial phase. Now it is the epicenter of the disease with 6.5 million positive cases of HIV,” he said. “We have the same culture and social environment and most of the cases come from the high-risk group.” The forum participants expressed their concerns and also assured that a strategy would be chalked out to encourage a friendly link between the programme and the people living with HIV/AIDS. In the end, the forum recommended the establishment of an ad-hoc committee comprising journalists associated with various organizations. A detailed work plan is to be devised during the next forum meeting, the date of which will be announced at a later date. Additional Secretary Health Niaz Memon, Public Health Director Khalid Shaikh, Member Provincial Assembly Naila Imam and Dr Salman Safdar were also present at the seminar. (By Shahzad Shah Jillani, DailyTimes-B1, 31/10/2007) 84 NOVEMBER Where there’s smoke, there’s garbage being burnt Hundreds of tonnes of solid waste and garbage, instead of being shifted to landfill sites, are being burnt daily by the administration of Jamshed Town in an open space adjacent to the Korangi Expressway, near a Nullah in Akhtar Colony, creating a serious health hazard for area residents. The illegal and immoral act is being carried out on a daily basis for the last three or four months in violation of relevant environmental laws as well as civic norms and values without taking into consideration its adverse effects on the health of thousands of people living in nearby localities. Thick clouds of smoke as well as the intolerant odor of burning garbage can be seen and smelt as soon as motorists venture onto the Korangi Expressway and the causeway that leads to the Korangi industrial area, making it immensely difficult to travel on the road. The smoke, containing highly poisonous gasses including carbon dioxide, carbon monoxide, dioxin and hydrogen cyanide, engulfs the nearby areas including Manzoor Colony, Akhtar Colony, Mahmoodabad and Defence View most of the time and has made the lives of people there miserable. According to area people, the practice of dumping and burning garbage in front of these colonies at the bank of the Malir river was started a few months back by the Jamshaid Town administration as a result of which they were in the grip of numerous kinds of diseases — especially chest and respiratory-tract ailments. Environmentalist Nasarul Islam Usmani, who travels daily on the Korangi Expressway to and from his office told The News that, in the evening, the smoke emitted by the burning garbage greatly reduces visibility on the road and also causes suffocation to motorists. “The thick clouds of smoke from the burning litter can result in fatal accidents on this highway. It is an extremely dangerous practice being carried out by the civic authorities and they would have to be blamed for any loss of life and health hazards to those living across the road,” he observed. Usmani, who is an M.Sc in Environmental Science and working at a waste treatment plant in the Korangi Industrial Area, termed the burning of municipal waste in a densely-populated area in the heart of the city as the, “height of civic neglect and a crime against citizens.” “The smoke emitted by the burning of domestic and market waste normally produces CO2, CO, as well as poisonous gasses like dioxin and hydrogen cyanide, which are highly carcinogenic (cancer-causing substances),” he claimed. On the other hand, the burning of garbage along the Malir River means that all the burnt waste is washed away by the rains into sea, which consequently posses a serious hazard to marine life and is a big cause of marine pollution, he added. Residents of Manzoor, Aktar colonies and Defence View were extremely concerned by the burning of huge piles of litter in front of their homes and claimed that the smoke had made their lives miserable and many were planning to shift to other areas of the city. A resident of Manzoor Colony, Niaz Ali, whose house is on the road facing the Korangi Expressway, told The News that not only does the smoke effect residents, but also that sometimes the ash is carried by strong winds into the houses directly facing the dump yard. “And when the air is stationary, the thick clouds of smoke remain suspended on the road and our locality, causing immense difficulties in breathing,” he said while coughing badly and spitting at frequent intervals. According to him, he had developed a chronic cough and other ailments, including a chest disease, due to the smoke and toxic gasses and appealed authorities to look into the issue and take some action against the illegal practice. Dr Shahid Ahmed Abbasi, a consultant at the Aga Khan University Hospital, when contacted by The News, said that prolonged exposure to smoke from the domestic waste could result in serious damage to the respiratory tract, especially the lungs as well as the central nervous system. He said that inhaling smoke for long periods could result in deposition of carbon in the respiratory tract and lungs and could not only cause asthma and cancer but could also result in other fatal diseases among children and elderly people. During a visit to the site of the garbage burning adjacent to Korangi Expressway, it was seen that the roads leading to dumping site had been narrowed by placing concrete blocks while two policemen were standing there to restrain Jamshed Town staff from throwing their garbage at the site. Korangi Association of Trade and Industry (KATI) Chairman Masood Naqi, when contacted by The News, said that the area where garbage was being thrown and burnt was actually a storm water drain and, if the practice continued, it could increase the water levels, which, in monsoon days, could enter into the adjoining localities. “We have not only written letters to Jamshed Town Nazim Javed Ahmed but also to City Nazim Syed Mustafa Kamal; but the practice is still continuing. We have requested the police to deploy some persons there to prevent the Jamshed town staff from dumping their garbage at the said place,” he informed. However, he deplored the fact that, despite their repeated intimations and requests, the practice was continuing in broad daylight in violation of all laws and added that, if not stopped, the illegal practice could result in serious problems for citizens. Despite repeated attempts, Director-General, Environment Protection Agency (EPA), Sindh, Abdul Malik Ghauri could not be approached as his cell-phone was not responding. The public relations officer of Jamshed Town administration Farhan Khan, when contacted, said that Town Nazim Javed Ahmed will call The News office back to convey his version. However, till the filing of this report, he had not done so. (By M. Waqar Bhatti, The News-13, 01/11/2007) 85 Teenager dies of dengue KARACHI, Nov 2: The Sindh health department on Friday confirmed another fatality caused by the dengue virus at a hospital, pushing the dengue death toll to 17 in the city. In-charge of the provincial dengue monitoring cell, Dr Shakeel Mullick, said that the latest death was reported from Dr Ziauddin Hospital on Oct 31. The deceased, a young man of 18, was admitted to the hospital with the tendency of bleeding and was tested positive for dengue. He said the government had been informed about a total of 14 dengue-related deaths during the past seven weeks. The statistics provided by the cell do not include a dengue-related death confirmed by the PNS Shifa about 12 days back and deaths of two other patients reported from private hospitals during the last two months. Meanwhile, hospitals received 56 new patients suspected of having contracted mosquito-borne diseases during the last 24 hours ending at 3pm on Friday. (Dawn-17, 03/11/2007) Doctors take to streets for demands A group of 250 doctors including house officers, and post-graduates, held a protest on Friday to demand that the government honour its committment to raise their salaries. However, they assured, medical services will not be affected. According to one of the agitating doctors, Dr Sarosh Khan, the medicos were demanding that all doctors including House Officers and post-graduates should receive more than the Rs6,200 they get as pay as they work at least 90 hours a week. “Even a secuirty guard who works for only 36 hours a week receives around Rs8,000,” they observed. Dr Khan claimed that they had been promised an increment of Rs15,000 per month by not only the Vice Chancellor, Dr Masood Hameed, but also by the Sindh Governor, but had not received the revised pay or arrears. He said that doctors would protest daily from 9am to 3pm in camps in the Civil Hospital till their pay was brought at par with their counterparts in other provinces. In this time, the doctors would only handle emergencies. During the time while they would boycott their duties, they would be alternated by the RMOs, and teaching faculty of the university. “We will not let the patients suffer. We only want what is our right. We will not let any casualties go unattended for after 3pm. Before that time, we will be helped out by our alternates,” he said. Meanwhile, there are reports that the House Officers were being pressurized and victimised and four women doctors were even told that they would be handed their termination letters, if the doctors did not stop protesting. It was learnt that a day before the protest, around Rs12,000 were transferred in each of the bank accounts of the doctors in order to stop them from going on strike. Doctors complained that this was ‘blackmail money’ and even then it was not in proper amount to what they were supposed to receive since the past year. They also said that there had been no official or financial statement regarding this transaction of money. (By Xari Jalil, The News-14, 03/11/2007) Revamped lab at ASH inaugurated KARACHI, Nov 3: Due to the preventive measures taken by the city government, the devastation caused by dengue has been nominal this year. This was stated by City Nazim Mustafa Kamal on Saturday. He was talking to newsmen after inaugurating an upgraded pathological laboratory at Abbasi Shaheed Hospital, run by the city government and also a teaching hospital of the Karachi Medical and Dental College. Mr Kamal said that generally the number of fatalities and patients multiplied if the dengue fever disease re-emerged the second year, but the situation in Karachi was well under control and the damage had been contained remarkably. “We have not only redeployed about 800 malaria coolies employed by the government, but also increased the number of machines in order to have extensive fumigation or fogging against the dengue carrying mosquitoes as well”, he said. Coming on to the pathological lab, the nazim said that after the acquisition of the latest diagnostic equipment and deployment of trained manpower, Abbasi Shaheed Hospital’s laboratory had now become the only lab in the government sector throughout the country with such a unique, sophisticated and computerised diagnostic system. Now pathological reports would be available at the computers of respective physicians or consultants in Abbasi Hospital simultaneously, he noted. “It cost the city government an amount to the tune of Rs40 million for undertaking civil/electrical works and supply of furniture and fixtures for the laboratory and electro-medical equipment and now 153 different tests can be performed at the lab”, the nazim said. He urged the staff to take care of the new facilities and package as their own and should not allow anybody to damage those or sabotage this integrated, reliable and accurate test system at any stage. He announced that in-house patients would not be charged for the tests while those seeking tests from outside the hospital would be required to pay only 10 per cent of what was being charged in the market. The nazim said that the condition of Abbasi Shaheed Hospital was not very good a few years back, now with the efforts of the government and dedication of its staff and doctors, the hospital had been able to regain the confidence of the people. The city government would provide some additional funds to the Abbasi Shaheed Hospital annually for the smooth working of the pathological laboratory, he said. (Dawn-18, 04/11/2007) 86 Energy foods supplied to girls’ schools hazardous to health At a press conference at the Karachi Press Club, on Monday, October 29, the District Coordinator (DC) of the Tawana Pakistan Programme, Qaiser Anees said that energy-giving foods — including milk and biscuits — being supplied to girls’ primary schools were in fact hazardous to human health. However, no action is being taken against the company involved, he said. Anees said that the company which was responsible for the supply of these energy foods to schools in all four provinces was Vita Pakistan Pvt. Ltd. He said that the programme had been started by President General Pervez Musharraf. Girls in government primary schools, especially in far-flung and under-privileged areas, were provided milk and biscuits containing 20 different types of nutritional elements. The project was started with an amount of Rs7.63 billion. It was agreed by the federal government that more girls would be enrolled in the schools over time, as a result of this programme. It was also decided that in more than 50 districts of Pakistan, girls from 7000 government primary schools within the age group of 5-12 years would be provided with energy foods. On March 20, 2007, President Musharraf launched the programme in the Gwadar district of Balochistan, after which three other districts from each of the other provinces was also started, including Badin (Sindh), Lakki Marwat (NWFP) and Dera Ghazi Khan (Punjab). At the launch, President Musharraf reiterated that because these young girls did not receive enough dietary elements from home, they would be given these energy foods which contained 20 different kinds of nutritional ingredients. This was done so that they could become healthier and, therefore, mentally and physically stronger, as these children are the future of the country. Likewise, the programme was also started in Badin, where 16,000 girls studying in 170 schools in the district received these packets of energy foods. The company was Vita Pakistan Pvt. Ltd, Lahore. The condition on which Vita Pakistan was allowed to work on behalf of the government in this project was that the food supplements be packed hygienically and contain all 20 nutritional elements. However this standard was not maintained, and by September 2007, various complaints regarding the food packets started coming in from Badin, including that the biscuits were not fully baked and smelt stale with black marks on them. The milk, too, seemed stale and did not dissolve properly. Upon receiving these complaints, Anees asked the Badin representative of Vita Pakistan, Umar Farooq Cheema, to retract the stale food and send in a fresh supply, but nothing has happened in this regard so far. Anees said he later met with Zainabunnisa, the headmistress of a primary school in Badin, who showed that the biscuits seemed expired. At this, he called Umar Farooq Cheema, made him sign on a monitoring form, and sent the stock to the Pakistan Council for Scientific and Industrial Research (PCSIR), Islamabad, for testing. The report said that the food which was being supplied to the children in the schools was hazardous to human health and that consumption should be immediately discontinued. A case was registered against Vita Pakistan, regarding this, but still the police have not arrested anyone yet. On the other hand, Anees said he has been receiving death threats and has been facing pressure to withdraw the FIR. (The News-20, 05/11/2007) Fixed rates of platelets bags urged KARACHI, Nov 5: The secretary of the Pakistan Medical Association, Dr Qaisar Sajjad, urged the Sindh government to fix the price of platelets bag so as to facilitate people affected by dengue fever. He was speaking at a seminar on “Prevention of haemorrhagic fever and dengue fever” at the PMA House recently. He said that people were facing a lot of problems in getting platelets bags. According to him, different blood banks or hospitals are charging differently for one mega unit of platelets, ranging from Rs7, 600 to Rs12, 500. They also have to provide a donor on an exchange basis which causes sever mental torture to the attendants of the patients. Dr Faisal Mehmood, Associate Professor Infectious Diseases, said that most dengue patients did not need admission to any hospital as long as the danger sign like bleeding from any location occurred. He advised to increase fluids intake and reduce the temperature with paracetamol only. “However, it is important to realise that platelets transfusion is only needed if the risk of bleeding is high and giving platelets does not help cure the infection or help the body’s own platelets to recover quickly”, he added. Dengue cases According to the provincial dengue monitoring cell, the number of patients suspected of having contracted dengue or haemorrhagic fever, who were brought to various government and private hospitals, in the city, has crossed the figure of 2,000. During the last 24 hours ending at 3pm on Monday, another 57 patients were rushed to hospitals for treatment of dengue fever. (Dawn-18, 06/11/2007) LGH gynae section lacks staff, basic facilities KARACHI, Nov 5: Despite being a major teaching hospital in the city functioning under the board of governors of the Civil Hospital Karachi, the Lyari General Hospital is one of the most neglected public sector hospitals. The numerous problems that plague the services of this hospital are only reflective of the government’s apathy to public health. Security concerns aside, the hospital lacks even basic amenities. This affects the staff of the gynaecology and obstetric department more as they work round the clock to attend to various obstetric emergencies. 87 “Ours is the only department at the hospital which provides round-the-clock emergency services. The department never closes and we do our duties no matter how critical the law and order situation in Lyari may be. This is not a favour, but rather a duty, but we should at least be supported in our efforts and the administration should provide us with basic facilities,” a group of doctors at the hospital said. Like the rest of the hospital, the department faces an acute shortage of water, power outages are a norm while paramedics and sweepers disappear by noon. More perturbed at the situation, though, are the trainee doctors who are finding it hard to face the reality. “The doctors have to administer injections, drips and change urine bags. There are not even registers for making the file of a patient and we have to do this by stapling loose papers together. I thought the CHK was bad, but this hospital is worse,” a trainee lady doctor says. Raising similar concerns, senior doctors said that the hospital administration knew well all the problems afflicting the entire hospital. They claimed that they had to bring water from home not only for drinking, but also for toilet purposes. The hospital generators were used only for operation theatres and labour rooms and there was complete darkness on the rest of the hospital premises during long power breakdowns, which made working at the hospital risky as there was no security guard. “There are no emergency lights in the operation theatres and we keep one on our own because the power supply system takes 15 minutes to half an hour to switch onto the generator,” said a doctor, adding that at times they had to ask patients to buy gloves for the operation. They further claimed that recently a case had to be referred to the CHK because there was no linen in the department. There was no surgical intensive-care unit at the hospital so expectant mothers with complaints of eclampsia or asthma are referred to either the Jinnah Postgraduate Medical Centre or the CHK. The doctors also criticised the hospital administration for not providing them with a separate delivery set for hepatitis patients. “Though all the equipment is sterilised, the standard procedure is to keep a separate delivery set for women suffering from any highly infectious disease. Hepatitis is reportedly more common in patients who either have blood transfusion or went through surgery,” a doctor pointed out. While the law and order situation remains a key issue in the locality, the lady doctors, also at times, have to bear with the hostile attitude of patients. “Aap ko pata nahi ye Lyari hai. This is how they react every time they feel they are being neglected in treatment,” said a lady doctor. Fewer than a thousand women, all of them from socially-deprived background, report at the outpatient department every month, most of whom have a poor record of antenatal attendance. Neonatal mortality (deaths occurring during the first four weeks after birth) and perinatal mortality (deaths in the first week of life and stillbirths) is high with maternal morbidity. “Most of the women are illiterate and believe that doctors opt for an operation to make money. They are not regular in antenatal checkups and report after being horribly attended to by the dais,” she said. According to doctors, almost half of the 500 childbirth operations that take place every month involve cases mishandled by the dais and the rest are registered ones. Another factor playing havoc with women’s health was drug addiction, a doctor said, and that involved even young girls. “This problem affects the health of the mother and can lead to premature deliveries. This compounds the misery of poor women who are already anaemic, living under stressful conditions,” said a doctor. The doctors also lamented the fact that the hospital did not provide a 24-hour blood bank service desperately required to attend to the needs of anaemic women. “We ask attendants to go to the Patients Welfare Association, CHK, and arrange blood for the operation. This is unfortunate since the blood bank at the hospital is unable to fully meet the patients’ needs here,” said one of them, adding that there was no facility at the hospital to have specific blood tests done for any pregnancy complication after 1pm. When contacted on the phone, Chairman of the Board of Governors of the CHK and the LGH Abu Shamim Arif attributed the deplorable conditions at the hospital to an acute shortage of funds while Medical Superintendent Dr Mukhtar Khwaja said steps were being taken to address the hospital’s myriad problems. “Water tankers have been arranged for the hospital while Rangers are also being deputed at the hospital,” he said while asserting that no case was ever referred to any other hospital and there were no problems with the paramedics either. (By Faiza Ilyas, Dawn-18, 06/11/2007) ‘People living near Kanupp exposed to radiation’ KARACHI, Nov 5: The Provincial Disaster Management Authority Chairman, Syed Anwar Haider, has expressed concern over growing fire incidents, re-erecting of hoardings and hazardous effects of Karachi Nuclear Power Plant. He was talking to media persons after the inaugural session of a five-day “Disaster Risk Management Training Workshop”, organised in collaboration with the United Nations Development Programme, on Monday. Mentioning that radiations from the nuclear power plant have put at risk the lives of those residing in its surroundings, he called for provision of safety area around the plant. He said that the ‘disabled’ department of Civil Defence must be reactivated on modern lines for which the city and district governments of the province must act. He also expressed concern over the state of affairs in building control authorities of the province and the state of railway bridges over rivers, which were at the risk of collapse. The PDMA chairman said that the draft of a provincial disaster management plan was being prepared, which after consultation with stake-holders would be presented to the chief minister in March 2008. He said the plan would be districtwise modified to cover the area in accordance with its needs. Recalling that National Disaster Management Authority’s efforts prevented loss of human lives in coastal areas of the province, he said that stock of 30,000 camps was available with the authority for emergency situation. 88 Anwar Haider said untreated industrial, chemical and sewage was getting mixed with potable water which could cause spread of waterborne diseases. Earlier addressing the participants of the workshop, UNDP representative Zafar Iqbal said that institutional infrastructure for disaster management was required at provincial level that must not just react at the time of disaster but for its prevention in collaboration with stakeholders. Other speakers expressed hope that the establishment of National Disaster Management Authority and the issuance of notification about PDMAs would bring radical positive change. (Dawn-18, 06/11/2007) Legislation against unsafe injections urged The Sindh government has sent recommendations to the federal government to bring the legislation for the registration of syringes and impose a ban on the reuse of disposable injections, said Special Secretary Health, Sindh, Captain Dr. Abdul Majid here on Wednesday. Such steps were necessary to control diseases as the main factor behind an increase in Hepatitis-B, Hepatitis-C and HIV/AIDS. Speaking at a seminar titled “Advancing injection safety”, organized by the Pakistan Medical Association (PMA) along with a private company, Dr Majid said that the Delta virus had hit Sindh province recently because of the use of unsafe injections and so far around 60-70 such cases have been detected in one district, Kamber Shahdadkot, only. He said the proper disposal of syringes is the main issue. Dr Majid pointed out that all government hospitals have the facility to destroy syringes but regrettably, this is not being done. Similarly, all hospitals have been provided cutters to cut needles-syringes but at one hospital, it was found that needle was being used as a paper pin. He said reuse of razors was causing diseases especially in rural areas. He hinted that the Sindh government was contemplating the provision of razors free of cost in interior Sindh to prevent diseases. Responding to the criticism of some speakers, he said it was not easy to ensure the sale of injections without the prescriptions of doctors. Dr Majid said that doctors were supposed to make three copies of their prescription but that was not being done. Similarly, if the government implements Drugs Act, which makes drug sale licences imperative before opening a pharmacy, then several medical stores including those owned by doctors could be closed. “Sometimes, we avoid strict implementation of laws as it can harm the public,” he said. He added that community behaviour is also important for the proper use of syringes as the government could not “effectively implement” laws. Dr Majid urged the firms to reduce the price of syringes. Dr. Qaiser Sajjad, general secretary, PMA, said that around 70,000 injections are being administered to the people in Karachi only and about 80 per cent of such syringes are being collected by sweepers. He said about 63,000 drug addicts were involved administering themselves injections. Dr Afia Zafar of the Aga Khan University Hospital (AKUH) said healthcare workers (HCW) were exposed to blood and other body fluids, which can lead to serious health problems for them if precautionary measures are not taken. She suggested the use of a needle driver or holder instead of using one’s fingers. She said the use of needles should be avoided where safe and effective alternatives are available. Dr Aamir Javed Khan said around 62 per cent cases of hepatitis-B, 82 per cent cases of hepatitis-C and 10 per cent cases of HIV/AIDS were caused by unsafe injections in the country. He said that in Sindh, eight injections are being administered to each person annually as a culture of injection is thriving, taking its toll on human lives. Zulfiqar Abbas Zaidi said that around 61 billion injections are being used in developing countries and many times, the injections are unjustified or unnecessary. He said that sometimes, the patients demand an injection for psychological reasons. Besides, financial incentives also induce doctors to administer it. He said that around 80-90 per cent injections are unsafe in the country. Dr Zaidi regretted that even for minor ailments, injections are being used. About medical waste, Dr Zaidi said that it was alarming to note the way in which waste is managed at hospitals. He said most of the used syringes and needles are dumped in open rubbish bins just outside hospitals, which are then collected by scavengers, mostly children who sell the same at a price of Rs8-15 per used syringe. He suggested that the government should invest in new technologies for the auto-disposal of medical waste. (By Imtiaz Ali, The News-20, 08/11/2007) Industrialisation ruining life in villages around city KARACHI, Nov 10: Scores of villages falling in the jurisdictions of Malir, Gadap and Bin Qasim towns have been facing, what local residents fear, an environmental disaster owing to the industrialisation of the originally and officially agricultural terrain. Many of these hundreds of industrial units sprung up over a couple of decades appeared to be illegal and oblivious of environmental laws and public health rules. Until recently called the rural areas of Karachi, these villages are inhabited by a big population with farming being their livelihood. Prior to the mushroom growth of Industrial units in these areas, the villages formed a lush green belt covering a vast and wide border of the city and served as picnic spots for the urban population. The villages exposed to environmental degradation and their population to all sorts of health hazards include Kohi Goth, Shafi Goth, Rehmat Bagh Goth, Haji Pir Goth, Achanak Para, Nazar Mohammad Goth, Saleh Mohammad Goth, Umar Bagh, Saeedabad, Piro Nawab Goth, Gharibabad, Baitullah Bagh, Mulla Moosa Goth, Wali Goth, Faqir Mohammad Goth, Juma Kando Goth, Punshumbe Goth, Sheedi Khan Goth, Lohani Goth, Moosa Jokhio Goth, Pir Sirandi Goth and Lashari Goth. 89 The first raiders The fertile lands of the beleaguered villages were first stricken by the suppliers of earth known commonly as the “reti-bajri mafia”. For many years, operators of trucks used to take away hundreds of tons of earth from these villages every day for sale to builders and developers. They left much of these lands barren and deprived the poor farmers of their only livelihood. The menace of widespread excavation by these earth traders was curbed to some extent when the starving farmers, with the help of local political leaders, made it a case through an extensive campaign for their right to live. However, the villagers are still faced with rapid industrialisation which has now become a major problem, posing a serious threat to the environment and public health in the entire agricultural belt. “Ironically, most of the industrial units in the rural pockets of the city have been established without any planning or permission from a competent authority,” said an educated villager. There is no mention of such industrial units in any master plan which makes one to believe that they are illegal,” he added. Most of the villagers interviewed by this scribe expressed the view that owners of these industrial units would just buy the lands at a throwaway price and use it for any purpose they want. “Their assault has rapidly turned the fertile agricultural lands into a jungle of industries,: said one of them. Fallout Narrating the ultimate outcome of the unplanned industrialisation, the villagers pointed out that mills and factories were being established within the proximity of the residential lanes and the local population was exposed to toxic discharge and air and noise pollution. “There is no concept of privacy and security in any village having a few industrial units,” they added. They further pointed out that untreated industrial waste and effluents were constantly being discharged into the nearby Sukkun and Malir rivers and the practice was continuing for years unchecked. Coupled with criss-cross water and sewerage lines, the hosepipes discharging effluents elsewhere have created unhygienic conditions all around and polluted the source of potable water, endangering the health of local population, which has a limited access to health care facilities and meagre resources to afford medical treatment. They said that water, power, sewerage and other basic amenities had been provided to the villages as per the requirement of the local population but these utilities were being shared by hundreds of factory workers without any expansion having been done by the government agencies. The agricultural lands of Bin Qasim Town, once starting from the Quaidabad locality, have vanished and industrial units could be seen functioning up to several kilometres ahead along the National Highway. The old PIA farms surrounded by lush green fields have also been converted into an industrial zone. More industrial units have been set up around the Karachi Export Processing Zone near Shafi Goth. A major industrial unit stretched over eight acres and a similar one next to it are in the process of construction. The two units alone have completely surrounded Kohi Goth and Haji Pir Goth. An industrial unit spread over 10 acres next to Kohi Goth and another one covering 30 acres along Kohi Goth, Achanak Para and Saleh Mohammad Goth have been planned to be set up soon. The concerned villagers argued that industrialists must be made to seek the required NOC or permission and for the establishment of such units and the relevant government agencies should issue such documents only after ensuring that these establishments did not cause any harm to the local population. They demanded that the industrial units set up illegally be dismantled and a strict check be maintained on such unlawful activities. The villagers also expressed the fear that the rapid industrialisation in the whole area could deprive them of their ancestral lands as was witnessed in other parts of Karachi. They said the city nazim had repeatedly been apprised of the situation but an appropriate action was yet to be taken. (By Latif Baloch, Dawn-19, 11/11/2007) 14 high-grade fever deaths in Keamari Town spark fears Fourteen people, including women and children, have died over the last month-and-a-half in 18 villages of Deh Allah Bano (Allah Obano), Keamari Town, reportedly of malaria or high grade fever, triggering fear and panic among the residents. It also prompted the Pakistan Medical Association (PMA), Karachi, to set up a medical camp along with a modern laboratory test facility on Sunday (today) to ascertain the exact causes of deaths as the government was allegedly taking “inadequate steps” to control deaths apparently caused by preventable diseases. The Town Health Officer (THO, Keamari, Dr Nazeer Kolachi, confirmed the death of seven people, which, according to him, was caused by ‘high grade fever.’ However, he said that blood samples of around six patients confirmed the existence of malaria in the area. “We are sending a team of specialists along with laboratory equipment to take blood samples,” Dr Qaiser Sajjad, secretarygeneral, PMA, said. He said they had already arranged for a test for five patients at the Civil Hospital, Karachi (CHK), and three of them were confirmed cases of malaria. He hinted that other patients might be suffering from a “viral problem”. He said that there was no proper diagnosis facility to detect different viruses. He said that, at present, only “kits” were available to detect dengue or Congo viruses only but there is no facility to detect the “Chicken Gunia” virus, which had claimed several lives in India. “We are not satisfied with the government’s efforts,” said Sami Memon, spokesman for Pakistan Fisherfolk’s Forum (PFF), a representative organisation of the fishermen. He said that Keamari Town had arranged a medical camp on Thursday just to “fulfill a formality”. He said that, so far, 14 people had died over the last month-and-a-half. They were identified as Wasim Ishaq, 18, Fayaz, 6, Mab Bibi, five days old, Sher Jan, 20, Hasil Dolat, 40, Ms Kalsoom, 50, Ms Malooka, 23, (full-term pregnant), Ms Zubaida, 27, Ms Hafeeza, 50, Asif, year-and-a-half, Allah Bux, 18, Mohammed Hashim, 15, Karim Bux, 43, and Sonia, 12 days old. 90 He said that Karim Bux and Sonia died around three days ago, which put a question mark over the tall claims of the local government that they have taken steps to improve the health conditions there. He said that transportation was also a problem as the villages were located around 50 kilometres away from the city. Dr Nazeer Kolachi said that they have conducted fumigation in all villages. (The News-13, 11/11/2007) One per cent of children are diabetic The world will be celebrating the International Diabetes Day on November 14, with this year’s theme focusing on ‘Diabetes in children and adolescents’. The ratio of children affected with diabetes in Karachi is less than one percent per 0.1 million people as compared to 40 in Finland and 14 in Kuwait, said Dr Ali Nawaz, senior child specialist at the Civil Hospital. There are estimated around nine million people affected with diabetes in Pakistan at present, according to the National Diabetic Survey of Pakistan conducted by the Diabetic Association of Pakistan (DAP) and World Health Organisation (Who). According to the International Diabetes Federation and Who, this number will rise to 17 million by 2025. “One of the major reasons behind an alarming increase in diabetes is over eating and less walking,” said Dr A. Samad Shera. Another major risk factor is what he called “weapons of mass destruction” namely burgers, bun kebabs, biryani, fried chicken, sweets, aerated drinks and other junk food. He said that the most disturbing thing is that these fast foods are being encouraged in schools where restaurants provide the same at subsidised rates. “Obesity is the biggest risk factor for diabetes, which is now starting from children,” claimed Shera. A lack of sports activities in schools and children sitting for long hours playing computer games is another reason for the increasing rate of diabetes among children. Regarding the complications arising out of diabetes, he said that if diabetes is not controlled, it can affect other organs as well. But if blood sugar is controlled in its initial stage, the chances for health complications are less or nil. “Diabetes adversely affects the eyes, kidneys, foot, heart and nerve system,” Shera added. Dr Habib Rehman Soomro, secretary general of the Pakistan Medical Association (PMA) said that around 11 per cent of the population is suffering from diabetes with a 90 per cent chance of developing retinopathy in their lifetime. Half of this group is at a huge risk of becoming blind if not treated by laser therapy. “A majority of the adult population with diabetes has no access to treatment for the complication of diabetes related to blindness,” he said. Except five or six government health facilities, a majority of government eye hospitals do not have a working laser therapy unit, Soomro added. Nawaz said that around 100 diabetes patients visit CHK daily. He said that women are more affected with diabetes because of stress and tension arising out of socio-economic problems, which is one of the causes of diabetes. (By Imtiaz Ali, The News-19, 11/11/2007) Rising drug sale in city affecting youth As the city is bogged into the price hike of commodities and other security concerns, the unnoticed flourishing narcotics trade is decaying youth day by day. Shahid, once a young and smart fellow of Frontier Colony site, is now among many of the citizens who spend their nights inhaling heroin in graveyards and garbage dumping sites. The dilemma of the flourishing trade of heroin and other narcotics seems to be least bothering for the official quarters. Life long drug addicts like Shahid are found in abundance, behind the Sindh Secretariat Building, the Provincial Headquarters of the Sindh government, which exposes apathy of leadership. Shahid has lost his fortune, health, family bond and circle of loyal friends. He wishes to quit the habit but actually is too addicted to do so. The sale of heroin and hashish is on the rise in slum areas and inner streets of SITE, Baldia, Lyari, Landhi, Orangi and other outskirts areas of city. The drugs are supplied to these areas from Hub. Local police have expressed helplessness in controlling small-scale trade of the drugs and urged monitoring at entry points of the city, however, Shahid said that without support of the area police, not a single “puri” of heroin can be sold. Besides residents of poor areas there have been reports about use of hashish in educational institutions of well-off areas too. Decaying of Shahid, like his fellows, rings an alarm of concern that celebrating global day is not enough to prevent the future generation from crumbling. Alongside providing healthy amusement, opportunities and health awareness is much needed to counter the narcotics menace. (The News-19, 11/11/2007) Dengue fever continues EVERY year for the past few years, authorities hope for a miracle which will make dengue fever disappear. This perhaps explains why despite knowing that preventive steps can be taken to ensure safety of citizens, various city administrations do very little to combat the fatal viral fever that kills scores of people each year. Because that miracle has yet to occur, it is high time health authorities, along with city administrations, took their jobs seriously and addressed the issue on a warfooting. It is shameful that other developing countries in Southeast Asia for instance, which have similar problems in bureaucracies, manage the dengue crisis better. They develop effective strategies to combat the virus by ensuring mass fumigations drives take place. Areas where the virus is reported are marked as red-zones, where extra measures of sanitation are taken. They also ensure that hospitals are well equipped to deal with the inflow of patients. 91 In Pakistan, there are half-hearted fumigation drives, few treatment camps set up and hospitals are rarely equipped to deal with the problem. This is despite knowing that the problem will occur every year right after the monsoons. So far this year, nearly 35 people have died of dengue fever and many of these deaths could have been prevented if authorities had handled the issue better. It requires a complete overhaul of strategies. Much of the problem has to do with the administration’s complete failure to maintain public hygiene. Leaking sewerage systems, stagnant pools of water everywhere, open garbage dumps, storm water drains that aren’t ever cleaned are all too familiar sights all across the country. These problems need to be addressed so as to prevent epidemics. It is now widely admitted that the government does not have resources to provide health care to the citizens. But surely it can ensure that they do not fall ill because of its negligence in the areas of sanitation. This cannot be overstressed as there is no known cure for the dengue, the government’s strategy should focus on prevention as well as early detection and treatment. (Dawn-7, 13/11/2007) The never-ending filth and potholes Even though the Liaquatabad Town Nazim Usama Qadri has seen to the construction of quite a few roads and sweepers are seen bending their backs laboriously brushing away the dust and the litter from the streets, it is still a disappointment to note that not all the areas of the town have been sprayed with insecticide. This was promised to counter the spread of the dengue virus. Also, accumulated garbage in the area also makes for a not-so-pleasant sight. It is commendable that, in general, the main roads of the town have now become cleaner and many residents say that they feel a rushing sense of pride of living in this area. Near the Nazimabad Petrol Pump stop, which used to be a crowded stop for public buses, one can now see an island with a neatly trimmed and well maintained lawn. One can also see children playing around the larger-than-life toy dinosaur. Over all, the lights on the main roads illuminate the area in a subtle way. Unfortunately, these are only the main roads. In the streets inside and the alleyways, there are hardly any streetlights. There are roads which still need repairs given the potholes on them. Right opposite the signal, at Nazimabad number seven, there is a lane that leads to the old National Database and Registration Authority (Nadra) office, but even while the office was functioning, there were absolutely no street lights. In fact, it is often at this point that there have been problems — women have been harassed by men, and several hold ups have occurred. The roads here are desolate and not many pass by them as it is a residential area. By night, the shops are all shut, and for the lone pedestrian going home, there is no security in terms of either street lights or any deployment of police personnel. A walk through Liaquatabad Town’s well-known encroachment, Mujahid Colony, which has now spread all over the circular railway tracks, reveals dirty narrow street corners and open gutters covered with a swarm of mosquitoes. Earlier in November, the town administration announced that there were machines being brought in for spraying after the city nazim had directed all towns to do so. In fact, it was stressed by the authorities that part of the city would be bereft of this drive so that the dengue-carrying mosquitoes could be eliminated. But here in the narrow lanes of Mujahid Colony, some of which are interlinked with the adjacent Moosa Colony, there are open gutters bubbling with sewage water and the whole area is filled with its stench. Mosquitoes swarm around, and flies sit on the open food being sold. A resident of the area, Zarmeena, says that many people do fall ill and almost every week, there is someone or the other in her neighbourhood who has been admitted in a hospital. When asked about whether or not any government vehicles had been seen carrying out the drive, she said that she had not seen any. She also said that there was no sweeper in this area, and no government truck came to collect the garbage. The town administration should concentrate on these low-lying areas, instead of only the main roads so that the overall condition of the town can be improved. (By Xari Jalil, The News-19, 13/11/2007) ‘Deranged’ woman kills her four children KARACHI, Nov 13: A young woman believed to be suffering from a mental disorder killed four of her children and wounded two other daughters and her husband in the early hours of Tuesday in Ayub Goth, Gadap town. Her shaken husband, Abdul Rehman, told Dawn that a scream woke him up at around 2am. “As I came out of the room, I saw my wife Gul Noor bent over my elder daughter, trying to smash in her head with a cleaver,” he said. “She told me, ‘I have killed your children’ and then hit me in the head. After that, my two elder daughters Muneera, 15, and Humaira, 12, both of whom were injured, helped me overpower Gul Noor. ” She earlier drowned four of her children – Hammad, eight months, Ali Mavia, 4, Mattah Bibi, 7, and Tehmoor, 10 — in the underground water tank. According to a neighbour, she weighed the tank cover down with concrete blocks after having dumped in the children. According to Abdul Rahman, his neighbour Liaquat was the first to arrive at the scene and attempt to get the children out of the water tank. He managed to recover three bodies. Another neighbour, Manthar Ali, told Dawn that on his fifth attempt he felt the last child’s body which floated upwards minutes later. As efforts were being made to recover the children’s bodies, Gul Noor sat still and silent as a stone in the room where her husband had sent her, said Manthar Ali. He added that the couple’s eldest child Muneera is a Hafiz-i-Quran and teaches at a nearby madressah. The police and Edhi services were subsequently informed and the three injured persons were taken to Abbasi Shaheed Hospital where they were treated for head wounds. Gul Noor was taken into police custody but had to be taken to Abbasi Shaheed Hospital after she collapsed. 92 ‘An ideal marriage’ Abdul Rehman, who used to work in a marble factory, is currently employed at a hosiery factory. He told Dawn that his wife had not been feeling well for the past four or five days and that he had taken her to Abbasi Shaheed Hospital where she was given medicines. He said that as a result of those medicines, her face had swollen up and he had thought that she had probably taken an overdose. “Despite her condition, she asked me not to take any time off work and assured me that she was alright,” said Rehman, adding that she had been feeling nauseous the night before the violent incidents. Recalling her medical history, Rehman said that in 1992, following the birth of their first child, Gul Noor had suffered some serious mental disorder. She had been in Gilgit, their native town, at the time. Since Rehman worked in Karachi, he brought her to the city for treatment. According to Abdul Jabbar Nasir, a relative of the family who was present at the tragedy-struck house, her treatment continued for a year and she finally got respite after receiving ‘spiritual treatment’ from somewhere in New Karachi. However, he added that the couple had been very happy together, a view endorsed by Rehman who said several times during the conversation that they had been ideally-married for the past 19 years. ‘Postpartum depression?’ A senior psychiatrist, Dr Syed Ali Wasif, said that the tragedy may have been the outcome of postpartum, or post-childbirth, depression. It frequently goes undetected amongst women in our society, he explained, saying that if directed inwards, the medical condition can lead to suicide while if directed outwards, it can result in the patient killing someone else. He quoted a survey conducted by a team of doctors a few years ago in different Karachi hospitals, which showed that roughly 40 per cent of new mothers suffered from the condition. Gadap town SP Mir Husain Lahri told Dawn that Gul Noor’s statement has not yet been recorded as she was unconscious and admitted to Abbasi Shaheed Hospital. However, the police have registered an FIR under Section 302 of the Pakistan Penal Code, he said while remarking “no sane person or mother can kill her own children.” (By S. Raza Hassan, Dawn-17, 14/11/2007) Diabetes puts the world at risk THE year 2006 was important for people suffering from diabetes. An aggressive campaign by health professionals won diabetes recognition from the United Nation as a disease that is a serious threat to global health. This was long over due. Today the world has 246 million diabetics and their number will grow to 380 million in 2025 if no intervention is made. The UN’s Landmark Resolution (61/225 of Dec 20, 2006) recognises diabetes as “a chronic, debilitating and costly disease associated with major complications that pose severe risks for families, countries and the entire world”. It designated Nov 14, the day of birth of Frederick Banting, the Canadian researcher who identified insulin, as the UN day for diabetes to be observed every year beginning in 2007. The International Diabetes Federation and World Health Organisation had introduced the day in 1991. Thus diabetes is the first non-communicable disease to receive a status similar to that accorded to malaria, tuberculosis and HIV/AIDS. Governments have been called upon to develop national policies for the prevention, care and treatment of diabetes. This should prompt the health authorities in Islamabad to address the issue at the policymaking level given the fact that the country faces a serious epidemic of diabetes. In 2003 the estimated number of diabetics in the 20-79 years age group in Pakistan was 8.5 million. This is projected to rise to 22.5 million by 2025. Lack of awareness, insufficient medical care and the absence of social security structures in the country are major factors contributing to the prevalence of the disease. With 26 per cent of the people (according to government sources) – though the number is believed to be higher -- living below the poverty line and a low literacy rate, diabetes does not get the attention it merits. It is not just the challenge high levels of blood sugar poses that is worrying. Equally hazardous are its devastating and insidious complications ranging from serious heart and kidney problems to amputations, strokes and blindness. Yet health programmes in Pakistan have conventionally focused on the control of malaria, tuberculosis and HIV/AIDS, maternal and child health, immunisation against communicable diseases, prevention of hepatitis, cancer treatment and drug abuse but overlooked diabetes. This issue must now be addressed and the government can help in many ways. The dietary factor plays a major role in the prevalence of diabetes because the disorder is attributed to the burden of the genetic factor of central obesity that leads to insulin resistance, a precursor of diabetes, found in Asian adults and children. Obesity acts as a trigger in those who are genetically disposed to diabetes. Today more and more children and adolescents who are obese are being diagnosed with diabetes. There are no countrywide figures on childhood obesity and type 2 diabetes in Pakistan. Only one survey by Jafar et al has been reported which finds 25 per cent of the population in Pakistan to be overweight. More worrying is the estimate given by a survey supported by the Higher Education Commission that 20 per cent of children from affluent families studying in private elite schools are obese and potential victims of diabetes. Nearly four per cent of children from low-income families were also found to be overweight and malnourished. The rise of obesity is linked to a sudden change in lifestyle. Consumption of dense calorie foods and decreased physical activity are the major factors. Karachi, a city of 15 million, has only 15 public and four private parks, many of which are not properly maintained and are under constant threat of encroachment by builders and developers. The inaccessibility to open spaces as well as cultural constraints discourage many people from taking physical exercise. Health awareness is low due to illiteracy which along with inflation promotes wrong eating habits. The obesity epidemic has entered Pakistan and has to be curbed by efforts from all quarters. The city governments should plan more secure open areas for exercise. There is need for awareness campaigns against obesity and stricter laws requiring packaged foods to be labeled with the ingredients listed. High caloric foods should have a warning similar to the one carried by cigarette packets. Schools should work out programmes for healthy eating and discourage canteens from serving fast food, the curse of modern living. It is time the authorities rethink their approach towards the advertising of food and drinks on bill boards, television and newspapers. We could learn a lesson or two from the anti-smoking lobby which had cigarette advertising banned. 93 It is time the responsibility of health professionals is shared by leaders of opinion such as teachers, the clergy and NGOs who interact with people at the grassroots. The importance of physical activity, consuming simple food and keeping one’s body weight in the normal range can not be overemphasised. It is not too late in the day to launch joint campaigns in which the government, the people -- children and adults-- health professionals, educators, religious leaders and media should participate to fight against the obesity epidemic. The future of the next generation is at stake and has to be secured. Those who have already crossed the red line and are suffering from the disease, especially those who are poor, need a helping hand. Many can manage on tablets but others need insulin. These drugs can be termed life-saving for a diabetic cannot survive without them. Since there is no cure for diabetes, the drugs have to be taken for life. On an average a person on insulin has to spend 2500 rupees a month on his medicines which include those for high blood pressure, heart disease and raised blood cholesterol. A patient who needs tablets spends less – about 1500 rupees per month. These drugs are more costly in Pakistan than in India and a family of modest means can ill afford to spend that much on drugs to keep one member alive. Usually more than one are affected. These are minimum costs. More is spent on laboratory tests, syringes, and other procedures. The price of insulin and tablets can be brought down if the government were to drop the taxes on these drugs and subsidise their cost. (By Dr. Fatema Jawad, Dawn-7, 14/11/2007) She brought them into this world and she took them out KARACHI: When 32-year-old Gul Noor fully regains consciousness in the Civil Hospital psychiatric ward she will have to come to terms with the fact that she killed four of her children on Tuesday morning. This, psychiatrist Dr Uzma Ambareen said, means she could become a danger to herself and needs to be quickly assessed. “Noor was so impassioned at that time and she was super strong,” recalled her husband Abdul Rehman, who works as a tailor at a textile mill. He was roused from a 2:00 a.m. slumber by the screams of his girls. “When I saw her in this condition, I grabbed her while my daughter took the knife from her hands.” Noor, who had learnt the Quran by heart, killed her three daughters Tanoor (8), Munteha (7), Ameer Mavia (4) and nine-month-old son Hammad in the morning in their Sohrab Goth home. She drowned the children one by one in their water tank and then tried to stab Munira (13) and Humaira (10). The screams were so bad that neighbour Ali was afraid to enter the house. He eventually ventured in with another neighbour Ashfaq. They found Gull Noor with a rope and her husband and surviving daughters bloody by the tank. The bodies and injured were rushed to Abbasi Shaheed Hospital. According to Rehman, when he and Noor got married 18 years ago, she was perfectly fine. She had studied till middle school in their village of Astoor near Gilgit and was counted as one of the more educated girls in her neighbourhood where mostly female education was limited to primary school. Her father was a teacher as well. One of Noor’s relatives recalled that when her first child, a daughter, was born in 1992, Noor had fits of anger. She would tear at her clothes, scream and throw things. At that time they were at their village. They showed her to doctors all the way in Rawalpindi to no avail. Her husband was in Karachi at the time. She was shown to various doctors here as well. When all this failed, they undertook ‘roohani’ healing and apparently she improved. This entire process took six months but during that time she tried to kill that child. She approached someone for a ‘chilla’ to help her conceive a son. “Noor was so happy after our son was born,” he said. “I don’t think the chilla had any bad effect on her.” Three days ago she had a light fever and her eyes turned red, the relatives said. The family took her to Abbasi Shaheed Hospital where doctors suspected that it had happened because she was taking some medication. They recommended eye drops. But from Monday, she grew lethargic. Nonetheless, she went about her usual chores, laid their beds etc. Rehman noticed, however, that she appeared upset but when he asked her, she said she would just do some work and then go to sleep. The two daughters who have survived were taken back home. Munira, whose ears were attacked, remembered opening her eyes to see her mother standing over her with a knife. “If my father hadn’t come running when I screamed I would have been dead as well,” she said. Dr Ambareen said that Noor could have been suffering from a psychotic episode but there was definitely something seriously psychiatrically wrong with her. Psychotic behaviour means a person has a markedly distorted connection to reality and may have paranoia. She could have been hearing voices and have strange delusional beliefs. Sometimes patients hear commands interpreted as divine voices ordering them to sacrifice their children, she said. It is also possible that Noor had a breakdown that no one noticed earlier on. In any case, she should be put on anti-psychotic medication and may even need ECT. Psychiatrist Dr Wasif added that as Noor had just had a baby, she could have been suffering from post-partum depression. He pointed out that inner aggression when divert inwards can lead to suicide but homicide when diverted outwards. The funerals took place at Ayub Goth near their house and the children were buried in the Lassi Goth graveyard in the presence of hundreds of neighbours. The Sohrab Goth police have lodged an FIR No. 685/07 (Under Sections 302, 324) on behalf of Rehman against his wife. Investigations Officer Manzoor Abbasi said that they were taking Noor as a “psychopath” and was in police custody. (By Faraz Khan and Razzak Abro, DailyTimes-B1, 14/11/2007) 94 (If you feel someone you know needs help you can contact the Pakistan Association for Mental Health (founded by Prof. S. Haroon Ahmed) at 90-A, Depot Lines, Behind Prince Cinema. Ph: 2257245, 2232423. They provide free mental health consultation and evaluation for all ages, psychiatric medication management, psychological assessment, counseling and psychotherapy for individuals and families and free psychiatric medications to needy patients) Aids awareness in schools IN what can only be described as a welcome initiative, the ministry of education, in collaboration with the National Aids Control Programme, will begin teaching students about HIV/Aids in public schools from January. This was a long overdue step as we all know too well that awareness about any ailment is crucial to its prevention and that can only come through education. That education will be imparted from a young age means that the message has finally sunk in with the authorities: they can no longer afford to sidestep an issue for fear that many may be uncomfortable with it. By the same token, it will be foolish not to include sex education in this initiative for that is essential in spreading awareness of HIV/Aids and other sexually transmitted diseases. One cannot ignore the subject of sex when discussing Aids and to couch it in other terms or be vague about it as one has seen in advertisements on the issue will be a great disservice. People need to be told the truth in an upfront and mature manner so that they can be better informed about their choices. By teaching youngsters that Aids can be contracted by also engaging in unsafe sex, we prepare them to make better decisions. Denying them this — and other information about reproductive health — spreads misinformation and, worse, puts them at risk of contracting diseases. Although observers believe that Aids does not pose as big a health risk as it does in say India or South Africa, it does not mean the issue should be taken lightly. There are 100,000 reported cases of Aids in Pakistan but that number could spiral out of control if awareness campaigns with direct messages aren’t launched. The government must partner itself with NGOs working in this field and ensure that the message is spread to every village in the country and all aspects of stigma associated with it are removed. (Dawn-7, 17/11/2007) Red tape binds govt effort on med supplies KARACHI: A monitoring committee in the provincial health department to check the quality and quantity of medicines received by medical institutions was formed about three weeks ago, wisely enough. However, Daily Times learnt Friday that it has not been functioning because someone has been sitting on the official notification. A committee was constituted by the provincial health department comprising four members: MPA Syed Talib Imam, health control board secretary Saleem Ishrat Hussain, Dr Khawar Mehdi and health control board deputy secretary Muhammed Saleh. The committee was endorsed by senior minister of health to monitor the purchase of medicines, X-ray films and other durables received by additional medical superintendent (AMS) or in-charge stores. The monitoring committee’s roles are to check the entries of new inventories, cross check those with entry gate passes and delivery bills, check payment schedules, make sure inventories are monitored, ensure supplier and manufacturer authenticity and more. “The medicines purchased are received by AMS or in-charge stores in accordance to the quality and quantity approved by the procurement committee after due process,” sources said. The medicines are delivered to the wards and units as soon as a requisition is received. Sources said that the senior minister of health sent a summary to the secretary of health about the monitoring committee on October 29. But a notification about the monitoring committee was never forwarded by the secretary, for unknown reasons, and it remains ineffective. One member of the monitoring committee, Syed Talib Imam, informed Daily Times that the notification for the monitoring committee will be issued in the next few days. He said, “How can we work unless it is officially gazetted ... I think it will take another two to three days for the notification to be issued,” he hoped. Daily Times contacted the secretary of health to ascertain why the notification was not issued and how the health budget is being monitored and the quality of medicine being controlled, but, he was not available. According to a source from Civil Hospital Karachi, the budget for medicines for year 2007/08 is Rs 298.1, Rs 8.2 million for X-ray and Rs 13.2 million for diet, amounting to Rs 319.5 million in total. The previous year’s budget was Rs 271 million for medicine, Rs 7.5 million for X-ray and Rs 12 million for diet, amounting to Rs 290.5 million for the year 2006/07. (By Shahzad Shah, DailyTimes-B1, 17/11/2007) No check on private healthcare providers Health dept fails to get draft ord approved KARACHI, Nov 18: Despite its enthusiasm for regulation of the business of private hospitals, clinics and diagnostic centres running across the province, the Sindh health department has not been able to get a set of relevant laws enacted by the outgoing public representatives. Sources in the health department attributed the failure to the bureaucracy, saying that a draft ordinance to ensure safe operation of private sector healthcare institutions, including teaching hospitals and charity healthcare providers, and to check unethical practices was forwarded to the Sindh Governor’s House about seven months back. At least two provincial ministers and some senior officials had stated on record that there was a dire need to have some legal provisions for regulation of private hospitals as a majority of them was a great source of concern for patients as well as their relatives, said a source. 95 Upon enquiries that continued till mid-October, Dawn was told by an official concerned that no draft had been received at the Governor’s House. “There does not arise a question of delay in promulgation of the ordinance, as it is a normal practice that the staffs concerned move promptly after receiving a duly-vetted document for an approval and promulgation by the governor,” the official said. Health minister When asked to comment on the subject, Health Minister Syed Sardar Ahmad confirmed that a revised draft ordinance pertaining to regulation and control of private hospitals, which was approved by Chief Minister Dr Arbab Ghulam Rahim in January this year, was very much with the Governor’s House. “Since I personally felt that grievances of people against private hospitals were on the rise, I had a track record of the draft,” he said, adding that the former principal secretary of the governor in some conversation had also acknowledged it some time back. Mr Ahmad said it was never too late and expressed hope that the governor would look into the matter and promulgate the much awaited ordinance at the earliest.It is pertinent to note here that the chief minister had asked the health department to prepare documents for enactment of appropriate laws for proper regulation and control of hospitals in June 2004. High-ups in the health department and the governor too gave favourable views about regulation and control of private hospitals on various occasions. Draft of health ord If the ordinance is promulgated, an accreditation and licensing authority will be established for regulating private hospitals, clinics, laboratories, physiotherapy centres, pathologist, nursing homes, maternity homes, diagnostic clinics and other health providers, including hakeem, operating in the province. According to the draft ordinance, the headquarters of the authority shall be located in Karachi and it will be headed by a chairman, nominated by the chief minister. It will pave the way for the aggrieved quarters to move against any private health centre involved in fleecing public. In addition to giving accreditation to health providers in the private sector, the authority can inspect in a checklist form by medical auditors, seek any medical information from a health provider and make regulations. Among other objectives, the legislation has also been sought after to eliminate quacks and so-called faith healers by making a prior permission from the authority mandatory to practise at any health centre in the province. The government through the ordinance will be able to set rules for classifications of health providers according to the services they have been providing to the patients or people coming for treatment or diagnostic purposes, and to define minimum safety standards for running a hospital. The ordinance has also been aimed at laying down standards/rules for ethical medical services, provision of medico-legal facilities in the private hospital, improving the handling of patients at such hospitals and clinics. Any immediate promulgation of the ordinance will also enable the provincial health department to determine a standard of fees/charges payable for services provided by the clinics and hospitals, said a source in the health department, adding that the department would also be in a position to get the details of communicable and contagious diseases from hospitals. (By Mukhtar Alam, Dawn-13, 19/11/2007) Tribute to organ donors DECEASED organ transplantation is a life-saving medical science which saved thousands of end-stage organ failure patients worldwide. This is practised in majority of countries, including in many Muslim countries like Saudi Arabia, Iran, Oman, Kuwait and Muscat. This is the need of the hour because people wish to live. Live and let live is a human norm of every society and every religion. When they were alive, Naveed and Shamim had dreamt of donating their organs which their parents fulfilled after their death. Naveed was the first deceased organ donor of Pakistan. He met with a road accident and was admitted to the Liaquat National Hospital, Karachi, where he was kept on ventilator (artificial respiratory machine). Doctors tried their best to save his life but did not succeed. He was diagnosed brain-dead by a neurophysician and an intensivist. The family took the decision to donate his organ because Naveed had wished it in his life. Naveed’s father contacted the Sindh Institute of Urology and Transplantation (SIUT), Karachi, which is a public-sector hospital providing health facilities free of cost to all patients and has been performing renal transplantation for the last 23 years.Both the kidneys were transplanted on two end-stage renal failure patients who had no donor in their families. His two corneas were transplanted on two blind persons. Four people are enjoying life with their children and families and back to society. One could imagine the joy and happiness of patients receiving the organs. Shamim was the second deceased organ donor of our country. A social worker belonging to the Hunza valley, she was ever keen to help others and wished for donating her organ after death. And it so happened that one day she met with an accident and died. Her family approached SIUT for organ donation. Her kidneys and cornea were transplanted on needy persons. After the promulgation of the Deceased Organ Donation Ordinance, many people from different walks of life have filled donor cards in a campaign organised by SIUT on Oct 25. Amongst them were Abdul Sattar Edhi, a well-known social worker, Justice Sabihuddin Ahmed and Justice Majida Rizvi, columnist Ardeshir Cowasjee, Vice-Chancellor of Karachi University S. Pirzada Qasim, educationist and former IBA director Dr Abdul Wahab, Prof. Haroon Ahmed, Dr Sethna and Dr Kaleem Butt, businessman Shaukat Tareen , lawyer Iqbal Haider, Zubeida Mustafa and Dr Jabbar Khattak from the print media, Anwar Maqsood and Sultana Siddiqui from the electronic media, sportsman Sikandar Bakht, engineers, doctors and paramedics from SIUT, social workers, students and people from Hindu, Christian and Parsi communities. 96 We should pay tribute to Naveed and Shamim who donated their organs and saved lives and set an example for others. We also praise those who wished to donate their organs after death. It shows that as a nation we are very humble, generous and helping. To help others in need is appreciable. DR MURLI LAL Sindh Institute of Urology and Transplantation, Karachi (Dawn-6, Letter to the Editor, 19/11/2007) Forty per cent blood transfusions not screened for HIV infection Forty per cent of the total annual blood transfusions in Pakistan are not screened for the Human Immunodeficiency Virus (HIV) infection, according to a study conducted by Dr Syed Abdul Mujeeb, an associate professor and in charge blood bank, Jinnah Postgraduate Medical Centre (JPMC) and Mark S. Pearce, a faculty member of the London School of Tropical Medicine and Hygiene. The study said that south-east Asia accounted for 25 per cent of the world’s population, but collected the equivalent of only nine per cent of the world’s blood supply. According to a national estimate, 1.5 million units of blood were transfused in Pakistan every year. However, as in other countries in the region, the demand far outstripped the supply. Pakistan has a high prevalence of thalassemia, communicable diseases, malnutrition, anemia, road traffic accidents, and surgical and obstetrical emergencies – all raising the demand for blood supplies. Anemia in pregnancies has a prevalence of 40 to 60 per cent. Maternal mortality is high with 20 per cent of the deaths occurring as a result of haemorrhage. Infectious diseases including tuberculosis, viral hepatitis, and malaria were the major causes of morbidity and mortality. The World Health Organisation (Who) and the joint United Nations programme on HIV/AIDS (UNAIDS) classified Pakistan as a “low prevalence, but high-risk” country for the spread of the HIV infection, the study said. According to UNAIDS estimates, some 70,000 to 80,000 persons were infected with HIV. By 2003, contaminated blood and blood products accounted for seven per cent of the total transmission of HIV/AIDS in Pakistan, the study said. Fifty per cent of the blood banks in Karachi employed regularly paid donors, with only 25 per cent of the facilities organised to recruit voluntary donors. Hepatitis B and Hepatitis C viral infections (HBV and HCV) were two major blood transmitted infections in the blood donor population of the country. A previous study of the first-time replacement donors in Karachi conducted in 2000 found that the HCV infection related to age, literacy, linguistic groups, and non-Karachi residences, while HBV infection was related to linguistic groups and non-Karachi residences. The prevalence of HCV infection was highest in the Sindhi, Punjabi and Pushto-speaking donors, while the prevalence of HBV was highest in the Saraiki, Sindhi and Balochi-speaking donors. The prevalence of both infections was higher in the donor’s residence outside Karachi than those that resided within. Considering the exclusion of all previously known high-risk blood donors from the study, a 6.5 per cent prevalence of the hepatitis infection in this population was alarming and reconfirmed that HCV and HBV infections were two major threats to blood transfusion safety in Pakistan. However, the magnitude of the risk of the hepatitis infection via donated blood appeared to vary with the demographic characteristics of the donor population. It was highest in the donors who were illiterate or had a mother tongue other than Urdu or Hindko, or were residing outside Karachi. The demographic characteristics of safe donors were voluntary donations and replacement donations; donors with intermediate or high level of literacy; donors who had provided three or more donations and donors aged younger than 30 years, the study confirmed. The study further said that Pakistan had the highest frequency of therapeutic injections in the world and the use of these injections in the country was generally not safe. The overall proportion of the population of Pakistan living in rural areas was 68 per cent, and except for the Urdu speaking population, all other linguistic groups had a tendency to live in rural areas. The high use of unsafe therapeutic injections by health care workers in the country may explain the particularly high prevalence of hepatitis infection in some subsets of the donor population, the study concluded. (By Shahid Husain, The News-19, 19/11/2007) Medical waste disposal MEDICAL waste in the twin cities poses a substantial hazard to human health and the environment because of mismanagement and the lack of an efficient disposal system. Many hospitals, public and private, and other healthcare concerns like clinics, medical laboratories and pharmacies usually dump their waste carelessly in piles in the open, bury them in the ground nearby or, worse still, throw them into streams and canals. Although an incinerator is a necessity for every hospital, most hospitals in Islamabad and Rawalpindi do not have incinerators, either because of the cost of procuring them or paying for the service of these machines. The few hospitals which have incinerators have found their operation and maintenance a daunting task as is the experience of a public hospital in Rawalpindi that has an incineration facility shared by two other major government hospitals in the city. Paradoxically the incineration of hospital waste is not free of hazards given the emission of potentially hazardous air pollutants, including toxic gases, particulates and ash, particularly when the conditions of combustion are not properly controlled. Thus many modern incinerators now include energy-recovering facilities that reduce emissions. But most of our hospitals already find getting and maintaining an ordinary incinerator beyond their reach what to speak of such modern mechanisms. What needs to be developed is a form of centralised healthcare waste disposal system, which is under consideration by the Capital Development Authority along with the Pakistan Environment Protection Agency. Under this system, healthcare waste will first need to be segregated at source to reduce the amount requiring special handling. A fifth 97 of hospital waste has been found to be hazardous, the rest being general waste which can be disposed of in the normal way or recycled, if it has not been contaminated. The hazardous waste will be collected from all hospitals to be transported to a billion-rupee scientific landfill on the outskirts of the capital. Here it will be treated and disinfected before being disposed of. But until such a system is put in place and the landfill site developed, our healthcare facilities will need to ensure that their hazardous waste is disposed of in a responsible manner that poses the least danger to human health and the environment. (Dawn-7, 20/11/2007) Keamari Town health infrastructure in shambles KARACHI, Nov 20: Keamari, the second largest town of the metropolis, is home to a huge labour force that comprised mostly factory workers, fishermen and vendors trading in different commodities. Notwithstanding their immense contribution to economy, successive governments have done a little towards provision of basic health and education facilities and an infrastructure for these vital sectors in the town. The majority population is, therefore, faced with abject poverty, that entails numerous serious social and health miseries. A survey of the coastal villages in the town shows that maternal mortality and morbidity rate is high and even deaths from preventable diseases are common. More painfully, most of the issues, including such deaths, go unnoticed and unreported, mainly due to the apathy of the successive governments towards the plight of the poor lot. The recent death of 14 people — two of them pregnant women — from a viral fever took place in a single locality, Deh Allah Bano which comprises 18 villages of UC Gabopat. Demise of such a big number of people over the past three months brought to light the serious inadequacies in the town’s health infrastructure. Residents of Deh Allah Bano fear that if the government continued to ignore the villagers’ health requirements, more people could fall victim to viral and other diseases. It is believed that deaths from such viruses often occur after heavy rainfall and this adds to the villagers’ concern as the metropolis has been registering a rising graph of rainfall for the past few years. Lack of transport facilities is seen linked with the mortality rate pertaining to health sector as most villagers cannot afford taking their ailing family members to some major hospital, located far away from the area. Having a population of over 0.7 million, the town has no government-run hospital. Still, what is worse is the absence of any maternity home. The only mother and childcare health care centre that exists in the town is located in Bhit Island, (UC-4) which serves only as a dispensary. Most deliveries in the town are performed at home while some at a rural health centre, known as the Shershah RHC. The other important health unit Keamari RHC provides only outpatient service for antenatal, eye and dental examination. The three-room centre has no diagnosis facility though it runs a TB unit. Most of about 20 dispensaries functioning in different union councils have been facing shortage of staff and medicines. Three dispensaries in Hussaini Goth, Mubarak Village and Deh Allah Bano have been lying closed for years. Another dispensary, in Mowachh Goth, has been taken over by Rangers for maintaining law and order and they have been staying in it for years. Town Health Officer Dr Nazeer Ahmed Kolachi acknowledged the lack of health infrastructure in the town and agreed that facilities needed to be upgraded. “There are about 22 health units, but the government has improved SNE of only seven units that includes five basic health units and two rural health centres. Therefore, we will have to distribute the staff and medicines meant for seven units among all units.” He also admitted that the units which were functional were also in a dilapidated state, adding that the Shershah and Keamari RHCs could be run round the clock since the units didn’t have accommodation for RMOs. Transport problem was another hitch, he added. About the recent deaths in Deh Allah Bano, he said these coastal areas didn’t have a proper road network which had made people’s access to health care units difficult. “We desperately need adequate funds for making all health units functional, especially those in the much neglected coastal villages,” he said. (By Faiza Ilyas, Dawn-18, 21/11/2007) Govt fails to reduce prices of medicines KARACHI, Nov 23: Sindh government efforts for a downward revision in the prices of medicines were unlikely to bear fruit any time soon due to the ‘apathy’ of federal health authorities, said a source in the health department. A health official disclosed that after receiving a well-documented report on soaring prices of drugs from the Sindh health department in the last week of September, President General Pervez Musharraf had desired that authorities concerned the ensure a downward revision in the prices at the earliest. The report, which was prepared under the supervision of former provincial health minister Syed Sardar Ahmad and sent to the president, prime minister and national forums, stated that the lower and middle income groups were not in a position to afford life-saving drugs in the because of their arbitrarily fixed high prices. The report, supported with some facts and figures, further stated that a number of medicines were even beyond the reach of patients from the higher income groups. In view of growing concerns among a large section of society, it had become all the more necessary to ensure a downward revision in the prices of medicines. Unfolding the details of the report on the soaring prices of imported and locally-manufactured medicines, the former health minister had blamed a faulty system of drug pricing, unethical practices by doctors who prescribe the medicines of expensive brands, and the greed of pharmaceutical firms. 98 The fact that remarkable difference in the prices of the products of same generic persisted not only between the multinational manufacturers but also between the local pharmaceutical companies called for a change in the approach of manufacturers and the price fixation team of the government, health officials said, underlining the need for provision of urgent relief to the common man. It was learnt that President Musharraf had asked the federal health ministry to arrange a meeting of stakeholders, including those from the private sector, to revise the prices of medicines. The prime minister secretariat too, asked the ministry to implement the earlier directives issued by the president and sought a complete report of steps taken in this regard by Oct 15. However, sources said, no meeting of stakeholders or provincial health authorities had been held in Sindh so far. About seven weeks back, the health ministry had told the Supreme Court that a drug price survey had already been conducted enabling the ministry to work out a policy for rationalisation of drug prices.The survey covered 42,000 brands of some 120 molecules being used in over 80 districts. Prices of the commonly used molecules being sold under different brands varied from 20 per cent to 400 per cent whereas the difference for the drugs in less demand was huge i.e. ranging from cent per cent to 1,100 per cent, it observed. When asked about the factors involved in price variations, a medicine dealer in the city said the prices of the same raw material imported from various countries differed which cast its effects on the retail price. He was of the view that the government could check the variation in prices of imported raw material to regulate the prices of drugs being sold in the local market. However, he said when the high-priced raw materials were preferred over the inexpensive raw materials of the same quality available in the international market and adopted as the basis for the determination of price, it was unfortunate that the prices of medicines, particularly the life-saving drugs, could not be regulated. (By Mukhtar Alam, Dawn-18, 24/11/2007) Around 27,000 people suffering from malaria Around 26,000 to 27,000 people suffer from malaria every year in Sindh, said the Director Malaria Control Programme (MCP), Sindh, Dr Nawaz Ali Kallar. Talking to The News, he said that around 17,000 cases of malaria have been reported till October 2007. Tracing the history of the MCP in the country, Kallar said the first serious efforts to control this disease started in 1961 with foreign assistance. However, a Malaria Eradication Programme (MEP) in Sindh was launched in 1963, mainly based on conducting sprays each year. However, the donor agencies did not provide financial assistance and the salary of the malaria staff became a problem. The MEP was abolished in 1976 and the government adopted new strategy based on carrying out fumigation where cases of malaria were found. “Apart from selective sprays, another feature of the Malaria Control Programme is provision of free treatment of the disease,” elaborated Kallar. Till 1978, the MCP was a separate entity but later it was merged with general health and is now a part of the health department. However, with the renewed interest of donor agencies, Roll Back Malaria (RBM) was launched in 2000-01 with the assistance of the World Health Organisation (Who), which is “multi-dimensional,” the director MCP believed. This new strategy to control malaria stressed on “early case detection and prompt treatment,” he said. The importance of early malaria case detection can be gauged from the fact that malaria is caused by particular female mosquito (anopheles), which need human blood for its nutrition (eggs). Hence, it takes parasites from the affected person, which is why early detection is imperative to prevent spread of malaria, Kallar explained. Another aspect of RBM is multiple prevention, as destroying mosquitoes is not a solution of the problem, he said. “Unless the root cause of malaria is not addressed, it is not easy to tackle this problem,” Kallar added. Then there is clean and stagnant water, which provides a breeding ground for mosquitoes. Besides this, the strategy also emphasises on the importance of taking measures for self-protection on part of the people. The public-private partnership is the third aspect of the RBM in order to take coordinated and integrated efforts for preventing the disease. The preventive measures required to make sure that malaria does not turn into an epidemic is another aspect of the RBM, Kallar said. As part of this strategy, the government is providing bed nets, which are known as insecticide treated nets (ITN). Kallar said that the federal government has recently provided 10,000 ITNs to Sindh: 5,000 for Karachi and rest for interior Sindh. Moreover, the MCP has also purchased 1,400 more ITNs to be distributed in the most affected areas of the province. He said that ‘selective indoor residual spray”’ is also a part of the RBM, which is conducted where falciparum (lethal kind of malaria) is found. To a question, Kallar admitted that no significant achievement has been made to overcome this disease as since 2002 “we have been receiving the same figure of malaria cases (26,000-27,000).” Talking about the problems being faced by the MCP, Sindh, he said the budget is “insufficient”, which till now was Rs10 million per year but has been increased to Rs35 million. Another problem is lack of staff as there were initially 16 districts in the province which have now increased to 23. Sadly, the seven new districts have no staff, he added. He said that there are a total 104 microscopists to take slides (blood samples) while 26 posts are vacant. The government plans to control malaria cases by half by 2010 but doctors believe that it did not appear to be achievable because of the lack of preventive steps. “When hundreds of basic and rural health centres are not functional, how can you achieve this target especially when only two years are remaining?” asked Dr Habib Rehman Soomro, secretary general, Pakistan Medical Association (PMA). The problem is stagnant water, which is found everywhere, even in the posh locales of the city. Earlier, it was assumed that malaria cases mostly occur in the far-flung and arid areas of the province and the numbers of deaths go unreported. But this time, malaria has hit the outskirts of Karachi, where around 14 deaths have been reported so far, mostly caused by malaria, he added. “We took slides of 25 patients out of which 18 are confirmed dangerous malaria cases in Deh Allahbano,” said Dr Samrina Hashmi. Most patients are suffering from a shortage of blood. Besides, their spleen has enlarged. (By Imtiaz Ali, The News-19, 25/11/2007) 99 Excesses of private health sector ONE fails to understand why, despite deploring for years the irregularities witnessed in private healthcare institutions, and subsequently readying an ordinance to curb these, the Sindh government chose not to promulgate the much-needed law. The draft was sent to the Governor House seven months ago but has been shelved ever since. Although there have been complaints that the draft was prepared without consultation with the major stakeholders, there was much in it that could have led to reforms in the private health sector, had the ordinance been promulgated. The draft sought to establish a provincial authority that would have maintained strict checks on private hospitals, clinics, diagnostic centres, etc, essentially to stop them from fleecing patients and to ensure that punitive measures were taken against medical malpractice or negligence. The government’s inaction on this front — and one might add the health department’s failure to press for the ordinance’s promulgation — speaks volumes for a serious lack of political will. Or are there other considerations at work — primarily the reluctance of private health facilities, some major hospitals among them, to be brought under the ambit of a law that limits their independence? Whatever the case, it is essential that there is legislation that holds private medical outlets accountable for their actions. It is the absence of such a law that has made medical malpractice so common. There is little compensation for the patient and no penalty for the erring doctor or hospital. The high fee structure at many private hospitals and clinics is also a worrisome aspect. With government hospitals in a shambles and unable to cater to the needs of patients, the poor have no option but to turn to quacks whose flawed prescriptions complicate matters even more. One can only hope that more resolve is shown by the authorities and that eventually a comprehensive law is enacted to check this wholesale commercialisation of the medical profession, while taking everybody on board and refraining from issuing arbitrary rules. It is equally important to work towards introducing positive changes in government hospitals and clinics so that private institutions are forced to review and improve their own performance. (Dawn-7, 26/11/2007) Cerebral malaria behind recent Keamari deaths: PMA KARACHI, Nov 26: Recent laboratory tests conducted by the Pakistan Medical Association (PMA) made it evident on Monday that a mosquito infestation in Deh Allah Bano in the Gabopat union council of Keamari has led to a wave of cerebral malaria cases. Dr Qaiser Sajjad, the secretary-general of the PMA Karachi, said that mosquitoes plagued the area’s residents even during the day, despite a reported fumigation some time ago. “The area needs regular medical services, hygiene facilities and a supply of fresh water for drinking and washing purposes,” he said. Following news reports concerning an unidentified viral fever that killed a number of people, including two pregnant women, in the 18-village Deh, the PMA recently organised a medical camp there. Free medical assistance and medicines were provided to the people and the PMA set up a laboratory facility to inquire into the cause of the recent deaths. Blood samples were taken from 75 patients and malaria tests were conducted. A PMA report issued on Monday said that the people of Deh Allah Bano, which is located about 15 kilometres from Hawkesbay, were traumatised by the deaths of 16 people due to an unknown fever in the past two months. The blood tests showed that Falciparum Malaria parasites, which cause severe brain complications known as cerebral malaria, were present in about 85 per cent of the samples. The samples were also tested for CBC, typhoid and LFT but no significant change was found in this regard, said the report, concluding that the Deh Allah Bano deaths were caused by cerebral malaria. No health facilities Referring to the non-availability of drinking water, the PMA report said that the area’s residents collected rainwater for drinking and washing, and there was an urgent need of a supply of fresh water. In terms of a general review of women’s and children’s health, it said that 60 per cent of the women were found to be anaemic and emaciated, while most of the children were suffering from abdominal, throat and eye-related problems. A number of patients were also found to be suffering skin diseases. The PMA said that it was the government’s responsibility to provide basic health facilities to all the citizens of Pakistan. All the dispensaries and clinics in Karachi, particularly those in Keamari town, should be made functional and fumigation drives should be regularly carried out twice a week. Expressing concern about the unavailability of a basic health facility of Deh Allah Bano, the PMA pointed out that there were 20 government dispensaries in Keamari town but only seven were in working order. The remaining 13 dispensaries had no basic medical facilities at all. There is currently no health facility in Deh Allah Bano. The only small, three-room dispensary wears a deserted look since it was not made functional after its inauguration in February 1995, claimed the PMA, adding that the people of the area do not even have access to public transport to take patients to a suitable hospital. (Dawn-17, 27/11/2007) Is that little bundle of joy making you throw up? Two weeks into her second pregnancy, Sajda began to experience nausea and vomiting. At first, she would only feel sick in the morning. Then, she began to feel nauseous all day long, often vomiting after every meal. In her tenth week, she vomited out so much food that she became dehydrated and was admitted into the hospital. She remained hospitalized for two days and was administered a rehydrating drip and intravenous medicines that stopped nausea. “I just couldn’t eat anything without throwing it up,” recalls Sajda. “If I remained anti-stomached, I would feel nauseous and light-headed. The minute I ate, I would begin to vomit. I couldn’t even drink water. Anti-vomiting medicines didn’t help at all. 100 My condition didn’t improve even after being released from the hospital. For nearly two more months I was so nauseous that my diet would often only contain soup and dry crackers.” Fortunately for Sajda, her nausea subsided around the end of her fourth month of pregnancy. “Nausea and vomiting slowly begin to decrease around the 16th week of pregnancy,” informs Dr Sadia Rizvi, consultant obstetrician and gynecologist at a private hospital. “It is a natural sign of pregnancy and often, there is not much that the mother can do. Taking dietary precautions may help. The expecting mother could avoid greasy food and restrict herself to dry food such as toast, crackers and bananas. Lemonade may also help. Efforts should be made to avoid medication but if absolutely necessary, antiemetic (anti-vomiting) medicines that contain vitamin B6 are usually prescribed by gynecologists. Normally, patients are advised to take these tablets early in the morning, usually around 45 minutes before they brush their teeth and begin their daily routine. If taken at night, these medicines can be helpful in dealing with morning sickness. However, in cases of severe nausea, these medicines may not work.” According to Dr Rizvi, nausea is caused by increased hormone production in the body. These hormones support the pregnancy up to the fourth month and their production is at its optimum around the ninth week. Nausea and vomiting is also usually at its peak at this time. Not everybody experiences nausea for just the initial four months of pregnancy. In some rare cases, expecting mothers continue to throw up food for the entire duration on nine months. “I vomited throughout my first pregnancy,” remembers Nargis. “Even when I was in the hospital with labor pains, I was throwing up. I felt weak and listless and even the sight of food disgusted me. Nine months is a very long time to suffer through nausea and it made me depressed and tearful. Thankfully, my nausea and vomiting subsided within days of giving birth.” Dr Razia Korejo, associate professor and gynecologist, says that although nausea may be disturbing for the mother, it isn’t really harmful for her. “The only time nausea and vomiting can be dangerous is when it causes dehydration,” she explains. “Naturally, in this case, the baby also does not receive sufficient nutrition. Otherwise, normally, the baby maintains a healthy growth even if the mother is unable to eat properly during the first few months. Whatever nutrients the baby needs, it takes from the mother’s body. This is why expecting mothers often lose weight during the first few months.” (By Maliha Rehman, DailyTimes-B1, 27/11/2007) Five more die of ‘high fever’ in Keamari Town Five more persons, including two pregnant women, died of ‘high fever’ in Deh Allahbano, Keamari Town as the authorities concerned have allegedly failed to take preventive steps despite confirmation of dangerous kind of malaria in the area by visiting the doctors team of Pakistan Medical Association (PMA) recently. Zubaida Bhand died of high fever in Goth Haji Ibrahim Bhand recently. Her sister-in-law, Rashida, who had come to offer condolence was also suddenly affected by high fever three days ago and died on Tuesday morning, her brother Sattar Bhand told The News. She was seven months pregnant and mother of three children. Mrs Zubaida was also mother of three children. Sattar said a doctor in Mauripur had administered drip to his sister, which had helped a lot. However, her health deteriorated on Monday night. He said they approached taxi drivers but they did not volunteer to take them as their village was located at a considerable distance from the main road. He complained that Keamari Town’s spray team had also refused to conduct fumigation in their village around 15-20 days ago, citing remoteness of the village. He claimed that the town’s medical team had once visited it several days ago and returned back ‘hurriedly.’ The residents said four other persons Ms Sat Bai, 50, Haji Siddiq, 50, 10-days old baby and Sonia, 12, also died of same symptoms in the last week, bringing the total number of deaths to 19 in the last three months in around 18 villages of UC Gabo Patt of Keamari Town. Town Health Officer, Keamari, Dr Nazeer Kolachi, expressed ignorance about the deaths. However, he admitted that they have taken blood samples of several persons and seven were confirmed cases of malaria. He later said that they also took slides of eight persons, one of them was malaria. He claimed that they have set up several camps there and treated around 5,000 patients. Pakistan Fisherfolk Forum (PFF) alleged that the officials concerned were not taking preventive steps to control malaria there. It urged for setting up a hospital there as the dispensary established in 1970s stood closed and to continue emergency medical camps so that the lives of poor fishermen could be saved from preventable diseases. Meanwhile, the Pakistan Medical Association (PMA) which organised a medical camp last week there in its report said they examined around 450 patients and collected blood samples of 75 patients and 85 per cent of the samples had the parasite Falciparum Malaria — a dangerous parasite for humans causing severe complications to the brain resulting in what is known as cerebral malaria. It held the government responsible for lack of health facilities in Deh Allahbano. (The News-13, 28/11/2007) Aids prevalence among women in Sindh rises KARACHI, Nov 28: The Sindh Aids Control Programme (SACP) has registered 45 women province-wide living with the human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (Aids) over the past one and a half years, till the end of Sept 2007. Sources in the SACP said that reports about the prevalence of HIV/Aids in women in Sindh had increased considerably during the last four to six years and if the trend continued, the proportion of women among Aids patients would increase further. At present, the ratio of men to women patients is 4:1, sources added. In developing countries, the women to men ratio of Aids patients is 3:2, while in India 39 per cent of such patients are women. Till March 2007 as many as 325 male and 44 female Aids patients were registered with Aids control agencies in Pakistan. 101 An Aids control official said that almost all the women victims of the deadly disease, who had been registered with the SACP, maintained families and reportedly got the disease from their infected spouses. The vast majority of male expatriates returning to the country are feared to have contracted HIV/Aids through the exchange of bodily fluids during their prolonged stay abroad. The official, however, said that one’s risk of contracting HIV also increased if one had a previous or current diagnosis of hepatitis, tuberculosis (TB) or sexually transmitted diseases (STDs) or if one had received a blood transfusion or clotting factor when blood is not screened for HIV antibodies. Among the reported cases, it was learnt, there were two such pregnant women, married to the same man, who got infected due to the unprotected practices of their husband. They found out that they were HIV-positive only when they got pregnant, a source said. According to a UNAIDS report, since 1985 the percentage of women among adults living with HIV/Aids has risen from 35 per cent to 48 per cent worldwide. Young women currently make up over 60 per cent of all the 15 to 24-year-olds living with HIV/Aids. A surveillance report on Pakistan said that there were 3,866 people living in the country with HIV/Aids till the end of March, 2007. The man to woman ratio remained 6:1. Dr Azra Ghayas, the Director of the SACP’s Centre of Excellence at Karachi, said that when she had started the counselling, testing and treatment centre in May 2006, about 10 women were registered as HIV/Aids patients at that time. Now, in November 2007, the number of women patients had increased to 41, which is the result of extensive counselling and increased awareness about the disease as infected male patients registered with the SACP agreed to bring their wives as well for examination, she added. The number of women patients is likely to swell further as the persons suffering from the disease, in a state of ignorance and shyness or due to social stigma in the initial years, are sure to show signs of infection now. Warning signals ignored Dr Azra said that the symptoms that could serve as warning signals of HIV infection went ignored also because women in this part of the world did not perceive themselves to be at risk. “It is unjust that infected men do not ensure proper use of barrier methods,” she remarked. A simple blood test that checks for the HIV-antibody is all that is required to determine whether a woman or man is infected or not. But, in a situation where the impact of gender autonomy is yet to be felt adequately, women in our society are largely not able to insist on their husbands taking precautions or are unable to take measures to protect themselves from HIV, said a health worker at a government hospital in the city. Discussing the crisis of HIV/Aids that women are confronting, the Deputy Programme Manager of the SACP, Dr Syed Qamar Abbas, said greater efforts were required to address the concrete needs of women and girls. “While there still exist major inequalities between women and men in all aspects of life, including education and awareness, employment, social and economic empowerment and choices in relationships, how can one expect that just remaining faithful to her husband would help a woman stay safe from HIV,” he observed. According to Dr Abbas, HIV prevention among women is the responsibility of both partners and men must play an equal role in this. Women are biologically more vulnerable to HIV so there is room for educating women on STDs, the use of condoms and violence against women, he emphasised. Record of HIV patients registered till Sept 2007 HIV Total HIV patients 1,838 Aids Male 120 Female 24 Total 144 Deaths Male 33 Female 3 Total 36 Source: Sindh Aids Control Programme (By Mukhtar Alam, Dawn-17, 29/11/2007) Putting an end to misery Shazia Kausar (not her real name) has been visiting a psychologist for a year now. In June 2005, she got married to the man of her choice. Little did she know that things at her new house would not be what she had expected them to be. The age-old issues concerning in-laws made her life miserable almost immediately and this finally led to her divorce in January 2006. During the time of her iddaat (three-month waiting period after being divorced before one can socialise again), she attempted suicide for the first time in her life. “I had been observing the change in her attitude by the way she had started talking and sitting with the family. One day she just locked herself in the room and took half a bottle of sleeping pills. When she didn’t open the door on our repeated requests, her elder brother broke in to find her lying unconscious with her lips turning blue,” recalls her mother, Naushaba. After the incident, the family consulted an expert to make sure that this never happened again. 102 Psychologist Samina Khan explains that such cases are fast becoming a norm in our society, especially in the middle and lower classes. “Abusing one’s wife is quite common in these classes, and this ultimately leads to suicide. Ironically, most of these cases go unreported,” says Khan. This is just one example of a woman who suffered a broken relationship and eventually attempted suicide. Shazia, however, was lucky as her family consulted a psychologist. However, this does not happen to everyone Ghazala Sohail was a teacher by profession. In June 2006, Ghazala’s husband lost his job and, as a result, she had to bear the responsibility of making ends meet. During such trying circumstances, even her husband was not very supportive and often demanded money from her to fulfil his needs. This led to constant conflicts and one day, she tried hanging herself from the fan. Her brother Zahid, while talking to The News, said, “The attempt was unsuccessful when her elder daughter cried for help and as a result some neighbours came and intervened.” However, this did not deter her and she used different means to commit suicide the next time: she slit her wrists when no one was home. When asked why she wasn’t taken to a psychologist or therapist after her first attempt, Zahid instantly replied, “My sister was not crazy.” According to studies, every normal being tries to commit suicide once in their lifetime. If unsuccessful, they then try it again and again in the false hope of failing every time, but that is not always the case. Samina Khan says that people who frequently attempt suicide get a perverse pleasure out of it because they can get sympathy from people around them. According to another study, suicidal tendencies are higher in men. In our part of the world, on the other hand, women are more likely to suffer at the hands of their husbands and families. “Cases of wife beating over different issues and other domestic problems often lead to suicides in females. Another reason is that such females are unable to share their grievances with anybody, often not even with their own parents,” explains Khan. Suicidal tendencies often include hysteria, with the result that most people confuse that with depression. However, psychologist Haider Rizvi says that this often a result of hopelessness. All over the world, there are different rehabilitation centres for people with suicidal tendencies. These centres help such people go back to their lives and change the way they think. These rehabilitation centres make the patient sign a contract with their psychotherapist according to which, the therapist has the right to call a regulatory helpline if the patient tries to commit any violent act, hurting himself or any member of the family. “On the contrary, no such laws or centres are present here,” says Rizvi. People who want to kill themselves often start giving cues of their suicidal intentions even before they are aware of them. The most common symptom in this regard is that such people start isolating themselves from others. “Their behaviour becomes inconsistent and the change is noticeable. Whenever any question is asked, their way of answering is also different and strange. They stop socialising and start giving away their precious belongings. The family should monitor the trends of any person who happens to have suffered any major or minor setback or trauma in their life. Otherwise, it can result in a suicide attempt,” explains Rizvi. Most importantly, families need to be educated about suicide and also need to be told that there is no harm in consulting a psychotherapist or a psychologist. For example, people like Ghazala’s brother still think that only the mentally ill are taken to psychologists. “Professional help always works for such patients. The hopelessness and tendencies of suicide can always be avoided,” says Rizvi. Some of the most common reasons for suicide attempts are failure of a relationship, unemployment, and poverty and social injustices, all of which seems to take its toll on women more than men in Pakistan. (By Sidra Rafique, The News-20, 29/11/2007) Women’s health a burning issue Ami was 15 years old when she got married in little village in Thar. A year later, she became pregnant but it was not easy for her to deliver the child because of her early marriage as well as her frail health. She was in constant pain while at home and eventually delivered a still-born baby. Due to the difficulties that she faced while giving birth, the complications increased and she developed fistula. The family took her to the nearest hospital in the city, a journey which took a whole day since the only means of transportation was a camel. Upon getting there, they found out to their utter disappointment, that there was no facility available for the treatment of fistula over there. When told that this facility was available only in Karachi or Hyderabad, the family, as a result, decided nothing to do about it since the travel expenses along with medical treatment was turning out to be quite expensive. As a result, Ami suffered fistula for almost 14 years before being treated by the doctors of the Pakistan National Forum on Women’s Health (PNFWH) with the assistance of United Nations Population Fund (UNFPA), which had launched the fistula project recently in the country. This incident was revealed in a documentary film by Dr Shershah Syed at a seminar at the Pakistan Medical Association (PMA) house recently. During the discussion, Dr Syed also disclosed the launch of a newly set-up Society of Obstetricians and Gynaecologists of Pakistan (SOGP) which published an annual report on the state of women’s health in the country. He recalled another such incident of a woman in Swat who suffered from fistula for the past 41 years. He said the problems for such women are often compounded when they are abandoned by in-laws and are not treated well by friends and family. Of course, those who don’t know any better think that this is the result of a sin committed on the part of the women. Dr Syed, however, dispelled this myth saying that “this punishment is the result of the lack of health facilities and illiteracy” and nothing more. Fistula’s treatment isn’t necessarily expensive or complex. “The surgery hardly takes 20 minutes and costs Rs350,” he said, adding that the main thing is that health has never been a priority of the successive regimes in the country. There is no accurate figure for the number of mothers suffering from this disease. But it is estimated that around 20,00030,000 women are suffering from fistula in the country. Around 15,000 women develop fistula every year due to a variety of reasons. “The main reason is poverty, which leads to insufficient nutrition and stunted growth,” he opined. He also criticised the untrained surgeons and the less-than-satisfactory training in the teaching hospitals. 103 The UN’s fistula project started in 2003 and is supposed to end in 2008, under which seven regional centres have been set up across the country where so far 548 women been operated upon. Another speaker, Anis Haroon, talked about the rehabilitation of such women as they often live in separate rooms due to the loss of bladder control. She recalled that one 20-year-old woman gave birth to five children in a village in Khairpur and developed fistula. She wondered who would take her for treatment. The “resource constraints prevented us from bringing her to Karachi while her in-laws were also reluctant to allow her,” she said. Anis was of the view that women’s health is not a medical issue. “Poverty, forced marriages, the status of women, health and education are basically political issues,” she said. The theme of the seminar that health should not been seen in isolation was also echoed at another seminar on mental health organised by the Pakistan Association for Mental Health (PAMH) where psychologists, intellectuals and city planners were of the opinion that health issue is closely linked to the social, economic and political structure of the country. They came to the consensus that the critical mass of intellect and political parties —favouring institution-building and rule of law and education based on charity not commercialism — is needed to address the problems, which are causing increasing stress and despair among the people. (By Imtiaz Ali, The News-19, 29/11/2007) DECEMBER 1982 AIDS patients in Sindh Enhanced HIV/AIDS Control Programme Sindh (ACPS), NGOs, UNAIDS, Unicef and Pakistan Medical Association (PMA) on Friday took part in ‘candle lighting’ at PMA House to raise awareness of HIV/AIDS. The caretaker minister for health, Ms Fauzia Lari lit the candles. Speaking on this occasion, Dr Arshad Mahmood Khan, head of ACPS said there were 1982 reported cases of HIV/AIDS in Sindh. Among them a total 144 were registered AIDS patients. He admitted that only 77 were getting anti-retro-viral (ARVs) medicines. He said around 30pc injection drug users (IDUs) in Karachi and 28pc IDUs in Hyderabad were involved in spreading HIV/AIDS. Ms Dierdre Kiernan, chief field officer, Unicef, Sindh, said that Pakistan was in a “concentrated epidemic” driven by injecting drug users (IDUs) and male and eunuch sex workers. She said as the concentrated epidemic in Pakistan matures amongst high-risk populations and migrant workers, and more data becomes available, the effect of HIV/AIDS on children and adolescents could be better understood. She said the country had one of the largest cohorts of young people in the world-60pc of the nearly 160 million were under the age of 24. These young people needed correct information on AIDS in order to protect themselves and their peers. Special secretary for health Capt (retd) Dr Abdul Majid said as misuse of syringes was one of the reasons behind the spread of AIDS, the government is providing syringes free of cost through NGOs. He said the provincial government had also suggested to the federal government to clamp a ban on disposal syringes. He said all hospitals have also been instructed to use needle cutters. He said behavioural change was vital for prevention of this disease. The provincial minister, in her brief speech, underlined the importance of creating awareness against this disease in the most affected areas and interior of Sindh like Larkana. Dr Maha, Shaukat Ali, Dr Khalid Sheikh, and others also spoke. They pointed out that there were around 90,000 HIV/AIDS patients in the country. (The News-13, 01/12/2007) Water-borne diseases heavy burden on healthcare Lack of resources, increasing population pressures and weak legislations are causing the deterioration of the environment, which is adversely affecting the health of the people in terms of the shortage of clean drinking water and efficient sanitation systems, according to the State Bank of Pakistan’s (SBP) annual report of 2006 to 2007. This is also corroborated by the Sindh government’s report on health, which is part of the Sindh Vision 2030. “Water-related environmental health risks impose the most significant health burden,” the report revealed. It added that the high pollution levels of rivers and groundwater had led to different environmental consequences such as a reduction in biodiversity, increase in water-related diseases and the decrease in agricultural productivity. Apart from that, the mismanagement of water resources has strong socio-economic repercussions, especially on food security and health, the report said. Although groundwater is still the primary source of drinking water supplies, it is estimated that 40 million residents depend on irrigation water for domestic use, especially in areas where the groundwater is brackish. “The associated health risks are grave as the bacteriological contamination of irrigation water often exceed the World Health Organisation’s (Who) limits for irrigation,” the report said, adding that the poor quality of drinking water had major socio-economic consequences. Diarrhoea, dysentery, cholera, helminthiasis and enteric fever are widely believed to be the result of contaminated water. “Exposure to water-borne diseases is an important contributing factor to infant mortality, which remains high despite improvements in demographic indicators,” the report said. 104 Who’s report of 2007 said that six out of a total 25 serious water related diseases are found in Sindh. These are arsenicosis, diarrhoea, Hepatitis A, lead poisoning, malaria and typhoid, which are taking a heavy toll on human lives. The National Conservation Strategy said that about 40 per cent of the deaths resulted from water-borne diseases. Lack of sanitation is also considered to be a major public health problem that causes disease, sickness and death. Poor farmers and wage earners are less productive because of these illnesses. “Without safe water and sanitation, sustainable development is impossible,” the report said, adding that improvements in the safe water supply and in particular hygiene and sanitation should be ensured. The report regretted that there was a general lack of awareness about water-related diseases and sanitation issues especially in rural Sindh. “The prevention of water related diseases would require alternate and cost-effective sanitation solutions as well as an overall awareness hygiene in rural as well as urban Sindh,” the Sindh Vision 2030 suggested, adding that widespread ‘existing initiatives’ awareness campaigns were required to mitigate losses and to arrest the further decline in the health of all Sindhis. “Most of the water-related diseases are curable and can be prevented from occurring,” the report said, adding that initiatives should be taken to create awareness of such diseases and their remedies. Awareness should also be created among the masses to avoid the occurrence of water-borne diseases. Meanwhile, the SBP’s report pointed out that Pakistan being an agrarian economy relies a lot on groundwater as a key resource. However, an over-reliance on this resource has now caused 70 per cent of the tube wells to provide “hazardous sodic water.” “The government needs to plan alternative sources to avoid further deterioration of the current situation,” the report suggested. The government of Pakistan has promised to provide clean water supply of up to 93 per cent under the Millennium Development Goal (MDG) by 2015 but the SBP’s report opines that this doesn’t appear to be achievable. It appreciated the government’s multi-billion projects like Clean Drinking Water Initiative and Clean Drinking Water for all by 2008 as a “step in the right direction” but questioned its realisation. “All these projects seem to have ambitious targets in view of the existing current status,” the report said. It may be mentioned here that the water-borne epidemic hit Karachi in 2005, taking several lives and adversely affecting the health of more than 1,000 people in Landhi. (By Imtiaz Ali, The News-19, 02/12/2007) Only 6% of med students knew of HIV/AIDS: study KARACHI: Only six percent of 357 medical students were discovered to have complete knowledge of the symptoms of HIV/AIDS, in a study ‘Knowledge and attitudes of Pakistani medical students towards HIV-positive and/or AIDS patients’ that appeared in Psychology, Health & Medicine (Vol 12, Issue 1 Jan 2007). Analysis showed that older and clinical students were more knowledgeable. Although the prevalence of HIV is only 0.1%, Pakistan is thought to be at high risk. It has been suggested that physicians in Karachi are deficient in appropriately managing and counseling HIV patients, that they lack sufficient knowledge of symptoms as well as therapy of sexually transmissible infections and, thus, do not know how to diagnose and treat these patients suitably. The average age of the students in the study was 22.5 years with 66% women. Ninety-one percent of the students were Muslims. The majority of the students who participated in the survey were clinical students as compared to 35% of preclinical students. Over 90% of the respondents though that there is a risk of contracting HIV through a blood transfusion. Nineteen percent of the students agreed or strongly agreed that they would refuse to have surgery that required a blood transfusion. Nearly 80% of the students agreed or strongly agreed that all patients should be HIV tested on admission to hospital. Seventy-six percent of them said that they would break confidentiality and inform an infected patient’s sexual partner. Over half of the students thought that HIV-infected children should be excluded from government schools. Over 30% of them would avoid someone with AIDS. Eighteen percent would not want a person with AIDS to touch them. Twenty-nine percent said that they would refuse them mouth-to-mouth resuscitation. Nearly one-third of the students agreed or strongly agreed that the probability of working with AIDS patients would affect their choice of a specialty. Only 7% would refuse to treat an AIDS patient and only 15% thought that they had a right to refuse to treat these patients. Pakistan has been lucky in that it has been spared a severe HIV epidemic up until this time. However, China and India that thought themselves immune have now discovered that not only are they in the midst of a large epidemic, but that they are not prepared. While India believed itself to have only a handful of HIV infections 10 years ago, the WHO forecasts that it may have as many as 25 million by 2010. China, which was estimated to have approximately 1,000,000 cases of HIV infection in 2003, is forecasted by WHO to have as many as 10 to 15 million by 2010. Located between these two massive epidemics, it is unlikely that Pakistan will be spared the ravages of this virus. (DailyTimes-B1, 02/12/2007) HIV/AIDS cases increasing among our young, married women KARACHI: Bound by ‘watta satta’, a cultural tradition of exchanged marriage between two families, Nuzhat (not her real name), 22, cannot disclose her HIV status. “I know well what will happen. I’ll be thrown out of my husband’s home and my own family will never accept me either. It will also mean my brother’s home will be ruined. His wife is my husband’s sister and she too will be sent packing. In any case, where will I go?” she says. Entrenched age-old social attitudes, practices and stereotyping, coupled with unequal access to economic resources, are hampering progress towards dealing with the spread of HIV/AIDS in women, which, according to the UNAIDS, the joint UN programme on AIDS, make up almost 40 percent of new HIV cases. At the Eighth International Congress on AIDS in Asia and the Pacific, held in August 2007 in Sri Lanka, the worrying trend of a rising rate of HIV among young married women was reported. 105 Dr Naseem Salahuddin, an infectious disease specialist at the Liaquat National Hospital, Karachi, notes the increasing transmission of the virus from husbands to their wives. “A third of the 200 HIV/AIDS-infected people that I have treated since 1998 are women, mostly wives. It’s not just a health issue and must be looked at as a socio-cultural one.” Nuzhat’s husband, Taufiq, is a daily wage earner. Not only is he an injecting drug user - including heroin - but he also consumes alcohol and has multiple sexual partners. He knows his HIV-positive status and that he has infected his wife, and possibly even his daughter, but the knowledge has made little difference to his life. Dr Saleem Azam, who has been working with injecting drug users (IDUs) for the last 25 years, convinced Nuzhat’s husband to have her tested. “When I first saw her six months ago, she was at a breaking point and I had to send her for psychiatric counseling. It’s not the stigma she thinks she will face, it’s the outright rejection from her family that she knows is there.” Azam agreed that discrimination, unequal power relations between men and women, and economic dependence have exacerbated the issue. “The unequal power makes women more vulnerable, leading to coercive and violent sex. This often puts them at a disadvantage, with little option to either refuse sex or negotiate for safe and protected sex.” Azam has 5,000 IDUs registered with his non-governmental organization and, in the last few years, he has seen a disturbing spread of the virus among IDUs. He fears the impact it will have on others, particularly women. Keeping the illness secret out of fear and receiving no treatment is putting unbearable pressure on women like Nuzhat. “I can’t keep up a brave face any longer,” she said. According to a report issued Thursday by the Integrated Regional Information Networks (IRIN), the information unit of the United Nations (UN), Nuzhat is a classic case of the feminisation of HIV and AIDS that seems to have taken a toll on younger women in the Asia-Pacific region, where the epidemic is being fuelled primarily by the gender inequality that prevails. When there was nothing to eat at home, Nuzhat decided to get a job, though she cannot step out without a male escort. Without proper qualification, she had few options but to work in a local beauty parlour. Taufiq maintains his lifestyle on his meagre and sometimes uncertain income. He often beats up Nuzhat and forces to part with her wages, or otherwise he borrows from his mother. Nuzhat’s health is deteriorating but her husband takes little notice. “I often get fevers. Boils erupt out of nowhere but I am too scared to seek medical help. I’m always accompanied by some family member. If I go to see a doctor, my mother-in-law will come. What if she suspects something and discloses it?” This fear not only stops her from seeking help from one of the centres run by the Sindh AIDS Control Programme (SACP), part of the National AIDS Control Programme (NACP), but keeps her from having her two-year-old daughter tested who is also often sick. “I can’t take the risk,” she says. Nuzhat feels that women in her family are never given the status of human beings. “We are treated like cattle and beaten up regularly on the slightest of pretexts. Our sole reason for existence seems to be to procreate or provide sexual pleasure for men. Even my mother thinks that way, as does my mother-in-law. They both live in the city, but it hasn’t changed their mindset. Sometimes I feel I’ll become like them if I continue living in this suffocating environment.” (DailyTimes-B1, 07/12/2007) Civil hospital spends only Rs 52 on medicine per patient KARACHI: Civil Hospital Karachi (CHK) caters to around 5,000 patients per day; with 90 percent of its 958.3-million-rupee fiscal budget spent on utility bills and employee salaries, only 10 percent goes to medicine. This means that Rs 52 is spent on each patient. “The budget for medicines is sufficient. The CHK gives the patients medicines for free. This includes injections for a hematological disorder that costs Rs 98,000,” CHK Medical Superintendent (MS) Dr Kaleem Butt told Daily Times. About 78 percent of the total budget is for salaries and other benefits for CHK employees. Around 12 percent of the budget is spent on utilities and the remaining 10 percent is left for medicines. A seven-member purchase committee approves the purchase of medicines, keeping in view the considerations, demands and needs of the different CHK medical and surgical departments, said Dr Kaleem. At present, the CHK has a total of 3,277 employees, out of which 125 are consultants, 590 are doctors, 820 are house officers and 405 are nurses. The annual patient turnover of the CHK is estimated at more than one million per year. Although the CHK has 1,860 beds, the high turnover means each ward is stuffed with 20 extra beds. There are 48 wards in the CHK with a capacity for 38 to 39 patients. The extra beds overload the CHK, making an average total of 2,820 patients. The budget was allocated according to the number of beds. Every month there are 2,000 in-patients, with 112 daily admissions and 700 daily emergencies, reported the CHK. The casualty ward, which was recently awarded the status of a department, has to facilitate around 1,000 patients and is currently supervised by an RMO, who should be a post-graduate surgeon at the least. However, a consultant doctor at the CHK told Daily Times that he had been to 31 countries and when it came to casualty and trauma centres that wasn’t necessary the case. The CHK was established in 1898 with 140 beds at the district level. Ninety-eight percent of the donors were Hindus and Parsis while two percent were Muslims and it is affiliated with the Dow University of Health Sciences (DUHS). There are six general surgical units in the department of surgery including neurosurgery, pediatric surgery, orthopedic surgery, urology, vascular surgery, maxillofacial surgery and plastic surgery. Magneto Resonance Imaging (MRI) facilities are not available at the CHK nor does it have a kidney transplantation unit or department. (By Irfan Aligi, DailyTimes-B1, 08/12/2007) 106 Delay raises CHK project cost KARACHI, Dec 9: A delay in the execution of a computerisation project at the Civil Hospital Karachi has increased its cost by around 47 per cent of the first outlay approved by the provincial working development party (PWDP) in October 2005. The project is aimed at the integration of clinical as well as financial and administrative applications at the Civil Hospital Karachi (CHK) and is not expected to be completed within the next two years. Six months back, the officials looking after the hospital project were confident that the long pending work would finally commence in September 2007 after the earlier delays. However, the hierarchy in the provincial information technology and health departments still seem to be dragging their feet on the project. The delay will push up the estimated project’s cost, approved by the provincial working development party (PWDP) on Oct 8, 2005, by 47 per cent which will be borne by the provincial government. “If things go in the right direction, any initiation of the project on ground can only be visible in March 2008 or so,” said a source privy to the venture. Sindh Information Techno-logy Secretary Mohammad Zakir said that the PWDP had very recently informed the IT department that it had approved a modified scheme pertaining to hospital management and information system (HMIS). Efforts were now on for an administrative approval and expenditure sanction from the finance department, he added. He said that the revised scheme would enable the IT department to execute the CHK project in a more transparent manner. “Now we can expect more bidders for the project while the entire system and servers would have to be branded ones,” he said, adding that the issuance of the required approval and floating of tenders would need three months more. The cost of the HMIS project as approved by the PWDP is Rs137.609 million while the IT department will have to submit a detailed year-wise procurement plan and training and work plans with specific targets. A timeline and identification of the parties responsible for each activity will also be required to be mentioned. According to the sources, the hospital automation scheme first approved on October 8, 2005 had put the cost at Rs93.127 million but the project could not take off for various reasons. Despite repeated administrative changes at different levels over the last two years, the hierarchy of the department obviously remained divided into two groups — the accountability-conscious and the politically-motivated — who failed to develop a consensus on some of the main issues, commented a source. People at the helm of affairs in the health department and the hospital also failed to play any proactive role in the IT project issue. Another source said that the hospital staff could also be questioned for the slow pace of the project. Perhaps some of the staff feared the transparency that was to prevail after computerisation, the source said, adding that during a study related to the project the provincial IT department team had come across the improper recording or reporting of patients’ data and non-indenting and indexing of records or files and other instruments. A feasibility report for hospital management information system (HMIS) of the CHK was prepared by a private firm, taking almost two months as technical staff did not exist for the purpose in the IT department. The administrative approval for the project was obtained from the Sindh finance department in May 2006 following which tenders were invited in October 2006. Four companies participated in the tender, whose bids ranged from Rs100 million to Rs110 million, while the IT department had received an amount to the tune of Rs71 million in its kitty for the procurement of hardware and software. Sindh Information Techno-logy Additional Secretary Mohammad Yousuf, who is also looking after the CHK project, said the HMIS would be a turnkey solution that would allow users to register and record not only patients’ information, about their admission, treatment, discharge but also about other functions like purchase and procurement inventories, information regarding doctors’ duties and any other data related to the organisation. He said the project was part of the Sindh ADP 2005-06 and envisaged the creation of a viable IT-based operational entity to improve the patient management performance. Once data was consolidated through computers, quick retrieval of patient’s history, medical records, stocks position, goods receivable and other relevant information would become possible. “We hope to deliver the CHK project in line with international standards, something latest and which could be replicated in other teaching hospitals of the province,” Mr Yousuf said, expressing hope that the hospital would nominate a dedicated and competent focal person for the project. (Dawn-14, 10/12/2007) Bird flu claims first two lives in Pakistan PESHAWAR: The administration of Khyber Teaching Hospital on Thursday confirmed that two brothers Mohammad Ilyas and Tariq, who were brought to the hospital from Mansehra on suspicion of carrying H5N1, died of bird flu Monday last. “The two brothers have been confirmed as bird flu victims and are the first human sufferers of the disease in our country,” Dr Siddiqur Rahman, Acting Chief Executive of KTH, told The News on Thursday. Mohammad Ilyas and Tariq were working at a poultry farm in Mansehra and were brought to KTH in a serious condition. They were suffering from pneumonia and were kept in the isolation ward, said Dr Rahman. One of them was in critical condition at the time of arrival, Dr Rahman said. He added that the Ministry of Health after their expiry took blood samples and sent them to Islamabad to verify if they were carrying Bird Flu virus (H5N1). “Then I don’t know what happened to the test,” he added. Meanwhile, some reports on Thursday suggested that the laboratory test conducted in Islamabad confirmed Bird Flu influenza. A spokesman of Health Ministry in Islamabad said that they had died of bird flu, adding both the brothers were working in a poultry farm in Mansehra and had direct link with the chickens that resulted in the transfer of the virus (H5N1) into them. (The News-1, 14/12/2007) 107 No end to organ trade A REPORT in this paper suggests that the illegal trade in human organs, supposedly banned by the Transplantation of Human Organs and Tissues Ordinance promulgated in August, continues to thrive in the Punjab capital. Although this is cause for dismay, it is not entirely unexpected. Given the deplorable state of implementation of laws in Pakistan even in normal times — and these are hardly ordinary times — one could have anticipated the kidney trade to surface again. Initially there seemed to have been a lull in the nefarious activities of the robber barons who feel no qualms about exploiting the poor and cheating the desperately ill. But now they appear to be back in business. With the ordinance not being fully operative, it has been possible for the middlemen to resume their business without any fear of punishment. They are again luring impoverished people to sell their organs — and their dignity as well. Worse still, the surgeons and hospitals involved have also been emboldened to revert to their unethical practices which give the country an ugly image. If the efforts put into getting the transplantation law in place are not to go to waste, it is important that the government should expedite the full implementation of the Transplantation of Human Organs and Tissues Ordinance. The mechanisms provided in the ordinance, notably the Transplantation Authority and the provincial monitoring committees, have still to become functional. The hospitals which qualify for transplant services are yet to be registered and in the absence of this documentation the organ traders enjoy a free hand to circumvent the law which remains only on paper. Meanwhile it is being speculated that the vested interests which were benefiting from the absence of a law regulating organ transplantation are now at work to ensure that the ordinance remains a dead letter. It is important that this does not happen. (Dawn-7, 20/12/2007) Infectious hospital waste spreading hepatitis KARACHI, Dec 20: Hepatitis-C is spreading rapidly among a large number of young garbage pickers, as they pick used syringes and other clinical waste from different hospitals of the city for recycling. Poor enforcement of the Hospitals’ Waste Management Rules (HWMR), 2006, is responsible for this sorry state of affairs, which aids the spread of diseases amongst wider sections of the population. Former director-general of the Environmental Protection Agency and current Additional Secretary Health Dr Iqbal Saeed Khan, said that the majority of the over 1,000 hospitals in the city are not properly disposing of their infectious clinical waste. He added that vulnerable children and youth, who pick recyclable items from the waste, get cuts and bruises, which transmit viruses and bacteria into them. “A random study of different hospitals suggests that over 50,000 garbage collectors, mainly young Afghani children, are suspected to be hepatitis-positive,” he said. Dr Khan regretted that even those hospitals that have incinerators were not segregating infectious and non-infectious waste before incinerating it. EPA Director Kiran Noman, said that the EPA was short of staff to monitor and enforce the HWMR, 2006, adding that there was a ban on recruitment. “But now we have got 10 monitoring inspectors that would inspect and ensure enforcement of the HWMR, 2006, in Karachi,” she said. Special Secretary Public Health, Sindh, Dr Captain Abdul Majid, said that the health department has some information about an organised business involving medical waste going on behind the Sobhraj Maternity Hospital, Saddar, but no one has been caught yet. He added that most of the big public hospitals in Karachi have incinerators but the smaller hospitals and dispensaries are yet to get incinerators. “The Sindh government had proposed to the federal government three months ago to legislate for the use of autodestructive syringes, so that the issue of reuse of disposable syringes could be settled,” he said. He held quacks responsible for the situation. According to him, they are the final beneficiaries of the recyclable clinical waste trade. The secretary public health regretted that he could not go “too far” as far as accountability of the quacks was concerned. “We can only lodge an FIR against someone according to the PMDC rules, which are not too effective. These quacks restart their business after some days,” Dr Captain Abdul Majid said while quoting the example of a hepatitis epidemic in Qambar district of Sindh due to the abundance of quacks there. (Dawn-17, 21/12/2007) Delays hit CHK uplift project KARACHI, Dec 23: Works pertaining to the maintenance and repairs at the Civil Hospital Karachi are at a virtual standstill for the last four months allegedly due to the indifferent attitude of the Sindh government’s works and services department. According to sources in the hospital, a number of outpatients departments and in-house patient units, including the plastic surgery and surgery units, are in shambles, while the face-lifting of different buildings and sanitation improvement works are either to be initiated or left halfway. Despite repeated reminders and requests, the works and maintenance department had failed to take any action, said a CHK official. He said that an executive engineer of the works department posted at the hospital was transferred on the recommendation of the former provincial health minister a few months back only in view of his alleged incompetence. It was officially stated that the failure of the works department was once again discussed at the 20th meeting of the CHK’s board of governors. The members were told that repair and maintenance fund was dedicatedly available for the hospital, but works on priority as well as those sanctioned under the annual development programme were failing to take off or see any completion due to the non-availability of an executive engineer, who was exclusively posted at the CHK with the powers of drawing and disbursing officer (DDO). 108 The second in command from the works and services department, posted at CHK, an assistant engineer (AE) is not in a position to execute plan as he does not have the authority to draw and disburse the fund for any purpose. The works department is neither posting an authorised engineer nor assigning the DDO powers to the AE at the CHK and as such the workers maintenance and repair works at the hospital are hampered. It was further learnt that posting of new executive engineer or delegation of the drawing and disbursing powers to the assistant engineer were also being delayed on the pretext that the provision of special status to the CHK in regard of fund utilisation and posting of a senior engineer exclusively at the hospital, which was approved by the former chief minister for one year had also expired and the CHK was again required to move the high-ups for a re-extension of the provision in question. However, the BoG has reportedly requested the Sindh government to ensure an immediate posting of an executive engineer (M&R) by the works and services department or delegation of DDO powers to the AE or any other officer. The Civil Hospital’s BoG had constituted a committee to look into the allegations of substandard maintenance and repair works having been carried out on the hospital’s premises in August last, but any relevant report was still awaited, said a source. In the meantime, the board, through a press release, also announced that the chairman of BoG and the vice-chancellor of the Dow University of Health Sciences would discuss the situation and also evolve a code of conduct aiming at a flawless relation between the two institutions. The BoG meeting was attended by medical superintendents of the CHK and the Lyari General Hospital, Dr Kaleem Butt and Dr Mukhtar Khawaja respectively, Ali Akbar Qureshi, Abdul Sami Khan, Saeed A. B. Mirza, Abdullah Feroze and Kauser Pervaiz. (By Mukhtar Alam, Dawn-13, 24/12/2007) Over 60 healthcare centres await promised govt funds KARACHI, Dec 25: As many as 61 healthcare facilities, including hospitals, maternity homes and dispensaries, constructed over a couple of years in different towns of Karachi are still not operational because of a lack of funds. The first half of the financial year is coming to an end, but the Sindh government has not yet provided the city government the promised sum to meet the salary and non-salary expenditures of the hospitals, said a senior health official of the city government. The city government needs to appoint and post 750 to 900 general physicians and specialists to make the dormant health facilities functional, besides running the existing hospitals and dispensaries efficiently. Commenting on the overall status of the CDKG-run hospitals and dispensaries, including 13 major facilities, a source in the district’s health department said that about 2,500 posts of doctors and 3,712 of paramedics had been included in the budgetary allocations of the government, but 15-20 per cent of the posts were virtually vacant since the retirement or death of the personnel initially occupying them. The prolonged ban on recruitment was among the reasons behind the vacancies, the source added. Since the city government alone cannot meet the burden of staff salary and other necessities, it requested the Sindh government about seven months back to approve the sanctioned new expenditures (SNE) for the 61 healthcare facilities. Consequently, the Sindh government announced a special allocation of Rs250 million for the city government’s expenditures on the eve of the 2007-08 budget. The Sindh government had decided to allocate a one-time special grant of Rs500 million to various district governments in the province in order to enable them to launch their dormant new and old facilities. There are about 240 healthcare units in the province, 61 of them in Karachi, that have been built and completed over the last couple of years but they have not yet been made functional because of the non-availability of the required funds with the district governments concerned. It has also been learnt that about 90 per cent of the city government health facilities have not been provided with appropriate furniture even for doctors. A relevant official said that district government would not be able to overcome the shortage of doctors, even if the Sindh government released them the promised grant, unless the ban on recruitment imposed by the chief minister was lifted. According to an estimate, there is one doctor for every 5,000 patients and one paramedic for every 3,000 patients living within the jurisdiction of the city district government. The issue of ‘ghost employees’ is another factor aggravating the situation. A big population in Shah Faisal, Malir, Orangi, Baldia, Gadap, Landhi, Nazimabad, Bin Qasim, Korangi, Jamshed, Site and Keamari towns is deprived of vital healthcare facilities which would, otherwise, have been available very close to their areas. (By Mukhtar Alam, Dawn-15, 26/12/2007) Miscarriages impact significantly on future births A previous abortion or miscarriage significantly increases a pregnant woman’s odds of having a low birth weight infant or giving birth pre term. The level of risk is directly related to the number of previous abortions a woman has. American researchers looked at more than 45,500 women who gave birth and found that women who had one prior miscarriage or abortion were roughly three times as likely to have a low birth weight baby as those who had no such history. This risk increased to roughly five-fold in women who had two previous abortions or miscarriages, and nine-fold in women who had a history of three abortions or miscarriages. 109 Likewise, women who had one previous abortion or miscarriage were 70 per cent more likely to experience a pre term birth. This risk increased two-fold in women with a history of two abortions or miscarriages and three-fold in those with three abortions or miscarriages. These risks were still apparent even after adjusting for potential confounding factors, such as smoking, high blood pressure, and heavy alcohol use. The researchers noted that many previous studies have failed to show a link between prior abortions and low birth weight or pre term birth. However, most of these studies have been smaller in size than the current one. Prior studies of comparable or larger size have generally supported these associations. The researchers suggest that women and healthcare providers should be informed of this potential risk. Also, future studies need to revisit the question of whether previous abortions can have a negative impact on fetal growth independent of prematurity. The findings appeared in latest issue of Journal of Epidemiology and Community Health. (The News-19, 27/12/2007) In poor health FOR a nation that has just turned 60, we are far from fighting fit. In fact our healthcare system has aged beyond its years due to poor maintenance and remains plagued with unfulfilled promises. What truly ails it is brutal apathy on the part of health authorities. The latest evidence of flagrant indifference is that as many as 61 health institutions in Karachi with another 180 in the rest of Sindh, which were built in the last few years, remain dormant due to paucity of funds. Despite the fact that we are approaching the second half of the fiscal year, the city government still awaits the assured finances from the Sindh government. These are not only to start the inoperative facilities but also to upgrade and manage existing services. Some six months ago, the Sindh administration had sanctioned a special one-off sum of Rs500m to different district governments of the province, but this has not seen the light of day yet. Other dismal statistics have also emerged from recent estimates that show one doctor for every 5,000 people living within the jurisdiction of the city district government. However, keeping our frail healthcare infrastructure in good shape is no mean task. It involves sustaining standards and financial stability. Perhaps, it may be an idea to focus on preventive medicine and also use the much pledged funds to develop an action plan whereby easy, efficient and subsidised dispensation of health amenities is made possible for all so that actual care does not begin in the emergency rooms. The strategy should focus on primary care, updated and vigilant emergency services, which include ambulances, paramedics and help lines, and information on avoiding infection and injury. Successful implementation of such a scheme is particularly dependent on governmental involvement that translates into accessibility of funds as well as the creation of a quality monitoring authority to prevent pilfering and negligence. Incentives to doctors, nurses, attendants and paramedics are of equal significance. After all, robust medical facilities promote both productivity and life expectancy of a nation. (Dawn-7, 28/12/2007) Another unsatisfactory year for the health sector Promulgation of Human Organs Ordinance, thanks to the sustained efforts of the Sindh Institute of Urology and Transplantation (SIUT), setting up of Dow University Limbs Centre with assistance of the Indian Jaipur Foot Society to provide limbs to people free of cost, uplifting of health facilities, launching of mother-neonatal child health are widely considered to be positive developments in the health sector of the city in 2007. However, death of over 22 people by dengue, loss of several lives by malaria, murder of prominent doctor of Jinnah Postgraduate Medical Centre (JPMC) and three medical students, and continued protests of doctors for better facilities indicates poor performance in health sector during 2007. Furthermore, the death of the two brothers at the end of the year reportedly caused by bird flu in the country prompted the city health officials to enhance vigilance against it and provide necessary training and guidelines to them. Dengue is considered to be a major new health challenge in the metropolis, which is going to stay here for considerable period as experience of other countries in the world showed. Around 3,000 people were affected by dengue in 2007 in the provincial capital, said deputy secretary health, Shakil Mullick. Among them 22 died. He believed that due to public awareness, ratio of death and dengue severity reduced considerably. The data of the year 2006 revealed that 5,000 people were affected by dengue, out of which 52 died. Taking notice of the situation, the government has provided facility of test at hospitals free of cost, the official claimed. “Dengue is a serious issue as authorities concerned have failed to address it properly,” said the general secretary Pakistan Medical Association (PMA), Dr Qaiser Sajjad. He admitted that providing facility of free test is a good step but much more needs to be done. He lamented the lack of “virology labs” to study all viruses. He said there is no facility for detection of Congo and Chicken Guinea viruses, which has already taken several lives in India. Sajjad said pollution has become a huge problem due to unprecedented increase of vehicles besides construction work that has compounded the problem. Despite the fact that judiciary took notice of pollution caused by smoke-emitting and old vehicles, the authorities concerned have failed to implement its instructions due to unknown reasons. Lack of proper disposal of garbage is another contributing factor towards health problems as around 3,000 tons garbage remains on road every day, the PMA believed. The scheme of CNG-fitted rickshaws has also not been implemented so far, resulting in increase in noise pollution. It is due to this factor that “hearing impairment problems” have become more acute in the city as compared to other parts of the country. Furthermore, Sajjad adds that it is extremely regrettable that people are dying because of preventable diseases. As no sufficient efforts have been taken to control breeding grounds of mosquitoes, malaria caused around 17 deaths in Keamari town, which prompted the PMA to hold medical camp there. Meanwhile, murder of three medical students at the JPMC during “clashes” among student groups is the most disturbing development, which adversely affected the functioning of the city’s biggest public hospital. Also, the killing of a doctor of the hospital enhanced insecurity among doctors. While the entire health sector gave a gloomy picture, the promulgation of human organs ordinance came as a ray of hope. The sustained struggle of SIUT finally became fruitful when the government promulgated the ordinance to curb “kidney 110 trade”, which had given a bad name to the country. It also launched “organ donation” campaign, one positive impact of which was conducting transplantation in the city on daily basis, said Dr Bakhsh Ali, spokesman for the SIUT. Frequency of carrying out hepatobiliary surgery for liver has also increased, he added. Moreover, the SIUT’s head, Dr Adib Rizvi also launched the ‘Institute of Transplantation Sciences’ on Super Highway near Kathor, which will likely be constructed within next two years. (By Imtiaz Ali, The News-20, 29/12/2007) SIUT performs landmark transplants KARACHI, Dec 30: The Sindh Institute of Urology and Transplantation achieved a milestone in its area of specialisation by performing the first deceased donor transplantation after the promulgation of the Transplantation of Human Organs and Tissues Ordinance 2007 in February. Dr Anwar Naqvi of the SIUT told Dawn on Sunday that his institute had performed at least two deceased donor transplantations before the passage of the new law. The new transplantation was performed at the SIUT by a team of surgeons led by Prof Adib Rizvi on Dec 29, 2007. “The donor was Prof Razak Memon, professor of pathology at the Sindh Medical College. The 59-year-old professor was from Pir Jo Goth and he sustained massive intracranial bleeding. All measures to save Prof Memon’s life had been instituted since his admission on Dec 25, 2007. However, according to the neurosurgeon, surgery was not possible due to massive brain injury,” said Dr Naqvi. “On Dec 27, Prof Memon sustained irreversible brain death. The diagnosis of brain death was certified by a team at the Civil Hospital’s surgical ICU consisting of neurosurgeon Prof Junaid Ashraf, neurophysician Prof Abdullah and intensivist Prof Saeeda Haider on two separate occasions.” He explained that the brain death protocol enunciated in the Transplantation of Human Organs and Tissues Ordinance 2007 was duly followed. According to an SIUT statement, Prof Memon’s family has been aware of all aspects of transplantation for over 20 years. “His brother received a renal transplantation from his mother in 1986 in London. Later on, his brother received a renal transplantation donated from his wife at SIUT in 1994. The benefits of renal transplantation were clear to the family as two of its members were beneficiaries of successful transplantation, which changed their quality of life so positively as to allow their full rehabilitation and restoration to a healthy life.” The SIUT statement adds that the family decided to donate both kidneys of Prof Memon to save the lives of at least two patients of dialysis in accordance with the donor’s wish made during his lifetime. “The kidneys were removed surgically on Dec 29. The recipients of the kidneys were 30-year-old Zarina, a housewife from Dadu, and 17-year-old Kashmala, a student from Dera Ghazi Khan. The first recipient has three children, the eldest being 10 years old. She had no donors in the family. The second recipient has three siblings but none of them matched with their sister on tissue typing. Both the patients are doing well after the surgery,” says the SIUT statement. (By Mukhtar Alam, Dawn-13, 31/12/2007) SIUT performs first deceased donor transplant KARACHI: The first deceased donor transplantation was performed at the Sindh Institute of Urology and Transplantation (SIUT) on Sunday. The donor was a Professor of Pathology at Sindh Medical College (SMC) Prof. Razak Memon who had sustained massive intracranial bleeding. Since December 25, all measures were taken to save his life but due to the fatal brain injury, the neurosurgeon claimed that surgery was impossible. On December 27, Memon sustained irreversible brain death. A surgical ICU team consisting of neurosurgeon Prof. Junaid Ashraf, neurophysician Prof. Abdullah and intensivist Prof Saeeda Haider at the Civil Hospital Karachi (CHK) confirmed the diagnosis. According to an SIUT statement issued Sunday, Memon’s family decided to donate both his kidneys to save the lives of two dialysis patients as Memon had expressed the desire to do so while he was alive. The kidneys were removed surgically on December 29 at SIUT by a team of surgeons led by Prof. Adib Rizvi. Both patients are doing well after surgery. (DailyTimes-B1, 31/12/2007) Children on an empty stomach on empty streets KARACHI: At a time when all the commerce in Karachi is facing a shutdown and there is an acute shortage of basic necessities in the city like food and fuel, no one is finding the going tougher than the street-children of Karachi. “I have not had a single bite to eat since yesterday morning as I was unable to find anything,” said nineteen-year-old Sajid, whose sustenance comes from the charity given at the shrines and different hotels of Karachi. Sajid was born in Multan. He has four sisters and three brothers. His father was a drug addict who regularly beat his wife and children compelling Sajid to run away from home. He first went to Sukkur but soon found himself living on the streets of Karachi, the commerce capital of Pakistan. According to the Society for the Protection of the Rights of the Child (SPARC), there are 25,000 homeless children living on the streets of Karachi. “These children are either orphans and have no one to look after them or they have fled from their homes because of unbearable living conditions,” SPARC regional manager Akhtar Baloch told Daily Times. 111 He said these children live near shrines, religious places, and areas with a large number of food shops as they rely on charity. Since most of the hotels have been closed for the last four days and there has been no one visiting the shrines, the street children have been hit hard. “I hangout with my friends on a small off-street of Burns Road, the food street of Karachi. There are six hotels there where hundreds of the people dine daily and some of them buy us food which last us the whole day,” said Sajid. Sajid was also unaware of what really happened that caused Karachi to become deserted all of a sudden. He has been moving from place to place looking for some activity (and food), but has had little luck yet. “After finding the bazaars and shops closed, we (Sajid and his friends) moved to where the big tower [Empress Market tower] is located, but strangely it was as deserted as the rest of the city,” said Sajid. The Abdullah Shah Ghazi shrine, where in normal days you can get food round-the-clock, also proved a disappointment for Sajid and his friends and they have been forced to look in the garbage for edible items. (By Amar Guriro, DailyTimes-B1, 31/12/2007) DAWN REVIEW Food for thought A little boy was rummaging through the garbage. Though he was searching diligently he could not find what he was looking for. Gaunt and weary, he left the area and headed further up the alley. Again he searched and picked his way through another pile of trash. The young boy’s face brightened for a moment as he found a few bare scraps of roti. There was no doubt the food was dirty but the boy ate it ravenously without a second thought. Asad is one of the thousands of children affected by malnutrition and hunger. For a large number of children in Pakistan, all that matters to them is their day-to-day survival — something to eat and somewhere to sleep. Despite several high-profile international initiatives, the number of children in our country who go hungry, has barely fallen in the past 15 years. Of these, thousands are victims of famines that attract headlines, TV coverage and emergency aid. Far more die unnoticed, killed by the effects of chronic hunger and malnutrition, a “covert famine” that stunts their development, saps their strength and cripples their immune systems. Shahnaz, 20, from a remote village of Sindh was married off by her parents when she was 13 to a much older man Rehman, aged 40. Five years later, she has four hungry children. Her mother 'sold' her to be married because her family of eight members did not have enough food to eat and the bride price of Rs50,000 enabled them to buy food for the family. “We do not have enough food to feed our children. My kids don’t drink milk because I can’t afford to buy it,” says Shahnaz. Many times the children sleep with empty stomachs. The husband, Rehman, is a bonded labourer who works in the fields of the landlord and is burdened by large debts. Rehman wastes whatever little money he manages to get on alcohol. Shanaz’s plight is common. Young girls, not yet ready to handle married life responsibilities, become victims of domestic violence, often giving birth to premature children. In many parts of Sindh, women work in the fields for long hours, many kilometres away from home, and are paid less than a dollar a day. Faiza, 40, said she was feeding her three-month-old daughter Nazia with just boiled water and sugar because she had nothing else. “My baby died because of lack of nutrition. I wanted to breastfeed her, but there was not enough milk.” Research shows that children born to mothers who go hungry during early pregnancy run a greater risk of heart disease as adults. The evidence comes from the Dutch famine of 1944-45, which occurred when the Allied Forces failed to take hold of the bridge spanning the Rhine at Arnhem. At birth such children also had smaller heads, born to undernourished mothers. According to reports, more than 50 per cent of children in Pakistan are malnourished. The four major causes of deaths in children are diarrhoea, acute respiratory illness, malaria and measles. Taken together, these four diseases account for almost half of all the deaths among children under the age of five. Analysis of data from hospitals and villages of Pakistan shows that all the four diseases are far more deadly for children who are stunted or underweight. In the case of diarrhoea, numerous studies show that the risk of death is as much as nine times higher for children who are significantly underweight, the most common indicator of chronic under-nutrition. The figures for underweight under-fives in India, Bangladesh, Pakistan and Nepal are 47 per cent, 48 per cent, 38 per cent and 47 per cent, respectively. According to Unicef, malnutrition is associated with over half of those deaths. That comes to 24 children each minute. 112 The dire situation in South Asia is not caused by shortage of food but by food that is low in quality and nutrients. Social issues also contribute to the problem. According to another Unicef report, more than a quarter of the children in the developing world are still critically undernourished. It also found that 146 million children go hungry everyday and 506 million die every year because they don’t get enough to eat. High mortality rate amongst mothers during pregnancy and delivery is also due to the adverse effect of hunger. Increased child labour and low literacy rate may also be attributed to this problem of food insecurity and hunger. The World Bank reported in the late `90s that more than 800 million people went without food everyday, and more than 500 million children were fed half their normal diet. In the census of the nineties, some 40,000 hunger-related deaths occurred everyday, mostly in the rural region. In 2007, nearly 854 million people are starving. That’s 17 per cent of the world’s population. The figure includes 11 million in the industrialised countries, 30 million in countries in transition and 799 million in the developing world. While world population reached one billion in 1830 (cut down drastically due to epidemics and wars over the centuries), it only took one hundred years to add a second billion (1930), 30 years for the third billion (1960), 16 years for the fourth billion (1976), and 11 years for the fifth billion (1987). The world’s population is expected to reach 8.5 billion by the year 2030. As the number increases, per capita availability of arable land decreases. The terrible irony is that the world can produce enough food to feed its expanding population. While some famines are caused by natural disasters, most of the starvation in the world can be avoided if it were not for man’s selfishness and inhumanity. The governments’ corruption and economic oppression are the main problems. While children starve, some rich nations destroy millions of tonnes of food in order to keep prices artificially high. In the last few months, the prices of flour, milk, potato and meat have increased persistently in Pakistan. According to flour mill owners, the provincial food authorities are not releasing wheat in accordance with the district’s wheat quota, resulting in a surge in flour prices. As the price of a 100kg wheat bag in the open market climbed to Rs1,600 from Rs1,350, it was impossible for them to provide flour at cheaper rates to the consumers. Shopkeepers are selling a 20kg bag of mixed flour which in reality weighs only 18kg, for Rs395 or more. Most of the people in the rural areas eat roti with onion or tea. In these circumstances, it has become an ongoing crisis in the rural households to combat starvation. The nutrition situation is expected to further deteriorate in the country. There has been a sharp increase in the prices of onion and tomatoes in recent months, with tomatoes being Rs150 per kg recently. It makes the situation even more tragic since a lot of money is spent to build sophisticated infrastructure for the rich investors that include highways, bridges, dams and underpasses. This clearly demonstrates the priority of the government. Lack of proper nutrition is one reason why an estimated 115 million school-aged children around the globe belong to primary schools. Many of these children also suffer from micronutrient deficiencies, lack of essential vitamins and mineral. This ‘hidden hunger’ affects brain development and compromises the immune system. The United Nations World Food Programme spends nearly $3 billion each year to combat food shortages around the world. Most of that money comes from governments’ and large corporations, which brings emergency food relief to some 90 million hungry people in 78 countries. Different nutrition projects such as Tawana Pakistan Project (TPP) -–– a joint initiative of the Ministry of Women Development, Pakistan Baitul Mal and the Aga Khan University (AKU) and Food Bank Project, a project of Pakistan Dietetic and Nutrition Association (PDNA) -–– were not able to reduce the number of hungry and malnourished children in the country. The TPP programme was supposed to be implemented in the 26 most malnourished districts of Pakistan. It had a targeted coverage of 650,000 girls, aged five to 12, with an equal proportion of school-enrolled and also out-of-school girls, and was designed to provide a daily mid-day meal at the rate of Rs7 per day per child, weekly micronutrient supplements and biannually de-worming medicine to girls of five to twelve years of age. The project goals, objectives and expected outcomes were incredible, but, even today, infant mortality rate is about 110/1000 births, which is extremely high as compared to 60/1000 births in the developing countries. Out of 2.5 million girls born in Pakistan each year, it is estimated that at least six hundred thousand are undernourished at birth, with an increased risk of mental and physical disabilities. The corresponding data can only confirm the alarming increase in the number of hungry and malnourished children in the country. Translated into more relatable expenses, for the price of one F16 aircraft, a school full of hungry children could eat lunch everyday for five years. Despite all these strategies and availability of basic tools, the programmes have not met the desired objectives or targets, and no marked improvement in indicators of child health and malnutrition could be observed. Adequate food supply with national average daily per capita availability of calories (2350) and proteins (62 g), malnutrition prevalence is very high in Pakistan, and remains a serious obstacle in improving maternal and child health. Like other objectives to be achieved, our national health policy-makers aim to reduce the maternal mortality rate to 250 per 100,000 live births by 2010. Data and analysis can only confirm the alarming increase in the number of hungry and malnourished children in the country. Children continue to die of hunger in huge numbers, despite a worldwide drive to combat it. Protests, campaigns and media releases to fight against hunger are now a prominent feature round the globe. 113 Many organisations have listed the campaign against hunger on the top of their charters. Policy researchers, advisors and nutritionists have taken up the task to challenge UN member states to fulfil their millennium commitments to halve hunger by 2015. The United Nations has so far failed to address the most alarming issue. The numbers, graphs and analysis on the situation does not seem to have any impact on the policies of our government to meet one of the most important MDGs. Too weak to work Nobel prize-winning economist Robert Fogel has pointed out that hungry people cannot work their way out of poverty. He estimates that 20 per cent of the population in England and France was effectively excluded from the labour force around 1790 because they were too weak and hungry to work. Improved nutrition, he calculates, accounted for about half of the economic growth in Britain and France between 1790 and 1880. Since many developing countries are as poor as Britain and France were in 1790, his analysis suggests reducing hunger could have a similar impact in developing countries today. —H.S. Food insecurity According to reports, the 2005 earthquake in northern Pakistan had left millions of people starving and homeless. Around 2.3 million people needed food aid and it was estimated that nearly 10,000 children could die of hunger. Six out of nine districts affected by the earthquake were already in the most ‘food insecure’ parts of Pakistan, where people depended on subsistence farming, livestock and wage labour during the lean season. The finding says more than half of rural households surveyed lost all or most of their grain stocks and one fourth of the livestock. A large number of children were found suffering from diarrhoea or respiratory illnesses and acute malnutrition. The reports also said that 20 per cent of mothers with children under two years old stopped breastfeeding because of inadequate breast milk. Many international and local organisations were involved in saving children from hunger and acute malnutrition. The government also claimed to have provided help. At present the situation remains grim. There have been alarming incidents of hunger and food deprivation in these areas. — H.S. Children in India A massive 440 million people languish at the bottom of the economic pyramid in India, and about 500,000 children are born deformed each year due to vitamin/mineral deficiencies. India’s child sex ratio is still a nettlesome 927 girls for every 1,000 boys, while even poor African countries (Ghana at 964 and Nigeria at 965) fair better, as does Pakistan with 958. Experts reiterate that child malnutrition is not only responsible for 22 per cent of India’s diseases but is also a serious economic hazard. —H.S. (By Hina Shahid, Dawn-The Review, 25/10/2007) The silence within I have read an upsetting news report in an international magazine recently. It is about abortion, its legal/illegal status and its ramifications on women’s health in different countries. It is an alarming report compiled by UN agencies; the findings have also been published in the British medical journal Lancet. As a person who has been through the procedure, I can relate to the pain, agony, fear, anxiety and, above all, an overwhelming sense of guilt which millions of women experience. Conducting research for this write up, I talked to my friends, neighbours, colleagues, gynaecologists and acquaintances to get an idea as to the prevalence of the phenomenon in our society. Like other taboo subjects, abortion is also swept under the carpet and everyone likes to believe that it simply does not exist. The available data prove otherwise. Abortion is, undoubtedly, not an easy option or decision for any person or family. Without going into the moral and ethical debate and concerns, it could be merely taken as a medical procedure, an option exercised because of resistance to using contraceptives, or simply as a matter of choice for women. The available statistics at the national level are simply disheartening, and prove that the issue is directly related to maternal health, the low status of women in society, their absence in the decision making process, a lack of control over their fertility and extensive discrimination they face throughout their lives. At another level, it is a symptom of the underlying problems which are rampant, more or less in many countries, irrespective of their developing and developed status. The report in question, the broadest international study of abortion ever undertaken, emphasises the fact that restricting abortion has little effect on the number of terminated pregnancies, as it still accounts for 13 per cent of maternal mortality globally. Contrary to common perception, it drives women to seek illegal, often unsafe backstreet procedures leading to an estimated 67,000 deaths a year. A further five million women require hospital treatment as an outcome of botched procedures. Internationally, approximately 20 million unsafe abortions are carried out every year, of which nearly 97 per cent are in 114 developing countries and half of these are in South-East Asia. “The continuing high incidence of unsafe abortion in developing countries represents a public health crisis and a human rights atrocity,” the report adds. Coming to the scenario in Pakistan, the available data are alarming. According to one estimate, 980,000 unsafe abortions are carried out here annually which in statistical terms mean one terminated pregnancy in every six. Officially, abortion is illegal and condemned as a murder and is only allowed in order to save women’s lives or to preserve their physical and mental health. However, due to the patriarchal structure of society, there is more focus on its moral, ethical and religious aspects, ignoring the medical and structural inequalities and discrepancies. Contrary to the popular perception that links prostitution and extramarital affairs to abortion, the fact is that 90 per cent of these cases involve married women with three or more kids, complicated pregnancies or bad foetal health. In such cases induced abortion is used to limit family size with the husbands’ concurrence. Still, owing to unsafe procedures nearly 250,000 women suffer post-abortion complications by inept handling by unskilled healthcare providers and some 3,000 of them die annually with resulting complications. It is also the case of simple economics for many families that opt for abortion. High inflation and rampant consumerism make it very difficult to support large families for many concerned. Then, because of a mindset and an overbearing patriarchal setup, many Pakistani men oppose the use of contraceptives but agree to abortion, which does not affect their own health, even though it may prove fatal for women. Seeking abortion reflects an unmet need for family planning. According to a survey report, although over 90 per cent of married couples have the knowledge about various contraceptive methods available, only 22 per cent use them with regularity. Coming to the measures that should be adopted to control the phenomenon, there is a need to understand that abortion is directly linked with the status of women in society. In order to save the lives of the women concerned there is a need to educate and empower them as well as include them in the decision making process. Couples should be educated on the benefits of the norms of smaller families to promote the use of contraceptives. That is the safest way to avoid unwanted pregnancies. (By Moniza Inam, Dawn-The Review, 22/11/2007) 115