COMPARATIVE INVITRO ACTIVITY OF GEMIFLOXACIN AND
advertisement

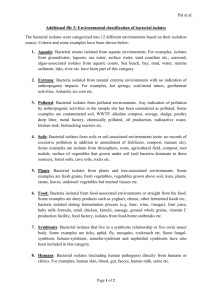
COMPARATIVE INVITRO ACTIVITY OF GEMIFLOXACIN AND SOME OTHER QUINOLONES AGAINST SOME CLINICAL BACTERIAL ISOLATES Ching, Fidelis Poh*1, Josephs, Godwin Chimechefulam2 and Ossai, Awele Maureen2 *1 Department of Pharmacology, Faculty of Basic Medical Sciences, College of Health Sciences, Niger Delta University, Wilberforce Island, Yenagoa, Bayelsa State, Nigeria. E-mail: fidelching@yahoo.ca Josephs, Godwin Chimechefulam 2Department of Pharmaceutical Microbiology, Faculty of Pharmacy, University of Benin, Benin City, Edo State, Nigeria E-mail:godwinjosephs@yahoo.com *Corresponding author: Dr Ching, Fidelis Poh Department of Pharmacology, Faculty of Basic Medical Sciences, College of Health Sciences, Niger Delta University, Wilberforce Island, Yenagoa, Bayelsa State, Nigeria. Phone: +2348067541738, E-mail: fidelching@yahoo.ca COMPARATIVE INVITRO ACTIVITY OF GEMIFLOXACIN AND SOME OTHER QUINOLONES AGAINST SOME CLINICAL BACTERIAL ISOLATES ABSTRACT Background: Resistance to antibacterial agents has become a global problem and has made many existing antibiotics less effective in the treatment of infections for which they were effective. Gemifloxacin is a third generation fluoroquinolone with broad spectrum antimicrobial and enhanced activity against both aerobic and anaerobic Gram – positive bacteria. It is recommended for the treatment of respiratory tract infections. Objectives: This study evaluated and compared with ciprofloxacin, ofloxacin and norfloxacin its in vitro antibacterial activity against Staphylococcus aureus, Escherichia Coli, Alcaligenes faecalis, Pseudomonas aeruginosa, Serratia marcescens, Enterobacter aerogenes, Proteus vulgaris and Klebseilla pneumoniae. Methods: The minimum inhibition concentration (MIC) and zones of inhibition assays were employed. In the MIC assays final nutrient agar extracts concentrations of 5, 7.5, 10, 15, 20, 25 and 30µg/ml of gemifloxacin, ciprofloxacin, ofloxacin, and norfloxacin were used. In the zones of inhibition assay 0.2ml of the MIC of gemifloxacin against each bacterium was used. Results: The MICs of gemifloxacin were 7.5µg/ml for Proteus vulgaris, 10µg/ml for Staph. aureus and Enterobacter aerogenes, 15µg/ml for E. coli, 20µg/ml for Pseudomonas aeruginosa, 25µg/ml for Klebsiella pneumonia and 30µg/ml for Alcaligenes faecalis and Serratia marcescens. The clinical isolates were most sensitive to ofloxacin with MICs of 7.5µg/ml for Proteus vulgaris and 10µg/ml for the other isolates. The isolates were least susceptible to norfloxacin with MICs of 10µg/ml for Proteus vulgaris and 30µg/ml for the other isolates. The results show that the clinical isolates were most sensitive to ofloxacin followed by gemifloxacin, ciprofloxacin and norfloxacin respectively. Conclusion: The study has shown that gemifloxacin possess antibacterial activity against the pathogenic bacteria and could have a place in the treatment of the infections caused by the organisms. Keywords: Gemifloxacin, urinary tract infections, invitro activity. INTRODUCTION The quinolones are synthetic broad spectrum antibiotics. The first quinolone, nalidixic acid was introduced essentially for the treatment of urinary tract infections. The newer quinolones, the fluoroquinolones, however, are used for urinary and respiratory tracts infections as well as other infections.1 The second generation quinolones which include ciprofloxacin, ofloxacin, and norfloxacin are used essentially for the treatment of urinary tract infections while the third generation such as gemifloxacin, levofloxacin and moxifloxacin are used essentially for the treatment of respiratory tract infections.2 Ciprofloxacin is also used for the treatment of other infections such as bones and joints, endocarditis, gastroenteritis, malignant otitis externa, lower respiratory tract infections, chronic bacterial prostatitis, anthrax, acute sinusitis although not as first line.3 Ofloxacin is also used for the treatment of acute bacterial exacerbation of chronic bronchitis, community acquired pneumonia, uncomplicated skin and skin structure infections, non-gonococcal urethritis and cervicitis, acute pelvic inflammatory disease and prostatitis. 4 In adult population, norfloxacin is used for the treatment of uncomplicated and complicated urinary tract infections.5 Gemifloxacin is effective in the treatment of penicillin-sensitive and penicillin-resistant Streptococcus pneumoniae and atypical pathogens which include mycoplasma pneumoniae and chlamydia pneumoniae.1 The development of resistance to existing antimicrobial agents has become a global concern. The treatment of urinary tract infections with the traditionally used quinolones is being threatened by the emergence of multidrug resistant pathogens.2,5,6 This emergence of the multidrug resistance pathogens necessitates the need to explore the other quinolones with broad spectrum activity in the treatment of urinary tract infections and other infections. Gemifloxacin which has shown potent activity against penicillin, macrolide and other quinolone resistant bacteria.6,7,8 could be of great importance in the treatment of urinary tract infections and other infections in this era of increasing antimicrobial resistance. This study evaluated the in vitro activity of gemifloxacin against clinical bacterial isolates and compared the activity with that of ciprofloxacin, ofloxacin and norfloxacin against the same isolates. MATERIALS AND METHODS Drugs and Chemicals The pure drugs which included gemifloxacin, ciprofloxacin, ofloxacin and norfloxacin were products of Sigma Aldrich Laborchemikallien, GmBH, Germany. They were in safe conditions for use whiles the microbiological media, nutrient agar, nutrient both and MacConkey agars were also products of Sigma Aldrich Laborchemikallien, GmBH, Germany. Clinical Bacterial Isolates Eight pathogenic bacteria were used. These included Staphylococcus aureus (Staph. aureus), Escherichia Coli (E. coli), Alcaligenes faecalis (A. faecalis), Pseudomonas aeruginosa (P. aeruginosa), Serratia marcescens (S. marcescens), Enterobacter aerogenes (E. aerogenes), Proteus vulgaris (P. vulgaris) and Klebseilla pneumoniae (K. pneumoniae). They were obtained from the University of Benin Teaching Hospital Medical Microbiology Laboratory stock Unit. They had been isolated from samples of patients for clinical diagnosis of their infections. They were authenticated using standard morphological and biochemical assays.9 in the Department of Pharmaceutical Microbiology, Faculty of Pharmacy, University of Benin. The bacterial isolates were maintained in nutrient agar slants and sub cultured at regular intervals to ensure their viability and purity. Preparation of Concentrations of drugs for Minimum Inhibitory Concentration (MIC) assays. From a stock solution of 1000 µg/ml of each of the drugs final concentrations of 5, 7.5, 10,15, 20, 25, and 30µg/ml in equivalent volumes of 0.1 ml, 0.15ml, 0.2ml, 0.3ml, 0.4, 0.5ml and 0.6ml respectively made up to 20 ml with nutrient agar were used for antibacterial assay. Preparation of inoculums The respective bacterial isolates from the nutrient agar slants were sub cultured in sterile nutrient broth and incubated at 370C overnight. The overnight nutrient broth culture was diluted serially to obtain 106CFU/ml and used after every fresh preparation. ANTIBACTERIAL ASSAY Minimum Inhibitory Concentrations (MIC) of the drugs The agar dilution method described by George and Robert was used.10 The minimum inhibitory concentrations of the drugs were evaluated using final concentrations of 5, 7.5, 10, 15, 20 and 30 mg/ml in equivalent volumes of 0.1ml, 0.15ml, 0.2ml, 0.3ml, 0.4, 0.5 and 0.6 ml respectively made up to 20 ml with nutrient agar. The minimum inhibitory concentrations were determined against Staphylococcus aureus, Escherichia Coli, Alcaligenes faecalis, Serratia marcescens, Enterobacter aerogenes, Klebseilla pneumoniae, Pseudomonas aeruginosa and Proteus vulgaris. Each concentration of each drug was in triplicate plates which were labelled accordingly with the clinical bacterial isolate. Each plate was inoculated with 0.1ml of 10 6 CFU/ml of overnight nutrient broth culture of the clinical bacterial isolate. The inoculums were spread uniformly on the surface of the agar with the aid of a sterile glass spreading rod. The plates were incubated at 37 oC and observed for growth after 24 hours. Evaluation of gemifloxacin antibacterial activity against the Clinical Isolates using Zones of Inhibition The agar well diffusion method as described by Perez et al. was used.11 The minimum inhibitory concentration (MIC) against each bacterium exhibited by gemifloxacin was used in the zones of inhibition assay. The zones of inhibition assay were evaluated against Staphylococcus aureus, Escherichia Coli, Alcaligenes faecalis, Serratia marcescens, Enterobacter aerogenes, Klebseilla pneumoniae, Pseudomonas aeruginosa and Proteus vulgaris. Petri dishes in triplicates were labelled with each of the clinical bacterial isolates and 20ml of nutrient agar pipetted into them aseptically. The nutrient agar was allowed to set and was inoculated with 0.1ml of 106 CFU/ml of an overnight culture of each of the clinical isolates, in separate petri dishes. The inoculums were spread uniformly on the surface of the agar with the aid of a sterile glass spreading rod. Using a sterile cork borer, wells of 6mm in diameter were made in the nutrient agar of each plate and labelled accordingly. In each of the wells, 0.2ml of each of gemifloxacin minimum inhibitory concentration against each bacterium was aseptically pipetted and labelled accordingly. The plates were left for a while for the drug to diffuse into the agar. The plates were incubated at 37 oC for 24 hours and examined for zones of inhibition around the wells. The zones of inhibition were measured and recorded. The mean and standard error of mean (Mean ± SEM) was determined for the triplicate plates in each case. RESULTS The results of the minimum inhibitory concentration assays of gemifloxacin, ciprofloxacin, ofloxacin and norfloxacin are presented in Tables 1, 2, 3 and 4. The MICs of gemifloxacin were 7.5µg/ml for Proteus vulgaris, 10µg/ml for Staph. aureus and Enterobacter aerogenes, 15µg/ml for E. coli, 20µg/ml for Pseudomonas aeruginosa, 25µg/ml for Klebsiella pneumonia and 30µg/ml for Alcaligenes faecalis and Serratia marcescens (Table 1). Table 1: Minimum inhibitory concentration (MIC) of gemifloxacin against the clinical bacteria isolates Clinical bacteria isolates Staphylococcus aureus Final concentrations in nutrient agar (µg/ml) 5.0 7.5 10.0 15.0 20.0 25.0 30.0 ++ + - Escherichia coli ++ ++ + - - - - Pseudomonas aeruginosa ++ + + + - - - Enterobacter aerogenes +++ ++ - - - - - + - - - - - - Alcaligenes faecalis +++ ++ ++ + + + - Serratia marcescens +++ ++ ++ + + + - Klebsiella pneumonia ++ ++ + + + - - Proteus vulgaris +++, heavy growth of colonies, ++, moderate growth of colonies, +, minimal growth and -, no growth of colonies The MICs of ciprofloxacin were 7.5µg/ml for Proteus vulgaris, 10µg/ml for Staph. aureus, 25µg/ml for E. coli and Pseudomonas aeruginosa, 30µg/ml for Enterobacter aerogenes, Klebsiella pneumonia, Alcaligenes faecalis and Serratia marcescens (Table 2). Table 2: Minimum inhibitory concentration (MIC) of ciprofloxacin against the clinical bacteria isolates Clinical bacteria isolates Staphylococcus aureus Final concentrations in nutrient agar (µg/ml) 5.0 7.5 10.0 15.0 20.0 25.0 30.0 ++ + - Escherichia coli +++ ++ ++ + + - - Pseudomonas aeruginosa +++ ++ ++ + + - - Enterobacter aerogenes +++ ++ ++ ++ + + - + - - - - - - Alcaligenes faecalis +++ +++ +++ ++ ++ + - Serratia marcescens +++ +++ ++ ++ ++ + - Klebsiella pneumonia +++ +++ ++ ++ ++ + - Proteus vulgaris +++, heavy growth of colonies, ++, moderate growth of colonies, +, minimal growth and -, no growth of colonies The MICs of ofloxacin were 7.5µg/ml for Pseudomonas aeruginosa and Proteus vulgaris, 10µg/ml for Staph. aureus, E. coli, Enterobacter aerogenes, Klebsiella pneumonia, Alcaligenes faecalis and Serratia marcescens (Table 3). Table 3: Minimum inhibitory concentration (MIC) of ofloxacin against the clinical bacteria isolates Clinical bacteria isolates Staphylococcus aureus Final concentrations in nutrient agar (µg/ml) 5.0 7.5 10.0 15.0 20.0 25.0 30.0 ++ + - Escherichia coli ++ + - - - - - Pseudomonas aeruginosa ++ - - - - - - Enterobacter aerogenes ++ + - - - - - Proteus vulgaris + - - - - - - Alcaligenes faecalis ++ + - - - - - Serratia marcescens ++ + - - - - - Klebsiella pneumonia ++ + - - - - - ++, moderate growth of colonies, +, minimal growth and -, no growth of colonies The MICs of norfloxacin were 10µg/ml for Proteus vulgaris, 30µg/ml for Staph. aureus, E. coli, Enterobacter aerogenes, Klebsiella pneumonia, Alcaligenes faecalis, Pseudomonas aeruginosa and Serratia marcescens (Table 4). Table 4: Minimum inhibitory concentration (MIC) of norfloxacin against the clinical bacteria isolates Clinical bacteria isolates Staphylococcus aureus Final concentrations in nutrient agar (µg/ml) 5.0 7.5 10.0 15.0 20.0 25.0 30.0 +++ ++ ++ ++ ++ + - Escherichia coli +++ +++ ++ ++ ++ ++ - Pseudomonas aeruginosa +++ +++ ++ ++ ++ ++ - Enterobacter aerogenes +++ +++ +++ +++ ++ ++ - Proteus vulgaris ++ + - - - - - Alcaligenes faecalis +++ +++ +++ ++ ++ ++ - Serratia marcescens +++ +++ +++ ++ ++ ++ - Klebsiella pneumonia +++ +++ +++ ++ ++ ++ - +++, heavy growth of colonies, ++, moderate growth of colonies, +, minimal growth and -, no growth of colonies In Table 5 is presented the MICs of gemifloxacin in comparison to ciprofloxacin, ofloxacin and norfloxacin. The results show that the clinical isolates were most sensitive to ofloxacin followed by gemifloxacin, ciprofloxacin and norfloxacin respectively (Table 5). Table 5: Minimum inhibitory concentration (MIC) values of gemifloxacin, ciprofloxacin, ofloxacin and norfloxacin against the clinical bacteria isolates Clinical bacteria isolates Staphylococcus aureus Minimum inhibitory concentration values (µg/ml) GEM CIP OFL NOR 10 10 10 30 Escherichia coli 15 25 10 30 Pseudomonas aeruginosa 20 25 10 30 Enterobacter aerogenes 10 30 7.5 30 Proteus vulgaris 7.5 7.5 10 10 Alcaligenes faecalis 30 30 7.5 30 Serratia marcescens 30 30 10 30 Klebsiella pneumonia 25 30 10 30 The zones of inhibition for gemifloxacin are show in Table 6. The zones of inhibition range from 17.0 ± 0.11mm to 42.0 ± 0.15mm for Enterobacter aerogenes and Serratia marcescens respectively (Table 6). Table 6: Antibacterial activity of gemifloxacin against clinical bacterial isolates using zones of inhibition Clinical bacteria isolates Staphylococcus aureus Zone of inhibition (mm) 17.5 ± 0.22 Escherichia coli 18.0 ± 0.30 Pseudomonas aeruginosa 32.5 ± 0.14 Enterobacter aerogenes 17.0 ± 0.11 Proteus vulgaris 25.0 ± 0.21 Alcaligenes faecalis 23.5 ± 0.23 Serratia marcescens 42.0 ± 0.15 Klebsiella pneumonia 37.0 ± 0.41 Zones of inhibition are Mean + SEM of measurements for triplicate plates. DISCUSSION The emergence of antibiotic resistance is on the increase and has become a global concern.12 Various efforts are being made to combat and cope with this menace which poses a serious problem to antimicrobial chemotherapy success. Current efforts are focused on the improvement of antimicrobial spectra of most antimicrobial agents. However, despite their improved activities, newer drugs still carry the risk of resistance selection, particularly Staphylococcus pathogens that have already intermediate resistance to antimicrobials.13 This is a clinical problem, especially with methicillin resistant Staphylococcus aureus (MRSA) isolates which are widely resistant to quinolones.13 Another possible approach to the problem could be to explore existing antimicrobial agents with broad spectra of activity for possible activity in infections for which they are not traditional indicated. Our study evaluated and compared the in-vitro antibacterial activity of gemifloxacin, a respiratory quinolone and other quinolones against clinical bacterial isolates of other infections. The bacterial isolates included Staphylococcus aureus, Escherichia coli, Alcaligenes faecalis, Serratia marcescens, Enterobacter aerogenes, Klebsiella pneumoniae, Pseudomonas aeruginosa and Proteus vulgaris. The results indicated marked invitro antibacterial activity against the isolates in the minimum inhibitory concentration assays. The MICs of the drugs evaluated ranged from 7.5µg/ml to 30µg/ml. The isolates were most sensitive to ofloxacin, a urinary tract infection quinolone, with a maximum MIC of 10µg/ml for most of the isolates tested followed by gemifloxacin. The MIC assays indicate that the isolates were least sensitive to norfloxacin with MIC of 30µg/ml for all the isolates compared to gemifloxacin and the other quinolones. The minimum inhibitory concentrations are important to confirm the resistance of microorganisms to an antimicrobial agent and also to monitor the activity of the new antimicrobial agents.14 That the drugs evaluated produced remarkable growth inhibitions at these concentrations suggest that they could be good candidates for infections against these isolates. Gemifloxacin in the zones of inhibition assays produced zones of inhibition for all the isolates tested. The largest zone of inhibition was observed for Serratia marcescens and the least for Enterobacter aerogenes. None of the isolates exhibited resistance to gemifloxacin. The zones of inhibition indicate the degree of susceptibility to the drugs. Gemifloxacin may have a place in the future, as an antibacterial agent in the treatment of infections caused by some of the isolates tested as is currently recommended mostly for respiratory tract infections. It can be concluded that the drugs evaluated in this study could be suitable candidates for treatment of infections caused by the isolates tested. However in vivo studies are required to ascertain the pharmacokinetics and Pharmacodynamics of the drugs in disease state. REFERENCES 1. Catherine M. Oliphant, Gary M and Green, M.D. Quinolones: A Comprehensive Review. American Family Physician, 2002; 65(3):455 - 465. 2. Owens, RC and Ambrose PG. Clinical use of the fluoroquinolones. Med Clin North Am, 2000; 84:1447–1469. 3. Donaldson, PM,Pallett, AP and Carroll, MP. Ciprofloxacin in general practice British Med Journal (Clinical Research Ed.), 1994; 308: 1437 – 1443 4. Monk JP and Campoli-Richards DM.. Ofloxacin: A review of its antibacterial activity ,pharmacokinetic properties and therapeutic uses. .Drugs, 1987; 33(4): 346 - 3491 5. Padeĭskaia, EN. Norfloxacin: more than 20 years of clinical use, the results and place among fluoroquinolones in modern chemotherapy for infections. Antibiot Khimioter, 2003; 48 (9): 28–36. 6. Jones RN and Pfaller, MA. In vitro activity of newer fluoroquinolones for respiratory tract infections and emerging patterns of antimicrobial resistance: data from the SENTRY antimicrobial surveillance program. Clinical Infectious Disease, 2000; 31:16 – 23. 7. McCloskey, L, Maore, T, Niconovich, N., Donald, B., Broskey, J., Jaklelasszek, Rettenhouse, S., and Coleman, K. In Vitro activity of gemifloxacin againsta broad range of recent clinical isolates from the USA. J. Antimicrobial Chemother, 2000; 45: 13 – 21. 8. Karageorgopoulos,DE, Giannopoulou, KP, Grammatikos, AP, Dimopoulos, G, and Falagas, ME. Fluoroquinolones compared with beta-lactam antibiotics for the treatment of acute bacterial sinusitis: a meta-analysis of randomized controlled trials. CMAJ, 2008; 178 (7): 845– 854. 9. Cheesbrough, M.. District Laboratory practice in Tropical Countries, Low price edition, Gambridge Univ. press, Gambridge, 2004; p. 63 – 70. 10. George ME and Robert CM. Antimicrobial combinations In: Antibiotics in medicine, 4th Ed. Victor,L. editor, Williams and Wilkens,1996; p. 334. 11. Perez C, Paul M and Bazerque P. Antibiotic assay by agar-well diffusion method. Acta Biol Med Exp, 1990; 15: 113 – 115. 12. Calva, JJ., Sifuentes-Osornio, J. and Ceron, C. Antimicrobial resistance in fecal flora: longitudinal community-based surveillance of children from urban Mexico. Antimicrob Agents Chemother, 1996; 40(1): 699-702. 13. Lau, SM, Peng MY and Chang, FY. Resistance rates to commonly used antimicrobials among pathogens of both bacteremic and non-bacteremic communityacquired urinary tract infection. Microbiol Immunol Infect, 2004; 37(3) :185-189. 14. Lau, SM, Peng MY and Chang, FY. Resistance rates to commonly used antimicrobials among pathogens of both bacteremic and non-bacteremic communityacquired urinary tract infection. Microbiol Immunol Infect, 2004; 37(3) :185-189.