Princip of internal medicine
advertisement

Module №2. Principles of internal medicine
Text test questions
1.What substances are reabsorbed in renal tubules completely?
A. *Aminoacids
B. Creatinine
C. Sodium
D. Potassium
E. Chlorum
2.What are the common findings of IgA nephropathy?
A. Heavy proteinurea
B. *Asymptomatic microscopic hematuria/proteinuria
C. White cells;
D. Isolated proteinurea
E. pyuria;
3.What are the common findings of IgA nephropathy?
A. Pyuria
B. Heavy proteinurea
C. White cells;
D. Isolated proteinurea
E. *Gross hematuria post exercise or viral illness
4.Acute course of glomerulonenhritis may occur on morphological case of
A. IgA nephropathy
B. minimal change disease
C. *Proliferative glomerulonephritis
D. Membranous nephropathy
E. Mesangioproliferative glomerulonephritis
5.Chronic course of glomerulonenhritis may occur on all morphological case except
A. IgA nephropathy
B. minimal change disease
C. *Proliferative glomerulonephritis
D. Membranous nephropathy
E. Mesangioproliferative glomerulonephritis
6.In case of IgA nephropathy the most appropriate treatment is
A. Corticosteroids
B. Cytotoxics
C. Antibiotics
D. *Memranostabilisative therapy
E. Plasmapheresis
7.In case of minimal change disease the most appropriate treatment is
A. *Corticosteroids
B. Cytotoxics
C. Antibiotics
D. Memranostabilisotion therapy
E. Plasmapheresis
8.What are the common findings of IgA nephropathy?
A. Heavy proteinurea
B. *Asymptomatic microscopic hematuria/proteinuria
C. White cells;
D. Isolated proteinurea
E. pyuria;
9.What are the common findings of IgA nephropathy?
A. Heavy proteinurea
B. White cells;
C. Isolated proteinurea
D. Pyuria
E. *Gross hematuria post exercise or viral illness
10. In case of acute poststreptococcal glomerulonephritisthe most appropriate treatment is
A. Corticosteroids
B. Cytotoxics
C. *Antibiotics, symptomatic treatment
D. Memranostabilisation therapy
E. Plasmapheresis
11. In case of Membranous nephropathy the most appropriate treatment is
A. Corticosteroids
B. *Cytotoxics
C. Antibiotics
D. Memranostabilisation therapy
E. Plasmapheresis
12. In case of nephrotic syndrome in diabetic nephropathy with normal renal function the most
appropriate treatment is
A. Corticosteroids
B. Cytotoxics
C. *Symptomatic treatment
D. Memranostabilisation therapy
E. Plasmapheresis
13. In case of nephrotic syndrome in diabetic nephropathy with ESRD the most appropriate treatment
is
A. Corticosteroids
B. Cytotoxics
C. symptomatic treatment
D. Memranostabilisotion therapy
E. *Renal replacement therapy
14. In case of resistant nephrotic syndrome in mesangiocapillary Glomerulonephritis the most
appropriate treatment is
A. Corticosteroids
B. Cytotoxics
C. symptomatic treatment
D. Memranostabilisotion therapy
E. *Plasmapheresis folowwed by corticosteroids
15. Nephrotic syndrome may occur in morphological case except
A. *IgA nephropathy
B. minimal change disease
C. Mesangiocapillary glomerulonephritis
D. Membranous nephropathe
E. Mesangioproliferative glomerulonephritis
16. Nephrotic syndrome may occur in morphological case of
A. minimal change disease
B. Mesangiocapillary glomerulonephritis
C. Membranous nephropathe
D. Mesangioproliferative glomerulonephritis
E. *All of them
17. Nephrotic syndrome may occur in morphological case of
A. minimal change disease
B. Proliferative glomerulonephritis
C. Membranous nephropathe
D. *All of them
E. None of them
18. Nephrotic syndrome may occur in morphological case except
A. Proliferative glomerulonephritis
B. *Pyelonephritis
C. Dibetic nephropathy
D. Amyloidosis
E. minimal change disease
19. The energy intake of diet in patients with nephritic syndrome is provided by increased
A. Increased content of Salt
B. Increased content of fats
C. Increased content of proteins
D. *Inceased content of carbohydrates
E. All of then
20. What percent of adult idiopathic nephrotic syndrome is caused by minimal change disease?
A. *20%
B. 30%
C. 40%
D. 50%
E. 10%
21. The common findings at presentation of focal segmental glomerulosclerosis are except
A. Nephrotic syndrome
B. Hypertension
C. Microscopic hematuria
D. Decreased GFR (30 ml/min)E. *Hyperfiltration
22. The mechanisms of proteinuria are except ?
A. Overflow of elevated normal or abnormal serum proteins
B. Decreased reabsorption of normal filtered proteins
C. Increased glomerular permeability
D. Changes in renal hemodyndamics
E. *Hypercoagubility
23. What is the most common form of idiopathic glomerulonephritis?
A. *IgA nephropathy
B. minimal change disease
C. Proliferative glomerulonephritis
D. Membranous nephropathe
E. Mesangioproliferative glomerulonephritis
24. What are common findings a presentation of RPGN expt?
A. Oligouria
B. Hypertension
C. Edema
D. Active sediment with erythrocytes and casts
E. *Isolated mild proteinurea
25. What is the most common cause of hematuria of glomerular origin?
A. *IgA nephropathy
B. minimal change disease
C. Proliferative glomerulonephritis
D. Membranous nephropathy
E. Mesangioproliferative glomerulonephritis
26. In IgA nephropathy, these patients commonly present with hematuria a few days after URI or GI
infection. What are the complement levels?
A. *Normal C4 and C3 levels
B. Increasedl C4 and C3 levels
C. Decreasedl C4 and C3 levels
D. Normal C1 and C2 levels
E. Increasedl C1 and C2 levels
27. Describe the FENA in the setting of glomerulonephritis?
A. *The FENA will be <1
B. The FENA will be <5
C. The FENA will be <3
D. The FENA will be <4
E. The FENA will be >2
28. Which RPGN is characterized by immune complex deposits?
A. *Type II RPGN
B. Type I RPGN
C. Type III RPGN
D. Type IV RPGN
E. All of them
29. What are common findings at presentation of membranous nephropathy?
A. Edema
B. Hypertension
C. Hypoalbuminemia
D. Normal GFR
E. *All of them
30. Describe the laboratory evaluation of complement in IgG and IgM mediated glomerulonephritis?
A. *low levels of C3 and C4
B. low levels of C1and C2
C. high levels of C3 and C4
D. high levels of C1 and C2
E. normal levels of C3 and C4
31. What is the most common etiology of nephrotic syndrome among Caucasians?
A. IgA nephropathy
B. minimal change disease
C. Proliferative glomerulonephritis
D. Membranous nephropathy
E. Mesangioproliferative glomerulonephritis
32. What is the most common underlying renal pathology of nephrotic syndrome in patients with solid
tumors?
A. IgA nephropathy
B. minimal change disease
C. Proliferative glomerulonephritis
D. Membranous glomerulopathy
E. *Mesangioproliferative glomerulonephritis
33. What are the common findings at presentation of acute glomerulonephritis?
A. Oliguria
B. Hypertension
C. Active urine sediment
D. Proteinuria which is rarely nephrotic range
E. *All of them
34. What is the specific target of the anti-GBM antibodies in Goodpasture's syndrome?
A. *The alpha-3 chian of type IV collagen
B. The alpha-3 chian of type I collagen
C. The alpha-3 chian of type II collagen
D. The alpha-3 chian of type III collagen
E. The alpha-4 chian of type IV collagen
35. What are causes of glomerulonephritis?
A. Post streptococcal
B. IgA nephropathy
C. Rapidly progressive glomerulonephritis
D. Crescentric glomerulonephritis
E. *All of them
36. What amount of proteinuria per day is indicative of nephrotic syndrome?
A. *Proteinuria of more than 3.5 grams/day
B. Proteinuria of more than 2.5 grams/day
C. Proteinuria of more than 1.5 grams/day
D. Proteinuria of more than 3.0 grams/day
E. Proteinuria of more than 2.0 grams/day
37. Describe important findings in post streptococcal glomerulonephritis following pharyngitis?
A. -20 day latent period
B. ASO >250 u/ml
C. Low C3
D. Following cutaneous strep infections there is a 14-21 day latent period and normal ASO titers
E. *All of them
38. What are six common etiologies of membranous nephropathies?
A. *Idiopathic, syphilis, Hepatitis B, SLE, gold salts, and malignancy
B. Idiopathic, chronic heart failure, Hepatitis B, SLE, gold salts, and malignancy
C. Idiopathic, syphilis, Hepatitis A, SLE, gold salts, and malignancy
D. Idiopathic, syphilis, Hepatitis B, SLE, NSAIDs, and malignancy
E. Idiopathic, syphilis, Hepatitis B, SLE, gold salts, and bronchial asthma
39. What is the most common etiology of nephrotic syndrome in African Americans?
A. Post streptococcal
B. IgA nephropathy
C. Rapidly progressive glomerulonephritis
D. Crescentric glomerulonephritis
E. *Focal segmental glomerulosclerosis
40. Which drugs should not be used in pregnancy.
A. *Fluoroquinolones;
B. Phospomycine;
C. Aminoglucosides;
D. macrocrystalline nitrofurantoin;
E. amoxicillin
41. The most common organism in acute bacterial pyelonephritis is
A. Klebsiella
B. Chlamydia
C. *E. Coli
D. Pseudomonas
E. Candida
42. Symptoms of acute pyelonephritis generally develop rapidly over a few hours or a day and may
include all of following except:
A. fever;
B. vomiting;
C. chills;
D. nausea;
E. *oedema
43. What is the most appropriate initial treatment for a patient with a nonobstructing radiolucent stone
in the right renal pelvis?
A. Hydrochlorothiazide
B. Low-sodium diet
C. Allopurinol
D. Oral sodium bicarbonate or potassium citrate
E. *Extracorporeal shock-wave lithotripsy
44. What percentage of the population will develop nephrolithiasis?
A. *1-5 %
B. 5-10 %
C. 10 -15 %
D. 30-50 %
E. 60-70 %
45. What are the signs and symptoms of hypercalcemia?
A. Stones
B. Bones
C. Abdominal groans
D. Psychiactric overtones
E. *All of them
46. What is the most common type of kidney stone?
A. *2/3 are calcium stones (calcium oxalate, calcium phosphate)
B. 2/3 are urate stones
C. 1/2 are mixed stones
D. 2/3 are phosphate stones
E. 2/3 are cholesterol stones
47. What is an autosomal dominant disease characterized by bilateral enlargement of kidneys
secondary to multiple large cysts. Patients present with hematuria, pain, hypertension, and progressive
renal failure. What is this disease?
A. *Adult polycystic kidney disease
B. Diabetic nephropathy
C. Alport’s syndrome
D. Goodpasture’s syndrome
E. Primary amuloidosis
48. Overflow proteinuria should be suspected in patients with clinical or laboratory evidence of:
A. multiple myeloma;
B. *pyelonephritis;
C. rheumatoid arthritis;
D. diabetic nephropathy;
E. drug-induced interstitial nephritis.
49. Nephrotic syndrome in adults occurs in these cases of:
A. minimal change disease (MCD),
B. focal and segmental glomerulosclerosis (FSGS),
C. membranous glomerulopathy,
D. *all of them;
E. one of the above.
50. The pathognomonic morphologic lesion in FSGS is sclerosis with hyalinosis involving portions
(segmental) of fewer than:
A. 10% (focal) of glomeruli on a tissue section;
B. 20% (focal) of glomeruli on a tissue section;
C. 30% (focal) of glomeruli on a tissue section;
D. *40% (focal) of glomeruli on a tissue section;
E. 50% (focal) of glomeruli on a tissue section.
51. Evaluation of the routine urine analysis includes everything except:
A. amount of the urine;
B. urine sediment;
C. transparence;
D. *the common diuresis;
E. reaction.
52. Idiopathic FSGS (Focal and Segmental Glomerulosclerosis) typically presents as nephrotic
syndrome (~66 %) or subnephrotic proteinuria (~33%) in association with
A. hypertension,
B. mild renal insufficiency,
C. abnormal urine sediment
D. *all of them;
E. none of the above.
53. Causes of Membranoproliferative (Mesangiocapillary) Glomerulonephritis (MPGN) associated
with chronic infections are all the following except:
A. Hepatitis B and C,
B. HIV,
C. bacterial endocarditis,
D. Leukemias,
E. *visceral abscess.
54. Causes of Membranoproliferative (Mesangiocapillary) Glomerulonephritis (MPGN) associated
with systemic immune-complex disease are:
A. systemic lupus erythematosus;
B. mixed cryoglobulinemia;
C. Sjogren's syndrome;
D. *all of them;
E. none of the above.
55. Most patients with type I MPGN present with all of the following except:
A. heavy proteinuria;
B. nephrotic syndrome;
C. *light proteinuria;
D. active urinary sediment;
E. normal or mildly impaired GFR.
56. Renal biopsy is particularly useful when clinical assessment and laboratory investigations suggest
diagnoses of all of following except:
A. glomerulonephritis,
B. hemolytic-uremic syndrome,
C. thrombotic thrombocytopenic purpura,
D. allergic interstitial nephritis.
E. *ischemic renal injury
57. Standard approach to screen for renovascular hypertension has following noninvasive techniques:
A. the captopril-enhanced radionuclide renal scan;
B. a duplex Doppler flow study;
C. magnetic resonance (MRI) angiography
D. *all of them;
E. none of the above.
58. The dipstick examination should includes everything except:
A. protein;
B. *creatinine;
C. glucose;
D. ketones;
E. bilirubin.
59. Microscopic examination should check for all of following except:
A. crystals;
B. cells;
C. casts;
D. infecting organisms;
E. *ketones.
60. Urinary examination according to Zimnitsky is needed for evaluation of all of following except:
A. the common diuresis;
B. daily urine;
C. *renal clearance;
D. night urine;
E. fluctuation of the specific gravity of urine in every portion.
61. Urinary examination according to Necheporenco determines:
A. amount of erythrocytes in 1 ml (or 1 L) of urine;
B. amount of leucocytes in 1 ml (or 1 L) of urine;
C. amount of casts in 1 ml (or 1 L) of urine
D. *all of them;
E. none of the above.
62. Which of the following antimicrobial therapies would be inappropriate and potentially harmful in a
patient receiving cyclosporine?
A. Amoxicillin-clavulanate
B. *Erythromycin
C. Cefuroxime axetil
D. Ciprofloxacin
E. Penicillin
63. Which is the most appropriate antihypertensive therapy for patient with glomerulonephritis?
A. Intensive lifestyle modification
B. Diuretic
C. Nondihydropyridine calcium channel blocker
D. *Angiotensin-converting enzyme inhibitor
E. Beta-blockers
64. What is the most appropriate method to evaluate this patients renal function?
A. Measure the serum creatinine
B. Perform 24-hour urine collection to assess creatinine and volume
C. Perform technetium-99m-diethylenetriam me pentaacetic acid renal flow scanning
D. Measure the fractional excretion of sodium
E. *Estimate by using a creatinine-based formula
65. What is the best test to evaluate the patients risk for diabetic nephropathy and cardiovascular
disease?
A. *Microalbumin-to-creatinine ratio
B. Serum protein electrophoresis
C. Urine amino acid levels
D. 24-hour urine total protein
E. Annual urine dipstick analysis
66. The indications for dialysis in renal failure are except?
A. Fluid overload
B. Refractory hyperkalemia
C. BUN > 130
D. Pericardial friction rub
E. *Hemorragi stroke
67. Hyperkalemia can be due to decreased GFR only if GFR is below level^
A. *GFR < 20 ml/min
B. GFR < 70 ml/min
C. GFR < 50 ml/min
D. GFR < 30 ml/min
E. GFR < 40 ml/min
68. What is the normal daily water losses in sweat?
A. *200-400 ml
B. 100-200 ml
C.
D.
E.
69.
A.
B.
C.
D.
E.
70.
A.
B.
C.
D.
E.
71.
A.
B.
C.
D.
E.
72.
A.
B.
C.
D.
E.
73.
A.
B.
C.
D.
E.
74.
A.
B.
C.
D.
E.
75.
A.
B.
C.
D.
E.
76.
A.
B.
C.
D.
E.
77.
A.
50-100 ml
150-200 ml
250-300 ml
Which analgesics are associated with analgesic nephropathy?
*Phenacitin and acetaminophen
Aspirin
Ibuprofen
Diclofenac
All of themd
What are the effects of hyperkalemia on the EKG?
Tent shaped T-waves
Decreased or absent p waves
Short QT interval
Widening QRS complex
*All of them
To delay onset of ESRD in patients with diabetic nephropathy, what are four clinical tactics?
Decrease BP to below 130/85
Use ACE inhibitors
Dietary protein restriction to 0.6-0.8 g/kg
Maintain strict glycemic control
*All of them
What is the most common cause of hypocalcemia?
*Chronic renal failure
Acute renal failure
Dietary restriction of calcium
Renal tubular acidosis
Nephrocalcinosis
What is the BUN to Creatinine ratio in patients with post-renal renal failure?
*Approximately >10 to 1
Approximately <10 to 1
Approximately >20 to 1
Approximately <2 to 1
Approximately 1 to 1
Findings that may be found in patients with chronic renal failure include all of following except:
anemia;
*hyperproteinemia;
hypercreatininemia;
radiologic evidence of renal osteodystrophy;
radiologic evidence of small scarred kidneys.
Characteristic ECG feature of hyperkalemia:
U waves
Narrow QRS complex
*Tall T waves
Sort PR interval
Pathologic Q wave
Absolute contraindication for recombinant erythropoietin prescription:
*Noncontrolled blood hypertension
uremic neuropathy
hypoparathyroidism
aseptic bone necrosis
carbohydrate disturbunces
What is the definition of oliguria?
Oliguria is <600 ml of urine per 24
B. *Oliguria is <400 ml of urine per 24
C. Oliguria is <800 ml of urine per 24 hours
D. Oliguria is is less than 100 ml urine per 24 hours
E. Oliguria is <500 ml of urine per 24
78. What is the definition of anuria?
A. anuria is less than 500 ml urine per 24 hours
B. anuria is less than 400 ml urine per 24 hours
C. anuria is less than 300 ml urine per 24 hours
D. anuria is less than 200 ml urine per 24 hours
E. *anuria is less than 100 ml urine per 24 hours
79. What is the definition of oliguria and anuria?
A. Oliguria is <600 ml of urine per 24 hours and anuria is less than 300 ml urine per 24 hours
B. Oliguria is <500 ml of urine per 24 hours and anuria is less than 200 ml urine per 24 hours
C. *Oliguria is <400 ml of urine per 24 hours and anuria is less than 100 ml urine per 24 hours
D. Oliguria is <650 ml of urine per 24 hours and anuria is less than 150 ml urine per 24 hours
E. Oliguria is <1000 ml of urine per 24 hours and anuria is less than 100 ml urine per 24 hours
80. What is the most common cause of intra-renal renal failure?
A. *Acute tubular necrosis
B. Hypovolemia;
C. Low cardiac output;
D. Renovascular obstruction;
E. Renal ischemia
81. What are the symptoms of hypernatremia?
A. Seizures
B. Confusion
C. Pulmonary or peripheral edema
D. Respiratory paralysis
E. *All of them
82. The symptoms of hypernatremia are all of the following except?
A. Seizures
B. Confusion
C. Pulmonary or peripheral edema
D. Respiratory paralysis
E. *Hypovolemia
83. Is there a difference in the effects of furosemide and thiazide diuretics on the calcium excretion by
the kidney?
A. *Yes, furosemide increase calcium excretion by the kidney and thiazide diuretics decrease calcium
excretion by the kidney
B. Yes, furosemide decrease calcium excretion by the kidney and thiazide diuretics increase calcium
excretion by the kidney
C. Yes, furosemide increase calcium excretion by the kidney and thiazide diuretics are neutral
D. Yes, thiazide diuretics decrease calcium excretion by the kidney
E. No, the difference is absent
84. What diuretics can cause worsening of hyperkaliemia in chronic renal failure patients
A. loop diuretics
B. thiazide diuretics
C. *aldoserone antagonists
D. all of them
E. none of them
85. In patients with pre-renal azotemia, would you expect the urine sodium to be increased or
decreased?
A. *The urine sodium in pre-renal azotemia is generally decreased <20
B. The urine sodium in pre-renal azotemia is generally increased >20
C. The urine sodium in pre-renal azotemia is normal
D. The urine sodium in pre-renal azotemia is generally decreased <40
E. The urine sodium in pre-renal azotemia is generally increased >40
86. What is the primary cause of volume overload in end stage renal disease?
A. *because of inablility of kidney to excrete sodium.
B. because of inablility of kidney to excrete potassium
C. because of inablility of kidney to excrete Magnesium
D. because of inablility of secondary hyperaldosteronism
E. none of them
87. Can cephalosporins affect the serum creatinine measurement?
A. No, Cephalosporins don”t affect the serum creatinine measurement?
B. *Cephalosporins can result in a false increase in the serum creatinine
C. Cephalosporins can result in a false decrease in the serum creatinine
D. Cephalosporins can result in a true increase in the serum creatinine
E. Cephalosporins can result in a true decrease in the serum creatinine
88. How quickly will the creatinine rise in the setting of complete renal failure?
A. *The creatinine will rise approximately 1-2 mg/dL per day
B. The creatinine will rise approximately 2-3 mg/dL per day
C. The creatinine will rise approximately 3-5 mg/dL per day
D. The creatinine will rise approximately 3-4 mg/dL per day
E. The creatinine wil not change
89. What are the classic urinary findings of acute tubular necrosis?
A. Hyaline casts
B. *Muddy brown granular casts
C. Fatty casts
D. Leucocyte casts
E. Erythrocte casts
90. What is the most likely diagnosis in a patient with positive Chvostek's and/or Trousseau's sign and
leg cramps?
A. *Hypocalcemia
B. Hypopotassemia
C. Hypophosphatemia
D. Hypermagnesiemia
E. Hypercalcemia
91. What are the common EKG changes seen in hypomagnesemia?
A. Prolonged PR or QT intervals,
B. T-wave flattening or inversion
C. ST straightening
D. *All of them
E. None of them
92. When metabolic alkalosis occurs because of volume contraction, how does the serum chloride
typically respond?
A. *The urinary chloride is typically low (<10 meq/L)
B. The urinary chloride is typically low (<20 meq/L)
C. The urinary chloride is typically high (>10 meq/L)
D. The urinary chloride is typically high (>20 meq/L)
E. The urinary chloride is typically normal
93. Ccommon findings in autosomal dominant polycystic kidney disease are except?
A. Flank or back pain
B. gross hematuria
C. abdominal mass
D. frequent UTI's
E. *nephrotic synrome
94. Common findings in autosomal dominant polycystic kidney disease are ?
A. Flank or back pain
B. gross hematuria
C. abdominal mass
D. frequent UTI's
E. *All of them
95. What are 6 common findings in autosomal dominant polycystic kidney disease?
A. *Flank or back pain, gross hematuria, abdominal mass, frequent UTI's, hypertension, and
nephrolithiasis
B. Flank or back pain, gross hematuria, small kidneys, frequent UTI's, hypertension, and
nephrolithiasis
C. Flank or back pain, gross hematuria, abdominal mass, nephritic syndrome, hypertension, and
nephrolithiasis
D. Flank or back pain, gross hematuria, abdominal mass, frequent UTI's, hypotension, and
nephrolithiasis
E. None of them
96. What are common findings in autosomal dominant polycystic kidney disease?
A. gross hematuria,
B. frequent UTI's,
C. arterial hypertension,
D. nephrolithiasis
E. *all of them
97. In a patient with hypercalciuric nephrolithiasis, which of the following is associated with increased
risk for stone formation?
A. Low-sodium diet
B. *Low-calcium diet
C. Low-oxalate diet
D. Low-protein diet
E. Low-purine diet
98. Can dobutamine affect the serum creatinine measurement?
A. *Dobutamine can falsely decrease the serum creatinine
B. Dobutamine can falsely increase the serum creatinine
C. Dobutamine don’t interfere the serum creatinine
D. Dobutamine can true decrease the serum creatinine
E. None of them
99. What is the normal daily water losses in urine?
A. 2.0-2.5 liters
B. *1.2-1.5 liters
C. 0.5-1.0 liters
D. 2.2-3.5 liters
E. 0.8-1.2 liters
100. Complications of long-term dialysis include all the following EXCEPT
A. *Increased risk of gastrointestinal malignancy
B. myocardial infarction
C. carpal tunnel syndrome
D. protein-calorie malnutrition
E. high-output congestive heart failure
101. In patients with chronic renal failure, all the following are important contributors to bone disease
EXCEPT
A. impaired renal production of 1,25-dihydroxyvitamin D3
B. hyperphosphatemia
C. aluminum-containing antacids
D. *loss of vitamin D and calcium via dialysis
E. metabolic acidosis
102. Why is hypomagnesemia associated with hypocalcemia?
A. Hypomagnesemia causes a shift of calcium into bone
B. *Hypomagnesemia inhibits the secretion and action of parathyroid hormone
C. Hypomagnesemia causes renal calcium wasting
D. Hypomagnesemia impairs the peripheral actions of vitamin
E. None of them
103. What is the most common cause of death in patients with acute tubular necrosis?
A. Hypophosphatemia
B. Hypermagnesiemia
C. Hypercalcemia
D. *Hyperkalemia
E. Hypocalcemia
104. What is the effect of lithium on the kidney?
A. *Lithium can result in a nephrogenic diabetes insipidus
B. Lithium can result in a diabetes mellitus
C. Lithium can result in a a acute tubular necrosis
D. Lithium can result in a toxic ebcephalopathy
E. Lithium can result in anemia
105. What are the findings of methanol ingestion?
A. Systemic acidosis
B. Direct neurotoxicity (secondary to the metabolites formic acid and formaldehyde)
C. Direct hepatotoxicity
D. *All of them
E. None of them
106. What are the steps to treating myoglobinuria?
A. Volume repletion with IVF
B. Mannitol diuresis
C. Alkalinize urine with IV bicarbonate
D. *All of them
E. None of them
107. List three signs on physical exam of hyperkalemia?
A. Decreased DTR's
B. Weakness
C. Respiratory failure
D. *All of them
E. None of them
108. What conditions result in a the fractional excretion of sodium (FENA) of <1%?
A. Prerenal azotemia,
B. acute glomerulonephritis,
C. hepatorenal syndrome,
D. renal transplant rejection
E. *All of them
109. What is the effect of hypercalcemia on the heart?
A. Short or absent ST segment
B. Decreased QT interval
C. Tachicardia
D. *All of them
E. None of them
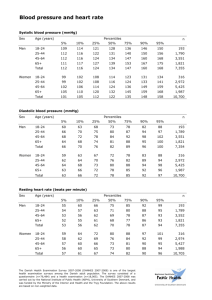
110. What is stage I hypertension?
A. *Stage I hypertension is characterized by a SBP of 140-159 or a DBP of 90-99 averaged from 2 or
more readings on two or more occassions
B. Stage I hypertension is characterized by a SBP of 120-139 or a DBP of 80-85 averaged from 2 or
more readings on two or more occassions
C. Stage I hypertension is characterized by a SBP of 150-159 or a DBP of 90-99 averaged from 2 or
more readings on two or more occassions
D. Stage I hypertension is characterized by a SBP of 160-179 or a DBP of 100-110 averaged from 2 or
more readings on two or more occassions
E. Stage I hypertension is characterized by a SBP of 130-159 or a DBP of 90-95 averaged from 2 or
more readings on two or more occassions
111. What are common findings associated with analgesic nephropathy?
A. Nocturia,
B. polyuria,
C. sterile pyuria,
D. predisposition to volume depletion,
E. *all of them
112. What are common findings associated with analgesic nephropathy?
A. renal colic,
B. hematuria,
C. hypertension
D. polyuria
E. *all of them
113. What are the most common causes of acute tubular necrosis?
A. *ischemia or toxic injury
B. Acute glomerulonephritis
C. Acute pyelonephritis
D. All of them
E. None of them
114. Which type of kidney stone is associated with urinary tract infections, particularly with urease
producing bacteria such as proteus, pseudomonas, and staphylococcus)?
A. *Struvite stones (staghorn calculi)
B. Urate stones
C. Oxalate stones
D. Phoaphate stones
E. Cholesterol stones
115. The common findings at presentation of focal segmental glomerulosclerosis are except
A. Nephrotic syndrome
B. Hypertension
C. Microscopic hematuria
D. Decreased GFR (30 ml/min)E. *All of them
116. What is the most common cause of hypokalemia?
A. *Diuretics
B. Chronic renal failure
C. Acute renal failure
D. Interstitial nephritis
E. Pyelonephritis
117. Name one drug commonly associated with distal renal tubule acidosis?
A. *Amphotericin B
B. Erythromycine
C. Sulphanilamides
D. NSAID’s
E. Diuretics
118. What underlying diagnosis is suggested in a patient with acute renal failure and white blood cells or
white blood cell casts?
A. *Interstitial nephritis
B. Glomerulonephritis
C. Pyelonephritis
D. Renal stones
E. Amyloidosis
119. What are the findings of nephritic syndrome on urinanalysis?
A. *RBC casts and hematuria
B. WBS casts and pyuria
C. Isolated proteinuria
D. Hematuria and pyuria
E. No pathological findings
120. What underlying diagnosis is suggested in a patient with acute renal failure and red blood cell casts
in the urine?
A. Interstitial nephritis
B. *Glomerulonephritis
C. Pyelonephritis
D. Renal stones
E. Amyloidosis
121. Methods of renal replacement therapy are:
A. Hemodialysis
B. Peritoneal dialysis
C. Kidney transplantation
D. *All of them
E. None of them
122. Methods of renal replacement therapy are except:
A. Hemodialysis
B. Peritoneal dialysis
C. Kidney transplantation
D. *Hemosorbtion
E. All of them
123. Methods of renal replacement therapy are except:
A. *Hemofiltration
B. Hemodialysis
C. Peritoneal dialysis
D. Kidney transplantation
E. All of them
124. Methods of renal replacement therapy are:
A. Hemofiltration
B. Hemosorbtion
C. Plasmapheresis
D. All of them
E. *None of them
125. Methods of renal replacement therapy are:
A. Hemofiltration
B. Hemosorbtion
C. Plasmapheresis
D. *Hemodialysis
E. All of them
126. How many nephrons are there in each kidney?
A. 100 – 200 thousands
B. 200 – 300 thousands
C. 500 – 700 thousands
D. *1,2 – 1,5 millions
E. 2 – 3 millions
127.
A.
B.
C.
D.
E.
128.
A.
B.
C.
D.
E.
129.
A.
B.
C.
D.
E.
130.
A.
B.
C.
D.
E.
131.
A.
B.
C.
D.
E.
132.
A.
B.
C.
D.
E.
133.
A.
B.
C.
D.
E.
134.
A.
B.
C.
D.
E.
135.
A.
B.
C.
D.
What does “kidney hyperplasia” mean?
*Congenital decrease of kidney sizes
Congenital increase of kidney sizes
Congenital cystic transformation of kidneys
Congenital tubular disorders of kidneys
Congenital glomerular disorders of kidneys
Describe the characteristics of iuxtaglomerulonephrones:
Presence of secondary capillary network
Greater diameter of efferent arterioles compared to afferent
Rennin production
*All of them
None of them
The characteristics of cortex nephrones include:
Presence of secondary capillary network
Greater diameter of efferent arterioles compared to afferent
Rennin production
All of them
*None of them
The kidney functions are:
Maintains of fluid load in body
Maintains of constant osmotic pressure plasma
Maintains of constant electrolyte balance
Maintains of blood acidity
*All of them
The kidney functions are except:
Hormone production
Maintains of constant osmotic pressure plasma
Maintains of constant electrolyte balance
Maintains of blood acidity
*Synthesis of urea and creatinine
The indices used to evaluate renal function are
Glomerular filtration rate
Plasma Creatinine level
Plasma Urea level
All of them
None of them
The indices used to evaluate renal function are except
Glomerular filtration rate
Plasma Creatinine level
Plasma Urea level
Zimnitsky test
*Nechiporenko test
Describe the characteristics of cortex nephrones:
Absence of secondary capillary network
Greater diameter of afferent arterioles compared to efferent
Cortex localization
*All of them
None of them
Normal levels of Glomerular filtration rate (GFR) are
140-190 ml/min
*90-120 ml/min
60-90 ml/min
30-60 ml/min
E.
136.
A.
B.
C.
D.
E.
137.
A.
B.
C.
D.
E.
138.
A.
B.
C.
D.
E.
139.
A.
B.
C.
D.
E.
140.
A.
B.
C.
D.
E.
141.
A.
B.
C.
D.
E.
142.
A.
B.
C.
D.
E.
143.
A.
B.
C.
D.
E.
144.
A.
B.
C.
90-190 ml/min
Processes of ultrafiltration in kidneys are stopped when systemic arterial blood pressure is ;
*<60 mm Hg
140 -160 mm Hg
120 -140 mm Hg
90 -100 mm Hg
70 -80 mm Hg
Normal levels of tubular water reabsorbing are
*97-99 %
95-96 %
93-94 %
90-92 %
87-90 %
Normal sizes of kidneys in adults are
*10-12 сm х 5-6 сm х 3-4 сm
15-16 сm х 7-8 сm х 5-6 сm
7-8 сm х 3-4 сm х 2-3 сm
5-7 сm х 2-4 сm х 1-3 сm
18-22 сm х 8-10 сm х 6-7 сm
What kidney cells have endocrine function?
Gumptreht’s cells
Juxtaglomerular cells
Interstitial cells
None of them
*All of them
Kidney cells have endocrine function except
Gumptreht’s cells
Juxtaglomerular cells
Interstitial cells
*Epithelial cells of distal tubuls
All of them
Anomalies of kidneys topic and shape are
Kidneys dystopia
L-like kinnney
C-like kidney
*All of them
None of them
Anomalies of kidneys topic and shape are except:
Kidneys dystopia
L-like kidney
C-like kidney
All of them
*Polycystic kidney
Anomalies of kidneys structure are:
Kidneys dystopia
L-like kinnney
C-like kidney
All of them
*None of them
Anomalies of kidneys structure are:
Polycystic kidney
Multicystic kidney
Megacalix
D.
E.
145.
A.
B.
C.
D.
E.
146.
A.
B.
C.
D.
E.
147.
A.
B.
C.
D.
E.
148.
A.
B.
C.
D.
E.
149.
A.
B.
C.
D.
E.
150.
A.
B.
C.
D.
E.
151.
A.
B.
C.
D.
E.
152.
A.
B.
C.
D.
E.
153.
A.
B.
*All of them
None of them
What kidney structures are visible on longitudinal incision
Cortex
Pelvis
Cerebral part
Calices
*All of them
What kidney structures are visible on longitudinal incision?
*Cortex, pelvis, cerebral part, calices
Cortex, cerebral part, calices
Cortex, pelvis, calices
Cortex, pelvis, cerebral part
Pelvis, cerebral part, calices
The structure of nephron includes:
Glomerulus
Glomerulus’s capsule
Renal tubules
*All of them
None of them
The most common organism in acute bacterial pyelonephritis is
Klebsiella
Chlamydia
*E coli
Pseudomonas
Candida
What is the definition of hematuria?
*Greater than 3-5 red cells per high power field
Greater than 0-1 red cells per high power field
Greater than 1-2 red cells per high power field
Greater than 2-3 red cells per high power field
Greater than 1-4 red cells per high power field
The risk factors for poor neurological outcome include
diuretic-induced hyponatremia,
malnutrition,
liver disease,alcoholism,
female gender
*All of them
What are the mechanisms of proteinuria?
Overflow of elevated normal or abnormal serum proteins
Decreased reabsorption of normal filtered proteins
Increased glomerular permeability
Changes in renal hemodyndamics
*All of them
How many nephrons are there in each kidney?
100 – 200 thousands
200 – 300 thousands
500 – 700 thousands
*1,2 – 1,5 millions
2 – 3 millions
What does “kidney hyperplasia” mean?
*Congenital decrease of kidney sizes
Congenital increase of kidney sizes
C.
D.
E.
154.
A.
B.
C.
D.
E.
155.
A.
B.
C.
D.
E.
156.
A.
B.
C.
D.
E.
157.
A.
B.
C.
D.
E.
158.
A.
B.
C.
D.
E.
159.
A.
B.
C.
D.
E.
160.
A.
B.
C.
D.
E.
161.
A.
B.
C.
D.
E.
162.
A.
Congenital cystic transformation of kidneys
Congenital tubular disorders of kidneys
Congenital glomerular disorders of kidneys
Describe the characteristics of cortex nephrones:
Absence of secondary capillary network
Greater diameter of afferent arterioles compared to efferent
Cortex localization
*All of them
None of them
Describe the characteristics of iuxtaglomerulonephrones:
Presence of secondary capillary network
Greater diameter of efferent arterioles compared to afferent
Rennin production
*All of them
None of them
The characteristics of cortex nephrones include:
Presence of secondary capillary network
Greater diameter of efferent arterioles compared to afferent
Rennin production
All of them
*None of them
The kidney functions are:
Maintains of fluid load in body
Maintains of constant osmotic pressure plasma
Maintains of constant electrolyte balance
Maintains of blood acidity
*All of them
The kidney functions are except:
Hormone production
Maintains of constant osmotic pressure plasma
Maintains of constant electrolyte balance
Maintains of blood acidity
*Synthesis of urea and creatinine
The indices used to evaluate renal function are
*Glomerular filtration rate
Plasma Creatinine level
Plasma Urea level
All of them
None of them
The indices used to evaluate renal function are except
Glomerular filtration rate
Plasma Creatinine level
Plasma Urea level
Zimnitsky test
*Nechiporenko test
Normal levels of Glomerular filtration rate (GFR) are
140-190 ml/min
*90-120 ml/min
60-90 ml/min
30-60 ml/min
90-190 ml/min
Processes of ultrafiltration in kidneys are stopped when systemic arterial blood pressure is ;
140 -160 mm Hg
B.
C.
D.
E.
163.
A.
B.
C.
D.
E.
164.
A.
B.
C.
D.
E.
165.
A.
B.
C.
D.
E.
166.
A.
B.
C.
D.
E.
167.
A.
B.
C.
D.
E.
168.
A.
B.
C.
D.
E.
169.
A.
B.
C.
D.
E.
170.
A.
B.
C.
D.
E.
171.
120 -140 mm Hg
90 -100 mm Hg
70 -80 mm Hg
*<60 mm Hg
Normal levels of tubular water reabsorbing are
*97-99 %
95-96 %
93-94 %
90-92 %
87-90 %
Normal sizes of kidneys in adults are
*10-12 сm х 5-6 сm х 3-4 сm
15-16 сm х 7-8 сm х 5-6 сm
7-8 сm х 3-4 сm х 2-3 сm
5-7 сm х 2-4 сm х 1-3 сm
18-22 сm х 8-10 сm х 6-7 сm
What kidney cells have endocrine function?
Gumptreht’s cells
Juxtaglomerular cells
Interstitial cells
None of them
*All of them
Kidney cells have endocrine function except
Gumptreht’s cells
Juxtaglomerular cells
Interstitial cells
*Epithelial cells of distal tubuls
All of them
Anomalies of kidneys topic and shape are
Kidneys dystopia
L-like kinnney
C-like kidney
*All of them
None of them
Anomalies of kidneys topic and shape are except:
Kidneys dystopia
L-like kidney
C-like kidney
All of them
*Polycystic kidney
Anomalies of kidneys structure are:
Kidneys dystopia
L-like kinnney
C-like kidney
All of them
*None of them
Anomalies of kidneys structure are:
Polycystic kidney
Multicystic kidney
Megacalix
*All of them
None of them
What kidney structures are visible on longitudinal incision
A.
B.
C.
D.
E.
172.
A.
B.
C.
D.
E.
173.
A.
B.
C.
D.
E.
174.
A.
B.
C.
D.
E.
175.
A.
B.
C.
D.
E.
176.
A.
B.
C.
D.
E.
177.
A.
B.
C.
D.
E.
178.
A.
B.
C.
D.
E.
179.
A.
B.
C.
D.
E.
Cortex
Pelvis
Cerebral part
Calices
*All of them
What kidney structures are visible on longitudinal incision?
*Cortex, pelvis, cerebral part, calices
Cortex, cerebral part, calices
Cortex, pelvis, calices
Cortex, pelvis, cerebral part
Pelvis, cerebral part, calices
The structure of nephron includes:
Glomerulus
Glomerulus’s capsule
Renal tubules
*All of them
None of them
The nephrotic syndrome is characterized by all of following except:
А heavy proteinuria;
hypoproteinaemia;
light proteinuria;
hyperproteinaemia;
generalized oedema.
Acute nephritic syndrome is characterized by sudden onset of all of following except:
acute renal failure ;
oliguria (<400 mL of urine per day);
hematuria;
hypertension;
*Proteinuria more3.5 g per 24 h.
Urinary tract infection has all of the following clues to diagnosis except:
Bacteriuria more 105 colonies per millilitre;
Pyuria;
Bladder tenderness;
*signs of renal osteodystrophy
urinary frequency.
Major causes of prerenal acute renal failure are all of the following except:
Hypovolemia;
Low cardiac output;
Renovascular obstruction;
*Hyperviscosity syndrome;
Altered renal systemic vascular resistance ratio.
Findings that suggest chronic renal failure include all of following except:
anemia;
*neuropathy;
rise in blood creatinine levels;
radiologic evidence of renal osteodystrophy;
radiologic evidence of small scarred kidneys.
ARF in association with:
oliguria,
hypertension,
an "active" urine sediment (nephritic syndrome);
*all of them;
none of the above.
180. ARF in association with fever, arthralgias, and a pruritic erythematous rash following exposure to a
new drug suggest:
A. vasculitis;
B. *allergic interstitial nephritis;
C. hemolytic-uremic syndrome;
D. thrombotic thrombocytopenic purpura;
E. glomerulonephritis.
181. White cell casts and nonpigmented granular casts suggest;
A. *pyelonephritis;
B. vasculitis;
C. thrombotic thrombocytopenic purpura;
D. glomerulonephritis;
E. amyloidosis.
182. Eosinophiluria (>5% of urine leukocytes) is a common finding (~90%) in:
A. *allergic interstitial nephritis induced by NSAIDs;
B. antibiotic-induced allergic interstitial nephritis;
C. thrombotic thrombocytopenic purpura;
D. amyloidosis;
E. glomerulonephritis.
183. Heavy proteinuria is a frequent finding in patients who develop combined allergic interstitial
nephritis and minimal change glomerulopathy when treated with:
A. *NSAIDs;
B. echinaceae;
C. heparinotherapy;
D. platelet aggregation inhibitor;
E. angiotensin-converting enzyme (ACE) inhibitors.
184. Renal biopsy is particularly useful when clinical assessment and laboratory investigations suggest
diagnoses of all of following except:
A. glomerulonephritis,
B. hemolytic-uremic syndrome,
C. thrombotic thrombocytopenic purpura,
D. allergic interstitial nephritis.
E. *ischemic renal injury
185. Standard approach to screen for renovascular hypertension has following noninvasive techniques:
A. the captopril-enhanced radionuclide renal scan;
B. a duplex Doppler flow study;
C. magnetic resonance (MRI) angiography
D. *all of them;
E. none of the above.
186. Evaluation of the routine urine analysis includes everything exept:
A. amount of the urine;
B. urine sediment;
C. transparence;
D. *the common diuresis;
E. reaction.
187. The dipstick examination should includes everything exept:
A. protein;
B. *creatinine;
C. glucose;
D. ketones;
E. bilirubin.
188. Microscopic examination should check for all of following except:
A. crystals;
B. cells;
C. casts;
D. infecting organisms;
E. *ketones.
189. Urinary examination according to Zimnitsky is needed for evaluation of all of following except:
A. the common diuresis;
B. daily urine;
C. *renal clearance;
D. night urine;
E. fluctuation of the specific gravity of urine in every portion.
190. Urinary examination according to Necheporenco determines:
A. amount of erythrocytes in 1 ml (or 1 L) of urine;
B. amount of leucocytes in 1 ml (or 1 L) of urine;
C. amount of casts in 1 ml (or 1 L) of urine
D. *all of them;
E. none of the above.
191. Specific indications to renal biopsy are all of following except:
A. adult nephritic syndrome
B. *uncontrolled hypertension
C. persistent proteinuria > 1 g/24 hours
D. adult acute nephritic syndrome
E. systemic diseases with renal involvement
192. Microscopic examination of urine in pyelonephritis reveals all of the following except:
A. numerous pus cells;
B. microorganisms;
C. *fatty casts;
D. some red cells;
E. some epithelial cells.
193. The nephrotic syndrome is a clinical complex characterized by a number of renal and extrarenal
features, the most prominent of which are:
A. proteinuria of >3.5 g (per 24 h);
B. hypoalbuminemia;
C. edema;
D. hyperlipidemia;
E. *all of them.
194. Low serum complement levels would be seen in patients with hematuria, proteinuria, and
hypertension resulting from all of the following EXCEPT
A. mixed essential cryoglobulinemia
B. hepatitis C-associated membranoproliferative glomerulonephritis
C. diffuse proliferative lupus nephritis
D. *Henoch-Schonlein purpura
E. poststreptococcal (or postinfectious) glomerulonephritis
195. Nephrotic syndrome is the hallmark of all the following. primary kidney diseases EXCEPT
A. membranous glomerulopathy
B. focal segmental glomerulosclerosis
C. minimal-change disease
D. *IgA nephropathy (Berger's disease)
E. HIV-associated nephropathy with or without
196. The presence of leucocyte casts is diagnostic of:
A. glomerular bleeding;
B. glomerulonephritis:
C. *pyelonephritis;
D. amyloidosis;
E.
197.
A.
B.
C.
D.
E.
198.
A.
B.
C.
D.
E.
199.
A.
B.
C.
D.
E.
200.
A.
B.
C.
D.
E.
201.
A.
B.
C.
D.
E.
202.
A.
B.
C.
D.
E.
203.
A.
B.
C.
D.
E.
204.
A.
B.
C.
D.
E.
205.
A.
B.
C.
deep vein thrombosis
Specific indications to renal biopsy are all of following except:
adult nephritic syndrome
*acute pyelonephritis
persistent proteinuria > 1 g/24 hours
adult acute nephritic syndrome
systemic diseases with renal involvement
Which of the following studies would you choose to confirm amiloidosis?
Intravenous pyelography
Ultrasonography
*Renal biopsy
Computed tomography
Renal flow scanning
Morphological forms of glomerulonephritis are exept:
minimal change disease (MCD),
focal and segmental glomerulosclerosis (FSGS),
membranous glomerulopathy,
proliferative glomerulonephritis;
masngioinflammatory glomerulonephritis
What is the definition of hematuria?
*Greater than 3-5 red cells per high power field
Greater than 0-1 red cells per high power field
Greater than 1-2 red cells per high power field
Greater than 2-3 red cells per high power field
Greater than 1-4 red cells per high power field
The risk factors for poor neurological outcome include
diuretic-induced hyponatremia,
malnutrition,
liver disease,alcoholism,
female gender
*All of them
What are the mechanisms of proteinuria?
Overflow of elevated normal or abnormal serum proteins
Decreased reabsorption of normal filtered proteins
Increased glomerular permeability
Changes in renal hemodyndamics
*All of them
How many nephrons are there in each kidney?
100 – 200 thousands
200 – 300 thousands
500 – 700 thousands
*1,2 – 1,5 millions
2 – 3 millions
What does “kidney hyperplasia” mean?
*Congenital decrease of kidney sizes
Congenital increase of kidney sizes
Congenital cystic transformation of kidneys
Congenital tubular disorders of kidneys
Congenital glomerular disorders of kidneys
Describe the characteristics of cortex nephrones:
Absence of secondary capillary network
Greater diameter of afferent arterioles compared to efferent
Cortex localization
D.
E.
206.
A.
B.
C.
D.
E.
207.
A.
B.
C.
D.
E.
208.
A.
B.
C.
D.
E.
209.
A.
B.
C.
D.
E.
210.
A.
B.
C.
D.
E.
211.
A.
B.
C.
D.
E.
212.
A.
B.
C.
D.
E.
213.
A.
B.
C.
D.
E.
214.
A.
B.
*All of them
None of them
Describe the characteristics of iuxtaglomerulonephrones:
Presence of secondary capillary network
Greater diameter of efferent arterioles compared to afferent
Rennin production
*All of them
None of them
The characteristics of cortex nephrones include:
Presence of secondary capillary network
Greater diameter of efferent arterioles compared to afferent
Rennin production
All of them
*None of them
The kidney functions are:
Maintains of fluid load in body
Maintains of constant osmotic pressure plasma
Maintains of constant electrolyte balance
Maintains of blood acidity
*All of them
The kidney functions are except:
Hormone production
Maintains of constant osmotic pressure plasma
Maintains of constant electrolyte balance
Maintains of blood acidity
*Synthesis of urea and creatinine
The indices used to evaluate renal function are
Glomerular filtration rate
Plasma Creatinine level
Plasma Urea level
*All of them
None of them
The indices used to evaluate renal function are except
Glomerular filtration rate
Plasma Creatinine level
Plasma Urea level
Zimnitsky test
*Nechiporenko test
Normal levels of Glomerular filtration rate (GFR) are
140-190 ml/min
*90-120 ml/min
60-90 ml/min
30-60 ml/min
90-190 ml/min
Processes of ultrafiltration in kidneys are stopped when systemic arterial blood pressure is ;
140 -160 mm Hg
120 -140 mm Hg
90 -100 mm Hg
70 -80 mm Hg
*<60 mm Hg
Normal levels of tubular water reabsorbing are
*97-99 %
95-96 %
C.
D.
E.
215.
A.
B.
C.
D.
E.
216.
A.
B.
C.
D.
E.
217.
A.
B.
C.
D.
E.
218.
A.
B.
C.
D.
E.
219.
A.
B.
C.
D.
E.
220.
A.
B.
C.
D.
E.
221.
A.
B.
C.
D.
E.
222.
A.
B.
C.
D.
E.
223.
A.
93-94 %
90-92 %
87-90 %
Normal sizes of kidneys in adults are
*10-12 сm х 5-6 сm х 3-4 сm
15-16 сm х 7-8 сm х 5-6 сm
7-8 сm х 3-4 сm х 2-3 сm
5-7 сm х 2-4 сm х 1-3 сm
18-22 сm х 8-10 сm х 6-7 сm
What kidney cells have endocrine function?
Gumptreht’s cells
Juxtaglomerular cells
Interstitial cells
None of them
*All of them
Kidney cells have endocrine function except
Gumptreht’s cells
Juxtaglomerular cells
Interstitial cells
*Epithelial cells of distal tubuls
All of them
Anomalies of kidneys topic and shape are
Kidneys dystopia
L-like kinnney
C-like kidney
*All of them
None of them
Anomalies of kidneys topic and shape are except:
Kidneys dystopia
L-like kidney
C-like kidney
All of them
*Polycystic kidney
Anomalies of kidneys structure are:
Kidneys dystopia
L-like kinnney
C-like kidney
All of them
*None of them
Anomalies of kidneys structure are:
Polycystic kidney
Multicystic kidney
Megacalix
*All of them
None of them
What kidney structures are visible on longitudinal incision
Cortex
Pelvis
Cerebral part
Calices
*All of them
What kidney structures are visible on longitudinal incision?
*Cortex, pelvis, cerebral part, calices
B. Cortex, cerebral part, calices
C. Cortex, pelvis, calices
D. Cortex, pelvis, cerebral part
E. Pelvis, cerebral part, calices
224. The structure of nephron includes:
A. Glomerulus
B. Glomerulus’s capsule
C. Renal tubules
D. *All of them
E. None of them
225. Complications of nephrotic syndrome that may require treatment include
A. edema,
B. hyperlipidemia,
C. thromboembolism,
D. vitamin D deficiency
E. *all of them.
226. All of the following may result in the nephrotic syndrome except:
A. diabetes mellitus
B. Hodgkin’s lymphoma
227. ?Which cellular elements predominate in areas of inflammation of kidney tissue during the late
stages of acute pyelonephritis?
A. *Macrophages, plasma cells, lymphocytes
B. Neutrophils, eosinophils, basophils
C. neutrophils, promyelocytes
D. lymphocytes, basophils
E. reticulocytes, neutrophils
228. How to determine the degree of proteinuria?
A. Determination of protein in the morning urine
B. Determination of protein in the daily urine
C. Determination of protein in a three-hour portion of urine
D. *Determination of protein in the urine after water loading
E. Determination of protein in the urine after water restriction
229. Which way of antibiotics administration is prescribed during the initial stage of acute
pyelonephritis treatment?
A. *parenteral
B. Oral
C. Rectal
D. Inhaled
E. Oral and parenteral
230. Is significant haematuria typical for cystitis?
A. *Yes
B. No
C. There is no right answer
D. All answers are correct
E. B and C
231. In event of which of the following diseases a positive Pasternatskyi symptom is determined?
A. Chronic glomerulonephritis
B. Renal amyloidosis
C. Hypoplasia of kidneys
D. *Infectious and inflammatory kidney disease
E. Cystitis
232. Which clinical sign is not typical for acute pyelonephritis?
A. Raising the temperature to febrile digits with a fever
B.
C.
D.
E.
233.
A.
B.
C.
D.
E.
234.
A.
B.
C.
D.
E.
235.
A.
B.
C.
D.
E.
236.
A.
B.
C.
D.
E.
237.
A.
B.
C.
D.
E.
238.
A.
B.
C.
D.
E.
239.
A.
B.
C.
D.
E.
240.
A.
B.
C.
D.
E.
241.
Backache
dysuric symptom
*The presence of hypertension
There is no right answer
What does the presence of human renal epithelium cells in urine show?
glomerulonephritis
*pyelonephritis
renal amyloidosis
kidney tumour
All answers are correct
What changes in the urine are typical for chronic pyelonephritis:
Hematuria, cylindruria
*Pyuria, cylindruria, proteinuria
Cylindruria
Hematuria, bakteriyuriya
Eritrotsituriya, cylindruria, proteinuria
What are characteristics of oedemas in acute nephritis?
Appear in the evening
First appear in the lower extremities
First appear in the upper extremities
*Appear on the face in the morning
Anasarca appears at once
What are characteristics of hypertensive form of chronic nephritis?
Normal blood pressure and urinary syndrome
High blood pressure and urinary syndrome
Oedema and urinary syndrome
*High blood pressure and swelling
Swelling of the whole body (anasarca) and high blood pressure
What is the origin of the modified red blood cells in urine?
*Acute nephritis
Urolithiasis
Acute cystitis
Paranefrit
Bladder Cancer
During which of diseases named pyuria can take place:
*Pyelonephritis
Paranefrit
Acute nephritis
Renal amyloidosis
Bladder Cancer
The amount of protein in urine during the urinary syndrome:
*to 1 g / day
to 3.5 g / day
to 4.5 g / day
to 5.5 g / day
to 9.5 g / day
The main clinical signs of tubular damage are the following, except:
Acidosis
Glycosuria
Hypo-, isosthenuria
*arterial hypertension;
Cylindruria
Proteinuria is a urinary protein excretion in the amount more than:
A.
B.
C.
D.
E.
242.
A.
B.
C.
D.
E.
243.
A.
B.
C.
D.
E.
244.
A.
B.
C.
D.
E.
245.
A.
B.
C.
D.
E.
246.
A.
B.
C.
D.
E.
247.
A.
B.
C.
D.
E.
248.
A.
B.
C.
D.
E.
249.
A.
B.
C.
D.
E.
10 mg per day
30 mg per day
50 mg per day
*100 mg per day
5 mg per day
What is meant by the term "dysuric symptom"?
Urination at night
Amount of daily urine increasing
Amount of daily urine reduction
*Hard discomfort feelings and pain when urinating, urinating dysrhythmia
Ratio of daytime and nighttime diuresis violation
What was the cause of proteinuria during the nephrotic syndrome?
Increased reabsorption of protein in tubules
Reduced reabsorption of protein in tubules
*Increased filtration of protein in glomerular
Reduced filtration of protein in glomerular
Increased filtration of red blood cells in glomerular
That prevails in the urine sediment during acute glomerulonephritis?
Bacteria
Oxalate
*Erythrocytes
Leukocytes
hyaloid cylinders
What is the cause of hypoproteinemia in chronic glomerulonephritis?
Hyperlipidemia
Arterial hypertension
*Proteinuria
Oedema
Abnormal liver function
Which proteins are mainly lost in patients who suffer from nephrotic syndrome?
*Albumins
Gamaglobulina
Alpha-1-globulins
Alpha-2 globulins
Betaglobuliny
What is important in the development of oedema during glomerulonephritis?
Arterial hypertension
Microalbuminuria
*Hypoproteinemia
Albuminosis
Hyperlipidemia
What changes of blood electrolytes are typical for nephrotic syndrome?
Increasing of potassium
Reduction of potassium
*Increasing of sodium
Reduced sodium
Increased phosphorus
During which kidney disease eclampsia can appear?
Acute pyelonephritis
Chronic pyelonephritis
Renal amyloidosis
*Acute glomerulonephritis
Myeloid nephropathy
250.
A.
B.
C.
D.
E.
251.
A.
B.
C.
D.
E.
252.
A.
B.
C.
D.
E.
253.
A.
B.
C.
D.
E.
254.
A.
B.
C.
D.
E.
255.
A.
B.
C.
D.
E.
256.
A.
B.
C.
D.
E.
257.
A.
B.
C.
D.
E.
258.
A.
B.
C.
D.
Which manifestations are untypical for renal eclampsia?
Intracranial hypertension
Attack
Spasm of cerebral vessels
*High Blood Pressure
Pulmonary edema
Which dietary factors can provoke an attack of renal eclampsia?
Sweet
*Salt
Fat
Bitter
Acute
Which microorganism is responsible for development of acute glomerulonephritis?
Colon bacillus
Klebsiella
*Beta hemolytic streptococcus
Aurococcus
Proteus vulgaris
Which diseases do not precede the development of acute glomerulonephritis?
Scarlet fever
Otitis
Sinusitis
Angina
*Laryngitis
Which triad of symptoms is typical for acute glomerulonephritis?
Pain, dysuria, leukocyturia
erythrocyturia, bacteriuria, swelling
Edema, hypertension, hypo- isosthenuria
*Hypertension, edema, proteinuria
Dysuria, erythrocyturia, oxaluria
Which macroscopic changes of urine can take place during acute glomerulonephritis?
Yellow urine
*Urine colour "meat slops"
Clear urine
Bright red urine
Pale yellow, opacity
What does not refere to complications of acute glomerulonephritis?
Acute heart failure
Acute renal failure
Hemorrhagic stroke
Eclampsia
*Acute abdomen
Which disease is transient oliguria typical for?
Acute pyelonephritis
*Acute glomerulonephritis
Initial stage of chronic renal failure
Uremia
Chronic pyelonephritis
During which desease is selective proteinuria often observed?
*Acute glomerulonephritis
Chronic glomerulonephritis
Renal amyloidosis
Diabetic nephrosclerosis
E. Tuberculosis of kidneys
259. Reberga sample lets determine:
A. Concentrational ability of the kidney
B. *Glomerular filtration
C. Plasma blood flow
D. Transport of electrolytes
E. Secretion of glucose
260. Which of these symptoms are more common during acute glomerulonephritis with absence of acute
kidney failure?
A. Headache
B. Asthma
C. Oliguria
D. *Increased blood pressure
E. Arthralgia
261. Name the factors that take part in the pathogenesis of oedema syndrome during acute
glomerulonephritis:
A. *All answers are correct
B. Increased capillary permeability
C. Sodium retention in the body
D. Secondary hyperaldosteronism
E. There is no right answer
262. The most reliable sign of rapidly progressing glomerulonephritis is:
A. Arterial hypertension
B. Nephrotic syndrome
C. *Manifestations of chronic renal failure increasing
D. Rack gross hematuria
E. Hypercholesterolemia
263. What play a leading role in the pathogenesis of chronic glomerulonephritis?
A. Autoimmune processes
B. Immune complexes
C. Disturbances in system of renal hemodynamic
D. *All answers are correct
E. There is no right answer
264. Which of the following symptoms are not typical for nephrotic syndrome?
A. massive proteinuria
B. Edema
C. Gross hematuria
D. Hypercholesterolemia
E. *Bacteriuria
265. Which of the following factors causes a decrease of glomerular filtration below 80 ml / min?
A. Blood pressure increasing to 170/95 mmHg
B. Blood pressure reduction to 110/65 mmHg
C. Proteinuria higher than 100 mg / day
D. Macrohematuria
E. *Reduction of number of functioning nephrons
266. Glomeruli and kidneys are typically increased in size in:
A. diabetic nephropathy;
B. renal amyloidosis;
C. polycystic kidney disease;
D. Renal tumor
E. *all of them;
267. What percentage of kidney stones are radio opaque?
A. *90%
B. 80%
C. 70%
D. 50%
E. 40%
268. What are three factors in limiting progression of chronic renal failure in Type I diabetics with
chronic renal failure,?
A. ACE inhibitors
B. Dietary protein restriction
C. Careful control of serum glucose level
D. *All of them
E. None of the
269. What is the most common renal complication of autosomal dominant polycystic kidney disease?
A. gross hematuria,
B. frequent UTI's,
C. *arterial hypertension,
D. nephrolithiasis
E. all of them
270. Аindings in Hepatorenal syndrome are?
A. Azotemia
B. Hyponatremia
C. Progressive oligouria
D. Hypotension
E. *All of them
271. What are indications for dialysis in the setting of renal failure?
A. Fluid overload
B. Refractory hyperkalemia
C. BUN > 130
D. Pericardial friction rub
E. *All of them
272. The metabolic complications of nephrotic syndrome include all of the following except:
A. protein malnutrition;
B. *iron-resistant microcytic hypochromic anemia;
C. Hypocalcemia;
D. hypolipidemia;
E. secondary hyperparathyroidism.
273. What percentage of patients with polycystic kidney disease develop adenocarcinoma of the kidney?
A. 5 %
B. 10 %
C. 15 %
D. 30%
E. *1.5 %
274. What percentage of adults by the age of 50 y/o will develop simple or solitary renal cysts?
A. *25-30%
B. 1-5 %
C. 5-10 %
D. 30-50 %
E. 10 -15 %
275. Is nephrolithiasis more common in men?
A. *Yes, more common 2:1
B. No, more common in female 2:1
C. No, equal in both
D. Yes, more common 3:1
E. None of them
276. The nephrotic syndrome is a clinical complex characterized by a number of renal and extrarenal
features, the most prominent of which are:
A. proteinuria of >3.5 g (per 24 h);
B. hypoalbuminemia;
C. edema;
D. hyperlipidemia;
E. *all of them.
277. Select the drug which is given in usual dosages, may be effective in treating urinary tract infections
in patients with acute renal failure. Why do you choose this drug?
A. Gentamicin;
B. Nitrofuratoin;
C. *Cephalexin;
D. Carbenicillin;
E. Chloramphenicol
278. The Diet of patient with nephrotic syndrome has to exclude
A. Increased content of Salt
B. Increased content of fats
C. Increased content of proteins
D. *All of then
E. None of them
279. What substances are reabsorbed in renal tubules completely?
A. *Glucose
B. Creatinine
C. Sodium
D. Potassium
E. Chlorum
280. Endocrine function of kidneys include synthesis of all except
A. Renin
B. Erythropoetin
C. Prostaglandins
D. *Aldosterone
E. Calcitriol
281. Endocrine function of kidneys include synthesis of all except
A. Renin
B. Erythropoetin
C. Prostaglandins
D. *Insulin
E. Calcitriol
282. Endocrine function of kidneys include synthesis of all except
A. Renin
B. Erythropoetin
C. Prostaglandins
D. *Cortizol
E. Calcitriol
283. What substance indicates the disturbed excretory function of kidneys best of all:
A. *Creatinine
B. Urea
C. Uric acid
D. Potassium
E. Sodium
284. Decreased GFR (Glomerular filtration rate) will be in a case of^
A. Acute pyelonephritis
B. Acute glomerulonephritis
C.
D.
E.
285.
A.
B.
C.
D.
E.
286.
A.
B.
C.
D.
E.
287.
A.
B.
C.
D.
E.
288.
A.
B.
C.
D.
E.
289.
A.
B.
C.
D.
E.
290.
A.
B.
C.
D.
E.
291.
A.
B.
C.
D.
E.
292.
A.
B.
C.
D.
E.
293.
A.
Renal amiloidosis
*Acute renal failure
Nephrolithiasis
Decreased GFR (Glomerular filtration rate) will be in a case of^
Acute pyelonephritis
Acute glomerulonephritis
Renal amiloidosis
*Chronic renal failure
Nephrolithiasis
The best method to evaluate renal function is to measure
*Glomerular filtration rate
Creatinine
Urea
Uric acid
Potassium
Glomerular filtration rate (GFR) can be calculated by means of^
Cockroft-Gault formula
MDRD formula
Inulin test
*All of them
None of them
Glomerular filtration rate (GFR) can be calculated by means of:
Cockroft-Gault formula
MDRD formula
Clearance of endogenic creatinine test
*All of them
None of the
Indication to renal biopsy are:
*Differential diagnosis of kidney disease
Suspicion for renal tumor
Suspicion for renal tuberculosis
Oedema
Suspicion for renal abscess
Indication to renal biopsy are:
*Nephrotic syndrome
Suspicion for renal tumor
Suspicion for renal tuberculosis
Oedema
Suspicion for renal abscess
Indication to renal biopsy are:
*Changes in urine analysis of unknown etiology
Suspicion for renal tumor
Suspicion for renal tuberculosis
Oedema
Suspicion for renal abscess
The purpose of renal biopsy is to evaluate
Renal function
Stage of renal failure
*Diagnosis and optimal treatment
All of them
None of them
Absolute contraindication to renal biopsy are:
Anemia
B.
C.
D.
E.
294.
A.
B.
C.
D.
E.
295.
A.
B.
C.
D.
E.
296.
A.
B.
C.
D.
E.
297.
A.
B.
C.
D.
E.
298.
A.
B.
C.
D.
E.
299.
A.
B.
C.
D.
E.
300.
A.
B.
C.
D.
E.
301.
A.
B.
C.
D.
E.
302.
Arterial hypertension
Hematuria
Oedema
*Single kidney
Absolute contraindication to renal biopsy are:
Anemia
Arterial hypertension
Hematuria
Edema
*Polycystic kidney
Absolute contraindication to renal biopsy are:
Anemia
Arterial hypertension
Hematuria
Edema
*Hydronephrosis
Complications of renal biopsy may be
Hepatitis B
Hepatitis C
HIV
Arterial hypertension
*Pain syndrome
Complications of renal biopsy may be
Hepatitis B
Hepatitis C
HIV
Arterial hypertension
*Arterio-venous fistula
Complications of renal biopsy may be
Hepatitis B
Hepatitis C
HIV
Arterial hypertension
*Hypertermic sundrome
Complications of renal biopsy may be
Hepatitis B
Hepatitis C
HIV
Arterial hypertension
*Collapse
Complications of renal biopsy may be
Hepatitis B
Hepatitis C
HIV
Arterial hypertension
*Temporary anuria
Complications of renal biopsy are except:
Collapse
Hypertermic syndrome
Temporary anuria
Pain syndrome
*Hepatitis C
Complications of renal biopsy are except:
A.
B.
C.
D.
E.
303.
A.
B.
C.
D.
E.
304.
A.
B.
C.
D.
E.
305.
A.
B.
C.
D.
E.
306.
A.
B.
C.
D.
E.
307.
A.
B.
C.
D.
E.
308.
A.
B.
C.
D.
E.
309.
A.
B.
C.
D.
E.
310.
A.
B.
C.
D.
E.
Collapse
Hypertermic syndrome
Temporary anuria
Pain syndrome
*Hepatitis B
Complications of renal biopsy are except:
Collapse
Hypertermic syndrome
Temporary anuria
Pain syndrome
*HIV
Complications of renal biopsy are except:
Collapse
Hypertermic syndrome
Temporary anuria
Pain syndrome
*Arterial hypertension
Risk factors of pyelonephritis are except
Diabetes malliyus
Pregnancy
Diturbancres of urodynamics
Refluxes
*Arterial hypertension
Risk factors of pyelonephritis are except
Diabetes malliyus
Pregnancy
Diturbancres of urodynamics
Refluxes
*Heart failure
Risk factors of pyelonephritis are
Diabetes malliyus
Pregnancy
Diturbancres of urodynamics
Refluxes
*All of them
The symptoms of acute pyelonephritis are
Intoxication
Low back pain
Dysuria
Leucocyturia
*All of them
The symptoms of acute pyelonephritis are except
Intoxication
Low back pain
Dysuria
Leucocyturia
*Arterial hypertension
The symptoms of acute pyelonephritis are except
Intoxication
Low back pain
Dysuria
Leukocyturia
*Renal osteodystrophy
311. Complications od acute pyelonephritis are except
A. Perinephritis
B. Renal abscess
C. Papillary necrosis
D. Urosepsis
E. *Xanthogranulomatosis pyelonephritis
312. Drug of choice for patient with rheumatoid artritis
A. *Methotrexate
B. NSAIDs
C. Hydroxychloroquine sulphate
D. Sulphasalazine
E. D-penicillamine
313. The best drug to treat SLE is :
A. Asprin
B. Indomethacin
C. Prostoglandines
D. Procainamide
E. *Steroids
314. Drug-induced systemic lupus erythematosus (SLE) can be characterized by all of the following
statements EXCEPT?
A. Twenty percent of patients receiving procainamide develop drug-induced lupus
B. *Most patients on hydralazine develop a positive antinuclear antibody (ANA) test; however, only
10 percent suffer from lupuslike symptoms
C. If patients with drug-induced lupus fail to respond within several weeks of discontinuing the
offending agent, a trial of corticosteroids is indicated
D. If a patient with drug-induced lupus has persistent symptoms for longer than 6 months, an anti-ds
antibody
E. None of the above
315. For the Systemic lupus erythematosus choose the most likely diagnostic antibody from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. *Anti-dsDNA
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
316. In which of the following diseases test for anticentromere antibody is positive?
A. *Scleroderma
B. Mixed connective tissue disorder
C. SLE
D. Rheumatoid arthritis
E. Polymyalgia rheumatica
317. Supporting evidence of a recent group A streptococcal infection may be all of the following except:
A. *recent malar rash
B. elevated or increasing streptococcal antibody test - antistreptolysin- O (ASO)
C. positive throat culture
D. recent scarlatine
E. all mentioned above
318. A 39-year-old male developed acute, severe pain and swelling of the left elbow. Within next few
hours, pain worsened and he was unable to move the elbow joint, which was tender, erythematous, and
swollen on examination. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis + synoviitis
D. *Gouty arthritis
E. Psoriatic arthritis
319. For the Systemic lupus erythematosus choose the most likely diagnostic antibody from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. *Antinuclea antibody
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
320. A 27-yr-old woman presents with a 3-week history of fever, pleuritic chest pain, stiffness and
swelling in the wrists, MCP joints and PIP joints. On examination, there is bilateral pretibial oedema.
Choose the most likely treatment from the below list of options.
A. Asprin
B. Indomethacin
C. Prostoglandines
D. Procainamide
E. *Steroids
321. A 52-yr-old woman complains of a 8-month history of Raynaud's phenomenon, progressive skin
tightness, thickening of fingers and hands, dyspnoea on exertion and dysphagia. Choose the most likely
diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Polymyalgia rheumatica
C. SLE
D. Polyarteritis nodosa
E. *Scleroderma
322. A 21-year-old woman is referred to you for evaluation of new-onset Raynaud’s phenomenon. She
has no other symptoms. Her physical examination is unremarkable except for dilated nail-fold capillaries
and a few scattered telangiectasias. Tests for specific ANA reveal the presence of antibodies to
topoisomerase I. The most likely eventual diagnosis for this patient is which of the following?
A. Isolated Raynaud’s disease
B. *Diffuse systemic sclerosis
C. Limited systemic sclerosis
D. Mixed connective tissue disease (MCTD)
E. SLE
323. A 25-year-old woman is referred to you for evaluation of new-onset Raynaud’s phenomenon. She
has no other symptoms. Her physical examination is unremarkable except for dilated nail-fold capillaries
and a few scattered telangiectasias. Tests for specific ANA reveal the presence of antibodies to
topoisomerase I.Choose the most likely treatment from the below list of options.
A. *D-penicillamine
B. Methotrexate
C. Indomethacin
D. Aspirin
E. Nifidipine
324. The bad prognostic indicator for scleroderma is:
A. *Renal involvement
B. Goose skin appearance
C. Oedema legs
D. Widening of pulse pressure
E. Calcification
325. Which of the following is a typical immune complex disease?
A. Osler-Weber-Rendu syndrome
B. Urticaria pigmentosa
C. *Lupus erythematosus
D. Gastric ulcer
E. Pneumonia
326. Which of the following statements regarding the use of cyclophosphamide in the treatment of
rheumatic disorders such as lupus nephritis and vasculitis is correct?
A. The dose of cyclophosphamide should be increased until substantial leukopenia is observed.
B. The absorption of oral cyclophosphamide is poor, so the intravenous route is preferred.
C. Oral cyclophosphamide should be administered at night and fluids restricted in order to decrease
the formation of urine.
D. *Regular monitoring of the patient’s complete blood cell count and urinalysis is required.
E. None of the above
327. A 42-yr-old woman complains of a 4-month history of Raynaud's phenomenon, progressive skin
tightness, thickening of fingers and hands, dyspnoea on exertion and dysphagia. Choose the most likely
treatment from the below list of options.
A. *D-penicillamine
B. Methotrexate
C. Indomethacin
D. Aspirin
E. Nifidipine
328. Woman of 35 years with Raynauds phenomenon, polyarthritis, dysphagia of 5 years and mild
sclerodactyly, blood showing Anticentromere antibody positive, the likely cause is:
A. *Scleroderma
B. Mixed connective tissue disorder
C. SLE
D. Rheumatoid arthritis
E. Polymyalgia rheumatica
329. A 29-yr-old woman presented with DVT of the left calf. She had a history of recurrent abortions
and arthritis. Choose the most likely diagnosis from the below list of options.
A. Protein C deficiency
B. Thrombotic thrombocytopenia
C. *Antiphospholipid syndrome
D. SLE
E. Polycythemia rubra vera
330. A 25-yr-old woman presents with deep venous thrombosis in the right leg. Her past history includes
three miscarriages. Her blood tests show mild thrombocytopenia and a positive serology test for syphilis.
Choose the most likely diagnosis from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. Mixed connective tissue disorder
D. *Antiphospholipid syndrome
E. Polyarteritis nodosa
331. Which of the following is an initiation for institution of therapy with hydroxychloroquine in a
patient with systemic lupus erythematosus (SLE)?
A. Thrombocytopenia
B. *Subacute cutaneous lupus
C. Central nervous system vasculitis
D. Diffuse proliferative glomerulonephritis (DPGN)
E. Gangrene of digits
332. Which of the following statements regarding cyclophosphamide therapy for life-threatening lupus,
including severe lupus nephritis, is true?
A. Cyclophosphamide is approved for use by the Food and Drug Administration (FDA) as therapy for
severe lupus nephritis.
B. The standard dose for cyclophosphamide intermittent intravenous therapy (0.5-1.0 g/m2 of body
surface area) has been shown to be more efficacious than lower doses.
C. *The standard protocol for intravenous use (once a month times 6, then quarterly for 2 more years)
has been shown to reduce posttreatment disease flares compared to once a month times six doses.
D. Hematopoietic ablation with very high doses of cyclophosphamide is superior to the standard
regimen in efficacy.
E. Hemorrhagic cystitis does not occur with intravenous dosage.
333. Which of the following APhS symptoms predictably respond(s) to treatment with heparin?
A. Livedo reticularis
B. Cardiac valve disease
C. *Recurrent fetal loss
D. Cognitive dysfunction
E. Renal microangiopathy
334. A 23-year-old woman who is 27 weeks pregnant is admitted to hospital with proteinuria, a “purple
cold toe,” and painful swollen metacarpophalangeal (MCP) joints, and wrists. She was diagnosed with
systemic lupus erythematosus (SLE) 1 year previously after miscarrying her first pregnancy. Which of
the following statements is/are correct?
A. She should stop all her medications because of the risks to her fetus.
B. Corticosteroid therapy should not be given because it will have teratogenic effects on the fetus.
C. *If antiphospholipid antibodies are positive, she should be placed on anticoagulants.
D. Her infant should be delivered immediately.
E. None of the above
335. Which of the following is one of the earliest predictors of whether a patient with Raynaud’s
phenomenon will go on to develop true scleroderma?
A. Constipation
B. Decreased vital capacity
C. Thickening of the forearm skin
D. *Dilated and dropout capillaries at the nail base of fingers
E. None of the above
336. Which of the following autoantibodies is more likely to be found in patients with systemic
sclerosis?
A. anti-Smith (anti-Sm)
B. Anti-ribonucleoprotein (RNP)
C. *Anti-DNA topoisomerase 1 (anti-Scl70)
D. Anti-citrullinated peptide
E. Anticentromere
337. Vegetations on undersurface of A.V. valves are found in:
A. Acute Rheumatic corditis
B. *Limban Sack's endocarditis
C. Non thrombotic bacterial endocarditis
D. Chronic rheumatic carditis
E. MVP
338. Drug-induced systemic lupus erythematosus (SLE) can be characterized by which of the following
statements?
A. Twenty percent of patients receiving procainamide develop drug-induced lupus
B. *Nephritis is a frequent consequence of hydralazine-induced lupus
C. If patients with drug-induced lupus fail to respond within several weeks of discontinuing the
offending agent, a trial of corticosteroids is indicated
D. If a patient with drug-induced lupus has persistent symptoms for longer than 6 months, an anti-ds
antibody and CH50 levels should be drawn
E. None of the above
339. Anti-double stranded DNA is highly specific for
A. Systemic sclerosis
B. *SLE.
C. Polymyositis
D. Dermatopolymyositis
E. Henoch schonlein purpura
340. A 35 year old lady complains dysphagia, Raynaud's phenomenon, sclerodactyly. Investigations
show anticentromere antinuclear antibody. The likely diagnosis is:
A. Systemic lupus erythematosis
B. *Systemic sclerosis
C. Mixed connective tissue disorder
D. Rheumatoid arthritis
E. Dermatopolymyositis
341. 33-year-old patient, presents with complaints of tightness of fingers. There is also history of
dysphagia. Choose the most likely results of the investigations from the below list of options.
A. *Anticentromere antibody
B. Anti dsDNA antibodies
C. ANCA
D. Antimitochondrial antibody
E. Smooth muscle antibody
342. A 41-year-old woman complains of weakness, fatigue, fever up to 38°C, rash on the face skin, pain
in the wrists and the elbows. On physical exam, erythematous rash on the cheeks with “butterfly”
appearance, the wrists and elbow joints are involved symmetrically, swollen, tender on motions, on
urinalysis: proteinuria, leukocyturia, casts. What is the main mechanism of disease development?
A. Production of antibodies to myocytes.
B. *Production of antibodies to double-stranded DNA.
C. Production of antibodies to endothelial cells.
D. Production of antibodies to myosin.
E. Production of antimitochondrial antibodies.
343. A 39-year-old woman presents with induration and atrophy of the fingertips and is diagnosed as
having systemic sclerosis (scleroderma). Visceral involvement may lead to all of the following EXCEPT
A. Esophageal hypomotility
B. *obstructive lung disease
C. right-sided heart failure
D. malabsorbtion
E. renovascular hypertension
344. A 30-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, painfull joints (ankles, knees), edema on legs, dyspnea on excursion,
palpitation, rash across the face, which occurred after sunbathe, hair losing. Physical examination revels
malar rash, enlargement of heart, tachycardia, edema on legs. The most likely diagnosis is
A. Dermatomyositis
B. Progressive muscule dystrophy
C. *Systemic lupus erythematosus
D. Myasthenia,
E. Polymyalgia rheumatica,
345. A 39-year-old woman presents with induration and atrophy of the fingertips and is diagnosed as
having systemic sclerosis (scleroderma). Which of the following drugs you will prescribe?
A. *D-penicillamine
B. Ampicillin
C. Allopurinol
D. Nitrates
E. digoxin
346. A 50-year-old woman has had Raynaud’s phenomenon of the hands for 15 years. The condition has
become worse during the last year, and she has developed arthralgia and arthritis involving the hands and
wrists as well as mild sclerodactyly and difficulty swallowing solid foods. Anticentromere antibodies are
present in high titers: antiribonucleoprotein antibodies are not detectable. The most likely diagnosis of
this woman’s disorder is
A. *systemic sclerosis
B. mixed connective-tissue disease
C. overlap syndrome
D. dermatomyositis
E. Systemic lupus erythematosus
347. A 32-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, painfull joints (ankles, knees), edema on legs, dyspnea on excursion,
palpitation, rash across the face, which occurred after sunbathe, hair losing. Physical examination revels
malar rash, enlargement of heart, tachycardia, edema on legs. All of the following drugs you can
prescribe (may be simultaneously) EXCEPT
A. Glucocorticoids
B. Methotrexate
C. *Procainamide
D. Diclofenac
E. Azathioprine
348. A 18-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, dyspnea on excursion. Physical examination revels malar rash, oral ulcer, signs
of pneumonitis, laboratory test revels severe anemia, leucopenia thrombocytopenia, ESR -53 mm/h, urine
analysis – protein 0,33, L- 5-8 in the field of vision, Er. – 8- 10 in the field of vision. Which of the
following drugs you prescribe?
A. *Glucocorticoids
B. Methotrexate
C. amoxacicllin
D. cyclophosphanum
E. chlorambucil
349. A 18-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, dyspnea on excursion. Physical examination revels malar rash, oral ulcer, signs
of pneumonitis, laboratory test revels anemia, leucopenia thrombocytopenia. All of the following criteria
are useful for diagnosis EXCEPT
A. Antinuclear antibodies
B. anti-phospholipid antibodies
C. Proteinuria > 0.5 g/d
D. lymphocytopenia
E. *The heliotrope rash
350. A 39-year-old woman presents with induration and atrophy of the fingertips and is diagnosed as
having systemic sclerosis (scleroderma). All of the following criteria are true for diagnosis EXCEPT
A. Digital pitting scars
B. Bibasilar pulmonary fibrosis
C. *Heart failure
D. Proximal scleroderma
E. Sclerodactyly
351. A 35-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, arthritis, edema on legs, dyspnea on excursion, palpitation, rash across the face,
which occurred after sunbathe, hair losing. Physical examination revels malar rash, enlargement of heart,
tachycardia, edema on legs. All of the following drugs you can prescribe (may be simultaneously)
EXCEPT
A. Glucocorticoids
B. Methotrexate
C. *Gold
D. Diclofenac
E. Azathioprine
352. A 22-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, dyspnea on excursion. Physical examination revels malar rash, oral ulcers, signs
of pneumonitis, laboratory test revels anemia, leucopenia thrombocytopenia, ESR -35 mm/h, urine
analysis – protein 0,33, L- 5-8 in the field of vision, Er. – 8- 10 in the field of vision. All of the following
criteria are useful for diagnosis EXCEPT
A. Antinuclear antibodies
B. anti-phospholipid antibodies
C. Proteinuria > 0.5 g/d
D. *lymphocytosis
E. anaemia
353. A 27-year-old woman was admitted to the rheumatological department complaining of malaise,
general weakness, fever, dyspnea on excursion. Physical examination revels malar rash, oral ulcers, signs
of pneumonitis, laboratory test revels anemia, leucopenia thrombocytopenia, ESR -35 mm/h, urine
analysis – protein 0,33, L- 5-8 in the field of vision, Er. – 8- 10 in the field of vision. All of the following
criteria are useful for diagnosis
A. Antimicrosomal antibody
B. Antireticulin antibody
C. *Anti-dsDNA
D. P-ANCA antibody
E. Rheumatoid factor
354. Serologic tests should be performed in patients with specific musculoskeletal complaints for
assessing all the following EXCEPT:
A. rheumatoid factor
B. antinuclear antibodies (ANA)
C. uric acid level
D. *GGT
E. antistreptolysin O (ASO) titer
355. 37-year-old patient, presents with induration and atrophy of the fingertips, dysphagia, Raynaud's
phenomenon. Choose the most likely results of the investigations from the below list of options.
A. *Anticentromere antibody
B. Anti dsDNA antibodies
C. ANCA
D. Antimitochondrial antibody
E. Smooth muscle antibody
356. Serological findings in patients with systemic lupus erythematosus (SLE) will NOT include which
one of the following:
A. A raised serum IgG level
B. Antibodies to double-stranded DNA
C. Decreased C3 and C4 levels
D. A positive ANA
E. *Antibodies to cyclic citrullinated peptide (anti-CCP antibodies)
357. Which one of the following statements about autoimmune diseases is true
A. Affect about 1 person in every 1000
B. *Are more common in women
C. Tend to begin in early childhood
D. Are an inevitable consequence of autoimmune responses
E. Are usually mediated by type I hypersensitivity
358. A 32-year-old woman is evaluated because of a 5-year history of Raynaud’s phenomenon and
thickened skin over the fingers, small patches of calcinosis on the distal fingers and dorsum of one hand.
She reports mild dyspnea when she climbs stairs. What changes reveals chest X-ray?
A. Bronchiolitis with organizing pneumonia
B. *Bibasal pneumofibrosis
C. Lung cancer
D. Emphysema
E. Pulmonary tromboembolism
359. Which of the following clinical features is NOT commonly found in limited systemic sclerosis?
A. Raynaud's phenomenon
B. Oesophageal dysfunction
C. *Eczema
D. Sclerodactyly
E. Telangiectasia
360. Which one of the following statements about systemic connective tissue diseases is not true?
A. Can cluster within families
B. Are often associated with particular HLA alleles
C. *Are usually mediated by type I hypersensitivity
D. May occur in humans with inherited defects in apoptosis
E. Are more common in women
361. Classification of Systemic Sclerosis includes all of the following EXCEPT
A. Limited cutaneous scleroderma
B. Diffuse cutaneous scleroderma
C. Scleroderma sine scleroderma
D. *Eczema
E. Overlap syndromes
362. Which of the following occurs rarely in Limited cutaneous scleroderma
A. Skin involvement
B. Raynaud phenomenon
C. Dilated nailfold capillary loops
D. *Renal disease
E. Anticentromere antibody
363. Which of the following doesn’t occur in Diffuse cutaneous scleroderma
A. *Vegetations on undersurface of A.V. valves
B. Raynaud phenomenon
C. Truncal and acral skin involvement
D. Nailfold capillary dilation
E. interstitial lung
364. Cardiac involvement in SSC are all of the following EXCEPT
A. Pericardial effusion
B. Cor pulmonale
C. Conduction abnormalities
D. *Vegetations on undersurface of A.V. valves
E. arrhythmias
365. 52 year old male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in
the DIP of the right first digit, with calcifications. Further questioning revealed a history of repeated
attacks of acute joint pain. There is bony erosion at multiple DIP's of the right hand that is periarticular,
well corticated and has a thin overhanging edge. There is no associated osteopenia. Choose the most
likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Chronic gouty arthritis
E. Psoriatic arthritis
366. 52 yo male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in the
DIP of the right first digit, with calcifications. Further questioning revealed a history of repeated attacks
of acute joint pain. Which of the following medications is indicated for the treatment of chronic arthritis?
A. colchicine
B. *allopurinol
C. corticosteroids
D. indomethacin
E. ibuprofen
367. 55 years old, came to a musculoskeletal specialist seeking advice for a 3-year history of
progressively worsening pain in both knees. Her knees were stiff for about 20 minutes when she arose in
the morning and for a few minutes after getting up from a chair during the day Her symptoms were worse
on humid or cold days, and she occasionally felt as if one of her knees would give out. Choose the most
likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
368. 55 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Chronic Gouty arthritis
C. Rheumatoid arthritis
D. Osteoarthritis
E. Psoriatic arthritis
369. 57 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is indicated for the treatment
of chronic arthritis?
A. colchicine
B. corticosteroids
C. indomethacin
D. *allopurinol
E. ibuprofen
370. 63 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is contraindicated for the
treatment of exacerbation of arthritis
A. corticosteroids
B. colchicine
C. indomethacin
D. ibuprofen
E. *allopurinol
371. 55 years old, came to a musculoskeletal specialist seeking advice for a 3-year history of
progressively worsening pain in both knees. Her knees were stiff for about 20 minutes when she arose in
the morning and for a few minutes after getting up from a chair during the day. She had difficulty
walking > 30 minutes because of pain, and her symptoms were exacerbated by kneeling, squatting, or
descending stairs. Although sitting, resting, and reclining relieved her pain, she became stiff if she stayed
in one position for too long. Which of the following changes will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
372. 59 yo female with swelling and pain of his fingers. Patient also with similar complaints regarding
his great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and
3rd digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and
3rd digits and metatarsophalangeal joints. Which of the following medications is indicated for the
treatment of exacerbation of arthritis?
A. allopurinol
B. corticosteroids
C. *colchicine
D. indomethacin
E. ibuprofen
373. 70-year-old, married, teacher. She has been under treatment for hypertension and is finally stable
on medication. Initial Chief complaint: painful right knee, arthritis in right hip. She had had arthritic pain
in her right hip confirmed by x-ray about 10 years ago. The knee pain is a newer problem and she
suspects it is also arthritis. There is slight crepitus with motion of the right knee. Which of the following
treatment do use?
A. Methotrexat
B. Colchicines
C. *Chondroitin sulfate
D. Tetracycline
E. Allopurinol
374. 70-year-old teacher. She has been under treatment for hypertension and is finally stable on
medication. Initial Chief complaint: painful right knee, arthritis in right hip. She had had arthritic pain in
her right hip confirmed by x-ray about 10 years ago. The knee pain is a newer problem and she suspects
it is also arthritis. There is slight crepitus with motion of the right knee. Which of the following changes
will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
375. A 38-year-old man with a 13-yr history of back pain, presented with acute pain and swelling of one
knee. On examination, the joint was tender and restricted in movement. The knee effusion was aspirated;
the fluid contained a polymorphonuclear leucocytosis but no organisms or rheumatoid factor. Fifteen
months later he developed an iritis in his left eye, low back pain and stiffness. He has peripheral joints
arthritis but pain could be elicited in both sacroiliac joints. X-rays of his spine is shown in the picture.
Choose the medications for patient with shown changes from the below list of options.
A. *Methotrexate
B. Actovegin
C. Mydocalm
D. Warfarin
E. Pentoxifylline
376. A 38-year-old man with a 13-yr history of back pain, presented with acute pain and swelling of one
knee. On examination, the joint was tender and restricted in movement. X-ray of the knee showed
periarticular osteoporosis. Fifteen months later he developed an iritis in his left eye, low back pain and
stiffness. His peripheral joints were normal but pain could be elicited in both sacroiliac joints. Choose the
most likely diagnosis from the below list of options for patient with shown changes
A. *Ankylosing spondylitis
B. Reactive arthritis
C. Osteoarthritis
D. Gout
E. Psoriatic arthritis
377. A 50-year-old male is evaluated because of pain in the right inguinal area, lower back, and hands.
The inguinal pain worsens as he walks, and all pain increases as the day progresses. On physical
examination, internal rotation of the right hip elicits the groin pain. The second, third, and fourth
metacarpophalangeal joints are swollen, warm, and tender to pressure. Radiographs show severe
osteoarthritis in the right hip. Which of the following is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. *Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. Serum uric acid
378. A 55-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The examination was also notable for a
subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpal-phalangeal joint, as well
as evidence of arthritis involving both hands. Which of the following is characteristic of the arthritis?
A. *Depositions of monosodium urate monohydrate crystals within the periarticular soft tissues
B. Overgrowth of bones within joints
C. Autoimmune synovitis
D. Osteoporosis
E. Rheumatoid nodules over joints
379. A 64-year-old woman presents with a 1-year history of pain in her thumbs. She also has nontender
bony overgrowth at the distal interphalangeal joints. The patient says that her mother had the same
fingers and she worries that she will become crippled. Choose the most likely diagnosis from the below
list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
380. A 68-year-old man is evaluated because of a 3-year history of bilateral knee pain and low back
pain. He has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, he has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
right knee. Which of the following treatment do use?
A. Methotrexat
B. *Glucosamine
C. Colchicines
D. Tetracycline
E. Allopurinol
381. A 38-year-old man with a 13-yr history of back pain, presented with acute pain and swelling of one
knee. On examination, the joint was tender and restricted in movement. Later he developed an iritis in his
left eye, low back pain and stiffness. His peripheral joints were normal but pain could be elicited in both
sacroiliac joints. X-rays of his spine is shown in the picture. Which of the following medications isn’t
indicated for the treatment of the disease?
A. *Pentoxifylline
B. Cyclosporine
C. Methotrexate
D. Sulfasalazine
E. Corticosteroids
382. A 57-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The examination was also notable for a
subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpal-phalangeal joint, as well
as evidence of arthritis involving both hands. Which of the following changes will reveal X-ray
examination?
A. Erosions
B. Subluxations
C. Osteophytes
D. Osteoporosis
E. *"punched-out" lytic lesion
383. A 58-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 4 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The examination was also notable for a
subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpal-phalangeal joint, as well
as evidence of arthritis involving both hands. Which of the following medications is indicated for the
treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
384. A 60-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, she has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. All the joints are brought through full
range of motion without pain. There is slight crepitus with motion of the right knee. Which of the
following treatment do use?
A. methotrexat
B. *intra-articular injection of sodium hyaluronate
C. probenecid
D. colchicine
E. allopurinol
385. A 64-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. On
physical examination, there is crepitus on passive motion of the left knee, which has a slight varus
deformity. Her feet turn out slightly, and the heels are in valgus. Which of the following changes will
reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
386. A 68-year-old woman has had four or five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. Her most recent episode was 4 months ago. On physical
examination, none of her joints is swollen or tender, but there is marked crepitus on extension of the
knee. She also has a positive bulge sign over the left knee and pain on full extension of the left elbow.
Which one of the following tests would confirm the diagnosis?
A. *Arthrocentesis of the knee and laboratory analysis of the synovial fluid
B. Measurement of serum uric acid
C. Measurement of serum rheumatoid factor
D. Radiograph of the knee
E. MRI of the knee with gadolinium contrast
387. A 72-year-old retired lawyer is evaluated because of swelling of his right knee. He has mild
osteoarthritis and stays active swimming and playing tennis and golf. On physical examination, he has an
effusion in the right knee. At a point in the mid-thigh (measured from the superior border of the patella),
the right thigh is 4 cm smaller in diameter than the left. There is crepitus with right knee flexion. The
knee is not warm. Which of the following is the best next step in the management of this patient?
A. Order radiographs of both knees and treat the patient with ibuprofen.
B. Order radiographs of the right hip and right knee.
C. *Aspirate the joint fluid in the right knee and refer the patient for physical therapy.
D. Aspirate the joint fluid in the right knee and obtain blood cultures.
E. Treat the patient with celecoxib, and advise him to stay off his feet for 48 hours.
388. On the third day of hospitalization, he developed acute, severe pain and swelling of the left elbow.
Within next few hours, pain worsened and he was unable to move the elbow joint, which was tender,
erythematous, and swollen on examination. Never investigated in the past, we also noted a firm 4 - 6 cm
mass on each elbow, and another one surrounding the proximal inter-phalangeal joint of right middle
finger. When asked particularly, he noticed similar episodes of arthritis of great toe in the past. Choose
the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis + synovitis
D. *Exacerbation of chronic gouty arthritis
E. Psoriatic arthritis
389. On the third day of hospitalization, he developed acute, severe pain and swelling of the left elbow.
Within next few hours, pain worsened and he was unable to move the elbow joint, which was tender,
erythematous, and swollen on examination. Never investigated in the past, we also noted a firm 4 - 6 cm
mass on each elbow, and another one surrounding the proximal inter-phalangeal joint of right middle
finger. When asked particularly, he noticed similar episodes of arthritis of great toe in the past. Which of
the following medications is indicated for the treatment of the arthritis?{
A. allopurinol
B. corticosteroids
C. *colchicine
D. tetracycline
E. mydocalmi
390. A 65-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, she has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
right knee. Which of the following treatment do use?
A. methotrexat
B. allopurinol.
C. probenecid
D. colchicine
E. *Intra-articular Hyaluronic Acid Injections
391. A 65-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, she has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
right knee. All of the following are X-ray signs of arthritis except
A. Joint space narrowing
B. Marginal osteophytes
C. Subchondral cysts
D. Bony sclerosis
E. *Marginal erosions
392. A 30-yr-old woman presents with fits and arthralgia. She is noted to have thinning of her hair and
oral ulceration. Choose the single most likely investigation from the list of options below.
A. Serum calcium
B. Serum glucose
C. Serum electrolytes
D. Serum urea and creatinine
E. *Anti-dsDNA
393. A 20-yr-old woman from Trinidad presents with pleuritic chest pain, breathlessness, arthralgia,
myalgia and facial rash. She has a small left pleural effusion. ESR is 80 mm/hr. C-reactive protein is 3
mg/l. Choose the most likely diagnosis from the below list of options.
A. Tuberculosis
B. Sarcoidosis
C. *SLE
D. Uraemia
E. Wadenstorm's macroglobulinaemia
394. For Positive fluorescent antinuclear antibody choose the single most likely diagnosis from the
below list of options.
A. Wegener's granulomatosis
B. Goodpasture's syndrome
C. Multiple myeloma
D. *Lupus nephritis
E. Diabetic neprtropathy
395. A 35-yr-old woman presented with arthralgia, myalgia, facial rash and blood pressure of 190/110
and impaired renal function. Urine microscopy showed scanty red cells and granular casts. Renal biopsy
showed linear IgG on glomerular basement membrane. Choose the most likely diagnosis from the below
list of options.
A. Tuberculosis
B. Renal tubular acidosis
C. *Lupus nephritis
D. Uraemia
E. Renal artery stenosis
396. For a hypertensive 48-yr-old lady who has been on hydralazine therapy choose the single most
likely diagnosis from the below list of options.
A. *SLE
B. Nephroblastoma
C. Haemolytic uraemic syndrome
D. Juvenile chronic arthritis
E. Henoch-Schonlein purpura
397. A 16-yr-old boy has had a pyrexia, rash, raised ESR, 1 week after faringitis. Subcutaneous nodules
and a generalised rash is noted on the trunk. Choose the single most likely diagnosis from the list of
options below.
A. *Erythema marginatum
B. Maculopapular rash
C. Erythema multiforme
D. Lichen planus
E. Erythema nodosum
398. A 17-year-old boy is brought by his father for evaluation of fever. All of the following would
suggest the diagnosis of acute rheumatic fever EXCEPT:
A. *shortened P-Q interval on ECG.
B. rapid, involuntary, purposeless movements
C. migratory polyarthritis
D. subcutaneous nodules
E. a rash on the trunk and proximal extremities
399. A 18-yr-old boy presents with polyarthritis and abdominal pain. He had a sore throat a week ago.
On examination he is noted to have an early blowing diastolic murmur at the left sternal edge. Choose the
single most likely diagnosis from the list of options below.
A. *Acute rheumatic fever
B. Congestive heart failure
C. Aortic stenosis
D. SLE
E. Mitral stenosis
400. A 27-yr-old woman with a heart condition has a rash on her arms. It is pink or red and ring like. It
moves up and down her arms and she can not get rid of it. Choose the single most likely diagnosis from
the list of options below.
A. *Erythema marginatum
B. Maculopapular rash
C. Erythema multiforme
D. Lichen planus
E. Erythema nodosum
401. A 43-yr-old drug addict is noted to have a PSM at the bottom of the sternum. Giant 'cv' waves are
present in the JVP. Choose the single most likely diagnosis from the list of options below.
A. *TR, infective endocarditis
B. Rheumatic MR
C. Congenital AS
D. Atrial myxoma
E. Congenital PS
402. A 44-yr-old woman presents with malaise and low-grade fever for 3 weeks. She recently had
treatment for a dental abscess. On examination she has splinter haemorrhages and an early diastolic
murmur. Choose the single most likely treatment from the list of options below.
A. *2 or more antibiotics together
B. Amoxycillin
C. Ciprofloxacin
D. Cefotaxime
E. Co-amoxiclav
403. A young man complains of red and sore eyes, painful urination and low back pain. Three months
ago he had UTI and was successfully treated for it. Choose the most likely diagnosis from the below list
of options.
A. *Reiter's syndrome
B. Psoriatic arthropathy
C. Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
404. Accurate statement about rheumatoid factors include all of the following EXCEPT?
A. They are antibodies to the Fc fragment of immunoglobulin G
B. They are associated with several conditions in which there is chronic antigenic stimulation
C. Their presence in the serum of persons with rheumatoid arthritis correlates with a worse prognosis
than that for persons with seronegative disease
D. Rheumatoid factor may be seen in association with many other diseases
E. *They are associated with Still's syndrome
405. A 20-yr-old man presents with urethitis and a painful swollen knee. Choose the most likely
diagnosis from the below list of options.
A. Rheumatoid arthritis
B. *Reactive arthritis
C. Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
406. A 22-yr-old male soldier presents with a 2-week history of a swollen right knee, conjunctivitis and
arthritis. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Reactive arthritis
C. Osteoarthritis
D. Gout
E. Psoriatic arthritis
407. This 43 year-old female had a history- old female had a history of shortness of breath and
palpitations for 7 years with a progressive increase one month before death. She was known to have both
systolic and diastolic murmurs, dilated chambers. Is the disease pericardial, myocardial or endocardial
A. Endocardial
B. Pericardial
C. *Myocardial
D. Pericardial, myocardial and endocardial
E. Pericardial and myocardial
408. This 43 year-old female had a history: old female had a history of shortness of breath and
palpitations for 7 years with a progressive increase one month before death. She was known to have both
systolic and diastolic murmus, dilated chambers. Choose the most likely diagnosis from the below list of
options.
A. *Dilated cardiomyopathy
B. Infective endocarditis
C. Degenerative valvular disease
D. Connective tissue disease
E. Congenital valvular disease
409. Vegetations on undersurface of A.V. valves are found in:
A. *Limban Sack's endocarditis
B. Acute Rheumatic corditis
C. Non thrombotic bacterial endocarditis
D. Chronic rheumatic carditis
E. MVP
410. What group of drugs has a significant role in the treatment of the patients with severe carditis
accompanied by congestive heart failure:
A. *steroids
B. salicylates
C. cefazolin
D. erythromycin
E. heparin
411. What investigation can detect vegetations in approximately 90% of patients with proven
endocarditis:
A. *Transoesophageal echocardiogram
B. Echocardiogram
C. ECG
D. Chest X-ray
E. CT
412. What is duration of the antibiotic treatment of the patients with acute rheumatic fever?
A. *not less then two weeks
B. not less then 20 days
C. not less then a week
D. not less then 5 days
E. not less then a month
413. Which cardiac valve is most frequently affected as a result of rheumatic fever?
A. *Mitral
B. Aortic
C. Tricuspid
D. Pulmonic
E. Mitral and Pulmonic
414. What is specific for rheumatic fever?
A. *Subcutaneous nodule
B. Erythema marginatum
C. Osler's nodes
D. Erythema nodosum
E. Janeways lesions
415. Which of the following are immune complex lesions in infective endocarditis
A. *Oslers nodes
B. mycotic aneurysms
C. anemia
D. vegetations
E. meningitis
416. Which of the following is the most common late manifestation of acute rheumatic fever?
A. *Chorea
B. Pharyngitis
C. Erythema marginatum
D. Iritis
E. Enthesopathy
417. Which of the following is not one of the major Jones criteria for the diagnosis of rheumatic fever?
A. *Urethritis
B. Carditis
C. Arthritis
D. Chorea
E. Erythema marginatum
418. Which of the following statements best characterized tricuspid regurgitation?
A. *Infective endocarditis is a common cause
B. The murmur heard in tricuspid regurgitation decreases with inspiration
C. Large a waves in jugular venous pulse are characteristic
D. Correction of coexistent left ventricular failure rarely improves the condition
E. Cardiac catheterization is required for the diagnosis
419. 79 y/o female with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly
elevated. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. Osteoarthritis
D. *Chronic Gouty arthritis
E. Psoriatic arthritis
420. A 25-yr-old man presents with a 10-yr history of back pain, peripheral arthritis, worse in the
morning and one episode of iritis. Choose the medications from the below list of options.
A. *Methotrexate
B. Actovegin
C. Mydocalm
D. Warfarin
E. Pentoxifylline
421. Echocardiographic findings for infective endocarditis are all of the following EXCEPT:
A. *New valvar stenosis
B. Mobile echo dense masses attached to valve leaflets or endocardium
C. Periannular abscesses
D. New dehiscence of a prosthetic valve
E. New valvar regurgitation
422. Feature that distinguish rheumatic fever from myocarditis:
A. *migratory arthritis
B. ST-T-wave abnormalities
C. Arrhythmias
D. heart failure
E. tachycardia.
423. Feature that distinguishes rheumatic heart diseases from infective endocarditis is:
A. *vegetations
B. Doppler echocardiographic restriction of mitral valve leaflets, their calcification
C. pulmonary hypertension
D. cardiomegaly
E. syncope.
424. Immunological phenomena in infective endocarditis are all of the following EXCEPT:
A. *Erythema marginatum
B. glomerular nephritis
C. rheumatoid factor
D. Osler's nodes
E. Roth spots
425. In which disease we expect to see vegetations?
A. *Infective endocarditis
B. Viral myocarditis
C. Acute pericarditis
D. Rheumatic heart disease
E. Hypertrophied cardiomyopathy
426. Low serum complement levels would be seen in patients with hematuria, proteinuria resulting from
all of the following EXCEPT
A. *Henoch-Schonlein purpura
B. diffuse proliferative lupus nephritis
C. hepatitis C-associated membranoproliferative glomerulonephritis
D. streptococcal infective endocarditis glomerulonephritis
E. rheumatism
427. Major criteria of rheumatic fever are the following EXCEPT:
A. *Recent group A streptococcal infection
B. Carditis
C. Migratory polyarthritis
D. Sydenham's chorea
E. Erythema marginatum
428. Migrating polyarthritis is characteristically seen in
A. *rheumatic arthritis
B. syphilitic arthritis
C. rheumatoid arthritis
D. psoriatic arthritis
E. gouty arthritis
429. Migratory polyarthritis in rheumatic fever most often affecting following joints except:
A. *small joints of hands
B. the ankles
C. wrists
D. knees
E. elbows
430. Minor criteria for infective endocarditis are all of the following EXCEPT:
A. *Migratory arthritis
B. Fever >38В°C
C. Embolic/vascular phenomena
D. Immunological phenomena
E. Blood cultures compatible but not typical for endocarditis
431. Minor Criterion of rheumatic fever is:
A. *Prolonged P-Q interval
B. sinus tachycardia
C. sinus bradycardia
D. inversion of T waves
E. ectopic beats
432. Noncardiac Manifestations of infective endocarditis are the following except:
A. *a rash on the trunk and proximal extremities
B. splenomegaly
C. petechiae
D. arterial emboli
E. Osler's nodes
433. Patients with acute rheumatic fever in initial attack have evidence of carditis, which may be
characterized by all are the following EXCEPT:
A. sinus tachycardia
B. the murmur of mitral regurgitation
C. an S3 gallop
D. *the first heart sound is accentuated
E. cardiomegaly
434. Patients with acute rheumatic fever in initial attack have evidence of carditis, which may be
characterized by all are the following EXCEPT:
A. *the first heart sound is accentuated
B. sinus tachycardia
C. the murmur of mitral regurgitation
D. an S3 gallop
E. cardiomegaly
435. Rheumatic fever caused by:
A. *beta-hemolytic streptococci.
B. Staphylococcus lugdunensis
C. Enterococci
D. The HACEK group
E. H. influenza
436. 79 y/o female with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly
elevated. Which of the following medications is indicated for the treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
437. 86 year old male with chronic gout presents with bilateral foot pain. Physician desired radiograph
for evaluation of extent of pathologic changes. Prominent erosive destruction of bilateral first metatarsals
and second distal phalanx with well-preserved joint spaces throughout. Choose the most likely changes
from the below list of options.
A. High ESR
B. Oseoporosis on X-ray
C. Positive blood culture
D. *Urate crystals on joint aspirate
E. Positive rheumatoid factor
438. A 27-yr-old man presents with a 10-yr history of back pain, peripheral arthritis worse in the
morning and one episode of iritis. Choose the medications for patient with shown changes from the
below list of options.
A. *Sulfasalazine
B. Actovegin
C. Mydocalm
D. Warfarin
E. Pentoxifylline
439. A 50-yr-old woman complains of stiffness in her fingers worse at the end of the day. The DIP joints
and the first metacarpophalangeal joints are affected. Choose the most likely diagnosis from the below
list of options.
A. *Osteoarthritis
B. Rheumatoid arthritis
C. Psoriatic arthropathy
D. Haemochromatosis
E. Gonococcal arthritis
440. A 50-yr-old woman complains of stiffness in her fingers worse at the end of the day. The DIP joints
and the first metacarpophalangeal joints are affected. Choose the most likely diagnosis from the below
list of options.
A. Rheumatoid arthritis
B. Psoriatic arthropathy
C. *Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
441. A 53-yr-old woman complains of redness, swelling and stiffness in the distal interphalangeal joints
of her hands, but has no other joint complaints. Choose the most likely diagnosis from the below list of
options.
A. Gout
B. Still's disease
C. Pseudogout
D. Rheumatoid arthritis
E. *Osteoarthritis
442. A 57-year-old woman has had five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. Her most recent episode was 4 months ago. Classical picture of
exacerbation of the arthritis includes all of the following except
A. Excruciating and sudden pain
B. Low-grade fever may also be present
C. *Overgrowth at the distal interphalangeal joints
D. Warmness
E. Redness
443. A 60-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint and a lesion
on the rim of the left pinna. Choose the investigation for diagnosis from the below list of options.
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
444. A 63-year-old man is evaluated because of a 2-year history of bilateral knee pain and low back
pain. He has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, he has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
right knee. Which of the following treatment do use?
A. Methotrexat
B. Colchicines
C. *Chondroitin sulfate
D. Tetracycline
E. Allopurinol
445. A 65-year-old man comes to your office complaining of knee pain that began insidiously about a
year ago. He has no other rheumatic symptoms. Which of the following signs is not sign of the arthritis?
A. Pain is related to use
B. Pain gets worse during the day
C. Minimal morning stiffness (<20 min) and after inactivity (gelling)
D. *Warmth of skin over effected joints
E. Range of motion decreases
446. A 65-year-old man comes to your office complaining of knee pain that began insidiously about a
year ago. He has no other rheumatic symptoms. Which of the following signs isn’t sign of the arthritis?
Which of the following signs isn’t sign of the arthritis?
A. Joint instability
B. Bony enlargement
C. Restricted movement
D. Crepitus
E. *Tophi
447. A 65-yr-old man has started chemotherapy for lymphoma. He has developed a painful swollen hot
right knee. He is apyrexial. Choose the most likely changes from the below list of options.
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
448. A 55-yr-old man has started chemotherapy for CML. He has developed a painful swollen hot right
knee. He is apyrexial. Choose the most likely diagnosis from the below list of options.
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
449. A 68-year-old man presents with an acutely red and swollen right great toe without history of
trauma. Which of the following findings is most useful for making a diagnosis of gout in this patient?
A. Persistent elevation of serum uric acid
B. Good response to colchicines trial
C. *Radiograph showing marginal joint erosion in the first metatarso-phalangeal (MTP) joint
D. An associated right ankle effusion
E. A painless elbow nodule
450. A 70-yr-old woman complains of arthritis in the fingers and big toe. On examination she has bony
swellings of the first carpometacarpal joint and the distal interphalangeal joints and has an affected
metatarsophalangeal joint. Choose the most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Hyperparathyroidism
C. Psoriatic arthropathy
D. *Osteoarthritis
E. Haemochromatosis
451. 73-yr-old fit farmer presents with pain on weight bearing and restricted movements of the right hip.
Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
452. All of the following are X-ray signs of Osteoarthritis except
A. Joint space narrowing
B. Marginal osteophytes
C. Subchondral cysts
D. Bony sclerosis
E. *Marginal erosions
453. A 73-yr-old fit farmer presents with pain on weight bearing and restricted movements of the right
hip. Choose the most likely X-ray changes from the below List of options.
A. Cystic changes and lytic lesions
B. *Joint spaces are narrowed with reactive subchondral sclerosis, osteophytes
C. Periarticular osteopenia, marginal erosions
D. acroosteolysis
E. Fluffy bone periostitis and erosions at the interphalangeal joints
454. All of the following physical findings may be seen in osteoarthritis except
A. Heberden nodes
B. Bouchar nodes
C. Bony crepitus on joint movement
D. Bounniere deformity
E. *Acute arthritis of metatarsophalangeal joints.
455. An elderly man presents with a red, warm swollen metatarsophalangeal joint following a right total
hip replacement operation. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Reactive arthritis
C. Osteoarthritis
D. *Acute Gouty arthritis
E. Psoriatic arthritis
456. An elderly man started frusemide 2-weeks ago and now presents with a red, hot, swollen first
metatarsal phalangeal joint. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Joint sepsis
C. Osteoarthritis
D. *Gout
E. Psoriatic arthritis
457. Classical picture of acute gouty arthritis includes all of the following except
A. Excruciating and sudden pain
B. Stiffness in the joint
C. Low-grade fever may also be present
D. Warmness
E. *Overgrowth at the distal interphalangeal joints
458. Each of the following agents may be useful in the treatment of acute gouty arthritis except
A. indomethacin
B. *allopurinol
C. colchicines
D. intraarticular glucocorticoids
E. aspirin
459. Each of the following may cause hyperuricemia and thereby may provoke an attack of gouty
arthritis except
A. thiazide diuretics
B. exercise
C. cyclosporine
D. methotrexate
E. *ascorbic acid
460. Gouty arthritis is characterized by:
A. chiefly involvement of the lumbosacral portion of spine;
B. gradual onset;
C. frequently associated with renal disease;
D. absence of renal disease;
E. *involvement of the first metatarsophalanges joint.
461. Hyperuricemia is defined as a serum uric acid concentration above
A. *7 mg per dL (420 Вµmol per L).
B. 4 mg per dL (240 Вµmol per L).
C. 5 mg per dL (300 Вµmol per L).
D. 8 mg per dL (480 Вµmol per L).
E. 9 mg per dL (540 Вµmol per L).
462. Overproduction of urate may be in all of the following except
A. Primary idiopathic hyperuricemia
B. *Hypertension
C. Hemolytic processes
D. Lymphoproliferative disease
E. Myeloproliferative disease
463. Overproduction of urate may be in all of the following except
A. Polycythemia vera
B. Psoriasis (severe)
C. *Peptic ulcer
D. Exercise
E. Alcohol
464. Patients with gouty arthritis characterized by any of the following clinical characteristics except:
A. tophaceous deposits
B. *rheumatoid factor positive
C. "punched out" erosive changes on radiographs
D. acute attack frequency of greater than or equal to 2 attacks per year
E. hyperuricemia
465. Risk factors and possible causes of osteoarthritis. Risk factors and possible causes of osteoarthritis
are all of the following except
A. Age
B. Obesity
C. *Stress
D. Prior injury
E. Acromegaly
466. Secondary osteoarthritis may be caused by all of except
A. Hemaphilia
B. Hemochromatosis
C. Gouty arthritis
D. *Diabetes mellitus
E. After trauma
467. Side effects of colchicines are all of the following except
A. Neutropenia
B. Nausea
C. Diarrhea
D. Anemia
E. *Headache
468. Signs of osteoarthritis are all of the following except
A. Limp
B. Muscle atrophy
C. Crepitus
D. Restricted movement
E. *Warmth of skin over effected joints
469. The client has just been diagnosed with chronic gout. Which tablets should be prepared to teach
about side effects and precautions to this client?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
470. The client is being admitted for a total hip replacement. She says that she is glad she will be having
anesthesia shortly because she has a painful abscessed tooth and is taking an antibiotic for it. What is the
best action?
A. Take the client's temperature
B. *Notify the surgeon immediately
C. Document the report as the only action
D. Arrange for the client to receive the antibiotic intravenously
E. Sent patient to dentist
471. The client with arthritis and all the following allergies is prescribed to take celecoxib (Celebrex)
daily. Which allergy is most important for the nurse to report to the physician?
A. Latex
B. Peanut
C. Shellfish
D. *Sulfa drugs
E. Aspirin
472. Which activity should be suggested to the client with osteoarthritis as being most likely to slow the
development of disabilities associated with osteoarthritis?
A. Eating less red meat and starchy vegetables
B. Avoiding any form of physical exercise
C. *Swimming 3 times per week
D. Taking an aspirin daily
E. Taking an ascorbic acid daily
473. Which client is most likely to develop secondary gout?
A. *60-year-old man with renal insufficiency
B. 60-year-old woman with type 2 diabetes mellitus
C. 40-year-old woman who has been taking oral contraceptives for 15 years
D. 40-year-old male athlete who has been taking NSAIDs for a sprained ankle
E. 40-year-old drug abuser
474. Which client is most likely to develop secondary gout?
A. *56-year-old man with Polycythemia vera
B. 56-year-old woman with type 2 diabetes mellitus
C. 33-year-old woman who has been suffering from SLE last 3 years
D. 40-year-old male athlete who has been taking NSAIDs for a sprained ankle
E. 40-year-old drug abuser
475. Which condition or action represents a modifiable risk factor for osteoarthritis?
A. *Obesity
B. Hypertension
C. Cigarette smoking
D. Walking as exercise
E. Fatty foods
476. Which condition or health problem demonstrates inflammation without invasion?
A. Allergic rhinitis
B. Viral hepatitis
C. *Osteoarthritis
D. Cellulitis
E. Septic arthritis
477. Which joints are most frequently affected by osteoarthritis?
A. Jaw and ankles
B. Neck and wrists
C. *Hips and knees
D. Elbows and shoulders
E. Thoracic spine and shoulders
478. Which of the following is a sign for Gouty arthritis?
A. Simultaneous involvement of the same joint areas on both sides of the body.
B. *Acute arthritis of first metatarsophalangeal joint
C. Symmetric sacroilitis
D. Asymmetric sacroilitis
E. Nonerosive arthritis
479. Which of the following is characteristic of Osteoarthritis?
A. Severe night pain
B. Morning stiffness
C. *Short starting stiffness
D. Weight loss
E. Asymmetric joint involvement
480. Which of the following joint findings is most suggestive of an inflammatory, rather than an
osteoarthritic, cause of joint pain?
A. Painful range of motion
B. Crepitus
C. Bony articular enlargement
D. *Swelling and warmth
E. Instability
481. Which of the following medications is contraindicated for the treatment of an acute attack of gout?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
482. Which physical change in the client with osteoarthritis indicates disease advancement?
A. The hands are involved
B. *The hip shows subluxation
C. Hip involvement is bilateral.
D. The client is older than 65 years
E. Shoulders involvement
483. Which statement made by the client with gout indicates a need for further teaching regarding the
management of this disorder?
A. have been drinking at least 3 liters of water each day
B. *When the pain is very bad, I have a drink of my favorite wine.
C. Although my favorite food is shrimp, I no longer have it on a regular basis.
D. My wife and I are substituting chicken and other poultry for red meat these days.
E. Although my favorite food is mushrooms, I no longer have it on a regular basis.
484. Which X-ray changes are specific for osteoartrosis?
A. Syndesmophytes
B. *Osteophytes
C. Fractures
D. Erosions
E. Osteoporosis
485. Male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in the DIP of
the right first toe, with calcifications. Further questioning revealed a history of repeated attacks of acute
joint pain. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Chronic gouty arthritis
E. Psoriatic arthritis
486. A 22-yr-old male soldier presents with a 2-week history of a swollen right knee, conjunctivitis and
arthritis. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Psoriatic arthritis
C. Joint sepsis
D. *Reactive arthritis
E. Rheumatoid arthritis
487. Disease-modifying' antirheumatic drugs for rheumatoid arthritis are all of the following except
A. *NSAIDs
B. Hydroxychloroquine sulphate
C. Sulphasalazine
D. Methotrexate
E. D-penicillamine
488. A 15-yr-old boy complains of pain in the temperomandibular joint for 3 months. On examination,
the SHO in A&E notices micrognathia, loss of neck extension and unequal lengths of the boy's lower
limbs. Tests for rheumatoid factor were negative. Choose the most likely diagnosis from the below list of
options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
489. A 25-yr-old man presents with urethritis, conjunctivitis and a swollen left knee. Choose the most
likely diagnosis from the below list of options.
A. *Reiter's syndrome
B. Psoriatic arthropathy
C. Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
490. A 30-yr-old flight attendant presents with gritty eyes and painful knees especially during standing.
He has just returned from Thailand Choose the most likely diagnosis from the below list of options.
A. *Reactive arthritis
B. Ankylosing spondylitis
C. Psoriatic arthritis
D. Joint sepsis
E. Rheumatoid arthritis
491. A 31-yr-old travel agent presents with painful knees, red eyes and dysuria. Choose the most likely
diagnosis from the below list of options.
A. Polyarteritis nodosa
B. Giant cell arteritis
C. Rheumatoid arthritis
D. Ankylosing spondylitis
E. *Reiter's syndrome
492. A 41-yr-old woman presents with painful knees, red eyes and dysuria. She has just returned from a
trip. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Psoriatic arthritis
C. Joint sepsis
D. *Reiter's syndrome
E. Polyarteritis nodosa
493. A 32-yr-old man presents with rash on his penis, pain in the left heel and right-sided stiffness in the
lower back upon rising in the morning. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Psoriatic arthritis
C. Joint sepsis
D. *Reactive arthritis
E. Polyarteritis nodosa
494. A 44-yr-old woman presents with stiff, sausage-shaped fingers and MCP joint swelling worse in the
morning. Choose the most likely diagnostic antibody for the disease from the below list of options.
A. Antimicrosomal antibody
B. Antireticulin antibody
C. Anti-dsDNA
D. P-ANCA antibody
E. *Rheumatoid factor, anti-CCP
495. A 35-yr-old woman has pain and stiffness in her hands, wrists, elbows, knees and ankles. There is
swelling of her MCP joints bilaterally. There is a nodule on her left elbow. Choose the most likely
diagnosis from the below list of options
A. High ESR
B. High serum urate
C. Positive blood culture
D. *Positive rheumatoid factor
E. High WBC count
496. A 36-yr-old lady presented with swollen tender knee joints. She says they feel stiff especially in the
mornings. On examination she was found to have splenomegaly, a temperature of 38В°C and ulcerated
lower limbs with Hb9 g/dl. WBC and platelets were decreased. Albumin was 20 g/l. Choose the most
likely diagnosis from the below list of options.
A. Gout
B. Still's disease
C. Felty's syndrome
D. *Rheumatoid arthritis
E. Osteoarthritis
497. A 43-year-old woman has experienced morning stiffness, swelling of the small joints of hands,
wrists, knees, ankles, elbows. The proximal interphalangeal joints are fusiform swelling. X-ray
examination of which joints you need for confirming diagnosis?
A. *Hands
B. Ankles
C. Knees
D. Elbows
E. Spine
498. A 52 -yr-old woman presents with stiff, sausage-shaped fingers and MCP joint swelling worse in
the morning (within 2 hours). Choose the most likely diagnostic antibody for the disease from the below
list of options.
A. *Rheumatoid factor
B. Antimicrosomal antibody
C. Antireticulin antibody
D. Anti-dsDNA
E. P-ANCA antibody
499. A 48-year-old man complains of joint pain and stiffness for the past 3 months. All of the following
are signs of rheumatoid arthritis (RA) except
A. early morning stiffness lasting 1 hour
B. *numbness and blanching of fingers on exposure to cold
C. symmetrical involvement of the metacarpophalangeal joints
D. a non-tender subcutaneous mass over the Achilles tendon
E. synovial fluid with high viscosity and 30,000 lymphocytes/mm3
500. 71-yr-old woman with longstanding polyarthritis on immunosuppressive drugs presents with
systemic malaise and fever and has severe pain, redness, heat and swelling of the wrist. Choose the most
likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Joint sepsis
C. Osteoarthritis
D. Gout
E. Psoriatic arthritis
501. A woman who has rheumatoid arthritis suddenly develops pain and swelling in the right calf. The
most likely diagnosis is
A. ruptured plantaris tendon
B. pes anserinus bursitis
C. *ruptured popliteal cyst
D. thrombophlebitis
E. Achilles tendonitis
502. A young man complains of red and sore eyes, painful urination and low back pain. Nine months
ago he had UTI and was successfully treated for it. Choose the treatment from the below list of options
A. Cyclophosphanum
B. Penicillin
C. Prednisone
D. Ceftriaxone
E. *Tetracycline
503. An 18-year-old woman comes to the emergency department complaining of severe right knee, right
wrist, and left ankle pain, morning stiffness. Physical examination also reveals tenderness and swelling of
involved joints. While awaiting results of laboratory testing, this patient should receive which of the
following treatments?
A. Corticosteroids
B. *Nonsteroidal anti-inflammatory drugs (NSAIDs)
C. Antibiotics
D. Local care of skin lesions
E. Splinting of painful joints
504. An 28-year-old woman comes to the emergency department complaining of severe knees, wrists,
and ankles pain, morning stiffness. Physical examination also reveals tenderness and swelling of
involved joints. Choose the most likely diagnosis for patient with shown changes from the below list of
options.
A. Ankylosing spondylitis
B. *Rheumatoid arthritis
C. Osteoarthritis
D. Gout
E. Psoriatic arthritis
505. Arthritis associated with rheumatoid arthritis can be manifest in several different ways. Which of
the following is characteristic of rheumatoid arthritis
A. asymmetric oligoarticular arthritis
B. *rheumatoid factor-positive symmetric polyarthritis
C. arthritis of distal interphalangeal joints
D. severe destructive polyarthritis (arthritis mutilans)
E. spondilitis and sacroiliitis with or without peripheral arthritis
506. Association of arthritis and urethritis is typical for:
A. Reynolds’s phenomen;
B. RA;
C. Psoriatic arthritis;
D. *Reiters syndrome;
E. ankylosing spondilitis;
507. Which disease has ulnar deviation more often?
A. *Rheumatoid arthritis
B. Gout
C. Still's disease
D. Pseudogout
E. Osteoarthritis
508. Choose the most likely diagnostic antibody for Rheumatoid arthritis from the below list of options.
A. Antimicrosomal antibody
B. Antireticulin antibody
C. Anti-dsDNA
D. P-ANCA antibody
E. *Rheumatoid factor
509. Each of the following agents has been demonstrated to alter the course of rheumatoid arthritis
except
A. gold
B. *omega-3 fatty acid
C. methotrexate
D. D-penicillamine
E. Hydroxychloroquine
510. Felty’s syndrome occurs in patients with seropositive rheumatoid arthritis with all of the following
except
A. Neutropenia
B. Thrombocytopenia
C. Anemia
D. *lymphocytopenia
E. splenomegaly
511. For arthritis in Rheumatoid arthritis more typical is:
A. starting pain;
B. night pain;
C. *morning stiffness;
D. weight loss;
E. asymmetric joint involvement;
512. For rheumatoid arthritis more typical is
A. *morning stiffness;
B. starting pain;
C. night pain;
D. weight loss;
E. asymmetric joint involvement;
513. How often patients with Rheumatoid arthritis have Rheumatoid factor positive?
A. 60 %
B. 65 %
C. 75 %
D. *85 %
E. 90 %
514. How often patients with Rheumatoid arthritis have anti-cyclic citrullinated peptide?
A. *98 %
B. 92 %
C. 67 %
D. 78 %
E. 85 %
515. Lung disorders in rheumatoid arthritis may include all of the following except
A. pleuritis (with effusions characterized by low glucose)
B. *pulmonary thromboembolism
C. interstitial fibrosis
D. nodules
E. Caplans syndrome
516. Reactive arthritis may be caused by all of the following enteric infection except
A. Salmonella typhimurium
B. Shigella flexneri
C. Yersinea enterocoliticas
D. *Chlamydia trachomatis
E. Campylobacter jejuni
517. Reiters syndrome is more frequently a response to
A. infection with shigella;
B. infection with staphylococci;
C. infection with salmonella;
D. infection with streptococci;
E. *infection with Chlamydia.
518. Side-effects of NSAIDs include all of the following except
A. fluid retention
B. upper gastrointestinal haemorrhage
C. *hypotension
D. interstitial nephritis
E. agranulocytosis
519. The diagnosis of rheumatoid arthritis is based entirely on clinical grounds. Choose correct clinical
characteristics associated with rheumatoid arthritis
A. *prolonged morning stiffness
B. migratory polyarthritis
C. arthritis involving the distal interphalangeal joints
D. arthritis involving the sacroiliac joints
E. night painfull arthritis
520. The client is being admitted for a total hip replacement. She says that she is glad she will be having
anesthesia shortly because she has a painful abscessed tooth and is taking an antibiotic for it. What is the
best action?
A. Take the client's temperature
B. *Notify the surgeon immediately
C. Document the report as the only action
D. Arrange for the client to receive the antibiotic intravenously
E. Sent patient to dentist
521. The client on long-term corticosteroid therapy for rheumatoid arthritis has developed abdominal
striae. Side effect of which drug may cause pitting edema of both legs?
A. *Prednisone
B. Methotrexat
C. Folic acid
D. NSAIDs
E. None of the above
522. Patient with arthritis and all the following allergies is prescribed to take celecoxib (Celebrex) daily.
Which allergy is most important for the nurse to report to the physician?
A. Latex
B. Nut
C. Shellfish
D. *Sulfasalasini
E. Diclofenacy
523. The older adult client taking prednisone, methotrexate, folic acid, NSAIDs for rheumatoid arthritis
now has pitting edema of both legs. Side effect of which drug may cause pitting edema of both legs?
A. Prednisone
B. Methotrexat
C. folic acid
D. *NSAIDs
E. None of the above
524. This patient will likely develop bilateral inflammation of the proximal interphalangeal and
metacarpophalangeal joints and the wrists.
A. This patient is positive for antinuclear antibody.
B. This patient has a history of antecedent bloody diarrhea.
C. Knee arthrocentesis will reveal intracellular monosodium urate crystals.
D. This patient has a history of antecedent UTI
E. *This patient is positive for rheumatoid factor.
525. What precaution is most important to teach the client with rheumatoid arthritis who will be taking
20 mg of prednisone daily?
A. Take this drug at bedtime.
B. *Avoid crowds and anyone who is ill
C. Drink at least 3 liters of fluid per day.
D. Wash your face 3 times per day with an antibacterial soap.
E. Avoid sunlight.
526. What factor or condition in the client who has joint stiffness and pain is more associated with
progressive systemic sclerosis than with rheumatoid arthritis?
A. The client is female
B. The pain is worse in the morning
C. The client has never been pregnant
D. *The fingers are sausage-like, with nonpitting edema
E. The client has limited motion
527. What precaution is most important to teach the client with rheumatoid arthritis who will be taking
methotrexate?
A. *Avoid sunlight.
B. Take this drug at bedtime.
C. Avoid crowds and anyone who is ill.
D. Drink at least 3 liters of fluid per day.
E. Wash your face 3 times per day with an antibacterial soap.
528. Which change is characteristic of Reiters syndrome?
A. *Dactylitis
B. Bamboo Spine
C. Erosive arthritis of wrists
D. Acute arthritis of metatarsophalangeal joint
E. Subcutaneous nodules
529. Which clinical manifestation in a male client with arthritis indicates or suggests the possibility of
Reiter's syndrome?
A. Stooped posture
B. Unplanned weight loss
C. *Pain/burning on urination
D. Ringing in the ears at night
E. Dry eyes
530. Which clinical manifestation would be an unexpected finding in a patient with rheumatoid arthritis?
A. Anemia
B. Warm, tender joints
C. Symmetric and bilateral joint involvement
D. Elevated ESR
E. *Crepitus of involved joints
531. Which following drug doesn’t alter the course of rheumatoid arthritis?
A. *NSAIDs
B. Hydroxychloroquine sulphate
C. Sulphasalazine
D. Methotrexate
E. D-penicillamine
532. Which joints of the body may be involved in rheumatoid arthritis mainly?
A. hips;
B. *small joints of hands
C. ankles;
D. shoulders;
E. sacroiliac joints
533. Which of the following clinical predictors is not associated with severe and progressive rheumatoid
arthritis?
A. Persistent swelling of the proximal interphalangeal joints
B. High C-reactive protein level or elevated erythrocyte sedimentation rate
C. *Swelling of the distal interphalangeal joints
D. Large number of swollen joints
E. High titers of rheumatoid factor
534. Which of the following conditions is LEAST likely to occur in late extraarticular seropositive
rheumatoid arthritis?
A. Neutropenia
B. Dry eyes
C. Leg ulcers
D. Sensorimotor polyneuropathy
E. *Hepatitis
535. A 70-yr-old fit farmer presents with pain on weight bearing and restricted movements of the right
hip. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
536. An elderly man started frusemide 4-weeks ago and now presents with a red, hot, swollen first
metatarsal phalangeal joint. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Joint sepsis
C. Osteoarthritis
D. *Gout
E. Psoriatic arthritis
537. A 50-yr-old woman complains of redness, swelling and stiffness in the distal interphalangeal joints
of her hands, but has no other joint complaints. Choose the most likely diagnosis from the below list of
options.
A. Gout
B. Still's disease
C. Pseudogout
D. Rheumatoid arthritis
E. *Osteoarthritis
538. A 55-yr-old woman complains of stiffness in her fingers worse at the end of the day. The DIP joints
and the first metacarpophalangeal joints are affected. Choose the most likely diagnosis from the below
list of options.
A. *Osteoarthritis
B. Rheumatoid arthritis
C. Psoriatic arthropathy
D. Haemochromatosis
E. Gonococcal arthritis
539. A 68-yr-old woman complains of arthritis in the fingers and big toe. On examination she has bony
swellings of the first carpometacarpal joint and the distal interphalangeal joints and has an affected
metatarsophalangeal joint. Choose the most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Hyperparathyroidism
C. Psoriatic arthropathy
D. *Osteoarthritis
E. Haemochromatosis
540. An 67-yr-old man presents with a red, warm swollen metatarsophalangeal joint following a surgical
treatment. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Reactive arthritis
C. Osteoarthritis
D. *Acute Gouty arthritis
E. Psoriatic arthritis
541. A 58-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint and a lesion
on the rim of the right pinna. Choose the investigation for diagnosis from the below list of options.
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
542. A 60-yr-old man has started chemotherapy for CML. He has developed a painful swollen hot right
knee. Choose the most likely changes from the below list of options.
A. *Hyperurecemia
B. Erosions on X-ray
C. Positive blood culture
D. Positive rheumatoid factor
E. High ESR
543. On physical examination, internal rotation of the left hip elicits the groin pain. The second, third,
and fourth metacarpophalangeal joints are swollen, warm, and tender to pressure. Radiographs show
severe osteoarthritis in the left hip. Which of the following is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. *Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. Serum uric acid
544. Which of the following is a sign for Gouty arthritis?
A. Simultaneous involvement of the same joint areas on both sides of the body.
B. *Acute arthritis of first metatarsophalangeal joint
C. Symmetric sacroilitis
D. Asymmetric sacroilitis
E. Positive RF
545. A 70-year-old woman has had four or five episodes of joint pain and swelling, lasting 2 to 7 days,
involving the right knee and left elbow. On physical examination, none of her joints is swollen or tender,
but there is marked crepitus on extension of the knee. She also has a positive bulge sign over the left knee
and pain on full extension of the left elbow. Which one of the following tests would confirm the
diagnosis?
A. *Arthrocentesis of the knee and laboratory analysis of the synovial fluid
B. Measurement of serum uric acid
C. Measurement of serum rheumatoid factor
D. Radiograph of the knee
E. MRI of the knee with gadolinium contrast
546. A 73-year-old retired patient is evaluated because of swelling of his right knee. On physical
examination, he has an effusion in the right knee. At a point in the mid-thigh (measured from the superior
border of the patella), the right thigh is 5 cm smaller in diameter than the left. There is crepitus with right
knee flexion. The knee is not warm. Which of the following is the best next step in the management of
this patient?
A. Order radiographs of both knees and treat the patient with ibuprofen.
B. Order radiographs of the right hip and right knee.
C. *Aspirate the joint fluid in the right knee and refer the patient for physical therapy.
D. Aspirate the joint fluid in the right knee and obtain blood cultures.
E. Treat the patient with celecoxib, and advise him to stay off his feet for 48 hours.
547. Which of the following joint findings is most suggestive of rheumatoid arthritis, rather than an
osteoarthritic, cause of joint pain?
A. Painful range of motion
B. Crepitus
C. Bony articular enlargement
D. *Swelling and warmth
E. Instability
548. A 62-year-old woman has ostheoarthritis II stage. Which of the following treatment do use?
A. methotrexat
B. *intra-articular injection of sodium hyaluronate
C. probenecid
D. colchicine
E. allopurinol.
549. All of the following physical findings may be seen in osteoarthritis except
A. Heberden’s nodes
B. Bouchar’s nodes
C. Bony crepitus on joint movement
D. Bounniere deformity
E. *Acute arthritis of metatarsophalangeal joints.
550. Each of the following may cause hyperuricemia and thereby may provoke an attack of gouty
arthritis except
A. thiazide diuretics
B. exercise
C. cyclosporine
D. methotrexate
E. *ascorbic acid
551. Each of the following agents may be useful in the treatment of acute gouty arthritis except
A. diclofenak
B. *allopurinol
C. colchicines
D. intraarticular injection of sodium hyaluronate
E. aspirin
552. Which condition or health problem demonstrates osteophytes?
A. Allergic rhinitis
B. Viral hepatitis
C. *Osteoarthritis
D. Cellulitis
E. Septic arthritis
553. Gouty arthritis is characterized by:
A. chiefly involvement of the lumbosacral portion of spine;
B. gradual onset;
C. frequently associated with renal disease;
D. absence of renal disease;
E. *Acute attack of the arthritis of first metatarsophalanges joint.
554. Which joints are often affected by osteoarthritis?
A. Jaw and ankles
B. Neck and wrists
C. *Distal interphalangeal joints
D. Elbows and shoulders
E. Thoracic spine and shoulders
555. Patient with which condition or action represents a modifiable risk factor for osteoarthritis?
A. *Obesity
B. Hypertension
C. Cigarette smoking
D. Walking as exercise
E. Fatty foods
556. Which physical change in the patient with osteoarthritis indicates disease advancement?
A. The hands are involved
B. *The hip shows aseptic necrosis
C. Hip involvement is bilateral.
D. The client is older than 65 years
E. Shoulders involvement
557. Which activity should be suggested to the client with osteoarthritis as being most likely to slow the
development of disabilities associated with osteoarthritis?
A. Eating less red meat and starchy vegetables
B. Avoiding any form of physical exercise
C. *Swimming 3 times per week
D. Taking an aspirin daily
E. Taking an ascorbic acid daily
558. Which statement made by the client with gout indicates a need for further teaching regarding the
management of this disorder?
A. “I have been drinking at least 3 liters of water each day.”
B. * “When the pain is very bad, I have a drink of my favorite wine.”
C. “Although my favorite food is shrimp, I no longer have it on a regular basis.”
D. “My wife and I are substituting chicken and other poultry for red meat these days.”
E. “Although my favorite food is mushrooms, I no longer have it on a regular basis.”
559. The client with arthritis and all the following allergies is prescribed to take celecoxib (Celebrex)
daily. Which allergy is most important for the nurse to report to the physician?
A. Latex
B. Peanut
C. Shellfish
D. *Sulfa drugs
E. Aspirin
560. The client is being admitted for a total hip replacement. She says that she is glad she will be having
anesthesia shortly because she has a painful abscessed tooth and is taking an antibiotic for it. What is the
best action?
A. Take the client's temperature
B. *Notify the surgeon immediately
C. Document the report as the only action
D. Arrange for the client to receive the antibiotic intravenously
E. Sent patient to dentist
561. The client has just been diagnosed with chronic gout. Which tablets should be prepared to teach
about side effects and precautions to this client?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
562. Which client is most likely to develop secondary gout?
A. *60-year-old man with renal insufficiency
B. 60-year-old woman with type 2 diabetes mellitus
C. 40-year-old woman who has been taking oral contraceptives for 15 years
D. 40-year-old male athlete who has been taking NSAIDs for a sprained ankle
E. 40-year-old drug abuser
563. Which client is most likely to develop secondary gout?
A. *56-year-old man with Polycythemia vera
B. 56-year-old woman with type 2 diabetes mellitus
C. 33-year-old woman who has been suffering from SLE last 3 years
D. 40-year-old male athlete who has been taking NSAIDs for a sprained ankle
E. 40-year-old drug abuser
564. Which of the following is characteristic of Osteoarthritis?
A. *Short starting stiffness
B. Severe night pain
C. Morning stiffness
D. Weight loss
E. Asymmetric joint involvement
565. A 64-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. The
patient says that her mother had “the same fingers” and she worries that she will become crippled.
Choose the most likely diagnosis from the below list of options.
A. *Osteoarthritis
B. Ankylosing spondylitis
C. Rheumatoid arthritis
D. Gout
E. Psoriatic arthritis
566. A 64-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. On
physical examination, there is crepitus on passive motion of the left knee, which has a slight varus (“bow
leg”) deformity. Her feet turn out slightly, and the heels are in valgus. Which of the following changes
will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
567. A 73-yr-old fit farmer presents with pain on weight bearing and restricted movements of the right
hip. Choose the most likely X-ray changes from the below List of options.
A. Cystic changes and lytic lesions
B. *Joint spaces are narrowed with reactive subchondral sclerosis, osteophytes
C. Periarticular osteopenia, marginal erosions
D. acroosteolysis
E. Fluffy bone periostitis and erosions at the interphalangeal joints
568. A 68-year-old woman has had four or five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. She is asymptomatic between attacks, and sulindac, 200 mg
twice daily, has usually relieved the symptoms. Her most recent episode was 4 months ago. On physical
examination, none of her joints is swollen or tender, but there is marked crepitus on extension of the
knee. She also has a positive bulge sign over the left knee and pain on full extension of the left elbow.
Which one of the following tests would confirm the diagnosis?
A. Arthrocentesis of the knee and laboratory analysis of the synovial fluid
B. *Measurement of serum uric acid
C. Measurement of serum rheumatoid factor
D. Radiograph of the knee
E. MRI of the knee with gadolinium contrast
569. A 50-yr-old woman complains of stiffness in her fingers worse at the end of the day. The DIP joints
and the first metacarpophalangeal joints are affected. Choose the most likely diagnosis from the below
list of options.
A. Rheumatoid arthritis
B. Psoriatic arthropathy
C. *Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
570. A 65-yr-old man has started chemotherapy for lymphoma. He has developed a painful swollen hot
right knee. He is apyrexial. Choose the most likely diagnosis from the below list of options.
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
571. Classical picture of acute gouty arthritis includes all of the following except
A. Excruciating and sudden pain
B. Stiffness in the joint
C. Low-grade fever may also be present
D. *Overgrowth at the distal interphalangeal joints
E. Warmness
572. Which of the following medications is contraindicated for the treatment of an acute attack of gout?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
573. A 57-year-old woman has had five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. She is asymptomatic between attacks, and sulindac, 200 mg
twice daily, has usually relieved the symptoms. Her most recent episode was 4 months ago. Classical
picture of exacerbation of the arthritis includes all of the following except
A. Excruciating and sudden pain
B. Low-grade fever may also be present
C. Overgrowth at the distal interphalangeal joints
D. *Warmness
E. Redness
574. A 57-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following changes
will reveal X-ray examination?
A. Erosions
B. Subluxations
C. Osteophytes
D. Osteoporosis
E. *"punched-out" lytic lesion
575. A 55-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following is
characteristic of the arthritis?
A. *Depositions of monosodium urate monohydrate crystals within the periarticular soft tissues
B. Overgrowth of bones within joints
C. Autoimmune synovitis
D. Osteoporosis
E. Rheumatoid nodules over joints
576. A 58-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 4 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following
medications is indicated for the treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
577. 79 y/o female with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly
elevated. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. Osteoarthritis
D. *Chronic Gouty arthritis
E. Psoriatic arthritis
578. Patients with gouty arthritis characterized by any of the following clinical characteristics except:
A. tophaceous deposits
B. *rheumatoid factor positive
C. "punched out" erosive changes on radiographs
D. acute attack frequency of greater than or equal to 2 attacks per year
E. hyperuricemia
579. 73-year-old male with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses consistent with tophaceous gout and
gouty arthritis. Choose the most likely changes from the below list of options.
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
580. 79 y/o female with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly
elevated. Which of the following medications is indicated for the treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
581. 79 y/o female with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly
elevated. Which of the following medications is indicated for the treatment of exacerbation of arthritis?
A. allopurinol
B. *colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
582. 55 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Chronic Gouty arthritis
C. Rheumatoid arthritis
D. Osteoarthritis
E. Psoriatic arthritis
583. 57 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is indicated for the treatment
of chronic arthritis?
A. colchicine
B. corticosteroids
C. indomethacin
D. *allopurinol
E. ibuprofen
584. 59 yo female with swelling and pain of his fingers. Patient also with similar complaints regarding
his great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and
3rd digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and
3rd digits and metatarsophalangeal joints. Which of the following medications is indicated for the
treatment of exacerbation of arthritis?
A. allopurinol
B. corticosteroids
C. *colchicine
D. indomethacin
E. ibuprofen
585. 57 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is contraindicated for the
treatment of exacerbation of arthritis?
A. corticosteroids
B. colchicine
C. indomethacin
D. ibuprofen
E. *allopurinol
586. 52 yo male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in the
DIP of the right first digit, with calcifications. Further questioning revealed a history of repeated attacks
of acute joint pain. There is bony erosion at multiple DIP's of the right hand that is periarticular, well
corticated and has a thin overhanging edge. There is no associated osteopenia. Choose the most likely
diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Chronic gouty arthritis
E. Psoriatic arthritis
587. 52 yo male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in the
DIP of the right first digit, with calcifications. Further questioning revealed a history of repeated attacks
of acute joint pain. There is bony erosion at multiple DIP's of the right hand that is periarticular, well
corticated and has a thin overhanging edge. There is no associated osteopenia. Which of the following
medications is indicated for the treatment of chronic arthritis?
A. colchicine
B. *allopurinol
C. corticosteroids
D. indomethacin
E. ibuprofen
588. A 39-year-old male was admitted with one-day history of acute left lower quadrant pain, and was
diagnosed with acute uncomplicated diverticulitis, confirmed by computed tomography (CT) of the
abdomen. He denied smoking or illicit drug use, but admitted occasional alcohol use on every other
weekend. He did not follow any particular diet. He had an average built. He was started on intravenous
antibiotics and pain medication, which led to significant clinical improvement within two days.On the
third day of hospitalization, he developed acute, severe pain and swelling of the left elbow. Within next
few hours, pain worsened and he was unable to move the elbow joint, which was tender, erythematous,
and swollen on examination. Never investigated in the past, we also noted a firm 4 ? 6 cm mass on each
elbow, and another one surrounding the proximal inter-phalangeal joint of right middle finger. When
asked particularly, he noticed similar episodes of arthritis of great toe in the past. Which of the following
medications is indicated for the treatment of the arthritis?
A. allopurinol
B. corticosteroids
C. *colchicine
D. tetracycline
E. mydocalmi
589. 86 year old male with chronic gout presents with bilateral foot pain. Physician desired radiograph
for evaluation of extent of pathologic changes. Prominent erosive destruction of bilateral first metatarsals
and second distal phalanx with well-preserved joint spaces throughout. Choose the most likely changes
from the below list of options.
A. High ESR
B. Oseoporosis on X-ray
C. Positive blood culture
D. *Urate crystals on joint aspirate
E. Positive rheumatoid factor
590. Side effects of colchicines are all of the following except
A. Neutropenia
B. Nausea
C. Diarrhea
D. Anemia
E. *Headache
591. Hyperuricemia is defined as a serum uric acid concentration above
A. *7 mg per dL (420 µmol per L).
B. 4 mg per dL (240 µmol per L).
C. 5 mg per dL (300 µmol per L).
D. 8 mg per dL (480 µmol per L).
E. 9 mg per dL (540 µmol per L).
592. Overproduction of urate may be in all of the following except
A. Primary idiopathic hyperuricemia
B. *Essential hypertension
C. Hemolytic processes
D. Lymphoproliferative disease
E. Myeloproliferative disease
593. Overproduction of urate may be in all of the following except
A. Polycythemia vera
B. Psoriasis (severe)
C. *Peptic ulcer
D. Exercise
E. Alcohol
594. A 65-year-old man comes to your office complaining of knee pain that began insidiously about a
year ago. He has no other rheumatic symptoms. Which of the following signs isn’t sign of the arthritis?
A. Pain is related to use
B. Pain gets worse during the day
C. Minimal morning stiffness (<20 min) and after inactivity (gelling)
D. *Warmth of skin over effected joints
E. Range of motion decreases
595. A 65-year-old man comes to your office complaining of knee pain that began insidiously about a
year ago. He has no other rheumatic symptoms. Which of the following signs isn’t sign of the arthritis?
Which of the following signs isn’t sign of the arthritis?
A. Joint instability
B. Bony enlargement
C. Restricted movement
D. Crepitus
E. *tophi
596. All of the following are X-ray signs of Osteoarthritis except
A. Joint space narrowing
B. Marginal osteophytes
C. Subchondral cysts
D. Bony sclerosis
E. *Marginal erosions
597. 55 years old, came to a musculoskeletal specialist seeking advice for a 3-year history of
progressively worsening pain in both knees. Her knees were stiff for about 20 minutes when she arose in
the morning and for a few minutes after getting up from a chair during the day. Her symptoms were
worse on humid or cold days, and she occasionally felt as if one of her knees would “give out.” Choose
the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
598. 55 years old, came to a musculoskeletal specialist because she had difficulty walking > 30 minutes
because of pain, and her symptoms were exacerbated by kneeling, squatting, or descending stairs.
Although sitting, resting, and reclining relieved her pain, she became stiff if she stayed in one position
for too long. Her symptoms were worse on humid or cold days, and she occasionally felt as if one of her
knees would “give out.” Which of the following changes will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
599. Secondary osteoarthritis may be caused by all of the following except
A. Hemaphilia
B. Hemochromatosis
C. Gouty arthritis
D. *CLL
E. After trauma
600. Risk factors and possible causes of osteoarthritis are all of the following except
A. Age
B. Obesity
C. *Stress
D. Prior injury
E. Acromegaly
601. Signs of osteoarthritis are all of the following except
A. Limp
B. Muscle atrophy
C. Crepitus
D. Restricted movement
E. *Warmth of skin over effected joints
602. A 65-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. There is slight crepitus with motion of the right knee. Which of the
following treatment do use?
A. methotrexat
B. *Intra-articular Hyaluronic Acid Injections
C. probenecid
D. colchicine
E. allopurinol.
603. A 65-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. here is slight crepitus with motion of the right knee. All of the following
are X-ray signs of еру arthritis except
A. Joint space narrowing
B. Marginal osteophytes
C. Subchondral cysts
D. Bony sclerosis
E. *Marginal erosions
604. A 68-year-old man is evaluated because of a 3-year history of bilateral knee pain and low back
pain. He has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. There is slight crepitus with motion of the right knee. Which of the
following treatment do use?
A. Methotrexat
B. *Glucosamine
C. Colchicines
D. Tetracycline
E. Allopurinol
605. A 63-year-old man is evaluated because of a 2-year history of bilateral knee pain and low back
pain. He has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, he has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
right knee. Which of the following treatment do use?
A. Methotrexat
B. Colchicines
C. *Chondroitin sulfate
D. Tetracycline
E. Allopurinol
606. 70-year-old, married, teacher. She has been under treatment for hypertension and is finally stable
on medication. Initial Chief complaint: painful right knee, arthritis in right hip. She had had arthritic pain
in her right hip confirmed by x-ray about 10 years ago. The knee pain is a newer problem and she
suspects it is also arthritis. There is slight crepitus with motion of the right knee. Which of the following
treatment do use?
A. Methotrexat
B. Colchicines
C. *Chondroitin sulfate
D. Tetracycline
E. Allopurinol
607. 70-year-oldpatient. Chief complaint: painful right knee, arthritis in right hip. She had had arthritic
pain in her right hip confirmed by x-ray about 10 years ago. The knee pain is a newer problem and she
suspects it is also arthritis. There is slight crepitus with motion of the right knee. Which of the following
changes will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
608. A 68-year-old man presents with an acutely red and swollen right great toe without history of
trauma. Which of the following findings is most useful for making a diagnosis of gout in this patient?
A. Persistent elevation of serum uric acid
B. Good response to colchicines trial
C. *Radiograph showing marginal joint erosion in the first metatarso-phalangeal (MTP) joint
D. An associated right ankle effusion
E. A painless elbow nodule
609. The best drug to treat SLE is :
A. Asprin
B. Indomethacin
C. Prostoglandines
D. Procainamide
E. *Steroids
610. Which condition or health problem demonstrates inflammation without invasion?
A. Allergic rhinitis
B. Viral hepatitis
C. *Gouty arthritis
D. Cellulitis
E. Septic arthritis
611. The following condition is not associated with an Anti-phopholipid syndrome:
A. Venous thrombosis
B. Recurrent fetal loss
C. *Thrombocytosis
D. Neurological manifestations
E. Recurrent thrombotic events
612. Drug-induced systemic lupus erythematosus (SLE) can be characterized by all of the following
statements EXCEPT?
A. Twenty percent of patients receiving procainamide develop drug-induced lupus
B. *Most patients on hydralazine develop a positive antinuclear antibody (ANA) test; however, only
10 percent suffer from lupuslike symptoms
C. If patients with drug-induced lupus fail to respond within several weeks of discontinuing the
offending agent, a trial of corticosteroids is indicated
D. If a patient with drug-induced lupus has persistent symptoms for longer than 6 months, an anti-ds
antibody
E. None of the above
613. For the Systemic lupus erythematosus choose the most likely diagnostic antibody from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. *Anti-dsDNA
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
614. For the Systemic lupus erythematosus choose the most likely diagnostic antibody from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. *Antinuclear antibody
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
615. In which of the following diseases test for anticentromere antibody is positive?
A. *Scleroderma
B. Mixed connective tissue disorder
C. SLE
D. Rheumatoid arthritis
E. Polymyalgia rheumatica
616. A 20-yr-old woman presents with deep venous thrombosis in the left leg. Her past history includes
three miscarriages. Her blood tests show mild thrombocytopenia and a positive serology test for syphilis.
Choose the most likely diagnosis from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. Mixed connective tissue disorder
D. *Antiphospholipid syndrome
E. Polyarteritis nodosa
617. A 28-yr-old woman presents with a plethora of signs and symptoms. She complains of arthralgia,
depression, alopecia, fits, oral ulceration and facial rash. She is found to have proteinuria and normocytic
normochromic anaemia. Choose the most likely investigation from the above list of options.
A. *Antinuclear antibodies
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
618. A 38 –year old patient presents to clinic with melaena normal renal function, hypertension and
mononeuritis multiples. The most probable diagnosis is
A. *Classical polyarteritis nodosa
B. Microscopic polyangiitis
C. Henoch-Schonlein purpura
D. Buerger's disease
E. Wegener's granulomatosis
619. A 28-yr-old woman presents with arthralgia, depression, alopecia, fits, oral ulceration and facial
rash. She is found to have proteinuria and normocytic normochromic anaemia. Choose the most likely
results of the investigations from the above list of options.
A. *Anti ds-DNA antibodies
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
620. A 35-yr-old woman presents with swellings and stiffness of her fingers. On examination she has
sausage-like fingers with flexion deformities. She is noted to have a beaked nose. X-ray of her hands
reveals deposits of calcium around her fingers and lysis of the distal phalanges. Choose the most likely
diagnosis from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. SLE
D. Polyarteritis nodosa
E. *Scleroderma
621. A 38-year-old man has had fever, weight loss, arthralgias, pleuritic chest pain, and midabdominal
pain for the last 3 months. One week ago he noticed difficulty dorsi flexing his left great toe. Blood
pressure is 160/95 mm Hg (he has always been normotensive), and laboratory studies reveal anemia of
chronic disease, high erythrocyte sedimentation rate, and polymorphonuclear leukocytosis. The chest xray is clear. The most likely diagnosis is
A. giant cell arteritis
B. allergic granulomatosis
C. Wegener's granulomatosis
D. *polyarteritis nodosa
E. hypersensitivity vasculitis
622. Low serum complement levels would be seen in patients with hematuria, proteinuria, and
hypertension resulting from all of the following EXCEPT
A. mixed essential cryoglobulinemia
B. hepatitis C-associated membranoproliferative glomerulonephritis
C. diffuse proliferative lupus nephritis
D. *Henoch-Schonlein purpura
E. poststreptococcal (or postinfectious) glomerulonephritis
623. A 60-yr-old previously fit man presented with a 2-month history of fatigue, dyspnoea on exertion,
abdominal pain and progressive numbness in his feet. He recently developed mild polyarthritis in his
hands. On examination there was evidence of left median nerve mononeuritis. Chest radiography showed
cardiomegaly. Choose the most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Polymyalgia rheumatica
C. Polymyositis
D. *Polyarteritis nodosa
E. Scleroderma
624. A 30-yr-old man presented with fever, myalgia and abdominal pain. On examination his
temperature was 38.7°C, BP was 200/120 and pulse was 130. His abdomen was tender with guarding and
absent bowel sounds. Choose the most likely diagnosis from the below list of options.
A. Kawaski's disease
B. Giant cell arteritis
C. Microscopic polyangitis
D. Antiphospholipid syndrome
E. *Polyarteritis nodosa
625. A 15-yr-old boy was admitted with a tender swollen right knee and a tender right elbow. His past
history included recurrent sore throats and dull abdominal pain for a 5 days. On examination his
temperature was 37.9°C and there was some periumbilical tenderness. Both urine and stools were
positive for blood. Choose the most likely diagnosis from the below list of options.
A. Kawaski's disease
B. *Henoch-Schonlein purpura
C. Giant cell arteritis
D. Microscopic polyangitis
E. Antiphospholipid syndrome
626. A 30-yr-old male presents with purpura, fever, malaise, weight loss and joint pain, chest pain.
Choose the single most likely treatment from the list of options given below.
A. Tetracycline
B. Ciprofloxacin
C. Beta 2 agonist
D. *Cyclophosphamide
E. IV aminophylline
627. A 38-yr-old woman presents with fever, malaise, weight loss and joint pains. She has high blood
pressure and swelling feet. She complains of persistent chest pain, legs paresthesia. She has purpuric rash
and skin nodules on legs. Choose the most likely diagnosis from the below list of options.
A. Hyperparathyroidism
B. *PAN
C. Systemic sclerosis
D. Henoch-Schonlein purpura
E. Diabetes mellitus
628. A 28-yr-old computer engineer with a long history of asthma and rhinitis presents with wheezing
cough and fever. A CXR shows patchy consolidation. Physical examination shows multiple tender
subcutaneous nodules and purpura. Choose the most likely diagnosis from the below list of options.
A. *Polyarteritis nodosa
B. Mitral stenosis
C. Pneumonia
D. SLE
E. Churg-Strauss syndrome
629. A 13-yr-old boy presents with purpura around the buttocks and upper thighs following upper
respiratory tract infection. He also complains of arthralgia and abdominal pain. Choose the most likely
diagnosis from the below list of options.
A. Membranous glomerulonephritis
B. Idiopathic crescenteric GN
C. *Henoch-Schonlein purpura
D. Goodpasture's syndrome
E. Postinfectious glomerulonephritis
630. Which of the following diseases occur primarily or exclusively in children?
A. Henoch-Schonlein purpura
B. Kawasaki’s disease
C. Behcet’s disease
D. Cogan’s syndrome
E. *Henoch-Schonlein purpura,
631. A 13-year-old boy presents with a faint leg rash, bloody diarrhoea and oliguria. Further
investigations reveal heavy proteinuria and an elevated serum IgA choose the single most likely
diagnosis from the below list of options.
A. Membranous glomerulonephritis
B. Idiopathic crescenteric GN
C. *Henoch-Schonlein purpura
D. Goodpasture's syndrome
E. Postinfectious glomerulonephritis
632. For a non-blanching maculopapular rash on flexor compartments of the lower limbs of a 13-yr-old
boy choose the single most likely diagnosis from the below list of options.
A. SLE
B. Nephroblastoma
C. Haemolytic uraemic syndrome
D. Juvenile chronic arthritis
E. *Henoch-Schonlein purpura
633. Which of the following statements concerning Henoch-Schonlein purpura and renal disease is the
best answer?
A. Most children with Henoch-Schonlein purpura progress to chronic renal insufficiency.
B. *Adults with Henoch-Schonlein purpura need long-term follow-up to monitor for renal disease.
C. Renal disease is a result of monoclonal immunoglobulin G deposition in the glomerulus.
D. Most adults with Henoch-Schonlein purpura progress to chronic renal insufficiency.
E. None of the above
634. A 17-yr-old boy has haematuria, hypertension, abdominal pain and a rash is noted on the flexor
surfaces of his lower limbs. Choose the single most likely diagnosis from the list of options below
A. *Henoch-Schonlein purpura
B. Kawasaki’s disease
C. Behcet’s disease
D. Cogan’s syndrome
E. None of the above
635. Which of the following statements regarding the use of cyclophosphamide in the treatment of
rheumatic disorders such as lupus nephritis and vasculitis is correct?
A. The dose of cyclophosphamide should be increased until substantial leukopenia is observed.
B. The absorption of oral cyclophosphamide is poor, so the intravenous route is preferred.
C. Oral cyclophosphamide should be administered at night and fluids restricted in order to decrease
the formation of urine.
D. *Regular monitoring of the patient’s complete blood cell count and urinalysis is required.
E. None of the above
636. ANCA is NOT associated with which of the following diseases:
A. Wegener's granulomatosis
B. *Henoch Schonlein purpura
C. Microscopic polyangiitis
D. Churg Strauss syndrome
E. drug-induced
637. Which of the following isn’t characteristic of polyarteritis nodosa :
A. Weight loss greater than/equal to 4 kg.
B. Livedo reticularis.
C. *Ig-A immune deposit.
D. Muscle pain, weakness, or leg tenderness.
E. Nerve disease
638. For Henoch-Schnlein purpura is characteristic:
A. Weight loss greater than/equal to 4 kg.
B. Livedo reticularis.
C. *Ig-A immune deposit.
D. Muscle pain, weakness, or leg tenderness.
E. Nerve disease
639. In polyarteritis nodosa, aneurysms are seen in all, EXCEPT:
A. Kidney
B. *Spleen
C. Liver
D. Pancreas
E. Liver
640. A patient presents with melaena normal renal function, hypertension and mononeuritis multiples.
The most probable diagnosis is
A. *Classical polyarteritis nodosa
B. Microscopic polyangiitis
C. Henoch-Schonlein purpura
D. Buerger's disease
E. Henoch-Schonlein purpura
641. Henoch Schonlein purpura is characterized by all except:
A. *Thrombocytopenia
B. Glomerulonephritis
C. Arthralgia
D. Abdominal pain
E. Skin rash
642. One of the following is a characteristic of Henoch - Schonlein Purpura:
A. *Blood in stool
B. Thrombocytopenia
C. Intracranial hemorrhage
D. Susceptibility to infection
E. Low ESR
643. One of the following is a characteristic of Henoch - Schonlein Purpura:
A. *Ig-A immune deposit
B. Thrombocytopenia
C. Intracranial hemorrhage
D. Susceptibility to infection
E. Low ESR
644. One of the following is a characteristic of Henoch - Schonlein Purpura:
A. *Skin purpura
B. Thrombocytopenia
C. Intracranial hemorrhage
D. Susceptibility to infection
E. Low ESR
645. A 23 year old woman presents with bilateral conductive deafness, palpable purpura on the legs and
hemoptysis. Radiograph of the chest shows a thin-walled cavity in left lower zone. Investigations reveal
total leukocyte count 14000/mm3, red cell casts in the urine and serum creatinine 3 mg/dL. What is the
most probable diagnosis?
A. Henoch-Schonlein purpura
B. *Polyarteritis nodosa
C. Wegener's granulomatosis
D. Disseminated tuberculosis
E. Behcet's syndrome
646. A 23year old woman presents with bilateral conductive deafness, palpable purpura on the legs and
hemoptysis. Radiograph of the chest shows a thin-walled cavity in left lower zone. Investigations reveal
total leukocyte count 14000/mm3, red cell casts in the urine and serum creatinine 3 mg/dL. Choose the
single most likely treatment from the list of options given below.
A. Tetracycline, prednisone
B. Ciprofloxacin, NSAIDs
C. Beta 2 agonist, heparin
D. *Cyclophosphamide, prednisone
E. IV aminophylline
647. All of the following are primary vasculitis EXCEPT
A. Wegener’s granulomatosis
B. microscopic polyangiitis
C. Henoch-Schonlein purpura
D. *Rheumatoid vasculitis
E. polyarteritis nodosa
648. A 25-yr-old computer engineer with malaise, fever, and weight loss. Physical examination shows
multiple tender subcutaneous nodules and livedo reticularis, peripheral neuropathy.
A. *Polyarteritis nodosa
B. leukocytoclastic vasculitis
C. Henoch-Schonlein purpura
D. Microscopic polyangiitis
E. Churg Strauss syndrome
649. An 15-year-old man presents with abdominal pain, nausea, and vomiting. He also notes the onset of
a rash and painful joints. Physical examination is remarkable for the presence of palpable purpura
distributed over the buttocks and lower extremities as well as guaiac-positive stool. Laboratory
evaluation is normal. Other serum studies are normal. Skin biopsy would likely reveal
A. necrotizing angiitis
B. eosinophilic angiitis
C. *leukocytoclastic vasculitis
D. extravasated red blood cells without vasculitis
E. mast cell infiltration
650. A 48-yr-old woman presents with fever, malaise, weight loss and joint pains. She has high blood
pressure and large feet. She complains of persistent chest pain. She has purpuric rash and skin nodules.
A. Acromegaly
B. *Polyarteritis nodosa
C. Systemic sclerosis
D. Herpes
E. leukocytoclastic vasculitis
651. A 50-yr-old man presented with a 6-month history of fatigue, abdominal pain and progressive
numbness in his feet. He recently developed mild polyarthritis in his hands. On examination there was
evidence of right median nerve mononeuritis, livedo reticularis, BP 180/110 mmHg (he has always been
normotensive), and laboratory studies reveal anemia of chronic disease, high erythrocyte sedimentation
rate. Chest radiography showed cardiomegaly.
A. Rheumatoid arthritis
B. SLE
C. Antiphospholipid syndrome
D. Henoch-Schonlein purpura
E. *Polyarteritis nodosa
652. A 38-yr-old man presented with fever, myalgia and abdominal pain and progressive numbness in
his feet. On examination his temperature was 38.9°C, BP was 200/120 and pulse was 128. His abdomen
was tender with guarding and absent bowel sounds. Choose the single most likely treatment from the list
of options given below.
A. Tetracycline, prednisone
B. Ciprofloxacin, NSAIDs
C. Beta 2 agonist, heparin
D. *Cyclophosphamide, prednisone
E. IV aminophylline
653. Polyarteritis nodosa is vasculitis of …
A. *Medium-sized and small muscular arteries
B. Large vessels
C. Small vassels
D. Medium-sized vessel
E. Postcapillary venule
654. Signs of kidney involvement in Polyarteritis nodosa are all of the following EXCEPT:
A. Systemic hypertension
B. Painless hematuria
C. *hydronephrosis
D. Intrarenal aneurysms
E. Multiple small cortical infarcts
655. Signs of skin involvement in Polyarteritis nodosa are all of the following EXCEPT:
A. *dermatitis
B. livedo reticularis
C. ulcers
D.
E.
656.
A.
B.
C.
D.
E.
657.
A.
B.
C.
D.
E.
658.
A.
B.
C.
D.
E.
659.
A.
B.
C.
D.
E.
660.
A.
B.
C.
D.
E.
661.
A.
B.
C.
D.
E.
662.
A.
B.
C.
D.
E.
663.
A.
B.
C.
D.
E.
664.
A.
B.
nodules
gangrene
Signs of skin involvement in Polyarteritis nodosa are all of the following EXCEPT:
purpura,
livedo reticularis,
ulcers,
nodules
*papules
Which isn’t characteristic for Polyarteritis nodosa?
Myocardial infarctions
*Erosive arthritis
Congestive heart failure
Systemic hypertension
Impaired kidney function
In which of the following Hepatitis B surface antigen is +ve in 30%?
*polyarteritis nodosa
microscopic polyangiitis
leukocytoclastic angiitis
Wegener's granulomatosis
Henoch-Schonlein purpura
Which of the following isn’t criterion for Polyarteritis nodosa?
Muscle pain, weakness, or leg tenderness.
Nerve disease (either single or multiple).
Diastolic blood pressure greater than 90mmHg (high blood pressure).
*Photosensitivity
Elevated kidney blood tests (BUN greater than 40 mg/dl or creatinine greater than 1.5 mg/dl).
Hypersensitivity vasculitis effects mainly …
Medium-sized and small muscular arteries
Large vessels
Small vassels
Medium-sized vessel
*Postcapillary venule
Hypersensitivity vasculitis effects mainly …
*vessels of skin
vessels of kidney
vessels of lung
coronary arteries
vessels of brain
Small-vessel involvement with immune complex deposition are all of the following EXCEPT
Hypersensitivity vasculitis
Henoch-Schonlein purpura
*Polyarteritis nodosa
Behcet’s syndrome
Cryoglobulinemia
IgA-dominant immune complexes is the cause of which of the following vasculitis
Hypersensitivity vasculitis
*Henoch-Schonlein purpura
Polyarteritis nodosa
Behcet’s syndrome
Cryoglobulinemia
Henoch-Schonlein purpura is a disease that involves all of the following EXCEPT
purple spots on the skin
joint pain
C. gastrointestinal problems
D. *pneumonitis
E. glomerulonephritis
665. Symptoms of Henoch-Schonlein purpura are all of the following EXCET
A. *Hemoptysis
B. Abdominal pain
C. Joint pain
D. Purple spots on the skin (purpura), usually over the buttocks, lower legs
E. Bloody stools
666. Which of the following serologic studies isn’t included in laboratory studies of vasculitis?
A. antinuclear antibody
B. ANCA
C. rheumatoid factor
D. *HLA B 27
E. cryoglobulins
667. Which of the following test isn’t included in laboratory studies of vasculitis?
A. complete blood count
B. erythrocyte sedimentation rate
C. *level of serum Ca
D. urinalysis
E. hepatitis B surface antigen
668. A 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs. He
had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving medium size arteries.
The hyperpigmented patches represent the new phase of the lesions - tender dermal nodules. Which of
the following diagnoses is the most likely cause of this patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Takayasus arteritis
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
669. A 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs. He
had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving medium size arteries.
The hyperpigmented patches represent the new phase of the lesions - tender dermal nodules. Choose the
single most likely treatment from the list of options given below.
A. *Prednisone
B. Tetracycline
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
670. A 43 year old woman had a 25 year history of recurrent painful nodules on the medial aspect of her
ankles. Episodes lasted for 4-6 months with complete resolution of the rash during symptom free periods
for several months. His BP 160/110 mm Hg. Serological test showed Hepatitis B surface antigen is +ve.
Which of the following diagnoses is the most likely cause of this patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Takayasus arteritis
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
671. A 43 year old woman had a 25 year history of recurrent painful nodules on the medial aspect of her
ankles. Episodes lasted for 4-6 months with complete resolution of the rash during symptom free periods
for several months. His BP 160/110 mm Hg. Serological test showed Hepatitis B surface antigen is +ve.
Choose the single most likely treatment from the list of options given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
672. A 41 year old woman has had fever, weight loss, arthralgias, his BP 160/110 mm Hg, temperature
is 37.2 °C. Serological test showed Hepatitis B surface antigen is +ve. Choose the single most likely
treatment from the list of options given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
673. A 41 year old woman has had fever, weight loss, arthralgias, his BP 160/110 mm Hg, temperature
is 37.2 °C. Serological test showed Hepatitis B surface antigen is +ve. Which of the following diagnoses
is the most likely cause of this patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Takayasus arteritis
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
674. A 41 year old woman has had fever, weight loss, arthralgias, his BP 160/110 mm Hg, temperature
is 37.2 °C. Serological test showed Hepatitis B surface antigen is +ve. Choose the single most likely
treatment from the list of options given below.
A. Tetracycline, Prednisone
B. Ciprofloxacin, Cyclophosphamide
C. Beta 2 agonist
D. *Prednisone, Cyclophosphamide
E. IV aminophylline
675. A 40-year-old man developed purpuric papules on his abdomen and legs several weeks earlier. He
also complained of tea colored urine. A skin biopsy confirmed the presence of small vessel
leukocytoclastic vasculitis. Which of the following diagnoses is the most likely cause of this patient’s
symptoms?
A. Systemic lupus erythematosus
B. *Henoch-Schonlein purpura
C. Polyarteritis nodosa
D. Lymphoma, with a paraneoplastic syndrome
E. Kawasaki’s disease
676. Henoch-Schonlein purpura (HSP) is a small-vessel vasculitis characterized by all of the following
EXCEPT
A. Skin purpura
B. Arthritis
C. abdominal pain
D. hematuria
E. *epistaxis
677. Henoch-Schonlein purpura (HSP) is a small-vessel vasculitis characterized by all of the following
EXCEPT
A. immunoglobulin A (IgA) deposition in capillaries
B. immune complex deposition in arterioles
C. *antibodies against cells of vascular wall
D. immune complex deposition in capillaries
E. immune complex deposition in venules
678. IgA vasculitis is …
A. *Henoch-Schonlein purpura
B. Systemic lupus erythematosus
C. Polyarteritis nodosa
D. Kawasaki’s disease
E. microscopic polyangiitis
679. Arthritis in Henoch-Schonlein purpura, most commonly involving
A. wrists
B. joints of hands
C. *knees and ankles
D. spine joints
E. hips and shoulders
680. A leukocytoclastic vasculitis involves …
A. *predominantly skin
B. predominantly kidney
C. predominantly bowel
D. predominantly heart
E. predominantly joints
681. Vessel damage in Vasculitis Syndromesathogenic immune complex formation and/or deposition are
all of the following EXCEPT
A. Henoch-Schonlein purpura
B. Vasculitis associated with collagen vascular diseases
C. Serum sickness and cutaneous vasculitis syndromes
D. Hepatitis B-associated polyarteritis nodosa
E. *Wegener's granulomatosis
682. Signs of heart involvement in Polyarteritis nodosa are all of the following EXCEPT:
A. Congestive heart failure
B. myocardial infarction
C. pericarditis
D. *myocarditis
E. hypertrophy of LV
683. Toxic Side Effects of cyclophosphamide are all of the following EXCEPT
A. Bone marrow suppression
B. *gastropathy
C. Cystitis
D. Bladder carcinoma
E. Gonadal suppression
684. Toxic Side Effects of gluccocorticoids are all of the following EXCEPT
A. Osteoporosis
B. Cataracts
C. Glaucoma
D. *Gonadal suppression
E. Hypertension
685. Predominantly cutaneous vasculitis (hypersensitivity vasculitis) are all of the following EXCEPT
A. *Wegener's granulomatosis
B. Drug-induced vasculitis
C. Serum sickness and serum sickness-like reactions
D. Vasculitis associated with infectious diseases
E. Vasculitis associated with connective tissue diseases
686. In the acute stages of which disease, polymorphonuclear neutrophils infiltrate all layers of the
vessel wall and perivascular areas, which results in intimal proliferation and degeneration of the vessel
wall is seen?
A. Henoch-Schonlein purpura
B. Systemic lupus erythematosus
C. *Polyarteritis nodosa
D. Kawasaki’s disease
E. microscopic polyangiitis
687. A 37-year-old man has had fever, weight loss, arthralgias, and midabdominal pain for the last 2
months. One week ago he noticed difficulty dorsiflexing his right great toe. Blood pressure is 150/95 mm
Hg (he has always been normotensive), and laboratory studies reveal anemia of chronic disease, high
erythrocyte sedimentation rate, and polymorphonuclear leukocytosis. Which of the organs isn’t affected
in the disease?
A. Kidney
B. *Stomach
C. Liver
D. Pancreas
E. Liver
688. A 39-year-old man has had fever, weight loss, arthralgias, and midabdominal pain for the last 3
months. One week ago he noticed difficulty dorsiflexing his right great toe. Blood pressure is 10/115 mm
Hg, and laboratory studies reveal anemia of chronic disease, high erythrocyte sedimentation rate, and
polymorphonuclear leukocytosis. He has been treated with prednisone 60 mm/d last month. Choose the
single most likely treatment from the list of options given below.
A. Tetracycline
B. *Ciprofloxacin
C. Plasmapheresis
D. Cyclophosphamide
E. IV aminophylline
689. A 53-year-old woman was referred to hospital for recurrent palpable purpura and cutaneous ulcers
over her lower legs. Her disease started 3 years ago with erythematous papules and palpable purpuric
lesions located over her lower legs including the dorsa of her feet. In the second year of her disease, she
experienced similar lesions located on the upper back. The disease responded well to mid-potency topical
steroids only to recur shortly after stopping them. On her lower legs we found several cutaneous ulcers
covered with hemorrhagic crusts along with hyper- and hypopigmented atrophic scars and a few
excoriated papules. The rest of physical examination including accessible mucosal surfaces and
peripheral pulses was normal. Which of the following diagnoses is the most likely cause of this patient’s
symptoms?
A. *Cutaneous small-vessel vasculitis
B. Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
690. The following condition is not associated with an Anti-phopholipid syndrome:
A. Venous thrombosis
B. Recurrent fetal loss
C. *Thrombocytosis
D. Neurological manifestations
E. Recurrent thrombotic events
691. The best group of drugs to treat SLE is :
A. Asparcam
B. Movalis
C. Prostoglandines
D. Procainamide
E. *Steroids
692. Drug-induced systemic lupus erythematosus (SLE) can be characterized by all of the following
statements EXCEPT?
A. Twenty percent of patients receiving procainamide develop drug-induced lupus
B. *Most patients on hydralazine develop a positive antinuclear antibody (ANA) test; however, only
10 percent suffer from lupuslike symptoms
C. If patients with drug-induced lupus fail to respond within several weeks of discontinuing the
offending agent, a trial of corticosteroids is indicated
D. If a patient with drug-induced lupus has persistent symptoms for longer than 6 months, an anti-ds
antibody
E. None of the above
693. Anticentromere antibody is positive in which of the following diseases?
A. *Scleroderma
B. Mixed connective tissue disorder
C. SLE
D. Rheumatoid arthritis
E. Polymyalgia rheumatica
694. A 48-year-old woman comes to hospital for recurrent palpable purpura and cutaneous ulcers over
her lower legs. Biopsy was taken from a periphery of the most recent, partially ulcerated, lesion and
processed for routine histopathology and direct immunofluorescence (DIF) study. Histopathology
showed partly ulcerated epidermis and foci of collagen necrosis with leukocytoclastic vasculitis of the
dermal blood vessels. Surprisingly, DIF disclosed intercellular deposits of IgG in the epidermis along
with IgG, IgM, C3 and fibrinogen deposits around dermal blood vessels in her lesional skin. Only
epidermal intercellular IgG deposits were found in the clinically uninvolved skin. Which of the following
diagnoses is the most likely cause of this patient’s symptoms?
A. Henoch-Schonlein purpura
B. Systemic lupus erythematosus
C. Polyarteritis nodosa
D. Kawasaki’s disease
E. *Cutaneous small-vessel vasculitis
695. For the Systemic lupus erythematosus choose the most likely diagnostic test from the below list of
options.
A. Antimicrosomal antibody
B. C-ANCA
C. *false positive test for syphilis
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
696. For the Systemic lupus erythematosus choose the most likely diagnostic antibody from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. *anti-Smith antibodies
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
697. A 23-yr-old woman presents with deep venous thrombosis in the left leg. Her past history includes
three miscarriages. Her blood tests show mild thrombocytopenia and a positive serology test for syphilis.
Choose the most likely diagnosis from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. Mixed connective tissue disorder
D. *Antiphospholipid syndrome
E. Polyarteritis nodosa
698. A 28-yr-old woman presents with a plethora of signs and symptoms. She complains of arthralgia,
depression, alopecia, fits, oral ulceration and facial rash. She is found to have proteinuria and normocytic
normochromic anaemia. Choose the most likely investigation from the above list of options.
A. *Antinuclear antibodies
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
699. A 28-yr-old woman presents with a plethora of signs and symptoms. She complains of arthralgia,
depression, alopecia, fits, oral ulceration and facial rash. She is found to have proteinuria and a
normocytic normochromic anaemia. Choose the most likely results of the investigations from the above
list of options.
A. *anti-Smith antibodies
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
700. A 43-yr-old woman presents with swellings and stiffness of her fingers. She is noted to have a
beaked nose. X-ray of her hands reveals lysis of the distal phalanges. Choose the most likely diagnosis
from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. SLE
D. Polyarteritis nodosa
E. *Scleroderma
701. Clinical findings in constrictive pericarditis may be all of the following EXCEPT:
A. Pulse pressure is normal or reduced
B. Edema
C. *Acute pulmonary edema
D. Distended cervical veins
E. Increased abdominal girth
702. Which of the following sings is more prominent in constrictive pericarditis?
A. Edema
B. *Ascites
C. Pulmonary edema
D. Hypertension
E. Thromboembolism
703. Which of the following investigation can’t help to distinguish constrictive pericarditis and cirrhosis
of the liver?
A. Distended neck veins
B. Chest roentgenography
C. chest CT
D. *EchoCG
E. ChestMRI
704. Differential diagnosis of the constrictive pericarditis we should do with all of the following diseases
EXCEPT:
A. Tricuspid stenosis
B. Cor pulmonale
C. *Pericardial effusion
D. Cirrhosis of the liver
E. Restrictive cardiomyopathy
705. Which of the following EchoCG changes is found in dilated cardiomyopathy?
A. *Left ventricular dilatation
B. Left ventricular diastolic dysfunction
C. Increased left ventricular wall thickness
D. Asymmetric septal hypertrophy
E. Systolic anterior motion (SAM) of the mitral valve
706. What is the main cause of death in patient with dilated cardiomyopathy?
A. Pulmonary embolism
B. Stroke
C. Myocardial infarction
D. Pulmonary edema
E. *Fatal arrhythmias
707. All of this drugs use for treatment of dilated cardiomyopathy except?
A. Diuretics
B. b-blockers
C. ACE inhibitors
D. *Warfarin
E. Aspirin
708. Which of the following EchoCG changes is found in restrictive cardiomyopathy?
A. Left ventricular dilatation
B. Left ventricular diastolic dysfunction
C. *Increased left ventricular wall thickness
D. Asymmetric septal hypertrophy
E. Systolic anterior motion (SAM) of the mitral valve
709. Which of the following EchoCG changes is found in hypertrophic cardiomyopathy?
A. Left ventricular dilatation
B. Left ventricular diastolic dysfunction
C. Increased left ventricular wall thickness
D. Symmetric septal hypertrophy
E. *Systolic anterior motion (SAM) of the mitral valve
710. Standard therapy of heart failure in dilated myocardiopathy includes all of the following EXCEPT:
A. Salt restriction
B. Angiotensin-converting enzyme (ACE) inhibitors
C. *Calcium channel blockers
D. Diuretics
E. Digitalis
711. Causes of Chronic Pericardial Effusion are all of the following EXCEPT:
A. Myxedema
B. SLE
C. Rheumatoid arthritis
D. Radiation therapy
E. *Viral
712. In chronic constrictive pericarditis EchoCG changes are all of the following EXCEPT:
A. The ventricular end-diastolic and stroke volumes are reduced
B. The end-diastolic pressures in both ventricles are elevated
C. The mean pressure in the atria is elevated,
D. The mean pressures in pulmonic veins is elevated
E. *The left ventricle chamber is dilated
713. All of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
714. All of the following conditions are associated with elevated RV diastolic pressures with the pattern
shown EXCEPT
A. *Cardiac tamponade
B. Constrictive pericarditis
C. Massive pulmonary embolism
D. Constrictive pericarditis
E. Restrictive cardiomyopathy
715. A middle aged man presents with fever and variable heart murmur. He also complains of fever,
malaise and night sweats. On examination you find clubbing and splenomegaly. Choose the single most
likely diagnosis from the list of options below.
A. *Infective endocarditis
B. Pericardial effusion
C. SLE
D. Bacteraemia
E. Acute myocarditis
716. A seventeen-year-old girl had a throat infection three weeks ago. Since then she has developed a
fever and an acute migratory polyarthritis involving the knees, ankles and wrists. Her parents have
noticed her legs twitching. She has a transient erythematous rash, with ring and crescent shaped patches.
Which is the SINGLE MOST likely diagnosis?
A. *Rheumatic fever
B. Allergic polyarthritis
C. Juvenile chronic arthritis
D. Lyme disease
E. Parvovirus
717. In which disease we expect to see vegetations?
A. *Infective endocarditis
B. Viral myocarditis
C. Acute pericarditis
D. Rheumatic heart disease
E. Hypertrophied cardiomyopathy
718. Etiology of rheumatic fever is:
A. *beta-hemolytic streptococci.
B. alfa-hemolytic streptococci
C. The HACEK group
D. H. influenza
E. Staphylococcus aureus
719. What investigation can detect vegetations in the sizes of 2-3mm:
A. *Transoesophageal echocardiogram
B. MRI
C. ECG
D. CT
E. Chest X-ray
720. Duration of antibiotic treatment of the patients with acute rheumatic fever?
A. *not less then two weeks
B. not less then 10 days
C. not less then a week
D. not less then 5 days
E. not less then a 3 month
721. A 21-yr-old patient presents with a 2-week history of a swollen left knee, conjunctivitis and
arthritis. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Psoriatic arthritis
C. Joint sepsis
D. *Reactive arthritis
E. Rheumatoid arthritis
722. A 31-yr-old man presents with urethritis, conjunctivitis and a swollen left knee. Choose the most
likely diagnosis from the below list of options.
A. *Reiter's syndrome
B. Psoriatic arthropathy
C. Osteoarthritis
D. Reactive arthritis
E. Gonococci arthritis
723. There is swelling of her MCP joints bilaterally and of wrists. There is a nodule on her left elbow.
Choose the most likely diagnosis from the below list of options
A. High ESR
B. High serum uric acid
C. Positive blood culture
D. *Positive rheumatoid factor
E. High WBC count
724. All of the following are signs of rheumatoid arthritis (RA) except?
A. early morning stiffness lasting 2 hour
B. *numbness and blanching of fingers on exposure to cold
C. symmetrical involvement of the metacarpophalangeal joints
D. a non-tender subcutaneous mass over the Achilles tendon
E. synovial fluid with high viscosity and 30,000 lymphocytes/mm3
725. 69-yr-old woman with longstanding polyarthritis on immunosuppressive drugs presents with
systemic malaise and fever and has severe pain, redness, heat and swelling of the wrist. Choose the most
likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Joint sepsis
C. Osteoarthritis
D. Gout
E. Cancer
726. Which of the following is characteristic of rheumatoid arthritis
A. asymmetric oligoarticular arthritis
B. *symmetric polyarthritis of hand joints
C. arthritis of distal interphalangeal joints
D. severe destructive polyarthritis (arthritis mutilans)
E. sacroiliitis with or without peripheral arthritis
727. Arthritis and urethritis is typical for:
A. Gout;
B. Rheumatoid arthritis ;
C. Psoriatic arthritis;
D. *Reiters syndrome;
E. ankylosing spondilitis;
728. Choose the most likely diagnostic antibody for Rheumatoid arthritis from the below list of options.
A. Antimicrosomal antibody
B. C-ANCA antibody
C. Anti-dsDNA
D. P-ANCA antibody
E. *Anti -CCP antibody
729. Drug of choice for patient with rheumatoid arhtritis
A. *Methotrexate
B. Diclofenac
C. Hydroxychloroquine sulphate
D. Leflunamide
E. D-penicillamine
730. Felty’s syndrome occurs in patients with seropositive rheumatoid arthritis with all of the following
except
A. Neutropenia
B. Hypoproteinemia
C. Anemia
D. *lymphocytopenia
E. splenomegaly
731. For arthritis in Rheumatoid arthritis diagnostic criterion is:
A. morning pain;
B. night pain;
C. *morning stiffness;
D. weight gain;
E. asymmetric joint involvement;
732. Side-effects of NSAIDs include all of the following except
A. Peptic ulcer
B. upper gastrointestinal haemorrhage
C. *hypotension
D. interstitial nephritis
E. agranulocytosis
733. Which clinical manifestation in a male with arthritis indicates or suggests the possibility of Reiter's
syndrome?
A. Stooped posture
B. Unplanned weight loss
C. *Pain/burning on urination
D. Ringing in the ears at night
E. Dry eyes
734. Which clinical manifestation would be typical in a client with rheumatoid arthritis?
A. Anemia
B. *Warm, tender, swollen joints
C. asymmetric joint involvement
D. Elevated ESR
E. Crepitation of involved joints
735. The best drug to treat RA is :
A. Aspirin
B. Indomethacin
C. Prostoglandines
D. NSAID’s
E. *Methotrexate
736. Confirmation of SLE with which test?
A. Antimicrosomal antibody
B. C-ANCA
C. *Anti-dsDNA
D. P-ANCA
E. Antiacetylcholine receptor antibody
737. For the Systemic lupus erythematosus choose the most suggestive diagnostic test from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. * complement system levels
D. Antiparietal cell antibody
E. Antiacetylcholine receptor antibody
738. Woman of 33 years with Raynauds phenomenon, polyarthritis, dysphagia of 6 years and mild
sclerodactyly, blood showing Anticentromere antibody positive, the most likely diagnosis is:
A. *Scleroderma
B. Sjogren’s syndrome
C. SLE
D. Rheumatoid arthritis
E. Polymyalgia rheumatica
739. A 29-yr-old woman presents with alopecia and oral ulceration. Choose the single most likely
investigation to confirm diagnosis.
A. Serum calcium
B. Serum glucose
C. Serum electrolytes
D. Serum urea and creatinine
E. *Anti-dsDNA
740. A 27-yr-old.patient with DVT of the left calf. She had a history of recurrent abortions and arthritis.
Choose the most likely diagnosis from the below list of options.
A. Protein C deficiency
B. Thrombotic thrombocytopenia
C. *Antiphospholipid syndrome
D. SLE
E. Polycythemia rubra vera
741. A 27-yr-old.patient with fluorescent antinuclear antibody choose the single most likely diagnosis
from the below list of options.
A. Wegener's granulomatosis
B. Goodpasture's syndrome
C. Multiple myeloma
D. *Lupus nephritis
E. Diabetic neprtropathy
742. The bad prognostic indicator for scleroderma is:
A. *Renal involvement
B. Dysphagia
C. Heart pain
D. Osteolysis
E. Arthritis
743. Which of the following autoantibodies is more likely to be found in patients with systemic
sclerosis?
A. anti-Smith (anti-Sm)
B. Anti-ribonucleoprotein (RNP)
C. *Anti SCL 70
D. Anti-CCP
E. Anticentromere
744. Heart damage in SLE:
A. Acute Rheumatic corditis
B. *Limban Sack's endocarditis
C. Non thrombotic bacterial endocarditis
D. Chronic rheumatic carditis
E. MVP
745. Anti-double stranded DNAand ANA ares highly specific for
A. Systemic sclerosis
B. *SLE.
C. Polymyositis
D. Dermatopolymyositis
E. Viral hepatitis
746. Dysphagia, Raynaud's phenomenon, sclerodactyly, dyspnea, anticentromere antinuclear antibody
are characteristic for:
A. Systemic lupus erythematosis
B. *Systemic sclerosis
C. Mixed connective tissue disorder
D. Rheumatoid arthritis
E. Dermatopolymyositis
747. Dysphagia, Raynaud's phenomenon, sclerodactyly, dyspnea. Choose the most likely results of the
investigations from the below list of options for confirming the diagnosis.
A. *Anticentromere antibody
B. Anti dsDNA antibodies
C. ANCA
D. Antimitochondrial antibody
E. Smooth muscle antibody
748. Serologic tests should be performed in patients with specific musculoskeletal complaints for
assessing all the following EXCEPT:
A. rheumatoid factor
B. antinuclear antibodies (ANA)
C. uric acid level
D. *albumin
E. Anti-CCP
749. Which of the following clinical features is NOT commonly found in limited systemic sclerosis?
A. Raynaud's phenomenon
B. Esophageal dysfunction
C. *Purpura
D. Sclerodactyly
E. Telangiectasia
750. Cardiac involvement in SSC are all of the following EXCEPT
A. Pericardial effusion
B. Cor pulmonale
C. Conduction abnormalities
D. *Vegetations on undersurface of A.V. valves
E. arrhythmias,
751. The bisphosphonate, alendronate, has clearly been established to be effective in randomised
controlled trials in which of the following conditions?
A. Osteomalacia
B. Bony metastases
C. Algodystrophy
D. *Postmenopausal osteoporosis
E. Hypercalcuria
752. Allopurinol is used in the management of gout. Which statement below is correct?
A. Allopurinol is effective by increasing glomerular filtration of uric acid.
B. Allopurinol is effective by reducing the tubular reabsorption of uric acid.
C. *Allopurinol is effective by inhibiting the conversion of xanthine to uric acid.
D. Allopurinol is indicated in a 37 year old man with a uric acid concentration of 0.42 mg/l and a
history of one attack of gout.
E. Allopurinol is associated with aplastic anaemia in 1% of cases.
753. All the following features favor ventricular tachycardia as the cause of broad-complex tachycardia,
EXCEPT:
A. QRS duration with right bundle branch block morphology (RBBB) is greater than 140 ms, and
greater than 160 ms with left LBBB morphology
B. LAD with RBBB morphology, extreme LAD (northwest axis) with LBBB morphology
C. AV dissociation
D. *Response to carotid sinus massage
E. Concordance of the QRS pattern in all precordial leads (i.e., all positive or all negative deflections)
754. Which of the following will most likely respond to verapamil?
A. RVOT tachycardia
B. *Idiopathic LV tachycardia
C. Bundle branch re-entry tachycardia
D. ARVD ventricular tachycardia
E. All of the above
755. The most common type of arrhythmia in WPW syndrome is....
A. Ventricular tachycardia
B. Ventricular fibrillation
C. Ventricular premature complexes
D. Atrial ectopics
E. *AV re-entry tachycardia
756. Use of echocardiogram in the assessment of AF:
A. It is not necessary to perform a TTE in patients with AF
B. TEE is always needed to allow better assessment of the MV and LA
C. *TTE should be performed at baseline to diagnose associated structural/functional heart disease
D. TTE is necessary to determine stroke risk stratification for thromboprophylaxis in all patients
E. When TTE is technically difficult, MRI is needed to exclude cardiac abnormalities
757. Which is the preferred initial treatment strategy for rate control in AF patients?
A. Digoxin
B. *Beta-blockers or rate limiting CCB
C. Combination therapy of beta-blockers and rate-limiting CCB’s
D. Amiodarone
E. Combination therapy of digoxin and beta-blockers
758. Which option is better in regard to cardioversion?
A. *Synchronised DC shock to restore sinus rhythm
B. Amiodarone in all patients to restore sinus rhythm
C. Flecainide in patients with IHD to maintain sinus rhythm
D. Digoxin to restore sinus rhythm
E. Propaphenone to restore sinus rhythm in HCMP patients
759. Regarding antithrombotic treatment in AF:
A. Patients with asymptomatic AF have less risk of embolism than symptomatic patients
B. Patients with atrial flutter do not need antithrombotic treatment due to the low risk of embolism of
this arrhythmia
C. *Warfarin is the best option in patients with high risk of thromboembolism
D. Aspirin has a similar effect in stroke reduction to placebo
E. Paroxysmal AF has the lowest risk of embolism
760. Sudden cardiac death in patients >35 years old is most commonly associated with:
A. Hypertrophic cardiomyopathy
B. *Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
761. Congenital long QT syndrome can lead to
A. Complete heart block
B. *Polymorphic ventricular tachycardia
C. Acute myocardial infarction
D. Recurrent supraventricular tachycardia
E. All of the above
762. Bundle branch re-entry ventricular tachycardia is most commonly associated with:
A. Enhanced automaticity in the right bundle
B. Enhanced automaticity in the left bundle
C. Supranormal conduction in the His bundle
D. *Abnormally slow conduction in the His bundle
E. All of the above
763. All of the following are ECG manifestations of Wolff-Parkinson-White syndrome EXCEPT
A. *Narrow QRS
B. Initial slurred QRS upstroke
C. Short PQ interval
D.
E.
764.
A.
B.
C.
D.
E.
765.
A.
B.
C.
D.
E.
766.
A.
B.
C.
D.
E.
767.
A.
B.
C.
D.
E.
768.
A.
B.
C.
D.
E.
769.
A.
B.
C.
D.
E.
770.
A.
B.
C.
D.
E.
771.
A.
B.
C.
D.
E.
772.
A.
B.
Normal QT interval
All of the above
The initial manifestations of WPW syndrome may include which of the following?
Atrial fibrillation
AV re-entry tachycardia
Ventricular fibrillation
Wide-QRS tachycardia
*All of the above
The presence of an r prime in V1 during narrow-QRS tachycardia is suggestive of...
AV re-entry
*AV node re-entry
Rate-dependent BBB
Atrial tachycardia
Atrial fibrillation
Ventricular ectopic beats (VEBs) occurring in apparently normal hearts are:
Associated with a bad prognosis
Never frequent or complex
Less frequent with increasing age
*May be associated with symptoms of “missed beats”
Always symptomatic
In patients with ventricular ectopic beats:
Caffeine restriction always reduces symptoms
*High caffeine intake should always be discouraged in symptomatic patients
There is good evidence that reducing caffeine intake reduces ectopics
Hypertension has no association with frequency of ectopic beats
LVH is not associated with increased frequency of ectopics
Regarding ventricular ectopics and exercise:
*Ectopics are usually benign if they are supressed on exercise
Exercise-induced VEBs are not associated with adverse prognosis
RVOT ectopics are usually supressed on exercise
Ectopics induced on recovery after exercise are benign
All of the above
An idiopathic left ventricular tachycardia (VT) shows the following...
Typical LBBB morphology
*LAD and RBBB morphology
Associated with a high risk of sudden cardiac death and almost always requires ICD therapy
Never responds to verapamil
All of the above
Beta blockers are accepted treatment to prevent VT in:
Brugada syndrome, RVOT-VT, short QT syndrome and long QT syndrome
Brugada syndrome, RVOT-VT and long QT syndrome
*RVOT-VT and long QT syndrome
Short QT syndrome and long QT syndrome
Brugada syndrome and short QT syndrome
Wenckebach phenomenon is defined as...
Progressive shortening of PR interval till a beat is dropped
*Progressive lengthening of PR interval till a beat is dropped
Irregular heart rate and PVC’s
Shortened QT intervals
Slurred QRS complex
Giant a waves in JVP (“cannon” waves) are seen in
Sinus bradycardia
Atrial fibrillation
C. First-degree AV-block
D. *Complete heart block
E. Atrial ectopic
773. All of the following findings are suggestive of LVH except:
A. (S in V1 + R in V5 or V6) > 35 mm
B. R in aVL > 11 mm
C. R in aVF > 20 mm
D. (R in I + S in III) > 25 mm
E. *R in aVR > 8 mm
774. All of the following findings are suggestive of RVH except:
A. R in V1=7 mm (15 mm with RBBB)
B. (R in V1 + S in V5 or V6) > 10 mm
C. R < S in V6
D. R or R’ in V1
E. *S in V3 + R in aVL > 28 mm (20 mm for women)
775. When present, each of the following heart sounds occurs shortly after S2 EXCEPT:
A. Opening snap
B. Third heart sound
C. *Ejection clic
D. Tumor plop
E. Pericardial knock
776. Each of the following statements regarding splitting of the second heart sound is true EXCEPT:
A. Severe pulmonic valvular stenosis is associated with a softened P2
B. Delayed closure of the pulmonic valve with inspiration contributes to physiologic splitting of S2
C. Fixed splitting of S2 is the auscultatory hallmark of an ostium secundum atrial septal defect
D. Paradoxical splitting of S2 is expected in patients with a right ventricular electronically paced
rhythm
E. *Right bundle branch block is associated with paradoxical splitting of S2
777. The timing of an "innocent" murmur is usually:
A. Early systolic
B. Presystolic
C. *Midsystolic
D. Holosystolic
E. Early diastolic
778. Which of the following pairs of medical conditions and antihypertensive medications would be
incorrect to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
779. Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
780. Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
781. You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
782. Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
783. All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
784. Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
785. Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
786. Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
787. Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
788. Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. * Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
789. Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
790. Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
791. Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
792. A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
793. The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
794. All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
795. All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. People of African descent commonly have a high renin type hypertension*
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
796. Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
797. Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
798. Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
799. Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
800. Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
801. All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
802. The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
803. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
804. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
805. In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
806. In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
807. The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
808. The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
809. In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
810. Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
811. All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
812. Which of the following diagnostic studies is most likely to demonstrate the cause of the headaches?
A. MRI of the head
B. MRI of the kidney
C. *MRI of the thorax
D. 24-h urinary 5-HIAA
E. 24-h urinary free cortisol
813. A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the likely diagnosis?
A. Congenital adrenal hyperplasia
B. Fibromuscular dysplasia
C. Cushing’s syndrome
D. *Conn’s syndrome
E. Pheochromocytoma
814. A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the best way to diagnose this disease ?
A. Renal vein renin levels
B. 24-h urine collection for metanephrines
C. MRI of the renal arteries
D. 24-h urine collection for cortisol
E. *Plasma aldosterone/renin ratio
815. A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What is the best medication for the management of this patient’s
hypertension?
A. *Phentolamine
B. Fenoldopam
C. Esmolol
D. Nicardipine
E. Diazoxide
816. A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What test would best determine the patient’s diagnosis?
A. Plasma catecholamines
B. 24-h urine collection for 5-HIAA
C. Abdominal CT scan
D. *24-h urine collection for metanephrines and vanilylmandelic acid
E. Adrenal vein sampling for renin levels
817. What is the correct feature of the hypertensive urgency?
A. It is always a life-threatening situation
B. Patient must be hospitalized
C. *Patients can be managed as outpatients
D. Therapy should not be given orally
E. None of the above
818. If there is suspicion of phaeochromocytoma, the first line drug is:
A. Sodium-nitroprusside
B. Nifedipine
C. *Phentolamine
D. Verapamil
E. Enalapril
819. If you are in your office and a patient sees you with the following symptoms: long history of
hypertension, home BP usually 160/100 mmHg, suddenly developed severe headache, blurred vision,
weakness in the right arm, blood pressure: 200/110 mmHg. What will you do:
A. Give the patient 20 mg nifedipine orally, and check the BP in 15 min. If it is still >200/100 mmHg,
give another dose of nifedipine
B. Give the patient 20 mg nifedipine, and check the BP in 30 min. If it is 160/80 mmHg, send the
patient home and give another appointment in two weeks
C. Give the patient 10 mg amlodipine, send the patient home and give another appointment in two
days
D. Call the ambulance and send the patient to the nearest hospital
E. *Give the patient some pain-killer drug (e.g. acetaminophen), call the ambulance and send the
patient to the nearest hospital with stroke-unit
820. A 28-year-old male with type 1 diabetes mellitus is seen in the clinic for routine follow-up. The
patient has hypertension. He is being maintained on an insulin pump and lisinopril 5 mg daily. He has
been on this dose of lisinopril for approximately 6 weeks. He has normal creatinine and no proteinuria.
BP is 140/90 mmHg. What do you recommend ?
A. Continue the current dose of lisinopril and return for follow-up in 3 months as the patient has
received his target BP of less than 140/90 mmHg
B. Ask a patient to return in 6 weeks; if his BP remains at this level, increase the dose of lisinopril
C. *Increase lisinopril to 10 mg daily to achieve a goal BP of less than 130/80 mmHg
D. Assure the patient that he is suffering from “white-coat hypertension” and plan no intervention
E. Switch the patient from lisinopril to losartan
821. A 49-year-old female presents to you for an initial visit to establish health care. She has no past
medical history and denies a family history of diabetes mellitus, early cardiovascular disease, or renal
disease. Her BP on presentation is 185/110 mmHg. She denies headache or visual complaints. She has no
chest pain, shortness of breath, or change in urine color. Her physical examination is normal with the
exception of an S4 gallop heard at the 4th intercostal space just to the left of the sternum. An ECG is
significant for LVH and LAD. there are no signs of cardiac ischemia. Urinalysis shows no red blood cells
or proteinuria. What is your recommendation for therapy for this patient?
A. *Initiate therapy with hydrochlorothiazide in combination with a beta-blocker
B. Initiate therapy with hydrochlorothiazide alone
C. Initiate therapy with an ACE inhibitor alone
D. Advise the patient to go to the nearest emergency department for further treatment for a
hypertensive emergency
E. Advise the patient on lifestyle modifications and plan a return visit in 3 weeks
822. What will you do if you are on duty in a hospital and a hypertensive patient, who has been treated
with long-acting ß-blocker, long-acting dihydropyridine calcium antagonist and long-acting a-1
adrenoceptor blocker, is admitted with the following symptoms: headache, dyspnea, ankle-swelling, BP
180/110 mmHg, pulmonary rales, LVH on ECG, echo: LVH, left ventricular diastolic dysfunction,
ejection fraction 46%.
A. Amlodipine orally
B. Nifedipine orally
C. Enalaprilate iv
D. *Enalaprilate iv + furosemide iv
E. Esmolol iv
823. Which of the following blood pressure levels in pregnancy should be considered an emergency
requiring hospitalization?
A. ≥140/90 mmHg
B. ≥150/95 mmHg
C. ≥160/100 mmHg
D. *≥170/110 mmHg
E. A rise in SBP ≥25 mmHg or a rise in DPB ≥15 mmHg compared to pre-pregnancy values, or those
in the first trimester
824. The following drug combinations are effective to treat hypertension EXCEPT
A. Diuretics + beta-blockers
B. Beta-blockers + dihydropiridine calcium channel blockers
C. Diuretics + ACE-inhibitors/ARB
D. ACE-inhibitors/ARB + calcium channel blockers
E. *Beta-blockers + ACE-inhibitors/ARB
825. Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
826. With respect to renovascular disease, all of the statements are true EXCEPT:
A. Worsening renal function with ACE-inhibitor therapy suggests bilateral renovascular disease
B. Atherosclerotic disease most commonly involves the proximal third of the main renal artery
C. The most common form of fibroplastic renovascular disease in adults involves the media
D. *The incidence of renovascular hypertension falls with increased age
E. Patients with severe, accelerated hypertension have the highest prevalence of renovascular disease
827. A newly diagnosed diabetic patient presents with BP readings that are 155/95 or higher. All of the
following statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blockade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
828. All of the following statements regarding the association of oral contraceptive pills and
hypertension are correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
829. Each of the following statements regarding pheochromocytoma is true EXCEPT:
A. Approximately 15% of pheochromocytomas are extra-adrenal
B. Ten percent of pheochromocytomas are malignant
C. Ten percent of adrenal pheochromocytomas are bilateral
D. *Hypertension related to pheochromocytoma is nearly always episodic and only rarely persistent
E. Pheochromocytoma can be inherited
830. All of the following are features of renovascular hypertension due to fibromuscular hyperplasia, as
opposed to atherosclerosis, EXCEPT:
A. Age <50 years
B. Female gender
C. *More likely to progress to complete renal artery occlusion
D. No family history of hypertension
E. Absence of carotid bruits
831. Which of the following ACE-inhibitors are not prodrugs?
A. Captopril, lisinopril, ramipril
B. Lisinopril, enalapril, banazepril
C. *Captopril, lisinopril, enalaprilat
D. Moexipril, captopril, lisinopril
E. Perindopril, ramipril, enalapril
832. Each of the following statements regarding hypertension is true EXCEPT:
A. The prevalence of hypertension rises progressively with age in both men and women
B. Systolic and diastolic hypertension are each associated with an increased crisk of coronary heart
disease
C. *The target blood pressure for hypertensive patients with cardiovascular disease or diabetes is
140/90 mmHg
D. Patients with prehypertension (SBP 120-139 mmHg or DBP 80-89 mmHg) benefit from lifestyle
modifications incl. weight reduction, regular exercise, and smoking cessation
E. Drug therapy of hypertension benefits patients greater than 80 years of age
833. All of the following interventions have a BP-lowering effect EXCEPT:
A. A diet that reduces caloric intake by 1000 calories per day
B. Reduction of dietary sodium
C. *Daily magnesium supplements
D. Tobacco cessation
E. Reduction of ethanol consumption to less than 30 ml/day
834. Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
835. Each of the following statements regarding hypertension is true EXCEPT:
A. Increased LV muscle mass in hypertension is an independent risk factor of cardiac mortality
B. The risk of ventricular arrhythmias in hypertension is increased 2-fold in the presence of LV
hypertrophy
C. Low birth weight is associated with an increased incidence of hypertension later in life
D. *Chronic caffeine consumption is associated with an increased risk of hypertension
E. In hypertensive adolescents, essential hypertension is the most likely etiology
836. The following statements regarding the association of oral contraceptive pills and hypertension are
correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
837. Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
838. Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
839. Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
840. All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
841. Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
842. Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
843. Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
844. Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
845. Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. *Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
846. Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
847. Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
848. Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
849. A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
850. The proportion of essential hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
851. All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
852. All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. *People of African descent commonly have a high renin type hypertension
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
853. Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
854. Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
855. Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
856. Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
857. Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
858. All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
859. At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
860. The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
861. In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
862. In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. ≥140 mmHg
D. *≥160 mmHg
E. ≥170 mmHg
863. The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
864. The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
865. In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
866. Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
867. All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
868. Which of the following is an effective adjunct to increase the rate of smoking cessation?
A. Aldosterone
B. *Bupropion
C. Sildenafil
D. Cimetidine
E. Buspirone
869. With which of the following is sildenafil acetate (Viagra) most likely to interact adversely?
A. Fibrinolytic therapy
B. Primary PCI
C. *Nitrates
D. Aspirin
E. Beta-blockers
870. Bupropion hydrochloride (Zyban) is contraindicated in patients with a history of which of the
following?
A. *Seizures
B. Insulin-dependent diabetes mellitus
C. Severe chronic obstructive pulmonary disease (with reversible component)
D. Longer than 40-year history of tobacco use
E. Recent MI
871. In which of the following has the high-sensitivity C-reactive protein (CRP) been shown to be
predictive of risk?
A. Acute MI
B. Acute coronary syndromes
C. Chronic stable angina
D. Peripheral vascular disease
E. *All of the above
872. Which of the following has been shown to decrease the level of the high-sensitivity CRP?
A. Unopposed estrogen
B. Amlodipine besylate (Norvasc)
C. *Simvastatin
D. All of the above
E. None of the above
873. All of the following statements regarding myocardial stunning are true EXCEPT:
A. *Stunning is a state of depressed myocardial function due to chronic hypoperfusion
B. Stunning can be global or regional
C. Stunning can follow cardiac surgery with cardiopulmonary bypass
D. Oxygen-free radicals and excess intracellular calcium likely contribute to stunning
E. Stunning affects both systolic and diastolic function
874. What is the most common coexisting congenital anomaly in patients with coarctation of the aorta?
A. Cleft mitral valve
B. *Bicuspid aortic valve
C. Ebstein's anomaly
D. VSD
E. PDA
875. All of the following are characteristic findings of ostium primum atrial septal defect (ASD)
EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Right axis deviation
D. Systolic ejection murmur
E. Prominent pulmonary vascular markings on CXR
876. Choose the adult congenital disorder corresponding to the following physical examination fingings:
RV lift with a loud systolic ejection murmur along the left sternal border, with a single S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
877. Choose the adult congenital disorder corresponding to the following physical examination fingings:
loud S1, holosystolic murmur in left sternal border, systolic ejection click, and hepatomegaly
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
878. Choose the adult congenital disorder corresponding to the following physical examination fingings:
weak or delayed femoral pulses, harsh systolic murmur in the back, and a systolic ejection click in the
aortic area
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
879. Choose the adult congenital disorder corresponding to the following physical examination fingings:
cyanosis, digital clubbing, loud P2, and a variable Graham-Steel murmur
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
880. Choose the adult congenital disorder corresponding to the following physical examination fingings:
wide pulse pressure, prominent LV impulse, and a continuous machinery murmur enveloping S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *Patent ductus arteriosus
D. Ebstein's anomaly
E. Tetralogy of Fallot
881. Bacterial endocarditis prophylaxis is indicated in all adults who have the following congenital heart
disease EXCEPT:
A. VSD
B. Coarctation of the aorta
C. *Secundum ASD
D. Hypertrophic obstructive cardiomyopathy
E. PDA
882. Besides pulmonary valve stenosis, which of the following is the most common associated cardiac
defect present in patients with PA stenosis?
A. *VSD
B. ASD
C. Coarctation of the aorta
D. PDA
E. Bicuspid aortic valve
883. All of the following statements regarding patent ductus arteriosus (PDA) are true EXCEPT:
A. *The majority of cases close spontaneously after infancy
B. There is a higher incidence in mothers who acquired rubella during pregnancy
C. A decrease in the duration and intensity of the murmur has a poor prognostic implication
D. Left ventricular hypertrophy precedes RV hypertrophy
E. If it is uncorrected, approximately one third of patients die by the age of 40 years
884. Ostium primum ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. *Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
885. Noonan's syndrome is commonly associated with...
A. Supravalvular aortic stenosis
B. *Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
886. Coronary sinus ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. *Persistent left superior vena cava
887. Williams syndrome is commonly associated with...
A. Supravalvular aortic stenosis
B. *Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
888. Sinus venosus ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. *Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
889. All of the following physical examination findings are usually associated with ostium secundum
ASD EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Lateral and inferior displacement of the apex beat
D. Soft systolic ejection murmur in the second left intercostal space
E. Normal S1
890. Which of the following is an absolute contraindication to pregnancy?
A. Surgically corrected transposition of great arteries (TGA)
B. Congenitally corrected TGA
C. Ebstein's anomaly
D. *Eisenmenger's syndrome
E. Status post Fontan operation
891. The lesions that constitute tetralogy of Fallot include all of the following EXCEPT
A. A ventricular septal defect
B. An overriding aorta
C. *An atrial septal defect
D. Right ventricular outflow obstruction
E. Right ventricular hypertrophy
892. Match the chest radiography findings (prominent central PAs and peripheral PA prunning) with the
corresponding congenital disorder
A. *Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
893. Match the chest radiography findings (marked cardiomegaly, severe right atrial enlargement, and
normal lung fields) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. *Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
894. Match the chest radiography findings (right aortic arch, RV enlargement, and a "boot-shaped"
heart) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. *Tetralogy of Fallot
E. Coarctation of the aorta
895. Match the chest radiography findings (pulmonary plethora, prominent ascending aorta, proximal
PA dilatation) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. *Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
896. All of the following are indications for surgical closure of an ASD EXCEPT:
A. Significant symptoms in a 65-year-old
B. RV dysfunction
C. *Pulmonary vascular resistance >15 Wood units that does not diminish with vasodilators
D. An asymptomatic 20-year-old with a Qp/Qs of 1,7 with no pulmonary hypertension
E. RV enlargement
897. The following cardiovascular malformations are all associated with congenital rubella EXCEPT:
A. PDA
B. PA stenosis
C. *Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
898. Which of the following syndromes is associated with pumonary arterio-venous fistula?
A. Williams syndrome
B. *Weber-Osler-Rendu syndrome
C. Bland-Garland-White syndrome
D. Kartagener's syndrome
E. Crouzon's syndrome
899. Congenital MR is commonly encountered in all of the following conditions EXCEPT:
A. *Cor triatriatum
B. Ostium primum ASD
C. Coarctation of the aorta
D. Congenitally corrected TGA
E. Subaortic stenosis
900. In which of the following cases is surgical correction recommended?
A. Asymptomatic small VSD to decrease risk of endocarditis
B. PDA with severe pulmonary hypertension
C. *Asymptomatic subaortic stenosis with severe aortic valve insufficiency
D. Coarctation of the aorta with a transcoarctation gradient of 20 mmHg
E. Small ASD to prevent paradoxical embolization
901. Which congenital disorder corresponds with the following chest radiography findings: prominent
central PAs (possible calcifications) and peripheral PA prunning?
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
902. Which congenital disorder corresponds with the following chest radiography findings: right aortic
arch, RV enlargement, and a "boot-shaped" heart?
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
903. Which congenital disorder corresponds with the following chest radiography findings: marked
cardiomegaly, severe right atrial enlargement, and normal lung fields
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
904. Which congenital disorder corresponds with the following chest radiography findings: posterior rib
notching and a "reverse E" or "3" sign
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
905. Which congenital disorder corresponds with the following chest radiography findings: pulmonary
plethora, prominent ascending aorta, proximal PA dilatation, and opacity at the confluence of the aortic
knob and descending aorta
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
906. Which of the following statements regarding Ebstein's anomaly is NOT correct?
A. An ASD or PFO is present in up to 80% of patients
B. The cardinal feature is an apically displaced tricuspid valve resulting in atrialization of ventricular
tissue
C. WPW syndrome is common in these patients and multiple tracts can exist
D. *A bicuspid aortic valve is commonly present
E. A "sail sound" is a common finding on physical examination
907. Which of the following syndromes and cardiac anomalies are INCORRECTLY matched?
A. Trisomy 21 – atrioventricular canal defects
B. Noonan syndrome – pulmonic stenosis
C. Holt-Oram syndrome – atrial septal defects
D. Marfan syndrome – mitral valve prolapse
E. *Williams syndrome – ventricular septal defects
908. All of the following statements regarding the effects of maneuvers on the auscultation of cardiac
murmurs are true EXCEPT:
A. In patent ductus arteriosus (PDA), the diastolic phase of the murmur is intensified by isometric
handgrip
B. *The murmur of hypertrophic obstructive cardiomyopathy becomes softer with standing or during a
Valsalva strain maneuver
C. The murmur of a ventricular septal defect (VSD) increases with isometric handgrip
D. Sudden squatting or isometric handgrip increases the diastolic murmur of aortic regurgitation
E. The mid-diastolic and presystolic murmurs of mitral stenosis become louder with exercise
909. Radiotherapy for malignant disease may affect the heart in all of the following ways EXCEPT
A. Pericarditis
B. Coronary artery disease
C. Valvular stenosis
D. Conduction abnormalities
E. *Asymmetrical septal hypertrophy
910. Sudden cardiac death due to ventricular tachyarrhythmias is an established complication of each of
the following EXCEPT:
A. Sarcoidosis
B. Giant cell myocarditis
C. Chagas disease
D. Idiopathic dilated cardiomyopathy
E. *Hyperthyroidism
911. Characteristics of arrhythmogenic RV dysplasia include all of the following EXCEPT
A. Fatty infiltration of the right ventricle
B. Fatty infiltration of the right atrium *
C. Monomorphic ventricular tachycardia
D. Abnormal signal-averaged ECG
E. Possible detection by cardiac MRI
912. All of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
913. Each of the statements about the evolution of the ECG in acute pericarditis is correct EXCEPT:
A. Four sequential stages of abnormalities of the ST segments and T waves are typical
B. *Initial ST segment elevation is usually most prominent in ECG lead aVR
C. The ratio of the height of ST segment elevation to the height of the T wave in acute pericarditis is
typically >0.25 in lead V6
D. In acute pericarditis, the ST segment usually returns to baseline before the appearance of T wave
inversion
E. T wave inversion may persist for months after the acute presentation
914. Which of the following statements regarding cardiac involvement in Lyme disease is CORRECT?
A. Cardiac manifestations of Lyme disease typically occur within several days of the development of
erythema chronicum migricans
B. *Ten percent of patients with Lyme disease develop cardiac manifestations
C. Supraventricular and ventricular tachyarrhythmias are the most common cardiac manifestations of
Lyme disease
D. Cardiomegaly and congestive heart failure are common among patients who develop Lyme carditis
E. Antibiotic therapy has been proven to shorten the course of active Lyme carditis
915. Each of the following statements regarding the infectious etiologies of pericarditis is correct
EXCEPT:
A. Enteroviruses are among the most common causes of viral pericarditis
B. The most common organisms that cause bacterial pericarditis are streptococci and staphylococci
C. The prognosis of patients with bacterial pericarditis is poor
D. *Tuberculosis is the leading cause of constrictive pericarditis in Western nations
E. Antifungal therapy is generally not necessary in pericarditis caused by histolasmosis
916. Each of the following statements regarding Chagas disease is correct EXCEPT
A. The level of parasitemia does not correspond to the severity of chronic Chagas disease
B. The disease is transmitted to humans by the reduviid bug (commonly called the kissing bug)
C. *The most common ECG abnormality in chronic Chagas disease is left bundle branch block
D. The classic echocardiographic findings are those of a dilated cardiomyopathy with an apical
aneurysm
E. All of the above statements are correct
917. Which of the following disorders is not associated with ventricular tachycardia as a cause of
syncope?
A. Hypertrophic obstructive cardiomyopathy
B. Prior myocardial infarction
C. *Atrial myxoma
D. Aortic valvular stenosis
E. Congenital long QT syndrome
918. Each of the following statements regarding the ECG in acute pericarditis is true EXCEPT:
A. The majority of patients demonstrate ECG abnormalities
B. Global ST elevation is seen in early pericarditis
C. Sinus tachycardia is a common finding
D. PR depression is common in the majority of patients
E. *T wave inversions develop before ST elevations return to baseline
919. Each of the following statements regarding endomyocardial fibrosis (EMF) is correct EXCEPT:
A. This condition is characteristically found in tropical and subtropical Africa
B. It is predominantly a disease of children and young adults
C. *Involvement of the mitral apparatus typically results in mitral stenosis
D. EMF involves the left ventricle in 90% of affected patients
E. Echocardiographic features include increased endocardial echoreflectivity, fibrotic obliteration of
apex, atrial enlargement, and pericardial effusion
920. All of the following statements with regard to primary endocardial fibroelastosis (EFE) are correct
EXCEPT:
A. The condition is often familial
B. The mitral and aortic valve leaflets are usually thickened and distorted
C. *The murmur of mitral stenosis is the most common auscultatory finding
D. Symptoms of primary EFE usually develop between 2 and 12 months of age
E. Echocardiographic features include a reduced ejection fraction and increased left atrial and left
ventricular dimensions
921. Which of the following therapies improves survival in patients with cor pulmonare secondary to
COPD?
A. Digoxin
B. *Oxygen
C. Beta-adrenergic agonists
D. Theophylline
E. Hydralazine
922. What is NOT a cause of chronic cor pulmonale?
A. COPD
B. Recurrent pulmonary emboli
C. *Mitral stenosis
D. Kyphoscoliosis
E. Obstructive sleep apnea
923. Which of the following conditions is associated with increased left ventricular preload?
A. Sepsis
B. Right ventricular infarction
C. *Mitral regurgitation
D. Dehydration
E. Pulmonary embolism
924. Each of the following conditions is associated with the development of pulmponary edema
EXCEPT:
A. Increased pulmonary venous pressure
B. High altitude
C. *Increased plasma oncotic pressure
D. Eclampsia
E. Heroin overdose
925. The statements about the diagnosis of PE include all of the following EXCEPT:
A. Arterial blood gas measurement is often unhelpful in the diagnosis of acute PE
B. The most common ECG finding in patients with PE is sinus tachycardia
C. Pulmonary infarction due to PE can be visualized on a standard chest radiograph
D. *Reduced intensity of the pulmonic component of the second heart sound is typical in patients with
large PE
E. Fibrin-degradation products (e.g., D-dimer) are commonly elevated in patients with PE
926. Heart failure is:
A. Decreasing in incidence and prevalence due to recent advances in the treatment of cardiovascular
disease
B. *One of the diagnoses with the highest readmission rate
C. A common condition across all ages
D. Can be diagnosed from a clinical response to treatment
E. All of the above statements are correct
927. According to the ESC guidelines, the following patients have heart failure:
A. An obese, dyspnoeic lady with swollen anckles but a normal echocardiogram
B. An asymptomatic man with a previous MI and area of hypokinesis on his echocardiogram
C. *A hypertensive man with LVH, fast atrial fibrillation and dyspnea
D. An elderly man with a few basal crepitations but a normal echocardiogram
E. All of the above
928. Which of the following sometimes occur when heart failure is absent?
A. Gallop rhythm
B. Anckle oedema
C. A past history of a MI
D. *Dyspnea
E. All of the above
929. B-type natriuretic secretion is regulated by:
A. Fluid accumulation in the lungs
B. *Pressure and volume of the left ventricle
C. Oedema in the anckles
D. Auricular end diastolic pressure
E. All of the above
930. Which of the following statements are true ?
A. A normal resting ECG is rare in angina pectoris
B. A normal resting ECG is common in heart failure
C. *Cardiomegaly plus pleural effusions make heart failure very likely
D. Atrial fibrillation commonly does not cause dyspnoea in patients with LVH and diastolic
dysfunction
E. All of the above
931. The value of BNP in the diagnosis of heart failure in the emergency room in patients with acute
dyspnoea:
A. *Is supported by a BNP concentration >500 pg/ml
B. Is excluded by a NT-proBNP concentration <1000 pg/ml
C. Is restricted to patients without a previous history of heart failure
D. Has not been evaluated in patients with renal dysfunction
E. All of the above statements are true
932. Which symptoms/signs only occur when the HF is relatively advanced – that is, they are commonly
absent in mild heart failure
A. Cardiomegaly on chest X-ray
B. Orthopnea
C. Exertional dyspnea
D. *A abd B
E. B and C
933. All patients with heart failure should be advised to:
A. Refrain from smoking
B. Restrict sodium intake
C. Avoid a flu shot
D. *A and B
E. All of the above
934. Exercise training in chronic heart failure
A. *Has been shown to increase peak oxygen consumption by 15-20% in randomized controlled trials
B. Has been shown to increase LV ejection fraction by 15-20% in randomized controlled trials
C. Is not recommended in heart failure
D. Has never been shown to reduce mortality and morbidity
E. None of above
935. Drugs that should be avoided in heart failure patients are:
A. Non-steroidal anti-inflammatory drugs (NSAIDS)
B. Corticosteroids
C. Beta-blockers
D. *A and B
E. All of the above
936. The followings improve the survival figure in chronic congestive heart failure as shown by many
studies...EXCEPT
A. Bisoprolol
B. Metoprolol succinate
C. *Atenolol
D. Spironolactone
E. Carvedilol
937. The following drugs have significantly improved survival in HF patients
A. *ACE inhibitors
B. Nitrates
C. Digoxin
D. Diuretics
E. All of the above
938. Which of the statements about beta-blocker treatment in HF is true?
A. Randomised clinical trials show that b blockers are beneficial in patients with heart failure and
preserved left ventricular function
B. Elderly patients are the most frequently studied population in blocker trials
C. * Blockers exert a favourable effect in heart failure due to ischaemic and non-ischaemic aetiology
D. Patients with diabetes should always be excluded from blocker treatment
E. There is clear evidence that end stage heart failure patients should be treated with blockers
939. Which of the statements about beta-blocker treatment in HF is true?
A. *Beta-blockers must be started at very low dosages
B. Treatment should be started when patients are unstable in order to stabilize them
C. When patients are treated with ACE inhibitors, blockers are contraindicated
D. Treatment should always be started during hospital stay
E. The most frequent adverse reaction to a blocker is cough
940. Which of the statements about antiarrhythmic therapy treatment in HF is NOT true?
A. Amiodarone is an antiarrhythmic drug whose use can improve symptoms of patients with heart
failure without affecting myocardial function and survival
B. *Class I antiarrhythmic agents reduce mortality of patients with heart failure
C. In patients with documented life threatening ventricular arrhythmias, implantable cardioverterdefribrillators (ICDs) can reduce sudden death
D. Sudden death is one of the most frequent causes of death in patients with heart failure
E. The reduction of the number of premature ectopic beats with antiarrhythmic drugs can prevent
sudden mortality of heart failure patients
941. A prophylactic ICD is useful for reducing total mortality in patients:
A. With previous myocardial infarction and low ejection fraction
B. With dilated cardiomyopathy and low ejection fraction
C. With previous myocardial infarction and low ejection fraction and broad QRS
D. A and C
E. *All of the above
942. Biventricular pacing in severe heart failure and broad QRS:
A. Improves NYHA class
B. Improves exercise tolerance
C. Reduces hospitalisation for heart failure
D. Reduces heart rate
E. *All of the above
943. Which of the following treatments most consistently improves EF in patients who have systolic
heart failure?
A. Diuretics
B. Beta-blockers
C. *ACE-inhibitors
D. Vasodilators
E. All of the above
944. BNP has which of the following properties?
A. Urine volume increases
B. Sodium excretion is enhanced
C. More BNP is secreted
D. A decrease in plasma aldosterone concentration occurs
E. *All of the above occur
945. All of the following are indications for heart transplantation EXCEPT
A. Dilated cardiomyopathy
B. Diabetes mellitus
C. Hypertrophic cardiomyopathy
D. Age 60 to 70 years
E. *Amyloid heart disease
946. When used chronically, all of the following drugs increase mortality EXCEPT
A. Milrinone
B. Dobutamine
C. Vesnarinone
D. Xamoterol
E. *Amlodipine
947. Primary causes of diatolic heart failure include all of the following EXCEPT
A. Hypertrophic cardiomyopathy
B. *Dilated cardiomyopathy
C. Hypertension
D. Ischemic cardiomyopathy
E. Infiltrative cardiomyopathy
948. Match the description with the associated form of therapy for pulmonary embolism: may be
effective in PE even 1 to 2 weeks after the onset of symptoms
A. Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. *Both
D. Neither
E. Not applicable
949. Match the description with the associated form of therapy for pulmonary embolism: dissolution of
recently formed thrombus is a major action
A. Unfractionated heparin or low molecular weight heparin
B. *Fibrinolytic therapy
C. Both
D. Neither
E. Not applicable
950. Match the description with the associated form of therapy for pulmonary embolism: in general,
should be administered along with an antiplatelet agent
A. Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. Both
D. *Neither
E. Not applicable
951. Match the description with the associated form of therapy for pulmonary embolism: may cause
aldosterone depression
A. *Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. Both
D. Neither
E. Not applicable
952. Match the ECG finding that is most closely associated with chronic Chagas disease:
A. Low QRS voltage
B. AV nodal block
C. *Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
953. Match the ECG finding that is most closely associated with sarcoidosis:
A. Low QRS voltage
B. *AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
954. Match the ECG finding that is most closely associated with apical hypertrophic cardiomyopathy
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. *Deeply inverted precordial T waves
955. Match the ECG finding that is most closely associated with cardiac amyloidosis
A. *Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
956. Heart may be affected by radiotherapy in all of the following ways EXCEPT
A. Pericarditis
B. Coronary artery disease
C. Valvular stenosis
D. Conduction abnormalities
E. *Asymmetrical septal hypertrophy
957. SCD (sudden cardiac death) due to ventricular tachyarrhythmias is an established complication of
each of the following EXCEPT:
A. Sarcoidosis
B. Giant cell myocarditis
C. Chagas disease
D. Idiopathic dilated cardiomyopathy
E. *Hyperthyroidism
958. Arrhythmogenic RV dysplasia is characterized by all of the following EXCEPT
A. Fatty infiltration of the right ventricle
B. *Fatty infiltration of the right atrium
C. Monomorphic ventricular tachycardia
D. Abnormal signal-averaged ECG
E. Possible detection by cardiac MRI
959. Each of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
960. All of the following statements regarding the infectious etiologies of pericarditis are correct
EXCEPT:
A. Enteroviruses are among the most common causes of viral pericarditis
B. The most common organisms that cause bacterial pericarditis are streptococci and staphylococci
C. The prognosis of patients with bacterial pericarditis is poor
D. *Tuberculosis is the leading cause of constrictive pericarditis in Western nations
E. Antifungal therapy is generally not necessary in pericarditis caused by histolasmosis
961. All of the following statements regarding Chagas disease are correct EXCEPT
A. The level of parasitemia does not correspond to the severity of chronic Chagas disease
B. The disease is transmitted to humans by the reduviid bug (commonly called the kissing bug)
C. *The most common ECG abnormality in chronic Chagas disease is left bundle branch block
D. The classic echocardiographic findings are those of a dilated cardiomyopathy with an apical
aneurysm
E. All of the above statements are correct
962. Of the following disorders, choose one which is not associated with ventricular tachycardia as a
cause of syncope?
A. Hypertrophic obstructive cardiomyopathy
B. Prior myocardial infarction
C. *Atrial myxoma
D. Aortic valvular stenosis
E. Congenital long QT syndrome
963. All of the following statements regarding the ECG in acute pericarditis is true EXCEPT:
A. The majority of patients demonstrate ECG abnormalities
B. Global ST elevation is seen in early pericarditis
C. Sinus tachycardia is a common finding
D. PR depression is common in the majority of patients
E. *T wave inversions develop before ST elevations return to baseline
964. All the following features favor ventricular tachycardia as the cause of broad-complex tachycardia,
EXCEPT:
A. QRS duration with right bundle branch block morphology (RBBB) is greater than 140 ms, and
greater than 160 ms with left LBBB morphology
B. LAD with RBBB morphology, extreme LAD (northwest axis) with LBBB morphology
C. AV dissociation
D. *Response to carotid sinus massage
E. Concordance of the QRS pattern in all precordial leads (i.e., all positive or all negative deflections)
965. Which of the following will most likely respond to verapamil?
A. RVOT tachycardia
B. *Idiopathic LV tachycardia
C. Bundle branch re-entry tachycardia
D. ARVD ventricular tachycardia
E. All of the above
966. The most common type of arrhythmia in WPW syndrome is....
A. Ventricular tachycardia
B. Ventricular fibrillation
C. Ventricular premature complexes
D. Atrial ectopics
E. *AV re-entry tachycardia
967. Use of echocardiogram in the assessment of AF:
A. It is not necessary to perform a TTE in patients with AF
B. TEE is always needed to allow better assessment of the MV and LA
C. *TTE should be performed at baseline to diagnose associated structural/functional heart disease
D. TTE is necessary to determine stroke risk stratification for thromboprophylaxis in all patients
E. When TTE is technically difficult, MRI is needed to exclude cardiac abnormalities
968. Which is the preferred initial treatment strategy for rate control in AF patients?
A. Digoxin
B. *Beta-blockers or rate limiting CCB
C. Combination therapy of beta-blockers and rate-limiting CCB’s
D. Amiodarone
E. Combination therapy of digoxin and beta-blockers
969. Which option is better in regard to cardioversion?
A. *Synchronised DC shock to restore sinus rhythm
B. Amiodarone in all patients to restore sinus rhythm
C. Flecainide in patients with IHD to maintain sinus rhythm
D. Digoxin to restore sinus rhythm
E. Propaphenone to restore sinus rhythm in HCMP patients
970. Regarding antithrombotic treatment in AF:
A. Patients with asymptomatic AF have less risk of embolism than symptomatic patients
B. Patients with atrial flutter do not need antithrombotic treatment due to the low risk of embolism of
this arrhythmia
C. *Warfarin is the best option in patients with high risk of thromboembolism
D. Aspirin has a similar effect in stroke reduction to placebo
E. Paroxysmal AF has the lowest risk of embolism
971. Sudden cardiac death in patients >35 years old is most commonly associated with:
A. Hypertrophic cardiomyopathy
B. *Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
972. Congenital long QT syndrome can lead to
A. Complete heart block
B. *Polymorphic ventricular tachycardia
C. Acute myocardial infarction
D. Recurrent supraventricular tachycardia
E. All of the above
973. Bundle branch re-entry ventricular tachycardia is most commonly associated with:
A. Enhanced automaticity in the right bundle
B. Enhanced automaticity in the left bundle
C. Supranormal conduction in the His bundle
D. *Abnormally slow conduction in the His bundle
E. All of the above
974. All of the following are ECG manifestations of Wolff-Parkinson-White syndrome EXCEPT
A.
B.
C.
D.
E.
975.
A.
B.
C.
D.
E.
976.
A.
B.
C.
D.
E.
977.
A.
B.
C.
D.
E.
978.
A.
B.
C.
D.
E.
979.
A.
B.
C.
D.
E.
980.
A.
B.
C.
D.
E.
981.
A.
B.
C.
D.
E.
982.
A.
B.
C.
D.
E.
*Narrow QRS
Initial slurred QRS upstroke
Short PQ interval
Normal QT interval
All of the above
The initial manifestations of WPW syndrome may include which of the following?
Atrial fibrillation
AV re-entry tachycardia
Ventricular fibrillation
Wide-QRS tachycardia
*All of the above
The presence of an r prime in V1 during narrow-QRS tachycardia is suggestive of...
AV re-entry
*AV node re-entry
Rate-dependent BBB
Atrial tachycardia
Atrial fibrillation
Ventricular ectopic beats (VEBs) occurring in apparently normal hearts are:
Associated with a bad prognosis
Never frequent or complex
Less frequent with increasing age
*May be associated with symptoms of “missed beats”
Always symptomatic
In patients with ventricular ectopic beats:
Caffeine restriction always reduces symptoms
*High caffeine intake should always be discouraged in symptomatic patients
There is good evidence that reducing caffeine intake reduces ectopics
Hypertension has no association with frequency of ectopic beats
LVH is not associated with increased frequency of ectopics
Regarding ventricular ectopics and exercise:
*Ectopics are usually benign if they are supressed on exercise
Exercise-induced VEBs are not associated with adverse prognosis
RVOT ectopics are usually supressed on exercise
Ectopics induced on recovery after exercise are benign
All of the above
An idiopathic left ventricular tachycardia (VT) shows the following...
Typical LBBB morphology
*LAD and RBBB morphology
Associated with a high risk of sudden cardiac death and almost always requires ICD therapy
Never responds to verapamil
All of the above
Beta blockers are accepted treatment to prevent VT in:
Brugada syndrome, RVOT-VT, short QT syndrome and long QT syndrome
Brugada syndrome, RVOT-VT and long QT syndrome
*RVOT-VT and long QT syndrome
Short QT syndrome and long QT syndrome
Brugada syndrome and short QT syndrome
Wenckebach phenomenon is defined as...
Progressive shortening of PR interval till a beat is dropped
*Progressive lengthening of PR interval till a beat is dropped
Irregular heart rate and PVC’s
Shortened QT intervals
Slurred QRS complex
983. Giant a waves in JVP (“cannon” waves) are seen in
A. Sinus bradycardia
B. Atrial fibrillation
C. First-degree AV-block
D. *Complete heart block
E. Atrial ectopic
984. All of the following findings are suggestive of LVH except:
A. (S in V1 + R in V5 or V6) > 35 mm
B. R in aVL > 11 mm
C. R in aVF > 20 mm
D. (R in I + S in III) > 25 mm
E. *R in aVR > 8 mm
985. All of the following findings are suggestive of RVH except:
A. R in V1=7 mm (15 mm with RBBB)
B. (R in V1 + S in V5 or V6) > 10 mm
C. R < S in V6
D. R or R’ in V1
E. *S in V3 + R in aVL > 28 mm (20 mm for women)
986. When present, each of the following heart sounds occurs shortly after S2 EXCEPT:
A. Opening snap
B. Third heart sound
C. *Ejection clic
D. Tumor plop
E. Pericardial knock
987. Each of the following statements regarding splitting of the second heart sound is true EXCEPT:
A. Severe pulmonic valvular stenosis is associated with a softened P2
B. Delayed closure of the pulmonic valve with inspiration contributes to physiologic splitting of S2
C. Fixed splitting of S2 is the auscultatory hallmark of an ostium secundum atrial septal defect
D. Paradoxical splitting of S2 is expected in patients with a right ventricular electronically paced
rhythm
E. *Right bundle branch block is associated with paradoxical splitting of S2
988. The timing of an "innocent" murmur is usually:
A. Early systolic
B. Presystolic
C. *Midsystolic
D. Holosystolic
E. Early diastolic
989. Which of the following pairs of medical conditions and antihypertensive medications would be
incorrect to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
990. Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
991. Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
992. You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
993. Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
994. All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
995. Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
996. Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
997. Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium restriction
C. Moderation of alcohol consumption
D. Vegetarian diet
E. Calcium supplement
998. Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
999. Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. *Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
1000.Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
1001.Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
1002.Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
1003.A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
1004.The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
1005.All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
1006.All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. *People of African descent commonly have a high renin type hypertension
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
1007.Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
1008.Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
1009.Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
1010.Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
1011.Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
1012.All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
1013.The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
1014.A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
1015.A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
1016.In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
1017.In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
1018.The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
1019.The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
1020.In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
1021.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
1022.All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
1023.Which of the following diagnostic studies is most likely to demonstrate the cause of the headaches?
A. MRI of the head
B. MRI of the kidney
C. *MRI of the thorax
D. 24-h urinary 5-HIAA
E. 24-h urinary free cortisol
1024.A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the likely diagnosis?
A. Congenital adrenal hyperplasia
B. Fibromuscular dysplasia
C. Cushing’s syndrome
D. *Conn’s syndrome
E. Pheochromocytoma
1025.A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the best way to diagnose this disease ?
A. Renal vein renin levels
B. 24-h urine collection for metanephrines
C. MRI of the renal arteries
D. 24-h urine collection for cortisol
E. *Plasma aldosterone/renin ratio
1026.A 21-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What is the best medication for the management of this patient’s
hypertension?
A. *Phentolamine
B. Fenoldopam
C. Esmolol
D. Nicardipine
E. Diazoxide
1027.A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What test would best determine the patient’s diagnosis?
A. Plasma catecholamines
B. 24-h urine collection for 5-HIAA
C. Abdominal CT scan
D. *24-h urine collection for metanephrines and vanilylmandelic acid
E. Adrenal vein sampling for renin levels
1028.What is the correct feature of the hypertensive urgency?
A. It is always a life-threatening situation
B. Patient must be hospitalized
C. *Patients can be managed as outpatients
D. Therapy should not be given orally
E. None of the above
1029.If there is suspicion of phaeochromocytoma, the first line drug is:
A. Sodium-nitroprusside
B. Nifedipine
C. *Phentolamine
D. Verapamil
E. Enalapril
1030.If you are in your office and a patient sees you with the following symptoms: long history of
hypertension, home BP usually 160/100 mmHg, suddenly developed severe headache
blurred vision, weakness in the right arm, blood pressure: 200/110 mmHg, What will you do:
A. Give the patient 20 mg nifedipine orally, and check the BP in 15 min. If it is still >200/100 mmHg,
give another dose of nifedipine
B. Give the patient 20 mg nifedipine, and check the BP in 30 min. If it is 160/80 mmHg, send the
patient home and give another appointment in two weeks
C. Give the patient 10 mg amlodipine, send the patient home and give another appointment in two
days
D. Call the ambulance and send the patient to the nearest hospital
E. *Give the patient some pain-killer drug (e.g. acetaminophen), call the ambulance and send the
patient to the nearest hospital with stroke-unit
1031.A 28-year-old male with type 1 diabetes mellitus is seen in the clinic for routine follow-up. The
patient has hypertension. He is being maintained on an insulin pump and lisinopril 5 mg daily. He has
been on this dose of lisinopril for approximately 6 weeks. He has normal creatinine and no proteinuria.
BP is 140/90 mmHg. What do you recommend ?
A. Continue the current dose of lisinopril and return for follow-up in 3 months as the patient has
received his target BP of less than 140/90 mmHg
B. Ask a patient to return in 6 weeks; if his BP remains at this level, increase the dose of lisinopril
C. *Increase lisinopril to 10 mg daily to achieve a goal BP of less than 130/80 mmHg
D. Assure the patient that he is suffering from “white-coat hypertension” and plan no intervention
E. Switch the patient from lisinopril to losartan
1032.A 49-year-old female presents to you for an initial visit to establish health care. She has no past
medical history and denies a family history of diabetes mellitus, early cardiovascular disease, or renal
disease. Her BP on presentation is 185/110 mmHg. She denies headache or visual complaints. She has no
chest pain, shortness of breath, or change in urine color. Her physical examination is normal with the
exception of an S4 gallop heard at the 4th intercostal space just to the left of the sternum. An ECG is
significant for LVH and LAD. there are no signs of cardiac ischemia. Urinalysis shows no red blood cells
or proteinuria. What is your recommendation for therapy for this patient?
A. *Initiate therapy with hydrochlorothiazide in combination with a beta-blocker
B. Initiate therapy with hydrochlorothiazide alone
C. Initiate therapy with an ACE inhibitor alone
D. Advise the patient to go to the nearest emergency department for further treatment for a
hypertensive emergency
E. Advise the patient on lifestyle modifications and plan a return visit in 3 weeks
1033.What will you do if you are on duty in a hospital and a hypertensive patient, who has been treated
with long-acting ß-blocker, long-acting dihydropyridine calcium antagonist and long-acting a-1
adrenoceptor blocker, is admitted with the following symptoms: headache, dyspnea, ankle-swelling, BP
180/110 mmHg, pulmonary rales, LVH on ECG, echo: LVH, left ventricular diastolic dysfunction,
ejection fraction 46%.
A. Amlodipine orally
B. Nifedipine orally
C. Enalaprilate iv
D. *Enalaprilate iv + furosemide iv
E. Esmolol iv
1034.Which of the following blood pressure levels in pregnancy should be considered an emergency
requiring hospitalization?
A. ≥140/90 mmHg
B. ≥150/95 mmHg
C. ≥160/100 mmHg
D. *≥170/110 mmHg
E. A rise in SBP ≥25 mmHg or a rise in DPB ≥15 mmHg compared to pre-pregnancy values, or those
in the first trimester
1035.The following drug combinations are effective to treat hypertension EXCEPT
A. Diuretics + beta-blockers
B. Beta-blockers + dihydropiridine calcium channel blockers
C. Diuretics + ACE-inhibitors/ARB
D. ACE-inhibitors/ARB + calcium channel blockers
E. *Beta-blockers + ACE-inhibitors/ARB
1036.Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
1037.With respect to renovascular disease, all of the statements are true EXCEPT:
A. Worsening renal function with ACE-inhibitor therapy suggests bilateral renovascular disease
B. Atherosclerotic disease most commonly involves the proximal third of the main renal artery
C. The most common form of fibroplastic renovascular disease in adults involves the media
D. *The incidence of renovascular hypertension falls with increased age
E. Patients with severe, accelerated hypertension have the highest prevalence of renovascular disease
1038.A newly diagnosed diabetic patient presents with BP readings that are 155/95 or higher. All of the
following statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blockade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
1039.All of the following statements regarding the association of oral contraceptive pills and
hypertension are correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
1040.Each of the following statements regarding pheochromocytoma is true EXCEPT:
A. Approximately 15% of pheochromocytomas are extra-adrenal
B. Ten percent of pheochromocytomas are malignant
C. Ten percent of adrenal pheochromocytomas are bilateral
D. *Hypertension related to pheochromocytoma is nearly always episodic and only rarely persistent
E. Pheochromocytoma can be inherited
1041.All of the following are features of renovascular hypertension due to fibromuscular hyperplasia, as
opposed to atherosclerosis, EXCEPT:
A. Age <50 years
B. Female gender
C. *More likely to progress to complete renal artery occlusion
D. No family history of hypertension
E. Absence of carotid bruits
1042.Which of the following ACE-inhibitors are not prodrugs?
A. Captopril, lisinopril, ramipril
B. Lisinopril, enalapril, banazepril
C. *Captopril, lisinopril, enalaprilat
D. Moexipril, captopril, lisinopril
E. Perindopril, ramipril, enalapril
1043.Each of the following statements regarding hypertension is true EXCEPT:
A. The prevalence of hypertension rises progressively with age in both men and women
B. Systolic and diastolic hypertension are each associated with an increased crisk of coronary heart
disease
C. *The target blood pressure for hypertensive patients with cardiovascular disease or diabetes is
140/90 mmHg
D. Patients with prehypertension (SBP 120-139 mmHg or DBP 80-89 mmHg) benefit from lifestyle
modifications incl. weight reduction, regular exercise, and smoking cessation
E. Drug therapy of hypertension benefits patients greater than 80 years of age
1044.All of the following interventions have a BP-lowering effect EXCEPT:
A. A diet that reduces caloric intake by 1000 calories per day
B. Reduction of dietary sodium
C. *Daily magnesium supplements
D. Tobacco cessation
E. Reduction of ethanol consumption to less than 30 ml/day
1045.Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
1046.Each of the following statements regarding hypertension is true EXCEPT:
A. Increased LV muscle mass in hypertension is an independent risk factor of cardiac mortality
B. The risk of ventricular arrhythmias in hypertension is increased 2-fold in the presence of LV
hypertrophy
C. Low birth weight is associated with an increased incidence of hypertension later in life
D. *Chronic caffeine consumption is associated with an increased risk of hypertension
E. In hypertensive adolescents, essential hypertension is the most likely etiology
1047.The following statements regarding the association of oral contraceptive pills and hypertension are
correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
1048.Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
1049.Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
1050.Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
1051.All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
1052.Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1053.Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
1054.Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
1055.Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
1056.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. * Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
1057.Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
1058.Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
1059.Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
1060.A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
1061.The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
1062.All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
1063.All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. *People of African descent commonly have a high renin type hypertension
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
1064.Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
1065.Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
1066.Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
1067.Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
1068.Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
1069.All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
1070.At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
1071.The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
1072.In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
1073.In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
1074.The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
1075.The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
1076.In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
1077.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
1078.All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
1079.Which of the following is an effective adjunct to increase the rate of smoking cessation?
A. Aldosterone
B. *Bupropion
C. Sildenafil
D. Cimetidine
E. Buspirone
1080.With which of the following is sildenafil acetate (Viagra) most likely to interact adversely?
A. Fibrinolytic therapy
B. Primary PCI
C. *Nitrates
D. Aspirin
E. Beta-blockers
1081.Bupropion hydrochloride (Zyban) is contraindicated in patients with a history of which of the
following?
A. *Seizures
B. Insulin-dependent diabetes mellitus
C. Severe chronic obstructive pulmonary disease (with reversible component)
D. Longer than 40-year history of tobacco use
E. Recent MI
1082.In which of the following has the high-sensitivity C-reactive protein (CRP) been shown to be
predictive of risk?
A. Acute MI
B. Acute coronary syndromes
C. Chronic stable angina
D. Peripheral vascular disease
E. *All of the above
1083.Which of the following has been shown to decrease the level of the high-sensitivity CRP?
A. Unopposed estrogen
B. Amlodipine besylate (Norvasc)
C. *Simvastatin
D. All of the above
E. None of the above
1084.All of the following statements regarding myocardial stunning are true EXCEPT:
A. *Stunning is a state of depressed myocardial function due to chronic hypoperfusion
B. Stunning can be global or regional
C. Stunning can follow cardiac surgery with cardiopulmonary bypass
D. Oxygen-free radicals and excess intracellular calcium likely contribute to stunning
E. Stunning affects both systolic and diastolic function
1085.What is the most common coexisting congenital anomaly in patients with coarctation of the aorta?
A. Cleft mitral valve
B. *Bicuspid aortic valve
C. Ebstein's anomaly
D. VSD
E. PDA
1086.All of the following are characteristic findings of ostium primum atrial septal defect (ASD)
EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Right axis deviation
D. Systolic ejection murmur
E. Prominent pulmonary vascular markings on CXR
1087.Choose the adult congenital disorder corresponding to the following physical examination fingings:
RV lift with a loud systolic ejection murmur along the left sternal border, with a single S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
1088.Choose the adult congenital disorder corresponding to the following physical examination fingings:
loud S1, holosystolic murmur in left sternal border, systolic ejection click, and hepatomegaly
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
1089.Choose the adult congenital disorder corresponding to the following physical examination fingings:
weak or delayed femoral pulses, harsh systolic murmur in the back, and a systolic ejection click in the
aortic area
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1090.Choose the adult congenital disorder corresponding to the following physical examination fingings:
cyanosis, digital clubbing, loud P2, and a variable Graham-Steel murmur
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1091.Choose the adult congenital disorder corresponding to the following physical examination fingings:
wide pulse pressure, prominent LV impulse, and a continuous machinery murmur enveloping S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *Patent ductus arteriosus
D. Ebstein's anomaly
E. Tetralogy of Fallot
1092.Bacterial endocarditis prophylaxis is indicated in all adults who have the following congenital heart
disease EXCEPT:
A. VSD
B. Coarctation of the aorta
C. *Secundum ASD
D. Hypertrophic obstructive cardiomyopathy
E. PDA
1093.Besides pulmonary valve stenosis, which of the following is the most common associated cardiac
defect present in patients with PA stenosis?
A. *VSD
B. ASD
C. Coarctation of the aorta
D. PDA
E. Bicuspid aortic valve
1094.All of the following statements regarding patent ductus arteriosus (PDA) are true EXCEPT:
A. *The majority of cases close spontaneously after infancy
B. There is a higher incidence in mothers who acquired rubella during pregnancy
C. A decrease in the duration and intensity of the murmur has a poor prognostic implication
D. Left ventricular hypertrophy precedes RV hypertrophy
E. If it is uncorrected, approximately one third of patients die by the age of 40 years
1095.Ostium primum ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. *Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1096.Noonan's syndrome is commonly associated with...
A. Supravalvular aortic stenosis
B. *Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1097.Coronary sinus ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. *Persistent left superior vena cava
1098.Williams syndrome is commonly associated with...
A. Supravalvular aortic stenosis
B. *Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1099.Sinus venosus ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. *Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1100.All of the following physical examination findings are usually associated with ostium secundum
ASD EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Lateral and inferior displacement of the apex beat
D. Soft systolic ejection murmur in the second left intercostal space
E. Normal S1
1101.Which of the following is an absolute contraindication to pregnancy?
A. Surgically corrected transposition of great arteries (TGA)
B. Congenitally corrected TGA
C. Ebstein's anomaly
D. *Eisenmenger's syndrome
E. Status post Fontan operation
1102.The lesions that constitute tetralogy of Fallot include all of the following EXCEPT
A. A ventricular septal defect
B. An overriding aorta
C. *An atrial septal defect
D. Right ventricular outflow obstruction
E. Right ventricular hypertrophy
1103.Match the chest radiography findings (Fig. 1.11) with the corresponding congenital disorder
A. *Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1104.Match the chest radiography findings (Fig. 1.12) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. *Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1105.Match the chest radiography findings (Fig. 1.13) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. *Tetralogy of Fallot
E. Coarctation of the aorta
1106.Match the chest radiography findings (Fig. 1.14) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. *Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1107.All of the following are indications for surgical closure of an ASD EXCEPT:
A. Significant symptoms in a 65-year-old
B. RV dysfunction
C. *Pulmonary vascular resistance >15 Wood units that does not diminish with vasodilators
D. An asymptomatic 20-year-old with a Qp/Qs of 1,7 with no pulmonary hypertension
E. RV enlargement
1108.The following cardiovascular malformations are all associated with congenital rubella EXCEPT:
A. PDA
B. PA stenosis
C. *Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1109.Which of the following syndromes is associated with pumonary arterio-venous fistula?
A. Williams syndrome
B. *Weber-Osler-Rendu syndrome
C. Bland-Garland-White syndrome
D. Kartagener's syndrome
E. Crouzon's syndrome
1110.Congenital MR is commonly encountered in all of the following conditions EXCEPT:
A. *Cor triatriatum
B. Ostium primum ASD
C. Coarctation of the aorta
D. Congenitally corrected TGA
E. Subaortic stenosis
1111.In which of the following cases is surgical correction recommended?
A. Asymptomatic small VSD to decrease risk of endocarditis
B. PDA with severe pulmonary hypertension
C. *Asymptomatic subaortic stenosis with severe aortic valve insufficiency
D. Coarctation of the aorta with a transcoarctation gradient of 20 mmHg
E. Small ASD to prevent paradoxical embolization
1112.Which congenital disorder corresponds with the following chest radiography findings: prominent
central PAs (possible calcifications) and peripheral PA prunning?
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1113.Which congenital disorder corresponds with the following chest radiography findings: right aortic
arch, RV enlargement, and a "boot-shaped" heart?
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
1114.Which congenital disorder corresponds with the following chest radiography findings: marked
cardiomegaly, severe right atrial enlargement, and normal lung fields
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
1115.Which congenital disorder corresponds with the following chest radiography findings: posterior rib
notching and a "reverse E" or "3" sign
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1116.Which congenital disorder corresponds with the following chest radiography findings: pulmonary
plethora, prominent ascending aorta, proximal PA dilatation, and opacity at the confluence of the aortic
knob and descending aorta
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1117.Which of the following statements regarding Ebstein's anomaly is NOT correct?
A. An ASD or PFO is present in up to 80% of patients
B. The cardinal feature is an apically displaced tricuspid valve resulting in atrialization of ventricular
tissue
C. WPW syndrome is common in these patients and multiple tracts can exist
D. *A bicuspid aortic valve is commonly present
E. A "sail sound" is a common finding on physical examination
1118.Which of the following syndromes and cardiac anomalies are INCORRECTLY matched?
A. Trisomy 21 – atrioventricular canal defects
B. Noonan syndrome – pulmonic stenosis
C. Holt-Oram syndrome – atrial septal defects
D. Marfan syndrome – mitral valve prolapse
E. *Williams syndrome – ventricular septal defects
1119.All of the following statements regarding the effects of maneuvers on the auscultation of cardiac
murmurs are true EXCEPT:
A. In patent ductus arteriosus (PDA), the diastolic phase of the murmur is intensified by isometric
handgrip
B. *The murmur of hypertrophic obstructive cardiomyopathy becomes softer with standing or during a
Valsalva strain maneuver
C. The murmur of a ventricular septal defect (VSD) increases with isometric handgrip
D. Sudden squatting or isometric handgrip increases the diastolic murmur of aortic regurgitation
E. The mid-diastolic and presystolic murmurs of mitral stenosis become louder with exercise
1120.Radiotherapy for malignant disease may affect the heart in all of the following ways EXCEPT
A. Pericarditis
B. Coronary artery disease
C. Valvular stenosis
D. Conduction abnormalities
E. *Asymmetrical septal hypertrophy
1121.Sudden cardiac death due to ventricular tachyarrhythmias is an established complication of each of
the following EXCEPT:
A. Sarcoidosis
B. Giant cell myocarditis
C. Chagas disease
D. Idiopathic dilated cardiomyopathy
E. *Hyperthyroidism
1122.Characteristics of arrhythmogenic RV dysplasia include all of the following EXCEPT
A. Fatty infiltration of the right ventricle
B. *Fatty infiltration of the right atrium
C. Monomorphic ventricular tachycardia
D. Abnormal signal-averaged ECG
E. Possible detection by cardiac MRI
1123.All of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
1124.Each of the statements about the evolution of the ECG in acute pericarditis is correct EXCEPT:
A. Four sequential stages of abnormalities of the ST segments and T waves are typical
B. *Initial ST segment elevation is usually most prominent in ECG lead aVR
C. The ratio of the height of ST segment elevation to the height of the T wave in acute pericarditis is
typically >0.25 in lead V6
D. In acute pericarditis, the ST segment usually returns to baseline before the appearance of T wave
inversion
E. T wave inversion may persist for months after the acute presentation
1125.Which of the following statements regarding cardiac involvement in Lyme disease is CORRECT?
A. Cardiac manifestations of Lyme disease typically occur within several days of the development of
erythema chronicum migricans
B. *Ten percent of patients with Lyme disease develop cardiac manifestations
C. Supraventricular and ventricular tachyarrhythmias are the most common cardiac manifestations of
Lyme disease
D. Cardiomegaly and congestive heart failure are common among patients who develop Lyme carditis
E. Antibiotic therapy has been proven to shorten the course of active Lyme carditis
1126.Each of the following statements regarding the infectious etiologies of pericarditis is correct
EXCEPT:
A. Enteroviruses are among the most common causes of viral pericarditis
B. The most common organisms that cause bacterial pericarditis are streptococci and staphylococci
C. The prognosis of patients with bacterial pericarditis is poor
D. *Tuberculosis is the leading cause of constrictive pericarditis in Western nations
E. Antifungal therapy is generally not necessary in pericarditis caused by histolasmosis
1127.Each of the following statements regarding Chagas disease is correct EXCEPT
A. The level of parasitemia does not correspond to the severity of chronic Chagas disease
B. The disease is transmitted to humans by the reduviid bug (commonly called the kissing bug)
C. *The most common ECG abnormality in chronic Chagas disease is left bundle branch block
D. The classic echocardiographic findings are those of a dilated cardiomyopathy with an apical
aneurysm
E. All of the above statements are correct
1128.Which of the following disorders is not associated with ventricular tachycardia as a cause of
syncope?
A. Hypertrophic obstructive cardiomyopathy
B. Prior myocardial infarction
C. *Atrial myxoma
D. Aortic valvular stenosis
E. Congenital long QT syndrome
1129.Each of the following statements regarding the ECG in acute pericarditis is true EXCEPT:
A. The majority of patients demonstrate ECG abnormalities
B. Global ST elevation is seen in early pericarditis
C. Sinus tachycardia is a common finding
D. PR depression is common in the majority of patients
E. *T wave inversions develop before ST elevations return to baseline
1130.Each of the following statements regarding endomyocardial fibrosis (EMF) is correct EXCEPT:
A. This condition is characteristically found in tropical and subtropical Africa
B. It is predominantly a disease of children and young adults
C. *Involvement of the mitral apparatus typically results in mitral stenosis
D. EMF involves the left ventricle in 90% of affected patients
E. Echocardiographic features include increased endocardial echoreflectivity, fibrotic obliteration of
apex, atrial enlargement, and pericardial effusion
1131.All of the following statements with regard to primary endocardial fibroelastosis (EFE) are correct
EXCEPT:
A. The condition is often familial
B. The mitral and aortic valve leaflets are usually thickened and distorted
C. *The murmur of mitral stenosis is the most common auscultatory finding
D. Symptoms of primary EFE usually develop between 2 and 12 months of age
E. Echocardiographic features include a reduced ejection fraction and increased left atrial and left
ventricular dimensions
1132.Which of the following therapies improves survival in patients with cor pulmonare secondary to
COPD?
A. Digoxin
B. *Oxygen
C. Beta-adrenergic agonists
D. Theophylline
E. Hydralazine
1133.What is NOT a cause of chronic cor pulmonale?
A. COPD
B. Recurrent pulmonary emboli
C. *Mitral stenosis
D. Kyphoscoliosis
E. Obstructive sleep apnea
1134.Which of the following conditions is associated with increased left ventricular preload?
A. Sepsis
B. Right ventricular infarction
C. *Mitral regurgitation
D. Dehydration
E. Pulmonary embolism
1135.Each of the following conditions is associated with the development of pulmponary edema
EXCEPT:
A. Increased pulmonary venous pressure
B. High altitude
C. *Increased plasma oncotic pressure
D. Eclampsia
E. Heroin overdose
1136.The statements about the diagnosis of PE include all of the following EXCEPT:
A. Arterial blood gas measurement is often unhelpful in the diagnosis of acute PE
B. The most common ECG finding in patients with PE is sinus tachycardia
C. Pulmonary infarction due to PE can be visualized on a standard chest radiograph
D. *Reduced intensity of the pulmonic component of the second heart sound is typical in patients with
large PE
E. Fibrin-degradation products (e.g., D-dimer) are commonly elevated in patients with PE
1137.Heart failure is:
A. Decreasing in incidence and prevalence due to recent advances in the treatment of cardiovascular
disease
B. *One of the diagnoses with the highest readmission rate
C. A common condition across all ages
D. Can be diagnosed from a clinical response to treatment
E. All of the above statements are correct
1138.According to the ESC guidelines, the following patients have heart failure:
A. An obese, dyspnoeic lady with swollen anckles but a normal echocardiogram
B. An asymptomatic man with a previous MI and area of hypokinesis on his echocardiogram
C. *A hypertensive man with LVH, fast atrial fibrillation and dyspnea
D. An elderly man with a few basal crepitations but a normal echocardiogram
E. All of the above
1139.Which of the following sometimes occur when heart failure is absent?
A. Gallop rhythm
B. Anckle oedema
C. A past history of a MI
D. *B and C
E. A, B, and C
1140.B-type natriuretic secretion is regulated by:
A. Fluid accumulation in the lungs
B. *Pressure and volume of the left ventricle
C. Oedema in the anckles
D. Auricular end diastolic pressure
E. All of the above
1141.Which of the following statements are true ?
A. A normal resting ECG is rare in angina pectoris
B. A normal resting ECG is common in heart failure
C. *Cardiomegaly plus pleural effusions make heart failure very likely
D. Atrial fibrillation commonly does not cause dyspnoea in patients with LVH and diastolic
dysfunction
E. All of the above
1142.The value of BNP in the diagnosis of heart failure in the emergency room in patients with acute
dyspnoea:
A. *Is supported by a BNP concentration >500 pg/ml
B. Is excluded by a NT-proBNP concentration <1000 pg/ml
C. Is restricted to patients without a previous history of heart failure
D. Has not been evaluated in patients with renal dysfunction
E. All of the above statements are true
1143.Which symptoms/signs occur when the HF is relatively advanced ?
A. Cardiomegaly on chest X-ray
B. Orthopnea
C. Exertional dyspnea
D. A abd B
E. *All of the above
1144.All patients with heart failure should be advised to:
A. Refrain from smoking
B. Restrict sodium intake
C. Receive a flu shot
D. A and B
E. *All of the above
1145.Exercise training in chronic heart failure
A. *Has been shown to increase peak oxygen consumption by 15-20% in randomized controlled trials
B. Has been shown to increase LV ejection fraction by 15-20% in randomized controlled trials
C. Is not recommended in heart failure
D. Has never been shown to reduce mortality and morbidity
E. Non of above
1146.Drugs that should be avoided in heart failure patients are:
A. Non-steroidal anti-inflammatory drugs (NSAIDS)
B. Corticosteroids
C. Beta-blockers
D. *A and B
E. All of the above
1147.The followings improve the survival figure in chronic congestive heart failure as shown by many
studies...EXCEPT
A. Bisoprolol
B. Metoprolol succinate
C. *Atenolol
D. Spironolactone
E. Carvedilol
1148.The following drugs have significantly improved survival in HF patients
A. *ACE inhibitors
B. Nitrates
C. Digoxin
D. Diuretics
E. All of the above
1149.Which of the statements about beta-blocker treatment in HF is true?
A. Randomised clinical trials show that b blockers are beneficial in patients with heart failure and
preserved left ventricular function
B. Elderly patients are the most frequently studied population in blocker trials
C. * Blockers exert a favourable effect in heart failure due to ischaemic and non-ischaemic aetiology
D. Patients with diabetes should always be excluded from blocker treatment
E. There is clear evidence that end stage heart failure patients should be treated with blockers
1150.Which of the statements about beta-blocker treatment in HF is true?
A. *Beta-blockers must be started at very low dosages
B. Treatment should be started when patients are unstable in order to stabilize them
C. When patients are treated with ACE inhibitors, blockers are contraindicated
D. Treatment should always be started during hospital stay
E. The most frequent adverse reaction to a blocker is cough
1151.Which of the statements about antiarrhythmic therapy treatment in HF is NOT true?
A. Amiodarone is an antiarrhythmic drug whose use can improve symptoms of patients with heart
failure without affecting myocardial function and survival
B. *Class I antiarrhythmic agents reduce mortality of patients with heart failure
C. In patients with documented life threatening ventricular arrhythmias, implantable cardioverterdefribrillators (ICDs) can reduce sudden death
D. Sudden death is one of the most frequent causes of death in patients with heart failure
E. The reduction of the number of premature ectopic beats with antiarrhythmic drugs can prevent
sudden mortality of heart failure patients
1152.A prophylactic ICD is useful for reducing total mortality in patients:
A. With previous myocardial infarction and low ejection fraction
B. With dilated cardiomyopathy and low ejection fraction
C. With previous myocardial infarction and low ejection fraction and broad QRS
D. A and C
E. *All of the above
1153.Biventricular pacing in severe heart failure and broad QRS:
A. Improves NYHA class
B. Improves exercise tolerance
C. Reduces hospitalisation for heart failure
D. Reduces heart rate
E. *All of the above
1154.Which of the following treatments most consistently improves EF in patients who have systolic
heart failure?
A. Diuretics
B. Beta-blockers
C. *ACE-inhibitors
D. Vasodilators
E. All of the above
1155.BNP has which of the following properties?
A. Urine volume increases
B. Sodium excretion is enhanced
C. More BNP is secreted
D. A decrease in plasma aldosterone concentration occurs
E. *All of the above occur
1156.All of the following are indications for heart transplantation EXCEPT
A. Dilated cardiomyopathy
B. Diabetes mellitus
C. Hypertrophic cardiomyopathy
D. Age 60 to 70 years
E. *Amyloid heart disease
1157.When used chronically, all of the following drugs increase mortality EXCEPT
A. Milrinone
B. Dobutamine
C. Vesnarinone
D. Xamoterol
E. *Amlodipine
1158.Primary causes of diatolic heart failure include all of the following EXCEPT
A. Hypertrophic cardiomyopathy
B. *Dilated cardiomyopathy
C. Hypertension
D. Ischemic cardiomyopathy
E. Infiltrative cardiomyopathy
1159.Match the description with the associated form of therapy for pulmonary embolism: may be
effective in PE even 1 to 2 weeks after the onset of symptoms
A. Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. *Both
D. Neither
E. Not applicable
1160.Match the description with the associated form of therapy for pulmonary embolism: dissolution of
recently formed thrombus is a major action
A. Unfractionated heparin or low molecular weight heparin
B. *Fibrinolytic therapy
C. Both
D. Neither
E. Not applicable
1161.Match the description with the associated form of therapy for pulmonary embolism: in general,
should be administered along with an antiplatelet agent
A. Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. Both
D. *Neither
E. Not applicable
1162.Match the description with the associated form of therapy for pulmonary embolism: may cause
aldosterone depression
A. *Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. Both
D. Neither
E. Not applicable
1163.Match the ECG finding that is most closely associated with chronic Chagas disease:
A. Low QRS voltage
B. AV nodal block
C. *Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
1164.Match the ECG finding that is most closely associated with sarcoidosis:
A. Low QRS voltage
B. *AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
1165.Match the ECG finding that is most closely associated with apical hypertrophic cardiomyopathy
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. *Deeply inverted precordial T waves
1166.Match the ECG finding that is most closely associated with cardiac amyloidosis
A. *Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
1167.Heart may be affected by radiotherapy in all of the following ways EXCEPT
A. Pericarditis
B. Coronary artery disease
C. Valvular stenosis
D. Conduction abnormalities
E. *Asymmetrical septal hypertrophy
1168.SCD (sudden cardiac death) due to ventricular tachyarrhythmias is an established complication of
each of the following EXCEPT:
A. Sarcoidosis
B. Giant cell myocarditis
C. Chagas disease
D. Idiopathic dilated cardiomyopathy
E. *Hyperthyroidism
1169.Arrhythmogenic RV dysplasia is characterized by all of the following EXCEPT
A. Fatty infiltration of the right ventricle
B. *Fatty infiltration of the right atrium
C. Monomorphic ventricular tachycardia
D. Abnormal signal-averaged ECG
E. Possible detection by cardiac MRI
1170.Each of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
1171.All of the following statements regarding the infectious etiologies of pericarditis are correct
EXCEPT:
A. Enteroviruses are among the most common causes of viral pericarditis
B. The most common organisms that cause bacterial pericarditis are streptococci and staphylococci
C. The prognosis of patients with bacterial pericarditis is poor
D. *Tuberculosis is the leading cause of constrictive pericarditis in Western nations
E. Antifungal therapy is generally not necessary in pericarditis caused by histolasmosis
1172.All of the following statements regarding Chagas disease are correct EXCEPT
A. The level of parasitemia does not correspond to the severity of chronic Chagas disease
B. The disease is transmitted to humans by the reduviid bug (commonly called the kissing bug)
C. *The most common ECG abnormality in chronic Chagas disease is left bundle branch block
D. The classic echocardiographic findings are those of a dilated cardiomyopathy with an apical
aneurysm
E. All of the above statements are correct
1173.Of the following disorders, choose one which is not associated with ventricular tachycardia as a
cause of syncope?
A. Hypertrophic obstructive cardiomyopathy
B. Prior myocardial infarction
C. *Atrial myxoma
D. Aortic valvular stenosis
E. Congenital long QT syndrome
1174.All of the following statements regarding the ECG in acute pericarditis is true EXCEPT:
A. The majority of patients demonstrate ECG abnormalities
B. Global ST elevation is seen in early pericarditis
C. Sinus tachycardia is a common finding
D. PR depression is common in the majority of patients
E. *T wave inversions develop before ST elevations return to baseline
1175.All the following features favor ventricular tachycardia as the cause of broad-complex tachycardia,
EXCEPT:
A. QRS duration with right bundle branch block morphology (RBBB) is greater than 140 ms, and
greater than 160 ms with left LBBB morphology
B. LAD with RBBB morphology, extreme LAD (northwest axis) with LBBB morphology
C. AV dissociation
D. *Response to carotid sinus massage
E. Concordance of the QRS pattern in all precordial leads (i.e., all positive or all negative deflections)
1176.Which of the following will most likely respond to verapamil?
A. RVOT tachycardia
B. *Idiopathic LV tachycardia
C. Bundle branch re-entry tachycardia
D. ARVD ventricular tachycardia
E. All of the above
1177.The most common type of arrhythmia in WPW syndrome is....
A. Ventricular tachycardia
B. Ventricular fibrillation
C. Ventricular premature complexes
D. Atrial ectopics
E. *AV re-entry tachycardia
1178.Use of echocardiogram in the assessment of AF:
A. It is not necessary to perform a TTE in patients with AF
B. TEE is always needed to allow better assessment of the MV and LA
C. *TTE should be performed at baseline to diagnose associated structural/functional heart disease
D. TTE is necessary to determine stroke risk stratification for thromboprophylaxis in all patients
E. When TTE is technically difficult, MRI is needed to exclude cardiac abnormalities
1179.Which is the preferred initial treatment strategy for rate control in AF patients?
A. Digoxin
B. *Beta-blockers or rate limiting CCB
C. Combination therapy of beta-blockers and rate-limiting CCB’s
D. Amiodarone
E. Combination therapy of digoxin and beta-blockers
1180.Which option is better in regard to cardioversion?
A. *Synchronised DC shock to restore sinus rhythm
B. Amiodarone in all patients to restore sinus rhythm
C. Flecainide in patients with IHD to maintain sinus rhythm
D. Digoxin to restore sinus rhythm
E. Propaphenone to restore sinus rhythm in HCMP patients
1181.Regarding antithrombotic treatment in AF:
A. Patients with asymptomatic AF have less risk of embolism than symptomatic patients
B. Patients with atrial flutter do not need antithrombotic treatment due to the low risk of embolism of
this arrhythmia
C. *Warfarin is the best option in patients with high risk of thromboembolism
D. Aspirin has a similar effect in stroke reduction to placebo
E. Paroxysmal AF has the lowest risk of embolism
1182.Sudden cardiac death in patients >35 years old is most commonly associated with:
A. Hypertrophic cardiomyopathy
B. *Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
1183.Congenital long QT syndrome can lead to
A. Complete heart block
B. *Polymorphic ventricular tachycardia
C. Acute myocardial infarction
D. Recurrent supraventricular tachycardia
E. All of the above
1184.Bundle branch re-entry ventricular tachycardia is most commonly associated with:
A. Enhanced automaticity in the right bundle
B. Enhanced automaticity in the left bundle
C. Supranormal conduction in the His bundle
D. *Abnormally slow conduction in the His bundle
E. All of the above
1185.All of the following are ECG manifestations of Wolff-Parkinson-White syndrome EXCEPT
A. *Narrow QRS
B. Initial slurred QRS upstroke
C. Short PQ interval
D. Normal QT interval
E. All of the above
1186.The initial manifestations of WPW syndrome may include which of the following?
A. Atrial fibrillation
B. AV re-entry tachycardia
C. Ventricular fibrillation
D. Wide-QRS tachycardia
E. *All of the above
1187.The presence of an r prime in V1 during narrow-QRS tachycardia is suggestive of...
A. AV re-entry
B. *AV node re-entry
C. Rate-dependent BBB
D. Atrial tachycardia
E. Atrial fibrillation
1188.Ventricular ectopic beats (VEBs) occurring in apparently normal hearts are:
A. Associated with a bad prognosis
B. Never frequent or complex
C. Less frequent with increasing age
D. *May be associated with symptoms of missed beats
E. Always symptomatic
1189.In patients with ventricular ectopic beats:
A. Caffeine restriction always reduces symptoms
B. *High caffeine intake should be discouraged in symptomatic patients
C. There is good evidence that reducing caffeine intake reduces ectopics
D. Hypertension has no association with frequency of ectopic beats
E. LVH is not associated with increased frequency of ectopics
1190.Regarding ventricular ectopics and exercise:
A. *Ectopics are usually benign if they are supressed on exercise
B. Exercise-induced VEBs are not associated with adverse prognosis
C. RVOT ectopics are usually supressed on exercise
D. Ectopics induced on recovery after exercise are benign
E. All of the above
1191.An idiopathic left ventricular tachycardia (VT) shows the following...
A. Typical LBBB morphology
B. *LAD and RBBB morphology
C. Associated with a high risk of sudden cardiac death and almost always requires ICD therapy
D. Never responds to verapamil
E. All of the above
1192.Beta blockers are accepted treatment to prevent VT in:
A. Brugada syndrome, RVOT-VT, short QT syndrome and long QT syndrome
B. Brugada syndrome, RVOT-VT and long QT syndrome
C. *RVOT-VT and long QT syndrome
D. Short QT syndrome and long QT syndrome
E. Brugada syndrome and short QT syndrome
1193.Wenckebach phenomenon is defined as...
A. Progressive shortening of PR interval till a beat is dropped
B. *Progressive lengthening of PR interval till a beat is dropped
C. Irregular heart rate and PVC’s
D. Shortened QT intervals
E. Slurred QRS complex
1194.Giant a waves in JVP (“cannon” waves) are seen in
A. Sinus bradycardia
B. Atrial fibrillation
C. First-degree AV-block
D. *Complete heart block
E. Atrial ectopic
1195.All of the following findings are suggestive of LVH except:
A. (S in V1 + R in V5 or V6) > 35 mm
B. R in aVL > 11 mm
C. R in aVF > 20 mm
D. (R in I + S in III) > 25 mm
E. *R in aVR > 8 mm
1196.All of the following findings are suggestive of RVH except:
A. R in V1=7 mm (15 mm with RBBB)
B. (R in V1 + S in V5 or V6) > 10 mm
C. R < S in V6
D. R or R’ in V1
E. *S in V3 + R in aVL > 28 mm (20 mm for women)
1197.When present, each of the following heart sounds occurs shortly after S2 EXCEPT:
A. Opening snap
B. Third heart sound
C. *Ejection clic
D. Tumor plop
E. Pericardial knock
1198.Each of the following statements regarding splitting of the second heart sound is true EXCEPT:
A. Severe pulmonic valvular stenosis is associated with a softened P2
B. Delayed closure of the pulmonic valve with inspiration contributes to physiologic splitting of S2
C. Fixed splitting of S2 is the auscultatory hallmark of an ostium secundum atrial septal defect
D. Paradoxical splitting of S2 is expected in patients with a right ventricular electronically paced
rhythm
E. *Right bundle branch block is associated with paradoxical splitting of S2
1199.The timing of an "innocent" murmur is usually:
A. Early systolic
B. Presystolic
C. *Midsystolic
D. Holosystolic
E. Early diastolic
1200.Which of the following pairs of medical conditions and antihypertensive medications would be
incorrect to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1201.Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
1202.Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
1203.You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
1204.Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
1205.All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
1206.Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1207.Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
1208.Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
1209.Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
1210.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. *Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
1211.Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
1212.Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
1213.Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
1214.A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
1215.The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
1216.All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
1217.All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. *People of African descent commonly have a high renin type hypertension
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
1218.Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
1219.Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
1220.Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
1221.Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
1222.Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
1223.All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
1224.The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
1225.A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
1226.A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
1227.In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
1228.In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
1229.The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
1230.The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
1231.In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
1232.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
1233.All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
1234.Which of the following diagnostic studies is most likely to demonstrate the cause of the headaches
in a patient with aortic coarctation?
A. MRI of the head
B. MRI of the kidney
C. *MRI of the thorax
D. 24-h urinary 5-HIAA
E. 24-h urinary free cortisol
1235.A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the likely diagnosis?
A. Congenital adrenal hyperplasia
B. Fibromuscular dysplasia
C. Cushing’s syndrome
D. *Conn’s syndrome
E. Pheochromocytoma
1236.A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the best way to diagnose this disease ?
A. Renal vein renin levels
B. 24-h urine collection for metanephrines
C. MRI of the renal arteries
D. 24-h urine collection for cortisol
E. *Plasma aldosterone/renin ratio
1237.A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What is the best medication for the management of this patient’s
hypertension?
A. *Phentolamine
B. Fenoldopam
C. Esmolol
D. Nicardipine
E. Diazoxide
1238.A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What test would best determine the patient’s diagnosis?
A. Plasma catecholamines
B. 24-h urine collection for 5-HIAA
C. Abdominal CT scan
D. *24-h urine collection for metanephrines and vanilylmandelic acid
E. Adrenal vein sampling for renin levels
1239.What is the correct feature of the hypertensive urgency?
A. It is always a life-threatening situation
B. Patient must be hospitalized
C. *Patients can be managed as outpatients
D. Therapy should not be given orally
E. None of the above
1240.If there is suspicion of phaeochromocytoma, the first line drug is:
A. Sodium-nitroprusside
B. Nifedipine
C. *Phentolamine
D. Verapamil
E. Enalapril
1241.If you are in your office and a patient sees you with the following symptoms: long history of
hypertension, home BP usually 160/100 mmHg , suddenly developed severe headache, blurred vision,
weakness in the right arm, blood pressure: 200/110 mmHg. What will you do:
A. Give the patient 20 mg nifedipine orally, and check the BP in 15 min. If it is still >200/100 mmHg,
give another dose of nifedipine
B. Give the patient 20 mg nifedipine, and check the BP in 30 min. If it is 160/80 mmHg, send the
patient home and give another appointment in two weeks
C. Give the patient 10 mg amlodipine, send the patient home and give another appointment in two
days
D. Call the ambulance and send the patient to the nearest hospital
E. *Give the patient some pain-killer drug (e.g. acetaminophen), call the ambulance and send the
patient to the nearest hospital with stroke-unit
1242.A 28-year-old male with type 1 diabetes mellitus is seen in the clinic for routine follow-up. The
patient has hypertension. He is being maintained on an insulin pump and lisinopril 5 mg daily. He has
been on this dose of lisinopril for approximately 6 weeks. He has normal creatinine and no proteinuria.
BP is 140/90 mmHg. What do you recommend ?
A. Continue the current dose of lisinopril and return for follow-up in 3 months as the patient has
received his target BP of less than 140/90 mmHg
B. Ask a patient to return in 6 weeks; if his BP remains at this level, increase the dose of lisinopril
C. *Increase lisinopril to 10 mg daily to achieve a goal BP of less than 130/80 mmHg
D. Assure the patient that he is suffering from “white-coat hypertension” and plan no intervention
E. Switch the patient from lisinopril to losartan
1243.A 49-year-old female presents to you for an initial visit to establish health care. She has no past
medical history and denies a family history of diabetes mellitus, early cardiovascular disease, or renal
disease. Her BP on presentation is 185/110 mmHg. She denies headache or visual complaints. She has no
chest pain, shortness of breath, or change in urine color. Her physical examination is normal with the
exception of an S4 gallop heard at the 4th intercostal space just to the left of the sternum. An ECG is
significant for LVH and LAD. there are no signs of cardiac ischemia. Urinalysis shows no red blood cells
or proteinuria. What is your recommendation for therapy for this patient?
A. *Initiate therapy with hydrochlorothiazide in combination with a beta-blocker
B. Initiate therapy with hydrochlorothiazide alone
C. Initiate therapy with an ACE inhibitor alone
D. Advise the patient to go to the nearest emergency department for further treatment for a
hypertensive emergency
E. Advise the patient on lifestyle modifications and plan a return visit in 3 weeks
1244.What will you do if you are on duty in a hospital and a hypertensive patient, who has been treated
with long-acting ß-blocker, long-acting dihydropyridine calcium antagonist and long-acting a-1
adrenoceptor blocker, is admitted with the following symptoms: headache, dyspnea, ankle-swelling, BP
180/110 mmHg, pulmonary rales, LVH on ECG, echo: LVH, left ventricular diastolic dysfunction,
ejection fraction 46%.
A. Amlodipine orally
B. Nifedipine orally
C. Enalaprilate iv
D. *Enalaprilate iv + furosemide iv
E. Esmolol iv
1245.Which of the following blood pressure levels in pregnancy should be considered an emergency
requiring hospitalization?
A. ≥140/90 mmHg
B. ≥150/95 mmHg
C. ≥160/100 mmHg
D. *≥170/110 mmHg
E. A rise in SBP ≥25 mmHg or a rise in DPB ≥15 mmHg compared to pre-pregnancy values, or those
in the first trimester
1246.The following drug combinations are effective to treat hypertension EXCEPT
A. Diuretics + beta-blockers
B. Beta-blockers + dihydropiridine calcium channel blockers
C. Diuretics + ACE-inhibitors/ARB
D. ACE-inhibitors/ARB + calcium channel blockers
E. *Beta-blockers + ACE-inhibitors/ARB
1247.Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
1248.With respect to renovascular disease, all of the statements are true EXCEPT:
A. Worsening renal function with ACE-inhibitor therapy suggests bilateral renovascular disease
B. Atherosclerotic disease most commonly involves the proximal third of the main renal artery
C. The most common form of fibroplastic renovascular disease in adults involves the media
D. *The incidence of renovascular hypertension falls with increased age
E. Patients with severe, accelerated hypertension have the highest prevalence of renovascular disease
1249.A newly diagnosed diabetic patient presents with BP readings that are 155/95 or higher. All of the
following statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blockade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
1250.All of the following statements regarding the association of oral contraceptive pills and
hypertension are correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
1251.Each of the following statements regarding pheochromocytoma is true EXCEPT:
A. Approximately 15% of pheochromocytomas are extra-adrenal
B. Ten percent of pheochromocytomas are malignant
C. Ten percent of adrenal pheochromocytomas are bilateral
D. *Hypertension related to pheochromocytoma is nearly always episodic and only rarely persistent
E. Pheochromocytoma can be inherited
1252.All of the following are features of renovascular hypertension due to fibromuscular hyperplasia, as
opposed to atherosclerosis, EXCEPT:
A. Age <50 years
B. Female gender
C. *More likely to progress to complete renal artery occlusion
D. No family history of hypertension
E. Absence of carotid bruits
1253.Which of the following ACE-inhibitors are not prodrugs?
A. Captopril, lisinopril, ramipril
B. Lisinopril, enalapril, banazepril
C. *Captopril, lisinopril, enalaprilat
D. Moexipril, captopril, lisinopril
E. Perindopril, ramipril, enalapril
1254.Each of the following statements regarding hypertension is true EXCEPT:
A. The prevalence of hypertension rises progressively with age in both men and women
B. Systolic and diastolic hypertension are each associated with an increased crisk of coronary heart
disease
C. *The target blood pressure for hypertensive patients with cardiovascular disease or diabetes is
140/90 mmHg
D. Patients with prehypertension (SBP 120-139 mmHg or DBP 80-89 mmHg) benefit from lifestyle
modifications incl. weight reduction, regular exercise, and smoking cessation
E. Drug therapy of hypertension benefits patients greater than 80 years of age
1255.All of the following interventions have a BP-lowering effect EXCEPT:
A. A diet that reduces caloric intake by 1000 calories per day
B. Reduction of dietary sodium
C. *Daily magnesium supplements
D. Tobacco cessation
E. Reduction of ethanol consumption to less than 30 ml/day
1256.Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
1257.Each of the following statements regarding hypertension is true EXCEPT:
A. Increased LV muscle mass in hypertension is an independent risk factor of cardiac mortality
B. The risk of ventricular arrhythmias in hypertension is increased 2-fold in the presence of LV
hypertrophy
C. Low birth weight is associated with an increased incidence of hypertension later in life
D. *Chronic caffeine consumption is associated with an increased risk of hypertension
E. In hypertensive adolescents, essential hypertension is the most likely etiology
1258.The following statements regarding the association of oral contraceptive pills and hypertension are
correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
1259.Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
1260.Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
1261.Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
1262.All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. Constriction of cerebral arterioles with decreased vascular permeability*
D. Proteinuria
E. Microangiopathic hemolytic anemia
1263.Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1264.Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
1265.Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
1266.Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
1267.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. * Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
1268.Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
1269.Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
1270.Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
1271.A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
1272.The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
1273.All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
1274.All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. People of African descent commonly have a high renin type hypertension*
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
1275.Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
1276.Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
1277.Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
1278.Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
1279.Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
1280.All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
1281.At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
1282.The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
1283.In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
1284.In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
1285.The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
1286.The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
1287.In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
1288.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
1289.All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
1290.Which of the following is an effective adjunct to increase the rate of smoking cessation?
A. Aldosterone
B. *Bupropion
C. Sildenafil
D. Cimetidine
E. Buspirone
1291.With which of the following is sildenafil acetate (Viagra) most likely to interact adversely?
A. Fibrinolytic therapy
B. Primary PCI
C. *Nitrates
D. Aspirin
E. Beta-blockers
1292.Bupropion hydrochloride (Zyban) is contraindicated in patients with a history of which of the
following?
A. *Seizures
B. Insulin-dependent diabetes mellitus
C. Severe chronic obstructive pulmonary disease (with reversible component)
D. Longer than 40-year history of tobacco use
E. Recent MI
1293.In which of the following has the high-sensitivity C-reactive protein (CRP) been shown to be
predictive of risk?
A. Acute MI
B. Acute coronary syndromes
C. Chronic stable angina
D. Peripheral vascular disease
E. *All of the above
1294.Which of the following has been shown to decrease the level of the high-sensitivity CRP?
A. Unopposed estrogen
B. Amlodipine besylate (Norvasc)
C. *Simvastatin
D. All of the above
E. None of the above
1295.All of the following statements regarding myocardial stunning are true EXCEPT:
A. *Stunning is a state of depressed myocardial function due to chronic hypoperfusion
B. Stunning can be global or regional
C. Stunning can follow cardiac surgery with cardiopulmonary bypass
D. Oxygen-free radicals and excess intracellular calcium likely contribute to stunning
E. Stunning affects both systolic and diastolic function
1296.What is the most common coexisting congenital anomaly in patients with coarctation of the aorta?
A. Cleft mitral valve
B. *Bicuspid aortic valve
C. Ebstein's anomaly
D. VSD
E. PDA
1297.All of the following are characteristic findings of ostium primum atrial septal defect (ASD)
EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Right axis deviation
D. Systolic ejection murmur
E. Prominent pulmonary vascular markings on CXR
1298.Choose the adult congenital disorder corresponding to the following physical examination fingings:
RV lift with a loud systolic ejection murmur along the left sternal border, with a single S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
1299.Choose the adult congenital disorder corresponding to the following physical examination fingings:
loud S1, holosystolic murmur in left sternal border, systolic ejection click, and hepatomegaly
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
1300.Choose the adult congenital disorder corresponding to the following physical examination fingings:
weak or delayed femoral pulses, harsh systolic murmur in the back, and a systolic ejection click in the
aortic area
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1301.Choose the adult congenital disorder corresponding to the following physical examination fingings:
cyanosis, digital clubbing, loud P2, and a variable Graham-Steel murmur
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1302.Choose the adult congenital disorder corresponding to the following physical examination fingings:
wide pulse pressure, prominent LV impulse, and a continuous machinery murmur enveloping S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *Patent ductus arteriosus
D. Ebstein's anomaly
E. Tetralogy of Fallot
1303.Bacterial endocarditis prophylaxis is indicated in all adults who have the following congenital heart
disease EXCEPT:
A. VSD
B. Coarctation of the aorta
C. *Secundum ASD
D. Hypertrophic obstructive cardiomyopathy
E. PDA
1304.Besides pulmonary valve stenosis, which of the following is the most common associated cardiac
defect present in patients with PA stenosis?
A. *VSD
B. ASD
C. Coarctation of the aorta
D. PDA
E. Bicuspid aortic valve
1305.All of the following statements regarding patent ductus arteriosus (PDA) are true EXCEPT:
A. *The majority of cases close spontaneously after infancy
B. There is a higher incidence in mothers who acquired rubella during pregnancy
C. A decrease in the duration and intensity of the murmur has a poor prognostic implication
D. Left ventricular hypertrophy precedes RV hypertrophy
E. If it is uncorrected, approximately one third of patients die by the age of 40 years
1306.Ostium primum ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. *Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1307.Noonan's syndrome is commonly associated with...
A. Supravalvular aortic stenosis
B. *Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1308.Coronary sinus ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. *Persistent left superior vena cava
1309.Williams syndrome is commonly associated with...
A. Supravalvular aortic stenosis
B. *Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1310.Sinus venosus ASD is commonly associated with...
A. Supravalvular aortic stenosis
B. Supravalvular pulmonic stenosis
C. Cleft mitral valve
D. *Anomalous pulmonary venous drainage
E. Persistent left superior vena cava
1311.All of the following physical examination findings are usually associated with ostium secundum
ASD EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Lateral and inferior displacement of the apex beat
D. Soft systolic ejection murmur in the second left intercostal space
E. Normal S1
1312.Which of the following is an absolute contraindication to pregnancy?
A. Surgically corrected transposition of great arteries (TGA)
B. Congenitally corrected TGA
C. Ebstein's anomaly
D. *Eisenmenger's syndrome
E. Status post Fontan operation
1313.The lesions that constitute tetralogy of Fallot include all of the following EXCEPT
A. A ventricular septal defect
B. An overriding aorta
C. *An atrial septal defect
D. Right ventricular outflow obstruction
E. Right ventricular hypertrophy
1314.Match the chest radiography findings (prominent central PAs and peripheral PA prunning) with the
corresponding congenital disorder
A. *Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1315.Match the chest radiography findings (marked cardiomegaly, severe right atrial enlargement, and
normal lung fields) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. *Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1316.Match the chest radiography findings (RV enlargement, and a "boot-shaped" heart) with the
corresponding congenital disorder
A. Eisenmenger's syndrome
B. Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. *Tetralogy of Fallot
E. Coarctation of the aorta
1317.Match the chest radiography findings (pulmonary plethora, prominent ascending aorta, proximal
PA dilatation) with the corresponding congenital disorder
A. Eisenmenger's syndrome
B. *Patent ductus arteriosus (PDA)
C. Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1318.All of the following are indications for surgical closure of an ASD EXCEPT:
A. Significant symptoms in a 65-year-old
B. RV dysfunction
C. *Pulmonary vascular resistance >15 Wood units that does not diminish with vasodilators
D. An asymptomatic 20-year-old with a Qp/Qs of 1,7 with no pulmonary hypertension
E. RV enlargement
1319.The following cardiovascular malformations are all associated with congenital rubella EXCEPT:
A. PDA
B. PA stenosis
C. *Ebstein's anomaly
D. Tetralogy of Fallot
E. Coarctation of the aorta
1320.Which of the following syndromes is associated with pumonary arterio-venous fistula?
A. Williams syndrome
B. *Weber-Osler-Rendu syndrome
C. Bland-Garland-White syndrome
D. Kartagener's syndrome
E. Crouzon's syndrome
1321.Congenital MR is commonly encountered in all of the following conditions EXCEPT:
A. *Cor triatriatum
B. Ostium primum ASD
C. Coarctation of the aorta
D. Congenitally corrected TGA
E. Subaortic stenosis
1322.In which of the following cases is surgical correction recommended?
A. Asymptomatic small VSD to decrease risk of endocarditis
B. PDA with severe pulmonary hypertension
C. *Asymptomatic subaortic stenosis with severe aortic valve insufficiency
D. Coarctation of the aorta with a transcoarctation gradient of 20 mmHg
E. Small ASD to prevent paradoxical embolization
1323.Which congenital disorder corresponds with the following chest radiography findings: prominent
central PAs (possible calcifications) and peripheral PA prunning?
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1324.Which congenital disorder corresponds with the following chest radiography findings: right aortic
arch, RV enlargement, and a "boot-shaped" heart?
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
1325.Which congenital disorder corresponds with the following chest radiography findings: marked
cardiomegaly, severe right atrial enlargement, and normal lung fields
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
1326.Which congenital disorder corresponds with the following chest radiography findings: posterior rib
notching and a "reverse E" or "3" sign
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1327.Which congenital disorder corresponds with the following chest radiography findings: pulmonary
plethora, prominent ascending aorta, proximal PA dilatation, and opacity at the confluence of the aortic
knob and descending aorta
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1328.Which of the following statements regarding Ebstein's anomaly is NOT correct?
A. An ASD or PFO is present in up to 80% of patients
B. The cardinal feature is an apically displaced tricuspid valve resulting in atrialization of ventricular
tissue
C. WPW syndrome is common in these patients and multiple tracts can exist
D. *A bicuspid aortic valve is commonly present
E. A "sail sound" is a common finding on physical examination
1329.Which of the following syndromes and cardiac anomalies are INCORRECTLY matched?
A. Trisomy 21 – atrioventricular canal defects
B. Noonan syndrome – pulmonic stenosis
C. Holt-Oram syndrome – atrial septal defects
D. Marfan syndrome – mitral valve prolapse
E. *Williams syndrome – ventricular septal defects
1330.All of the following statements regarding the effects of maneuvers on the auscultation of cardiac
murmurs are true EXCEPT:
A. In patent ductus arteriosus (PDA), the diastolic phase of the murmur is intensified by isometric
handgrip
B. *The murmur of hypertrophic obstructive cardiomyopathy becomes softer with standing or during a
Valsalva strain maneuver
C. The murmur of a ventricular septal defect (VSD) increases with isometric handgrip
D. Sudden squatting or isometric handgrip increases the diastolic murmur of aortic regurgitation
E. The mid-diastolic and presystolic murmurs of mitral stenosis become louder with exercise
1331.Radiotherapy for malignant disease may affect the heart in all of the following ways EXCEPT
A. Pericarditis
B. Coronary artery disease
C. Valvular stenosis
D. Conduction abnormalities
E. *Asymmetrical septal hypertrophy
1332.Sudden cardiac death due to ventricular tachyarrhythmias is an established complication of each of
the following EXCEPT:
A. Sarcoidosis
B. Giant cell myocarditis
C. Chagas disease
D. Idiopathic dilated cardiomyopathy
E. *Hyperthyroidism
1333.Characteristics of arrhythmogenic RV dysplasia include all of the following EXCEPT
A. Fatty infiltration of the right ventricle
B. *Fatty infiltration of the right atrium
C. Monomorphic ventricular tachycardia
D. Abnormal signal-averaged ECG
E. Possible detection by cardiac MRI
1334.All of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
1335.Each of the statements about the evolution of the ECG in acute pericarditis is correct EXCEPT:
A. Four sequential stages of abnormalities of the ST segments and T waves are typical
B. *Initial ST segment elevation is usually most prominent in ECG lead aVR
C. The ratio of the height of ST segment elevation to the height of the T wave in acute pericarditis is
typically >0.25 in lead V6
D. In acute pericarditis, the ST segment usually returns to baseline before the appearance of T wave
inversion
E. T wave inversion may persist for months after the acute presentation
1336.Which of the following statements regarding cardiac involvement in Lyme disease is CORRECT?
A. Cardiac manifestations of Lyme disease typically occur within several days of the development of
erythema chronicum migricans
B. *Ten percent of patients with Lyme disease develop cardiac manifestations
C. Supraventricular and ventricular tachyarrhythmias are the most common cardiac manifestations of
Lyme disease
D. Cardiomegaly and congestive heart failure are common among patients who develop Lyme carditis
E. Antibiotic therapy has been proven to shorten the course of active Lyme carditis
1337.Each of the following statements regarding the infectious etiologies of pericarditis is correct
EXCEPT:
A. Enteroviruses are among the most common causes of viral pericarditis
B. The most common organisms that cause bacterial pericarditis are streptococci and staphylococci
C. The prognosis of patients with bacterial pericarditis is poor
D. *Tuberculosis is the leading cause of constrictive pericarditis in Western nations
E. Antifungal therapy is generally not necessary in pericarditis caused by histolasmosis
1338.Each of the following statements regarding Chagas disease is correct EXCEPT
A. The level of parasitemia does not correspond to the severity of chronic Chagas disease
B. The disease is transmitted to humans by the reduviid bug (commonly called the kissing bug)
C. *The most common ECG abnormality in chronic Chagas disease is left bundle branch block
D. The classic echocardiographic findings are those of a dilated cardiomyopathy with an apical
aneurysm
E. All of the above statements are correct
1339.Which of the following disorders is not associated with ventricular tachycardia as a cause of
syncope?
A. Hypertrophic obstructive cardiomyopathy
B. Prior myocardial infarction
C. *Atrial myxoma
D. Aortic valvular stenosis
E. Congenital long QT syndrome
1340.Each of the following statements regarding the ECG in acute pericarditis is true EXCEPT:
A. The majority of patients demonstrate ECG abnormalities
B. Global ST elevation is seen in early pericarditis
C. Sinus tachycardia is a common finding
D. PR depression is common in the majority of patients
E. *T wave inversions develop before ST elevations return to baseline
1341.Each of the following statements regarding endomyocardial fibrosis (EMF) is correct EXCEPT:
A. This condition is characteristically found in tropical and subtropical Africa
B. It is predominantly a disease of children and young adults
C. *Involvement of the mitral apparatus typically results in mitral stenosis
D. EMF involves the left ventricle in 90% of affected patients
E. Echocardiographic features include increased endocardial echoreflectivity, fibrotic obliteration of
apex, atrial enlargement, and pericardial effusion
1342.All of the following statements with regard to primary endocardial fibroelastosis (EFE) are correct
EXCEPT:
A. The condition is often familial
B. The mitral and aortic valve leaflets are usually thickened and distorted
C. *The murmur of mitral stenosis is the most common auscultatory finding
D. Symptoms of primary EFE usually develop between 2 and 12 months of age
E. Echocardiographic features include a reduced ejection fraction and increased left atrial and left
ventricular dimensions
1343.Which of the following therapies improves survival in patients with cor pulmonare secondary to
COPD?
A. Digoxin
B. *Oxygen
C. Beta-adrenergic agonists
D. Theophylline
E. Hydralazine
1344.What is NOT a cause of chronic cor pulmonale?
A. COPD
B. Recurrent pulmonary emboli
C. *Mitral stenosis
D. Kyphoscoliosis
E. Obstructive sleep apnea
1345.Which of the following conditions is associated with increased left ventricular preload?
A. Sepsis
B. Right ventricular infarction
C. *Mitral regurgitation
D. Dehydration
E. Pulmonary embolism
1346.Each of the following conditions is associated with the development of pulmponary edema
EXCEPT:
A. Increased pulmonary venous pressure
B. High altitude
C. *Increased plasma oncotic pressure
D. Eclampsia
E. Heroin overdose
1347.The statements about the diagnosis of PE include all of the following EXCEPT:
A. Arterial blood gas measurement is often unhelpful in the diagnosis of acute PE
B. The most common ECG finding in patients with PE is sinus tachycardia
C. Pulmonary infarction due to PE can be visualized on a standard chest radiograph
D. *Reduced intensity of the pulmonic component of the second heart sound is typical in patients with
large PE
E. Fibrin-degradation products (e.g., D-dimer) are commonly elevated in patients with PE
1348.Heart failure is:
A. Decreasing in incidence and prevalence due to recent advances in the treatment of cardiovascular
disease
B. *One of the diagnoses with the highest readmission rate
C. A common condition across all ages
D. Can be diagnosed from a clinical response to treatment
E. All of the above statements are correct
1349.According to the ESC guidelines, the following patients have heart failure:
A. An obese, dyspnoeic lady with swollen anckles but a normal echocardiogram
B. An asymptomatic man with a previous MI and area of hypokinesis on his echocardiogram
C. *A hypertensive man with LVH, fast atrial fibrillation and dyspnea
D. An elderly man with a few basal crepitations but a normal echocardiogram
E. All of the above
1350.Which of the following sometimes occur when heart failure is absent?
A. Gallop rhythm
B. Anckle oedema
C. A past history of a MI
D. *B and C
E. A, B, and C
1351.B-type natriuretic secretion is regulated by:
A. Fluid accumulation in the lungs
B. *Pressure and volume of the left ventricle
C. Oedema in the anckles
D. Auricular end diastolic pressure
E. All of the above
1352.Which of the following statements are true ?
A. A normal resting ECG is rare in angina pectoris
B. A normal resting ECG is common in heart failure
C. *Cardiomegaly plus pleural effusions make heart failure very likely
D. Atrial fibrillation commonly does not cause dyspnoea in patients with LVH and diastolic
dysfunction
E. All of the above
1353.The value of BNP in the diagnosis of heart failure in the emergency room in patients with acute
dyspnoea:
A. *Is supported by a BNP concentration >500 pg/ml
B. Is excluded by a NT-proBNP concentration <1000 pg/ml
C. Is restricted to patients without a previous history of heart failure
D. Has not been evaluated in patients with renal dysfunction
E. All of the above statements are true
1354.Which symptoms/signs only occur when the HF is relatively advanced – that is, they are commonly
absent in mild heart failure
A. Cardiomegaly on chest X-ray
B. Orthopnea
C. Exertional dyspnea
D. *A abd B
E. B and C
1355.All patients with heart failure should be advised to:
A. Refrain from smoking
B. Restrict sodium intake
C. Avoid a flu shot
D. *A and B
E. All of the above
1356.Exercise training in chronic heart failure
A. *Has been shown to increase peak oxygen consumption by 15-20% in randomized controlled trials
B. Has been shown to increase LV ejection fraction by 15-20% in randomized controlled trials
C. Is not recommended in heart failure
D. Has never been shown to reduce mortality and morbidity
E. Non of above
1357.Drugs that should be avoided in heart failure patients are:
A. Non-steroidal anti-inflammatory drugs (NSAIDS)
B. Corticosteroids
C. Beta-blockers
D. *A and B
E. All of the above
1358.The followings improve the survival figure in chronic congestive heart failure as shown by many
studies...EXCEPT
A. Bisoprolol
B. Metoprolol succinate
C. *Atenolol
D. Spironolactone
E. Carvedilol
1359.The following drugs have significantly improved survival in HF patients
A. *ACE inhibitors
B. Nitrates
C. Digoxin
D. Diuretics
E. All of the above
1360.Which of the statements about beta-blocker treatment in HF is true?
A. Randomised clinical trials show that b blockers are beneficial in patients with heart failure and
preserved left ventricular function
B. Elderly patients are the most frequently studied population in blocker trials
C. * Blockers exert a favourable effect in heart failure due to ischaemic and non-ischaemic aetiology
D. Patients with diabetes should always be excluded from blocker treatment
E. There is clear evidence that end stage heart failure patients should be treated with blockers
1361.Which of the statements about beta-blocker treatment in HF is true?
A. *Beta-blockers must be started at very low dosages
B. Treatment should be started when patients are unstable in order to stabilize them
C. When patients are treated with ACE inhibitors, blockers are contraindicated
D. Treatment should always be started during hospital stay
E. The most frequent adverse reaction to a blocker is cough
1362.Which of the statements about antiarrhythmic therapy treatment in HF is NOT true?
A. Amiodarone is an antiarrhythmic drug whose use can improve symptoms of patients with heart
failure without affecting myocardial function and survival
B. *Class I antiarrhythmic agents reduce mortality of patients with heart failure
C. In patients with documented life threatening ventricular arrhythmias, implantable cardioverterdefribrillators (ICDs) can reduce sudden death
D. Sudden death is one of the most frequent causes of death in patients with heart failure
E. The reduction of the number of premature ectopic beats with antiarrhythmic drugs can prevent
sudden mortality of heart failure patients
1363.A prophylactic ICD is useful for reducing total mortality in patients:
A. With previous myocardial infarction and low ejection fraction
B. With dilated cardiomyopathy and low ejection fraction
C. With previous myocardial infarction and low ejection fraction and broad QRS
D. A and C
E. *All of the above
1364.Biventricular pacing in severe heart failure and broad QRS:
A. Improves NYHA class
B. Improves exercise tolerance
C. Reduces hospitalisation for heart failure
D. Reduces heart rate
E. *All of the above
1365.Which of the following treatments most consistently improves EF in patients who have systolic
heart failure?
A. Diuretics
B. Beta-blockers
C. *ACE-inhibitors
D. Vasodilators
E. All of the above
1366.BNP has which of the following properties?
A. Urine volume increases
B. Sodium excretion is enhanced
C. More BNP is secreted
D. A decrease in plasma aldosterone concentration occurs
E. *All of the above occur
1367.All of the following are indications for heart transplantation EXCEPT
A. Dilated cardiomyopathy
B. Diabetes mellitus
C. Hypertrophic cardiomyopathy
D. Age 60 to 70 years
E. *Amyloid heart disease
1368.When used chronically, all of the following drugs increase mortality EXCEPT
A. Milrinone
B. Dobutamine
C. Vesnarinone
D. Xamoterol
E. *Amlodipine
1369.Primary causes of diatolic heart failure include all of the following EXCEPT
A. Hypertrophic cardiomyopathy
B. *Dilated cardiomyopathy
C. Hypertension
D. Ischemic cardiomyopathy
E. Infiltrative cardiomyopathy
1370.Match the description with the associated form of therapy for pulmonary embolism: may be
effective in PE even 1 to 2 weeks after the onset of symptoms
A. Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. *Both
D. Neither
E. Not applicable
1371.Match the description with the associated form of therapy for pulmonary embolism: dissolution of
recently formed thrombus is a major action
A. Unfractionated heparin or low molecular weight heparin
B. *Fibrinolytic therapy
C. Both
D. Neither
E. Not applicable
1372.Match the description with the associated form of therapy for pulmonary embolism: in general,
should be administered along with an antiplatelet agent
A. Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. Both
D. *Neither
E. Not applicable
1373.Match the description with the associated form of therapy for pulmonary embolism: may cause
aldosterone depression
A. *Unfractionated heparin or low molecular weight heparin
B. Fibrinolytic therapy
C. Both
D. Neither
E. Not applicable
1374.Match the ECG finding that is most closely associated with chronic Chagas disease:
A. Low QRS voltage
B. AV nodal block
C. *Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
1375.Match the ECG finding that is most closely associated with sarcoidosis:
A. Low QRS voltage
B. *AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
1376.Match the ECG finding that is most closely associated with apical hypertrophic cardiomyopathy
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. *Deeply inverted precordial T waves
1377.Match the ECG finding that is most closely associated with cardiac amyloidosis
A. *Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment elevation
E. Deeply inverted precordial T waves
1378.Heart may be affected by radiotherapy in all of the following ways EXCEPT
A. Pericarditis
B. Coronary artery disease
C. Valvular stenosis
D. Conduction abnormalities
E. *Asymmetrical septal hypertrophy
1379.SCD (sudden cardiac death) due to ventricular tachyarrhythmias is an established complication of
each of the following EXCEPT:
A. Sarcoidosis
B. Giant cell myocarditis
C. Chagas disease
D. Idiopathic dilated cardiomyopathy
E. *Hyperthyroidism
1380.Arrhythmogenic RV dysplasia is characterized by all of the following EXCEPT
A. Fatty infiltration of the right ventricle
B. *Fatty infiltration of the right atrium
C. Monomorphic ventricular tachycardia
D. Abnormal signal-averaged ECG
E. Possible detection by cardiac MRI
1381.Each of the following may cause elevation of serum troponin EXCEPT:
A. Congestive heart failure
B. Myocarditis
C. Myocardial infarction
D. *Pneumonia
E. Pulmonary embolism
1382.All of the following statements regarding the infectious etiologies of pericarditis are correct
EXCEPT:
A. Enteroviruses are among the most common causes of viral pericarditis
B. The most common organisms that cause bacterial pericarditis are streptococci and staphylococci
C. The prognosis of patients with bacterial pericarditis is poor
D. *Tuberculosis is the leading cause of constrictive pericarditis in Western nations
E. Antifungal therapy is generally not necessary in pericarditis caused by histolasmosis
1383.All of the following statements regarding Chagas disease are correct EXCEPT
A. The level of parasitemia does not correspond to the severity of chronic Chagas disease
B. The disease is transmitted to humans by the reduviid bug (commonly called the kissing bug)
C. *The most common ECG abnormality in chronic Chagas disease is left bundle branch block
D. The classic echocardiographic findings are those of a dilated cardiomyopathy with an apical
aneurysm
E. All of the above statements are correct
1384.Of the following disorders, choose one which is not associated with ventricular tachycardia as a
cause of syncope?
A. Hypertrophic obstructive cardiomyopathy
B. Prior myocardial infarction
C. *Atrial myxoma
D. Aortic valvular stenosis
E. Congenital long QT syndrome
1385.All of the following statements regarding the ECG in acute pericarditis is true EXCEPT:
A. The majority of patients demonstrate ECG abnormalities
B. Global ST elevation is seen in early pericarditis
C. Sinus tachycardia is a common finding
D. PR depression is common in the majority of patients
E. *T wave inversions develop before ST elevations return to baseline
1386.All the following features favor ventricular tachycardia as the cause of broad-complex tachycardia,
EXCEPT:
A. QRS duration with right bundle branch block morphology (RBBB) is greater than 140 ms, and
greater than 160 ms with left LBBB morphology
B. LAD with RBBB morphology, extreme LAD (northwest axis) with LBBB morphology
C. AV dissociation
D. *Response to carotid sinus massage
E. Concordance of the QRS pattern in all precordial leads (i.e., all positive or all negative deflections)
1387.Which of the following will most likely respond to verapamil?
A. RVOT tachycardia
B. *Idiopathic LV tachycardia
C. Bundle branch re-entry tachycardia
D. ARVD ventricular tachycardia
E. All of the above
1388.The most common type of arrhythmia in WPW syndrome is....
A. Ventricular tachycardia
B. Ventricular fibrillation
C. Ventricular premature complexes
D. Atrial ectopics
E. *AV re-entry tachycardia
1389.Use of echocardiogram in the assessment of AF:
A. It is not necessary to perform a TTE in patients with AF
B. TEE is always needed to allow better assessment of the MV and LA
C. *TTE should be performed at baseline to diagnose associated structural/functional heart disease
D. TTE is necessary to determine stroke risk stratification for thromboprophylaxis in all patients
E. When TTE is technically difficult, MRI is needed to exclude cardiac abnormalities
1390.Which is the preferred initial treatment strategy for rate control in AF patients?
A. Digoxin
B. *Beta-blockers or rate limiting CCB
C. Combination therapy of beta-blockers and rate-limiting CCB’s
D. Amiodarone
E. Combination therapy of digoxin and beta-blockers
1391.Which option is better in regard to cardioversion?
A. *Synchronised DC shock to restore sinus rhythm
B. Amiodarone in all patients to restore sinus rhythm
C. Flecainide in patients with IHD to maintain sinus rhythm
D. Digoxin to restore sinus rhythm
E. Propaphenone to restore sinus rhythm in HCMP patients
1392.Regarding antithrombotic treatment in AF:
A. Patients with asymptomatic AF have less risk of embolism than symptomatic patients
B. Patients with atrial flutter do not need antithrombotic treatment due to the low risk of embolism of
this arrhythmia
C. *Warfarin is the best option in patients with high risk of thromboembolism
D. Aspirin has a similar effect in stroke reduction to placebo
E. Paroxysmal AF has the lowest risk of embolism
1393.Sudden cardiac death in patients >35 years old is most commonly associated with:
A. Hypertrophic cardiomyopathy
B. *Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
1394.Congenital long QT syndrome can lead to
A. Complete heart block
B. *Polymorphic ventricular tachycardia
C. Acute myocardial infarction
D. Recurrent supraventricular tachycardia
E. All of the above
1395.Bundle branch re-entry ventricular tachycardia is most commonly associated with:
A. Enhanced automaticity in the right bundle
B. Enhanced automaticity in the left bundle
C. Supranormal conduction in the His bundle
D. *Abnormally slow conduction in the His bundle
E. All of the above
1396.All of the following are ECG manifestations of Wolff-Parkinson-White syndrome EXCEPT
A. *Narrow QRS
B. Initial slurred QRS upstroke
C. Short PQ interval
D. Normal QT interval
E. All of the above
1397.The initial manifestations of WPW syndrome may include which of the following?
A. Atrial fibrillation
B. AV re-entry tachycardia
C. Ventricular fibrillation
D. Wide-QRS tachycardia
E. *All of the above
1398.The presence of an r prime in V1 during narrow-QRS tachycardia is suggestive of...
A. AV re-entry
B. *AV node re-entry
C. Rate-dependent BBB
D. Atrial tachycardia
E. Atrial fibrillation
1399.Ventricular ectopic beats (VEBs) occurring in apparently normal hearts are:
A. Associated with a bad prognosis
B. Never frequent or complex
C. Less frequent with increasing age
D. *May be associated with symptoms of “missed beats”
E. Always symptomatic
1400.In patients with ventricular ectopic beats:
A. Caffeine restriction always reduces symptoms
B. *High caffeine intake should always be discouraged in symptomatic patients
C. There is good evidence that reducing caffeine intake reduces ectopics
D. Hypertension has no association with frequency of ectopic beats
E. LVH is not associated with increased frequency of ectopics
1401.Regarding ventricular ectopics and exercise:
A. *Ectopics are usually benign if they are supressed on exercise
B. Exercise-induced VEBs are not associated with adverse prognosis
C. RVOT ectopics are usually supressed on exercise
D. Ectopics induced on recovery after exercise are benign
E. All of the above
1402.An idiopathic left ventricular tachycardia (VT) shows the following...
A. Typical LBBB morphology
B. *LAD and RBBB morphology
C. Associated with a high risk of sudden cardiac death and almost always requires ICD therapy
D. Never responds to verapamil
E. All of the above
1403.Beta blockers are accepted treatment to prevent VT in:
A. Brugada syndrome, RVOT-VT, short QT syndrome and long QT syndrome
B. Brugada syndrome, RVOT-VT and long QT syndrome
C. *RVOT-VT and long QT syndrome
D. Short QT syndrome and long QT syndrome
E. Brugada syndrome and short QT syndrome
1404.Wenckebach phenomenon is defined as...
A. Progressive shortening of PR interval till a beat is dropped
B. *Progressive lengthening of PR interval till a beat is dropped
C. Irregular heart rate and PVC’s
D. Shortened QT intervals
E. Slurred QRS complex
1405.Giant a waves in JVP (“cannon” waves) are seen in
A. Sinus bradycardia
B. Atrial fibrillation
C. First-degree AV-block
D. *Complete heart block
E. Atrial ectopic
1406.All of the following findings are suggestive of LVH except:
A. (S in V1 + R in V5 or V6) > 35 mm
B. R in aVL > 11 mm
C. R in aVF > 20 mm
D. (R in I + S in III) > 25 mm
E. *R in aVR > 8 mm
1407.All of the following findings are suggestive of RVH except:
A. R in V1=7 mm (15 mm with RBBB)
B. (R in V1 + S in V5 or V6) > 10 mm
C. R < S in V6
D. R or R’ in V1
E. *S in V3 + R in aVL > 28 mm (20 mm for women)
1408.When present, each of the following heart sounds occurs shortly after S2 EXCEPT:
A. Opening snap
B. Third heart sound
C. *Ejection clic
D. Tumor plop
E. Pericardial knock
1409.Each of the following statements regarding splitting of the second heart sound is true EXCEPT:
A. Severe pulmonic valvular stenosis is associated with a softened P2
B. Delayed closure of the pulmonic valve with inspiration contributes to physiologic splitting of S2
C. Fixed splitting of S2 is the auscultatory hallmark of an ostium secundum atrial septal defect
D. Paradoxical splitting of S2 is expected in patients with a right ventricular electronically paced
rhythm
E. *Right bundle branch block is associated with paradoxical splitting of S2
1410.The timing of an "innocent" murmur is usually:
A. Early systolic
B. Presystolic
C. *Midsystolic
D. Holosystolic
E. Early diastolic
1411.Which of the following pairs of medical conditions and antihypertensive medications would be
incorrect to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1412.Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
1413.Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
1414.You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
1415.Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
1416.All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
1417.Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1418.Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
1419.Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
1420.Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
1421.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. * Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
1422.Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
1423.Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
1424.Fundus picture of stage 2 of Keith-Wegener classification includes
A. *Copper wire AV nipping and focal spasm
B. Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
1425.A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
1426.The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
1427.All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
1428.All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. *People of African descent commonly have a high renin type hypertension
E. An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
1429.Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
1430.Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
1431.Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
1432.Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
1433.Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
1434.All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
1435.The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
1436.A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
1437.A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
1438.In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
1439.In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
1440.The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
1441.The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
1442.In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
1443.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
1444.All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
1445.In a patient with suspected aortic coarctation which of the following diagnostic studies is most
likely to demonstrate the cause of the headaches?
A. MRI of the head
B. MRI of the kidney
C. *MRI of the thorax
D. 24-h urinary 5-HIAA
E. 24-h urinary free cortisol
1446.A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the likely diagnosis?
A. Congenital adrenal hyperplasia
B. Fibromuscular dysplasia
C. Cushing’s syndrome
D. *Conn’s syndrome
E. Pheochromocytoma
1447.A 27-year-old female has hypertension that is difficult to control. She was diagnosed at age 25.
Since that time she has been on increasing amounts of medication. Her current regimen consists of
labetalol 1000 mg bid, lisinopril 40 mg qd, clonidine 0.1 mg bid, and amlodipine 5 mg qd. On physical
examination she appears to be without distress. Her BP is 170/100, and HR is 84 bpm. Cardiac exam is
unremarkable, without rubs, gallops, or murmurs. She has good peripheral pulses and has no edema.
Laboratory studies reveal a potassium of 2.8 mEq/dL and a serum bicarbonate of 32 mEq/dL. Fasting
blood glucose 114 mg/dL. What is the best way to diagnose this disease ?
A. Renal vein renin levels
B. 24-h urine collection for metanephrines
C. MRI of the renal arteries
D. 24-h urine collection for cortisol
E. *Plasma aldosterone/renin ratio
1448.A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What is the best medication for the management of this patient’s
hypertension?
A. *Phentolamine
B. Fenoldopam
C. Esmolol
D. Nicardipine
E. Diazoxide
1449.A 20-year-old female is seen in the ED with symptoms of periodic headaches, sweating, and nausea
with vomiting. She also complains of feeling light-headed with standing. Her BP on presentation is
230/135, with a HR of 92. On standing, the patient has BP of 205/100, with a HR of 136. On
ophthalmologic examination the patient has mild blurring of the optic discs without hemorrhage. The
examination is otherwise normal. What test would best determine the patient’s diagnosis?
A. Plasma catecholamines
B. 24-h urine collection for 5-HIAA
C. Abdominal CT scan
D. *24-h urine collection for metanephrines and vanilylmandelic acid
E. Adrenal vein sampling for renin levels
1450.What is the correct feature of the hypertensive urgency?
A. It is always a life-threatening situation
B. Patient must be hospitalized
C. *Patients can be managed as outpatients
D. Therapy should not be given orally
E. None of the above
1451.If there is suspicion of phaeochromocytoma, the first line drug is:
A. Sodium-nitroprusside
B. Nifedipine
C. *Phentolamine
D. Verapamil
E. Enalapril
1452.If you are in your office and a patient sees you with the following symptoms: long history of
hypertension, home BP usually 160/100 mmHg, suddenly developed severe headache, blurred vision,
weakness in the right arm, blood pressure: 200/110 mmHg. What will you do:
A. Give the patient 20 mg nifedipine orally, and check the BP in 15 min. If it is still >200/100 mmHg,
give another dose of nifedipine
B. Give the patient 20 mg nifedipine, and check the BP in 30 min. If it is 160/80 mmHg, send the
patient home and give another appointment in two weeks
C. Give the patient 10 mg amlodipine, send the patient home and give another appointment in two
days
D. Call the ambulance and send the patient to the nearest hospital
E. *Give the patient some pain-killer drug (e.g. acetaminophen), call the ambulance and send the
patient to the nearest hospital with stroke-unit
1453.A 28-year-old male with type 1 diabetes mellitus is seen in the clinic for routine follow-up. The
patient has hypertension. He is being maintained on an insulin pump and lisinopril 5 mg daily. He has
been on this dose of lisinopril for approximately 6 weeks. He has normal creatinine and no proteinuria.
BP is 140/90 mmHg. What do you recommend ?
A. Continue the current dose of lisinopril and return for follow-up in 3 months as the patient has
received his target BP of less than 140/90 mmHg
B. Ask a patient to return in 6 weeks; if his BP remains at this level, increase the dose of lisinopril
C. *Increase lisinopril to 10 mg daily to achieve a goal BP of less than 130/80 mmHg
D. Assure the patient that he is suffering from “white-coat hypertension” and plan no intervention
E. Switch the patient from lisinopril to losartan
1454.A 49-year-old female presents to you for an initial visit to establish health care. She has no past
medical history and denies a family history of diabetes mellitus, early cardiovascular disease, or renal
disease. Her BP on presentation is 185/110 mmHg. She denies headache or visual complaints. She has no
chest pain, shortness of breath, or change in urine color. Her physical examination is normal with the
exception of an S4 gallop heard at the 4th intercostal space just to the left of the sternum. An ECG is
significant for LVH and LAD. there are no signs of cardiac ischemia. Urinalysis shows no red blood cells
or proteinuria. What is your recommendation for therapy for this patient?
A. *Initiate therapy with hydrochlorothiazide in combination with a beta-blocker
B. Initiate therapy with hydrochlorothiazide alone
C. Initiate therapy with an ACE inhibitor alone
D. Advise the patient to go to the nearest emergency department for further treatment for a
hypertensive emergency
E. Advise the patient on lifestyle modifications and plan a return visit in 3 weeks
1455.What will you do if you are on duty in a hospital and a hypertensive patient, who has been treated
with long-acting ß-blocker, long-acting dihydropyridine calcium antagonist and long-acting a-1
adrenoceptor blocker, is admitted with the following symptoms: headache, dyspnea, ankle-swelling, BP
180/110 mmHg, pulmonary rales, LVH on ECG, echo: LVH, left ventricular diastolic dysfunction,
ejection fraction 46%.
A. Amlodipine orally
B. Nifedipine orally
C. Enalaprilate iv
D. *Enalaprilate iv + furosemide iv
E. Esmolol iv
1456.Which of the following blood pressure levels in pregnancy should be considered an emergency
requiring hospitalization?
A. ≥140/90 mmHg
B. ≥150/95 mmHg
C. ≥160/100 mmHg
D. *≥170/110 mmHg
E. A rise in SBP ≥25 mmHg or a rise in DPB ≥15 mmHg compared to pre-pregnancy values, or those
in the first trimester
1457.The following drug combinations are effective to treat hypertension EXCEPT
A. Diuretics + beta-blockers
B. Beta-blockers + dihydropiridine calcium channel blockers
C. Diuretics + ACE-inhibitors/ARB
D. ACE-inhibitors/ARB + calcium channel blockers
E. *Beta-blockers + ACE-inhibitors/ARB
1458.Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. *When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
1459.With respect to renovascular disease, all of the statements are true EXCEPT:
A. Worsening renal function with ACE-inhibitor therapy suggests bilateral renovascular disease
B. Atherosclerotic disease most commonly involves the proximal third of the main renal artery
C. The most common form of fibroplastic renovascular disease in adults involves the media
D. *The incidence of renovascular hypertension falls with increased age
E. Patients with severe, accelerated hypertension have the highest prevalence of renovascular disease
1460.A newly diagnosed diabetic patient presents with BP readings that are 155/95 or higher. All of the
following statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blockade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
1461.All of the following statements regarding the association of oral contraceptive pills and
hypertension are correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
1462.Each of the following statements regarding pheochromocytoma is true EXCEPT:
A. Approximately 15% of pheochromocytomas are extra-adrenal
B. Ten percent of pheochromocytomas are malignant
C. Ten percent of adrenal pheochromocytomas are bilateral
D. *Hypertension related to pheochromocytoma is nearly always episodic and only rarely persistent
E. Pheochromocytoma can be inherited
1463.All of the following are features of renovascular hypertension due to fibromuscular hyperplasia, as
opposed to atherosclerosis, EXCEPT:
A. Age <50 years
B. Female gender
C. *More likely to progress to complete renal artery occlusion
D. No family history of hypertension
E. Absence of carotid bruits
1464.Which of the following ACE-inhibitors are not prodrugs?
A. Captopril, lisinopril, ramipril
B. Lisinopril, enalapril, banazepril
C. *Captopril, lisinopril, enalaprilat
D. Moexipril, captopril, lisinopril
E. Perindopril, ramipril, enalapril
1465.Each of the following statements regarding hypertension is true EXCEPT:
A. The prevalence of hypertension rises progressively with age in both men and women
B. Systolic and diastolic hypertension are each associated with an increased crisk of coronary heart
disease
C. *The target blood pressure for hypertensive patients with cardiovascular disease or diabetes is
140/90 mmHg
D. Patients with prehypertension (SBP 120-139 mmHg or DBP 80-89 mmHg) benefit from lifestyle
modifications incl. weight reduction, regular exercise, and smoking cessation
E. Drug therapy of hypertension benefits patients greater than 80 years of age
1466.All of the following interventions have a BP-lowering effect EXCEPT:
A. A diet that reduces caloric intake by 1000 calories per day
B. Reduction of dietary sodium
C. *Daily magnesium supplements
D. Tobacco cessation
E. Reduction of ethanol consumption to less than 30 ml/day
1467.Each of the following statements regarding hypertension is true EXCEPT:
A. Pure "white coat hypertension is found in 20 to 30% of patients
B. When measuring BP, an inappropriately small cuff size results in a spuriously low systolic
measurement
C. Pseudohypertension may occur in patients with sclerotic brachial arteries
D. Chronic renal disease is the second most common cause of hypertension after essential
hypertension
E. Coarctation of the aorta, Cushing disease, primary aldosteronism account for approximately 1% of
all hypertensive patients
1468.Each of the following statements regarding hypertension is true EXCEPT:
A. Increased LV muscle mass in hypertension is an independent risk factor of cardiac mortality
B. The risk of ventricular arrhythmias in hypertension is increased 2-fold in the presence of LV
hypertrophy
C. Low birth weight is associated with an increased incidence of hypertension later in life
D. *Chronic caffeine consumption is associated with an increased risk of hypertension
E. In hypertensive adolescents, essential hypertension is the most likely etiology
1469.The following statements regarding the association of oral contraceptive pills and hypertension are
correct EXCEPT:
A. The likelihood of developing hypertension is increased by significant alcohol consumption
B. The incidence of hypertension is about twice as great in pill users as in non-users
C. The likelihood of developing hypertension is dependent on the age of the user
D. *Hypertension resolves in almost all cases after discontinuation of oral contraceptives
E. The mechanism for contraceptive-induced hypertension likely involves renin-aldosterone-mediated
volume expansion
1470.Thiazide diuretics can contribute to each of the following metabolic effects EXCEPT:
A. Hypomagnesemia
B. *Hypouricemia
C. Hypercalcemia
D. Hypercholesterolemia
E. Hyponatremia
1471.Which of the following statements regarding prevention of stroke is correct?
A. Treatment of systolic hypertension does not decrease the risk of stroke in patients older than age 60
B. Hypertension should not be a target of secondary prevention after an ischemic stroke because
elevated BP is desirable to maintain adequate cerebral perfusion
C. *Treatment with HMG-CoA reductase inhibitors reduces the risk of recurrent stroke
D. The combination of aspirin and clopidogrel is superior to aspirin alone for prevention of recurrent
stroke
E. None of the above
1472.Which of the following antihypertensive agents is a known cause of autoimmune hemolytic
anemia?
A. Metoprolol
B. *Methyldopa
C. Captopril
D. Losartan
E. Monoxidine
1473.All of the following characteristics are typical of hypertensive crisis EXCEPT:
A. Diastolic BP >120 mmHg
B. Retinal hemorrhages
C. *Constriction of cerebral arterioles with decreased vascular permeability
D. Proteinuria
E. Microangiopathic hemolytic anemia
1474.Which of the following pairs of medical conditions and antihypertensive medications would be
INCORRECT to use in a patient with essential hypertension?
A. Beta-blocker and a history of myocardial infarction
B. Alpha-blocker and prostatic hypertrophy
C. *Thiazide diuretic and gout
D. Amlodipine and heart failure
E. ACE-inhibitor and diabetes mellitus
1475.Which of the following statements regarding antihypertensive agents and atrial fibrillation (AF) is
TRUE?
A. *Losartan has been shown to decrease new-onset AF more effectively than atenolol
B. Valsartan has been shown to decrease new-onset AF more effectively than amlodipine
C. Atenolol has been shown to decrease new-onset AF more effectively than captopril
D. Nifedipine has been shown to decrease new-onset AF more effectively than diltiazem
E. All of the above are false
1476.Which lifestyle change has been shown to produce the biggest reduction in systolic blood pressure?
A. *10-kg weight loss
B. Dietary sodium reduction
C. Moderation of alcohol consumption
D. Change to a vegetarian diet
E. Magnesium supplement
1477.Which of these statements is true regarding renin-angiotensin system-blocking agents?
A. Less effective when combined with a diuretic than when used alone
B. More effective in patients of African descent than in white patients
C. *Preserve kidney function in addition to lowering blood pressure
D. Are the first-line antihypertensive medications in pregnancy
E. All of the above
1478.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. *Hydrochlorthiazide – diabetes mellitus
E. Loop diuretic – heart failure
1479.Which of the following statements about microalbuminuria is TRUE?
A. To be of clinixal value, microalbuminuria must be measured in a timed 12- to 24-hour sample
B. *Microalbuminuria is a cardiovascular risk factor that is independent of traditional Framingham
risk factors
C. Microalbuminuria is a predictor of risk only in patients with diabetes
D. Microalbuminuria is present when the “spot” urine albumin-to-creatinine ration is >500 mg/g
E. All of the above statements are correct
1480.Renin-dependent hypertension includes:
A. Primary hyperaldosteronism
B. Essential hypertension
C. *Renovascular hypertension
D. Pheochromocytoma
E. Cushing syndrome
1481.Fundus picture of stage 2 of Keith-Wegener classification includes
A. Copper wire AV nipping and focal spasm
B. *Silver wire increased reflex
C. Exudate and hemorrhagic spots
D. Papilloedema
E. Retinal hemorrhages
1482.A young hypertensive patient has serum potassium 2.8 mEq/l and increased aldosterone level with
decreased plasma renin activity. The likely diagnosis is....
A. Renal artery stenosis
B. Ectopic ACTH syndrome
C. *Conn syndrome
D. Liddle syndrome
E. Cushing syndrome
1483.The proportion of essential (primary) hypertension among all hypertension causes is as high as
A. 25-30%
B. 40-45%
C. 60-65%
D. 70-75%
E. *90-95%
1484.All of the following are risk factors for hypertension, EXCEPT
A. Increased body weight
B. Family history of hypertension
C. Excessive intake of sodium
D. *Regular use of one glass of wine per day
E. Cigarette smoking
1485.All of the following statements concerning hypertension are true, EXCEPT
A. In a western adult population the prevalence of hypertension exceeds 20%
B. Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
C. The pathophysiology of hypertension differs in black adults compared to South Asians and whites
D. People of African descent commonly have a high renin type hypertension
E. *An increase in potassium intake may significantly reduce blood pressure in hypertensive patients
1486.Optimal blood pressure (BP) is defined as a BP level of
A. *<120/80 mmHg
B. <130/80 mmHg
C. <140/90 mmHg
D. <160/100 mmHg
E. <125/80 mmHg
1487.Which parameter of arterial blood pressure (BP) yields the best prognostic information in patients
at risk for cardiovascular disease?
A. Systolic BP
B. Diastolic BP
C. Mean arterial BP
D. *Pulse pressure
E. None
1488.Which BP profile below identifies the patient with the highest risk for development of
cardiovascular complications?
A. 160/90 mmHg
B. *160/65 mmHg
C. 140/100 mmHg
D. 130/90 mmHg
E. 120/70 mmHg
1489.Physicians should diagnose isolated office hypertension (so-called “white-coat hypertension”)
whenever office BP is ≥140/90 mmHg at several visits, while 24-h ambulatory BP is
A. <160/100 mmHg
B. <140/90 mmHg
C. *<130/85 mmHg
D. <125/80 mmHg
E. <120/70 mmHg
1490.Target organs in hypertension include all of the following EXCEPT
A. Brain and eyes
B. Heart
C. Kidneys
D. Peripheral arteries
E. *Liver
1491.All of the following statements concerning target organ damage are true EXCEPT
A. Microalbuminuria is a sensitive marker of hypertension-induced renal damage
B. *An increase in serum creatinine when antihypertensive therapy is intensified is a sign of
progressive renal deterioration
C. Electrocardiography should be part of all routine assessment of subjects with high BP
D. Echocardiography is much more sensitive than electrocardiography in diagnosing left ventricular
hypertrophy
E. Grades 1 and 2 arteriolar retinal changes do not have a significant prognostic value
1492.At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
1493.The initial antihypertensive medication recommended for patients who have no compelling
indications or contraindications is
A. ACE-inhibitor
B. Calcium-channel blocker
C. Diuretics
D. Beta blocker
E. *Any of the above
1494.In patients with a history of stroke or TIA the preferred drug combination is:
A. *ACE-inhibitor and diuretic
B. Calcium-channel blocker and beta-blocker
C. Beta-blocker and diuretic
D. Angiotensin receptor blocker and beta blocker
E. Beta- and alpha blocker
1495.In the elderly with systolic hypertension antihypertensive therapy should be initiated if SBP
A. ≥120 mmHg
B. ≥130 mmHg
C. *≥140 mmHg
D. ≥160 mmHg
E. ≥170 mmHg
1496.The best medication for the treatment of isolated systolic hypertension in the elderly:
A. ACE-inhibitor and diuretic
B. *Dihydropiridine calcium-channel blocker and diuretic
C. Beta-blocker and diuretic
D. Non-dihydropiridine calcium-channel blocker and diuretic
E. Beta- and alpha blocker
1497.The following medications can be used in pregnancy EXCEPT
A. Methyldopa
B. Labetalol
C. *ACE-inhibitor / ARB
D. Hydralazine
E. Nifidipine
1498.In patients of African descent the drug of choice for initial treatment of hypertension is:
A. Verapamil
B. Atenolol
C. Perindopril
D. *Hydrochlorothiazide
E. Amlodipine
1499.Which of the following antihypertensive agents is INCORRECTLY matched with the indication for
therapy?
A. ACE inhibitor – diabetic nephropathy
B. Beta-blocker – coronary artery disease
C. Calcium channel blocker – angina pectoris
D. Diuretics – heart failure
E. *Loop diuretic – gout
1500.All the following patients should be evaluated for secondary causes of hypertension EXCEPT
A. *A 47-year-old male with strong family history hypertension who presents to your office with a BP
of 150/100
B. A 26-year-old female with hematuria and a family history of early renal failure who has a BP of
160/90
C. A 73-year-old male with no past history with a BP of 165/90
D. A 58-year-old male with a history of hypertension since age 45 whose BP has become increasingly
difficult to control on four antihypertensive agents
E. A 31-year-old female with complaints of severe headaches, weight gain, and new-onset DM with a
BP of 145/90
1501.Which of the following is an effective adjunct to increase the rate of smoking cessation?
A. Aldosterone
B. *Bupropion
C. Sildenafil
D. Cimetidine
E. Buspirone
1502.With which of the following is sildenafil acetate (Viagra) most likely to interact adversely?
A. Fibrinolytic therapy
B. Primary PCI
C. *Nitrates
D. Aspirin
E. Beta-blockers
1503.Bupropion hydrochloride (Zyban) is contraindicated in patients with a history of which of the
following?
A. *Seizures
B. Insulin-dependent diabetes mellitus
C. Severe chronic obstructive pulmonary disease (with reversible component)
D. Longer than 40-year history of tobacco use
E. Recent MI
1504.In which of the following has the high-sensitivity C-reactive protein (CRP) been shown to be
predictive of risk?
A. Acute MI
B. Acute coronary syndromes
C. Chronic stable angina
D. Peripheral vascular disease
E. *All of the above
1505.Which of the following has been shown to decrease the level of the high-sensitivity CRP?
A. Unopposed estrogen
B. Amlodipine besylate (Norvasc)
C. *Simvastatin
D. All of the above
E. None of the above
1506.All of the following statements regarding myocardial stunning are true EXCEPT:
A. *Stunning is a state of depressed myocardial function due to chronic hypoperfusion
B. Stunning can be global or regional
C. Stunning can follow cardiac surgery with cardiopulmonary bypass
D. Oxygen-free radicals and excess intracellular calcium likely contribute to stunning
E. Stunning affects both systolic and diastolic function
1507.What is the most common coexisting congenital anomaly in patients with coarctation of the aorta?
A. Cleft mitral valve
B. *Bicuspid aortic valve
C. Ebstein's anomaly
D. VSD
E. PDA
1508.All of the following are characteristic findings of ostium primum atrial septal defect (ASD)
EXCEPT:
A. Precordial heave
B. Fixed split S2
C. *Right axis deviation
D. Systolic ejection murmur
E. Prominent pulmonary vascular markings on CXR
1509.Choose the adult congenital disorder corresponding to the following physical examination fingings:
RV lift with a loud systolic ejection murmur along the left sternal border, with a single S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. *Tetralogy of Fallot
1510.Choose the adult congenital disorder corresponding to the following physical examination fingings:
loud S1, holosystolic murmur in left sternal border, systolic ejection click, and hepatomegaly
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. *Ebstein's anomaly
E. Tetralogy of Fallot
1511.Choose the adult congenital disorder corresponding to the following physical examination fingings:
weak or delayed femoral pulses, harsh systolic murmur in the back, and a systolic ejection click in the
aortic area
A. Eisenmenger's syndrome
B. *Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1512.Choose the adult congenital disorder corresponding to the following physical examination fingings:
cyanosis, digital clubbing, loud P2, and a variable Graham-Steel murmur
A. *Eisenmenger's syndrome
B. Coarctation of the aorta
C. PDA
D. Ebstein's anomaly
E. Tetralogy of Fallot
1513.Choose the adult congenital disorder corresponding to the following physical examination fingings:
wide pulse pressure, prominent LV impulse, and a continuous machinery murmur enveloping S2
A. Eisenmenger's syndrome
B. Coarctation of the aorta
C. *Patent ductus arteriosus
D. Ebstein's anomaly
E. Tetralogy of Fallot
1514.Bacterial endocarditis prophylaxis is indicated in all adults who have the following congenital heart
disease EXCEPT:
A. VSD
B. Coarctation of the aorta
C. *Secundum ASD
D. Hypertrophic obstructive cardiomyopathy
E. PDA
1515.Besides pulmonary valve stenosis, which of the following is the most common associated cardiac
defect present in patients with PA stenosis?
A. *VSD
B. ASD
C. Coarctation of the aorta
D. PDA
E. Tetralogy of Fallot
Situational tasks
1.52 year old male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in the
DIP of the right first digit, with calcifications. Further questioning revealed a history of repeated attacks
of acute joint pain. There is bony erosion at multiple DIP's of the right hand that is periarticular, well
corticated and has a thin overhanging edge. There is no associated osteopenia. Choose the most likely
diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Chronic gouty arthritis
E. Psoriatic arthritis
2.52 yo male with chronic joint pain. There is asymmetric soft tissue swelling, predominantly in the DIP
of the right first digit, with calcifications. Further questioning revealed a history of repeated attacks of
acute joint pain. There is bony erosion at multiple DIP's of the right hand that is periarticular, well
corticated and has a thin overhanging edge. There is no associated osteopenia. Which of the following
medications is indicated for the treatment of chronic arthritis?
A. colchicine
B. *allopurinol
C. corticosteroids
D. indomethacin
E. ibuprofen
3.55 years old, came to a musculoskeletal specialist seeking advice for a 3-year history of progressively
worsening pain in both knees. Her knees were stiff for about 20 minutes when she arose in the morning
and for a few minutes after getting up from a chair during the day. She had difficulty walking > 30
minutes because of pain, and her symptoms were exacerbated by kneeling, squatting, or descending
stairs. Although sitting, resting, and reclining relieved her pain, she became stiff if she stayed in one
position for too long. Her symptoms were worse on humid or cold days, and she occasionally felt as if
one of her knees would give out. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
4.55 years old, came to a musculoskeletal specialist seeking advice for a 3-year history of progressively
worsening pain in both knees. Her knees were stiff for about 20 minutes when she arose in the morning
and for a few minutes after getting up from a chair during the day. She had difficulty walking > 30
minutes because of pain, and her symptoms were exacerbated by kneeling, squatting, or descending
stairs. Although sitting, resting, and reclining relieved her pain, she became stiff if she stayed in one
position for too long. Her symptoms were worse on humid or cold days, and she occasionally felt as if
one of her knees would give out. Which of the following changes will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
5.55 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Chronic Gouty arthritis
C. Rheumatoid arthritis
D. Osteoarthritis
E. Psoriatic arthritis
6.57 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is indicated for the treatment
of chronic arthritis?
A. colchicine
B. corticosteroids
C. indomethacin
D. *allopurinol
E. ibuprofen
7.54 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the right foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is contraindicated for the
treatment of exacerbation of arthritis
A. corticosteroids
B. colchicine
C. indomethacin
D. ibuprofen
E. *allopurinol
8.59 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the right foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is indicated for the treatment
of exacerbation of arthritis?
A. allopurinol
B. corticosteroids
C. *colchicine
D. indomethacin
E. ibuprofen
9.70-year-old, married, teacher. She has been under treatment for hypertension and is finally stable on
medication. Initial Chief complaint: painful right knee, arthritis in right hip. She had had arthritic pain in
her right hip confirmed by x-ray about 10 years ago. The knee pain is a newer problem and she suspects
it is also arthritis. There is slight crepitus with motion of the right knee. Which of the following treatment
do use?
A. Methotrexat
B. Colchicines
C. *Chondroitin sulfate
D. Tetracycline
E. Allopurinol
10. 65-year-old, women. She has been under treatment for hypertension and is finally stable on
medication. Initial Chief complaint: painful left knee, arthritis in left hip. She had had arthritic pain in her
right hip confirmed by x-ray about 10 years ago. The knee pain is a newer problem and she suspects it is
also arthritis. There is slight crepitus with motion of the right knee. Which of the following changes will
reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
11. A 38-year-old man with a 13-yr history of back pain, presented with acute pain and swelling of one
knee. On examination, the joint was tender and restricted in movement. X-ray of the knee showed
periarticular osteoporosis. On investigation, he had a raised erythrocyte sedimentation rate of 32 mm/h, a
mild anemia (Hb 106g/l) but no detectable serum rheumatoid factor. The knee effusion was aspirated; the
fluid contained a polymorphonuclear leucocytosis but no organisms or rheumatoid factor. Fifteen months
later he developed an iritis in his left eye, low back pain and stiffness. His peripheral joints were normal
but pain could be elicited in both sacroiliac joints. Choose the medications for patient with shown
changes from the below list of options.
A. *Methotrexate
B. Actovegin
C. Mydocalm
D. Warfarin
E. Pentoxifylline
12. A 38-year-old man with a 13-yr history of back pain, presented with acute pain and swelling of one
knee. On examination, the joint was tender and restricted in movement. X-ray of the knee showed
periarticular osteoporosis. On investigation, he had a raised erythrocyte sedimentation rate of 102mm/h, a
mild anaemia (Hb 106g/l) but no detectable serum rheumatoid factor. The knee effusion was aspirated;
the fluid contained a polymorphonuclear leucocytosis but no organisms or rheumatoid factor. Fifteen
months later he developed an iritis in his left eye, low back pain and stiffness. His peripheral joints were
normal but pain could be elicited in both sacroiliac joints. Choose the most likely diagnosis from the
below list of options for patient with shown changes
A. *Ankylosing spondylitis
B. Reactive arthritis
C. Osteoarthritis
D. Gout
E. Psoriatic arthritis
13. A 50-year-old male is evaluated because of pain in the right inguinal area, lower back, and hands.
The inguinal pain worsens as he walks, and all pain increases as the day progresses. On physical
examination, internal rotation of the right hip elicits the groin pain. The second, third, and fourth
metacarpophalangeal joints are swollen, warm, and tender to pressure. Radiographs show severe
osteoarthritis in the right hip. Which of the following is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. *Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. Serum uric acid
14. A 55-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following is
characteristic of the arthritis?
A. *Depositions of monosodium urate monohydrate crystals within the periarticular soft tissues
B. Overgrowth of bones within joints
C. Autoimmune synovitis
D. Osteoporosis
E. Rheumatoid nodules over joints
15. A 64-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has non tender bony overgrowth at the distal interphalangeal joints.
The patient says that her mother had the same fingers and she worries that she will become crippled.
Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
16. A 68-year-old man is evaluated because of a 3-year history of bilateral knee pain and low back
pain. He has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, he has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
right knee. Which of the following treatment do use?
A. Methotrexat
B. *Glucosamine
C. Colchicines
D. Tetracycline
E. Allopurinol
17. A 38-year-old man with a 13-yr history of back pain,presented with acute pain and swelling of one
knee. On examination, the joint was tender and restricted in movement. X-ray of the knee showed
periarticular osteoporosis. On investigation, he had a raised erythrocyte sedimentation rate of 32 mm/h, a
mild anemia (Hb 106g/l) but no detectable serum rheumatoid factor. The knee effusion was aspirated; the
fluid contained a polymorphonuclear leucocytosis but no organisms or rheumatoid factor. Fifteen months
later he developed an iritis in his left eye, low back pain and stiffness. His peripheral joints were normal
but pain could be elicited in both sacroiliac joints. Which of the following medications is indicated for
the treatment of the disease?
A. *Sulfasalazine
B. Cyclosporine
C. Diclofenac
D. Pentoxifylline
E. Corticosteroids
18. A 57-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following changes
will reveal X-ray examination?
A. Erosions
B. Subluxations
C. Osteophytes
D. Osteoporosis
E. *"punched-out" lytic lesion
19. A 58-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 4 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following
medications is indicated for the treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
20. A 60-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. As she describes her pain, she slides her hand down the anterior thigh to
her knee on the right to show where the pain is most severe. On physical examination, she has slight
swelling and tenderness to pressure of the distal interphalangeal joints 2-5 on both hands. All the joints
are brought through full range of motion without pain. There is slight crepitus with motion of the right
knee. Which of the following treatment do use?
A. methotrexat
B. *intra-articular injection of sodium hyaluronate
C. probenecid
D. colchicine
E. allopurinol
21. A 64-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. On
physical examination, there is crepitus on passive motion of the left knee, which has a slight varus
deformity. Her feet turn out slightly, and the heels are in valgus. Which of the following changes will
reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
22. A 68-year-old woman has had four or five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. She is asymptomatic between attacks, and sulindac, 200 mg
twice daily, has usually relieved the symptoms. Her most recent episode was 4 months ago. On physical
examination, none of her joints is swollen or tender, but there is marked crepitus on extension of the
knee. She also has a positive bulge sign over the left knee and pain on full extension of the left elbow.
Which one of the following tests would confirm the diagnosis?
A. *Arthrocentesis of the knee and laboratory analysis of the synovial fluid
B. Measurement of serum uric acid
C. Measurement of serum rheumatoid factor
D. Radiograph of the knee
E. MRI of the knee with gadolinium contrast
23. A 72-year-old retired lawyer is evaluated because of swelling of his right knee. He has mild
osteoarthritis and stays active swimming and playing tennis and golf. On physical examination, he has an
effusion in the right knee. At a point in the mid-thigh (measured from the superior border of the patella),
the right thigh is 4 cm smaller in diameter than the left. There is crepitus with right knee flexion. The
knee is not warm. Which of the following is the best next step in the management of this patient?
A. Order radiographs of both knees and treat the patient with ibuprofen.
B. Order radiographs of the right hip and right knee.
C. *Aspirate the joint fluid in the right knee and refer the patient for physical therapy.
D. Aspirate the joint fluid in the right knee and obtain blood cultures.
E. Treat the patient with celecoxib, and advise him to stay off his feet for 48 hours.
24. On the third day of hospitalization, he developed acute, severe pain and swelling of the left elbow.
Within next few hours, pain worsened and he was unable to move the elbow joint, which was tender,
erythematous, and swollen on examination. Never investigated in the past, we also noted a firm 4-6 cm
mass on each elbow, and another one surrounding the proximal inter-phalangeal joint of right middle
finger. When asked particularly, he noticed similar episodes of arthritis of great toe in the past. Choose
the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis + synovitis
D. *Exacerbation of chronic gouty arthritis
E. Psoriatic arthritis
25. On the third day of hospitalization, he developed acute, severe pain and swelling of the left elbow.
Within next few hours, pain worsened and he was unable to move the elbow joint, which was tender,
erythematous, and swollen on examination. Never investigated in the past, we also noted a firm 4- 6 cm
mass on each elbow, and another one surrounding the proximal inter-phalangeal joint of right middle
finger. When asked particularly, he noticed similar episodes of arthritis of great toe in the past. Which of
the following medications is indicated for the treatment of the arthritis?
A. allopurinol
B. corticosteroids
C. *colchicine
D. tetracycline
E. mydocalmi
26. A 65-year-old woman is evaluated because of a 3-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. On physical examination, she has slight swelling and tenderness to
pressure of the distal interphalangeal joints 2-5 on both hands. There is slight crepitus with motion of the
left knee. Which of the following treatment do use?
A. methotrexat
B. allopurinol
C. probenecid
D. colchicine
E. *Intra-articular Hyaluronic Acid Injections
27. A 69-year-old woman is evaluated because of a 5-year history of bilateral knee pain. She has some
stiffness for approximately 15 minutes when she awakens in the morning, and during the afternoon her
pain is worse. On physical examination, she has slight swelling and tenderness to pressure of the distal
interphalangeal joints on both hands. There is slight crepitus with motion of the right knee. All of the
following are X-ray signs of arthritis except
A. Joint space narrowing
B. Marginal erosions
C. Subchondral cysts
D. Bony sclerosis
E. *Marginal osteophytes
28. 70 year old man presented with a three month history of malaise, lethargy, and 8 kg weight loss.
Five months previously he had a transurethral resection of the prostate (TURP) for benign prostatic
hypertrophy. The early postoperative period was complicated by retention of urine requiring reinsertion
of a temporary catheter. On examination there was a pansystolic murmur consistent with mitral
regurgitation. The apex beat was not displaced and no other cardiac abnormality was documented. The
patient had a temperature of 37°C. Which investigation you will do to cofirm the diagnosis?
A. *Echocardiograghy
B. ECG
C. Chest X-ray
D. Biochemical blood anylisis
E. ASLO titre
29. 70 year old man presented with a three month history of malaise, lethargy, and 8 kg weight loss.
Five months previously he had a transurethral resection of the prostate (TURP) for benign prostatic
hypertrophy. The early postoperative period was complicated by retention of urine requiring reinsertion
of a temporary catheter. On examination there was a pansystolic murmur consistent with mitral
regurgitation. The apex beat was not displaced and no other cardiac abnormality was documented. The
patient had a temperature of 37В°C. Which diagnosis do you suspect?
A. *infective endocarditis
B. rheumatic fever
C. pyelonephritis
D. myocarditis
E. pneumonia
30. Allopurinol is used in the management of gout. Which statement below is correct?
A. *Allopurinol is effective by inhibiting the conversion of xanthine to uric acid.
B. Allopurinol is effective by increasing glomerular filtrationof uric acid.
C. Allopurinol is effective by reducing the tubular reabsorption of uric acid.
D. Allopurinol is indicated in a 37 year old man with a uric acid concentration of 0.42 mg/l
E. Allopurinol is associated with aplastic anaemia in 1% of cases.
31. 57 year old man presented with a month history of malaise, lethargy, and 10 kg weight loss. Three
months previously he had a transurethral resection of the prostate (TURP) for benign prostatic
hypertrophy. The early postoperative period was complicated by retention of urine requiring reinsertion
of a temporary catheter. On examination there was a pansystolic murmur consistent with mitral
regurgitation. The apex beat was not displaced and no other cardiac abnormality was documented. The
patient had a temperature of 37-38°C. Which diagnosis do you suspect?
A. *infective endocarditis
B. rheumatic fever
C. pyelonephritis
D. myocarditis
E. pneumonia
32. A 22-year-old IV drug user presents complaining of fevers, hemoptysis, and pleuritic chest pain
over the preceding 2 weeks. On physical examination, his temperature is 38.2°C, pulse rate is 100/min,
and BP is 110/68. His LV impulse is normal and no murmurs are appreciated on cardiac auscultation. His
lungs are clear to auscultation. Three sets of blood cultures are positive for Staphylococcus aureus. What
is the most likely diagnosis?
A. *Infective endocarditis
B. Pneumonia
C. Viral syndrome
D. Pericarditis
E. Congenital cardiac shunt
33. A 15-year-old boy residing with his parents on a military base presents with a fever of 38.6 ° C and
complains of lower back, knee, and wrist pain. The arthritis is not localized to any one joint. He gives a
history of a severe sore throat several weeks earlier. Physical examination of the skin reveals pea-sized
swellings over the elbows and wrists. He also has two serpiginous, erythematous pink areas on the
anterior trunk, each about 5 cm in diameter. Laboratory investigation includes negative blood cultures,
negative throat cultures, normal CBC, and erythrocyte sedimentation rate (ESR) of 50. An
antistreptolysin- O (ASO) titer is elevated. This point, appropriate therapy would consist of
A. *parenteral penicillin and aspirin
B. supportive care alone
C. parenteral penicillin
D. parenteral penicillin and glucocorticoids
E. parenteral penicillin, aspirin, and diazepam
34. A 15-year-old girl is evaluated for a fever and joint pains. Three weeks earlier, she had a sore throat
that resolved without treatment. Four days ago, she developed pain and swelling of the right ankle and
the right elbow. Today she complains of pain and swelling of the left knee. Physical examination reveals
a temperature of 101°F and an HR of 110. A soft HSM and an S3 are audible at the cardiac apex. The left
knee is erythematous and tender; it has an effusion. Laboratory evaluation demonstrates an elevated
antistreptococcal antibody. You make the clinical diagnosis of acute rheumatic fever. In regard to this
patient, which of the following statements is true?
A. *She should receive benzathine PCN every 3 weeks until she is 25 years old.
B. Blood cultures are likely to be positive for group A streptococci.
C. Cardiac examination is also likely to disclose an OS and a low-pitched middiastolic murmur at the
cardiac apex.
D. Acute antibiotic treatment is not required, as the patient's sore throat has resolved.
E. She may have residual deformity of her left knee.
35. A 25-year-old IV drug user presents complaining of fevers, hemoptysis over the preceding 2 weeks.
On physical examination, his temperature is 38.2°C, pulse rate is 100/min, and BP is 110/70. His LV
impulse is normal and no murmurs are appreciated on cardiac auscultation. His lungs are clear to
auscultation. Three sets of blood cultures are positive for Staphylococcus aureus and echocardiography
shows a tricuspid valve vegetation with trace tricuspid regurgitation. Which of the following is the
strongest indication to consider valve replacement surgery in the patient?
A. *Progressive congestive heart failure (CHF)
B. Hematuria
C. Positive cultures for Staphilococcus aureus on the second day of therapy
D. Splinter hemorrhages and Osler nodes
E. Splenomegaly
36. A 26-year-old man seeks your advice because he was diagnosed as having a heart murmur as a
baby. At that time, his parents were told that he would likely outgrow the murmur, but no specific
recommendations were made. Physical examination shows blood pressure and heart rate are normal. The
apical impulse is nondisplaced. S1 is normal, and S2 is physiologically split. A thrill is noted in the third
left intercostal space, and a 4/6 holosystolic murmur is noted along the left sternal border, radiating to the
right. No S3 or S4 is audible. Echocardiogram shows a small perimembranous ventricular septal defect.
The dimensions of the cardiac chambers and the estimated pulmonary artery pressure are normal. Which
of the following is the most appropriate feature of the management of this patient?
A. *Recommendation for treatment with amoxicillin, 2 g orally 1 hour before dental procedures
B. Referral to a cardiothoracic surgeon for surgical closure of the ventricular septal defect
C. Referral to an interventional cardiologist for percutaneous closure of the defect
D. Initiation of treatment with lisinopril, 10 mg/d orally
E. Referral to a cardiothoracic surgeon for surgical closure of the ventricular septal defect and
Initiation of treatment with lisinopril
37. A 32-year-old IV drug user presents complaining of fevers, hemoptysis, and pleuritic chest pain
over the preceding 2 weeks. On physical examination, his temperature is 38.2°C, pulse rate is 100/min,
and BP is 110/60. His LV impulse is normal and no murmurs are appreciated on cardiac auscultation. His
lungs are clear to auscultation. Echocardiography shows a tricuspid valve vegetation with trace tricuspid
regurgitation. What is the most likely diagnosis?
A. *Infective endocarditis
B. Pneumonia
C. Viral syndrome
D. Pericarditis
E. Congenital cardiac shunt
38. A 34-year-old man with a history of a bicuspid AV is diagnosed with endocarditis. Despite 2 weeks
of appropriate antibiotic therapy, he has persistent fevers and bacteremia. A diagnostic study is
performed and a paravalvular abscess discovered. What is the next step in this patient's management?
A. *Refer for surgery
B. Continue current antibiotic therapy
C. Add gentamicin
D. Change nafcillin to vancomycin
E. Change nafcillin to ceftriaxone
39. A 23-year-old IV drug user presents complaining of fevers, hemoptysis, and pleuritic chest pain
over the preceding 2 weeks. On physical examination, his temperature is 38.2°C, pulse rate is 110/min,
and BP is 110/60. His LV impulse is normal and no murmurs are appreciated on cardiac auscultation. His
lungs are clear to auscultation. Three sets of blood cultures are positive for Staphylococcus aureus and
echocardiography shows a tricuspid valve vegetation with trace tricuspid regurgitation. He is started on
IV antibiotic therapy with nafcillin. Despite 2 weeks of appropriate antibiotic therapy, he continues to
have intermittent fevers and has developed a grade 2/6 pansystolic murmur along his left sternal border
as well as a first-degree AV block on his ECG. His repeat blood cultures remain positive for S. aureus.\n
Which diagnostic test is most appropriate at this time?
A. *TEE
B. Electrophysiologic study
C. TTE
D. Bronchoscopy
E. Cardiac catheterization
40. A 35-year-old construction worker reports having had fevers and chills for several days.
Examination reveals a temperature of 102°F, HR of 110 bpm, and BP of 120/85 mm Hg. His teeth are in
poor condition. His lungs are clear, and cardiac examination is unremarkable. Blood cultures are drawn
and grow Streptococcus viridans. He is diagnosed with SBE. Despite antibiotics, the patient continues to
have persistent fever and develops acute dyspnea on the fifth hospital day. Physical examination is likely
to reveal:
A. *An HSM at the apex
B. An early-peaking, crescendo-decrescendo murmur at the upper sternal border
C. Weak and delayed carotid upstrokes
D. An apical middiastolic murmur with presystolic accentuation and an OS
E. A three-component pericardial friction rub
41. A 35-year-old woman comes to your office for the first time. A cardiologist in another city told her
that she has mitral valve prolapse and therefore needs to take antibiotics prior to dental procedures. A
copy of her echocardiogram report states that she has Doppler-demonstrated mitral regurgitation. She
will have a tooth extracted in 4 days and asks for a 2-day supply of clindamycin, which she was given
previously. She states that she is allergic to penicillin. According to current guidelines from the American
Heart Association, which of the following is most appropriate for prophylaxis prior to this patients dental
procedure? \n Tell her that she does not need prophylaxis for this procedure?
A. *Prescribe a single 600-mg dose of clindamycin to be taken 1 hour before the procedure
B. Prescribe a 2-day course of cephalexin to start 30 minutes before the procedure
C. Prescribe a 7-day course of cephalexin to start today
D. Prescribe a 2-day course of clindamycin to start 30 minutes before the procedure
E. Prescribe a 7-day course of clindamycin to start 30 minutes before the procedure
42. A 36-year-old man is transferred to the intensive care unit because of abrupt onset of hypotension
and hypoxemia. He was admitted to the hospital earlier in the day with a 1-week history of fever and
night sweats that occurred after dental cleaning. Physical examination shows a temperature of 38.1 °C
(100.4 °F), heart rate of 121/min, and blood pressure of 88/30 mm Hg. Diffuse pulmonary crackles are
noted. Heart sounds are regular, with a summation gallop. No murmurs are heard. Electrocardiogram
shows sinus tachycardia. The hemoglobin level is 14.2 g/dL, and leukocyte count is 18,100/1iL.
Transesophageal echocardiography shows a bicuspid aortic valve with associated oscillating soft tissue
densities that suggest vegetations. Partial destruction of both cusps is seen, with severe aortic
regurgitation. Left ventricular size and systolic function are normal. You order blood cultures and initiate
broad-spectrum antimicrobial therapy. Which of the following interventions is indicated?
A. *Initiate treatment with nitroprusside.
B. Initiate treatment with a ОІ-blocker.
C. Insert an intra-aortic balloon counterpulsation catheter.
D. Refer the patient for heart catheterization with coronary arteriography.
E. Transfer the patient to surgery for emergent aortic valve replacement.
43. A 60-year-old man, a smoker, presents with intermittent fevers over a several week period. He has
no significant past medical history but was told that he had a murmur at some point in the past. His
temperature is 100°F, HR 85 bpm, and BP 135/70 mm Hg. Physical examination reveals digital clubbing
and splenomegaly. Small, erythematous, nontender spots are noted over the palmar aspect of his hands.
His lungs are clear to auscultation. Cardiac examination reveals a midsystolic click and a faint apical
holosystolic murmur. What is the most likely diagnosis?
A. *Infective endocarditis
B. Pneumonia
C. Viral syndrome
D. Pericarditis
E. Congenital cardiac shunt
44. A 65-year-old man presents with fevers, chills, weight loss, and malaise. His examination
demonstrates splinter hemorrhages in his nail beds and conjunctival petechiae. A lll/VI HSM is heard at
the cardiac apex. Echocardiography demonstrates a vegetation on his mitral valve and moderate MR.
Blood cultures are obtained and grow Streptococcus bovis. He is placed on appropriate antibiotics and
remains hemodynamically stable. Further evaluation at this stage should include:
A. *TEE
B. Colonoscopy
C. Thoracic CT scan
D. scan of the head
E. Cardiac catheterization
45. A 37-year-old man is evaluated because of fatigue, backache, and intermittent fever of 3 months
duration. He has no history of cardiac disease or drug allergies. On physical examination discloses a soft
diastolic murmur of aortic insufficiency, which is a new finding. There is splenomegaly. Four sets of
blood cultures grow a microorganism of the viridans streptococci group, which is sensitive to penicillin.
A transthoracic echocardiogram shows a thickened bicuspid aortic valve with evidence of mild aortic
insufficiency. Which of the following intravenous agents is the most appropriate initial antibiotic therapy
for this patient?
A. *Penicillin G for 4 weeks
B. Vancomycin for 4 weeks
C. Penicillin G plus gentamicin, both for 4 weeks
D. Penicillin G plus gentamicin, both for 6 weeks
E. Ceftriaxone for 8 weeks
46. A 54-year-old man is evaluated because of fatigue, backache, and intermittent fever of 3 months
duration. He has no history of cardiac disease or drug allergies. On physical examination, there are three
splinter hemorrhages under his fingernails but no other abnormalities of his skin. Ophthalmologic
examination reveals a right conjunctival hemorrhage. Cardiac examination discloses a soft diastolic
murmur of aortic insufficiency, which is a new findingA transesophageal echocardiogram confirms these
findings and also shows an oscillating mass on the aortic valve. Which of the following intravenous
agents is the most appropriate initial antibiotic therapy for this patient?
A. *Penicillin G for 4 weeks
B. Vancomycin for 4 weeks
C. Penicillin G plus gentamicin, both for 4 weeks
D. Penicillin G plus gentamicin, both for 6 weeks
E. Ceftriaxone for 8 weeks
47. An 86-year-old woman is evaluated for recent abrupt onset of dyspnea. She underwent
bioprosthetic aortic valve replacement 16 years ago because of calcific aortic stenosis. She has no history
of recent febrile illness, and she has had no recent medical or dental procedures. Physical examination
shows a harsh, crescendo-decrescendo systolic murmur at the right upper sternal border, radiating to the
carotids. Which of the following is the most likely cause of the patients symptoms?
A. *Prosthetic valve failure
B. Paraprosthetic leak
C. Thrombus formation
D. Infective endocarditis
E. rheumatic fever
48. Two years after undergoing mitral valve replacement, a 48-year-old man has a cerebrovascular
accident. Except for fever, general physical examination is noncontributory. A transesophageal
echocardiogram shows an oscillating mass on the mitral valve but no evidence of perivalvular extension
or abscess. Six sets of blood cultures grow Enterococcus faecalis, which is resistant to penicillin and
ampicillin but sensitive to vancomycin. A decision is made to treat medically, and the patient is begun on
vancomycin, 1 g intravenously every 12 hours, and gentamicin, 80mg intravenously every 8 hours. The
technician notes that the vancomycin peak and trough levels and the gentamicin trough level are in the
desirable range but that the laboratory therapeutic peak range for gentamicin is 4 to 8 Oјg/mL. Repeat
blood cultures show no growth, and complete blood count and serum creatinine values are normal.
Which of the following is most appropriate at this time?
A. *Keep both the gentamicin and the vancomycin doses unchanged
B. Increase the gentamicin dose; keep the vancomycin unchanged
C. Decrease the interval between the gentamicin doses; keep the vancomycin unchanged
D. Increase the vancomycin dose; keep the gentamicin unchanged
E. Increase the gentamicin dose; keep the vancomycin unchanged and decrease the interval between
the gentamicin doses.
49. A 78-year-old man is admitted to the intensive care unit because of severe congestive heart failure
that requires monitoring with a central venous catheter. After 2 days, he develops diaphoresis,
tachycardia, and a temperature of 39.5 °C (103.1 В°F). A small amount of purulent material is noted at
the catheter site. The catheter is removed, blood culture specimens are drawn, and empiric vancomycin is
begun. The patient improves, but the catheter tip and both sets of blood cultures grow Staphylococcus
aureus that is reported to be sensitive to oxacillin. Vancomycin is changed to nafcillin, 2 g intravenously
every 4 hours. No signs of endocarditis are noted on physical examination, and repeat blood cultures
show no growth. On hospital day 7, the patient appears ready for discharge, based on cardiac and
hemodynamic parameters. Which of the following is the most appropriate management at this time?
A. *Obtain a transesophageal echocardiogram; if this does not show signs of endocarditis, continue the
intravenous nafcillin for a total of 14 days
B. No additional diagnostic studies are needed; stop the intravenous nafcillin
C. No additional diagnostic studies are needed; continue the intravenous nafcillin for a total of 8
weeks
D. No additional diagnostic studies are needed; substitute oral dicloxacillin for the intravenous
nafcillin for a total of 10 days of antibiotics
E. Obtain a transesophageal echocardiogram; if this does not show signs of endocarditis, continue the
intravenous nafcillin for a total of 6 weeks
50. A 30-year-old IV drug user presents complaining of fevers, hemoptysis, and pleuritic chest pain
over the preceding 2 weeks. Despite 2 weeks of appropriate antibiotic therapy, he continues to have
intermittent fevers and has developed a grade 2/6 pansystolic murmur along his left sternal border as well
as a first-degree AV block on his ECG. His repeat blood cultures remain positive for S. aureus. Which
diagnostic test is most appropriate at this time?
A. *TEE
B. Electrophysiologic study
C. TTE
D. Bronchoscopy
E. Cardiac catheterization
51. A 40-year-old man complaining of fevers, hemoptysis, and pleuritic chest pain over the preceding
2 weeks. On physical examination, his temperature is 38.2°C, pulse rate is 100/min, and BP is 110/60.
His LV impulse is normal and no murmurs are appreciated on cardiac auscultation. His lungs are clear to
auscultation. Echocardiography shows a tricuspid valve vegetation with trace tricuspid regurgitation.
What is the most likely diagnosis?
A. *Infective endocarditis
B. Pneumonia
C. Viral syndrome
D. Pericarditis
E. Congenital cardiac shunt
52. A 44-year-old man with a history of a bicuspid AV is diagnosed with endocarditis. Despite 2 weeks
of appropriate antibiotic therapy, he has persistent fevers and bacteremia. A diagnostic study is
performed and a paravalvular abscess discovered. What is the next step in this patient's management?
A. Add gentamicin
B. *Refer for surgery
C. Continue current antibiotic therapy
D. Change nafcillin to ceftriaxone
E. Change nafcillin to vancomycin
53. Two years after undergoing mitral valve replacement, a 48-year-old man has a cerebrovascular
accident. Except for fever, general physical examination is noncontributory. A transesophageal
echocardiogram shows an oscillating mass on the mitral valve but no evidence of perivalvular extension
or abscess. Six sets of blood cultures grow Enterococcus faecalis, which is resistant to penicillin and
ampicillin but sensitive to vancomycin. A decision is made to treat medically, and the patient is begun on
vancomycin, 1 g intravenously every 12 hours, and gentamicin, 80mg intravenously every 8 hours. The
technician notes that the vancomycin peak and trough levels and the gentamicin trough level are in the
desirable range but that the laboratory’s therapeutic peak range for gentamicin is 4 to 8 μg/mL.
Repeat blood cultures show no growth, and complete blood count and serum creatinine values are
normal.
A. *Keep both the gentamicin and the vancomycin doses unchanged
B. Increase the gentamicin dose; keep the vancomycin unchanged
C. Decrease the interval between the gentamicin doses; keep the vancomycin unchanged
D. Increase the vancomycin dose; keep the gentamicin unchanged
E. Increase the gentamicin dose; keep the vancomycin unchanged and decrease the interval between
the gentamicin doses.
54. A 46-year-old woman with rheumatoid arthritis is evaluated because the subcutaneous nodules that
were present on her elbows have increased in size, and she has developed some nodules on the Achilles
tendons bilaterally. She has been treated for 8 months with methotrexate in an ascending dose schedule.
She is currently taking 17.5 mg/week, along with enteric-coated aspirin, 3 g/d. This regimen has
alleviated her joint pain; her morning stiffness is limited to 35 minutes, as opposed to the previous
duration of 2 hours. On examination the nodules are not warm, and her joints appear much improved. No
other physical abnormalities are found. Which of the following is the most appropriate next step in this
patients management?
A. Biopsy a newly developed nodule.
B. *Reassure the patient that these nodules occur occasionally with methotrexate therapy.
C. Initiate antituberculosis therapy.
D. Measure fasting serum lipids, including triglycerides.
E. Measure serum uric acid.
55. A 77-yr-old woman with long-standing rheumatoid arthritis presented with fever and dysuria. Her
past history included recurrent chest and urinary infections. On examination she was hyperpigmented and
emaciated. Her hands and feet were severely deformed. Abdominal examination revealed splenomegaly
but no hepatomegaly or lymphadenopathy. Choose the most likely diagnosis from the below list of
options.
A. Gout
B. Still's disease
C. *Felty's syndrome
D. Rheumatoid arthritis
E. Osteoarthritis
56. A 39-year-old woman with a 3-year history of rheumatoid arthritis is evaluated because of slight
shortness of breath of new onset when she climbs the stairs in her home. She also has a dry hacking
cough of 3 weeks duration. She has been active, working part-time as a secretary as well as caring for
two young children at home. She has been taking methotrexate, 20 mg by mouth each week, and folic
acid, 1 mg/d, for 1 year, and she says her joints have been great. On physical examination, her
temperature is 37.7 °C (99.8 °F). Fine crackles are audible at the bases of both lungs on deep inspiration.
There is some tenderness with full palmar flexion and dorsi flexion of the right wrist; the rest of the joints
are brought through full range of painless motion. Complete blood count and serum albumin levels are
normal. Chest radiograph is normal. Which of the following is the best next step in this patient
management?
A. Order liver biopsy.
B. Obtain radiographs of wrists.
C. *Stop the methotrexate.
D. Chest X-ray
E. Initiate prednisone therapy.
57. A 50-year-old woman presents with a 2-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. The patient hemoglobin is 10 g/dL,
erythrocyte sedimentation rate is 50 mm/h, and serum rheumatoid factor positive. Choose the most likely
diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Rheumatoid arthritis
C. Osteoarthritis
D. Gout
E. Psoriatic arthritis
58. A 63-year-old woman with a history of rheumatoid arthritis since age 42 is seen for the first time by
a new physician. The patient has been doing poorly of late. Though her joint disease has not been a
problem, she has lost weight and has been plagued by chronic foul smelling diarrhea, easy bruising,
profound fatigue, and peripheral edema. On examination she has waxy skin plaques clustered in the
axillary folds, a large tongue, a quiet precordium, hepatosplenomegaly, guaiac-positive stool, and
peripheral neuropathy. Laboratory evaluation includes the findings of proteinuria (5 g/d), normal serum
chemistry except slightly low albumin and slightly elevated alkaline phosphatase, and low-voltage QRS
complexes on electrocardiography. In order to expeditiously diagnose the problem, one could
A. perform a bone marrow aspirate and biopsy
B. obtain three serial sputum samples for acid-fast bacillus (AFB) culture
C. perform an abdominal CT examination
D. perform joints X-ray
E. *perform a rectal biopsy
59. A 45-year-old woman presents with a 2-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. The patient has hemoglobin is 10 g/dL,
erythrocyte sedimentation rate is 50 mm/h, and serum rheumatoid factor positive. Choose the most likely
diagnosis from the below list of options. Which of the following systemic manifestations is LEAST
characteristic of early adult rheumatoid arthritis?
A. Vague musculoskeletal symptoms
B. Fatigue
C. *High fever
D. Weight loss
E. Muscle wasting
60. A 45-year-old man presents because of a painful, swollen knee and ankle of 2 weeks' duration. He
has never had joint disease prior to this time. The patient also complains of low back pain and a recent
history of clear penile discharge. On examination he has vesicles (some of which have crusted over) on
the palms, soles, and glans penis; injected conjunctivae; a swollen right index finger; and arthritis of the
right knee and left ankle. Correct statements regarding this patient include all of the following EXCEPT
A. he is probably HLA-B27-positive
B. *his joint disease will probably improve after a course of benzylpenicilline
C. he will probably benefit from indomethacin
D. may be seen as late sequelae his erythrocyte sedimentation rate is likely to be elevated
E. Sacroiliitis and spondyloarthropathy
61. A 34-year-old woman presents with a 23-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. Which one of the following statements
about rheumatoid arthritis is true?
A. *Serum C-reactive protein measurement is a useful measure of joint inflammation
B. Most patients progress to complete disability
C. Oral corticosteroids form the mainstay of drug therapy
D. Epstein-Barr virus is known to be the causative agent.
E. Always responds to plasma exchange therapy
62. A 25-year- woman develops acute abdominal pain and bloody diarrhea. Several weeks later, she
complains of diffuse musculoskeletal pain involving the neck, left wrist, left knee, and low back. On
examination she has marked swelling, warmth, and loss of motion of the left wrist and left knee, as well
as pain and restricted motion of the neck and lower lumbar spine. Choose the most likely diagnosis from
the below list of options.
A. *Reactive arthritis
B. Rheumatoid arthritis
C. Haemochromatosis
D. Osteoarthritis
E. Gonococcal arthritis
63. A 31-yr-old male presented to A&E with a markedly swollen and tender left knee. He says it's
been present for about a month but has only recently become painful. He admitted losing weight and on
examination a temperature of 39,5 °C was found. He had no other complaints apart from a 2-month
history of cough, which he attributed to his heavy smoking. Choose the most likely diagnosis from the
below list of options.
A. *Reiter's syndrome
B. Felty's syndrome
C. Osteoarthritis
D. Infective arthritis
E. Rheumatoid arthritis
64. A 42-year-old woman presents with a 2-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. The patient has hemoglobin is 10 g/dL,
erythrocyte sedimentation rate is 50 mm/h, and serum rheumatoid factor positive. Choose the most likely
diagnosis from the below list of options. Which of the following tests is most likely to yield the
diagnosis?
A. Pelvic examination and cervical culture
B. Joint fluid aspiration
C. Antinuclear antibody (ANA) testing
D. *Rheumatoid factor testing
E. Streptococcal enzyme testing
65. A 38-year-old woman presents with a 24-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. X-ray findings of Rheumatoid arthritis
are all of the following except:
A. juxtra-articular osteoporosis;
B. enlarged of joint space;
C. *erosions at the margins of joints;
D. osteophytes;
E. ankylosis and subluxations.
66. A 28-year-old woman presents with a 18-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. . Which of the following conditions is
LEAST likely to occur in late extraarticular seropositive rheumatoid arthritis?
A. Neutropenia
B. Dry eyes
C. Leg ulcers
D. Sensorimotor polyneuropathy
E. *Hepatitis
67. A 28-year-old woman presents with a 12-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 37.8 °C. Examination of the joints reveals thickening and tenderness of
the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists lack complete
flexion and extension and are warm to the touch. Choose the most likely diagnostic antibody for the
disease from the below list of options.
A. Antimicrosomal antibody
B. Antireticulin antibody
C. Anti-dsDNA
D. P-ANCA antibody
E. *Rheumatoid factor
68. A 37-year-old woman presents with a 6-month history of morning stiffness, pain, and swelling in
her hands and wrists. She has noticed general fatigue, and the hand stiffness lasts about an hour. Joints of
all her extremities are involved symmetrically. The patient does not smoke or drink. On physical
examination, her temperature is 38 °C (100.4 °F). Examination of the joints reveals thickening and
tenderness of the metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists
lack complete flexion and extension and are warm to the touch. X-ray examination of which joints you
need for confirming diagnosis?
A. *Hands
B. Ankles
C. Knees
D. Elbows
E. Spine
69. A 33-yr-old woman has pain and stiffness in her hands, wrists, elbows, knees and ankles. There is
swelling of her MCP joints bilaterally. The patient does not smoke or drink. On physical examination,
her temperature is 37.8 °C. Examination of the joints reveals thickening and tenderness of the
metacarpophalangeal joints and proximal interphalangeal joints bilaterally. Both wrists lack complete
flexion and extension and are warm to the touch. Choose the most likely diagnosis from the below list of
options
A. High ESR
B. High serum urate
C. Positive blood culture
D. *Positive rheumatoid factor
E. High WBC count
70. A 30-yr-old woman has pain and stiffness in her hands, wrists, elbows, knees and ankles. There is
swelling of her MCP joints bilaterally. On physical examination, her temperature is 38 °C (100.4 °F).
Examination of the joints reveals thickening and tenderness of the metacarpophalangeal joints and
proximal interphalangeal joints bilaterally. Both wrists lack complete flexion and extension and are warm
to the touch. Choose the most likely diagnostic antibody for Rheumatoid arthritis from the below list of
options.
A. Antimicrosomal antibody
B. Antireticulin antibody
C. Anti-dsDNA
D. P-ANCA antibody
E. *Rheumatoid factor
71. A 73-yr-old fit farmer presents with pain on weight bearing and restricted movements of the right
hip. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
72. An elderly man started frusemide 2-weeks ago and now presents with a red, hot, swollen first
metatarsal phalangeal joint. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Joint sepsis
C. Osteoarthritis
D. *Gout
E. Psoriatic arthritis
73. A 41-yr-old woman has pain and stiffness in her hands, wrists, elbows, knees and ankles. There is
swelling of her MCP joints bilaterally. On physical examination, her temperature is 38 °C (100.4 °F).
Examination of the joints reveals thickening and tenderness of the metacarpophalangeal joints and
proximal interphalangeal joints bilaterally. Both wrists lack complete flexion and extension and are warm
to the touch. Choose the most likely diagnosis from the below list of options. Drug of choice for patient
with rheumatoid artritis
A. *Methotrexate
B. NSAIDs
C. Hydroxychloroquine sulphate
D. Sulphasalazine
E. D-penicillamine
74. A 53-yr-old woman complains of redness, swelling and stiffness in the distal interphalangeal joints
of her hands, but has no other joint complaints. Choose the most likely diagnosis from the below list of
options.
A. Gout
B. Still's disease
C. Pseudogout
D. Rheumatoid arthritis
E. *Osteoarthritis
75. A 50-yr-old woman complains of stiffness in her fingers worse at the end of the day. The DIP joints
and the first metacarpophalangeal joints are affected. Choose the most likely diagnosis from the below
list of options.
A. *Osteoarthritis
B. Rheumatoid arthritis
C. Psoriatic arthropathy
D. Haemochromatosis
E. Gonococcal arthritis
76. A 70-yr-old woman complains of arthritis in the fingers and big toe. On examination she has bony
swellings of the first carpometacarpal joint and the distal interphalangeal joints and has an affected
metatarsophalangeal joint. Choose the most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Hyperparathyroidism
C. Psoriatic arthropathy
D. *Osteoarthritis
E. Haemochromatosis
77. An elderly man presents with a red, warm swollen metatarsophalangeal joint following a right total
hip replacement operation. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Reactive arthritis
C. Osteoarthritis
D. *Acute Gouty arthritis
E. Psoriatic arthritis
78. A 60-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint and a lesion
on the rim of the left pinna. Choose the investigation for diagnosis from the below list of options.
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
79. A 65-yr-old man has started chemotherapy for lymphoma. He has developed a painful swollen hot
right knee. He is apyrexial. Choose the most likely changes from the below list of options.
A. *High ESR
B. Erosions on X-ray
C. Positive blood culture
D. Positive rheumatoid factor
E. Urate crystals on joint aspirate
80. A 50-year-old male is evaluated because of pain in the right inguinal area, lower back, and hands.
The inguinal pain worsens as he walks, and all pain increases as the day progresses. On physical
examination, internal rotation of the right hip elicits the groin pain. The second, third, and fourth
metacarpophalangeal joints are swollen, warm, and tender to pressure. Radiographs show severe
osteoarthritis in the right hip. Which of the following is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. *Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. Serum uric acid
81. A 67-year-old woman has had four or five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. She is asymptomatic between attacks, and sulindac, 200 mg
twice daily, has usually relieved the symptoms. Her most recent episode was 3 months ago. On physical
examination, none of her joints is swollen or tender, but there is marked crepitus on extension of the
knee. She also has a positive bulge sign over the left knee and pain on full extension of the left elbow.
Which one of the following tests would confirm the diagnosis?
A. *Arthrocentesis of the knee and laboratory analysis of the synovial fluid
B. Measurement of serum uric acid
C. Measurement of serum rheumatoid factor
D. Radiograph of the knee
E. MRI of the knee with gadolinium contrast
82. A 72-year-old retired lawyer is evaluated because of swelling of his right knee. He has mild
osteoarthritis and stays active swimming and playing tennis and golf. On physical examination, he has an
effusion in the right knee. At a point in the mid-thigh (measured from the superior border of the patella),
the right thigh is 4 cm smaller in diameter than the left. There is crepitus with right knee flexion. The
knee is not warm. Which of the following is the best next step in the management of this patient?
A. Order radiographs of both knees and treat the patient with ibuprofen.
B. Order radiographs of the right hip and right knee.
C. *Aspirate the joint fluid in the right knee and refer the patient for physical therapy.
D. Aspirate the joint fluid in the right knee and obtain blood cultures.
E. Treat the patient with celecoxib, and advise him to stay off his feet for 48 hours.
83. A 64-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. The
patient says that her mother had “the same fingers” and she worries that she will become crippled.
Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
84. A 65-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. On
physical examination, there is crepitus on passive motion of the left knee, which has a slight varus (“bow
leg”) deformity. Her feet turn out slightly, and the heels are in valgus. Which of the following changes
will reveal X-ray examination?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
85. A 73-yr-old fit farmer presents with pain on weight bearing and restricted movements of the right
hip. Choose the most likely X-ray changes from the below List of options.
A. Cystic changes and lytic lesions
B. *Joint spaces are narrowed with reactive subchondral sclerosis, osteophytes
C. Periarticular osteopenia, marginal erosions
D. acroosteolysis
E. Fluffy bone periostitis and erosions at the interphalangeal joints
86. A 60-year-old woman is evaluated because of a 1-year history of bilateral knee pain and low back
pain. She has some stiffness for approximately 15 minutes when she awakens in the morning, and during
the afternoon her pain is worse. As she describes her pain, she slides her hand down the anterior thigh to
her knee on the right to show where the pain is most severe. On physical examination, she has slight
swelling and tenderness to pressure of the distal interphalangeal joints 2-5 on both hands. All the joints
are brought through full range of motion without pain. There is slight crepitus with motion of the right
knee. Which of the following treatment do use?
A. methotrexat
B. *intra-articular injection of sodium hyaluronate
C. probenecid
D. colchicine
E. allopurinol.
87. A 68-year-old woman has had four or five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. She is asymptomatic between attacks, and sulindac, 200 mg
twice daily, has usually relieved the symptoms. Her most recent episode was 4 months ago. On physical
examination, none of her joints is swollen or tender, but there is marked crepitus on extension of the
knee. She also has a positive bulge sign over the left knee and pain on full extension of the left elbow.
Which one of the following tests would confirm the diagnosis?
A. Measurement of uric acid
B. *Arthrocentesis of the knee and laboratory analysis of the synovial fluid
C. Measurement of serum rheumatoid factor
D. Radiograph of the knee
E. MRI of the knee with gadolinium contrast
88. A 51-yr-old woman complains of stiffness in her fingers worse at the end of the day. The DIP joints
and the first metacarpophalangeal joints are affected. Choose the most likely diagnosis from the below
list of options.
A. Rheumatoid arthritis
B. Psoriatic arthropathy
C. *Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
89. A 65-yr-old man has started chemotherapy for lymphoma. He has developed a painful swollen hot
right knee. He is apyrexial. Choose the most likely diagnosis from the below list of options.
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
90. A 57-year-old woman has had five episodes of joint pain and swelling, lasting 3 to 8 days,
involving the right knee and left elbow. She is asymptomatic between attacks, and sulindac, 200 mg
twice daily, has usually relieved the symptoms. Her most recent episode was 4 months ago. Classical
picture of exacerbation of the arthritis includes all of the following except
A. Excruciating and sudden pain
B. Low-grade fever may also be present
C. Overgrowth at the distal interphalangeal joints
D. *Warmness
E. Redness
91. A 55-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 3 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following changes
will reveal X-ray examination?
A. Erosions
B. Subluxations
C. Osteophytes
D. Osteoporosis
E. *"punched-out" lytic lesion
92. A 59-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 2 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following is
characteristic of the arthritis?
A. *Depositions of monosodium urate monohydrate crystals within the periarticular soft tissues
B. Overgrowth of bones within joints
C. Autoimmune synovitis
D. Osteoporosis
E. Rheumatoid nodules over joints
93. A 60-year-old man presented to the clinic with a nodule on his elbow. He reported that the nodule
had been bothering him for 4 years and had steadily increased in size recently. Further questioning
revealed a history of repeated attacks of acute joint pain. The physical examination revealed a rounded,
subcutaneous nodule over the elbow, which was tender and rubbery to the touch. The examination was
also notable for a subcutaneous nodule at the left metatarsal-phalangeal joint and left metacarpalphalangeal joint, as well as evidence of arthritis involving both hands. Which of the following
medications is indicated for the treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
94. 79 y/o male with foot pain and swelling for many years. There are "punched out" articular erosions
with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly elevated.
Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. Osteoarthritis
D. *Chronic Gouty arthritis
E. Psoriatic arthritis
95. 53-year-old male with foot pain and swelling for many years. There are "punched out" articular
erosions with overhanging cortex and associated soft tissue masses consistent with tophaceous gout and
gouty arthritis. Choose the most likely changes from the below list of options.
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
96. 59 y/o male with foot pain and swelling for many years. There are "punched out" articular erosions
with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly elevated.
Which of the following medications is indicated for the treatment of chronic arthritis?
A. *allopurinol
B. colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
97. 49 y/o male with foot pain and swelling for many years. There are "punched out" articular erosions
with overhanging cortex and associated soft tissue masses. Serum uric acid was markedly elevated.
Which of the following medications is indicated for the treatment of exacerbation of arthritis?
A. allopurinol
B. *colchicine
C. corticosteroids
D. indomethacin
E. ibuprofen
98. 55 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. *Chronic Gouty arthritis
C. Rheumatoid arthritis
D. Osteoarthritis
E. Psoriatic arthritis
99. 57 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is indicated for the treatment
of chronic arthritis?
A. colchicine
B. corticosteroids
C. indomethacin
D. *allopurinol
E. ibuprofen
100. 28-year-old patient, presents with complaints of tightness of fingers. There is also history of
dysphagia. Which of the following is the probable diagnosis:
A. Dermatomyositis
B. *Scleroderma
C. Rheumatoid arthritis
D. Polyarteritis nodosa
E. SLE
101. 59 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is indicated for the treatment
of exacerbation of arthritis?
A. allopurinol
B. corticosteroids
C. *colchicine
D. indomethacin
E. ibuprofen
102. 57 yo male with swelling and pain of his fingers. Patient also with similar complaints regarding his
great toe of the left foot. Soft tissue swelling with subtle soft tissue nodules primarily of the 2nd and 3rd
digits. Erosions with overhanging edges at the distal aspects of the proximal phalanges of the 2nd and 3rd
digits and metatarsophalangeal joints. Which of the following medications is contraindicated for the
treatment of exacerbation of arthritis?
A. corticosteroids
B. colchicine
C. indomethacin
D. ibuprofen
E. *allopurinol
103. A 32-year-old woman is evaluated because of a 5-year history of Raynaud’s phenomenon and
thickened skin over the fingers, small patches of calcinosis on the distal fingers and dorsum of one hand.
She reports mild dyspnea when she climbs stairs. She takes a proton pump inhibitor for reflux
esophagitis. Physical examination reveals sclerodactyly, with one digital tip ulcer, minimal calcinosis.
Lung and heart examination, and radiograph are normal. Results of routine laboratory tests are normal,
including renal function. Echocardiogram suggests mild right ventricular diastolic dysfunction. The
diffusing capacity for carbon monoxide (DLCO) is 44% of normal. Within the next 5 years, she is at high
risk for developing which of the following?
A. Fine, dry crackles indicative of pulmonary fibrosis
B. Renovascular hypertension with hyperreninemia
C. Sclerodermatous changes on the forearms and face
D. *Pulmonary hypertension
E. Esophageal varices
104. A 35-year-old woman is evaluated because of a 5-year history of Raynaud’s phenomenon and
thickened skin over the fingers, small patches of calcinosis on the distal fingers and dorsum of one hand.
She reports mild dyspnea when she climbs stairs. She takes a proton pump inhibitor for reflux
esophagitis. Physical examination reveals sclerodactyly, with one digital tip ulcer, minimal calcinosis,
and two telangiectasias on her face. Which of the following is the probable diagnosis:
A. Dermatomyositis
B. *Scleroderma
C. Rheumatoid arthritis
D. Polyarteritis nodosa
E. SLE
105. A 23-year old woman has experienced episodes of myalgias, erythema on the cheeks, pleural
effusion, pericarditis and arthralgias without joint deformity over course of several years. The best
laboratory screening test to diagnose her disease would be:
A. CD4 lymphocyte count
B. Erythrocyte sedimentation rate
C. *Antinuclear antibody
D. Assay for thyroid hormones
E. Leucocytosis
106. A 28-year old woman has experienced episodes of myalgias, erythema on the cheeks, pleural
effusion, pericarditis and arthralgias without joint deformity over course of several years. Which of the
following is the probable diagnosis:
A. Dermatomyositis
B. Scleroderma
C. Rheumatoid arthritis
D. Polyarteritis nodosa
E. *SLE
107. A 25-year-old woman is evaluated because of a 3-month history of progressive dyspnea and the
development of a dry hacking cough. She has Raynaud’s disease and polymyositis, which have
responded to treatment with prednisone and methotrexate. On physical examination, the patient is
afebrile, with bibasilar crackles in her chest. A chest radiograph shows diffuse reticulonodular changes,
predominantly in the lung bases.
Which of the following diagnoses is most likely?
A. Aspiration due to pharyngeal or esophageal dysfunction
B. *Interstitial lung disease
C. Pneumonitis due to Pneumocystis carinii
D. Methotrexate-induced lung disease
E. Bronchiolitis with organizing pneumonia
108. 108. A 34-year-old woman has a 4-month history of arthralgia of knees, elbows, and hands and
swelling of the lower extremities. She has noted increased fatigue. Her only pregnancy, which occurred 1
year ago, ended in a spontaneous abortion at 4 months of gestation. Temperature 37.1 °C (98.8 °F). A
malar rash is present on the skin. The lungs are clear, and the heart is in regular sinus rhythm, with no
murmur or rub. The patient has 2+ pitting edema below the knees. She has no swelling or redness of the
joints. Laboratory studies: Serum creatinine
1.9 mg/dL, Serum antinuclear antibodies <1.5, Antidouble-stranded DNA antibodies Positive. Which of the following is the probable diagnosis:
A. Dermatomyositis
B. Scleroderma
C. Rheumatoid arthritis
D. Polyarteritis nodosa
E. *SLE
109. A 28-year-old black woman has a 2-month history of arthralgia of knees, elbows, and hands and
swelling of the lower extremities. She has noted increased fatigue. Her only pregnancy, which occurred 1
year ago, ended in a spontaneous abortion at 4 months of gestation. Temperature 37.1 °C (98.8 °F). A
malar rash is present on the skin. The lungs are clear, and the heart is in regular sinus rhythm, with no
murmur or rub. The patient has 2+ pitting edema below the knees. She has no swelling or redness of the
joints. Laboratory studies: Serum creatinine
1.9 mg/dL, Serum antinuclear antibodies <1.5, Antidouble-stranded DNA antibodies Positive, 24-hour urine protein
4.6 g, Urinalysis pH 6.0; specific
gravity 1.010; 4+ proteinuria, 4+ hemoglobinuria, Urine microscopy shows many granular and
erythrocyte casts, dysmorphic erythrocytes, and one mixed-cell cast. What is the most likely diagnosis?
A. Post-streptococcal glomerulonephritis
B. *Diffuse lupus nephritis (World Health Organization type IV)
C. Focal proliferative lupus nephritis (World Health Organization type II)
D. Polyarteritis nodosa
E. Rheumatoid arthritis with renal involvement
110. A 46-year-old man is evaluated because of ankle edema and exertional dyspnea without angina. For
several years, he has had fatigue, dysphagia with symptomatic gastroesophageal reflux, and pain with
blanching in his fingers while shoveling snow. On physical examination, he has perioral skin tightening,
numerous telangiectasias on both sun-exposed and protected surfaces, and ‘sausage shaped” fingers
without digital ulcerations. His lungs are clear. On cardiac examination, he has a right parasternal lift
with a loud pulmonic valve component. The S2 does not split on inspiration. He has pitting edema to the
mid-shin bilaterally and 8 cm of jugular venous distention while seated at 45 degrees from horizontal.
Both the right atrium and right ventricle are dilated with moderate tricuspid regurgitation on transthoracic
echocardiogram. Pulmonary artery pressure is estimated to be 52 mm Hg by echocardiography. Which of
the following statements is true about patients with these symptoms?
A. *Pulmonary hypertension is a frequent cause of death.
B. Pulmonary hypertension indicates an overlap syndrome.
C. Pulmonary hypertension occurs only in the setting of an associated interstitial lung disease.
D. Recurrent venous thromboembolism due to an associated hypercoagulable state is the usual cause
of pulmonary hypertension.
E. None of the above
111. A 26-year-old woman with systemic lupus erythematosus (SLE) is noted to have a prolonged
partial thromboplastin time. This abnormality is associated with
A. leukopenia
B. drug-induced lupus
C. central nervous system vasculitis
D. central nervous system hemorrhage
E. *deep venous thrombosis
112. A patient with diffuse cutaneous scleroderma (systemic sclerosis) who had been stable for several
years is recently noted to have hypertension. This patient is at significant risk of dying from
A. thrombotic stroke
B. central nervous system hemorrhage
C. *renal failure
D. pulmonary hypertension
E. pulmonary fibrosis
113. A 52-year-old woman is evaluated because of transient numbness on the right side of her face and
blurred vision lasting up to 24 hours. The patient has a history of migraine headache, but her current
symptoms are distinct from those associated with her usual migraines. Physical examination is
unremarkable except for livedo reticularis, which she has had for the past decade. Neurologic
examination is within normal limits. Results of MRI of the head, transesophageal echocardiography, and
carotid ultrasound examination and complete blood count and serum chemistry studies are all within
normal limits. The prothrombin time is within normal limits, but the partial thromboplastin time is 55 s
(normal limit as high as 34 s). Results of a lupus anticoagulant panel are positive. The cardiolipin IgG is
elevated at 50 GPL U/mL (reference range <16 GPL U/mL); 1gM antibody level is normal.
Which of the following is the best therapy for this patient?
A. Aspirin, 325 mg/d
B. Warfarin, with a target INR of 2 to 3, and aspirin, 81 mg/d
C. *Warfarin, with a target INR of 3 to 4
D. Aspirin, 325 mg/d, and clopidogrel
E. Continue medications that she takes for her migraine headaches
114. A 50-year-old woman has had Raynaud's phenomenon of the hands for 15 years. The condition has
become worse during the last year, and she has developed arthralgias and arthritis involving the hands
and wrists as well as mild sclerodactyly and difficulty swallowing solid foods. Laboratory studies reveal
a positive serum antinuclear antibody assay at a dilution of 1:160. Anticentromere antibodies are present
in high titers; antiribonucleoprotein antibodies are not detectable. The most likely diagnosis of this
woman's disorder is
A. *systemic sclerosis
B. mixed connective-tissue disease
C. overlap syndrome
D. dermatomyositis
E. systemic lupus erythematosus
115. A 45-year-old woman with long-standing systemic lupus erythematosus who has had intermittent
bouts of acute renal failure over the last 6 years presents with anorexia. Physical examination is
noncontributory. Laboratory evaluation includes hematocrit 29 percent, white count 5000 with a normal
differential, and platelet count 27,500/uX. Renal biopsy shows sclerosis of 14/15 glomeruli, tubular
atrophy, and interstitial fibrosis. The following values are also found: Serum electrolytes (mmol/L): K+
6; HCO3- 2 0 Serum creatinine: 665 jjumol/L (7.5 mg/dL), Anti-double-strand DNA and C3 levels have
been stable. Renal biopsy shows obliterative sclerosing glomerular lesions. The most appropriate
management strategy would be
A. high-dose intravenous methylprednisolone
B. high-dose intravenous methylprednisolone and azathioprine
C. high-dose intravenous methylprednisolone and intravenous cyclophosphamide (500 mg/m2)
D. intravenous cyclophosphamide (500 mg/m2) plus low-dose prednisone
E. *dialysis
116. A 38-yr-old man presented with progressive breathlessness, unproductive cough and difficulty in
swallowing. He also noted that his hands become painful and pale in cold weather. Chest radiographs
show patchy shadows in both midzones and bases. Radiography of hands showed calcification. Choose
the most likely diagnosis from the below list of options.
A. *CREST syndrome
B. Polymyositis
C. SLE
D. Polyarteritis nodosa
E. Sjogrens' syndrome
117. A 52-yr-old woman complains of a 8-month history of Raynaud's phenomenon, progressive skin
tightness, thickening of fingers and hands, dyspnoea on exertion and dysphagia. Choose the most likely
diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Polymyalgia rheumatica
C. SLE
D. Polyarteritis nodosa
E. *Scleroderma
118. A 36-yr-old woman complains of recurrent chest pain, which is worse on inspiration, and
progressive breathlessness. She also suffers from Raynaud's phenomenon. On examination she has a
butterfly rash and a pericardial rub is audible. Choose the most likely diagnosis from the below list of
options.
A. Sjogrens' syndrome
B. Polymyositis
C. *SLE
D. Polyarteritis nodosa
E. Giant cell arteritis
119. A 36-yr-old woman complains of recurrent chest pain, which is worse on inspiration, and
progressive breathlessness. She also suffers from Raynaud's phenomenon. On examination she has a
butterfly rash and a pericardial rub is audible. Choose the most likely diagnostic antibody from the below
list of options.
A. Antimicrosomal antibody
B. C-ANCA
C. Antiparietal cell antibody
D. *Anti-dsDNA
E. Antiacetylcholine receptor antibody
120. A 22-yr-old woman presents with a 2-month history of fever, pleuritic chest pain, stiffness and
swelling in the wrists, MCP joints and PIP joints. On examination, there is bilateral pretibial oedema.
Choose the most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Polymyalgia rheumatica
C. *SLE
D. Polyarteritis nodosa
E. Scleroderma
121. A 27-yr-old woman presents with a 3-week history of fever, pleuritic chest pain, stiffness and
swelling in the wrists, MCP joints and PIP joints. On examination, there is bilateral pretibial oedema.
Choose the most likely treatment from the below list of options.
A. Asprin
B. Indomethacin
C. Prostoglandines
D. Procainamide
E. *Steroids
122. A 42-yr-old woman complains of a 4-month history of Raynaud's phenomenon, progressive skin
tightness, thickening of fingers and hands, dyspnoea on exertion and dysphagia. Choose the most likely
treatment from the below list of options.
A. *D-penicillamine
B. Methotrexate
C. Indomethacin
D. Aspirin
E. Nifidipine
123. Woman of 35 years with Raynauds phenomenon, polyarthritis, dysphagia of 5 years and mild
sclerodactyly, blood showing Anticentromere antibody positive, the likely cause is:
A. *Scleroderma
B. Mixed connective tissue disorder
C. SLE
D. Rheumatoid arthritis
E. Polymyalgia rheumatica
124. A 25-yr-old woman presents with deep venous thrombosis in the right leg. Her past history includes
three miscarriages. Her blood tests show mild thrombocytopenia and a positive serology test for syphilis.
Choose the most likely diagnosis from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. Mixed connective tissue disorder
D. *Antiphospholipid syndrome
E. Polyarteritis nodosa
125. A 20-yr-old woman presents with a plethora of signs and symptoms. She complains of arthralgia,
depression, alopecia, fits, oral ulceration and facial rash. She is found to have proteinuria and normocytic
normochromic anaemia. Choose the most likely investigation from the above list of options.
A. *Antinuclear antibodies
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
126. A 23-yr-old woman presents with a plethora of signs and symptoms. She complains of arthralgia,
depression, alopecia, fits, oral ulceration and facial rash. She is found to have proteinuria and a
normocytic normochromic anaemia. Choose the most likely results of the investigations from the above
list of options.
A. *Anti ds-DNA antibodies
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
127. A 45-yr-old woman presents with swellings and stiffness of her fingers. On examination she has
sausage-like fingers with flexion deformities. She is noted to have a beaked nose. X-ray of her hands
reveals deposits of calcium around her fingers and lysis of the distal phalanges. Choose the most likely
diagnosis from the below list of options.
A. Takayasu's arteritis
B. Polymyalgia rheumatica
C. SLE
D. Polyarteritis nodosa
E. *Scleroderma
128. A 35-yr-old woman presents with swellings and stiffness of her fingers. On examination she has
sausage-like fingers with flexion deformities. She is noted to have a beaked nose. X-ray of her hands
reveals deposits of calcium around her fingers and lysis of the distal phalanges. Choose the most likely
results of the investigations from the below list of options.
A. * Anticentromere antibody
B. Anti dsDNA antibodies
C. ANCA
D. Antimitochondrial antibody
E. Smooth muscle antibody
129. A 40-yr-old woman presents with flexion deformities of her fingers. She has soft tissue swelling of
her digits. She also complains of difficulty swallowing and is noted to have a beaked nose and facial
telengiectasia. Choose the most likely investigation from the above list of options.
A. *Anti-scl70
B. ANCA
C. Antimitochondrial antibody
D. Antiplatelet antibody
E. Smooth muscle antibody
130. A 30-yr-old woman presents with painful digits worse in the cold and difficulty swallowing. She is
noted to have a fixed facial expression with facial telangiectasia. X-ray reveals calcium around her
fingers. Choose the most likely investigation from the above list of options.
A. Antinuclear antibody
B. ANCA
C. Antimitochondrial antibody
D. *Anticentromere antibody
E. Smooth muscle antibody
131. A 29-year-old woman is evaluated because of a year history of skin ulcers on her lower extremities,
and myalgias. The ulcers usually begin with tender, erythematous nodules that then ulcerate and are
resistant to treatment. A previous punch biopsy of the skin allegedly showed thrombotic lesions in small
blood vessels of the dermis, polymorphonuclear neutrophils infiltrate all layers of the vessel wall and
perivascular areas. The physical examination is remarkable for the ulcers, and also for a diffuse livedo
reticularis pattern of skin discoloration and wasting of the web space between the thumb and index finger
on the left hand. Her ability to grasp with that hand is minimal. She has a right foot drop. Which of the
following diagnoses is the most likely cause of this patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Takayasus arteritis
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
132. A 24-year-old graduate student has a several-week history of aching pains in knees, ankles, and
elbows and intermittent abdominal pain. Three days ago, he had two episodes of painless hematuria. He
has had an intermittent, nonpruritic rash located below the knees bilaterally. He takes acetaminophen
occasionally for the aching joints. He has no history of kidney disease or intravenous drug use. On
examination, the patient appears well, temperature is 37.2 °C (99 °F). The lungs and heart are normal. On
abdominal examination, the liver and spleen are not palpable, and no mass or tenderness is present.
Pulses in the extremities are normal and there is no edema, but the patient has a petechial macular
papular rash over the lower extremities. Laboratory studies: Leukocyte count, Hemoglobin, Hematocrit –
normal, Serum creatinine 1.1 mg/dL, Serum antinuclear antibody Negative, Urinalysis Specific gravity
1.030, pH 5.0, 1 + proteinuria, 4+ hematuria. Biopsy of skin lesion shows IgA depositio. What is the
most likely cause of renal disease in this patient?
A. Lupus nephritis
B. Acute poststreptrococcal glomerulonephritis
C. *Henoch-Schenlein purpura
D. Allergic interstitial nephritis
E. Goodpastures syndrome
133. A patient presents with melaena normal renal function, hypertension and mononeuritis multiples.
The most probable diagnosis is A. *Classical polyarteritis nodosa
B. Microscopic polyangiitis
C. Henoch-Schonlein purpura
D. Buerger's disease
E. Wegener's granulomatosis
134. Dyspnoea on exertion, abdominal pain and progressive numbness in his feet. He recently developed
mild polyarthritis in his hands. On examination there was evidence of left median nerve mononeuritis.
Chest radiography showed cardiomegaly. Choose the most likely diagnosis from the below list of
options.
A. Rheumatoid arthritis
B. Polymyalgia rheumatica
C. Polymyositis
D. *Polyarteritis nodosa
E. Scleroderma
135. A 28-yr-old man presented with fever, myalgia and abdominal pain. On examination his
temperature was 38.8°C, BP was 190/110 and pulse was 120. His abdomen was tender with guarding and
absent bowel sounds. Choose the most likely diagnosis from the below list of options.
A. Kawaski's disease
B. Giant cell arteritis
C. Microscopic polyangitis
D. Antiphospholipid syndrome
E. *Polyarteritis nodosa
136. A 40-yr-old male presents with fever, malaise, weight loss and joint pain, chest pain. Choose the
single most likely treatment from the list of options given below.
A. Tetracycline
B. Ciprofloxacin
C. Beta 2 agonist
D. *Cyclophosphamide
E. IV aminophylline
137. A 47-year-old man has had fever, weight loss, arthralgias, pleuritic chest pain, and midabdominal
pain for the last 2 months. One week ago he noticed difficulty dorsiflexing his right great toe. Blood
pressure is 150/95 mm Hg (he has always been normotensive), and laboratory studies reveal anemia of
chronic disease, high erythrocyte sedimentation rate, and polymorphonuclear leukocytosis. The chest xray is clear. The most likely diagnosis is
A. giant cell arteritis
B. allergic granulomatosis
C. Wegener's granulomatosis
D. *polyarteritis nodosa
E. hypersensitivity vasculitis
138. A 13-yr-old boy was admitted with a tender swollen left knee and a tender right elbow. His past
history included recurrent sore throats and dull abdominal pain for a few days. On examination his
temperature was 37.9°C and there was some periumbilical tenderness. Both urine and stools were
positive for blood. Choose the most likely diagnosis from the below list of options.
A. Kawaski's disease
B. *Henoch-Schonlein purpura
C. Giant cell arteritis
D. Microscopic polyangitis
E. Antiphospholipid syndrome
139. A 48-yr-old woman presents with fever, malaise, weight loss and joint pains. She has high blood
pressure and largefeet. She complains of persistent chest pain, legs paresthesia. She has purpuric rash and
skin nodules on legs. Choose the most likely diagnosis from the below list of options.
A. Hyperparathyroidism
B. *PAN
C. Systemic sclerosis
D. Henoch-Schonlein purpura
E. Diabetes mellitus
140. A 30-yr-old computer engineer with a long history of asthma and rhinitis presents with wheezing
cough and fever. A CXR shows patchy consolidation. Physical examination shows multiple tender
subcutaneous nodules and purpura. Choose the most likely diagnosis from the below list of options.
A. *Polyarteritis nodosa
B. Mitral stenosis
C. Pneumonia
D. SLE
E. Churg-Strauss syndrome
141. A 15-year-old boy presents with purpura around the buttocks and upper thighs following upper
respiratory tract infection. He also complains of arthralgia and abdominal pain. Choose the most likely
diagnosis from the below list of options.
A. Membranous glomerulonephritis
B. Idiopathic crescenteric GN
C. *Henoch-Schonlein purpura
D. Goodpasture's syndrome
E. Postinfectious glomerulonephritis
142. A 14-year-old boy presents with a faint leg rash, bloody diarrhoea and oliguria. Further
investigations reveal heavy proteinuria and an elevated serum IgA choose the single most likely
diagnosis from the below list of options.
A. Membranous glomerulonephritis
B. Idiopathic crescenteric GN
C. *Henoch-Schonlein purpura
D. Goodpasture's syndrome
E. Postinfectious glomerulonephritis
143. For a non-blanching maculopapular rash on flexor compartments of the lower limbs of a 15-yr-old
boy choose the single most likely diagnosis from the below list of options.
A. SLE
B. Nephroblastoma
C. Haemolytic uraemic syndrome
D. Juvenile chronic arthritis
E. *Henoch-Schonlein purpura
144. A 14-yr-old boy has haematuria, hypertension, abdominal pain and a rash is noted on the flexor
surfaces of his lower limbs. Choose the single most likely diagnosis from the list of options below
A. *Henoch-Schonlein purpura
B. Kawasaki’s disease
C. Behcet’s disease
D. Cogan’s syndrome
E. None of the above
145. A patient presents with melaena normal renal function, hypertension and mononeuritis multiples.
The most probable diagnosis is A. *Classical polyarteritis nodosa
B. Microscopic polyangiitis
C. Henoch-Schonlein purpura
D. Buerger's disease
E. Henoch-Schonlein purpura
146. A 20 year old woman presents with bilateral conductive deafness, palpable purpura on the legs and
hemoptysis. Radiograph of the chest shows a thin-walled cavity in left lower zone. Investigations reveal
total leukocyte count 12000/mm3, red cell casts in the urine and serum
creatinine 3 mg/dL. What is the most probable diagnosis?
A. Henoch-Schonlein purpura
B. *Polyarteritis nodosa
C. Wegener's granulomatosis
D. Disseminated tuberculosis
E. Behcet's syndrome
147. A 20 year old woman presents with bilateral conductive deafness, palpable purpura on the legs and
hemoptysis. Radiograph of the chest shows a thin-walled cavity in left lower zone. Investigations reveal
total leukocyte count 12000/mm3, red cell casts in the urine and serum creatinine 3 mg/dL. Choose the
single most likely treatment from the list of options given below.
A. Tetracycline, prednisone
B. Ciprofloxacin, NSAIDs
C. Beta 2 agonist, heparin
D. *Cyclophosphamide, prednisone
E. IV aminophylline
148. An 18-year-old man presents with abdominal pain, nausea, and vomiting. He also notes the onset of
a rash and painful joints. Physical examination is remarkable for the presence of palpable purpura
distributed over the buttocks and lower extremities as well as guaiac-positive stool. Laboratory
evaluation is remarkable for urinalysis that discloses mild proteinuria and red blood cell casts. Other
serum studies are normal. Skin biopsy would likely reveal
A. necrotizing angiitis
B. eosinophilic angiitis
C. *leukocytoclastic vasculitis
D. extravasated red blood cells without vasculitis
E. mast cell infiltration
149. A 35-year-old woman comes to the local health clinic because for the last 6 months she has had
recurrent urticarial lesions, which occasionally leave a residual discoloration. She also has had
arthralgias. Sedimentation rate obtained now is 85 mm/h. The procedure most likely to yield the correct
diagnosis in the case would be
A. a battery of wheal-and-flare allergy skin tests
B. measurement of total serum immunoglobulin E (IgE) concentration
C. measurement of CI esterase inhibitor activity
D. *skin biopsy
E. patch testing
150. A 48-yr-old woman presents with fever, malaise, weight loss and joint pains. She has high blood
pressure and large feet. She complains of persistent chest pain. She has purpuric rash and skin nodules.
A. Acromegaly
B. *Polyarteritis nodosa
C. Systemic sclerosis
D. Herpes
E. leukocytoclastic vasculitis
151. A 30-yr-old computer engineer with malaise, fever, and weight loss. Physical examination shows
multiple tender subcutaneous nodules and livedo reticularis, peripheral neuropathy.
A. *Polyarteritis nodosa
B. leukocytoclastic vasculitis
C. Henoch-Schonlein purpura
D. Microscopic polyangiitis
E. Churg Strauss syndrome
152. A 32-year-old woman is evaluated because of a year history of skin ulcers on her lower extremities,
and myalgias. The ulcers usually begin with tender, erythematous nodules that then ulcerate and are
resistant to treatment. Two ulcers (one on each leg, just superior to the medial malleolus) have been as
large as 5 or 6 cm in diameter. A previous punch biopsy of the skin allegedly showed thrombotic lesions
in small blood vessels of the dermis, polymorphonuclear neutrophils infiltrate all layers of the vessel wall
and perivascular areas. The physical examination is remarkable for the ulcers, and also for a diffuse
livedo reticularis pattern of skin discoloration and wasting of the web space between the thumb and index
finger on the left hand. Her ability to grasp with that hand is minimal. She has a right foot drop. Choose
the single most likely treatment from the list of options given below.
A. Tetracycline, prednisone
B. Ciprofloxacin, NSAIDs
C. Beta 2 agonist, heparin
D. *Cyclophosphamide, prednisone
E. IV aminophylline
153. A 54-yr-old man presented with a 5-month history of fatigue, abdominal pain and progressive
numbness in his feet. He recently developed mild polyarthritis in his hands. On examination there was
evidence of left median nerve mononeuritis, livedo reticularis, BP 160/110 mmHg (he has always been
normotensive), and laboratory studies reveal anemia of chronic disease, high erythrocyte sedimentation
rate. Chest radiography showed cardiomegaly.
A. Rheumatoid arthritis
B. SLE
C. Antiphospholipid syndrome
D. Henoch-Schonlein purpura
E. *Polyarteritis nodosa
154. A 28-yr-old man presented with fever, myalgia and abdominal pain and progressive numbness in
his feet. On examination his temperature was 38.8°C, BP was 190/110 and pulse was 120. His abdomen
was tender with guarding and absent bowel sounds. Choose the single most likely treatment from the list
of options given below.
A. Tetracycline, prednisone
B. Ciprofloxacin, NSAIDs
C. Beta 2 agonist, heparin
D. *Cyclophosphamide, prednisone
E. IV aminophylline
155. A 33-year-old man is evaluated because of 4-year history of skin ulcers on his lower extremities.
The ulcers usually begin with tender, erythematous nodules that then ulcerate and are resistant to
treatment. A previous punch biopsy of the skin allegedly showed thrombotic lesions in small blood
vessels of the dermis, polymorphonuclear neutrophils infiltrate all layers of the vessel wall and
perivascular areas. The physical examination is remarkable for the ulcers, and also for a diffuse livedo
reticularis pattern of skin discoloration and wasting of the web space between the thumb and index finger
on the left hand. His ability to grasp with that hand is minimal. He has a right foot drop. Choose the
single most likely treatment from the list of options given below.
A. Tetracycline, prednisone
B. *Prednisone
C. Ciprofloxacin, NSAIDs
D. Beta 2 agonist, heparin
E. IV aminophylline
156. A 47-yr-old man presented with a 7-month history of fatigue, abdominal pain and progressive
numbness in his feet. He recently developed moderate polyarthritis. On examination there was evidence
of left median nerve mononeuritis, livedo reticularis, BP 160/110 mmHg (he has always been
normotensive), and laboratory studies reveal anemia of chronic disease, high erythrocyte sedimentation
rate. Urine analysis reveals proteinuria, erythrocyturia. Chest radiography showed cardiomegaly. Choose
the single most likely treatment from the list of options given below.
A. Tetracycline, prednisone
B. *Prednisone
C. Ciprofloxacin, NSAIDs
D. Beta 2 agonist, heparin
E. IV aminophylline
157. A 44-yr-old man presented with a 2-month history of fatigue, abdominal pain and progressive
numbness in his feet. He recently developed moderate polyarthritis. On examination there was evidence
of left median nerve mononeuritis, livedo reticularis, BP 160/110 mmHg (he has always been
normotensive), and laboratory studies reveal anemia of chronic disease, erythrocyte sedimentation rate –
47 mm/h. Choose the single most likely treatment from the list of options given below.
A. Prednisone 20 mg/d
B. Prednisone 15 mg/d
C. Ciprofloxacin, NSAIDs
A. *Prednisone 1 mg/kg/d
D. Tetracycline, prednisone
158. A 18-year-old student has a several-days history of aching pains in knees, ankles, and intermittent
abdominal pain. Three days ago, he had two episodes of painless hematuria. He has had an intermittent,
nonpruritic rash located below the knees bilaterally. He has no history of kidney disease or intravenous
drug use. On examination, the patient appears well, temperature is 37.2 °C (99 °F). The lungs and heart
are normal. On abdominal examination, the liver and spleen are not palpable, and no mass or tenderness
is present. Pulses in the extremities are normal and there is no edema, but the patient has a petechial
macular papular rash over the lower extremities. Laboratory studies: Leukocyte count, Hemoglobin,
Hematocrit – normal, Serum antinuclear antibody Negative, Urinalysis Specific gravity 1.030, pH 5.0, 4+
hematuria, Biopsy of skin lesion shows IgA deposition and leukocytoclastic change. What is the most
likely cause of disease in this patient?
A. SLE
B. Polyarteritis nodosa
C. *Henoch-Schenlein purpura
D. Microscopic polyangiitis
E. Goodpastures syndrome
159. What is the most specific indicator of Raynaud’s phenomenon commonly associated with SLE or a
related connective tissue (CT) disease?
A. Alopecia
B. Diffuse myalgias and arthralgias
C. *Dilated capillary loops on capillary microscopy
D. History of a first-degree relative with SLE
E. Onset of severe fatigue in the last 2 months
160. A 32-year-old woman with longstanding SLE presents with severe headache. Her blood pressure is
200/110 mm Hg, the cardiac examination is remarkable for an S4, and a new heart murmur is noted at the
left sternal border. Her medical history includes 3 spontaneous abortions and multiple episodes of
pleurisy, arthritis, and thrombocytopenia. Dipstick urinalysis is positive for protein and trace blood.
Microscopic examination shows 3 to 5 erythrocytes per high power field and an occasional granular cast.
Serum creatinine level is 4.0 mg/dL. What is a renal biopsy likely to show?
A. Diffuse proliferative glomerulonephritis
B. Focal segmental glomerulonephritis
C. IgA deposits
D. Mesangial deposits (seen by electron microscopy only)
E. *Thrombotic microangiopathy
161. A 33-year-old female with systemic lupus erythematosus (SLE) and a remote histoiy of nephritis
has recently moved to your city and comes to your office for management of her SLE. Her nephritis was
treated with cyclophosphamide for two years, following which she was placed on azathioprine. However,
her renal disease has progressed; the most recent serum creatinine measured 5.54 mg/dL (490 mmol/L)
(normal = 0.57 to 1.24 mg/dL [50 to 110 mmol/L]). She has decided not to pursue further therapy; she
has no extrarenal manifestations of SLE. At this point, she seeks your opinion regarding the role of
dialysis and renal transplantation. Which one of the following statements regarding renal function in
patients with SLE is INCORRECT?
A. Progressive loss of nephrons due to active renal disease may not be reflected by changes in
measured creatinine clearance.
B. Despite initial maintenance of the glomerular filtration rate, many patients gradually progress to
end-stage renal
disease, often in the absence of clinical or serologic evidence of active lupus.
C. Patient survival with either hemodialysis or continuous ambulatory peritoneal dialysis appears to be
similar to that in the general population of patients with end-stage renal disease.
D. *The measurement of serologic parameters, such as complement levels and titers of anti-double
stranded DNA antibodies help predict disease recurrence in the renal allograft.
E. The rate of recurrent renal disease in the transplant patient with lupus is less than 10 percent.
162. A 25year-old man presents because of a painful, swollen knee and ankle of 2 weeks' duration. He
has never had joint disease prior to this time. The patient also complains of low back pain and a recent
history UTI. On examination he has vesicles (some of which have crusted over) on the palms, soles, and
glans penis; injected conjunctivae; a swollen right index finger; and arthritis of the right knee and left
ankle. Choose the most likely diagnosis from the below list of options.
A. *Reiter's syndrome
B. Psoriatic arthropathy
C. Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
163. A 23-yr-old man presented with low back pain, pain in the right knee and sore eyes. His past
history included an episode of diarrhea 3 weeks earlier and he had a positive history of back pain. Pelvic
radiography shows no changes in joints. Choose the most likely diagnosis from the below list of options.
A. *Reiter's syndrome
B. Ankylosing spondylitis
C. Psoriatic arthritis
D. Joint sepsis
E. Polyarteritis nodosa
164. A 27-year-old man presents because of a painful, swollen knee and ankle of 2 weeks' duration. He
has never had joint disease prior to this time. The patient also complains of low back pain and a recent
history of clear penile discharge. On examination he has vesicles (some of which have crusted over) on
the palms, soles, and glans penis; injected conjunctivae; a swollen right index finger; and arthritis of the
right knee and left ankle. Correct statements regarding this patient include all of the following EXCEPT
A. he will probably benefit from indomethacin
B. *his joint disease will probably improve after a course of benzylpenicilline
C. he is probably HLA-B27-positive
D. Sacroiliitis and spondyloarthropathy
E. may be seen as late sequelae his erythrocyte sedimentation rate is likely to be elevated
165. A 27-year-old man presents because of a painful, swollen knee and ankle of 2 weeks' duration. He
has never had joint disease prior to this time. The patient also complains of low back pain and a recent
history of clear penile discharge. On examination he has vesicles (some of which have crusted over) on
the palms, soles, and glans penis; injected conjunctivae; a swollen right index finger; and arthritis of the
right knee and left ankle. Choose the most likely treatment from the below list of options.
A. Cyclophosphanum
B. Penicillin
C. *Tetracycline
D. Prednisone
E. Ceftriaxone
166. A 29-yr-old homosexual male presented to A&E with a markedly swollen and tender left knee. He
says it's been present for about a month but has only recently become painful. He admitted losing weight
and on examination a temperature of 38В°C was found. He had no other complaints apart from a 2month history of cough, which he attributed to his heavy smoking. Choose the most likely diagnosis from
the below list of options.
A. Rheumatoid arthritis
B. Osteoarthritis
C. *Reiter's syndrome
D. Infective arthritis
E. Felty's syndrome
167. A 46-yr-old lady presented with swollen tender knee joints. She says they feel stiff especially in the
mornings. On examination she was found to have splenomegaly, a temperature of 38В°C and ulcerated
lower limbs with Hb—9 g/dl. WBC, neutrophiles and platelets were decreased. Albumin was 20 g/l.
Choose the most likely diagnosis from the below list of options.
A. Gout
B. Still's disease
C. *Felty's syndrome
D. Rheumatoid arthritis
E. Osteoarthritis
168. A 35-year-old woman who works in a nursing home develops acute abdominal pain and bloody
diarrhea. Many residents of the nursing home developed a similar disorder. Several weeks later, she
complains of diffuse musculoskeletal pain involving the neck, left wrist, left knee, and low back. On
examination she has marked swelling, warmth, and loss of motion of the left wrist and left knee, as well
as pain and restricted motion of the neck and lower lumbar spine. A diagnosis of reactive arthritis is
strongly suspected. Which one of the following statements is most likely to be true of this patient?
A. Her gastroenteritis was caused by Escherichia coli.
B. *Her arthritis will resolve completely within 4 to 6 months, without complications.
C. Antibiotic treatment of the underlying infection would have prevented her arthritis.
D. Shigella flexneri, more than any other organism associated with reactive arthritis, is predictive of a
recurrent course.
E. Neisseria gonorrhoeae, more than any other organism associated with reactive arthritis, is predictive
of a recurrent course.
169. A 37-year-old man develops acute abdominal pain and bloody diarrhea. Several weeks later, he
complains of diffuse musculoskeletal pain involving the neck, left wrist, left knee, and low back. On
examination he has marked swelling, warmth, and loss of motion of the left wrist and left knee, as well as
pain and restricted motion of the neck and lower lumbar spine. Choose the most likely treatment from the
below list of options.
A. Cyclophosphanum
B. Penicillin
C. *Tetracycline
D. Prednisone
E. Ceftriaxone
170. A 37-year-old woman develops acute abdominal pain and bloody diarrhea. Several weeks later, she
complains of diffuse musculoskeletal pain involving the neck, left wrist, left knee, and low back. On
examination she has marked swelling, warmth, and loss of motion of the left wrist and left knee, as well
as pain and restricted motion of the neck and lower lumbar spine. Choose the most likely diagnosis from
the below list of options.
A. Rheumatoid arthritis
B. *Reactive arthritis
C. Osteoarthritis
D. Haemochromatosis
E. Gonococcal arthritis
171. A 20-year-old man with SLE presents to the emergency department with chest pain that started 10
days ago. He has become increasingly dyspneic over the last 48 hours and has been too exhausted to
make meals. He will not lay flat on the examination table and insists on leaning slightly forward. Blood
pressure is 94/50 mm Hg and heart rate is 100 bpm. The heart sounds are quiet, and tubular breath sounds
are heard at the left scapular border. There is 1+ peripheral edema. Chest radiograph shows a possible
cardiomegaly. What is the next step in this patient’s management?
A. Arterial blood gas
B. Diuresis with intravenous furosemide
C. *Echocardiogram
D. High-dose nonsteroidal medication
E. Infusion of stress dose steroids
172. What is the most specific indicator of Raynaud’s phenomenon commonly associated with SLE or a
related connective tissue (CT) disease?
A. Alopecia
B. Diffuse myalgias and arthralgias
C. *Dilated capillary loops on capillary microscopy
D. History of a first-degree relative with SLE
E. Onset of severe fatigue in the last 2 months
173. A 23-year-old woman was diagnosed with systemic lupus erythematosus (SLE) at age 13 years
when she presented with polyarticular joint swelling. On a regimen of methotrexate and
hydroxychloroquine, her joint pain and swelling have been relatively well controlled. The patient’s
fingers exhibit both boutonniere and swan-neck deformities, but she is able to make a normal closed fist.
What will radiographs of the patient’s hands likely reveal?
A. Bone fragmentation
B. Carpal fusion
C. Erosions in the proximal joints
D. Marked subchondral cysts
E. *Normal joints
174. A 32-year-old woman with longstanding SLE presents with severe headache. Her blood pressure is
200/110 mm Hg, the cardiac examination is remarkable for an S4, and a new heart murmur is noted at the
left sternal border. Her medical history includes 3 spontaneous abortions and multiple episodes of
pleurisy, arthritis, and thrombocytopenia. Dipstick urinalysis is positive for protein and trace blood.
Microscopic examination shows 3 to 5 erythrocytes per high power field and an occasional granular cast.
Serum creatinine level is 4.0 mg/dL. What is a renal biopsy likely to show?
A. Diffuse proliferative glomerulonephritis
B. Focal segmental glomerulonephritis
C. IgA deposits
D. Mesangial deposits (seen by electron microscopy only)
E. *Thrombotic microangiopathy
175. A 20-year-old man with SLE presents to the emergency department with chest pain that started 10
days ago. He has become increasingly dyspneic over the last 48 hours and has been too exhausted to
make meals. He will not lay flat on the examination table and insists on leaning slightly forward. Blood
pressure is 94/50 mm Hg and heart rate is 100 bpm. The heart sounds are quiet, and tubular breath sounds
are heard at the left scapular border. There is 1+ peripheral edema. Chest radiograph shows a possible
cardiomegaly. What is the next step in this patient’s management?
A. Arterial blood gas
B. Diuresis with intravenous furosemide
C. *Echocardiogram
D. High-dose nonsteroidal medication
E. Infusion of stress dose steroids
176. What is the most specific indicator of Raynaud’s phenomenon commonly associated with SLE or a
related connective tissue (CT) disease?
A. Alopecia
B. Diffuse myalgias and arthralgias
C. *Dilated capillary loops on capillary microscopy
D. History of a first-degree relative with SLE
E. Onset of severe fatigue in the last 2 months
177. A 33-year-old female with systemic lupus erythematosus (SLE) and a remote histoiy of nephritis
has recently moved to your city and comes to your office for management of her SLE. Her nephritis was
treated with cyclophosphamide for two years, following which she was placed on azathioprine. However,
her renal disease has progressed; the most recent serum creatinine measured 5.54 mg/dL (490 mmol/L)
(normal = 0.57 to 1.24 mg/dL [50 to 110 mmol/L]). She has decided not to pursue further therapy; she
has no extrarenal manifestations of SLE. At this point, she seeks your opinion regarding the role of
dialysis and renal transplantation. Which one of the following statements regarding renal function in
patients with SLE is INCORRECT?
A. Progressive loss of nephrons due to active renal disease may not be reflected by changes in
measured creatinine clearance.
B. Despite initial maintenance of the glomerular filtration rate, many patients gradually progress to
end-stage renal disease, often in the absence of clinical or serologic evidence of active lupus.
C. Patient survival with either hemodialysis or continuous ambulatory peritoneal dialysis appears to be
similar to that in the general population of patients with end-stage renal disease.
D. *The measurement of serologic parameters, such as complement levels and titers of anti-double
stranded DNA antibodies help predict disease recurrence in the renal allograft.
E. The rate of recurrent renal disease in the transplant patient with lupus is less than 10 percent.
178. A 64-year-old man with ankylosing spondylitis (AS) whom you have known for many years comes
to clinic with the complaint of weakness and numbness of the hands and difficulty climbing stairs for the
past three days. He has painful paresthesias in his hands. He has noticed some urinary frequency and
constipation. He denies any trauma to his neck or back. On physical examination, temperature is 98.8°F
(37-40C), pulse is 98 beats/min, respirations are 16/min and blood pressure is 160/95 mmHg. General
physical examination is unremarkable. His spine is unchanged compared to his baseline, namely rigid
and nontender. Neurologic examination reveals bilateral grip weakness, decreased sensation of light
touch in the hands and forearms, and decreased strength in the lower extremities. He has mild
hyperreflexia in the upper and lower extremities. What is the most likely cause of the patient's
symptoms?
A. Herniated cervical disc at C4-5
B. Cauda equina syndrome
C. *Atlantoaxial subluxation
D. Syndesmophyte fracture at the C5-6 interspace
E. Compression fracture with secondary spinal stenosis
179. A 54-year-old woman presents with a 30-year history of low back pain and stiffness. For many
years she has been under the care of a chiropractor, who has "manipulated" her spine on a weekly basis.
Following his retirement, her new chiropractor obtained some new spine radiographs and informed her
that she has ankylosing spondylitis (AS), You are intrigued by this history and pull out the films before
examining her. Which one of the following radiograph_ic features is LEAST likely to be associated with
AS?
A. Atlantoaxial subluxation.
B. Calcification of the anterior longitudinal ligament
C. Erosions and osteitis at the ischial tuberosities
D. Apical pulmonary fibrosis
E. *Aortic valvular calcification
180. A 42-year-old female is seen for evaluation of diffuse polyarthralgias which began one week ago.
She developed a flu_like illness with headache, joint pain, and a fever of ioo°F (37.8°С). A skin rash
developed over her face and cheeks, which resolved after five days. Her joints continue to ache,
especially her hands and toes. Past medical histoiy is unremarkable. No recent vaccinations. She coaches
a soccer team and recalls that two chil_dren recently had been sick due to the "flu". The physical exam is
notable for mild arthralgias over the wrists and several MCP joints. There are small knee effu_sions.
Which one of the following laboratory findings would NOT be consistent with a parvovirus B19
infection?
A. Rheumatoid factor (RF) 185 U
B. *ESR 65 mm/hr
C. Synovial fluid WBC 1,900 with 75 percent neutrophils, 25 percent lymphocytes
D. Hemoglobin 9.8 gm/dL
E. The finding of parvovirus B19 DNA in synovial fluid specimens
181. A 34-year-old female librarian consults you to hear your opinion regarding the management of her
rheumatoid arthritis (RA). She was recently diagnosed with this condition and her primary care physician
recommended the ini_tiation of sulfasalazine therapy. She has researched a number of Internet sites and
has listed five statements about sulfasalazine that she wishes to discuss with you. You review this list of
five, and conclude that four statements are correct. Which one of the following is INCORRECT?
A. The risk of developing adverse effects with sulfasalazine appeai-s to be at least partly genetically
determined.
B. Serious episodes of agranulocytosis are usually observed within the first three months and often
within the first six weeks of therapy.
C. Unlike inflammatory bowel disease in which 5-ASA is the active metabolite, sulfapyridine is the
active moiety in patients with RA.
D. *Adverse reactions are common with sulfasalazine. Approximately 20 to 25 percent of patients
withdraw from clinical trials because of skin rash.
E. Oligospermia and infertility are reversible side effects.
182. A 28-year-old African-American female with systemic lupus erythematosus (SLE) is referred to
your office for con_sultation because she has developed severe edema. She reports that in the last two
months she has developed increasing lower, and more recently, upper extremity swelling. Current
medications include hydroxychloroquine 400 mg QD and prednisone 5 mg QD. On physical
examination: T 98.3 BP 135/82, P 90 R 15- She weighs 28 pounds more than her baseline 155 pounds of
three months ago. There is 3+ lower extremity, 1+ upper extremity, and trace facial edema. Laboratory
evaluation: CBC normal Creatinine = 1.1 mg/dL (97 mmol/L) (normal = 0.57 to 1.24 mg/dL [50 to 110
mmol/L]) Serum albumin = 1.8 g/dL (normal = 4.0 to 6.0 g/dL) C3 and C4 normal Anti-dsDNA antibody
12 Units. Urinalysis reveals 3+ protein but is otherwise unremarkable. 24-hour urine protein 12.3 grams.
Which one of the following statements regarding the renal biopsy in patients with lupus nephritis is
correct?
A. *The one pathologic finding that is relatively specific for SLE is the presence of numerous
tubuloreticular structures in the glomerular endothelial cells.
B. Deposits in the subepithelial space are associated with the influx of neutrophils and mononuclear
cells.
C. Anti-DNA antibodies that are associated with membranous nephropathy tend to be IgGi and IgG3.
D. Isolated membranous nephropathy is observed in about 50 percent of patients with SLE undergoing
renal biopsy.
E. Most patients with membranous nephropathy are noted to have elevated anti-dsDNA antibodies or
depressed
serum complement levels.
183. A 33-year-old male is referred to you for evaluation of a persistent fever, skin rash, and systemic
illness. You suspect that he has adult Still's disease. Which one of the following features is NOT a
characteristic feature of adult Still's disease?
A. Hyperferritinemia
B. Nonerosive narrowing of the carpometacarpal joints
C. Elevated serum lactate dehydrogenase (LDH) levels
D. Lymph node biopsy showing immunoblastic hyperplasia
E. *Lymphocytosis
184. A 33-year-old graduate student from the Czech Republic has been referred to you for further care.
She has a six-year history of rheumatoid arthritis. Last year, while studying in England, she was started
on infliximab. She has done extremely well with a marked improvement in her functional status.
However, for the past month she describes a low-grade fever, malaise, and night sweats. She does not
recall whether a PPD (purified protein derivative) was planted prior to initiation of infliximab. Which
one of the following statements regarding development of tuberculosis (ТВ) in infliximab treated patients
is INCORRECT?
A. Development of active ТВ is mostly due to reactivation of latent disease.
B. More than three-quarters of cases of ТВ are evident by the sixth infusion.
C. About one-quarter of cases are disseminated at presentation.
D. *A minority of cases exhibit extrapulmonary disease.
E. Most cases have been observed in European patients.
185. A 65-year-old man with a history of Wegener's granulomatosis (WG) presents to your office for
follow-up. He was diagnosed with WG at age 59. He had sinus, pulmonary, and renal involvement and
was treated with prednisone and cyclophosphamide. He received a total of 14 months of
cyclophosphamide, approximately 2 mg/kg per day along with a tapering dose of prednisone and had a
complete response to therapy. He has been off these medications for over three years and has been
treated with prophylactic therapy consisting of daily trimethoprim-sulfamethoxazole since. The patient
feels "great" and is completely asymptomatic with an unremarkable physical exam. Laboratory studies
reveal: Hemoglobin = 10.4 g/dL (6.5 mmol/L) (normal - 13 to 18 g/dL [8.1 to 11.2 mmol/L]) ESR = 41
mm/hr (normal = о to 20 mm/hr). Creatinine = 1.1 mg/dL (97.2 umol/L) (normal = 0.8 to 1.3 mg/dL [70
to 114 umol/L]) ANCA = 55 Ш. Urinalysis = 25 RBC/HPF, no casts and trace protein. Liver function:
normal Chest x-ray: normal The most appropriate management at this time would be?
A. Begin cyclophosphamide 2 mg/kg/day
B. Begin cyclophosphamide 2 mg/kg/day with prednisone 60 mg/day
C. Renal biopsy
D. *Urological evaluation including cystoscopy
E. Begin methotrexate 20 mg/week
186. A 22-year-old woman with a histoiy of recently diagnosed systemic lupus erythematosus (SLE) is
seen for a follow-up visit. Three weeks ago, you started her on prednisone 20 mg daily for treatment of a
lupus flare. She has definitely improved; however, she is concerned about corticosteroid-associated
toxicities. Which one of the following statements regarding these toxicities is INCORRECT?
A. *Use of corticosteroids increases the risk of development of peptic ulcer disease by more than twofold.
B. The average daily prednisone dose is the strongest predictor of a serious adverse effect potentially
attributable to
corticosteroid therapy.
C. Corticosteroids may cause peripheral insulin resistance, hyperinsulinemia, and increased hepatic
VLDL synthesis.
D. Sudden death has been reported in occasional patients who have been given pulse infusions of
corticosteroids.
E. Clinically significant hypokalemia is uncommon with routine exogenous corticosteroid use.
187. A previously healthy, 22-year-old, male college student had an upper respiratory tract infection two
weeks ago and was treated with oral penicillin for one week. Yesterday, he developed bilateral ankle pain
and swelling along with raised purpuric lesions over his lower extremities. Laboratory results: Serum
creatinine = 3.0 mg/dL (265 umol/L) (normal = 0.8 to 1.3 mg/dL [70 to 114 umol/L]) BUN = 46 mg/dL
ў16 mmol/L) (normal = 10 to 20 mg/dL [3.6 to 7.1 mmol/L]) AST = 22 IU/L ў0.47 ukat/L)(normal = о
to 35 IU/L [0 to 0.58 ukat/L]) ALT = 31 IU/L (0.52 ukat/L)(normal = о to 35 IU/L [0 to 0.58 ukat/L])
ANA = 1:80. Urinalysis - 4+ proteinuria, 2+ RBCs, several RBC casts/high power field. Which one
would be the most likely histopathology on renal biopsy?
A. Mesangial proliferation with IgA deposition on immunofluorescence
B. *Crescentic glomerulonephritis with IgA deposition on immunofluorescence
C. Crescentic glomerulonephritis with negative immunofluorescence and no deposits on electron
microscopy
D. Proliferative glomerulonephritis with IgG and complement on immunofluorescence and
subendothelial deposits and subepithelial "humps" on electron microscopy
E. Crescentic glomerulonephritis with positive immunofluorescence and no deposits on electron
microscopy
188. A 19-year-old patient with systemic lupus erythematosus (SLE) has been treated with high dose
corticosteroids and hydroxychloroquine for three years. An ophthalmologist recently noted the
development of cataracts. Which one of the following statements regarding the development of cataracts
associated with corticosteroid use is correct?
A. *Children are more susceptible than adults.
B. They are rarely bilateral.
C. They occur in an anterior subcapsular location.
D. They progress rapidly despite the reduction in steroid dose.
E. They occur in an posterior subcapsular location.
189. A 64-year-old man comes to the office complaining of left flank pain and gross hematuria. The pain
is non-radiating, dull in nature, and not associated with any nausea or vomiting. The hematuria is
painless, intermittent, and not associated with any fevers or chills. The patient has not had any medical
care in over 20 years. His vital signs and physical examination are unremarkable. A complete blood
count and biochemical profile are normal. A urinalysis shows full field red blood cells. A CT scan of
abdomen and pelvis reveals a contrast enhancing 5cm mass in the lower pole of the left kidney. A chest
x-ray shows no signs of metastasis. The most appropriate intervention at this time is to
A. order a CT guided percutaneous needle biopsy
B. order an MRI with gadolinium
C. schedule chemotherapy
D. schedule radiation therapy
E. *send him to a urologist for a radical nephrectomy
190. A 26-year-old men is brought to the office because of a "red rash" that she noticed today. She says
that 3 days ago he had a cough, runny nose, and fever that responded to ibuprofen. In the office, his
temperature is 37 oC (98.6 F) and he has a normal physical examination with the exception of an
erythematous, blanching macular rash on his legs. You diagnose him with a viral exanthem and advise to
drink liquids and to use ibuprofen as needed for fever. One week later, the men comes back to the office
and reports that the rash has "changed", he has developed colicky abdominal pain several times per day,
and he is complaining of left knee pain. In the office, his temperature is 37.2 C (99 F), blood pressure is
100/65 mm Hg, pulse is 100/min, and respiratory rate is 15/min. A physical examination reveals a wellappearing patient with palpable purpura of both lower extremities, normal neck examination, clear lungs,
and a soft, non-tender abdomen. His left knee is painful on flexion, but it is not erythematous or warm,
and there does not seem to be an effusion. His gait is normal. The most appropriate study at this time is
A. arthrocentesis
B. colonoscopy
C. cultures of blood, urine, and cerebrospinal fluid
D. echocardiography
E. *urinalysis
191. A 23-year-old woman comes to the clinic for a pre-employment examination. She recently moved
to the area from out of state and got a job at a local small business. Her past medical history is significant
only for diabetes mellitus type I, which she has had since age 13. Her only medication is insulin, which is
infused via an insulin pump. She denies smoking or using illicit drugs. She admits to social alcohol
consumption less than once a week and says she runs 2 miles daily. She is not sexually active. You
perform a full physical examination. Her temperature is 37.1 (98.8 F), blood pressure is 136/89 mm Hg,
pulse is 54/min, and respirations are 12/min. Her skin is warm and dry. Cardiovascular examination
reveals a normal S1, S2 with no murmurs appreciated. Respirations are equal bilaterally without any
abnormal breath sounds. Extremities show no clubbing, cyanosis, or edema. Strength is equal bilaterally
and sensation is full throughout. The patient exhibits normal reflexes. She returns to the clinic several
more times and her blood pressure remains elevated. The most appropriate initial pharmacotherapy for
this patient is
A. amlodipine
B. atenolol
C. *enalapril
D. furosemide
E. hydrochlorothiazide
192. A 57-year-old woman with diabetes and hypertension comes to the office because of a 5-day
history of weakness and lethargy. The symptoms developed slowly but have worsened over the last 2
days. She denies any chest pain, dyspnea, fever, cough, abdominal pain, or dysuria, but has noticed a
decrease in her urine output. One week prior to admission she underwent a CT scan of the abdomen with
intravenous contrast for routine follow up of an abdominal aortic aneurysm, which is stable at 4 cm. She
regularly takes hydrochlorothiazide, glyburide, captopril, and aspirin. Her temperature is 37.0 C (98.6 F),
blood pressure is 165/94 mm Hg, pulse is 92/min, and respirations are 14/min. Physical examination
shows 2+ pitting edema in the lower extremities and 1+ peripheral pulses. Urinalysis shows trace protein,
1-3 white blood cells, tubular casts and no red casts. This condition most likely would have been
prevented by
A. *administering acetylcysteine prior to the contrast for the CT scan
B. holding her captopril 2 days prior to the CT scan
C. giving her intravenous ampicillin during the CT scan
D. giving her intravenous furosemide 1 hour prior to the CT scan
E. premedicating her with nifedipine 2 days prior to the CT scan
193. A 42-year-old woman comes into the clinic complaining of intermittent easy bruising around her
eyes and chest, especially after surfing and boogie boarding with her son. She recently suffered a
syncopal episode and a work up, which included a stress echocardiogram, revealed a hypertrophic heart
with a speckled pattern. When she was discharged from the hospital, she was given a diagnosis of
congestive heart failure with a restrictive pattern. An endomyocardial biopsy is scheduled for next week.
She denies any significant family history and has been healthy with the exception of easy bruising,
occasionally with vomiting. Routine urinalysis from her recent admission revealed proteinuria. Upon
further questioning, she has suffered carpal tunnel syndrome bilaterally and occasional numbness and
tingling of her toes. The most useful study to diagnose this patient's condition is
A. complete blood count
B. liver function test
C. morning cortisol level
D. *protein immunoelectrophoresis
E. thyroid function tests
194. A 55-year-old man comes to the emergency department with pain on urination, fever and chills. He
also complains of perineal and suprapubic tenderness as well as dysuria and hesitancy. His allergies
include codeine, sulfonamides, and quinidine. Temperature is 38.5 C (101.3 F), blood pressure is 132/90
mm Hg, pulse is 88/min, and respirations are 18/min. Abdominal examination is remarkable for
suprapubic tenderness. Digital rectal examination demonstrates a swollen, boggy, and exquisitely painful
prostate gland. Laboratory studies show a leukocyte count of 11,500/mm3, creatinine of 0.9 mg/dL, and
blood urea nitrogen of 16 mg/dL. A urinalysis shows too numerous to count white blood cells and Gramnegative rods. The most appropriate treatment for this patient is
A. amoxicillin/clavulanate 875 mg by mouth twice daily for 14 days
B. ceftriaxone 1 gram intravenously daily for 5 days
C. *ciprofloxacin 500 mg by mouth twice daily for 14 days
D. clindamycin 300 mg 4 times daily for 10 days
E. trimethoprim-sulfamethoxazole 1 double strength tablet twice daily for 14 days
195. A 38-year-old man is admitted to the hospital for acute deterioration in renal function. He was seen
in your office 2 days prior for some mild upper respiratory complaints, including a sore throat, cough,
and fever. He was prescribed cephalexin and sent home. Today, his laboratory data returned and shows a
blood urea nitrogen level of 67 mg/dL and a creatinine level of 2.1 mg/dL. You called him and told him
to meet you at the hospital for further evaluation. On admission his BUN is now 109 mg/dL and his
creatinine is 4.2 mg/dL. The appropriate tests are ordered and an electrocardiogram shows QRS complex
widening and tall, peaked T waves. His temperature is 38.3 C (101.0 F). He has an erythematous
oropharynx with some mild tonsillar exudate. His lungs are clear. It is observed that he has urinated only
5-10 cc in the past 2 hours since his hospitalization. A urinalysis shows red cell casts and dysmorphic red
blood cells. The most appropriate next step is to
A. *administer high-dose methyl-prednisolone, intravenously
B. administer low-dose methyl-prednisolone, intravenously
C. administer penicillin, intravenously
D. prescribe high-dose cyclophosphamide, orally
E. prescribe penicillin, orally
196. A 40-year-old man complained of headache in occipital area. On physical examination, the skin
was pale; there was face and hand edema, blood pressure of 170/130 mm Hg. On EchoCG, there was
concentric hypertrophy of the left ventricle. Ultrasound examination of the kidneys revealed thinned
cortical layer. Urinalysis showed proteinuria of 3.5 g/day. What is the diagnosis
A. *Chronic glomerulonephritis
B. Essential arterial hypertension
C. Chronic pyelonephritis
D. Polycystic disease of the kidneys.
E. Cushing’s disease
197. A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating,
aching pain in lumbar area, a discomfort in urination, and frequent voiding. Pasternatsky’s sigh is
positive in both sides. On lab exam, WBC of 20.000/mcL; on urinalysis protein of 0.6g/L, leukocyturia,
bacteriuria. Your preliminary diagnosis.
A. *Acute pyelonephritis
B. Exacerbation pf chronic pyelonephritis
C. Acute glomerulonephritis
D. Acute cystitis
E. Nephrolithiasis
198. A 25-year-old woman complained of fatigue, hair loss, and brittle nails. On exam, pallor of skin,
PR of 94/min, BP of 110/70 mm Hg. On blood cell count, Hb of 90 g/L, RBC 3.5·1012/L, color index of
0.7, ESR of 20 mm/h. Serum iron level was 8.7 mcmol/L. What treatment would you initiate?
A. *Ferrous sulfate orally
B. Iron dextrin injections
C. Vitamin B12 intramuscularly
D. Blood transfusion
E. Packed RBCs transfusion
199. A 58-year-old alcoholic with hepatitis C cirrhosis is admitted to the hospital for management of his
ascites. He has been managed as an outpatient with diuretics and oral lactulose, but over the past few
weeks, he reports increasing abdominal girth, weight gain and lower extremity edema. He has been
noncompliant with his low-sodium diet. His medications include furosemide, spironolactone, lactulose,
ciprofloxacin, and thiamine. On physical examination, he appears grossly edematous and appropriately
responsive. His lungs are clear and his heart is without extra sounds or murmurs. His abdomen is tense
with a fluid wave and shifting dullness on percussion. He has numerous non-blanching telangiectasias on
his torso and abdomen. His testes are small for his age and there is no asterixis. Admission laboratory
studies show: Sodium 121 mEq/L, Potassium 4.3 mEq/L, Bicarbonate 29 mEq/L, BUN 38 mg/dL,
Creatinine 1.5 mg/dL. Urinalysis shows some granular casts and a urinary sodium concentration of <10
mmol/L. The most appropriate therapy is to
A. administer hypertonic saline
B. administer sodium chloride tablets
C. increase the dose of furosemide
D. increase the dose of spironolactone
E. *salt restrict
200. A 20- year-old patient with a history of preceding streptococcal infection complains of malaise,
headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of
100/min, RR of 20/min, the urinalysis showed increased protein, red cell casts and hyaline casts. What is
your diagnosis
A. *Acute glomerulonephritis
B. Acute pyelonephritis
C. Rheumatic fever
D. Essential hypertension
E. Bacterial endocarditis
201. A 29-year-old woman, who has been undergoing treatment for hypertension for the past 2 years,
comes to the office because of chills and right-sided flank pain. She has had chronic "low back pain" that
you have been treating unsuccessfully with nonsteroidal anti-inflammatory drugs. She has never had any
diagnostic studies performed to evaluate her hypertension or back pain. She is estranged from her family,
but she knows that her mother and brother have been treated for hypertension starting at age 25. She has
not spoken to them in 10 years and so she is unaware of any other medical conditions. Her temperature is
38.1 C (100.6 F), blood pressure is 130/90 mm Hg, and pulse is 65/min. On physical examination today
there is marked right-sided flank tenderness. Cardiac examination reveals a mid-systolic click. Urinalysis
shows pyuria and white blood cell casts. You prescribe a 14-day course of trimethoprimsulfamethoxazole, schedule a renal ultrasound and a follow-up visit. You tell her to call your office
immediately if the symptoms worsen. On the return visit, she says that she feels much better, but still has
dull flank pain. Her temperature is 37.0 C (98.6 F). The ultrasound report is in the chart and states that
there are 7 cysts in her right kidney and 5 cysts in her left kidney. At this time the most correct statement
about her condition is:
A. Her hypertension is unrelated to the kidney disease
B. Long-term treatment with trimethoprim-sulfamethoxazole will eradicate the cysts
C. She has a 20% chance of developing end-stage renal disease by age 70
D. *She is at an increased risk for developing colonic diverticular disease with perforation
E. There is a 70% chance that she has an intracranial aneurysm and will suffer from a subarachnoid
hemorrhage
202. A 27-year-old woman comes to the office for a periodic health maintenance examination. She
started a new job at a prestigious law firm 3 months ago and has been working very long hours. She feels
"a bit forgetful" lately, but she attributes that to the "midnight coffee runs" at the office. Her last
menstrual period was 3 weeks ago. She tells you that for the past 6 months, starting 7-10 days before she
is scheduled to get her period, she has been noticing some pinkish-red blood on the toilet paper after she
goes to the bathroom. It continues until she gets her period on the regularly scheduled day. It has been
somewhat annoying because it seems like she is bleeding for more than half of the month. She is sexually
active and she uses condoms as contraception. Her Pap smears over the past 10 years have been normal.
Her pelvic examination and physical examination are unremarkable. You perform a Pap smear and send
it for pathologic examination. A urine pregnancy test is negative. You notice that she is putting lotion on
her arms and hands as you are leaving the room. The most appropriate next step is to
A. begin a therapeutic trial of leuprolide acetate, parenterally
B. begin a therapeutic trial of naproxen, orally
C. determine thyroid stimulating hormone concentration
D. *refer her for cervical dilatation and curettage of the entire uterine cavity
E. schedule a diagnostic laparoscopy
203. A 30-year-old woman comes to the clinic complaining of loss of control of urination and
"dribbling" of urine. She has had recurrent urinary tract infections over the past 11 months, which were
treated with antibiotics. She has been following safe sex practices and denies any history of sexually
transmitted diseases, but complains of moderate pain during intercourse. Physical examination and pelvic
examination are normal. The most appropriate next investigation in this patient is
A. CT scan of the abdomen and pelvis
B. laparoscopy
C. pelvic sonography
D. renal sonography
E. *voiding cystourethrogram
204. A 78-year-old woman is admitted to the hospital because of fever, flank pain, and mental
obtundation. On arrival to the hospital, she was minimally responsive and was found to have a white
blood cell count of 43,000/mm3 with a profound left shift. Urinalysis revealed packed white cells. A
renal ultrasound demonstrated a left hydronephrosis and hydroureter. A CT scan confirmed the presence
of an obstructing stone. Her vital signs on admission showed a temperature of 39.5 C (103.1 F), blood
pressure of 80/40 mm Hg, pulse of 112/min, and respirations of 18/min. Intravenous pressors were
initiated. Three sets of blood cultures came back positive for Gram-negative rods within 2 hours. The
most appropriate next step in management is to
A. *insert a nephrostomy tube, percutaneously
B. administer antibiotics, intravenously, and observe
C. perform extracorporeal shock wave lithotripsy (ESWL)
D. schedule cystoscopy and ureteral stent placement
E. schedule a nephrectomy
205. A 37-year-old comes to the clinic for a required pre-employment physical examination. She has no
past medical history and has no complaints. Her temperature is 37.0 C (98.6 F), blood pressure is 110/60
mm Hg, pulse is 63/min, and respirations are 14/min. She is currently menstruating. A urine culture,
which is required by her new job, reveals greater than 100,000 E. Coli colony-forming units. The most
appropriate next step in management of this patient's urine culture findings is
A. *no further management is indicated
B. prescribe ciprofloxacin, orally, for 14 days
C. prescribe trimethoprim-sulfamethoxazole, orally, for 3 days
D. repeat urine culture in 2 weeks
E. send her for urological evaluation
206. A 58-year-old woman comes to the office for a periodic health maintenance examination. She has
no complaints and is generally in good health. She takes no medications and does not drink or smoke.
You notice in her chart that her last menstrual period was two years ago, and at that time, she was not
interested in discussing hormone replacement therapy. Now she says that she has noticed that a few of
her friends have been "shrinking" and she is ready to take something "for osteoporosis." She has been
doing some research on the Internet and read that women with thromboembolic disease should not take
estrogen. She vaguely remembers having a few "blood clots" many years ago, before you were her
doctor, and so she wants to try "one of the newer drugs." You are not sure if she is "remembering" this
correctly, so you try to explain the benefits of estrogen replacement anyway, but she still is not
interested. Dual energy absorptiometry (DEXA) shows a bone mineral density that is more than 2.5
standard deviations below the mean. Alendronate is prescribed. The patient should be advised to
A. avoid weight-bearing exercise
B. continue taking alendronate, even if she experiences some mild chest pain and gastrointestinal
symptoms, and return to the office as needed
C. return to the office in one week for a complete blood count (CBC)
D. take the alendronate, along with calcium, after breakfast
E. *take the alendronate first thing in the morning, on an empty stomach, with a full glass of water,
and remain upright for at least 30 minutes
207. A 35-year-old woman is in the hospital for a flare of nephritis related to systemic lupus
erythematosus (SLE). On rounds in the morning, she complains of right hip pain. She states that for the
last several weeks, she has had a deep aching in the hip and now it is getting much worse since she was
in the hospital. It hurts her both at rest and with motion. She denies any history of trauma, and has not
started any new activities. There have been no fevers. Her only outpatient medication is prednisone 10
mg daily, and she takes ibuprofen for pain relief, which has helped minimally. However, now she is on a
higher dose of intravenous steroid. Her temperature is 37.2 C (99 F), blood pressure is 132/82 mm Hg,
and pulse is 72/min. There is no pain on palpation over the hip but pain is present with range of motion.
Laboratory studies show a leukocyte count 8,100mm3 and a hematocrit 34%. A plain x-ray of the pelvis
and hip is normal. The next most appropriate step is to
A. assure her that her pain will resolve spontaneously
B. continue the patient on oral ibuprofen and follow her symptoms as an outpatient in 1 month
C. increase the duration of her intravenous steroids
D. *order an MRI of the hip
E. send her for an arthrogram of the hip
208. A 31-year-old woman presents to your office complaining of flank pain and fever for the past 2
days. She has a history of multiple urinary tract infections. She has suffered 2 in the previous 18 months
that were treated successfully with trimethoprim-sulfamethoxazole. She is sexually active and her last
menstrual period was 6 days ago. She takes no routine medications. Her temperature is 39.5 oC (103.1 F),
blood pressure is 130/65 mm Hg, and pulse is 110/min. She has prominent right costovertebral angle
(CVA) tenderness. The most appropriate management of this patient is to
A. admit her to the intensive care unit
B. initiate therapy with ampicillin and gentamicin
C. obtain blood cultures and send her home pending results
D. *obtain urine cultures and initiate therapy with ampicillin and gentamicin
E. obtain urine cultures and send her home pending results
209. A 37-year-old alcoholic patient with multiple organ failure is found to have an arterial pH of 7.15.
The anion gap is determined to be 22 mEq/L (normal is 10 to 14 mEq/L). All of the following arelikely
causes of this disorder EXCEPT
A. *ammonium chloride ingestion
B. renal failure
C. actate accumulation
D. diabetic ketosis
E. methanol ingestion
210. A 27-year-old college freshman complains of dysuria and urinary frequency. Urinalysis reveals 8to
10 WBCs per high-power field and numerousgram-negative bacteria. All of the following statements
concerning this disease are true EXCEPT that
A. a single dose of an antibiotic may be sufficient treatment
B. pregnant women with bacteriuria should be treated, even if asymptomatic
C. patients with flank pain or fever should be treated for 10 to 14 days
D. *patients with indwelling catheters should receive long-term suppression
E. radiological investigation is appropriate formales of any age after their first infection
211. A 28-year-old man has the acute onset of colicky pain in the left costovertebral angle radiating into
the groin, as well as gross hematuria. Abdominal x-ray discloses a stone in the left ureter. All of the
following are true statements concerning this disease EXCEPT that
A. the majority of renal stones are radiopaque
B. radiolucent stones are usually composed of uric acid
C. staghorn calculi are associated with alkaline urine
D. *radiopaque stones usually contain cystine
E. urate stones are associated with acidic urine
212. The 39-year-old patient described above spontaneously passes the stone, which is found to contain
calcium oxalate. The most likely cause of this stone is
A. chronic urinary tract infections
B. vitamin D excess
C. primary hyperparathyroidism
D. *idiopathic hypercalciuria
E. renal tubular acidosis
213. A 71-year-old woman is receiving parenteral methicillin for leg cellulitis. Over 2 days she develps
macroscopic hematuria, oliguria, and marked deterioration in renal functioning. Features suggestive of
methicillin-induced acute interstitial nephritis include all of the following EXCEPT
A. fever and arthralgias
B. RBC casts in the urine
C. *eosinophils in the urine
D. return of renal functioning on discontinuing the drug
E. return of renal functioning after prednisone therapy
214. A 39-year-old woman presents with indurationand atrophy of the fingertips and is diagnosed as
having systemic sclerosis. Visceral involvement may lead to all of the following EXCEPT
A. esophageal hypomotility
B. *obstructive lung disease
C. congestive heart failure
D. bronchogenic carcinoma
E. renovascular hypertension
215. At a routine company physical examination, anasymptomatic 46-year-old man is found to have a
BP of 150/110 mm Hg, but no other abnormalities are present. What do you do next?
A. reassure the patient and repeat the physical examination in 12 months
B. order an outpatient hypertensive pyelogram
C. initiate antihypertensive therapy
D. *obtain repeated BP recordings in your office and/or the patient's home or work site
E. hospitalize the patient for renal arteriogra phy
216. A 72-year-old man has the sudden onset of suprapubic pain and oliguria. His temperature is 38.0°C
(100.4°F), pulse is 100/minute, respirations are 12/minute, and BP is 110/72 mm Hg. Abdominal
examination is only remarkable for a tender, distended urinary bladder. Immediate management of this
patient should be to
A. obtain a flat plate of the abdomen
B. perform abdominal ultrasonography
C. *insert a urethral catheter
D. administer furosemide IV
E. obtain an IVP
217. A 40-year-old man complained of headache in occipital area. On physical examination, the skin
was pale; there was face and hand edema, blood pressure of 170/130 mm Hg. On EchoCG, there was
concentric hypertrophy of the left ventricle. Ultrasound examination of the kidneys revealed thinned
cortical layer. Urinalysis showed proteinuria of 3.5 g/day. What is the diagnosis?
A. *Chronic glomerulonephritis
B. Essential arterial hypertension
C. Chronic pyelonephritis
D. Polycystic disease of the kidneys
E. Chronic renal failure
218. A man, aged 25, presents with facial edema, moderate back pains, body temperature of 37,5 С, BP
180/100 mmHg, hematuria [ up to 100 in v/f], proteinuria [2,0 g/L], hyaline casts - 10 in v/f., specific
gravity -1020. The onset of the disease is probably connected with acute tonsillitis 2 weeks ago. The
most likely diagnosis is:
A. Acute pyelonephritis
B. *Acute glomerulonephritis
C. Cancer of the kidney
D. Urolithiasis
E. Chronic glomerulonephritis
219. A 45-year-old woman who has had slowly progressive renal failure begins to complain of
increasing numbness and prickling sensations in her legs. Examination reveals loss of pinprick and
vibration sensation below the knees, absent ankle jerks, and impaired pinprick sensation in the hands.
Serum creatinine concentration, checked during her most recent clinic visit, is 0,790 mmol/L (8.9
mg/dL). The woman's physician should now recommend
A. a therapeutic trial of phenytoin
B. a therapeutic trial of pyridoxine (vitamin B6)
C. a therapeutic trial of cyanocobalamin (vitamin B12)
D. *initiation of renal replacement therapy
E. neurologic referral for nerve conduction studies
220. A 25 -year-old woman complained of edema on the face and legs, elevation in blood pressure up to
160/100 mm Hg, and weakness. She fell ill 3 weeks after sore throat. On urinalysis, protein of 0.5 g/L,
erythrocytes of 17 – 20/field, leukocytes of 2 – 3/field, erythrocyte casts. What treatment should be
initiated after establishing of the exact diagnosis?
A. Heparin
B. *Penicillin OS
C. Tetracycline
D. Dipyridamole
E. Ciprofloxacine
221. A 29-year-old woman is critically ill. The illness was manifested by oliguria, edema, severe
headache. Pasternatsky’s sigh is negative in both sides. On lab exam, WBC of 10.000/mcL; on urinalysis
protein of 1,6g/L, erythrocyturia. Your preliminary diagnosis.
A. *Acute pyelonephritis
B. Acute glomerulonephritis
C. Cancer of the kidney
D. Urolithiasis
E. Chronic glomerulonephritis
222. A 31-year-old man with a history of preceding tonsillitis complained of headache in occipital area,
edema. On physical examination, the skin was pale; there was face and extremitas edema, blood pressure
of 140/90 mm Hg. On EchoCG, there was concentric hypertrophy of the left ventricle. Ultrasound
examination of the kidneys revealed thinned cortical layer. Urinalysis showed proteinuria of 3.5 g/day,
hematurea. The level of protein in blood was 58 g/l. What treatment will be the most effective?
A. ceftriaxon
B. enalapril
C. furosemid
D. *prednisolone
E. dicinone
223. A 20- year-old patient with a history of preceding streptococcal infection complains of malaise,
headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of
100/min, RR of 20/min, the urinalysis showed increased protein, red cell casts and hyaline casts. What is
your diagnosis?
A. Chronic glomerulonephritis
B. Bacterial endocarditis
C. Rheumatic fever
D. Acute pyelonephritis
E. *Acute glomerulonephritis
224. A 55-year-old man undergoes intravenous pyelography (IVP) as part of a workup for hypertension.
A 3-cm solitary radiolucent mass is noted in the left kidney; the study otherwise is normal. The man
complains of no symptoms referable to the urinary tract, and examination of urinary sediment is within
normal limits. Which of the following studies should be performed next?
A. Repeat intravenous pyelography in 6 months
B. Early-morning urine collections for cytology (three samples)
C. Selective renal arteriography
D. *Renal ultrasonography
E. CT scanning (with contrast enhancement) of the left kidney
225. A 22- year-old patient with a history of preceding streptococcal infection complains of malaise,
headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of
100/min, RR of 20/min, the urinalysis showed increased protein, red cell casts and hyaline casts. What is
your diagnosis?
A. Bacterial endocarditis
B. Essential hypertension
B. Rheumatic fever
C. Acute pyelonephritis
D. *Acute glomerulonephritis
226. A 29-year-old woman is critically ill. The illness was manifested by oliguria, edema, severe
headache. Pasternatsky’s sigh is negative in both sides. On lab exam, WBC of 10.000/mcL; on urinalysis
protein of 1,6g/L, erythrocyturia. Your preliminary diagnosis.
A. Acute pyelonephritis
B. *Acute glomerulonephritis
C. Cancer of the kidney
D. Urolithiasis
E. Chronic glomerulonephritis
227. The patient after acute respiratory viral infection [10th day of disease] has complaints on headache,
oliguria, cola-colour urine. Urinalysis – hematuria [100-200 RBC in eyeshot spot], specific gravity –
1002. The blood creatinin level is 0,18 mmol/l, potassium level - 5,4 mmol/l. Make the previous
diagnosis.
A. Acute interstitial nephritis
B. Acute renal failure
C. *Acute glomerylonephritis
D. Acute cystitis
E. Acute renal colic
228. An 18-year-old white man is seen in your office because of blood on urine dipstick analysis during
a sports physical. He has no history of gross hematuria, recent fever or chills, or upper respiratory illness.
He has been in good health. He takes cetirizine for seasonal allergies. He has no family history of renal
disease. Review of systems is negative. On examination, blood pressure is 140/98 mm Hg, weight is 80
kg (176 Ib), and height is 170 cm (67’). He has a muscular build. The remainder of the physical
examination is normal. Repeated urinalysis at2 p.m. reveals a pH of 5.0, specific gravity of 1.015,2+
blood, 2+ protein. Which test is the best option to assist in diagnosis?
A. Renal computed tomography
B. Renal ultrasonography
C. Cystoscopy
D. Magnetic resonance angiography of renal arteries
E. *Urinary protein-to-creatinine ratio
229. A 19-year-old woman has painless hematuria. Five days ago, she developed a sore throat, fever
(temperature, 37.8 °C [100 °F]), and dry cough. Four days ago, she noted painless gross hematuria on
two occasions. Six months ago, at the time of a college physical examination, she was told of
microscopic hematuria and advised to have this rechecked. She does not use recreational drugs. She has
taken acetaminophen for the past several days. At presentation, the patients sore throat is improved and
she no longer has fever. On examination, she is alert and in no distress. Blood pressure is 135/85 mm Hg,
pulse rate is 78/min, and temperature is 37 °C (98.6 °F). Skin examination is normal, and the fundi are
normal. No exudate is present in the pharynx. Neck examination shows no significant lymphadenopathy.
The lungs are clear. The heart is in regular sinus rhythm, with no murmur or rub. Abdominal examination
is normal. The joints are normal. Laboratory studies: Leukocyte count -9400/?L. Hemoglobin -13.5 g/dL.
Hematocrit -39%. Blood urea nitrogen -12 mg/dL. Serum creatinine -1.0 mg/dL. Serum antinuclear
antibodies Negative. Serum C3 90 mg/dL. Serum C4 -20 mg/dL. Urine protein :creatinine ratio -0.5.
Urinalysis pH 5.5; specific gravity - 1.012; trace proteinuria, 3+ hematuria. Urine microscopy shows red
blood cells, occasional red blood cell casts, and 1 to 3 Ieukocytes/hpf. What is the most likely cause of
renal disease in this patient?
A. Lupus nephritis
B. Post-streptococcal glomerulonephritis
C. Acute interstitial nephritis
D. *IgA nephritis
E. Renal papillary necrosis
230. A 45-year-old man is hospitalized after 5 days of severe diarrhea and anorexia. He has a history of
renal failure secondary to chronic glomerulonephritis and received a living related renal transplant 2
years earlier. He takes cyclosporine, mycophenolate mofetil, and prednisone, as well as amlodipine to
treat hypertension. He has had no rejection episodes or opportunistic infections. The remainder of his
history is unremarkable. On admission, blood pressure is 100/70 mm Hg and pulse rate is 100/min while
supine; blood pressure is 80/50mm Hg and pulse rate is 120/min while standing. Body temperature is
37.5°C (99.5 °F). Physical examination reveals a thin man in no distress. Mucus membranes are dry, and
neck veins are flat at 30-degree elevation. Cardiopulmonary examination is unremarkable except for
resting tachycardia. Abdominal palpation reveals diffuse tenderness without peritoneal signs. No
peripheral edema is present. Laboratory studies: Blood urea nitrogen 40 mg/dL Serum creatinine - 1.0
mg/dL. Serum sodium - 134 mmol/L. Serum potassium - 3.8 meq/L. Serum chloride - 108 meq/L. Serum
bicarbonate - 16 meq/L. Which urinalysis results best correspond to this patients condition?
A. No protein, pH 7, specific gravity 1.005
B. No protein, pH 7, specific gravity 1.030
C. 1 + protein, pH 5, specific gravity 1.005
D. *1 + protein, pH 5, specific gravity 1.030
E. No protein, pH 5, specific gravity, 1.005
231. A 17-year-old student presents with a 2-week history of periorbital and lower extremity swelling
that developed over 3 to 4 days. The patient had been well until this point. He takes no medications and
has no history of recreational drug use. On examination, blood pressure is 110/70 mm Hg, pulse rate is
92/min, and temperature is 37 °C (98.6 °F). Skin examination is normal. He has marked periorbital
edema. No jugulovenous distention is present. The lungs are clear, and the heart is in regular sinus
rhythm, with no murmur or gallop. The abdomen is nontender, and the liver and spleen are not palpable.
Scrotal edema is present, as is 4+ edema of the legs and thighs. Laboratory studies: Complete blood
count Normal Blood urea nitrogen
25 mg/dL Serum creatinine 1.2 mg/dL Serum total protein
6.5 g/dL Serum albumin
2.0 g/dL Urine protein:creatinine ratio 18 Urinalysis pH 6.0; specific
gravity 1.020; 4+ proteinuria, trace hematuria; many hyaline, granular, and fatty casts Renal biopsy
shows 15 glomeruli. Light microscopy is normal. Immunofluorescence shows nonspecific staining for
C3. Electron microscopy shows fusion of podocyte foot processes. What is the renal diagnosis in this
patient?
A. Membranous nephropathy
B. *Minimal change disease
C. Membranoproliferative glomerulonephritis
D. Focal and segmental glomerulonephritis
E. Alports disease
232. The condition of a 50-year-old obese woman with a 5-year history of mild hypertension controlled
by a thiazide diuretic is being evaluated because proteinuria was noted during her routine yearly medical
visit. Physical examination disclosed a height of 167.6 cm (66 in.), weight 91 kg (202 lb), blood pressure
130/80 mmHg, and trace pedal edema. Laboratory values are as follows:Serum creatinine: 106 jxmol/L
(1.2 mg/dL) Creatinine clearance: 87 mL/min Urinalysis: pH 5.0; specific gravity 1.018; protein 3 + ; no
glucose; occasional coarse granular cast Urine protein excretion: 5.9 g/d The results of a renal biopsy are
:sixty percent of the glomeruli appeared sclerotic as “halfmoons”; the remainder were unremarkable. The
most likely diagnosis is
A. hypertensive nephrosclerosis
B. focal and segmental sclerosis
C. minimal-change (nil) disease
D. membranous glomerulopathy
E. *crescentic glomerulonephritis
233. A 33-year-old obese woman has four healthy children from three previous uncomplicated term
pregnancies. She has a strong family history of hypertension but has never had hypertension in the
presence or absence of pregnancy. She was first seen for prenatal care by a physician 2 months after her
last menstrual period. Her pregnancy had been uneventful, and she had gained 3.6 kg (8 Ib). She was
seen 3 months after her last menstrual period. Blood pressure was 158/94 mm Hg, and she had trace
edema. Laboratory values at the time were as follows: Hematocrit 33.4%. Blood urea nitrogen 9 mg/dL.
Serum creatinine 0.4 mg/dL. Serum uric acid 1 mg/dL. 24-hour urinary protein - 100 mg. Creatinine
clearance - 150 mL/min. Urinalysis Trace proteinuria by dipstick. The patient is seen 1 week later. Her
blood pressure is 162/92 mm Hg. She has trace proteinuria, and laboratory values have not changed
significantly. What is the best course of action?
A. Start ramipril therapy
B. *Start methyldopa therapy
C. Start atenolol therapy
D. Check her blood pressure in 1 week and advise the patient that better control of blood pressure will
reduce her risk for preeclampsia
E. Advise termination of pregnancy
234. A 31-year-old white woman with diabetes presents for management of her hypertension. She
developed type 1 diabetes mellitus at 9 years of age and claims that the condition is under reasonable
control. However, she knows that she has diabetic retinopathy and proteinuria. Her blood pressure had
been elevated in the range of 140 to 150/90 mm Hg at the last three visits to her family physician. The
patient does not smoke, drink alcohol, or use recreational drugs. She adheres to a no-added-salt diet. The
only medication that she takes is insulin. On examination, blood pressure is 152/90 mm Hg seated and
146/88 mm Hg standing. Body weight is 82 kg (181 Ib). The examination is normal other than
nonproliferative diabetic retinopathy. What is the most appropriate antihypertensive therapy for this
patient?
A. Dihydropyridine calcium channel blocker
B. Angiotensin receptor blocker
C. *Angiotensin-converting enzyme inhibitor
D. Intensified lifestyle modification
E. none of them
235. A 59-year-old white male computer analyst is referred for evaluation of hypertension (185/95 mm
Hg) discovered during a blood pressure screening at his workplace. The patient states that he is well and
has not seen a physician in many years. He describes himself as “a fitness freak, as he is an active jogger,
abstains from alcohol, and limits his salt and fat intake. He denies any knowledge of hypertension,
cardiovascular disease, renal disease, or diabetes mellitus. He takes no medications regularly. Family
history is significant in that his father was known to be hypertensive and died of a stroke at 64 years of
age. His older brother is being treated for hypertension. On examination, the patient appears well, with a
blood pressure of 174/98 mm Hg while seated and standing. Body weight is 71 kg (157 Ib), and height is
178 cm (70). Optic fundus examination is significant for grade II hypertensive retinopathy. The
remainder of the examination is normal. Complete blood count, electrolyte panel, blood urea nitrogen
level, creatinine concentration, thyroid-stimulating hormone level, and results of urinalysis are normal.
Electrocardiography demonstrates normal sinus rhythm with left ventricular hypertrophy. To reduce the
patient’s cardiovascular morbidity and mortality, which therapy would you prescribe?
A. Doxazosin
B. *Losartan
C. Atenolol
D. Hydralazine
E. Niphedipdin
236. Two weeks after therapy is initiated in the 31-year-old white woman with diabetes presents for
management of her hypertension Who developed type 1 diabetes mellitus at 9 years of age and claims
that the condition is under reasonable control, her blood pressure decreases from 150/90 mm Hg to
128/80mm Hg, and she feels well. Repeated laboratory testing reveals an increase in serum creatinine
concentration from 1.9 mg/dL to 2.1 mg/dL. The potassium concentration is 4.2 mgld L. Which of the
following is the most appropriate course of action?
A. Discontinue antihypertensive therapy
B. Perform noninvasive screening for possible renal artery stenosis
C. Perform renal angiography
D. *Continue antihypertensive therapy and monitor kidney function
E. none of them
237. A 50-year-old previously healthy man presents with acute shortness of breath, right pleuritic chest
pain, and pink sputum. He has no fever or chills. For the past month, he has noticed swelling of the
ankles. He has had no prior symptoms of dyspnea on exertion, paroxysmal nocturnal dyspnea, or
orthopnea. He has had no joint pain or skin rash. He takes no medications and does not smoke. On
examination, the patient is alert but in mild respiratory distress. Blood pressure is 152/100 mm Hg, pulse
rate is 100/min, and respiratory rate is 22/min. There is no jugulovenous distention and no rash. The
lungs are clear. Cardiac examination shows regular sinus rhythm, with no gallop, murmur, or rub.
Abdominal examination shows no hepatosplenomegaly. The patient has 2+ to 3+ edema of the ankles
and legs. Laboratory studies: Leukocyte count 8,5 109L Platelet count – 200 109 /L. Hemoglobin - 14
g/dL. Hematocrit - 42%. Blood urea nitrogen 18 mg/dL. Serum creatinine - 1.4 mg/dL. Serum sodium 138 meq/L. Serum chloride - 105 meq/L. Serum potassium - 4.1 meq/L. Serum bicarbonate - 23 meq/L.
Serum total protein - 5.9 g/dL. Serum albumin - 1 .9 g/dL. Serum cholesterol - 300 mg/dL. Urinalysis
Specific gravity 1.015; 4+ proteinuria; oval fat bodies, granular casts, 3-5 erythrocytes/hpf 24-hour urine
protein 10g Arterial blood gasespH 7.46; Po280 mm Hg; Pco233 mm Hg Serum C380 mg/dL Serum
C425 mg/dL Antinuclear antibodies Negative Chest radiography shows clear lung fields and normal
heart size. Ventilation-perfusion scanning reveals a mismatch in the right lower lung field. Sonography
of lower extremities shows right femoral vein thrombosis. Which renal disease is most likely in this
patient?
A. Goodpastures syndrome
B. *Membranous nephropathy
C. Wegener’s granulomatosis
D. Lupus nephritis
E. Microscopic polyangiitis
238. A 59-year-old white male computer analyst is referred for evaluation of hypertension (185/95 mm
Hg) discovered during a blood pressure screening at his workplace. The patient states that he is well and
has not seen a physician in many years. He describes himself as “a fitness freak, as he is an active jogger,
abstains from alcohol, and limits his salt and fat intake. He denies any knowledge of hypertension,
cardiovascular disease, renal disease, or diabetes mellitus. He takes no medications regularly. Family
history is significant in that his father was known to be hypertensive and died of a stroke at 64 years of
age. His older brother is being treated for hypertension. On examination, the patient appears well, with a
blood pressure of 174/98 mm Hg while seated and standing. Body weight is 71 kg (157 Ib), and height is
178 cm (70). Optic fundus examination is significant for grade II hypertensive retinopathy. The
remainder of the examination is normal. Complete blood count, electrolyte panel, blood urea nitrogen
level, creatinine concentration, thyroid-stimulating hormone level, and results of urinalysis are normal.
Electrocardiography demonstrates normal sinus rhythm with left ventricular hypertrophy. To reduce the
patient’s cardiovascular morbidity and mortality, which therapy would you prescribe?
A. Doxazosin
B. *Losartan
C. Atenolol
D. Hydralazine
E. Niphedipdine
239. A 58-year-old black woman presents for routine follow-up of diabetes mellitus and hypertension.
She feels well but states that she stopped taking verapamil because of constipation. Current medications
include glipizide, pravastatin, and aspirin; evidence of drug intolerance includes angiotensin-converting
enzyme inhibitor cough. On examination, blood pressure is 156/92 mm Hg seated and standing. Except
for the patient’s findings for background diabetic retinopathy, the remainder of the examination is
normal. Recent laboratory values are a serum creatinine concentration of 1.6 mg/dL, 24-hour urinary
protein excretion of 1.5 g/d, and creatinine clearance of 45 mL/min. On the basis of recent evidence,
what is the most efficacious therapy to slow the progression of the patient’s type 2 diabetic nephropathy?
A. Angiotensin-converting enzyme inhibitor
B. *Angiotensin receptor blocker
C. Dihydropyridine calcium antagonist
D. β-Blocker
E. none of them
240. A 66-year-old man has had a several-week history of fatigue and ankle swelling. His appetite is
normal, but his body weight has increased 4.5 kg (10 Ib). There is no history of exertional dyspnea,
paroxysmal nocturnal dyspnea, or orthopnea. He has had hypertension for 10 years, and diabetes was
diagnosed 4 months ago. He takes hydrochlorothiazide, 25 mg/d, and metoprolol, 50 mg/d. On
examination, the patient is alert and in no distress. Blood pressure is 120/75 mm Hg, pulse rate is 82/min,
and temperature is 36.9 °C (98.4 °F). Skin examination is normal. The lungs are clear. Cardiac
examination shows regular sinus rhythm, with no murmur or gallop. The abdomen is slightly protuberant
with shifting dullness, but no hepatosplenomegaly is noted. There is 4+ edema of the legs and thighs and
1+ edema of the sacrum. Laboratory studies: Complete blood count Normal Hemoglobin A1c 7.4%.
Blood urea nitrogen - 20 mg/dL. Serum creatinine - 0.9 mg/dL. Serum sodium - 141 meq/L. Serum
chloride - 104 meq/L. Serum potassium - 4.3 meq/L. Serum total protein - 4.4 g/dL. Serum albumin - 1.7
g/dL. Serum cholesterol - 376 mg/dL. 24-hour urine protein 8.5 g. Urinalysis pH 5.5; specific gravity 1
.020; protein 4+, trace hemoglobin Urine microscopy shows many granular and hyaline casts and oval fat
bodies. Monoclonal protein is identified on urine immunoelectrophoresis. Plasma immunoelectrophoresis
shows an IgG level of 452 mg/dL, IgA of 284 mg/dL, 1gM of 122 mg/dL, K of 550 mg/dL, and 2 of 193
mg/dL with a homogenous M band. What renal disease is most likely in this patient?
A. Idiopathic membranous glomerulopathy
B. Diabetic nephropathy
C. Focal and segmental glomerulosclerosis
D. AA amyloidosis
E. *AL amyloidosis
241. A 33-year-old obese woman has four healthy children from three previous uncomplicated term
pregnancies. She has a strong family history of hypertension but has never had hypertension in the
presence or absence of pregnancy. She was first seen for prenatal care by a physician 2 months after her
last menstrual period. Her pregnancy had been uneventful, and she had gained 3.6 kg (8 Ib). She was
seen 3 months after her last menstrual period. Blood pressure was 158/94 mm Hg, and she had trace
edema. Laboratory values at the time were as follows: Hematocrit - 33.4%. Blood urea nitrogen - 9
mg/dL. Serum creatinine - 0.4 mg/dL. Serum uric acid - 3.1 mg/dL. 24-hour urinary protein - 100 mg.
Creatinine clearance - 150 mL/min. Urinalysis Trace proteinuria by dipstick. The patient is seen 1 week
later. Her blood pressure is 162/92 mm Hg. She has trace proteinuria, and laboratory values have not
changed significantly. What is the best course of action?
A. Start ramipril therapy
B. *Start methyldopa therapy
C. Start atenolol therapy
D. Check her blood pressure in 1 week and advise the patient that better control of blood pressure will
reduce her risk for preeclampsia
E. Advise termination of pregnancy
242. A 60-year-old woman with adult polycystic kidney disease is seen urgently in the office for high
fever. The illness started abruptly and involves chills and dysuria. She has had hypertension for the past 5
years, treated with quinapril and hydrochlorothiazide. She has lost approximately 8 kg (17 Ib) of weight
over the last 3 months. On physical examination, the patient appears thin and frail. Body weight is 48 kg
(106 Ib). Blood pressure is 90/70 mm Hg, pulse rate is 110/min, respiratory rate is 24/min, and body
temperature is 39 °C (102 °F). The kidneys are palpable bilaterally, and she has right costovertebral angle
tenderness. Serum creatinine concentration is 1.1 mg/dL, and urinalysis shows pyuria and bacteriuria.
The patient is admitted and prescribed intravenous ampicillin and gentamicin to treat pyelonephritis.
Why does the dosage of antibiotic need to be adjusted in this patient?
A. The infection is in a cyst
B. *The glomerular filtration rate is reduced
C. The patient is septic
D. The patient has hypertension
E. none of them
243. A 46-year-old man with chronic kidney disease secondary to biopsy-proven focal and segmental
glomerulosclerosis returns for routine follow-up. The hematocrit is 28%, and potentially correctable
causes of anemia have been excluded. Therapy with recombinant human erythropoietin is recommended.
In patients with chronic kidney disease and pre-end-stage renal disease, what is a benefit of therapy with
erythropoietin to effectively treat anemia?
A. Reduced mortality
B. Decreased cardiovascular event rates
C. Normalization of hypertension
D. *Regression of left ventricular hypertrophy
E. none of them
244. A 42-year-old man complained of headache in occipital are. On physical examination, the skin was
pale; there was face and hand edema, blood pressure of 170/135 mm Hg. On EchoCG, there was
concentric hypertrophy of the left ventricle Ultrasound examination of the kidneys revealed thinned
cortical layer. Urinalysis showed proteinuria of 3.6 g/day. What is the diagnosis?
A. Essential arterial hypertension
B. Chronic pyelonephritis
C. *Chronic glomerulonephritis
D. Allergic interstitial nephritis
E. Goodpastures syndrome
245. A 21- year-old patient with a history of preceding streptococcal infection complains of malaise,
headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of
100/min, RR of 20/min, the urinalysis showed increased protein, red cell casts and hyaline casts. What is
your diagnosis in this patient?
A. *Acute glomerulonephritis
B. Acute pyelonephritis
C. Chronic renal failure
D. Acute tubular necrosis
E. Rheumatic fever
246. A 71-year-old man had non-Hodgkins lymphoma diagnosed 4 months ago. Treatment included
chemotherapy with rituximab and cyclosphosphamide, prednisone, and vincristine and doxorubicin,
followed by radiation therapy. He has had persistent anemia. He has had hypertension for 15 years and
prostatic hypertrophy, treated with doxazosin, for 10 years. He presents to the emergency department
with polyuria, weakness, and lassitude. On physical examination, blood pressure is 124/78 mm Hg, with
no orthostatic changes; pulse rate, 96/min; respiratory rate, 18/min; and temperature 36.8 °C (98.2 °F).
Mucous membranes are moist. There is no neck vein distention or hepatojugular reflux. The cardiac
examination is normal, and the chest is clear. The abdomen is benign. No lower extremity edema is
present. The electrocardiogram is normal. Hematocrit is 31%, and leukocytosis is present, with a normal
platelet count. The serum creatinine concentration, previously normal, is now 2.4 mg/dL. Urinalysis
shows a pH of 6.0 and 1 + proteinuria, but no hematuria or ketonuria. No formed elements appear on
microscopic examination. Urine sodium and osmolality values have been requested. What is the most
important next test to determine the reason for decreased renal function in this patient?
A. Calculate the ratio of blood urea nitrogen to creatinine
B. *Perform renal ultrasonography
C. Perform renal scanning
D. Administer 1.5 L of normal saline as a fluid trial
E. Perform renal biopsy
247. A 58-year-old black woman presents for routine follow-up of diabetes mellitus and hypertension.
She feels well but states that she stopped taking verapamil because of constipation. Current medications
include glipizide, pravastatin, and aspirin; evidence of drug intolerance includes angiotensin-converting
enzyme inhibitor cough.
On examination, blood pressure is 156/92 mm Hg seated and standing. Except for the patient’s findings
for background diabetic retinopathy, the remainder of the examination is normal. Recent laboratory
values are a serum creatinine concentration of 1.6 mg/dL, 24-hour urinary protein excretion of 1.5 g/d,
and creatinine clearance of 45 mL/min. On the basis of recent evidence, what is the most efficacious
therapy to slow the progression of the patient’s type 2 diabetic nephropathy?
A. Angiotensin-converting enzyme inhibitor
B. *Angiotensin receptor blocker
C. Dihydropyridine calcium antagonist
D. β-Blocker
E. None of them
248. A 39-year-old black man presents for hypertension discovered during a pre-employment
examination. He is healthy but has a family history of hypertension in both parents and two siblings. He
has no history of cardiovascular disease and does not use tobacco, alcohol, or recreational drugs. He is
taking no medications. The patient appears well. Height is 173 cm (68), body weight is 78 kg (172 Ib),
and blood pressure is 160/1 02 mm Hg seated and standing. The physical examination is otherwise
normal. A complete blood count and electrolyte panel are normal. The serum creatinine concentration is
1 .8 mg/dL, and urinalysis reveals 2+ proteinuria. Which is the most appropriate antihypertensive therapy
for this patient?
A. Intensive lifestyle modification
B. *Angiotensin-converting enzyme inhibitor
C. Diuretic
D. Nondihydropyridine calcium channel blocker
E. None of them
249. A 57-year old woman comes to the emergency department because of a "very high fever." She has
diabetes mellitus and hemodialysis-dependent renal failure. She also has hypertension and is status-post
total abdominal hysterectomy. She is frail appearing and diaphoretic. Her blood pressure is 170/90 mm
Hg and temperature is 38.3 C (101.0 F). Her neck is supple without any specific meningismus. She has a
Tesio catheter in her left subclavian vein. Her lungs are clear and she has no costovertebral angle
tenderness. Her laboratory studies show a white blood cell count of 23,000/mm3 and a hematocrit of
31%. Her urinalysis is dipstick negative for white blood cells. The most appropriate next step in
management is to
A. begin antibiotic therapy with gentamycin
B. *begin antibiotic therapy with vancomycin and gentamycin
C. order urinalysis analysis and culture
D. perform a lumbar puncture and send CSF for analysis and culture
E. schedule emergent surgical removal of her Tesio catheter
250. An 18-year-old male high school student presents to the emergency department with confusion,
nausea, headache, and decreased vision after a camping trip. The patient’s friends state that he became ill
12 to 14 hours ago. Laboratory studies: Blood urea nitrogen 14 mg/dL Serum creatinine 1.0 mg/dL
Serum sodium
140 meq/L Serum chloride 100 meq/L Serum potassium 4 meq/L Serum bicarbonate
12 meq/L Serum glucose
108 mg/dL Measured serum osmolality
326 Serum ketones
Negative Serum lactate
0.7 meq/L Arterial blood gases pH 7.29, PCO2
26 mm Hg What
ingestion best explains the acid-base abnormalities?
A. Ethanol
B. *Methanol
C. Isopropyl alcohol
D. Salicylate
E. None of them
251. Two weeks after therapy is initiated in the 31-year-old white woman with diabetes presents for
management of her hypertension Who developed type 1 diabetes mellitus at 9 years of age and claims
that the condition is under reasonable control, her blood pressure decreases from 150/90 mm Hg to
128/80mm Hg, and she feels well. Repeated laboratory testing reveals an increase in serum creatinine
concentration from 1.9 mg/dL to 2.1 mg/dL. The potassium concentration is 4.2 mgld L. Which of the
following is the most appropriate course of action?
A. Start bicarbonate supplementation and add insulin to control blood glucose
B. *Continue antihypertensive therapy and monitor kidney function
C. Institute plasma exchange to treat acidemia
D. Initiate ethanol drip and continue insulin supplementation
E. Perform emergency contrast computed tomography of the abdomen and pelvis
252. A 72-year-old white man returns for a follow-up visit subsequent to admission to another hospital
for hypertension. He was seen in the local emergency department for severe musculoskeletal back pain,
where the treating physician noted elevated blood pressure (200/92 mm Hg) and a serum creatinine
concentration of 1.6 mg/dL. Results of other laboratory tests were normal. The patient was admitted for
evaluation and management of back pain, and the attending physician obtained additional studies relating
to the patients hypertension. Renal ultrasonography was negative for calculus, mass, or obstruction;
kidney size was 11 cm on the right and 12 cm on the left. Renal artery duplex ultrasonography was
suggestive of right renal artery stenosis. Renal angiography revealed a normal left renal artery and 50%
stenosis in the right renal artery. Analysis of renal vein renin activity showed a low inferior vena cava
value of 1.5 ?g/L/h, right renal vein value of 2.0 ?g/L/h, left renal vein value of 2.0 ?g/L/h, and a high
inferior vena cava value of 2.0 ?g/L/h. The plasma renin activity is 1 .0 mg/LIh, and the plasma
aldosterone level is 8.0 ng/dL.The thyroid-stimulating hormone level is 1.0 ?U/mL. Review of your
office records confirms that the patient has a 22-year history of hypertension controlled with a ?-blocker
and diuretic therapy. The serum creatinine concentration has been stable at 1.6 mgldL for more than 3
years, and urinalysis shows 1 + proteinuria. What is the cause of this man’s hypertension?
A. *Primary hypertension
B. Hypothyroidism
C. Primary hyperaldosteronism
D. Renovascular hypertension
E. Pheochromocytoma
253. An 18-year-old white man is seen in your office because of blood on urine dipstick analysis during
a sports physical. He has no history of gross hematuria, recent fever or chills, or upper respiratory illness.
He has been in good health. He takes cetirizine for seasonal allergies. He has no family history of renal
diseasReview of systems is negativOn examination, blood pressure is 140/98 mm Hg, weight is 80 kg
(176 Ib), and height is 170 cm (67’). He has a muscular builThe remainder of the physical examination is
normal. Repeated urinalysis at2 p.m. reveals a pH of 5.0, specific gravity of 1.015,2+ blood, 2+ protein.
Which test is the best option to assist in diagnosis?
A. Renal ultrasonography
B. Cystoscopy
C. Magnetic resonance angiography of renal arteries
D. *Urinary protein-to-creatinine ratio
E. Renal computed tomography
254. A 34-year-old pregnant woman with a 5-year history of biopsy-diagnosed hypertensive
nephropathy has been followed in obstetric clinic for 3 months after her last menstrual period. One year
ago, her serum creatinine concentration was 1 .6 mg/dL. Her pregnancy has been uneventful. Her blood
pressure has been well controlled on a combination of methyldopa and hydralazine and is currently
130/85 mm Hg. She has trace edema. Laboratory studies: Hematocrit 37% Leukocyte count Normal
Platelet count
Normal Peripheral smear No schistocytes Blood urea nitrogen 14 mg/dL Serum
creatinine 1.8 mg/dL Serum uric acid 4.9 mg/dL Urinalysis Specific gravity, 1.010; urinary protein 4+ by
dipstick; no glucosuria, hematuria, or ketonuria Microscopic urine examination shows rare broad casts.
Liver function tests are normal. Which one of the following statements about the patients course is true?
A. She has developed preeclampsia.
B. *The course is most consistent with progression of her chronic renal disease.
C. She has developed microangiopathic hemolytic anemia.
D. She has developed prerenal azotemia.
E. Her blood pressure is likely to improve during the course of her pregnancy.
255. A 58-year-old nun comes to your office because of lethargy, mild nausea, and weakness for the past
2 weeks. Three years ago, pulmonary sarcoidosis was diagnosed by biopsy. Three months ago, the
patient began taking oral calcium (1500 mg/d) and 25-hydroxyvitamin D as treatment for osteoporosis
that was diagnosed by screening bone density testing. She has chronic hypertension that is well
controlled with metoprolol, 50 mg/d. On examination, the patient appears thin but well nourished and is
in no distress. She is oriented to time, date, and place. Blood pressure is 140/80 mm Hg, pulse rate
80/min, temperature 37 °C (98.6°F). The thyroid is normal, and the neck veins are not distended. The
lungs are clear. Cardiac examination shows regular sinus rhythm, no murmur, and normal first and
second heart sounds. The abdomen is not tender, the liver and spleen are not palpable, and no mass is
present. There is no edema in the lower extremities, and reflexes are 1 + and symmetrical. Laboratory
studies: Hemoglobin
13.8 g/dL Hematocrit
38% Leukocyte count
5600/?L Blood urea
nitrogen 24 mg/dL Serum creatinine 2.2 mg/dL (was 1.0 mg/dL 3 months ago) Serum sodium 141
meq/L Serum potassium 4.4 meq/L Serum chloride
105 meq/L Serum bicarbonate
24 meq/L
Serum calcium 12.8 mg/dL Serum phosphorus
3.5 mg/dL Serum parathyroid hormone 18 pg/mL
Urinalysis pH 5.5; specific gravity 1.010; no proteinuria, hematuria, or glucosuria; no cells on
microscopy Serum and urine immunoglobulins showed no monoclonal protein. A polyclonal increase in
IgG is present. Renal ultrasonography demonstrates no hydronephrosis and no calculi. What is the most
likely cause of this patients acute renal failure?
A. Myeloma kidney
B. *Acute interstitial nephritis
C. Hypercalcemia
D. Acute glomerulonephritis
E. Bilateral renal artery stenosis
256. A 47-year-old man calls Monday morning seeking help with “the worst headache ever” Friday
night and Saturday. The headache was associated with severe lethargy and intermittent confusion. He
recovered and has felt well for the past 24 hours. He states that he does not have fever or neurologic or
cardiovascular symptoms. His medical history is significant for hypertension and recurrent urinary tract
infections related to his known autosomal dominant polycystic kidney disease. He is concerned because
his father died of a stroke during dialysis. The serum creatinine concentration is 2.6 mg/dL. What do you
recommend for this patient?
A. Make an office appointment for him to see you this week
B. Arrange a consultation with the neurology/headache clinic
C. Order computed tomography of the head without contrast
D. *Arrange urgent magnetic resonance angiography of the head
E. None of them
257. A 35-year-old man had HIV infection diagnosed 2 months ago. His serum creatinine concentration
was 0.6 mg/dL. Treatment with highly active antiretroviral therapy with zidovudine, lamivudine, and
abacavir was recommended, but he wished to wait before starting treatment. He is brought to clinic by a
friend who states that the patient has had fever, confusion, and disorientation for 1 day. Physical
examination reveals blood pressure 110/70 mm Hg and pulse rate 1 00/min that is regular supine and
standing. The chest is clear, without cardiac murmur or gallop, and the abdomen is normal. Moderate
bilateral lower extremity edema is present. Laboratory studies: Hemoglobin - 7.8 g/dL Leukocyte count 10,2000/?L Platelet count - 19,000/?L Blood urea nitrogen 37 mg/dL Serum creatinine - 2.7 mg/dL
Serum sodium - 136 meq/L Serum potassium 5.2 meq/L Serum chloride - 99 meq/L Serum bicarbonate
- 22 meq/L Urinalysis Specific gravity 1.030; 3+ hematuria, trace proteinuria, trace ketonuria, no
glucosuria Urinary microscopic examination shows a few erythrocytes, but no erythrocyte casts. The
lactate dehydrogenase level is elevated. Peripheral blood smear shows many schistocytes. What is the
most likely cause of this patient’s renal failure?
A. *Thrombotic thrombocytopenic purpura
B. HIV-associated nephropathy
C. Surreptitious ingestion of antiretroviral drugs
D. Outpatient acute tubular necrosis
E. HIV-associated immune-mediated glomerulonephritis
258. 48-year-old white male plumber transfers to your practice after a change of insurance status. His
medical history is positive for primary hypertension without target organ damage. He has no history of
renal or prostatic disease. Laboratory values obtained from his former primary care physician show
normal results for blood urea nitrogen, serum creatinine, electrolytes, urinalysis, prostate-specific
antigen, and electrocardiography. He takes the ?-blocker doxazosin, 2 mg at bedtime. On examination,
blood pressure is 146/92 mm Hg seated and standing. Body weight is 84 kg (185 Ib). The remainder of
the examination is normal. What is the appropriate course of action regarding the patient’s
antihypertensive therapy?
A. Increase doxazosin to 4 mg
B. Advise high dietary intake of calcium and potassium
C. *Discontinue doxazosin therapy and consider an alternative agent
D. Advise a low-sodium diet
E. none of them
259. 24-year-old graduate student has a several-week history of aching pains in knees, ankles, and
elbows and intermittent abdominal pain. Three days ago, he had two episodes of painless hematuria. He
has no fever, chills, or weight loss. There is no history of hair loss, but he has had an intermittent,
nonpruritic rash located below the knees bilaterally. There has been no recent upper respiratory infection.
He takes acetaminophen occasionally for the aching joints. He has no history of kidney disease or
intravenous drug use. On examination, the patient appears well. Weight is 84.4 kg (186 Ib). Blood
pressure is 120/84 mm Hg, pulse rate is 70/min, and temperature is 37.2 °C (99 °F). No jugulovenous
distention is present. The lungs are clear, and cardiac examination shows regular sinus rhythm with no
murmur. On abdominal examination, the liver and spleen are not palpable, and no mass or tenderness is
present. Pulses in the extremities are normal and there is no edema, but the patient has a petechial
macular papular rash over the lower extremities. Laboratory studies: Leukocyte count - 8400/?L
Hemoglobin - 14.1 mgldL Hematocrit - 41 % Blood urea nitrogen - 12 mg/dL Serum creatinine
1.1
mg/dL Serum sodium - 138 meq/L Serum chloride - 104 meq/L Serum potassium - 4.0 meq/L Serum
bicarbonate - 26 meq/L Serum antinuclear antibody Negative Serum C3 - 85 mg/dL Serum C4 - 21
mg/dL Urine protein :creatinine ratio0.2 Urinalysis Specific gravity 1.030, pH 5.0, 1 + proteinuria, 4+
hematuria Urine microscopy reveals many dysmorphic erythrocytes and erythrocyte casts. The lung
fields are clear on chest radiography. Biopsy of skin lesion shows IgA deposition and leukocytoclastic
change. What is the most likely cause of renal disease in this patient?
A. Lupus nephritis
B. Acute post—streptrococcal glomerulonephritis
C. *Henoch-Sch nlein purpura
D. Allergic interstitial nephritis
E. Goodpastures syndrome
260. A 38-year-old black man presents for hypertension discovered during a pre-employment
examination. He is healthy but has a family history of hypertension in both parents and two siblings. He
has no history of cardiovascular disease and does not use tobacco, alcohol, or recreational drugs. He is
taking no medications. The patient appears well. Height is 173 cm (68), body weight is 78 kg (172 Ib),
and blood pressure is 158/1 02 mm Hg seated and standing. The physical examination is otherwise
normal. A complete blood count and electrolyte panel are normal. The serum creatinine concentration is
1 .8 mg/dL, and urinalysis reveals 2+ proteinuria. Which is the most appropriate antihypertensive therapy
for this patient?
A. Intensive lifestyle modification
B. Diuretic
C. Nondihydropyridine calcium channel blocker
D. *Angiotensin-converting enzyme inhibitor
E. none of them
261. A 28-year-old woman presents for evaluation of recurrent kidney stones that she says ‘contain
calcium.” She estimates that she has passed four stones during the past 4 years. She currently has no
symptoms of renal colic. For several years, she has had dry eyes and dry mouth. She also describes
symptoms of Raynauds phenomenon. Crohns disease was diagnosed 10 years ago; the patient is currently
asymptomatic and passes one formed stool daily. She takes no medications. There is no family history of
renal stone disease. On examination, the patient is alert and healthy. Blood pressure is 115/74 mm Hg,
pulse rate is 72/min, and temperature is 37 °C (98.6 °F). The skin is clear, and the joints are normal. The
lungs are clear. Cardiac examination shows regular sinus rhythm and no murmur. The liver and spleen
are not palpable, and the abdomen is not tender. Plain abdominal radiography shows multiple
calcifications overlying both renal shadows. Laboratory studies: Hemoglobin - 13.2 g/dL Hematocrit 39% Leukocyte count - 7400/?L Blood urea nitrogen - 18 mg/dL Serum creatinine - 0.9 mg/dL Serum
sodium - 138 meq/L Serum potassium - 2.8 meq/L Serum chloride - 109 meq/L Serum bicarbonate - 19
meq/L Serum calcium - 9.1 mg/dL Serum phosphorus - 3.2 mg/dL Urinalysis pH 6.0; specific gravity
1.020; trace hematuria, no proteinuria Arterial blood pH 7.29 What is the most likely etiology of this
patients renal stone disease?
A. Idiopathic hypercalciuria
B. Primary hyperthyroidism
C. *Distal renal tubular acidosis
D. Enteric hyperoxaluria
262. A 40-year-old man has recurrent nephrolithiasis due to idiopathic hypercalciuria. He has had more
than 40 calcium oxalate stones in the past 5 years. He is started on hydrochlorothiazide therapy and a
low-sodium diet. During treatment, his 24-hour urinary calcium concentration decreases from 385 mg/d
to 180 mg/d. No new stones have formed in the past 6 months; however, hypokalemia has developed
(serum potassium level, 2.9 meq/L). Taking the hypokalemia into account, what therapy should the
patient receive for hypercalciuric stone disease?
A. High-potassium diet plus hydrochlorothiazide
B. Acetazolamide plus hydrochlorothiazide
C. Magnesium oxide plus hydrochlorothiazide
D. *Amiloride plus hydrochlorothiazide
E. none of them
263. 75. A 58-year-old nun comes to your office because of lethargy, mild nausea, and weakness for
the past 2 weeks. Three years ago, pulmonary sarcoidosis was diagnosed by biopsy. Three months ago,
the patient began taking oral calcium (1500 mg/d) and 25-hydroxyvitamin D as treatment for
osteoporosis that was diagnosed by screening bone density testing. She has chronic hypertension that is
well controlled with metoprolol, 50 mg/d. On examination, the patient appears thin but well nourished
and is in no distress. She is oriented to time, date, and place. Blood pressure is 140/80 mm Hg, pulse rate
80/min, temperature 37 °C (98.6°F). The thyroid is normal, and the neck veins are not distended. The
lungs are clear. Cardiac examination shows regular sinus rhythm, no murmur, and normal first and
second heart sounds. The abdomen is not tender, the liver and spleen are not palpable, and no mass is
present. There is no edema in the lower extremities, and reflexes are 1 + and symmetrical. Laboratory
studies: Hemoglobin
13.8 g/dL Hematocrit
38% Leukocyte count
5600/?L Blood urea
nitrogen 24 mg/dL Serum creatinine 2.2 mg/dL (was 1.0 mg/dL 3 months ago) Serum sodium 141
meq/L Serum potassium 4.4 meq/L Serum chloride
105 meq/L Serum bicarbonate
24 meq/L
Serum calcium 12.8 mg/dL Serum phosphorus
3.5 mg/dL Serumparathyroid hormone 18 pg/mL
Urinalysis pH 5.5; specific gravity 1.010; no proteinuria, hematuria, or glucosuria; no cells on
microscopy Serum and urine immunoglobulins showed no monoclonal protein. A polyclonal increase in
IgG is present. Renal ultrasonography demonstrates no hydronephrosis and no calculi. What is the most
likely cause of this patients acute renal failure?
A. Myeloma kidney
B. *Acute interstitial nephritis
C. Hypercalcemia
D. Acute glomerulonephritis
E. Bilateral renal artery stenosis
264. A 40-year-old man complained of headache in occipital area. On physical examination, the skin
was pale; there was face and hand edema, blood pressure of 170/130 mm Hg. On EchoCG, there was
concentric hypertrophy of the left ventricle. Ultrasound examination of the kidneys revealed thinned
cortical layer. Urinalysis showed proteinuria of 3.5 g/day. What is the diagnosis
A. *Chronic glomerulonephritis
B. Essential arterial hypertension
C. Chronic pyelonephritis
D. Polycystic disease of the kidneys.
E. Cushing’s disease
265. A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating,
aching pain in lumbar area, a discomfort in urination, and frequent voiding. Pasternatsky’s sigh is
positive in both sides. On lab exam, WBC of 20.000/mcL; on urinalysis protein of 0.6g/L, leukocyturia,
bacteriuria. Your preliminary diagnosis.
A. *Acute pyelonephritis
B. Exacerbation pf chronic pyelonephritis
C. Acute glomerulonephritis
D. Acute cystitis
E. Nephrolithiasis
266. A 55-year-old man comes to the emergency department with pain on urination, fever and chills. He
also complains of perineal and suprapubic tenderness as well as dysuria and hesitancy. His allergies
include codeine, sulfonamides, and quinidine. Temperature is 38.5 C (101.3 F), blood pressure is 132/90
mm Hg, pulse is 88/min, and respirations are 18/min. Abdominal examination is remarkable for
suprapubic tenderness. Digital rectal examination demonstrates a swollen, boggy, and exquisitely painful
prostate gland. Laboratory studies show a leukocyte count of 11,500/mm3, creatinine of 0.9 mg/dL, and
blood urea nitrogen of 16 mg/dL. A urinalysis shows too numerous to count white blood cells and Gramnegative rods. The most appropriate treatment for this patient is
A. amoxicillin/clavulanate 875 mg by mouth twice daily for 14 days
B. ceftriaxone 1 gram intravenously daily for 5 days
C. *ciprofloxacin 500 mg by mouth twice daily for 14 days
D. clindamycin 300 mg 4 times daily for 10 days
E. trimethoprim-sulfamethoxazole 1 double strength tablet twice daily for 14 days
267. A 30-year-old woman comes to the clinic complaining of loss of control of urination and
"dribbling" of urine. She has had recurrent urinary tract infections over the past 11 months, which were
treated with antibiotics. She has been following safe sex practices and denies any history of sexually
transmitted diseases, but complains of moderate pain during intercourse. Physical examination and pelvic
examination are normal. The most appropriate next investigation in this patient is
A. CT scan of the abdomen and pelvis
B. laparoscopy
C. pelvic sonography
D. renal sonography
E. *voiding cystourethrogram
268. A 78-year-old woman is admitted to the hospital because of fever, flank pain, and mental
obtundation. On arrival to the hospital, she was minimally responsive and was found to have a white
blood cell count of 43,000/mm3 with a profound left shift. Urinalysis revealed packed white cells. A
renal ultrasound demonstrated a left hydronephrosis and hydroureter. A CT scan confirmed the presence
of an obstructing stone. Her vital signs on admission showed a temperature of 39.5 C (103.1 F), blood
pressure of 80/40 mm Hg, pulse of 112/min, and respirations of 18/min. Intravenous pressors were
initiated. Three sets of blood cultures came back positive for Gram-negative rods within 2 hours. The
most appropriate next step in management is to
A. administer antibiotics, intravenously, and observe
B. *insert a nephrostomy tube, percutaneously
C. perform extracorporeal shock wave lithotripsy (ESWL)
D. schedule cystoscopy and ureteral stent placement
E. schedule a nephrectomy
269. A 37-year-old comes to the clinic for a required pre-employment physical examination. She has no
past medical history and has no complaints. Her temperature is 37.0 C (98.6 F), blood pressure is 110/60
mm Hg, pulse is 63/min, and respirations are 14/min. She is currently menstruating. A urine culture,
which is required by her new job, reveals greater than 100,000 E. Coli colony-forming units. The most
appropriate next step in management of this patient's urine culture findings is
A. *no further management is indicated
B. prescribe ciprofloxacin, orally, for 14 days
C. prescribe trimethoprim-sulfamethoxazole, orally, for 3 days
D. repeat urine culture in 2 weeks
E. send her for urological evaluation
270. A 31-year-old woman presents to your office complaining of flank pain and fever for the past 2
days. She has a history of multiple urinary tract infections. She has suffered 2 in the previous 18 months
that were treated successfully with trimethoprim-sulfamethoxazole. She is sexually active and her last
menstrual period was 6 days ago. She takes no routine medications. Her temperature is 39.5 C (103.1 F),
blood pressure is 130/65 mm Hg, and pulse is 110/min. She has prominent right costovertebral angle
(CVA) tenderness. The most appropriate management of this patient is to
A. admit her to the intensive care unit
B. initiate therapy with ampicillin and gentamicin
C. obtain blood cultures and send her home pending results
D. *obtain urine cultures and initiate therapy with ampicillin and gentamicin
E. obtain urine cultures and send her home pending results
271. A 27-year-old college freshman complains of dysuria and urinary frequency. Urinalysis reveals 8to
10 WBCs per high-power field and numerousgram-negative bacteria. All of the following statements
concerning this disease are true EXCEPT that
A. a single dose of an antibiotic may be sufficient treatment
B. pregnant women with bacteriuria should be treated, even if asymptomatic
C. patients with flank pain or fever should be treated for 10 to 14 days
D. *patients with indwelling catheters should receive long-term suppression
E. radiological investigation is appropriate formales of any age after their first infection
272. A 72-year-old man has the sudden onset of suprapubic pain and oliguria. His temperature is 38.0°C
(100.4°F), pulse is 100/minute, respirations are 12/minute, and BP is 110/72 mm Hg. Abdominal
examination is only re_markable for a tender, distended urinary bladder.Immediate management of this
patient should be to
A. obtain a flat plate of the abdomen
B. perform abdominal ultrasonography
C. *insert a urethral catheter
D. administer furosemide IV
E. obtain an IVP
273. A man, aged 25, presents with facial edema, moderate back pains, body temperature of 37,5 С, BP
180/100 mmHg, hematuria [ up to 100 in v/f], proteinuria [2,0 g/L], hyaline casts - 10 in v/f., specific
gravity -1020. The onset of the disease is probably connected with acute tonsillitis 2 weeks ago. The
most likely diagnosis is:
A. Acute pyelonephritis
B. *Acute glomerulonephritis
C. Cancer of the kidney
D. Urolithiasis
E. Chronic glomerulonephritis
274. A 29-year-old woman is critically ill. The illness was manifested by oliguria, edema, severe
headache. Pasternatsky’s sigh is negative in both sides. On lab exam, WBC of 10.000/mcL; on urinalysis
protein of 1,6g/L, erythrocyturia. Your preliminary diagnosis.
A. *Acute pyelonephritis
B. Acute glomerulonephritis
C. Cancer of the kidney
D. Urolithiasis
E. Chronic glomerulonephritis
275. A 57-year-old man undergoes intravenous pyelography (IVP) as part of a workup for hypertension.
A 3-cm solitary radiolucent mass is noted in the left kidney; the study otherwise is normal. The man
complains of no symptoms referable to the urinary tract, and examination of urinary sediment is within
normal limits. Which of the following studies should be performed next?
A. Repeat intravenous pyelography in 6 months
B. Early-morning urine collections for cytology (three samples)
C. Selective renal arteriography
D. *Renal ultrasonography
E. CT scanning (with contrast enhancement) of the left kidney
276. A 24- year-old patient with a history of preceding streptococcal infection complains of malaise,
headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of
100/min, RR of 20/min, the urinalysis showed increased protein, red cell casts and hyaline casts. What is
your diagnosis?
A. Bacterial endocarditis
B. Essential hypertension
C. Rheumatic fever
D. Acute pyelonephritis
E. *Acute glomerulonephritis
277. A 31-year-old woman is critically ill. The illness was manifested by oliguria, edema, severe
headache. Pasternatsky’s sigh is negative in both sides. On lab exam, WBC of 10.000/mcL; on urinalysis
protein of 1,6g/L, erythrocyturia. Your preliminary diagnosis.
A. Acute pyelonephritis
B. *Acute glomerulonephritis
C. Urolithiasis
D. Cancer of the kidney
E. Chronic glomerulonephritis
278. Which area is more vulnerable to ischemic damage?
A. Subepicardium
B. Midmyocardium
C. *Subendocardium
D. Pericardium
E. Endocardium
279. A 40-year-old man complained of headache in occipital area. On physical examination, the skin
was pale; there was face and hand edema, blood pressure of 170/130 mm Hg. On EchoCG, there was
concentric hypertrophy of the left ventricle. Ultrasound examination of the kidneys revealed thinned
cortical layer. Urinalysis showed proteinuria of 3.5 g/day. What is the diagnosis?
A. *Chronic glomerulonephritis.
B. Essential arterial hypertension.
C. Chronic pyelonephritis.
D. Polycystic disease of the kidneys.
E. Chronic renal failure
280. A 19 year-old guy fell ill with acute nephritis after exposure. 2 weeks ago he suffered a sore throat.
Indicate the most likely etiology of nephritis.
A. Aurococcus
B. Pseudomonas aeruginosa
C. *hemolytic streptococcus
D. Candida
E. Colon bacillus
281. A patient A, aged 22, was diagnosed with chronic renal failure. The blood serum showed reductions
in the amount of calcium, increasing of alkaline phosphatise degree, and the radiograph of the forearm
bones and wrist confirmed signs of osteoporosis. Which of these drugs should be applied for treatment of
the patient’s osteopathy?
A. multivitamins and manganese
B. Calcium without vitamin D
C. Phosphorus and Vitamin B1
D. Zinc and molybdenum
E. *Vitamin D and calcium
282. A patient on the third day after the beginning of an acute respiratory infection complaints low back
pain, nausea, dysuria, oligouriya appeared. In urine there was hematuria. The blood creatinine 0.20 mmol
/ L, potassium - 6.5 mmol / liter. The urine: the specific gravity 1003, the red blood cells (leached) - 150200 in the field of view. What is the diagnosis?
A. *tubulointerstitial nephritis
B. Acute glomerulonephritis
C. acute renal failure
D. Acute cystitis
E. Acute renal colic
283. A 18 year old guy gets ampicillin for treatment of acute respiratory illness complicated by acute
bronchitis. On the 5th day of treatment symptoms of intoxication increased, mild oedema on face, pain in
the joints appeard. On the skin of the trunk papular rash came out. Blood pressure: 140/90 mm Hg
Throughout the day he singled out 210 ml of urine (fluid was 2000 ml). The blood test: creatinine 0.24
mmol / l, urea 11.8 mmol / L, potassium 3.8 mmol / l, sodium 125 mmol / liter. The urine test:
proteinuria 0.99 g / l, erythrocyturia, eosinophilic leukocyturia. The relative density of urine during the
day ranged from 1002 to 1010. Urine culture for sterility gave no growth. What is the most likely
diagnosis?
A. Acute pyelonephritis
B. *Acute interstitial nephritis
C. Acute glomerulonephritis with nephritic syndrome
D. Acute glomerulonephritis with nephrotic syndrome
E. Dysmetabolic nephropathy
284. The 22 year old patient during 5 months was worried about trump pain, low-grade fever, frequent
urination. The urine test: moderate proteinuria, white blood cells in the entire field of view, the
bacteriuria. The blood - leukocytosis, erythrocyte sedimentation rate increasing. Which of the following
diagnoses is most likely?
A. Renal amyloidosis.
B. *Chronic pyelonephritis.
C. Acute glomerulonephritis.
D. Acute pyelonephritis.
E. Chronic glomerulonephritis.
285. Patient K., 24 years old, is cured in the intensive care unit from a long compression syndrome,
acute renal failure. The laboratory examination: urea 28.4 mmol / l, creatinine 820 micromol / l,
potassium 8.4 mmol / l, hemoglobin 76 g / l, hematocrit 0.26 l / l, erythrocytes 2.4 T / L. Which
complications can directly threaten the patient's life?
A. *hyperkalemic cardiac arrest
B. Anemia
C. Respiratory distress syndrome
D. DIC
E. hemic hypoxia
286. Patient M., 19 years old, was taken to hospital in serious condition with complaints of general
weakness, thirst, dry mouth, dull headaches. The first time he felt himself bad a year ago, when blood
pressure began to rise (180/110 mmHg. Art..) Treatment was not regular. His well-being became worse a
few days ago. During examination: face puffiness, pale skin and mucous membranes, muscle twitching.
Tongue was covered with gray bloom, bleeding gums. There was mild oedema on the shins. Pulse is 94
in 1 minute, rhythmic, tense. BP 175/120 mm Hg. Art. The first tone over the top of the heart is
weakened; the second is stronger above the aorta. In the lower parts of lungs breathing is hard. The liver
acts 2 cm from the edge of the rib arch, it is a little condensed, sensitive during palpation. Blood tests: er.
- 2.2 h1012 / l Hb - 82 g / l, ESR-26 mm / hour. Urine test: some density 1.016 protein, 1.35 g / l,
leukocytes 6 n / s, erythrocytes. - densely cover the field of vision, single hyaline cylinders. What is your
diagnosis?
A. Pyelonephritis
B. *Glomerulonephritis
C. Nephrolithiasis
D. Focal nephritis
E. Amyloidosis
287. Patient D, aged 20, complains about headaches, dizziness, general weakness, nausea and vomiting
after every meal. One year ago, it was accidentally discovered increased blood pressure. Further was
neither observed nor treated. He felt worse a week ago. 10 years ago, changes in urine test were found,
but he was not examined or treated. During examination: the patient feels malnutrition, is of serious
condition, pale, and has puffy face. Tongue is dry, covered with gray patina. Gums are bleeding. Pulse
counts 84 beats per minute, is tight, rhythmic, blood pressure is 180/110 mm Hg Cardiac impulse is
spilled, the left border of the heart is displaced to the left for 2 cm. The first tone above the top of the
heart is weakened, systolic murmur over the top is heard, the second tone is stronger above the aorta. In
the lower parts of lungs breathing is hard, abdomen is soft, the liver acts 2 cm from the edge of the rib
arch, it is dense, sensitive during palpation. On the skin of the trunk there are traces of scratching. What
is your preliminary diagnosis?
A. Multiple myeloma
B. Polycystic
C. Pyelonephritis
D. *Primary chronic glomerulonephritis. CRF V st.
E. Nephrolithiasis
288. A 24 year old patient was diagnosed with acute glomerulonephritis. Urine test: specific gravity
1010, Protein - 1.65 g / l, erythrocytes. 5-7 p / s, lakes. 2-3 p / h. blood Creatinine - 0.587 mmol / liter.
What is the main reason of hyperazotemia which suffers the patient with acute glomerulonephritis?
A. Reduced tubular reabsorption.
B. The decrease in renal blood flow.
C. Strengthening the collapse of erythrocytes and leukocytes in the glomerular filtrate.
D. *Reduced glomerular filtration rate.
E. Violation of protein metabolism.
289. A 34 year old patient, 3 months ago began to suffer from headache, shortness of breath when
walking, loss of appetite, nausea and weakness. He has been suffering from chronic glomerulonephritis
for10 years. It was suspected that during glomerulonephritis chronic renal insufficiency was complicated.
Which laboratory parameters will be the most informative in this case?
A. *Blood creatinine 0.46 mmol / l
B. Blood urea 7.3 mmol / liter.
C. Blood sodium 130 mmol / liter.
D. Urea nitrogen 20 - 40% of the residual nitrogen.
E. Potassium blood 5.2 mmol / liter.
290. A doctor discovered high blood pressure in a 19 year old patient. Urine test: leukocytes - 6-7,
erythrocytes - 3-4 in n / view, protein 0.066 g / litre. Which instrumental examination should be
appointed for clarification of the kidneys’ state?
A. *Ultrasound of the kidneys
B. radioisotope renography
C. CT
D. Survey radiography of the kidneys
E. renal angiography
291. The 25-year-old patient with rheumatoid arthritis of joint and visceral form blood pressure and
proteinuria have been increasing during the last six months. Development of renal amyloidosis was
suspected. Necessary examinations are:
A. *Kidney biopsy, biopsy of the rectal mucosa, a biopsy of the gums
B. Definition of haematuria, renal biopsy
C. Determination of proteinuria, kaliyuria, uraturia
D. Determination of proteinuria, renal biopsy
E. Biopsy of intestinal mucosa, the definition of pyuria
292. During the examination at clinic of 23 year old girl acute glomerulonephritis, nephrotic syndrome
without renal dysfunction were defined. Assign the leading drug of etiological treatment for the patient.
A. Prednisolone
B. *Augmentin
C. Biseptol
D. Heparin
E. saluretic
293. A 63-year-old man is admitted with acute somnolence, disorientation, and right upper and lower
extremity weakness. He has a 3-year history of renal insufficiency and congestive heart failure attributed
to long-standing hypertension, which has been poorly controlled in part because of poor adherence. On
physical examination, the blood pressure is 160/96 mm Hg, pulse rate 11 0/min, respiratory rate 14/min,
and temperature 38 °C (100.4 °F). There is three-fingerbreadth neck vein distention while sitting and
hepatojugular reflux. Cardiac examination shows an S3 gallop; pulmonary examination reveals bilateral
crackles. The abdomen is benign, and 2+ lower extremity edema is present. Right biceps and patellar
reflexes are increased, and a right Babinski response is noted. Laboratory studies: Hematocrit - 33%.
Leukocyte count - 10,700/?L. Platelet count- Normal Blood urea nitrogen - 35 mg/dL. Serum creatinine 2.3 mg/dL Serum sodium - 128 meq/L. Serum potassium - 4.3 meq/L. Serum chloride - 93 meq/L. Serum
bicarbonate - 16 meq/L. Arterial blood gas pH 7.30, PCO2 - 33 mm Hg. Urinalysis pH 6.0, specific
gravity 1.014, 2+ proteinuria, no hematuria or ketonuria; no formed elements on microscopy Noncontrast
computed tomography of the head shows only an ill-defined mass effect. Neurology and neurosurgical
consultants request contrast computed tomography to more precisely demarcate the suspected tumor and
thus pinpoint a site for biopsy or resection. What is the most important next step to prepare this patient
for a contrast study?
A. *Administer acetylcysteine
B. Administer half-normal saline
C. Administer dopamine
D. Administer bicarbonate
E. Administer calcium channel blocker
294. A 70-year-old woman is admitted because she has had malaise and anorexia for 1 week. She has
been previously healthy, except for hypertension and hypercholesterolemia, treated with
hydrochlorothiazide and atorvastatin. On physical examination, the supine blood pressure is 150/95 mm
Hg, pulse rate 80/min, respiratory rate 20/min, and temperature 37.4 °C (99.3 °F). The blood pressure is
125/80 mm Hg and the pulse rate 96/min while standing. There is no neck vein distention or
hepatojugular reflux. Cardiac, breast, abdominal, and pulmonary examinations are normal. No lower
extremity edema is present. Laboratory studies: Hematocrit 29% Leukocyte count 3,200/?L Platelet
count - 90,000/?L. Blood urea nitrogen - 62 mg/dL. Serum creatinine - 4.6 mg/dL. Serum sodium - 134
meq/L. Serum potassium - 5.0 meq/L. Serum chloride - 114 meq/L. Serum bicarbonate - 15 meq/L.
Serum glucose - 105 mg/dL. Serum calcium - 12.5. mg/dL. Serum inorganic phosphate 8.5 mg/dL. Urine
creatinine - 25 mg/dL. Urine sodium - 50 meq/L. Urinalysis Specific gravity 1 .007; trace proteinuria; no
glucosuria or ketonuria Arterial blood gaspH 7.30, PCO2 28 mm Hg. Microscopic analysis shows
scattered tubular epithelial cells. Posteroanterior and lateral films of the chest are normal. What is the
most likely diagnosis?
A. Milk-alkali syndrome
B. Sarcoidosis
C. *Multiple myeloma
D. Primary hyperparathyroidism
E. Clinical consequence of hydrochlorothiazide therapy
295. 28-year-old man has the acute onset of colicky pain in the left costovertebral angle radiating into
the groin, as well as gross hematuria. Abdominal x-ray discloses a stone in the left ureter. All of the
following are true statements concerning this disease EXCEPT that
A. the majority of renal stones are radiopaque
B. radiolucent stones are usually composed of uric acid
C. staghorn calculi are associated with alkaline urine
D. *radiopaque stones usually contain cystine
E. urate stones are associated with acidic urine
296. A 69-year-old white man is referred for worsening hypertension over the past 2 to 3 months. He has
had hypertension for the past 18 months. It had been controlled by ?-blocker therapy, which was begun
after he had an inferior myocardial infarction. A recent blood pressure measurement was 200/120mm Hg,
requiring additional therapy with amlodipine. His medical history is significant for the myocardial
infarction and a right femoral popliteal bypass. He smokes two packs of cigarettes daily and drinks
alcohol socially. On examination, blood pressure is 178/104 mm Hg seated and standing, and body
weight is 72 kg (159 Ib). Optic funduscopy reveals background hypertensive retinopathy. A left carotid
bruit is heard. Cardiopulmonary and neuromuscular examinations are normal. Abdominal examination
showed no organomegaly, but an epigastric bruit is present. No peripheral edema is noted. Serum
creatinine concentration is 2.3 meq/dL, and serum potassium concentration is 3.9 mg/dL. Urinalysis
shows 1 + proteinuria without hematuria. Electrocardiography is positive for left ventricular hype
rtrophy. What is the most appropriate noninvasive screening test for possible renal artery stenosis in this
patient?
A. *Magnetic resonance angiography with gadolinium
B. Computed tomographic angiography with contrast
C. Captopril renography
D. Captopril plasma renin activity test
E. none of them
297. A 61-year-old woman with a previously normal serum creatinine concentration is admitted with
abdominal pain. Abdominal aortic aneurysm was diagnosed after an intravenous contrast study, and the
patient underwent emergency aneurysmectomy. On the third hospital day, in the intensive care unit, the
patient was oliguric. She was given an intravenous furosemide infusion but was still oliguric several
hours later. On physical examination, the blood pressure is 90/62 mm Hg, with no orthostatic changes;
pulse rate 11 5/min; respiratory rate 22/min; and temperature 36.8 °C (98.2 °F). Three-fingerbreadth
neck-vein distention at 45 degrees and hepatojugular reflux are present. Cardiac examination shows an
S3 gallop. There are scattered bibasilar rales. The abdomen has a fresh surgical scar. Bowel sounds are
not heard, and there is diffuse tenderness. The patient has 2+ lower extremity edema. She is arousable but
somnolent and moves all extremities in response to commands. She complains of dyspnea. Laboratory
studies: Hematocrit - 37% Leukocyte count Leukocytosis Platelet count - Low Blood urea nitrogen 75
mg/dL Serum creatinine - 4.4 mg/dL Serum sodium - 130 meq/L Serum potassium - 6.3 meq/L Serum
chloride - 90 meq/L Serum bicarbonate - 16 meq/L Arterial blood gaspH 7.26, Pco2 - 25 mm Hg, Po2 65 mm Hg Urinalysis pH 6.0, specific gravity 1.009, 2+ proteinuria, no hematuria or ketonuria There are
muddy brown casts on microscopic examination. The electrocardiogram shows prominent, peaked T
waves. What is the next step in treatment of this patient with acute renal failure?
A. Administer fenoldopam
B. Start ultrafiltration
C. *Start continuous venovenous hemofiltration
D. Start peritoneal dialysis
E. Initiate plasma exchange
298. A 52-year-old man is referred by his primary care physician for hypertension and hypokalemia over
the past 6 months. Blood pressure and routine chemistries were normal last year at the time of an
executive physical. He has no history of cardiovascular disease, stroke, or renal disease. Family history is
negative for hypertension. He uses alcohol socially and does not smoke but chews tobacco. He takes no
medications regularly. On examination, the patientweighs 77kg (168 Ib). Blood pressure is 164/102mm
Hg seated and standing. Except for trace pedal edema, the remainder of examination is normal. The
primary care physician provides the following laboratory values: Blood urea nitrogen - 21 mg/dL Serum
creatinine - 0.9 mg/dL Serum sodium - 141 meq/L Serum potassium 3.1 meq/L Serum chloride 100
meq/L Serum bicarbonate
28 meq/L A 24-hour urine test during salt loading reveals the following
values: Creatinine - 1.1 g Sodium - 252 meq Potassium 128 meq The daily aldosterone excretion rate is 6
mg (normal, 5 to 15 mg), plasma renin activity is 1 ?g/L/h, and plasma aldosterone level is 9 ng/dL.
Which diagnostic test would you order next?
A. Computed tomography of the adrenal glands
B. *Serum cortisol and urinary free cortisol measurement
C. Magnetic resonance angiography with gadolinium
D. Adrenocorticotropin hormone stimulation test
E. none of them
299. A 64-year-old black woman has had hypertension for 25 years. On therapy, her blood pressure has
been in the range of 140 to 160/95 to 100 mm Hg. She presents for blood pressure management. Review
of past laboratory data shows that the serum creatinine concentration was 1 .2 mg/dL 10 years ago, 1.7
mg/dL 5 years ago, 2.0 mg/dL 1 year ago, and 1.9 mg/dL 2 months ago. Recent urinalysis shows 2+
proteinuria, no hematuria, and occasional granular and hyaline casts. Urine protein:creatinine ratio is 0.5.
Renal ultrasonography shows no hydronephrosis with kidney sizes at 9.5 cm bilaterally. On examination,
body weight is 84 kg (185.2 Ib) and temperature is 36.9 °C (98.4°F). Blood pressure is 148/96 mm Hg in
both arms. Optic funduscopy shows moderate arteriolar sclerosis and constriction. No jugulovenous
distention is present. The lungs are clear. Cardiac examination shows regular sinus rhythm, S4 but no S3,
and no murmur. There is no edema of the extremities. What is the most likely cause of this patient’s renal
disease?
A. Membranous glomerulopathy
B. Obstructive uropathy
C. IgA nephritis
D. *Nephrosclerosis
E. Obesity-related glomerular disease
300. A 63-year-old man is hospitalized with chest pain. The patient has had hypercholesterolemia for 10
years and hypertension for 8 years. He has been treated most recently with atorvastatin, furosemide, and
losartan. His last serum creatinine concentration as an outpatient 2 months ago was 0.9 mgldL.
Evaluation in the cardiac care unit with coronary angiography revealed right and left coronary artery
disease, and he underwent emergent percutaneous angioplasty and stenting of the involved coronary
arteries. During the procedure, he developed chest pain, and a dissection of the right coronary artery was
noted, along with acute increased ST-segments in the inferior leads. He underwent immediate coronary
artery bypass. On the day after the procedure, he is alert and oriented. His pulse rate is 1 06/min supine
and 1 08/min seated. Blood pressure is 96/70 mm Hg supine and 100/75 mm Hg seated. Neck vein
distention is not noted when the patient is lying flat, and there is no hepatojugular reflux. The chest is
clear. No murmur or gallop is present. The abdomen lacks rebound and rigidity. There is no abdominal
bruit and no sacral or lower extremity edema. Distal pulses and the skin of the lower extremity digits are
normal. Laboratory studies: Blood urea nitrogen
30 mg/dL Serum creatinine - 1.9 mg/dL Serum
sodium - 145 meq/L Serum potassium - 3.4 meq/L Serum chloride - 109 meq/L Serum bicarbonate
21 meq/L Urinalysis Specific gravity 1.013, trace proteinuria, trace ketonuria, no glucosuria Urine
microscopy Rare tubular cells, muddy brown casts, cellular debris Urinary sodium 36 meq/L Urinary
creatinine l3 mg/dL Urine osmolality 110 mosmol/kg H2O What is the correct therapy?
A. Administer endothelin antagonist
B. Administer insulin-like growth factor
C. Administer low-dose dopamine
D. Administer thyroxine
E. *Observe
301. A 56-year-old black man with diabetic nephropathy is seen in clinic for routine follow-up.
Laboratory studies: Serum calcium - 9.6 mg/dL Serum phosphorus - 6.0 mg/dL Serum parathyroid
hormone 387 pg/mL Serum albumin
- 3.9 dg/L Serum creatinine- 2.6 mg/dL Estimated glomeru mar
filtration rate 38 mL/min Because the patient has adhered to a phosphate-restricted diet, phosphate binder
therapy with calcium acetate, 667 mg, two tablets three times daily with meals is begun. Three weeks
later, repeated calcium and phosphorus measurements are 11.9 mg/dL and 5.4 mg/dL, respectively. What
would be the most appropriate action?
A. Refer for parathyroidectomy as definitive therapy for secondary hyperparathyroidism
B. Discontinue calcium acetate therapy and avoid use of phosphate binders in the future
C. *Discontinue calcium acetate therapy and, once calcium normalizes, start sevelamer therapy as a
non-calcium-based phosphate binder
D. Discontinue calcium acetate and, once calcium normalizes, restart phosphate binder therapy with
aluminum hydroxide
E. none of them
302. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Nitroglycerine
E. Any of the above
303. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely CONTRAINDICATED to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifidipine
304. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
305. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Thiazide diuretic
C. No treatment at this time
D. ACE-inhibitor
E. Beta-blocker
306. You see a 62-year-old man with isolated essential hypertension, currently taking
hydrochlorothiazide 25 mg PO daily, comes to you for his first clinic visit. He notes that his BP at home
is always less than 140/80 mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Search for secondary causes of hypertension
E. Start metoprolol
307. A 36-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
308. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
309. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Hydrochlorothiazide
B. *Metoprolol
C. Lisinopril
D. Amlodipine
E. All of the above
310. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
311. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
312. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
313. You see a 44-year-old male for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment required at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
314. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
315. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
316. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
317. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
318. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
319. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
320. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension. On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal. CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
321. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal. What is the appropriate
course of action regarding the patient’s antihypertensive therapy?
A. Advise a low-sodium diet
B. *Discontinue doxazosin therapy and consider an alternative agent
C. Advise high dietary intake of calcium and potassium
D. Increase the doxazosin to 4 mg a day
E. Advise magnesium supplements
322. At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
323. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
324. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. RBBB
E. Tricuspid atresia
325. A 55-year-old male with diabetes mellitus presents to his cardiologist with a BP of 165/95 mmHg.
According to the JNC 7 guidelines, he would be classified as what stage of hypertension and what is his
target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
326. A 63-year-old man with long-standing insulin-requiring diabetes presented to the physician's office
for management of hypertension (160/94 mmHg). Urine and serum chemistries at that time were normal
except for serum creatinine = 1,6 mg/dl (0,141 mcmol/l) and blood urea nitrogen (BUN) = 30 mg/dl. A
potassium-sparing diuretic (triamterene-hydrochlorothiazide) was prescribed. When he returns 2 weeks
later, the serum potassium level is 6,8 mmol/l with no significant change in BUN or creatinine. The most
likely explanation is:
A. Excessive consumption of tomatoes and bananas
B. A recent urinary tract infection
C. Primary hyperaldosteronism
D. *Hyporeninemic hypoaldosteronism
E. Cushing syndrome
327. A 30-year-old male with no past medical history presents to his primary care physician complaining
of new-onset morning headaches that have been ongoing for the past few weeks. His BP is noted to be
220/110 mmHg with a gradient between his brachial and popliteal arteries. On auscultation there is a 2/6
systolixc crescendo-decrescendo murmur heard across the precordium. His ECG is significant for LVH.
A CXR shows cardiomegaly with evidence of rib notching. The patient most likely has what valvular
abnormality?
A. Mitral regurgitation
B. *Bicuspid aortic valve
C. Mitral stenosis
D. Tricuspid regurgitation
E. Pulmonary stenosis
328. A 36-year-old female with diabetes mellitus and hyperlipidemia and no history of hypertension is
noted at her yearly clinic visit to have new-onset hypertension with a BP of 180/110 mmHg. She
undergoes screening for secondary causes of hypertension and is found to have a pheochromocytoma.
What of the following medications is contraindicated as monotherapy?
A. *Metoprolol
B. Lisinopril
C. Phentolamine
D. Hydrochlorothiazide
E. Captopril
329. A 50-year-old male with chronic kidney disease and hypertension has a BP of 165/110 mmHg.
What is this patient's target BP according to the JNC 7 guidelines?
A. 140/90 mmHg
B. *130/80 mmHg
C. 120/80 mmHg
D. 115/70 mmHg
E. 110/70 mmHg
330. As a cardiologist you see a 55-year-old male with diabetes mellitus and a BP of 165/95 mmHg.
According to the JNC 7 guidelines, he would be classified as what stage of hypertension and what is his
target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
331. You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
332. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Hydrochlorothiazide
B. *Metoprolol
C. Perindopril
D. None of the above
E. All of the above
333. A 54-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
334. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
335. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
336. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. Start a calcium channel blocker
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
337. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Add amlodipine
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
338. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
339. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
340. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of perindopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
341. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 59-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
342. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
343. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension.On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal.CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
344. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal.
A. What is the appropriate course of action regarding the patient’s antihypertensive therapy?
B. Advise a low-sodium diet
C. *Discontinue doxazosin therapy and consider an alternative agent
D. Advise high dietary intake of calcium and potassium
E. Increase the doxazosin to 4 mg a day
F. Advise magnesium supplements
345. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
346. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
347. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Aorticl stenosis
C. Preexcitation syndrome
D. Left bundle branch block
E. Pulmonary atresia
348. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
349. A 19-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. WPW-syndrome
D. Right bundle branch block
E. Tricuspid atresia
350. A 54-year old man with a history of hypertension presents with chest pain that started 2 hours ago
and is diagnosed in the Emergency Department with anterior STEMI. His BP is 200/100 mmHg. He
receives i.v. metoprolol and the BP falls to 170/85 mmHg. What is the most appropriate reperfusion
strategy?
A. *Fibrinolytic therapy
B. Angiography and PCI
C. Medical therapy alone and PCI at a later date
D. CABG
E. None of the above
351. A 75-year old woman presents to a community hospital (without invasive capabilities) with 6 hrs of
chest pain and is diagnosed with inferior STEMI. The anticipated transfer to a medical center with
primary PCI capability will take 2 hours. What is the preferred reperfusion therapy?
A. *Fibrinolytic therapy at presentation to the hospital
B. Transfer for angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa inhibition at the presentation hospital and transfer for rescue
PCI if it fails to produce reperfusion
D. PCI at a later date
E. CABG
352. A 48-year old man with an anterior STEMI receives fibrinolytic therapy with reteplase. Thirty min.
after the second bolus he continues to have chest pain and his ECG demonstrates mild (estimated 30%
resolution) of the ST segment elevations. What is the next correct step in his management?
A. Readministration of a different fibrinolytic agent
B. Administration of GP IIb/IIIa inhibitor
C. *Immediate coronary angiography and rescue PCI
D. Symptomatic relief of angina and heart failure
E. Medical therapy and PCI at a later date
353. A 50-year old man presents to the emergency room about 1.5 hrs after the onset of chest pain. An
ECG showed 3 mm ST elevation in the anterior and lateral leads. Which of the following statements
regarding his management is correct?
A. Primary PCI is recommended over thrombolytics because PCI has short-term mortality benefit,
reduced reinfarction risk, and reduced risk of stroke
B. *Thrombolysis is recommended because door-to-baloon time is >90 min.
C. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
D. The patient should be referred for emergency CABG for better survival advantage.
E. Scheduled CABG
354. A 65-year old woman developed cardiogenic shock 10 hrs after presenting with anterior wall MI.
The most appropriate management strategy is....
A. Administration of thrombolytics
B. Watchful waiting after initiation of inotropic support and insertion of an intra-aortic balloon pump
C. *Coronary angiography with revascularization within 18 hrs of shock onset
D. Half-dose fibrinolysis and GP IIb/IIIa
E. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
355. A 62-year old woman, current smoker, diabetic, hypertensive and hyperlipidemic, presented to the
ER with a 2 day history of intermittent chest pain. The patient does not have any signs of heart failure.
An ECG showed 2-mm depression in V2-V6. The coronary angiogram showed 90% stenosis in the
proximal third of the LAD, 80% stenosis in the proximal RCA, with 30% disease in the middle
circumflex artery. The best plan of treatment for this patient is
A. PCI to both the LAD and RCA now
B. *Referral for two-vessel CABG
C. PCI to the LAD with staged intervention to the RCA
D. Medical management with no PCI or CABG
E. Thrombolysis is recommended
356. A 60-year-old male patient on aspirin, nitrates, and a beta blocker, being followed for chronic stable
angina, presents to the ER with a history of two to three episodes of more severe and long-lasting anginal
chest pain each day over the past 3 days. His ECG and cardiac enzymes are normal. The best course of
action of the following is to
A. Admit the patient and begin intravenous digoxin.
B. *Admit the patient and begin intravenous heparin
C. Admit the patient and give prophylactic thrombolytic therapy
D. Admit the patient for observation with no change in medication
E. Discharge the patient from the ER with increases in nitrates and beta blockers
357. A 60-year-old white female presents with epigastric pain, nausea and vomiting, heart rate of 50, and
pronounced first-degree AV block on ER cardiac monitor. Blood pressure is 130/80. The coronary artery
most likely to be involved in this process is the
A. *Right coronary
B. Left main
C. Left anterior descending
D. Circumflex
E. Left coronary
358. 80-year old woman with chest discomfort for the last 15 hours and progressively worsening
dyspnea over the last few hours presents to the Emergency Department and is diagnosed with anterior
STEMI. What, if any, reperfusion strategy should be undertaken?
A. Fibrinolysis
B. Immediate coronary angiography and PCI
C. *Symptomatic relief of angina and heart failure
D. CABG
E. None of the above
359. A 77-year old woman with a history of GERD presents in the first hour of an acute inferior STEMI.
The BP is normal. Invasive facilities are not readily available. What is the preferred strategy for
reperfusion therapy?
A. *Fibrinolytic therapy
B. Transfer for immediate coronary angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa
D. Symptomatic relief of angina only
E. CABG
360. You are seeing in your office a patient with the chief complaint of relatively sudden onset of
shortness of breath and weakness but no chest pain. ECG shows nonspecific ST-T changes. You would
be particularly attuned to the possibility of painless, or silent, myocardial infarction in the
A. Advanced coronary artery disease patient with unstable angina on multiple medications
B. *Elderly diabetic
C. Premenopausal female
D. Inferior MI patient
E. MI patient with PVCs
361. A 75-year-old female is admitted with acute myocardial infarction and congestive heart failure,
then has an episode of ventricular tachycardia. She is prescribed multiple medications and soon develops
confusion and slurred speech. The most likely cause of this confusion is
A. Captopril
B. Digoxin
Furosemide
C. *Lidocaine
D. Nitroglycerin
362. Two weeks after hospital discharge for documented myocardial infarction, a 65-year-old returns to
your office very concerned about low-grade fever and pleuritic chest pain. There is no associated
shortness of breath. Lungs are clear to auscultation and heart exam is free of significant murmurs,
gallops, or rubs. ECG is unchanged from the last one in the hospital. The most effective therapy is likely
A. Antibiotics
B. Anticoagulation with warfarin (Coumadin)
C. *An anti-inflammatory agent
D. An increase in antianginal medication
E. An antianxiety agent
363. A 48-year-old man is admitted to the coronary care unit with an acute inferior myocardial
infarction. Two hours after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per
minute with sinus rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 g/min
364. A 55-year-old patient presents to you with a history of having recently had a myocardial infarction
with a 5-day hospital stay while away on a business trip. He reports being told he had mild congestive
heart failure then, but is asymptomatic now with normal physical exam. You recommend which of the
following medications?
A. *An ACE inhibitor
B. Digoxin
C. Diltiazem
D. Furosemide (Lasix)
E. Hydralazine plus nitrates
365. A 57-year-old man is admitted to the CCU with an acute inferior myocardial infarction. Two hours
after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per minute with sinus
rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 mcg/min
366. A 70-year-old retired banker with no past medical history presents to the emergency department 4 h
after the onset of severe substernal crushing chest pain with radiation to the left arm and neck.
Electrocardiography reveals significant ST-segment elevation in leads I, L, V5, and V6. The patient has
no clear-cut medical contraindications to anticoagulation. Which of the following would be the optimal
management strategy at this time?
A. Intravenous tissue plasminogen activator alone
B. Intravenous tissue plasminogen activator and aspirin
C. Intravenous tissue plasminogen activator and heparin
D. *Intravenous tissue plasminogen activator, heparin, and aspirin
E. Thrombolytic therapy is contraindicated because of the patient's age
367. A previously healthy 58-year-old man is admitted to the hospital because of an acute inferior
myocardial infarction. Within several hours, he becomes oliguric and hypotensive (blood pressure is
90/60 mmHg). Insertion of a pulmonary artery (Swan-Ganz) catheter reveals the following pressures:
pulmonary capillary wedge, 4 mmHg; pulmonary artery, 22/4 mmHg; and mean right atrial, 11 mmHg.
This man would best be treated with
A. *fluids
B. digoxin
C. norepinephrine
D. dopamine
E. intraaortic balloon counterpulsation
368. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block. Chest plain film is normal. Which of the following is likely to be found in addition
on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
369. A 42-year-old man presents with Löffler endocarditis. Expected findings include all of the
following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
370. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
371. A 24-year-old previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
372. A 78-year-old woman with CHF (EF, 25%), chronic AFib, GERD, HTN, hyperlipidemia, diabetes,
and osteoporosis takes 12 different pills. Recently her neighbour, a nurse told her that she does not need
to take digoxin because she is on amiodarone. She wants to eliminate digoxin from her medication
regimen, and she wants to know why you put her on it in the first place. What is your answer?
A. Digoxin improves survival
B. *Digoxin reduces hospitalizations
C. Digoxin improves contractility
D. Digoxin decreases the volume of distribution of amiodarone
E. Digoxin reduces sympathetic nervous system activity
373. A 59-year-old woman with CHF and an EF of 30% comes to your office for follow-up. She is on
carvedilol, enalapril, aspirin, atorvastatin calcium, digoxin, and furosemide. She has been doing well
without any rehospitalization. However, she wants to improve her exercise tolerance. What should you
recommend?
A. Cardiac transplantation
B. I.V. dobutamine
C. Higher doses of ACE inhibitor
D. Adding spironolactone
E. *Enrolling her in an exercise training program
374. You see a 37-year-old man who presents with Löffler endocarditis. Expected findings include all of
the following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
375. A 23-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
376. A 34-y.o. previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
377. is an obese 54-yer-old man denies exertional chest discomfort or dyspnea, but lives a fairly
sedentary lifestyle. Physical exam reveals an obese man with normal BP, an unremarkable cardiac exam.
His fasting lipids are as follows: TC 240 mg/dL, TG 250 mg/dL, HDL-C 35 mg/dL, LDL-C
(calculated)155. Initial therapy should include:
A. *Therapeutic lifestyle correction (TLC) only
B. TLC plus a statin with a goal of reducing LDL-C to <130 mg/dL
C. TLC plus niacine or fibrate, with the goals of reducing LDL-C to <100 mg/dL and TG <150 mg/dL
D. TLC plus a statin with a goal of reducing LDL-C to <100 mg/dL
E. TLC plus a statin, as well as niacin or a fibrate, with the goals of reducing LDL-C to <100 mg/dL
and TG <150 mg/dL
378. S. is a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. Initial therapy should include:
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. Therapeutic lifestyle correction (TLC) plus a statin to reduce LDL-C to <130
D. *TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
379. N. is a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=24), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. If N. were found to have untreated hypertension (SBP of 160), with all other data the
same, what would be the preferred initial treatment in addition to BP control?
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. Therapeutic lifestyle correction (TLC) plus a statin to reduce LDL-C to <100 *
D. TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
380. V. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
what is your first goal of drug treatment?
A. Increase the HDL-H
B. Lower the LDL-C
C. Lower the TG
D. Lower the TG and increase the HDL-C
E. *Lower the non-HDL-C
381. G. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
which of the following would allow you to achieve the goal of lowering the non-HDL-C?
A. Increase the dose of atorvastatin
B. Add a fibrate
C. Add niacin
D. Add ezetimibe
E. *Any of the above
382. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of CHD.
He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel is as
follows: TC 220, HDL-C 40, LDL-C 120, TG 600. After recommending lifestyle modifications, what
would be your next step in lipid management?
A. Increase the HDL-H
B. Lower the LDL-C
C. *Lower the TG
D. Lower the TG and increase the HDL-C
E. Lower the non-HDL-C
383. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
sinus bradycardia at a rate of 40 with hypotension. Choose the best next step in antiarrhythmic
management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
384. A 58-year-old female smoker admitted to the ICU with respiratory distress due to pneumonia. This
was complicated by an anterior MI, with management including cautious use of beta-blockers. She now
develops 10 to 12 PVC’s per hour, occasional couplets, and a few short runs of ventricular tachycardia,
although BP and oxygen saturation remain stable. Choose the best next step in antiarrhythmic
management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Observation
E. Quinidine
385. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
386. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely CONTRAINDICATED to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifidipine
387. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
388. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
389. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
390. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
391. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
392. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Hydrochlorothiazide
B. *Atenolol
C. Lisinopril
D. None of the above
E. All of the above
393. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
394. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
395. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
396. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
397. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
398. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
399. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
400. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
401. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
402. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
403. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension. On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal. CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
404. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal. What is the appropriate
course of action regarding the patient’s antihypertensive therapy?
1.A. Advise a low-sodium diet
B. *Discontinue doxazosin therapy and consider an alternative agent
C. Advise high dietary intake of calcium and potassium
D. Increase the doxazosin to 4 mg a day
E. Advise magnesium supplements
405. At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
406. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
407. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral valve stenosis
C. Preexcitation syndrome
D. Congenital heart block
E. Tricuspid atresia
408. 108. A 55-year-old male with diabetes mellitus presents to his cardiologist with a BP of 165/95
mmHg. According to the JNC 7 guidelines, he would be classified as what stage of hypertension and
what is his target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
409. A 63-year-old man with long-standing insulin-requiring diabetes presented to the physician's office
for management of hypertension (160/94 mmHg). Urine and serum chemistries at that time were normal
except for serum creatinine = 1,6 mg/dl (0,141 mcmol/l) and blood urea nitrogen (BUN) = 30 mg/dl. A
potassium-sparing diuretic (triamterene-hydrochlorothiazide) was prescribed. When he returns 2 weeks
later, the serum potassium level is 6,7 mmol/l with no significant change in BUN or creatinine. The most
likely explanation is:
A. Excessive consumption of tomatoes and bananas
B. A recent urinary tract infection
C. Primary hyperaldosteronism
D. *Hyporeninemic hypoaldosteronism
E. Cushing syndrome
410. A 30-year-old male with no past medical history presents to his primary care physician complaining
of new-onset morning headaches that have been ongoing for the past few weeks. His BP is noted to be
220/110 mmHg with a gradient between his brachial and popliteal arteries. On auscultation there is a 2/6
systolixc crescendo-decrescendo murmur heard across the precordium. His ECG is significant for LVH.
A CXR shows cardiomegaly with evidence of rib notching. The patient most likely has what valvular
abnormality?
A. Mitral regurgitation
B. *Bicuspid aortic valve
C. Mitral stenosis
D. Tricuspid regurgitation
E. Pulmonary stenosis
411. A 36-year-old female with diabetes mellitus and hyperlipidemia and no history of hypertension is
noted at her yearly clinic visit to have new-onset hypertension with a BP of 180/110 mmHg. She
undergoes screening for secondary causes of hypertension and is found to have a pheochromocytoma.
What of the following medications is contraindicated as monotherapy?
A. *Propranolol
B. Lisinopril
C. Am;odipine
D. Hydrochlorothiazide
E. Captopril
412. A 50-year-old male with chronic kidney disease and hypertension has a BP of 165/110 mmHg.
What is this patient's target BP according to the JNC 7 guidelines?
A. 140/90 mmHg
B. *130/80 mmHg
C. 120/80 mmHg
D. 115/70 mmHg
E. 110/70 mmHg
413. As a cardiologist you see a 55-year-old male with diabetes mellitus and a BP of 165/95 mmHg.
According to the JNC 7 guidelines, he would be classified as what stage of hypertension and what is his
target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
414. You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
415. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Furosemide
B. *Metoprolol
C. Lisinopril
D. Felodipine
E. Perindopril
416. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
417. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
418. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
419. A 42-year-old male presents for a routine physical examination. He is noted to have a BMI of 31,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
420. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start bisoprolol
421. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start bisoprolol
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
422. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Bisoprolol
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
423. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of an ACE-inhibitor. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
424. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
425. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
426. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension.On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal.CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
427. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal.
A. What is the appropriate course of action regarding the patient’s antihypertensive therapy?
B. Advise a low-sodium diet
C. *Discontinue doxazosin therapy and consider an alternative agent
D. Advise high dietary intake of calcium and potassium
E. Increase the doxazosin to 4 mg a day
F. Advise magnesium supplements
428. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
429. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
430. You see a 23-year old with the recent onset of headaches. The headaches are described as
“pounding” and occur during the day and night. He has minimal relief with acetaminophen. Physical
examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min, arteriovenous
nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced pulses in both
lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The patient
described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. Atrial septal defect
E. Ventricular septal defect
431. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
432. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. RBBB
E. Tricuspid atresia
433. A 54-year old man with a history of hypertension presents with chest pain that started 2 hours ago
and is diagnosed in the Emergency Department with anterior STEMI. His BP is 200/100 mmHg. He
receives i.v. metoprolol and the BP falls to 170/85 mmHg. What is the most appropriate reperfusion
strategy?
A. *Fibrinolytic therapy
B. Angiography and PCI
C. Medical therapy alone and PCI at a later date
D. CABG
E. None of the above
434. A 75-year old woman presents to a community hospital (without invasive capabilities) with 6 hrs of
chest pain and is diagnosed with inferior STEMI. The anticipated transfer to a medical center with
primary PCI capability will take 2 hours. What is the preferred reperfusion therapy?
A. *Fibrinolytic therapy at presentation to the hospital
B. Transfer for angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa inhibition at the presentation hospital and transfer for rescue
PCI if it fails to produce reperfusion
D. PCI at a later date
E. CABG
435. A 48-year old man with an anterior STEMI receives fibrinolytic therapy with reteplase. Thirty min.
after the second bolus he continues to have chest pain and his ECG demonstrates mild (estimated 20%
resolution) of the ST segment elevations. What is the next correct step in his management?
A. Readministration of a different fibrinolytic agent
B. Administration of GP IIb/IIIa inhibitor
C. *Immediate coronary angiography and rescue PCI
D. Symptomatic relief of angina and heart failure
E. Medical therapy and PCI at a later date
436. A 50-year old man presents to the emergency room about 1.5 hrs after the onset of chest pain. An
ECG showed 3 mm ST elevation in the anterior and lateral leads. Which of the following statements
regarding his management is correct?
A. Primary PCI is recommended over thrombolytics because PCI has short-term mortality benefit,
reduced reinfarction risk, and reduced risk of stroke
B. *Thrombolysis is recommended because door-to-baloon time is >90 min.
C. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
D. The patient should be referred for emergency CABG for better survival advantage.
E. Scheduled CABG
437. A 67-year old woman developed cardiogenic shock 10 hrs after presenting with anterior wall MI.
The most appropriate management strategy is....
A. Administration of thrombolytics
B. Watchful waiting after initiation of inotropic support and insertion of an intra-aortic balloon pump
C. *Coronary angiography with revascularization within 18 hrs of shock onset
D. Half-dose fibrinolysis and GP IIb/IIIa
E. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
438. A 62-year old woman, current smoker, diabetic, hypertensive and hyperlipidemic, presented to the
ER with a 2 day history of intermittent chest pain. The patient does not have any signs of heart failure.
An ECG showed 2-mm depression in V2-V6. The coronary angiogram showed 90% stenosis in the
proximal third of the LAD, 80% stenosis in the proximal RCA, with 30% disease in the middle
circumflex artery. The best plan of treatment for this patient is
A. PCI to both the LAD and RCA now
B. *Referral for two-vessel CABG
C. PCI to the LAD with staged intervention to the RCA
D. Medical management with no PCI or CABG
E. Thrombolysis is recommended
439. A 60-year-old male patient on aspirin, nitrates, and a beta blocker, being followed for chronic stable
angina, presents to the ER with a history of two to three episodes of more severe and long-lasting anginal
chest pain each day over the past 3 days. His ECG and cardiac enzymes are normal. The best course of
action of the following is to
A. Admit the patient and begin intravenous digoxin.
B. *Admit the patient and begin intravenous heparin
C. Admit the patient and give prophylactic thrombolytic therapy
D. Admit the patient for observation with no change in medication
E. Discharge the patient from the ER with increases in nitrates and beta blockers
440. A 60-year-old white female presents with epigastric pain, nausea and vomiting, heart rate of 50, and
pronounced first-degree AV block on ER cardiac monitor. Blood pressure is 130/80. The coronary artery
most likely to be involved in this process is the
A. *Right coronary
B. Left main
C. Left anterior descending
D. Circumflex
E. Left coronary
441. An 80-year old woman with chest discomfort for the last 15 hours and progressively worsening
dyspnea over the last few hours presents to the Emergency Department and is diagnosed with anterior
STEMI. What, if any, reperfusion strategy should be undertaken?
A. Fibrinolysis
B. Immediate coronary angiography and PCI
C. *Symptomatic relief of angina and heart failure
D. CABG
E. None of the above
442. A 77-year old woman with a history of GERD presents in the first hour of an acute inferior STEMI.
The BP is normal. Invasive facilities are not readily available. What is the preferred strategy for
reperfusion therapy?
A. *Fibrinolytic therapy
B. Transfer for immediate coronary angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa
D. Symptomatic relief of angina only
E. CABG
443. You are seeing in your office a patient with the chief complaint of relatively sudden onset of
shortness of breath and weakness but no chest pain. ECG shows nonspecific ST-T changes. You would
be particularly attuned to the possibility of painless, or silent, myocardial infarction in the
A. Advanced coronary artery disease patient with unstable angina on multiple medications
B. *Elderly diabetic
C. Premenopausal female
D. Inferior MI patient
E. MI patient with PVCs
444. A 71-year-old female is admitted with acute myocardial infarction and congestive heart failure,
then has an episode of ventricular tachycardia. She is prescribed multiple medications and soon develops
confusion and slurred speech. The most likely cause of this confusion is
A. Captopril
B. Digoxin
C. Furosemide
D. *Lidocaine
E. Nitroglycerin
445. Two weeks after hospital discharge for documented myocardial infarction, a 65-year-old returns to
your office very concerned about low-grade fever and pleuritic chest pain. There is no associated
shortness of breath. Lungs are clear to auscultation and heart exam is free of significant murmurs,
gallops, or rubs. ECG is unchanged from the last one in the hospital. The most effective therapy is likely
A. Antibiotics
B. Anticoagulation with warfarin (Coumadin)
C. *An anti-inflammatory agent
D. An increase in antianginal medication
E. An antianxiety agent
446. A 48-year-old man is admitted to the coronary care unit with an acute inferior myocardial
infarction. Two hours after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per
minute with sinus rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 g/min
447. A 55-year-old patient presents to you with a history of having recently had a myocardial infarction
with a 5-day hospital stay while away on a business trip. He reports being told he had mild congestive
heart failure then, but is asymptomatic now with normal physical exam. You recommend which of the
following medications?
A. *An ACE inhibitor
B. Digoxin
C. Diltiazem
D. Furosemide (Lasix)
E. Hydralazine plus nitrates
448. A 57-year-old man is admitted to the CCU with an acute inferior myocardial infarction. Two hours
after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per minute with sinus
rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 mcg/min
449. A 70-year-old retired banker with no past medical history presents to the emergency department 4 h
after the onset of severe substernal crushing chest pain with radiation to the left arm and neck.
Electrocardiography reveals significant ST-segment elevation in leads I, L, V5, and V6. The patient has
no clear-cut medical contraindications to anticoagulation. Which of the following would be the optimal
management strategy at this time?
A. Intravenous tissue plasminogen activator alone
B. Intravenous tissue plasminogen activator and aspirin
C. Intravenous tissue plasminogen activator and heparin
D. *Intravenous tissue plasminogen activator, heparin, and aspirin
E. Thrombolytic therapy is contraindicated because of the patient's age
450. A previously healthy 58-year-old man is admitted to the hospital because of an acute inferior
myocardial infarction. Within several hours, he becomes oliguric and hypotensive (blood pressure is
90/60 mmHg). Insertion of a pulmonary artery (Swan-Ganz) catheter reveals the following pressures:
pulmonary capillary wedge, 4 mmHg; pulmonary artery, 22/4 mmHg; and mean right atrial, 11 mmHg.
This man would best be treated with
A. *fluids
B. digoxin
C. norepinephrine
D. dopamine
E. intraaortic balloon counterpulsation
451. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block. Chest plain film is normal. Which of the following is likely to be found in addition
on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
452. A 42-year-old man presents with Löffler endocarditis. Expected findings include all of the
following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
453. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
454. A 24-year-old previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
455. A 78-year-old woman with CHF (EF, 25%), chronic AFib, GERD, HTN, hyperlipidemia, diabetes,
and osteoporosis takes 12 different pills. Recently her neighbour, a nurse told her that she does not need
to take digoxin because she is on amiodarone. She wants to eliminate digoxin from her medication
regimen, and she wants to know why you put her on it in the first place. What is your answer?
A. Digoxin improves survival
B. *Digoxin reduces hospitalizations
C. Digoxin improves contractility
D. Digoxin decreases the volume of distribution of amiodarone
E. Digoxin reduces sympathetic nervous system activity
456. A 59-year-old woman with CHF and an EF of 30% comes to your office for follow-up. She is on
carvedilol, enalapril, aspirin, atorvastatin calcium, digoxin, and furosemide. She has been doing well
without any rehospitalization. However, she wants to improve her exercise tolerance. What should you
recommend?
A. Cardiac transplantation
B. I.V. dobutamine
C. Higher doses of ACE inhibitor
D. Adding spironolactone
E. *Enrolling her in an exercise training program
457. You see a 37-year-old man who presents with Löffler endocarditis. Expected findings include all of
the following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
458. A 23-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
459. A 28-y.o. previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
460. J. is an obese 54-yer-old man with peripheral arterial disease revealed by arterial duplex study. He
denies exertional chest discomfort of dyspnea, but lives a fairly sedentary lifestyle. Physical exam reveals
an obese man with normal BP, an unremarkable cardiac exam. His fasting lipids are as follows: TC 240
mg/dL, TG 250 mg/dL, HDL-C 35 mg/dL, LDL-C (calculated)155. Initial therapy should include:
A. TLC (therapeutic lifestyle correction) only
B. *TLC plus a statin with a goal of reducing LDL-C to <100 mg/dL
C. TLC plus niacine or fibrate, with the goals of reducing LDL-C to <100 mg/dL and TG <150 mg/dL
D. TLC plus a statin with a goal of reducing LDL-C to <130 mg/dL
E. TLC plus a statin, as well as niacin or a fibrate, with the goals of reducing LDL-C to <100 mg/dL
and TG <150 mg/dL
461. L. is a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. Initial therapy should include:
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. TLC plus a statin to reduce LDL-C to <130
D. TLC to reduce LDL-C to <130 *
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
462. V. is a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. If V. were found to have untreated hypertension (SBP of 160), with all other data the
same, what would be the preferred initial treatment in addition to BP control?
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. *TLC plus a statin to reduce LDL-C to <100
D. TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
463. H. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
what is your first goal of drug treatment?
A. Increase the HDL-H
B. Lower the LDL-C
C. Lower the TG
D. Lower the TG and increase the HDL-C
E. *Lower the non-HDL-C
464. G. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
which of the following would allow you to achieve the goal of lowering the non-HDL-C?
A. Increase the dose of atorvastatin
B. Add a fibrate
C. Add niacin
D. Add ezetimibe
E. *Any of the above
465. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of CHD.
He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel is as
follows: TC 220, HDL-C 40, LDL-C 120, TG 600. After recommending lifestyle modifications, what
would be your next step in lipid management?
A. Increase the HDL-H
B. Lower the LDL-C
C. *Lower the TG
D. Lower the TG and increase the HDL-C
E. Lower the non-HDL-C
466. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
sinus bradycardia at a rate of 40 with hypotension. Choose the best next step in antiarrhythmic
management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
467. A 58-year-old female smoker admitted to the ICU with respiratory distress due to pneumonia. This
was complicated by an anterior MI, with management including cautious use of beta-blockers. She now
develops 10 to 12 PVC’s per hour, occasional couplets, and a few short runs of ventricular tachycardia,
although BP and oxygen saturation remain stable. Choose the best next step in antiarrhythmic
management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Observation
E. Quinidine
468. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
469. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely CONTRAINDICATED to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifidipine
470. Z. is a 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus. He presents
to the outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing
to consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant
for the presence of microalbuminuria. Which of the following medications would be the most
appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
471. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
472. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
473. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
474. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
475. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Torasemide
B. *Metoprolol
C. Lisinopril
D. Nifedipine XR
E. All of the above
476. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
477. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
478. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
479. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
480. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
481. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
482. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
483. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
484. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
485. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
486. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension. On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal. CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
487. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal. What is the appropriate
course of action regarding the patient’s antihypertensive therapy?
A. Advise a low-sodium diet
B. *Discontinue doxazosin therapy and consider an alternative agent
C. Advise high dietary intake of calcium and potassium
D. Increase the doxazosin to 4 mg a day
E. Advise magnesium supplements
488. At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
489. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
490. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
most likely diagnosis is:
A. *Aortic coarctation
B. Conn syndrome
C. Liddle syndrome
D. Cushing syndrome
E. Essential hypertension
491. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Mitral regurgitation
D. Pulmonary artery stenosis
E. Tricuspid atresia
492. 190. A 55-year-old male with diabetes mellitus presents to his cardiologist with a BP of 165/95
mmHg. According to the JNC 7 guidelines, he would be classified as what stage of hypertension and
what is his target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
493. A 63-year-old man with long-standing insulin-requiring diabetes presented to the physician's office
for management of hypertension (160/94 mmHg). Urine and serum chemistries at that time were normal
except for serum creatinine = 1,6 mg/dl (0,141 mcmol/l) and blood urea nitrogen (BUN) = 30 mg/dl. A
potassium-sparing diuretic (triamterene-hydrochlorothiazide) was prescribed. When he returns 2 weeks
later, the serum potassium level is 6,8 mmol/l with no significant change in BUN or creatinine. The most
likely explanation is:
A. Excessive consumption of tomatoes and bananas
B. A recent urinary tract infection
C. Primary hyperaldosteronism
D. *Hyporeninemic hypoaldosteronism
E. Cushing syndrome
494. A 30-year-old male with no past medical history presents to his primary care physician complaining
of new-onset morning headaches that have been ongoing for the past few weeks. His BP is noted to be
220/110 mmHg with a gradient between his brachial and popliteal arteries. On auscultation there is a 2/6
systolixc crescendo-decrescendo murmur heard across the precordium. His ECG is significant for LVH.
A CXR shows cardiomegaly with evidence of rib notching. The patient most likely has what valvular
abnormality?
A. Mitral regurgitation
B. *Bicuspid aortic valve
C. Mitral stenosis
D. Tricuspid regurgitation
E. Pulmonary stenosis
495. A 36-year-old female with diabetes mellitus and hyperlipidemia and no history of hypertension is
noted at her yearly clinic visit to have new-onset hypertension with a BP of 180/110 mmHg. She
undergoes screening for secondary causes of hypertension and is found to have a pheochromocytoma.
What of the following medications is contraindicated as monotherapy?
A. *Atenolol
B. Lisinopril
C. Felodipine
D. Hydrochlorothiazide
E. Captopril
496. A 50-year-old male with chronic kidney disease and hypertension has a BP of 165/110 mmHg.
What is this patient's target BP according to the JNC 7 guidelines?
A. 140/90 mmHg
B. *130/80 mmHg
C. 120/80 mmHg
D. 115/70 mmHg
E. 110/70 mmHg
497. As a cardiologist you see a 55-year-old male with diabetes mellitus and a BP of 165/95 mmHg.
According to the JNC 7 guidelines, he would be classified as what stage of hypertension and what is his
target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
498. You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
499. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Hydrochlorothiazide
B. *Metoprolol
C. Perindopril
D. Nifedipine XR
E. All of the above
500. A 52-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 160 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
501. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
502. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Torasemide
E. Terazozin
503. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate lisinopril
E. Initiate metoprolol
504. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
505. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
506. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
507. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
508. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
509. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
510. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension.On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal.CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
511. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal.
A. What is the appropriate course of action regarding the patient’s antihypertensive therapy?
B. Advise a low-sodium diet
C. *Discontinue doxazosin therapy and consider an alternative agent
D. Advise high dietary intake of calcium and potassium
E. Increase the doxazosin to 4 mg a day
F. Advise magnesium supplements
512. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
513. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Thiazide diuretics
514. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. Mitral regurgitation
E. Tricuspid atresia
515. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
516. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. RBBB
E. Tricuspid atresia
517. A 54-year old man with a history of hypertension presents with chest pain that started 2 hours ago
and is diagnosed in the Emergency Department with anterior STEMI. His BP is 200/100 mmHg. He
receives i.v. metoprolol and the BP falls to 170/85 mmHg. What is the most appropriate reperfusion
strategy?
A. *Fibrinolytic therapy
B. Angiography and PCI
C. Medical therapy alone and PCI at a later date
D. CABG
E. None of the above
518. A 75-year old woman presents to a community hospital (without invasive capabilities) with 6 hrs of
chest pain and is diagnosed with inferior STEMI. The anticipated transfer to a medical center with
primary PCI capability will take 2 hours. What is the preferred reperfusion therapy?
A. *Fibrinolytic therapy at presentation to the hospital
B. Transfer for angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa inhibition at the presentation hospital and transfer for rescue
PCI if it fails to produce reperfusion
D. PCI at a later date
E. CABG
519. A 48-year old man with an anterior STEMI receives fibrinolytic therapy with reteplase. Thirty min.
after the second bolus he continues to have chest pain and his ECG demonstrates mild (estimated 30%
resolution) of the ST segment elevations. What is the next correct step in his management?
A. Readministration of a different fibrinolytic agent
B. Administration of GP IIb/IIIa inhibitor
C. *Immediate coronary angiography and rescue PCI
D. Symptomatic relief of angina and heart failure
E. Medical therapy and PCI at a later date
520. A 50-year old man presents to the emergency room about 1.5 hrs after the onset of chest pain. An
ECG showed 3 mm ST elevation in the anterior and lateral leads. Which of the following statements
regarding his management is correct?
A. Primary PCI is recommended over thrombolytics because PCI has short-term mortality benefit,
reduced reinfarction risk, and reduced risk of stroke
B. *Thrombolysis is recommended because door-to-baloon time is >90 min.
C. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
D. The patient should be referred for emergency CABG for better survival advantage.
E. Scheduled CABG
521. A 65-year old woman developed cardiogenic shock 10 hrs after presenting with anterior wall MI.
The most appropriate management strategy is....
A. Administration of thrombolytics
B. Watchful waiting after initiation of inotropic support and insertion of an intra-aortic balloon pump
C. *Coronary angiography with revascularization within 18 hrs of shock onset
D. Half-dose fibrinolysis and GP IIb/IIIa
E. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
522. A 62-year old woman, current smoker, diabetic, hypertensive and hyperlipidemic, presented to the
ER with a 2 day history of intermittent chest pain. The patient does not have any signs of heart failure.
An ECG showed 2-mm depression in V2-V6. The coronary angiogram showed 90% stenosis in the
proximal third of the LAD, 80% stenosis in the proximal RCA, with 30% disease in the middle
circumflex artery. The best plan of treatment for this patient is
A. PCI to both the LAD and RCA now
B. *Referral for two-vessel CABG
C. PCI to the LAD with staged intervention to the RCA
D. Medical management with no PCI or CABG
E. Thrombolysis is recommended
523. A 60-year-old male patient on aspirin, nitrates, and a beta blocker, being followed for chronic stable
angina, presents to the ER with a history of two to three episodes of more severe and long-lasting anginal
chest pain each day over the past 3 days. His ECG and cardiac enzymes are normal. The best course of
action of the following is to
A. Admit the patient and begin intravenous digoxin.
B. *Admit the patient and begin intravenous heparin
C. Admit the patient and give prophylactic thrombolytic therapy
D. Admit the patient for observation with no change in medication
E. Discharge the patient from the ER with increases in nitrates and beta blockers
524. A 60-year-old white female presents with epigastric pain, nausea and vomiting, heart rate of 50, and
pronounced first-degree AV block on ER cardiac monitor. Blood pressure is 130/80. The coronary artery
most likely to be involved in this process is the
A. *Right coronary
B. Left main
C. Left anterior descending
D. Circumflex
E. Left coronary
525. An 80-year old woman with chest discomfort for the last 15 hours and progressively worsening
dyspnea over the last few hours presents to the Emergency Department and is diagnosed with anterior
STEMI. What, if any, reperfusion strategy should be undertaken?
A. Fibrinolysis
B. Immediate coronary angiography and PCI
C. *Symptomatic relief of angina and heart failure
D. CABG
E. None of the above
526. A 77-year old woman with a history of GERD presents in the first hour of an acute inferior STEMI.
The BP is normal. Invasive facilities are not readily available. What is the preferred strategy for
reperfusion therapy?
A. *Fibrinolytic therapy
B. Transfer for immediate coronary angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa
D. Symptomatic relief of angina only
E. CABG
527. You are seeing in your office a patient with the chief complaint of relatively sudden onset of
shortness of breath and weakness but no chest pain. ECG shows nonspecific ST-T changes. You would
be particularly attuned to the possibility of painless, or silent, myocardial infarction in the
A. Advanced coronary artery disease patient with unstable angina on multiple medications
B. *Elderly diabetic
C. Premenopausal female
D. Inferior MI patient
E. MI patient with PVCs
528. A 75-year-old female is admitted with acute myocardial infarction and congestive heart failure,
then has an episode of ventricular tachycardia. She is prescribed multiple medications and soon develops
confusion and slurred speech. The most likely cause of this confusion is
A. Captopril
B. Digoxin
Furosemide
C. *Lidocaine
D. Nitroglycerin
529. Two weeks after hospital discharge for documented myocardial infarction, a 65-year-old returns to
your office very concerned about low-grade fever and pleuritic chest pain. There is no associated
shortness of breath. Lungs are clear to auscultation and heart exam is free of significant murmurs,
gallops, or rubs. ECG is unchanged from the last one in the hospital. The most effective therapy is likely
A. Antibiotics
B. Anticoagulation with warfarin (Coumadin)
C. *An anti-inflammatory agent
D. An increase in antianginal medication
E. An antianxiety agent
530. A 48-year-old man is admitted to the coronary care unit with an acute inferior myocardial
infarction. Two hours after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per
minute with sinus rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 g/min
531. A 55-year-old patient presents to you with a history of having recently had a myocardial infarction
with a 5-day hospital stay while away on a business trip. He reports being told he had mild congestive
heart failure then, but is asymptomatic now with normal physical exam. You recommend which of the
following medications?
A. *An ACE inhibitor
B. Digoxin
C. Diltiazem
D. Furosemide (Lasix)
E. Hydralazine plus nitrates
532. A 57-year-old man is admitted to the CCU with an acute inferior myocardial infarction. Two hours
after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per minute with sinus
rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 mcg/min
533. A 70-year-old retired banker with no past medical history presents to the emergency department 4 h
after the onset of severe substernal crushing chest pain with radiation to the left arm and neck.
Electrocardiography reveals significant ST-segment elevation in leads I, L, V5, and V6. The patient has
no clear-cut medical contraindications to anticoagulation. Which of the following would be the optimal
management strategy at this time?
A. Intravenous tissue plasminogen activator alone
B. Intravenous tissue plasminogen activator and aspirin
C. Intravenous tissue plasminogen activator and heparin
D. *Intravenous tissue plasminogen activator, heparin, and aspirin
E. Thrombolytic therapy is contraindicated because of the patient's age
534. A previously healthy 58-year-old man is admitted to the hospital because of an acute inferior
myocardial infarction. Within several hours, he becomes oliguric and hypotensive (blood pressure is
90/60 mmHg). Insertion of a pulmonary artery (Swan-Ganz) catheter reveals the following pressures:
pulmonary capillary wedge, 4 mmHg; pulmonary artery, 22/4 mmHg; and mean right atrial, 11 mmHg.
This man would best be treated with
A. *fluids
B. digoxin
C. norepinephrine
D. dopamine
E. intraaortic balloon counterpulsation
535. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block. Chest plain film is normal. Which of the following is likely to be found in addition
on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
536. A 42-year-old man presents with Löffler endocarditis. Expected findings include all of the
following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
537. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. Hypertrophic cardiomyopathy *
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
538. A 27-year-old previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
539. A 78-year-old woman with CHF (EF, 25%), chronic AFib, GERD, HTN, hyperlipidemia, diabetes,
and osteoporosis takes 12 different pills. Recently her neighbour, a nurse told her that she does not need
to take digoxin because she is on amiodarone. She wants to eliminate digoxin from her medication
regimen, and she wants to know why you put her on it in the first place. What is your answer?
A. Digoxin improves survival
B. *Digoxin reduces hospitalizations
C. Digoxin improves contractility
D. Digoxin decreases the volume of distribution of amiodarone
E. Digoxin reduces sympathetic nervous system activity
540. A 59-year-old woman with CHF and an EF of 30% comes to your office for follow-up. She is on
carvedilol, enalapril, aspirin, atorvastatin calcium, digoxin, and furosemide. She has been doing well
without any rehospitalization. However, she wants to improve her exercise tolerance. What should you
recommend?
A. Cardiac transplantation
B. I.V. dobutamine
C. Higher doses of ACE inhibitor
D. Adding spironolactone
E. *Enrolling her in an exercise training program
541. You see a 37-year-old man who presents with Löffler endocarditis. Expected findings include all of
the following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
542. A 23-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
543. A 28-y.o. previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
544. is an obese 54-yer-old man with peripheral arterial disease revealed by arterial duplex study. He
denies exertional chest discomfort of dyspnea, but lives a fairly sedentary lifestyle. Physical exam reveals
an obese man with normal BP, an unremarkable cardiac exam. His fasting lipids are as follows: TC 240
mg/dL, TG 250 mg/dL, HDL-C 35 mg/dL, LDL-C (calculated)155. Initial therapy should include:
A. *TLC only
B. TLC plus a statin with a goal of reducing LDL-C to <130 mg/dL
C. TLC plus niacine or fibrate, with the goals of reducing LDL-C to <100 mg/dL and TG <150 mg/dL
D. TLC plus a statin with a goal of reducing LDL-C to <100 mg/dL
E. TLC plus a statin, as well as niacin or a fibrate, with the goals of reducing LDL-C to <100 mg/dL
and TG <150 mg/dL
545. You see a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. Initial therapy should include:
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. TLC plus a statin to reduce LDL-C to <130
D. *TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
546.
You see a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is
very worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke,
and keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA
symptoms. Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. If she were found to have untreated hypertension (SBP of 160), with all other data the
same, what would be the preferred initial treatment in addition to BP control?
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. *TLC plus a statin to reduce LDL-C to <100
D. TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
547. J. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
what is your first goal of drug treatment?
A. Increase the HDL-H
B. Lower the LDL-C
C. Lower the TG
D. Lower the TG and increase the HDL-C
E. *Lower the non-HDL-C
548. G. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
which of the following would allow you to achieve the goal of lowering the non-HDL-C?
A. Increase the dose of atorvastatin
B. Add a fibrate
C. Add niacin
D. Add ezetimibe
E. *Any of the above
549. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of CHD.
He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel is as
follows: TC 220, HDL-C 40, LDL-C 120, TG 600. After recommending lifestyle modifications, what
would be your next step in lipid management?
A. Increase the HDL-H
B. Lower the LDL-C
C. *Lower the TG
D. Lower the TG and increase the HDL-C
E. Lower the non-HDL-C
550. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
sinus bradycardia at a rate of 40 with hypotension. Choose the best next step in antiarrhythmic
management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
551. A 58-year-old female smoker admitted to the ICU with respiratory distress due to pneumonia. This
was complicated by an anterior MI, with management including cautious use of beta-blockers. She now
develops 10 to 12 PVC’s per hour, occasional couplets, and a few short runs of ventricular tachycardia,
although BP and oxygen saturation remain stable. Choose the best next step in antiarrhythmic
management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Observation
E. Quinidine
552. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
553. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely CONTRAINDICATED to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifidipine
554. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
555. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
556. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
557. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
558. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
559. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Torasemise
B. *Metoprolol
C. Captopril
D. Enalapril
E. Amlodipine
560. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
561. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
562. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
563. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
564. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
565. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
566. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
567. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
568. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
569. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
570. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension. On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal. CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
571. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal. What is the appropriate
course of action regarding the patient’s antihypertensive therapy?
A. Advise a low-sodium diet
B. *Discontinue doxazosin therapy and consider an alternative agent
C. Advise high dietary intake of calcium and potassium
D. Increase the doxazosin to 4 mg a day
E. Advise magnesium supplements
572. At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
573. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
574. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. RBBB
E. Tricuspid atresia
575. 262. A 55-year-old male with diabetes mellitus presents to his cardiologist with a BP of 165/95
mmHg. According to the JNC 7 guidelines, he would be classified as what stage of hypertension and
what is his target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
576. A 59-year-old man with long-standing insulin-requiring diabetes presented to the physician's office
for management of hypertension (160/94 mmHg). Urine and serum chemistries at that time were normal
except for serum creatinine = 1,6 mg/dl (0,141 mcmol/l) and blood urea nitrogen (BUN) = 30 mg/dl. A
potassium-sparing diuretic (triamterene-hydrochlorothiazide) was prescribed. When he returns 2 weeks
later, the serum potassium level is 6,8 mmol/l with no significant change in BUN or creatinine. The most
likely explanation is:
A. Excessive consumption of tomatoes and bananas
B. A recent urinary tract infection
C. Primary hyperaldosteronism
D. *Hyporeninemic hypoaldosteronism
E. Cushing syndrome
577. A 30-year-old male with no past medical history presents to his primary care physician complaining
of new-onset morning headaches that have been ongoing for the past few weeks. His BP is noted to be
220/110 mmHg with a gradient between his brachial and popliteal arteries. On auscultation there is a 2/6
systolixc crescendo-decrescendo murmur heard across the precordium. His ECG is significant for LVH.
A CXR shows cardiomegaly with evidence of rib notching. The patient most likely has what valvular
abnormality?
A. Mitral regurgitation
B. *Bicuspid aortic valve
C. Mitral stenosis
D. Tricuspid regurgitation
E. Mitral regurgitation
578. A 36-year-old female with diabetes mellitus and hyperlipidemia and no history of hypertension is
noted at her yearly clinic visit to have new-onset hypertension with a BP of 180/110 mmHg. She
undergoes screening for secondary causes of hypertension and is found to have a pheochromocytoma.
What of the following medications is contraindicated as monotherapy?
A. *Metoprolol
B. Lisinopril
C. Phentolamine
D. Hydrochlorothiazide
E. Captopril
579. A 50-year-old male with chronic kidney disease and hypertension has a BP of 165/110 mmHg.
What is this patient's target BP according to the JNC 7 guidelines?
A. 140/90 mmHg
B. *130/80 mmHg
C. 120/80 mmHg
D. 115/70 mmHg
E. 110/70 mmHg
580. As a cardiologist you see a 55-year-old male with diabetes mellitus and a BP of 165/95 mmHg.
According to the JNC 7 guidelines, he would be classified as what stage of hypertension and what is his
target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
581. You see a diabetic patient presents with BP readings that are 155/95 or higher. All of the following
statements about the treatment of this patient's hypertension are correct EXCEPT:
A. Pharmacologic blocade of the renin-angiotensin system reduces the risk of both microvascular and
macrovascular events
B. Aggressive BP control reduces cardiovascular events more in diabetics than in nondiabetics
C. *Calcium channel blockers show no benefit in reducing cardiovascular events
D. The goal BP for this patient is <130/80 mmHg
E. All the above statements are correct
582. A 45-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Hydrochlorothiazide
B. *Metoprolol
C. Lisinopril
D. None of the above
E. All of the above
583. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
584. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
585. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
586. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
587. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
588. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
589. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
590. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
591. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
592. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
593. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension.On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal.CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
594. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal.
A. What is the appropriate course of action regarding the patient’s antihypertensive therapy?
B. Advise a low-sodium diet
C. *Discontinue doxazosin therapy and consider an alternative agent
D. Advise high dietary intake of calcium and potassium
E. Increase the doxazosin to 4 mg a day
F. Advise magnesium supplements
595. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. Which BP profile represents the best therapeutic goal for this patient?
A. <160/90
B. <140/90
C. *<130/85
D. <125/75
E. <140/85
596. A 40-year-old diabetic patient presents with a blood pressure (BP) of 145/90 mmHg and
proteinuria. What is the best medication for the initial management of this patient’s hypertension?
A. Calcium channel blockers
B. Beta blockers
C. *ACE-inhibitors / angiotensin receptor blockers
D. Alpha blockers
E. Diuretics
597. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. RBBB
E. Tricuspid atresia
598. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
599. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Preexcitation syndrome
D. Long QT syndrome
E. Short QT syndrome
600. A 54-year old man with a history of hypertension presents with chest pain that started 2 hours ago
and is diagnosed in the Emergency Department with anterior STEMI. His BP is 200/100 mmHg. He
receives i.v. metoprolol and the BP falls to 170/85 mmHg. What is the most appropriate reperfusion
strategy?
A. *Fibrinolytic therapy
B. Angiography and PCI
C. Medical therapy alone and PCI at a later date
D. CABG
E. None of the above
601. A 75-year old woman presents to a community hospital (without invasive capabilities) with 6 hrs of
chest pain and is diagnosed with inferior STEMI. The anticipated transfer to a medical center with
primary PCI capability will take 2 hours. What is the preferred reperfusion therapy?
A. *Fibrinolytic therapy at presentation to the hospital
B. Transfer for angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa inhibition at the presentation hospital and transfer for rescue
PCI if it fails to produce reperfusion
D. PCI at a later date
E. CABG
602. A 48-year old man with an anterior STEMI receives fibrinolytic therapy with reteplase. Thirty min.
after the second bolus he continues to have chest pain and his ECG demonstrates mild (estimated 30%
resolution) of the ST segment elevations. What is the next correct step in his management?
A. Readministration of a different fibrinolytic agent
B. Administration of GP IIb/IIIa inhibitor
C. *Immediate coronary angiography and rescue PCI
D. Symptomatic relief of angina and heart failure
E. Medical therapy and PCI at a later date
603. A 50-year old man presents to the emergency room about 1.5 hrs after the onset of chest pain. An
ECG showed 3 mm ST elevation in the anterior and lateral leads. Which of the following statements
regarding his management is correct?
A. Primary PCI is recommended over thrombolytics because PCI has short-term mortality benefit,
reduced reinfarction risk, and reduced risk of stroke
B. *Thrombolysis is recommended because door-to-baloon time is >90 min.
C. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
D. The patient should be referred for emergency CABG for better survival advantage.
E. Scheduled CABG
604. A 65-year old woman developed cardiogenic shock 10 hrs after presenting with anterior wall MI.
The most appropriate management strategy is....
A. Administration of thrombolytics
B. Watchful waiting after initiation of inotropic support and insertion of an intra-aortic balloon pump
C. *Coronary angiography with revascularization within 18 hrs of shock onset
D. Half-dose fibrinolysis and GP IIb/IIIa
E. Half-dose thrombolysis should be recommended; then the patient should be transferred for PCI.
605. A 62-year old woman, current smoker, diabetic, hypertensive and hyperlipidemic, presented to the
ER with a 2 day history of intermittent chest pain. The patient does not have any signs of heart failure.
An ECG showed 2-mm depression in V2-V6. The coronary angiogram showed 90% stenosis in the
proximal third of the LAD, 80% stenosis in the proximal RCA, with 30% disease in the middle
circumflex artery. The best plan of treatment for this patient is
A. PCI to both the LAD and RCA now
B. *Referral for two-vessel CABG
C. PCI to the LAD with staged intervention to the RCA
D. Medical management with no PCI or CABG
E. Thrombolysis is recommended
606. A 60-year-old male patient on aspirin, nitrates, and a beta blocker, being followed for chronic stable
angina, presents to the ER with a history of two to three episodes of more severe and long-lasting anginal
chest pain each day over the past 3 days. His ECG and cardiac enzymes are normal. The best course of
action of the following is to
A. Admit the patient and begin intravenous digoxin.
B. *Admit the patient and begin intravenous heparin
C. Admit the patient and give prophylactic thrombolytic therapy
D. Admit the patient for observation with no change in medication
E. Discharge the patient from the ER with increases in nitrates and beta blockers
607. A 60-year-old white female presents with epigastric pain, nausea and vomiting, heart rate of 50, and
pronounced first-degree AV block on ER cardiac monitor. Blood pressure is 130/80. The coronary artery
most likely to be involved in this process is the
A. *Right coronary
B. Left main
C. Left anterior descending
D. Circumflex
E. Left coronary
608. An 80-year old woman with chest discomfort for the last 15 hours and progressively worsening
dyspnea over the last few hours presents to the Emergency Department and is diagnosed with anterior
STEMI. What, if any, reperfusion strategy should be undertaken?
A. Fibrinolysis
B. Immediate coronary angiography and PCI
C. *Symptomatic relief of angina and heart failure
D. CABG
E. None of the above
609. A 77-year old woman with a history of GERD presents in the first hour of an acute inferior STEMI.
The BP is normal. Invasive facilities are not readily available. What is the preferred strategy for
reperfusion therapy?
A. *Fibrinolytic therapy
B. Transfer for immediate coronary angiography and PCI
C. Half-dose fibrinolysis and GP IIb/IIIa
D. Symptomatic relief of angina only
E. CABG
610. You are seeing in your office a patient with the chief complaint of relatively sudden onset of
shortness of breath and weakness but no chest pain. ECG shows nonspecific ST-T changes. You would
be particularly attuned to the possibility of painless, or silent, myocardial infarction in the
A. Advanced coronary artery disease patient with unstable angina on multiple medications
B. *Elderly diabetic
C. Premenopausal female
D. Inferior MI patient
E. MI patient with PVCs
611. A 75-year-old female is admitted with acute myocardial infarction and congestive heart failure,
then has an episode of ventricular tachycardia. She is prescribed multiple medications and soon develops
confusion and slurred speech. The most likely cause of this confusion is
A. Captopril
B. Digoxin
Furosemide
C. *Lidocaine
D. Nitroglycerin
612. Two weeks after hospital discharge for documented myocardial infarction, a 65-year-old returns to
your office very concerned about low-grade fever and pleuritic chest pain. There is no associated
shortness of breath. Lungs are clear to auscultation and heart exam is free of significant murmurs,
gallops, or rubs. ECG is unchanged from the last one in the hospital. The most effective therapy is likely
A. Antibiotics
B. Anticoagulation with warfarin (Coumadin)
C. *An anti-inflammatory agent
D. An increase in antianginal medication
E. An antianxiety agent
613. A 48-year-old man is admitted to the coronary care unit with an acute inferior myocardial
infarction. Two hours after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per
minute with sinus rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 g/min
614. A 55-year-old patient presents to you with a history of having recently had a myocardial infarction
with a 5-day hospital stay while away on a business trip. He reports being told he had mild congestive
heart failure then, but is asymptomatic now with normal physical exam. You recommend which of the
following medications?
A. *An ACE inhibitor
B. Digoxin
C. Diltiazem
D. Furosemide (Lasix)
E. Hydralazine plus nitrates
615. A 57-year-old man is admitted to the CCU with an acute inferior myocardial infarction. Two hours
after admission, his blood pressure is 86/52 mmHg; his heart rate is 40 beats per minute with sinus
rhythm. Which of the following would be the most appropriate initial therapy?
A. Immediate insertion of a temporary transvenous pacemaker
B. *Intravenous administration of atropine sulfate, 0.6 mg
C. Administration of normal saline, 300 mL over 15 min
D. Intravenous administration of dobutamine, 0.35 mg/min
E. Intravenous administration of isoproterenol, 5.0 mcg/min
616. A 70-year-old retired banker with no past medical history presents to the emergency department 4 h
after the onset of severe substernal crushing chest pain with radiation to the left arm and neck.
Electrocardiography reveals significant ST-segment elevation in leads I, L, V5, and V6. The patient has
no clear-cut medical contraindications to anticoagulation. Which of the following would be the optimal
management strategy at this time?
A. Intravenous tissue plasminogen activator alone
B. Intravenous tissue plasminogen activator and aspirin
C. Intravenous tissue plasminogen activator and heparin
D. *Intravenous tissue plasminogen activator, heparin, and aspirin
E. Thrombolytic therapy is contraindicated because of the patient's age
617. A previously healthy 58-year-old man is admitted to the hospital because of an acute inferior
myocardial infarction. Within several hours, he becomes oliguric and hypotensive (blood pressure is
90/60 mmHg). Insertion of a pulmonary artery (Swan-Ganz) catheter reveals the following pressures:
pulmonary capillary wedge, 4 mmHg; pulmonary artery, 22/4 mmHg; and mean right atrial, 11 mmHg.
This man would best be treated with
A. *fluids
B. digoxin
C. norepinephrine
D. dopamine
E. intraaortic balloon counterpulsation
618. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block. Chest plain film is normal. Which of the following is likely to be found in addition
on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
619. A 42-year-old man presents with Löffler endocarditis. Expected findings include all of the
following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
620. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
621. A 24-year-old previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
622. A 78-year-old woman with CHF (EF, 25%), chronic AFib, GERD, HTN, hyperlipidemia, diabetes,
and osteoporosis takes 12 different pills. Recently her neighbour, a nurse told her that she does not need
to take digoxin because she is on amiodarone. She wants to eliminate digoxin from her medication
regimen, and she wants to know why you put her on it in the first place. What is your answer?
A. Digoxin improves survival
B. *Digoxin reduces hospitalizations
C. Digoxin improves contractility
D. Digoxin decreases the volume of distribution of amiodarone
E. Digoxin reduces sympathetic nervous system activity
623. A 59-year-old woman with CHF and an EF of 30% comes to your office for follow-up. She is on
carvedilol, enalapril, aspirin, atorvastatin calcium, digoxin, and furosemide. She has been doing well
without any rehospitalization. However, she wants to improve her exercise tolerance. What should you
recommend?
A. Cardiac transplantation
B. I.V. dobutamine
C. Higher doses of ACE inhibitor
D. Adding spironolactone
E. *Enrolling her in an exercise training program
624. A 34-year-old man is diagnosed with Löffler endocarditis. Expected findings include all of the
following EXCEPT:
A. Eosinophilia
B. Signs and symptoms of heart failure
C. *Asthma and nasal polyposis
D. Right ventricular pressure tracing showing "dip and plateau" pattern
E. Normal left ventricular ejection fraction
625. A 23-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. The murmur is
probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
626. A 28-y.o. previously healthy woman presents to the emergency department because of sudden
shortness of breath and right-sided pleuritic chest pain. She has been using oral contraceptives for the last
several years. The physical examination demonstrates a normotensive, tachycardic, and tachypneic
woman. Which of the following would be the most useful in EXCLUDING the diagnosis of pulmonary
embolism (PE)?
A. Normal PaO2 by arterial blood gas determination
B. Absence of right heart strain on ECG
C. Intermediate probability V/Q (ventilation/perfusion) lung scan
D. *Normal plasma level of D-dimer by ELISA (enzyme-linked immunosorbent assay)
E. Normal cardiopulmonary examination
627. X. is an obese 54-yer-old man with peripheral arterial disease revealed by arterial duplex study. He
denies exertional chest discomfort of dyspnea, but lives a fairly sedentary lifestyle. Physical exam reveals
an obese man with normal BP, an unremarkable cardiac exam. His fasting lipids are as follows: TC 240
mg/dL, TG 250 mg/dL, HDL-C 35 mg/dL, LDL-C (calculated)155. Initial therapy should include:
A. *TLC (therapeutic lifestyle correction) only
B. TLC plus a statin with a goal of reducing LDL-C to <130 mg/dL
C. TLC plus niacine or fibrate, with the goals of reducing LDL-C to <100 mg/dL and TG <150 mg/dL
D. TLC plus a statin with a goal of reducing LDL-C to <100 mg/dL
E. TLC plus a statin, as well as niacin or a fibrate, with the goals of reducing LDL-C to <100 mg/dL
and TG <150 mg/dL
628. Z. is a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. Initial therapy should include:
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. TLC plus a statin to reduce LDL-C to <130
D. *TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
629. W. is a 71-year-old retired female whose father died at age 52 of a “massive MI”. She is very
worried about her own risk of a heart attack. She watches her weight (BMI=23), does not smoke, and
keeps physically fit. She denies angina or dyspnea on exertion, claudication, or history of TIA symptoms.
Her fasting lipids are as follows: TC 250 mg/dL, TG 120 mg/dL, HDL-C 42 mg/dL, LDL-C
(calculated)151. If W. were found to have untreated hypertension (SBP of 160), with all other data the
same, what would be the preferred initial treatment in addition to BP control?
A. Nothing beyond her current lifestyle measures
B. Weight loss to bring BMI<20
C. *TLC plus a statin to reduce LDL-C to <100
D. TLC to reduce LDL-C to <130
E. Statin plus a niacin to reduce LDL-C<130 and increase HDL-C>50 mg/dL
630. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of CHD.
He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel is as
follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications, what is
your first goal of drug treatment?
A. Increase the HDL-H
B. Lower the LDL-C
C. Lower the TG
D. Lower the TG and increase the HDL-C
E. *Lower the non-HDL-C
631. Q. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of
CHD. He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel
is as follows: TC 220, HDL-C 40, LDL-C 120, TG 450. After recommending lifestyle modifications,
which of the following would allow you to achieve the goal of lowering the non-HDL-C?
A. Increase the dose of atorvastatin
B. Add a fibrate
C. Add niacin
D. Add ezetimibe
E. *Any of the above
632. is an obese nonsmoking 44-year-old man with treated hypertension and no family history of CHD.
He has had elevated LDL-C in the past and is taking atorvastatin 20 mg daily. His latest lipid panel is as
follows: TC 220, HDL-C 40, LDL-C 120, TG 600. After recommending lifestyle modifications, what
would be your next step in lipid management?
A. Increase the HDL-H
B. Lower the LDL-C
C. *Lower the TG
D. Lower the TG and increase the HDL-C
E. Lower the non-HDL-C
633. A 74-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
sinus bradycardia at a rate of 40 with hypotension. Choose the best next step in antiarrhythmic
management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
634. A 58-year-old female smoker admitted to the ICU with respiratory distress due to pneumonia. This
was complicated by an anterior MI, with management including cautious use of beta-blockers. She now
develops 10 to 12 PVC’s per hour, occasional couplets, and a few short runs of ventricular tachycardia,
although BP and oxygen saturation remain stable. Choose the best next step in antiarrhythmic
management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Observation
E. Quinidine
635. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
636. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely CONTRAINDICATED to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifidipine
637. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Methyldopa
C. *Lisinopril
D. Chlorthalidone
E. Terazozin
638. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
639. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
640. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. Start hydrochlorothiazide and lisinopril*
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
641. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
642. A 42-year-old female with chronic obstructive pulmonary disease is found on multiple office visits
to have elevated BP measurements. Which of the following medications is contraindicated?
A. Hydrochlorothiazide
B. *Metoprolol
C. Lisinopril
D. Furosemide
E. All of the above
643. A 48-year-old male with diabetes mellitus, hypertension, and hyperlipidemia presents to the ER
with hypertensive emergency. His mean arterial pressure is 150 mmHg. Which medications would be
most appropriate therapy for this patient?
A. *Nitroprusside
B. Enteral metoprolol
C. Fenoldopam
D. Intravenous nitroglycerine
E. Any of the above
644. A 34-year-old female with hypertension is considering becoming pregnant. Which of the following
medications would be absolutely contraindicated to control her BP during pregnancy?
A. Methyldopa
B. Metoprolol
C. Labetalol
D. *Captopril
E. Nifedipine
645. A 48-year-old obese male with hypertension, dyslipidemia, and diabetes mellitus presents to the
outpatient clinic for his yearly physical. He has refused medications in the past, but now is willing to
consider treatment. His BP is 145/95 mmHg with a HR of 80 bpm. His laboratory data are significant for
the presence of microalbuminuria. Which of the following medications would be the most appropriate?
A. Carvedilol
B. Amlodipine
C. *Lisinopril
D. Torasemide
E. Doxazozin
646. A 42-year-old male comes in for a routine physical examination. He is noted to have a BMI of 30,
impaired fasting glucose, and a BP of 135/85 mmHg. What is the best treatment plan for this individual?
A. *Aggressive lifestyle modification
B. Institute thiazide diuretic regimen
C. No treatment at this time
D. Initiate an ACE-inhibitor
E. Initiate a beta-blocker
647. A 62-year-old man with isolated essential hypertension, currently taking hydrochlorothiazide 25 mg
PO daily, comes to you for his first clinic visit. He notes that his BP at home is always less than 140/80
mmHg, but in clinic it is always at least 155/95 mmHg. What is the next step?
A. Increase dose of thiazide
B. Addition of second antihypertensive medication
C. *Do nothing as he has white coat hypertension
D. Evaluate for secondary causes of hypertension
E. Start metoprolol
648. A 34-year-old male with isolated essential hypertension presents to clinic and is found to have a BP
of 180/100 mmHg after failure of behavioral modifications. What is the most appropriate next step?
A. Start hydrochlorothiazide
B. *Start hydrochlorothiazide and lisinopril
C. Repeat BP in 4 weeks
D. Start amlodipine
E. Start doxazozin
649. A 56-year-old male on hydralazine, hydrochlorothiazide, lisinopril, and metoprolol begins to
develop a malar rash and arthralgias. Which of the above antihypertensive agents is known to cause druginduced lupus?
A. Hydrochlorothiazide
B. Lisinopril
C. *Hydralazine
D. Metoprolol
E. None of the above
650. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 45-year old female has been on diuretic, but BP remains elevated at 145/95, leading
to the proposed addition of lisinopril. Which key potential adverse effect should be discussed?
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. *Cough
E. Gynecomastia
651. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 58-year old male truck driver has significant hypertension, still not controlled on a
diuretic plus calcium channel blocker. Clonidine is being considered as the next medication, but in this
patients the concerns are sedation, sexual dysfunction, and ..... this side effect.
A. Increased triglyceride levels
B. Cough
C. Gynecomastia
D. *Rebound hypertension
E. Urinary retention
652. For the case below, select the most significant adverse effect of the antihypertensive and/or cardiac
agent in question: a 68-year old male with advanced chronic heart failure and BP 145/90 will have
spironolactone added to his regimen, but should be informed about .... this possible side effect.
A. Increased triglyceride levels
B. Peripheral edema
C. Lupus-like syndrome
D. Cough
E. *Gynecomastia
653. A 55-year old man is referred for evaluation of hypertension (BP 185/95 mmHg), discovered
during a BP screening at his workplace. The patient states that he is well and has not seen a physician in
many years. He is an active jogger, abstains from alcohol, and limits his salt and fat intake. He denies any
knowledge of hypertension, cardiovascular disease, or diabetes mellitus. He takes no medications
regularly. Family history is significant in that his father was known to be hypertensive and died of a
stroke. His older brother is being treated for hypertension. On examination, the patient appears well, with
a BP of 180/95 mmHg while seated and standing. Body weight is 71 kg, and height is 178 cm. Optic
fundus examination is significant for grade II hypertensive retinopathy. The remainder of the
examination is normal. CBC, electrolyte panel, BUN, creatinine, TSH levels, and results of urinalysis are
normal. ECG demonstrates normal sinus rhythm with LVH. To reduce the patient’s cardiovascular
morbidity and mortality, which therapy would you prescribe?
A. Hydralazine
B. Atenolol
C. *Losartan
D. Doxazosin
E. Clonidine
654. A 51-year-old man transfers to your practice. His medical history is positive for primary
hypertension without TOD. He has no history of renal or prostatic disease. Laboratory values obtained
from his former primary care physician show normal results for BUN, serum creatinine, electrolytes,
urinalysis, PSA, and ECG. He takes the alpha-blocker doxazosin, 2 mg at bedtime.On examination, BP is
150/90 mmHg seated and standing. The remainder of the examination is normal. What is the appropriate
course of action regarding the patient’s antihypertensive therapy?
A. Advise a low-sodium diet
B. *Discontinue doxazosin therapy and consider an alternative agent
C. Advise high dietary intake of calcium and potassium
D. Increase the doxazosin to 4 mg a day
E. Advise magnesium supplements
655. At a routine examination, an asymptomatic 46-year-old man is found to have a BP of 150/110
mmHg, but no other abnormalities are present. What do you do next?
A. Reassure the patient and repeat the physical examination in 12 months
B. Initiate antihypertensive therapy
C. *Obtain repeated BP recordings in your office and/or the patient’s home or work site
D. Hospitalize patient for renal arteriography
E. Order a 24-h ambulatory BP monitoring
656. A 60-year old white man consults you with a headache. Examination is unremarkable, except that
the blood pressure is raised and subsequent measurements confirm readings of 170/106 mmHg. He is
overweight, smokes 15 cigarettes per day and drinks 2 pints of beer per day. His investigations reveal a
fasting cholesterol of 6 mmol/l with a normal blood sugar and electrolyte profile and normal renal
function. There is no evidence of target organ damage.
A. This man needs immediate treatment with antihypertensive drugs, aspirin and a statin
B. *Initiate antihypertensive therapy with two-drug combination
C. At this age it is far more important to control the hyperlipidaemia than the BP
D. This man’s blood pressure could be wholly ascribed to his alcohol intake
E. This patient can be observed and counseled on maintaining a reasonable BMI
657. A 23-year old male seeks medical attention for the recent onset of headaches. The headaches are
described as “pounding” and occur during the day and night. He has minimal relief with acetaminophen.
Physical examination is notable for a BP of 185/115 mmHg in the right arm, a HR of 70/min,
arteriovenous nicking on funduscopic examination, normal jugular veins and carotid arteries, reduced
pulses in both lower extremities. Review of symptoms is positive only for leg fatigue with exertion. The
patient described in above is most likely to have which of the following associated cardiac abnormalities?
A. *Bicuspid aortic valve
B. Mitral stenosis
C. Atrial septal defect
D. Long QT syndrome
E. Tricuspid atresia
658. A 57-year-old male with diabetes mellitus presents to his cardiologist with a BP of 165/95 mmHg.
According to the JNC 7 guidelines, he would be classified as what stage of hypertension and what is his
target BP measurement?
A. Prehypertension, 140/90 mmHg
B. *Stage 2, 130/80 mmHg
C. Stage 1, 140/90 mmHg
D. Stage 2, 140/90 mmHg
E. Stage 3, 120/70 mmHg
Test questions for pictures
1.A patient in whom this echo image was obtained (Fig. 158) is most likely to have which of the
following cardiac abnormalities?
A. *Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Preexitation syndrome
D. Right bundle branch block
E. Tricuspid atresia
2.Match the ECG finding that is most closely associated with condition shown on Fig. 158
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment depression
E. *Deeply inverted precordial T waves
3.A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play collegiate
sports. He has no symptoms, has never had syncope, and has no known family history of cardiac disease.
A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur decreases in
intensity, and on sustained handgrip, the murmur alsop is decreased. An echo image is obtained (Fig.
158). The murmur is probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
4.A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Pericardial effusion
B. *Mitral valve disease
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic valve disease
5.On echo image (Fig. 159) arrows point:
A. A bulging aortic arch
B. *Anterior mitral leaflet
C. Enlarged left ventricle
D. Pulmonary artery
E. Double shadow (border of the right and left atria)
6.On echo image (Fig. 159) arrows shows:
A. A bulging aortic arch
B. A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. *Mitral valve
7.A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. *Mitral stenosis
E. Tricuspid regurgitation
8.A patient in whom this echo image was obtained (Fig. 160) is most likely to have which of the
following cardiac abnormalities?
A. *Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
9.This echocardiographic image (Fig. 161) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click and murmur on
auscultation
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, elevated jugular venous pressure,
and diffuse lung crackles on auscultation
D. *A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of systolic murmur who presents with syncope
10. Match the tracing (Fig. 162) with the correct interpretation:
A. *Sick sinus syndrome
B.
Junctional Rhythm
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
11. Match the tracing (Fig. 162) with the correct interpretation:
A. Idioventricular Rhythm
B. Junctional Rhythm
C. *Sick sinus syndrome
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
12. A 36-year-old white female nurse comes to the ER due to a sensation of irregular heart rate, slight
dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained
(Fig. 162), which shows...
A. Atrial fibrillation
B. Atrial flutter
C. *Sick sinus syndrome
D. Ventricular tachycardia
E.
13.
A.
B.
C.
D.
E.
14.
A.
B.
C.
D.
E.
15.
A.
B.
C.
D.
E.
16.
A.
B.
C.
D.
E.
17.
A.
B.
C.
D.
E.
18.
A.
B.
C.
D.
E.
19.
A.
B.
C.
D.
E.
20.
A.
B.
C.
D.
E.
21.
A.
B.
C.
Accelerated idioventricular rhythm
Match the tracing (Fig. 165) with the correct interpretation:
Sino-atrial block
*High-grade 2:1 AV block
AV II° block (Mobitz 1)
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 164) with the correct interpretation:
Sino-atrial block
AV I° block
AV II° block (Mobitz 1)
*AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 163) with the correct interpretation:
Sino-atrial block
AV I° block
*AV II° block (Mobitz 1)
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 165) with the correct interpretation:
*Advanced AV block
AV I° block
AV II° block (Mobitz 1)
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 165) with the correct interpretation:
Sino-atrial block
AV I° block
*Advanced 2:1 AV block
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Rate-dependent LBBB
Anterior hemiblock
*Bifascicular block
Normal ECG
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
*Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
*Bifascicular block
Anterior hemiblock
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
D.
E.
22.
A.
B.
C.
D.
E.
23.
A.
B.
C.
D.
E.
24.
A.
B.
C.
D.
E.
25.
A.
B.
C.
D.
E.
26.
A.
B.
C.
D.
E.
27.
A.
B.
C.
D.
E.
28.
A.
B.
C.
D.
E.
29.
A.
B.
C.
D.
E.
30.
A.
B.
Posterior hemiblock (PHB)
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 9) with the correct interpretation:
*Right bundle branch block (RBBB)
Bifascicular block
Anterior fascicular block
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior fascicular block
Bifascicular block (RBBB+AHB)
What type of arrhythmia is shown on ECG (Fig. 162) ?
*Sick sinus syndrome
AV nodal re-entry tachycardia
Sick sinus syndrome
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is shown on ECG (Fig. 165)?
V re-entry tachycardia in WPW
* Advanced AV block
Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is seen here (Fig. 165)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Advanced AV block
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 164)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Mobitz type 2 AV block
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 162)?
Premature junctional contractions (PJCs)
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Sick sinus syndrome
Supraventricular premature beats
What is seen in this ECG (Fig. 163)?
PJC (Premature junctional complex)
Atrial flutter
C. *Wenckebach type AV block
D. AV nodal reentrant tachycardia
E.
Accelerated junctional rhythm
31. What is seen in this ECG (Fig. 163)?
A. Sinus tachycardia
B. Paroxysmal supraventricular tachycardia
C. 3rd degree AV block
D. Atrial fibrillation
E. *Mobitz type I AV block
32. Match the tracing (Fig. 162) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. *Sick sinus syndrome
D. Atrial flutter
E. Accelerated idioventricular rhythm
33. Match the tracing (Fig. 162) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. WPW
D. Atrial flutter with rate-dependent LBBB
E. *SSS
34. Match the tracing (Fig. 163) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. Intermittent WPW
D. *Wenckebach type AV block
E. Accelerated idioventricular rhythm
35. Match the tracing (Fig. 163) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. *Wenckebach type AV block
D. Atrial flutter with 4:1 and 2:1 conduction and rate-dependent LBBB
E. Accelerated idioventricular rhythm
36. Match the tracing (Fig. 163) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. Intermittent WPW
D. *Mobitz type I AV block
E. Accelerated idioventricular rhythm
37. What is on this ECG (Fig. 163)?
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. Intermittent WPW
D. *Second degree AV block
E. Accelerated idioventricular rhythm
38. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
following rhythm (Fig. 164). Choose the best next step in antiarrhythmic management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
39. A 60-year old male during his first day post-MI in the CCU develops the following rhythm (Fig.
164). Choose the best next step in antiarrhythmic management.
A. Amiodarone
B. *Atropine
C. Digoxin
D. Diltiazem
E. Observation
40. Sudden cardiac death in patients <35 years old is most commonly associated with (Fig. 158)
A. *Hypertrophic cardiomyopathy
B. Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
41. This ECG of a 45-year-old man (Fig. 9) is consistent with:
A. *Right bundle branch block
B. Abnormal SCN5A channel (Brugada syndrome)
C. Abnormal KCQN1 channel (short QT syndrome)
D. Old anteroseptal myocardial infarction with an aneurysm
E. Congenital long QT syndrome
42. Match the tracing (Fig. 10) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. *Bifascicular block
E. AV second-degree block
43. Match the tracing (Fig. 165) with the correct interpretation:
A. Complete AV block
B. *High-grade AV block
C. Nonconducted premature atrial complex
D. AV first-degree block
E. AV second-degree block
44. Match the tracing (Fig. 164) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. AV first-degree block
E. *AV second-degree block
45. Match the tracing (Fig. 162) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. *Sick sinus syndrome
D. AV first-degree block
E. AV second-degree block
46. Match the tracing (Fig. 163) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. AV first-degree block
E. *AV second-degree block
47. Wenckebach phenomenon (Fig. 6) is defined as...
A. Progressive shortening of PR interval till a beat is dropped
B. *Progressive lengthening of PR interval till a beat is dropped
C. Irregular heart rate and PVC’s
D. Shortened QT intervals
E. Slurred QRS complex
48. A 65-year-old man with diabetes, on an oral hypoglycemic, presents to the ER with a sports-related
shoulder injury. His heart rate was noted to be irregular, and the following ECG was obtained (Fig. 163).
Which of the following is the best immediate therapy?
A. Atropine
B. Isoproterenol
C. Pacemaker placement
D. *Observation
E. Electrical cardioversion
49. Choose the correct interpretation of the tracing (Fig. 162):
A. *Sick sinus syndrome
B. Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
50. Choose the correct interpretation of the tracing (Fig. 162):
A. Idioventricular Rhythm
B. *Sick sinus syndrome
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
51. Choose the correct interpretation of the tracing (Fig. 163) :
A. Sino-atrial block
B. AV I° block
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
52. Choose the correct interpretation of the tracing (Fig. 164):
A. Sino-atrial block
B. AV I° block
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Complete AV block
53. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block (Fig. 164). Chest plain film is normal. Which of the following is likely to be found
in addition on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
54. A patient in whom this echo image was obtained (Fig. 158) is most likely to have which of the
following cardiac abnormalities?
A. *Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Restrictive cardiomyopathy
D. Aortic stenosis
E. Mitral stenosis
55. Match the ECG finding that is most closely associated with condition shown on Fig. 158
A. Low QRS voltage
B. Left bundle branch block
C. Right bundle branch block
D. Diffuse ST segment depression
E. *Deeply inverted precordial T waves
56. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. An echo image is
obtained (Fig. 185). The murmur is probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic stenosis
57. A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Pericardial effusion
B. *Mitral stenosis
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic stenosis
58. On echo image (Fig. 159) arrows point:
A. A bulging aortic arch
B. *Anterior mitral leaflet
C. Posterior mitral leaflet
D. Pulmonary artery
E. Double shadow (border of the right and left atria)
59. On echo image (Fig. 159) arrows shows:
A. A bulging aortic arch
B. A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. *Mitral anterior leaflet
60. A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. *Mitral stenosis
E. Pulmonary stenosis
61. A patient in whom this echo image was obtained (Fig. 160) is most likely to have which of the
following cardiac abnormalities?
A. *Aortic stenosis
B. Pulmonary regurgitation
C. Pulmonary regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
62. This echocardiographic image (Fig. 161) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click
B. A 22-year-old female who grew up in Central America who presents with dyspnea and atrial
fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, and diffuse lung crackles
D. *A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history MI who presents with syncope
63. Match the tracing (Fig. 162) with the correct interpretation:
A. *Sick sinus syndrome
B. AV I degree block
C. Complete AV block
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
64. Match the tracing (Fig. 162) with the correct interpretation:
A. Second degree AV block
B. Junctional Rhythm
C. *Sick sinus syndrome
D. Sino-atrial block
E. Complete AV block
65. A 36-year-old white female nurse comes to the ER due to a sensation of irregular heart rate, slight
dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained
(Fig. 162), which shows...
A. Atrial fibrillation
B. Sino-atrial block
C. *Sick sinus syndrome
D. Second degree AV block
E. Accelerated idioventricular rhythm
66. Match the tracing (Fig. 165) with the correct interpretation:
A. Sick sinus syndrome
B. *High-grade 2:1 AV block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. AV III° block
67. Match the tracing (Fig. 164) with the correct interpretation:
A. Sino-atrial block
B. Junctional rhythm
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Sick sinus syndrome
68. Match the tracing (Fig. 163) with the correct interpretation:
A. Sino-atrial block
B. Sick sinus syndromeS
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. High-grade AV block
69. Match the tracing (Fig. 165) with the correct interpretation:
A. *High-grade AV block
B. AV I° block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
70. Match the tracing (Fig. 165) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. *Advanced 2:1 AV block
D. AV II° block (Mobitz 2)
E. Complete AV block
71.
A.
B.
C.
D.
E.
72.
A.
B.
C.
D.
E.
73.
A.
B.
C.
D.
E.
74.
A.
B.
C.
D.
E.
75.
A.
B.
C.
D.
E.
76.
A.
B.
C.
D.
E.
77.
A.
B.
C.
D.
E.
78.
A.
B.
C.
D.
E.
79.
A.
B.
C.
D.
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Rate-dependent LBBB
Anterior fascicular block
*Bifascicular block
Left posterior fascicular block
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior fascicular block (AHB)
Posterior fascicular block (PHB)
*RBBB+AHB
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block
*Bifascicular block
Anterior hemiblock
Posterior hemiblock
Left bundle branch block
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Complete heart block
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block
Bifascicular block
Anterior fascicular block
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior fascicular block
Bifascicular block (RBBB+AHB)
What type of arrhythmia is shown on ECG (Fig. 162) ?
*Sick sinus syndrome
AV second-degree block
Sick sinus syndrome
PSVT (Paroxysmal Supraventricular Tachycardia)
Complete heart block
What type of arrhythmia is shown on ECG (Fig. 165)?
V re-entry tachycardia in WPW
*Advanced AV block
Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
E. AV second-degree block
80. What type of arrhythmia is seen here (Fig. 165)?
A. Right bundle branch block
B. Rate related bundle branch block
C. Premature atrial contractions conducted with aberrancy
D. *Advanced AV block
E. Supraventricular premature beats
81. What type of arrhythmia is seen here (Fig. 164)?
A. Premature junctional contractions
B. Wenckebach type AV block
C. Premature atrial contractions conducted with aberrancy
D. *Mobitz type 2 AV block
E. Supraventricular premature beats
82. What type of arrhythmia is seen here (Fig. 162)?
A. Complete heart block
B. Wenckebach type AV block
C. Premature atrial contractions conducted with aberrancy
D. *Sick sinus syndrome
E. Supraventricular premature beats
83. What is seen in this ECG (Fig. 163)?
A. Mobitz type 2 AV block
B. Sick sinus syndrome
C. *Wenckebach type AV block
D. AV nodal reentrant tachycardia
E.
Accelerated junctional rhythm
84. What is seen in this ECG (Fig. 163)?
A. Sinus tachycardia
B. Mobitz type II AV block
C. 3rd degree AV block
D. Atrial fibrillation
85. A patient in whom this echo image was obtained (Fig. 54) is most likely to have which of the
following cardiac abnormalities?
A. *Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Preexitation syndrome
D. Right bundle branch block
E. Tricuspid atresia
86. Match the ECG finding that is most closely associated with condition shown on Fig. 54
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment depression
E. *Deeply inverted precordial T waves
87. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. An echo image is
obtained (Fig. 54). The murmur is probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
88. A patient in whom this chest X-ray image was obtained (Fig. 55) is most likely to have which of the
following cardiac abnormalities?
A. Pericardial effusion
B. *Mitral valve disease
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic valve disease
89. On plain chest X-ray image (Fig. 55) arrow “a” shows:
A. A bulging aortic arch
B. *A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. Double shadow (border of the right and left atria)
90. On plain chest X-ray image (Fig. 55) arrow “b” shows:
A. A bulging aortic arch
B. A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. *Double shadow (border of the right and left atria)
91. The left ventricular enlargement seen on plain chest X-ray image (Fig. 55) is most likely due to:
A. Aortic stenosis
B. *Mitral regurgitation
C. Aortic regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
92. A patient in whom this echo image was obtained (Fig. 56) is most likely to have which of the
following cardiac abnormalities?
A. *Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
93. This echocardiographic image (Fig. 57) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click and murmur on
auscultation
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, elevated jugular venous pressure,
and diffuse lung crackles on auscultation
D. *A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of systolic murmur who presents with syncope
94. Match the tracing (Fig. 58) with the correct interpretation:
A. *Sick sinus syndrome
B. Junctional Rhythm
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
95. Match the tracing (Fig. 74) with the correct interpretation:
A. Idioventricular Rhythm
B. Junctional Rhythm
C. *Premature Ventricular Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
96. A 36-year-old white female nurse comes to the ER due to a sensation of fast heart rate, slight
dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained
(Fig. 69), which shows...
A. Atrial fibrillation
B. Atrial flutter
C. *Atrial tachycardia with 2:1 AV block
D. Ventricular tachycardia
E. Accelerated idioventricular rhythm
97. Match the tracing (Fig. 61) with the correct interpretation:
A. Sino-atrial block
B. *High-grade 2:1 AV block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
98. .Match the tracing (Fig. 60) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Complete AV block
99. Match the tracing (Fig. 59) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
100. Match the tracing (Fig. 61) with the correct interpretation:
A. *Advanced AV block
B. AV I° block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
101. Match the tracing (Fig. 61) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. *Advanced 2:1 AV block
D. AV II° block (Mobitz 2)
E. Complete AV block
102. Match the tracing (Fig. 63) with the correct interpretation:
A. Right bundle branch block (RBBB)
B. Rate-dependent LBBB
C. Anterior hemiblock
D. *Bifascicular block
E. Normal ECG
103. Match the tracing (Fig. 63) with the correct interpretation:
A. Right bundle branch block (RBBB)
B. Left bundle branch block (LBBB)
C. Anterior hemiblock (AHB)
D. Posterior hemiblock (PHB)
E. *Bifascicular block (RBBB+AHB)
104. Match the tracing (Fig. 63) with the correct interpretation:
A.
B.
C.
D.
E.
105.
A.
B.
C.
D.
E.
106.
A.
B.
C.
D.
E.
107.
A.
B.
C.
D.
E.
108.
A.
B.
C.
D.
E.
109.
A.
B.
C.
D.
E.
110.
A.
B.
C.
D.
E.
111.
A.
B.
C.
D.
E.
112.
A.
B.
C.
D.
E.
Right bundle branch block (RBBB)
*Bifascicular block
Anterior hemiblock
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 62) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Normal ECG
Match the tracing (Fig. 64) with the correct interpretation:
Right bundle branch block (RBBB)
*Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 62) with the correct interpretation:
*Right bundle branch block (RBBB)
Bifascicular block
Anterior hemiblock
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 62) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock
Bifascicular block (RBBB+AHB)
What type of arrhythmia is shown on ECG (Fig. 65) ?
*AV re-entry tachycardia
.AV nodal re-entry tachycardia
.Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is shown on ECG (Fig. 66)?
AV re-entry tachycardia in WPW
*AV nodal re-entry tachycardia
Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is seen here (Fig. 76)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Premature ventricular contractions
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 60)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Couplet of premature ventricular contractions
Supraventricular premature beats
113.
A.
B.
C.
D.
E.
114.
A.
B.
C.
D.
E.
115.
A.
B.
C.
D.
E.
116.
A.
B.
C.
D.
E.
117.
A.
B.
C.
D.
E.
118.
A.
B.
C.
D.
E.
119.
A.
B.
C.
D.
E.
120.
A.
B.
C.
D.
E.
121.
A.
B.
C.
D.
What type of arrhythmia is seen here (Fig. 74)?
Premature junctional contractions (PJCs)
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Premature ventricular contractions
Supraventricular premature beats
What is seen in this ECG (Fig. 71)?
PJC (Premature junctional complex)
Atrial flutter
*Atrial fibrillation
AV nodal reentrant tachycardia
Accelerated junctional rhythm
What is seen in this ECG (Fig. 70)?
Sinus tachycardia
Paroxysmal supraventricular tachycardia
3rd degree AV block
Atrial fibrillation
*Atrial flutter
Match the tracing (Fig. 67) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
*WPW
Atrial flutter
Accelerated idioventricular rhythm
Match the tracing (Fig. 68) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
Atrial flutter with 4:1 and 2:1 conduction and rate-dependent LBBB
*Atrial premature beats
Match the tracing (Fig. 72) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
*Ventricular fibrillation
Accelerated idioventricular rhythm
Match the tracing (Fig. 73) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
*Torsade de pointes followed by idioventricular rhythm
Atrial flutter with 4:1 and 2:1 conduction and rate-dependent LBBB
Accelerated idioventricular rhythm
Match the tracing (Fig. 69) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
*Atrial tachycardia with 2:1 conduction
Accelerated idioventricular rhythm
What is on this ECG (Fig. 77)?
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
*Run of ventricular tachycardia
E. Accelerated idioventricular rhythm
122. All the following features favor ventricular tachycardia (Fig. 77) as the cause of broad-complex
tachycardia, EXCEPT:
A. QRS duration with right bundle branch block morphology (RBBB) is greater
than 140 ms, and
greater than 160 ms with left LBBB morphology
B. LAD with RBBB morphology, extreme LAD (northwest axis) with LBBB morphology
C. AV dissociation
D. *Response to carotid sinus massage
E. Concordance of the QRS pattern in all precordial leads (i.e., all positive or all negative deflections)
123. The most common type of arrhythmia in WPW syndrome is (Fig. 65)....
A. Ventricular tachycardia
B. Ventricular fibrillation
C. Ventricular premature complexes
D. Atrial ectopics
E. *AV re-entry tachycardia
124. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
sinus bradycardia at a rate of 40 with hypotension (Fig. 79). Choose the best next step in antiarrhythmic
management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
125. A 58-year-old female smoker admitted to the ICU with respiratory distress due to pneumonia. This
was complicated by an anterior MI, with management including cautious use of beta-blockers. She now
develops 10 to 12 PVC’s per hour, occasional couplets, and a few short runs of ventricular tachycardia
(Fig. 77), although BP and oxygen saturation remain stable. Choose the best next step in antiarrhythmic
management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Observation
E. Quinidine
126. A 60-year old male during his first day post-MI in the CCU develops the following rhythm (Fig.
77). Choose the best next step in antiarrhythmic management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Diltiazem
E. Observation
127. A 27-year-old woman is evaluated on follow-up examination. She has a history of syncope and has
been treated with a β-blocker. She had discontinued β-blocker therapy while she was pregnant, but
recently resumed therapy. She has had no recent syncopal episodes, but she has been having palpitations.
Her sister died suddenly at age 32 years. Her physical examination is normal. Her electrocardiogram is
shown (Fig. 73). She is on no other medications.
A. What is the most likely diagnosis in this patient?
B. Wolff-Parkinson-White syndrome
C. Hypertrophic cardiomyopathy
D. *Long QT syndrome
E. Familial dilated cardiomyopathy Arrhythmogenic RV dysplasia
128. Use of echocardiogram in the assessment of AF (Fig. 71):
A. It is not necessary to perform a TTE in patients with AF
B. TEE is always needed to allow better assessment of the MV and LA
C. *TTE should be performed at baseline to diagnose associated structural/functional heart disease
D. TTE is necessary to determine stroke risk stratification for thromboprophylaxis in all patients
E. When TTE is technically difficult, MRI is needed to exclude cardiac abnormalities
129. Which is the preferred initial treatment strategy for rate control in AF patients (Fig. 71)?
A. Digoxin
B. *Beta-blockers or rate limiting CCB
C. Combination therapy of beta-blockers and rate-limiting CCB’s
D. Amiodarone
E. Combination therapy of digoxin and beta-blockers
130. Regarding antithrombotic treatment in AF (Fig.71):
A. Patients with asymptomatic AF have less risk of embolism than symptomatic patients
B. Patients with atrial flutter do not need antithrombotic treatment due to the low risk of embolism of
this arrhythmia
C. *Warfarin is the best option in patients with high risk of thromboembolism
D. Aspirin has a similar effect in stroke reduction to placebo
E. Paroxysmal AF has the lowest risk of embolism
131. Sudden cardiac death in patients <35 years old is most commonly associated with (Fig. 54)
A. *Hypertrophic cardiomyopathy
B. Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
132. Congenital long QT syndrome can lead to (Fig. 73)…
A. Complete heart block
B. *Polymorphic ventricular tachycardia
C. Acute myocardial infarction
D. Recurrent supraventricular tachycardia
E. All of the above
133. All of the following are ECG manifestations of Wolff-Parkinson-White syndrome (Fig. 67)
EXCEPT
A. *Narrow QRS
B. Initial slurred QRS upstroke
C. Short PQ interval
D. Normal QT interval
E. All of the above
134. For a patient with Wolff-Parkinson-White syndrome who presents with a wide QRS tachycardia
(Fig. 65), all of the following are possible treatment choices EXCEPT:
A. Procainamide
B. Cardioversion
C. Amiodarone
D. Propafenone
E. *Adenosine
135. The initial manifestations of WPW (Fig. 67) syndrome may include which of the following?
A. Atrial fibrillation
B. AV re-entry tachycardia
C. Ventricular fibrillation
D. Wide-QRS tachycardia
E. *All of the above
136. Ventricular ectopic beats (VEBs) occurring in apparently normal hearts are (Fig. 276):
A. Associated with a bad prognosis
B. Never frequent or complex
C. Less frequent with increasing age
D. *May be associated with symptoms of “missed beats”
E. Always symptomatic
137. In patients with ventricular ectopic beats (Fig. 74):
A. Caffeine restriction always reduces symptoms
B. *High caffeine intake should always be discouraged in symptomatic patients
C. There is good evidence that reducing caffeine intake reduces ectopics
D. Hypertension has no association with frequency of ectopic beats
E. LVH is not associated with increased frequency of ectopics
138. Regarding ventricular ectopics (Fig. 74) and exercise:
A. *Ectopics are usually benign if they are supressed on exercise
B. Exercise-induced VEBs are not associated with adverse prognosis
C. RVOT ectopics are usually supressed on exercise
D. Ectopics induced on recovery after exercise are benign
E. All of the above
139. A 36-year-old male comes with the sensation of a racing heart. His BP is 110/70 mmHg, respiratory
rate normal, and O2 saturation 98%. His ECG shows a narrow QRS complex tachycardia, which you
correctly diagnose as paroxysmal atrial tachycardia (Fig. 69). Which of the following is the initial
therapy of choice in this hemodynamically stable patient?
A. *Adenosine 6 mg rapid i.v. bolus
B. Verapamil 2.5 to 5 mg i.v. over 1 to 2 min.
C. Digoxin 0.5 mg i.v. slowly
D. Lidocaine 1.5 mg/kg i.v. bolus
E. Electrical cardioversion at 50 joules
140. This ECG of a 45-year-old man (Fig. 25) is consistent with:
A. Acute anterolateral myocardial infarction
B. Abnormal SCN5A channel (Brugada syndrome)
C. Abnormal KCQN1 channel (short QT syndrome)
D. Old anteroseptal myocardial infarction with an aneurysm
E. Congenital long QT syndrome
141. Match the tracing (Fig. 78) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. *Atrial premature beats
E. AV second-degree block
142. Match the tracing (Fig. 61) with the correct interpretation:
A. Complete AV block
B. *High-grade AV block
C. Nonconducted premature atrial complex
D. AV first-degree block
E. AV second-degree block
143. Match the tracing (Fig. 60) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. AV first-degree block
E. *AV second-degree block
144. Match the tracing (Fig. 58) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. *Sick sinus syndrome
D. AV first-degree block
E. AV second-degree block
145. Match the tracing (Fig. 59) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. AV first-degree block
E. *AV second-degree block
146. Wenckebach phenomenon (Fig. 59) is defined as...
A. Progressive shortening of PR interval till a beat is dropped
B. *Progressive lengthening of PR interval till a beat is dropped
C. Irregular heart rate and PVC’s
D. Shortened QT intervals
E. Slurred QRS complex
147. A 63-year old man presents with severe chest pain, nausea, and near syncope. His BP is 80/55 mm
Hg, pulse 40 bpm, respiration 22 breaths/minute. The ECG (Fig. 79) recorded in the ER shows which of
the following?
A. Inferior MI
B. Atrial fibrillation
C. Complete AV block
D. Anterolateral MI
E. Brugada syndrome
148. An 80-year-old with a past history of MI is found to have left bundle branch block on ECG (Fig.
64). She is asymptomatic, with BP 130/80 mmHg, lungs clear to auscultation, and no leg edema. On
cardiac auscultation, which of the following is the most likely finding?
A. Fixed (wide) split S2
B. *Paradoxical (reversed) split S2
C. S3
D. Opening snap
E. Midsystolic click
149. A 65-year-old man with diabetes, on an oral hypoglycemic, presents to the ER with a sports-related
shoulder injury. His heart rate was noted to be irregular, and the following ECG was obtained (Fig. 59).
Which of the following is the best immediate therapy?
A. Atropine
B. Isoproterenol
C. Pacemaker placement
D. *Observation
E. Electrical cardioversion
150. Choose the correct interpretation of the tracing (Fig. 77)
A. Normal Sinus Rhythm
B. Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. *Run of ventricular Tachycardia
151. Choose the correct interpretation of the tracing (Fig. 18)
A. Normal Sinus Rhythm
B. Ventricular Fibrillation
C. *Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
152. Choose the correct interpretation of the tracing (Fig. 58):
A. *Sick sinus syndrome
B. Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
153. Choose the correct interpretation of the tracing (Fig. 72):
A. Normal Sinus Rhythm
B. *Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
154. Choose the correct interpretation of the tracing (Fig. 67):
A. Idioventricular Rhythm
B. Junctional Rhythm
C. Premature Atrial Contraction
D. Ventricular Fibrillatio
E. *WPW
155. Choose the correct interpretation of the tracing (Fig. 72):
A. Idioventricular Rhythm
B. Junctional Rhythm
C. Premature Atrial Contraction
D. *Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
156. Choose the correct interpretation of the tracing (Fig. 86):
A. Idioventricular Rhythm
B. Junctional Rhythm
C. *Premature Atrial Contractions
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
157. Choose the correct interpretation of the tracing (Fig. 58):
A. Idioventricular Rhythm
B. *Sick sinus syndrome
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
158. Choose the correct interpretation of the tracing (Fig. 70) with the correct interpretation:
A. *Atrial flutter
B. Junctional Rhythm
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
159. A 42-year-old female comes to the ER due to a sensation of fast heart rate, slight dizziness, and
vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained (Fig. 69), which
shows...
A. Atrial fibrillation
B. Atrial flutter
C. *Supraventricular tachycardia
D. Ventricular tachycardia
E. Idioventricular rhythm
160. Choose the correct interpretation of the tracing (Fig. 59) :
A. Sino-atrial block
B. AV I° block
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
161. Choose the correct interpretation of the tracing (Fig. 60):
A. Sino-atrial block
B. AV I° block
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Complete AV block
162. A 48-year-old patient presents to the hospital with syncope, dyspnea of sudden onset and
hypotension. His ECG is shown on (Fig. 83). What is the most likely diagnosis?
A. Acute anterior MI
B. Acute inferior MI
C. Acute pericarditis
D. *Acute pulmonary embolism
E. Non-cardiogenic syncope
163. A 28-year-old man presents to the hospital with chest pain that began at a party. On further
questioning, he was using cocaine at a party. His ECG is shown on Fig. 78. The most likely cause of his
chest pain is
A. Acute inferior MI
B. *Acute anterior MI
C. Acute pericarditis
D. Acute pulmonary embolism
E. Right ventricular MI
164. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block (Fig. 60). Chest plain film is normal. Which of the following is likely to be found in
addition on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
165. This echocardiographic image (Fig. 80) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click and murmur on
auscultation
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, elevated jugular venous pressure,
and diffuse lung crackles on auscultation
D. A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. *A 77-year-old male with a history of MI who presents with syncope
166. This ECG (Fig. 81) was most likely obtained from which of the following patients?
A. *A patient with mitral stenosis
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, and diffuse lung crackles on
auscultation
D. A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of systolic murmur who presents with syncope
167. This ECG (Fig. 71) was most likely obtained from which of the following patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click and murmur on
auscultation
B. *A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, and diffuse lung crackles on
auscultation
D. A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of systolic murmur who presents with syncope
168. This ECG (Fig. 81) was most likely obtained from which of the following patients?
A. *A patient with mitral stenosis
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, and diffuse lung crackles on
auscultation
D. A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of MI who presents with syncope
F. *Mobitz type I AV block
169. A patient in whom this echo image was obtained (Fig. 158) is most likely to have which of the
following cardiac abnormalities?
A. *Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Preexitation syndrome
D. Right bundle branch block
E. Tricuspid atresia
170. Match the ECG finding that is most closely associated with condition shown on Fig. 158
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment depression
E. *Deeply inverted precordial T waves
171. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. An echo image is
obtained (Fig. 158). The murmur is probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
172. A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Pericardial effusion
B. *Mitral valve disease
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic valve disease
173. On echo image (Fig. 159) arrows point:
A. A bulging aortic arch
B. *Anterior mitral leaflet
C. Enlarged left ventricle
D. Pulmonary artery
E. Double shadow (border of the right and left atria)
174. On echo image (Fig. 159) arrows shows:
A. A bulging aortic arch
B. A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. *Mitral valve
175. A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. *Mitral stenosis
E. Tricuspid regurgitation
176. A patient in whom this echo image was obtained (Fig. 160) is most likely to have which of the
following cardiac abnormalities?
A. *Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
177. This echocardiographic image (Fig. 161) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click and murmur on
auscultation
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, elevated jugular venous pressure,
and diffuse lung crackles on auscultation
D. *A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of systolic murmur who presents with syncope
178. Match the tracing (Fig. 162) with the correct interpretation:
A. *Sick sinus syndrome
B.
Junctional Rhythm
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
179. Match the tracing (Fig. 162) with the correct interpretation:
A. Idioventricular Rhythm
B. Junctional Rhythm
C. *Sick sinus syndrome
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
180. A 36-year-old white female nurse comes to the ER due to a sensation of irregular heart rate, slight
dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained
(Fig. 162), which shows...
A. Atrial fibrillation
B. Atrial flutter
C. *Sick sinus syndrome
D. Ventricular tachycardia
E. Accelerated idioventricular rhythm
181. Match the tracing (Fig. 165) with the correct interpretation:
A. Sino-atrial block
B.
C.
D.
E.
182.
A.
B.
C.
D.
E.
183.
A.
B.
C.
D.
E.
184.
A.
B.
C.
D.
E.
185.
A.
B.
C.
D.
E.
186.
A.
B.
C.
D.
E.
187.
A.
B.
C.
D.
E.
188.
A.
B.
C.
D.
E.
189.
A.
B.
C.
D.
E.
190.
*High-grade 2:1 AV block
AV II° block (Mobitz 1)
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 164) with the correct interpretation:
Sino-atrial block
AV I° block
AV II° block (Mobitz 1)
*AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 163) with the correct interpretation:
Sino-atrial block
AV I° block
*AV II° block (Mobitz 1)
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 165) with the correct interpretation:
*Advanced AV block
AV I° block
AV II° block (Mobitz 1)
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 165) with the correct interpretation:
Sino-atrial block
AV I° block
*Advanced 2:1 AV block
AV II° block (Mobitz 2)
Complete AV block
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Rate-dependent LBBB
Anterior hemiblock
*Bifascicular block
Normal ECG
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
*Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
*Bifascicular block
Anterior hemiblock
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
A.
B.
C.
D.
E.
191.
A.
B.
C.
D.
E.
192.
A.
B.
C.
D.
E.
193.
A.
B.
C.
D.
E.
194.
A.
B.
C.
D.
E.
195.
A.
B.
C.
D.
E.
196.
A.
B.
C.
D.
E.
197.
A.
B.
C.
D.
E.
198.
A.
B.
C.
D.
E.
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 9) with the correct interpretation:
*Right bundle branch block (RBBB)
Bifascicular block
Anterior fascicular block
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior fascicular block
Bifascicular block (RBBB+AHB)
What type of arrhythmia is shown on ECG (Fig. 162) ?
*Sick sinus syndrome
AV nodal re-entry tachycardia
Sick sinus syndrome
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is shown on ECG (Fig. 165)?
V re-entry tachycardia in WPW
* Advanced AV block
Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is seen here (Fig. 165)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Advanced AV block
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 164)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Mobitz type 2 AV block
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 162)?
Premature junctional contractions (PJCs)
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Sick sinus syndrome
Supraventricular premature beats
What is seen in this ECG (Fig. 163)?
PJC (Premature junctional complex)
Atrial flutter
*Wenckebach type AV block
AV nodal reentrant tachycardia
Accelerated junctional rhythm
199. What is seen in this ECG (Fig. 163)?
A. Sinus tachycardia
B. Paroxysmal supraventricular tachycardia
C. 3rd degree AV block
D. Atrial fibrillation
E. *Mobitz type I AV block
200. Match the tracing (Fig. 162) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. *Sick sinus syndrome
D. Atrial flutter
E. Accelerated idioventricular rhythm
201. Match the tracing (Fig. 162) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. WPW
D. Atrial flutter with rate-dependent LBBB
E. *SSS
202. Match the tracing (Fig. 163) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. Intermittent WPW
D. *Wenckebach type AV block
E. Accelerated idioventricular rhythm
203. Match the tracing (Fig. 163) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. *Wenckebach type AV block
D. Atrial flutter with 4:1 and 2:1 conduction and rate-dependent LBBB
E. Accelerated idioventricular rhythm
204. Match the tracing (Fig. 163) with the correct interpretation:
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. Intermittent WPW
D. *Mobitz type I AV block
E. Accelerated idioventricular rhythm
205. What is on this ECG (Fig. 163)?
A. Ventricular trigeminy
B. Wandering atrial pacemeker
C. Intermittent WPW
D. *Second degree AV block
E. Accelerated idioventricular rhythm
206. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
following rhythm (Fig. 164). Choose the best next step in antiarrhythmic management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
207. A 60-year old male during his first day post-MI in the CCU develops the following rhythm (Fig.
164). Choose the best next step in antiarrhythmic management.
A. Amiodarone
B. *Atropine
C.
D.
E.
208.
A.
B.
C.
D.
E.
209.
A.
B.
C.
D.
E.
210.
A.
B.
C.
D.
E.
211.
A.
B.
C.
D.
E.
212.
A.
B.
C.
D.
E.
213.
A.
B.
C.
D.
E.
214.
A.
B.
C.
D.
E.
215.
A.
B.
C.
D.
E.
Digoxin
Diltiazem
Observation
Sudden cardiac death in patients <35 years old is most commonly associated with (Fig. 158)
*Hypertrophic cardiomyopathy
Coronary artery disease
Congenital long QT syndrome
Long QT syndrome secondary to various medications
arrhythymogenic RV cardiomyopathy
This ECG of a 45-year-old man (Fig. 9) is consistent with:
*Right bundle branch block
Abnormal SCN5A channel (Brugada syndrome)
Abnormal KCQN1 channel (short QT syndrome)
Old anteroseptal myocardial infarction with an aneurysm
Congenital long QT syndrome
Match the tracing (Fig. 10) with the correct interpretation:
Complete AV block
Nonconducted premature atrial complex
Nonconducted premature atrial complex, followed by a junctional beat
*Bifascicular block
AV second-degree block
Match the tracing (Fig. 165) with the correct interpretation:
Complete AV block
*High-grade AV block
Nonconducted premature atrial complex
AV first-degree block
AV second-degree block
Match the tracing (Fig. 164) with the correct interpretation:
Complete AV block
Nonconducted premature atrial complex
Nonconducted premature atrial complex, followed by a junctional beat
AV first-degree block
*AV second-degree block
Match the tracing (Fig. 162) with the correct interpretation:
Complete AV block
Nonconducted premature atrial complex
*Sick sinus syndrome
AV first-degree block
AV second-degree block
Match the tracing (Fig. 163) with the correct interpretation:
Complete AV block
Nonconducted premature atrial complex
Nonconducted premature atrial complex, followed by a junctional beat
AV first-degree block
*AV second-degree block
Wenckebach phenomenon (Fig. 6) is defined as...
Progressive shortening of PR interval till a beat is dropped
*Progressive lengthening of PR interval till a beat is dropped
Irregular heart rate and PVC’s
Shortened QT intervals
Slurred QRS complex
216. A 65-year-old man with diabetes, on an oral hypoglycemic, presents to the ER with a sports-related
shoulder injury. His heart rate was noted to be irregular, and the following ECG was obtained (Fig. 163).
Which of the following is the best immediate therapy?
A. Atropine
B. Isoproterenol
C. Pacemaker placement
D. *Observation
E. Electrical cardioversion
217. Choose the correct interpretation of the tracing (Fig. 162):
A. *Sick sinus syndrome
B. Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
218. Choose the correct interpretation of the tracing (Fig. 162):
A. Idioventricular Rhythm
B. *Sick sinus syndrome
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
219. Choose the correct interpretation of the tracing (Fig. 163) :
A. Sino-atrial block
B. AV I° block
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
220. Choose the correct interpretation of the tracing (Fig. 164):
A. Sino-atrial block
B. AV I° block
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Complete AV block
221. A 55-year-old male presents with severe substernal chest pain for the last hour. It began at rest and
is associated with dyspnea and nausea. The electrocardiogram shows bradycardia with a Mobitz type II
second-degree block (Fig. 164). Chest plain film is normal. Which of the following is likely to be found
in addition on the electrocardiogram?
A. ST elevation in V1-V3
B. Wellen’s T waves
C. *ST elevation in II, III, aVF
D. ST depression in I and aVL
E. No other abnormality
222. A patient in whom this echo image was obtained (Fig. 158) is most likely to have which of the
following cardiac abnormalities?
A. *Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Restrictive cardiomyopathy
D. Aortic stenosis
E. Mitral stenosis
223. Match the ECG finding that is most closely associated with condition shown on Fig. 158
A. Low QRS voltage
B. Left bundle branch block
C. Right bundle branch block
D. Diffuse ST segment depression
E. *Deeply inverted precordial T waves
224. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. An echo image is
obtained (Fig. 185). The murmur is probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic stenosis
225. A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Pericardial effusion
B. *Mitral stenosis
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic stenosis
226. On echo image (Fig. 159) arrows point:
A. A bulging aortic arch
B. *Anterior mitral leaflet
C. Posterior mitral leaflet
D. Pulmonary artery
E. Double shadow (border of the right and left atria)
227. On echo image (Fig. 159) arrows shows:
A. A bulging aortic arch
B. A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. *Mitral anterior leaflet
228. A patient in whom this echo image was obtained (Fig. 159) is most likely to have which of the
following cardiac abnormalities?
A. Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. *Mitral stenosis
E. Pulmonary stenosis
229. A patient in whom this echo image was obtained (Fig. 160) is most likely to have which of the
following cardiac abnormalities?
A. *Aortic stenosis
B. Pulmonary regurgitation
C. Pulmonary regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
230. This echocardiographic image (Fig. 161) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click
B. A 22-year-old female who grew up in Central America who presents with dyspnea and atrial
fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, and diffuse lung crackles
D. *A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history MI who presents with syncope
231. Match the tracing (Fig. 162) with the correct interpretation:
A. *Sick sinus syndrome
B. AV I degree block
C. Complete AV block
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
232. Match the tracing (Fig. 162) with the correct interpretation:
A. Second degree AV block
B. Junctional Rhythm
C. *Sick sinus syndrome
D. Sino-atrial block
E. Complete AV block
233. A 36-year-old white female nurse comes to the ER due to a sensation of irregular heart rate, slight
dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained
(Fig. 162), which shows...
A. Atrial fibrillation
B. Sino-atrial block
C. *Sick sinus syndrome
D. Second degree AV block
E. Accelerated idioventricular rhythm
234. Match the tracing (Fig. 165) with the correct interpretation:
A. Sick sinus syndrome
B. *High-grade 2:1 AV block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. AV III° block
235. Match the tracing (Fig. 164) with the correct interpretation:
A. Sino-atrial block
B. Junctional rhythm
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Sick sinus syndrome
236. Match the tracing (Fig. 163) with the correct interpretation:
A. Sino-atrial block
B. Sick sinus syndromeS
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. High-grade AV block
237. Match the tracing (Fig. 165) with the correct interpretation:
A. *High-grade AV block
B. AV I° block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
238. Match the tracing (Fig. 165) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. *Advanced 2:1 AV block
D. AV II° block (Mobitz 2)
E. Complete AV block
239. Match the tracing (Fig. 167) with the correct interpretation:
A. Right bundle branch block (RBBB)
B. Rate-dependent LBBB
C.
D.
E.
240.
A.
B.
C.
D.
E.
241.
A.
B.
C.
D.
E.
242.
A.
B.
C.
D.
E.
243.
A.
B.
C.
D.
E.
244.
A.
B.
C.
D.
E.
245.
A.
B.
C.
D.
E.
246.
A.
B.
C.
D.
E.
247.
A.
B.
C.
D.
E.
248.
A.
Anterior fascicular block
*Bifascicular block
Left posterior fascicular block
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior fascicular block (AHB)
Posterior fascicular block (PHB)
*RBBB+AHB
Match the tracing (Fig. 167) with the correct interpretation:
Right bundle branch block
*Bifascicular block
Anterior hemiblock
Posterior hemiblock
Left bundle branch block
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Complete heart block
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block
Bifascicular block
Anterior fascicular block
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 166) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior fascicular block
Bifascicular block (RBBB+AHB)
What type of arrhythmia is shown on ECG (Fig. 162) ?
*Sick sinus syndrome
AV second-degree block
Sick sinus syndrome
PSVT (Paroxysmal Supraventricular Tachycardia)
Complete heart block
What type of arrhythmia is shown on ECG (Fig. 165)?
V re-entry tachycardia in WPW
*Advanced AV block
Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
AV second-degree block
What type of arrhythmia is seen here (Fig. 165)?
Right bundle branch block
B. Rate related bundle branch block
C. Premature atrial contractions conducted with aberrancy
D. *Advanced AV block
E. Supraventricular premature beats
249. What type of arrhythmia is seen here (Fig. 164)?
A. Premature junctional contractions
B. Wenckebach type AV block
C. Premature atrial contractions conducted with aberrancy
D. *Mobitz type 2 AV block
E. Supraventricular premature beats
250. What type of arrhythmia is seen here (Fig. 162)?
A. Complete heart block
B. Wenckebach type AV block
C. Premature atrial contractions conducted with aberrancy
D. *Sick sinus syndrome
E. Supraventricular premature beats
251. What is seen in this ECG (Fig. 163)?
A. Mobitz type 2 AV block
B. Sick sinus syndrome
C. *Wenckebach type AV block
D. AV nodal reentrant tachycardia
E.
Accelerated junctional rhythm
252. What is seen in this ECG (Fig. 163)?
A. Sinus tachycardia
B. Mobitz type II AV block
C. 3rd degree AV block
D. Atrial fibrillation
253. A patient in whom this echo image was obtained (Fig. 54) is most likely to have which of the
following cardiac abnormalities?
A. *Hypertrophic cardiomyopathy
B. Dilated cardiomyopathy
C. Preexitation syndrome
D. Right bundle branch block
E. Tricuspid atresia
254. Match the ECG finding that is most closely associated with condition shown on Fig. 54
A. Low QRS voltage
B. AV nodal block
C. Right bundle branch block
D. Diffuse ST segment depression
E. *Deeply inverted precordial T waves
255. A 19-year-old male is referred for evaluation of a cardiac murmur before clearance to play
collegiate sports. He has no symptoms, has never had syncope, and has no known family history of
cardiac disease. A 3/6 stystolic murmur is heard at the apex with no radiation. On squatting, the murmur
decreases in intensity, and on sustained handgrip, the murmur alsop is decreased. An echo image is
obtained (Fig. 54). The murmur is probably to which of the following?
A. *Hypertrophic cardiomyopathy
B. Mitral valve prolapse
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic regurgitation
256. A patient in whom this chest X-ray image was obtained (Fig. 55) is most likely to have which of the
following cardiac abnormalities?
A. Pericardial effusion
B. *Mitral valve disease
C. Dilated cardiomyopathy
D. Pulmonary stenosis
E. Aortic valve disease
257. On plain chest X-ray image (Fig. 55) arrow “a” shows:
A. A bulging aortic arch
B. *A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. Double shadow (border of the right and left atria)
258. On plain chest X-ray image (Fig. 55) arrow “b” shows:
A. A bulging aortic arch
B. A markedly enlarged left atrium
C. Enlarged left ventricle
D. Pulmonary artery
E. *Double shadow (border of the right and left atria)
259. The left ventricular enlargement seen on plain chest X-ray image (Fig. 55) is most likely due to:
A. Aortic stenosis
B. *Mitral regurgitation
C. Aortic regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
260. A patient in whom this echo image was obtained (Fig. 56) is most likely to have which of the
following cardiac abnormalities?
A. *Aortic stenosis
B. Mitral regurgitation
C. Aortic regurgitation
D. Mitral stenosis
E. Tricuspid regurgitation
261. This echocardiographic image (Fig. 57) was most likely obtained from which of the following
patients?
A. A 17-year-old athlete with atypical chest pain who has a midsystolic click and murmur on
auscultation
B. A 22-year-old female who grew up in Central America who presents with 2 years of dyspnea and
newly diagnosed atrial fibrillation
C. A 33-year-old postpartum female with hypotension, tachycardia, elevated jugular venous pressure,
and diffuse lung crackles on auscultation
D. *A 63-year-old male with a history of lung cancer who presents with hypotension, tachycardia,
jugular venous distension, clear lungs, and enlarged heart on CXR
E. A 77-year-old male with a history of systolic murmur who presents with syncope
262. Match the tracing (Fig. 58) with the correct interpretation:
A. *Sick sinus syndrome
B. Junctional Rhythm
C. Premature Atrial Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
263. Match the tracing (Fig. 74) with the correct interpretation:
A. Idioventricular Rhythm
B. Junctional Rhythm
C. *Premature Ventricular Contraction
D. Ventricular Fibrillation
E. Paroxysmal Supraventricular Tachycardia
264. A 36-year-old white female nurse comes to the ER due to a sensation of fast heart rate, slight
dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained
(Fig. 69), which shows...
A. Atrial fibrillation
B. Atrial flutter
C. *Atrial tachycardia with 2:1 AV block
D. Ventricular tachycardia
E. Accelerated idioventricular rhythm
265. Match the tracing (Fig. 61) with the correct interpretation:
A. Sino-atrial block
B. *High-grade 2:1 AV block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
266. .Match the tracing (Fig. 60) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. AV II° block (Mobitz 1)
D. *AV II° block (Mobitz 2)
E. Complete AV block
267. Match the tracing (Fig. 59) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. *AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
268. Match the tracing (Fig. 61) with the correct interpretation:
A. *Advanced AV block
B. AV I° block
C. AV II° block (Mobitz 1)
D. AV II° block (Mobitz 2)
E. Complete AV block
269. Match the tracing (Fig. 61) with the correct interpretation:
A. Sino-atrial block
B. AV I° block
C. *Advanced 2:1 AV block
D. AV II° block (Mobitz 2)
E. Complete AV block
270. Match the tracing (Fig. 63) with the correct interpretation:
A. Right bundle branch block (RBBB)
B. Rate-dependent LBBB
C. Anterior hemiblock
D. *Bifascicular block
E. Normal ECG
271. Match the tracing (Fig. 63) with the correct interpretation:
A. Right bundle branch block (RBBB)
B. Left bundle branch block (LBBB)
C. Anterior hemiblock (AHB)
D. Posterior hemiblock (PHB)
E. *Bifascicular block (RBBB+AHB)
272. Match the tracing (Fig. 63) with the correct interpretation:
A. Right bundle branch block (RBBB)
B. *Bifascicular block
C.
D.
E.
273.
A.
B.
C.
D.
E.
274.
A.
B.
C.
D.
E.
275.
A.
B.
C.
D.
E.
276.
A.
B.
C.
D.
E.
277.
A.
B.
C.
D.
E.
278.
A.
B.
C.
D.
E.
279.
A.
B.
C.
D.
E.
280.
A.
B.
C.
D.
E.
281.
A.
Anterior hemiblock
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 62) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Normal ECG
Match the tracing (Fig. 64) with the correct interpretation:
Right bundle branch block (RBBB)
*Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock (PHB)
Bifascicular block (RBBB+AHB)
Match the tracing (Fig. 62) with the correct interpretation:
*Right bundle branch block (RBBB)
Bifascicular block
Anterior hemiblock
Posterior hemiblock
Normal ECG
Match the tracing (Fig. 62) with the correct interpretation:
*Right bundle branch block (RBBB)
Left bundle branch block (LBBB)
Anterior hemiblock (AHB)
Posterior hemiblock
Bifascicular block (RBBB+AHB)
What type of arrhythmia is shown on ECG (Fig. 65) ?
*AV re-entry tachycardia
.AV nodal re-entry tachycardia
.Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is shown on ECG (Fig. 66)?
AV re-entry tachycardia in WPW
*AV nodal re-entry tachycardia
Atrial premature beats
PSVT (Paroxysmal Supraventricular Tachycardia)
Torsade de pointes
What type of arrhythmia is seen here (Fig. 76)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Premature ventricular contractions
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 60)?
Premature junctional contractions
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Couplet of premature ventricular contractions
Supraventricular premature beats
What type of arrhythmia is seen here (Fig. 74)?
Premature junctional contractions (PJCs)
B.
C.
D.
E.
282.
A.
B.
C.
D.
E.
283.
A.
B.
C.
D.
E.
284.
A.
B.
C.
D.
E.
285.
A.
B.
C.
D.
E.
286.
A.
B.
C.
D.
E.
287.
A.
B.
C.
D.
E.
288.
A.
B.
C.
D.
E.
289.
A.
B.
C.
D.
E.
Rate related bundle branch block
Premature atrial contractions conducted with aberrancy
*Premature ventricular contractions
Supraventricular premature beats
What is seen in this ECG (Fig. 71)?
PJC (Premature junctional complex)
Atrial flutter
*Atrial fibrillation
AV nodal reentrant tachycardia
Accelerated junctional rhythm
What is seen in this ECG (Fig. 70)?
Sinus tachycardia
Paroxysmal supraventricular tachycardia
3rd degree AV block
Atrial fibrillation
*Atrial flutter
Match the tracing (Fig. 67) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
*WPW
Atrial flutter
Accelerated idioventricular rhythm
Match the tracing (Fig. 68) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
Atrial flutter with 4:1 and 2:1 conduction and rate-dependent LBBB
*Atrial premature beats
Match the tracing (Fig. 72) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
*Ventricular fibrillation
Accelerated idioventricular rhythm
Match the tracing (Fig. 73) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
*Torsade de pointes followed by idioventricular rhythm
Atrial flutter with 4:1 and 2:1 conduction and rate-dependent LBBB
Accelerated idioventricular rhythm
Match the tracing (Fig. 69) with the correct interpretation:
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
*Atrial tachycardia with 2:1 conduction
Accelerated idioventricular rhythm
What is on this ECG (Fig. 77)?
Ventricular trigeminy
Wandering atrial pacemeker
Intermittent WPW
*Run of ventricular tachycardia
Accelerated idioventricular rhythm
290. All the following features favor ventricular tachycardia (Fig. 77) as the cause of broad-complex
tachycardia, EXCEPT:
A. QRS duration with right bundle branch block morphology (RBBB) is greater
than 140 ms, and
greater than 160 ms with left LBBB morphology
B. LAD with RBBB morphology, extreme LAD (northwest axis) with LBBB morphology
C. AV dissociation
D. *Response to carotid sinus massage
E. Concordance of the QRS pattern in all precordial leads (i.e., all positive or all negative deflections)
291. The most common type of arrhythmia in WPW syndrome is (Fig. 65)....
A. Ventricular tachycardia
B. Ventricular fibrillation
C. Ventricular premature complexes
D. Atrial ectopics
E. *AV re-entry tachycardia
292. A 72-year-old male with a 2-h history of chest pain, ST segment elevation in leads II, III, aVF, and
sinus bradycardia at a rate of 40 with hypotension (Fig. 79). Choose the best next step in antiarrhythmic
management.
A. Amiodarone
B. *Atropine
C. Diltiazem
D. Metoprolol
E. Observation
293. A 58-year-old female smoker admitted to the ICU with respiratory distress due to pneumonia. This
was complicated by an anterior MI, with management including cautious use of beta-blockers. She now
develops 10 to 12 PVC’s per hour, occasional couplets, and a few short runs of ventricular tachycardia
(Fig. 77), although BP and oxygen saturation remain stable. Choose the best next step in antiarrhythmic
management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Observation
E. Quinidine
294. A 60-year old male during his first day post-MI in the CCU develops the following rhythm (Fig.
77). Choose the best next step in antiarrhythmic management.
A. *Amiodarone
B. Atropine
C. Digoxin
D. Diltiazem
E. Observation
295. A 27-year-old woman is evaluated on follow-up examination. She has a history of syncope and has
been treated with a β-blocker. She had discontinued β-blocker therapy while she was pregnant, but
recently resumed therapy. She has had no recent syncopal episodes, but she has been having palpitations.
Her sister died suddenly at age 32 years. Her physical examination is normal. Her electrocardiogram is
shown (Fig. 73). She is on no other medications.
A. What is the most likely diagnosis in this patient?
B. Wolff-Parkinson-White syndrome
C. Hypertrophic cardiomyopathy
D. *Long QT syndrome
E. Familial dilated cardiomyopathy Arrhythmogenic RV dysplasia
296. Use of echocardiogram in the assessment of AF (Fig. 71):
A. It is not necessary to perform a TTE in patients with AF
B. TEE is always needed to allow better assessment of the MV and LA
C. *TTE should be performed at baseline to diagnose associated structural/functional heart disease
D. TTE is necessary to determine stroke risk stratification for thromboprophylaxis in all patients
E. When TTE is technically difficult, MRI is needed to exclude cardiac abnormalities
297. Which is the preferred initial treatment strategy for rate control in AF patients (Fig. 71)?
A. Digoxin
B. *Beta-blockers or rate limiting CCB
C. Combination therapy of beta-blockers and rate-limiting CCB’s
D. Amiodarone
E. Combination therapy of digoxin and beta-blockers
298. Regarding antithrombotic treatment in AF (Fig.71):
A. Patients with asymptomatic AF have less risk of embolism than symptomatic patients
B. Patients with atrial flutter do not need antithrombotic treatment due to the low risk of embolism of
this arrhythmia
C. *Warfarin is the best option in patients with high risk of thromboembolism
D. Aspirin has a similar effect in stroke reduction to placebo
E. Paroxysmal AF has the lowest risk of embolism
299. Sudden cardiac death in patients <35 years old is most commonly associated with (Fig. 54)
A. *Hypertrophic cardiomyopathy
B. Coronary artery disease
C. Congenital long QT syndrome
D. Long QT syndrome secondary to various medications
E. arrhythymogenic RV cardiomyopathy
300. Congenital long QT syndrome can lead to (Fig. 73)…
A. Complete heart block
B. *Polymorphic ventricular tachycardia
C. Acute myocardial infarction
D. Recurrent supraventricular tachycardia
E. All of the above
301. All of the following are ECG manifestations of Wolff-Parkinson-White syndrome (Fig. 67)
EXCEPT
A. *Narrow QRS
B. Initial slurred QRS upstroke
C. Short PQ interval
D. Normal QT interval
E. All of the above
302. For a patient with Wolff-Parkinson-White syndrome who presents with a wide QRS tachycardia
(Fig. 65), all of the following are possible treatment choices EXCEPT:
A. Procainamide
B. Cardioversion
C. Amiodarone
D. Propafenone
E. *Adenosine
303. The initial manifestations of WPW (Fig. 67) syndrome may include which of the following?
A. Atrial fibrillation
B. AV re-entry tachycardia
C. Ventricular fibrillation
D. Wide-QRS tachycardia
E. *All of the above
304. Ventricular ectopic beats (VEBs) occurring in apparently normal hearts are (Fig. 276):
A. Associated with a bad prognosis
B. Never frequent or complex
C. Less frequent with increasing age
D. *May be associated with symptoms of “missed beats”
E. Always symptomatic
305. In patients with ventricular ectopic beats (Fig. 74):
A. Caffeine restriction always reduces symptoms
B. *High caffeine intake should always be discouraged in symptomatic patients
C. There is good evidence that reducing caffeine intake reduces ectopics
D. Hypertension has no association with frequency of ectopic beats
E. LVH is not associated with increased frequency of ectopics
306. Regarding ventricular ectopics (Fig. 74) and exercise:
A. *Ectopics are usually benign if they are supressed on exercise
B. Exercise-induced VEBs are not associated with adverse prognosis
C. RVOT ectopics are usually supressed on exercise
D. Ectopics induced on recovery after exercise are benign
E. All of the above
307. A 36-year-old male comes with the sensation of a racing heart. His BP is 110/70 mmHg, respiratory
rate normal, and O2 saturation 98%. His ECG shows a narrow QRS complex tachycardia, which you
correctly diagnose as paroxysmal atrial tachycardia (Fig. 69). Which of the following is the initial
therapy of choice in this hemodynamically stable patient?
A. *Adenosine 6 mg rapid i.v. bolus
B. Verapamil 2.5 to 5 mg i.v. over 1 to 2 min.
C. Digoxin 0.5 mg i.v. slowly
D. Lidocaine 1.5 mg/kg i.v. bolus
E. Electrical cardioversion at 50 joules
308. This ECG of a 45-year-old man (Fig. 25) is consistent with:
A. Acute anterolateral myocardial infarction
B. Abnormal SCN5A channel (Brugada syndrome)
C. Abnormal KCQN1 channel (short QT syndrome)
D. Old anteroseptal myocardial infarction with an aneurysm
E. Congenital long QT syndrome
309. Match the tracing (Fig. 78) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. *Atrial premature beats
E. AV second-degree block
310. Match the tracing (Fig. 61) with the correct interpretation:
A. Complete AV block
B. *High-grade AV block
C. Nonconducted premature atrial complex
D. AV first-degree block
E. AV second-degree block
311. Match the tracing (Fig. 60) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. AV first-degree block
E. *AV second-degree block
312. Match the tracing (Fig. 58) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. *Sick sinus syndrome
D. AV first-degree block
E. AV second-degree block
313. Match the tracing (Fig. 59) with the correct interpretation:
A. Complete AV block
B. Nonconducted premature atrial complex
C. Nonconducted premature atrial complex, followed by a junctional beat
D. AV first-degree block
E. *AV second-degree block
314. Wenckebach phenomenon (Fig. 59) is defined as...
A. Progressive shortening of PR interval till a beat is dropped
B. *Progressive lengthening of PR interval till a beat is dropped
C. Irregular heart rate and PVC’s
D. Shortened QT intervals
E. Slurred QRS complex
315. A 63-year old man presents with severe chest pain, nausea, and near syncope. His BP is 80/55 mm
Hg, pulse 40 bpm, respiration 22 breaths/minute. The ECG (Fig. 79) recorded in the ER shows which of
the following?
A. Inferior MI
B. Atrial fibrillation
C. Complete AV block
D. Anterolateral MI
E. Brugada syndrome
316. An 80-year-old with a past history of MI is found to have left bundle branch block on ECG (Fig.
64). She is asymptomatic, with BP 130/80 mmHg, lungs clear to auscultation, and no leg edema. On
cardiac auscultation, which of the following is the most likely finding?
A. Fixed (wide) split S2
B. *Paradoxical (reversed) split S2
C. S3
D. Opening snap
E. Midsystolic click
317. A 65-year-old man with diabetes, on an oral hypoglycemic, presents to the ER with a sports-related
shoulder injury. His heart rate was noted to be irregular, and the following ECG was obtained (Fig. 59).
Which of the following is the best immediate therapy?
A. Atropine
B. Isoproterenol
C. Pacemaker placement
D. *Observation
E. Electrical cardioversion
318. Choose the correct interpretation of the tracing (Fig. 77)
A. Normal Sinus Rhythm
B. Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. *Run of ventricular Tachycardia
319. Choose the correct interpretation of the tracing (Fig. 18)
A. Normal Sinus Rhythm
B. Ventricular Fibrillation
C. *Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
320. Choose the correct interpretation of the tracing (Fig. 58):
A. *Sick sinus syndrome
B. Ventricular Fibrillation
C. Atrial Fibrillation
D. Wandering Atrial Pacemaker
E. Ventricular Tachycardia
321. Disease shown at Figure 53.is characterized by:
A. chiefly involvement of the lumbosacral portion of spine;
B. gradual onset;
C. frequently associated with renal disease;
D. absence of renal disease;
E. *involvement of the first metatarsophalanges joint.
322. Disease shown at Figure.129 is characterized by:
A. chiefly involvement of the lumbosacral portion of spine;
B. gradual onset;
C. frequently associated with renal disease;
D. *involvement of the first metatarsophalanges joint.
E. absence of renal disease;
323. Choose the most likely diagnosis for patient with shown changes (Figure 128.) from the below list
of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
324. Choose the most likely diagnosis for patient with shown changes (Figure 127.) from the below list
of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
325. Choose the most likely diagnosis for patient with shown changes (Figure 126.) from the below list
of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
326. Choose the most likely diagnosis for patient with shown changes (Figure 123.) from the below list
of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
327. Which drug should be prescribed for patient with shown changes (Figure 52.)?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
328. Which drug should be prescribed for patient with shown changes (Figure 123.)?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
329. Which drug should be prescribed for patient with shown changes (Figure 126.)?
A. *Allopurinol (Zyloprim)
B.
C.
D.
E.
330.
A.
B.
C.
D.
E.
331.
A.
B.
C.
D.
E.
332.
A.
B.
C.
D.
E.
333.
A.
B.
C.
D.
E.
334.
A.
B.
C.
D.
E.
335.
A.
B.
C.
D.
E.
336.
A.
B.
C.
D.
E.
337.
A.
B.
C.
D.
E.
338.
Furosemide (Lasix)
Cortisol (prednisone)
Diphenhydramine (Benadryl)
Indometacin (Indocin)
Which drug should be prescribed for patient with shown changes (Figure 127)?
*Allopurinol (Zyloprim)
Furosemide (Lasix)
Cortisol (prednisone)
Diphenhydramine (Benadryl)
Indometacin (Indocin)
Which drug should be prescribed for patient with shown changes (Figure 128.)?
*Allopurinol (Zyloprim)
Furosemide (Lasix)
Cortisol (prednisone)
Diphenhydramine (Benadryl)
Indometacin (Indocin)
Which drug should be prescribed for patient with shown changes (Figure 129.)?
*Allopurinol (Zyloprim)
Furosemide (Lasix)
Cortisol (prednisone)
Diphenhydramine (Benadryl)
Indometacin (Indocin)
Which changes will reveal X-ray examination of patient with shown changes (Figure 64.)?
Marked erosions
Subluxations
*Osteophytes
Osteoporosis
Ankylosis
Which changes will reveal X-ray examination of patient with shown changes (Figure 102.)?
Marked erosions
Subluxations
*Osteophytes
Osteoporosis
Ankylosis
Which changes will reveal X-ray examination of patient with shown changes (Figure 105.)?
Marked erosions
Subluxations
*Osteophytes
Osteoporosis
Ankylosis
Which changes will reveal X-ray examination of patient with shown changes (Figure 106.)?
Marked erosions
Subluxations
*Osteophytes
Osteoporosis
Ankylosis
Which changes will reveal X-ray examination of patient with shown changes (Figure 64.)?
Marked erosions
Subluxations
*Osteophytes
Osteoporosis
Ankylosis
Which changes will reveal X-ray examination of patient with shown changes (Figure 125.)?
A. Marked erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
339. A 60-year-old male is evaluated because of pain in the left inguinal area, lower back, and hands.
The inguinal pain worsens as he walks, and all pain increases as the day progresses. On physical
examination, internal rotation of the right hip elicits the groin pain. The second, third, and first
metatarsophalangeal joints are swollen, warm, and tender to pressure. Radiographs show severe
osteoarthritis in the right hip. X-ray of hand is shown in the picture (Figure 127). Which of the following
is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. *Serum uric acid
340. An 60 y.o. man with chronic polyarthritis started frusemide 3-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot shown in the (Figure 129). Choose the
most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Sepsis arthritis
C. Osteoarthritis
D. *Exacerbation of gouty arthritis
E. Psoriatic arthritis
341. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 52) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
342. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 123) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
343. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 126) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
344. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 127) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
345. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 128) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
346. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 129) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
347. Choose the most likely laboratory findings for patient with shown changes (Figure 52) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
348. Choose the most likely laboratory findings for patient with shown changes (Figure 103) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
349. Choose the most likely laboratory findings for patient with shown changes (Figure 123) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
350. Choose the most likely laboratory findings for patient with shown changes (Figure 126) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
351. Choose the most likely laboratory findings for patient with shown changes (Figure 127) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
352. Choose the most likely laboratory findings for patient with shown changes (Figure 128) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
353. Choose the most likely laboratory findings for patient with shown changes (Figure 129) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
354. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 103)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
355. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 123)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
356. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 126)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
357. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 127)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
358. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 128)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
359. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 129)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
360. A 65-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint. Choose the
investigation for diagnosis from the below list of options, watch (Figure 129):
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
361. A 65-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint. Choose the
investigation for diagnosis from the below list of options, watch (Figure 126):
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
362. A 65-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint . Choose the
investigation for diagnosis from the below list of options, watch (Figure 103):
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
363. A 65-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint. Choose the
investigation for diagnosis from the below list of options, watch (Figure 128):
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
364. Each of the following agents may be useful in the treatment of disease shown at (Figure 128) of
except
A. indomethacin
B. colchicines
C. allopurinol
D. intraarticular glucocorticoids
E. *aspirin
365. Each of the following agents may be useful in the treatment of disease shown at (Figure 126) of
except
A. indomethacin
B. colchicines
C. allopurinol
D. intraarticular glucocorticoids
E. *aspirin
366. Each of the following agents may be useful in the treatment of disease shown at (Figure 123) of
except
A. indomethacin
B. colchicines
C. allopurinol
D. intraarticular glucocorticoids
E. *aspirin
367. Look at the (Fig. 59) Choose the most likely diagnosis for patient with shown X-ray of hands from
the below list of options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
368. Look at the (Fig. 59) Choose the most likely diagnosis for patient with shown X-ray of hands from
the below list of options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
369. Look at the (Fig. 112) Choose the most likely diagnosis for patient with shown X-ray of hands from
the below list of options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
370. Look at the (Fig. 59). Which changes are shown on X-ray:
A. osteophytes;
B. dense subchondral bone;
C. loss of joint space;
D. *erosions at the margins of joints
E. subchondral bone cyst;
371. Look at the (Fig. 112). Which changes are shown on X-ray:
A. osteophytes;
B. dense subchondral bone;
C. loss of joint space;
D. *erosions at the margins of joints
E. subchondral bone cyst;
372. Look at the (Fig. 61). For shown arthritis more typical is:
A. starting pain;
B. night pain;
C. *morning stiffness;
D. weight loss;
E. asymmetric joint involvement;
373. Look at the (Fig. 112). For shown arthritis more typical is:
A. starting pain;
B. night pain;
C. *morning stiffness;
D. weight loss;
E. asymmetric joint involvement;
374. Look at the (Fig. 60). Drug of choice for patient with shown disease is
A. NSAIDs
B. Hydroxychloroquine sulphate
C. Sulphasalazine
D. *Methotrexate
E. D-penicillamine
375. Look at the (Fig. 58). X-ray findings of this disease following except:
A. juxtra-articular osteoporosis;
B. enlarged of joint space;
C. *osteophytes;
D. erosions at the margins of joints;
E. ankylosis and subluxations.
376. Look at the (Fig. 112). X-ray findings of this disease following except:
A. juxtra-articular osteoporosis;
B. enlarged of joint space;
C. *osteophytes;
D. erosions at the margins of joints;
E. ankylosis and subluxations.
377. Look at the (Fig. 60). Which joints of the body may be involved in this disease mainly?
A. hips;
B. *small joints of hands
C. ankles;
D. shoulders;
E. sacroiliac joints
378. Look at the (Fig. 61). Which joints of the body may be involved in this disease mainly?
A. hips;
B. *small joints of hands
C. ankles;
D. shoulders;
E. sacroiliac joints
379. Look at the (Fig. 60). Each of the following agents has been demonstrated to alter the course of
this disease except
A. gold
B. *omega-3 fatty acid
C. methotrexate
D. D-penicillamine
E. Hydroxychloroquine
380. Look at the (Fig. 112). Each of the following agents has been demonstrated to alter the course of
this disease except
A. gold
B. *omega-3 fatty acid
C. methotrexate
D. D-penicillamine
E. Hydroxychloroquine
381. Look at the (Fig. 58). Each of the following agents has been demonstrated to alter the course of
this disease except
A. gold
B. *omega-3 fatty acid
C. methotrexate
D. D-penicillamine
E. Hydroxychloroquine
382. Look at the (Fig. 59). Each of the following agents has been demonstrated to alter the course of
this disease except
A. gold
B. *omega-3 fatty acid
C. methotrexate
D. D-penicillamine
E. Hydroxychloroquine
383. Look at the (Fig. 58) representation of the hand demonstrating the frequent sites of early erosion in
…
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
384. Look at the (Fig. 59) representation of the hand demonstrating the frequent sites of early erosion in
…
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
385. Look at the (Fig. 112) representation of the hand demonstrating the frequent sites of early erosion
in …
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
386. Look at the (Fig. 60) Choose the most likely change shown in the picture.
A. Heberden’s nodes
B. Bouchar’s nodes
C. Dupuytren contracture
D. Bounniere deformity
E. *Ulnar deviation.
387. Look at the (Fig. 60) How often patients with Rheumatoid arthritis have Rheumatoid factor
positive?
A. 60 %
B. 65 %
C. 75 %
D. *85 %
E. 90 %
388. Look at the (Fig. 61) How often patients with Rheumatoid arthritis have Rheumatoid factor
positive?
A. 60 %
B. 65 %
C. 75 %
D. *85 %
E. 90 %
389. Look at the (Fig. 60). Which clinical manifestation would be an unexpected finding in a client
with this arthritis?
A. Anemia
B. Warm, tender joints
C. Symmetric and bilateral joint involvement
D. Elevated ESR
E. *Crepitus of involved joints
390. Look at the (Fig. 61). Which clinical manifestation would be an unexpected finding in a client
with this arthritis?
A. Anemia
B. Warm, tender joints
C. Symmetric and bilateral joint involvement
D. Elevated ESR
E. *Crepitus of involved joints
391. Look at the (Fig. 112). Which clinical manifestation would be an unexpected finding in a client
with this arthritis?
A. Anemia
B. Warm, tender joints
C. Symmetric and bilateral joint involvement
D. Elevated ESR
E. *Crepitus of involved joints
392. Look at the (Fig.60). The client on long-term corticosteroid therapy for this disease developed
abdominal striae. Side effect of which drug may cause pitting edema of both legs?
A. *Prednisone
B. Methotrexat
C. Folic acid
D. NSAIDs
E. None of the above
393. Look at the (Fig. 61). The client on long-term corticosteroid therapy for this disease developed
abdominal striae. Side effect of which drug may cause pitting edema of both legs?
A. *Prednisone
B. Methotrexat
C. Folic acid
D. NSAIDs
E. None of the above
394. On the Fig. 125 choose the most likely diagnosis for patient with shown changes from the below
list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gouty arthritis
E. Psoriatic arthritis
395. On the Fig. 64 choose the most likely diagnosis for patient with shown changes from the below list
of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gouty arthritis
E. Psoriatic arthritis
396. On the Fig. 105 choose the most likely diagnosis for patient with shown changes from the below
list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gouty arthritis
E. Psoriatic arthritis
397. On the Fig. 106 choose the most likely diagnosis for patient with shown changes from the below
list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gouty arthritis
E. Psoriatic arthritis
398. On the Fig. 125 which changes will reveal X-ray examination of patient with shown changes?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
399. On the Fig. 105 which changes will reveal X-ray examination of patient with shown changes?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
400. On the Fig. 106 which changes will reveal X-ray examination of patient with shown changes?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
401. On the Fig. 64 shown changes. Who suffer from this disease more often?
A. Young men
B. Children
C. Young women
D. Old men
E. *Old obese women
402. On the Fig. 105 shown changes. What is the name of this change?
A. *Heberden’s nodes
B. Bouchar’s nodes
C. Swan neck deformity
D. Bounniere deformity
E. Acute arthritis of metatarsophalangeal joints.
403. On the Fig. 106 shown changes. What is the name of this change?
A. *Heberden’s nodes
B. Bouchar’s nodes
C. Swan neck deformity
D. Bounniere deformity
E. Acute arthritis of metatarsophalangeal joints.
404. On the Fig. 53 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
405. On the Fig. 126 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
406. On the Fig. 127 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
407. On the Fig. 128 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
408. On the Fig. 129 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
409. On the Fig. 103 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
410. On the Fig. 126 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
411. On the Fig. 127 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
412. On the Fig. 128 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
413. On the Fig. 129 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
414. On the Fig. 103 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
415. On the Fig. 53 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
416. This 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs
(Fig. 116). He had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving
medium size arteries. The hyperpigmented patches represent the new phase of the lesions - tender dermal
nodules. Which of the following diagnoses is the most likely cause of this patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Takayasus arteritis
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
417. On the Fig. 116 shown changes, which are characterized for disease, other diagnostic criteria of its
exclude:
A. *Lymphoma
B. Testes pain
C. Diastolic pressure > 90
D. Decrease of BMI
E. Livedo reticularis
418. On the Fig. 116 shown changes, which are characterized for disease, that affected more often?
A. * Mild-year men
B. Mild-year women
C. Children
D. Both men and women
E. Boys less than 20 years old
419. This 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs
(Fig. 116). He had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving
medium size arteries. The hyperpigmented patches represent the new phase of the lesions - tender dermal
nodules. Choose the single most likely treatment from the list of options given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
420. This 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs
(Fig. 119). He had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving
medium size arteries. The hyperpigmented patches represent the new phase of the lesions - tender dermal
nodules. Choose the single most likely treatment from the list of options given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
421. On the Fig. 117 shown case of history: a 40-year-old man developed rash on his abdomen and legs
several weeks earlier. He also complained of tea colored urine. A skin biopsy confirmed the presence of
small vessel leukocytoclastic vasculitis. Which of the following diagnoses is the most likely cause of this
patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. *Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
422. On the Fig. 122 shown case of history: a 40-year-old man developed rash on his abdomen and legs
several weeks earlier. He also complained of tea colored urine. A skin biopsy confirmed the presence of
small vessel leukocytoclastic vasculitis. Which of the following diagnoses is the most likely cause of this
patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. *Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
423. On the Fig.117 shown changes, which are characterized for disease, that affected more often?
A. * Boys, less than 20 years old
B. Mild-year women
C. Men
D. Both men and women
E. Girls, from 5-25 years old
424. On the Fig.120 shown changes, which are characterized for disease, that affected more often?
A. * Boys, less than 20 years old
B. Mild-year women
C. Men
D. Both men and women
E. Girls, from 5-25 years old
425. On the Fig.122 shown changes, which are characterized for disease, that affected more often?
A. * Boys, less than 20 years old
B. Mild-year women
C. Men
D. Both men and women
E. Girls, from 5-25 years old
426. Choose the single most likely treatment from the list of options given below for patient, shown on
the Fig. 69
A. Aspirin
B. *Prednisone
C. Cefatoxim
D. NAIDs
E. IV aminophylline
427. Choose the single most likely treatment from the list of options given below for patient, shown on
the Fig. 117
A. Aspirin
B. *Prednisone
C. Cefatoxim
D. NAIDs
E. IV aminophylline
428. Choose the single most likely treatment from the list of options given below for patient, shown on
the Fig. 120
A. Aspirin
B. *Prednisone
C. Cefatoxim
D. NAIDs
E. IV aminophylline
429. Choose the single most likely treatment from the list of options given below for patient, shown on
the Fig. 122
A. Aspirin
B. *Prednisone
C. Cefatoxim
D. NAIDs
E. IV aminophylline
430. Disease shown at Figure 103.is characterized by:
A. chiefly involvement of the lumbosacral portion of spine;
B. gradual onset;
C. frequently associated with renal disease;
D. absence of renal disease;
E. *involvement of the first metatarsophalanges joint.
431. Choose the most likely diagnosis for patient with shown on X-ray changes (Figure 106.) and
tell,what you are looking for at hands such patients?
A. *Heberden’s nodes
B. Bouchar’s nodes
C. Swan neck deformity
D. Bounniere deformity
E. Acute arthritis of metatarsophalangeal joints.
432. Which changes will reveal X-ray examination of patient with shown changes (Figure 99.)?
A. Marked erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
433. Choose the most likely diagnosis for patient with shown changes (Figure 103.) from the below list
of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
434. Which drug should be prescribed for patient with shown changes (Figure 53.)?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
435. A 59-year-old woman presents with a 1-year history of pain in her thumbs. A focused examination
reveals squaring at the base of both first digits, worse on the right, and pain on pressure over the first
carpal metacarpal joints. She also has nontender bony overgrowth at the distal interphalangeal joints. Xray of hand is shown in (Figure 106). Choose the most likely diagnosis from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
436. A 60-year-old male is evaluated because of pain in the left inguinal area, lower back, and hands.
The inguinal pain worsens as he walks, and all pain increases as the day progresses. On physical
examination, internal rotation of the right hip elicits the groin pain. The second, third, and fourth
metacarpophalangeal joints are swollen, warm, and tender to pressure. Radiographs show severe
osteoarthritis in the right hip. X-ray of hand is shown in the picture (Figure 104.). Which of the following
is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. *Serum uric acid
437. An 60 y.o. man with chronic polyarthritis started frusemide 3-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot shown in the (Figure 53). Choose the
most likely diagnosis from the below list of options.
A. Rheumatoid arthritis
B. Sepsis arthritis
C. Osteoarthritis
D. *Exacerbation of gouty arthritis
E. Psoriatic arthritis
438. An elderly man with chronic polyarthritis started frusemide 2-weeks ago and now presents with a
red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is shown in the picture. Choose the most
likely laboratory findings for patient with shown changes (Figure 53) from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum
439. Choose the most likely diagnosis for patient with shown changes (Figure 53.) from the below list of
options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
440. Choose the most likely diagnosis for patient with shown changes (Figure 52.) from the below list of
options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
441. Choose the most likely laboratory findings for patient with shown changes (Figure 53) from the
below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
442. Which of the following is clinical characteristic of the disease for patient with shown changes
(Figure 53)?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
443. A 65-yr-old alcoholic man presents with a hot swollen first metatarsophalangeal joint. Choose the
investigation for diagnosis from the below list of options, watch (Figure 53):
A. HLA-B27
B. *Synovial fluid analysis
C. X-ray
D. Anti-dsDNA antibody
E. Rheumatoid factor
444. A 65-yr-old man has started chemotherapy for lymphoma. He has developed a painful swollen
hot right knee. He is apyrexial. Choose the most likely changes from the below list of options, watch
(Figure 53):
A. *Urate crystals on joint aspirate
B. High ESR
C. Erosions on X-ray
D. Positive blood culture
E. Positive rheumatoid factor
445. Each of the following may cause hyperuricemia and thereby may provoke an attack of disease
shown at (Figure 53) except:
A. thiazide diuretics
B. exercise
C. cyclosporine
D. methotrexate
E. *ascorbic acid
446. Each of the following agents may be useful in the treatment of disease shown at (Figure 53) of
except
A. indomethacin
B. colchicines
C. allopurinol
D. intraarticular glucocorticoids
E. *aspirin
447. Which condition or health problem demonstrates inflammation without invasion shown at (Figure
52) ?
A. Osteoarthritis
B. Viral hepatitis
C. *Gout arthritis
D. Cellulitis
E. Septic arthritis
448. Which condition or action represents a modifiable risk factor for disease shown at (Figure 64) ?
A. *Obesity
B. Hypertension
C. Cigarette smoking
D. Walking as exercise
E. Fatty foods
449. Which change is shown in the (Figure 97)?
A. *Erythema marginatum
B. Osler's nodes
C. Erythema nodosum
D. Splinter hemorrhages
E. Janeway’s lesions
450. Look at the (Figure 97) Noncardiac Manifestations of infective endocarditis are the following
except:
A. splenomegaly
B. *a rash on the trunk and proximal extremities
C. petechiae
D. arterial emboli
E. Osler's nodes
451. A 14-yr-old boy has had a pyrexia, rash, raised ESR, 2 weeks after pharingitis. Subcutaneous nodules
and a generalised rash is noted on the trunk. Choose the single most likely diagnosis from the list of options
below,l ook at the(Figure 97):
A. Maculopapular rash
B. Erythema multiforme
C. *Erythema marginatum
D. Lichen planus
E. Erythema nodosum
452. In which disease nail changes shown in the (Figure 97) are seen?
A. Viral myocarditis
B. Acute pericarditis
C. *Rheumatic fever
D. Infective endocarditis
E. Hypertrophied cardiomyopathy
453. On this figure 97 you see erythema marginatum tell the diagnosis?
A. Viral myocarditis
B. Acute pericarditis
C. *Rheumatic fever
D. Infective endocarditis
E. Hypertrophied cardiomyopathy
454. This 23 year-old female had a history of shortness of breath and palpitations for 7 years with a
progressive increase one month before death. She was known to have both systolic and diastolic
murmurs. What is your favoured diagnosis (Figure 97)?
A. Infective endocarditis
B. Degenerative valvular disease
C. *Rheumatic heart disease
D. Connective tissue disease
E. Congenital valvular disease
455. Look at the (Figure 98). A 45-yr-old woman with previous rheumatic heart disease presents with
malaise and low-grade fever for a month. She recently had treatment for a dental abscess. On
examination she has splinter haemorrhages and an early diastolic murmur. Choose the single most likely
diagnosis from the list of options below.
A. Left atrial myxomaq
B. Pericarditis
C. SLE
D. *Infective endocarditis
E. Bacteraemia
456. Look at the (Figure 97). Major criteria of rheumatic fever are the following EXCEPT:
A. Carditis
B. Migratory polyarthritis
C. Sydenham's chorea
D. *Recent group A streptococcal infection
E. Erythema marginatum
457. In which disease nail changes shown in the (Figure 98) are seen?
A. *Infective endocarditis
B. Viral myocarditis
C. Acute pericarditis
D. Rheumatic heart disease
E. Hypertrophied cardiomyopathy
458. Look at the (Figure 97). Minor criteria for this disease are all of the following EXCEPT:
A. Fever >38°C
B. Embolic/vascular phenomena
C. Immunological phenomena
D. *Migratory arthritis
E. Blood cultures compatible but not typical for endocarditis
459. Look at the (Figure 98). Immunological phenomena in this disease are all of the following
EXCEPT:
A. glomerular nephritis
B. rheumatoid factor
C. Osler's nodes
D. Roth spots
E. *Erythema marginatum
460. Look at the (Figure 97). Causative organism in this disease is?
A. staphylococcus aureus
B. *streptococcus viridians
C. pneumococcus
D. streptococcal pyogenes
E. group A streptococcus
461. Look at the (Figure 97) Migrating polyarthritis is characteristically seen in
A. syphilitic arthritis
B. rheumatoid arthritis
C. psoriatic arthritis
D. *rhematic arthritis
E. gouty arthritis
462. Look at the (Figure 98) Which of the following are immune complex lesions in this disease?
A. *Osler’s nodes
B. mycotic aneurysms
C. anemia
D. vegetations
E. glomerylonephritis
463. Look at the (Figure 97) Echocardiographic findings for this disease are all of the following
EXCEPT:
A. Mobile echo dense masses attached to valve leaflets or endocardium
B. *Periannular abscesses
C. New dehiscence of a prosthetic valve
D. New valvular regurgitation
E. New valvular stenosis
464. Look at the (Figure 98) What investigation can detect vegetations in approximately 90% of patients
with this disease:
A. Echocardiogram
B. *Transoesophageal echocardiogram
C. ECG
D. CT
E. Chest X-ray
465. This 43 year-old female had a history of shortness of breath and palpitations for 7 years with a
progressive increase one month before death. She was known to have both systolic and diastolic
murmurs. Is the disease (Figure 98) pericardial, myocardial or endocardial?
A. Pericardial
B. Myocardial
C. *Endocardial
D. Pericardial and myocardial
E. Pericardial, myocardial and endocardial
466. Which change is shown in the (Figure 98)?
A. Palmar erythema
B. Osler's nodes
C. Septic vasculitis
D. *Splinter hemorrhages
E. Janeway’s lesions
467. Look on the (Figure 98). Patients with acute rheumatic fever in initial attack have evidence of
carditis, which may be characterized by all are the following EXCEPT:
A. *the first heart sound is accentuated
B. sinus tachycardia
C. the murmur of mitral regurgitation
D. an S3 gallop
E. Cardiomegaly
468. Look on the (Figure 97) Minor Criterion of rheumatic fever is:
A. sinus tachycardia
B. sinus bradycardia
C. *Prolonged P-Q interval
D. inversion of T waves
E. ectopic beats
469. Look on the (Figure 97) Migratory polyarthritis in rheumatic fever most often affecting following
joints except:
A. the ankles
B. wrists
C. *small joints of hands
D. knees
E. elbows
470. Look on the (Figure 97) Feature that distinguish rheumatic fever from myocarditis:
A. ST-T-wave abnormalities
B. *migratory arthritis
C. Arrhythmias
D. heart failure
E. tachycardia.
471. Look on the (Figure 97). This disease caused by:
A. Staphylococcus lugdunensis
B. Enterococci
C. Enterococci
D. The HACEK group
E. *beta-hemolytic streptococci
472. Look at the (Figure 57). Feature that distinguishes rheumatic heart diseases from infective
endocarditis is:
A. Doppler echocardiographic restriction of mitral valve leaflets, their calcification
B. pulmonary hypertension
C. cardiomegaly
D. *vegetations
E. syncope.
473. Look at the (Figure 97). All patients with this disease should be treated by:
A. diltiazem
B. ergotamine
C. *intramuscular benzathine penicillin G
D. heparin
E. streptokinase
474. Look at the (Figure 98) What is duration of the antibiotic treatment of the patients with this
disease?
A. *not less then two weeks
B. not less then 20 days
C. not less then a week
D. not less then 5 days
E. not less then a month
475. Look at the (Figure 97) What group of drugs has a significant role in the treatment of the patients
with this disease accompanied by congestive heart failure:
A. *steroids
B. salicylates
C. cefazolin
D. erythromycin
E. heparin
476. Look at the (Fig. 58) Choose the most likely diagnosis for patient with shown X-ray of hands from
the below list of options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
477. Look at the (Fig. 58). Which changes are shown on X-ray:
A. osteophytes;
B. dense subchondral bone;
C. loss of joint space;
D. *erosions at the margins of joints
E. subchondral bone cyst;
478. Look at the (Fig. 60). For shown arthritis more typical is:
A. starting pain;
B. night pain;
C. *morning stiffness;
D. weight loss;
E. asymmetric joint involvement;
479. Look at the (Fig. 61). Drug of choice for patient with shown disease is
A. NSAIDs
B. Hydroxychloroquine sulphate
C. Sulphasalazine
D. *Methotrexate
E. D-penicillamine
480. Look at the (Fig. 59). X-ray findings of this disease following except:
A. juxtra-articular osteoporosis;
B. enlarged of joint space;
C. *osteophytes;
D. erosions at the margins of joints;
E. ankylosis and subluxations.
481. Look at the (Fig. 58). Which joints of the body may be involved in this disease mainly?
A. hips;
B. *small joints of hands
C. ankles;
D. shoulders;
E. sacroiliac joints
482. Look at the (Fig. 61). Each of the following agents has been demonstrated to alter the course of
this disease except
A. gold
B. *omega-3 fatty acid
C. methotrexate
D. D-penicillamine
E. Hydroxychloroquine
483. Look at the (Fig. 61) representation of the hand demonstrating the frequent sites of early erosion in
…
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
484. Look at the (Fig. 112) Choose the most likely change shown in the picture.
A. Heberden’s nodes
B. Bouchar’s nodes
C. Dupuytren contracture
D. Bounniere deformity
E. *Ulnar deviation.
485. Look at the (Fig. 112) Choose the most likely diagnosis of patient with shown changes from the
below list of options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
486. Look at the (Fig. 58) Lung disorders in this disease include all of the following except
A. pleuritis (with effusions characterized by low glucose)
B. *pulmonary thromboembolism
C. interstitial fibrosis
D. nodules
E. Caplan’s syndrome
487. Look at the (Fig. 58) How often patients with Rheumatoid arthritis have Rheumatoid factor
positive?
A. 60 %
B. 65 %
C. 75 %
D. *85 %
E. 90 %
488. Look at the (Fig. 58) how often patients with Rheumatoid arthritis have anti-cyclic citrullinated
peptide?
A. *98 %
B. 92 %
C. 67 %
D. 78 %
E. 85 %
489. Look at the (Fig. 59) which of the following systemic manifestations is LEAST characteristic of
early adult rheumatoid arthritis?
A. *High fever
B. Weight loss
C. Muscle wasting
D. Vague musculoskeletal symptoms
E. Fatigue
490. Look at the (Fig. 58) Which of the following conditions is LEAST likely to occur in late
extraarticular seropositive rheumatoid arthritis?
A. Neutropenia
B. Dry eyes
C. Leg ulcers
D. Sensorimotor polyneuropathy
E. *Hepatitis
491. Look at the (Fig. 59) Choose the most likely diagnosis for patient with shown X-ray of feet from
the below list of options.
A. Gout
B. Still's disease
C. Pseudogout
D. *Rheumatoid arthritis
E. Osteoarthritis
492. Look at the (Fig. 59). Which changes are shown on X-ray?
A. osteophytes;
B. dense subchondral bone;
C. loss of joint space;
D. *erosions at the margins of joints
E. subchondral bone cyst;
493. Look at the (Fig. 59). For shown arthritis more typical is:
A. starting pain;
B. night pain;
C. *morning stiffness;
D. weight loss;
E. asymmetric joint involvement;
494. Look at the (Fig. 60). Drug of choice for patient with shown disease is
A. NSAIDs
B. Hydroxychloroquine sulphate
C. Sulphasalazine
D. *Methotrexate
E. D-penicillamine
495. Look at the (Fig. 59). Which clinical manifestation would be an unexpected finding in a client
with this arthritis?
A. Anemia
B. Warm, tender joints
C. Symmetric and bilateral joint involvement
D. Elevated ESR
E. *Crepitus of involved joints
496. Look at the (Fig. 59). The older adult client taking prednisone, methotrexate, folic acid, NSAIDs
for this disease now has pitting edema of both legs. Side effect of which drug may cause pitting edema of
both legs?
A. Prednisone
B. Methotrexat
C. folic acid
D. *NSAIDs
E. None of the above
497. Look at the (Fig. 59). The client on long-term corticosteroid therapy for this disease developed
abdominal striae. Side effect of which drug may cause pitting edema of both legs?
A. *Prednisone
B. Methotrexat
C. Folic acid
D. NSAIDs
E. None of the above
498. Look at the (Fig. 58). What factor or condition in the client who has joint stiffness and pain is
more associated with progressive systemic sclerosis than with this disease?
A. The client is female
B. The pain is worse in the morning
C. The client has never been pregnant
D. *The fingers are sausage-like, with nonpitting edema
E.
The client has limited motion
499. On the Fig. 102 choose the most likely diagnosis for patient with shown changes from the below
list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. *Osteoarthritis
D. Gouty arthritis
E. Psoriatic arthritis
500. On the Fig. 102 which changes will reveal X-ray examination of patient with shown changes?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
501. On the Fig. 102 shown changes. What is the name of this change?
A. *Heberden’s nodes
B. Bouchar’s nodes
C. Swan neck deformity
D. Bounniere deformity
E. Acute arthritis of metatarsophalangeal joints.
502. On the Fig. 102 shown changes. What can help us to confirm diagnosis?
A. High level of serum uric acid
B. Positive rheumatoid factor
C. High ESR
D. *Osteophytes on X-ray
E. Positive blood culture
503. On the Fig. 102 shown changes. Who suffer from this disease more often?
A. Young men
B. Young men with obesity
C. Young women
D. Old men
E. *Old women
504. On the Fig. 52 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Calcinosis
B. Hondroydosis
C. Ulcers
D. *Tophi
E. Cancer
505. On the Fig. 102 shown changes. What is the name of this change?
A. *Heberden’s nodes
B. Bouchar’s nodes
C. Swan neck deformity
D. Bounniere deformity
E. Acute arthritis of metatarsophalangeal joints.
506. On the Fig. 52 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
507. On the Fig. 53 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
508. On the Fig. 52 shown changes. Choose the most likely laboratory findings for patient with shown
changes from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
509. On the Fig. 52 shown changes. Which of the following is clinical characteristic of the disease for
patient with shown changes?
A. Short starting stiffness
B. *Acute night pain
C. Morning stiffness
D. Wight loss
E. Asymmetric joint involvement
510. On the Fig. 103 shown changes. Which changes will reveal X-ray examination of patient with
shown changes?
A. Marked erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
511. On the Fig. 103 shown changes. Choose the most likely diagnosis for patient with shown changes
from the below list of options.
A. Ankylosing spondylitis
B. Erythema nodosum
C. Osteoarthritis
D. *Gouty arthritis
E. Psoriatic arthritis
512. On the Fig. 103 shown changes. Which drug should be prescribed for patient with this changes?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
513. On the Fig. 104 shown changes. Which changes reveals shown X-ray examination of patient with
polyarthritis?
A. Marked destruction in joints
B. Subluxations of joints
C. *Fractures of bones
D. Osteoporosis of bones
E. Ankylosis of joints
514. On the Fig. 104 shown changes. Choose the most likely laboratory findings for patient with shown
changes from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
515. On the Fig. 104 shown changes. Which drug should be prescribed for patient with shown changes?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
516. On the Fig. 104 shown changes. Choose the most likely laboratory findings for patient with shown
changes from the below list of options.
A. High ESR
B. *High level of serum uric acid
C. Positive blood culture
D. Positive rheumatoid factor
E. High level of serum iron
517. On the Fig.52 shown changes. Which of following drugs should be prescribed for patient with
shown changes?
A. *Allopurinol (Zyloprim)
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
518. On the Fig. 53 shown changes. An elderly man with chronic polyarthritis started furosemide 2weeks ago and now presents with a red, hot, swollen first metatarsal phalangeal joint. X-ray of foot is
shown in the picture. Which of following drugs should be prescribed for patient with shown changes?
A. *Colchicine
B. Furosemide (Lasix)
C. Cortisol (prednisone)
D. Diphenhydramine (Benadryl)
E. Indometacin (Indocin)
519. On the Fig. 105 shown changes. Which changes reveals X-ray examination of patient with shown
changes?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Osteoporosis
E. Ankylosis
520. On the Fig. 106 shown changes. A 59-year-old woman presents with a 1-year history of pain in her
thumbs. A focused examination reveals squaring at the base of both first digits, worse on the right, and
pain on pressure over the first carpal metacarpal joints. She also has nontender bony overgrowth at the
distal interphalangeal joints. X-ray of hand is shown in the picture. Choose the most likely diagnosis
from the below list of options.
A. Ankylosing spondylitis
B. Rheumatoid arthritis
C. *Osteoarthritis
D. Gout
E. Psoriatic arthritis
521. On the Fig. 106 shown changes. A 53-year-old male is evaluated because of pain in the right
inguinal area, lower back, and hands. The inguinal pain worsens as he walks, and all pain increases as the
day progresses. On physical examination, internal rotation of the right hip elicits the groin pain. The
second, third, and fourth metacarpophalangeal joints are swollen, warm, and tender to pressure.
Radiographs show severe osteoarthritis in the right hip. X-ray of hand is shown in the picture. Which of
the following is the best test to confirm the diagnosis?
A. Rheumatoid factor
B. HLA-B27
C. Serum iron and iron-binding capacity
D. Fasting plasma glucose
E. *Serum uric acid
522. On the Fig. 106 shown changes. Which changes reveals X-ray examination of patient with shown
changes?
A. Erosions
B. Subluxations
C. *Osteophytes
D. Fracture
E. Ankylosis
523. This 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs
(Fig. 114). He had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving
medium size arteries. The hyperpigmented patches represent the new phase of the lesions - tender dermal
nodules. Which of the following diagnoses is the most likely cause of this patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Takayasus arteritis
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
524. On the Fig. 114 shown changes, which are characterized for disease, other diagnostic criteria of its
exclude:
A. *Lymphoma
B. Testes pain
C. Diastolic pressure > 90
D. Decrease of BMI
E. Livedo reticularis
525. On the Fig. 114 shown changes, which are characterized for disease, that affected more often?
A. * Mild-year men
B. Mild-year women
C. Children
D. Both men and women
E. Boys less than 20 years old
526. This 25-year-old man had a 7 month history of progressive, painful, pruritic ulcers on both legs
(Fig. 114). He had no evidence of systemic disease. A skin biopsy revealed a vasculitis involving
medium size arteries. The hyperpigmented patches represent the new phase of the lesions - tender dermal
nodules. Choose the single most likely treatment from the list of options given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
527. On the Fig. 70 shown case of history: a 40-year-old man developed rash on his abdomen and legs
several weeks earlier. He also complained of tea colored urine. A skin biopsy confirmed the presence of
small vessel leukocytoclastic vasculitis. Which of the following diagnoses is the most likely cause of this
patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. *Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
528. On the Fig.70 shown changes, which are characterized for disease, that affected more often?
A. * Boys, less than 20 years old
B. Mild-year women
C. Men
D. Both men and women
E. Girls, from 5-25 years old
529. Choose the single most likely treatment from the list of options given below for patient, shown on
the Fig. 70
A. Aspirin
B. *Prednisone
C. Cefatoxim
D. NAIDs
E. IV aminophylline
530. On the Fig. 70 shown case of history: a 40-year-old man developed rash on his abdomen and legs
several weeks earlier. He also complained of tea colored urine. A skin biopsy confirmed the presence of
small vessel leukocytoclastic vasculitis. Choose the single most likely treatment from the list of options
given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
531. On the Fig. 70 shown case of history: a 40-year-old man developed purpuric papules on his legs
several weeks earlier. He also complained of tea colored urine. A skin biopsy confirmed the presence of
small vessel leukocytoclastic vasculitis. Which of the following diagnoses is the most likely cause of this
patient’s symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. *Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
532. On the Fig.117 shown case of history: a 40-year-old man developed purpuric papules on his legs
several weeks earlier. He also complained of tea colored urine. A skin biopsy confirmed the presence of
small vessel leukocytoclastic vasculitis. Choose the single most likely treatment from the list of options
given below.
A. Prednisone 20 mg/d
B. Prednisone 15 mg/d
C. Ciprofloxacin, NSAIDs
D. *Prednisone 60 mg/d
E. Tetracycline, prednisone
533. On the Fig. 118 shown case of history: a 17-year-old girl developed purpuric papules consistent
with a leukocytoclastic vasculitis on her distal extremities several weeks after a viral upper respiratory
infection. She had migratory swelling of the hands and feet and intermittent crampy abdominal pain. Her
urinalysis and blood pressure were normal. A skin biopsy from a lesion on the top of the foot showed a
leukocytoclastic vasculitis, and direct immunofluorescence demonstrated deposition of IgA around
dermal blood vessels. Which of the following diagnoses is the most likely cause of this patient’s
symptoms?
A. Lymphoma, with a paraneoplastic syndrome
B. Kawasaki’s disease
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. *Henoch-Schonlein purpura
534. On the Fig. 118 shown case of history: a 37-year-old man developed purpuric papules consistent
with a leukocytoclastic vasculitis on her distal extremities several weeks after a viral upper respiratory
infection. She had migratory swelling of the hands and feet and intermittent crampy abdominal pain. Her
urinalysis and blood pressure were normal. A skin biopsy from a lesion on the top of the foot showed a
leukocytoclastic vasculitis, and direct immunofluorescence demonstrated deposition of IgA around
dermal blood vessels. Choose the single most likely treatment from the list of options given below.
A. Tetracycline
B. *Prednisone
C. Ciprofloxacin
D. Beta 2 agonist
E. IV aminophylline
535. On the Fig. 119 shown case of history: a 43-year-old woman was referred to hospital for recurrent
palpable purpura and cutaneous ulcers over her lower legs. Her disease started 3 years ago with
erythematous papules and palpable purpuric lesions located over her lower legs including the dorsa of her
feet. On her lower legs we found several cutaneous ulcers covered with hemorrhagic crusts along with
hyper- and hypopigmented atrophic scars and a few excoriated papules. A multitude of hypopigmented
oval atrophic scars were distributed over her upper back. The rest of physical examination including
accessible mucosal surfaces and peripheral pulses was normal. Which of the following diagnoses is the
most likely cause of this patient’s symptoms?
A. *Cutaneous small-vessel vasculitis
B. Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
536. On the Fig. 119 shown case of history: a 49-year-old woman was referred to hospital for recurrent
palpable purpura and cutaneous ulcers over her lower legs. Her disease started 3 years ago with
erythematous papules and palpable purpuric lesions located over her lower legs including the dorsa of her
feet. On her lower legs we found several cutaneous ulcers covered with hemorrhagic crusts along with
hyper- and hypopigmented atrophic scars and a few excoriated papules. A multitude of hypopigmented
oval atrophic scars were distributed over her upper back. She also complained of tea colored urine. The
rest of physical examination including accessible mucosal surfaces and peripheral pulses was normal.
Choose the single most likely treatment from the list of options given below.
A. Tetracycline 250 mg/d
B. *Prednisone 0.05-2 mg/kg/d PO divided bid/qid;
C. Ciprofloxacin 250 mg 2 times a day
D. Beta 2 agonist
E. IV aminophylline
537. On the Fig. 120 shown case of history: a 26-year-old previously healthy man presented to hospital
department with fever and rash of 5 days’ duration. He had initially noted small, erythematous, “red
spots” on the soles of his feet, which had evolved into diffusely tender and coalescent blisters, with
progressive involvement of both thighs. Self-treatment with antifungal cream had given no relief.
Physical examination revealed numerous violaceous, palpable, nonblanching, and indurated purpuric
lesions of differing sizes on the lower and upper extremities. All the lesions were tender to palpation.
Urinalysis showed microscopic hematuria. Biopsy of the lesions showed granular dermal perivascular
deposition of immunoglobulin (Ig) A containing immune complexes. Which of the following diagnoses
is the most likely cause of this patient’s symptoms?
A. Cutaneous small-vessel vasculitis
B. *Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. Polyarteritis nodosa
E. Kawasaki’s disease
538. On the Fig. 120 shown case of history: a 26-year-old previously healthy man presented to hospital
department with fever and rash of 5 days’ duration. He had initially noted small, erythematous, “red
spots” on the soles of his feet, which had evolved into diffusely tender and coalescent blisters, with
progressive involvement of both thighs. Self-treatment with antifungal cream had given no relief.
Physical examination revealed numerous violaceous, palpable, nonblanching, and indurated purpuric
lesions of differing sizes on the lower and upper extremities. All the lesions were tender to palpation.
Urinalysis showed microscopic hematuria. Henoch-Schonlein purpura was diagnosed. Which of the
following investigation is specific for diasgnosis?
A. a battery of wheal-and-flare allergy skin tests
B. measurement of total serum immunoglobulin E (IgE) concentration
C. measurement of CI esterase inhibitor activity
D. *skin biopsy
E. patch testing
539. On the Fig. 121 shown case of history: this 25-year-old woman had a 7 month history of skin rash.
She had no evidence of systemic disease. What kind of skin rash she has?
A. Erythema nodosum
B. *Livedo reticularis
C. Psoriasis
D. Vitiligo
E. Erythema annulare
540. On the Fig.121 shown case of history: this 29-year-old man had a 7 month history of skin rash. He
has had hypertension, progressive numbness in his feet. He recently developed mild polyarthritis in his
hands. Which of the following diagnoses is the most likely cause of this patient’s symptoms?
A. Cutaneous small-vessel vasculitis
B. Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s disease
541. On the Fig. 122 shown case of history: direct immunofluorescence (DIF) showed deposits of IgA
about dermal vessels. Which of the following diagnoses is the most likely cause of this patient’s
symptoms?
A. Cutaneous small-vessel vasculitis
B. Henoch-Schonlein purpura
C. Systemic lupus erythematosus
D. *Polyarteritis nodosa
E. Kawasaki’s diseasе