Click here to this article as a Word Document - e
advertisement

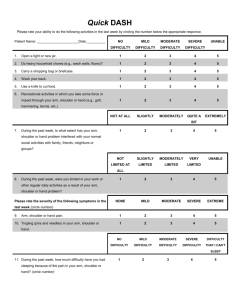
Shoulder Dystocia & Erb’s Palsy (Brachial Plexus Injury) Author: Craig V. Towers, M.D., F.A.C.O.G. Objectives: Upon the completion of this article the reader will be able to: 1. Define shoulder dystocia and brachial plexus injury and discuss the relationship between these two entities. 2. Discuss the warning signs and risk factors surrounding shoulder dystocia and whether a shoulder dystocia event is predictable. 3. Explain the various maneuvers that may be performed in order to relieve a shoulder dystocia. 4. Describe the issues of informed consent regarding shoulder dystocia and how brachial plexus injury can occur in non-shoulder dystocia deliveries. Definition Shoulder dystocia is defined as a delivery in which the fetal shoulders do not delivery following gentle downward traction on the baby’s head that requires the use of additional obstetrical maneuvers in order to complete the delivery. This article will discuss all of the issues listed below that are related to this obstetrical emergency. 1 Incidence and general overview 2 Risk factors / potential warning signs / & predictability 3 Obstetrical maneuvers that can be utilized 4 Informed consent and scheduled cesarean section 5 Other facts Incidence and General Overview Understanding the statistics of shoulder dystocia and Erb’s palsy is probably one of the most important areas of this article. The overall incidence of shoulder dystocia is approximately 1% of all deliveries. In studies, the rate varies between about 0.5% to 1.5% depending on the definition for shoulder dystocia that was used and the population studied. What is true is that this rate increases as birthweight increases. On average, the risk of shoulder dystocia is probably about 0.5 % for births under 4000 grams, 2% to 3% for births between 4000 and 4500 grams, and 4% to 15% for births greater than 4500 grams. Even thought the risk for shoulder dystocia is greater in births over 4000 grams, the overall number of shoulder dystocia deliveries is about 50/50 for births under 4000 grams and births over 4000 grams. This is because 85% to 90% of all births result in babies that are less than 4000 grams. This is an important fact when we discuss the predictability of shoulder dystocia later on in this article. The incidence of brachial plexus injury is somewhat different. It is important to understand that most shoulder dystocia deliveries do not result in Erb’s palsy. Likewise, approximately half of the Erb’s palsies that are seen come from deliveries in which there was no shoulder dystocia. This is a fact that needs to be understood. For years, nearly every textbook in obstetrics and pediatrics stated that if a baby was found to have an Erb’s palsy following birth, then a shoulder dystocia must have occurred and the delivering healthcare provider probably applied excessive downward traction in the delivery of the anterior shoulder. It was not until the mid to late 1990’s that research began to look at this question and has now shown that in fact this belief was terribly incorrect. Using one of the largest studies ever published on brachial plexus injury, the incidence of Erb’s palsy is approximately 0.15% of all deliveries (which is about 1 in every 650 to 700 births). It is now a truth that only about half of these brachial plexus injuries come from a delivery complicated by shoulder dystocia. The other half comes from deliveries in which NO shoulder dystocia occurred. This fact has now been demonstrated in numerous studies that total more than 2600 Erb’s palsies (seen in the table below). Shoulder dystocia, however, is definitely a risk factor when it comes to brachial plexus injuries and this statistic will be further clarified under the heading of “Risk Factors” seen below. Author Erb’s with SD Erb’s without SD Total Levine 1984 8 28 36 Gonik 1991 14 13 27 Jennett 1992 17 22 39 Nocon 1993 28 5 33 Lipscomb 1995 7 5 12 Perlow 1996 12 4 16 Sandmire 1996 19 17 36 Graham 1997 8 7 15 Peleg 1997 15 36 51 Brown 1997 17 13 30 Ecker 1997 43 37 80 Gherman 1998 23 17 40 Shivvers 1998 78 108 186 Gilbert 1999 860 751 1611 Raio 2003 58 36 94 Evans-Jones 2003 206 117 323 Totals 1413 (53.7%) 1216 (46.3%) 2629 In conjunction with the large numbers seen in the table above, there are two other compelling facts that verify the issue that most brachial plexus injuries are not caused by the delivering healthcare provider. These are cesarean section and the posterior arm. Before these facts can be discussed, the origin of a brachial plexus injury / Erb’s palsy must be understood. These injuries are caused by a stretching of the nerves in the neck region in the area of C-5 to T-1 (cervical nerve roots 5, 6, 7, & 8 and thoracic nerve root 1). These nerves will be further discussed under “other facts” seen below. However, to say it again, these injuries are caused by stretching of the nerves beyond their capacity. Pulling on the baby’s head straight out does not cause the injury (this would result in further shoulder impaction and possible spinal cord injury for the baby). Erb’s palsy is a traction or vector injury. The fact that numerous case reports exist of brachial plexus injuries identified following cesarean section verifies that this stretching can occur in utero. In fact, 60 of the 1611 Erb’s palsies (4%) seen in the Gilbert study occurred in a cesarean section delivery. Therefore, not all brachial plexus injuries occur in vaginal deliveries. Furthermore, everyone would agree that human anatomy varies from person to person. If we examine the population of the world, we will see some individuals with very long necks and some with very short necks and everything in between. Likewise, the birth canals of women also vary. The distance from behind the pubic bone to the perineum (or just outside the birth canal) is not the exact same distance for all pregnant women. Thus, if a baby with a relatively short neck delivers vaginally in a woman with a long distance from behind the pubic bone to the perineum, the nerves in the neck region can be stretched beyond their capacity upon delivery of the head before any healthcare provider applies any downward traction. In this same mother-baby delivery scenario, the nerves in the neck may be stretched up to their capacity upon delivery of the head but are stretched beyond their capacity when the normal amount of gentle downward traction is applied. Finally, in the face of a shoulder dystocia, the nerves in the baby’s neck can be damaged if excessive downward traction is applied. This is why excessive downward traction (for the most part) should be avoided and other maneuvers utilized when a shoulder dystocia is encountered (these maneuvers will be discussed below). The posterior arm is the second compelling finding that verifies that the delivering healthcare provider does not cause most brachial plexus injuries. Again, in the past it was presumed that all brachial plexus injuries occurred because of excessive traction on the anterior shoulder in a delivery complicated by a shoulder dystocia. Along with the fact that numerous studies now show that approximately half of the injuries are seen in deliveries with no shoulder dystocia, several recent studies have now identified that approximately one-third of all Erb’s palsies are seen in the posterior arm of the baby. The theory behind this occurrence is that during the labor process of some pregnancies, the baby’s posterior shoulder becomes entrapped on the sacral promontory. When the head delivers, the stretch from this point to just outside the birth canal is tremendous and is much further than the distance from behind the pubic bone to just outside the birth canal. In addition, when a baby’s head delivers in this situation, the gentle downward traction that is applied will actually shorten the distance between this entrapped posterior shoulder and would be beneficial rather than harmful. The importance of this finding is that none of the maneuvers applied by the delivering healthcare provider will actually further stretch the nerves in a posterior arm injury. If anything, they will actually shorten the distance. Thus, a brachial plexus injury of a posterior arm occurs with the delivery of the head prior to any maneuvers utilized by the healthcare provider. It should be mentioned that upward traction on a baby’s head prior to the delivery of the anterior shoulder is not a recognized obstetrical maneuver, will not result in the delivery of the posterior shoulder before the anterior shoulder, and should not be used. Therefore to summarize the four possibilities, the stretching of the nerves in a baby’s neck can occur in utero prior to the onset of labor; can occur following the delivery of the head before any downward traction is applied; can occur with the normal amount of downward traction applied in normal deliveries; and can occur with excessive traction in the face of a shoulder dystocia. Risk Factors / Potential Warning Signs / & Predictability Numerous studies have been published over the years that have looked at shoulder dystocia and potential risk factors. However, from a simplistic point of view, there are 2 basic risk factors for shoulder dystocia and these are a baby that is too large for the mother’s birth canal (macrosomia, most commonly defined as > 4500 grams) or a mother’s pelvis that is too small or poorly shaped for the birth of the baby (non-macrosomic baby) or a combination of the two. A third potential risk factor is diabetes, which will be discussed in more detail below. Numerous other “described” risk factors have been studied, but none of them alone or in combination can accurately predict when a shoulder dystocia will occur. In the majority of studies, the ability to predict a shoulder dystocia was well below 50%. Only a few have had a prediction rate of greater than 50%, none were above 75%, and none have been re-producible. Therefore, shoulder dystocia cannot be accurately predicted nor prevented (a statement concurred by ACOG). This means that every healthcare provider who performs vaginal deliveries will experience a shoulder dystocia and will need to know how to handle the situation when it arises. Nevertheless, even though shoulder dystocia cannot be accurately predicted, warning signs and other “described” risk factors need to be reviewed. It should be noted that many of the “described” risk factors that have been associated with shoulder dystocia are really risk factors for macrosomia and if macrosomia is not present, then these are of no significance. Warning signs of an impending shoulder dystocia primarily occur in a patient that is in labor. The only exception is a prior history of a shoulder dystocia, especially one that occurred in a baby that was non-macrosomic. This might imply that the primary factor lies with the size and/or shape of the mother’s pelvis. As a review, there are 4 primary shapes to a mother’s pelvis. The most common shape is gynecoid, which is seen in approximately 45% to 50% of women and is considered to be the most round in shape. The second most common is the anthropoid pelvis, which is seen in about 30% of women and is oval in an anteroposterior direction and could predispose to a persistent occiput posterior (OP) position of the baby’s head in labor. The third most common pelvis is the android pelvis, which occurs in about 20% of women and is heart shaped. Finally, the platypelloid pelvis is the least common seen in only 3% of women and is oval from side to side (thus, the distance between the pubic arch and sacrum is short). The platypelloid pelvis is the one that could predispose to a shoulder dystocia, especially in the presence of a non-macrosomic baby. There are 2 basic warning signs that occur in labor. These are a prolonged second stage of labor and the need for instrumentation (use of a vacuum or forceps). Unfortunately, neither of these alone or in combination can predict the occurrence of a shoulder dystocia. Therefore, if either of these or both exist, the best approach is to be prepared for a shoulder dystocia in case one occurs (preparation for a shoulder dystocia is discussed below). As a start, a few studies have suggested that induction of labor, the use of epidural anesthesia, and the length of the first stage of labor might be risk factors for a shoulder dystocia; however, the overwhelming data have shown that they are not. Furthermore, the size and position of the fetal shoulders is unlikely to affect whether or not the cervix will dilate to complete (which involves the first stage of labor). The size and shape of the fetal shoulders may, however, affect how well the baby traverses the birth canal once the mother has dilated to complete (which is the second stage of labor). Therefore, a prolonged second stage of labor could be a warning sign for an impending shoulder dystocia. In addition, a prolonged second stage of labor often goes hand-in-hand with the potential need for the use of forceps or a vacuum to accomplish the delivery. It is extremely important to remember that there needs to be an indication for the use of forceps and/or vacuum. The indications for the use of forceps or vacuum (and the definition of a prolonged second stage of labor) are as follows: (1) maternal indications such as cardiac disorders, severe pulmonary disorders, hemorrhage, etc. (or) (2) fetal indications such as non-reassuring fetal heart tracings, etc. (or) (3) prolonged second stage – ACOG has defined the length of the second stage and if these times are exceeded, then a diagnosis of a prolonged second stage can be entertained. For nulliparous women – 2 hours without regional anesthesia, 3 hours with regional anesthesia; For multiparous women – 1 hour without regional anesthesia, 2 hours with regional anesthesia. Maternal exhaustion is often listed as an indication for an instrumented delivery, but this diagnosis cannot be made in a short period of time once the patient becomes completely dilated. Some attempt needs to be made in coaching and educating the patient regarding how to create effective pushing, including a discussion on the potential need for cesarean section, if she does not at least attempt some pushing effort. In addition, there are basic requirements that need to be met when using forceps or a vacuum and these requirements ARE THE SAME for both instruments. They are a fully dilated cervix with an engaged fetal head at > +2 cm station (which corresponds to a minimum of a low pelvic delivery). Midpelvic and/or high pelvic deliveries, for the most part, should not be done. Many other “described” risk factors have been evaluated over the years, including obesity, excessive maternal weight gain (defined as > 20 kilograms or 44 pounds), postterm (> 42 weeks gestation), large fundal height measurements, and a prior delivery of a baby > 4000 grams. These, however, are primarily risk factors for macrosomia. Again, if macrosomia is not present, then these do not increase the risk for a shoulder dystocia. Finally, regarding “risk factor” issues for shoulder dystocia, diabetes, especially insulin dependent diabetes, produces two dilemmas. To begin with, diabetes can increase the risk for macrosomia and macrosomia can increase the risk for shoulder dystocia. In addition, diabetes, especially when poorly controlled, probably increases the risk for shoulder dystocia in babies that are not macrosomic because of its potential effect on the final dimensions of the baby that delivers. The reason for this is easier to explain with an example. Let’s say a given pregnancy was destined to have a baby of 3200 grams and 21 inches in length. If this pregnancy were complicated by poorly controlled diabetes, the baby may end up at 3700 grams but is still 21 inches in length, making the dimensions of the baby “fatter” for its length increasing the chance for a shoulder dystocia. Turning our attention to brachial plexus injury, shoulder dystocia is definitely a risk factor. To show this, we need to review some statistics. To begin with, there are approximately 4 million births in the United States every year. It has now been demonstrated in over 15 studies that about 50% of the Erb’s palsy cases occur in a shoulder dystocia delivery and the other 50% occur in deliveries without a shoulder dystocia. If the incidence of Erb’s palsy is approximately 1 in 650 to 700 births, then about 6000 cases of brachial plexus injury will occur in a given year. If the overall incidence of shoulder dystocia is 1%, then there are about 40,000 cases of shoulder dystocia per year. Since approximately half of the Erb’s palsies that occur are seen in deliveries with a shoulder dystocia, then 3000 brachial plexus injuries occur in these 40,000 deliveries or about 1 in 13 deliveries (7.5%). The other 3000 cases occur in the 3,960,000 births in which a shoulder dystocia did not occur or about 1 in 1320 deliveries (.075%). Thus, a brachial plexus injury is about 100 times more likely to be seen in a shoulder dystocia delivery, which is why most healthcare clinicians had the belief that the disorder could only occur in the presence of a shoulder dystocia. However, when we only examine shoulder dystocia deliveries, fortunately, the majority do not result in a brachial plexus injury. In fact, the risk of having any level of Erb’s palsy develop in a shoulder dystocia delivery is approximately 20% (plus or minus 5%). Of these, approximately 15% are permanent (plus or minus 5%). Thus, in a 100 shoulder dystocia deliveries there will be approximately 15-25 brachial plexus injuries and of these only 2-5 will be permanent (a 2% to 5% overall permanent rate). Obstetrical Maneuvers That Can Be Utilized Numerous maneuvers (that might be utilized once a shoulder dystocia is recognized) have been reported and evaluated over the years. Categorically, there are 5 basic groups, which are the McRoberts maneuver, suprapubic pressure, rotational maneuvers, delivery of the posterior arm, and heroic procedures. One of the easiest and most often utilized maneuvers is McRoberts, which was described in 1983 and involves hyper-flexing the legs back toward the mother’s abdomen. An assistant may also apply suprapubic pressure as the operator performs normal downward traction on the baby’s head. Suprapubic pressure involves the application of downward pressure just cephalic to the mother’s pubic bone (in the area of the mother’s bladder). The term “rotational maneuvers” is used in this manuscript because the words are often intermixed and loosely applied by healthcare providers (i.e. Woods maneuver, corkscrew maneuver, Woods screw maneuver, Rubin maneuver, etc.). As a purist, in 1943, Woods described a maneuver of placing a hand on the chest side of the posterior shoulder of the baby and trying to rotate the posterior shoulder upward 180 degrees. This would cause the anterior shoulder to fall below the pubic bone and conceptually, the baby would move in a corkscrew pattern. In 1964, Rubin described placing a hand (on the back side of the baby) behind either the anterior or posterior shoulder (which ever was the easiest to access), and applying pressure to fold the shoulders toward the chest. In essence, rotational maneuvers involve placing a hand on the baby’s shoulders and applying pressure that rotates the position of the baby in the birth canal. Delivery of the posterior arm involves the operator placing a hand into the vaginal canal posteriorly up to a distance where the posterior arm of the baby is identified. The arm is then grasped and swept across the baby’s chest and out the birth canal, which will result in the anterior shoulder dropping below the pubic bone allowing for delivery. This procedure, though very successful, can often result in a fracture of the baby’s humerus. Heroic maneuvers have also been described but should only be utilized if the above 4 categories are not successful. In addition, some of these maneuvers require extra training. These include the deliberate fracture of the baby’s clavicle (which is extremely difficult to do), cleidotomy (which is transecting the baby’s clavicle with the use of scissors), symphysiotomy (which is transecting the fibrous tissue between the pubic bones of the mother’s pelvis), and the Zavanelli maneuver, also called cephalic replacement (reported in 1985 and involves placing the baby’s head back into the birth canal and performing a cesarean section). The published reports on the Zavanelli maneuver have shown mixed results ranging from normal outcomes to severe injuries and stillbirth. Regarding the maneuvers, three other areas need to be discussed. The first is the use of fundal pressure. This maneuver can be used PRIOR to the delivery of the baby’s head and as a purist; fundal pressure is utilized in nearly every term cesarean section to effectuate the delivery. However, fundal pressure should not be used once the head has delivered because it will not help in delivering the shoulders, can further impact the anterior shoulder against the mother’s pubic bone, and if applied while the operator uses downward traction on the baby’s head could lead to injury. The second area is the use of an episiotomy. An episiotomy will not result in the delivery of the baby in the case of a shoulder dystocia because the baby is not impacted on soft tissue. However, an episiotomy can allow more room for the operator’s hand to perform rotational maneuvers or delivery of the posterior arm. The third issue is the use of traction. Downward traction IS USED in the overwhelming majority of deliveries. In fact, the definition of a shoulder dystocia is when the baby’s shoulders do not deliver following the use of normal downward traction. Once the diagnosis is made, the maneuvers above should be utilized. Excessive downward traction, however, can result in injury to the baby’s brachial plexus and should be avoided unless all other maneuvers fail and the decision is made to potentially sacrifice the arm in order to prevent neonatal brain injury or death. Though very few studies exist on this topic, it appears that neonatal brain injury can begin to occur if the shoulder dystocia extends beyond 5 minutes (though this area is not black and white and also involves the status of the baby prior to the delivery of the head). Again, upward traction on the baby’s head should not be performed prior to the delivery of the anterior shoulder because it is not a recognized obstetrical maneuver and will not result in the delivery of the posterior shoulder before the anterior shoulder. Informed Consent and Scheduled Cesarean Section One could argue that informed consent and shoulder dystocia are words that should not occur in the same sentence. The reason is because shoulder dystocia is unpredictable. However, informed consent can still play a role in this arena. Good labor management still involves an attempt at estimating fetal weight. Though our ability to accurately estimate fetal weight is often abysmal, we as healthcare providers should still make an assessment and if we believe the fetal weight might be macrocosmic, options should be given to the patient. These include the options of a cesarean section and its associated risks versus the risks of a vaginal delivery in the face of potential macrosomia. Also included in this discussion is that our estimate may be off and an unnecessary procedure might occur. This estimated fetal weight can occur by either ultrasound or physical examination (Leopold maneuvers). Studies have not really shown one to be superior to the other. In fact, one study showed that the mother’s prediction was closer than either an ultrasound or physical evaluation. If the healthcare provider believes that macrosomia might be present, and the patient chooses to proceed with a vaginal delivery, it would be prudent to have extra help present at the time of delivery. In addition, though no studies exist on this issue, the use of forceps or a vacuum in this setting may also not be warranted. If the patient is unable to push the baby out, the safest approach might be to proceed with a cesarean section (especially if the labor has a prolonged second stage). Regarding the issue of a scheduled cesarean section for the purpose of preventing a shoulder dystocia, ACOG has recommended that it be considered if the estimated fetal weight exceeds 5,000 grams in non-diabetics or 4,500 grams in women with diabetes. Again, these recommendations were made because of the high error rate in accurately predicting macrosomia combined with the overall risks of permanent injury with vaginal delivery in cases of macrosomia versus the risks of cesarean section. Other Facts One concept that may be difficult for some healthcare providers to comprehend is how brachial plexus injuries can occur without a shoulder dystocia or the use of excessive traction. To begin with, numerous injuries and findings are seen in normal spontaneous (non-instrumented) vaginal deliveries, both to the mother and the neonate. Some of the reported injuries for the mother include significant cervical and perineal tears, pelvic nerve injuries, a fractured coccyx, and a separated symphysis pubis. For the neonate, there is significant molding of the head, fractured skulls, subdural hematomas, fractured clavicles, and brachial plexus injuries. All of these and more can occur because the power of the uterine muscle is formidable. It should be noted that nearly all healthcare providers who perform deliveries are not strong enough to replace an inverted uterus without the aid of some uterine muscle relaxation medication. This is because the force of the uterus (endogenous), especially when combined with the force of the mother’s valsalva pushing efforts, will often exceed 100 pounds. This endogenous force is 4 to 9 times greater than the exogenous force utilized in deliveries by the healthcare provider. The explanation of this point is very technical and involves the use of physics and is presented in the next paragraph for those who are interested. We measure the strength of uterine contractions by millimeters of mercury (mmHg). A mmHg is a pressure measurement that is roughly equal to 30 pounds of force per square meter of area. Using intrauterine pressure catheter data, the force of a uterine contraction combined with the mother’s expulsive forces often equals 80 mmHg, which equates to about 2,400 pounds of force per square meter of area. The cross-sectional area of the birth canal when the cervix is completely dilated is about 80 square centimeters. If the force of a labor contraction and pushing were equally distributed throughout the uterus (meaning that the force upward against the uterine wall in the fundus were equal to the force downward through the birth canal), then the force in the birth canal when a mother is completely dilated and is pushing would only be about 19 pounds. However, we know that a labor contraction actually begins in the muscle fibers of the fundus and propagates down the uterus toward the birth canal because its purpose is to push out what is contained inside (i.e. the baby). Likewise, the direction of the valsalva-pushing maneuver is also downward toward the birth canal. If the force of a labor contraction with pushing were equally distributed in all directions within the uterus, the baby would not move. Thus, the amount of force that is directed downward through the birth canal is 6 to 8 times greater than the force that would be pushing upward on the wall of the uterus in the fundus. This equates to more than 100 pounds of force, which explains why injuries can occur. Finally, throughout this article we have used the words brachial plexus injury and Erb’s palsy. The brachial plexus is a network of nerves that was briefly discussed at the beginning and includes the nerves that are located in the neck from C-5 to T-1. For clarification purposes, an Erb’s palsy is defined as an injury to the nerve fibers of C-5 and C-6, and mainly involves the mobility of the shoulder. A Klumpke’s palsy is defined as injury to nerve fibers C-8 and T-1 and involves the mobility of the hand. The C-7 nerve fibers primarily innervate the triceps muscle. Though these explanations have been simplified and generalized, one should know that the C-5 through T-1 nerve fibers intermix with each other and the extent of immobility will vary from injury to injury. For completion purposes, the C-4 nerve fibers innervate the diaphragm and if this is damaged, the baby will often have significant problems with respiration. Also, there are sympathetic nerve fibers that come off the lower cervical / upper thoracic nerve roots and these fibers return back up to innervate portions of the face and eyelid. If these nerves are injured, Horner’s syndrome with a drooping eyelid might be seen. Conclusion In conclusion, shoulder dystocia cannot be accurately predicted nor prevented. Therefore, delivering healthcare providers need to be prepared in handling these obstetrical emergencies when they occur. Likewise, nothing can be done to prevent the brachial plexus nerve injuries that occur in cesarean section births or deliveries with no shoulder dystocia. Therefore, protocols that involve shoulder dystocia deliveries will only have the potential of impacting half of the brachial plexus cases that occur. Because these injuries can occur in deliveries without a shoulder dystocia, if a baby sustains a brachial plexus injury in a delivery complicated by shoulder dystocia, this does not mean that excessive traction was utilized. With that said, being prepared for shoulder dystocia is good medicine. Preparation: 1. Perform an estimated fetal weight, document this, and discuss options with the patient if there is a belief that macrosomia (> 4500 grams) might exist. 2. Observe the length of the second stage of labor and do not hesitate to ask for more help at the time of delivery, especially if the decision is made to use forceps or a vacuum. 3. If forceps or vacuum are utilized, have a recognizable indication and be sure that all of the requirements are met (completely dilated, engaged head at > +2 cm station). 4. If a vaginal delivery attempt is made on a patient with diabetes (especially one with insulin dependence that is poorly controlled), again do not hesitate to ask for more help at the time of delivery (regardless of the estimated fetal weight). 5. When a shoulder dystocia is encountered – call for help – both obstetrical and pediatric. 6. Remember the maneuvers: McRoberts – hyper-flexing the legs back toward the mother’s abdomen; Apply suprapubic pressure; Rotational maneuvers – Rubin’s or Wood’s Delivery of the posterior arm 7. Avoid fundal pressure once the baby’s head delivers. An episiotomy may give more room for rotational maneuvers and / or delivery of the posterior arm. 8. Write a note of the maneuvers utilized and the position of the baby’s head at the time it delivered – remember these notes are for future healthcare providers to understand what occurred at the delivery. References or Suggested Reading: 1. Shoulder dystocia. ACOG Practice Bulletin; Number 40, November 2002. 2. Fetal macrosomia. ACOG Practice Bulletin; Number 22, November 2000. 3. Operative vaginal delivery. ACOG Practice Bulletin; Number 17, June 2000. 4. Evans-Jones G, Kay SPJ, Weindling AM, et al. Congenital brachial palsy: incidence, causes, and outcome in the United Kingdom and Republic of Ireland. Arch Dis Child Neonatal Ed 2003;88:F185-F189. 5. Raio L, Ghezzi F, DiNaro E, et al. Perinatal outcome of fetuses with a birth weight greater than 4500 g: an analysis of 3356 cases. Europ J Obstet Gynecol Reprod Bio 2003;109:160-65. 6. Gilbert AM, Nesbitt TS, Danielsen B. Associated risk factors in 1611 cases of brachial plexus injury. Obstet Gynecol 1999;93:536-540. 7. Shivvers S, McIntire D, Leveno K, et al. Risk of brachial plexus injury in shoulder dystocia deliveries by birthweight. Am J Obstet Gynecol 1998;178:S77. 8. Gherman RB, Ouzounian JG, Miller D, et al.. Spontaneous vaginal delivery: A risk factor for Erb’s plalsy? Am J Obstet Gynecol 1998;178:423-7. 9. Ecker JL, Greenberg JA, Norwitz ER, et al. Birth weight as a predictor of brachial plexus injury. Obstet Gynecol 1997;89:643-7. 10. Brown B, Karmin I, Lapinski R, et al. Dual mechanism responsible for brachial plexus injuries. Am J Obstet Gynecol 1997;176:S137. 11. Peleg D, Hasnin J, Shalev E. Fractured clavicle and Erb’s palsy unrelated to birth trauma. Am J Obstet Gynecol. 1997;177:1038-40. 12. Graham EM, Forouzan I, Morgan MA. A retrospective analysis of Erb’s palsy cases and their relation to birth weight and trauma at delivery. J Matern Fetal Med 1997;6:1-5. 13. Sandmire HF, DeMott RK. The Green Bay cesarean section study. AM J Obstet Gynecol 1996;174:1557-64. 14. Perlow JH, Wigton T, Hart J, et al. Birth trauma. A five-year review of incidence and associated perinatal factors. J Reprod Med 1996;41:754-60. 15. Lipscomb KR, Gregory K, Shaw K. The outcome of macrosomic infants weighing at least 4500 grams: Los Angeles County plus University of Southern California experience. Obstet Gynecol 1995;85:558-64. 16. Nocon JJ, McKenzie DK, Thomas LJ, et al. Shoulder dystocia: an analysis of risks and obstetric maneuvers. Am J Obstet Gynecol 1993;168:1732-9. 17. Jennett RJ, Tarby TJ, Kreinick CJ. Brachial plexus palsy: an old problem revisited. Am J Obstet Gynecol 1992;166:1673-7. 18. Gonik B, Hollyer VL, Allen R. Shoulder dystocia recognition: differences in neonatal risk for injury. Am J Perinatol 1991;8:31-4. 19. Levine MG, Holroyde J, Woods JR, et al. Birth trauma: incidence and predisposing factors. Obstet Gynecol 1984;63:792-5. 20. Walle T, Hartikainen-Sorri AL. Obstetric shoulder injury. Associated risk factors, prediction and prognosis. Acta Obstet Gynecol Scand 1993;72:450-4. 21. Ouzounian JG, Korst LM, Phelan JP. Permanent Erb palsy: A traction-related injury? Obstet Gynecol 1997;89:139-41. 22. Gherman RB, Ouzounian JG, Goodwin TM. Brachial plexus palsy: An in utero injury? Am J Obstet Gynecol 1999;180:1303-7. 23. Gonik B, Stringer CA, Held B. An alternative maneuver for management of shoulder dystocia. Am J Obstet Gynecol 1983;145:882-4. 24. Woods CE. A principle of physics as applicable to shoulder dystocia. Am J Obstet Gynecol 1943;45:796-804. 25. Rubin A. Management of shoulder dystocia. JAMA 1964;189:835-7. 26. Sandberg EC. The Zavanelli maneuver: a potentially revolutionary method for the resolution of shoulder dystocia. Am J Obstet Gynecol 1985;152:479-84. 27. Vollebergh JHA, van Dongen PWJ. The Zavanelli manoeuvre in shoulder dystocia: case report and review of the published cases. Europ J Obstet Gynecol Reprod Bio 2000;89:81-4. 28. Ouzounian JG, Korst LM, Ock Ahn M, et al. Shoulder dystocia and neonatal brain injury: significance of the head-shoulder interval. Am J Obstet Gynecol 1998;178:S76. 29. Chauhan SP, Sullivan CA, Lutton TD, et al. Parous patients’ estimate of birth weight in postterm pregnancy. J Perinatol 1995;15:192-4. 30. Lewis DF, Raymond RC, Perkins MB, et al. Recurrence rate of shoulder dystocia. Am J Obstet Gynecol 1995;172:1369-71. 31. Allen R, Sorab J, Gonik B. Risk factors for shoulder dystocia: an engineering study of clinician-applied forces. Obstet Gynecol 1991;77:352-5. 32. Gonik B, Walker A, Grimm M. Mathematic modeling of forces associated with shoulder dystocia: a comparison of endogenous and exogenous sources. Am J Obstet Gynecol 2000;182:689-91. About the Author: Dr. Towers is currently on a sabbatical writing a series of books that deal with the safety of over-the-counter drugs, herbal medications, and natural remedies used during pregnancy. The first book is in print entitled “I’m Pregnant & I Have a Cold – Are Over-the-Counter Drugs Safe to Use?” published by RBC Press, Inc. Before his sabbatical, Dr. Towers was an Associate Professor in the Department of Obstetrics and Gynecology at the University of California, Irvine. He also was the Director of Perinatal Medicine at Long Beach Memorial Women’s Hospital in Long Beach California. He has practiced clinically in the states of Kansas, California, and Wisconsin. Dr. Towers has multiple publications in peer review medical journals and he has given lectures on a wide variety of obstetrical and medical topics nationwide. Examination: 1. The overall incidence of shoulder dystocia is approximately ______ of all deliveries. A. 0.01% B. 0.1% C. 1% D. 3% E. 5% 2. Approximately ______ of the Erb’s palsies that are seen come from deliveries in which there was no shoulder dystocia. A. 5% B. 15% C. 25% D. 50% E. 65% 3. The incidence of Erb’s palsy is approximately about 1 in every ________ births. A. 6500 to 7000 B. 1000 to 1500 C. 650 to 700 D. 400 to 500 E. 150 to 200 4. There are two other compelling facts that verify the issue that most brachial plexus injuries are not caused by the delivering healthcare provider which are A. fundal pressure and a generous episiotomy B. C. D. E. cesarean section and the posterior arm the posterior arm and a generous episiotomy Rubin maneuver and fundal pressure diabetes and cesarean section 5. Several recent studies have now identified that approximately _______ of all Erb’s palsies are seen in the posterior arm of the baby. A. 1/10 B. 1/7 C. 1/5 D. 1/4 E. 1/3 6. The stretching of the nerves in a baby’s neck can occur in all of the following ways EXCEPT A. with excessive pitocin usage in the first stage of labor B. in utero prior to the onset of labor C. following the delivery of the head before any downward traction is applied D. following the normal amount of downward traction applied in normal deliveries E. with excessive traction in the face of a shoulder dystocia 7. The ability to accurately predict when a shoulder dystocia will occur is A. less than 0.5% B. less than 50% C. greater than 50% D. greater than 75% E. nearly 100% 8. The maternal pelvic shape that is most likely to predispose to a shoulder delivery, especially in the presence of a non-macrosomic baby is A. platypelloid B. android C. arthropoid D. gynecoid E. anthropoid 9. There are 2 basic warning signs that occur in labor that may suggest a shoulder dystocia could occur and these are A. diabetes and an estimated fetal weight of > 4000 grams B. epidural anesthesia and a prolonged first stage of labor C. an estimated fetal weight of > 4500 grams and the use of pitocin D. excessive maternal weight gain and a large fundal height E. a prolonged second stage of labor and the need for instrumentation 10. Which of the following statements accurately defines a prolonged second stage of labor according to ACOG? A. nulliparous woman at > 3 hours without regional anesthesia B. nulliparous woman at > 2 hours with regional anesthesia C. D. E. multiparous woman at > 2 hour without regional anesthesia multiparous woman at > 2 hours with regional anesthesia. multiparous woman at > 3 hours with regional anesthesia 11. All of the following definitions are true EXCEPT A. excessive maternal weight gain is defined as > 20 kilograms or 44 pounds B. a postterm pregnancy is defined as > 42 weeks gestation C. the basic requirements that need to be met when using a vacuum are different than the requirements that need to be met when using forceps D. a low pelvic delivery is defined as an engaged fetal head at > +2 cm station E. macrosomia is most commonly defined as > 4500 grams 12. A brachial plexus injury is about _______ times more likely to be seen in a shoulder dystocia vaginal delivery when compared to a non-shoulder dystocia vaginal delivery. A. 5 B. 25 C. 50 D. 75 E. 100 13. The maneuver that involves hyper-flexing the legs back toward the mother’s abdomen is called the A. Rubin’s B. Woods C. McRoberts D. Zavanelli E. cleidotomy 14. The maneuver that is most likely to result in a fracture of the baby’s humerus (if this fracture were to occur) is A. delivery of the posterior arm B. McRoberts C. Rubin’s D. Woods E. Zavanelli 15. Which of the following maneuvers is an heroic maneuver that should only be utilized if all the other recognized maneuvers are not successful A. Woods B. a generous episiotomy C. Rubin’s D. delivery of the posterior arm E. Zavanelli 16. Regarding an episiotomy, which of the following statements is true? A. It should be performed prior to the use of fundal pressure. B. This maneuver can result in the delivery of the baby in the case of a shoulder. C. It should be performed in order to facilitate the Zavanelli maneuver. D. E. It can allow more room for the operator’s hand to perform rotational maneuvers or delivery of the posterior arm. It will help minimize the amount of upward traction that is applied in order to deliver the posterior shoulder prior to the anterior shoulder. 17. Though very few studies exist on this topic, it appears that neonatal brain injury can begin to occur if the shoulder dystocia extends beyond ____ minutes. A. 2 B. 5 C. 9 D. 12 E. 15 18. Regarding the issue of a scheduled cesarean section for the purpose of preventing a shoulder dystocia, ACOG has recommended that it be considered if the estimated fetal weight exceeds _______ grams in a non-diabetic. A. 3500 B. 4000 C. 4500 D. 5000 E. 5500 19. The endogenous force of the uterus, especially when combined with the force of the mother’s valsalva pushing efforts is ________ than the exogenous force utilized in deliveries by the healthcare provider. A. 2 to 4 times greater B. 4 to 9 times greater C. 10 to 15 times greater D. 5 to 10 times less E. 3 to 5 times less 20. In general terms, an Erb’s palsy is defined as an injury to the nerve fibers of ______, and mainly involves the mobility of the shoulder. A C-5 and C-6 B. C-7 only C. C-7 and C-8 D. C-8 and T-1 E. C-4 only