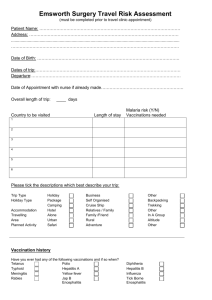
Travel Vaccinations and Information Form
advertisement

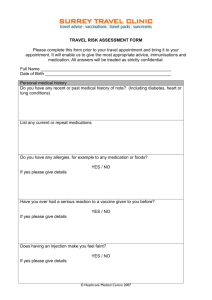
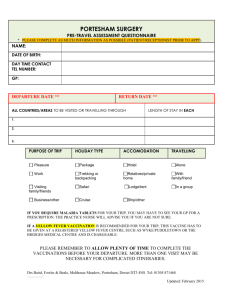
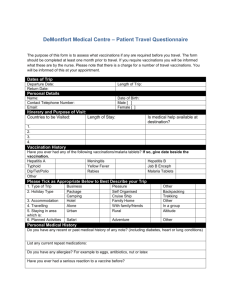
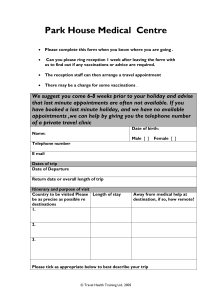
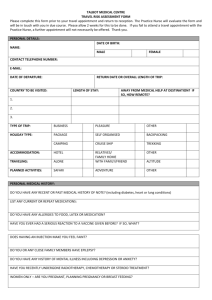
VICTORIA ROAD SURGERY 50 VICTORIA ROAD WORTHING BN11 1XE Telephone: (01903) 230656 Fax: (01903) 520094 Dr Birgit Woolley. Dr Jonathan Price. Dr Navdeep Sandhu. Dr Madeleine Babicki. Dr Mohammed Haque. Dr Rachel Butler. Dr Eugenie McCreanor. TRAVEL VACCINATIONS Vaccines are currently available for many infectious diseases. The immunity from vaccines is never immediate or total. As the vaccines may need several trips to the Practice you must plan your vaccinations well in advance of the trip, 4-6 weeks if possible. Please complete and return the attached travel vaccination form (complete one for each patient) to the Surgery at least THREE DAYS before your appointment with the Practice Nurse so they can check your requirements and order the vaccines needed. Unfortunately the NHS does not fund vaccinations for holidaymakers travelling abroad and they must be classed as part of the cost of the holiday, something people do not realise. At this Practice, we charge the fees that are recommended by the British Medical Association. The following vaccinations are available to patients of this Practice: VACCINE FEE Diphtheria/Tetanus/Polio (booster 10 years) Typhoid (booster 3 years) Hepatitis A (booster 6-12 months, then 20 years) free free free Rabies (course of 3 injections) Rabies booster (after 2 – 3 years) Hepatitis B (Course of 3 injections) Hepatitis B booster Yellow fever Meningitis ACWY (booster 5 years) Japanese Encephalitis (Course of 2 injections) (Ixiaro for over 18 years only) Japanese Encephalitis booster (after 1-3 years) Tick-Borne Encephalitis (course of 2 injections) Tick-Borne Encephalitis booster (after 3 years) Private Prescription for Malaria tablets for travel Price on application Price on application £77.00 £36.00 £75.00 Price on application Price on application Price on application Price on application Price on application £15 Payment for vaccinations must be made at the reception desk before seeing the Nurse and you will be given a receipt for payment, which must be in cash following the discontinuation of the cheque card guarantee system by banks in the UK. Vaccinations are also available at private travel clinics. The Sussex Travel Clinic: 01273 749100 www.sussextravelclinic.com OFFICE USE ONLY TRAVEL APPOINTMENT DATE & TIME: TRAVEL IMMUNISATION QUESTIONNAIRE PERSONAL INFORMATION Name: DOB: Address: Tel Number: Mobile Number: Email: What vaccinations have you had in the past? (Please fill in date if known) Yes/No Date last had NURSES USE ONLY Recommended Given Booster (date) due Tetanus Diphtheria Polio Typhoid Cholera Hepatitis A Yellow Fever Meningitis Rabies Hepatitis B BCG Tick Borne Encephalitis Japanese Encephalitis MMR Influenza Pneumococcal Other Anti Malarials TRAVEL INFORMATION When are you leaving: How long are you away for: Country to be Visited Exact Location or Region City or Rural Length of Stay TYPE OF TRAVEL AND PURPOSE OF TRIP – TICK ALL THAT APPLY Holiday Business Expatriate Volunteer Work Healthcare Worker Pilgrimage Medical Tourism Adventure Diving Visiting family / friends Hotel Stay Cruise Ship Safari Backpacking Camping / Hostels Are there any specific hazards associated with this holiday: ………………………… ………………………………………………………………………………………………. MEDICAL INFORMATION Yes Are you fit and well today Any allergies including food, latex, medication Severe reaction to a vaccine before Tendency to faint with injections Any surgical operations in the past, including e.g. your spleen or thymus gland removed Recent chemotherapy / radiotherapy / organ transplant Anaemia Bleeding / clotting disorder (including history of DVT) Heart disease (e.g. angina, high blood pressure) Diabetes Epilepsy / seizures Gastrointestinal (stomach) complaints Liver or kidney problems HIV / Aids Immune system conditions Mental Health issues (including anxiety / depression) Neurological (nervous system ) illness Respiratory (lung)disease Rheumatology (joint) condition Spleen problems Any other conditions WOMEN ONLY Are you pregnant Are you breast feeding Are you planning pregnancy while away No Details MEDICATION Are you currently taking any medication (including prescribed, purchased or a contraceptive pill ADDITIONAL INFORMATION Have you taken out travel insurance for this trip? Do you plan to travel abroad again in the future? Any additional information Signature: Date: CONSENT: There may be occasions when the Surgery needs to get in touch with you. It may be that the quickest form of contact is to phone you. By signing this consent you will be agreeing to us: leaving a message with a third party or on your voice mail sending you a text message to your mobile phone. No medical information will be left or disclosed. I the undersigned agree that messages may be left with a third party or my voice mail requesting that I make contact with the Surgery and that we can send you text messages: Signature: ………………………………………………………………………………………….. Print Name: ………………………………………………………………………………………. ESSENTIAL INFORMATION FOR TRAVELLERS FOOD, DRINK AND HYGIENE There are many diseases that are caught by eating contaminated food or by drink. These include travellers’ diarrhoea, hepatitis A, salmonella, typhoid and cholera. You can help avoid catching them by paying strict attention to food, drink and general hygiene. If in doubt about the water available for drinking, washing food or cleaning teeth boil it, sterilise it with disinfectant tablets, or use bottled water in sealed containers. Avoid both ice cubes and ice cream unless you are sure they are made from clean water. Avoid food which has been reheated, kept warm or exposed to flies. Avoid uncooked food – unless you peel it or shell it yourself. Eating shellfish – even cooked can be suspect. Remember that salads will be washed with untreated water. Avoid unpasteurised milk or boil it before use. Avoid fruit juice (if sold by a street vendor). Avoid eggs, mayonnaise and sauces. Avoid peeled fruit. Food and drink that are generally safe to eat include: sealed bottled water that is produced by a recognised international manufacturer cooked food, such as soup or stir-fry canned food or food in sealed packs fresh bread unpeeled fruit tea and coffee TRAVELLERS’ DIARRHOEA Dehydration following fluid loss from sweating, diarrhoea and fever if left untreated can kill. Any diarrhoea must be treated with liberal quantities of re-hydration fluid made up of the cleanest water available. Sachets of re-hydration salts are available without a prescription and should always be carried, especially with children. Seek medical advice if you have a temperature, on-going symptoms or blood is passed. MALARIA Many countries have insects and animals that pose potential threat to travellers. To avoid insect bites use insect repellent preparations and cover arms and legs. Malaria is a blood disease caused by a parasite which is caught from the bite of an infected mosquito. Whilst anti-malarial tablets can reduce the risk of catching malaria they are not 100% effective so it is essential that you take steps to avoid being bitten. Cover arms and legs, especially between dusk and dawn as malaria mosquitoes are most active at night. Use an insect repellent containing 50% DEET (Diethyltoluamide) they are very effective. Impregnated ankle and wristbands are also effective If your accommodation does not have insect screens or windows which close sleep under a mosquito net. If possible stay in air-conditioned accommodation. Use an insecticide to clear a room and a vaporiser to keep it clear. Mosquito nets are more effective if impregnated with insecticide such as permethrin. Take malaria tablets as instructed and you must finish the course. If you are pregnant or planning pregnancy or taking young children please ask the doctor or practice nurse for advice. Protection against malaria cannot be guaranteed and some strains of the disease have become resistant to medication. Tell your GP as soon as possible if you develop a fever or an unexplained illness while you are away or up a year later after your return. HEPATITIS B AND AIDS (HIV INFECTION) These can be caught by contact with infected body fluid (blood, saliva etc.) and from unprotected sex or drug abuse. These infections are world wide. Always practice safe sex, use a condom (in some parts of the world locally produced condoms may not be as reliable as the ones available in the UK ), and never share needles. You may be at risk in places where screening of blood products and sterilisation of medical equipment is inadequate. If unsure take a sterile medical kit with you. SUNBURN AND HEATSTROKE Ultraviolet light (UVA and UVB rays) is radiated by the sun. The ozone layer filters out most of the harmful UVA and UVB rays before they reach earth, but some rays are still able to get through and can cause skin damage. It is very important to take precautions when travelling to hot climates. Try not to get burnt – repeated sunburn can cause various skin diseases including cancer. Particularly take care of children and babies. A particular risk of overexposure to the sun is sunstroke or heatstroke caused by overheating. Avoid strenuous activity during the hottest hours and drink plenty of non-alcoholic drinks. Some useful tips for avoiding sunburn are listed below: Do not wait until your skin feels uncomfortable before taking preventative action. Defence is the best form of protection. Once your skin is burnt, the damage has already been done, so cover up with loose-fitting clothes. Make sure your legs and arms are covered. Tightly woven fabrics provide the best protection from the sun. Avoid direct exposure to sunlight when the sun is at its strongest. Remember that the sun can be strong during the early and late part of the day, so you still need to take adequate precautions if you go out in the sun in the morning or evening. Cover your arms and legs with clothes, wear a wide-brimmed hat and a pair of good-quality sunglasses, and apply plenty of sun lotion with the right skin protection factor (SPF) for your skin type. Always use a sun protection lotion with an SPF of at least 15. If you have very fair skin, use lotions with an SPF of up to 40. This is also the case for children, whose skin is very sensitive. Most skin damage caused by the sun occurs before the age of 18. Make sure that your entire body is covered by sun protection lotion. This includes your face, hands, feet and neck. The most vulnerable parts of your body are those that are not usually exposed to sunlight. Apply sun lotion at least 30 minutes before you go out in the sun. Reapply it every couple of hours because sweat and contact with clothing and towels will cause it to wear off. Reapply sun lotion immediately after swimming, even if your lotion is waterproof. Use waterproof sun lotion while swimming because UVA and UVB rays can penetrate through about a metre of water. Cloud and fog do not protect skin from ultraviolet rays. Cover up with clothing and use SPF 15 sun lotion, even on cloudy days. Wear a hat, and sunglasses that have UVA and UVB filters when you are in the sun. Ultraviolet rays can damage the retinas in your eyes, causing cataracts. Drink plenty of fluids, particularly after exercise. Isotonic drinks that replace the salt lost through sweating are ideal, but water is also sufficient. Avoid drinking alcoholic drinks when you are out in the sun. Keep a careful eye on any moles on your body and visit your GP if you notice any changes in their appearance. Signs to look out for are darkening of the mole, an increase in size, ragged edges, multiple colours within the mole, itchiness, redness and swelling or bleeding. INSURANCE AND ACCIDENTS Do not travel without insurance. Try to assess the potential risks of some of the more adventurous holiday activities before trying them. Remember that some activities will not be covered by standard holiday insurance. Be aware that your insurance will not be valid if you knowingly do not declare an existing medical condition. Accidents are the most common cause of holiday disasters. A European Health Insurance Card (EHIC) entitles you to free or reduced-cost medical treatment in a European Economic Area (EEA) country or Switzerland. The EEA includes all European Union countries as well as Iceland, Liechtenstein and Norway. The EHIC is usually valid for five years and covers any medical treatment necessary as a result of an accident or illness. The card entitles you to state-run medical services only, and you will be treated on the same basis as an 'insured citizen’ of the country you are visiting. This may not cover all the treatment and services you would usually get free of charge from the NHS, and you may have to contribute to the cost of your care. The EHIC is not a substitute for travel insurance and you should take out a private travel insurance policy before you travel. AIR TRAVEL There is some evidence that long haul flights, especially when passengers have little or no exercise, may increase the risk of developing DVT (Deep Vein Thrombosis). While it is difficult to be certain what the exact causes of travel-related DVT are, experts agree that lack of exercise or immobility are major underlying risks. The signs of a DVT are that you may get swelling, pain, tenderness and redness especially at the back of the leg below the knee. This is different from the ankle swelling that many people get during long-haul flights, and DVT usually, though not always, affects only one leg. These complaints may develop during the journey but more commonly hours or even days later. If you get any signs please seek medical opinion. You can minimise the risk by doing the following: Wear flight socks Get comfortable in you seat and reline as much as possible. Bend and straighten your legs, feet and toes while seated every half-hour or so during the flight Press the balls of your feet down and hard against the floor or foot-rest to increase the blood flow in you legs and reduce clotting Do upper body breathing exercises to further improve circulation Take occasional short walks around the cabin whilst cruising at altitude Where possible during refuelling stopovers get off the plane and walk about Drink plenty of water and avoid alcohol which in excess leads to dehydration and immobility Avoid taking sleeping pills Travel health information is available from: The Travel Health Section of the nhs web site www.nhs.uk www.masta-travel-health.com www.fitfortravel.nhs.uk www.malariahotspots.co.uk www.nathnac.org