10-1
Mallory Ditchfield
N00881902
MNT1- 81395
11/13/14
Case Study #3: Irritable Bowel Syndrome (IBS)
1.
IBS is considered to be a functional disorder. What does this mean? How does this relate to Mrs. Clarke’s
history of having a colonoscopy and her physician’s order for a hydrogen breath test and measurements of
anti-tTG? (3 points)
A functional disorder is a certain issue where the body’s normal role or duties are disrupted, but the
disruptions cannot be seen by x-ray, endoscopy, or even blood tests. Since there are no structural
abnormalities in the body that can hold evidence to a disorder, functional-type disorders are diagnosed or
identified by certain types and frequencies of symptoms.1 Functional disorders, like irritable bowel syndrome
(IBS), can cause disturbances and limitations to daily activities. IBS can be defined as an assortment of bowel
disorders distinguished by abdominal distress or pain associated with defecation or a change in bowel habit.2
The colonoscopy listed in her history was ordered to rule out any other types of disorders that might be
the cause of her discomfort. Colonoscopies are necessary to view any damage such as ulcers, inflammation,
or bleeding in the large intestine.2
A hydrogen breath test was ordered by the physician to measure, as it states, the amount of hydrogen
expelled in the breath. This test can help diagnose conditions that have side effects of gastrointestinal
irritation. An elevated amount of hydrogen detected is evidence that the bacteria in the GI tract are being
exposed to unabsorbed food, particularly sugars and carbohydrates. 3 The presence of lactose intolerance can
be detected by the hydrogen breath test. Also, small intestinal bacterial overgrowth (SIBO) may be the cause
of elevated hydrogen in the breath. This elevated level is seen in 22%-54% of individuals with IBS. Because
the symptoms of IBS overlap with SIBO, it has been found that many patients with IBS may have underlying
SIBO.4
Anti-tTG (anti-transglutaminase) measurements can be used in the diagnosis of celiac disease.5 The
occurrence of celiac disease has been reported to be four times greater in individuals diagnosed with IBS than
in individuals without IBS.4 Along with that, it has also been reported that approximately 3% of patients with a
“clinical” presentation of IBS were subsequently diagnosed with celiac disease. 6
2.
What are the ACG and the Rome III criteria? Using the information from Mrs. Clarke’s history and physical,
determine how Dr. Cryan made her diagnosis of IBS-D. (2 point)
The American College of Gastroenterology, or ACG, advances in gastroenterology and strives to improve
patient care. There are more than 12,000 GI professionals worldwide that represent the ACG. These expert
members develop new guidelines on gastrointestinal and liver diseases. They base their findings and
guidelines strictly off of evidence-based research and medicine.7
The Rome criteria is a system developed to classify the functional gastrointestinal disorders. 8 Diagnosis of
IBS is based on international consensus criteria, or Rome criteria, and diagnostic algorithms that help separate
other medical or surgical disorders that have similar symptoms. Based on the Rome criteria, abdominal
discomfort or painful symptoms must occur for at least three days each month for the past three months.
Also, the patient must be experiencing at least two of these three indicators: discomfort relieved by
defecation, onset associated with a change in frequency of stool, and onset associated with a change in form
of stool.4
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-2
In order to properly diagnose the patient with irritable bowel syndrome, the physician must refer back to
the ACG and Rome III guidelines. Once the patient meets specified criteria, the physician can be fully
confident with his/her verdict.
Mrs. Clarke stated in her onset of disease history that she has been experiencing diarrhea and
constipation for many years, with ongoing abdominal pain almost every day. This meets the Rome III criteria
of length and frequency of pain and discomfort. She has also stated that she has been experiencing more
bouts of diarrhea in recent months and it is constantly becoming more frequent- stating several episodes per
day. These symptoms all meet the Rome III criteria for IBS-D (diarrhea predominant.) Other factors that lead
to this diagnosis could be her colonoscopy results. Her results came back negative for active disease, thus
pointing to a functional disorder such as IBS.
3.
Discuss the primary factors that may be involved in IBS etiology. You must include in your discussion the
possible roles of genetics, infection, and serotonin. (3 points)
Since IBS is a functional disorder that is based on a variety of symptoms, the etiology will vary. Although
diet, psychological factors, infection, and environmental exposures may cause IBS symptoms, there is no one
answer to the problem. The specific cause of IBS is still unknown. Proposed etiological factors may be studied
in the framework of what is already known about the normal physiology of the gastrointestinal tract.9
In certain cases, an increased sensitivity to specific foods may activate IBS symptoms. There are
numerous reports of food-induced aggravation of IBS with an improvement after elimination of those foods in
the diet.6
IBS has been shown to cluster in families and affect several generations. Genetics may play a role in IBS in
relation to having a strong family history of an allergy or hypersensitivity to certain foods. These factors may
promote or agitate the symptoms.4 Relatives of an individual with IBS are two to three times as likely to have
IBS (both genders affected.)10 This data does not take into consideration that a family as a whole may be
exposed to the same environmental exposures that can cause IBS such as poor nutrition, abuse, or even stress
in the household.
Some evidence suggests that an infection may cause the initial gastrointestinal disturbance and that
tissue sensitization persists after the infection dissipates.11 Post-infectious IBS typically appears abruptly after
gastroenteritis and is essentially managed with the same approach as other forms of IBS.
IBS is commonly described as a “brain-gut disorder” because of the association with serotonin. The
enteric nervous system found in the gut is very similar to the brain. This system sends and receives impulses,
records experiences, and responds to emotions. The nerve cells in the gut are influenced by the same
neurotransmitters found in the brain. The neurotransmitter serotonin can also be found in the gut. If
serotonin is over stimulated, the automatic motion of peristalsis begins.12 This activity can cause diarrhea,
constipation, and discomfort. The mediators of gastrointestinal responses may be abnormal secretion of
peptide hormones or signaling agents such as neurotransmitters secreted in response to the hormones. 4
Leading a stressful life can be a main factor when diagnosing IBS. Also, antidepressant medications like
selective serotonin reuptake inhibitors (SSRI) increase serotonin levels, promoting the same issues.12
4.
Mrs. Clarke’s physician prescribed two medications for her IBS. What are they and what is the proposed
mechanism of each? She discusses the potential use of Lotronex if these medications do not help. What is this
medication and what is its mechanism? Identify any potential drug–nutrient interactions for these
medications. (3 points)
The physician has prescribed the medication Elavil (25mg/day) which is a tricyclic antidepressant. Since
Mrs. Clarke meets the criteria of diarrhea-predominant IBS, a low dose of a trycyclic antidepressant can
decrease her symptoms. This type of antidepressant will not promote diarrhea unlike other types such as
SSRI’s mentioned in the previous question.13 Tricyclic antidepressants (in low doses) have also been shown to
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-3
reduce discomfort in some cases.4 Low doses of antidepressants are known to block signals of pain to the
brain. This type of antidepressant can, however, can cause dry mouth, a sour or metallic taste, and even
blurred vision.13
Mrs. Clarke was also order the supplementation Metamucil (1 tbsp, 2x/day). Metamucil is a fiber
supplement that can be used to help relieve some symptoms of IBS. Metamucil can help increase the bulk in
stool when ingested in the correct dosage.4
The physicians at the American College for Gastroenterology found that Lotronex can be successful for
treatment of all symptoms related to IBS-D, including abdominal pain, discomfort, urgency, and diarrhea itself.
These results, though, were only found to be significant in female patients. Lotronex works to block
serotonin's effect on the digestive system. Lotronex is able to slow down the colon and reduces the frequency
of bowel movements. Unfortunately, there is a high risk of side effects that may cause serious complications
while taking this medication. Due to these severe risks, this medication is strictly approved for women with
severe IBS-D who have not responded to other treatments. 13
5.
6.
For each of the following foods, outline the possible effect on IBS symptoms. (2 point)
a.
lactose: A simple carbohydrate that causes frequent gas and/or painful bloating. The existence of lactose
indigestion does not automatically mean that it is a cause of IBS, but there is a possibility that the
intolerance can coexist with IBS.9
b.
fructose: A simple carbohydrates that causes gas and bloating.9
c.
sugar alcohols: May cause or worsen diarrhea in patients with IBS or IBS-D.2
d.
high-fat foods: Can cause discomfort, diarrhea, and abdominal cramping.2
What is FODMAP? What does the current literature tell us about this intervention? (2 point)
FODMAP is an acronym that stands for fermentable oligo-, di-, and monosaccharide’s and polyols. These
foods are not well digested and contribute to fermentation which leads to the abdominal discomfort
associated with IBS. A diet low in these saccharides and sugar alcohols has been shown to reduce
gastrointestinal symptoms in patients with IBS.
This diet limits foods that contain fructose, lactose, fructo- and galactooloigosaccharides, and sugar
alcohols. Food sources of FODMAPs are certain fruits such as stone fruits, fruits with high sugar content, dried
fruit, fruit juice, fruit pastes, and fructose as an added sweetener. Honey, coconut, fortified wines, certain
vegetables (onion, leek, asparagus, cabbage), legumes, wheat, and artificial sweeteners are also sources of
FODMAPs.4,9
7.
Define the terms prebiotic and probiotic. What does the current research indicate regarding their use for
treatment of IBS? (2 point)
Foods with fiber, resistant starches, and oligosaccharides may serve as prebiotic foods, which favor the
maintenance of healthy microflora and resistance to pathogenic infections. Probiotics and prebiotics will
increase the amount of short-chained fatty acids produced. In recent studies, short-chain fatty acids have
shown positive results in the absorption of water and electrolytes, thus, reducing the occurrence of diarrhea.
Other research has been conducted illustrating the improvement of mucosal defense in the GI tract when
supplementing with probiotics, along with reducing the growth of other harmful bacteria.
Potential benefits of prebiotics may be shadowed by poor absorption. Some probiotic supplements may
offer benefits in IBS. In larger studies, probiotics have demonstrated improvement for the symptoms of
bloating and gas production. Adding probiotic foods/supplements may be beneficial within the general
nutrition therapy plan, but not as a substitution to conventional medicine. 9 Unfortunately, current results of
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-4
initial studies on the use of prebiotic and probiotic supplements with IBS have been mixed; more studies are
needed.
8.
Assess Mrs. Clarke’s weight and BMI. What is her desirable weight? (3 points)
Current Weight: 191 lbs./86.6 kg
Height: 5’5”/1.65 m
BMI9: kg/m2
[86.6/(1.65)2]= 31.8
%IBW11: (current weight/ideal weight) X 100
(191/132) X 100= 144.7%
Mrs. Clarke’s current weight is 191 lbs. Based on the BMI calculation of 31.8, she is considered obese. Obesity
in adults is often defined as having a body mass index of 30 or higher.9 Mrs. Clarke’s percent ideal body
weight (%IBW) has calculated to 144.7%. To assess desirable weight, the individual’s current weight is
compared with an ideal weight calculated from a BMI table. In adults, the midpoint for a healthy BMI is
approximately 22; the weight found at this range is used. For a woman of her height, a BMI of 22 yields
roughly 132 lbs. Her %IBW of 144.7% places her at an increased nutritional risk since she is almost 50% over
her desirable weight.11
9.
Identify any abnormal laboratory values measured at this clinic visit and explain their significance for the
patient with IBS. (3 points)
Upon reviewing Mrs. Clarke’s lab values, I found some test results with slight elevation: glucose is 5 mg
over the suggested range; cholesterol is 2 mg over the suggested range; A1C test showing a 0.9% elevation
based on the normal range. The greatest abnormal lab value it her triglyceride levels. For an adult female, the
suggested range is between 35 and 135 mg/dL. Mrs. Clarke’s triglyceride values resulted with 171 mg/dL.
When assessing current evidence-based research, it is concluded that these lab values do not have any
high significance to an IBS patient. What her lab values do show, however, is her obesity level. Her glucose is
slightly elevated, along with her A1C test placing at high risk for prediabetes. 11 Her obesity is a reflection of
her eating habits, and this is displayed in these elevated lab results.
10. List Mrs. Clarke’s other medications and identify the rationale for each prescription. Are there any drug–
nutrient interactions you should discuss with Mrs. Clarke? (3 points)
Omeprazole (50mg/2xday): Prilosec: Proton pump inhibitor (PPI). PPI’s block the H+, K+-ATPase enzyme
which is a factor in HCL production.9 Mrs. Clarke is prescribed this medicine to control her gastroesophageal
reflux disease (GERD). Approximately 40% of IBS patients have GERD symptoms, therefore PPI therapy is
familiar in IBS patients.14 Long term use for medications for GERD may impair calcium absorption and iron and
B12 status.9 In certain clinical trials, omeprazole may have been a contributor to decreased levels of
magnesium and sodium. Omeprazole/Prilosec should not be taken at the same time as other medications.15
Levothyroxine (25mg): Mrs. Clarke was prescribed this medication due to her hypothyroidism. This is a
condition where the thyroid gland does not produce enough thyroid hormone. Levothyroxine influences
growth and maturation of tissues, is involved in normal growth and metabolism and development, along with
producing stable levels of T3 and T4. There is a decreased absorption rate with iron, calcium, and magnesium
when taking this medication. Decreased absorption is also reported with high-fiber foods.9
Lomotil (prn): Patients with IBS-D might benefit from an antidiarrheal agent such as Lomotil. These types
of medications aid by decreasing motility and increasing consistency of the stool. 9 There is a moderate
interaction with Lomotil and alcohol consumption. The combination results in dizziness, drowsiness, and
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-5
decreased mental alertness. Since Mrs. Clarke consumes alcohol three to four times a week, this
drug/nutrient interaction will need to be discussed. 16
11. Determine Mrs. Clarke’s energy and protein requirements. Be sure to explain what standards you used to
make this estimation. (3 points)
The DRI committee has formatted an isolated set of equations for calculating energy requirements in
individuals that are overweight or obese.
Total Energy Expenditure (TEE) for obese females aged 19 years and older 9:
TEE= 448 – 7.95 X age + PA X (11.4 X weight + 619 X height)
TEE= 448 – 7.95 X 42 + 1.16 X (11.4 X 86.6 + 619 X 1.65)= 2,280.65
RDA for Protein9: 0.8g per kg body weight
0.8 X 86.6= 69.28g
Since Mrs. Clarke leads a sedentary life with little exercise, her need for protein is reduced.
12. Assess Mrs. Clarke’s recent diet history. How does this compare to her estimated energy and protein needs?
Identify foods that may potentially aggravate her IBS symptoms. (3 points)
In order to estimate Mrs. Clarke’s usual intake of calories, I used the USDA’s Choose My Plate food
tracker.17 Based on her reported intake for the past several months, she consumes approximately 2,000
calories each day. This is just below her TEE that was calculated in the previous question. Her diet is high in
refined grains and empty calories. Unfortunately, her diet is also exceedingly high in common IBS food
triggers. Her RDA for protein calculated to be ~70g per day. Based on her usual daily intake, she is meeting
her requirements with roughly 75g.
Mrs. Clarke’s intake of 2-3 cups of coffee for breakfast and diet Pepsi at lunch may be exacerbate her
gastrointestinal symptoms. Caffeine has been shown to have negative effects in people suffering with IBS.
Also, her consumption of alcohol could be creating the same painful contributions. 11
Other foods in her diet that are familiar triggers for IBS: peaches and cherries (stone fruits), dried fruit,
wheat-based breakfast cereal, asparagus, kidney beans, lentils, wheat pasta, wheat/white bread, wheat-based
cookies, cakes and crackers, and artificial sweeteners.
13. Prioritize two nutrition problems and complete the PES statement for each. (5 points)
Altered GI function related to suspected IBS-D as evidenced by recurrent abdominal pain/discomfort for
at least 6 months, symptoms experienced on at least 3 days of at least 3 months, alternating constipation
and diarrhea, and predominant diarrhea with several episodes per day.
Poor nutrition choices and intake related to lack of knowledge as evidenced by BMI in obesity range, usual
intake from dietary recall, and frequent ingestion of IBS-triggering foods.
14. The RD that counsels Mrs. Clarke discusses the use of an elimination diet. How may this be used to treat Mrs.
Clarke’s IBS? (2 point)
Given that Mrs. Clarke is consuming many of the common IBS generating foods, an elimination diet is
vital in pin-pointing those certain foods. A traditional elimination or exclusion diet removes all possible foods
related to the patient’s symptoms. Once the foods are removed, they are slowly added back within a certain
time period. Once these foods are being eaten again, if the patient experiences no added symptoms these
foods can be categorized as non-IBS triggering foods and are acceptable in the diet. 9
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-6
15. The RD discusses the use of the FODMAP assessment to identify potential trigger foods. Describe the use of
this approach for Mrs. Clarke. How might a food diary help her determine which foods she should avoid? (2
point)
Since FODMAP foods are not well digested and contribute to fermentation, abdominal distress and pain
may arise. A FODMAP assessment to identify potential trigger foods in Mrs. Clarke’s diet may help alleviate
certain symptoms. Fermentable oligo-, di-, and monosaccharides, and polyols consumed on a regular basis
are potential triggers for IBS and they are recurrent in Mrs. Clarke’s diet. Fruits with high sugar content and
stone fruits, dried fruit, wheat-based breakfast cereal, asparagus, kidney beans, lentils, wheat pasta,
wheat/white bread, wheat-based cookies, cakes and crackers, and artificial sweeteners are all common in her
diet and are all FODMAP foods.
Keeping a food diary and writing entries each day can help determine what foods, habits, or
environmental factors are causing her symptoms. Logging foods eaten with symptom levels after each meal is
necessary to the food diary. It might also be helpful to add energy levels and moods throughout the day.
Once a certain food is eliminated, it is important to write down how she is feeling immediately after, and
possibly the day after. After a week or so, if she is still experiencing no signs or symptoms after that food was
eliminated, the food can be labeled in the diary as a non-triggering food.
16. Should the RD recommend a probiotic supplement? If so, what standards might the RD use to make this
recommendation? (2 point)
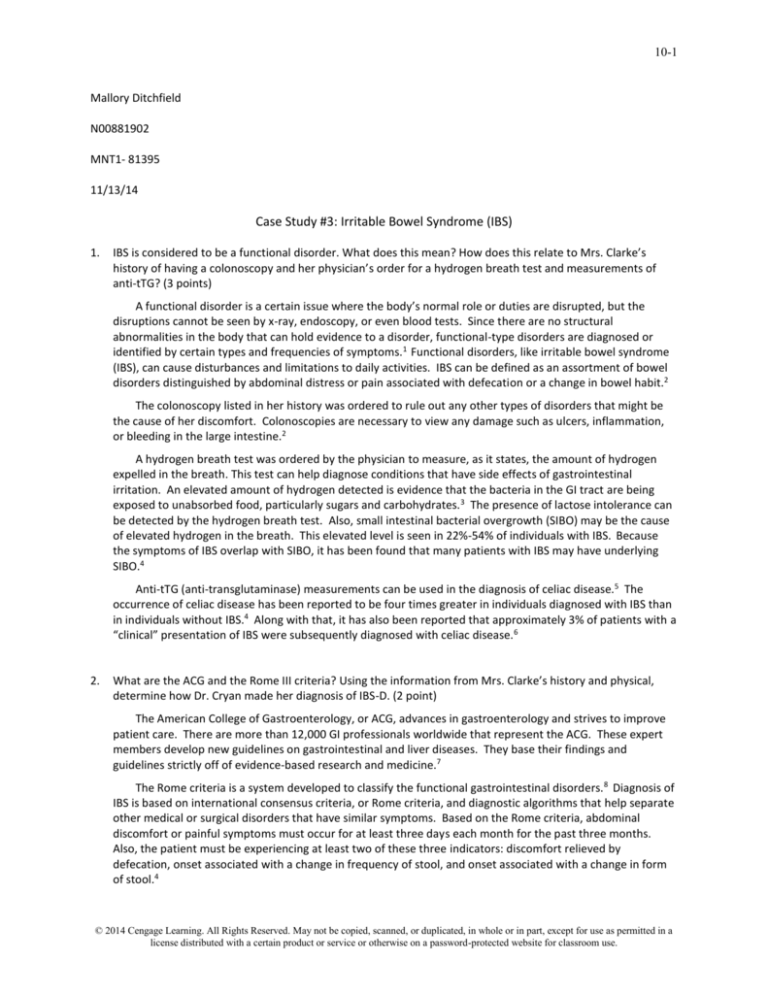
Probiotics, when compared against a placebo, show an improvement in IBS symptoms. These studies
illustrate a decrease in abdominal distress, bloating, and gas. The two strains, Bifidobacterium and
Lactobacillus, have both been studied for their impending use in prevention and management of IBS. 18 One
study found that probiotic treatment significantly improved IBS symptoms along with an enhanced quality of
life. The researchers mainly used the bacteria Lactobacillus acidophilus and Bifidobacteria infantis. The
results showed that these improvements and positive effects began to occur after taking the probiotics
consistently over a four week period.13
Based on the patient and their specific type of gastrointestinal disorder, probiotics can be of some
assistance to discomfort in the abdominal region. Adding probiotics may be beneficial within the overall
nutrition plan. It is necessary, first, to ensure the patient does not have an intolerance to lactose. Since the
presence of lactose indigestion causes similar discomfort, it is important to note that lactose intolerance is not
the cause of IBS, but the two can co-exist.9
17. Mrs. Clarke is interested in trying other types of treatment for IBS including acupuncture, herbal supplements,
and hypnotherapy. What would you tell her about the use of each of these in IBS? What is the role of the RD
in discussing complementary and alternative therapies? (2 point)
Since stress has been shown to complicate or increase symptoms of IBS, behavioral therapy might be a
suitable alternate route when considering treatment. Behavioral therapy includes a long list of different
methods and practices to better understand how to cope with stress, pain, and uncomfortable situations.
These strategies can help improve symptoms in patients suffering with IBS. Relaxation therapy, hypnotherapy,
cognitive behavioral therapy, and psychotherapy are all suggested options when considering this form of
management. It might be helpful to the client to suggest other forms of complementary or alternative
therapies. These may be found in meditation, exercise, having an ample amount of sleep, or even becoming
involved in enjoyable activities.13
Other alternative therapies, such as acupuncture and herbal supplements, have not yet been scientifically
proven to show any effectiveness in the treatment for IBS. Some smaller-scale studies have been done in
relation to acupuncture and IBS, resulting in a positive effect on quality of life. Regardless of this information,
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-7
there is still no medical or science-based evidence that would qualify this as a successful alternative therapy.15
I would not disapprove of the clients use of acupuncture, but I would reiterate the lack of evidence-based
research behind it.
Herbal remedies and supplementation are very popular among people suffering with IBS. The majority of
research regarding herbal use has taken place in China. Unfortunately, the studies done are of meager quality
and show very limited and weak evidence. However, peppermint oil (an antispasmodic9) was studied and has
proven useful in relieving some symptoms such as abdominal discomfort caused by bloating and gas. 14 If the
client showed interest in herbal remedies, I would explain the current research for that specific herb and base
my suggestions off of the studies. If the client were to ask which herbal supplementation I would suggest,
based on the evidence, I would most likely recommend the supplementation of peppermint oil or tea.
The role of the RD when discussing the use of these alternative choices is, simply, to counsel and make
recommendations to the client. It is important to be non-judgmental in this type of setting and to back up any
suggestions with evidence. If a client spoke of interest in complementary and alternative medicines, it is
important to discuss each alternate choice individually. Coaching is needed to help educate the client on the
reason for use or non-use, dosage information, and any safety concerns or interactions. Registered Dieticians
should be in the know and fairly knowledgeable in regards to the more common types of complementary and
alternative medicines/therapies in order to fully advise the client/patient.
18. Write an ADIME note for your initial nutrition assessment with your plans for education and follow-up. (5
points)
Assessment:
42 year old female, gastrointestinal discomfort with constipation and diarrhea, history of hypothyroidism,
GERD, and obesity. Height 5’5”, weight 191 lbs., BMI 31.8, obesity I. Patient is a divorced kindergarten teacher
who lives with her two children and mother. She eats three meals a day with snacks (cookies, cakes, dried
fruit and nuts), and visits restaurants/take-out once per week. Drinks diet soda often and alcohol three to
four times a week. Meals usually consist of a meat source (mostly chicken), a starch, and vegetables with a
dinner roll. Low activity level.
Diagnosis:
Altered GI function related to suspected IBS-D as evidenced by recurrent abdominal pain/discomfort for at
least 6 months, symptoms experienced on at least 3 days of at least 3 months, alternating constipation and
diarrhea, and predominant diarrhea with several episodes per day.
Also, many undesirable food choices and intake related to lack of knowledge as evidenced by nutrition history,
BMI in obesity range, usual intake from dietary recall, and frequent ingestion of IBS-triggering foods.
Intervention:
Provided basic education on IBS symptoms, triggers, eating smaller meals, and common nutrition in relation to
her diet high in refined grains, sugar, alcohol, and sodium. Introduced the use of elimination/exclusion diet
with a food diary. Patient will use information given in our sessions to adjust her diet and also begin to
eliminate the triggering foods discussed. Will return in three weeks with food diary to assess progress.
Monitoring and Evaluating:
Will monitor patient’s weight, intake, and clinical symptoms in response to elimination diet. Lab values may
also be monitored if necessary. Food diary will continue until the patient can gain a better understanding of
what triggers her symptoms (also will keep on hand for records). Will keep up with education and assistance
for any new questions or problems with the patient that may arise in the future.
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.
10-8
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
International Foundation for Functional Gastrointestinal Disorders. Functional GI Disorders. Available at:
http://www.iffgd.org/site/gi-disorders/functional-gi-disorders/. Accessed on: November 10, 2014.
International Foundation for Functional Gastrointestinal Disorders. About Irritable Bowel Syndrome.
Available at: http://www.aboutibs.org/. Accessed on November 10, 2014.
Medicine Net. Hydrogen Breath Test. Available at:
http://www.medicinenet.com/hydrogen_breath_test/article.htm. Accessed on: November 10, 2014.
Krause’s Food and Nutrition Therapy, 13th Edition. Mahan K, Escott-Stump S. Elsevier/Saunders, 2012.
PubMed. Role of anti-transglutaminase (anti-tTG), anti-gliadin, and anti-endomysium serum antibodies in
diagnosing celiac disease: a comparison of four different commercial kits for anti-tTG determination.
Available at: http://www.ncbi.nlm.nih.gov/pubmed/11344524. Accessed on: November 10, 2014.
National Center for Biotechnology Information PMC. Between Celiac Disease and Irritable Bowel
Syndrome: The “No Man’s Land” of Gluten Sensitivity. Available at:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3480312/. Accessed on: November 11, 2014.
American College of Gastroenterology. Membership and Clinical Guidelines. Available at: http://gi.org/.
Accessed on: November 12, 2014.
Rome Foundation. Rome III Disorders and Criteria. Available at: http://www.romecriteria.org/criteria/.
Accessed on: November 11, 2014.
Nutrition Therapy and Pathophysiology Nelms M, Sucher K, Long S. Thomson/Wadsworth, Australia, Third
Edition, 2010- 2011.
National Center for Biotechnology Information PMC. The Role of Genetics in IBS. Available at:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056499/. Accessed on: November 10, 2014.
Rolfes SR, Pinna K, Whitney E. Understanding Normal and Clinical Nutrition, 8 th ed. Cengage Learning;
2011.
PubMed. Enteric nervous system, serotonin, and the irritable bowel syndrome. Available at:
http://www.ncbi.nlm.nih.gov/pubmed/17031157. Accessed on: November 10, 2014.
WebMD. Treating Irritable Bowel Syndrome (IBS) and Diarrhea. Available at:
http://www.webmd.com/ibs/treating-diarrhea?page=2. Accessed on: November 10, 2014.
Medscape. Proton Pump Inhibitors, Irritable Bowel Syndrome, and Small Intestinal Bacterial Overgrowth.
Available at: http://www.medscape.com/viewarticle/723772. Accessed on: November 12, 2014.
Rx List. Prilosec. Available at: http://www.rxlist.com/prilosec-drug/side-effects-interactions.htm. Accessed
on: November 12, 2014.
Drugs.com. Lomotil (atropine / diphenoxylate) and Alcohol / Food Interactions. Available at:
http://www.drugs.com/food-interactions/atropine-diphenoxylate,lomotil.html. Accessed on: November
12, 2014.
Choose My Plate. Super Tracker. Available at: https://www.supertracker.usda.gov/foodtracker.aspx.
Accessed on: November 12, 2014.
NIH, National Center for Complementary and Alternative Medicine (NCCAM). Irritable Bowel Syndrome
and Complementary Health Practices. Available at:
http://nccam.nih.gov/health/digestive/IrritableBowelSyndrome.htm. Accessed on: November 11, 2014.
© 2014 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in a
license distributed with a certain product or service or otherwise on a password-protected website for classroom use.