Sweat-gl-handout
advertisement

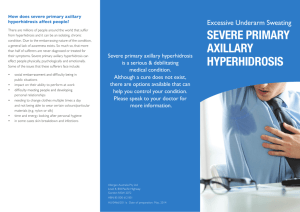
SWEAT GLANDS DISORDERS Prof. Ihab Younis There are between 2 and 4 million sweat glands found across the human body. There are two types of sweat glands, eccrine sweat glands and apocrine sweat glands. ECCRINE GLAND DISORDERS HYPERHIDROSIS (Excessive production of sweat) Types 1- Generalized hyperhidrosis:Affects the whole body 2- Localized hyperhidrosis:Usually affects the palms, soles, and/or axillae Etiology I-Generalized hyperhidrosis: Neurologic diseases eg Parkinson’s disease Metabolic disorders or processes (eg thyrotoxicosis, diabetes, hypoglycemia, gout, menopause Febrile illnesses Use of medications (eg, propranolol, pilocarpine, tricyclic antidepressants) Chronic alcoholism Hodgkin disease or tuberculosis (in nocturnal hyperhidrosis) II-Localized hyperhidrosis Emotional hyperhidrosis:occurs mainly on palmoplantar and axillary areas. Mental activity even devoid of any clear emotional content may provoke sweating Gustatory hyperhidrosis:Sweating on the lips, forehead and nose after eating certain foods especially hot spicy foods. It may be physiologic but also occurs in areas with damaged sympathetic nerves eg after parotid surgery Hyperhidrosis with cutaneous disease: Increased sweating may occur in the region of : Glomus tumor, and blue rubber bleb nevus Clinically Visible signs of hyperhidrosis are clearly evident Investigations Thyroid function tests may reveal underlying hyperthyroidism or thyrotoxicosis Blood glucose levels may reveal diabetes mellitus or hypoglycemia Uric acid levels may reveal gout A purified protein derivative (PPD) test can be performed to screen for tuberculosis Treatment I-Eccrine duct blocking agents: 1-20% aluminum chloride in absolute anhydrous ethyl alcohol (Drysol ) is the most effective topical agent. It should be applied nightly on dry skin with or without occlusion until a positive result is obtained, after which the intervals between applications may be lengthened eg every 1–4 weeks. To minimize irritation, the remainder of the medication should be washed off when the patient awakes, and the area may be neutralized with the topical application of baking soda. 2-Formalin 1%soaks may be used for treatment of hyperhidrosis of the feet, but is unsuitable for the hands and axillae II-Systemic anticholinergic medications e.g. benztropine.They are effective because the preglandular neurotransmitter for sweat secretion is acetylcholine (although the sympathetic nervous system innervates the eccrine sweat glands). The use of anticholinergics may be unappealing because their adverse effect profile includes mydriasis, blurry vision, dry mouth and eyes, difficulty with micturition, and constipation 1 III-Iontophoresis The affected area is immersed in water or a solution containing an anticholonergic drug A low electrical current is passed across the skin surface daily for 20 minutes. This is repeated for several weeks and after reducing sweat production,treatments are then required weekly or less often IV-Botulinum toxin injections(Botox) It produces prolonged blockade of neuronal acetylcholine release at the neuromuscular junction 0.1mL of appropriately diluted is administered by high intradermal injections given to 1cm2 areas of skin appropriately anaesthetized by topical lignocaine/prilocaine in axillary skin, but palms and soles require regional nerve blockade. Each axilla usually requires 12 injections, hands 20 and each foot 24–36 injections. It will produce reduction in sweating within 48 h and the benefit will last for up to 8 months in axillary and 6 months in palmar hyperhidrosis V-Surgical intervention Sympathectomy, performed cervically, transaxillary or endoscopically. Sweating may return after a period of some years,due either to regeneration of sympathetic fibres or to fibres which do not pass through the sympathetic ganglia. Complications include haemothorax, pneumothorax and Horner’s syndrome. The palms or soles may become excessively dry. Postoperative compensatory hyperhidrosis may occur in up to 80% of those treated MILIARIA Etiology Hot humid conditions Lead to excessive sweating. In susceptible persons, overhydration of the stratum corneum leads to transient blockage of the acrosyringium. This blockage results in the leakage of sweat en route to the skin Skin bacterial flora Such as S. epidermidis and S. aureus, are thought to play a role in the pathogenesis of miliaria: -Patients with miliaria have 3 times as many bacteria per unit area of skin as healthy control subjects -Antimicrobial agents are effective in suppressing experimentally induced miliaria Factors leading to excessive sweating Miliaria may be caused by excessive sweating e.g. ultraviolet radiation, and exertion Clinically Three types are recognized: 1- Miliaria crystallina:Sweat leaks in the stratum corneum 2-Miliaria rubra:Sweat leaks in subcorneal layers 3-Miliaria profunda:sweat leaks in the papillary dermis Miliaria crystallina Clear, thin-walled vesicles, 1–2 mm in diameter.There is no inflammatory areola. Lesions are symptomless and develop in crops, mainly on the trunk Miliaria rubra Affects neonates aged 1-3 weeks and adults who live in hot, humid environments. Lesions are uniform, small, erythematous papules and vesicular papules on a back-ground of erythema Lesions cause intense pruritus and stinging that is exacerbated by fever, heat, or exertion In infants, lesions occur on the neck and in the groin and axillae. In adults, lesions occur on covered skin where friction occurs; these areas include the neck, scalp, upper part of the trunk, and flexures. The face and volar areas are spared. Lesions resolve within days after the patient is removed from the hot, humid environment.Lesions may occur within days of exposure to hot conditions, but they tend to appear after months of exposure. In late stages, anhidrosis is observed in affected skin 2 Miliaria profunda This form occurs in individuals who usually live in a tropical climate and have had repeated episodes of miliaria rubra. Lesions develop within minutes or hours after the stimulation of sweating. These lesions resolve quickly, usually in less than an hour after the stimulus that causes sweating is removed.The lesions are asymptomatic.Lesions are firm, flesh-colored, nonfollicular papules that are 1-3 mm in diameter.Lesions occur primarily on the trunk, but they can also appear on the extremities. Patients may report increased sweating in unaffected skin; swollen lymph nodes and hyperpyrexia. Affected skin shows diminished or absent sweating. Histopathology In miliaria crystallina, intracorneal or subcorneal vesicles communicate with eccrine sweat ducts, without surrounding inflammatory cells. Obstruction of the eccrine duct may be observed in the stratum corneum In miliaria rubra, spongiosis and spongiotic vesicles are observed in the stratum malpighian, in association with eccrine sweat ducts. Periductal inflammation is present. In early lesions in miliaria profunda, a predominantly lymphocytic periductal infiltrate is present in the papillary dermis and lower epidermis. A PAS-positive diastase-resistant eosinophilic cast may be seen in the ductal lumen. In later lesions, inflammatory cells may be present lower in the dermis, and lymphocytes may enter the eccrine duct. Spongiosis of the surrounding epidermis and parakeratotic hyperkeratosis of the acrosyringium may be observed Complications Secondary infection may appear as impetigo or as multiple discrete abscesses Heat intolerance is most likely to develop in patients with miliaria profunda; it is recognized by anhidrosis of the affected skin, weakness, fatigue, dizziness, and even collapse Treatment No reason to treat miliaria crystallina because this condition is asymptomatic and self-limited. The prevention and treatment of miliaria primarily consists of controlling heat and humidity so that sweating is not stimulated. Measures may involve treating a febrile illness; removing occlusive clothing; limiting activity; providing air conditioning; or, as a last resort, having the patient move to a cooler climate Topical treatments involve lotions containing calamine, with or without menthol; frequent showering; topical corticosteroids.The topical application of anhydrous lanolin to affected areas before exercise in hot weather has resulted in dramatic improvement in patients with miliaria profunda as it is believed to prevent ductal blockage. Oral ascorbic acid 500 mg b.d. was found to diminish the severity of miliaria . Bromhidrosis Excessive unpleasant odor that comes out from the skin Etiology Inadequate hygiene, medical (e.g. obesity, DM)or dermatologic conditions (e.g. Intertrigo,erythrasma) associated with hyperhidrosis or overgrowth of bacteria may further contribute to its development Apocrine bromhidrosis Axillary bacterial florae produce the distinctive axillary odor by decomposition of apocrine secretion into ammonia and short-chain fatty acids, with their characteristic strong odors. These acids are released through the action of an aminoacylase from Corynebacterium species. This aminoacylase has recently been demonstrated to also release other odiferous acids from glutamine conjugates in sweat, which may be the basis of individual body odor Eccrine bromhidrosis Less commonly eccrine secretion, which is typically odorless, assumes an offensive aroma due to: -When eccrine sweat softens keratin, bacterial degradation of the keratin yields a foul smell -Ingestion of some foods, including garlic, onion, curry, alcohol, certain drugs (e.g. penicillin, bromides), and toxins -Underlying metabolic or endogenous causes 3 Bromhidrosis exhibits a male predominance, which may be a reflection of greater apocrine gland activity in men than in women. Axillary bromhidrosis depends on apocrine function and therefore manifests exclusively after puberty. It occurs only rarely in the elderly population. Clinically Patients present with particularly offensive body odor that most commonly originates from the axillary region. However, the condition may also occur as genital or plantar bromhidrosis. The skin appears normal, except when bromhidrosis is associated with concomitant skin conditions such as erythrasma. In contrast, individuals with eccrine bromhidrosis caused by bacterial degradation of keratin may have maceration and a thick mat of moist keratin. This finding is most common on the plantar and intertriginous surfaces. Differential diagnosis Liver failure : There is a characteristic rotten-eggs odor in the breath and urine Renal failure: There is an amonia-like odor Schizophrenia: There is a characteristic unpleasant body odor Olfactory hallucinations: The patient's perception of body odor may be presenting sign of neurologic disease or organic brain lesions Treatment 1-Conservative measures, which aim to reduce bacterial flora and maintain a dry environment, include: Hygienic measures, such as adequate washing of the axillary vault, prompt removal of sweaty clothing, and the use of topical deodorant (which covers the odor and decreases bacterial counts). Regular shaving of axillary hair prevents the accumulation of sweat and bacteria on the hair shafts Use of topical antibiotics (e.g.clindamycine sol.) and antiseptic soaps limits the growth of contributory bacteria and may yield clinical benefit Treatment of coexisting skin conditions, such as intertrigo, erythrasma, and trichomycosis axillaris is important Omission of certain foods(eg curry spices, onions, garlic) may be of value if these factors can be isolated or identified as contributory factors. 2-Measures to enhance drying and limit maceration such as the use of aluminum chloride, iontophoresis, and systemic anticholinergic agents 3-Surgery Surgical removal of the apocrine glands is accomplished by means of en bloc excision of the axillary skin or superficial liposuction curettage CHROMHIDROSIS A rare condition characterized by the secretion of colored sweat Etiology Approximately 10% of people without the disease have colored sweat that is regarded as acceptable and within the normal range. It results from the secretion of lipofuscins in apocrine sweat which is a yellowish brown pigment. In chromhidrosis lipofuscin is found in a higher-than-normal concentration or a higher than normal state of oxidation in apocrine glands Clinically An odorless yellow, green, blue, brown, or black secretion can be manually expressed from apocrinebearing skin. History taking should include a detailed investigation of the patient's environment and lifestyle to exclude pseudo-chromhidrosis in which a chemical on the surface of the skin reacts with eccrine secretions and produces the color transformation. The yellow, green, and blue apocrine secretions produce a yellow fluorescence under a Wood lamp. 4 Differential diagnosis Pseudomonas infection Bleeding diathesis (red sweat, hematohidrosis) Alkaptonuria (ochronosis) Copper exposure (blue sweat) Treatment Patients can manually or pharmacologically empty the glands to achieve a symptom-free period of about 48-72 hours. Capsaicin, a crystalline alkaloid found in red peppers . Capsaicin cream depletes neurons of substance P, a neurotransmitter important in apocrine sweat production. Clinical relapse occurs when therapy is stopped. Botox injections have been attempted in 3 cases with mixed results. APOCCRINE GLAND DISORDERS FOX-FORDYCE DISEASE Fox-Fordyce disease is an infrequent condition. A distinct predilection for women exists; the female to male ratio is 9:1. It is most common in women aged 13-35 years; it is rare before or after this age. There is a keratin plug in the hair follicle infundibulum obstructing the apocrine acrosyringium. Rupture of the apocrine excretory duct occurs, and dermal spongiotic inflammation results. Extravasation of sweat and inflammation is postulated to cause the intense itching. The exact pathophysiology is still unknown. A number of factors have been implicated, including 1) emotional and/or hormonal influences. 2) alterations in sweat components. Clinically This condition frequently appears under conditions of heat, humidity, and friction, often appearing suddenly. The primary lesion is a skin-colored to reddish, smooth, dome-shaped, discrete, and follicular or perifollicular papule. Most patients report intense pruritus that disturbs sleep Lesions are most often found in the axillae, where they tend to be bilateral Lesions may also affect the periareolar, inframammary, and pubic areas The papules usually appear to affect every follicle in a given area Excoriations and lichenification may be seen as a consequence of scratching Sweating is often absent in the affected area Histopathology A keratin plug occludes the apocrine acrosyringium. Apocrine duct rupture results in spongiotic inflammation. Plasma cells may be noted.The dermis may show fibrosis and chronic inflammation. Treatment Based on the observations of follicular occlusion, topical tretinoin 0.1-0.5%cream was proposed as therapy but irritation has limited their long-term use. Success with systemic antibiotics, topical clindamycin, ultraviolet light,dermabrasion, were reported. Topical and intralesional steroids provide some benefit, but their use is limited by atrophy. Hormonal therapy with high-estrogen oral contraceptives, estrogen creams, and testosterone creams has been reported, but often with failure. 5 The short-term success of oral isotretinoin (15-30 mg/day) for 4 months was reported. The condition returned 3 months after cessation of therapy. Pimecrolimus (Elidel) 1% cream topically bid until relief, then 1-2 times/wk over a prolonged period produced very "impressive”results. HIDRADENITIS SUPPURATIVA Etiology Recent studies have indicated that hidradenitis suppurativa is caused by occlusion of the terminal follicular epithelium located in the apocrine gland-bearing skin areas. Therefore, it is better be termed as acne inverse. It is confined to areas of the body that contain apocrine glands. These areas are the axillae, areola of the nipple, groin, perineum, circumanal, and periumbilical regions. Family history is present in 38% of patients, so there may be a genetic predisposition. Excessive perspiration, often observed in athletes and the obese, may contribute to blocking of the apocrine glands. Disease activity may be related to stress and to cigarette smoking. The problem is somewhat common, thought to occur in 1-2% of the population Ingrown hairs are a predisposing factor, thus an increased incidence of the disease occurs in patients with tightly curled hair. The incidence is greater in females than in males, thought to be in the range of 4:1. Flare-ups have been associated with menses. It is not present prior to puberty because the apocrine glands are inactive. The condition may be observed in patients of any age after puberty. Hidradenitis may be observed as a primary condition without any obvious cause, but it may be observed in association with the following conditions: Crohn disease Down syndrome Certain forms of arthritis Graves disease or Hashimoto thyroiditis Herpes simplex Clinically The most common presentation is that of very painful,with multiple, tender,red, nodules in areas where apocrine glands are concentrated. The nodules may open and drain pus spontaneously.Nodules will heal slowly, with or without drainage, over 10-30 days The patient may present with a chronic condition in which the multiple nodules have coalesced and are surrounded by a fibrous reaction. This results in scarred and unsightly appearance of the area Investigations Culture of any exudate obtained (if aspiration or drainage of larger nodules is necessary) will yield a variety of saprophytic and pathogenic bacteria with a preponderance of staphylococci and streptococci. Thyroid function studies may be useful if clinically indicated because an association with Graves disease or Hashimoto thyroiditis may occasionally occur. If a patient appears toxic or is febrile, laboratory tests should include the following: - CBC - Blood cultures - Culture of exudate Complications • Lymphedema due to lymphatic injury from inflammation and scarring • Contracture formation at the sites of lesions • Squamous cell carcinoma (may develop in indolent sinus tracts) • Disseminated infection (rare) • Restricted limb mobility from scarring 6 • Urethral/rectal fistula • Anemia secondary to chronic infection • Arthritis secondary to inflammatory injury Treatment Tetracycline (250 mg PO qid or 500 mg PO tid) and erythromycin (500 mg q12h)may be helpful on a long-term basis Cephalosporins will help in acute cellulitis On a short-term basis, dicloxacillin(125-500 mg PO qid 1-2 h ac or 2 h pc for 7-10 d) is considered a good choice. But because of the growing presence of MRSA, using a sulfonamide(160 mg TMP/800 mg SMZ PO q12h for 10-14 d )or clindamycin (150-300 mg/dose PO q6-8h) may be useful Topical benzoyl peroxide, may be helpful Topical and intralesional injections of corticosteroids are sometimes helpful Hormonal therapy have reported some success. In a double-blinded study, the anti-androgen, cyproterone acetate (50 mg), in conjunction with ethinyl estradiol (50 µg), resulted in complete or partial clearance at 18 months post-treatment in 50 percent of patients. The 5α-reductase inhibitor, finasteride (1 mg), may also have a weak limited effect on disease management Infliximab, a chimeric monoclonal antitumor necrosis factor antibody, has demonstrated efficacy in several case reports Case reports or small case series have also shown therapeutic success with other systemic therapies, including systemic corticosteroids, azathioprine, cyclosporine, dapsone, and methotrexate Surgical interference: The nodules may need to be drained, particularly if they are very large, fluctuant, and painful Surgery may be needed for removal of sinus tracts, curettage, and exteriorization of the gland Excision and skin grafting may be helpful for severe intractable cases CO2 laser has been used to strip away glandular tissue 7