Singapore Health System
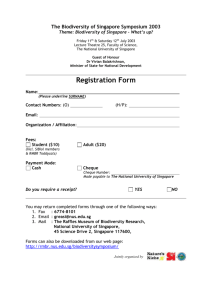
advertisement

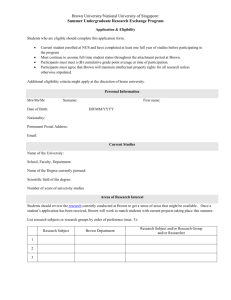
What the United States Can Learn from Singapore’s Health System by Allie Smith Abstract The United States faces a health care crisis with skyrocketing health care costs, growing ranks of uninsured Americans, and relatively poor health outcomes. Suggested possible responses to the crisis range from implementing a socialized national health care system to decreasing government intervention to allow market correction. To solve this crisis, the United States should look to innovative solutions crafted by other nations for providing national health care programs. Singapore possesses a unique program which provides its citizen a level of universal health coverage, yet it still boasts financial efficiency and impressive community health outcomes. The program successfully encourages individuals to assume personal responsibility for both their own health and their health expenditures. Singapore’s program consists of three main components: Compulsory individual medical savings accounts funded by employer and employee payroll tax contributions to pay for both current and future health care expenses; Catastrophic coverage for serious health conditions available from both the government and private insurers; and Need-based government subsidized coverage that fills the gaps between funds available from medical savings accounts and catastrophic coverage. The individual accounts, coupled with the structure of the catastrophic coverage, provide individual ownership of, and insight into, the real cost of health care. Private payors both individuals and insurers also bear a large portion of the costs of health care. Additionally, Singapore aggressively disseminates information regarding health care costs and outcomes and encourages preventive care. Price pressures stemming from government regulation of health care supply and demand serve to control health care inflation. While Singapore’s health system has proved a successful system for its citizens, importing the system wholesale to the United States would prove difficult, if not impossible. Societal and cultural influences may make it difficult to replicate. Nevertheless, the United States can still learn a great deal from the Singapore health system. The most important lessons from Singapore center on developing programs that encourage individual responsibility for health care decision making. The lesson is that the best solution to the health care crisis may be a hybrid of a public and private health care system. Second, the United States should provide individuals with the tools to become informed stakeholders in the health care system. Finally, reducing reliance on employer-based coverage for the majority of health care will help United States companies compete globally, prevent coverage loss tied to employment changes, increase 1 insurance options, and encourage consumer choice between plans. Table of Contents INTRODUCTION ............................................................................................................................... 2 HEALTH CRISIS IN THE UNITED STATES ....................................................................................... 4 SKYROCKETING COSTS ................................................................................................................. 4 POOR HEALTH OUTCOMES ............................................................................................................ 7 RISING NUMBER OF UNINSURED ................................................................................................... 9 EMPLOYMENT-BASED HEALTH INSURANCE COVERAGE ............................................................. 11 SINGAPORE HEALTH SYSTEM ...................................................................................................... 15 STRUCTURE OF THE SINGAPORE HEALTH SYSTEM ...................................................................... 16 Medisave Accounts ................................................................................................................. 16 Funding of Medisave Accounts .......................................................................................... 20 Problems with Medisave Accounts ..................................................................................... 24 Medishield & Private Health Insurance Coverage ................................................................ 27 Problems with Medishield .................................................................................................. 29 MediFund ............................................................................................................................... 31 GOVERNMENT CONTROL OVER HEALTH CARE DELIVERY & PRICING ......................................... 34 LESSONS FROM SINGAPORE’S HEALTH SYSTEM ........................................................................ 36 IMPLEMENTATION DIFFICULTIES ................................................................................................. 37 PUBLIC-PRIVATE HYBRID HEALTH CARE SYSTEM...................................................................... 38 DECREASED RELIANCE ON EMPLOYER-PROVIDED HEALTH INSURANCE COVERAGE .................. 40 INCREASED PERSONAL RESPONSIBILITY AND HEALTH CARE CONSUMERISM ............................. 40 CONCLUSION................................................................................................................................. 42 INTRODUCTION Presidential elections and an increasingly dismal picture of health care in the United States have once again brought debates about a national healthcare solution bubbling to the surface. Liberals advocate handing off the entire program to the federal government; 2 conservatives, on the other hand, argue that leaving health care to the whims of the market will eventually solve the problem.1 The traditional view of socialized medicine is that it “inevitably leads to poor quality, inefficiency, rising taxes and rationing.”2 Singapore, however, proves the exception to this rule. Singapore has implemented a national healthcare system that not only provides a measure of universal health coverage for all Singaporeans, but encourages personal responsibility for individual and family health.3 The system exhibits not only health outcomes that far surpass those recognized in the United States, but health care in Singapore costs substantially less than that in the United States.4 While the United States spends approximately 16 percent of its gross domestic product (GDP), Singapore only devotes about 3 percent of its GDP to health care.5 As the United States seeks a solution to the national health care crisis, Singapore’s system may provide guidance in the development of possible solutions. Part II explores the health care crisis in the United States and its detrimental impact on achieving economic justice in the delivery of health care. Part III analyzes the components of the Singapore health system and discusses the successes and shortcomings of each aspect of the system. Part IV suggests that the United States may benefit from adopting modified versions of certain components of Singapore’s system. 1 Karl Rove, Republicans Can Win on Health Care, WALL ST. J., September 18, 2007. Id. 3 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study of Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 94 (2004). 4 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST: A PRIMER 2 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 5 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Studyof Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 91 (2004). 2 3 HEALTH CRISIS IN THE UNITED STATES Political pundits, as well as average citizens, have recognized that the United States health care system has reached a crisis state.6 While the individual worries about access to affordable health care, the problems with the health care system are multiple and complex.7 Nevertheless, four issues represent the heart of the health care crisis. These four issues are rapidly rising costs, poor health outcomes, the growing number of uninsured, and the deteriorating employer-provided health insurance system. SKYROCKETING COSTS Almost $2 trillion is spent on health care in the United States annually, or 16% of the United States gross domestic product (GDP).8 On a per capita basis, the United States spends $6,697 per person annually.9 In fact, the United States spends more per capita on healthcare than any other country in the world.10 Reaching $2 trillion in health care spending is the result of decades of growth in health care spending that has exceeded the growth in income.11 Figure 1 illustrates this growth. In 1970, the United States spent a mere $356 per person on health care, only 7.2 percent of GDP.12 Health care spending has grown an average of 9.8 percent each year since.13 This growth rate averaged 2.5 percent higher than the annual growth in income each 6 See Daniel Gotoff, The Changing U.S. Voter, http://usinfo.state.gov/journals/itdhr/1007/ijde/gotoff.htm (last visited Nov. 29, 2007) (indicating that health care is voters’ number one domestic concern). 7 Id. 8 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST A PRIMER 2 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 9 Id. 10 ORG. FOR ECON. COOPERATION AND DEV., OECD HEALTH DATA 2007 HOW DOES THE UNITED STATES COMPARE 1 (2007), available at http://www.oecd.org/dataoecd/46/2/38980580.pdf. 11 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST A PRIMER 3 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 12 Id. at 2. 13 Id. at 3. 4 year.14 Unfortunately, the rampant growth in health care spending appears poised to continue for the foreseeable future. The United States government predicts that health care spending will more than double to reach $4.1 trillion by 2016 or 20 percent of GDP.15 While discussing health care spending in the aggregate illustrates the trend, most people more readily identify with the direct impact that health care cost increases have on their own lives. Many feel the impact in the form of health insurance premiums because health insurance of some kind represents the dominant means of financing health care expenses.16 Between 2002 and 2007 alone, health insurance premiums have grown cumulatively by 78%.17 This growth has outpaced both inflation and growth in worker income.18 Today, premiums for single health insurance coverage equate to about $4,479 annually; family coverage costs $12,106 annually.19 14 Id. Id. at 2. 16 THE HENRY J. KAISER FAMILY FOUND., TRENDS IN HEALTH CARE COSTS AND SPENDING 2 (2007), available at http://www.kff.org/insurance/upload/7692.pdf. 17 THE HENRY J. KAISER FAMILY FOUND., EMPLOYER HEALTH BENEFITS 2007 ANNUAL SURVEY 11 (2007), available at http://www.kff.org/insurance/7672/upload/EHBS-2007-Full-Report-PDF.pdf. 18 See THE HENRY J. KAISER FAMILY FOUND., TRENDS IN HEALTH CARE COSTS AND SPENDING 2 (2007), available at http://www.kff.org/insurance/upload/7692.pdf (indicating that cumulative inflation for the period has been 17 percent and cumulative wage growth has been 19 percent). 19 THE HENRY J. KAISER FAMILY FOUND., EMPLOYER HEALTH BENEFITS 2007 ANNUAL SURVEY 11 (2007), available at http://www.kff.org/insurance/7672/upload/EHBS-2007-Full-Report-PDF.pdf. 15 5 Figure 120 While recognizing the huge cost increases is simple, determining the manifold causes of the health care cost increases poses a more difficult problem. Increased medical technology plays a large role in the costs increase.21 While better technology promises more efficient care and treatment that could ultimately result in cost savings, these potential cost savings have yet to 20 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST A PRIMER 2 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 21 Id. at 12. 6 materialize.22 Instead, technology often provides costly treatments for heart burn, erectile dysfunction, and other diseases that largely went untreated in the past.23 As the baby boomer generation gets older, the population of the United States ages bringing with it the concomitant higher health costs generated by older individuals.24 In addition to being older, the population of the United States has grown more sedentary and heavier, as well. Obesity carries higher risk factors for a variety of costly health conditions such as diabetes.25 Finally, the structure of the United States health care financing system encourages cost increases.26 Dependence on employer-provided insurance to provide the bulk of financing isolates consumers from both the true cost of care and the true cost of coverage; the low cost sharing at the point of service may further encourage consumption.27 Unfortunately, the factors creating the growth in health care spending have not necessarily led to corresponding improvements in health outcomes. POOR HEALTH OUTCOMES Although the United States spends more on healthcare than any other nation in the world, the United States lags behind many other developed nations both in health outcomes. The lag in health outcomes appears in a variety of health statistics. Table 1 compares various health statistics of the United States with those of several other nations. The United States has shorter life spans and higher child mortality rates than most other developed nations.28 In fact, the 22 Douglas Hotz-Eakin, Health Care Reform in the United States: Why, When and How? 1 (Networks Fin. Inst., Policy Brief No. 2006-PB-16, 2006), available at http://papers.ssrn.com/sol3/papers.cfm?abstract_id=947906. 23 Id. 24 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST A PRIMER 12 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 25 Id. 26 Id. 27 Id. 28 WORLD HEALTH ORG., WORLD HEALTH STATISTICS 2007 22-31 (2007). 7 probability of dying under the age of 5 in the United exceeds that of many considerably less affluent nations such as Croatia and Cuba.29 Not only are individuals in the United States prone to die earlier, but individuals in the United States are also more likely to have illnesses that diminish activities and productivity during life.30 Compared to better performing nations, more adults in the United States—almost 15 percent of the population—experienced limitations on activities due to health conditions.31 Similar results appear for children; over 5 percent of children miss more than 11 days of school due to health conditions.32 Although some of these health outcomes may result from other societal influences such as increased obesity in the United States, each of these health statistics suggests that the huge amounts of money spent on health care in United States fail to create a healthier population.33 Table 134 Comparison of Health Statistics & National Cost of Health care Country Heath Factors United Singapore Japan Sweden States Life expectancy at M 75 / F 80 M 78 / F 82 M 79 / F 86 M 79 / F 83 birth (years) Healthy life expectancy at birth M 67 / F71 M 69 / F 71 M 72 / F 78 M 72 / F 75 (years, 2002) Probability of dying under age of 5 (per 8 3 4 4 1000 live births) Probability of dying M 137 / M 83 / F48 M 92 / F 45 M 78 / F 50 between 15 and 60 F81 29 United Kingdom M 77 / F 81 M 69 / F 72 6 M 101 / F 62 Id. Cathy Schoen et al., U.S. Health System Performance: A National Scorecard, 25 HEALTH AFF. 460 (2006). 31 Id. 32 Id. 33 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST A PRIMER 12 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 34 Data taken from the World Health Organization 2005 data on each country. 30 8 years (per 1000 population) Total expenditure on health per capita (Intl $, 2004) Total expenditure on health as % of GDP (2004) 6,096 1,118 2,293 2,828 2,560 15.4 3.7 7.8 9.1 8.1 RISING NUMBER OF UNINSURED No figure captures the failures of the health care system more clearly than the soaring number of uninsured individuals in the United States. Due in large part to the skyrocketing costs of health insurance coverage and decreases in employers offering coverage, the ranks of the uninsured continue to grow. Currently, almost 47 million non-elderly people in the United States are uninsured. This figure represents an increase of more than 27% from the 36.5 million uninsured in 1994.35 The 47 million figure for uninsured individuals may not even fully capture the true extent of the problem. Since these figures are based on Census Bureau data, they only represent the number of uninsured at one moment in time and fail to include those that suffer temporary periods without insurance coverage at other points during the year.36 Other studies show that at least 89.6 million non-elderly, almost 1 out of 3 people, were uninsured for at least one month in 2006-2007.37 The ranks of the uninsured are disproportionately filled with minorities and the poor. Although 64.1 percent of the population under 65 is Caucasian, Caucasians only represent 45.1 35 Paul Fronstein, Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2007 Current Population Survey 1 (Emp. Benefits Res. Inst., Issue Brief 310, 2007). 36 Laura D. Hermer, Private Health Insurance in the United States: A Proposal for a More Functional System, 6 HOUS. J. HEALTH L. & POL'Y 1, 59 (2005). 37 Kim Bailey, Wrong Direction: One Out of Three Americans are Uninsured 2 (Families USA, Publication No. 07108, 2007), available at http://familiesusa.org/assets/pdfs/wrong-direction.pdf. 9 percent of the uninsured.38 In contrast, black individuals comprise 12.6 percent of the population and 15.4 percent of the uninsured; Hispanics comprise 16.3 percent of the population, but a colossal 32.5 percent of the uninsured.39 Part of this disparity may stem from the fact that minorities are more likely to fall in lower income categories.40 “The uninsured tend to be members of low-income families.”41 Almost one-third of the uninsured come from families with annual incomes less than $20,000, yet families in this income bracket represent less than 17 percent of the population.42 Although most of the uninsured are low income, the majority, 82%, of the uninsured come from families of the working poor where at least one member works. In fact, 71% of the uninsured come from families where at least one member works full time. The number of the uninsured is huge; however, the impact on society is even more staggering. “[D]iminished health and shorter life spans of the uninsured” cost the United States up to $135 billion annually.43 The uninsured receive less medical care, both preventative care and treatment for health conditions, than insured individuals.44 As a result, they experience worse health outcomes and have a 25 percent higher mortality rate than individuals with health insurance.45 Additionally, the care that the uninsured receive places a strain on the United States 38 Paul Fronstein, Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2007 Current Population Survey 14 (Emp. Benefits Res. Inst., Issue Brief 310, 2007). 39 Id. at 17. 40 Id. at 14. 41 Id. 42 Id. 43 Id. at 17. 44 See Jack Hadley, Insurance Coverage, Medical Care Use, and Short-term Health Changes Following an Unintentional Injury or the Onset of a Chronic Condition, 297 J. AM. MED. ASS’N 1073 (2007) (indicating that the uninsured receive less care and experience worse health outcomes for both chronic conditions and for injuries). 45 Paul Fronstein, Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2007 Current Population Survey 17 (Emp. Benefits Res. Inst., Issue Brief 310, 2007). 10 health care system.46 The uninsured often seek inappropriate levels of care. Unable to pay for physician’s visits in private clinics, the uninsured seek more costly care in public hospital emergency rooms that cannot refuse care.47 Much of the care that the uninsured receive goes unpaid.48 Medical debt, often linked to a lack of health insurance is the second leading cause of bankruptcy.49 These unpaid medical bills place financial stresses on the health care providers.50 In turn, many of these costs are passed on to insured consumers.51 This additional cost to insured consumers equates to about $922 annually for family coverage and $341 for individual coverage.52 EMPLOYMENT-BASED HEALTH INSURANCE COVERAGE Employment-based health insurance coverage forms the backbone of the United States health care financing system. Figure 2 illustrates the dominance of employment-based coverage over other source of health insurance coverage. Employment-based coverage comprises 64.1% of health insurance coverage. As indicated by the growing number of uninsured, employmentbased coverage has decreased in recent years.53 Businesses unable to afford the increasing cost of health insurance premiums have either discontinued coverage or increased cost sharing of 46 Id. Id. 48 Id. 49 Edward J. Larsen & Marc Dettmann, The Impact of HSAs on Health Care Reform Preliminary Results After One Year, 40 WAKE FOREST L. REV. 1087, 1093 (2005). 50 Paul Fronstein, Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2007 Current Population Survey 17 (Emp. Benefits Res. Inst., Issue Brief 310, 2007). 51 Kathleen Stoll, Paying a Premium: The Added Cost of Care for the Uninsured 2 (Families USA, Publication No. 05-101, 2005), available at http://familiesusa.org/assets/pdfs/Paying_a_Premium_rev_July_13731e.pdf. 52 Id. 53 John Holahan & Allison Cook, What Happened to Insurance Coverage of Adults and Children in 2006? 6 (The Henry J. Kaiser Family Found. Issue Brief, 2007), available at http://www.kff.org/uninsured/upload/7694.pdf. 47 11 premiums to the point that some workers can no longer afford to participate.54 54 Id. 12 Figure 255 United States: Composition of Health Insurance Coverage 2002 Other Private, 8.3% Uninsured, 14.0% Other Government, 3.0% Medicare, 13.4% Private, Employment Based, 64.1% Medicaid, 10.4% Although employment-based health insurance offers some positive aspects, the system’s flaws outweigh its benefits. One of the strongest benefits of health insurance paid in part by employers is that it provides a voluntary funding source, rather than being paid directly from tax revenues. Additionally, linking health insurance to employment encourages individuals to work.56 Nevertheless, employment-based coverage suffers from many problems. Some of these flaws are readily apparent. For example, if medical insurance is linked to employment, losing a job or switching jobs often results in a coverage loss.57 Additionally, providing coverage saddles 55 Richard L. Kaplan, Who’s Afraid of Personal Responsibility? Health Savings Accounts and the Future of American Health Care, 36 MCGEORGE L. REV. 535, 538 (2005). 56 JONATHAN BARRY FORMAN, MAKING AMERICA WORK 251-52 (Urban Institute Press 2006) (2006). 57 Id.at 252. 13 employers with huge costs.58 For many employers, employee benefits are the largest cost item after wages.59 For example, Starbucks spends more on health care annually then it spends on the raw materials for brewing its coffee.60 These huge costs threaten the global competitiveness of corporations that continue to offer health insurance.61 Other flaws in the employer-provided health coverage system are less obvious. The largest flaw in the system is that it actually encourages the growth of health care costs and creates an inefficient market. Employer-provided coverage not only effectively limits the coverage choices of the health care consumer to the plans offered by the employer, but also shields the health care consumer from both the cost of coverage and the actual cost of care.62 Tax breaks provided for purchasing employer-provided coverage make it less palatable for employees to select coverage from a source other than their employer.63 Employers shield employees from the true cost of health coverage by fully or partially subsidizing the coverage.64 Since employees recognize only a fraction of coverage increases caused by their consumption, employees have no incentive to change their behavior.65 Although out-of-pocket spending accounts for approximately 20 percent of all health expenditures, point-of-service cost-sharing still provides 58 Devon M. Herrick, Why Employer-Based Health Coverage is Unraveling, HEALTH CARE NEWS, Nov. 1, 2005, http://www.heartland.org/Article.cfm?artId=17950 59 Id. 60 Id. 61 Id. 62 THE HENRY J. KAISER FAMILY FOUND., HEALTH CARE COST A PRIMER 12 (2007), available at http://www.kff.org/insurance/upload/7670.pdf. 63 JONATHAN BARRY FORMAN, MAKING AMERICA WORK 247 (Urban Institute Press 2006) (2006). 64 Donald J. Palmisano et al, Expanding Insurance Coverage Through Tax Credits, Consumer Choice, and Market Enhancements, 291 J. AM. MED. ASS’N 2237, 2238-39 (2004). 65 14 little visibility into the true cost of care or a means for consumers to make effective choices.66 Finally, the prevailing fee-for-service payment systems encourage health care providers to perform as many services as possible without regard to the marginal benefits provided.67 These flaws in the United States system and its deterioration leading to increasing numbers of uninsured individuals should encourage the United States to look for solutions to the health care crisis in the successful systems of other countries such as Singapore. SINGAPORE HEALTH SYSTEM Singapore, in contrast to the United States, spends a mere 3.7 percent of it GDP on health care, yet boasts both impressive health outcome indicators and some degree of universal health coverage. Table 1 illustrates the comparisons between cost of care and health outcomes for Singapore and United States among others. In Singapore, people live longer than those in the United States. Men and women in Singapore not only enjoy longer lives, but they can also expect more of their life to be healthy. These health outcomes are also demonstrated by a reduced infant mortality rate. Only 3 children out of every 1,000 live births die before the age of 5. Per capita, Singapore’s total health expenditures equate to only $1,118 annually. While a variety of factors influence these health outcomes, Singapore’s health system and culture of personal responsibility for health care deserve a large part of the credit for achieving such impressive results. 66 Distribution of Out-of-Pocket Spending for Health Care Services, http://www.kff.org/insurance/snapshot/chcm050206oth.cfm#3 (last visited Nov. 29, 2007). 67 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 89 (2004). 15 STRUCTURE OF THE SINGAPORE HEALTH SYSTEM Singapore’s health system embraces and encourages the country’s emphasis on taking personal responsibility for health care. The basic structure of Singapore’s health system revolves around what are commonly referred to as the 3M’s, Medisave, Medishield, and Medifund. These components work to ensure a measure of universal coverage for hospital care yet still encourage individuals to make efficient health care decisions. Medisave is a series of compulsory individual savings accounts that fund both current and future health care. Medishield is the government’s voluntary catastrophic health insurance plan that provides benefits for very serious health conditions. Finally, Medifund is a needs-based program that helps provide health care when an individual’s Medisave and Medishield benefits are insufficient to cover the cost of care. The 3M’s supplement the government’s system of subsidies for hospital care. The government also helps control costs and ensure access to both primary care and hospital services by regulating a system composed of both public and private health care delivery systems. In addition, private payors including individuals, private insurance, and employer-provided insurance help finance health care in Singapore.68 Medisave Accounts Medisave accounts form the cornerstone of Singapore’s health care financing system. Over 80% of Singapore citizens have Medisave Accounts.69 Singapore has long touted these accounts as the most efficient means of providing universal health care to its citizens.70 These 68 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 86 (2004). 69 W. von Eiff, et al., Medical Savings Accounts: A Core Feature of Singapore’s Health Care System, 3 EUR. J. HEALTH. ECON. 188, 192 (2002). 70 LEE KUAN YEW, FROM THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 -2000 101-02(HARPERCOLLINS 2000). 16 accounts are compulsory tax-advantaged savings accounts funded by both employer and employee tax contributions.71 Account holders can use the accumulated funds for a variety of health-related purposes such as paying for certain current health expenses, paying health insurance premiums, and even funding health care during retirement.72 At first glance, Medisave Accounts seem very similar to several voluntary tax-advantaged health savings accounts available in the United States. The closest United States parallel is the relatively new Health Savings Account (HSA) designed to complement high-deductible health plans.73 HSAs may not only fund current health expenses, but the accounts could also serve as a savings vehicle for health care expenses during retirement.74 HSA account holders can use account funds to pay for any health expenses that could normally be deductible on taxes.75 This includes medications, medical equipment, and most outpatient and inpatient medical services.76 Singapore’s Medisave Accounts actually differ a great deal from the HSAs offered in the United States. First, the Medisave Accounts do not merely complement another health insurance 71 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 79-80 (2006). 72 A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited Oct. 27, 2007). 73 Medisave Accounts also resemble more loosely Medical Flexible Spending Accounts and Health Reimbursement Arrangements. More information on these plans may be found at www.irs.gov. 74 United States Department of Treasury HSA Frequently Asked Questions, http://www.ustreas.gov/offices/publicaffairs/hsa/faq_basics.shtml (last visited Oct. 27, 2007). 75 See INTERNAL REVENUE SERVICE, MEDICAL AND DENTAL EXPENSES, PUB. 502 (2006) (describing example deductible medical expenses as well as non-deductible expenses). 76 Id. 17 plan; Singapore has treated the Medisave Accounts as the primary health care funding vehicle.77 Second, Singapore intensively regulates how the Medisave Accounts may be used.78 From their inception in 1984, Medisave Accounts have sought to fill the role of Singapore’s primary mechanism for financing universal health care.79 Singapore recognized the need to provide quality, affordable health care to its citizens, but struggled with finding a solution that provided efficient service and cost containment.80 Singapore rejected plans providing free national health care as impractical plans that lead to rationing of services and ballooning costs.81 Singapore also rejected what it deemed “American-style medical insurance schemes” because it deemed them too expensive and feared they would lead to increased consumption of wasteful diagnostic tests.82 Instead, Singapore felt that people took more responsibility for their health if they bore a share of the cost of their health care.83 Medisave Accounts attempted to balance the competing needs of providing a mechanism for financing current and future health care services, but also encouraging personal responsibility for health care to encourage efficient health care choices. While the accounts offer a readily available source of funds that each individual may use for health care, the money essentially belongs to the individual ensuring that the account holder thinks carefully about health care decisions. 77 LEE KUAN YEW, FROM THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 -2000 101-02(HARPERCOLLINS 2000). 78 A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited Oct. 27, 2007). 79 LEE KUAN YEW, FROM THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 -2000 101-02(HARPERCOLLINS 2000). 80 Id. 81 Id. 82 Id. 83 Id. 18 Medisave Accounts extended the focus on personal responsibility for health care decision-making even further by placing limits on expenses capable of payment from the accounts.84 Medisave Accounts actually have a strict schedule of benefits that limits covered services.85 The list mimics the type of schedule of benefits one would expect to see on a traditional private health insurance plan. The primary goal of Medisave accounts is to cover inpatient hospitalization expenses. 86 Therefore, Singapore prohibits the use of Medisave funds for most physician visits and only allows the use of the funds for a few expensive outpatient services. 87 Singapore also places stringent limits on use of Medisave funds to cover maternity expenses.88 In addition to placing limits on the types of Medisave-eligible services, Singapore limits the amounts available for withdrawal for each type of service.89 The withdrawal rates generally will cover the full cost of inpatient care only in the lower-cost, government-subsidized hospital wards.90 For other services or more premium hospital care, the government sets the withdrawal rates below the costs of the service.91 These lower withdrawal rates force individuals to pay a portion of the cost of their care directly from their monthly budgets. Since the 84 A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited Oct. 27, 2007). 85 Id. 86 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 79-80 (2006). 87 See A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited October 27, 2007) (allowing payments for treatments such as dialysis and HIV treatment). 88 See Id. (limiting use of Medisave to the first four children born alive to a mother). 89 Id. 90 Id. 91 LEE KUAN YEW, FROM THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 -2000 101-02(HARPERCOLLINS 2000). 19 individuals directly bear a portion of the cost of premium hospital services, Singapore believes that individuals will think carefully before making health care purchasing decisions.92 In addition to providing a means for health care financing, Medisave Accounts, coupled with the other individual accounts within the Central Provident Fund, represent the largest individual accumulation of wealth for many in Singapore. For the lowest wage earners in Singapore, the funds held in these compulsory savings accounts represent the bulk of their savings. At retirement, individuals may withdraw excess Medisave.93 Additionally, funds remaining in the accounts at death pass directly to those designated as beneficiaries.94 Although Medisave Accounts provide a formidable tool for saving for health care, the program represents a significant tax on both employers and employees. Funding of Medisave Accounts Employer and employee tax contributions made to Singapore’s Central Provident Fund provide the funding for the individual Medisave Accounts.95 Employer and employee contributions to the Central Provident Fund vary based on the type of employee and the age of the employee.96 For employees younger than 50, the employee contributes 20% of wages; the employer contributes 14.5% of the employee’s wages.97 The percentage of wages contributed by 92 Id. A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited Oct. 27, 2007). 94 Id. 95 Self-employed individuals also make contributions to the Central Provident Fund. These contributions vary with the individual’s age and net trade income. The amount attributed to the individual’s Medisave account ranges from 2.17% of net trade income to 8.5% of net trade income with a maximum annual contribution of S$4,590 for 2007. Medisave for the Self-Employed, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Others/se_Medisave.htm#Tbl_B (last visited October 27, 2007). 96 CPF Contribution and Allocation Rates from 1 July 2007, http://mycpf.cpf.gov.sg/Employers/Gen-Info/cpfContri/ContriRa.htm (last visited Oct. 27, 2007). 97 Id. 93 20 both the employer and the employee decreases with the age of the employee.98 The decreased tax cost to employers for older employees offers an economic incentive for employers to hire and retain older employees. Table 2 illustrates the change in contribution levels based on age for private sector employees. Table 2 Contribution Rates & Allocation of Central Provident Funds for Private Sector Credited Into Contribution Contribution Total Employee By Ordinary Special Medisave By Employer Contribution Age Employee Account Account Account (% of (% of (years) (% of (Ratio of (Ratio of (Ratio of wage) wage) wage) Contribution) Contribution) Contribution) 35 & below Above 35 - 45 Above 45 - 50 Above 50 - 55 Above 55 - 60 Above 60 - 65 Above 65 14.5 20 34.5 0.6667 0.1449 0.1884 14.5 20 34.5 0.6088 0.1739 0.2173 14.5 20 34.5 0.5509 0.2028 0.2463 10.5 18 28.5 0.4562 0.2456 0.2982 7.5 12.5 20 0.575 0 0.425 5 7.5 12.5 0.28 0 0.72 5 5 10 0.1 0 0.9 Table taken from the Singapore Central Provident Fund Board. The Singapore Central Provident Fund allocates the contributions made on behalf of each employee to three individual accounts that comprise the employee’s share of the Central Provident Fund.99 In addition to the Medisave Accounts, the Central Provident Fund contains an 98 99 Id. Id. 21 individual’s Special Account and Ordinary Account.100 The Special Account serves as a retirement funding vehicle; the Ordinary Account contains funds accessible for purchasing a home, insurance or education.101 Just as the contribution rates change with the employee’s age, the amounts allocated to each type of account also change as the employee ages.102 As the employee grows older, the percentage of the contributions devoted to the Medisave Account increases.103 Table 2 shows the change in allocation rates between the three accounts. This increase serves two purposes. First, the change parallels the age-based increase in premiums for Medishield or other health insurance coverage.104 Additionally, the increase in allocation reflects the need to build a large balance in the Medisave Account as an older employee so that the account can fund health care expenses during retirement. Medisave Account balances also earn interest.105 Unlike other portions of the Central Provident Fund, the government protects Medisave Accounts from any risk of market loss and guarantees a standard interest rate of 2.5% on Medisave Accounts.106 Although the accounts receive guaranteed interest, they may earn interest in excess of this rate.107 Beginning in 2008, the standard rate of interest will be 1% above the rate of interest paid on 10-year government 100 Introduction to CPF, http://mycpf.cpf.gov.sg/CPF/About-Us/Intro/Intro.htm (last visited Oct.27, 2007). Id. 102 CPF Contribution and Allocation Rates from 1 July 2007, http://mycpf.cpf.gov.sg/Employers/Gen-Info/cpfContri/ContriRa.htm (last visited Oct. 27, 2007). 103 Id. 104 Ngee-Choon Chia & Albert K.C. Tsui, Medical Savings Accounts in Singapore: How Much is Adequate?, 24 J. HEALTH ECON. 855, 861 (2005). 105 A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited Oct. 27, 2007). 106 Central Provident Fund Board, More $ for Your Retirement, 4 (2007), http://mycpf.cpf.gov.sg/NR/rdonlyres/B28B91BF-9645-4E0A-9F1D-B47FFD577093/0/CartoonBooklet.pdf. 107 Id. 101 22 securities.108 Singapore also promotes economic justice by providing a 1% higher rate of interest on Medisave Account balances up to a decreed dollar amount.109 This ensures that those individuals with the lowest amounts of medical savings benefit the most from the government funded interest accruals. Medisave Accounts enjoy several tax advantages. Contributions to Medisave accounts, interest earned on the accounts, and withdrawals from the accounts are exempt from Singapore’s income tax.110 These exemptions, however, benefit only a small segment of the population since only one in three people in Singapore earn enough to be subject to income tax.111 Critics have contended that these tax advantages actually make the health care financing arrangement regressive and minimize the importance of the individual income tax as a revenue source.112 To combat the wealthy accumulating large tax-sheltered account balances, the government places a limit on the account balance allowed in a Medisave Account. For 2007, each Medisave Account may only contain S$33,500.113 Contributions in excess of this amount are reallocated to either the individual’s Special Account or Ordinary Account.114 While Singapore seeks to limit excessive accumulated wealth in tax-sheltered Medisave Accounts, Singapore balances this against the need to ensure that each account contains a 108 Id. See Id. (indicating that the higher interest rate applies to the first S$60,000 of combined funds in individuals’ Ordinary Account and Medisave Account). 110 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 88 (2006). 111 Id. 112 See Id. (criticizing the regressive nature of the exemption and its effect on the individual income tax, one of few progressive taxes in Singapore’s tax system). 113 A Guide to Medisave, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/Health care/MED.htm (last visited Oct.27, 2007). 114 Id. 109 23 sufficient balance to fund not only current health care expenditures, but also to fund retirement health expenditures. Singapore promotes account balances adequate to fund future health expenditures in two ways. First, the government limits the kinds of services that may be funded with Medisave funds and the amount that may be withdrawn for each occurrence.115 Second, although retirees may normally withdraw a portion of their Central Provident Funds balance immediately upon retirement, they may not withdraw any funds form the Medisave Account unless a certain minimum sum remains. For 2007, the minimum sum is S$28,500.116 Despite these efforts to ensure adequate funding for health care, Medisave Accounts demonstrate many shortcomings. Problems with Medisave Accounts Although Medisave Accounts possess many positive aspects, the accounts still have many weaknesses. The accounts actually provide little health care funding. Medisave Accounts in some cases fail to provide adequate coverage for post-retirement health care expenses.117 The accounts may create inefficiencies by not taking advantage of social risk pooling strategies to control costs and more evenly distribute health care expenses.118 Critics debate the ability of the accounts to really control costs since health care costs continue to increase, albeit at a lower rate than in the United States.119 Additional inefficiencies may really from the accounts failure to provide little if any coverage for preventive services or outpatient care and management for 115 Id. Id. 117 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 89 (2006). 118 Id. at 87. 119 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 91 (2004). 116 24 chronic diseases through the Medisave Accounts. Finally, Medisave Accounts do little to promote economic justice by redistributing wealth in order to ensure Singapore’s lowest wage earners receive adequate health care.120 Singapore’s government has long touted Medisave Accounts as its primary funding mechanism for health care; however, Medisave Accounts actually provide little of the funding.121 Consistently, Medisave withdrawals represent less than 10% annually of funds spent on health care.122 Instead, other private expenditures represent over 60% of the amount spent annually on health care.123 Singapore’s government contributes only 30% to the cost of health care. Figure 3 illustrates the breakdown of annual health care expenses in Singapore. These statistics suggest that universal coverage funded by Medisave Accounts may prove more idealistic vision rather than reality.124 While most Singaporeans have Medisave Accounts, the accounts provide them little actual coverage. Instead, private individuals truly fund most of the health care in the country with their own out-of-pocket spending.125 120 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL'Y & L. 709, 710-13 (2001). 121 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 86 (2006). 122 Id. 123 Id. 124 Id. 125 Id. 25 Figure 3126 Besides representing a somewhat ineffectual funding mechanism, Medisave Accounts also may not accomplish the goals for which they were designed. Research suggests that despite Medisave accounts Singapore continues to experience fairly dramatic health care cost increases.127 Additionally, Medisave account balances also rarely reach the levels to actually fund each individual’s retirement health expenses.128 Instead, childrens’ Medisave accounts often end up funding their parent’s healthcare.129 126 Table taken from Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 86 (2006). 127 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 91 (2004). 128 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 88 (2006). 129 Id. 26 Finally, Medisave Accounts may create more inefficiences in health care financing than they solve.130 Medisave’s focus on individual responsibility prevents Singapore from benefiting from social risk pooling arrangements which are generally thought to more efficient than individual health care purchasing.131 Medisave’s complicated withdrawal schedules and claims procedures place a heavy administrative burden on the Central Provident Fund Board.132 This administrative burden results in an inefficient use of resources that could perhaps better be spent on increased health care services and funding. Medishield & Private Health Insurance Coverage Medishield serves as the government’s low cost catastrophic health insurance plan.133 Singapore implemented Medishield in 1990 to help insure against serious health conditions whose care and treatment would far exceed the amounts saved in Medisave Accounts.134 Just as with Medisave, Medishield continues to encourage personal responsibility for individual and family health.135 Individuals still must pay deductibles, coinsurance and copayments even for eligible services that they receive under the plan.136 Singapore advocates that this continued personal liability for health services encourages individuals to make intelligent choices regarding care.137 The basic Medishield plan also bases the amount that it pays on the expenses that would 130 Id. at 87. Id. 132 Id. 133 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 713 (2001). 134 LEE KUAN YEW, FROM THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 -2000 101-02(HARPERCOLLINS 2000). 135 Id. 136 Id. 137 Id. 131 27 be incurred for services rendered in the lower-cost, government subsidized hospital wards.138 Therefore, individuals seeking premium services must bear a larger portion of the costs since Medishield will cover a mere fraction of the cost. Unlike Medisave, coverage under Medishield is voluntary, and individuals may opt out of the plan.139 Although Medishield is a government program, the plan operates in many ways like a private insurer. Individuals must apply for coverage and acceptance is conditioned upon good health.140 Those individuals that have serious pre-existing health conditions may face denial of coverage or an exclusion for treatment of the pre-existing condition.141 Additionally, individuals over the age of 75 may not apply for coverage.142 Medishield has evolved, since its 1990 genesis, to include more than just the basic level of coverage. Singapore not only offers two levels of Medishield coverage, but it has developed a symbiotic relationship with private insurers that allows individuals who wish to seek unsubsidized care or treatment in higher-cost hospital ward classes to purchase integrated private health insurance plans.143 Although individuals apply directly to private insurers, Medishield integrates coverage with the private insurance to provide a higher level of benefits.144 Additionally, Medisave may be used to pay part or all of the premiums for certain of these 138 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 713 (2001). 139 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 80 (2006). 140 Medishield Scheme, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/HealthCare/MSH.htm (last visited Nov. 25, 2007). 141 Id. 142 Id. 143 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 80-83 (2006). 28 integrated private health insurance plans.145 These integrated plans are fairly new and have yet to be adopted by many individuals. Problems with Medishield While Medishield provides access to catastrophic health coverage for most Singaporeans, the system has quite a few flaws. Like Medisave, Medishield actually provides little of the funding for the healthcare services in Singapore. Figure 3 shows that Medishield represents the smallest piece of healthcare funding at just 1.7% of total healthcare spending. Medishield’s limited role in providing health care funding results from adverse selection, its strictly limited schedule of benefits, and its exclusion of Singapore’s most costly health consumers.146 Medishield suffers from adverse selection because it is a voluntary program. Adverse selection describes the phenomenon in which higher risk individuals choose to purchase a particular level of health coverage while lower risk individuals opt to forego the higher level of coverage.147 Rather than allocating the catastrophic healthcare expenses across the broader population, only the larger healthcare consumers opt to purchase Medishield.148 Currently, Medishield covers only a little over half of Singapore’s population even though Singapore has attempted to combat adverse selection in a variety of ways.149 144 Medishield Scheme, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/HealthCare/MSH.htm (last visited Nov. 25, 2007). 145 Id. 146 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 80-83 (2006). 147 Id. 148 Id. 149 First, Singapore has made coverage very affordable for younger individuals to encourage people to join the plan early. Additionally, Singapore provides loyalty discounts of up to 40% for those who have been long-term Medishield participants. Finally, requiring an application to reinstate lapsed Medishield coverage and limiting coverage for pre-existing conditions further discourages adverse selection. See Medishield Scheme, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/HealthCare/MSH.htm (last visited Nov. 25, 2007). 29 The limited benefits provided by Medishield also contribute to Medishield’s limited role as a healthcare financing vehicle. Singapore designed Medishield to assist primarily with hospitalization benefits in the lower cost, government-subsidized wards.150 Due to government subsidies, the daily cost of the lower cost wards is very low.151 Since the benefit is based on these figures, the actual benefit paid does not result in high dollar claims even when staying in a premium ward.152 Further, the deductible for hospitalization services is very high.153 An individual utilizing government-subsidized wards would have an inpatient stay of 52 days before Medishield would pay any benefits at all.154 Singapore has recently expanded Medishield to provide first dollar coverage for a limited number of outpatient procedures and approved day surgeries.155 However, this change has not yet resulted in a marked increase in the role of Medishield in providing healthcare financing. Finally, Medishield’s role as a healthcare financing vehicle is limited by the fact that the plan is designed to deny coverage to some of Singapore’s most expensive healthcare consumers. Medishield coverage ends at age 85.156 Therefore, coverage terminates even though the elderly rank among those most in need of catastrophic coverage. Additionally, the government does not extend coverage to those that suffer serious pre-existing health conditions.157 If the coverage is 150 Medishield Scheme, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/HealthCare/MSH.htm (last visited Nov. 25, 2007). 151 Mukul G. Asher & Amarendu Nandy, Health Financing in Singapore: A Case for Systemic Reforms, 59 INT’L. SOC. SEC. REV. 75, 80-83 (2006). 152 Id.. 153 Id. 154 Id. 155 Medishield Scheme, http://mycpf.cpf.gov.sg/Members/Gen-Info/FAQ/HealthCare/MSH.htm (last visited Nov. 25, 2007). 156 Id. 157 Id. 30 extended, the government excludes the pre-existing condition which would ordinarily account for the bulk of the individual’s health care consumption.158 MediFund The third of the 3M’s, Medifund, seeks to fill a few of the health coverage gaps left by Medisave and Medishield. Medifund represents Singapore’s primary attempt to promote economic justice by ensuring that lower-income individuals receive necessary hospital care. The government implemented Medifund in 1993 only after it became clear that Medisave and Medishield still left some individuals unable to pay for health care services.159 Rather than discounting services for lower income individuals, Medifund assists with health care expenses much like a charity would.160 The government views Medifund as Singapore’s safety net for the poor and indigent unable to fund their health care via Medisave, Medishield or from their own monthly budgets.161 Unlike needs-based programs such as Medicaid in the United States, Medifund acts as an endowment fund.162 The fund awards grants to approved public hospitals and medical 158 Id. W. von Eiff, et al., Medical Savings Accounts: A Core Feature of Singapore’s Health Care System, 3 EUR. J. HEALTH. ECON. 188, 193 (2002). Cf. LEE KUAN YEW, FROM THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 2000 102 (HARPERCOLLINS 2000) (indicating that Medifund is for those who have exhausted other financing wources and no family to help them). 160 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 713 (2001). 161 Singapore Ministry of Health Medifund Scheme Frequently Asked Questions, http://www.moh.gov.sg/mohcorp/hcfinancing.aspx?id=308# (follow the “Check out the Frequently Asked Questions on Medifund” hyperlink) (last visited Oct. 27, 2007). 162 As a government endowment fund, Medifund’s financing structure differs a great deal from both Medisave and Medishield. Singapore only provides makes additional to contributions the fund if it has a budgetary surplus and continued economic growth. To ensure sustainability of the program, only the interest actually funds grants. See Singapore Ministry of Health Medifund Scheme Frequently Asked Questions, http://www.moh.gov.sg/mohcorp/hcfinancing.aspx?id=308# (follow the “Check out the Frequently Asked Questions on Medifund” hyperlink) (last visited October 27, 2007); W. von Eiff, et al., Medical Savings Accounts: A Core Feature of Singapore’s Health Care System, 3 EUR. J. HEALTH. ECON. 188, 193 (2002). Cf. LEE KUAN YEW, FROM 159 31 institutions.163 These organizations then administer the program by assessing eligibility, rendering health care services, and covering part of the costs of those services with the grant money.164 Private health care entities do not receive Medifund grants, nor can Medifund pay for treatment in most private facilities.165 Medifund operates more like a nationally-funded charity than a traditional government welfare program. By delegating the administration to outside entities, the government may enjoy administrative efficiencies as a result of not having to manage the day-to-day minutiae of the Medifund program. However, the government also cannot ensure that all individuals receive adequate health care in spite of inability to pay.166 Although individual hospitals or institutions assess the eligibility for receipt of Medifund assistance, Singapore’s government actually determines the eligibility criteria for participation in Medifund.167 The organizations receive applications for assistance on a per occurrence basis to treat a specific health need unlike Medicaid in the United States which provides assistance for any covered health condition while the participant remains eligible for the program. Eligibility primarily consists of means testing.168 However, Medifund also grants preference to those who regularly contribute to Medisave and who are covered by Medishield.169 Medifund also benefits THIRD WORLD TO FIRST THE SINGAPORE STORY: 1965 -2000 102 (HARPERCOLLINS 2000) (indicating that Medifund is for those who have exhausted other financing sources and have no family to help them). 163 Singapore Ministry of Health Medifund Scheme Frequently Asked Questions, http://www.moh.gov.sg/mohcorp/hcfinancing.aspx?id=308# (follow the “Check out the Frequently Asked Questions on Medifund” hyperlink) (last visited Oct. 27, 2007). 164 Id. 165 Id. 166 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 719 (2001). 167 Singapore Ministry of Health Medifund Scheme Frequently Asked Questions, http://www.moh.gov.sg/mohcorp/hcfinancing.aspx?id=308# (follow the “Check out the Frequently Asked Questions on Medifund” hyperlink) (last visited Oct.r 27, 2007). 168 Id. 169 Id. 32 the elderly who lack sufficient Medisave because it was implemented too late for them to accumulate sufficient funds.170 While these preference encourage personal responsibility, they may prevent Singapore’s most needy individuals from benefiting from the Medifund program.171 Medifund, like both Medisave and Medishield, really only assists with inpatient hospital expenses and a few outpatient specialist treatments.172 Individuals needing Medifund assistance, however, get to make far fewer choices regarding their own health care than those able to fund care through Medisave. In order to qualify for Medifund, individuals must choose a Medifund eligible public hospital or institution.173 Once accepted for Medifund care at one of these institutions, individuals must stay in a lower-cost, government-subsidized ward.174 In these wards, individuals cannot even choose their own doctors.175 Medisave, Medishield, and Medifund serve as the primary government-sponsored vehicles for financing health care. These programs, however, represent just a portion of Singapore’s system for providing basic health care services and controlling health care costs; Singapore actively controls and subsidizes the health care delivery system in Singapore. 170 Id. Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 719 (2001). 172 Singapore Ministry of Health Medifund Scheme Frequently Asked Questions, http://www.moh.gov.sg/mohcorp/hcfinancing.aspx?id=308# (follow the “Check out the Frequently Asked Questions on Medifund” hyperlink) (last visited Oct. 27, 2007). 173 Id. 174 Id. 175 SINGAPORE MINISTRY OF HEALTH, COMPARISON OF WARD CLASSES (2007), http://www.moh.gov.sg/mohcorp/uploadedFiles/News/Press_Releases/2001/14Sep2001A.pdf. 171 33 GOVERNMENT CONTROL OVER HEALTH CARE DELIVERY & PRICING The government of Singapore takes an active role not just in financing health care, but also in the delivery of health care.176 Singapore’s delivery role includes its subsidized public hospitals and primary care poly clinics.177 Additionally, the government actively disseminates both cost and quality information on health care services and providers.178 Finally, Singapore also attempts to exert control over health care pricing by controlling the supply of health care.179 Singapore’s 13 public hospitals and specialty centers provide 80% of all hospital services in the country.180 The government heavily subsidizes much of the care provided in the public hospitals.181 The public hospitals divide their beds into five ward types.182 As Table 3 indicates, the wards differ dramatically both in the subsidy rate and in the amenities offered to patients. While the clinical care provided in the wards does not differ, the spartan conditions in the heavily subsidized wards encourage individuals with greater means to self select the premium wards or private hospital care.183 Therefore, those able to afford more amenities do not exhaust subsidies necessary to provide care to the poor.184 Additionally 80 percent of the public hospital beds are 176 Singapore Healthcare System, http://www.moh.gov.sg/mohcorp/hcsystem.aspx?id=102 (last visited Nov. 27, 2007). 177 Id. 178 See Hospital Bill Size, http://www.moh.gov.sg/mohcorp/billsize.aspx (last visited Nov. 27, 2007) (providing an interactive comparison tool for hospital costs for common procedures). 179 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 716-720 (2001). 180 Hospital Services, http://www.moh.gov.sg/mohcorp/hcservices.aspx?id=394 (last visited Nov. 27, 2007). 181 SINGAPORE MINISTRY OF HEALTH, COMPARISON OF WARD CLASSES (2007), http://www.moh.gov.sg/mohcorp/uploadedFiles/News/Press_Releases/2001/14Sep2001A.pdf. 182 Id. 183 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 91 (2004). 184 Id. 34 in heavily subsidized C and B2 wards to ensure the poor adequate access to care.185 As a result the government actually subsidizes the cost of much of expensive hospital care enabling all in Singapore to receive care regardless of means.186 Table 3187 Comparison of Ward Classes Differences Ward Attached TV & Choice of Class Air-con Toilet/Showe Phone doctor r A Y Y Y Y B1 Y Y Y Y B2+ Y Y N N B2 N N N N C N N N N *More than 6 beds in open ward. No. of beds per Room 1-2 4 5 6 >6* Target subsidy rate Nil 20% 50% 65% 80% In addition to ensuring the poor access to hospital care, Singapore leverages its role as the leading health care provider to help regulate the supply of health services and to exert price pressure on the private health care market.188 Singapore influences both the supply of hospital beds and the introduction of technology and high cost medical treatments.189 The government also aggressively disseminates information not only on the costs of hospital services, but information on outcomes, as well.190 Additionally, Singapore places price caps not only on room 185 Hospital Services, http://www.moh.gov.sg/mohcorp/hcservices.aspx?id=394 (last visited Nov.27, 2007). Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 91 (2004). 186 187 SINGAPORE MINISTRY OF HEALTH, COMPARISON OF WARD CLASSES (2007), http://www.moh.gov.sg/mohcorp/uploadedFiles/News/Press_Releases/2001/14Sep2001A.pdf. 188 Hospital Services, http://www.moh.gov.sg/mohcorp/hcservices.aspx?id=394 (last visited Nov. 27, 2007). Hospital Services, http://www.moh.gov.sg/mohcorp/hcservices.aspx?id=394 (last visited Nov. 27, 2007). 190 See Hospital Bill Size, http://www.moh.gov.sg/mohcorp/billsize.aspx (last visited Nov. 27, 2007) (providing an interactive comparison tool for hospital costs for common procedures). 189 35 rates in the public hospitals, but also places caps on the costs of services such as surgeries.191 These caps place pressure on private providers to prevent uncapped escalation of private health care costs, as well.192 While the government role in primary care is more limited, the government provides about 20 percent of all primary care through its network of 18 polyclinics.193 Singapore’s robust system of more than 2,000 private clinics provides the remainder of primary care.194 “Each polyclinic serves as a one-stop health centre that provides outpatient medical care, follow-up of patients discharged from hospitals, immunisation, health screening and education, investigative facilities and pharmacy services.”195 The clinics provide heavily subsidized care with extra subsidies for children and the elderly.196 The average visit cost is only S$8.197 The government’s network of polyclinics ensure that lower-income Singaporeans have access to affordable primary care services, as well. LESSONS FROM SINGAPORE’S HEALTH SYSTEM At first glance, the flagships of the Singapore health system, the 3M’s, seem to offer little insight to the United States as it seeks to resolve its health care crisis. Combined, Medisave, Medishield, and Medifund finance only about 10 percent of health care. The lesson seems to be an instruction guide to constructing a system of universal health coverage that provides no 191 Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 716-720 (2001). 192 Id. 193 Primary Services, http://www.moh.gov.sg/mohcorp/hcservices.aspx?id=392 (last visited Nov. 27, 2007). 194 Id. 195 Id. 196 Id. 197 Id. 36 coverage. Nevertheless, this conclusion too readily discounts the effectiveness of Singapore’s health system when viewed as a whole. Singapore has constructed an extremely effective health care system that is a hybrid of both public and private payors. The 3M’s supplement a graduated series of subsidized medical care services that ensure no one in Singapore goes without care due to inability to pay. At the same time, the system encourages personal responsibility for individual health by leaving a portion of the payment for health care in the hands of the ultimate consumer rather than shifting the entirety of the burden to the government or third parties like employers. Personal responsibility is also supported by a system that provides individuals with the information needed to become effective health care consumers. Finally, the role of the government as a major player in the health care market allows it to exert price pressure on health care providers to prohibit unchecked growth in health care costs. IMPLEMENTATION DIFFICULTIES Duplicating Singapore’s multi-part system in the United States would prove difficult. Singapore became a nation in 1965, and its health plan was able to evolve in response to the growing needs.198 The United States will be forced to retrofit its current system to adapt to the needs of a new health system. Additionally, Singapore has the benefit of being a small citystate.199 Regulating health care supply and implementing a robust public health care system in a small essentially urban area is easier than trying to implement a similar system in a huge country that is a heterogenous mix of both rural and urban areas with very different socioeconomic levels 198 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 85 (2004). 199 Id. 37 and costs of living. Although wholesale adoption of the Singapore system is not a viable solution for the United States, Singapore offers some guidance that could be used in crafting the ultimate solution. First, the United States should eschew a solution that is either an entirely public or entirely private solution. A hybrid solution would allow the United States to tap the relative strengths of both public and private health care systems. Second, any possible solution to the health care crisis should decrease the reliance on employer-provided coverage. Finally, any possible solution should encourage the personal responsibility of health care consumers not just through cost-sharing, but through increased consumer education. PUBLIC-PRIVATE HYBRID HEALTH CARE SYSTEM A hybrid public and private system of health care remains the best solution to the United States health care crisis. Politician’s proposed solutions to the health care crisis often seem to represent polar opposites. At one extreme is a socialized health system reminiscent of Canada or the United Kingdom; at the other extreme is an entirely private system that relies on market forces to correct inefficiencies. The problem with each of these systems is that to adopt one system, the United States loses the benefits inherent in the other. Singapore has recognized the necessity of a balance between the two systems and leveraged the strengths of each in one integrated system.200 The United States already has a system that depends on both public and private payors for health care financing, yet has failed to exploit the benefits of each or integrate the systems. In both the United States and Singapore, public financing of health care rests around 25 percent of all health care financing. The way that each country uses the funding differs radically. 200 Id. 38 In the United States, public health care serves one part of the population, and private health care spending serves another. Public health care funding takes the form of a welfare benefit rather than subsidies on a particular service. This dichotomy prevents the public health care system from exerting any price pressure on the private sector. Instead, health care providers can pass on greater costs to the private health care system. In contrast, Singapore offers public health care to all at differing levels of subsidies. The care does not differ clinically, but in the amenities offered at that level. Individuals then self select the level of care that they can afford. In the resulting system, those who can pay more voluntarily choose to do so, reserving the highest subsidies and the lowest cost care for those who truly need it.201 Additionally while private health care providers can and do charge more than public providers in Singapore, they must exercise some level of cost control or risk losing patients to the public health care sector.202 Although it may be feasible in some large metropolitan areas, the United States is unlikely to be able to implement a system of national hospitals across the urban rural continuum in the United States to put price pressure on private providers. An alternative might be to allow the public to buy into health care plans that take advantage of the lower capitated rates for medical services already a part of the Medicaid and Medicare welfare benefits. If the underlying health care costs increase for private providers or in private insurer fee schedules, individuals could flock to the plans that use the public plan rates. This would allow the United States public health care system to exert similar price pressures on private providers that the Singapore public health care system does. 201 Id. Michael D. Barr, Medical Savings Accounts in Singapore: A Critical Inquiry, 26 J. HEALTH POL. POL’Y & L. 709, 716-720 (2001). 202 39 DECREASED RELIANCE ON EMPLOYER-PROVIDED HEALTH INSURANCE COVERAGE In order to make a plan such as this feasible, employees cannot be locked into employerprovided health insurance. Singapore does not rely on employers to provide the bulk of health insurance coverage; however, it still taps them as a source of health care financing. While Singapore employers may provide supplemental health insurance coverage if they desire, they do not bear the burden of being their employees’ entire safety net. Instead, employers make a relatively small tax payment as a percentage of wages paid into a fund for health coverage for the employee. The portion of the tax payment devoted to health funding represents no more than about 5 percent of wages. This tax burden pales in comparison to what employers must spend to provide health coverage to employees in the United States. Additionally, individuals can spend the funds on health insurance that they select from among both public and private insurance offerings without any negative tax ramifications. The problems with employer-provided coverage have reached epic proportions in the United States culminating in a growing number of uninsured individuals even among those with full-time jobs. Rather than forcing employers to provide health coverage to employees, the United States should require a small tax contribution with which workers can fund health insurance coverage that they choose from a variety of health insurance plans. Employers that desire to and can afford to provide more generous benefits can either purchase coverage that supplements basic health insurance plans or they can make an additional tax advantaged contribution with which workers can purchase more premium plans. INCREASED PERSONAL RESPONSIBILITY AND HEALTH CARE CONSUMERISM 40 Giving workers the ability to select between a variety of health plans based on a true view of both actual costs and coverage is the first of several steps in introducing greater personal responsibility for health care to individuals in the United States. Surprisingly, individuals in the United States and Singapore actually spend similar percentages out-of-pocket on health care. In the United States, out-of-pocket spending represents about 20 percent of health care spending. In Singapore, out-of-pocket spending represents about 25 percent of health care spending. Yet Singapore has much more engaged health care consumers. This suggests that the cost to consumers is not necessarily the most important factor in encouraging personal responsibility for health care. Some of the difference may be cultural and therefore difficult to duplicate. However, Singapore’s unified government message regarding personal responsibility for health is also an important factor. This message of personal responsibility is reflected in all communication pieces issued by the Ministry of Health, in health care cost and outcome information disseminated by the government, in the structure of the 3M’s, and even in patients interactions with the health care financing system. When seeking hospital care in a public hospital, patients are even counseled on the costs and levels of care available in different wards and how the care works into their respective budgets.203 The United States fails to issue any real message on personal responsibility, let alone a cohesive one. To encourage this sense of personal responsibility, the United States government needs to encourage a sense of ownership for health care in its communication with the population. Perhaps, the United States could encourage this communication process by including health care education as a small part of the public school 203 Meng-Kin Lim, Shifting the Burden of Health Care Finance: A Case Study pf Public-Private Partnership in Singapore, 69 HEALTH POL’Y 83, 85 (2004). 41 curriculum. In addition, the government needs to disseminate cost and outcome to individuals to allow them be effective consumers. The United States through its role in providing Medicare and Medicaid has some access to this kind of information and an ability to obtain more information. Compiling the data and making it accessible to individuals will allow the increased visibility into health care costs to become better health care consumers. CONCLUSION Singapore has crafted a very efficient health care system that provides some measure of universal coverage and a safety net for its poorest citizens, yet the system has helped control costs and minimize health care expenditures. Unfortunately, the system does not represent the panacea for the health crisis the United States faces currently. At the same time, aspects of Singapore’s system present promising possibilities as the United States seeks to craft its own solutions. First, the United States should not entirely abandon its current system that embraces both public and private health care delivery and financing. Second, the United States should reduce its reliance on employers as the primary source of health coverage. Finally, any successful United States health system needs a population that takes personal responsibility and ownership for its own health instead of viewing health care as an entitlement. 42