CVA
advertisement

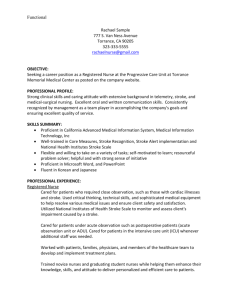
………………………………………………………………………… …………..TABLE OF CONTENTS TITLE PAGE NO. I. Introduction 1-2 II. Objectives 2-3 III. Nursing Assessment 1. Personal History 1.1. Patient’s Profile 3-4 1.2. Family and Individual Information 4 1.3. Level of Growth and Development IV. 1.3.1. Normal Development at Particular Stage 5-7 1.3.2. Ill Person at Particular Stage of Patient 8 2. Diagnostic Results 8-11 3. Present Profile of Functional Health Pattern 11-14 4. Pathophysiology and Rationale 14-22 Nursing Intervention 1. Care Guide of Patient 22-25 2. Actual Patient Care 2.1. Nursing Assessment 26-27 2.2. Nursing Care Plan 27-32 2.3. Drug Study 33-34 2.4. Health Teaching Plan 35-36 V. Evaluation and Recommendation 36 VI. Evaluation and Implication 36-37 VII. Referral and Follow –up 37-38 VIII. Bibliography 38-39 1 I. Introduction “Cerebrovascular disorders” is an umbrella term that refers to any functional abnormality of the central nervous system (CNS) that occurs when the normal blood supply to the brain is disrupted. It also refers to any functional or structural abnormality of the brain caused by a pathological condition of the cerebral vessels or of the entire cerebrovascular system. This pathology either causes hemorrhage from a tear in the vessel wall or impairs the cerebral circulation by a partial or complete occlusion of the vessel lumen with transient or permanent effects. Stroke is the primary cerebrovascular disorder and it is the third leading cause of death after heart disease and cancer and is the leading cause of disability among nations. Stroke is a term used to describe neurologic changes caused by an interruption in the blood supply to a part of the brain. The most common vessels involved are the carotid arteries and those of the vertebrobasilar system at the base of the brain. The two major types of stroke are ischemic and hemorrhagic. Ischemic stroke is caused by a thrombotic or embolic blockage of blood flow to the brain, with thrombosis being the main cause of both CVA’s and transient ischemic attacks (TIAs). A thrombotic CVA causes a slow evolution of symptoms, usually over several hours, and is “completed” when the condition stabilizes. An embolic CVA occurs when a clot is carried into cerebral circulation and causes a localized cerebral infarct. Ischemia may be transient and resolve within 24 hours, reversible with resolution of symptoms over a period of 1 week (reversible ischemic neurologic deficit [RINDI]), or progress to cerebral infaction with variable effects and degrees of recovery. Bleeding into the brain tissue or the subarachnoid space causes a hemorrhagic stroke. It is caused by other conditions such as a ruptured aneurysm, hypertension, arteriovenous (AV) malformations, or other bleeding disorders. Symptoms depend on distribution of the cerebral vessels involved. Ischemic strokes account for approximately 83% of all strokes. The remaining 17% of strokes are hemorrhagic. 2 Cerebrovascular disorder are the third leading cause of death in the United State. And in the Philippine setting, it ranked as the second leading causes of mortality with a 62.3 rate per 100,000 population in both sexes and with a percentage of 12.5 by the year 2002. Therefore, giving emphasis in the study of this disease condition is very relevant. Breakthroughs could happen and may help in the welfare of not just to Filipinos but to all people at risk in this condition. The advent of thrombolytic therapy for the treatment of acute ischemic stroke has revolutionized the care of the client following a stroke. Before, health care professionals could offer only supportive measures and rehabilitation to stroke survivors. New therapies can now prevent or limit the extent of brain tissue damage caused by acute ischemic stroke. Thrombolytic therapy must be administered as soon as possible after the onset of the stroke; a treatment window of 3 hours from the onset of manifestations has been established. To convey this sense of urgency regarding the evaluation and treatment of stroke, health care professionals now refer to stroke as brain attack. Public education is focused on prevention, recognition of manifestations, and early treatment of brain attack. II. Objectives Student Nurse General Objectives After 2 days of giving holistic nursing care to the patient who have viral meningitis, the nurse will be able to gain adequate knowledge, attitude and skills in taking care of a patient who is suffering from this disease condition. Specific Objectives After 8 hours of giving holistic nursing care, the nurse will be able to: 1. relate the patients history and level of growth and development 2. explain the significance of the diagnostic results 3. review the anatomy and physiology of the brain 3 4. explain the disease process and organ involved 5. compare the chart in classical and clinical symptoms of the disease process 6. formulated appropriate nursing care plan based on identified problem of patient 7. impart health teachings to the patient and significant others on viral meningitis Patient and Family General Objective After 2 days of nurse- client interaction the client and family will be able to acquire adequate knowledge, attitude and skills in the promotion of health and prevention of injuries and disease as well as rehabilitation from the condition. Specific Objective After 8 hours of giving holistic nursing care, the patient and significant others will be able to: 1. establish a trusting relationship with the nurse 2. verbalize feelings and thoughts to the nurse 3. share information about self and the family and life experiences to the nurse 4. explain the disease process in their own level of understanding 5. show willingness in the implementation of planned nursing care III. Nursing Assessment 1. Personal History 1.1Patient’s Profile Name: Lee, George Ang Age: 54 years Old 4 Sex: Male Civil Status: Married Religion: Buddhist Date of Admission: January 2, 2006 Room number: 221 Complaints: Right sided weakness and slurred speech Impression/Diagnosis: Cerebrovascular Accident (Bleed- left basal ganglia) Physician: Dr. M. Lim, Dr. W. Briones, Dr. G. Lim, Dr. E. Hernandez Hospital Number: 782349 1.2 Family and Individual Information, Social and Health History A case of Mr. George Ang Lee, 54 year old, male, Filipino and Buddhist. He is a businessman living at 515 MJ Cuenco Avenue, Cebu City. Patient is a known hypertensive for many years already with a usual blood pressure of 140/90. He has a maintenance medication when systolic blood pressure reaches to 170. He is non-diabetic and non-asthmatic. Inspite, his condition, he has no previous hospitalization until January 2, 2006 when he experienced a sudden onset of weakness at the right side of his body. Patient was later noted to be on the floor with slurred speech and drowsiness, then was rushed immediately to Chong Hua Hospital- Emergency Room and later transferred to Cebu Doctor’s University Hospital after basic diagnostic procedures were taken. CT Scan taken revealed 25 cc bleed at left basal ganglia with medial shift to the right. BP was noted to be elevated with highest BP at 190/110 and captopril was given. The patient doesn’t smoke and drink alcoholic beverages. His usual diet consist of vegetable and no meat. He also has a regular exercise schedule everyday but he has a strong heredofamilial disease of hypertension. His wife shared that lately his husband was under stress due to increase sales in their business on the month of December and missed to have his regular exercise and only sleeps a lesser hour per night compared to his usual sleep. 5 1.3 Level of Growth and Development 1.3.1 Normal Development at Particular Stage Physical Appearance Changes Hair begins to thin, and gray hair appears. Skin turgor and moisture decreases, subcutaneous fat decreases and wrinkling occurs. Fatty tissue is redistributed, resulting in fat deposits in the abdominal area. Cardiovascular Changes Blood vessels lose elasticity and become thicker. Gastrointestinal Changes Gradual decrease in tone of large intestine may predispose the individual to constipation. Sensory Perception Changes Visual acuity declines, often by the late forties, especially for near vision (presbyopia). Auditory acuity for high-frequency sounds (presbycusis) also decreases, particularly in men. Taste sensation also diminish. Metabolism Changes Metabolism slows, resulting in weight gain. Urinary changes Nephron units are lost during this time, and glomerular filtration rate decreases. Sexuality Changes Hormonal changes takes place. Musculoskeletal Changes Skeletal muscle bulk decreases at about age 60. Thinning of the intervertebral disks causes a decrease in height of about 1 inch. Calcium loss from bone tissue may occur. Muscle growth continues in proportion to use. 6 Psychosocial Erickson viewed the development tasks of middle-aged adult as generativity versus stagnation. Generativity is defined as the concern for establishing and guiding the nest generation. In other words, there is concern about providing for the welfare of humankind that is equal to the concern of providing for self. In middle age, the self seems more altruistic, and concepts of service to others and love and compassion gain prominence. These concepts motivate charitable and altruistic actions, such as church work, social work, political work, community fund-raising drives, and cultural endeavors. Marriage partners have more time for companionship and recreation; thus, marriage can be more satisfying in the middle years of life. Generative middle-aged persons are able to feel a sense of comfort in their life-style and receive gratification form charitable endeavors. Erickson believes that persons who are unable to expand their interests at this time and who do not assume the responsibility of middle age suffer a sense of boredom and impoverishment, that is, stagnation. These persons have difficulty accepting their aging bodies and become withdrawn and isolated. They are preoccupied with self and unable to give to others. Some may regress to younger patterns of behavior. Cognitive The middle-aged adult’s cognitive and intellectual abilities change very little. Cognitive processes include reaction time that stays much the same or diminishes during the later part of the middle years, perception, learning that continues and can be enhanced by increased motivation oat the time in life, memory and problem solving that are maintained through middle adulthood, and creativity. Middle-aged adults are able to carry out all the strategies described in Piaget’s phase of formal operations. operations strategies to assist Some may use post-formal them in understanding the 7 contraindications that exist in both personal and physical aspects of reality. The experiences of the professional, social and personal life of middle-aged persons will be reflected in their cognitive performance. Thus, approaches to problem solving and task completion will vary considerably in a middle-aged group. The middle-aged adult can “reflect on the past and current experiences and can imagine, anticipate, plan and hope” Moral According to Kohlberg, the adult can move beyond the conventional level to the postconventional level. Kohlberg believes that extensive experience of personal moral choice and responsibility is required before people can reach to postconventional level. Kohlberg found that few of his subjects achieved that highest level of moral reasoning. To move from stage 4, a law and order orientation, to stage 5, a social contract orientation, requires that the individual move to a stage in which rights of others take precedence. People in stage 5 take steps to support another’s right. Spiritual Not all adults progress through Fowler’s stages to the fifth, called the paradoxical-consolidative stage. At this stage, the individual can view the “truth” from a number of viewpoints. Fowler’s fifth stage corresponds to Kohlberg’s fifth stage of moral development. Fowler believes that only some individuals after the age of 30 years reach this stage. In middle age, people tend to be less dogmatic about religious beliefs, and religion often offers more comfort to the middle-aged person than it did previously. People in this age group often rely on spiritual beliefs to help them deal with illness, death and tragedy. 8 1.3.2 The Ill Person at a Particular Stage of Patient The three most common causes of death in older adults are heart disease, cancer and stroke. Other frequently reported causes of death are lung disease, accidents/falls, diabetes, kidney disease, and liver disease. Heart disease is the leading cause of death in older adults. Common cardiovascular disorders are hypertension and coronary artery disease. Cancer or malignant neoplasms are the second most common cause of death among older adults. Cerebrovascular accidents, the third leading cause of death, occurring as brain ischemia or brain hemorrhage. Cigarette smoking has been recognized as a risk factor in the four most common cause of death for older adults: heart disease, cancer, stroke and lung disease. Dental carries, gingivitis, broken or missing teeth and ill-fitting or missing dentures may affect nutritional adequacy, cause pain, and lead to infection. 2. Diagnostic Results Diagnostic Test Normal Values Patient’s Significance Result Hematology Hemoglobin 11.5-16 g/dl 11.5 g/dl Normal Hematocrit 35-49 vol % 35 vol % Normal 4.5-5.3x10^6/dl 4.73x10^6/dl Normal RBC Elevated WBC 4.5-15.0x10^3/dl 12.2x10^3/dl in acute disease. Source: Brunner and Suddarth’s Textbook of Medical – Surgical Nursing, 9th Ed. Smeltzer, Suzanne C. Bare, Brenda G., p.1954 MCV 72-98 fl. 91 fl. Normal MCH 25-35 pg 30.3 pg Normal MCHC 30-37 g/dl 33.3 g/dl Normal 9 Platelets 150,000-450000 361,000 cu/mm Normal 84% Elevated cu/mm Segmenters 54-62% in acute disease. Source: Brunner and Suddarth’s Textbook of Medical – Surgical Nursing, 9th Ed. Smeltzer, Suzanne C. Bare, Brenda G., 1953 Eosinophils 1-3% 01% Normal 25-33% 10% Normal Yellow Yellow Normal Clear Slightly cloudy 5.5-7.5 6.0 Normal 1.001-1.045 1.020 Normal Protein Negative Trace Not normal Glucose Negative Negative Normal Ketones Negative Negative Normal Blood Negative Negative Normal RBC <3 RBC’s/HFF 0-1 Normal WBC 0-5 WBC/ HPF 3-5 Normal Epithelial Cells Rare Few Normal Mucus Threads Rare Rare Normal Bacteria None Negative Normal Leukocytes Negative Negative Normal Nitrites Negative Negative Normal Trace Normal Normal Negative Negative Normal Lymphocytes Urinalysis Macroscopic Color Appearance Reaction Specific gravity Not normal Macroscopic Urobilinogen Bilirubin 10 Serum Glucose 65-110 142 Increased in infections Source: Brunner and Suddarth’s Textbook of Medical – Surgical Nursing, 9th Ed. Smeltzer, Suzanne C. Bare, Brenda G., 1960 Creatinine .7-1.5 .9 Normal Sodium 137-145 137 Normal Potassium 3.6-5.0 4.6 Normal Chloride 98-107 103 Normal Calcium 8.4-10.2 8.8 Normal ELECTROCARDIOGRAPHIC REPORT Atrial Rate: 120/min. Ventricular: 120/min. PR Interval: 0.14 sec. QRS Complex: Transition zone in V3-V4 ST Segment: Isoelectric T-wave: Upright QRS: 0.08 sec. AXIS: 0 degree P-wave: upright Interpretation: Sinus tachycardia with non specific ST-T wave changes ECHOCARDIOGRAPHY REPORT 1. Quality of study- Optimal 2. Sinus Tachycardia- 107 beats/ min 3. Cardiac Measurements- IVSd= 1.05 cm LVIDd= 5.75 cm LVPWd= 1.67 cm LVIDs= 3.89 cm 11 Ejection Fraction= 61% Ao rest= 2.97 cm LA diameter= 3.40 cm 4. Cardiac Values: normal 5. Color and Doppler exam- Normal Pulmonic Valve/ Aortic/ left ventricular outflow tract velocities. Normal mitral inflow pattern. 6. Left Ventricular Systolic Function- preserved global and regional with visual ejection fraction estimate 70%. 7. Right Ventricular Systolic Function- preserved 8. No pericardial Effusion CONCLUSION: 1. Well preserved biventricular systolic function. 2. Left ventricular hypertrophy. 3. Mild diastolic dysfunction. CT SCAN IMPRESSION: (as compared to the previous study done January 6, 2006.) 1. Further interval decrease in volume and density of the intraparenchymal (hemorrhage in the left putamen/ left external capsule now measuring approximately 34cc in volume (previous was 39cc), as described above. 2. Slight further decrease in the small amount of intraventricular hemorrhage (extension) within the lateral ventricular. 3. No change in the subfalcine deviation (midline shift) to the right, still by 0.6 cm. 4. Chronic lacunar infarct in the right thalamus. 3. Present Profile of Functional Health Patterns 3.1 Health perceptions/ Health management According to Mr. Lee’s wife, his husband take a great deal with regards to his health. He disciplined his self well to achieve an optimum health cause he 12 believes in the saying “health is wealth”. He values it well enough since it’s something that gives him greater favor in his business. Whenever he experiences sickness he manages it using Chinese herbal medications. Mrs. Lee believes that her husband will recover gradually because he is a determined and disciplined person who strongly value his health. As of the moment, the family religiously follows the doctor’s instruction in restoring Mr. Lee’s health. 3.2 Nutritional/Metabolic pattern According to Mrs. Lee, prior to admission, patient usually eats 3 meals a day which usually consist of vegetables and fruits, rice, and less meat but more on fish. He usually drinks tea every after meal or whenever he feels drinking. He has no allergies to foods. His water consumption is replaced with tea. He has Chinese drug supplements and has a maintenance medication for his hypertension. Currently, he is on nasogastric tube feeding (blenderized) with 1800 calories in 1800 u volume. He is also allowed to take sip of water with strict aspiration precaution. 3.3 Elimination Patterns According to Mrs. Lee, before her husband’s admission, Mr. Lee voids and defecates normally and has no problems/complaints in defecating and urinating. He defecated about once a day usually at the morning. In the hospital he is on diaper and lactulose is given to soften his stool. His skin is dry and rough because he can’t take a bath but lotion is given to prevent further dryness. 3.4 Activity/ Exercise Pattern According to Mrs. Lee, before her husband’s admission, his usual activity is managing and supervising his own wholesale business of different stuffs. He helps in transferring boxes from the truck to the stock rooms, without any complaint of dyspnea or fatigue after. Every morning he takes time to go to his 13 gym and exercise. And during breakfast he reads newspaper or watch news from television. Currently, in the hospital passive exercise is done by Mrs. Lee or the Private Nurse. Turning on the television whenever he is awake is recommended by the doctor to rehabilitate his senses. 3.5 Cognitive/Perceptual Pattern According to Mrs. Lee, her husband manages to read newspaper without the aid of eye glasses, he still has a 20/20 vision and can also hear clearly prior to admission. He was also able to comprehend well. But at the moment, he doesn’t respond to any questions asked of him, he can’t speak yet. But he can show some facial expressions like grimacing his face whenever he feels pain at some parts of his body. 3.6 Rest/ Sleep Pattern According to Mrs. Lee, he sleeps about 7 hours a day, usually goes to bed early around 9 PM and arises early as well around 4 AM. He has no problems or difficulty in sleeping. Before sleeping he usually pray with his Buddha beads. In the hospital he sleeps most of the time, waking up occasionally. He is drowsy. 3.7 Self- Perception Pattern According to Mrs. Lee, he is a very responsible father to his children as well as a good husband to her. She believes that Mr. Lee is also cooperating for his quick recovery since he is looking forward to visit his relatives in China as soon as he gets well. 3.8 Roles- Relationship Pattern According to Mrs. Lee, he speaks Bisaya and Mandarin. He can’t speak at the moment yet. He has 3 children. The two has a family of their own already 14 and is presently residing in China. One son ,the eldest who is still single, is left in Cebu with them who’ll take care of him at the hospital. In time of needs he usually turns to his wife 3.10 Coping- Stress Management Pattern According to Mrs. Lee, whenever problems occur especially with business matters, both of them are solving it but most of the time his decision influenced a lot. He also have his friends and relatives who’ll listen and advices him. He also has a strong faith that he always pray whenever he has problems. Mrs. Lee decided to have a private nurse to monitor his husband closely. 3.11 Values- Belief System According to Mrs. Lee, they are Buddhist. They are religious in the practices and faith of the Buddhist. Most spare time of Mr. Lee is spend in prayers. They have their prayer room at the house. They are also active in their temple activities and tries not to miss it. In the hospital they requested to play a Buddhist chant which they believe could help him recover early. They also have incenses that can soothe or make him sleep well. 4. Pathophysiology and Rationale 4.1 Normal Anatomy and Physiology of Organ System Affected The Nervous system is the body’s most organized and complex structural and functional system. It profoundly affects both psychological and physiologic function. The brain is the largest and most complex part of the nervous system. It is composed of more than 100 billion neurons and associated fibers. The brain tissues have a gelatin-like consistency. This semi-solid organ weighs about 1400 g in the adult. It is divided into three major areas: 15 the cerebrum, the brain stem and the cerebellum. The cerebrum is composed of two hemispheres, the thalamus, the hypothalamus and the basal ganglia and connections of the olfactory and optic nerves. The brain stem includes the midbrain, pons, medulla, and connections of cranial nerve II, IV and VII. The cerebellum is located under the cerebrum and behind the brain stem. The BASAL GANGLIA consist of several structures of subcortical gray matter buried deep in the cerebral hemisphere. These structures include the caudate nucleus, putamen, globus pallidus, substantia nigra, and subthalamic nucleus. The basal ganglia serve a processing stations linking the cerebral cortex to thalamic nuclei. Almost all the motor and sensory fibers connecting the cerebral cortex and the spinal cord travel through the white matter pathways near the caudate nucleus and putamen ganglia. These pathways are known as the internal capsule. The basal ganglia, along with the corticospinal tract, is important in controlling complex motor activity. CEREBRAL CIRCULATION. The cerebral circulation receives approximately 15% of the cardiac output, or 750 ml per minute. The brain does not store nutrients and has a high metabolic demand that requires the high blood flow. The brain’s blood pathway is unique because it flows against gravity; it’s arteries fill from below and the veins drain from above. In contrast to other organs that may tolerate decreases in blood flow because of their adequate collateral circulation, the brain lacks additional collateral blood flow, which may result in irreversible tissue damage when blood flow is occluded for even short periods of time. 16 Brain: Basal ganglia Coronal slices of human brain showing the basal ganglia, globus pallidus: external segment (GPe), subthalamic nucleus (STN), globus pallidus: internal segment (GPi), and substantia nigra (SN). Coronal section of brain immediately in front of pons. (Not all basal ganglia are visible, but caudate nucleus and substantia nigra are labeled. Subthalamic nucleus would be between thalamus and internal capsule.) 4.2 Schematic Drawing on Pathophysiology of Disease 17 Predisposing Factors Precipitating Factors Heredity Age – 54 years old History of stroke Stress High sodium diet High blood pressure Etiology Plaque formation Thrombi formation Bloodstream is loaded High blood pressure Dislodgment of thrombi Emboli Occlusion of cerebral vessels and Rupture of arteriosclerotic hypertensive vessels Hemorrhage Cerebral anoxia CVA Clinical symptoms Facial asymmetry Slurring of speech Aphasia Hemiparesis Classical symptoms Facial asymmetry Slurring of speech Aphasia Hemiparesis Apraxia Hemiplegia Confusion 18 4.3 Disease process and Effects on Different Organ System Stroke, ischemic damage of the brain owing to a blockage in blood flow, or to a hemorrhage of blood vessels in the brain. Without blood, sections of brain tissue quickly deteriorate or die, resulting in paralysis of limbs or organs controlled by the affected brain area. Most strokes are associated with high blood pressure (hypertension), atherosclerosis (development of fatty plaques in artery walls), or both. Some of the signs of major stroke are facial weakness, inability to talk, loss of bladder control, difficulty in breathing and swallowing, and paralysis or weakness, particularly on one side of the body. Stroke is also called cerebral apoplexy and cerebrovascular accident. The majority of stroke cases are due to arterial blockage caused by either thrombosis or embolism. Thrombosis involves the clotting of the surface of an atherosclerotic plaque, in a branch of one or more of the four main arteries leading to the brain. As these arteries become narrowed, a potential stroke victim often experiences recurrent warnings, which take the form of transient paralysis (such as in one arm or leg or on one side of the face), or discovers impairments in speech, vision, or other motor functions. At this stage, deposits in the linings of the cerebral arteries can often be treated by surgical removal or bypass of blockages. Embolism occurs when a cerebral artery suddenly becomes blocked by material—such as clotted blood, air, or fat—coming from another part of the bloodstream. Such masses, known as emboli, often form as clots in a diseased or malfunctioning heart, but can also come from dislodged fragments of atherosclerotic plaque or even an air bubble. Treatment is largely preventive, consisting of monitoring of the diet, and, if possible, use of anticoagulants. Hemorrhaging of cerebral blood vessels, a less frequent but usually more serious cause of stroke, can occur where aneurysms, or blister-like bulges, develop on the forks of large cerebral arteries on the brain surface. The rupture of aneurysms causes brain damage, owing to the seepage of blood into brain tissue or to the reduced flow of blood to the brain beyond the point of rupture. 19 4.4 Comparative Chart Classical Symptom Clinical Symptom Rationale a. Motor changes: contralateral hemiparesis or hemiplegia hemiplegia; - affectation in the middle cerebral artery Sensory changes: contralateral contralateral hemisensory hemisensory alterations; alterations neglect of involved extremities; Visual changes: homonymous hemianopia; inability to turn eyes toward the affected side; Speech changes: dyslexia, Dysphagia, aphasia dysgraphia, aphasia; Others: vomiting may occur b. Motor changes: contralateral hemiparesis, foot Footdrop, contralateral - affectation in the anterior and leg deficits greater than hemiparesis cerebral artery arm, footdrop gait disturbances; Sensory changes: contralateral Contralateral hemisensory alterations; hemisensory alteration Visual changes: deviation of eyes toward affected side; Speech changes: expressive Expressive aphasia aphasia; Mental changes: confusion, Amnesia, shortened amnesia; flat affect, apathy; attention span shortened attention span; loss 20 of mental acuity; Others: apraxia (inability to carry out purposeful movements in nonaffected areas) c. Motor changes: mild contralateral hemiparesis (with Memory deficit thalamic or subthalamic - affectation of the posterior cerebral artery involvement); intention tremor; Sensory changes: diffuse sensoryloss (thalamic); Visual changes: papillary dysfunction (brain stem); loss of conjugate gaze, nystagmus; loss of depth perception; cortical blindness; homonymous hemianopia; Speech changes: perseveration; dyslexia; Mental changes: memory deficits; Others: visual hallucinations d. Motor changes: contralateral hemiparesis with Contralateral hemiparesis - affectation of the internal facial asymmetry; dysarthia; dysphagia carotid artery Sensory changes: contralateral sensory alterations; Visual changes: hemianopia; ipsilateral periods of blindness 21 (amaurosis fugax); Speech changes: dysphagis; Others: mild Horner’s syndrome; carotid bruits e. Motor changes: alternating Dysarthia, dysphagia, - affectation of the motor weaknesses; ataxic gait, temporary memory loss, vertebral – basilar system dysmetria (uncoordinated disorientation actions); Sensory changes: numbness of the tongue; Visual changes: double vision; homonymous hemianopis; nystagmus, conjugate gaze paralysis; Speech changes: dysarthia; dysphagia; Mental changes: memory loss; disorientation; Others: drop attacks; tinnitus, hearing loss f. Motor changes: Ipsilateral None - affectation of the ataxia; facial paralysis; anteroinferior cerebellar Sensory changes: ipsilateral (lateral pontine) loss of sensation in face, sensation changes on trunks and limbs; Visual changes: nystagmus; Others: Horner’s syndrome; tinnitus, hearing loss 22 g. Motor changes: ataxia; Dysarthia, dysphagia, - affectation of the paralysis of larynx and soft coughing, hiccoughs. posteroinferior cerebellar palate; Sensory changes: ipsilateral loss of sensation on face, contralateral on body; Visual changes: nystagmus; Speech changes: dysarthia; dysphagia; dysphonia; Others: Horner’s syndrome; hiccoughs and coughing IV. Nursing Interventions 1. Care Guide of Patient with Disease Condition IDENTIFY STROKE EARLY. A critical factor in the early intervention and treatment of stroke is the proper identification of stroke manifestations. The initial assessment of the client who is thought to have had a stroke includes level of consciousness, papillary response to light, visual fields, movement of extremities, speech, sensation, reflexes, ataxia, and vital signs. This data are recorded and scored on the Glasgow Coma Scale. Intracranial pressure is also monitored, the baseline pressure values and waveforms should be noted. MAINTAIN CEREBRAL OXYGENATION. Always maintain a patent airway. The client should be turned on the affected side if he or she is unconscious, to promote drainage of saliva in the airway. The collar of the shift should be loosened to facilitate venous return. The head should be elevated, but the neck should not be flexed. Oxygen should be supplied an if the client demonstrates poor ventilatory effort, intubation and mechanical ventilation may be required to prevent hypoxia and increased cerebral ischemia. ECG is performed and blood pressure is evaluated, and hypertension may be reduced with vasodilators. Caution is exercised when treating blood pressure, as 23 lowering the blood pressure too far may lower cerebral perfusion pressure and increase cerebral ischemia. Laboratory test for hematology, chemistry and coagulation are obtained to rule out stroke-mimicking conditions and to detect bleeding disorders that would increase the risk of bleeding during thrombolytic therapy. PREVENT COMPLICATION. Such as bleeding, cerebral edema, stroke recurrence, aspiration and other potential complication. REHABILITATION AFTER STROKE. Early premobilization efforts are aimed at preventing the complications of neurologic deficit and immobility. Relearning can take place even though damage in the CNS is irreversible. It is extremely important that relearning take place as soon as possible after the injury. An interdisciplinary rehabilitation team is necessary to assist and support clients and their families during this time. The recommended plan of care includes using interdisciplinary services to : document the client’s condition and course fully, including deficits, status of other disease, complications, changes in status, and functional status before stroke. Begin physical activity as soon as the client’s medical condition is stable; use caution with early mobilization in clients with progressing neurologic deficit, subarachnoid or intracerebral hemorrhage, severe orthostatic hypotension, acute myocardial infarction, or acute deep vein thrombosis Assist n managing general health functions throughout all stages of treatment such as managing dysphagia, nutrition, hydration, bladder and bowel function, sleep and rest, co-morbid conditions, and acute illnesses. Prevent complications, including deep vein thrombosis and pulmonary embolism, aspiration, skin breakdown, urinary tract infections, falls, spasticity and contractures, shoulder injury and seizures. Prevent recurrent strokes through control of modifiable risk factors, oral anticoagulation, antiplatelet therapy, or surgical intervention. Assess throughout acute and rehabilitation stages Use reliable standardized instruments for evaluation Evaluate for formal rehabilitation during acute stage 24 Choose individual or interdisciplinary program based on the client’s and family’s needs; success of the program requires full support and active participation of the client and family; families must be involved at the outset Choose the local rehabilitation program that best meets the client’s and family’s needs INTERDISCIPLINARY MANAGEMENT. Physical therapy, occupational therapy, speech therapy. PHARMACOLOGIC MANAGEMENT. Steroids and osmotic diuretics may be used to reduce ICP. Hypertension is commonly controlled with antihypertensives and diuretics. Anticoagulants are commonly used initially through intravenous routes and then orally. Monitoring of clotting times is important for preventing overanticoagulation, which increases the risk of bleeding. Headache and neck stiffness can usually be treated with mild analgesics, such as codeine and acetaminophen. Stronger narcotics are usually avoided; these agents sedate the client and can make neurologic assessment inaccurate. If the client develops seizures, phenytoin (Dilantin) or Phenobarbital may be used. Barbiturates and other sedative agents are avoided. If the client develops fever, antipyretics may be prescribed. DIETARY MANAGEMENT. Because of the high risk for aspiration; choking, excessive coughing, and vomiting, oral food and fluids are generally withheld for 24 to 48 hours. If the client cannot eat or drink after 48 hours, alternative feeding routes are used, such as tube feedings or hyperalimentation. When the swallowing mechanism has returned, the client can be fed orally. SURGICAL MANAGEMENT. Several criteria are used to determine candidates for rapid evacuation of hematoma in clients with hemorrhagic stroke or bleeding on the dominant side. Another guide commonly used in the determination of the need for surgery is ICP. Pressures below 20 mm HG are usually managed without surgery; pressures above 30 mm Hg often require surgery. Clients who have large areas of blood removed have been shown to recover a substantial portion of speech. Clients with relatively large areas of 25 superficial cerebral bleeding or shifts may also require surgery. Likewise, clients who suddenly deteriorate to from lethargy to unconsciousness may benefit from surgery. Surgery is usually not performed on clients with bleeding in the basal ganglia or thalamus. Surgery is also performed on some intracranial aneurysms and on the carotid arteries (carotid endarterectomy) to reduce the risk of CVA. NURSING MANAGEMENT. The initial assessment of the client with CVA is very important. The assessment must be complete and accurate to provide a baseline for ongoing assessments. The client who is awake and alert should be taught about the pathologic process and instructed to inform the nurse about any changes in sensation, movement, or function regardless of how minor they may seem. Increasing neurologic deficits may indicate either progression of the infarct or ischemia of the area from cerebral edema or bleeding. Changes in neurologic assessments must be reported promptly to the physician. A complete history of the presenting problem as well as past medical and social history will provide data about the problem source of the CVA. Ongoing assessments of the neurologic status and vital signs are imperative. These assessments may be required as often as hourly for unstable clients. Assessment of hemiplegia includes the repeated assessment of motor function, sensation, and reflex activity. 26 2. Actual Patient Care 2.1 Nursing Assessment Name of Patient: Mr. George Ang Lee Impression/Diagnosis: Cerebrovascular accident Attending Physician: Dr. M. Lim, Dr. W. Briones, Dr. G. Lim, Dr. E. Hernandez ACTIVITY/REST Difficulty with activity due to generalized weakness, loss of sensation, or paralysis (hemiplegia) tires easily; difficulty resting. Altered muscle tone and level of consciousness. Incoherent. CIRCULATORY Electrocardiogram (ECG) changes. Elevated BP 160/100. strong peripheral pulses. EGO INTEGRITY Feelings of helplessness and hopelessness, emotional liability an inappropriate response to anger, sadness and happiness, difficulty expressing self. ELIMINATION Constipated. FOOD/ FLUID Mastication problems. Loss of sensation in tongue, cheek. NEUROSENSORY Weakness on the right side of the body, drowsy, sensory loss on contralateral side (right side of body) in extremities and some part of the left face. Disturbances in senses of taste and smell. Aphasia: defect or loss of language function may be global. PAIN/ DISCOMFORT Guarding behavior on the GUT (scrutom). RESPIRATION On tracheostomy. 27 SAFETY Swallowing difficulty, inability to meet own nutritional needs. Diminish response to heat and cold. SOCIAL INTERACTION Speech problems, inability to communicate. TEACHING/LEARNING Family history of hypertension, strokes. Requires medication regimen/ therapeutic treatments. 2.2 Nursing Care Plan Name of Patient: Mr. George Ang Lee Age: 5 4 Room/Ward: 221 Sex: Male Chief Complaints: Right sided weakness and slurred speech Needs/ Problems/ Cues NCP 1 Subjective: no subjective cues Objective: -on semiFowler’s position -with NGT in place -with D5NSS 1L @ 20 gtts/min -with O2 @ 2LPM -with Nursing Scientific Objectives Nursing Diagnosis Basis of Care Intervention After eight hours of nursing interventions, the patient will be able to maintain usual/ improved level of consciousnes s, cognition, and motor sensory function. Specifically, he shall be able to: 1.demonstrat e stable vital signs and absence of Independent 1. Determine factors related to individual situation/ cause for decreased cerebral perfusion, and potential for increased ICP. Cerebral infarction cerebral is deprivation tissue of blood perfusion supply to a localized related to area of the interruption brain. The extent of of blood infarction flow depends on factors (occlusive such as the disorder / location and the size hemorrhag of an e) occluded vessel and the adequacy of Altered 2. Monitor/ document neurologic status frequently and compare with baseline. Rationale 1. Influences choice of interventions. Deterioration in neurologic signs and symptoms or failure to improve after initial insult may require surgical intervention and/or that the patient be transferred to critical care area for monitoring of ICP. (Doenges,p293) 2. Assesses trends in LOC and potential for increased ICP and is useful in determining location, extent, and progression/ resolution of CNS damage. May 28 FBC-UB -lethargy noted -slurring of speech noted -with the ff. V/S: BP – 170/100 mm Hg PR – 90 bpm RR – 24 cpm T – 37.5*C collateral circulation to the area supplied by the occluded vessel. If cerebral circulation is interrupted extensively , cerebral anoxia develops, that is, lack of oxygen to the brain. (Black:199 any signs of increased ICP. 2.displays no further deterioration/ recurrence of deficits. also reveal presence of TIA, which may warn of impending thrombotic CVA. (Doenges p293) 3. Monitor vital signs, note: - Hypertension / hypotension, compare BP readings in both arm. 3,p707) - Heart rate and rhythm, auscultate for murmurs. - Respirations, noting patterns and rhythm, e.g., periods of apnea after hyperventilation. 4. Document changes in vision. 3. Variations may occur because of cerebral pressure / injury in vasomotor area of the brain. Hypoertension or postural hypotension may have been a precipitating factor. Hypotension may occur because of shock (circulatory collapse). Increased ICP may occur (tissue edema, clot formation). Subclavian artery blockage may be revealed by difference in pressure readings between arms. - Changes in rate especially bradycardia can occur because of the brain damage. Dysrhythmias and murmurs may reflect cardiac disease, which may have precipitated CVA. - Irregularities can suggest location of cerebral insult/ increasing ICP and need for further intervention, including possible respiratory support. (Doenges,p293) 4. Specific visual alterations reflect are of brain involved, indicate safety concerns, and influence choice of interventions. (Doenges,p293) 29 5. Assess higher functions, including speech, if patient is alert. 5. Changes in cognition and speech content are indicator of location/ degree of cerebral involvement and may indicate deterioration / increased ICP. (Doenges,p293) 6. Position with head slightly elevated and in neural position. 6. Reduces arterial pressure by promoting venous drainage and may improve cerebral circulation/ perfusion. (Doenges,p293) 7. Maintain bed rest; provide quiet environment. Provide rest periods in between care activities, limit duration of procedures. 7. Continual stimulation/ activity can increase ICP. Absolute rest and quiet may be needed to prevent rebleeding in the case of hemorrhage. 8. Prevent straining at stool, holding breath. 8. Valsalva maneuver increases ICP and potentiates risk of rebleeding. (Doenges,p293) 9. Assess for nuchal rigidity, twitching, increased restlessness, irritability, onset of seizure activity. 9. Indicative of meningeal irritation, especially in hemorrhagic disorders. Seizures may reflect increased ICP/ cerebral injury, requiring further evaluation and intervention. (Doenges,p293) Collaborative 1. Administer supplemental oxygen as indicated. 2. Administer 1. Reduces hypoxemia, which can cause cerebral vasodilation and increase pressure/ edema formation. (Doenges,p293) 2. Preexisting / chronic 30 medications (Antihypertensive) as indicated. hypertension requires cautious treatment, because aggressive management increases the risk of extension of tissue damage. (Doenges,p293) 3. Monitor lab studies as indicated, e.g., PT/PTT time. 3. Provides information about drug effectiveness/ therapeutic level. (Doenges,p293) NCP2 Subjective: -no subjective cues Objective: -on semiFowler’s position -with NGT in place -with D5NSS 1L @ 20 gtts/min -with O2 @ 2LPM -with FBC-UB -lethargy noted -slurring of speech noted -inability to purposely move noted Impaired physical mobility related to paralysis Hemiplegia results from damage to the motor area of the cortex or pyramidal tract fibers. Hemorrhag e or clot in the brain’s left side causes right-sided hemiplegia, and viceversa. This is because the nerve fibers cross over in the pyramidal tract as they pass from the brain to the spinal cord. (Black:199 3,p709) After eight hours of nursing interventions, the patient will be able to maintain optimal position of function. Specifically, he shall be able to: 1.demonstrat e absence of contractures, footdrop. 2.maintain/ increase strength and function of affected or compensator y body part 3. maintain in integrity. Independent 1. Assess functional ability/ extent of impairment initially and on a regular basis. 1. Identifies strengths/ deficiencies and may provide information regarding recovery. Assist in choice of interventions, because different techniques are used for flaccid or spastic paralysis. (Doenges,p296) 2. Change position at least every two hours and possibly more often when place on affected side. 2. Reduces risk of tissue ischemia/ injury. Affected side has poorer circulation and reduced sensation and is more predisposed to skin breakdown / decubitus. (Doenges,p296) 3. Begin active/passive ROM to all extremities on admission. Encourage exercises such as squeezing rubber ball, extension of fingers and legs/ feet. 3. Minimizes muscle atrophy, promotes circulation, helps prevent contractures. Reduces risk of hypercalciuria and osteoporosis if underlying problem is hemorrhage. (Doenges,p296) -impaired 31 coordinati on noted 4. Elevate arm and hand. 4. Promotes venous return and helps prevent edema formation. (Doenges,p296) 5. Place knee and hip in extended position. 5 Maintains functional position. (Doenges,p296) -limited ROM noted -decreased muscle strength and control observed Collaborative 1. Provide egg crate 1. Promotes even mattress, as indicated. weight distribution decreasing pressure on bony points and helping prevent skin breakdown/ decubitus formation. (Doenges,p296) -with the ff. V/S: BP – 170/100 mm Hg PR – 90 bpm RR – 24 cpm T – 37.5*C 2. Consult with physical therapist regarding active, resistive exercises, and patient ambulation 2. Individualized program can be developed to meet particular needs/ deal with deficits in balance, coordination and strength. (Doenges,p296) NCP3 Subjective: -no subjective cues Self-care deficit (inability to Objective: -on semiFowler’s position perform -with NGT in place paralysis. -with D5NSS 1L @ 20 gtts/min -with O2 @ 2LPM -with ADLs) related to Hemiplegia results from damage to the motor area of the cortex or pyramidal tract fibers. Hemorrhag e or clot in the brain’s left side causes right-sided hemiplegia, and viceversa. This is because the nerve fibers cross After eight hours of nursing interventions, the patient will be able to perform self-care activities within level of own ability. Specifically, he shall be able to: 1.demonstrat e techniques/ lifestyle changes to meet selfcare needs. Independent 1. Assess abilities and level of deficit for performing ADLs. 1. Aids in anticipating for meeting individual needs. (Doenges,p302) 2. Avoid doing things for the patient that the patient can do. 2. These patients may become fearful and dependent, and although assistance is helpful in preventing frustration, it is important for the patient to do as much as possible for self to maintain self esteem and promote recovery. (Doenges,p302) 3. Be aware of impulsive behaviors/ 3. May indicate need for additional 32 FBC-UB -lethargy noted -slurring of speech noted -inability to purposely move noted -impaired coordinati on noted -limited ROM noted -decreased muscle strength and control observed -inability to perform ADLs observed over in the pyramidal tract as they pass from the brain to the spinal cord. When voluntary muscle control is destroyed, strong flexor muscles overbalanc e the extensors. This can cause serious deformities . (Black:199 2. identify personal/ community resources that can provide assistance as needed actions suggestive of impaired judgment. interventions and supervision to promote patient safety. (Doenges,p302) 4. Maintain a supportive, firm attitude. Allow patient sufficient time to accomplish tasks. 4. Patients will need empathy but need to know caregivers will be consistent in their assistance. (Doenges,p302) 5. Provide positive feedback for efforts/ accomplishments. 5 Enhances sense of self-worth, promotes independence, and encourages patient to continue endeavors. (Doenges,p302) Collaborative 1. Administer suppositories and stool softeners. 3,p709) 2. Consult with physical / occupational therapist. 1. May be necessary at first to aid in establishing regular bowel function. (Doenges,p302) 2. Provides expert assistance for developing a therapy plan and identifying special equipment needs. (Doenges,p302) -inability to perform oral care noted -with the ff. V/S: BP – 170/100 mm Hg PR – 90 bpm RR – 24 cpm T – 37.5*C 33 2.3 Drug Therapy Record Hospital No.:782349 Service: Medical Physician: Dr. M. Lim, Dr. W. Briones, Impression:Cerebrovascular Dr. G. Lim, Dr. E. Hernandez Drug/ Route/ Frequency/ Route Ranitidine (Zantac) 150 mg 1 tab BID Classification/ Mechanism of Contraindications/ Action Histamine2 Antagonist Competitively inhibits the action of histamine at the histamine2 (H2) receptors of the parietal cells of the stomach, inhibiting basal gastric acid secretion and gastric acid secretion that is stimulated by food, insulin, histamine, cholinergic agonists, gastrin, and pentagastrin. (Karch,p1039) Ciprofloxacin (ciprobay) 500 mg 1 tab q 12H Indications/ Inhibits bacterial DNA synthesis, mainly by Side Effects Indicated for duodenal ulcer (short-term treatment), pathologic hepersecretory conditions, maintenance therapy for duodenal or gastric ulcer, erosive esophagitis, heartburn and gastroesophageal reflux dse. Contraindicated for patients hypersensitive to drugs. CNS: vertigo, malaise, headache EENT: blurred vision Hepatic: jaundice. Indicated for mild to moderate urinary tract infections, severe or Accident Principles of Care Have regular medical follow-up to evaluate your response. Use cautiously in patient with hepatic dysfunction. Drug may cause falsepositive results in urine protein test using Multistix. May be added to total parenteral nutrition solutions. Use cautiously with patients Treatment Evaluation Take drug with meals and at bedtime. Therapy may continue for 4–6 wk or longer. Continually given to prevent further complication If you also are on an antacid, take it exactly as prescribed, being careful of the times of administration. Adjust dosage in patients with impaired renal function Assess patient for abdominal pain. Note presence of blood in emesis, stool or gastric aspirate Obtain specimen for culture and sensitivity test before giving Continually given to prevent further complication 34 blocking DNA gyrase; bactericidal complicated UTI’s, mild to moderate bone infections, chronic bacterial prostatitis, Contraindicated in patients sensitive to fluoroquinolones. CV: edema, chest pain CNS: headache, restlessness and tremor GI: abdominal pain or discomfort, constipation, flatulence Musculoskeletal: arthralgia, joint inflammation, joint or back pain Indicated to control for tonic-clonic and complex partial seizures, for patient requiring a loading dose, status epilecticus. Phenytoin (dilantin) 100 mg I tab TID Unknown. A hydantoin dereivative that probably stabilizes neuronal membranes and limits seizure activity by either increasing efflux or decreasing influx of sodium ions across cell membranes in the motor cortex during generation of nerve impulse. Contraindicated for hypersensitivity and in those with sinus bradychardia, SA block, second or third degree AV block, and Adam-Strokes syndrome. CNS: ataxia, slurred speech and dizziness CV: periarteritis nodosa EENT: nystagmus, diplopia, blurred vision GI: nausea, vomiting and constipation Hapatic: toxic hepatitis with CNS disorders the first dose. Food doesn’t delay absorption but may delay peak serum levels Monitor patient’s intake and output and observe for signs of crystalluria. Tendon rupture has been reported in patients receiving quinolones. Give oral forms 2 hours after a meal or 2 hours before or after taking antacids. Lon g-term therapy may result in overgrowth of organism resistant to ciprofloxacin. Discontinue in pain, inflammation, or tendon rupture occurs. Use cautiously in patients with hepatic dysfunction, hypotension Divided doses given with or after meals may decrease adverse GI reactions. Elderly patient tends to metabolize phenytoin slowly and may need reduced dosages. Stop drug if rash appears. Use only clear solution for injection. Continually given to prevent further complication Don’t withdraw drug suddenly because seizures may worsen 35 2.4 Health Teaching Plan Patient’s Name: Mr. George Ang Lee Impression: Cerebrovascular Accident Complaints: Right sided weakness and slurred speech Physician: Dr. M. Lim, Dr. W. Briones, Dr. G. Lim, Dr. E. Hernandez Objectives Content Methodology Evaluation After the period of nursing The family care, the patient and family were able shall be able to acquire basic to knowledge, positive attitude, assimilate and beginning skills in the rendering wholistic care to the information patient post hospitalization. given. Specifically, the patient and family shall be able to: 1. be reminded of medication Medication should be Interaction schedule. administered as ordered. (discussion) 15-20 mins 2. establish exercise routine. 3. adhere to dietary management. 4. provide psychological support to patient. Provide basic ROM exercises Demonstration to prevent contractures. Low salt, low fat diet should be facilitated It is always important to maintain an open communication with the patient to relieve patient’s anxiety. 5. visit the attending Usually when CVA patient is physician post discharged, constant medical hospitalization to consultation should be 36 provide continuity of maintained. care. V. Evaluation and Recommendation After rendering holistic care, the patient and the nurse were able to achieve the specific objectives. The degree of outcome attainment should be evaluated on an ongoing basis. After CVA, some outcomes are achieved early (e.g., cerebral perfusion); others may require rehabilitation (e.g., self-care deficit). It is important to monitor progress toward outcomes, working with both the client and the family. Continuing medications even after symptoms abate is recommended. Continue encouraging the client to verbalizes and express his feelings, this would always be effective and therapeutic to the client. Emotional support must be provided to both the client and family members. If the client is to be discharged home, the family needs clear understanding of the residual deficits. The family and client need to have realistic expectations about the client’s abilities; yet encourage independence when the client is able. VI. Evaluation and Implication of This Case Study To: Nursing Practice This case study would make a contribution to the practice of medical nursing as it would serve as a documentation that would then contribute to the appropriate plan of care in patients with cerebrovascular accident (CVA). This would also provide information about cerebrovascular accident (CVA) and nursing interventions and therapeutic techniques used with patients who have this 37 disorder. It also provides information about the plan of care for patients who have this condition for efficient nursing care. Nursing Education To nursing education, this case study would help by providing information about the disease condition, cerebrovascular accident (CVA). The student nurses, as well as the clinical instructors could gain additional information about this disorder that ranks 2nd in the ten leading causes of death in the Philippines, so that it could better equip them for efficient nursing care in the future. This study would explain the future nurses’ adequate background knowledge regarding medical nursing before one is to be exposed to the clinical setting. This would help expand knowledge regarding the disease and would correct misconceptions toward this case. It would then promote awareness. Nursing Research Research is now an integral part of nursing. Through research, betterment or improvement of nursing education to be practiced competitively in the clinical setting will be achieved. In Nursing Research, this case study may broaden the scope or extent of research done previously for cerebrovascular accident (CVA). This may lead to another breakthrough study in the details of the condition. This can also contribute in upgrading and updating the interventions made for this condition. VII. The Referral and Follow-up Rehabilitation from stroke requires specialized help from neurologists, physiotherapists, physical therapist, occupational therapist and speech therapists—especially during the first six months, when most progress is made. Passive stretching exercises and thermal applications are used to regain motor 38 control of limbs, which become rigidly flexed after a stroke has occurred. A patient may recover enough to do pulley and bicycle exercises for the arms and legs and, through speech therapy, may regain the language abilities often lost following a stroke; the degree of recovery varies greatly from patient to patient. VIII. Bibliography Black, Joyce M., Hawks, Jane Hokanson, and Keene, Annabelle. Medical-Surgical Nursing Clinical Management for Positive Outcomes. 6th Edition. Philadelphia, PA: W.B. Saunders Company. 2001 Doenges, Marilynn, Moorhouse, Mary Frances and Geissler-Murr, Alice. Nursing Care Plans Guidelines for Individualizing Patient Care. 6th Edition. Philadelphia: F.A Davis Company. 2002 Deglin, Judith and Vallerand, April. Davis’s Drug Guide for Nurses. 5th Edition. Philadelphia, Pennsylvania: 1997 Kozier, Barbara, ET. Al. Fundamentals of Nursing: Concept, Process and Practice. 5th Edition. USA: Addison-Wesley Longman, Inc., 1998. Potter, Patricia and Perry, Anne Griffin. Fundamentals of Nursing.5th Edition. St. Louis, Missouri: Mosby, Inc., 2001 Smeltzer, Suzanne and Bare, Brenda. Textbook of Medical Surgical Nursing. 10th Edition. Philadelphia, PA: Lippincott Williams and Williams, 2004. Nettina, Sandra M. Manual of Nursing Practice. 7th Edition. Philadelphia: Lippincott, 1996 Bates, Barbara, MD. A Guide to Physical Examination. 2nd Edition. Philadelphia: Lippincott, 1996 39 Positive Outcomes. Vol. 2, 6th Edition. Philadelphia: W. B. Saunders Company, 2001. Doenges, Marilyn E. et al. Nurses Pocket Guide. 8th Edition F. A. Davis Company, 2002 Porth, Carol Matson. Pathophysiology, Concepts of Altered Health States. 6th Edition. Lippincott Williams and Wilkins, 2002 MIMS, Philippines Index of Medical Specialties Established Since 1968, 100th Ed., 2004. Oxford Reference. Dictionary of Nursing, Published by Oxford Melbourne, Oxford University Press, Market House Books Ltd. 1990. 40