Use of Traditional Chinese Acupuncture for treatment of pain and
advertisement

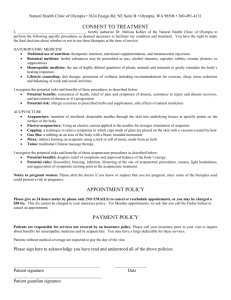
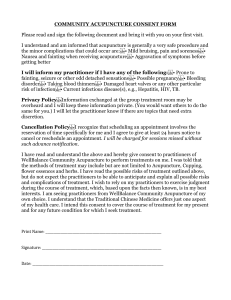
USE OF TRADITIONAL CHINESE ACUPUNCTURE FOR TREATMENT OF PAIN AND SKIN RASH ASSOCIATED WITH SHINGLES IN A 67-YEAR-OLD PATIENT: A CASE REPORT Arkady Kotlyar* (PhD, CAc), Rina Brener (MD), Michael Lis (MD) Pain Clinic, Kaplan Medical Center, Israel *Corresponding author Authors' Information Arkady Kotlyar, PhD, CAc dr.kotlyar@chi-point.com ABSTRACT Introduction There are several treatment options for pain associated with herpes zoster (HZ; shingles). However, many patients, especially the elderly, experience side effects of medication. Therefore, pain associated with the HZ infection remains a challenge for effective management. Recently, the efficacy of acupuncture has been evaluated for pain therapy in acute HZ. This case report describes the use of traditional Chinese acupuncture for the treatment of pain and skin rash associated with HZ in a clinical setting. Case Presentation A 67-year-old Caucasian female with lower back pain (LBP) and lateral irradiation to the left leg, accompanied by a skin rash in the lower back and pelvic area that was caused by acute HZ, was observed at a Health Management Organization (HMO) clinic. The patient was prescribed analgesic, antispasmodic, and antiviral medication. These medications caused urinary retention, and the patient was directed to the Outpatient Pain Clinic of a Medical Center for further treatment. At the Pain Clinic, the patient was prescribed an urgent epidural steroid injection to prevent the suspected development of peripheral neuropathy, a selective serotonin and norepinephrine reuptake inhibitor, and acupuncture. The patient refused to receive pharmacological treatment and was treated with weekly 20minute sessions of Chinese acupuncture for five weeks. Conclusions The present case report describes a conceivable effect of acupuncture on acute pain caused by HZ in a patient who could not be treated pharmacologically. Additional studies are warranted to investigate the effect acupuncture in the management of acute and neuropathic pain caused by HZ. Introduction Herpes zoster (HZ; shingles) is a viral disease caused by the varicella zoster virus (VZV), which reactivates following primary infection with varicella (ie, chicken pox), usually during childhood.(1) After the resolution of the original infection, the virus remains dormant for years in the dorsal root ganglia of cranial or spinal nerves.(1) Acute HZ is usually caused by re-activation of a latent VZV as a result of a decrease in cellular immunity.(1) Re-activation can occur at any age; however, because it is primarily associated with an age-related decline in cell-mediated immunity, it is more frequent in older adults.(2,3) After re-activation, the virus is transported along peripheral nerves, producing an acute neuritis.(1) Thus, the disease is characterized by a painful, unilateral vesicular eruption, usually in a restricted dermatomal distribution. Pain associated with the HZ infection is known as herpetic neuralgia. It is classified as acute (pain preceding or accompanying the eruption of a rash that persists up to 30 days from its onset), sub-acute (pain that persists beyond the healing of the rash but resolves itself within four months after onset), or post-herpetic neuralgia (pain persisting for more than four months from the initial onset of the rash).(4) Post-herpetic neuralgia is a neuropathic pain syndrome (NPS), and is the most common complication of HZ, mainly in patients aged 50 years and older.(3) Older age is also associated with a greater likelihood of a more severe HZ rash.(4) In immunocompetent patients, the primary goal of treatment for HZ is pain reduction. Early intervention with antiviral medication can reduce the risk of complications, lower rash severity, and accelerate its healing.(4,5) The addition of corticosteroids to antiviral medication may further alleviate short-term HZ-related pain.(4,5) However, pharmacological treatment can be associated with an increased risk of serious adverse effects, especially among older adults.(5) If a patient does develop postherpetic neuralgia, such medication as gabapentin, pregabalin, opioids, tricyclic antidepressants, lidocaine, and capsaicin may be used for palliative treatment.(5) However, for individuals with treatment-refractory postherpetic neuralgia, non-pharmacological approaches, which are beneficial to patient well-being in general(4), may be considered as alternative or intregrative treatment options, and a pain management specialist should be consulted.(5, 6) Case Presentation A 67-year-old Caucasian female suffering for a week from lower back pain (LBP) and lateral irradiation to the left leg was observed at a Health Management Organization (HMO) clinic. The patient was a heavy smoker, previously diagnosed with pneumonia and moderate-to-severe chronic obstructive lung disease (COPD). Also, in the past, the patient underwent ablation for atrial fibrillation and flutter. During the first two weeks of observation at the HMO clinic, the patient was symptomatically prescribed oral Spasmalgin (Acetaminophen, Atropine SO4, Codeine PO4, and Papaverine HCl) and thereafter Tramadex (Tramadol Contramid). Both medications had no therapeutic effect but caused urinary retention and dryness in the mouth. Ten days post-onset of LBP, unilateral itching and a painful rash appeared in the lower back and pelvic area. About three weeks post-onset of LBP, after the appearance of the rash, the patient was diagnosed with acute HZ. The diagnosis was based on the anamnesis and the clinical picture. Considering the symptoms and the patient’s age, no additional analyses were required to confirm the diagnosis.(1-4) Therefore, the patient was prescribed daily oral Zovirax (Acyclovir) for a week. During the treatment, the patient began to experience severe pain in the abdominal area. As a result, the treatment with Zovirax was discontinued after three days. About four weeks post-onset of LBP, the patient went through an abdominal computer tomography (CT) examination that did not reveal any dysfunction. Because pharmacological treatment had no positive effect, five weeks post-onset of LBP, the patient was prescribed oral Optalgin (Dipyrone) and Bondormin (Thienodiazepine, a Benzodiazepine analog), and directed to the Outpatient Pain Clinic of a Medical Center for further treatment. Six weeks post-onset of LBP, the patient presented herself at the Outpatient Pain Clinic. Considering the duration of the disease, and to prevent the suspected development of postherpetic neuralgia and peripheral neuropathy, the patient was prescribed an urgent epidural steroid injection (ESI) and treatment with Cymbalta (Duloxetine HCl). In addition, acupuncture was recommended. The patient refused to receive pharmacological treatment and started the acupuncture treatment on the same day. The patient was treated with two 20-minute sessions of Chinese acupuncture per week for the first two weeks and thereafter, with three additional weekly 20-minute sessions. Acupuncture Treatment Pain Severe deep and distending pain originated in the left-side lower back area and worsened at night. The pain irradiated laterally through the pelvic area, along the route of the Gallbladder (GB) meridian, particularly through the GB 30 (Huantiao) point to the right foot. Rash The observed rash was manifested by clusters of brownish crusted grain-sized vesicles categorized in Chinese medicine as snake string sores (she chuan chuang). The rash was distributed along a dermatome innervated by certain peripheral nerves. Pulse Diagnosis The pulse was Floating (fumai). On the left hand, in the Guan and Chi positions, Gallbladder (GB) and Pericardium (PC) excess (shi), respectively, was detected. On the right hand, in the Cun and Chi positions, Lung (LU) and Kidney (KI) deficiency (xu), respectively, was detected. Tongue Diagnosis The tongue was slightly red, without coating. Red points (dian) were located between the center and the tip of the tongue (chest area). Treatment Protocol The following acupuncture points were used: 1st session – GB41 (Zulinqi) left, SP6 (Sanyinjiao) bilaterally, ST36 (Zusanli) bilaterally, LI4 (Hegu) bilaterally, LU10 (Shousanli) bilaterally, LI11 (Quchi) bilaterally, KI27 (Shufu) bilaterally, KI3 (Taixi) bilaterally; 2nd session – LV3 (Taichong) bilaterally, KI3 (Taixi) bilaterally, LU9 (Taiyuan) bilaterally, LU10 (Shousanli) bilaterally, M-HN3 (Yintang), KI27 (Shufu) bilaterally; 3rd session – GB41 (Zulinqi) left, ST36 (Zusanli) left, KI 3 (Taixi) bilaterally, LU10 (Shousanli) left, LU7 (Lieque) left, TH5 (Waiguan) right, LI11 (Quchi) bilaterally; 4th session – LV3 (Taichong) left, SP3 (Taibai) left, KI3 (Taixi) bilaterally, LU7 (Lieque) bilaterally, PC6 (Neiguan) right, M-HN3 (Yintang); 5th session – LV3 (Taichong) bilaterally, SP3 (Taibai) bilaterally, SP6 (Sanyinjiao) bilaterally, PC6 (Neiguan) bilaterally, M-HN54 (Anmian) bilaterally, M-HN3 (Yintang); After the fifth session, the patient no longer felt any pain and discontinued the treatment. Discussion Pain is the most common complication of HZ that significantly reduces the quality of life of the affected individual.(1,7) Recently, the efficacy of acupuncture therapy for herpetic pain has been evaluated in controlled clinical trials.(7,8,9) According to a review by the World Health Organization, the use of acupuncture in HZ therapy is classified in the category “Diseases, symptoms or conditions for which the therapeutic effect of acupuncture has been shown but for which further proof is needed”.(9) In the present case, considering the adverse reactions to pharmacological treatment and the patient’s refusal to receive ESI or any additional pharmacological treatment, not many treatment options were available. On the other hand, considering the age of the patient, a high risk of postherpetic neuralgia and peripheral neuropathy was a concern.(3) Therefore, acupuncture was suggested as preferred treatment and started at the acute to sub-acute phase of HZ. Pain and Rash Symptoms The localization of the pain indicated that an external pathogen invaded the nerve ganglia along the affected segment of the corresponding dermatome. The character of the pain was interpreted as a sign of Qi stagnation and Blood stasis.(10,11) Usually, skin rash appears in the initial phases of HZ, a couple of days post-onset of the pain.(12) In the present case, the rash appeared 10 days post-onset of the pain. Considering that the patient had COPD and cardiac problems in the past, the severity of the pain and the delay in the appearance of the skin rash can be explained by a deficiency of the Defensive (Wei) Qi and Blood stasis.(13) Thus, the invasion of the external pathogen increased the existing internal imbalances of Qi and Blood.(13,14) The rash was itching and painful and corresponded to Wind-Heat when it first appeared. However, by the time that the patient presented herself at the Outpatient Pain Clinic, the rash became crusted and did not itch, although it remained painful. This changed character of the rash indicated Damp-Heat. The changes in the character of the rash were interpreted as an invasion of Toxic Wind that was challenged by Qi and Blood circulation.(10) Conceivably, the increase of Qi and Blood circulation, which was already imbalanced, obstructed the channels and vessels, and augmented the pain. Pulse and Tongue Diagnosis Pulse diagnosis corresponded to Wind-Heat shi, and LU and KI xu. The color and shape of the tongue represented Heat. Lack of coating represented empty Heat derived from Yin xu, while dian in the chest area represented Heat in the lungs.(15,16) According to Five Elements, the clinical manifestations corresponded to the pattern of Fire insulting Water.(13) Treatment principle Point selection was based on the patient’s complaints, conventional diagnosis, and the findings obtained in the pulse and tongue diagnostics prior and during each acupuncture session. To alleviate pain and heal the rash, the treatment rationale was to expel Wind-Heat and fortify LU and KI.(Error! Reference source not found.18,18) The acupuncture points were selected to achieve the following: LU7 (Lieque), LU9 (Taiyuan) to pacify Wind and tonify the Lung; LU10 (Shousanli) to clear Lung Heat; LI4 (Hegu), LI11 (Quchi), GB41 (Zulinqi), TH5 (Waiguan) to expel Wind Heat; ST36 (Zusanli), SP3 (Taibai), SP6 (Sanyinjiao) to tonify Qi, nourish blood and Yin, calm the spirit, and alleviate pain; SP10 (Xuehai) to cool blood and benefit the skin; KI3 (Taixi) to tonify Kidney Yang, anchor the Qi, benefit the Lung, and alleviate pain; KI27 (Shufu), PC6 (Neiguan) LV3 (Taichong) to clear Heat, calm the spirit, unbind the chest, and regulate Qi; M-HN3 (Yintang) to pacify Wind, calm the spirit, and alleviate pain; M-HN54 (Anmian) to calm the spirit; After the first session, the skin rash turned pale, and the patient felt a significant decrease in the severity of the pain. The reduction in pain severity continued throughout the course of treatment. After the fifth session, the patient no longer felt any pain and discontinued treatment. According to the classification of herpetic pain, prior to acupuncture treatment, the patient was experiencing acute to sub-acute pain.(4) Acupuncture affected the course of the disease, and NPS did not develop. Taking into consideration that in the absence of NPS, HZ is time-limited, it is impossible to claim that acupuncture alone resolved the disease. Additional studies are necessary to investigate the effect of acupuncture on HZ-related pain and the development of the disease. Conclusions The present case report describes a conceivable effect of acupuncture on acute to subacute pain caused by HZ in a patient who could not be treated pharmacologically. Therefore, in the present case acupuncture was the available treatment method. However, additional studies are warranted to investigate the effect acupuncture in the management of acute and neuropathic pain caused by HZ. References 1. Johnson RW. Herpes Zoster and Postherpetic Neuralgia. Expert Rev Vaccines. 2010;9(3s):21-26. 2. McElhaney JE. Herpes zoster: a common disease that can have a devastating impact on patients' quality of life. Expert Rev Vaccines. 2010 Mar;9 (3 Suppl):27-30. 3. Sampathkumar P, Drage LA, Martin DP: Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc 2009, 84(3):274-280. 4. Schmader KE, Dworkin RH. Natural history and treatment of herpes zoster. J Pain. 2008 Jan;9(1 Suppl 1):S3-9. 5. Tyring SK. Management of herpes zoster and postherpetic neuralgia. J Am Acad Dermatol 2007;57:S136-42. 6. Fleckenstein J, Kramer S, Hoffrogge P, et al. Acupuncture in acute herpes zoster pain therapy (ACUZoster) – design and protocol of a randomized controlled trial. BMC Complement Altern Med. 2009 Aug 12; 9:31. 7. Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007, 82(11):1341-1349. 8. Tan EK, Millington GWM, Levell NJ. Acupuncture in dermatology: an historical perspective. Int J Dermatol 2009, 48,648 –652. 9. Acupuncture: review and analysis of controlled clinical trials. World Health Organization 2003. 10. Flaws B, Sionneau P. The Treatment of Modern Western Diseases with Chinese Medicine: A Textbook & Clinical Manual. Blue Poppy Press 2001. 11. Maciocia G. Diagnosis in Chinese Medicine: A Comprehensive Guide. Churchill Livingstone 2003. 12. Furuta Y, Ohtani F, Mesuda Y, Fukuda S, Inuyama Y. "Early diagnosis of zoster sine herpete and antiviral therapy for the treatment of facial palsy". Neurology 2000; 55 (5): 708–10. 13. Maciocia G. The Foundations of Chinese Medicine. Churchill Livingstone 1989. 14. Liu Xiao-Juan. The Treatment of 58 Cases of Post-herpetic Neuralgia by Acupuncturing the Paravertebral Points. Sichuan Chinese Medicine 5, 2008. 15. Kirschbaum. B. Atlas of Chinese Tongue Diagnosis, Vol. 1. Eastland Press 2000. 16. Maciocia G. Tongue Diagnosis in Chinese Medicine. Eastland Press 1995. 17. Maciocia G., Zhong Z. The Practice of Chinese Medicine: The Treatment of Diseases with Acupuncture and Chinese Herbs. Churchill Livingstone 1994. 18. Deadman P. Al-Khafaji M. Baker K. A Manual of Acupuncture. The Journal of Chinese Medicine 1998.