2014Local25MedicalPlanSPD(00325915-3)-c(2)
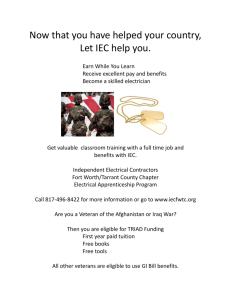
advertisement
INTERNATIONAL UNION OF OPERATING ENGINEERS LOCAL 25, MARINE DIVISION MEDICAL PLAN SUMMARY PLAN DESCRIPTION Effective July 1, 2014 International Union of Operating Engineers Local 25 Marine Division Medical Plan 461 State Route 33 Millstone Township, New Jersey 08535 (800) 548-6662 FAX (732) 446-9167 00325915.3 TABLE OF CONTENTS TRUSTEES AND PROFESSIONALS.......................................................................................... iv FROM THE BOARD OF TRUSTEES........................................................................................... v PLAN INFORMATION ................................................................................................................. vii FUNDING METHOD AND TYPE OF ADMINISTRATION ................................................... viii GRANDFATHERED HEALTH PLAN ........................................................................................ ix DEFINITIONS ................................................................................................................................ x ELIGIBILITY ................................................................................................................................. 1 CONTINUATION OF COVERAGE ................................................................................................ 5 COVERAGE WHILE ON MILITARY DUTY (USERRA) ........................................................ 10 CONTINUATION OF COVERAGE DURING LEAVE COVERED BY THE FAMILY MEDICAL LEAVE ACT (FMLA) .................................................................................. 11 HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA).............. 12 PLAN BENEFITS ........................................................................................................................ 14 HOSPITAL BENEFITS................................................................................................................ 17 MEDICAL BENEFITS ................................................................................................................. 20 PRESCRIPTION DRUG BENEFITS ....................................................................................... 28 BENEFITS FOR PENSIONERS ............................................................................................... 32 BENEFITS FOR MEDICARE ELIGIBLE PENSIONERS ......................................................... 33 BENEFITS FOR NON-MEDICARE AND ELIGIBLE PENSIONERS ..................................... 35 OPTICAL BENEFITS .................................................................................................................. 36 GENERAL EXCLUSIONS .......................................................................................................... 37 DENTAL BENEFITS ................................................................................................................... 40 LIFE INSURANCE BENEFITS................................................................................................... 41 COORDINATION OF BENEFITS .............................................................................................. 42 ii CLAIMS AND APPEALS PROCEDURES ................................................................................ 44 NOTICE OF DECISION .............................................................................................................. 48 APPEALS PROCEDURE ............................................................................................................ 49 DESIGNATED AUTHORIZED REPRESENTATIVES ............................................................. 52 SUBROGATION AND RESTITUTION RIGHTS ...................................................................... 53 MISREPRESENTATION AND FRAUD .................................................................................... 55 OVERPAYMENTS ...................................................................................................................... 56 ASSIGNMENTS........................................................................................................................... 57 RESERVATION OF RIGHTS ..................................................................................................... 58 TERMINATION OF PLAN ......................................................................................................... 59 YOUR RIGHTS ............................................................................................................................ 66 STATEMENT OF ERISA RIGHTS ............................................................................................. 70 iii INTERNATIONAL UNION OF OPERATING ENGINEERS MARINE DIVISION LOCAL 25 MEDICAL PLAN 461 STATE ROUTE 33, MILLSTONE TOWNSHIP, NEW JERSEY 08535 (800) 548-6662 TRUSTEES AND PROFESSIONALS UNION TRUSTEES Scott A. Winter - Co-Chair IUOE Marine Division Local 25 463 Highway 33 East Millstone Township, NJ 08535 UNION ALTERNATE TRUSTEES Michael J. Curry IUOE Marine Division Local 25 463 Highway 33 East Millstone Township, NJ 08535 Paul J. Abell IUOE Marine Division Local 25 12610 Henderson Road Tampa, FL 33625 Anthony J. Gonsiewski, Jr. IUOE Marine Division Local 25 463 Highway 33 East Millstone Township, NJ 08535 Scott Reeves, Sr. IUOE Marine Division Local 25 463 Highway 33 East Millstone Township, NJ 08535 John A. Zappala IUOE Marine Division Local 25 463 Highway 33 East Millstone Township, NJ 08535 EMPLOYER TRUSTEES Stephen Newton - Co-Chair Norfolk Dredging P.O. Box 1706 Chesapeake, VA 23320 EMPLOYER ALTERNATE TRUSTEES Michael D. Ernst Weeks Marine, Inc. Inwood Business Park/304 Gaille Drive Covington, LA 70433 Christine Schuver Great Lakes Dredge & Dock Co. 2122 York Road Oak Brook, IL 60523 Steven O’Hara Great Lakes Dredge & Dock Co. 2122 York Road Oak Brook, IL 60523 Patrick J. Whelan Weeks Marine, Inc. 4 Commerce Drive, 2d Floor Cranford, NJ 07016 Dudley D. Ware, Jr. Norfolk Dredging Co. P.O. Box 1706 Chesapeake, VA 23327 Administrator Larry H. Schleyer Plan Auditors Buchbinder Tunick & Company Plan Counsel Cohen, Weiss and Simon LLP Plan Consultants O’Sullivan & Associates iv FROM THE BOARD OF TRUSTEES To All Participants: We are pleased to provide you with this updated booklet describing the benefits available under the International Union of Operating Engineers Local 25 Marine Division Medical Plan, effective June 1, 2014. This booklet constitutes the Medical Plan’s “plan document” and supersedes all prior booklets, rules and regulations, summary plan descriptions and other notices. This booklet describes the Plan’s eligibility rules, the benefits provided, the procedures for filing claims for benefits and appealing denied claims, your rights to continuation coverage under the Plan when coverage terminates and other important information about your rights and obligations under the Plan. We urge you to read this booklet carefully and share it with your family. Note that there have been certain changes to the Plan since the last summary plan description was issued. These changes were communicated to you through summaries of material modifications and other notices sent by the Plan Office. The changes are reflected in this description, unless modified further. The Trustees strive to provide benefits that will contribute to the security, health and well-being of the participants of the Plan. The changing economic conditions require a constant assessment of the Plan and the benefits it provides to maintain its financial stability. Your assistance is critical to combat the rising costs of health care and ensure future coverage. This Plan offers both network and non-network coverage, as described more fully herein. We strongly urge you to use in-network providers as much as possible. Doing so benefits both you and the Plan as a whole. You will notice that certain words in this booklet are capitalized. These words are defined terms and have specific meaning for purposes of this booklet. We specifically reserve the right to change, eliminate or add to the benefits provided to participants, including pensioners, and their dependents and beneficiaries. We also reserve the right to adopt new Plan rules and regulations, to modify the existing rules and regulations and to terminate the Plan. The continuance of the Plan is subject to the maintenance of collective bargaining agreements which provide for employer contributions to the Plan. No benefits or v rules described in this booklet are guaranteed (vested) for any participant, including any pensioner, or eligible dependent. All benefits and rules may be changed, reduced or eliminated at any time by the Board of Trustees, in our sole discretion. All material modifications to the Plan will be communicated in writing and distributed to participants, as required by law, so that participants may have current information concerning their rights and benefits under the Plan. Please keep all Plan notices with this booklet so that you will always have the most up-to-date information about the Plan. Please note that no local union, local union officer, business agent, employee, employer or employer representative, individual Trustee, consultant, attorney or any other person may speak for or on behalf of the Plan, or commit or legally bind the Board of Trustees of this Plan in any matter whatsoever relating to this Plan, unless such person has express authority from the Board of Trustees to act in such manner. Statements from the Plan Office, whether oral or written, other than official Summaries of Material Modifications, cannot modify the specific benefits and terms set forth in this booklet. Every effort has been made to keep this booklet easy to understand. After you read the booklet, the Plan Office will be glad to help if you have any questions about the Plan. Fraternally Yours, The Board of Trustees International Union of Operating Engineers Marine Division Local 25 Medical Plan vi PLAN INFORMATION PLAN NAME: International Union of Operating Engineers Local 25 Marine Division Medical Plan 461 State Route 33 Millstone Township, New Jersey 08535 PLAN SPONSOR: Board of Trustees of the International Union of Operating Engineers Local 25 Marine Division Medical Plan 461 State Route 33 Millstone Township, New Jersey 08535 PLAN ADMINISTRATOR: Board of Trustees of the International Union of Operating Engineers Local 25 Marine Division Medical Plan 461 State Route 33 Millstone Township, New Jersey 08535 TAXPAYER IDENTIFICATION NUMBER OF PLAN ADMINISTRATOR: 13-1931288 PLAN NUMBER: PLAN YEAR ENDS: 501 December 31 AGENT FOR SERVICE OF LEGAL PROCESS: Larry H. Schleyer, Administrator International Union of Operating Engineers Local 25 Marine Division Medical Plan 461 State Route 33 Millstone Township, New Jersey 08535 Service of legal process may also be made on a Plan Trustee or the Plan Administrator. vii FUNDING METHOD AND TYPE OF ADMINISTRATION The Plan was established in February 1960 as a result of collective bargaining between the International Union of Operating Engineers Marine Division Local 25 (the “Union”) and certain employers. The Plan is funded entirely by employer contributions made pursuant to collective bargaining agreements between the employers and the Union and certain participant contributions. A complete list of the employers participating in the Plan may be obtained by participants and beneficiaries upon written request to the Plan Administrator. The Medical Plan is an employee welfare benefit plan governed by the Employee Retirement Income Security Act of 1974, 29 U.S.C. 1001 et seq. (“ERISA”). With the exception of life insurance and accidental death and dismemberment benefits, all benefits provided by the Plan are self-insured, which means that benefits are paid directly out of Plan assets. Life insurance and accidental death and dismemberment benefits are insured through CIGNA, which means that the Plan pays premiums to CIGNA and CIGNA guarantees those benefits. The Plan is jointly administered by a Board of Trustees with equal representation of the Union and the contributing employers. viii GRANDFATHERED HEALTH PLAN This group health plan believes this Plan is a “grandfathered health plan” under the Patient Protection and Affordable Care Act (the Affordable Care Act). As permitted by the Affordable Care Act, a grandfathered health plan can preserve certain basic health coverage that was already in effect when that law was enacted. Being a grandfathered health plan means that your plan may not include certain consumer protections of the Affordable Care Act that apply to other plans, for example, the requirement for the provision of preventive health services without any cost sharing. However, grandfathered health plans must comply with certain other consumer protections in the Affordable Care Act, for example, the elimination of lifetime limits on benefits. Questions regarding which protections apply and which protections do not apply to a grandfathered health plan and what might cause a plan to change from grandfathered health plan status can be directed to the plan administrator at the International Union of Operating Engineers Local 25 Marine Division Medical Plan at 461 State Route 33, Millstone Township, New Jersey, 08535. telephone 800-548-6662. You may also contact the Employee Benefits Security Administration, U.S. Department of Labor at 1-866-444-3272 or www.dol.gov/ebsa/healthreform. This website has a table summarizing which protections do and do not apply to grandfathered health plans. ix DEFINITIONS When reading this booklet you may encounter ,you may encounter some terms with which you may not be familiar or which may have a specific meaning for purposes of this booklet. The following definitions are provided to help you understand what these terms mean and how they are applied. Accidental: a loss due to solely to violent, external, and unintentional means. Beneficiary: a person designated by an active Employee to receive any death benefits payable under the Plan. Board of Trustees or Trustees: the Joint Board of Trustees of the International Union of Operating Engineers Marine Division Local 25 Medical Plan. Collective Bargaining Agreement(s): the labor agreement(s) between the Union and participating Employers, which provide(s) for the payment of contributions to the Plan. COBRA: the Consolidated Omnibus Budget Reconciliation Act of 1985, P.L. 99272, April 7, 1986, as amended. Covered Employment: work for which an Employer is required to and does make contributions to the Plan under a Collective Bargaining Agreement or a Participation Agreement. Covered Expense: a charge that is allowable under the Plan for a Medically Necessary service or supply. Custodial Care: all services and supplies, including room and board, which are provided primarily to assist an eligible Participant or his/her eligible Dependent in the activities of daily living require the continuous attention of trained medical or paramedical personnel. Such care may include but are not limited to, preparation of special diets, supervision over medication that can be self-administered, assistance in getting in or out of bed, walking, bathing, dressing, and eating. Services and supplies may be deemed to be Custodial Care without regard to the practitioner or provider by whom or by which they are prescribed, recommended or performed. Deductible: the out-of-pocket expense that you must pay each year before certain benefits are payable under the Plan. x Dentist: a person who is duly licensed and acting within the scope of his license to practice dentistry, including a Physician furnishing dental care which he is licensed to provide. Disability or Disabled: your inability to perform substantially all of the duties of your occupation in Covered Employment because of a medically determined physical or mental Illness or Injury. Eligible Dependent: For Eligible Employees, an Eligible Dependent is: 1) a legal spouse of an Eligible Employee; 2) a child of an Eligible Employee if such child is under 26 years of age; and 3) a child of an Eligible Employee over 26 years of age who became totally disabled before reaching the age of 26, and who is dependent on his or her parents for support. In the case of a Pensioner, your Eligible Dependent is only your legal spouse, provided such spouse was eligible for benefits on the effective date of your pension and provided that you and your spouse were legally married to each other for at least one year prior to the date of retirement. The word “child” as used in this definition includes a biological child, a legally adopted child or a child placed with you for adoption, as well as a stepchild. No individual will be considered a child of an Eligible Employee unless such Employee has provided the Plan with a certified copy of the child’s birth certificate, and other proof of eligibility that may be requested by the Administrator. Eligible Employee: an Employee who meets the requirements for eligibility as set forth in the Plan. Employee: a person employed by an Employer in work covered under a Collective Bargaining Agreement or a Participation Agreement on whose behalf contributions are required to be made to the Plan. This includes all International Union of Operating Engineers Marine Division Local 25 Fund Office employees and Union officials. Employer: any Employer that is obligated, under a Collective Bargaining Agreement or other written agreement, to make contributions to the Plan on behalf of its covered Employees. ERISA: the Employee Retirement Income Security Act of 1974, P.L. 93406, Sept. 2, 1974, as amended. xi Experimental: (i) any medical procedure, equipment, treatment or course of treatment, or drug or medicine that is meant to investigate and is limited to research; (ii) techniques that are restricted to use at centers which are capable of carrying out disciplined clinical efforts and scientific studies; (iii) procedures which are not proven in an objective way to have therapeutic value or benefit; and/or (iv) any procedure or treatment which is obsolete or whose effectiveness is medically questionable. Government approval of a procedure, equipment, treatment, drug, medicine or technique is not necessarily sufficient to prove that it is beneficial or appropriate or effective for a particular diagnosis or, treatment of a covered person’s particular condition. Any or all of the following criteria may, within the Trustees’ sole discretion, be applied in determining whether such procedure, etc., is experimental or investigative, obsolete or ineffective: Any medical device, drug or biological product must have received final approval to market by the U.S. Food and Drug Administration (FDA) for the particular diagnosis or condition. Once FDA approval has been granted for a particular diagnosis or condition, use of the medical device, drug or biological product for another diagnosis or condition may require that any or all of these criteria be met: 1. Conclusive evidence from the published peer-reviewed medical literature must exist that the procedure has a definite positive effect on health outcomes. 2. Demonstrated evidence as reflected in the published peer reviewed medical literature must exist that over time the procedure leads to improvement in health outcomes, i.e., the beneficial effects outweigh any harmful effects. 3. Proof, as reflected in the published peer-reviewed medical literature, must exist that the procedure is least as effective in improving health xii outcomes as established procedure, or is usable in appropriate clinical contexts in which established procedure is not employable. 4. Proof, as reflected in the published peer-reviewed medical literature, must exist that improvement in health outcomes (as defined in #3 above) is possible in standard conditions of medical practice, outside clinical investigatory settings. Hospital: an institution that: (1) is duly licensed as a Hospital (if licensing is required in the state); (2) operates primarily for the diagnosis, treatment and rehabilitation of sick, injured or disabled persons as inpatients; (3) provides 24hour nursing services by registered or graduate nurses on duty or call; (4) has a staff of one or more licensed physicians available at all times; (5) provides organized facilities for diagnosis and surgery either on its premises or at an institution with which the establishment has a formal arrangement for the provision of such facilities; (6) is not primarily a clinic, nursing, rest or convalescent home or an extended care facility or a similar establishment and is not (other than incidentally) a place for treatment of alcoholism or drug addiction, and (7) has accreditation under one of the programs of the Joint Commission on Accreditation of Hospitals. Confinement in a special unit of a Hospital used primarily as a nursing, rest or convalescent home or extended care facility is deemed to be confinement in an institution other than a Hospital. Illness: a sickness, disorder or disease resulting in an unsound condition of the mind or body, including, but not limited to, pregnancy, child birth and related conditions. Injury: a wound or damage sustained accidentally and by external force. Maintenance Drugs: drugs which are prescribed for an extended period of time and are necessary to sustain good health. Examples are drugs used to treat high blood pressure, diabetes and arthritis. Medically Necessary: any service, treatment or supply, including a Hospital confinement, furnished or prescribed by a Physician or other licensed provider to identify or treat an Illness or injury, that: is necessary for the diagnosis and treatment of the Illness or Injury for which it is performed; is based upon valid medical need; meets generally accepted standards of medical practice; xiii is required for reason other than the convenience of the patient or provider; and is the most appropriate level of service or supply that can safely be provided for the patient. Medicare: any health insurance benefits provided under Title XVIII of the Social Security Act of 1965, as amended. Mental or Nervous Disorder: a neurosis, psychoneurosis, psychopathy or other mental or emotional disease or disorder. Participant: an Eligible Employee. Participation Agreement: an Agreement between the Plan and an Employer that provides for the payment of contributions to the Plan on behalf of Employees not covered by a Collective Bargaining Agreement. Pensioner: someone who retires with pension under the IUOE Local 25 Marine Pension Plan or the Central Pension Fund of the International Union of Operating Engineers and Participating Employers. Physician: a duly licensed doctor of medicine, podiatry or osteopathy acting within the scope of his license. The Plan covers expenses for professional medical services of licensed social workers, and chiropractors certified in the state where their practice is located. Plan: the International Union of Operating Engineers Marine Division Local 25 Medical Plan. Plan Office: International Union of Operating Engineers Marine Division Local 25 Medical Plan, 461 Route 33 East, Millstone Township, New Jersey 08535. Preferred Provider Organization (“PPO”): a group of selected physicians, specialists, Hospitals, and other treatment centers which have agreed to provide their services to Plan Participants and beneficiaries at a negotiated rate under the terms of an agreement with a PPO network. These medical providers are sometimes referred to as “Network providers” or “Panel providers” interchangeably throughout this booklet. Similarly, medical providers that are not under contract to provide services at negotiated rates are referred to as “Nonnetwork”, “Out-of-Network” and “Nonpanel providers”. xiv Reasonable and Customary or R&C: the fee regularly charged and received by a person, group or entity for services, treatments or supplies covered under the Plan, as determined by the Trustees of the Plan. Union: the International Union of Operating Engineers Marine Division Local 25. xv ELIGIBILITY ELIGIBILITY FOR ACTIVE EMPLOYEES* Becoming Eligible for Benefits and Maintaining Eligibility If you are a new Employee on the payroll of a Contributing Employer, you and your Eligible Dependents will become eligible for benefits on the first day of the month following your completion of 500 hours of Covered Employment within three (3) consecutive calendar months. You will maintaining your eligibility after you establish initial eligibility if you work at least 325 hours in Covered Employment on the preceding 4-month period. If you do not work in Covered Employment for more than twelve (12) consecutive months, you will lose your eligibility, and you will have to reestablish your eligibility for benefits by again working at least 500 hours in Covered Employment within three (3) consecutive months. For example, if you first became employed on June 1, 2014 and worked 500 hours between June 1 and August 31, you and your dependents would be eligible for benefits on September 1, 2014. Therefore, in general, if you were admitted to the hospital on September 15, 2014 you would be eligible for benefits for the hospital stay and related medical services. If, instead, you were admitted to the hospital March 2015, in general, you would be eligible for benefits during the month of March 2015 if you worked at least 325 hours in Covered Employment in the four (4) preceding months (November, December, January, February). * These rules apply to Active Employees only. Eligibility rules for Pensioners are set forth starting on page 32 of this booklet. Dependent Eligibility If each of your dependents meet the definition of an eligible Dependent, and if you provide the necessary information to establish each of your dependents’ eligibility in a timely manner, your Eligible Dependent(s) will be covered under this Plan. Establishing Dependent Eligibility To cover any or all of your Eligible Dependents, you must list them on an Enrollment Data Card and file it with the Plan Office and provide a copy of the applicable marriage and birth certificates. An Enrollment Card may be obtained 1 from your Shop Steward, the Medical Plan Office, or the Local 25 Union Offices in Norfolk or Tampa. If you do not have a properly completed Enrollment Card on file in the Plan Office, and you file a claim for your spouse or child (ren), you will be required to submit the original or a certified copy of your marriage certificate and/or the original or certified copies of your dependent’s birth certificate(s) before your claim can be processed. If you marry or have a child while you are eligible for benefits, you may enroll your new Dependent for coverage under the Plan as of the date of the marriage or birth if you provide the Plan office with written notice of the marriage or birth, together with a copy of the marriage or birth certificate, within 30 days of the event. Claims will not be paid on behalf of the new Dependent until the applicable documentation is received by the Plan Office. If both you and one of your Dependents qualify as participants in this Plan (i.e, you and your spouse work in covered employment and are eligible to participate in this Plan), the Plan will cover each of you as participants as well as dependents of each other for purposes of coordination of benefits. Employment Credit For Non-Working Periods In some circumstances you may receive credit for Covered Employment even though you are not actively at work and no contributions are made on your behalf. If you miss work because you are confined in a hospital as an inpatient, you will receive credit for 8 hours of covered employment for each day you are hospitalized. If you are covered by the Family Medical Leave Act (FMLA), your Employer is required to make contributions on your behalf for FMLA leave, and you will be entitled to credit for Covered Employment under this Plan for the time you are on FMLA leave. See page 11 of this booklet for additional information concerning FMLA leave. If you become unemployed due to an occupational injury or illness, your Employer may be required to continue to make contributions on your behalf for all or a part of the time you are unemployed, in which case you will be entitled to credit for Covered Employment under this Plan for this period. Check your Collective Bargaining Agreement for additional information as to whether your Employer is required to continue contributions on your behalf in this situation. 2 You will also receive credit toward your eligibility based on vacation benefits you receive under the International Union of Operating Engineers Local 25, Marine Division Vacation Plan, provided you did not already receive credit for the same period based upon actual Covered Employment. You will receive Covered Employment credit for the actual hours of Vacation Plan benefits you receive. NOTE: In no event will an Employee be entitled to receive double credit for Covered Employment for the same period. Termination of Eligibility for Benefits Your coverage under the Plan will terminate: if you do not maintain your eligibility by working the required number of hours in Covered Employment, as set forth above; if your Employer fails to make required contributions on your behalf, and the Trustees of the Plan decide, in their sole discretion to terminate your eligibility, subject to reinstatement upon payment of the amounts owed; if you engage in an act of fraud against the Plan, and the Trustees of the Plan decide, in their sole discretion, to terminate your eligibility; on the date a change in the Plan results in the termination of your coverage; or on the date the Plan terminates. Coverage for your Eligible Dependents will terminate on the earlier of the date on which your coverage terminates or the date on which a Dependent ceases to meet the Plan’s definition of an Eligible Dependent. If your Dependent loses eligibility due to divorce, his or her coverage will end as of the date of the divorce. Remember that it is your obligation to promptly notify the Plan if you divorce your dependent spouse. You must notify the Plan within no later than 60 days of the date of the divorce. If you fail to do so, your former spouse will not be eligible for COBRA continuation coverage (see the provisions regarding COBRA starting on page 5) and your former spouse’s coverage will be terminated retroactive to the date of the divorce and you will be 3 responsible for reimbursing the Plan for any benefits incorrectly paid after the divorce. If your Dependent loses coverage due to age, coverage will end as of the date of the date he or she turns age 26. In the event of death of an Employee who was eligible for Plan benefits on the date of death, coverage for the Employee’s Eligible Dependents will terminate on the last day of the third month following the month in which the death occurred (i.e., if the Employee dies on January 15th, coverage for his Eligible Dependents will terminate on April 30th). Once coverage under this Plan terminates, you and your Eligible Dependents may be entitled to continue coverage under this Plan at your own expense under certain circumstances. For information on continued coverage options, see the next section of this booklet on “Continuation of Coverage”, starting on page 5. You must notify the Plan immediately if you and your spouse become divorced, if your child who is an Eligible Dependent turns age 26, or in the case of any other event that would result in a termination of your Eligible Dependent’s eligibility. If such notification is not received by the Plan, the Plan will seek reimbursement from you for any benefits paid to the ineligible person, including by offsetting against your or your family members’ medical claims any claims wrongfully paid and/or through legal action for damages, including attorneys’ fees and costs. Also, in any case of fraud or an intentional misrepresentation of a material fact by you or by your dependent, the Plan will have the right to cancel coverage retroactively and seek recovery as noted above. 4 CONTINUATION OF COVERAGE This notice has important information about your right to COBRA continuation coverage, which is a temporary extension of coverage under the Plan. This notice explains COBRA continuation coverage, when it may become available to you and your family, and what you need to do to protect your right to get it. When you become eligible for COBRA, you may also become eligible for other coverage options that may cost less than COBRA continuation coverage. The right to COBRA continuation coverage was created by a federal law, the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA). COBRA continuation coverage can become available to you and other members of your family when group health coverage would otherwise end. You may have other options available to you when you lose group health coverage. For example, you may be eligible to buy an individual plan through the Health Insurance Marketplace. By enrolling in coverage through the Marketplace, you may qualify for lower costs on your monthly premiums and lower out-ofpocket costs. Additionally, you may qualify for a 30-day special enrollment period for another group health plan for which you are eligible (such as a spouse’s plan), even if that plan generally doesn’t accept late enrollees. What is COBRA continuation coverage? COBRA continuation coverage is a continuation of Plan coverage when it would otherwise end because of a life event. This is also called a “qualifying event.” Specific qualifying events are listed later in this notice. After a qualifying event, COBRA continuation coverage must be offered to each person who is a “qualified beneficiary.” You, your spouse, and your dependent children could become qualified beneficiaries if coverage under the Plan is lost because of the qualifying event. Under the Plan, qualified beneficiaries who elect COBRA continuation coverage must pay for COBRA continuation coverage. If you’re a participant, you’ll become a qualified beneficiary if you lose your coverage under the Plan because of the following qualifying events: Your hours of employment are reduced, or Your employment ends for any reason other than your gross misconduct. If you’re the spouse of a participant, you’ll become a qualified beneficiary if you lose your coverage under the Plan because of the following qualifying events: 5 Your spouse dies; Your spouse’s hours of employment are reduced; Your spouse’s employment ends for any reason other than his or her gross misconduct; Your spouse becomes entitled to Medicare benefits (under Part A, Part B, or both); or You become divorced or legally separated from your spouse. Your dependent children will become qualified beneficiaries if they lose coverage under the Plan because of the following qualifying events: The parent-participant dies; The parent-participant’s hours of employment are reduced; The parent-participant’s employment ends for any reason other than his or her gross misconduct; The parent-participant becomes entitled to Medicare benefits (Part A, Part B, or both); The parents become divorced or legally separated; or The child stops being eligible for coverage under the Plan as a “dependent child.” When is COBRA continuation coverage available? The Plan will offer COBRA continuation coverage to qualified beneficiaries only after the Plan Administrator has been notified that a qualifying event has occurred. The employer must notify the Plan Administrator of the following qualifying events: The end of employment or reduction of hours of employment; Death of the employee-participant; The employee-participant’s becoming entitled to Medicare benefits (under Part A, Part B, or both). 6 For all other qualifying events (divorce or legal separation of the employee and spouse or a dependent child’s losing eligibility for coverage as a dependent child), you must notify the Plan Administrator within 60 days after the qualifying event occurs. You must provide notice of divorce in writing by mail or facsimile to: Plan Administrator, I.U.O.E. Local 25 Marine Division Medical Plan, 461 State Route 33, Millstone Township, NJ 08535 (fax number 732-446-9167) but you can provide notice of a child’s loss of dependent status by telephone to the Plan Office by calling 800-548-6662. You must notify the Plan of the name(s), social security number(s), address(es) and telephone number(s) of the Employee and the eligible dependent(s) whose coverage under the Medical Plan will be lost due to the Qualifying Event, the nature of the Qualifying Event and the date on which it occurred. The written notice of divorce must be signed and notarized. If the Qualifying Event is divorce, you must include a copy of the divorce decree. Be advised that if you fail to provide timely notification to the Plan of an occurrence of a Qualifying Event, you may forfeit your right to COBRA continuation coverage, and you will be responsible for reimbursement to the Plan of any claims paid on your behalf after the time that you were no longer eligible for coverage. How is COBRA continuation coverage provided? Once the Plan Administrator receives notice that a qualifying event has occurred, COBRA continuation coverage will be offered to each of the qualified beneficiaries. Each qualified beneficiary will have an independent right to elect COBRA continuation coverage. Covered participants may elect COBRA continuation coverage on behalf of their spouses, and parents may elect COBRA continuation coverage on behalf of their children. COBRA continuation coverage is a temporary continuation of coverage that generally lasts for 18 months due to employment termination or reduction of hours of work. Certain qualifying events, or a second qualifying event during the initial period of coverage, may permit a beneficiary to receive a maximum of 36 months of overage. There are also ways in which this 18-month period of COBRA continuation coverage can be extended: 7 Disability extension of 18-month period of COBRA continuation coverage If you or anyone in your family covered under the Plan is determined by Social Security to be disabled and you notify the Plan Administrator in a timely fashion, you and your entire family may be entitled to get up to an additional 11 months of COBRA continuation coverage, for a maximum of 29 months. The disability would have to have started at some time before the 60th day of COBRA continuation coverage and must last at least until the end of the 18-month period of COBRA continuation coverage. You must provide to the Plan Office the original determination letter from the Social Security Administration before the 18-month period of COBRA continuation coverage expires and within 60 days of the latest of i). the date of the Social Security Administration’s determination, ii). the date on which the Qualifying Event occurs, iii). the date on which the Employee or Eligible Dependent loses coverage, or iv). the date on which the Employee or Eligible Dependent is informed of the responsibility to provide such notice. This extension period will end at the earlier of the end of 29 months, when the disabled person becomes entitled to Medicare, or the date as of which the Social Security Administration determines that the disabled person is no longer disabled. Notice must be provided to the Medical Plan office in writing by mail or fax at the address or number provided above within 30 days of the later of the date of the Social Security Administration’s final determination that the individual is no longer disabled or the date on which the Employee or Eligible Dependent is advised of the obligation to provide such notice. Second qualifying event extension of 18-month period of continuation coverage If your family experiences another qualifying event during the 18 months of COBRA continuation coverage, the spouse and dependent children in your family can get up to 18 additional months of COBRA continuation coverage, for a maximum of 36 months, if the Plan is properly notified about the second qualifying event. This extension may be available to the spouse and any dependent children getting COBRA continuation coverage if the employee or former employee dies; becomes entitled to Medicare benefits (under Part A, Part B, or both); gets divorced or legally separated; or if the dependent child stops being eligible under the Plan as a dependent child. This extension is only available if the second qualifying event would have caused the spouse or dependent child to lose coverage under the Plan had the first qualifying event not occurred. 8 Are there other coverage options besides COBRA Continuation Coverage? Yes. Instead of enrolling in COBRA continuation coverage, there may be other coverage options for you and your family through the Health Insurance Marketplace, Medicaid, or other group health plan coverage options (such as a spouse’s plan) through what is called a “special enrollment period.” Some of these options may cost less than COBRA continuation coverage. You can learn more about many of these options at www.healthcare.gov. If you have questions Questions concerning your Plan or your COBRA continuation coverage rights should be addressed to the contact or contacts identified below. For more information about your rights under the Employee Retirement Income Security Act (ERISA), including COBRA, the Patient Protection and Affordable Care Act, and other laws affecting group health plans, contact the nearest Regional or District Office of the U.S. Department of Labor’s Employee Benefits Security Administration (EBSA) in your area or visit www.dol.gov/ebsa. (Addresses and phone numbers of Regional and District EBSA Offices are available through EBSA’s website.) For more information about the Marketplace, visit www.HealthCare.gov. Keep your Plan informed of address changes To protect your family’s rights, let the Plan Administrator know about any changes in the addresses of family members. You should also keep a copy, for your records, of any notices you send to the Plan Administrator. Plan contact information For information about COBRA, contact the Administrator at 461 State Route 33, Millstone Township, New Jersey 08535 (800) 548-6662. 9 COVERAGE WHILE ON MILITARY DUTY (USERRA) If you are covered by this Plan and you enter military service (including the U.S. Armed Forces, the Coast Guard, the Army National Guard, the commissioned corps of the Public Health Service and certain other categories of service), you may be entitled to continue you and your Eligible Dependents’ Plan coverage during your military service for a period up to 24 months. If your military service is 30 days or less, your coverage continues the same as before. If your service exceeds 30 days, you will need to pay the applicable COBRA premium in order to remain covered. Even if you do not elect to continue coverage under COBRA during your military service, you may be entitled to have your coverage reinstated when you return to employment with the same covered Employer following honorable discharge, provided that you return to employment within the time periods prescribed by law. No waiting period or exclusion will be imposed in connection with such reinstatement (unless the waiting period would have been imposed if you remained covered during your military service) except in the case of illness or injury determined by the Secretary of Veterans’ Affairs to be connected to your military service. Separation for uniformed service that is dishonorable or based upon bad conduct, on grounds less than honorable, AWOL, or ending in a conviction under court martial would disqualify you from any rights under USERRA. 10 CONTINUATION OF COVERAGE DURING LEAVE COVERED BY THE FAMILY MEDICAL LEAVE ACT (FMLA) You may be entitled to have contributions made on your behalf while you are not working under the Family Medical Leave Act (FMLA). The FMLA entitles Eligible Employees to take up to a maximum of 12 weeks of unpaid leave during any 12-month period for specified family or medical reasons, such as the birth of a child, child care for the Employee’s children, the adoption of a child by the Employee, the need to care for a family member with a serious health condition, or the Employee’s inability to perform the duties of his position due to a serious health condition. You may also be entitled to up to a maximum of 12 weeks of unpaid leave because of a “qualifying exigency” (as defined in Department of Labor Regulations) arising out of the fact that your spouse, son, daughter or parent is on active duty, or has been notified of an impending call or order to active duty in the Armed Forces in support of a contingency operation. (This new category of leave became effective January 16, 2009. If you believe you are entitled to leave due to a “qualifying exigency,” you should contact your Employer.) In addition, the FMLA now permits a spouse, son, daughter, parent, or next of kin to take up to 26 work weeks of leave (including any other FMLA leave in the same 12-month period) to care for a member of the Armed Forces, including a member of the National Guard or Reserves, who is undergoing medical treatment, recuperation, or therapy, is otherwise in outpatient status, or is otherwise on the temporary disability retired list, for a serious injury or illness. Check with your Employer to determine whether your Employer is subject to the FMLA and whether leave you wish to take is covered by the FMLA. Your Employer has an obligation to continue your coverage under this Plan during a leave of absence that is covered by the FMLA. In order to continue your Plan coverage, your Employer must continue to make contributions on your behalf for any period that you are on approved FMLA leave. Please contact the Plan Office if you intend to take FMLA leave so that we are aware of your Employer’s obligation to make contributions during your absence. Note that if you do not return to work after your FMLA leave ends, you may be required to repay the amount your Employer paid to the Plan for your coverage while on leave. 11 HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA) If you are or expect to be covered by another group health plan, a federal law known as HIPAA guarantees you certain rights under that plan. You should consider your HIPAA rights, as set forth below, in making your decision about COBRA continuation coverage. Under HIPAA, the period during which a group health plan may exclude or limit coverage for pre-existing conditions is reduced or eliminated if the person had previous coverage under another group health plan. However, credit is not given for earlier coverage if you allowed that coverage to lapse, without replacement, for at least 63 days. If there will be some delay between your termination of coverage under this Plan and your enrollment in the new Plan, a break in health coverage can be avoided by maintaining COBRA continuation coverage in the meantime. Starting in 2014, however, plans will no longer be able to impose preexisting condition limitations. You should also consider whether other available coverage has a pre-existing condition that applies to you. You can contact the plan administrator of the other plan to determine whether that plan has a pre-existing condition that applies to you. Certificates of Creditable Coverage (effective through December 31, 2014) When your coverage ends, you and your Eligible Dependents are entitled by law to receive, without charge, a certificate of creditable coverage to participants or dependents who are or were covered under the Plan upon the occurrence of certain events, or upon request. The purpose of these certificates is to provide evidence of the individuals’ coverage to reduce a preexisting condition exclusion period under other plans, to help them enroll in other plans, or to obtain certain types of individual health coverage even if they have health problems. A creditable coverage certificate will be issued to participants and dependents automatically upon cessation of coverage under the Plan. Additionally, a certificate will be provided at any time upon request, as provided below. 12 Who may request a creditable coverage certificate? Any individual who is covered under the Plan, or whose coverage has ceased within the previous 24 months, may request a certificate through December 31, 2014. Additionally, a certificate may be requested by a person or entity designated to make such a request on the individual’s behalf; for instance, by a subsequent plan seeking to verify the individual’s coverage. Certificates will be issued upon request regardless of whether the individual has previously received a certificate. When will a certificate be provided after a request is made? Certificates will be provided in a reasonable and prompt fashion after the request is received. To whom are requests made? All requests for certificates of creditable coverage should be made in writing and should be directed to: Larry Schleyer, Administrator I.U.O.E. Local 25 Marine Division Medical Plan 461 State Route 33 Millstone Township, New Jersey 08535 13 PLAN BENEFITS The Medical Plan provides hospitalization and medical (including physicians’ care, prescription drug, diagnostic, optical, and dental surgery) benefits, optical benefits, dental benefits and death and accidental death and dismemberment benefits, sometimes referred to individually or collectively as “Covered Services”, as described in the following pages. If the benefit or service is not described in this booklet, you should assume that it is not covered by the Plan. Please contact the Plan Office with any questions concerning benefits available under this Plan. Keep in mind that except as specifically described in the following pages, the Medical Plan covers only Medically Necessary care and treatment. The fact that service or supplies are furnished or prescribed by a Physician or other licensed provider does not prove that they are Medically Necessary or covered by this Medical Plan. HOSPITAL AND MEDICAL BENEFITS Network and Non-Network Benefits One important aspect of the Plan is the use of a Preferred Provider Organization (PPO). The Plan has contracted with the PHCS/MultiPlan Network and Horizon Blue Cross Blue Shield of NJ to make available a network of physicians, hospitals and healthcare providers at a reduced cost to you and the Plan. The Plan has also contracted with CVS/Caremark to manage the Plan’s prescription drug program. Essentially, these providers (or any other network the Plan may retain in the future) agree to accept the reduced fees agreed upon with the network as payment in full for Covered Services. You are responsible for a share of the agreed-upon network fee or allowance, generally called your co-payment. The Plan pays the rest, subject to any special limitations on the type of service as described herein. The arrangements between the Plan and the PPOs are flexible, meaning that there is no requirement that you go to a specific hospital, health care provider or pharmacy. You still may choose your hospital, health care provider or pharmacy at the time you receive care. However, as described in more detail below, you will save a significant amount of money if the hospital, health care provider or pharmacy you use participates in the applicable PPO. In most cases, as described below, if you use network providers you will not pay a deductible, and the cost will be covered with the exception of a nominal copayment, subject to specific benefit limits described below. If you use non14 network medical providers, there is a $150 annual deductible applicable to each covered person, and then the Plan pays 80% of Reasonable and Customary charges for the Covered Services provided, subject to specific benefit limitations described herein.. You are responsible for the rest of the provider’s bill. Where applicable, the deductible is charged annually for you and each of your Eligible Dependents, except that if any of you have medical expenses that count toward the deductible in the last three months of a calendar year, the amount payable in those months will also count toward that person’s deductible for the following calendar year. You will receive a Horizon Blue Cross Blue Shield ID card, a PHCS/MultiPlan ID card and a CVS/Caremark prescription ID card. The Horizon Blue Cross Blue Shield card is for the hospitals only; the PHCS/MultiPlan card is for medical providers such as doctors, radiologists, labs, diagnostic centers and other similar providers; the CVS/Caremark prescription card is for retail pharmacies and the Mail Service program for maintenance medication. Please contact PHCS/MultiPlan for up-to-date information if you want to locate a physician and to confirm that a medical provider or facility participates in the PHCS/MultiPlan network. You should contact Horizon Blue Cross Blue Shield of NJ if you want to confirm whether a hospital is in the network. You should also contact CVS/Caremark to confirm whether your pharmacy is participating in the network. Use the toll-free numbers on your ID cards. You may also access Horizon Blue Cross Blue Shield’s provider directory online at www.bcbsnj.com (click on “Provider Directory” at the top of the page). PHCS/MultiPlan’s directory is also available online, at http://www.multiplan.com/patients/. Basic and Major Medical Benefits Benefits under the Medical Plan are divided between Basic and Major Medical benefits. The Basic benefits cover the majority of your hospital stays and, in general, a small portion of other medical Covered Services, excluding pharmacy benefits. The Major Medical benefits cover a significant portion of the balance of Covered Services not covered under Basic benefits. Whether an expense is covered as part of the Basic or Major Medical benefits is generally relevant only in connection with the lifetime limits under the Medical Plan. The amount of the Covered Service that is payable by you will depend more on whether you use a network provider, as described above, than on whether the benefit for the Covered 15 Service in question is payable under the Basic or Major Medical portion of the Plan. 16 HOSPITAL BENEFITS When you or any of your Eligible Dependents requires confinement in a PPO or network hospital, you will be responsible for a copayment of $100 per day, up to a maximum of $500 per admission. The Plan will pay the balance of the PPOnegotiated rate for confinement in a semi-private room for the first 21 days of such confinement. Starting with the 22nd day of such confinement up to a maximum of 120 days, the Plan will pay 90% of the PPO negotiated rate. If you are confined at a non-PPO or non-network hospital, a $200 per day copayment will apply, up to a maximum of $1,000 per admission. The Plan will pay 100% of the Hospital facility charge for confinement in a semi-private room for the first 21 days of such confinement. Starting with the 22nd day of such confinement up to a maximum of 120 days, the Plan will pay 90% of such charges. Hospital benefits (including confinements for rehabilitation, mental and nervous disorders and for alcohol and drug abuse, as described below) are considered Basic. Therefore the copayments described above do not count toward the Major Medical deductible. ALL INPATIENT HOSPITAL CONFINEMENTS MUST BE PREAUTHORIZED. Contact Horizon at (800) 664-2583 to obtain preauthorization, or ask whether the Hospital has contacted Horizon for preauthorization. If you do not obtain preauthorization, coverage for your confinement may be denied in whole or in part if it is later determined that the confinement was not Medically Necessary or was otherwise not covered by the Plan. Related Hospital Confinements If you or one of your Eligible Dependents requires a second Hospital confinement due to an Injury or Illness related to your first confinement, the second confinement shall be considered as a continuation of your first confinement and subject to the 120-day maximum. However, if the cause of any subsequent confinement is not related to the cause of a prior confinement, or if you or your Eligible Dependent had completely recovered from the Injury or Illness which caused a previous confinement, the new confinement shall be considered as a new claim period. 17 Hospital Benefit Exclusions In addition to the General Exclusions set forth starting on page 37, the Plan will not provide Hospital benefits if you are or one of your Eligible Dependents is confined in a Hospital for one of the reasons listed below: 1. surgery for obesity including gastric and intestinal bypass surgery; 2. sex-change surgery; 3. reversal of voluntary sterilization; 4. cosmetic surgery, except for treatment of accidental bodily injuries or unless incurred for treatment of a congenital anomaly in an Eligible Dependent child; 5. confinements commencing on a weekend unless certified by the attending physician as an emergency; 6. surgery for insertion of an inflatable penile prosthesis; 7. injuries sustained while involved in the commission of a criminal act; 8. confinements that are not Medically Necessary or are for treatment or services that are Experimental or otherwise not covered by the Medical Plan. Hospital Confinement in Rehabilitation Hospitals If you or any of your Eligible Dependents requires confinement in an approved rehabilitation Hospital, the Plan will pay for 30 days of confinement in a semiprivate room, provided such confinement occurs within 30 days of a previous confinement in a Hospital for which benefits were previously paid by this Plan. Maternity Benefits Under the Newborns’ and Mothers’ Health Protection Act of 1996, the Plan may not restrict benefits for any hospital length of stay in connection with childbirth for a mother or newborn child to (1) less than 48 hours following normal vaginal delivery; or (2) less than 96 hours following a Caesarean section. In addition, the Plan may not require that an attending provider such as your physician obtain additional authorization for prescribing a length of stay within these limits. 18 The Plan covers doctor visits for the newborn child during the mother’s maternity confinement, provided that the newborn child is an Eligible Dependent. Please note that the Plan covers maternity expenses incurred only by a female Employee or Eligible Dependent wife. The Plan will also cover maternity expenses incurred by an Eligible Dependent child of a Participant if the Eligible Dependent child resides in the state of Massachusetts. Outpatient Surgery If you or one of your Eligible Dependents requires surgery on an outpatient basis in a Hospital or a free-standing surgicenter, the Plan will pay the facility charges under the Hospital benefits. 19 MEDICAL BENEFITS The Plan’s Medical Benefits for in-network Covered Services are paid partially as basic benefit and partially as Major Medical, even though it is paid in full. All Medical Benefits for out-of-network Covered Services are paid as Major Medical benefits, as described more fully below. MAJOR MEDICAL BENEFITS For PPO providers, the Major Medical benefit pays 100% of the network allowance for Covered Services, net of any Basic benefits payable (the “PPO Benefit”). For non-PPO providers, the Major Medical benefits provide 80% of the Reasonable and Customary charges for Covered Services, after satisfaction of a $150 deductible (unreimbursable out-of-pocket) per eligible person per calendar year (the “non-PPO Benefit”). The deductible applies annually for you and each of your Eligible Dependents, except that if you or an Eligible Dependent has Major Medical expenses that count toward the deductible in the last three months of a calendar year, the amount payable in those months will also count toward that person’s deductible for the following calendar year (known as the “carry-over deductible”). What are Medical Covered Services? When you or one of your Eligible Dependents requires treatment for an Illness or an Injury, reasonable expenses for all of the following services and supplies prescribed by your doctor or other approved licensed Provider are Covered Services, subject to the following limits: Physician Office Visits For PPO network physicians, after you pay a $25.00 copayment, the Plan pays the PPO Benefit, described above. The in-network office visit is payable as a Major Medical benefit. 20 For non-PPO providers, the Plan pays the non-PPO Benefit described above. Physician Visits During a Hospital Confinement The Plan pays 100% of the PPO-negotiated rate for a Hospital visit billed by a PPO network physician. $15.00 of the first day’s visit and $12.00 per day thereafter, up to a maximum of 120 days, is a Basic benefit. The remainder is paid as a Major Medical benefit. For non-PPO providers, the Plan pays the non-PPO Benefit, as a Major Medical benefit. Doctor Visits During Confinement in Rehabilitation Hospital The Plan pays $15.00 of the first day’s visit and $12.00 per day thereafter, up to a maximum of 30 days, as a Basic benefit for doctor visits during a confinement of the Employee or an Eligible Dependent in a Rehabilitation Hospital. There is no separate in-network benefit available for these doctor visits. Surgical Benefits Network Surgeons: For surgeries performed by a PPO surgeon, the Plan will pay 100% of the PPO-negotiated rate for the surgery. There is no copayment charged for the surgery. Of the amount paid, a portion is paid as a Basic benefit in accordance with the Plan’s surgical schedule, up to a maximum of $750.00. The balance of the network allowance paid is a Major Medical benefit. Non-network Surgeons: Fees for surgeries performed by a non-network surgeon are payable as a non-PPO Benefit under the Major Medical benefits. Assistant Surgeons: For surgeries where a PPO assistant surgeon is used, the Plan will pay 25% of the PPO-negotiated rate of the primary surgeon for the procedure. For surgeries where a non-network assistant surgeon is used, the Plan will pay 25% of the Reasonable and Customary charges billed by the primary surgeon for the procedure. What Happens If You Have More Than One Operation? Network Surgeons: If two or more surgical procedures are performed through the same incision, the Plan will pay 100% of the PPO-negotiated rate for the procedures. The Plan will apply its surgical schedule to the procedure with the highest network allowance first, as a Basic benefit. The surgical schedule amounts 21 for any subsequent procedures will be reduced by 50% and paid as a Basic benefit. The total amount counted towards the Basic benefit shall not exceed $750.00. The remainder of the network allowance not covered by the Basic benefit shall be covered as a Major Medical benefit. Non-network Surgeons: If two or more surgical procedures are performed through the same incision, the Plan will determine the Reasonable and Customary charges for each of the procedures (the “payable amount”). The Plan will pay, as a Major Medical benefit, 80% of the highest payable amount and no more than 50% of the payable amount(s) for the remaining procedure(s), subject to the $150 deductible. If you or one of your Eligible Dependents requires a second operation that is related to the condition that required the first operation, the total Basic benefit payable for both operations, related to the same Illness or Injury, and performed before either you or your dependent completely recovers from the same Injury or Illness shall not exceed $750.00. All surgical procedures will be considered to be related to the same Injury or Illness unless you furnish acceptable evidence that: The cause of the latest procedure cannot be connected with the cause of any of the prior procedures, or If there is a connection with prior procedures, you had returned to work for at least two weeks (10 working days), or had been registered on the Union’s Out Of Work List for at least two weeks following such related prior procedures, or If there is a connection with prior procedures, your dependent, if employed, had returned to work for at least two weeks (10 working days) or if not employed, had not undergone surgery for any cause for at least 90 days prior to the most recent operation. Dental Surgery Benefit The Plan provides benefits only for the following dental surgeries: 1. Alveolectomy (surgical removal or plastic repair of alveolar process); 2. Apicoectomy (root Amputation); 3. Gingivectomy (cutting of gum); 22 4. Removal of impacted tooth; 5. Odontectomy (removal of unerupted tooth); 6. Osseous surgery (cutting of bone). These specific dental surgeries will be covered as Major Medical benefits and paid at the non-PPO Benefit level. There are no network benefits available for these surgeries. Anesthesia The Plan will provide benefits for anesthesia administered by a licensed anesthesiologist or a certified registered nurse anesthesiologist (CRNA). If the anesthesia is administered by a network provider, the Plan pays 100% of the network allowance as a Basic benefit. If it is administered by a non-network provider, the Plan pays 80% of Reasonable and Customary charges after satisfaction of the deductible as a Major Medical benefit. Diagnostic Benefits For in-network X-ray expenses not related to a Hospital confinement, the Plan will cover 100% of the PPO-negotiated rate after your payment of a $25 copayment. For network labs, the Plan will cover 100% of the PPO-negotiated rate. For MRIs, cat scans and ultrasounds performed by a PPO provider, the Plan will pay 100% of the PPO-negotiated rate, subject to your payment of a $50.00 copayment for each MRI, cat scan or ultrasound procedure performed. This is paid as a Basic benefit. For all diagnostic benefits provided by a non-network provider, the Plan will cover 80% of Reasonable and Customary expenses, subject to the $150 annual deductible. This is paid as a Major Medical benefit. Private Duty Nursing The Plan pays eighty percent (80%) of the first $2,000 of charges, and one hundred percent (100%) of the balance of charges incurred during each calendar year for private duty nursing care rendered by a registered nurse (RN) or a licensed practical nurse (LPN) in or out of the Hospital. No benefits are payable for charges by a nurse who ordinarily resides in an Employee’s household or is a member of his or her immediate family. This is paid as a Major Medical benefit. 23 Chemotherapy & Radiation Therapy The Plan pays 100% of the PPO- negotiated rate for services rendered by a PPO network Physician. For non-PPO providers, the Plan pays 80% of Reasonable and Customary charges. This is paid as a Major Medical benefit. Durable Medical Equipment The Plan will pay for the rental or purchase (whichever is more cost effective as determined by the Plan) of durable medical equipment. Durable medical equipment is equipment or supplies designed for prolonged use that is: primarily and customarily used only to serve a medical purpose; prescribed by a Physician; Medically Necessary; generally useful only to a person with an Illness or Injury. Durable medical equipment includes such items as a wheelchair, hospital-type bed, etc. Only equipment recognized and approved as covered equipment by Medicare will be reimbursable under this benefit. For PPO providers, the Plan pays 100% of the network allowance. For non-PPO providers, the Plan pays 80% of Reasonable and Customary charges. This is paid as a Major Medical benefit whether provided in or out of network. Medical Supplies and Prosthetic Devices The Plan will pay for the cost of 1) medical supplies such as braces, artificial limbs and eyes; 2) the original purchase of trusses, braces, crutches orthotics or similar orthopedic appliances; 3) original purchase of and the fitting with prosthetic appliances required for the initial replacement of natural body parts [lost while you or your dependents are eligible for this coverage], but not dentures or dental prosthetics, except as otherwise provided herein. For PPO providers, the Plan pays 100% of the network allowance. For non-PPO providers, the Plan pays 80% of reasonable and customary charges. This is paid as a Major Medical benefit. 24 Ambulance Services For services provided by a PPO provider, the Plan pays 100% of the negotiated rate as a Basic benefit. For non-PPO providers, the Plan pays 80% of the billed charges as a Major Medical benefit. Chiropractic Services For chiropractic services rendered by a licensed chiropractor, payments will be made for up to twenty (20) visits during each calendar year. The maximum allowance for any one visit will be $35.00. This is paid as a Basic benefit. There is no network benefit available for chiropractic services. Preventive Care Preventive tests, well-care for children, immunizations and other similar preventive services will be covered by the Plan. Covered services include, but are not limited to, mammograms, sigmoidoscopy, colonoscopy, blood tests for cholesterol, PSA or other indicators of possible current or future medical conditions, pap smears, tonometry, breast examinations and vaccinations. Treatment Resulting from Accidental Injury Dental work (including office visit, x-ray) required as a result of an accidental injury is payable at 80% of the negotiated rate for services provided by an innetwork provider. There are no non-network benefits. These benefits are paid as Major Medical benefits. Cosmetic surgery required as a result of an accidental injury is payable as any other surgery (see Surgical Benefits starting on page 21). Physical Therapy, Speech Therapy, Occupational Therapy The Plan pays the PPO Benefit for network providers and the non-PPO Benefit for non-network providers. All benefits are paid as Major Medical benefits. Reconstructive Surgery The Women’s Health and Cancer Rights Act, which was signed into law in 1998, provides that any group health plan that provides medical and surgical benefits with respect to a mastectomy must also provide coverage for reconstructive surgery following the mastectomy. Specifically, if a participant or beneficiary is 25 receiving benefits in connection with a mastectomy, the plan must also provide coverage for: reconstruction of the breast on which the mastectomy was performed; surgery and reconstruction of the other breast to produce a symmetrical appearance; prosthesis and physical complications at all stages of mastectomy, including lymphedemas. This Plan provides coverage for a mastectomy and related reconstructive surgery, as set forth above, under the Surgical Benefits (see page 21). Coverage for the prostheses and for treatment of physical complications is provided under the Major Medical benefits, as set forth above. Hearing Aids The Plan will pay up to $1,000 per hearing aid. The Plan will not pay for more than two (2) hearing aids per Employee or Eligible Dependent in his or her lifetime. This is paid as Basic benefits. NETWORK, PRECERTIFICATION AND REFERRAL PROGRAM FOR MENTAL HEALTH AND SUBSTANCE ABUSE CLAIMS The Medical Plan contracts with the Allied Trades Assistance Program (ATAP) to make available a network of hospitals, physicians and other providers at a reduced cost to you and the Medical Plan for mental health and substance abuse claims. For mental health and substance abuse Hospital or Major Medical claims, you must use a facility or provider within the ATAP Network for the Medical Plan to treat the claims as in-Network claims. Please contact ATAP at (800) 258-6376 (24 hours a day, 7 days a week) to locate an ATAP Network facility or provider. As set forth on page 17 of this Summary Plan Description, all inpatient hospital confinements must be preauthorized. For inpatient Hospital confinements related to a mental health or substance abuse disorder, you must contact ATAP at (800) 258-6376 (24 hours a day, 7 days a week) to obtain preauthorization. You may also ask the facility whether it has obtained the necessary preauthorization from ATAP. If preauthorization is no obtained, coverage for your confinement may be denied in whole or in part if it is later determined that the confinement was not Medically Necessary or was otherwise not covered by the Medical Plan. 26 The Medical Plan offers all participants and dependents access to ATAP’s confidential information and referral service for individuals in need of assistance with the appropriate health care professionals for mental health and substance abuse issues. You can contact ATAP at (800) 259-6376 24 hours a day, seven days a week to access ATAP’s confidential referral and information service. While you are not required to contact ATAP before receiving services (except for preauthorizations of inpatient hospital confinements, as set forth above), we strongly encourage you to contact ATAP for assistance. We understand that it can sometimes be difficult to determine who to turn to and what type of assistance you or a loved one may need when faced with mental health or substance abuse issues. ATAP can help connect you with the most appropriate level of care and with a facility or provider within the ATAP Network. 27 PRESCRIPTION DRUG BENEFITS Your prescription drug benefits are administered by CVS/Caremark, Inc. A prescription drug is a drug that is obtainable only with a prescription written by a Physician. It must be dispensed by a licensed pharmacist and approved for its intended use by the U.S. Food and Drug Administration. This Plan provides benefits only when you fill your prescription through one of CVS/Caremark’s participating retail pharmacies or through CVS/Caremark’s Mail Service Program. To find a participating pharmacy, check www.caremark.com or call: (800) 2412784. When you fill a prescription at a pharmacy, your copayment will depend on whether the drug is a brand name or generic and whether you fill the prescription at a retail pharmacy or through CVS/Caremark’s Mail Service Program. Closed Formulary The Medical Plan has adopted CVS/Caremark’s Standard Formulary for prescription drugs, which is a closed formulary. Medications not included in the Standard Formulary are excluded from coverage, and no benefits will be payable from the Medical Plan for those drugs. Please contact the Medical Plan or call CVS/Caremark at (800) 213-0879 to obtain information about the current Standard Formulary list. Generics and Brand Name Drugs Please check with your prescribing Physician to determine whether a generic form of the medication is available. Using a generic alternative instead of a brand name version of medication saves both you and the Plan money. When a generic is available but the pharmacy dispenses the brand name drug for any reason, you are responsible for the difference between the calculated average wholesale price of the brand name drug and the calculated average wholesale price of the generic drug, in addition to the co-payment set forth below. This rule does not apply to the following drugs: Premarin, Lanoxin, Coumadin and Synthroid. Participating Retail Pharmacies When you fill a prescription at a participating retail pharmacy, the co-payment for generic drugs is $15.00 and the copayment for brand name drugs is $25.00. You may purchase up to a 30-day supply at a time. 28 Out of Network Pharmacy If you fill a prescription at an out-of-network pharmacy, or if you forget to bring your CVS/Caremark identification card, the Plan will cover the amount payable under CVS/Caremark’s allowance for that drug. Mail Service Program When you fill a prescription through the Mail Service Program, the copayment for generic drugs is $30.00 and the copayment for brand name drugs is $50.00. For that copayment, you will receive up to a 90-day supply of the prescription drug. For information on filing claims for Prescription Drugs, please see the Claim and Appeals Procedures section of this booklet, starting on page 44. Maintenance Drug Limitation The Plan limits the number of times you can fill prescriptions for Maintenance Drugs at a retail pharmacy. You may call CVS/Caremark toll-free at 1-866-7503633 to find out whether any medicine you are taking is considered a Maintenance Drug. The Plan will cover two (2) fills per calendar year at the retail pharmacy. Once the annual retail fill limit of two (2) is reached, you must fill the prescriptions through the CVS/Caremark Mail Service Program or at a CVS Pharmacy through the Maintenance Choice program for each 90-day supply as illustrated in the chart below. If you fill the prescription at the retail pharmacy more than two times (other than through Maintenance Choice), you will be required to pay a copayment of $30.00 for generic drugs, $50.00 for brand name drugs for a 30-day supply. Co-Payment Structure For Maintenance Medicines Type of Medicine Retail Pharmacy Us to 2 Fills Retail Pharmacy 3+ Fills Mail Service Pharmacy* Generic $15 co-payment $30 co-payment $30 co-payment Brand Name $25 co-payment $50 co-payment $50 co-payment Days Supply Limit Up to 30-day 90-day 29 Up to 30-day *Includes mediations obtained through a 90-day supply at a CVS pharmacy through the Maintenance Choice program. Prescription Drug Exclusions In addition to the General Exclusions set forth on page 37, the following are excluded from coverage unless otherwise specifically listed as covered: non-federal legend drugs medications not included in the CVS/Caremark Standard Formulary medications not approved by the FDA or approved by the FDA for a different use than that prescribed; cosmetic products and drugs used for cosmetic purposes; medications, including but not limited to vitamins, that can be purchased without a prescription; contraceptive jellies, foams or devices; or contraceptive emergency kits; non-insulin syringes fertility drugs (other than oral medications), sexual or erectile dysfunction drugs; growth hormones; Lupron or sex hormones except for in treatment of menopause; anorexiants; amphetamines; acne medications (Retin-A, Differin) on or after the covered person attains age 24; Renova; glucose monitors; nutritional supplements; prescription devices other than respiratory devices; respiratory therapy supplies; 30 vaccines (covered under the Medical benefit) and toxoids If you have questions concerning the Plan’s prescription drug benefits, you may contact a CVS/Caremark Customer Care representative at 800-213-0879 Monday through Friday from 7:00 a.m. to 9:00 p.m. CST, and from 8:00 a.m. to 12:00 noon CST on Saturday. For those participants with hearing loss requiring TTY assistance, call toll-free 800-231-4403. 31 BENEFITS FOR PENSIONERS ELIGIBILITY FOR PENSIONERS Pensioners and their legal spouses are eligible for Pensioner Benefits as outlined in this section, provided the Pensioner either remained in Covered Employment and was eligible for benefits under this Plan after reaching age 61 1/2; or earned fifteen (15) years of vesting service, regardless of age, from the Local 25 Pension Plan or the IUOE Central Pension Fund and received a Certificate of Award of Total and Permanent Disability from the Social Security Administration. Coverage for the Pensioner’s legal spouse under the Pensioner benefits will terminate as of the earlier of 1) the date the Participant and spouse are divorced; 2) the date such coverage terminates due to a change in the Plan; 3) the last day of the third month following the month in which the Pensioner dies; or 4) the date the Pensioner becomes eligible for coverage under this Plan as an active Employee, as set forth below. If the Pensioner returns to Covered Employment and his or her pension benefits are suspended as a result thereof, the Pensioner and his or her legal spouse’s eligibility for Pensioner Benefits will terminate if and when the Pensioner satisfies the requirements for eligibility for active Employees, set forth starting page 1 of this booklet. Pensioner benefits will resume upon the loss of eligibility as an active Employee. 32 BENEFITS FOR MEDICARE ELIGIBLE PENSIONERS Enrollment In Medicare Parts A And B Is Mandatory All eligible Pensioners and their eligible Dependents must enroll in both Medicare Part A (hospital) and Part B (medical). Part A enrollment is automatic, but you must sign up for Part B. If you do not enroll in Part B, no benefits will be paid by this Plan. Reimbursement Of Part B and Part D Medicare Premium This Plan will reimburse the Medicare eligible Pensioner and his Eligible Dependent $52.00 towards the cost of the monthly Medicare Part B and Part D premiums. This will be the maximum amount reimbursed even if Medicare increases the cost of the Part B or Part D premium. * You must notify the Plan immediately of the death of a Pensioner or Spouse The following benefits are the only benefits provided to Medicare eligible Pensioners and their spouses. These benefits are paid as Basic benefits. Hospital Benefits (Medicare Part A) The Plan will pay the first-day deductible in effect at the time of confinement, not payable by Medicare, for a Hospital confinement. This amount will be considered one day’s benefits. This first day deductible is subject to a deductible imposed by the Plan of $100 per confinement. Medicare will then pay for the next 59 days in full making a total of 60 days. After 60 days, the Plan will pay the coinsurance amount in effect as of the date of service for the next 90 days. For the following 30 days, that is from the 150th day through the 180th day, the Plan will pay the full cost of semi-private accommodations in a Hospital. Medical Expenses Incurred in Connection With Hospital Confinements (Medicare Part B) The Plan will pay the unpaid balance of the approved Medicare amount for physicians, surgeons, radiologists and laboratory charges incurred during a Hospital confinement. 33 Outpatient Surgery The Plan will pay the unpaid balance of the approved Medicare amount for outpatient surgery, as designated by Medicare. Out-Patient Chemotherapy and Radiation Therapy The Plan will pay the unpaid balance of the approved Medicare amount for maintenance chemotherapy or radiation therapy on an outpatient basis. OutPatient Holter Monitor Testing The Plan will pay the unpaid balance of the approved Medicare amount for Hotter monitor testing on an outpatient basis. Prescription Drug Benefits There are no prescription drug benefits available under this Plan to retired Medicare-eligible Pensioners. 34 BENEFITS FOR NON-MEDICARE AND ELIGIBLE PENSIONERS Pensioners and their eligible Dependents who are not yet Medicare-eligible receive the same Hospital benefits described in this booklet for active Employees, as well as all other expenses related to Hospital confinement. The Plan will also pay surgical benefits and radiology benefits for such individuals at the same levels provided for active Employees. Out-Patient Chemotherapy and Radiation Therapy For maintenance chemotherapy or radiation therapy provided on an outpatient basis, the Plan will pay 100% of the negotiated rate for services rendered by a PPO provider and 80% of the R&C charges for services rendered by a nonnetwork provider. Holier Monitor Testing The Plan will pay 80% percent of the R&C charges incurred for out-patient testing of a Holter Monitor. Prescription Drug Benefit For Pensioners who are not yet Medicare eligible and their Eligible Dependents, the Plan will reimburse $100 per calendar year and $2.00 per prescription thereafter to each eligible Pensioner and his legal spouse after they each satisfy a calendar year deductible of $100. No further prescription drug benefits are available under this Plan. 35 OPTICAL BENEFITS The Plan will reimburse you, as a basic benefit for you or any of your Eligible Dependents who are 19 years of age or older, up to $150 for an eye examination, frames and single vision lenses from an optometrist or ophthalmologist. If you require bifocal lenses, the benefit will increase to $175. Benefits are not limited for anyone under the age of 19. You may use any optical provider you choose. In order to claim Optical Benefits, send in a copy of your paid receipt for frame, lenses and /or optometrist’s or ophthalmologist’s paid bill. The paid bill and/or receipt should clearly state your name, the date you or your Eligible Dependent received glasses, the total cost, the optometrist’s or ophthalmologist’s name, and whether you received single vision lenses or bifocals This benefit is available once every two (2) years. The two-year period for eligibility begins to run on the date of the examination or the receipt of frames or lenses. Special Cataract Glasses If you or one of your Eligible Dependents is over age 18 or over and undergoes surgery for the removal of a cataract or a corneal transplant, the Plan will pay up to $250.00 for the cost of cataract contact lenses or special glasses required after such surgery. For any one who is under the age of 19, there is no limit on the cost of cataract contact lenses or special glasses required after such surgery. 36 GENERAL EXCLUSIONS The Plan does not cover the following: Services or supplies provided or paid for by the U.S. government or any other government, except if there would be a legal obligation for you to pay for the charges without regard to the existence of any insurance or employee benefit plan; 1. or other provider to himself for his immediate family (including grandchildren). 2. Experimental drugs. Charges for dentures, dentistry or dental X-rays except as provided herein. 3. Charges for cosmetic surgery, except as provided herein. 4. Charges incurred for care and treatment of sickness or injury caused or contributed to by an act of war. 5. Charges for injuries sustained in connection with a) travel in or on a snowmobile, three- or four-wheeled all-terrain vehicles or any other motorized vehicle not requiring licensing as a motor vehicle; b) participation in hazardous recreational activities including, but not limited to, skydiving, parasailing, hang gliding, bungee jumping, or the use of jet skis (or other like personal watercraft) or motorized scooters. 6. Charges related to an Illness or Injury that is employment-related or that is covered under workers compensation law, occupational disease law the Jones Act or similar laws. 7. Services, supplies or treatments which are not Medically Necessary; 8. Experimental procedures or treatments. 9. Fees which are in excess of the Reasonable and Customary charges for such services, supplies or treatments. 10. Charges that are not submitted, along with all information and documentation necessary to process the claim, within 12 months of the date services were rendered. 11. Infertility procedures. 37 12. Artificial insemination, in-vitro fertilization, G.I.F.T. or similar procedures, and any services associated with such procedures. 13. Expenses incurred as a result of past or present services in the armed forces of any government. 14. Expenses incurred for care related to military service provided in a veterans’ facility or a Hospital operated by the U.S. government, unless required by law. 15. Charges that you or your Dependent are not legally required to pay, including charges that would not have been assessed if no insurance coverage existed. 16. Services for which there is no legally enforceable charge. 17. Charges for Custodial Care. 18. Charges for meals, meal preparation, personal comfort or convenience items. housekeeping services and protective or companion services. 19. Charges incurred in the completion of forms and mailing fees. 20. Handling fees. 21. Expenses incurred in connection with the failure to keep a scheduled appointment. 22. Interest or other penalties. 23. Service provided by a Physician 24. Charges for lasik eye surgery or refractive eye surgery, including 25. Charges for services rendered by a naturopath, homeopathic, hypnotherapy, faith-healer or other like services. 26. Expenses related to surrogate parenting. 27. Charges for Injuries that are sustained in connection with the commission of a criminal act by the injured person. 28. Travel expenses, except as specifically provided herein. 38 keratotomy. 29. Services rendered by interns, residents and Physicians in training. 30. Charges related to the medical treatment of obesity. 31. Services or supplies for or in connection with acupuncture (unless performed by licensed Physician). 32. Expenses relating to transsexual surgery or counseling. 33. Services rendered in connection with the treatment of TMJ. 39 DENTAL BENEFITS Dental benefits for eligible Employees their eligible Dependents is self-insured by the Plan but administered by Delta Dental. Information concerning the dental benefits available to you under this Plan is set forth in a separate booklet that is included with this Summary Plan Description. The dental benefit information is incorporated and made a part of this Summary Plan Description as if fully set forth herein, and all general provisions, exclusions and limitations apply. 40 LIFE INSURANCE BENEFITS Life insurance for eligible Employees and Pensioners is provided through CIGNA, an insurance company. For eligible Employees, the amount of the basic life insurance benefit is $10,000 and the amount of the accidental death benefit is $10,000. For eligible Pensioners, the amount of the basic life insurance benefit is $3,000. Pensioners are not eligible for the accidental death benefit. The proceeds of the life insurance and accidental death benefits are not taxable to the beneficiary. A Group Life Insurance Certificate and a Group Accident Insurance Certificate from CIGNA describing the important details of your life insurance and accidental death and dismemberment benefits are included as appendices to this Summary Plan Description. The Certificates are incorporated and made a part of this Summary Plan Description as if fully set forth herein, and all general provisions, exclusions and limitations apply. 41 COORDINATION OF BENEFITS There are certain circumstances when the Plan will not provide benefits for medical expenses because either your or your dependents have other health insurance coverage. In these circumstances, either you or your dependents’ health insurance coverage will have primary responsibility for paying the medical expenses incurred. These circumstances are listed below: If your spouse or any of your dependent children are employed and have group insurance through their employer, then your spouse’s employer or children employer’s insurance company is primarily responsible for paying benefits for their medical expenses. If your spouse has group insurance through her employer, and you have dependent children, the primary responsibility falls with that Plan covering the parent whose birthday falls earlier in the year. Only the month and day of each parent’s birthday will be used to determine the primary carrier. If the primary insurance carrier does not cover all medical expenses, then the Plan, as secondary carrier, will pay any balance not paid by the other Group or Individual carrier, subject to the limits of this Plan. What Happens If You Have Your Own Individual Insurance? If you have arranged for your own individual health insurance for yourself and your family, your individual insurance coverage is responsible for paying benefits for any medical expenses you incur. What Happens If You Or Your Spouse Are Covered By More Than One Group Plan? If either you or your spouse are covered by more than one group insurance, the Group Plan which has insured either of you longer will provide benefits. What Happens If You Or Your Dependents Are In An Accident involving an Automobile or Motorcycle? No benefits shall be paid by the Plan for expenses related to Injuries sustained in an automobile or motorcycle accident, except to the extent such expenses exceed the limits of coverage for medical payments provided under the participant’s or 42 injured dependent’s automobile or motorcycle insurance (including, but not limited to no fault insurance, personal injury protection (PIP) or MedPay; referred to collectively herein as “medical payments coverage”). Each participant or dependent who maintains a vehicle or motorcycle is required to obtain at least $250,000 of medical payments coverage or similar coverage if that coverage is available in the state in which the vehicle is insured (regardless of whether such coverage is required in your state). If medical payments coverage is available, but only at an amount less than $250,000, then you are required to obtain the maximum amount available. Where medical payments coverage is available in the amount of $250,000 or more, you must obtain coverage at no less than $250,000. If you demonstrate to the Plan Office that no such coverage is available at all in your state, and you cannot obtain it, then and only then will you be excused from obtaining such coverage. In the event that a medical claim is filed arising out of an automobile or motorcycle accident, and you have either no medical payments coverage or less than $250,000 of such coverage, the Medical Plan will investigate whether you are excused from having had full $250,000 in coverage. 43 CLAIMS AND APPEALS PROCEDURES What Is A Claim? In reading these procedures, please keep in mind that a claim for benefits is a request for Plan benefits made in accordance with the Plan’s claims procedures, as set forth herein, and requires submission of a written claim form. Simple inquiries about the Plan’s provisions or eligibility that are unrelated to any specific benefit claim will not be treated as claim for benefits. In addition, a request for prior approval of a benefit that does not require prior approval by the Plan is not a claim for benefits. HOW TO FILE A CLAIM Claims for Hospital, Major Medical or Surgical Benefits In-Network You generally do not need to submit a claim form or any other paperwork when you receive services from a provider who participates (a “participating provider”) in the PHCS/MultiPlan or Horizon Blue Cross Network. You need only present your PHCS/MultiPlan or Horizon identification card at the time services are rendered and pay the applicable co-payment. The network provider is responsible for submitting the claim and any required information. Out-of-Network If you receive services from a non-participating provider, you or your provider must submit a claim directly to the Plan. The claim must include the following information procedure code diagnosis code date(s) of service location of services services rendered provider’s name, address and Employer Identification Number 44 provider’s charges for services participant’s name, address, home phone number, date of birth and social security number patient’s name, address, home phone number, date of birth and social security number such other information or proof reasonably required by the Plan Preauthorization You must obtain preauthorization for any Hospital confinement. Contact Horizon at: (800) 664-2538 to obtain preauthorization, or check to see whether the Hospital has contacted Horizon on your behalf. For inpatient confinements related to mental health or substance abuse, contact ATAP at (800) 258-6376 for preauthorization. Claims for Prescription Drug Benefits 1. In-Network If you obtain a prescription from a CVS/Caremark participating retail pharmacy, you need only submit your CVS/Caremark identification card to the pharmacist and pay the applicable copayment. You may contact CVS/Caremark at the telephone number listed on your identification card to locate a participating pharmacy in your area. To use the Mail Order Program, ask your Physician to write you a prescription for a 90-day supply with enough refills to cover you until your next doctor’s appointment. Contact the Plan Office or CVS/Caremark at (866) 750-3633 to obtain a Mail Service Order form. Complete the Mail Service Order Form and send it with your prescription and the applicable co-payment to: CVS/Caremark, P.O. Box 52196, Phoenix, AZ 85072-2196 Your payment may be made by check, money order or credit card. For credit card payments, simply include your Visa, Discover or 45 MasterCard number and expiration date in the space provided on the Mail Service Order Form. You will receive your prescription within 10-14 days after CVS/Caremark receives your order. 2. Out of Network If you get your prescription filled at a pharmacy that does not participate in the applicable network, or if a participating pharmacy refuses to fill your prescription without payment in advance (such as when you do not have your prescription ID card), you must pay the pharmacy directly and submit a completed claim reimbursement form to CVS/Caremark with your original receipt. You will be reimbursed based upon the Plan’s discount fee arrangement, which will be less than what you pay the pharmacy. Contact the Plan Office to obtain a claim form. 3. Prescription Drug Claims for Pensioners and Eligible Dependents that are Not Medicare Eligible In order for Non-Medicare eligible Pensioners and their Eligible Dependents to claim the Plan’s Prescription Drug benefit, the claims must submit to the Plan Office: a) the bill(s) from the pharmacist(s) for the prescriptions for which you are seeking reimbursement; and b) prior pharmacy bills for the claimant for that calendar year showing that the claimant has already incurred $100 in out-of-pocket prescription drug costs and satisfied the $100 deductible. All pharmacy bills must include the date the prescription drug was received, the name of the person receiving the medicine, the prescription number, the name of the prescription drug and the name of the physician who prescribed the medicine. Claims for Optical Benefits In order to obtain optical benefits, you can either pay the provider directly and submit the paid itemized bill to the Plan Office for reimbursement according to the Plan’s fee schedule, or your provider can submit the itemized bill to the Plan Office for reimbursement. 46 Claims for Death, Accidental Death or Dismemberment Benefits In order to obtain death, accidental death or dismemberment benefits, contact the Plan Office for an application. The Plan Office will advise you of any documentation necessary to process your claim (i.e., certified copy of death certificate). Please refer to your CIGNA Insurance Certificates for additional information. TIME FRAMES FOR SUBMITTING CLAIMS All claims must be submitted within twelve (12) months of (1) the date the service/treatment was rendered; (2) for inpatient hospital admissions, the date of discharge from the hospital. Any claim that is not submitted within this twelve (12) month time frame shall be denied as untimely. Please refer to your CIGNA Insurance booklets for information regarding filing deadlines for life insurance and accidental death and dismemberment claims. TIME FRAMES FOR PROCESSING CLAIMS You will ordinarily be notified of the decision on your claim within 30 days from the Plan’s receipt of your claim. The Plan may extend this period one time for up to 15 days if the extension is necessary due to matters beyond the control of the Plan provided that, prior to the expiration of the initial 30-day period, the Plan notifies you of the circumstances requiring the extension of time and the date by which the Plan expects to render a decision. If an extension is needed because the Plan needs additional information from you, the extension notice will specify the information needed. In that case you will have 45 days from your receipt of the notification to supply the additional information. If the information is not provided within that time, your claim will be denied. During the 45-day period you are given to supply additional information, the 30-day period for making a decision on the claim will be suspended. The deadline is suspended from the date of the extension notice until the earlier of (1) 45 days or (ii) until the date you respond to the request (whichever is earlier). The Plan then has 15 days to decide your claim and notify you of the determination. 47 NOTICE OF DECISION You will be provided with written notice of a denial of a claim. This notice will state: The specific reason(s) for the determination Reference to the specific Plan provision(s) on which the determination is based A description of any additional material or information necessary to perfect the claim, and an explanation of why the material or information is necessary A description of the appeal procedures and applicable time limits A statement of your right to bring a lawsuit under ERISA following an adverse benefit determination on review If an internal rule, guideline or protocol was relied upon in deciding your claim, you will receive either a copy of the rule or a statement that it is available upon request at no charge If the determination was based on the absence of medical necessity, or because the treatment was experimental or investigational, or other similar exclusion, you will receive an explanation of the scientific or clinical judgment for the determination applying the terms of the Plan to your claim, or a statement that it is available upon request at no charge 48 APPEALS PROCEDURE If your claim is denied in whole or in part, or if you disagree with the decision made on a claim, you may appeal the Plan’s determination to the Board of Trustees (the “Trustees”). Your appeal must be made in writing within 180 days after you receive notice of denial of your claim and must set forth the reasons why you believe the Plan’s decision is incorrect. For hospital claims, send your written appeal within one year of your receipt of the explanation of benefits to Horizon BCBSNJ, Attn: Appeals Coordinator, PO Box 317, Newark, NJ 07101. For mental health and alcohol/substance abuse claims, send your written appeal within one year of your receipt of the explanation to the Fund Office, 461 State Route 33, Millstone Township, New Jersey 08535. You MUST exhaust the appeals procedures set forth below prior to filing any legal action on a claim for benefits from the Plan. Right to Review Documents and to Obtain Other Information You have the right to review documents relevant to your claim. A document, record or other information is relevant if it was relied upon by the Plan in making the decision; it was submitted, considered or generated (regardless of whether it was relied upon); it demonstrates compliance with the Plan’s administrative processes for ensuring consistent decision making; or it constitutes a statement of the Plan’s policy regarding the denied treatment or service. Upon request, you will be provided with the identification of medical experts, if any, who advised the Plan concerning your claim, without regard to whether the advice was relied upon in deciding your claim. Right to Independent Review A different person(s) will consider your appeal than the one who originally denied the claim. The reviewer(s) will not give deference to the initial denial. The decision will be made on the basis of the record, including such additional documents and comments that you submit. Cases Involving a Medical Judgment If your claim was denied on the basis of a medical judgment (such as a determination that the treatment or service was not medically necessary, or was 49 investigational or experimental), a health care professional who has appropriate training and experience in a relevant field of medicine will be consulted. Time Frames for Appeals For appeals on hospital claims, you will be advised of Horizon’s decision within 60 days of their receipt of your request. If you wish to challenge that decision, you have the option to submit a voluntary appeal to the Board of Trustees of the Plan or to pursue legal remedies. If you want to submit a voluntary appeal to the Trustees, send your written appeal to the Plan Office within 60 days after your receipt of Horizon’s decision. Your appeal should explain why you think their decision was incorrect. Decisions by the Trustees on voluntary appeals will be made within the same time frames as decisions on post-service appeals, set forth below. We encourage you to pursue an appeal before the Trustees on a claim denied by Horizon prior to commencing legal action, however, it is not required. For all other appeals, a decision will generally be made at the next regularly scheduled meeting of the Board of Trustees following receipt of your appeal. However, if your appeal is received within 30 days of the next regularly scheduled meeting, your appeal will be considered at the second regularly scheduled meeting following receipt of your appeal. In special circumstances, a delay until the third regularly scheduled meeting following receipt of your appeal may be necessary. You will be advised in writing in advance if this extension will be necessary. You will be notified of the Trustees’ decision concerning your appeal as soon as possible, but no later than 5 days after the decision has been reached. NOTICE OF THE DETERMINATION ON YOUR APPEAL The Trustees’ decision on your appeal will be in writing and will include the following information: The specific reason(s) for the determination Reference to the specific Plan provision(s) on which the determination is based A statement that you are entitled to receive reasonable access to and copies of all documents relevant to your claim, upon request and free of charge A statement of your right to bring a lawsuit under ERISA following denial of your appeal 50 If an internal rule, guideline or protocol was relied upon by the Plan, you will receive either a copy of the rule or a statement that it is available upon request at no charge If the determination was based on medical necessity, or because the treatment was experimental or investigational, or other similar exclusion, you will receive an explanation of the scientific or clinical judgment for the determination applying the terms of the Plan to your claim, or a statement that it is available upon request at no charge. The Trustees shall, subject to the requirements of applicable law, be the sole judges of the standard of proof required in any claim and the application and interpretation of this Plan and any of the plan documents. Without limiting the generality of the foregoing, the Trustees shall have the sole and absolute discretionary authority to: Take all actions and make all decision with respect to the eligibility for and the amount of benefits payable under the Plan; Formulate, interpret and apply rules, regulations and policies necessary to administer the Plan in accordance with its terms; Decide questions, including legal and factual questions, relating to the payment of benefits under the Plan; Resolve and/or clarify any ambiguities, inconsistencies and omissions arising under the summary plan description or other Plan documents; Process and approve or deny benefit claims and rule on any benefit exclusions; and Decide all matters arising in connection with the operation or administration of the Plan. The decision of the Board of Trustees or its designated committee will be final and binding on all parties and shall be given deference in all courts of law to the greatest extent allowed by applicable law. You must exhaust the Plan’s administrative appeal process prior to filing any lawsuit regarding a claim for benefits. 51 DESIGNATED AUTHORIZED REPRESENTATIVES You may submit a claim and appeal a denial of a claim on your own behalf. Alternatively, you may designate another individual to act as your representative. If you choose to designate someone else to act on your behalf, you must do so in writing on a form provided by the Plan. Contact the Plan Office to obtain the form. The Plan will not recognize designations unless they are done on the form provided by the Plan. The designation will not be effective until it is received by the Plan. Once you have designated an Authorized Representative, all communications and notices from the Plan that would otherwise be sent to you will only be sent to your Authorized Representative, unless you advise us to the contrary. In addition, if you designate an Authorized Representative, we will disclose protected health information related to the appeal to that Authorized Representative. You may revoke your designation of an Authorized Representative but such revocation will not be effective until received by the Plan. The revocation must be in writing in order to be effective. LIMITATION ON TIME TO FILE LAWSUITS FOR CLAIMS FOR BENEFITS If an appeal for Medical Plan benefits is denied in whole or in part or if any other adverse benefit determination is made with respect to the benefits available under this Plan, and the appeals process has been exhausted, the participant (or his or her authorized representative) may, to the extent provided by law, file a lawsuit in a court of appropriate jurisdiction challenging the denial or benefit determination. Effective for denials and other benefit determinations made on or after October 1, 2014, however, any such lawsuits must be filed within no later than one year from the date of the Medical Plan’s notice of denial of the appeal or other final adverse benefit determination, ad also within any statute of limitations which may be applicable. 52 SUBROGATION AND RESTITUTION RIGHTS If you or your Eligible Dependent suffer an injury or illness through the act or omission of someone else, the Plan shall pay benefits related to such injury or illness to the extent benefits are payable under the terms of the Plan, provided that the benefits have not already been paid by the third party. By accepting benefits from this Plan related to such an injury or illness, you agree to hold any reimbursement or other recovery received by you (or your Eligible Dependent, legal representative or agent) in trust on behalf of the Plan to cover all benefits paid by the Plan with respect to such injury or illness and to reimburse the Plan promptly for the benefits paid. Benefits are paid by the Plan subject to the condition that you and your Eligible Dependent do not take any action that would prejudice the Plan’s ability to recover benefits paid and that you will cooperate in doing what is reasonably necessary to assist the Plan in obtaining reimbursement. The Plan must be reimbursed in full up to the total amount of all benefits paid by the Plan in connection with the injury or illness from any recovery you receive from a third party, even if the recovery is not specifically identified as a reimbursement of medical expenses. All recoveries from a third party (whether by lawsuit, settlement, insurance or otherwise) must be used to reimburse the Plan for benefits paid. The Plan has the right of first reimbursement out of any recovery obtained, even if you are not fully compensated (“made whole”) for your loss, and the Plan’s claim has first priority over all other claims and rights. In addition, the Plan’s claim is not subject to reduction for attorney’s fees or costs under the “common fund” doctrine or otherwise. Any reduction of the Plan’s claim is subject to prior written approval by the Trustees of the Plan in their sole discretion. You are required to notify the Plan promptly of any third party claim you may have for an injury or illness for which the Plan has paid or may pay benefits and any demand made or suit filed against any third party. You are required to notify the Plan of any third party recovery, whether in or out of court, that you or your Eligible Dependent obtain. If you choose not to pursue the liability of a third party, the Plan will be subrogated to your right of recovery and may pursue your claims against the third party. You agree to cooperate with the Plan with respect to any attempt to recover Plan benefits paid to you or your Eligible Dependent related to an injury or illness caused by the act or omission of a third party. You must sign a subrogation agreement and provide the Plan with any other relevant information about the claim if we ask you to do so. However, a subrogation agreement is not necessary to enforce the Plan’s rights. You must forward any recovery to the Plan within 10 days of receipt or notify the Plan of why you are 53 unable to do so. The Plan shall have a lien on any recovery until you reimburse the Plan for the amount of its claim. The Plan may offset its subrogation claim against any other Plan benefits otherwise due or payable to you or your Eligible Dependents. Note that this Plan may exclude or limit coverage under certain circumstances where the injury or illness may have been the result of the act or omission of a third-party (e.g., workers’ compensation cases, certain automobile accidents, etc.). Please refer to the Plan documents for information on specific limitations and exclusions. 54 MISREPRESENTATION AND FRAUD If a Participant or other individual received benefits as a result of a misleading representation or any other type of false information provided to the Plan, such person(s) will be required to repay all amounts incorrectly paid by the Plan. Fraud includes such person’s failure to disclose any other group health coverage under which such person is entitled to receive reimbursement of a claim submitted to the Plan. The Board of Trustees commence legal action against a Participant or other individual for restitution and hold them liable for all costs of collection, including interest and attorneys’ fees. The Trustees may also revoke eligibility and offset future claim payments with respect to the Participant or Dependent to recoup the amount owed. The Trustees reserve the right, in their sole discretion, to determine what proof is necessary to determine whether the medical expenses for which a claim is made were actually incurred on the dates specified. The Plan further reserves the right to require a medical examination, by a Physician chosen by the Plan, of a Participant or Dependent whose injury or illness is the basis of a claim, when and as often as the Trustees may determine is necessary and appropriate. 55 OVERPAYMENTS If a payment made to a Participant or Dependent or assigned to a provider is determined to be paid in error or otherwise an overpayment, the Board of Trustees may revoke the Participant’s and the Dependent’s eligibility, commence legal action to recover the overpayment and offset future claim payments to recover the amount overpaid. 56 ASSIGNMENTS A Participant or Dependent may assign payment of benefits only to the provider that rendered the services or supplies by executing a proper assignment of benefits. No benefit payable under the terms of this Plan shall otherwise be subject to the debts, contracts or liabilities of any individual covered by this Plan. 57 RESERVATION OF RIGHTS While we anticipate that the Medical Plan will remain in effect indefinitely, the Trustees reserve the right, in their sole discretion, to amend, modify or terminate the Plan at any time. The Trustees specifically reserve the right to change, reduce, eliminate or add to the benefits provided to Employees, Pensioners, Eligible Dependents, and survivors under the Plan, and may amend the eligibility rules applicable to all benefits, including those provide to Pensioners and Eligible Dependents and survivors. The continuance of the Plan is subject to the maintenance of Collective Bargaining Agreements which provide for Employer contributions to the Plan. No benefits or rules described in this booklet are guaranteed or vested for any Employee or Pensioner, Eligible Dependent or survivor of any Employee or Pensioner. All benefits may be changed, reduced or eliminated at any time by the Trustees of the Plan, in their sole discretion. 58 TERMINATION OF PLAN If it ever becomes necessary to terminate the Plan, the Plan’s trust document provides that assets then remaining in the Plan, after providing for claims, liabilities and administrative expenses, will be applied in such manner as the Board of Trustees may determine to provide, to the extent possible, for the payment of benefits provided under the Plan to eligible Participants and their covered dependents. In no event will the assets of the Plan revert to any Employer or the Union, except in the case of an overpayment where a refund may be permitted by law. 59 NOTICE OF PRIVACY PRACTICES THIS NOTICE DESCRIBES HOW MEDICAL INFORMATION ABOUT YOU MAY BE USED AND DISCLOSED AND HOW YOU CAN GET ACCESS TO THIS INFORMATION. PLEASE REVIEW IT CAREFULLY. THIS NOTICE ALSO APPLIES TO YOUR ELIGIBLE DEPENDENTS. PLEASE SHARE IT WITH THEM. Introduction The Medical Plan (“Plan”) is a covered entity within the meaning of the Health Insurance Portability and Accountability Act of 1996, commonly known as “HIPAA.” Under HIPAA, the Plan is legally required to provide you with notice of our legal duties and privacy practices with respect to protected health information (“PHI”). PHI includes any individually identifiable information that relates to your physical or mental health, the health care that you have received or payment for your health care, including name, address, date of birth and Social Security number. We are legally required to maintain the privacy of your PHI. The primary purpose of this notice is to describe the legally permitted uses and disclosures of PHI, some of which may not apply to this Plan in practice. This notice also describes your right to access and control your PHI. We are required to abide by the terms of this Notice of Privacy Practices (“Notice”). However, we reserve the right to change the terms of this or any subsequent Notice at any time. If we elect to make a change, the revised Notice will be effective for all PHI that we maintain at that time. Within 60 days of any material revision of our privacy practices we will distribute a new Notice. Additionally, you may contact the Plan directly at any time to obtain a copy of the most recent Notice, or visit our website at www.iuoelocal25.org to view or download the current Notice. This Notice is effective September 23, 2013. 60 Permitted Uses And Disclosures We use and may disclose your PHI1 in connection with your receiving treatment, our payment for such treatment and for health care operations. Contact the Privacy Officer at (800) 548-6662 to obtain a copy of the appropriate form to authorize the people who may receive this information or download the form from our website at www.iuoelocal25.org. Generally we will make every effort to disclose only the minimum necessary amount of PHI to achieve the purpose of the use or disclosure. Treatment: means the provision, coordination or management of your health care. As a health plan, while we do not provide treatment, we may use or disclose your PHI to support the provision, coordination or management of your care. For example, we may disclose the fact that you are eligible for benefits to a provider who contacts us to verify your eligibility for benefits under the health plan. Payment: means activities in connection with processing claims for your health care. We may need to use or disclose your PHI to determine eligibility for coverage, medical necessity and for utilization review activities. For example, we could disclose your PHI to physicians engaged by the Plan for their medical expertise in order to help us determine medical necessity and eligibility for coverage under the plan. We may also disclose your PHI to third parties who are known as “Business Associates” that perform various activities (e.g., hospital pre-authorization, case management) for us. In such circumstances, we will have a written contract with the Business Associate, which requires the Business Associate to protect the privacy of your PHI. We may also disclose your PHI, and your dependents’ PHI, on explanations of benefit forms (“EOBs”) and other payment related correspondence, such as precertifications, which are sent to you. If you appeal a benefit determination on behalf of an eligible dependent, we may disclose PHI related to that appeal to you. If you appeal a benefit determination and you designate an Authorized Representative to act on your behalf, we will disclose PHI related to that appeal to that Authorized Representative. 1 Except for psychotherapy notes, which require your specific authorization. The Plan does not routinely use or disclose psychotherapy notes. 61 Health Care Operations: generally means general administrative and business functions that the Plan must perform in order to function as a health plan. For example, we may need to review your PHI as part of the Plan’s efforts to uncover instances of provider abuse and fraud. In addition, we may combine the PHI of many participants or their eligible dependents to help us decide on the services for which we should provide coverage. We may disclose your PHI, including your eligibility for health benefits and specific claim information to other covered entities, such as health plans, in order for us to coordinate benefits between this Plan and/or another plan under which you or a covered dependent may have coverage. Reminders: We may use your PHI to provide you with reminders. For example, we may use your child’s date of birth to remind you that you may purchase continuation coverage for your 26-year old child who would otherwise lose coverage under the Plan. Treatment Alternatives: We may use your PHI to inform you about treatment alternatives. Health-Related Benefits And Services: We may use or disclose your PHI to inform you about other health-related benefits and services that may be of interest to you. Disclosure To Trustees Of The Plan: We may disclose your PHI to the Trustees of the Plan in connection with requests for extension of disability due to temporary disability or appeals that you file following a denial of a benefit claim or a partial payment. Trustees may also receive PHI if necessary for them to fulfill their fiduciary duties with respect to the Plan. Such disclosures will be the minimum necessary to achieve the purpose of the use or disclosure. In accordance with the Plan documents, the Trustees must agree not to use or disclose PHI other than as permitted in this Notice or as required by law and not to use or disclose the PHI with respect to any employment-related actions or decisions or with respect to any other benefit plan maintained by the Trustees. Others Involved In Your Health Care Or Payment For Your Health Care: Unless we agree to your request that we not do so, we may disclose your spouse or to another member of your immediate family PHI that is directly relevant to that person’s involvement in your health care or payment of your health care. For instance your spouse may be told whether or not a claim for services rendered to 62 you has been paid. We may also disclose your PHI to any authorized public or private entities assisting in disaster relief efforts. Personal Representatives: We may disclose your PHI to your Personal Representative in accordance with applicable state law or the HIPAA Privacy Rule. A Personal Representative is someone authorized by court order or power of attorney, and a parent of a child, in most cases. In addition, your Personal Representative can exercise your personal rights with respect to PHI. While generally a parent is the Personal Representative of an unemancipated minor child, under certain circumstances we may require parents to submit requests in writing regarding PHI, other than payment information of such children, in order to evaluate the request. Required By Law: We may use or disclose your PHI to the extent that we are required to do so by federal, state or local law. You will be notified, if required by law, of any such uses or disclosures. Public Health: We may disclose your PHI for public health purposes to a public health authority that is permitted by law to collect or receive the information. The disclosure will be made for the purpose of preventing or controlling disease (including communicable diseases), injury or disability. If directed by the public health authority, we may also disclose your PHI to a foreign government agency that is collaborating with the public health authority. Health Oversight: We may disclose your PHI to a health oversight agency for activities authorized by law, such as audits, investigations, inspections and legal actions. Oversight agencies seeking this information include government agencies that oversee the health care system, government benefit programs, other government regulatory programs and civil rights laws. Abuse Or Neglect: We may disclose your PHI to any public health authority authorized by law to receive reports of child abuse or neglect. In addition, if we reasonably believe that you have been a victim of abuse, neglect or domestic violence we may disclose your PHI to the governmental entity or agency authorized to receive such information. In this case, the disclosure will be made consistent with the requirements of applicable federal and state laws. We will promptly inform you that such a disclosure has been or will be made, unless we reasonably believe that informing you would place you at risk of serious harm, or we’d be informing a personal representative of yours who we reasonably believe is responsible for the abuse, neglect, or injury. 63 Food And Drug Administration : Our Prescription Benefits Manager may disclose your PHI to a person or company subject to the jurisdiction of the Food and Drug Administration (“FDA”) with respect to an FDA-regulated product or activity for which that person has responsibility, for the purpose of activities related to the quality, safety or effectiveness of such FDA-regulated product or activity. Legal Proceedings: We may disclose your PHI in the course of any judicial or administrative proceeding, in response to an order of a court or administrative tribunal. In addition, we may disclose your PHI under certain conditions in response to a subpoena, discovery request or other lawful process, in which case, reasonable efforts must be undertaken by the party seeking the PHI to notify you and give you an opportunity to object to this disclosure. Law Enforcement: We may also disclose your PHI, if requested by a law enforcement official as part of certain law enforcement activities. Coroners, Funeral Directors, And Organ Donation: We may disclose your PHI to a coroner or medical examiner for identification purposes, determining cause of death or other duties authorized by law. We may also disclose your PHI to a funeral director, as authorized by law, in order to permit the funeral director to carry out his/her duties. We may disclose such information in reasonable anticipation of death. PHI may be used and disclosed for cadaveric organ, eye or tissue donation and transplantation purposes. Research: We are permitted to disclose your PHI to researchers when their research has been approved by an institutional review board that has established protocols to ensure the privacy of your PHI. However, the Plan does not routinely disclose PHI to researchers. Criminal Activity: Consistent with applicable federal and state laws, we may disclose your PHI, if we believe that the use or disclosure is necessary to prevent or lessen a serious and imminent threat to the health or safety of a person or the public. We may also disclose PHI if it is necessary for law enforcement authorities to identify or apprehend an individual. Military Activity And National Security: When the appropriate conditions apply, we may use or disclose PHI of individuals who are Armed Forces personnel (1) for activities deemed necessary by military command authorities; or (2) to a foreign military authority if you are a member of that foreign military service. We may also disclose your PHI to authorized federal officials conducting national security and intelligence activities including the protection of the President. 64 Workers’ Compensation/Jones Act: We may disclose your PHI to comply with workers’ compensation laws, the Jones Act and other similar legally established programs. Inmates: If you are an inmate of a correctional institution or under the custody of a law enforcement official, we may disclose your PHI to the institution or law enforcement official if the PHI is necessary for the institution to provide you with health care; to protect the health and safety of you or others; or for the security of the correctional institution. Required Uses And Disclosures: We must make disclosures to you and to the Secretary of the U.S. Department of Health and Human Services to investigate or determine our compliance with the federal regulations regarding privacy. Authorization For Other Uses And Disclosures Of Your PHI: Most uses and disclosures of psychotherapy notes relating to you, uses and disclosures of your PHI for marketing purposes, and disclosures that constitute sales of your PHI require your authorization. Other uses and disclosures of your PHI not described in this Notice will be made only with your written authorization, unless otherwise permitted by law as described above. If you authorize us to use or disclose your PHI for purposes other than set forth in the Notice, you may revoke that authorization, in writing, at any time, except to the extent that we have already taken action based upon the authorization. Thereafter, we will no longer use or disclose your PHI for the reasons covered by your written authorization. The Fund will not use or disclose your PHI that is “genetic information” for “underwriting” purposes, as defined by the Genetic Information Nondiscrimination Act of 2008. You have the right to opt-out of receiving fundraising communications from us. 65 YOUR RIGHTS Right To Inspect And Copy: As long as we maintain it, you may inspect and obtain a copy of your PHI that is contained in a Designated Record Set. “Designated Record Set” means a group of records that comprise the enrollment, payment, claims adjudication, case or medical management record systems maintained by or for the Plan. If the Plan uses or maintains an electronic health record with respect to your PHI, you may request such PHI in an electronic format, and direct (in a signed written request) that such PHI be sent to another person or entity. Under federal law, however, you may not inspect or copy psychotherapy notes or information compiled in reasonable anticipation of, or use in, a civil, criminal, or administrative action or proceeding. We may decide to deny access to your PHI. Depending on the circumstances, our decision to deny access may be reviewable by a licensed health professional who was not involved in the initial denial of access and who has been designated by the Plan to act as a reviewing official. To request access to inspect and/or obtain a copy of any of your PHI, you must submit your request in writing on a form the Plan shall provide to our Privacy Officer at the address below indicating the specific information requested. We shall impose a fee to cover the costs of copying, postage, supplies for creating the paper or electronic media and to prepare a summary of explanation. If you want to inspect your PHI, we will make an appointment for you to come to the Plan Office at a reasonable time during normal business hours. Right To Request A Restriction Of Your PHI: You may ask us not to use or disclose any part of your PHI for the foregoing purposes. You may also request that we not disclose particular portions of your PHI to personal representatives or to family members who may be involved in your care, or for notification purposes as described above. We are not required to agree to a restriction that you may request. However, if we do agree to the request, we will not use or disclose your PHI in violation of that restriction unless it is needed to provide emergency treatment, or we terminate the restriction with or without your agreement. If you do not agree to the termination, the restriction will continue to apply to PHI created or received prior to our notice to you of our termination of the restriction. To request a restriction you must write 66 to our Privacy Officer at the address below indicating what information you want to restrict, whether you want to restrict use, disclosure or both, and to whom you want the restriction to apply. Right To Request To Receive Confidential Communications From Us By Alternative Means Or At An Alternative Location: You may request in writing and we must accommodate your reasonable requests to receive communications of PHI from us by alternative means or at alternative locations. For example, you can ask that we only contact you at work or by mail or at another address. Your request must affirm that you believe that the disclosure of the information could endanger you. Your written request for such confidential communication must be addressed to our Privacy Officer at the address below. Right To Amend Your PHI: You have the right to request an amendment of your PHI if you believe the information maintained by the Fund about you is incorrect or incomplete. Your request must be made in writing and submitted to our Privacy Officer. In addition, you must provide a reason that supports your request. You have this right as long as the Fund maintains your PHI in a designated record set. We will make an amendment to PHI we created or if you demonstrate that the person or entity that created the PHI is no longer available to make the amendment. However, we cannot amend PHI that we determine is accurate and complete. We may deny your request for an amendment if it is not in writing or does not include a reason to support the request. In addition, we may deny your request if you ask us to amend information that: Did not originate with us, unless the person or entity that originate the PHI is no longer available to make the amendment; > Is not contained in the records maintained by the Plan; > Is not part of the information which you would be legally permitted to inspect and copy; and Is accurate and complete. If we deny your request for amendment, you have the right to file a written statement of disagreement with us or you can request us to include your request for amendment along with the information sought to be amended if and when we disclose it in the future. We may prepare a rebuttal to your statement and will provide you with a copy of any such rebuttal. 67 Right To An Accounting Of Disclosures: You have the right to request an accounting or list of disclosures of your PHI made by the Plan or its Business Associates. We are required to comply with your request except with respect to disclosures: Made in connection with your receiving treatment, our payment for such treatment and for health care operations; Made to you regarding your own PHI; Pursuant to your written authorization; To a person involved in your health care or payment of your health care or for other permitted notification purposes; For national security or intelligence purposes; To correctional institutions or law enforcement officials; and That are merely incidental to another permissible use or disclosure. To request an accounting of disclosures, you must submit your request in writing to our Privacy Officer. You have the right to receive an accounting of disclosures of PHI made within six years (or less) of the date on which the accounting is requested, but not prior to April 14, 2003. Your request should indicate the form in which you want the list (e.g., paper or electronic). The first request within a 12month period will be free of charge. For additional requests within the 12-month period, we will charge you for the costs of providing the accounting. We will notify you of the cost involved and you may choose to withdraw or modify your request at that time before any cost is incurred. Right to Receive Notice of Certain Breaches of PHI: If your “unsecured” PHI is accessed, acquired, used or disclosed in a manner that is considered a breach and not permitted under the HIPAA privacy rules we will notify you. Unsecured PHI is PHI that is not rendered unusable, unreadable, or indecipherable to unauthorized persons through certain specified technologies and methodologies. Right To Obtain A Paper Copy Of This Notice: You may request a paper copy of our Notice at any time. Additionally, you may visit our website at www.iuoelocal25.org to view or download the current Notice. 68 Complaints If you believe that your privacy rights have been violated, you may file a complaint with us or to the Secretary of the U.S. Department of Health and Human Services at Hubert H. Humphrey Building, 200 Independence Avenue S.W., Washington, D.C. 20201. To file a complaint with us, you must submit your complaint in writing to our Privacy Officer at the address below. We will not retaliate against you for filing a complaint. For Questions Or Requests If you have any questions regarding this Notice or would like to submit a written request as described above, please contact: Larry Schleyer, Privacy Officer, International Union of Operating Engineers, Marine Division, Local 25 Medical Plan 461 State Hwy. 33 Millstone Township, New Jersey 08535 69 STATEMENT OF ERISA RIGHTS As a participant in this Plan you are entitled to certain rights and protections under the Employee Retirement Income Security Act of 1974 (ERISA). ERISA provides that all plan participants shall be entitled to: Examine, without charge, at the plan administrator’s office and at other specified locations, such as worksites and union halls, all documents governing the plan, including insurance contracts and collective bargaining agreements, and a copy of the latest annual report (Form 5500 Series) filed by the plan with the U.S. Department of Labor and available at the Public Disclosure Room of the Employee Benefits Security Administration. Obtain, upon written request to the plan administrator, copies of documents governing the operation of the plan, including insurance contracts and collective bargaining agreements, and copies of the latest annual report (Form 5500 Series) and updated summary plan description. The administrator may make a reasonable charge for the copies. Receive a summary of the plan’s annual financial report. The plan administrator is required by law to furnish each participant with a copy of this summary annual report. Continue health care coverage for yourself, spouse or dependents if there is a loss of coverage under the plan as a result of a qualifying event. You or your dependents may have to pay for such coverage. Review this summary plan description and the documents governing the plan on the rules governing your COBRA continuation coverage risks. Reduction or elimination of exclusionary periods of coverage for preexisting conditions under your group health plan, if you have creditable coverage from another plan. You should be provided a certificate of creditable coverage, free of charge, from your group health plan or health insurance issuer when you lose coverage under the plan, when you become entitled to elect COBRA continuation coverage, when your COBRA continuation coverage ceases, if you request it before losing coverage, or if you request it up to 24 months after losing coverage. Without evidence of creditable coverage, you may be subject to a pre-existing condition exclusion for 12 months (18 months for late enrollees) after your enrollment date in your coverage. 70 In addition to creating rights for plan participants ERISA imposes duties upon the people who are responsible for the operation of the employee benefit plan. The people who operate your plan, called “fiduciaries” of the plan, have a duty to do so prudently and in the interest of you and other plan participants and beneficiaries. No one, including your employer, your union, or any other person, may fire you or otherwise discriminate against you in any way to prevent you from obtaining a welfare benefit or exercising your rights under ERISA. If your claim for a welfare benefit is denied in whole or in part you must receive a written explanation of the reason for the denial. You have the right to have plan review and reconsider your claim. Under ERISA, there are steps you can take to enforce the above rights. For instance, if you request materials from the plan and do not receive them within 30 days, you may file suit in a Federal court. In such a case, the court may require the plan administrator to provide the materials and pay you up to $110 a day until you receive the materials, unless the materials were not sent because of reasons beyond the control of the administrator. If you have a claim for benefits which is denied, or ignored, in whole or in part, you may file suit in a state or Federal court. In addition, if you disagree with the plan’s decision or lack thereof concerning the qualified status of a medical child support order, you may file suit in Federal court. If it should happen that plan fiduciaries misuse the plan’s money, or if you are discriminated against for asserting your rights, you may seek assistance from the U.S. Department of Labor, or you may file suit in a Federal court. The court will decide who should pay court costs and legal fees. If you are successful the court may order the person you have sued to pay these costs and fees. If you lose, the court may order you to pay these costs and fees, for example, if it finds your claim is frivolous. If you have any questions about your plan, you should contact the plan administrator. If you have any questions about this statement or about your rights under ERISA, or you need assistance in obtaining documents from the plan administrator, you should contact the nearest office of the Employee Benefits Security Administration, U.S. Department of Labor, listed in your telephone directory or the Division of Technical Assistance and Inquiries, Employee Benefits Security Administration, U.S. Department of Labor, 200 Constitution Avenue N.W., Washington, D.C. 20210. You may also obtain certain publications about your rights and responsibilities under ERISA by calling the publications hotline of the Employee Benefits Security Administration. 71