Factors associated with Subjective Well

Factors Associated With Subjective Well-Being in People Treated With Long-Acting
Injectable Antipsychotic Medication
Scott McGreal, B.A. – Psychology (Hons.)
School of Psychology
University of Sydney
Submitted in fulfilment of the requirements for the degree of Master of Science
March, 2011
1
Certificate of Originality
I hereby declare that this submission is my own work and that, to the best of my knowledge and belief, it contains no material previously published or written by another person nor material which to a substantial extent has been accepted for the award of any other degree or diploma of the University or other institute of higher learning, except where due acknowledgement is made in the text.
I also declare that the intellectual content of this thesis is the product of my own work, even though I may have received assistance from others on style, presentation and language expression.
Signature _____________________________
2
Acknowledgements
To my principal supervisor, Professor Tim Lambert, I would like to acknowledge his encouragement and support during all phases of the project.
Thanks also to Dr Niko Tiliopolous, my associate supervisor for his feedback and statistical advice.
Thanks to Dr Sharon Naismith for advice on neuropsychological assessment.
I would also like to thank Ally Ryder for assistance during the early phases of the research.
I would also like to acknowledge invaluable help from the staff at Concord Hospital and at
Marrickville Community Health Centre where recruitment of participants took place.
Finally, I would like to thank all my participants who generously provided their time to make my research possible.
3
Abstract
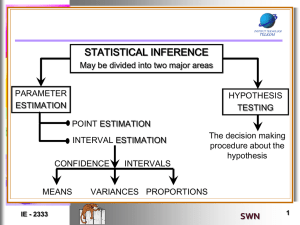
The concept of subjective well-being (SW) in people with schizophrenia has come to the attention of clinical researchers in recent years. SW has been defined as satisfaction with the subjective aspects of one’s quality of life. Naber and colleagues (1995) argue that its importance lies in its representation of the patient’s perspective on psychiatric treatment.
These authors viewed SW as mainly a state phenomenon strongly influenced by antipsychotic drug treatment and devised a research measure to quantify SW while receiving antipsychotic drugs. This was called the SWN (Subjective Well-being under Neuroleptics). Research by
Naber and colleagues (e.g. Naber, 1995) suggested that treatment with oral secondgeneration antipsychotics (SGA) improves the patient’s subjective well-being (SWN) compared to treatment with first generation antipsychotics (FGA) due to the better subjective tolerability of the former medications. However, recent research has called into question some of the apparent advantages of SGA with respect to subjective wellbeing in general and
SWN in particular. Furthermore, there is evidence that SWN tends to be relatively stable over time and might therefore have a trait-like quality. The present study aimed to compare SWN in patients with persistent psychotic disorders treated with either long-acting injectable (LAI)
FGA or SGA medications. The study examined a number of variables that could influence reports of SWN, including personality traits, comorbid depression, anxiety and, stress, neurocognitive function and self-assessed global health. The stability of the SWN score over time was also investigated. Finally, the factor structure of the SWN was examined.
77 patients, 56 with schizophrenia, 19 with schizoaffective disorder, and two with bipolar disorder, taking LAI medication were assessed on a battery of questionnaires. These included
SWN, personality traits, negative affect, side-effects, attitudes to adherence, insight, cognitive functioning, and psychopathology symptoms. 30 of these patients received an LAI SGA
4
medication (predominantly risperidone), the rest received a variety of LAI FGA medications.
61 patients were additionally taking oral antipsychotic medications.
Differences in SWN associated with type of LAI medication were small and inconsistent.
There were strong effects from personality traits, so that patients who were higher on extraversion, agreeableness, conscientiousness, and openness to experience and lower on neuroticism, reported higher levels of SWN. Depression, anxiety, stress, cognitive/disorganised symptoms, and side-effect severity were associated with lower SWN.
Exploratory factor analysis revealed two SWN factors, one named negative SWN, strongly associated with neuroticism and depression, and to a lesser extent medication side-effects; the other named positive SWN, strongly associated with health, agreeableness, and extraversion.
Regression analysis suggested that extraversion, agreeableness, depression, disorganised symptoms, and self-assessed health were independent predictors of total SWN. Performance on neurocognitive tests had modest positive associations with SWN, but these mostly became non-significant when controlling for openness to experience. Attitudes to adherence were strongly associated with insight but had little association with SWN.
With respect to stability, 21 patients completed a follow up assessment after three or more months. Changes in SWN were strongly related to changes in depression, anxiety, and to some extent side-effect severity. Most patients showed high levels of stability in their SWN scores and in depression between baseline and follow up. Improvements in some aspects of cognitive functioning, such as memory, were also evident, but these were weakly and inconsistently related to changes in SWN.
With respect to SWN, SGA medications lacked advantages over FGA in patients in long-term maintenance therapy. There were non-significant trends suggesting that long acting injectable monotherapy may be associated with better SWN than antipsychotic polypharmacy.
5
Patients’ SWN and hence perceived quality of life seemed to be most strongly related to depression, self-assessed global health and stable features of personality. Current psychopathology (cognitive/disorganised symptoms) was related to SWN to a lesser extent.
Subjective well-being may have both a stable trait-like character due to its relationship with personality features as well as a relationship to state related factors in this population.
6
Table of Contents
Factors associated with Subjective Well-Being in Long Acting Injectable Antipsychotic Medication
7
Comparisons of oral risperidone, olanzapine and other drugs combined with LAI groupings ........ 99
Changes in SWN inversely associated with changes in depression, anxiety and side-effects .... 184
List of Figures
Figure 2. Interaction between Affective Symptoms and Long acting injectable group for Negative
SWN ................................................................................................................................................... 110
Figure 3. Interaction between Affective Symptoms and Long acting injectable group for Emotional
List of Tables
Table 8. Demographic characteristics of participants broken down by LAI medication grouping........................70
Table 9. LAI medications taken by number of patients.........................................................................................71
Table 18 Relationships of personality with distress, side-effects, and lifestyle questions...................................84
Table 20 Marital status by gender .......................................................................................................................86
Table 21 SWN means as a function of marital status……………………………………………………………………………………….86
12
Table 22 Diagnostic groups by oral antipsychotic treatment ............................................................................... 87
Table 23 Diagnostic groups by mood stabiliser use .............................................................................................. 87
Table 24 Benztropine use by each diagnostic group ............................................................................................ 88
Table 25 Mean CPZE dosages for diagnostic groups ............................................................................................ 88
Table 26 SWN scale scores for diagnostic groups ................................................................................................ 89
Table 27 PANSS Factor scores for each LAI group ……………………………………………………………………………………………92
Table 28 Means scores on SWN scales, LUNSERS, DASS and RBANS in each LAI group…………………………………… 93
Table 29. SWN scale scores of Combined LAI and Oral medication groups ......................................................... 97
Table 31. SWN scale scores for combined oral and long acting injectable medication groupings. .................... 102
Table 32. SWN scales as a function of combined long acting injectable and specific oral medications ............ 103
Table 33. Pairwise comparison of estimated marginal means of medication groupings ................................... 104
Table 34. SWN scores as a function of Affective symptoms and antipsychotic medications ............................ 107
Table 35. Estimated Marginal means of negative SWN and emotional regulation ............................................ 109
Table 36. Estimated Marginal means of negative SWN for oral medication groups .......................................... 109
Table 37. Mean differences in SWN for patients on antidepressants vs. others ............................................... 111
Table 39. SWN scales as a function of mood stabiliser use, and long acting injectable and oral medication .... 114
Table 40. Estimated Marginal Means for Mood stabiliser use controlling for long acting injectable and oral medication and dosage ...................................................................................................................................... 116
Table 42. Estimated Marginal Means for oral antipsychotic medication use .................................................... 119
Table 46. Test of mediation of influence of neuroticism on SWN by depression .............................................. 126
Table 49. Predictors of Negative and Positive SWN Factors............................................................................... 130
Table 50. Multivariate predictors of SWN subscales .......................................................................................... 132
Table 52. Predictors of self-control .................................................................................................................... 133
Table 53. Predictors of emotional regulation .................................................................................................... 134
Table 54. Predictors of social integration ........................................................................................................... 134
Table 55. Predictors of physical functioning ....................................................................................................... 135
Table 56. Predictors of total SWN, factor and subscale scores .......................................................................... 136
13
Table 58 Big five predictors of health ................................................................................................................. 140
Table 59 LAI medications taken by number of patients at follow up ................................................................. 142
Table 60. Correlations between baseline and follow up SWN scale scores…………………………………………………….144
Table 61 Changes in SWN scale scores between baseline and follow up ........................................................... 144
Table 62. Differences between LAI groups in changes in SWN scale scores ...................................................... 145
Table 64 Change in DASS and side-effects scale scores between baseline and follow up ................................. 147
Table 66 Correlations between changes in SWN scales and side-effects scales ................................................ 148
Table 67 Changes in PANSS scores in each LAI group ........................................................................................ 149
Table 69 RBANS scores for each LAI group at follow up ..................................................................................... 151
Table 71 Correlations between changes in SWN scales and RBANS indexes ..................................................... 153
Table 72 SWN cluster status at baseline and at follow up ................................................................................. 154
14
Factors associated with Subjective Well-Being in Long Acting Injectable
Antipsychotic Medication Patients
Overview
Research interest in subjective well-being in schizophrenia and other persistent psychotic disorders has grown since the 1990’s (Naber & Karow, 2001). Subjective wellbeing has been defined as the patient’s satisfaction with the subjective aspects of their quality of life (QOL) (Naber 1995). Subjective well-being and QOL more broadly are increasingly considered treatment outcomes in their own right. Naber and colleagues argue that novel drugs known collectively as ‘second generation antipsychotics’ (SGA) are more effective than older-style conventional drugs known as ‘first generation antipsychotics’ (FGA) in improving patients’ subjective well-being, although some more recent studies have found no advantage for SGA over FGA (Balestrieri et al., 2009; de Haan et al., 2003). Subjective wellbeing related studies reviewed in this thesis are shown in Table 1. These studies were selected on the basis that they compare two or more antipsychotic medication treatments rather than examining SWN in relation to only a single treatment. Research has largely focused on the effects of oral antipsychotic agents on subjective well-being, although treatment with longacting injectable (LAI) antipsychotic drugs is relatively common in long-term treatment.
Apart from one poster abstract (Balanza et al., 2008) no published studies appear to have examined the relationship between use of LAI (also known as ‘depot’) antipsychotic medications and subjective well-being. The aim of this thesis was to identify factors associated with subjective well-being in patients treated with either FGA or SGA long-acting injectable (LAI) antipsychotic drugs, including participant characteristics. Previous studies have examined differential drug effects on subjective well-being and the clinical correlates of this construct, including symptomatology, especially depression, and the detrimental effects of side-effects (Kim, Ann, & Kim, 2010; Kim & Kim, 2009; Naber & Karow, 2001).
15
However, no studies to date appear to have examined whether subjective well-being correlates with personality traits or self-assessed global health. Research on ‘objective’ quality of life has found that patient characteristics, particularly personality traits, appear to substantially correlate with QOL (Kentros et al., 1997a; Kentros, Terkelsen, Hull, Smith, &
Goodman, 1997b; Masthoff, Trompenaars, Van Heck, Hodiamont, & De Vries, 2007), as well as a range of other important outcomes in people with schizophrenia (Dinzeo &
Docherty, 2007). Studies in the normal population have found that subjective well-being related constructs, such as happiness and life satisfaction, are strongly predicted by both personality traits (Steel, Schmidt, & Shultz, 2008) and self-assessed global health (Okun &
George, 1984). The study additionally aimed to explore the factor structure of the SWN scale used by Naber to assess subjective well-being in order to further understand how subjective well-being relates to other variables such as personality and health.
A considerable amount of research has focused on the influence of antipsychotic drugs on performance on tests of cognitive ability (Keefe et al., 2007; Keefe, Silva, Perkins,
& Lieberman, 1999; Keefe et al., 2006). Some studies found that SGA were somewhat more effective than FGA in improving some aspects of cognitive ability compared to FGA but other studies have found no differences. No studies appear to have examined this in relation to long acting injectable medications, or to have established whether subjective well-being and neurocognitive status are related. This thesis examined whether either LAI SGA or FGA drugs were associated with differences in cognitive ability test performance. Furthermore, the thesis examined whether cognitive ability test performance correlated with subjective wellbeing. Finally, the thesis aimed to assess the stability of subjective well-being over time in patients treated with LAI drugs.
16
Table1. Studies comparing effects of various antipsychotic agents on SWN
Study author/
Design
Naber (1995,
1996)
Prospective and cross-sectional naturalistic design
Drugs
Clozapine vs. haloperidol and flupenthixol
Sample size
53
66/80 1
(28/40 on clozapine, 38/40 on FGA)
Follow up period
3 – 4 months after discharge
None
Results
SWN highly stable in patients
(n = 37) whose medication was unchanged. Changes in medication regime associated with ‘marked changes’ in all
SWN scales (n = 16)
Clozapine patients had higher
SWN scores (total scale and all subscales) compared to
FGA treated patients ( d =
.41).
48
Naber, et al.
(2001)
Prospective naturalistic design de Haan et al.
(2003)
Random assignment
Olanzapine, clozapine, risperidone
Low-dose haloperidol vs. low-dose olanzapine
38
100
24
4 – 6 months after discharge
Patients rated as noncompliant (n=14) had lower
SWN (total score and 3 subscales) than those rated as compliant (n=34) ( d = .95)
None
Unspecified treatment period
6 weeks treatment
SWN scores significantly positively correlated with rating of health-related quality of life, mood, depression (reverse scored) and subjective well-being.
SWN significantly negatively correlated with negative and general symptoms. No significant correlation with positive symptoms. SWN not significantly correlated with
EPS
Improvement in SWN (total score and three subscales) over treatment was greatest in olanzapine cohort
SWN significantly improved over treatment period within haloperidol group, but not within olanzapine group.
Between-group difference in
SWN improvement was nonsignificant but favoured haloperidol group ( d = -.58).
1 Naber (1995) provides two conflicting sample sizes for this comparison. Effect size estimates were calculated based on t-test values provided in Naber (1996).
17
Table 1 continued
Naber, et al. (2005)
Randomised double-blind
Olanzapine and clozapine
114
Lambert et al.
(2006)
Prospective naturalistic design
Wehmeier, et al.
(2007)
Prospective naturalistic design
SGA (more than half received olanzapine) vs. FGA (13.6% of sample) (various agents in both categories)
Olanzapine (n =
1007), another SGA
(n = 335), FGA (n =
32), or unspecified polypharmacy (n =
88)
2960
1462
(Balanza, et al.,
2008)
Cross-sectional naturalistic design
LAI risperidone vs.
LAI FGA
(unspecified)
49
Balestrieri (2009)
Cross-sectional naturalistic design
Lambert et al.
(2009)
Prospective naturalistic design
Four SGA
(clozapine, risperidone, olanzapine, & quetiapine) and haloperidol
SGA vs. FGA (both unspecified)
145
2842
Lambert et al.
(2010)
Prospective naturalistic design
SGA vs. FGA (both unspecified)
2224
26 weeks treatment
3, 6, 9, 12,
18, & 24 months
SWN improved equally in both treatment groups.
Changes in SWN and PANSS scores had an inverse correlation ( r = -.45)
Variability in change scores was higher than the mean, suggesting negative change was not uncommon
Adequate SWN at endpoint was more likely to occur with initial treatment with an SGA compared to an FGA
12 months treatment
None
All groups experienced (some) improvements in SWN. SWN response (improvement by
20% and at least 10 points from baseline), was significantly greater in olanzapine monotherapy compared to other SGA or
FGA monotherapy but did not significantly differ from polypharmacy.
No significant differences in
SWN between treatment groups. Rates of adherence were similar in both groups even though risperidone was administered twice as frequently.
No significant differences in
SWN between treatment groups.
3 years of treatment
3 years of treatment
Long-term patterns of SWN tended to be highly stable.
Membership of stable low cluster predicted by initial
FGA treatment. Membership of early improvement cluster predicted by initial SGA treatment.
SGA treatment group had significantly higher SWN than
FGA group at 6 months ( d
=.20) and at 3 years ( d =.36)
18
Quality of Life as a Treatment outcome in Schizophrenia
According to Naber and Karow (2001), research on schizophrenia outcomes prior to the 1990s largely ignored quality of life due to the ineffectiveness of conventional treatments at the time in improving patient quality of life. In fact, Naber and Karow (2001) argued that conventional FGA treatment tended to be detrimental to subjective quality of life or subjective well-being. However, interest in this field has recently grown due to development of SGA that appear to have a more tolerable side-effect profile and hence are believed by some researchers to have a beneficial influence on the patient’s QOL (Siamouli et al., 2009).
Subjective well-being appears to be an important treatment outcome because some studies found that higher subjective well-being was associated with better adherence with medication and treatment (Naber & Karow, 2001). Additionally, improvements in subjective well-being in response to antipsychotic therapy early in treatment have been found to be predictive of longer term symptomatic recovery in two studies (de Haan, Nimwegen, Amelsvoort,
Dingemans, & Linszen, 2008; Lambert, Schimmelmann, et al., 2009).
Objective and subjective quality of life
Quality of life is a multidimensional construct that includes both ‘objective’ indicators including health and living conditions, demographic factors and psychosocial functioning, and ‘subjective’ indicators including satisfaction with life generally and in specific life domains the patient considers important to their sense of well-being (Yamauchi et al., 2008).
The distinction between ‘objective’ QOL, usually rated by experts, and ‘subjective’ QOL, usually rated by self-report, is important because the relationship between the two perspectives tends to be moderate at best (Karow & Naber, 2002). Additionally, some adverse effects of antipsychotic drugs on drive, emotion and cognition (also known as the
Neuroleptic Induced Deficit Syndrome, NIDS) may not be readily detected by objective
19
examination by a physician yet are readily reported by patients (Lewander, 1994; Naber &
Karow, 2001).
Development of the construct of Subjective Well-Being under Neuroleptics (SWN)
Although antipsychotic drugs used in the treatment of schizophrenia are usually effective in relieving positive symptoms, such as hallucinations and delusions, severe sideeffects can impair subjective QOL. People with schizophrenia on antipsychotic drugs have often reported reductions in emotionality, straight thinking, will power, and spontaneity.
These side-effects have been referred to as ‘pharmacogenic depression’ ‘neuroleptic-induced anhedonia’ and NIDS (Lewander, 1994; Naber & Karow, 2001). Long-term studies found that drug-free patients felt less depressed compared to medicated patients (Harrow, Yonan,
Sands, & Marengo, 1994). Depression was also higher in those on higher doses (Naber,
1995). Symptoms of pharmacogenic depression are not always evident upon examination by treating clinicians (Naber & Karow, 2001), therefore Naber (1995) argued that it is important to consider the patient’s perspective on treatment.
A number of instruments have been developed to assess subjective aspects of patients’ experiences during antipsychotic treatment (Wolters, Knegtering, van den Bosch, &
Wiersma, 2009). These include the Drug Attitudes Inventory (DAI) (Hogan, Awad, &
Eastwood, 1983), the Liverpool University Neuroleptic Side-Effects Scale (LUNSERS) (Day,
Wood, Dewey, & Bentall, 1995), the Subjects’ Response to Antipsychotics questionnaire
(SRA) (Wolters, Knegtering, Wiersma, & van den Bosch, 2006), the Subjective well-being under Neuroleptics form (Naber, 1995), and the Personal evaluation of transitions in treatment (PETiT) (Voruganti & Awad, 2002). These instruments differ from each other to various degrees in their scope and purpose (Wolters, et al., 2009). The DAI assesses attitudes and beliefs towards treatment and health that may influence compliance. The LUNSERS assesses side-effects of antipsychotic medications. The SWN was developed to assess
20
changes in mental, emotional, social and physical functioning, independently of patient attributions about the effects of treatment (Naber, 2006). The SRA assesses responses to changes in mental, emotional, and physical domains attributed to antipsychotics and includes
‘desired’ and ‘undesired’ subscales. The PETiT assesses subjective tolerability, and subjective aspects of quality of life, and a number of items on the PETiT appear to be conceptually similar to SWN items (e.g. ‘my mind is sharp and clear’) although items are included that assess more general aspects of subjective well-being (e.g. ‘I am unhappy’).
Additionally, there the PETiT has several items assessing attitudes to treatment and adherence.
A review by Wolters (2009) of the DAI, LUNSERS, SRA, and the SWN, found that all four of these instruments were significantly correlated (negatively for the LUNSERS and the SRA undesired subscale, positively for all the others) with a generic measure of quality of life. The SWN had the strongest correlation with quality of life of all the measures (r = .78).
The LUNSERS (r = -.58) and the SRA undesired (-.46) had substantial negative correlations, whereas the DAI (r = .30) and the SRA desired (r = .25) had modest positive correlations with quality of life. Internal consistency was moderate to good for all measure except the
DAI which was poor. The psychometric properties of the PETiT were examined by
Voruganti and Awad (2002). The PETiT had good internal consistency, but had only a modest positive correlation (r = .21) with the Quality of Life Scale (QLS), a physician rated scale developed specifically for people with schizophrenia. This is in contrast with the SWN, which had a strong positive correlation with the QLS and a number of physician-rated measures of quality of life in a number of studies (Vothknecht, Schoevers, & de Haan, 2011).
Of the instruments discussed, the SWN appears to have been the most frequently used in research on the subjective aspects of quality of life in people with schizophrenia, having
21
been examined in over 50 published papers (Vothknecht, et al., 2011). For this reason, and because the SWN appears to have the strongest correlation with quality of life measures compared to the other instruments discussed, the present study focuses primarily on the
SWN. Additionally, the study incorporates measures of attitudes to adherence and of selfreported medication side-effects, as the SWN does not directly assess these constructs.
Naber (1995) originally developed the SWN as a 54-item measure. In a pilot study, patients rated the importance of each item to their well-being. The original scale was then reduced to 38 items. Naber identified five subscales through confirmatory factor analysis.
These subscales were called mental functioning, emotional regulation, social integration, selfcontrol, and physical functioning. Confirmatory factor analysis is used to test specific hypotheses about factor structure based on an underlying theory (Tabachnick & Fidell, 2001).
However, the SWN scale items were empirically derived and it seems unclear whether a theory was used to develop the subscales or if items were assigned to the subscales based on conceptual similarities. Naber (1995) did not report the correlations of the subscales. The short form of the SWN scale was later developed so that each subscale would have only four items. See Appendix A for a list of the items pertaining to each subscale. Item analysis was used to ensure that each item correlated most strongly with its subscale rather than other subscales (Naber, et al., 2001). Naber et al. (2001) reported what they described as ‘only modest intercorrelations’ among the subscales (correlations ranged from .41 to .64).
However, Cohen (1992) considered correlations of .30 to be ‘medium’ sized and those .50 or greater to be ‘large’, so the intercorrelations reported by Naber et al. can be described as substantially more than ‘modest’. Schmidt et al. (2006) used confirmatory factor analysis to construct a shortened version (ten items) of the SWN scale. Their model contained five factors representing the five subscales. All of the factors were highly correlated (all rvalues
> .75) suggesting the subscales in their abbreviated scale were closely related. Exploratory
22
factor analysis is used to explore what the underlying factors of a scale are rather than testing a pre-existing theory (Tabachnick & Fidell, 2001). There do not appear to have been any studies using exploratory factor analysis to investigate the SWN scale. Therefore, how well the subscales reflect the actual number of factors underlying the scale remains an open question.
Initial Claims that SGA improve subjective QOL/SWN compared to FGA
Naber and Karow (2001) claimed that SGA are superior to FGA in improving the patient’s subjective QOL because they are less likely to produce pharmacogenic depression due to their more benign side-effect profile. Therefore, patients prescribed SGA are presumed to be more likely to adhere to treatment. Evidence that this might be the case appears in an early naturalistic non-randomised study assessing subjective QOL through standardised interviews inquiring about patients’ satisfaction with important areas of their lives. The study found that patients treated with clozapine and risperidone reported a significantly higher general subjective quality of life compared to patients treated with the FGA haloperidol or fluphenazine (Franz, Lis, Pluddemann, & Gallhofer, 1997). The study by Naber and Karow
(2001) however did not provide a direct comparison of SGA versus FGA treatment. They cited results from a study of treatment with quetiapine (an SGA) with no comparison group finding that the vast majority of patients preferred quetiapine treatment to previous antipsychotics due to better tolerability and efficacy. Furthermore, claims have been made that SGA are more effective than FGA in treating a range of schizophrenia symptoms and in enhancing cognitive ability. Claims for the superiority of SGA compared to FGA in regards to QOL and SWN are based on the pharmacological differences between the two classes of agents which lead to the designation of SGA as ‘atypical’ or ‘novel’ compared to the ‘typical’ or ‘conventional’ FGA.
23
The spectrum of ‘typical’ vs. ‘atypical’ antipsychotics
Drugs known as FGA include chlorpromazine and haloperidol and as a class tend to be strong dopamine antagonists, particularly of D
2 receptors (Casey, 2004). As a result, use of
FGA is associated with an increased risk of movement disorders, such as extrapyramidal symptoms (EPS; e.g. inability to sit still, difficulty initiating movement) and tardive dyskinesia (repetitive involuntary movements that may become permanent). Long-term studies suggest that FGA treatment is associated with an incidence of tardive dyskinesia of approximately 5% per year in adults (Correll, Leucht, & Kane, 2004). The key feature leading to the designation of SGA as ‘atypical’ is that they produce relatively few EPS compared to conventional or ‘typical’ antipsychotics due to their different effects on the dopamine system (Meltzer, 2004). This has led to claims that patients find SGA subjectively more tolerable than FGA (Naber & Karow, 2001), although some researchers have recently questioned whether this is actually the case (Geddes, Freemantle, Harrison, & Bebbington,
2000; Miller et al., 2008). Furthermore, some SGA, such as olanzapine and risperidone, are associated with adverse metabolic effects and weight gain that have long-term health implications (Tandon & Jibson, 2003). Although, FGA are effective in reducing positive symptoms, they are less effective in reducing negative symptoms, and seem to be largely ineffective in treating mood disturbances or cognitive impairments. Some SGA on the other hand have been found to be somewhat more effective in reducing negative symptoms, improving mood stability and perhaps cognitive functioning, although this latter claim is more controversial (Keefe, et al., 1999; Marder, 2003). Although antipsychotic drugs are classified for convenience as being either ‘typical’ (i.e. FGA) or ‘atypical’ (i.e. SGA), it is worth noting that it is also possible to consider that drugs may fall on a spectrum ranging from strongly ‘typical’ at one end, represented by haloperidol for example, to strongly
‘atypical’ at the other end, exemplified by clozapine (Hertling et al., 2003). From this
24
perspective, olanzapine may be considered somewhat more ‘atypical’ than risperidone due to the latter’s somewhat higher risk of EPS, although risperidone generally has a lower risk of
EPS than most FGA (Tandon & Jibson, 2003). Furthermore, some FGA appear to have relatively milder side-effect profiles, particularly at low doses. For example, sulpiride has been referred to as the most ‘atypical’ of the FGA (Naber & Lambert, 2009). SGA focused on in the present study are risperidone and olanzapine, as these SGA have recently become available in long-acting injectable formulations (Cañas & Möller, 2010).
Effectiveness and tolerability of SGA vs. FGA
Clozapine is usually considered the most effective antipsychotic in terms of relieving symptoms, yet potentially dangerous adverse effects, such as agranulocytosis, limit its use
(Meltzer, 2004). A number of studies have attempted to assess the validity of claims that
SGA besides clozapine actually are superior to FGA with regard to effectiveness, tolerability, effects on cognitive ability, and in improving aspects of quality of life. These studies are summarised in Tables 2 – 3. A meta-analysis by Leucht, Pitschel-Walz, Abraham, and
Kissling (1999) found that olanzapine and risperidone were somewhat more effective than haloperidol in reducing global and negative symptoms. SGA produced fewer EPS and were associated with less use of antiparkinson medication than haloperidol, although risperidone was more likely to produce EPS than olanzapine. However, some researchers have argued that EPS produced by FGA are dose-related (Geddes, et al., 2000; Leucht, Wahlbeck,
Hamann, & Kissling, 2003). They argued that the use of low doses of high-potency FGA such as haloperidol or the use of low-potency FGA such as chlorpromazine reduces the risk of EPS to levels comparable to those seen in SGA. Geddes, Freemantle, Harrison and
Bebbington (2000) reported in their meta-analysis that low-dose haloperidol was equivalent in effectiveness (symptom reduction) and tolerability (EPS) to SGA. Leucht, Wahlbeck,
Hamann, and Kissling (2003) reported in their meta-analysis that only clozapine produced
25
clear evidence of producing fewer EPS when compared to low-potency FGA, although there was a marginal trend for olanzapine to produce fewer EPS than low-potency FGA.
However, another meta-analysis (Davis, Chen, & Glick, 2003) that included the raw data from the 30 studies examined by the Geddes et al. (2000) review in a larger metaanalysis found evidence for the superiority of four different SGA compared to FGA in treating symptoms and no evidence that haloperidol dose (or dose equivalent when other
FGA were studied) affected these results. They argued that the Geddes et al. finding may have been an artefact due to the fact that high doses of FGA were used as a comparator in studies of treatment resistant patients in which clozapine was used. Additionally, low doses of haloperidol were compared in relation to less effective SGA, such as quetiapine.
Specifically, they found that clozapine was the most effective SGA, and that olanzapine, risperidone, and amisulpride were more effective than all FGA in reducing symptoms,
although the advantages for the latter three drugs appear to be rather modest. (See Table 2 for
effect sizes.)
26
Table 2. Comparative effectiveness, tolerability and QOL outcomes of SGA vs. FGA.
Trial
Sanger et al. (1999)
Leucht, Pitschel-Walz,
Abraham, & Kissling
(1999)
Geddes, Freemantle,
Harrison & Bebbington
(2000)
Drugs compared
Olanzapine vs. haloperidol
Olanzapine, risperidone, quetiapine, and sertindole, with FGA
(mainly haloperidol) and placebo
Various SGA vs. FGA
N/Number of studies
83 first episode
(FE) patients
1913 multiple episode patients
Meta-analysis
Meta-analysis of 30 studies
Results
Symptom reduction : olanzapine was more effective than haloperidol in FE. Olanzapine was more effective in FE than in multiple episode patients. Haloperidol effectiveness did not differ between first and multiple episode groups.
EPS: EPS reduced in olanzapine but worsened in haloperidol FE group. EPS were worse in FE compared to multiple episode haloperidol groups.
Symptom reduction : All drugs more effective than placebo (modest effect sizes). Risperidone and olanzapine were more effective than haloperidol (quetiapine and sertindole were not) in reducing global symptoms.
Negative symptoms: All drugs, including haloperidol, were somewhat effective in reducing negative symptoms. Risperidone and olanzapine were somewhat superior to haloperidol, sertindole was equally effective, and quetiapine was less effective in reducing negative symptoms.
EPS: all SGA produced fewer EPS compared to haloperidol and were associated with less use of antiparkinson medication.
Risperidone somewhat inferior to other SGA with regard to EPS, but still superior to haloperidol
Symptom reduction : low dose haloperidol was equivalent in efficacy to SGA; high-dose haloperidol less effective than SGA
EPS: low doses of haloperidol do not produce more EPS than SGA
Leucht, et al.(2003)
Davis, Chen, & Glick
(2003)
Various SGA vs. low potency FGA
Various SGA vs. FGA
Meta-analysis of 31 studies
Meta-analysis
EPS: only clozapine clearly superior to FGA; Olanzapine produced only a marginally significant reduction in EPS compared to chlorpromazine ( p =.08).
The authors concluded that low doses of FGA (<600mg of chlorpromazine or its equivalent) had no higher risk of EPS than
SGA.
Symptom reduction : four SGA were more effective than FGA in reducing global symptoms – clozapine ( d = .49), amisulpride ( d = .29), risperidone ( d = .25), and olanzapine ( d = .21). Six other SGA (zotepine, quetiapine, aripiprazole, sertindole, ziprasidone, and remoxipride) were not significantly superior to FGA, although zotepine was marginally different.
No evidence that haloperidol dose (or dose equivalent when other FGA were studied) affected these results.
Rosenheck et al. (2003)
Correll, Leucht, & Kane
(2004)
Olanzapine vs. haloperidol combined with benztropine
309
Risperidone, olanzapine, quetiapine, ziprasidone, amisulpride vs. haloperidol
One study of LAI risperidone.
Meta-analysis of 11 studies lasting 1 year or longer
Symptom reduction : No difference between treatment groups
EPS: Haloperidol treatment combined with benztropine did not produce greater EPS than olanzapine treatment, although the latter produced less akathisia. Olanzapine treatment was associated with improvements in memory compared to haloperidol, possibly due to adverse effects of benztropine.
QOL: No difference between treatment groups in clinician-rated QOL
Tardive dyskinesia: SGA have a reduced risk of TD compared to haloperidol: incidence appears to about one-fifth WITH
SGA.
Dose effects cannot be excluded.
There are indications that higher doses of risperidone increase the risk of TD, EPS, and the need for anticholinergic medication.
27
Table 2 continued
Ritsner, Perelroyzen,
Ilan, & Gibel (2004)
Ritsner et al. (2004)
Olanzapine, risperidone vs. a wide range of FGA
133
CATIE
Lieberman et al. (2005)
Olanzapine, risperidone, ziprasidone & quetiapine vs. perphenazine
1500
CUtLASS
Jones et al. (2006)
Miller, et al. (2008) Olanzapine, risperidone, quetiapine, ziprasidone, versus perphenazine
(modest doses)
277
1440 chronic patients
RCT
Subjective tolerability: SGA treatment group reported higher subjective tolerability compared to FGA group ( d = .42).
Subjective and objective quality of life: SGA & FGA treated groups reported similar subjective QOL; when adjusting for dosage (FGA patients were on higher doses), an advantage for SGA was found for subjective but not objective QOL. Longer duration of antipsychotic treatment was associated with better QOL in both treatment groups.
74% discontinuation rate with a median time to discontinuation of 4.6 months. Olanzapine had the best time to discontinuation rate (9.2 months). The other SGA did not differ from each other or from perphenazine in time to discontinuation.
Symptom reduction : modest effects; there were no significant differences between FGA and SGA treatment arms. Olanzapine was concluded to be more effective than the other drugs, although it was associated with greater weight gain. The remaining
SGA were not considered to be superior to perphenazine.
QOL: No significant differences between groups in improvements in psychosocial functioning.
No significant differences in QOL outcomes between FGA and SGA treatments and no significant differences in how many patients remained in their allocated treatment arm after one year.
EPS: No difference between perphenazine and SGA or between any pair of SGA
Change in global rating of akathisia was highest in perphenazine group ( p = .07), data not shown. Incidences of adding medications for akathisia not significant ( p = .056), perphenazine and risperidone had higher rates of added medications, no data shown.
Higher rate of treatment discontinuation with perphenazine.
Concludes that apparent superiority of SGA was due to high dosage of haloperidol.
28
Table 3. Studies of effects of antipsychotics on neurocognition
Study author/
Design
Mortimer & Dye (1999)
Mortimer, Tyson, & Dye (1998)
Naturalistic longitudinal design
Drugs
Clozapine vs. FGA
Sample size/number of studies
19
(Keefe, et al., 1999)
Meta-analysis of 15 double-blind and open-label studies
Clozapine, risperidone, zotepine, aripiprazole, ziprasidone vs. FGA
15 studies
Purdon et al. (2000)
Double-blind randomised treatment
Cuesta, Peralta, and Zarzuela
(2001)
Naturalistic longitudinal design
Gurpegui et al. (2007)
Randomised open-label treatment
Olanzapine, risperidone, and haloperidol
Olanzapine, risperidone, various
FGA
Olanzapine and risperidone
Keefe, et al. (2006)
Double-blind randomised treatment
Keefe, et al. (2007)
Randomized, double-blind treatment (Sample drawn from
CATIE trial)
Olanzapine, risperidone, and haloperidol
Olanzapine, risperidone, & quetiapine vs. perphenazine
65
38
235
414
817
Follow up period Results
6 months, then 12 months of treatment
Clozapine treatment improved global cognition, memory, and executive function, as well as negative symptoms and behavioural problems at 6 and 12 months. FGA treatment resulted in no improvements. although the results did not reach significance in the openlabel studies. Learning and memory were not significantly improved by SGA compared to FGA.
6, 30, & 54 weeks treatment Olanzapine was effective in improving neurocognitive deficits compared to haloperidol, whereas risperidone produced no improvements compared to haloperidol.
3 and 6 months
SGA were significantly more effective in improving cognitive functioning than FGA. Verbal fluency, digit-symbol substitution and executive functioning were most responsive to treatment with SGA. Attention was also responsive,
1 year
Olanzapine improved verbal memory, risperidone improved executive function. FGA treatment resulted in no improvement.
Olanzapine and risperidone improved negative symptoms, modestly improved attention and executive function.
8, 24, & 52 weeks
Olanzapine improved social functioning, risperidone did not.
All treatment groups experienced small neurocognitive improvements and there were no differences between groups.
2 months All treatment groups experienced small neurocognitive improvements and there were no differences between groups.
29
Although SGA such as olanzapine appear to have modest advantages in regards to effectiveness compared to FGA, the results of at least one study suggest that differences in clinical effectiveness between olanzapine and FGA tend to be greater in first-episode patients than in multi-episode patients (Sanger et al., 1999). Sanger et al. (1999) found that olanzapine treatment was more effective in reducing positive and negative symptoms in first-episode compared to multi-episode patients, whereas the efficacy of haloperidol did not differ between first-episode and multi-episode patients, although olanzapine treatment tended to be more effective than haloperidol in both groups. Interestingly, EPS associated with haloperidol treatment were worse in first-episode compared to multi-episode patients. This finding suggests that haloperidol may become more tolerable in regards to EPS over the course of illness, and the superiority of olanzapine in clinical effectiveness may diminish to some extent over the course of illness.
Davis, Chen and Glick (2003) pointed out that Geddes et al. (2000) based conclusions drawn about tolerability on number of dropouts. Dropouts can occur due to lower efficacy or other reasons besides poorer tolerability. Better tolerability of SGA is supported by another meta-analysis of 11 studies assessing risk for Tardive Dyskinesia (TD) during treatment with
SGA lasting for one year or longer (Correll, et al., 2004). All studies used rating scales rather than dichotomous measures and the mean annual incidence of TD was 0.8% for all SGA combined (0.7% for risperidone and 0 – 0.5% for olanzapine respectively). Three of the 11 trials used haloperidol as a comparator, which had an annual rate of TD of 5.4%, considerably higher than the rate for SGA. These three trials did use high doses of haloperidol, so dose effects cannot be excluded.
Another factor affecting the tolerability of FGA besides dosage is the use of concomitant anticholinergic medication to control EPS. Rosenheck et al. (2003) found that
30
combining haloperidol treatment with prophylactic prescription of an anticholinergic agent, such as benztropine, tended to reduce most EPS apart from akathisia to a level comparable to that found in olanzapine treatment. Rosenheck et al. argued that in previous studies, anticholinergic agents were normally prescribed after EPS have already appeared and that prescribing these agents at the onset of treatment can prevent or reduce the incidence of EPS.
Findings from the studies reviewed suggest that patients may actually find FGA to be equivalent in tolerability to SGA when doses of FGA are low, when anticholinergic medication is used, and if they have been on medication for a long time.
Effectiveness and tolerability of Long Acting Injectable medication
Recent studies suggest that even though SGA medications may be more tolerable, non-adherence with oral medication is still a major problem (Bhanji, Chouinard, &
Margolese, 2004). Many patients find adherence with oral medication difficult for a variety of reasons, including cognitive impairment, poor insight, or a poor therapeutic alliance with the treatment team (Cañas & Möller, 2010). Furthermore, there is evidence from studies using electronic devices to detect non-adherence, that adherence with medication is greatly underestimated by both physicians and patients alike (Cañas & Möller, 2010). Non-adherence with treatment is associated with increased risk of relapse. To improve adherence, patients may be given long-acting injectable (LAI) rather than oral medications. In addition to improving adherence, LAIs increase the stability of blood plasma medication levels, and reduce the probability of rapid symptomatic decompensation due to missing regular medication (Lasser, Bossie, Gharabawi, & Turner, 2004). Furthermore, a systematic review revealed that five out of six studies comparing patients’ attitudes to LAI versus oral medication found that patients tend to prefer the former (Walburn, Gray, Gournay, Quraishi,
& David, 2001).
31
Long acting injectable treatments using FGA have been in use since the 1960s, but
LAI SGA treatments have only recently become available. Risperidone is the first SGA antipsychotic medication to become available as an LAI. A number of studies suggest that
LAI risperidone is safe and efficacious and has fewer extrapyramidal side-effects compared to FGA medications (Bhanji, et al., 2004; Lasser, et al., 2004). Lasser et al. (2004) reported that a group of patients who were switched from an LAI FGA to LAI risperidone experienced significant reductions in severity of EPS over a year of treatment according to both subjective (patient-rated) and objective (physician-rated) measures. These results concur with a 50-week open-label study that found low rates of emergent Tardive Dyskinesia (1.19%) and a decrease in existing dyskinesia in patients initiated on treatment with LAI risperidone
(Gharabawi, Bossie, Zhu, Mao, & Lasser, 2005). The design of these studies does not allow direct comparison of LAI risperidone with LAI FGA, as there were no comparison groups. A review of studies on LAI risperidone published between 2006 and 2009 (Cañas & Möller,
2010) found that treatment-emergent tardive dyskinesia occurred in 0.7 – 0.9% of patients in long-term studies. Patients switched from LAI FGA were found to experience significant reductions in EPS (Möller, 2006). Additionally, patients randomised to LAI risperidone experienced less severe EPS compared to patients randomised to oral risperidone or oral haloperidol (Cañas & Möller, 2010). Cañas and Möller concluded that the safety and tolerability of LAI risperidone are comparable to its oral form.
LAI preparations of olanzapine became available more recently than LAI risperidone, so it has been studied less extensively and long-term data are currently available only in presentation abstracts (Cañas & Möller, 2010). A trial comparing oral olanzapine with the
LAI form found that EPS were minimal during the treatment period and did not differ between groups (Citrome, 2009, cited in Cañas & Möller, 2010).
32
Effects of drugs on neurocognitive deficits
In addition to concerns about tolerability and effectiveness, there has been debate about the advantages of SGA compared to FGA regarding their effects on improving neurocognitive deficits. Cognitive deficits have a major impact on features of QOL, such as social and occupational functioning in patients with schizophrenia that actually appears to be greater than the impact of positive and negative symptoms (Cuesta, Peralta, & Zarzuela,
2000). A number of early longitudinal studies found that improvements in aspects of cognitive functioning occurred during treatment with clozapine (A. M. Mortimer & Dye,
1996; A. M. Mortimer, et al., 1998) and also with other SGA, particularly olanzapine and risperidone (Cuesta, et al., 2001; Gurpegui, et al., 2007; Keefe, et al., 1999; Purdon, et al.,
2000), whereas treatment with FGA did not seem to result in any improvement in cognitive functioning. Keefe et al. (1999) reported that although SGA improved some aspects of cognitive functioning (e.g. verbal fluency, digit-symbol substitution and executive functioning), learning and memory were not significantly improved by either SGA or FGA.
Furthermore, improvements that occurred tended to be modest and patients who improved still did not reach normal levels of functioning. Interestingly, Keefe et al. (1999) suggested that some of the improvements associated with SGA may have related to the fact that EPS associated with FGA can have detrimental effects on performance in neurocognitive tests involving fine motor skills.
However, two more recent studies comparing FGA agents, haloperidol (Keefe, et al.,
2006) and perphenazine (Keefe, et al., 2007) with several SGA (both studies included risperidone and olanzapine treatment) found that all treatment groups experienced small neurocognitive improvements, and that there were no differences between groups. This contrasts with the majority of previous findings. One possible explanation is that in the study using haloperidol as the comparator (Keefe, et al., 2006) patients in the haloperidol arm
33
received a substantially lower dose (410mg chlorpromazine equivalent) compared to those in the SGA arms (736mg chlorpromazine equivalent). Furthermore, perphenazine is associated with fewer EPS than haloperidol, the comparator most frequently used in previous studies.
Negative effects associated with high dose haloperidol treatment, rather than special superiority of atypical agents, might explain this discrepancy. Therefore, it is possible that control of EPS might actually be more important to improving neurocognition than the specific properties of the antipsychotic.
A wide range of factors, including social and psychological as well as biological ones, affects cognitive performance. For example, mood and personality, physical fitness, pain and fatigue can influence performance on cognitive tests (Heinrichs, 2007). Antipsychotic drugs might improve performance due to non-specific factors, such as decreased distress and psychopathology symptoms, rather than improvements in the underlying neurological functions that underlie cognitive capacity (Heinrichs, 2007). Furthermore, it is unclear whether cognitive functioning relates to SWN.
Results from the CATIE and CUtLASS trials
Due to continued concerns that SGA might not be superior to FGA at low doses, and concerns about adverse effects of SGA including weight gain and metabolic effects, two independent clinical trials with no industry sponsorship were conducted, the CATIE (Clinical
Antipsychotic Trials Of Intervention Effectiveness) (Lieberman, et al., 2005) and CUtLASS
(Cost Utility of the Latest Antipsychotic Drugs In Schizophrenia Study) (Jones, et al., 2006) trials (Naber & Lambert, 2009). The CATIE trial found that olanzapine had the longest time to discontinuation of all drugs and was considered more effective in this regard. The
CUtLASS trial however found no significant differences in how many patients remained in their allocated treatment arm after one year (Jones, et al., 2006). No significant differences in reduction of symptoms were found between medication groups in either of these trials.
34
Additionally, both trials assessed ‘objective’ QOL outcomes (such as psychosocial functioning) and found no superiority of SGA over FGA. A significantly greater percentage of patients taking perphenazine discontinued their medication, specifically because of EPS, than did patients on any of the other study drugs (Casey, 2006). The authors of the CATIE and CUtLASS trials argued that SGA do not appear to be more effective than FGA and are not associated with better QOL. Naber and Lambert (2009) argued that methodological flaws contributed to these outcomes, and these need to be considered.
Criticism of CATIE and CUtLASS trials
Naber and Lambert (2009) argued that one of the methodological problems in the
CATIE trials was that patients with Tardive Dyskinesia (TD) at baseline were withheld from randomisation to perphenazine treatment, and this could have biased quality of life and time to discontinuation results. In spite of patients with initial TD being excluded, patients in the perphenazine arm actually had the highest rate of EPS (17%) (Casey, 2006) even though the modal dose was considered ‘moderate’ and discontinuation due to EPS was significantly highest in this treatment arm (8% compared to 2-4% in the SGA arms). The dose range in the
CATIE study was deliberately kept low to minimise the risk of EPS. Casey (2006) argued that effective doses of perphenazine used in normal clinical practice are substantially higher than those used in the CATIE study and that severity of EPS is known to be dose-related.
Therefore, routine clinical use of perphenazine would be expected to produce higher rates of
EPS than observed in the study.
Regarding the CUtLASS trials Naber and Lambert (2009) were concerned that the comparison of FGA with SGA may have been biased because the most commonly used FGA was sulpiride, prescribed to 49% of patients in the FGA arm. Sulpiride has an unusually specific D
2 receptor action and does not block adrenergic, cholinergic, or serotonergic receptors to any noticeable extent (Omori & Wang, 2009). A Cochrane review suggests that it
35
may produce fewer EPS compared to most FGA although evidence for its effectiveness compared to other drugs is somewhat limited by the small number of studies (Soares, Fenton,
& Chue, 1999). Even though sulpiride has been in use for treatment of symptoms since the
1960s and is therefore classified as an FGA, some authors consider it to be an ‘atypical’ antipsychotic due to its more benign EPS profile (Omori & Wang, 2009). On the other hand,
Jones et al. (2006) have argued that sulpiride would have to be remarkably effective to negate a real advantage of SGA in the CUtLASS trials, particularly as the effects would have been diluted by the inclusion of other FGA. Unfortunately, trials comparing sulpiride exclusively with other SGA appear to be lacking (Omori & Wang, 2009; Soares, et al., 1999).
Furthermore, Naber and Lambert (2009) argued that the QLS, as a clinician-rated measure is not sufficiently sensitive to the patient’s subjective experience to detect differences in subjective perceptions of treatment related to well-being. A naturalistic longitudinal study assessing subjective (self-reported) and objective (clinician-rated) aspects of QOL by Ritsner et al. (2004) found no significant differences between SGA-treated and
FGA-treated patients. However, FGA-treated patients needed higher doses of medication to achieve the same therapeutic effects as SGA-treated patients. When controlling for daily dose, SGA-treated patients were superior to FGA-treated patients in overall subjective QOL although there were no differences in their objective QOL. Naber and Lambert have argued that measures of subjective aspects of QOL, such as the SWN, are needed to understand the patient’s perspective on treatment.
SWN as a measure of subjective QOL
Although improvements in objective outcomes such as symptoms and cognitive functioning are important outcomes, the patient’s perspective on treatment is an important consideration due to its effect on treatment adherence and on subjective quality of life. As noted earlier, Naber (1995) developed the SWN scale to assess effects of antipsychotic drugs
36
on subjective aspects of QOL and a number of studies have compared the effects of various drugs on SWN. See Table 1 for a summary of these studies. Naber (1995) found that patients treated with clozapine (due to treatment resistance or major side-effects) had significantly better SWN compared to patients treated with an FGA (either haloperidol or flupenthixol).
Clozapine is regarded as the most effective drug in treating schizophrenia in patients who fail to respond to other drugs (Meltzer, 2004). However, because clozapine has potentially lethal side-effects, it is regarded as a treatment of last resort (at least in Western countries) and therefore newer atypical drugs, such as olanzapine and risperidone, are more commonly used.
Subsequent research has examined how other SGA, such as olanzapine and risperidone, compare in their effects on SWN with clozapine and also with FGA, and have produced conflicting results.
A subsequent study by Naber et al. (2001) found that SWN was significantly more improved overall in patients taking olanzapine, compared to patients taking either clozapine or risperidone. Olanzapine was superior in relation to overall subjective well-being, and also in relation to the domains of physical functioning, mental functioning, and social integration.
However, it is worth noting that the patients treated with risperidone had higher subjective well-being scores and less psychopathology at admission compared to those receiving the other drugs. Naber et al. (2001) point out that EPS in risperidone treatment are most likely to occur in the first few weeks of treatment, whereas weight gain, the major side effect of olanzapine, becomes prominent later in treatment. Therefore, the superiority of olanzapine in regards to improving subjective well-being may have related to the timing of these sideeffects. However, a later study by Naber et al. (2005) found that olanzapine and clozapine produced equivalent improvements in SWN.
37
Two studies directly comparing SWN in SGA versus FGA treatment did not find an advantage for SGA. In a randomised trial, de Haan et al. (2003) found that six-week treatment with low doses of haloperidol produced significant within-group improvements in
SWN whereas olanzapine treatment did not. The between-group difference in improvement did not reach significance due to the small sample, but the effect was of medium size. De
Haan et al. (2003) found a relationship between SWN score and dopamine D
2
receptor occupancy, as patients with D
2
receptor occupancy in the range of 60 – 70% had the highest
SWN, whereas those with occupancy over 70% had the lowest SWN. Interestingly, haloperidol patients achieved optimal levels of D
2
receptor occupancy whereas olanzapine patients were in the suboptimal range. Most patients in this study did not experience EPS, suggesting reasonably good tolerability in the haloperidol group. De Haan et al. suggested that excessively high D
2 receptor occupancy in the FGA group may have been a confounding factor in previous SWN studies finding an advantage for SGA. Alternatively, de Haan et al. considered that olanzapine patients may have had higher D
2 receptor occupancy due to higher dosages than in de Haan et al.’s study. De Haan et al. pointed out that receptors other than D
2 may also be important for SWN. This latter point highlights the fact that little is yet known about the pharmacological basis of subjective well-being.
A naturalistic study again comparing haloperidol treatment with four different SGA also found no differences between treatment groups in their SWN scores (Balestrieri, et al.,
2009). SGA treatment groups in this study included clozapine and olanzapine treatment and the findings of this study suggest that strongly ‘atypical’ SGA might not be associated with better SWN than strongly ‘typical’ haloperidol. Haloperidol patients in this study were more likely than the other cohorts to be treated with anticholinergic drugs used to treat EPS.
Unfortunately, EPS were not assessed in this study. The results of the studies by de Haan et
38
al. (2003) and Balestrieri et al. (2009) suggest that when EPS are adequately managed, FGA might not be disadvantageous compared to SGA in regards to SWN.
On the other hand, naturalistic longitudinal studies by Wehmeier, Kluge, Schneider, et al. (2007) and Lambert, et al.(2006) found that initial SGA treatment was associated with higher SWN scores at follow up assessments compared to initial FGA treatment. Wehmeier et al. (2007) notably found that olanzapine treatment in particular was associated with greater
SWN improvement than treatment with other SGA or FGA treatment. However, improvement in the olanzapine cohort was not significantly greater than in the combination therapy (simultaneous treatment with two different antipsychotics) and the authors did not specify if the combination cohort involved treatment combining an SGA with an FGA or a combination of two SGA. It should be noted that SWN significantly improved in all treatment cohorts, including the FGA treatment cohort. Additionally, the FGA cohort was relatively small, whereas the olanzapine cohort had over a thousand participants, and unequal sample sizes may have biased the results. Improvements in SWN were also associated with decreases in ratings of clinical severity of illness across cohorts. Lambert et al. (2006) found that one of the predictors of adequate SWN at endpoint was initial treatment with an SGA.
The authors did not state that olanzapine had an advantage over other SGA in this regard.
Results reported by Lambert, Schimmelmann, et al. (2009) showed that initial treatment with FGA was associated with low levels of SWN over a three year period whereas early improvement followed by stably high levels of SWN was associated with initial SGA treatment. Additionally, preliminary results from a study by Lambert et al. (2010) found that
SWN scores were higher in SGA treatment compared to FGA treatment, although the difference was modest in size. Full details of the Lambert et al. (2010) study are not yet available and actual drugs compared were not specified.
39
Long-term stability of SWN
A longitudinal study conducted over three years suggests that SWN scores tend to have long-term stability and are a good predictor of chance of recovery (Martin Lambert,
Schimmelmann, et al., 2009). The researchers found that patients in the study clustered into four groups based on their long-term patterns of subjective well-being: patients with stable low; stable moderate; stable high; and patients with early improvement followed by stable high subjective well-being (“early improvement”). Table 4 lists the predictors of cluster affiliation for each cluster. Notably, low baseline SWN predicted continuing low SWN, whereas high baseline SWN predicted continuing high SWN over the three year period.
High stable subjective well-being related to good chance of recovery in terms of symptoms, functioning and subjective well-being, and complete recovery. In contrast, low stable subjective well-being was associated with a very low chance of recovery in these areas.
The authors point out that the finding that initial treatment with either a FGA or an SGA predicted cluster affiliation needs to be treated with caution. Medication was not randomly assigned in this study and choice of medication might have been influenced by factors, such as previous treatment response, that might be favourable to SGA. This study is important because it demonstrates that subjective well-being as measured by the SWN can help to distinguish between patients who have a good chance of recovery from those who have poorer chances of recovery. Furthermore, it suggests that subjective well-being has long-term stability and perhaps a trait-like character. Therefore, it seems plausible that stable characteristics of the patient, such as their personality traits could substantially relate to their long-term subjective well-being as measured by the SWN.
40
Table 4. Predictors of SWN cluster affiliation
Cluster Percentage of sample
Predictors of cluster affiliation
Stable low
Stable moderate
Stable high
Early improvement
32.8%
31.3%
16.1%
19.9%
Low baseline SWN
Initial FGA treatment
Medication non-adherence
Lack of symptomatic and functional recovery at 3 months
Long duration of illness
Higher baseline SWN
Employment
Medication non-adherence
High baseline SWN
Good functional level at baseline
Initial SGA treatment
Symptomatic recovery at 3 months
Further evidence of the long-term stability of subjective well-being comes from another longitudinal naturalistic study of outpatients, this time conducted over 12 months.
Patients could be clustered into four groups based on stability of subjective well-being, similar to those found in the previous study (Wehmeier et al., 2008). This study examined objective QOL, based on the QLS, as well as subjective well-being using the SWN. They found that patients in the stable high QOL group were less likely to have changed medication due to lack of efficacy and also had the lowest ratings of clinical severity. In the cluster with stable moderate QOL, medication with an oral FGA was predictive. Membership of the stable low QOL cluster was predicted by medication change due to lack of efficacy and by high ratings of clinical severity of illness at baseline. The cluster with improving QOL was less likely to be treated at baseline with an oral FGA and was also predicted by no medication change due to lack of efficacy. This study therefore confirmed the finding that subjective
41
well-being tends to be stable over time, and suggests that changes in medication due to lack of efficacy tend to predict poorer outcomes.
SWN in LAI treatment
To date the only published study to have compared SWN in patients treated with either an FGA or SGA LAI is a poster abstract (Balanza, et al., 2008). This was a naturalistic cross-sectional outpatient study conducted over a 12 month period. Patients’ subjective responses as measured by the SWN and the Drug Attitudes Inventory were mostly positive and actually did not significantly differ between those treated with LAI risperidone and those treated with an LAI FGA. Furthermore, there were no between-group differences in adherence even though risperidone was administered more frequently (once a fortnight versus once every 28 days). A full report of this study has not yet been published and therefore it is not clear why these results occurred. The authors did not state whether they controlled for the effects of dosage. As noted previously, Ritsner et al. (2004) found that adjusting for dosage revealed that SGA were associated with better QOL compared to FGA. Additionally, it is not known how similar patients were in each LAI group in regards to their demographic characteristics and their duration of treatment, another important covariate identified by
Ritsner et al. This study did not appear to have assessed between group differences in depression and side-effects or their impact on SWN. A number of research studies have found that these factors adversely affect SWN (Kim, et al., 2010; Kim & Kim, 2009) one of the aims of the present study is to address these factors in patients treated with LAI medications.
Correlates of SWN: Psychiatric symptoms, depression and Medication side-effects
Although SWN research began with a primary focus on the impact of antipsychotic medication, research has attempted to identify other factors that may influence or be related to SWN. Concerning demographic characteristics, Naber et al. (2001) reported that age,
42
gender, length of illness, and duration of hospitalisation, were unrelated to differences in
SWN. There is evidence that psychiatric symptoms, depression and medication side-effects correlate with SWN. See Table 5 for a summary of the relevant studies.
With regard to the relationship between medication side-effects and SWN, there is somewhat mixed evidence. Two studies using clinician-rated measures of EPS, found that
EPS were either unrelated (Naber, 1995) or only weakly negatively related to SWN (Kim,
Ann, & Kim, 2010). However, a number of other studies using clinician-rated EPS (Naber et al., 2001; Schimmelmann et al., 2005) and a study using self-reported side-effects (Kim &
Kim, 2009) found substantial negative relationships between side-effects (both EPS and autonomic side-effects) and SWN. Naber and Karow (2001) argued that medication sideeffects, particularly EPS, have a detrimental influence on patients’ subjective quality of life.
Studies have found SWN to be only weakly negatively related to positive symptoms if at all, and to have moderate negative associations with negative symptoms and ‘general psychopathology’ (Naber, 1995; Naber et al., 2001), although Kim, Ann, and Kim (2010) reported no significant relationships between these symptoms and SWN. ‘General psychopathology’ encompasses mood symptoms, such as depression, as well as cognitive/disorganised symptoms or cognitive deficits. Interestingly in this regard, Karow,
Moritz, Lambert, Schoder, and Krausz (2005) found that changes in cognitive deficits over treatment were significantly related to changes in the SWN self-control subscale.
Furthermore, all studies assessing depression found depression moderately to strongly associated with lower SWN. Kim, Ann, and Kim (2010) additionally found that depression remained significantly negatively correlated with SWN after controlling for drug attitudes,
EPS, and severity of psychotic symptoms. However, the causal relationship between depression and SWN remains unclear, as it has not been established whether depression
43
causes low SWN or vice versa or even whether there is a bidirectional relationship. There may be some conceptual overlap between the SWN scale and depression that could account for this relationship. For example, item 4 of the SWN scale assesses hopelessness, a common feature of depression. Reductions in emotionality and mental functioning assessed by the
SWN subscales may also overlap with anhedonia and depressive slowing of both motor and cognitive functions, core symptoms of depression (Clark & Watson, 1991). There is evidence that anhedonia in schizophrenia may be a stable characteristic of some patients that is relatively independent of symptom status (Horan, Blanchard, Clark, & Green, 2008).
Anhedonia may fall on the opposite end of a spectrum with trait positive affect, a construct closely related to extraversion.
Naber originally developed the SWN construct to assess the effects of medication on subjective QOL and the studies by Naber and colleagues have largely focused on this.
However, the study by Kim et al. showed that the influence of depression on SWN is to some degree independent of side-effects and drug attitudes. Although antipsychotic drugs may have an influence on depressive symptoms (potentially either for better or worse), there is considerable evidence that personality traits have an independent influence on depression and
QOL related constructs in people with schizophrenia and psychiatric patients more generally
(Dinzeo & Docherty, 2007; Hansson, 2006; Masthoff, et al., 2007). However, research on the relationship between SWN and personality traits appears to be lacking.
44
Table 5. Correlates of SWN identified in published studies
Study/design Drug treatment
Naber (1995)
Cross-sectional
Naber et al. (2001)
Sample size
280
212
Unspecified
Various FGA vs.
SGA
SGA (mean treatment duration 40 days)
Results
Negative symptoms, general psychopathology, mood and depression significantly negatively correlated with SWN. Positive symptoms and EPS
(clinician-rated) not significantly correlated with
SWN.
SWN positively correlated with another subjective well-being scale (Bf-s)
Side-effects (clinician-rated), negative and positive symptoms and general psychopathology negatively correlated with SWN. Bf-s positively correlated with
SWN.
Baseline negative symptoms and EPS (clinicianrated), plus changes in positive symptoms during treatment predicted SWN at endpoint
Schimmelmann et al. (2005)
Longitudinal
Karow, Moritz,
Lambert, Schoder,
& Krausz (2005)
Longitudinal
Kim & Kim (2009)
Cross-sectional
Kim, Ann, & Kim
(2010)
Cross-sectional
63
84
30
80
Kim, Ann, & Kim
(2011)
Longitudinal
35
SGA (12 months treatment)
Risperidone
Various SGA (n =
28) or no treatment
SGA (8 week treatment)
Depression and negative symptoms significantly negatively correlated with SWN. Cognitive deficits were a significant time-dependent covariate of the self-control subscale.
SWN significantly negatively correlated with selfreported EPS, akathisia and autonomic symptoms.
Depression only significantly negatively correlated with SWN. EPS (clinician-rated) had a weak, nonsignificant relationship. Positive and negative symptoms not significant.
Depression strongly negatively correlated with baseline and endpoint SWN. General psychopathology negatively correlated with SWN at endpoint. Changes in depression over treatment predicted changes in SWN.
Personality traits in schizophrenia
Personality traits in people with schizophrenia have been studied using a number of models, including the Five Factor Model (FFM). The FFM proposes the existence of five broad personality dimensions – extraversion, neuroticism, agreeableness, conscientiousness, and openness to experience – that provide a comprehensive description of the variance in personality traits (McCrae & Costa, 1999). Neuroticism is a predisposition to react to stressful events with negative emotions such as depression, anxiety, and anger. Extraversion relates to sociability, assertiveness, cheerfulness, and liveliness. Agreeableness relates to trust, sympathy, and modesty. Conscientiousness refers to self-discipline and striving to achieve important goals. Openness to experience includes intellectual and artistic interests, as
45
well as awareness of one’s thoughts and feelings (Costa & McCrae, 1992). Studies suggest that the FFM is a highly comprehensive model that substantially encompasses the variance in most well-known personality trait assessment measures (O'Connor, 2002). These personality dimensions have been assumed to underlie both normal and abnormal personality characteristics (Masthoff, et al., 2007).
Furthermore, personality measures from the FFM have been used to investigate a wide range of phenomena relevant to schizophrenia (Dinzeo & Docherty, 2007). A number of studies suggest that people with schizophrenia may differ from healthy control subjects in
their personality traits, possibly in relation to all five factors. See Table 6.
relevant studies. Many studies have found that people with schizophrenia have higher levels of neuroticism and lower levels of extraversion compared to controls or community norms
(Bagby et al., 1997; Berenbaum & Fujita, 1994; Camisa et al., 2005; Lysaker, Wilt, Plascak-
Hallberg, Brenner, & Clements, 2003). A number of studies have also found lower agreeableness (Bagby, et al., 1997; Camisa, et al., 2005; Lysaker, et al., 2003) and lower conscientiousness (Camisa, et al., 2005; Gurrera, Nestor, & O'Donnell, 2000) in people with schizophrenia. Findings in relation to openness to experience have been mixed in that some studies have found no significant differences from controls (Bagby, et al., 1997; Furukawa et al., 1998; Kentros, et al., 1997a), whilst others have found lower openness in people with schizophrenia, either marginally (Gurrera, et al., 2000) or significantly (Camisa, et al., 2005).
It should be noted that the studies that found no differences in openness to experience compared to community norms all had small sample sizes. On the other hand, Gurrera et al.
(2000) used an all-male sample and Camisa et al. (2005) used a predominantly male sample, therefore these findings may or may not apply to females with schizophrenia.
46
Table 6. Studies on Five Factor Model personality traits in schizophrenia
Study
Berenbaum & Fujita
(1994)
Sample size
Review of 15 studies
Personality traits assessed
Neuroticism
Extraversion
Results
People with schizophrenia had higher neuroticism ( d = 1.02) and lower extraversion ( d = -.54) compared to healthy controls
Kentros et al. (1997a)
Bagby, et al. (1997)
Furukawa, et al. (1998)
Gurrera, et al. (2000)
Lysaker et al. (2003)
Camisa, et al. (2005)
21 patients (15 male) compared to community norms
41 people with schizophrenia (25 male), 62 recovered from unipolar depression, 34 people with bipolar disorder compared with community norms
Neuroticism
Extraversion
Agreeableness Conscientiousness
Openness to experience
Neuroticism
Extraversion,
Agreeableness Conscientiousness
Openness to experience
19 people with schizophrenia; 84 controls
Neuroticism
Extraversion,
Agreeableness Conscientiousness
Openness to experience
24 male people with schizophrenia;
46 male community controls
59 schizophrenia/schizoaffective patients (57 male); 17 male controls
Neuroticism
Extraversion,
Agreeableness Conscientiousness
Openness to experience
Neuroticism
Extraversion,
Agreeableness
63 people with schizophrenia (61 male), 24 people with cluster A personality disorders; 55 normal controls
Neuroticism
Extraversion,
Agreeableness Conscientiousness
Openness to experience
Higher neuroticism, lower conscientiousness in patients.
Extraversion, agreeableness, & openness to experience same as community sample
All diagnostic groups higher on neuroticism and lower on conscientiousness compared to community sample. Schizophrenia group lower than community sample on agreeableness.
Schizophrenia and unipolar depression groups lower than community sample on extraversion. Openness to experience in the schizophrenia group in the normal range.
Differences were non-significant for all traits. However, effect sizes were medium for neuroticism ( d = .65), extraversion ( d = -
.55), and conscientiousness ( d = .50) in the expected directions.
There was a modest effect for people with schizophrenia to be lower on agreeableness ( d = .31)
People with schizophrenia were significantly higher on neuroticism
( d = .94) and lower on conscientiousness ( d = .50), with nonsignificant trends to be lower on extraversion ( d =.41) and openness to experience ( d = .48).
Patients higher than controls on neuroticism, lower on extraversion and agreeableness compared to controls
People with schizophrenia were higher on neuroticism, and lower on all other four traits compared to controls.
47
Personality trait predictors of clinical outcomes
Many studies have found that FFM traits predict a number of important clinical outcomes (Berenbaum & Fujita, 1994; Camisa, et al., 2005). A number of prospective studies using large cohorts have found that high neuroticism and low extraversion in adolescence and early adulthood predict an increased risk of developing schizophrenia later in life (Goodwin,
Fergusson, & Horwood, 2003; Jan-Erik et al., 2007; Krabbendam et al., 2002; Lönnqvist et al., 2009; van Os & Jones, 2001). Furthermore, low extraversion is associated with poor premorbid functioning and is predictive of poor prognosis in schizophrenia (Berenbaum &
Fujita, 1994). Furthermore, a number of prospective and follow-back studies examining childhood characteristics of people who develop schizophrenia have found that prior to onset of their illness, patients are more introverted, socially withdrawn and socially incompetent compared to controls (Berenbaum & Fujita, 1994). This finding suggests that low extraversion may play a role in the development of schizophrenia, rather than suggesting that developing schizophrenia causes people to become less extraverted. Additionally, there is evidence that personality traits in people with schizophrenia remain stable over time independently of clinical symptoms status (Kentros, et al., 1997a).
The reasons why these personality traits are associated with increased risk of developing schizophrenia are not well understood. However, researchers have speculated that high neuroticism fosters the development of negative cognitive schemas that contribute to greater levels of negative affect and the tendency to interpret anomalous perceptual experiences in negative and threatening ways (Dinzeo & Docherty, 2007). People with schizophrenia have been found to be significantly more shy and less sociable compared to community controls (Goldberg & Schmidt, 2001). Furthermore, low extraversion is
48
associated with reduced positive affect and reduced sociability that may reduce the quality and amount of social support a person receives (Dinzeo & Docherty, 2007).
Although people with schizophrenia tend to differ from community norms in their levels of neuroticism and extraversion, individuals differences in neuroticism and extraversion are associated with a number of important outcomes in this population (Dinzeo
& Docherty, 2007). Patients with high levels of neuroticism tend to experience greater emotional distress and have higher rates of substance use, including smoking and tobacco as well as a range of recreational drugs (Dinzeo & Docherty, 2007). On the other hand, people with schizophrenia who are more extraverted tend to have larger social networks (Kentros, et al., 1997b), whereas more neurotic patients tend to have fewer interpersonal relationships
(Dinzeo & Docherty, 2007). Additionally, greater shyness and more limited sociability in people with schizophrenia are associated with more interpersonal dysfunction, and poor sociability is associated with greater negative symptoms (Goldberg & Schmidt, 2001).
Furthermore, low dispositional positive affect and high dispositional negative affect have been associated with greater social anhedonia and social anxiety within schizophrenia samples (Horan, et al., 2008). Dispositional positive and negative affect are considered proxy measures for extraversion and neuroticism respectively (Horan, et al., 2008). Social support has been found to be beneficial for both physical and mental health. Therefore, neuroticism and extraversion have clear health implications for people with schizophrenia and it is not surprising that a number of studies have found that better quality of life in schizophrenia and schizoaffective disorder is associated with lower neuroticism and higher extraversion
(Kentros, et al., 1997b; Ritsner, Farkas, & Gibel, 2003).
Agreeableness, conscientiousness, and openness to experience in schizophrenia have not been as intensively researched as neuroticism and extraversion, and there do not appear to
49
have been any prospective studies examining any aetiological role they might have (Dinzeo
& Docherty, 2007). However, there is evidence that individual differences in these traits are related to a number of important outcomes (Dinzeo & Docherty, 2007). High agreeableness is associated with prosocial concern and hence with the quality of one’s interpersonal relationships. Low agreeableness on the other hand, associated with cynicism and distrust, tends to be associated with aggressive, antisocial behaviour (Gaughan, Miller, Pryor, &
Lynam, 2009). A number of studies suggest that low agreeableness is associated with more severe schizophrenia psychopathology, including positive and excitement symptoms, such as uncooperativeness, poor impulse control and hostility (Lysaker, et al., 2003). Furthermore, another study found that lower agreeableness was associated with greater depression and more severe negative symptoms, whereas higher agreeableness was associated with better
QOL (Kentros, et al., 1997b).
Conscientiousness is associated with self-discipline and self-control, whereas low conscientiousness tends to be associated with impulsivity, disinhibition and lack of planning
(Costa & McCrae, 1992). Low conscientiousness and low agreeableness have been found to be associated with higher rates of antisocial behaviour and psychopathy (Gaughan, et al.,
2009). Low conscientiousness in patients with schizophrenia has been reported to be associated with suicidal behaviour, a finding in line with research that found that male college students low in conscientiousness had higher suicidal ideation (Dinzeo & Docherty,
2007). Low conscientiousness is associated with a reduced sense of competence as well as greater impulsivity, factors that may increase the risk of suicide.
The role of openness to experience in schizophrenia has not been researched as extensively as the other personality factors. Openness to experience has a modest positive association with intelligence (Chamorro-Premuzic, Furnham, & Ackerman, 2006) and with
50
education (Dinzeo & Docherty, 2007). Bagby et al. (1997) found that low openness to experience in people with schizophrenia was associated with lower socioeconomic status and lower education. It is possible that low openness to experience in people with schizophrenia is a consequence of the disorder itself as onset of illness may disrupt educational and vocational achievement (Dinzeo & Docherty, 2007). A study by Kentros et al. (1997) found that higher openness to experience was associated with better social functioning, less depression and fewer negative symptoms. Perhaps high openness to experience in people with schizophrenia is associated with intact cognitive functioning and therefore acts as a protective factor. However, published studies on schizophrenia do not appear to have addressed whether this personality trait relates to cognitive status.
Openness to experience is associated with greater awareness of one’s thoughts and feelings (Costa & McCrae, 1992), and low openness to experience has been found to be strongly associated with alexithymia (Czernecka & Szymura, 2008). Alexithymia involves deficits in the ability to recognise and express one’s emotions. A study on alexithymia in schizophrenia showed that male patients in particular had more difficulty verbalising and identifying their emotions than controls, while at the same time they experienced higher levels of emotional arousal. Female patients on the other hand did not demonstrate this impairment (van 't Wout, Aleman, Bermond, & Kahn, 2007). Researchers have speculated that alexithymia causes deficits in social functioning due to problems in affect regulation.
Therefore, openness to experience, at least in male patients, due to its relationship with alexithymia, may be relevant to the SWN emotional regulation subscale, and possibly the mental functioning subscale as this concerns aspects of one’s mental life.
Relationships between personality traits and subjective well-being related constructs
Researchers have found that FFM dimensions are related to QOL-related concepts such as happiness and life satisfaction in the normal population (DeNeve & Cooper, 1998;
51
Steel, et al., 2008) and to measures of QOL in psychiatric populations (Kentros, et al., 1997b;
Masthoff, et al., 2007) and therefore may be correlated with SWN. For example, two metaanalyses of personality traits and subjective well-being in the general population, found that personality traits significantly correlated with both trait-like measures of subjective wellbeing (life satisfaction; happiness; quality of life) and state-like measures (positive and negative affect) (DeNeve & Cooper, 1998; Steel, et al., 2008). Specifically, neuroticism predicts poorer subjective well-being whilst the other traits tend to predict higher subjective well-being. Steel, Schmidt and Schultz (2008) found that neuroticism was the strongest predictor of subjective well-being, especially for negative affect and quality of life.
Additionally, extraversion and conscientiousness were ‘strong’ predictors of quality of life, and extraversion notably had the largest impact on positive affect. Agreeableness was also a significant predictor of aspects of subjective well-being, including quality of life and positive affect, although less strongly than extraversion, conscientiousness, or neuroticism.
Interestingly, openness to experience had a small yet significant positive effect on quality of life and positive affect.
Although SWN and QOL are distinct constructs, there is evidence that they tend to be correlated (Wehmeier, et al., 2007). Personality predictors of objective QOL in schizophrenia might therefore be relevant to SWN. A study of patients with diagnoses of schizoaffective disorder and schizophrenia found that low neuroticism, and high extraversion and agreeableness were strongly and significantly associated with a measure of QOL assessing the patients’ subjective global life satisfaction (Kentros, et al., 1997b). Interestingly, there were medium-sized non-significant positive correlations with openness to experience and conscientiousness. As the sample size was small (n = 21) it would be interesting to see if these dimensions were significantly related to aspects of QOL, such as SWN, in a larger sample.
52
A study examining QOL in relation to social functioning in schizophrenia found that better scores on the interpersonal relationships subscale (frequency of social contacts) of an objective QOL measure significantly related to low neuroticism and high agreeableness, although only agreeableness remained significant in a regression analysis. Better scores on the intrapsychic foundations subscale (qualitative aspects of social functioning such as empathy for others and capacity for intimacy) significantly related to low neuroticism, and high openness to experience, agreeableness, and conscientiousness. In a regression analysis, agreeableness was the strongest personality predictor, and conscientiousness and openness to experience remained significant though weak predictors (Lysaker & Davis, 2004). These results seemed to indicate that people with schizophrenia who were lower in neuroticism and higher in agreeableness tended to have more social ties, and that capacity for intimacy was associated with lower neuroticism, and higher openness to experience, agreeableness, and conscientiousness. Unexpectedly, extraversion did not predict any of the QOL measures.
Additionally neurocognitive status predicted levels of these interpersonal variables although to a lesser degree than agreeableness did. Better verbal memory and premorbid intellectual function predicted more social ties, while better verbal memory predicted a greater capacity for intimacy. Unfortunately, this study did not examine relationships between neurocognitive status and personality traits. This sample was exclusively male. Although the SWN does not assess frequency or quality of social relationships, it does assess aspects of social functioning, such as ease of staying in contact with people. Therefore, it seems reasonable that social functioning as assessed by the SWN could relate to personality traits such as agreeableness.
Relationships between personality and SWN have not been examined
Steel, Schmidt, and Shultz (2008) proposed that one of the reasons that subjective well-being measures in the general population and personality are strongly related is because they involve very similar constructs. Some of the constructs assessed by the SWN scale also
53
seems to be relevant to features of personality. For example, the SWN includes items assessing shyness, imagination, optimism/pessimism, self-control and sociability.
Extraversion tends to be associated with optimism, sociability and (low) shyness, neuroticism with pessimism, conscientiousness and agreeableness with self-control, and openness to experience with imagination. Although the scale instructs users to consider how these constructs applied to themselves in the last seven days, it seems plausible that stable features of their personality that are relevant to these items are likely to influence their responses.
Steel, Schmidt, and Shultz (2008) stressed the fact that conceptual overlap between personality and subjective well-being should not simply be dismissed as merely a form of method variance where the two are related simply because they share similar items. They argued that conceptual overlap reflects legitimate relationships between correlated variables.
Well-validated measures of positive and negative affect ask participants to rate their mood states from the last seven days and a person’s frequently occurring mood states are strongly correlated with their personality traits (Steel, et al., 2008). Measures of extraversion for example do not typically ask about optimism directly, yet measures of optimism tend to correlate with extraversion. Similarly, stable personality traits of people with psychosis, in addition to more transient factors may well influence their self-reported subjective wellbeing. No published studies known to the present author have assessed the relationship between SWN and personality traits. Personality traits have been shown to be stronger predictors of outcomes related to subjective well-being in the general population than demographic factors (Diener, Suh, Lucas, & Smith, 1999) and there is evidence that personality traits influence QOL outcomes in psychiatric patients and those with schizophrenia in particular. Furthermore, personality traits, particularly neuroticism, have been shown to be strong predictors of depression in people with schizophrenia (Lysaker, Bell,
Kaplan, Greig, & Bryson, 1999a) and in the general population (Kenneth S. Kendler, Gatz,
54
Gardner, & Pedersen, 2006), and depression has been shown to have a strong negative influence on SWN.
Personality and side-effects
As well as depression, side-effects have been shown to have a negative influence on
SWN (Kim & Kim, 2009) and no published studies have examined whether self-reported side-effects are related to personality traits. Neuroticism has been found to be correlated with more physical health complaints (Charles, Gatz, Kato, & Pedersen, 2008) and illness-related behaviours and is related to hypochondriacal symptoms (Charles, et al., 2008). Neuroticism seems to be related to increased internal self-focus leading to preoccupation with physical symptoms and hypervigilance concerning possible health complaints. Additionally, there is evidence that higher neuroticism has an objectively detrimental effect on health due to its association with chronic emotional distress, which has been linked to poorer immune functioning (Charles, et al., 2008). Therefore, patients with higher neuroticism may be more likely to complain of adverse side-effects for a number of reasons, such as greater preoccupation with symptoms, increased depression, and possibly greater vulnerability to poorer physical functioning due to poorer immune functioning.
Self-assessed health and subjective well-being
Although personality is associated with both subjective well-being and self-assessed health, there is evidence that self-assessed health is an important predictor of subjective wellbeing in the general population in its own right (Okun, Stock, Haring, & Witter, 1984b).
Naber (1995) found that SWN was correlated with ratings of physical health. However, no studies on SWN appear to have assessed whether self-assessed health predicts SWN when controlling for other potentially related variables, such as depression, side-effects or personality.
55
Personality and neurocognitive test performance in schizophrenia
In addition to being linked to symptomatology and QOL, personality traits in schizophrenia have been linked to neurocognitive test performance (Gurrera, Nestor,
O'Donnell, Rosenberg, & McCarley, 2005). In the Gurrera et al. (2005) sample, patients were lower than community controls on extraversion, and agreeableness, and higher on neuroticism, and they were non-significantly lower on conscientiousness and openness to experience. However, when controlling for variance in performance on neuropsychological tests, there were no between-group differences in personality traits. In fact, neuropsychological status seemed to be a more important predictor of personality traits than diagnostic status (i.e. schizophrenia vs. control group) when both of these were controlled for in a regression analysis. The sample was predominantly male. The study was cross-sectional and correlational in nature, therefore no conclusions about cause-effect relations between personality and neurocognitive functioning can be drawn. This study did not assess premorbid intelligence. Differences in intelligence are likely to contribute to variation in neuropsychological performance. Differences in education and socioeconomic status were taken into account however.
In a related finding, Tien et al. (1992) found that in a community sample with selfreported schizophrenia-spectrum symptoms, FFM personality traits predicted performance on a number of neuropsychological tests. Performance on a test of cognitive flexibility positively correlated with openness to experience. Performance on this test requires executive ability to shift cognitive sets and higher openness to experience involves facility with abstract concepts. The finding that persons with schizophrenia spectrum traits who were low on openness to experience performed poorly on a test of cognitive flexibility suggests that low openness to experience may be associated with deficits in executive functions required for abstract thought. Furthermore, agreeableness and conscientiousness were also associated with
56
better performance on the same test. Participants who were low in conscientiousness may have made more errors due to carelessness. More agreeable participants might have performed better due to greater willingness to cooperate with the experimenter (Tien, et al.,
1992). Disturbances in cognitive functioning might affect aspects of premorbid and comorbid personality. In healthy volunteers, smaller frontal lobe volume is associated with more pathological personality traits as assessed by the MMPI (Gurrera, et al., 2005). Alternatively, personality traits could affect performance on these tests. More neurotic participants might make more errors due to test anxiety (Tien, et al., 1992).
As previously noted, some studies have found that SGA may be associated with improvements in neurocognitive performance in addition to improvements in SWN. It is not known whether neurocognitive status is associated with SWN levels or whether these are independent of each other. Assessing personality traits may help to clarify a possible source of variance relating to both neurocognitive status and SWN.
Aims of the present study
The present study aims to investigate variables such as personality, depression, sideeffects, self-assessed health and neurocognitive status that could be associated with SWN in patients taking long acting injectable antipsychotic medication in naturalistic settings.
Naturalistic, non-randomised designs have the advantage over randomised designs that the former better reflect the realities of clinical practice (Ritsner, et al., 2004). In RCTs, patients are carefully selected predominantly with specific symptom clusters and according to multiple exclusion criteria. In RCTs only the selected compound is administered, whereas polypharmacy, the practice of prescribing more than one antipsychotic agent at a time, as well as the simultaneous use of adjunctive medications, has become very common in clinical practice (Ritsner et al., 2002). Apart from the poster abstract by Balanza et al. (2008) no published studies have examined SWN in long acting injectable-treated patients.
57
Furthermore, the Balanza et al. study does not appear to have controlled for dosage, depression, or psychopathology, factors that prior research suggests have some influence on
SWN. Additionally, no previous studies have examined the relationship between personality traits and SWN, in spite of the established relationship between personality and measures of quality of life. The factor structure of the SWN scale does not appear to have been examined using exploratory methods. Therefore, the present study will use exploratory factor analysis to identify the scale’s possible factor structure. The relationship between the underlying factors and other potentially relevant variables such as personality and depression will then be examined. Previous research has found that personality traits such as neuroticism are risk factors for depression. Therefore, the study will examine if depression mediates the relationship between personality and SWN, although the causal relationship between depression and SWN is unknown. Additionally, the possible relationship between personality traits and self-reported side-effects has not been researched, therefore this will be examined.
Although there is evidence that SWN relates to health status, personality traits that could also influence SWN may influence ratings of self-assessed health. Therefore, the present study will examine whether health is an independent predictor of SWN when controlling for personality and other variables that may relate to both health and SWN. Furthermore, the relationship between long acting injectable medication and neurocognitive status, after controlling for premorbid IQ and personality traits, will be examined. Although previous studies have examined the effects of antipsychotic medication on SWN and on neurocognitive status separately, no previous studies have examined whether aspects of neurocognitive status relate to SWN.
Hypotheses
Based on previous research suggesting that oral SGA are associated with better SWN compared to oral FGA, it is hypothesised that SWN will be higher in patients treated with an
58
SGA long acting injectable compared to those treated with an FGA long acting injectable.
Similarly, it is hypothesised that SGA long acting injectable treatment will be associated with better neurocognitive functioning compared to FGA long acting injectable treatment. It is further hypothesised that better SWN will be associated with better neurocognitive status.
Based on research suggesting that personality traits are associated with subjective well-being and quality of life, it is hypothesised that better SWN will be associated with higher extraversion, agreeableness, conscientiousness, openness to experience, and with lower neuroticism. Another hypothesis is that SWN and depression will be inversely related.
Furthermore, it is hypothesised that the relationship between personality traits and SWN may be mediated by depression. A tentative hypothesis is that side-effect severity will be associated with higher neuroticism and possibly lower levels of the other personality traits, such as extraversion. It is hypothesised that better self-assessed health will be positively associated with SWN. The relationship between health and SWN will be examined in multivariate analyses controlling for personality, depression and other relevant variables, but no directional hypotheses are made. No hypotheses about the factor structure of the SWN scale are made as this is an exploratory investigation.
Method
Design
This was a multi-site, observational study. Patients were recruited through inpatient wards of psychiatric hospitals located in Sydney and through a Community Mental health
Centre. Written informed consent was obtained after providing patients with a detailed written information sheet about the purpose and nature of the study. Patients were assessed at two time points (baseline and 12 weeks). The study was approved by the South West Sydney
Area Health Service and University of Sydney Human Research ethics Committees.
59
Participants
Inclusion criteria in the present study were current treatment with a long acting injectable antipsychotic due to diagnosis of schizophrenia, schizoaffective disorder, or psychotic bipolar disorder. Exclusion criteria were inability to speak English and inability to complete self-report measures in a sensible manner. Inclusion criteria were broad to ensure a representative sample of patients seen in routine clinical practice.
Materials
Demographic questionnaire and lifestyle questions. Participants were asked to provide information about their age, gender, marital status, current living arrangements, educational attainment and vocational history. Additionally, they were asked several lifestyle questions. They were asked to rate their health on a four-point scale anchored between ‘poor’ and ‘excellent’ (Okun & George, 1984). Life Difficulties compared to others was rated on a scale consisting of ‘fewer’, ‘same’, or ‘more.’ Feelings of loneliness in the last month were rated on a four-point scale anchored between ‘never’ and ‘always’. They were asked to complete the statement ‘Compared to others, my mental problems are…’ with a response from a four-point scale anchored between ‘no problem’ and ‘severe problem’. Exercise during a typical week was assessed using a five-point scale anchored between ‘none’ and
‘athlete’. They were also asked to provide their contact details and those of a relative or friend to facilitate the follow-up assessment.
Drug and alcohol screen. Patients were asked to estimate their usage of alcohol and other drugs in the last month, and to indicate any past usage. Substances specified were alcohol, cannabis, tobacco, cocaine, opiates, amphetamines, sedatives or sleeping pills, hallucinogens, ecstasy, and any ‘other drugs’. Tobacco use was assessed as number of cigarettes per day. All other substances were assessed using a 7-point scale anchored with
60
‘never’ and ‘daily or almost daily’. In the case of hallucinogens they were additionally asked to estimate the number of occasions these had been taken.
Subjective Well-being under Neuroleptics.
Patients’ subjective well-being was assessed using the Subjective Well-being under Neuroleptics Short form (SWN-K; Naber et al., 2001), a 20-item version of the original 38-item SWN long form. The SWN-K consists of five subscales assessing emotional regulation, mental functioning, self-control, physical functioning and social functioning. The subscale items are randomly ordered. Items are endorsed with a six-point Likert scale, anchored at one extreme with ‘not at all’ and with
‘very much’ at the other. Subscale scores are additionally combined to yield a total score.
Each subscale consists of four items, and these consist of two positive and two negative statements. The SWN short form is highly correlated with the long form. Naber et al. (2001) reported high internal consistency for the total scale (Cronbach’s α = 0.92) and moderate to good internal consistency for the subscales, with Cronbach’s α ranging from 0.63 (selfcontrol) to 0.82 (physical functioning). In the current study, the total scale had high internal consistency (α = .82), but the subscales had low to moderate internal consistency (mental functioning α = .66; self-control α = .46; emotional regulation α = .55; social integration α =
.52; physical functioning α = .44). Items belonging to each subscale are listed in Appendix A.
Personality. When the study began personality traits were assessed using the Big-Five
Inventory – 10 (BFI-10) (John, Donahue, & Kentle, 1991; Rammstedt & John, 2007), a tenitem scale designed to assess the personality factors of extraversion, agreeableness, conscientiousness, neuroticism, and openness to experience. The scale uses a five-point
Likert scale ranging from ‘strongly disagree’ to ‘strongly agree’. As the study progressed, a decision was made to assess personality traits using the Big Five Inventory (BFI-44) (John,
Donahue, & Kentle, 1991; John, Naumann, & Soto, 2007), a 44 item scale designed to assess
61
the same personality factors as the BFI-10, using the same scale, as this provides a more detailed assessment and has higher reliability than the BFI-10. The BFI-10 was designed as an abbreviated version of the BFI-44, and the BFI-10 has been shown to have good levels of validity and reliability (Rammstedt & John, 2007). The BFI-44 scale factors have been found to have high internal consistencies (Cronbach’s α ranges from .79 for agreeableness to .87 for neuroticism). Internal consistency in the present study for the BFI-44 was moderate to good
(extraversion α = .74; agreeableness α = .69; conscientiousness α = .80; neuroticism α = .70; openness to experience α = .81). The BFI factors are highly correlated with the corresponding scales of the NEO Five Factor Inventory, a well-validated measure of the Big Five
Personality factors (convergent correlations range from .87 for extraversion to .99 for agreeableness). The BFI-44 takes about 5 minutes to complete compared to about 15 minutes for the NEO-FFI, hence the BFI has the advantage of saving time and being easier for participants to complete (Rammstedt & John, 2007). See Appendix A for BFI questionnaire items belonging to each factor.
Negative affect measures.
The Depression Anxiety and Stress Scales (DASS-21;
Lovibond & Lovibond, 1995) were used to assess negative emotional states (depression, anxiety, and stress) in the last seven days. The DASS-21 is a 21-item measure using a 4-point
Likert scale anchored with ‘did not apply to me at all’ (0) at one extreme and ‘applied to me very much, or most of the time’ (3) at the other. Scores for depression, anxiety and stress are obtained by summing the scores for the relevant items. There are seven items per scale. The
DASS has been found to be a valid and reliable measure of depression and anxiety in psychotic patients (Huppert, Smith, & Apfeldorf, 2002). Internal consistency of the scales in the present study was good (depression α = .86; anxiety α = .76; stress α = .85).
62
Attitudes towards adherence to medication.
Patients’ attitudes to adherence with medication were assessed using the Ratings of Medication Influence (ROMI), semistructured interview. Patients are asked to state their overall attitude towards treatment and taking antipsychotic medication, and to provide their main reason why they were willing to take their medication and their main reason why they may have been reluctant or unwilling to take their medication in the last month. Additionally, patients are asked to rate the degree of influence of each of 20 factors on their attitudes towards taking medication. Degree of influence of each factor is rated as ‘none’, ‘mild’, ‘strong’ or ‘not applicable’. Seven items assess factors contributing to the patient’s willingness to take medication and were averaged to form an adherence scale. The 13 remaining items assess factors contributing to the patient’s reluctance to take medication and were averaged to form a non-adherence scale. The non-adherence score was subtracted from the adherence score to form a total scale score.
Insight. Patient insight was assessed using the Insight and Treatment Attitudes
Questionnaire (ITAQ; McEvoy et al., 1989), a semi-structured interview consisting of 11 questions. Questions concern the patient’s recognition of having mental problems, their current need for psychiatric treatment, hospitalization, and medication, as well as the possibility of future mental illness, the need for psychiatric follow-up, the need for medication, and willingness to take medication. The items are rated on a 3-point scale representing poor, partial, or good insight. Items are totaled to yield a score ranging from 0 to
22 where higher scores represent better insight. Internal consistency of the scale in the present study was high (α = .96).
Side-effects of medication. Side-effects of medication were assessed using the
Liverpool University Neuroleptic Side-Effect Rating Scale (LUNSERS; Lambert, Cock,
Alcock, Kelly, & Conley, 2003), that measures 51 possible side-effects occurring within the
63
past month. It uses a five-point Likert scale anchored from ‘not at all’ to ‘very much’. Ten of these items are ‘Red Herrings’ referring to uncommon symptoms that are not known to be caused by any antipsychotic medication and are included to assess the reliability of the patient’s responses. The remaining 41 items are totaled and the total ‘red herring’ score is subtracted from this total to produce a total side-effects score, ranging from -40 to 205.
Additional subscales can be calculated for specific side-effect categories. These include neurological (extra-pyramidal side-effects, e.g. restlessness; 6 items), autonomic (relating to sympathetic nervous system activation, e.g. dry mouth, palpitations; 7 items), psychic (e.g. difficulties in staying awake or concentrating, poor memory; 9 items), and sexual (e.g. reduced or increased sex drive; 5 items) side-effects. Subscales are scored by summing all component items. Internal consistency of the total scale was high (α = .90). Internal consistency of the subscales was generally good (neurological α = .74; autonomic α = .80; psychic α = .76) except for the sexual subscale (α = .43).
Pre-morbid IQ. Pre-morbid intellectual functioning was assessed using two measures.
The Wechsler Test of Adult Reading (WTAR) (Wechsler, 2001) requires participants to pronounce each of 50 words that are arranged in order of progressive difficulty. The WTAR has been normed against the Wechsler Adult Intelligence Scale, a well-validated measure of
IQ, and performance on the WTAR has been shown to be relatively insensitive to the effects of various neurological disorders (Wechsler, 2001). The Information subtest of the Wechsler
Adult Intelligence Scale consists of 28 items assessing general knowledge arranged in order of progressive difficulty (Wechsler, 1997). Each of these measures provides an age-normed
IQ estimate.
Current intellectual functioning. Current intellectual functioning was assessed using the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS;
64
Randolph, 1996). The RBANS has been found to be sensitive to cognitive deficits in schizophrenia (Gold, Queern, Iannone, & Buchanan, 1999) and provides a general measure of cognitive ability (Hobart, Goldberg, Bartko, & Gold, 1999). The battery may be completed in
20 to 30 minutes. The battery consists of 14 tests and provides index scores in five domains of cognitive functioning: immediate memory, visuospatial-constructional, language, attention, and delayed memory. A global index based on the sum of all index scores is also obtained. All index scores are age-normed so that a score of 100 is considered Average, so that scores may be compared to IQ scores. The Battery has two alternate forms to allow retesting. Form A was used during the initial assessment; Form B in the follow-up assessment.
Psychopathology. Psychopathology was assessed with the Positive and Negative
Syndrome Scale (PANSS) (Kay, Opler, & Fiszbein, 1996), a 30-item structured interview.
The present author was given special training to administer and score the PANNS. Each item is scored on a seven-point scale, ranging from absent to extremely severe. The original
PANSS scoring system produces three composites scores: Positive symptoms (based on seven items); Negative symptoms (based on seven items); and General Psychopathology
(based on 16 items). Subsequent research has found that PANSS items can be scored to yield five factors: Positive, Negative, Cognitive/Disorganised, Affective/Depressive, and Hostile
Excitement symptoms (Bell, Lysaker, Beam-Goulet, Milstein, & Lindenmayer, 1994). The
PANSS items composing each of the five factors are listed in Appendix B.
Procedure
Participants were allowed to take breaks as required during the assessments. The total protocol was sometimes split over two different days if the participant desired. Participants completed a follow-up assessment approximately three months after completing the initial assessment. The follow-up assessment consisted of the same protocols as the initial
65
assessment, with the exception that premorbid IQ, personality, and demographic information
(apart from lifestyle questions) were not reassessed. Participants were compensated for their time with a $15 shopping voucher.
Data analysis
Statistical analyses were conducted using SPSS, version 17. The factor structure of the SWN scale was identified using exploratory factor analysis and factor scales were developed. A series of bivariate correlations were performed using the SWN total score, the factor scores, and the subscale scores. Additional bivariate correlations were performed to identify relationships between personality traits and other relevant variables. Variables with significant correlations with the SWN scales were retained for inclusion in subsequent multivariate analyses. Multiple regressions were used to identify which of the personality traits remained independent predictors of SWN scale scores, depression, health, and sideeffects when controlling for the other traits. Mediation analysis was conducted according to the guidelines proposed by Baron and Kenny (Baron & Kenny, 1986).
LAI medication groups, groupings based on use of adjunctive medications, including oral antipsychotic medications, and diagnostic groups (schizophrenia versus schizoaffective disorders) were compared on demographic and clinical variables using independent samples t -tests or ANOVA/ANCOVA as appropriate. These tests were also used to compare gender differences and differences based on inpatient versus outpatient status and based on marital status.
ANCOVA and MANCOVA were used to test differences between medication groups
(LAI and oral antipsychotic medications) controlling for covariates that had been previously identified as significant predictors of the SWN scales. ANCOVA was used when total SWN score was the dependent variable. MANCOVA was used to assess first the SWN factor scales
66
together and then the SWN subscales as grouped dependent variables in a separate analysis.
Testing a group of related dependent variables together in MANCOVA reduces Type I error compared to performing a series of ANCOVAs for each dependent variable separately
(Tabachnick & Fidell, 2001).
Due to the relatively modest sample size in the present study, it was considered that adjustment of alpha values to correct for multiple comparisons would lead to a lack of power to detect statistically significant effects. Hence, alpha values were set at .05 for all tests.
Therefore, statistically significant results may be need to be treated with caution, and the magnitude of the effect sizes needs to be taken into account when considering the practical significance of the results.
Note on estimation of effect sizes
The conventions for estimating the magnitude of the effects are shown in Table 7. The criteria used for partial eta-squared (partial η
2
) derive from Kinnear and Gray (2009); the criteria used for the other effect size statistics derive from Cohen (1992).The use of partial eta-squared as an effect size measure for analyses involving covariates is recommended by
Tabachnick and Fidell (2001).
Table 7. Effect size estimation criteria
Test Effect size
Statistic t
Correlation
-test r
Cohen’s d
Multiple regression f 2
ANCOVA/MANCOVA Partial η 2
Small
.10
.20
.02
< .06
Magnitude descriptors
Medium
.30
.50
.15
.06 < .14
Large
.50
.80
.35
.14
67
Results
Missing data
Nine patients did not complete one or more assessment items at baseline. Therefore, there was data missing for most scales, although all patients completed the SWN. Ten patients completed the BFI-10 and 67 the BFI-44, therefore all patients completed some form of personality assessment. Data from these two personality measures was pooled together, as they both assess the same constructs and are known to be highly correlated (Rammstedt &
John, 2007). Numbers of cases with missing data in each LAI group for each measure are shown in Appendix C. Cases with missing data were excluded in bivariate analyses. In multivariate analyses missing values were imputed using the expectation maximisation method so that all cases could be retained. The expectation maximisation method is recommended by Tabacnick and Fidell (2001) as one of the bests ways of imputing missing data. Analyses were also performed without imputing data and results from the two methods were compared.
Assumption testing
In all analyses, assumptions of normality and linearity were tested by inspecting P-P plots of the standardised residuals. Multicollinearity was assessed using tolerance values.
Univariate outliers were screened for using standardised values, while multivariate outliers were screened for using Mahalanobis distance values. No outliers were found. Independence was tested using the Durbin-Watson statistic. In ANCOVA and MANCOVA, homogeneity of variance/covariance was assessed using Levene’s test and Box’s M respectively. All assumptions were satisfied for all analyses, unless otherwise specified.
Demographic characteristics of Participants
All participants gave written informed consent to participate. Seventy-seven patients taking LAI antipsychotic medication for a psychotic disorder were recruited for this study.
68
Twenty-one participants completed the follow up assessment. Demographic characteristics of
the participants in each LAI medication group are shown in Table 8. Most patients had a
primary diagnosis of schizophrenia although patients diagnosed with schizoaffective or bipolar disorders were included. The age of participants ranged from 24 to 68 years, and 48 were male and 29 were female. Participants at the initial assessment were predominantly inpatients with some outpatients recruited through a community health centre. Patients had a mean educational level of 11.2 years of school ( SD = 2.23), with a range of 6 to 17 years.
The majority of participants (73%) were of Caucasian background. Most (69%) had never married, and 46 percent stated that they normally lived alone.
Baseline medication use
Forty-seven patients were treated with an LAI FGA, whilst 30 were treated with an
LAI SGA. See Table 9 for number of participants taking specific LAI medications. Sixty-one
patients were also taking an oral antipsychotic (7 took an oral FGA and the others an oral
SGA). See Table 10 for breakdowns of oral medication use in each LAI grouping. Five of these were taking a second oral antipsychotic (2 took an oral FGA, 3 took an oral SGA). (See
Appendix D for details of patients taking two oral antipsychotics.)
69
Table 8. Demographic characteristics of participants broken down by LAI medication grouping
LAI FGA LAI SGA Total n n = 47
% n n = 30
% n n = 77
%
Gender
Male
Female
Ethnicity
Caucasian
Asian/Southeast Asian
Middle eastern
Pacific Islander
Indigenous Australian
Marital status
Never married
Currently married/engaged/de facto
Divorced/separated
Usual living arrangements
Live alone
Live with parents/family members
Share accommodation
Live with partner
Homeless
Patient status
Inpatient
Voluntary
Involuntary
Outpatient
Diagnosis
Schizophrenia
Schizoaffective disorder
Bipolar disorder
Age
31
16
66
34
4
2
0
42
15
27
5
31
3
13
23
18
36
4
2
3
2
32
14
1
M (SD)
68.1
29.8
1.1
5.2
2.6
0
89.4
31.9
57.4
10.6
76.6
8.5
4.3
3.8
4.3
66
6.4
27.6
48.9
23.4
43.85 (12.80)
17
13
57
43
4
0
2
29
10
19
1
22
2
6
12
12
20
5
3
1
1
13.3
0
6.7
96.7
33.3
63.3
3.3
66.7
16.7
10
3.3
3.3
73.3
6.7
20
40
40
24
5
80
16.7
1 3.3
M (SD)
48
29
62
38
8
2
2
71
25
46
6
53
5
19
35
30
56
9
5
4
3
10.4
2.6
2.6
92.2
32.5
59.7
7.8
72.7
11.7
6.5
5.2
3.9
68.8
6.5
24.7
45.5
39
56
19
72.7
24.7
2 2.6
M (SD)
37.53 (13.51) 41.39 (13.36)
Education in years
Years on any antipsychotic medication
Years on current depot
10.61 (2.07)
17.07 (12.10)
4.64 (7.22)
12.10 (2.29)
9.76 (9.93)
0.57 (1.19)
11.20 (2.27)
14.25 (11.79)
3.18 (6.12)
In the group taking FGA LAI medication, the most commonly prescribed adjunctive oral antipsychotic drug was olanzapine, whereas in the SGA LAI group the most commonly prescribed adjunctive oral antipsychotic drug was risperidone. The difference in prescription
70
of oral antipsychotics between LAI groups was significant (χ 2
= .79, df = 9, p = < .001), indicating that patients taking FGA LAI medication were also more likely to be additionally taking oral olanzapine than another oral drug, and those in the SGA LAI medication group were more likely to be additionally taking oral risperidone than another oral drug.
Dosages of LAI and oral antipsychotic medication were converted to daily chlorpromazine equivalents (CPZE) using special software designed for this purpose
(Lambert, 2011) to enable comparison of dosages of differing medications. CPZE dosages of oral and LAI medications were summed for each patient to determine a total daily antipsychotic dosage. Mean CPZE doses in each LAI group are shown in Table 10.
Independent samples t -tests showed that there were no between-group differences in LAI
CPZE dosage or in total daily CPZE dosage, although there was a non-significant trend for
LAI FGA patients to be on a higher daily oral CPZE dose compared to LAI SGA patients, t
(75) = 1.80, p = .06, d = .43.
Table 9. LAI medications taken by number of patients
LAI
First generation
Haloperidol
Flupenthixol
Zuclopenthixol decanoate
Fluphenazine decanoate
Total FGA
Second generation
Risperidone consta
Olanzapine pamoate
Total SGA
28
2
30 n
2
23
20
2
47
%
2.6
29.9
26
2.6
61
36.4
2.6
39
71
Oral antipsychotic taken
None
FGA oral
Haloperidol
Zuclopenthixol
Total FGA
SGA oral
Risperidone
Olanzapine
Clozapine
Ziprasidone
Quetiapine
Aripiprazole
Paliperidone
Total SGA
Mood stabiliser
None
Sodium valproate
Lithium carbonate
Carbamazepine
Lamotrigine
Antidepressant
Benztropine
Benzodiazepine use in the last week
Dosage converted to daily CPZE
Depot dosage
Oral dosage
Combined dosage
Table 10. Number of participants taking oral antipsychotics and other adjunctive medications plus antipsychotic dosages in CPZE
3
16
1
3
5
2
0
30
1
6
7
0
1
4
32
12
2 n
10
LAI FGA
%
13
6
11
7.8
14.3
M (SD)
292.98 (132.59)
335.96 (244.75)
630.96 (313.13)
3.9
20.8
1.3
3.9
6.5
2.6
0
39
1.3
7.8
9.1
41.6
15.6
2.6
0
1.3
5.2
19
22
2
3
5
2
1
54
1
6
7
1
1
6
50
21
4 n
16
Total
%
20.8
8
18
10.4
23.4
M (SD)
289.76 (132.56)
299.16 (227.71)
590.28 (284.32)
9.1
1.3
7.8
24.7
28.6
2.6
3.9
6.5
2.6
1.3
70.2
65
27.3
5.2
1.3
1.3
7.8
16
6
1
0
0
0
1
24
0
0
0
1
0
2
18
9
2 n
LAI SGA
%
6 7.8
2
7
2.6
9.1
M (SD)
284.72 (134.61)
241.50 (187.72)
526.55 (222.33)
20.8
7.8
1.3
0
0
0
1.3
31.2
0
0
0
23.4
11.7
2.6
1.3
0
2.6
72
Numbers of participants using adjunctive medications are shown in Table 10. Twenty-
seven patients were prescribed a mood stabiliser, six were prescribed an antidepressant, eight were prescribed anti-Parkinson medication, and 18 had been prescribed benzodiazepines in the week prior to assessment. Chi-square tests revealed that the two LAI medication groups did not differ significantly in their prescription rates of any of these medications. (See
Appendix D for statistics.)
Eleven patients had either ever been prescribed clozapine or its use was planned.
Clozapine use is usually an indicator of resistance to treatment. Additionally, ten patients had previous history of use of electroconvulsive treatment (ECT), an indicator of illness severity.
Independent samples t -tests showed no significant differences in PANSS scores, SWN,
DASS, or LUNSERS scores based on history of clozapine or ECT treatment. (See Appendix
D for statistics.)
Factor Analysis
The SWN subscales as defined by Naber (1995) were found to be substantially intercorrelated (see Appendix F, Table F1) and tended to have moderate to low internal consistency, although the total scale had high internal consistency (see Method section for
Cronbach’s α values). Therefore, the subscales might not closely match the actual factors composing the total scale. Factor analysis was performed to examine how many underlying factors the SWN scale contains. All twenty items in the scale were therefore entered into a principal components analysis. Negatively worded items were reverse scored.
2 Direct oblimin rotation was used rather than varimax because varimax assumes that the underlying factors are uncorrelated which seems unjustified in the present study. The Kaiser-Meyer Olkin
Measure of Sampling Adequacy had a value of .72, suggesting a reasonable level of
2 Factor analysis was also conducted without reverse scoring of the negatively worded items. Results were identical, suggesting that the factor structure might not simply be an artefact of the way items are worded.
73
relatedness among the variables. Examination of the Scree plot suggested the presence of two factors (see Figure 1). The two factors were positively correlated ( r = .30) and cumulatively explained 41.07% of the variance.
Figure 1.
Scree Plot derived from Factor Analysis of SWN scale
Table 11 show the pattern matrix with factor loadings for each item. A cut-off loading of .40 was used to determine which items to retain on each factor. Factor 1 consisted of all ten negatively worded items, whereas Factor 2 consisted entirely of nine positively worded items. Item 5, ‘my body feels familiar’, had low and approximately equal loadings on each factor.
3
Based on item content, Factor 1 was called ‘negative SWN’ and Factor 2 was called
‘positive SWN’. Note that because the negative SWN items were reverse scored, higher scores on this measure indicate better subjective well-being, in line with the scoring of the other SWN scales.
3 This item was frequently queried by participants who found it hard to understand.
74
Table 11. SWN item loadings on each factor
11
12
13
14
15
16
7
8
9
10
17
18
19
20
5
6
3
4
Item no.
1
2
Descriptor
I feel powerless
Comfortable in my body
Easy to think
No hope
Body feels familiar
Shy
Imaginative
Environment friendly
Weak & exhausted
Emotions dull
Thinking difficult
Inappropriate behaviour
Keep in touch
Threatening environment
Draw a line
Body a burden
Flighty thoughts
Interested
Appropriate behaviour
Full of confidence
Percentage of variance explained
Loadings > .40 are in bold type.
Negative SWN Positive SWN
.74 .06
.66 .13
.07 .79
.32 .46
.24 .21
.05 .50
.05 .61
.51 .02
.58
.70
.26
.01
.74
.63
.06
.04
.16
.49
.10
.69
.73
.04
.00
.13
28.80
.60
.04
.50
.03
.04
.43
.66
.79
12.26
Six components had eigenvalues greater than 1. Solutions with three to six factors were examined (see Appendix E for Item loadings for these alternative factor solutions), but none of them were readily interpretable. That is, all of these solutions had at least two items with cross-loadings greater than .40 on two factors, and therefore lacked the simple structure
75
of the two-factor solution. Item 4 cross-loaded on two factors in every solution examined.
Furthermore, the factors in these models each had loadings with items from several different subscales. The five-factor solution in particular did not replicate any of the subscales proposed by Naber (1995). One of the factors in this solution consisted only of two items and hence was likely to be unreliable. Factor one in all of these models consisted exclusively of at least eight negatively worded items, similar to the two-factor solution. Even when varimax rotation was applied cross-loadings still occurred in each of the three to six factor solutions.
Therefore, the two factor solution was preferred.
According to Guadagnoli and Velicer (1988), factors with four or more variables loading above .60 are reliable and may be interpreted regardless of sample size. Both of the factors in this analysis had six variables with loadings above .60. Therefore, the two factor solution may be considered reliable in spite of the relatively small sample size (that is, less than 150). Scales based on the two factors were computed using the sum of the items loading on each factor as shown in Table 4. (Item 5 was excluded due to low loadings.) This additive approach was chosen over direct computation approaches as the latter tend to overfit the data
(Tabachnick & Fidell, 2001). The two scales are scored in the same direction to maintain consistency with the other scales. Hence, it is important to note that higher scores on the
Negative SWN scale actually indicate better subjective well-being, the same as for the
Positive SWN scale. The two factor scales were significantly positively correlated ( r = .39, p
< .001). Internal consistency for the two factors was high (negative SWN α = .82; positive
SWN α = .83).
SWN correlates
A series of bivariate correlations were conducted to determine the variables associated with SWN and therefore likely to be important covariates in later between-group comparisons. Although the five SWN subscales tended to have low internal consistency, they
76
were still included in analyses to allow comparisons with published research. All results shown are two-tailed. See Table 12. Age, education, years on medication, and time on current
LAI were not significantly correlated with any of the SWN scales. (See Appendix F for these non-significant correlations.)
Negative affect
All of the SWN scales significantly negatively correlated with depression, anxiety, and stress respectively. Notably, total and negative SWN, and all of the subscales except mental functioning each had their largest sized correlations with depression.
Personality
SWN total score, all subscales, and the positive factor were significantly positively correlated with extraversion, agreeableness, and conscientiousness, and significantly negatively correlated with neuroticism. Additionally, openness to experience significantly positively correlated with SWN total score, three subscales, and positive SWN. Negative
SWN significantly positively correlated with extraversion and agreeableness, and significant negatively correlated with neuroticism. These correlations were all in the expected direction.
Side-effects
SWN total score, all subscales, and both positive and negative SWN significantly negatively correlated with the total side-effects score and subscales (as well as the Red
Herrings) with the one exception that the correlation between physical functioning and sexual side-effects was not significant. The Red Herrings scale assesses over-reporting of symptoms, and although the total score is adjusted for this, the subscales are not. Therefore, it was considered that correlations between the side-effects subscales and the SWN scales might be inflated by over-reporting. Hence, partial correlations between the side-effects subscales and the SWN scales were conducted controlling for Red Herrings scores. These are shown in
Table 13. Psychic side-effects remained significantly negatively correlated with all of the
77
SWN scales, the strongest correlations being with negative SWN and mental functioning.
Neurological side-effects remained significantly negatively correlated with total and negative
SWN and with mental and physical functioning. Autonomic side-effects remained significantly negatively correlated with mental functioning and social integration only.
Sexual side-effects remained significantly negatively correlated with total, negative and positive SWN, and with mental functioning and social integration.
Health and lifestyle factors
SWN was significantly correlated with answers to the lifestyle questions, indicating that better SWN scores were associated with self-ratings of better global health (all scales), more frequent exercise (3 subscales, negative factor and total score), fewer life difficulties compared to others (2 subscales, negative factor, and total score), less loneliness in the past month (all scales except positive factor), and less severe ratings of one’s mental problems (4 subscales, both factors, and total score).
78
Depression
Anxiety
Stress
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Total side-effects
Red Herrings
Neurological side-effects (EPS)
Autonomic side-effects
Psychic side-effects
Sexual side-effects
Health
Exercise
Life Difficulties
Loneliness Last Month
Mental Problems
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
Hostile Excitement symptoms
PANSS total
Insight
Cigarettes per day
Table 12. SWN correlations with lifestyle, personality, side-effects, and psychopathology
Total Negative Positive MF SC ER
-.71*** -.74*** -.46*** -.60*** -.60*** -.64***
-.57*** -.59*** -.37** -.49*** -.54*** -.47***
-.56*** -.63***
.55*** .37**
.50***
.41**
.27*
.20
-.32** -.48*** -.46*** -.46***
.55*** .45*** .49***
.55***
.48***
.34**
.31**
.48***
.35**
.56***
.49***
.45***
-.59*** -.50*** -.52*** -.53*** -.59*** -.50***
.33** .16 .39*** .40*** .27* .46***
-.55*** -.57***
-.40*** -.39**
-.48*** -.52***
-.42*** -.36**
-.40**
-.30**
-.29*
-.36**
-.50***
-.24*
-.36**
-.35**
-.43***
-.41***
-.37**
-.38**
-.43***
-.38*
-.40***
-.34**
-.55*** -.61***
-.43*** -.43***
.59***
.34**
.41***
.33**
-.36** -.55*** -.45*** -.43***
-.32** -.43*** -.34**
.58*** .65*** .40***
.26* .29** .20
-.36**
.55***
.30**
-.31**
-.33**
-.35**
-.01
-.40***
-.40***
-.31**
-.16
-.19 -.06
-.52*** -.52***
-.26* -.21
-.14
-.17
-.25*
.13
-.21
-.26*
-.21
-.33**
-.28*
-.25*
.15
-.21
-.26*
-.34**
-.01
-.18
-.25*
-.29*
.05
-.14 -.13 -.31**
-.40*** -.48*** -.49***
-.09 -.33** -.23*
.03
-.36**
-.19
-.21
.00
-.32**
-.17
-.15
.09
-.24
-.10
-.24*
.08
-.18
-.21
-.20
-.01
-.31**
-.25*
-.24*
-.00
-.35**
-.04
-.25*
-.43***
.11
-.45***
-.30**
-.35**
-.36**
-.41***
-.35**
.35**
.36**
SI
-.58***
-.42***
-.50***
.41***
.37*
.29**
-.21
-.26*
-.19
-.03
-.12
-.36**
-.21
.07
-.25*
-.14
-.22
-.05
-.33**
-.08
-.09
Key: Total = Total SWN; MF = Mental functioning; SC = Self-control; ER = Emotional Regulation; SI = Social integration; Negative = Negative SWN (reverse scored); Positive = Positive SWN
-.32**
.11
-.39**
-.29*
-.43***
-.24*
-.36**
-.22
.41***
.22
PF
-.44***
-.36**
-.34**
.28*
.33**
.25*
-.33**
-.26*
-.34**
-.21
-.06
-.35**
-.22
79
Psychopathology and insight
Among the PANSS factors, total SWN was significantly negatively correlated with the Affective factor (plus four subscales, and both positive and negative SWN), the cognitive/disorganised factor (plus three subscales, and the positive factor), and the total
PANSS score (plus four subscales, and the negative factor). Negative symptoms had a modest negative correlation with the emotional regulation subscale only. Positive and excitement symptoms did not correlate with any SWN scale. Insight as measured by the
ITAQ had a modest negative correlation with the self-control subscale only.
Table 13. Partial correlations between side-effects subscales and the SWN scales controlling for Red Herrings score
Total SWN
Negative SWN
Positive SWN
Mental functioning
Self-control
Emotional regulation
Social integration
Physical functioning
Neurological
-.30*
-.38**
-.12
-.29*
-.14
-.19
-.20
-.34**
Autonomic
-.21
-.16
-.19
-.36**
-.06
-.10
-.24*
-.03
Psychic
-.43***
-.52***
-.26*
-.52***
-.30*
-.30*
-.30**
-.25*
Sexual
-.29*
-.30**
-.23*
-.37**
-.19
-.21
-.25*
-.10
Substance use
Number of cigarettes smoked per day negatively correlated with self-control, emotional regulation, and the positive factor. Use of alcohol and other drugs did not significantly correlate with any of the SWN scales (see Appendix F for all correlations).
Attitudes to adherence
See Appendix F for all correlations with the ROMI scales. The ROMI adherence scale was negatively correlated with social integration ( r = -.25, p = .042), and with negative SWN
( r = -.28, p = .021). These correlations suggest that willingness to adhere to medication was actually associated with worse social integration and worse negative SWN (as this was
80
reverse scored). The ROMI non adherence scale and total scale had no significant correlations with any SWN scale. This finding suggests that SWN was unrelated to reasons for unwillingness to take antipsychotic medications.
Performance on cognitive tests
SWN did not significantly correlate with measures of premorbid IQ. (See Appendix F,
Table F5.) SWN total score had modest significant positive correlations with immediate and delayed memory from the RBANS. See Appendix F, Table F6 for the zero-order correlations.
Because neurocognitive status is likely to vary based on premorbid IQ, partial correlations between SWN and RBANS scores were conducted, controlling for premorbid IQ. An estimate of premorbid IQ was obtained by averaging participants’ IQ scores based on the
WTAR and the Information test, as these two measures were strongly correlated, r = .64, p <
.001. The results, seen in Table 14, show that there were a number of modest significant correlations between total SWN score and immediate memory (plus 3 subscales), language
(plus 1 subscale), delayed memory (plus 1 subscale), and overall RBANS index score (plus 3 subscales).
Table 14. Partial correlations between SWN scales and RBANS scores controlling for premorbid IQ
RBANS Scale Language Attention
Total SWN
Immediate memory
.29*
Visuospatial constructional
.18 .26* .05
Negative SWN .15 .12 -.07 .04
Delayed memory
.27*
.19
Positive SWN .28* .14 .43*** .00 .22
Total score
.29*
.13
.27*
Mental Functioning
.22
.31**
.14
.20
.20
.28*
.03
.01
.20
.21
.20
.29*
Self Control
.41*** .08 .20 .05 .30* .28*
Emotional Regulation
Social Integration
Physical Functioning
-.03
.26*
.06
.23
.23
.09
-.11
.23
.15
.21
.07
.30*
81
Personality and neurocognitive test performance
Correlations between personality traits and neurocognitive test performance were examined. Openness to experience had significant positive correlations with premorbid IQ estimated from both the WTAR and the Information test, and with immediate memory, language, delayed memory and the RBANS total score. See Table 15. Immediate memory also had a significant positive correlation with conscientiousness ( r = .29, p = .017). There were no other significant correlations with personality traits. Because openness to experience was significantly correlated with several SWN scales and with several of the neurocognitive measures, partial correlations between SWN and RBANS scores were conducted, controlling for premorbid IQ and openness to experience. See Table 16 below. Very few correlations were significant.
Table 15. Correlations between Openness to experience and neurocognitive measures.
Openness
WTAR Information IM
.32** .45** .38**
VisCon
.13
Language Attention DM
.33** .14 .27*
RBANS Total
.32**
IM = Immediate memory; VisCon = Visuospatial Constructional; DM = Delayed memory
Table 16 Partial correlations between SWN scales and RBANS scores controlling for openness to experience and premorbid
IQ
RBANS Scale
Total SWN
Immediate memory
.18
Visuospatial constructional
.18
Language Attention
.15 .03
Delayed memory
.20
Total score
.19
Negative SWN
Positive SWN
Mental Functioning
Self Control
Emotional Regulation
Social Integration
-.10
.14
.08
.23*
.29*
-.08
.22
-.12
.14
.14
.18
.09
.05
.23*
.12
.39**
.09
.20
.08
.18
.04
-.03
-.03
.00
-.01
.03
-.13
.20
-.16
.14
.11
.15
.23*
.12
.20
-.08
.16
.10
.21
.19
.03
.25*
Physical Functioning
82
Additional personality correlates
Overall scores for the BFI personality factors are shown in Table 17. All of the BFI factors were significantly intercorrelated. See Appendix F for these correlations. Personality traits were correlated with a number of variables, including DASS and side-effects scores, as well as the lifestyle questions, as shown in Table 18. Correlations were generally in the expected directions, for example, depression positively correlated with neuroticism and negatively with the other four factors, whereas health showed the opposite pattern of correlations. Total side-effects and three of the subscales significantly correlated with four of the personality traits, and sexual side-effects significantly correlated with neuroticism only.
Table 17. Mean and standard deviations for the BFI factors
Factor Mean Std Dev. Range
Extraversion 3.13 .89 1.0 – 5.0
Agreeableness
Conscientiousness
3.78
3.65
.73
.83
1.5 – 5.0
1.5 – 5.0
Neuroticism
Openness to experience
2.79
3.41
.83
.85
1.0 – 4.5
1.36 – 5.0
The Red Herrings scale significantly correlated with three of the personality traits.
Correlations between personality and side-effects could be influenced by over-reporting of symptoms, therefore partial correlations were conducted between personality traits and the subscales controlling for red herring scores. (The total score already takes Red Herrings into
account.) The results are shown in Table 19. The psychic subscale remained significantly
correlated with extraversion, conscientiousness, and neuroticism. The neurological subscale remained significantly correlated with neuroticism only. The autonomic and sexual subscales did not significantly correlate with any traits.
83
Table 18 Relationships of personality with distress, side-effects, and lifestyle questions
Extraversion Agreeableness Conscientiousness Neuroticism
Depression
Anxiety
-.43***
-.29*
-.33**
-.35**
-.36**
-.37**
.51***
.42***
Stress
Total side-effects
-.31**
-.30**
-.26*
-.28*
-.37**
-.33**
.46***
.47***
Red Herrings
Neurological SE
Autonomic SE
Psychic side-effects
-.13
-.24*
-.23*
-.34**
-.29*
-.29*
-.34**
-.29*
-.26*
-.25*
-.27*
-.34**
.28*
.39**
.35**
.56***
Sexual SE
Health
Exercise
Life Difficulties
Loneliness
Mental Problems
-.21
.39**
.18
-.20
-.19
-.41***
-.18
.24*
.00
.10
.11
-.20
-.23
.22*
.14
.01
.05
-.31**
.31**
-.39**
-.27*
.27*
.21
.44***
Table 19. Relationships of personality with side-effects subscales controlling for Red Herrings
Extraversion Agreeableness Conscientiousness Neuroticism Openness
Neurological SE -.20 -.11 -.12 .29* .02
Autonomic SE
Psychic sideeffects
Sexual SE
-.20
-.32**
-.16
-.17
-.16
-.05
-.13
-.26*
-.13
.22
.50***
.21
-.09
-.14
-.11
Openness
-.24*
-.08
.00
.01
.13
.09
.04
-.06
-.05
.34**
.16
-.12
-.03
-.22
Correlates of insight
Although not a main focus of the present study, correlates of ITAQ insight are presented in Appendix F, Table F13. Insight strongly correlated with all of the ROMI scales, suggesting a strong relationship between attitudes towards adherence and insight. Insight
84
correlated negatively with both positive and negative symptoms, and the total PANSS score, but not with the other PANSS factors. Insight positively correlated with anxiety and stress, but not depression. Insight positively correlated with neuroticism, but not with any other personality factor. The only side-effect scale significantly (positively) correlated with insight was psychic side-effects. Correlations between insight and premorbid IQ or neurocognitive test performance were all non-significant (all r-values < .12).
Gender
Independent samples t -tests were used to compare men and women on demographic and clinical variables. There were no significant gender differences in age, years of education, SWN, DASS, side effects, PANSS, personality traits, RBANS, or WTAR estimated premorbid IQ. However, males scored significantly higher on the Information test used to estimate premorbid IQ. Furthermore, controlling for Information test estimated IQ using ANCOVA showed that males performed worse than females on immediate memory ( F
(1, 66) = 4.12, p = .046, partial η
2
= .06). No other differences in RBANS scores were significant. Males reported significantly more use of cannabis and amphetamines. See
Appendix G, Table G1 for statistics. No other gender differences were found in use of other substances including tobacco and alcohol. Chi-square analyses found no gender differences in diagnosis (psychosis type) or in current living arrangements. Women were more likely than men to either be currently or ever married (55.2% vs. 18.4%), χ 2
= 11.33, df = 2, p =.002. See
Marital status and SWN
An ANOVA test revealed that there was a significant main effect of marital status on
SWN total score and the emotional regulation and physical functioning subscales. See Table
21. Post hoc Tukey tests showed that those who were never married had significantly lower
scores on the emotional regulation subscale compared to those currently married ( p = .034)
85
and those previously married ( p = .005). The never married also had lower scores compared to the currently married on positive SWN ( p = .049), the physical functioning subscale ( p =
.023) and on the total SWN scale ( p = .029). No other contrasts were significant. Due to the low number of participants in the currently married category, marital status was not considered in further analyses.
Table 20 Marital status by gender
Marital status
Never married
Currently married/engaged or de facto
Divorced/separated or widowed
Total
Male
40
1
7
48
Female
13
4
12
29
Total
53
5
19
77
Table 21 SWN means as a function of marital status
Never married Currently married Formerly married F (2, 74) pvalue
M SD M SD M SD
SWN Total scale 63.58 18.140 84.60 6.877 72.84 15.87 4.76* .011
Negative SWN
Positive SWN
Mental functioning
Self control
Emotional regulation
Social integration
35.89
25.19
13.02
12.53
13.00
12.45
11.17
10.28
4.684
4.384
4.332
4.572
43.60
36.20
15.20
16.80
17.80
16.80
12.58 4.483 18.00
4.278 40.47
4.15
.447
1.789
2.950
1.581
29.16
14.68
3.347 13.84
16.53
14.00
13.79
7.24
10.83
4.96
3.67
3.42
4.84
4.10
2.43
3.30*
1.24
2.77
7.52**
2.54
3.86*
.10
.042*
.30
.07
.001
.09
.025 Physical functioning
Diagnostic groups
Comparisons were made between diagnostic categories. Because there were only two patients with bipolar disorder, these patients were grouped together with those diagnosed
86
with schizoaffective disorder. These were compared with those diagnosed with schizophrenia. The medications taken by each diagnostic group are shown in the Tables 22 –
24. Chi-square tests were performed to assess differences in allocations. The diagnostic groups did not significantly differ in how many were taking either an LAI FGA or an SGA, χ 2
= 1.31, df = 1, p = .19. All of the patients not taking an oral antipsychotic were diagnosed with schizophrenia and this difference was significant, χ2
= 9.63, df = 2, p = .008. Patients diagnosed with schizoaffective disorder were significantly more likely to be prescribed sodium valproate than patients diagnosed with schizophrenia, χ
2
= 24.06, df = 2, p < .001.
There were no significant between-group differences in prescription of benztropine, χ
2
= .47, df = 1, p = .68. All six of the patients taking antidepressant medication were diagnosed with schizophrenia, although this difference did not reach significance. There were no significant between-group differences in regard to prescription of benzodiazepines in the previous week,
χ 2
= 1.93, df = 1, p = .59.
Table 22 Diagnostic groups by oral antipsychotic treatment
Schizophrenia
Schizoaffective
Total
None
16 (28.6%)
Oral antipsychotic
FGA
3 (5.4%)
SGA
37 (66.1%)
0 (0%)
16 (20.8%)
4 (19.0%)
7 (9.1%)
17 (81%)
54 (70.1%)
Total
56 (100%)
21 (100%)
77 (100%)
Table 23 Diagnostic groups by mood stabiliser use
Schizophrenia
Mood stabiliser taken
None
45 (80.4%)
Sodium valproate Other Total
7 (12.5%) 4 (7.1%) 56 (100%)
Schizoaffective
Total
5 (23.8%) 14 (66.7%) 2 (9.5%) 21 (100%)
50 (64.9%) 21 (27.3%) 6 (7.8%) 77 (100%)
87
Table 24 Benztropine use by each diagnostic group
Schizophrenia
Schizoaffective
Total
None
51 (91.1%)
18 (85.7%)
69 (89.6%)
Benztropine
5 (8.9%)
3 (14.3%)
8 (10.4%)
Total
56 (100%)
21 (100%)
77 (100%)
The mean CPZE dosages for LAI, oral, and combined antipsychotic medications are
shown in Table 25. The diagnostic groups did not differ significantly in their LAI dosage, but
the schizoaffective diagnosis patients’ oral and combined antipsychotic dosage were both significantly higher than for the schizophrenia diagnosis patients.
Table 25 Mean CPZE dosages for diagnostic groups
LAI dosage CPZE
Oral dosage CPZE
Total dosage CPZE
Diagnostic group
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Mean
285.17
Std.
Deviation
141.66
302.01 t
-.49 p
.62
106.62
236.23 -2.21* .03
Cohen’s d
-.13
264.91
390.48
-.60
551.96
692.49
177.58
305.32 -2.42* .019
189.03
-.55
The means and standard deviations of SWN scores for the diagnostic groups are
shown in Table 26. Independent samples
t -tests revealed that the schizoaffective group had significantly higher scores on positive SWN and social integration. There were also nonsignificant trends for the schizoaffective group to have higher total SWN, mental functioning, and emotional regulation.
88
Table 26 SWN scale scores for diagnostic groups
Total SWN
Negative SWN
Positive SWN
Mental functioning
Self control
Emotional regulation
Social integration
Physical functioning
Diagnostic group
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Schizophrenia
Schizoaffective
Mean
65.02
Std.
Deviation
17.59
73.14 18.20
37.39
37.86
9.71
11.83
24.89
32.19
13.02
15.05
12.75
14.14
13.61
15.71
12.36
15.14
13.29 t
-1.80
.18 p
.08
.86
10.21 -2.84** .006
9.54
4.59
4.57
-1.73 .09
3.99
4.89
4.09
4.78
-1.28
-1.92
.20
.06
4.88 -2.41* .018
3.34
4.39 .17 .86
Cohen’s d
-.45
-.04
-.31
-.47
-.66
-.44
-.66
.04
13.10 4.69
The diagnostic groups did not differ on depression, anxiety or stress. There were no significant between-group differences in any of the PANSS scores, although there was a nonsignificant trend for the schizophrenia group to score higher on negative symptoms. The schizophrenia group scored significantly higher on sexual side-effects. There were no other significant differences in the remaining side-effects scales. The schizophrenia group scored significantly higher on the WTAR estimate of premorbid IQ, but there were no significant differences in the Information estimated or composite premorbid IQ. The schizophrenia
89
group also scored significantly higher on the Attention index, but there were no significant
differences on any of the remaining RBANS indexes. See Appendix G, Table G2 for these
statistics. There were no significant differences between diagnostic groups in ITAQ insight scores, or scores on the ROMI adherence scales. There were no significant between group differences in their BFI personality scores.
Inpatient vs. outpatient status
Independent samples t-tests found no significant differences between inpatients and outpatients on SWN scales, the DASS, side-effects, lifestyle questions, PANSS symptoms, or insight (ITAQ). Inpatients were (unexpectedly) significantly higher on conscientiousness than outpatients ( M = 3.72, SD = .83 vs. M = 2.98, SD = .42), t (75) = 2.15, p = .035. There were no other significant differences on personality traits.
Simple comparisons of LAI medication groups
Dosage
See Table 10 for mean dosages. Independent samples t -tests were used to compare patients in each LAI group on demographic and clinical variables. There were no betweengroup differences in LAI CPZE dosage or in total daily CPZE dosage, although there was a non-significant trend for LAI FGA patients to be on a higher daily oral CPZE dose compared to LAI SGA patients, t (75) = 1.80, p = .06, d = .43.
Durations of treatments
See Table 8 for durations of medication treatment. Patients treated with LAI FGA had been on any antipsychotic medication for more years compared to patients on LAI SGA, t
(63) = 2.53, p = .014, d = .66. Additionally, patients in the FGA group had been on their current LAI medication longer than those in the SGA group, t (51) = 2.43, p = .019, d = .68.
These results are not surprising, given the longer availability of FGA LAI medications.
4
4 LAI FGA were first developed in the 1960s, LAI SGA only became available in the last decade.
90
Number of years on any antipsychotic medication was significantly correlated with age ( r =
.73, p < .001), therefore an ANCOVA was conducted to determine if LAI treatment groups differed on their length of time on any antipsychotic medication when controlling for age.
There was a significant main effect of age, F (1, 61) = 58.23, p < .001, but the main effect of
LAI type did not reach significance, F (1, 61) = 1.79, p = .19. There was a significant interaction between age and LAI type, F (1, 61) = 4.21, p = .045. There was no significant correlation between age and time on current LAI.
Clozapine use and history of ECT
LAI groups were compared to see if there were any differences in clozapine use (ever or planned) as this is usually an indicator of resistance to treatment. There were 7 participants in the FGA LAI group and 5 participants in the SGA LAI group of clozapine use (ever or planned) and a chi-square test indicated that this difference was not significant, χ
2
= .04, df
= 1, p = .83. LAI groups were also compared to see if there were any differences in history of use of ECT, an indicator of illness severity. There were exactly 5 participants in each of the
FGA and SGA LAI groups with a history of ECT use, and a chi-square test indicated that there was no significant difference between groups, χ 2
= .59, df = 1, p = .44.
Demographic differences and symptom profiles
Demographic characteristics of each LAI group are shown in Table 8. Patients treated with LAI SGA had more years of education compared to LAI FGA patients ( t (74) = -2.94, p
= .004, d = .68), and were younger ( t (75) = 2.07, p = .042, d = -.48). Additionally, LAI SGA patients smoked fewer cigarettes per day, reported smoking less cannabis, and were less
likely to have used amphetamines. See Appendix G, Table G3 for these statistics. There were
no between-group differences in gender balance, diagnosis, or personality traits. A chi-square analysis showed that there were no between-group differences in whether patients had ever been married or engaged. The mean scores of patients on the five PANSS factors for each
91
LAI group are shown in Table 27. Independent samples
t -tests revealed that LAI FGA patients scored higher on positive, hostile excitement, and affective symptoms, and on the total score. There were no significant differences on negative symptoms or cognitive/disorganised symptoms.
Table 27 PANSS Factor scores for each LAI group
Positive factor
Negative factor
N Mean
FGA 43 3.11
SGA
Total
FGA
26
68
43
2.38
2.84
1.86
Std.
Deviation Minimum Maximum
1.16 1.00 5.80
.97
1.14
.71
SGA 26 2.13
Total 68 1.96
Cognitive/disorganised FGA 43 2.67
SGA 26 2.54
Hostile Excitement factor
Total 68 2.62
FGA 43 2.08
SGA 26 1.61
Total 68 1.91
Affective factor FGA 43 2.36
PANSS Total
.99
.83
.92
.93
.92
1.05
.70
.96
.80
SGA 26 1.89
Total 68 2.19
.99
.90
FGA 43 72.09 13.99
1.00
1.00
1.00
1.00
1.00
1.00
1.20
1.00
1.00
1.00
1.00
1.00
1.00
1.00
38.00
4.40
5.80
3.88
4.75
4.75
4.80
4.40
4.80
4.25
3.75
4.25
3.75 t p
2.32 .023
.19 -
1.33
.60 .55
2.09 .04
2.69 .009
5.00
5.00
95.00 2.00 .049
SGA 26 64.69 16.27 36.00 94.00
Total 68 69.30 15.20 36.00 95.00
Cohen’s d
.68
-.31
.14
.53
.52
.49
SWN, side-effects, negative affect, insight and neurocognitive test performance
Means scores on the SWN, the LUNSERS, DASS, Insight (ITAQ), premorbid IQ and
the RBANS are shown in Table 28 . Independent samples t-tests found no significant
differences between FGA and LAI SGA patients on any of the SWN scales, the DASS, sideeffects, lifestyle questions, insight, ROMI scales, or measures of premorbid IQ. Members of the FGA LAI group scored significantly and moderately higher on the language scale of the
92
RBANS ( t (67) = 2.34, p = .022). There were no significant differences on any of the other scales or the total RBANS scale.
5
Table 28 Means scores on SWN scales, LUNSERS, DASS and RBANS in each LAI group
SWN Total scale
LAI FGA
67.60 (17.47)
LAI SGA Total
66.67 (19.11) 67.23 (18.01)
Cohen’s d
.05
Negative SWN
Positive SWN
SWN mental functioning
SWN self control
37.19
27.68
13.83
13.23
(10.47)
(10.60)
(4.50)
(4.20)
38.03
25.63
13.17
12.97
10.07
(10.37)
(4.91)
(4.42)
37.52
26.88
13.57
13.13
(10.26)
(10.49)
(4.64)
(4.27)
-.08
.19
.14
.06
SWN emotional regulation
SWN social integration
SWN physical functioning
Total side-effects
Neurological side-effects
(EPS)
14.38
13.34
12.81
31.00
5.74
(4.54)
(4.77)
(4.22)
(19.11)
(4.43)
13.87
12.77
13.90
30.75
4.65
(4.11)
(4.54)
(4.77)
(20.60)
(4.97)
14.18
13.12
13.23
30.91
5.41
(4.36)
(4.66)
(4.44)
(19.55)
(4.67)
.12
.12
-.24
.01
.23
Autonomic side-effects
Psychic side-effects
Sexual side-effects
Red Herrings
Depression
Anxiety
Stress
Insight
Information test IQ estimate
8.59
11.39
3.02
5.87
13.26
12.00
14.65
9.98
95.80
(8.16)
(6.58)
(3.18)
(5.23)
(10.82)
(8.73)
(10.58)
(7.75)
(16.77)
9.71
9.93
3.68
6.14
(9.24)
(6.94)
(3.09)
(5.54)
9.12
10.91
3.32
5.97
(8.53)
(6.69)
(3.15)
(5.35)
12.29 (11.49) 12.89 (11.01)
15.29 (20.51) 13.24 (14.32)
14.14 (11.44) 14.46 (10.84)
9.08 (7.28) 9.65 (7.54)
96.73 (18.76) 96.14 (17.41)
-.13
.22
-.21
-.05
.09
-.21
.05
.12
-.05
*Difference is significant, p < .05
5 Similar results were found when controlling for premorbid IQ using ANCOVA.
93
Table 28 continued
WTAR IQ estimate
Immediate memory
Visuospatial constructional
Language
Attention
Delayed memory
RBANS total scale score
Exercise
Health
Life difficulties
Loneliness
Mental problems
ROMI adherence
ROMI nonadherence
ROMI total
(11.14)
(16.10)
(16.21)
(15.64)
(19.02)
(17.89)
(14.38)
(.98)
(.91)
(.81)
(1.06)
(1.02)
(.42)
(.35)
(.53)
1.14
1.76
1.33
.43
68.55
67.20
1.68
1.85
.91
1.03
93.30
60.09
80.07
86.77
73.41
96.26 (11.12) 94.31 11.14
62.16 (17.67) 60.84 (16.59)
83.08 (20.59) 81.16 (17.83)
77.36 (16.79) 83.36 (16.59)
68.04 (15.36) 71.46 (17.86)
1.00
1.72
1.29
.43
61.80 (18.01) 66.10 (18.10)
64.08 (14.73) 66.07 (14.48)
1.70
1.67
.93
.90
(.92)
(1.06)
(.78)
(.99)
1.69
1.77
.92
.98
(.94)
(.97)
(.79)
(1.02)
(.98)
(.46)
(.36)
(.70)
1.09
1.75
1.32
.43
(.99)
(.43)
(.35)
(.59)
Simple comparisons of oral antipsychotic groups
SWN scores
Because the majority of patients were taking oral antipsychotics in addition to their
LAI medication, comparisons were performed of those taking no oral medication, an FGA, or
.14
.09
.11
.00
.38
.21
-.02
.18
.02
.13
-.27
-.12
-.16
.58*
.31 an SGA. See Table 29 for means and standard deviations. One-way ANOVA showed there was a significant between-group difference for the SWN self-control scale ( F (2, 72) = 3.18, p = .047) and a non-significant trend for the SWN total scale ( F (2, 72) = 2.64, p = .08). The other subscales showed no significant differences. Post Hoc tests using Tukey’s HSD showed there was a marginally non-significant trend ( p = .07) for patients taking no oral medication to have higher self-control than patients taking an SGA. The FGA oral group did not differ significantly from the others. There was also a marginally non-significant trend ( p = .09) for
94
patients taking no oral medication to have higher SWN total score than patients taking an
SGA. The FGA oral group did not differ significantly from the others.
These findings suggest that patients on LAI monotherapy (no oral medication prescribed) had a tendency to be better off than patients prescribed oral SGA on total SWN and the self-control subscale.
Other measures
There were no significant between-group differences in DASS scores, any of the sideeffect scales, or any of the PANSS factors.
Analyses controlling for oral dosage
A series of ANCOVAs were performed using oral CPZE dosage as a covariate. When controlling for oral dosage, oral medication group had no significant effects on any SWN scale, DASS, side-effects scales, or any of the PANSS factors. There was a significant main effect of oral dosage on sexual side-effects ( F (1, 70) = 4.53, p = .037, partial
η 2
= .06). The regression coefficient was in the negative direction (B = -.01) indicating that higher dosages were associated with lower sexual side-effects. There was also a significant main effect of oral dosage on hostile excitement symptoms ( F (1, 65) = 10.27, p = .002, partial
η 2
= .14).
The regression coefficient was in the positive direction (B = .002) indicating that higher dosages were associated with more pronounced hostile excitement. There were no other significant effects of oral dosage on SWN, DASS, other side-effects, or other PANSS scales.
95
Table 29 SWN scale scores of Combined LAI and Oral medication groups
SWN total LAI FGA
No oral
72.90 (15.04)
FGA oral
72.86 (20.38)
LAI SGA
Total
78.17
74.88
(15.38)
(14.89) 72.86 (20.38)
Mental functioning LAI FGA
LAI SGA
Total
14.90
15.00
14.94
(3.99)
(3.80)
(3.79)
15.57
15.57
(4.12)
(4.12)
Self-control
Emotional regulation
Social integration
Physical functioning
Negative SWN
Positive SWN
LAI FGA
LAI SGA
Total
LAI FGA
LAI SGA
Total
LAI FGA
LAI SGA
Total
LAI FGA
LAI SGA
Total
LAI FGA
LAI SGA
Total
LAI FGA
LAI SGA
Total
14.70
15.50
15.00
15.40
15.50
15.44
14.10
13.17
14.94
13.80
15.83
14.56
40.70
45.00
42.31
29.70
29.83
29.75
(2.79)
(4.09)
(3.23)
(3.84)
(3.15)
(3.48)
(5.55)
(4.50)
(4.75)
(4.24)
(3.31)
(3.93)
(10.44)
(4.82)
(8.81)
(8.31)
(11.87)
(9.41)
14.86
14.86
14.71
14.71
13.00
13.00
14.71
14.71
36.57
36.57
32.14
32.14
(4.10)
(4.10)
(5.59)
(5.59)
(5.42)
(5.42)
(3.95)
(3.95)
(9.54)
(9.54)
(10.37)
(10.37)
Comparison of olanzapine, risperidone, and other oral antipsychotics
Patients in the FGA LAI group were more likely to be prescribed oral olanzapine than
12.37
12.33
12.35
13.97
13.46
13.74
13.17
11.88
12.59
12.03
13.42
12.65
36.17
36.30
36.22
25.97
24.58
25.35
SGA oral
64.60 (17.39)
63.79
64.24
(19.12)
(18.01)
13.07
12.71
12.91
(4.68)
(5.11)
(4.83)
(4.20)
(5.00)
(4.58)
(10.76)
(10.34)
(10.48)
(11.20)
(9.96)
(10.59)
(4.47)
(4.36)
(4.38)
(4.60)
(4.27)
(4.42)
(4.50)
(4.48)
(4.49) those in the SGA group, who were more likely to be prescribed oral risperidone. Naber
96
(2001) found that olanzapine had a more beneficial effect on SWN than risperidone.
Therefore, patients were categorised based on whether their oral medication was olanzapine, risperidone, another SGA, an FGA, or none and a one-way ANOVA was performed. No between-group differences approached significance on any SWN scale, or on DASS, sideeffects, or PANSS scores.
Analyses combining LAI and oral medication
A series of two-way ANCOVAs were performed to assess the combined impact of kind of LAI and oral medication on SWN. Total antipsychotic dosage (LAI and oral combined) in daily CPZE units was included as a covariate in all analyses. There were no significant main effects for LAI kind, oral kind, or dosage, and there were no significant interactions for LAI and oral kinds for any SWN scale. See Table 29 for descriptive statistics and Table 30 for ANCOVA results.
97
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Mental functioning
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Self-control
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Emotional regulation
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Social integration
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Table 30 Effects of LAI and oral type on SWN scales
F
SWN total R 2 = .08
.13
R 2 = .09
.07
2.15
.55
.21
R 2 = .04
.05
.33
1.06
.17
R 2 = .07
.13
1.48
.03
1.56
.13
1.70
.85
.54
R 2 = .07
.03
1.27
1.31 p
Adj. R 2 = .02
.72
.19
.36
.47
Adj. R 2 = .00
.86
.29
.26
.72
Adj. R 2 = .02
.78
.12
.46
.65
Adj. R 2 =.03
.82
.72
.31
.68
Adj. R 2 = .00
.72
.23
.87
.22
Partial η 2
.00
.04
.00
.02
.00
.01
.02
.00
.00
.04
.02
.00
.00
.05
.01
.01
.00
.06
.01
.00
98
Table 30 continued.
Physical functioning
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Negative SWN
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
Positive SWN
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Interaction between LAI and oral type
R 2 = .08
1.58
1.62
.93
.17
R 2 = .07
.51
1.30
.14
.57
R 2 = .07
.12
1.26
.91
.24
Adj. R 2 = .02
.21
.21
.34
.68
Adj. R 2 = .00
.48
.28
.71
.45
Adj. R 2 = .00
.73
.29
.34
.62
.00
.03
.01
.00
.01
.04
.00
.01
.02
.04
.01
.00
Comparisons of oral risperidone, olanzapine and other drugs combined with LAI groupings
To compare whether the combination of specific type of oral medication with either an FGA or LAI SGA made a difference to SWN, a series of ANCOVAs were performed, controlling for the total (oral and LAI combined) CPZE dosage. Patients were grouped according to the kind of LAI (FGA vs. SGA) and whether they were taking oral risperidone, olanzapine, another SGA oral, an FGA oral, or no oral medication (monotherapy). The groupings LAI FGA plus oral risperidone and LAI SGA plus another oral SGA were excluded from the analysis due to low numbers of cases (three and two respectively). The
analyses therefore compared seven groupings. See Table 31 for means. None of the main
effects for medication group or dosage were significant (see Table 32 ). However, post hoc
Tukey’s HSD revealed some significant or near-significant between-group differences and
99
many of the effect sizes for specific medication group comparisons were substantial (see
Table 33 for Cohen’s d values). Overall, there was a trend for patients on an LAI SGA combined with oral olanzapine to actually have worse SWN scores than other patient groups on the total SWN score, the two SWN factors and all of the subscales except self-control.
Patients on LAI SGA monotherapy were significantly better off than those on LAI SGA plus olanzapine on total SWN, negative SWN, social integration and physical functioning, and marginally non-significantly better off on two of the other subscales. Patients on LAI FGA plus an FGA oral were significantly better off than those on LAI SGA plus olanzapine on total SWN, positive SWN, mental functioning, emotional regulation, and physical functioning. Patients on LAI FGA monotherapy were significantly better off than those on
LAI SGA plus olanzapine on negative SWN, and marginally non-significantly better off on total SWN. Patients on LAI SGA and risperidone were significantly better off than those on
LAI SGA plus olanzapine on physical functioning, and had a non-significant trend to be better off than those on LAI SGA plus olanzapine on total SWN, negative SWN, and two subscales. Interestingly, patients on LAI FGA plus olanzapine had a non-significant trend to be better off than those on LAI SGA plus olanzapine on total SWN, positive SWN, and emotional regulation.
These medication groupings were also compared on depression, anxiety, and stress, and no differences were significant. See Appendix D, tables D7 and D8 for statistics. In summary patients on LAI SGA plus olanzapine tended to be worse off on most measures than other patient groups, including LAI FGA plus olanzapine. This latter finding suggests the possibility that it may not be olanzapine itself but the combination of olanzapine with an LAI
SGA that is not beneficial to SWN. Due to the small and unequal group sizes and the nonsignificant main effects, these results need to be treated with caution.
100
Table 31 SWN scale scores for combined oral and LAI medication groupings.
LAI FGA only LAI FGA & olanzapine
LAI FGA & other SGA
LAI FGA &
FGA oral
LAI SGA only
N
SWN Total
Mental
Physical
Functioning
Social
10 16 11 7
M SD M SD M SD M SD M
72.9 (15.0) 64.5 (17.7) 63.7 (18.2) 72.9 (20.4) 78.2
14.9 (3.99) 12.3 (4.64) 13.9 (4.87) 15.6 (4.12) 15.0
Functioning
Self Control 14.70 (2.79) 12.3 (4.61) 11.8 (4.40) 14.9 (4.10) 15.5
Emotional
Regulation
15.40 (3.84) 13.8 (4.92) 14.4 (4.23) 14.7 (5.59) 15.5
13.80 (4.24) 12.4 (4.66) 11.1 (3.81) 14.7 (3.95) 15.8
14.10 (5.55) 13.8 (4.25) 12.6 (5.41) 13.0 (5.41) 16.3
6
SD
(15.4)
(3.80)
(4.09)
(3.15)
(3.31)
(2.87)
Integration
Negative 40.70 (10.4) 35.7 (10.1) 34.3 (12.0) 36.6 (9.54) 45.0 (4.81)
SWN
Positive SWN 27.47 (3.91) 27.7 (2.86) 27.28 (3.21) 33.60 (4.18) 27.96 (4.61)
LAI SGA & risperidone
16
M
67.1
13.75
SD
(18.5)
(4.39)
M
50.3
9.17
LAI SGA & olanzapine
6
SD
(15.0)
(5.64)
12.94
14.19
(4.74)
(4.10)
11.5
10.0
(2.43)
(2.76)
14.31 (4.50) 9.33 (4.55)
11.88 (4.82) 10.33 (2.88)
38.56 (8.96) 29.17 (11.87)
25.33 (2.62) 19.54 (4.23)
101
Table 32 SWN scales as a function of combined LAI and specific oral medications
F p
SWN total R 2 = .15 Adj. R 2 = .05
Total dosage converted into CPZE
Medication grouping
Mental functioning
Total dosage converted into CPZE
Medication grouping
Self-control
Total dosage converted into CPZE
Medication grouping
Emotional regulation
Total dosage converted into CPZE
Medication grouping
Social integration
Total dosage converted into CPZE
Medication grouping
Physical functioning
Total dosage converted into CPZE
Medication grouping
SWN negative factor
Total dosage converted into CPZE
Medication grouping
SWN positive factor
Total dosage converted into CPZE
Medication grouping
.62
1.33
R 2 = .14
.75
.98
R 2 = .10
.00
1.03
R 2 = .17
.37
1.73
R 2 = .14
.02
1.31
R 2 = .13
1.42
1.22
1.38
R 2 = .11
.44
.83
R 2 = .12
1.07
.44
.26
Adj. R 2 = .05
.39
.24
Adj. R 2 = .01
.51
.55
Adj. R 2 = .02
.30
.45
Adj. R 2 = .00
.99
.42
Adj. R 2 = .08
.55
.13
Adj. R 2 = .04
.88
.26
Adj. R 2 = .01
.24
.31
Partial η 2
.00
.11
.01
.14
.02
.11
.00
.09
.02
.08
.01
.11
.01
.07
.01
.12
102
Table 33 Pairwise comparison of estimated marginal means of medication groupings (Results for Self-control subscale are not shown)
SWN total p
Cohen’s d
LAI SGA & olanzapine
LAI FGA only
Mean difference
-19.10 .06 -1.51
LAI FGA & olanzapine
LAI FGA & other SGA
LAI FGA & FGA oral
LAI SGA only
-15.02 .08
-13.52 .14
-23.67* .02
-24.81* .026
-.87
-.80
-1.26
-1.84
LAI SGA & risperidone -15.75 .07 -1.00
Mental functioning
LAI SGA & olanzapine
LAI FGA only -4.75 .07 -1.17
LAI FGA & olanzapine -3.39 .13 -.61
LAI FGA & other SGA -4.78* .04 -.90
LAI FGA & FGA oral
LAI SGA only
LAI SGA & risperidone
-6.73*
-4.97
-4.31
.01
.08
.053
-1.30
-1.21
-.91
Emotional regulation
LAI SGA & olanzapine
LAI FGA only
LAI FGA & olanzapine
LAI FGA & other SGA
LAI FGA & FGA oral
Social integration
LAI SGA only
LAI SGA & risperidone
LAI SGA only
LAI SGA & risperidone
LAI SGA & olanzapine
-4.28
-4.09
-4.40*
-5.08*
-4.53
-3.87
4.45
5.98*
.09
.053
.048
.039
.09
.07
.07
.046
-1.61
-.95
-1.23
-1.07
-1.86
-1.20
1.11
2.08
103
Table 33 continued
Physical functioning
LAI SGA & olanzapine
Negative SWN
LAI SGA & olanzapine
Positive SWN
LAI SGA & olanzapine
LAI FGA only
LAI FGA & olanzapine
LAI FGA & other SGA
LAI FGA & FGA oral
LAI SGA only
LAI SGA & risperidone
LAI FGA only
LAI FGA & olanzapine
LAI FGA & other SGA
LAI FGA & FGA oral
LAI SGA only
LAI SGA & risperidone
LAI FGA only
LAI FGA & olanzapine
LAI FGA & other SGA
LAI FGA & FGA oral
LAI SGA only
LAI SGA & risperidone
-3.81
-3.20
-1.78
-5.60*
-5.93*
-4.80*
-11.92* .044
-6.36 .20
-5.09
-7.28
.33
.21
-16.17* .012
-9.51 .056
-9.40 .14
-8.13
-9.79
.11
.08
-14.06* .02
-9.98 .14
-7.31 .17
.13
.13
.42
.024
.029
.024
Comparison of LAI groups controlling for affective symptoms
Patients in the LAI FGA group differed from those in the LAI SGA group on a
-1.50
-.94
-.94
-1.48
-1.21
-.86
-1.03
-.59
-.43
-.69
-1.75
-.89
-1.02
-.67
-.42
-1.26
-1.63
-1.10 number of variables, but most of these did not significantly correlate with any SWN scale.
Affective symptoms correlated with all SWN scales. Therefore, a series of ANCOVAs were performed to control for affective symptoms and test for possible interactions between
affective symptoms and LAI group. See Table 34 for results. The ratio of residual variances
104
in the two groups was .65, which is slightly below the cut-off value of .67 indicating a violation of homogeneity assumptions (DeShon & Alexander, 1996). There were no significant main effects of LAI group, although there were marginally non-significant trends
( p = .07) for patients in the LAI FGA group to have higher scores on negative SWN and emotional regulation, contrary to expectations (see Tables 35 – 36 for estimated marginal means). There were no significant main effects of kind of oral antipsychotic, or of combined antipsychotic dosage. However, a post hoc test LSD for negative SWN showed that patients not receiving oral medication had higher scores (hence better SWN) than patients taking an
SGA oral. See Table 36 for estimated marginal means. (The score for FGA oral patients was only slightly higher compared to SGA oral patients but did not significantly differ from patients on no oral, probably due to the low number of patients involved.) There were significant main effects of the affective factor for every SWN scale, indicating that more affective symptoms were associated with worse SWN. There were significant interactions between LAI group and the affective factor for negative SWN and emotional regulation. The interaction shown in Figure 2 suggests that patients in the FGA group who were one standard deviation below the mean in affective symptoms were substantially higher in negative SWN than LAI SGA patients who were also one standard deviation below the mean in affective symptoms. Conversely, patients in the FGA group who were one standard deviation above the mean tended to be lower in negative SWN than SGA group patients who were also one standard deviation above the mean. The interaction shown in Figures 3 suggests that patients in the FGA group who were one standard deviation below the mean in affective symptoms were substantially higher in emotional regulation scores compared to their SGA group counterparts. There is a slightly opposite trend for those who are one standard deviation above the mean. Both negative SWN and emotional regulation appear to have a stronger relationship with affective symptoms in the FGA group than in the SGA group. This indicates
105
that those who were low in affective symptoms tended to score more favourably on negative
SWN and emotional regulation if they were receiving FGA rather than SGA LAI treatment.
Table 34 SWN scores as a function of Affective symptoms and antipsychotic medications
F p Partial η 2
SWN total R
2
= .37 Adj. R
2
= .31
LAI type
Oral antipsychotic type
1.97
1.48
.17
.24
.03
.04
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
Negative SWN
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
28.24***
.36
2.80
.52
1.59
<.001
.55
.10
R 2 = .35 Adj. R 2 = .30
.47
.21
.29
.01
.04
.01
.04
.25
.00
.09
Positive SWN
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
23.01***
.02
<.001
.90
7.10* .01
R
2
= .24 Adj. R
2
= .17
3.34 .07
.98
15.55***
.56
.32
.38
<.001
.46
.58
.05
.03
.18
.01
.00
106
Table 34 continued
Mental functioning
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
Self-control
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
Emotional regulation
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
Social integration
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
R
2
= .26 Adj. R
2
= .20
2.15 .10
1.12
15.66***
.33
<.001
.87 .35
2.00 .16
R 2 = .31 Adj. R 2 = .25
1.66 .20
1.86
22.64***
.16
<.001
.28 .60
.16 .69
R
2
= .08 Adj. R
2
= .02
3.42 .07
.25 .78
27.32***
.51
<.001
.48
9.99** .002
R 2 = .21 Adj. R 2 = .14
1.58 .21
1.36
12.14**
.45
1.84
.26
.001
.51
.18
.05
.01
.28
.01
.13
.02
.04
.15
.01
.03
.01
.03
.02
.03
.03
.18
.05
.24
.00
.00
107
Table 34 continued
Physical functioning
LAI type
Oral antipsychotic type
Affective factor
Total dosage converted into CPZE
Interaction between LAI and affective factor
R
2
= .17 Adj. R
2
= .10
.21 .65
1.33
7.78*
.27
.01
.67
.02
.42
.89
Table 35 Estimated Marginal means of negative SWN and emotional regulation
Negative SWN
LAI FGA
34.60
LAI SGA
29.79
Emotional regulation 15.48 13.78
Table 36 Estimated Marginal means of negative SWN for oral medication groups
Negative SWN
No oral
42.30
a
FGA oral
37.08
ab
Means with superscripts that differ are significantly different
SGA oral
37.00
b
.00
.04
.10
.01
.00
108
Figure 2. Interaction between Affective Symptoms and LAI group for Negative SWN
Figure 3. Interaction between Affective Symptoms and LAI group for Emotional Regulation
Comparison of LAI groups controlling for DASS scores
The LAI groups did not differ on DASS scores even though the DASS and affective symptoms assess highly overlapping constructs and are moderately strongly correlated (see
109
Appendix F, Table F11 for correlations). To assess whether there were any interactions between LAI group and DASS scores, a variable called ‘Negative affect’ was created by combining the scores for the three DASS scales. ANCOVAs were conducted similar to those used to assess affective symptoms, but using negative affect as a covariate. Although negative affect had a significant main effect on all SWN scales, there were no significant interactions with LAI group.
Comparison of LAI groups controlling for RBANS Language
The Language scale of the RBANS significantly correlated with total SWN, positive
SWN, and self-control. Therefore, a series of ANCOVAs were performed to control for language scores and test for possible interactions between language and LAI group. The ratio of residual variances in the two groups was .87, within the range of values between .67 and
1.5 that do not violate homogeneity assumptions (DeShon & Alexander, 1996). Results for all three of these scales revealed no significant main effects for LAI or oral group, combined
dosage, or language. There were no significant interactions. See Appendix G for statistics.
Adjunctive medications that could influence SWN
Antidepressant medications
A number of patients were taking antidepressants, mood stabilisers, antiparkinson medication, or benzodiazepines. Independent samples t -tests revealed that patients on antidepressants were significantly much lower on all SWN scales than other patients. See
Table 37.
110
Table 37 Mean differences in SWN for patients on antidepressants vs. others
Scale Mean (Std. D.)
SWN Total
Antidepressant
46.67 (9.91)
Others
68.97 (17.49) t
3.07
Negative SWN
Positive SWN
Mental Functioning
Self Control
Emotional Regulation
Social Integration
Physical Functioning
28.00 (9.27)
19.83 (7.94)
9.33 (2.33)
9.17 (2.40)
10.67 (2.73)
8.83 (4.36)
8.67 (3.93)
38.32 (9.98)
27.73 (10.28)
13.93 (4.62)
13.46 (4.23)
14.48 (4.35)
13.48 (4.53)
13.62 (4.29)
2.44
2.53
2.40
2.45
2.10
2.42
2.73 p
.003
.017
.014
.019
.017
.039
.018
.008 d
.55
.57
.48
.56
.63
.71
.56
.58
Additionally, they were significantly higher on depression, and anxiety, and nonsignificantly higher on stress, significantly higher on affective symptoms, and significantly lower on excitement symptoms. They did not differ on positive, negative, cognitive/disorganised symptoms, or on the total PANSS score. Patients taking antidepressants scored significantly higher on psychic side-effects, and marginally higher on sexual side-effects and total side-effects. There were no significant differences on the neurological and autonomic side-effects. See Appendix D for details of the statistics.
Mood stabilisers
The majority of patients who were taking mood stabilisers were prescribed sodium valproate ( n = 21), whereas only six patients were taking other mood stabilisers, mainly lithium carbonate. To examine effects of taking a mood stabiliser on SWN an ANOVA was conducted comparing patients taking sodium valproate, a different mood stabiliser, or none.
See Table 38. There were significant main effects for the emotional regulation and social integration subscales, and a marginally non-significant trend for positive SWN. The main
111
effect for total SWN did not quite reach significance. Post hoc tests using Tukey’s HSD revealed that patients taking sodium valproate scored significantly higher than patients not taking a mood stabiliser on emotional regulation ( p= .013), on social integration ( p= .036), and were marginally higher on positive SWN ( p= .051) and SWN total score ( p= .08). There were no significant effects for the other mood stabilisers. There were no significant differences in PANSS, DASS, or LUNSERS scores between mood stabiliser groups (all F <
1.0).
Antiparkinson medication
Regarding antiparkinson medication (benztropine in every case), independent samples t -tests revealed no significant differences on any SWN scale between those taking or not taking this agent. There were no significant differences in DASS scores, although there was a trend for patients taking benztropine to be higher on stress ( M = 21.25, SD = 10.19 vs. M =
13.64, SD = 10.69, t (72) = -1.91, p = .06, d = .73). Benztropine patients also scored significantly higher on the affective factor ( M = 2.90, SD = .92 vs. M = 2.18, SD = .74, t (72)
= -2.54, p = .013, d = .86), but did not differ from other patients on any of the other PANSS factors. They were non-significantly higher on psychic side-effects ( M = 14.75, SD = 7.17 vs. M = 10.36, SD = 6.55, t (72) = -1.77, p = .08, d = .63) and did not significantly differ on any of the other side-effect scales.
112
Table 38 Mean differences in SWN as a function of mood stabiliser use
Scale Mean (Std. D.)
SWN Total
No mood stabiliser
64.74 (17.84)
Sodium valproate
74.67 (13.10)
Other mood stabiliser
62.00 (28.22)
Negative SWN
Positive SWN
36.66 (10.32)
25.24 (10.34)
40.29 (9.46)
31.57 (7.90)
35.00 (12.23)
24.17 (15.72)
Mental
Functioning
Self Control
12.88 (4.57) 15.38 (3.63) 13.00 (7.13)
12.96 (4.03)
13.30 (4.230
14.00 (4.43)
16.48 (3.06)
11.50 (5.72)
13.50 (6.72) Emotional
Regulation
Social
Integration
Physical
Functioning
12.32 (4.90)
13.28 (4.52)
15.29 (3.09)
13.52 (4.12)
12.17 (5.420
11.83 (5.42)
F (2, 74) p
2.63
1.12
3.07
2.27
.91
4.36
3.32
.34
.41
.016
.042
.71
.08
.33
.052
.11
Benzodiazepines
Furthermore, independent samples t -tests revealed no significant differences on any
SWN scale between those who had taken a benzodiazepine in the week prior to assessment.
There was also no significant correlation between number of times a benzodiazepine had been taken in the prior week and SWN (all rvalues < .07).
Analyses incorporating adjunctive medications with LAI and oral medications
A series of three-way ANCOVAs were performed to assess the impact of mood stabiliser use combined with kind of LAI and oral medication on SWN. Combined LAI and oral dosage in daily CPZE units was included as a covariate in all analyses. No interactions were included in the analyses.
6
Patients were categorised as taking either no mood stabiliser, sodium valproate, or another mood stabiliser. See Tables 39 – 40. There were no significant
6 Analyses containing LAI x mood stabiliser interaction terms were conducted and none of the interactions were significant.
113
main effects for LAI kind, oral kind, or antipsychotic dosage for any SWN scale. However, there were significant main effects for mood stabiliser use for the total SWN scale, the mental functioning, emotional regulation, and social integration subscales, and positive SWN.
Results for the self-control and physical functioning subscales, and negative SWN were not significant. In every case where there was a significant main effect for mood stabiliser, post hoc Tukey’s HSD tests showed that there was a significant difference favouring users of sodium valproate over those not taking a mood stabiliser. No other contrasts were significant.
Table 39 SWN scales as a function of mood stabiliser use, and LAI and oral medication
F p Partial η 2
SWN total R 2 = .16 Adj. R 2 = .09
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
Mental functioning
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
Self-control
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
1.76
1.01
3.12*
R 2 = .11
.00
2.31
.27
1.06
.02
2.31
.41
3.59*
R 2 = .14
.32
.90
.11
.53
.033
Adj. R 2 = .07
.57
.18
.32
.05
Adj. R 2 = .04
.99
.11
.60
.35
.00
.06
.00
.03
.01
.05
.01
.08
.00
.06
.01
.09
114
Table 39 continued
Emotional regulation
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
Social integration
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
Physical functioning
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
SWN negative factor
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
SWN positive factor
LAI type
Oral antipsychotic type
Total dosage converted into CPZE
Mood stabiliser use
.24
.42
.85
Adj. R 2 = .03
.75
.18
.92
.20
Adj. R 2 = .09
.48
.15
.45
.03
Adj. R 2 = .10
.49
.43
.41
.01
Adj. R 2 = .09
.62
.09
.54
.01
Adj. R 2 = .00
.23
1.45
.66
.16
R 2 = .10
.10
1.75
.01
1.67
R 2 = .16
.51
1.97
.59
3.87
R 2 = .17
.49
.86
.68
5.37**
R 2 = .16
.24
2.54
.38
4.71**
R 2 = .08
1.50
.01
.02
.01
.13
.00
.07
.01
.12
.02
.04
.01
.01
.00
.05
.00
.05
.01
.05
.01
.10
115
Table 40 Estimated Marginal Means for Mood stabiliser use controlling for LAI and oral medication and dosage
SWN Total**
No Mood stabiliser
67.42
a
Sodium Valproate
79.65
b
Other mood stabiliser
69.90
ab
13.53
a 16.50
b
Mental Functioning*
13.69
a 15.24
a
Self Control
13.53
a 17.15
b
Emotional Regulation **
14.17
a 14.64
a
Physical Functioning
12.50
a 16.13
b
Social Integration**
37.35
a 42.22
a
Negative SWN
26.77
a 34.19
b
Positive SWN **
* p < .05 ** p < .01 Means with different superscripts are significantly different
14.99
ab
13.41
a
14.78
13.54
13.18
37.71
28.625
ab a ab a ab
Analyses controlling for other adjunctive medications
A further ANCOVA was conducted to assess the effects of mood stabiliser use when controlling for other adjunctive medications, as well as antipsychotics. Antidepressant, benztropine, and benzodiazepine use were added into the analysis. Benzodiazepine use was coded dichotomously to indicate whether these had been used or not during the previous week. An additional covariate was the number of medications taken by a patient in the previous week in addition to their LAI. Results for mood stabiliser use were similar to those in the previous analysis in that sodium valproate showed a significant advantage compared to no mood stabiliser use. Antidepressant use was non-significant ( p = .09). Benztropine and benzodiazepine use did not approach significance (F-values < 1.00). Benztropine and benzodiazepine use were not considered in subsequent analyses due to the low probability of their being associated with significant effects. Antidepressant use was also not considered in subsequent analyses due to the low number of patients (six) using these agents, and therefore results would be lacking generalisability.
Analyses controlling for diagnosis in relation to mood stabiliser use
Patients diagnosed with schizoaffective disorder were significantly more like to be prescribed sodium valproate than people with schizophrenia. Therefore, a series of four-way
116
ANCOVAs were conducted to test whether the effects of mood stabiliser remained significant when controlling for diagnosis. Patients taking mood stabilisers other than sodium valproate were excluded, because the five cases in this category were split across the two diagnostic groups and hence the subsample was too small to analyse meaningfully. This exclusion left 71 cases in the analyses. See Table 41.
Table 41 SWN as a function of medication group, mood stabiliser use and diagnosis
SWN total
F p
R 2 = .21 Adj. R 2 = .14
Partial η 2
LAI type
Oral antipsychotic type
Mood stabiliser
Diagnostic group
Total dosage converted into CPZE
Positive SWN
LAI type
Oral antipsychotic type
Mood stabiliser
Diagnostic group
Total dosage converted into CPZE
.07
2.87
2.24
2.28
.79
.06
.14
.14
.26 .61
R
2
= .21 Adj. R
2
= .12
.18 .67
1.93
.82
3.84
.69
.15
.45
.054
.41
.00
.05
.02
.05
.01
.00
.08
.03
.03
.00
117
Table 41 continued
Mental functioning
LAI type
Oral antipsychotic type
Mood stabiliser
Diagnostic group
Total dosage converted into CPZE
Emotional regulation
LAI type
Oral antipsychotic type
Mood stabiliser
Diagnostic group
Total dosage converted into CPZE
Social integration
LAI type
Oral antipsychotic type
Mood stabiliser
Diagnostic group
Total dosage converted into CPZE
R
2
= .19 Adj. R
2
= .11
.71 .40
1.88
2.08
.53
.16
.16
.47
1.72 .19
R 2 = .23 Adj. R 2 = .15
1.24 .27
1.14
4.69
.33
.034
.58 .45
1.65 .20
R
2
= .20 Adj. R
2
= .13
.07 .79
3.24
2.55
.32
2.73
.046
.12
.57
.10
Users of sodium valproate had significantly higher emotional regulation scores
(estimated marginal mean difference 2.72, p = .034), but there were no significant effects for mood stabiliser use in any of the other SWN scales. Patients in the schizoaffective group showed a marginally non-significant trend to have higher positive SWN (estimated marginal mean difference 6.38, p = .054), and there were no other significant differences between diagnostic groups in any other SWN scales. There was a significant main effect for oral medication type for social integration, as well as a non-significant trend for SWN total score.
Pairwise comparison showed that patients taking an SGA oral had significantly lower scores
118
.01
.03
.02
.01
.06
.03
.03
.07
.01
.03
.00
.09
.04
.01
.04
on both of these scales. See Table 42 for estimated marginal means. There were no significant
effects for LAI group or CPZE dosage.
Table 42 Estimated Marginal Means for oral antipsychotic medication use
SWN Total*
No oral antipsychotic
80.48
a
FGA oral
74.47
ab
17.45
a 12.82
ab
Social Integration**
* p < .05 ** p < ..01 Means with different superscripts are significantly different
SGA oral
67.50
b
13.34
b
In summary, regarding LAI treatment, no differences were found between FGA and
SGA medications on any aspect of subjective well-being. Regarding oral antipsychotics, patients on SGA tended to report worse total subjective well-being and social integration compared to patients taking no oral medication. Sodium valproate use was associated with better emotional regulation compared to no mood stabiliser use. When controlling for use of these medications, patients diagnosed with schizoaffective disorder showed a marginal trend to experience higher positive SWN than patients diagnosed with schizophrenia, but did not differ on any of the other SWN scales.
Personality, DASS and SWN
Regression analyses were performed to assess the relationships between personality traits and SWN and the relationships between DASS factors and SWN. In order to estimate effect sizes, the f
2 statistic was computed for individual predictors from the semi-partial correlation (sr 2 ) . See Method section for effect size descriptors.
Personality predictors of SWN
The total SWN scale, factor scales, and the subscales all had many significant correlations with the big five personality traits. Regression analyses were performed to assess which personality factors remained significant independent predictors when controlling for
119
the remaining personality factors. Only personality factors significantly correlated with each scale were entered as predictors into each model. Extraversion, agreeableness, and neuroticism were significant predictors of total SWN. Effect sizes were small to medium. For negative SWN, the only significant predictor was neuroticism. For positive SWN, the only significant predictors were extraversion and agreeableness. For mental functioning the only significant predictor was neuroticism, although openness to experience approached significance ( p = .06). The significant predictors of self-control were extraversion, agreeableness, and neuroticism. The significant predictors of emotional regulation were extraversion and agreeableness, although openness to experience approached significance ( p
= .056). None of the personality traits significantly predicted social integration although extraversion approached significance ( p = .056) and the overall model was significant. None of the personality traits significantly predicted physical functioning even though the overall model was significant. See Table 43 for regression statistics.
120
Table 43 Personality predictors of total SWN, factor scales and subscales
B β sr
2
Total SWN R 2 = .48 Adj. R 2 = .44 p < .001
Extraversion 5.87* .29 .04
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Negative SWN
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Positive SWN
6.59*
-.24
-6.40**
.84
R 2 = .27
2.22
1.18
1.05
-4.92**
.53
R 2 = .49
.27
-.01
-.30
.04
Adj. R 2 = .22
.19
.09
.09
-.40
.04
Adj. R 2 = .45
.04
.00
.05
.00 p < .001
.00
.00
.00
.03
.00 p < .001
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Mental Functioning
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
* p < .05 ** p < .01 ^ p < .10
3.34*
4.83**
.73
-1.94
1.21
R 2 = .36
.77
.55
-.14
-1.96**
1.15^
.30
.33
.06
-.16
.10
Adj. R 2 = .31
.15
.09
-.03
-.35
.21 p < .001
.01
.01
.00
.07
.03
.04
.07
.00
.01
.01 f 2
.08
.14
.00
.02
.02
.02
.02
.00
.11
.05
.08
.08
.00
.10
.00
.00
.00
.00
.04
.00
121
Table 43 continued
Self-Control
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Emotional Regulation
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Social Integration
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Physical Functioning
Extraversion
Agreeableness
Conscientiousness
Neuroticism
1.53**
1.68*
.12
-.69
.99^
R 2 = .26
1.34^
1.36^
-.18
-1.11
R 2 = .16
.60
1.29
.10
-.81
R 2 = .44
1.19*
1.61*
-.29
-1.79**
-.05
R 2 = .44
Adj. R 2 = .40
.25
.28
-.06
-.35
-.01
Adj. R 2 = .40
.31
.28
.02
-.13
.19
Adj. R 2 = .22
.26
.21
-.03
-.20
Adj. R 2 = .11
.12
.21
.02
-.15 p < .001
.03
.05
.00
.07
.00 p < .001
.05
.05
.00
.01
.03 p < .001
.04
.03
.00
.03 p < .014
.01
.03
.00
.01
.05
.09
.00
.13
.00
.09
.09
.00
.02
.05
.05
.04
.00
.04
.01
.04
.00
.01
DASS predictors of SWN
Depression, anxiety and stress were very highly intercorrelated (all r -values > .70, see
Appendix F). Regression analyses were performed to determine if any of these would remain independent predictors of total SWN, the factor scales, and the subscales when controlling for
the others. See Table 44 . Depression was the only significant predictor for each of these
122
scales. Anxiety approached significance ( p = .056) only in relation to the self-control scale.
Stress did not approach significance for any scale.
Table 44 DASS predictors of total SWN, factor scales and subscales
B β
Total SWN R 2 = .52 Adj. R 2 = .50
Depression -1.16*** -.73
Anxiety
Stress
Negative SWN
Depression
Anxiety
Stress
Positive SWN
Depression
Anxiety
Stress
Mental Functioning
-.24
.21
R 2 = .55
-.61***
-.03
-.06
R 2 = .22
-.49**
-.20
.24
R 2 = .37
-.13
.13
Adj. R 2 = .53
.67
.02
.07
Adj. R 2 = .18
-.51
-.17
.24
Adj. R 2 = .34
Depression
Anxiety
Stress
Self-Control
Depression
Anxiety
Stress
* p < .05 ** p < .01 *** p < .001
-.23**
-.06
.03
R 2 = .40
-.23**
-.15^
.11
-.57
-.12
.07
Adj. R 2 = .37
-.57
-.33
.27 sr 2 p < .001
.17
.01
.00 p < .001
.14
.00
.00 p < .001
.08
.01
.01 p < .001
.10
.00
.00 p < .001
.10
.03
.02 f
2
.16
.00
.00
.17
.05
.03
.35
.02
.00
.31
.00
.00
.10
.01
.01
123
Table 44 continued
Emotional Regulation
Depression
Anxiety
Stress
Social Integration
Depression
Anxiety
Stress
Physical Functioning
Depression
Anxiety
Stress
R 2 = .40
-.30***
-.03
.09
R 2 = .35
-.23**
.06
-.07
R 2 = .21
-.18*
-.06
.05
Adj. R 2 = .38
-.76
-.07
.23
Adj. R 2 = .32
-.54
.12
-.13
Adj. R 2 = .17
-.45
-.13
.12 p < .001
.19
.00
.01 p < .001
.10
.00
.01 p = .001
.07
.01
.00
Mediation analysis
A mediation analysis was performed to test the possibility that the relationship
.09
.01
.00
.15
.00
.02
.32
.00
.02 between personality and SWN was mediated by depression. Results of regression analysis showed that when all five personality factors were entered simultaneously as predictors of depression, only neuroticism was significant. See Table 45. Therefore, neuroticism was used as the independent variable in mediation analysis.
124
Table 45 Big five predictors of depression
R 2 = .32
Extraversion
Agreeableness
B
-2.20
-1.21
Conscientiousness
Neuroticism
Openness to experience
-.72
4.50**
-.50
Adj. R 2 = .29
β
-.18
-.08
-.06
.35
-.04 p < .001 sr 2
.02
.00
.00
.07
.00 f 2
.03
.00
.00
.10
.00
** p < .01
Mediation results are shown in Table 46. Neuroticism and depression separately were significant predictors of SWN, and neuroticism was a significant predictor of depression.
Effect sizes were large to very large. When neuroticism and depression were entered together, both remained significant predictors of SWN. The relationship between neuroticism and SWN decreased from large to medium size after statistically controlling for depression.
The effect size of depression decreased but remained large. Results of Sobel’s test (Sobel statistic = -4.42, SE = 1.75, p < .001) showed that depression was a significant mediator of neuroticism. Therefore, the results are consistent with partial mediation. This indicates that depression only partially explains the relationship between neuroticism and SWN.
Neuroticism retains some direct influence on SWN when controlling for depression, as well as having an indirect effect mediated by depression. Figure 4 illustrates the mediation relationship.
125
Figure 4. Mediation of the relationship between Neuroticism and SWN by depression
Depression
.52***
-.31**
-.53***
Neuroticism
Neuroticism and depression as predictors of SWN
R 2 = .55
Neuroticism
B
-6.75**
Depression .89***
** p < .01 *** p < .001
Adj. R 2 = .54
β
-.31
-.53
Table 46 Test of mediation of influence of neuroticism on SWN by depression
Neuroticism as a predictor of depression
R 2 = .27 Adj. R 2 = .26 p < .001
Neuroticism
B
6.71***
β
.52 sr 2
.27
Neuroticism as a predictor of SWN
R 2 = .34
Neuroticism
B
-12.69***
Adj. R 2 = .34
β
.59 p < .001 sr 2
.34
Depression as a predictor of SWN
R 2 = .48
Depression
B
-1.15***
Adj. R 2 = .47
β
-.69 p < .001 sr 2
.48 p < .001 sr 2
.07
.21 f 2
.43 f 2
.52 f 2
.16
.47 f 2
.92
SWN
126
Comparison of LAI Groups controlling for personality, depression and other covariates
A series of analyses were performed to determine the main predictors of SWN scale scores (total, factor scales, and subscales) when controlling for LAI and oral antipsychotic medications. Analyses were conducted using imputation of missing data, and also with deletion of cases with missing data. Except where otherwise noted, results from the two methods were highly similar. Therefore, results using the latter method are presented here.
Results using the imputation method are shown in Appendix I for comparison.
ANCOVA examining Total SWN
To determine the main predictors of SWN total score a series of ANCOVAs were performed with LAI and oral medication groups as the between-group factors with total combined dosage as a covariate. Extraversion, agreeableness, neuroticism, and depression had previously been identified as significant predictors in regression analyses. Additionally, cognitive/disorganised and affective symptoms, side-effects, lifestyle questions, mood stabiliser use and diagnosis were entered. ROMI adherence was entered because poor adherence to oral medication is a potential confounding factor in assessing any medication effects, and an adherence scale might help control for this factor. Because entering total sideeffects and the side-effects subscales in the same analysis could create multicollinearity problems, two analyses were performed, one containing the total scale, the other used the subscales, and the results compared. In all analyses, the significant covariate predictors were extraversion, agreeableness, depression, health, and cognitive/disorganised symptoms.
Neuroticism did not approach significance in any analysis, most likely because of the inclusion of depression and highly correlated personality variables. Neither diagnosis nor mood stabiliser use approached significance. See Appendix H for details of these analyses.
The analysis was re-performed using only extraversion, agreeableness, health, depression, and cognitive/disorganised symptoms, as covariates. All of these covariates remained
127
significant. There were no significant main effects for LAI or oral medication groups nor was the interaction between LAI and oral medication significant. See Table 47. The total amount of variance explained by this model (73%) was extremely large.
Table 47 SWN as a function of medication groupings, personality, depression and other covariates
Extraversion
Agreeableness
Depression
Health
Cognitive/disorganised symptoms
Long acting injectable type
Oral antipsychotic type
R 2 = .77
F
9.78**
9.09**
21.03***
15.42***
5.93*
1.16
1.35 p
.003
.004
<.001
<.001
.018
.29
.27
.96
Adj. R 2 = .73
Partial η 2
.14
.13
.26
.21
.09
.02
.04
.00 Interaction between long acting injectable and oral type
Analysis with deletion of cases with missing data (n = 69)
.00
Multivariate analysis of LAI groups: factor scales and subscales
In order to identify the significant multivariate predictors of the SWN factors and subscales, a series of MANCOVAs were conducted. The first series used the positive and negative SWN factors as dependent variables; the second series used the SWN subscales.
Combining two or more dependent variables in MANCOVA analyses reduces the probability of Type I errors related to multiple significance tests (Tabachnick & Fidell, 2001). LAI and oral medication groups were between-group factors and combined medication dosage was entered as a covariate. Interaction terms were not considered as all previous analyses had failed to find any significant interactions between LAI and oral medication groups.
Additional covariates were selected from variables significantly correlated with the SWN scales.
128
Predictors of Negative and positive SWN
Extraversion, agreeableness, neuroticism, and depression had previously been identified as significant predictors in regression analyses. Additionally, cognitive/disorganised and affective symptoms, side-effects, lifestyle questions including self-assessed health, mood stabiliser use and diagnosis were entered. ROMI adherence was entered because it was significantly correlated with negative SWN and because it was thought it might be a predictor of poor adherence to oral medication. Two analyses were performed to avoid creating multicollinearity problems, one containing the total side-effects scale, the other the subscales, and the results compared. Agreeableness, depression, and health were significant multivariate predictors, and extraversion closely approached significance. Total side-effects significantly predicted negative SWN. None of the sideeffects scales approached significance in any analysis. See Appendix H for details of these analyses. The analysis was performed again with extraversion, agreeableness, depression, health, and total side-effects as covariates. See Table 48. All covariates except side-effects were significant multivariate predictors. There were no significant multivariate effects of LAI or oral medication group. Tests of between-subjects effects showed that negative SWN and positive SWN had different significant predictors. See Table 49. Depression and total sideeffects were significant predictors of negative SWN. The significant predictors of positive
SWN were extraversion, agreeableness, health, and oral antipsychotic medication type.
Pairwise comparisons of estimated marginal means using Bonferroni adjustment showed that patients prescribed an FGA oral had significantly higher positive SWN ( M = 32.93) compared to patients prescribed an SGA oral ( M = 26.14) ( p = .044). Monotherapy patients
(no oral medication) ( M = 26.51) were not significantly different from either FGA or SGA patients.
129
Table 48 Multivariate predictors of SWN factors
Extraversion
Agreeableness
Wilks’ λ
.88
.73
F p
4.31* .018
12.33*** <.001
Partial η 2
.12
.28
Depression
Health
.74
.80
11.17*** <.001
7.91** .001
.26
.20
Total side-effects
LAI type
Oral antipsychotic type
.93
.99
.90
2.15
.69
1.78
.13
.51
.14
.06
.02
.05
Cases with missing data were deleted leaving 73 cases in this analysis
Table 49 Predictors of Negative and Positive SWN factor scales
Extraversion
R 2 =
F
.58
.86
Negative SWN
Adj. R 2 p
= .53
.357
Partial η
.01
2
Agreeableness
Depression
.11
20.25***
.74
<.001
.00
.24
Health
Total side-effects
LAI type
Oral antipsychotic type
.48
4.35*
.57
.58
.49
.041
.45
.56
.01
.06
.01
.02
R 2 = .68
F
7.54**
24.64***
1.61
15.19***
.07
.74
3.18*
Positive SWN
Adj. R 2 = .64 p
.008
<.001
.21
<.001
.79
.39
.048
Partial η 2
.11
.28
.03
.19
.00
.01
.09
Predictors of the SWN subscales
Extraversion, agreeableness, neuroticism, and depression had previously been identified as significant predictors in regression analyses. Additionally, cognitive/disorganised, negative (because it was correlated with emotional regulation) and affective symptoms, side-effects, insight, and lifestyle questions were entered. ROMI adherence was entered because it was significantly correlated with social integration. Two
130
analyses were initially performed, one containing the total side-effects scale and the other the side-effects subscales and the results compared.
In the analysis using total side-effects, the significant multivariate predictors were agreeableness, health, and insight. Neuroticism and depression were marginally nonsignificant. The analysis using the side-effects subscales produced somewhat similar results, although depression was significant, and neuroticism did not reach significance. All of these variables except neuroticism were also significant or marginally non-significant univariate predictors in both analyses. Additional significant univariate predictors were ROMI adherence, and LAI. None of the side-effects subscales approached significance. The analysis was re-performed using the significant or near-significant covariates. The significant multivariate predictors were agreeableness, health, and depression. There was a nonsignificant trend for neuroticism. There were no significant multivariate effects for LAI or oral medication groups. See Table 50.
Table 50 Multivariate predictors of SWN subscales
Wilks’ λ
Extraversion .84
F
2.03
Agreeableness
Neuroticism
.75
.82
3.39*
2.28
Health
Insight
Depression
ROMI adherence
Long acting injectable group
Oral group
.70
.83
.70
.86
.85
.81 1.15
4.50**
2.13
4.37**
1.76
1.85
.002
.08
.002
.14
.12 p
.09
.01
.06
.33
Partial η 2
.16
.25
.18
.30
.17
.30
.14
.15
.10
131
See Tables 51 – 55 for predictors of each subscale. The significant predictors of mental functioning were health and depression. The significant predictors of self-control were agreeableness, depression, and cognitive/disorganised symptoms. However, there was also a non-significant trend for kind of oral medication ( p = .09). Pairwise comparison of estimated marginal means showed that oral FGA patients scored significantly higher than oral SGA patients ( p = .029) and had a non-significant trend to score higher than patients taking no oral medication ( p = .061). The only significant predictor of self-control was agreeableness, although there were non-significant trends for depression ( p = .055) and neuroticism ( p =
.064).The significant predictors of emotional regulation were extraversion, agreeableness, health and depression. The only significant predictor of social integration was depression.
The significant predictors of physical functioning were agreeableness, health, ROMI adherence, and LAI medication. Patients in the LAI SGA group had significantly higher estimated marginal means for physical functioning, a difference of 2.60 points ( p = .009).
Table 51 Predictors of mental functioning
Extraversion
Agreeableness
Neuroticism
Health
Insight
Depression
ROMI adherence
Long acting injectable group
Oral group
R 2 = .66
F
2.84
.05
1.46
19.57***
.26
10.71**
.11
.32
2.53
Adj. R 2 = .60 p
.10
.83
.23
<.001
.61
.002
.74
.58
.09
Partial η 2
.00
.01
.08
.05
.00
.03
.26
.01
.16
132
Table 52 Predictors of self-control
R 2 = .59
F
Extraversion
Agreeableness
Neuroticism
Health
Insight
Depression
ROMI adherence
Long acting injectable group
Oral group
Table 53 Predictors of emotional regulation
R 2 = .66
Extraversion
Agreeableness
Neuroticism
Health
Insight
Depression
ROMI adherence
Long acting injectable group
Oral group
F
10.02**
8.99**
.001
7.97**
2.23
8.34**
.01
.90
.69
.39
6.88*
3.56
1.83
1.22
3.86
.00
.15
1.84
Adj. R 2 p
=
.54
.011
.06
.18
.27
.055
.96
.70
.17
.52
Adj. R 2 = .60 p
.003
.004
.97
.007
.14
.005
.93
.35
.51
Partial η 2
.13
.00
.02
.15
.14
.00
.13
.04
.02
Partial η 2
.03
.02
.06
.00
.00
.06
.01
.11
.06
133
Table 54 Predictors of social integration
R 2 = .45 Adj. R 2 = .36
F p Partial η 2
Extraversion
Agreeableness
Neuroticism
Health
Insight
Depression
ROMI adherence
Long acting injectable group
Oral group
Table 55 Predictors of physical functioning
R 2 = .47
1.03
2.15
.00
.32
1.08
10.51**
2.51
.46
.31
.32
.15
.97
.58
.30
.002
.12
.50
.73
Adj. R 2 = .38
.01
.02
.16
.04
.01
.01
.02
.04
.00
F p Partial η 2
Extraversion
Agreeableness
Neuroticism
Health
Insight
Depression
ROMI adherence
Long acting injectable group
Oral group
.89
6.90*
1.11
7.38**
2.91
1.75
5.94*
7.32**
2.04
.09
.19
.018
.009
.14
.35
.011
.30
.009
.05
.03
.10
.12
.07
.02
.11
.02
.12
Final models of SWN predictors
Antipsychotic medication treatment regimes were not significant predictors of SWN scales scores in most of the previous ANCOVA and MANCOVA analyses. Further multiple
134
regression analyses were performed using only the significant predictors identified in these analyses in order to allow comparisons of the relative importance of each variable in predicting the SWN scales. Results using either imputation of missing data or deletion of cases with missing data tended to be very similar, therefore, the following analyses used the latter method. Since oral medication was a significant predictor of positive SWN, medication categories were dummy coded according to procedures recommended by Tabachnick and
Fidell (2001) and entered into regression analysis as two variables, one comparing FGA to
SGA oral, the other comparing both oral types with no oral medication. See Table 56 for results for all SWN scales.
135
Total side-effects
Positive SWN
Extraversion
Agreeableness
Health
FGA vs. SGA oral
Oral vs. no oral
Mental functioning
Health
Depression
Self-control
Neuroticism
Agreeableness
Depression
Table 56. Predictors of total SWN, factor scale, and subscale scores
B β
Total SWN R 2 = .76 Adj. R 2 = .74
Extraversion 4.45** .22
Agreeableness 5.82** .234
Depression
Health
Cognitive/disorganised symptoms
Negative SWN
Depression
-.60***
4.58**
-3.59*
R 2 = .55
-.52***
-.377
.250
-.169
Adj. R 2 = .54
-.58
-.13*
R 2 = .61
3.24**
5.26***
4.05***
3.24*
.47
R 2 = .56
2.22***
-.17***
R 2 = .52
-1.52**
1.34*
-.15***
-.25
Adj. R 2 = .58
.28
.37
.37
.20
.06
Adj. R 2 = .55
.48
-.41
Adj. R 2 = .50
-.30
.23
-.37 f 2
.15
.31
.28
.08
.00
.45
.32
.13
.08
.21
.13
.17
.38
.17
.08
.51
.09 p < .001
.06
.12
.11
.03
.00 p < .001
.20
.14 p < .001
.06
.04
.10 sr 2 p < .001
.03
.04
.09
.04
.02 p < .001
.23
.04
136
Table 56 continued
Emotional regulation
Extraversion
Agreeableness
Health
Depression
Physical functioning
Agreeableness
Health
ROMI Adherence
LAI group
R 2 = .63
1.29**
1.64**
1.03**
-.13***
R 2 = .36
2.07**
1.80***
-1.74
1.60
Adj. R 2 = .61
.27
.28
.23
-.32
Adj. R 2 = .32
.32
.39
-.16
.17 p < .001
.05
.07
.04
.07 p < .001
.10
.14
.03
.03
.14
.16
.11
.19
.16
.22
.05
.05
Significant predictors of total SWN
In a multiple regression analysis, extraversion, agreeableness, depression, health, and cognitive/disorganised symptoms were all significant independent predictors of total SWN score. Depression had the largest effect size, followed by health with a medium-to-large sized effect. Agreeableness had a slightly larger effects size compared to extraversion, and both had roughly medium sized effects. The effect size of cognitive/disorganised symptoms was small-to-medium.
Predictors of the SWN factor scales
For negative SWN, depression had a very large effect size, whereas the effect size of total side-effects was small-to-medium. For positive SWN, agreeableness had the strongest effect, followed by health, both with medium-to-large sized effects. Extraversion had a medium sized effect. Oral FGA medication was significantly better compared to oral SGA,
137
with a small-to-medium effect. The contrast between any oral and no oral medication was not significant with a zero effect-size.
7
Predictors of the SWN subscales
For mental functioning, the effect size for health was quite large and that for depression tended to be large. For self-control, the strongest predictor was depression with a medium-sized effect, followed by neuroticism and then finally agreeableness, with small-tomedium effects. For emotional regulation, depression had the strongest effect, followed closely by agreeableness, then extraversion, then health, all with roughly medium sized effects. As depression was the only significant predictor of social integration, regression analysis was unnecessary. Correlational analysis had already revealed a large association between depression and social integration. For physical functioning, LAI group was included in the regression analysis, but was no longer significant. Health was the strongest predictor, followed by agreeableness, both with medium sized effects. ROMI adherence score was no longer significant.
Personality predictors of side-effects
One of the aims of the study was to examine whether personality traits were predictors of side-effects. All of the big five traits except openness to experience were significant predictors of total side-effects. The four remaining traits were entered into a multiple regression analysis. See Table 57. Neuroticism was the only significant predictor of total side-effects. Multiple regression analyses were also performed for each of the sideeffects subscales and the Red Herrings. Neuroticism was the only significant predictor of neurological and psychic side-effects. None of the personality traits significantly predicted autonomic or sexual side-effects, or Red Herrings.
7 Dummy coding contrasting FGA oral with no oral (not significant), and SGA oral with both FGA oral and no oral (significant) produced virtually identical effect sizes.
138
Personality predictors of health
Health has been a robust predictor of SWN in previous analyses, and health is also correlated with all five personality traits. A multiple regression analysis was performed to determine if any of the personality traits would remain independent predictors when controlling for the other traits. Results are shown in Table 58. None of the personality traits were significant independent predictors of health.
Table 57 Big five predictors of total side-effects and side-effects scales
Total side effects R 2
B
= .24
β
Adj. R 2 = .20
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Neurological
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Autonomic side-effects
Extraversion
Agreeableness
Conscientiousness
Neuroticism
.08
-.30
-3.70
9.00**
R 2 = .17
.19
-.47
-.64
1.83*
R 2 = .16
-.36
-2.68
-.78
1.60
.00
-.01
-.16
.40
Adj. R 2 = .13
.04
-.07
-.12
.33
Adj. R 2 = .12
-.04
-.23
-.08
.16 sr 2 p = .001
.00
.00
.02
.10 p = .01
.00
.00
.01
.07 p = .013
.00
.03
.00
.01 f
2
.00
.00
.03
.13
.00
.00
.01
.08
.00
.04
.00
.01
139
Table 57 continued
Psychic side-effects
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Sexual side-effects
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Red Herrings
Agreeableness
Conscientiousness
Neuroticism
Table 58. Big five predictors of health
R 2 = .24
Extraversion
B
.23
Agreeableness
Conscientiousness
.10
-.11
Neuroticism
Openness to experience
-.25
.24
R 2 = .33
.23
.47
-1.45
4.20***
R 2 = .26
.05
.13
-.59
1.00
R 2 = .12
-1.35
-.44
1.03
Adj. R 2 = .20
β
.21
.08
-.09
-.21
.21
Adj. R 2 = .30
.03
.05
-.18
.53
Adj. R 2 = .22
.02
.03
-.16
.27
Adj. R 2 = .08
-.19
-.07
.16 p = .001 sr 2
.02
.00
.00
.03
.03 p < .001
.00
.00
.02
.17 p < .001
.00
.00
.01
.04 p = .03
.02
.00
.02 f 2
.03
.00
.00
.04
.04
.00
.00
.01
.05
.00
.00
.03
.25
.02
.00
.02
140
Follow up data
Follow up assessments were performed for 21 patients (9 female). Fifteen of these participants were diagnosed with schizophrenia, five with schizoaffective, and one with bipolar. Of the 56 patients not included in the follow up assessment, twelve either refused to participate in the second assessment or did not show up for their appointments, and the remainder could not be contacted.
Medications taken by follow up participants
One patient had ceased LAI treatment in favour of oral monotherapy, 12 patients were on an LAI FGA and 8 were on an LAI SGA. See Table 59. Oral antipsychotic and adjunctive medications taken by participants in each LAI group are shown in Appendix J, Table 1. Daily
CPZE dosages for LAI and oral medications are shown in Appendix J, Table 2. There were no significant differences between LAI groups in any dosage levels. Of the patients who participated in the follow up assessment, two declined to participate in the PANSS, and one of these in the ITAQ and the ROMI. Two patients declined to complete the RBANS. All 21 patients completed the SWN, the DASS, and the LUNSERS.
Changes in LAI medication from baseline
Of the nine patients who had been treated with risperidone consta at baseline, five were still being treated with this LAI, two had been switched to olanzapine pamoate, one had been switched to flupenthixol LAI, and 1 had ceased LAI treatment. Of the twelve patients who had been treated with an LAI FGA at baseline, ten were still being treated with their original LAI, one had been switched to risperidone, and one had been switched to a different
FGA.
Changes in oral medication use from baseline assessment are shown in Appendix J,
Table 3. Three of four patients who initially took no oral medication were still taking no oral
141
medication, and one had been started on an SGA. Two patients remained on their original
FGA oral medication. Six out of 15 patients who were originally on an SGA oral were either no longer on oral medication (4 cases) or had been switched to an FGA oral (2 cases). Two patients were switched from their original SGA oral to a different SGA oral (paliperidone).
Table 59 LAI medications taken by number of patients
LAI Baseline
First generation
Haloperidol
Flupenthixol
Zuclopenthixol decanoate
Total FGA
1
7
4
12
Second generation
No LAI
Risperidone consta
Olanzapine pamoate
Total SGA
0
9
9
0
Second assessment
1
6
5
12
2
8
6
1
Differences between follow up participants and non-participants
A series of independent samples ttests were performed to assess how follow up participants may have differed from the remainder of participants assessed at baseline who did not participate in the second assessment. Statistical results are shown in Appendix J,
Table 4. Follow up participants tended to have lower scores on all SWN scales, although this difference was only significant for self-control. There were no significant differences in personality traits, although there was trend for follow up participants to have slightly lower extraversion. There were no significant differences in any of the DASS or side-effects scales.
There were no significant differences in any of the PANSS factors, although there was a marginal trend for follow up participants to score higher cognitive/disorganised symptoms.
There were no significant differences in premorbid IQ, or WTAR estimated IQ, but follow up
142
participants scored significantly lower on information estimated IQ. Follow up participants scored significantly lower on immediate and delayed memory, and on total RBANS score.
There were no significant differences in insight or ROMI adherence scale scores.
SWN scale scores
SWN scale scores at baseline and again at follow up, with their correlations are shown in Table 60. All scales strongly positively correlated with the baseline equivalents.
Independent samples ttests revealed no significant differences between FGA and LAI SGA groups. In order to assess the stability of the SWN scales, change scores were computed by subtracting the baseline score from the score at follow up. These are shown in Table 61.
Paired-samples t -tests showed that there were no significant changes in any SWN scale between baseline and follow up. Independent samples ttests revealed no significant differences between FGA and LAI SGA groups in amount of change in SWN scale scores, although there were trends for the LAI SGA group to have a slight decrease in scores on most scales. See Table 62.
Table 60 Correlations between baseline and follow up SWN scale scores
SWN total
Negative SWN
Positive SWN
Mental functioning
Self control
Emotional regulation
Social integration
Physical functioning
Baseline Mean Std. Deviation
61.67 18.39
35.90 11.15
23.71
12.24
11.52
12.95
12.33
12.62
10.32
4.46
4.47
4.20
4.53
4.41
Follow up
Mean
60.57
13.381
Std.
Deviation
17.80
10.20
21.95
11.71
9.76
4.60
11.52
13.19
12.76
11.38
4.11
4.62
4.45
4.70 r
.83***
.63**
.69**
.59**
.63**
.83***
.76***
.50*
143
Table 61 Change in SWN scale scores between baseline and follow up
SWN total
Negative SWN
Minimum
-24.00
-19.00
Maximum
17.00
23.00
Mean
-1.10
.71
Std.
Deviation
10.61
9.25
Positive SWN -17.00
-12.00
11.00
5.00
-1.76
-.53
7.92
4.09
Mental functioning
Self control
-5.00 13.00 .00 3.70
-5.00 5.00 .24 2.62
Emotional regulation
Social integration -5.00
-16.00
7.00
5.00
.43
-1.24 Physical functioning
Table 62 Differences between LAI groups in changes in SWN scale scores
3.09
4.55
SWN change between assessments
Negative SWN
Positive SWN
Mental functioning
Self-control
Emotional regulation
Social functioning
Physical functioning
LAI group at follow up
FGA
SGA
FGA
SGA
FGA
SGA
FGA
SGA
FGA
SGA
FGA
SGA
FGA
SGA
FGA
SGA
.00
-1.63
-.17
-1.38
.92
-.13
.33
.50
-.75
-2.25
Mean
.33
-4.88
1.17
.13
-1.17
-4.25
3.19
5.40
2.48
1.77
1.93
3.00
3.58
2.67
3.84
5.80
Std.
Deviation
10.26
10.58
9.33
10.33
6.94
8.53
.85
1.19
.95
-.11
.70 t
1.10
.24
.89
.37
.56
.42
-.05
.30
Cohen’s d
.50
.11
.42
.35
.91
.41
.25
.49 p
.29
.82
.39
Correlations
See Appendix J, Tables 4 – 5 for correlations between SWN scales at follow up and
DASS, LUNSERS, PANSS, and lifestyle questions, also assessed at follow up. Appendix J,
Tables 6 – 7 shows correlations between follow up SWN scales and the same variables from baseline assessment. Depression assessed at baseline was moderately strongly correlated with
144
follow up SWN scores ( r = -.45). Follow up depression score had a larger correlation with follow up SWN score ( r = -.72).
DASS and LAI groups
DASS means for each LAI group are shown in Table 63. Independent samples ttests revealed no significant between-group differences, although there were small to medium sized trends for the FGA group to score higher on all three scales.
Table 63 DASS score means for LAI groups
Depression
Anxiety
Stress
LAI at follow up
FGA
SGA
FGA
SGA
FGA
SGA
Mean
15.00
10.25
15.67
12.25
18.17
13.50
Std.
Deviation
11.07
8.51
10.75
12.16
11.39
12.18 t
1.03
.66
.87 p
.32
.52
.39
Cohen’s d
.48
.30
.40
Correlation between changes in SWN and changes in DASS scores
To determine whether changes in SWN scale scores related to changes in depression and other variables related to SWN, change scores were computed by subtracting the baseline score from the score at follow up and correlations between baseline and follow up scores were computed. See Table 64. There were no significant differences between baseline and follow up scores on the DASS or any of the side-effects scales. Correlations between changes in SWN scales and DASS scales are shown in Table 65. Changes in depression strongly negatively correlated with total SWN, negative SWN and social integration. Changes in anxiety strongly negatively related to changes in total SWN and mental functioning. Changes in stress did not significantly relate to changes in any SWN scale although some correlations were of moderate size.
145
Table 64 Change in DASS and side-effects scale scores between baseline and follow up
Depression
Minimum
-14.00
Maximum
20.00
Mean
-2.00
Std. Deviation
10.12 r
.55*
Anxiety -18.00 20.00 .86 9.37 .63**
Stress -26.00 26.00 .10 12.61 .37
Total side-effects -30.00 50.00 .10 21.73 .50*
Neurological SE -9.00 10.00 -.43 5.38 .48*
Autonomic SE -8.00 37.00 2.76 10.56 .47*
Psychic side-effects -16.00 18.00 .67 8.37 .40
Sexual SE -8.00 8.00 -.19 3.64 .33
Side-effects and LAI groups
Mean scores on the side-effects scales are shown in Table 64. Independent samples ttests revealed no significant between-group differences, although there were medium sized trends for the FGA group to score higher on total side-effects, and neurological and autonomic side-effects.
Changes in total side-effects moderately to strongly negatively correlated with changes in total SWN, negative SWN, and two subscales. See Table 66. Changes in neurological SE strongly negatively correlated with changes in total and positive SWN and two subscales. Changes in psychic side-effects strongly negatively correlated with changes in total and negative SWN and two subscales. Changes in autonomic and sexual SE did not significantly correlate with changes in any SWN scales.
146
Table 65 Correlations between changes in SWN scales and DASS scales
SWN scale change Depression change Anxiety change
SWN total -.58** -.53*
Negative SWN
Positive SWN
-.57**
-.03
-.39
-.26
Mental functioning
Self-control
Emotional regulation
Social integration
Physical functioning
-.37
-.23
-.24
-.56**
-.30
-.66**
-.16
-.29
-.27
-.16
Table 66 Correlations between changes in SWN scales and changes in side-effects scales
SWN scale change
SWN total
Total SE change
-.55**
Neurological
SE change
-.62**
Autonomic SE change
-.20
Psychic sideeffects change
-.56**
Negative SWN
Positive SWN
Mental functioning
Self-control
-.44*
-.21
-.20
-.21
-.52*
-.16
-.31
.03
-.14
-.55*
-.20
-.30
-..26
-.25
-.34
-.134
.07
-.05
-.04
-.49* Emotional regulation
Social integration
Physical functioning
-.52**
-.40
-.65**
-.51*
-.27
-.19
-.46*
-.41
Stress change
-.37
-.34
-.13
-.29
-.15
.04
-.36
-.26
Sexual SE change
-.42
-.29
-.21
-.42
-.28
-.37
-.17
-.04
PANSS scores and LAI groups
PANSS scores are shown in Appendix J, Table J9. The LAI FGA groups scored
significantly higher than the LAI SGA group in affective symptoms. There were no significant differences for the other PANSS factors. Changes in PANSS factor scores were
147
also calculated. There was a non-significant trend for the LAI FGA group to have an increase in positive symptoms, whilst the LAI SGA group decreased, although mean changes in each group were quite small. All other differences in changes in PANSS factors were nonsignificant and mostly were small to negligible in size. See table 67.
Table 67 Changes in PANSS scores in each LAI group.
LAI FGA LAI SGA Total
Mean Std.
Deviation
Mean Std.
Deviation
Mean Std.
Deviation t
Positive symptoms
Negative symptoms
.30
-.78
Cognitive/disorganised symptoms
-.29
Affective symptoms -.11
Excitement symptoms -.18
PANSS total -7.00
.81
.91
.61
.67
.72
14.42
-.45
-.33
-.43
-.06
-.21
-6.57
.70
.33
.42
.44
.31
9.22
.11
-.59
-.41
-.04
-.18
-6.10
.93
.74
.60
.60
.57
12.40 p
2.02 .06
-1.45 .16
.54 .60
-.18
.11
-.07
.86
.91
.95
Cohen’s d
.99
-.66
.27
-.09
.05
-.04
Correlations between changes in SWN scale scores and PANSS symptoms scores are shown in the Table 68. Changes in positive symptoms significantly negatively correlated with changes in negative SWN, and, unexpectedly, positively correlated with changes in positive
SWN and self-control. Changes in negative symptoms did not significantly correlate with changes in any SWN scale. Changes in cognitive/disorganised symptoms significantly negatively correlated with changes in self-control. Changes in affective symptoms did not significantly correlate with any of the SWN scales, although there was a moderate sized nonsignificant negative correlation for negative SWN and an unexpected non-significant positive correlation for positive SWN. Changes in excitement symptoms did not significantly correlate with any of the SWN scales. Changes in the total PANSS score were significantly negatively correlated with negative SWN. There were moderate sized non-significant
148
correlations for two of the other subscales. Therefore, the overall trend was for improvements in symptoms to be associated with improvements in SWN although there were some trends in the opposite direction. The majority of correlations tended to be small in size.
Table 68 Correlations between changes in SWN scores and changes in PANSS symptoms
SWN scale change
Positive symptoms
Negative symptoms
Cognitive/disorganised symptoms
Affective symptoms
Excitement symptoms
PANSS total
SWN total
Negative
SWN
Positive
SWN
Mental functioning
Self-control
Emotional regulation
Social integration
Physical functioning
.06
-.48*
.48*
-.02
.64**
-.32
-.31
.03
-.13
-.15
.09
-.13
.02
-.07
-.02
-.15
-.25
-.25
-.12
-.37
-.49*
.37
-.04
-.04
.10
-.39
.43
-.02
.27
-.14
-.02
.11
.11
-.21
.28
-.03
.03
-.11
.07
.29
-.20
-.60**
.34
-.24
.30
-.29
-.31
-.12
RBANS and LAI groups
RBANS index scores for each LAI group are shown in Table 69. Independent samples ttests showed that the LAI SGA group scored significantly higher than the LAI FGA group on delayed memory, and this was a large effect. There were no significant differences on the other index scores, although there were medium sized differences favouring the LAI SGA group in immediate memory, visuospatial/constructional and the total RBANS score.
149
Table 69 RBANS scores for each LAI group
Immediate memory
Visuospatial/constructional
Language
Attention
Delayed memory
RBANS total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
10.83
14.42
11.88
15.85
17.56
16.06
15.78
12.42
17.61
11.80
13.06
12.59
Std.
Deviation
15.87
22.66
18.91
21.64
19.10
20.55
86.45
81.29
84.32
68.09
71.57
70.26
53.18
73.14
62.11
59.73
68.43
63.68
Mean
53.82
65.00
59.11
72.55
85.00
76.95
.87
-.44
-2.83
-1.47 t
-1.24
-1.24
.41
-.21
-1.20
-.70
Cohen’s d
-.57
-.61
.40
.67
.012
.16 p
.23
.23
In order to assess the stability of the RBANS indexes, change scores were computed by subtracting the baseline score from the score at follow up and correlations between baseline and follow up scores were computed. These are shown in Table 70. All scales strongly positively correlated with their baseline equivalents. Paired-samples t -tests showed that there were significant improvements in the language index and the total RBANS score between baseline and follow up. There was also a non-significant trend for an improvement in immediate memory. Independent samples t -tests using the change scores as dependent variables showed that the LAI groups did not differ in changes in any RBANS index. See
Appendix J, Table 8 for the means for each LAI group. The LAI groups did not differ significantly on any RBANS change scores.
150
Table 70 Change in RBANS index scores between baseline and follow up
Attention
Immediate memory
Visuospatial constructional
Language
Delayed memory
RBANS total
Mean
5.3158
.3158
5.7368
.5263
4.1579
3.7368
Std.
Deviation Minimum Maximum
12.71942 -17.00 33.00
17.91043
11.63253
-32.00
-15.00
47.00
31.00 t
-1.82 p
.09 r
.75***
-.08 .94 .54*
-2.15* .045 .69**
11.34494
15.23980
6.40175
-19.00
-23.00
-9.00
22.00
35.00
14.00
-.20
-1.19
-2.54*
.84
.25
.02
.75***
.60**
.86***
Correlations between RBANS change scores and SWN scale change scores are shown in Table 71. Total SWN, self-control, social regulation, and physical functioning did not significantly correlate with changes in any RBANS index, although a few of these (negative) correlations were of moderate size. Negative SWN change had a significant negative correlation with change in the visuospatial/constructional index, and all other correlations were non-significant and modest in size. Positive SWN change had non-significant negative correlations with changes in immediate memory and total RBANS score. Mental functioning had a significant positive correlation with change in the visuospatial/constructional index.
Emotional regulation had significant negative correlations with changes in delayed memory and the total RBANS score.
151
Table 71 Correlations between changes in SWN scales and RBANS indexes
SWN scale change
Immediate memory
Visuospatial constructional
Language Attention
SWN total
Negative
SWN
Positive
SWN
Mental functioning
Self-control
Emotional regulation
Social integration
Physical functioning
-.40
.05
-.45
-.12
.14
-.38
-.44
-.42
.30
-.49*
-.05
.47*
-.10
.13
.06
.22
-.07
.24
.07
-.27
.12
-.27
-.09
.20
-.25
.04
-.24
-.09
-.44
.04
.04
-.19
Delayed memory
-.16
.15
-.11
-.20
.30
-.75
**
-.09
.06
RBANS total
-.20
-.05
-.34
-.05
.13
-.58
**
-.20
-.05
Insight and attitudes to adherence
Change scores for ITAQ insight and the ROMI scales were computed. Change in insight did not significantly correlate with change in any of the ROMI scales. Changes in insight and in the ROMI scales did not significantly correlate with changes in any of the
SWN scales, with the exception of a significant positive correlation between change in self-
control and change in ROMI nonadherence. Means and correlations are shown in Appendix J,
Tables J11 – J12.
Examination of SWN Clusters
In order to examine the stability of SWN scores in more detail, patients were assigned to clusters based on their SWN scores at baseline and again at follow up. Cluster cut-offs were assigned based on the criteria used in the study by Lambert et al. (2009). The Low cluster was defined as a total score < 40; the medium cluster was defined as 40 to < 60, and
152
the High cluster was defined as 60 and above. Numbers of patients in each cluster category are shown in Table 72.
Table 72 SWN cluster status at baseline and at follow up
SWN cluster
Low (<40)
Medium ( ≥40 < 60)
High (≥60)
N
2
9
10
Baseline
%
9.5
42.9
47.6
N
1
11
9
Follow up
%
4.8
52.4
42.9
Only four participants changed their cluster status between baseline and follow up.
Figure 4 shows each patient’s cluster position at baseline and at follow up. Two patients went from a higher to a lower cluster (both from high to medium – centre-right area) and two patients went from a lower to a higher cluster (one from low to medium – centre-left area, the other from medium to high – upper-centre area). The remainder, that is 81% of patients followed up, remained in the same cluster (lower left, centre, and upper right areas).
153
Figure 4 SWN scores at baseline and at follow up.
154
Discussion
Overview of Factors associated with SWN
In the present study, one of the aims was to identify factors significantly associated with subjective well-being in patients treated with LAI antipsychotic medications.
Additionally, the study aimed to investigate the factor structure of the SWN and examine correlates of these factors. Correlational analyses identified a large number of variables significantly associated with total SWN and subscale scores. Factor analysis identified two correlated SWN factors, named positive and negative SWN, also correlated with a large number of variables. Multivariate analyses suggested that the most robust predictors of SWN in the current study were depression, self-assessed global health, agreeableness, extraversion, and to a lesser extent cognitive/disorganised symptoms. Neuroticism significantly predicted
SWN even after controlling for other personality traits, but became non-significant when controlling for depression. Neuroticism was a strong predictor of depression, and there was evidence that depression mediated the relationship between neuroticism and SWN. Sideeffects significantly predicted the negative SWN factor, but not positive or total SWN when controlling for other important predictors.
In spite of past claims for the superiority of SGA in relation to subjective well-being, results showed no evidence of any differences between LAI medication groups in their SWN scores. In the multivariate analysis of the subscales, a statistically significant difference in the physical functioning subscale favouring the SGA group appeared when controlling for several covariates. This difference was of small to medium size. However, no other analyses found statistically significant differences in this subscale. Note that the physical functioning subscale had the lowest internal consistency of all the subscales and hence had poor reliability. Differences between LAI groups for the other SWN scales all tended to be small to negligible. Additionally, there was no evidence that oral SGA were associated with more
155
favourable SWN scores compared to oral FGA or no use of oral medications. Quite the contrary, the small group of patients prescribed oral FGA actually scored significantly higher on positive SWN when controlling for personality and self-assessed health. Contrary to suggestions by Naber et al. (2001), there was evidence that the combination of treatment with an SGA LAI and oral olanzapine was associated with lower levels of SWN compared to other treatment regimes, such as SGA LAI monotherapy and the combination of FGA LAI with an oral FGA.
A further aim of the study was to compare performance on neurocognitive tests between FGA and SGA LAI treatment groups. Differences in performance between groups tended to be negligible, although unexpectedly the FGA LAI group scored higher in language tests. SWN scores tended to modestly positively correlate with a number of neurocognitive tests when controlling for premorbid intelligence. However, when controlling for openness to experience, there were very few significant correlations between SWN and these tests.
An additional aim of the study was to examine possible relationships between medication side-effects and personality. Side-effects correlated negatively with extraversion, agreeableness, and conscientiousness, and positively with neuroticism. When all these personality traits were considered in a regression analysis, neuroticism remained a significant predictor of total side-effects and the neurological and psychic subscales. None of the personality traits significantly predicted the autonomic or sexual subscales or the Red
Herrings.
Since so much SWN research has examined the impact of antipsychotic medications, these findings will be considered first.
156
Long acting injectable antipsychotic treatment and SWN
LAI groups tended to be equivalent in their SWN scores in most analyses. SGA LAI treatment had an advantage over FGA LAI treatment only in regards to the physical functioning subscale in a multivariate analysis controlling for personality, depression, health, insight, adherence, and oral medication. In regards to total SWN, and the remaining SWN scales, differences between LAI groups were negligible in nearly all analyses.
Additionally, there appeared to be no significant differences in severity of sideeffects, or self-reported ratings of depression, anxiety, and stress. Differences in total sideeffects between LAI groups were negligible. Note that both LAI groups had comparable rates of use of anticholinergic medication (benztropine) to control parkinsonian side-effects, and did not differ in their use of other adjunctive medications such as mood stabilisers. (See
Appendix D for details of additional adjunctive medications used in each LAI group.)
The reasons why patients were treated with either an FGA or an LAI SGA could be related to their pre-existing characteristics that guided treatment choice. However, the reasons why clinicians prescribe particular drugs are not well-understood (Hamann, Kolbe, Cohen,
Leucht, & Kissling, 2005; Hamann, Langer, Leucht, Busch, & Kissling, 2004; Ren et al.,
2002). One study found that older physicians (aged over 50 years) were more likely than younger ones to prescribe FGA than SGA probably due to greater familiarity with older agents (Hamann, et al., 2004). LAI SGA drugs are relatively new and therefore less likely to be familiar to clinicians than LAI FGA. Hamann et al. (2004) found that patients with more severe positive symptoms were more likely to be prescribed an FGA. In the present study,
LAI FGA patients did have more severe positive, hostile excitement, and affective symptoms.
However, positive and hostile excitement symptoms were unrelated to SWN, although affective symptoms negatively correlated with SWN. However, there was no evidence of a significant difference in SWN between long acting injectable groups when controlling for
157
affective symptoms. There was a significant interaction between affective symptoms and the negative SWN and emotional regulation scales suggesting that members of the FGA LAI group were more strongly impacted by affective symptoms than members of the SGA group in some respects. Previous research suggests that SGA treatment has a substantially beneficial impact on mood symptoms compared to FGA treatment, although this is more true of olanzapine than risperidone (Dawkins, Lieberman, Lebowitz, & Hsiao, 1999). However, this would not explain why FGA LAI patients who had low affective symptoms tended to score higher on negative SWN and emotional regulation than SGA LAI patients similarly low on affective symptoms. Putzhammer, Perfahl, Pfeiff, and Hajak (2005) found that SWN in
SGA-treated patients was more strongly related to general psychopathology and negative symptoms than in FGA treated patients. The results of the present study do not seem to support this finding at least as far as LAI treatment is concerned. Furthermore, although the
FGA LAI group did have higher interviewer-rated affective symptoms than the SGA group, their self-reported distress as measured by the DASS differed very little between groups.
Furthermore, self-reported depression seemed to be a stronger predictor of SWN than interviewer-rated affective symptoms. PANSS ratings of affective symptoms substantially overlapped with distress as measured by the DASS, and when affective symptoms were entered into a regression analysis simultaneously with depression, the former became nonsignificant. Only patients can truly rated their depression, and since SWN is self-reported, self-reported measures of depression might be more sensitive to patient’s perceptions of their state of functioning.
Evidence from a naturalistic study of LAI prescription suggested that patients treated with LAI risperidone were more likely to be treatment resistant than patients treated with LAI
FGA (Citrome, Jaffe, & Levine, 2010). However, this seems unlikely to be the case in the present study, as patients treated with LAI FGA had more severe psychopathology in terms
158
of positive symptoms and so on. Additionally, patients on LAI SGA were not more likely than FGA patients to have been ever trialled on clozapine or been treated with ECT, indicators of treatment resistance and illness severity.
There were a number of other baseline differences between patients in each LAI group, such as age, education, time on medication and substance use. However, it seems unlikely that these factors acted as confounds masking any real differences between medication groups. Age, education, time on medication, and substance use, apart from tobacco use, did not significantly correlate with SWN. This finding seems to parallel findings by Naber (1995) and Ritsner et al. (2004) that demographic factors were unrelated to subjective response to antipsychotic drugs.
A potentially serious confounding factor is the substantial use of polypharmacy in the present sample. Specifically, the majority of patients were prescribed oral antipsychotic medications in addition to LAI medication, despite this being at odds with most clinical practice guidelines (Gardos, 2005). Antipsychotic polypharmacy in the treatment of LAI patients was found to be prevalent in another study comparing LAI risperidone treatment with FGA treatment, as more than 86% of patients in both types of LAI treatment were also treated with oral antipsychotics (Citrome, et al., 2010). Furthermore, the majority of oral medications prescribed in the present study were SGA, meaning that most patients prescribed an LAI FGA were also taking SGA oral medication. Patients on a LAI FGA were most likely to be prescribed oral olanzapine whereas patients on LAI SGA were most likely to be prescribed oral risperidone. When patients were grouped into medication categories based on the combination of LAI (FGA vs. SGA) and oral (none vs. FGA. vs. SGA), no significant between group differences were found. Unexpectedly, an analysis categorising patients based on whether their oral medication was olanzapine, risperidone, another SGA, an FGA, or
159
none, combined with their LAI medication, found that patients on an LAI SGA who were also taking olanzapine (SGA/O) had the lowest average SWN scores compared to other medication groups. This group had significantly lower SWN (including total score, negative
SWN, and three subscales) than patients on an LAI SGA monotherapy (no oral medication).
This latter group actually had the highest SWN although they did not differ significantly from the remaining medication groups. The SGA/O group also tended to have lower SWN than
LAI FGA patients taking an FGA oral (significantly on total score, positive SWN, and three subscales) and LAI FGA monotherapy patients (significantly on negative SWN). These findings, although not conclusive due to the small and unequal subsample sizes involved, seems to concur with a previous finding that antipsychotic monotherapy is associated with higher SWN than polypharmacy (Libiger, Masopust, & Köhler, 2008). However, the finding that patients taking an FGA oral tended to have higher SWN than those taking olanzapine combined with an LAI SGA seems to contradict previous findings that olanzapine treatment is associated with better SWN than treatment with FGA or other SGA (Naber, et al., 2001;
Wehmeier, et al., 2007). Oral olanzapine may have been prescribed to these patients if these patients were depressed (Tollefson, Sanger, Lu, & Thieme, 1998) but in the current sample there were no significant differences between SGA/O patients and patients on other treatment regimes in depression. It seems worth noting that when FGA LAI patients were prescribed an oral FGA, the latter agent was usually the oral form of their injectable agent. That is, patients prescribed LAI zuclopenthixol for example, were also prescribed oral zuclopenthixol. Future research should examine whether supplementing an LAI with its oral equivalent has advantages for subjective well-being compared to prescribing different types of LAI and oral agents.
The finding in the present study that olanzapine was not associated with higher levels of SWN compared to other agents might possibly relate to patients’ stage of treatment. The
160
studies by Naber et al. (2001) and Wehmeier et al. (2007) both found that olanzapine was associated with initially rapid improvements in SWN. Naber et al. cautioned that weight gain associated with olanzapine tends to occur later in treatment than the early gains in SWN noted in their study and noted that the effects of particular agents might be related to the stage of treatment. Risperidone, for example, is most likely to produce EPS in the first few weeks of treatment, which could explain why olanzapine was associated with higher SWN than risperidone in the study by Naber et al. (2001). A study by Sanger et al. (1999) found that
EPS associated with haloperidol treatment tended to be less severe in multi-episode compared to first-episode patients, suggesting that EPS severity may actually reduce in long-term haloperidol treatment. Additionally, clinical effectiveness of olanzapine tended to be greater in first-episode patients than in multi-episode patients. These findings suggest the possibility that patients in long-term treatment may find FGA, even agents as strongly ‘typical’ as haloperidol, more tolerable in regards to EPS if they have been using it for a long time, and the superiority of olanzapine in clinical effectiveness may diminish to some extent in those who have received it over a long period.
Findings of the present study raise the possibility that although olanzapine may be associated with better SWN than other agents in the early stages of treatment, olanzapine might not be associated with better SWN in patients in long-term maintenance treatment, such as LAI-treated patients tend to be. It is possible that adverse effects associated with olanzapine, such as weight gain might be associated with poorer SWN, although the data from the current study cannot address this. A previous study found that weight gain associated with antipsychotic use is associated with poorer self-reported health, vitality, and quality of life (Allison, Mackell, & McDonnell, 2003). Furthermore, SGA treated patients who have metabolic disturbances, such as weigh gain and diabetes, tended to have poorer self-reported quality of life, including poorer health, more impaired memory, and less sense
161
of being clearheaded, compared to SGA treated patients without metabolic disturbances
(Dubisar, Stoner, Reynolds, Khan, & Ramlatchman, 2004). On the other hand, an intervention study for patients with weight problems found no relationship between maintaining or decreasing weight and improvements in total SWN, although there were improvements in the emotional regulation subscale (Porsdal et al., 2010). Participation in the weight loss program may have had a positive impact on aspects of this subscale such as hope for the future. Furthermore, in the present study treatment with sodium valproate was associated with higher SWN compared to no mood stabiliser use, when controlling for antipsychotic use, even though this agent is associated with significant weight gain (Dinesen,
Gram, Andersen, & Dam, 1984). However, sodium valproate use was also most common in patients diagnosed with schizoaffective disorder rather than schizophrenia, and when diagnosis was controlled for, the apparent advantage of sodium valproate became nonsignificant.
Libiger, Masopust, and Köhler (2008) found that lower antipsychotic dosage was associated with better SWN. Medication dosage in the present study was controlled for in analyses of between LAI-group differences in SWN and was not found to have a significant impact. Furthermore, dosage did not correlate with SWN scores. Surprisingly, dosage was not associated with side-effect severity. Side-effect severity scores were reasonably low in both
LAI groups yet all of the side-effect scales had significant negative correlations with the
SWN scales. Krakowski, Czobor, and Volavka (1997) found that EPS in their study were not related to medication plasma levels. They suggested that benztropine use may have obscured any relationship between EPS and plasma levels. However, in the present study only eight patients used benztropine. De Haan et al. (2003) found that there was substantial interindividual variability in the relationship between antipsychotic dosage and occupancy of dopamine D
2
receptors in patients with recent onset schizophrenia. A previous study found
162
that D
2
receptor occupancy levels above 78% create a risk of EPS (Kapur, Zipursky, Jones,
Remington, & Houle, 2000). The finding that individuals vary greatly in their dose-related D
2 receptor occupancy levels suggests that how much medication enters the brain, and therefore the severity of side-effects experienced, may to some degree be independent of the dosage and more dependent on the peculiarities of the patient’s characteristics, including their physiology.
Results from the current study therefore, do not provide evidence that kind of LAI medication prescribed has any noticeable relationship with SWN. Most of the LAI SGA patients in the present study were treated with risperidone consta, and only two with olanzapine pamoate. It remains possible that LAI olanzapine could be superior to risperidone consta and LAI FGA in its effect on SWN, but this remains to be tested. As noted, it is also possible that olanzapine might not be associated with better SWN in patients in long-term maintenance treatment. It is possible that particular medication types do not consistently have an advantage regarding SWN in chronic patients who have been stabilised on medication for long periods. This could be because treating clinicians have been reasonably successful in individually tailoring treatment regimes to optimise tolerability in terms of adverse effects.
Naber and Karow (2001) acknowledged that each drug has particular advantages and disadvantages and that no specific drug may be best for all patients under all circumstances.
SGA tend to have more benign EPS profiles but have disadvantages relating to metabolic effects, such as hyperprolactinaemia in risperidone (but also in most FGA) and weight gain in olanzapine, and these costs and benefits need to be weighed up carefully. Furthermore, it is possible that FGA may become more tolerable with time as the study by Sanger et al. (1999) suggests. Additionally, the influence of polypharmacy on SWN appears to have been examined in only one study, the full details of which have not yet been published (Libiger, et al., 2008). Combining oral olanzapine with LAI risperidone might be associated with
163
particular disadvantages. The pharmacology of antipsychotic polypharmacy is not well understood even though it has become increasingly prevalent, as is augmentation of antipsychotic agents with adjunctive medications (Correll, Rummel-Kluge, Corves, Kane, &
Leucht, 2009). A naturalistic study of patients initiated on SGA found that antipsychotic polypharmacy was highly prevalent and that only a third of patients were treated predominantly with monotherapy (Faries, Ascher-Svanum, Zhu, Correll, & Kane, 2005).
Furthermore, Faries et al. stated that polypharmacy seemed to be a prolonged and deliberate choice rather than an interim measure associated with changing medication regimes.
Although polypharmacy may have been a factor in the lack of differences between medication groups in the present study, it is also possible that SGA treatment may not be as advantageous for SWN as previously thought. As previously noted studies by de Haan et al.
(2003) and Balestrieri, et al. (2009) found that patients treated with haloperidol did not have worse SWN than SGA treated patients. SGA treatment might not have an advantage for SWN when EPS are reasonably well controlled, for example due to anticholinergic treatment
(Rosenheck, et al., 2003) or perhaps due to appropriately low dosage (de Haan, et al., 2003;
Geddes, et al., 2000). The finding of the present study generally did not find advantages for
SGA treatment over FGA and this finding extended to neurocognitive test performance as well as SWN.
LAI antipsychotic treatment and neurocognitive functioning
LAI treatment groups did not differ in their overall neurocognitive performance as measured by the RBANS total score. However, the LAI FGA group did have moderately superior performance on the Language index, contrary to expectations. The LAI groups did not differ significantly in their estimated premorbid IQ, so these effects are puzzling. Studies on the efficacy of SGA in improving neurocognition have produced mixed results. For example, Keefe et al. (1999) found that risperidone improved cognition compared to FGA,
164
but Purdon et al. (2000, cited in Gurpegui et al. 2006) found no advantage for risperidone over haloperidol. The studies by Keefe et al. (2006) and Keefe et al. (2007) found no advantage for SGA, including risperidone over haloperidol and perphenazine respectively.
Keefe et al. (2007) suggested that EPS are detrimental to performance on cognitive tests and that when these reduce to tolerable levels FGA may actually have beneficial effects on neurocognition, comparable to those of SGA. Therefore, the apparent superiority of SGA in improving cognition compared to FGA may disappear when EPS are well managed.
Differences in EPS (neurological side-effects) in the present study were not significantly different between LAI groups. Therefore, the equivalence of LAI groups in neurocognitive functioning in the present study may reflect comparable tolerability of their medications.
Keefe et al. (2007) also noted that anticholinergic agents, such as benztropine, may impair cognitive performance. There were low rates of benztropine use in the present study that did not differ significantly between LAI groups. Furthermore, it is worth noting that neurocognitive benefits of treatment with any kind of antipsychotic tend to be small.
SWN and performance on cognitive tests
One of the aims of the present study was to assess the possible relationship between
SWN and neurocognitive performance. SWN was found to have modest yet significant positive relationships between general cognitive ability (RBANS total score), immediate and delayed memory, and language ability, particularly when controlling for premorbid IQ.
However, this relationship became non-significant when controlling for openness to experience. Openness to experience is modestly associated with intelligence. It is unknown whether openness to experience in schizophrenia has a protective influence on cognitive status, or whether preserved neurocognitive functioning protects openness to experience from decline (Dinzeo & Docherty, 2007). Openness to experience had a moderate positive association with SWN and it may be that participants with better cognitive performance had
165
somewhat better SWN because they were also higher in openness to experience. Openness to experience is associated with the richness of one’s mental life (Costa & McCrae, 1992), and higher openness to experience might provide some protection against perceived reductions in the ability to think and feel associated with pharmacogenic depression. Alternatively, less pharmacogenic depression might lead participants to rate themselves as having higher openness to experience.
Factor structure of the SWN
The SWN subscales all had moderate to strong intercorrelations, suggesting that they are based on overlapping constructs. Additionally, the subscales in the present study tended to have low reliabilities, although the reliability of the mental functioning subscale was reasonably acceptable. The generally low reliability of the subscales suggests that the subscales are probably not a good fit to the underlying factor structure of the scale, at least in this population. This is in contrast to results reported by Naber et al. (2001) who found substantially higher reliabilities for the subscales. Exploratory factor analysis identified two correlated factors that were readily interpretable. Interestingly, item 5, ‘My body feels familiar’ did not load strongly on either factor. In the present study, this item seemed to be the one most frequently queried by participants, who had trouble understanding its meaning.
This might help to explain why the physical functioning subscale had such poor reliability in this sample.
Scales based on the two SWN factors had good internal consistency, comparable to that of the total scale. This suggests a close conceptual relationship between the items within each factor scale. The fact that the first factor consisted entirely of negatively worded items and that the second factor consisted almost entirely of the positively worded items raises the possibility that these factors are artefacts of the wording of the scale. However, there is correlational evidence for the conceptual validity of the factors. In multiple regression
166
analysis of the five personality traits, neuroticism was the only significant predictor of the negative SWN factor. Neuroticism is strongly associated with negative affect and low selfesteem, and therefore, it makes sense that negative aspects of subjective well-being would be associated with neuroticism. Extraversion and agreeableness were the significant predictors of the positive SWN factor. Both of these personality traits are associated with positive affect and high self-esteem, and therefore, it again makes sense that positive aspects of subjective well-being would be associated with these traits. The personality scales used in the present study consisted of positively worded and reverse keyed items. If the SWN factors were an artefact of response style then it would seem unlikely that the personality scales would predict them in a sensible way because the personality scales contain a mixture of positive and negative items.
Furthermore, in multivariate analyses, depression was the only significant predictor of negative SWN, but depression did not significantly predict positive SWN. This provides further evidence that the negative SWN factor conceptually relates to negative aspects of the patient’s experience. Furthermore, health, extraversion, and agreeableness were significant predictors of positive SWN, providing evidence that this factor conceptual relates to positive aspects of the patient’s experience. Interestingly, patients diagnosed with schizoaffective disorder reported higher positive SWN compared to patients diagnosed with schizophrenia.
This suggests that possibility that manic-like symptoms associated with feelings of euphoria might be associated with elevated positive SWN. This seems consistent with findings by
Lambert, Naber, et al. (2009) that patients diagnosed with schizophrenia tended to have worse SWN than those diagnosed with schizoaffective or bipolar disorder, and that mania was associated with better SWN compared to depression.
167
A number of subjective well-being constructs used with the general population have been found to possess distinct dimensions associated with positively worded and negatively worded items. There is research evidence suggesting that these method effects associated with wording actually have substantive meaning rather than simply representing measurement error (Quilty, Oakman, & Risko, 2006). The tendency to endorse negative items on a self-esteem scale has been found to be associated with avoidance motivation and neuroticism for example (Quilty, et al., 2006). Owens (1993) argued that self-esteem has both positive and negative self-evaluative components representing ‘self-confidence’ (confidence in one’s capacities and belief in one’s moral worth) and self-deprecation (the tendency to disparage one’s worth and capacities) respectively. Owens (1993) found that depression, anxiety and alienation related more strongly to self-deprecation than self-confidence. This parallels the finding of the present study that depression related more strongly to negative
SWN than positive SWN. A study on self-esteem in people with schizophrenia found that self-deprecation was correlated with severity of positive symptoms and depression; whereas positive self-esteem was inversely correlated with negative symptoms and depression
(Barrowclough et al., 2003). Furthermore, there is evidence that optimism and pessimism are distinct constructs rather than polar opposites (Herzberg, Glaesmer, & Hoyer, 2006). High optimism (the belief that good things will happen) seems to be conceptually distinct from low pessimism (the belief that bad things will not happen) (Segerstrom, Evans, & Eisenlohr-
Moul, 2011). There is evidence that optimism and pessimism are actually substantively distinct constructs rather than artefacts of method bias (Kubzansky, Kubzansky, & Maselko,
2004). Additionally, affect has also been found to consist of two separable and independent positive and negative dimensions (Diener & Emmons, 1984). There is evidence that negative aspects of subjective well-being, such as pessimism and negative affect are strongly related to neuroticism, whereas optimism and positive affect are related to extraversion (DeNeve &
168
Cooper, 1998; Marshall, Wortman, Kusulas, Hervig, & Vickers, 1992). Again, this parallels the findings of the present study where neuroticism strongly predicted negative SWN, whereas positive SWN was strongly predicted by agreeableness and extraversion. These parallels with subjective well-being related constructs, combined with the finding that positive and negative SWN related to different dimensions of personality suggest that these may be substantive constructs rather than artefacts.
Associations between SWN and side-effects
SWN scores, including the factors and subscales, had substantial significant negative correlations with nearly all of the side-effects scales, suggesting that severity of side-effects was associated with poorer subjective well-being. The psychic and neurological (EPS) sideeffects subscales had the largest correlations with SWN, although the autonomic and sexual subscales were moderately large. Psychic and neurological (EPS) side-effects subscales had large correlations with negative SWN and moderate correlations with positive SWN, suggesting that side-effects related more closely to the former scale. This fits in with the interpretation of negative SWN as relating to sensitivity to negative aspects of one’s experience. Interestingly, the Red Herrings scale had moderate negative correlations with all of the SWN scales. The Red Herrings scale assesses symptoms not known to relate to sideeffects of antipsychotic medication and endorsement of many of these items suggests overreporting of symptoms. When correlations between SWN scales and the side-effects subscales were adjusted for Red Herrings scores, there was a reduction in the number of significant correlations. The autonomic subscale remained significantly correlated with only two of the SWN subscales. Neurological side-effects, or EPS, remained moderately correlated with total and negative SWN, and with two subscales. Sexual side-effects remained moderately correlated with total, negative and positive SWN, and with two subscales. The psychic subscale remained significantly correlated with all of the SWN scales.
169
These results suggest that medication side-effects affecting mental alertness due to feelings of sedation have the most consistent negative impact on subjective well-being, although EPS and sexual side-effects also appear to be moderately important, particularly for negative
SWN. Claims regarding the alleged superior tolerability of SGA medications in general usually focus on the lower incidence of EPS associated with SGA compared to FGA (e.g.
Davis, Chen & Glick, 2003). While EPS appear to be important to subjective well-being, psychic side-effects, such as sedation may have a yet larger impact on subjective well-being.
A recent meta-analysis found that SGA, including olanzapine and risperidone were equivalent to FGA in regard to sedating effects (Stefan Leucht et al., 2009). This might help explain why a number of studies (e.g. Balestrieri et al., 2009) have found no apparent advantages for SGA over FGA in relation to SWN.
Notably, all of the side-effects subscales negatively affected the SWN mental functioning subscale, suggesting that reductions in the ability to think clearly are broadly associated with medication side-effects. Although side-effects, especially psychic sideeffects, were substantially negatively relayed to subjective well-being, multivariate analyses found that the contribution of side-effects became non-significant when controlling for other factors, particularly depression, health, and personality. Therefore, while controlling sideeffects may remain important for subjective well-being, it appears that other factors may have a more substantial impact in this regard.
Associations between side-effects and personality traits
All of the side-effects scales positively correlated with neuroticism. Apart from sexual side-effects, all of the remaining side-effects scales negatively correlated with extraversion, agreeableness, and conscientiousness. Multiple regression analyses controlling for all of these traits found that neuroticism alone significantly predicted total side-effects, and the psychic
170
and neurological subscales. None of the personality traits significantly predicted autonomic or sexual side-effects. The Red Herrings scale also had modest negative associations with agreeableness and conscientiousness and a modest positive association with neuroticism.
However, none of these traits predicted Red Herrings in a regression analysis. Associations between personality and side-effects could reflect biases in reporting, yet could also reflect associations between personality and physical health and well-being. Higher agreeableness and conscientiousness might be associated with more careful reporting of symptoms, hence lower scores on the Red Herrings scale. Conversely, higher neuroticism might be associated with a general tendency to complain about feelings of discomfort, perhaps due to hypervigilance about health concerns. When controlling for Red Herrings, neurological sideeffects remained moderately correlated with neuroticism, and psychic side-effects remained moderately negatively correlated with extraversion and agreeableness, and more strongly positively correlated with neuroticism. These findings suggest that at least some of the relationship between side-effects and personality might not be due to over-reporting.
Neuroticism has been found to be associated with more physical health complaints and objectively poorer long-term health in longitudinal studies (Charles, et al., 2008). Psychic side-effects in particular seem to have a robust relationship with neuroticism, suggesting that patients that are more neurotic might be more vulnerable to sedation effects and thinking difficulties in response to antipsychotic treatment. Future research might examine possible treatment implications of the relationships between personality and side-effects.
Associations between SWN and personality
Results of the present study showed that there were strong and consistent relationships between personality traits and SWN. Total and positive SWN and three subscales (mental functioning, self-control, and emotional regulation) were associated with all five personality traits. These associations were in the predicted directions, so that higher SWN was associated
171
with higher extraversion, agreeableness, conscientiousness, openness to experience, and with lower neuroticism. Social integration and physical functioning were associated with all of the personality traits except openness to experience, again in the predicted directions. Negative
SWN was significantly associated only with extraversion, agreeableness, and neuroticism.
Even though the five personality traits substantially correlated, multiple regression revealed that extraversion, agreeableness, and neuroticism remained independent predictors of total
SWN when controlling for the overlap between personality traits. Therefore, conscientiousness and openness to experience seem to be somewhat less important for predicting SWN than the three remaining factors. Multiple regression analyses also revealed that neuroticism was a significant independent predictor of the mental functioning and selfcontrol subscales, whereas extraversion and agreeableness were significant independent predictors of self-control and emotional regulation. None of the personality traits were significant independent predictors of social integration and physical functioning, even though four personality traits were significantly correlated with these subscales.
Agreeableness
In multivariate analyses, agreeableness had a stronger association with SWN, particularly positive SWN, than extraversion. In multivariate analyses of the subscales, the only personality trait that was a significant multivariate predictor was agreeableness. This indicates that when considering all five subscales together, agreeableness remained an independent predictor, after controlling for many other factors, including depression and health. This seems to suggest that agreeableness is particularly important to the subjective well-being of people with schizophrenia. Low agreeableness in people with schizophrenia appears to be associated with many interpersonal problems (Lysaker, Wilt, Plascek-Hallberg,
Brenner, & Clements, 2003a). Agreeableness appears to be important for effortful selfcontrol and regulation of negative affect, particularly anger (Jensen-Campbell et al., 2002;
172
Ode & Robinson, 2007; Ode, Robinson, & Wilkowski, 2008). A longitudinal study in the general population found that low agreeableness in adults was predicted by poor self-control, uncooperativeness, and poor socialisation in childhood and adolescence. The authors suggested that low agreeableness results from an inability to regulate emotions and behaviour. This difficulty in self-regulation leads to maladaptive behaviour and interpersonal problems. Interestingly, in the multivariate analysis of the subscales, agreeableness remained a significant predictor of self-control when controlling for the other factors. Note that the agreeableness measure used in this study did not explicitly enquire about feelings of selfcontrol, instead focusing on qualities such as kindness, cooperation, and courtesy. (See
Appendix A for specific questionnaire items.) Therefore, associations between agreeableness and self-control are unlikely to be due to simple overlap between measures. Agreeableness was also a significant predictor of emotional regulation in the multivariate analysis.
Agreeableness might be associated with SWN due to its association with the ability to regulate emotions and behaviour. Patients high in agreeableness might feel more in control of their behaviour and the way they express their emotions, and hence might have better interpersonal relationships. Patients low in agreeableness might on the other hand feel unable to regulate their emotions and behaviour, have poorer interpersonal relationships, and therefore feel more distressed. Future research could investigate self-regulation of emotions and behaviour in people with schizophrenia to determine how it relates to SWN.
Extraversion
Extraversion also emerged as a significant predictor of total and positive SWN even after controlling for many other variables including depression and health. Additionally, in the multivariate analysis of the subscales, extraversion significantly predicted emotional regulation, although it did not significantly predict any of the remaining subscales.
Extraversion is strongly associated with positive emotions and sociability in the general
173
population (Costa & McCrae, 1980; Costa & McCrae, 1992) and in people with schizophrenia (Dinzeo & Docherty, 2007). People with schizophrenia low in extraversion tend to experience more shyness and interpersonal problems (Goldberg & Schmidt, 2001) and social anhedonia (Horan, et al., 2008). Patients higher in extraversion might tend to have higher subjective well-being due to better social support, greater cheerfulness, and possibly a more positive outlook on life than those who are more introverted. The emotional regulation subscale includes items assessing optimism about the future and reduced emotionality.
Patients who are more extraverted might be dispositionally more optimistic, more engaged with positive emotions, and therefore less prone to experience lack of emotions. The fact that extraversion was not a significant predictor of the social integration subscale seems surprising considering that this scale includes items assessing feelings of shyness and ability to socialise. However, there was a trend for agreeableness to predict this subscale that neared significance. Agreeableness relates to the quality of social interaction, and therefore might be more important than extraversion in this regard. Additionally, the two other items on this subscale assess how friendly or threatening one’s environment seems, and might therefore be expected to assess specifically psychotic perceptions of being in strange or hostile surroundings. However, positive symptoms did not significantly correlate with this subscale.
The low reliability of this subscale might partly explain why it lacked strong relationships with personality traits compared to some of the other subscales.
Neuroticism
In multivariate analyses controlling for depression, neuroticism was no longer a significant predictor of any of the individual SWN scales, in spite of large correlations with many of the scales, particularly negative SWN. The strong relationship between neuroticism and depression might account for this. Neuroticism is a risk factor for depression (Kendler, et al., 2006; Lysaker, et al., 1999a) and there is evidence that they share a common underlying
174
genetic liability (Kendler & Myers, 2010). Mediation analysis suggested that because neuroticism predicts both depression and SWN, and depression predicts low SWN, depression might mediate the relationship between neuroticism and SWN. When neuroticism and depression only were entered into regression analysis, the relationship between neuroticism and SWN was reduced somewhat but still remained significant. This suggests that the relationship between SWN and neuroticism is partly but not completely due to overlap with depression. Neuroticism also strongly correlated with other personality traits in this study, including extraversion and agreeableness. When these traits, along with a number of other factors, were entered into a combined analysis, neuroticism was no longer a significant predictor of SWN. This suggests that the relationship between neuroticism and
SWN also partly relates to the overlap between neuroticism and these other traits.
Neuroticism is associated with negative emotions and a pessimistic view of life (Costa &
McCrae, 1980) and in people with schizophrenia tends to be associated with social anxiety
(Horan, et al., 2008) and fewer interpersonal relationships (Dinzeo & Docherty, 2007).
Therefore, patients high in neuroticism may tend to have low SWN for a range of interacting reasons, such as poorer social support and more depression.
Conscientiousness
Conscientiousness and openness to experience did not significantly relate to any of the SWN scales when controlling for the other personality traits. Conscientiousness tends to be related to persistence in striving for goals, particularly in academic and occupational domains (Costa & McCrae, 1992). It therefore might not be especially relevant to subjective well-being in this population, many of whom are not working or studying. Furthermore, very few participants appeared to have detailed long term goals, as revealed during PANSS interviews. As conscientiousness is thought to be associated with impulse control in people with schizophrenia (Dinzeo & Docherty, 2007) one might have expected that
175
conscientiousness would be especially relevant to the self-control subscale. However, in the present study, conscientiousness had a strong positive relationship with agreeableness, and the latter trait was a significant predictor of this subscale. Agreeableness appears to be more important for self-control than conscientiousness in this sample.
Openness to experience
Openness to experience is associated with awareness of one’s thoughts and feelings
(Costa & McCrae, 1992). The trends connecting this trait with mental functioning and emotional regulation suggest that higher openness to experience might have a modest protective effect against reductions in emotionality and clear thinking. However, extraversion, agreeableness and neuroticism seem to play roles that are more prominent in this regard, perhaps because these latter traits have stronger relationships with positive and negative emotions. As noted previously, openness to experience was moderately associated with neurocognitive test performance. Openness to experience in people with schizophrenia may be more important as a marker of intellectual ability (Dinzeo & Docherty, 2007) than of subjective well-being.
According to Diener (1984) theories of subjective well-being distinguish between topdown and bottom-up approaches. From a bottom-up perspective, happiness represents an accumulation of happy experiences. Bottom-up influences include broad situational factors, including health and marital status, factors associated with better SWN in the present study.
In the top-down view, global features of personality influence the way a person perceives events. Individuals may therefore have a global tendency to perceive life in a consistently positive or negative manner, depending on their personality traits (DeNeve, 1999). The two
SWN factors found in the present study may therefore represent global tendencies to view one’s experiences and day-to-day psychosocial functioning in a globally positive and/or
176
negative manner respectively. The way a person views the self, that is, their self-esteem, is strongly associated with personality traits (Robins, Tracy, Trzesniewski, Potter, & Gosling,
2001), and therefore personality traits may influence the perception of subtle aspects of the self that are assessed by SWN. Research examining the relationship between the SWN factors and the positive and negative dimensions of self-esteem is a potentially interesting avenue of enquiry.
Naber (1995) originally developed the SWN scale to assess aspects of patients’ functioning that are sensitive to neuroleptic treatment, such as feelings of sedation. It seems plausible that stable features of personality may influence how an individual responds to neuroleptic treatment, particularly over the long-term. There is evidence that people high in neuroticism, for example, are more prone to complain of common physical symptoms and distress (Williams, O'Brien, & Colder, 2004). In the current study, neuroticism was a significant predictor of side-effects, even though side-effects presumably relate to pharmacological factors. This suggests that neurotic traits may exacerbate some of the adverse effects of medications.
Could SWN be related to a General Factor of Personality?
As noted, total and positive SWN correlated with all five personality traits, and so were four of the subscales. Furthermore, all the personality traits moderately to strongly correlated with each other. Although proponents of the five-factor model of personality have argued that the factors are basic and independent (Costa & McCrae, 1992), small to moderate correlations between the factors have been replicated in the general population (e.g. Steel, et al., 2008), although they tend not to be as large as in the current study. A number of researchers have proposed the existence of a general factor of personality (GFP) positively associated with extraversion, agreeableness, conscientiousness, openness to experience, and
177
negatively with neuroticism (Erdle, Gosling, & Potter, 2009; Musek, 2007). The GFP appears to be a combination of positively valued personality dimensions and has been found to be correlated with self-esteem, satisfaction with life and happiness (Musek, 2007). Therefore, in the present study it appears that SWN relates to some degree to positively valued personality dimensions. Positive SWN correlated with all the big Five whereas negative SWN significantly correlated with only extraversion, agreeableness and neuroticism. Positive SWN might be more closely related to the GFP than negative SWN. Because these dimensions of personality are positively valued, the possibility that social desirability influenced SWN scores needs to be considered. It is possible that participants who wished to present a positive self-image gave biased responses to indicate higher SWN and more positive personality traits. The present study cannot address to what extent social desirability influenced the results. However, Rushton and Erdle (2010) found that the relationship between the GFP, self-esteem, and subjective well-being (high positive affect and low negative affect) remained significant even when controlling for social desirability. These results suggested that the relationship between positively valued aspects of personality and subjective well-being is not simply an artefact of socially desirable responding. Future research controlling for social desirability, for example by incorporating measures of impression management, would help determine to what extent SWN relates to social desirability.
SWN and depression
The present study confirmed previous research findings of consistent negative relationships between SWN and depression (e.g. Kim, et al., 2010). In the present study, the correlation between SWN and depression was extremely large, and depression remained a significant predictor of SWN in nearly all multivariate analyses. Depression was the only significant multivariate predictor of negative SWN, but did not predict positive SWN. The depression measure used in the present study includes items related to hopelessness and
178
anhedonia. Low SWN may therefore share certain features in common with depression, such as hopelessness, and reductions in emotionality and mental functioning. Naber (1995) proposed that side-effects of antipsychotic drugs include difficulties with thinking and feeling that have a detrimental effect on the patient’s subjective well-being. This syndrome has been referred to as ‘pharmacogenic depression’ and also ‘neuroleptic induced deficit syndrome’, among other things, and therefore it seems plausible that this strongly overlaps with depression as assessed by the DASS. The causal relationship between SWN and depression is not yet known (Kim, et al., 2010) and it is possible that depression in schizophrenia and low
SWN may, at least in some cases, have a common underlying cause.
Furthermore, although anxiety and stress had large correlations with SWN, these variables became non-significant when controlling for depression. Depression and anxiety have been found to share a common core of negative affect (Brown, Chorpita, Korotitsch, &
Barlow, 1997). Depression, however, seems to involve certain core symptoms not found in anxiety. Core symptoms of depression include anhedonia and depressive slowing of both motor and cognitive functions (Clark & Watson, 1991). Anhedonia in schizophrenia has been linked to use of antipsychotic drugs and it was proposed that anhedonia may result from drug interference with the mesolimbic dopamine reward system (Harrow, et al., 1994). However, anhedonia in schizophrenia appears to be a stable characteristic that is relatively independent of symptom status and may reflect stable features of personality, such as low extraversion
(Horan, et al., 2008). Furthermore, depression in schizophrenia can manifest without anhedonia being present (Harrow, et al., 1994). Depression in schizophrenia is highly prevalent (Sands & Harrow, 1999) and probably has multiple causes (Harrow, et al., 1994).
179
Additional factors associated with SWN
Health
Results of multivariate analyses showed that additional significant predictors of total
SWN were self-assessed health and cognitive/disorganised symptoms. Health had a large effect on total SWN, as well as positive SWN and mental functioning. It had moderate sized effects on emotional regulation and physical functioning. The direction of causality is unknown, so it is possible that better health improves one’s overall sense of well-being; or that higher SWN leads to perceptions of better health; or that both share an underlying cause.
There is evidence from the general population that positive emotions have a beneficial influence on subsequent health and on recovery from disease (Pressman & Cohen, 2005). The present study did not assess whether SWN is associated with positive emotions, but considering the robust relationship between extraversion and SWN, it seems reasonable to speculate that positive emotions could have a beneficial influence on SWN, especially positive SWN, and on health. Health had moderate relationships with all the personality traits in positively valued directions (that is, negatively with neuroticism and positively with the other four). However, none of the personality traits significantly predicted health in a multiple regression analysis, suggesting that self-ratings of health are to some extent independent of personality traits. Health had moderate negative relations with depression, anxiety, and stress, and all of the side-effect scales. Therefore, not surprisingly, those who rated their health better were less distressed and less troubled by side-effects. However, health predicted SWN, particularly positive SWN, independently of these factors. The singleitem measure of health used in the present study has been validated in the general population and has been found to be reliably correlated with physician ratings of health (Okun &
George, 1984). However, its relationship to objective health status in people with psychotic disorders is unknown, although a previous study used a global self-rating of health in people
180
with schizophrenia (Theme-Filha, Szwarcwald, & Souza-Junior, 2005). Therefore, future studies could assess how the relationship between SWN and objective indices of health status. Furthermore, the self-assessed health measure used in the present study did not specify physical or mental health. Future research could clarify whether self-ratings of physical and of mental health relate to SWN in similar ways.
Cognitive/disorganised symptoms
Cognitive/disorganised symptoms were associated with moderately worse SWN, and in multivariate analyses had a medium sized effect on total SWN and the self-control subscale. Cognitive/disorganised symptoms are a specific feature of schizophrenia psychopathology and the findings of the present study suggest that these symptoms have a more important impact on SWN than positive or negative symptoms. Cognitive/disorganised symptoms had a substantial negative association with neurocognitive performance, and the latter had a modest association with subjective well-being as well. Both cognitive/disorganised symptoms and deficits in neurocognition in schizophrenia seem to reflect frontal lobe impairment (Glahn et al., 2005; Liddle et al., 1992; Liddle & Morris,
1991). Research using neural imaging, such as functional magnetic resonance imaging studies, may help elucidate possible relationships between subjective well-being and frontal lobe functioning.
Exercise
Ratings of health and exercise moderately correlated, although exercise became nonsignificant in the final analyses. Exercise had a moderate negative relationship with neuroticism, indicating that less neurotic patients reported doing more exercise. Exercise did not significantly relate to depression, anxiety, or stress. However, it was significantly negatively related to total side-effects and all of the subscales except sexual, indicating that people who reported exercising more experienced fewer side-effects. The causal relationship
181
here is of course unknown, as it is possible that people with more severe side-effects are less inclined to do exercise. There is evidence that engaging an exercise program can have a beneficial impact on one’s daily mood (Lyubomirsky, Sheldon, & Schkade, 2005). It remains to be seen whether encouraging patients to increase their daily exercise would have a beneficial impact on SWN, especially over a longer time course.
SWN and attitudes towards adherence
The present study found that attitudes to adherence only modestly and negatively related to SWN scores at baseline. Most of these correlations did not reach statistical significance, although there were significant negative correlations between willingness to adhere to medication and negative SWN and social integration. These findings appear contrary to previous research findings that improvements in SWN are positively related to subsequent adherence to treatment assessed using both physician and self-ratings (Karow et al., 2007). However, it is worth noting that another study examining SWN in relation to attitudes towards adherence found that changes in SWN scores were not significant predictors of attitudes to adherence at discharge (Schennach-Wolff et al., 2009). The Schennach-Wolff et al. study found that reductions in psychopathology and greater insight into mental illness were significant predictors of positive attitudes to adherence. This accords with the finding of the present study that attitudes to adherence strongly related to insight. The study by Karow et al. examined adherence to oral medication, whereas the present study primarily focused on
LAI treatment. LAI treatment is generally indicated in patients who have difficulty adhering to oral medication, and the use of long-acting injections is a way of ensuring adherence, provided the patient shows up for regular appointments. There is evidence that adherence to
LAI medication among outpatients tends to be very high (Heyscue, Levin, & Merrick, 1998).
Furthermore, most of the patients in the present study were inpatients and therefore had less choice about adhering to treatment. It is possible that SWN may more closely relate to
182
attitudes to adherence in patients treated only with oral antipsychotics, and that in LAI-treated patients SWN is less relevant to attitudes to adherence. The fact that SWN tended to be negatively rather than positively related to attitudes to adherence, albeit modestly, suggests that patients with poorer subjective quality of life seem to be more likely to see the need for treatment perhaps because they are more distressed. Willingness to adhere to medication modestly positively correlated with anxiety and stress, suggesting that distress may actually motivate patients to some extent to accept treatment. This might be the case if patients believe that antipsychotic medication helps reduce their anxiety for example, although this needs to be tested empirically.
The relationship between SWN and attitudes to adherence could have been so weak in the present study because the patients might have attributed their subjective well-being mainly to factors other than their medication. The SWN scale does not mention medication effects and it is possible that most patients in long-term maintenance therapy might not see medication as an important influence on aspects of their mental and emotional functioning assessed by the SWN. Therefore, they might not see the relevance of medication adherence or non-adherence to their subjective well-being.
Findings from follow up study
Stability of SWN
Results from the follow up survey showed that SWN scale scores tended to remain highly stable more than three months after the original assessment, as shown by strong to very strong correlations between baseline and follow up scores. This finding accords with that of Lambert et al. (2009) who found that baseline SWN score was a strong predictor of
SWN score three years later. In fact, membership of the stable high SWN cluster in Lambert et al.’s study was predicted solely by high baseline SWN. Lambert et al. also found that the
183
majority of patients tended to remain in stable clusters, although there was a subset of patients who moved from a lower to a higher cluster over time. Of the 21 patients who were followed up in the present study, 17 (81% of the sample) remained in the same cluster (low, medium, or high) they were in at baseline, two improved, and two worsened. Furthermore, depression, anxiety, total side-effects, and neurological and autonomic side-effects scores tended to remain quite stable as well. Previous research suggests that personality traits remain stable over time in people with schizophrenia independently of fluctuations in clinical status
(Kentros, et al., 1997a). Stability of personality traits was not assessed in the present study.
Assuming the stability of personality traits as well, the stability of SWN probably relates to the stability of its main predictors including depression.
Changes in SWN inversely associated with changes in depression, anxiety and side-effects
Interestingly, changes in SWN scores, particularly the total score and negative SWN, negatively correlated with changes in depression, anxiety, and side-effects. This suggests that decreases in depression, anxiety, and side-effects were associated with improvements in
SWN. Notably, changes in negative SWN had strong associations with changes in depression and side-effects (particularly psychic side-effects). Total SWN change was strongly associated with changes in EPS, whereas negative SWN change had a much more modest association. Changes in positive SWN on the other hand were unrelated to changes in depression, although there was a strong association between positive SWN changes and change in EPS. These findings suggest that negative SWN is sensitive to changes in depression and total side-effects, whereas positive SWN appears to be more sensitive to changes in EPS. This accords with the finding that depression was a strong predictor of negative SWN but not of positive SWN. It also suggests that psychic side-effects, for example, feelings of sedation, are particularly important to negative SWN, whereas EPS, such as the common neuroleptic-induced movement disorders are particularly important to
184
positive SWN. Psychic side-effects also negatively correlated with emotional regulation as well as social integration. Perhaps the emotional regulation subscale is sensitive to feelings associated with ‘pharmacogenic depression’ such as reductions in emotionality and drive that appear to be associated with psychic side-effects. EPS were strongly negatively associated with social integration and physical functioning. Perhaps EPS interfere with one’s ability to enjoy day-today activities, such as socialising or physical activity that may be important to positive SWN. Schimmelmann et al. (2005) found that changes in sexual side-effects over treatment predicted SWN at endpoint. Although the correlation between SWN change and changes in sexual side-effects did not reach significance in the present study, the correlation was of moderate to large size. Schimmelmann et al. found that baseline neurological sideeffects, predicted endpoint SWN, but apparently, change in neurological side-effects was not a significant predictor in their study. This contrasts with the present results that showed that change in both neurological and psychic side-effects had a substantial association with changes in SWN over treatment.
SWN and psychopathology
There was mixed evidence concerning the relationships between changes in psychopathology and changes in SWN scales. Negative SWN change negatively correlated with changes in positive symptoms and total PANSS score. This suggests that reductions in psychopathology, particularly in positive symptoms are beneficial for negative SWN, whereas exacerbation of these symptoms is accompanied by worsened negative SWN. This accords with the finding of Schimmelman et al. (2005) that reductions in positive symptoms over treatment were modestly correlated with improvements in SWN. Negative SWN seems to be associated with sensitivity to negative aspects of one’s experience. Research suggests that high neuroticism in schizophrenia is associated with a tendency to react negatively to psychotic experiences (Dinzeo & Docherty, 2007). Negative SWN was associated with
185
neuroticism in the present study, and therefore, the association between changes in positive symptoms and negative SWN might be associated with these neurotic tendencies to make negative appraisals of abnormal perceptual experiences. On the other hand, changes in the self-control scale seemed to have a mixed relationship with changes in psychopathology, as changes in this subscale were positively associated with changes in positive symptoms, but negatively associated with changes in cognitive/disorganised symptoms. It seems very understandable that worsening of cognitive/disorganised symptoms would be associated with reductions in one’s sense of self-control. However, it seems puzzling that increases in positive symptoms would lead to a heightened sense of self-control. There was also a substantial trend for changes in positive SWN to positively relate to changes in positive symptoms, suggesting that increases in positive symptoms are associated with improvements in positive SWN, quite the opposite trend that was found for negative SWN. It is possible that the relationship between positive symptoms and SWN could depend on the content of the symptoms. For example, delusional ideas about having special status could increase one’s self-esteem and therefore improve positive SWN, whereas delusions of persecution or hearing abusive voices could have an opposite effect and worsen negative SWN in particular.
This accords with findings by Karow, Schäfer, Hirdes, Osterwald, and Naber that certain kinds of positive symptoms such as grandiosity are less distressing than symptoms such as command hallucinations (2008).
Note also that mean changes in positive symptoms were very small (less than one point on a seven-point scale). Furthermore, out of the large number of possible correlations between changes in PANSS factors and changes in SWN scales (48 in total) only four reached significance and the majority were small to negligible. Correlations between total
SWN change and PANSS changes ranged from negligible to modest. Therefore, some of the significant correlations may reflect Type II error rather than true relationships.
186
SWN and neurocognitive performance
Relationships between changes in SWN scales and changes in neurocognitive functioning as measured by the RBANS were also somewhat inconsistent and there were few significant relationships out of a large possible number. Most of the significant relationships were in the negative direction indicating an unexpected finding that improvements in neurocognition were associated with worsening of SWN. For example, emotional regulation was negatively associated with improvements in delayed memory and total RBANS score.
This is spite of the fact that at baseline better neurocognitive functioning was generally associated with better SWN. Furthermore, improvements in visuospatial skills were associated with worsening of negative SWN but improvement in mental functioning. It is possible that improvements in neurocognitive functioning might be detrimental to some features of SWN, perhaps due to increasing awareness of one’s difficulties, but this would seem to contradict the positive association between SWN and neurocognitive functioning found at baseline. Once again, some of the significant correlations may reflect Type II error rather than true relationships.
Patients in the SGA LAI group scored significantly higher on delayed memory scores at follow up compared to those in the FGA LAI group. No other differences were significant.
Regarding, changes in scores between baseline and follow up, there were significant improvements in language skills and general cognitive ability as assessed by total RBANS score compared to baseline. Differences between LAI groups in changes in performance from baseline to follow up were mostly small to negligible. Previous research suggests that antipsychotic treatment, including FGA treatment can have modest beneficial effects on cognition (e.g. Keefe, et al., 2007). Practice effects are one possible explanation, though it would seem remarkable if one practice could have a beneficial effect several months later.
The present results seem to suggest, albeit tentatively, that even patients in long-term
187
maintenance therapy can experience improvements in neurocognitive functioning, even though these tend to be modest, in accordance with findings by Gurpegui (2007) that improvements can occur in chronic patients.
Proposed model of factors influencing SWN
Ritsner et al. (2002) proposed a model in which subjective quality of life is influenced by the interplay of objective aspects of quality of life, protective factors (such as social support, coping strategies, self-esteem, and insight), and distress/clinical factors (such as psychological distress, adverse effects of medication, and psychopathology). Interestingly,
Ritsner et al. found that side-effects had less impact on subjective quality of life than psychosocial and clinical factors. Based on the findings of the current study, it is possible to propose a model of factors affecting subjective well-being somewhat similar to that proposed by Ritsner et al. Due to the design of the current study this is not a causal model, and it is possible that the direction of causation between the proposed factors and SWN is bidirectional.
In the current study, protective factors associated with higher subjective well-being included self-assessed health as well as personality traits, particularly agreeableness and extraversion. Distress/clinical factors included neuroticism, depression, and cognitive/disorganised symptoms. Side-effects had an adverse association with subjective well-being, particularly the negative aspects, but were less important for the positive aspects or global subjective well-being. This finding tends to support the finding by Ritsner et al.
(2002) that side-effects appear to have less impact on quality of life than a number of other psychosocial and clinical factors. There was evidence that being married can have a beneficial impact on subjective well-being, but this conclusion is somewhat tentative due to the small number of married participants in the current study. Very few of the participants
188
who had ever been married were male and therefore it was not possible to determine if being married was more beneficial to one gender or the other.
The factors identified in the present study might affect patients’ subjective well-being through both direct and indirect pathways. Personality traits could influence subjective wellbeing directly through their association with self-esteem and with positive and negative emotions and also indirectly through their impact on interpersonal relationships and healthrelated behaviour. For example, neuroticism in the present study was associated with more cigarette smoking and less exercise, health-related behaviours that seemed to affect SWN.
Cognitive/disorganised symptoms could also have both direct and indirect effects on SWN.
Perhaps the neurological abnormalities associated with cognitive/disorganised symptoms have a direct relationship with the experience of subjective dysphoria in schizophrenia, although this has not been investigated. A consequence of these symptoms could be that patients perceive their own difficulty in thinking and acting normally, with adverse effects on their sense of well-being. Additionally, bizarre speech and behaviour may place a strain on their interpersonal relationships, as well as having an adverse effect on psychosocial functioning that could be detrimental to SWN.
Ritsner et al. (2002) proposed that psychosocial factors influence subjective quality of life, but studies to date do not appear to have examined how psychosocial factors might influence SWN. The present study found that never married patients had lower subjective well-being than those who had been or were married. Due to the small number of married participants in the current study, conclusions about the relationship of marital status to SWN must remain tentative. Future studies could examine marital status and SWN in larger samples. Additionally, other psychosocial factors relating to family support and friendship networks, as well as access to support services have not been examined.
189
Insight and distress
Insight in the current study was not significantly associated with overall subjective well-being, and actually had a negative association with the self-control subscale and negative SWN. This seems to contradict the proposal by Ritsner et al. (2002) that insight is a protective factor in regards to subjective quality of life. Insight is an important treatment consideration as patients with better insight are more likely to cooperate with treatment and to have better psychosocial functioning (Staring, Van der Gaag, Van den Berge,
Duivenvoorden, & Mulder, 2009). In accordance with these findings, insight in the present study was associated with more positive attitudes to treatment adherence. However, a number of previous studies have found that insight into mental illness is associated with greater distress, perhaps because of the stigma associated with schizophrenia (M. Cooke et al., 2007).
In the present study, insight was positively associated with higher neuroticism and higher anxiety and stress but not depression. Previous research on insight has found that poor insight is associated with self-deception (Moore, Cassidy, Carr, & O'Callaghan, 1999) and higher self-esteem (M. A. Cooke et al., 2007). Neuroticism is associated with lower self-esteem
(Robins, et al., 2001) and hence with a more negative view of oneself. Patients that are more neurotic may therefore be more willing to acknowledge unpleasant truths about themselves.
Denial of mental illness on the other hand may allow some patients to maintain a more positive view of the self. A study on hope and insight suggested that good insight combined with lack of hope is associated with poor adaptive coping whereas good insight combined with high hope is associated with highly adaptive coping (Lysaker, Campbell, & Johannesen,
2005). Therefore, insight may be a protective factor as long as it is associated with optimism about the future rather than despair. Furthermore, stigma may influence the relationship between insight and distress (Staring, et al., 2009). Good insight combined with stigmatising beliefs, such as the idea that having a psychiatric illness is a sign of personal failure, was
190
found to be associated with low self-esteem, depression, and poor quality of life. On the other hand, patients with good insight who do not have such stigmatising beliefs are less likely to have such poor outcomes. Therefore, attempts by clinicians to improve insight may need to address stigma and help patients maintain self-esteem (Staring, et al., 2009).
Strengths and limitations of the present study
The naturalistic design of the present study has both advantages and disadvantages.
Naturalistic studies present a more accurate portrayal of the realities of clinical practice than
Randomised Controlled Trials (RCTs). RCTs tend to have highly selective inclusion criteria and therefore do not always present a representative cross-section of the patient population.
The present study, like most naturalistic studies, had few exclusion criteria and therefore is more likely to have a representative sample of the population concerned. Additionally, RCTs normally restrict patient treatment options to antipsychotic monotherapy, whereas polypharmacy appears to be the rule in current clinical practice. A disadvantage of naturalistic designs is that inferences about causality cannot be made. Additionally, the practice of polypharmacy, while a clinical reality, makes it difficult to separate possible influences of oral versus LAI medications. Furthermore, the sample size was relatively small, making it difficult to differentiate between treatment subgroups. LAI monotherapy patients were under-represented in the present study due to the low proportion of patients who receive this kind of treatment in routine practice. Follow up assessments were often difficult to conduct in the present study, because most patients assessed at baseline were seen in inpatient settings, and most of these were subsequently discharged into the community and hence became difficult to contact for follow up assessment. As a result, the follow up sample was rather small. A strength of this study was that psychopathology was assessed using a fivefactor model of PANSS symptoms rather than the older three-factor model, which assesses positive and negative symptoms, and ‘general psychopathology.’ Previous SWN studies, such
191
as Naber et al. (2001) reported relationships between SWN and ‘general psychopathology’, which term encompasses disturbances in mood, cognition, and hostility. The present study examined the relationship between SWN and more specific symptoms than ‘general psychopathology’, such as cognitive/disorganised, affective, and hostile excitement symptoms.
There may be both strengths and limitations to the use of the SWN measure itself as an indicator of subjective quality of life, as opposed to the use of related measures. A feature of the SWN is that it was intended to assess subjective response independently of patient attributions about the causes of their distress or well-being (Naber, 2005). Naber (2005) argued that causal attributions should be assessed separately from subjective well-being. On the other hand, Wolters et al. (2006) argued that the SWN lacks validity as a measure of subjective response to antipsychotics because it does not mention any relationship with antipsychotic medication. Wolters et al. (2006) argued that their instrument, the Subjective
Response to Antipsychotics questionnaire (SRA) is a more valid measure of medication effects because it specifically enquires about patient attributions of changes in their subjective state to medication. Wolters et al. (2009) found that the SWN correlated more strongly with a generic measure of quality of life than the SRA scales. Subjective quality of life appears to be an important outcome in its own right and therefore the SWN may be a more valid measure of this construct than the SRA. On the other hand, the SRA does measure specific outcomes with important health implications, such as weight gain, that the SWN does not. Future research might consider whether responses to the SRA are associated with any of the same variables associated with SWN or self-reported side-effects, such as depression and personality. Patients who are depressed or high on neuroticism might self-report more adverse effects compared to euthymic or emotionally stable patients.
192
Another issue concerns the sensitivity of the SWN to change compared to other instruments. Lambert et al. (2009) found that the majority of patients fell into clusters that maintained relatively stable subjective well-being over a three year period, whereas about
20% steadily improved over time. Whether the stability of SWN in most patients is due to a feature of the instrument itself, patient features, treatment factors or other factors remains unclear. Voruganti and Awad (2002) found that patients reported significant changes in scores on the PETiT, a self-report measure of subjective response to treatment, after six months and again after 12 months. However, the authors did not report what proportion of patients actually did experience clinically significant improvement over treatment and what proportion may have remained stable. Future research could compare the stability versus sensitivity to change of instruments such as the PETiT with the SWN. If the PETiT proved to be more sensitive to change than the SWN, it might be more useful as a measure of response to treatment.
Clinical implications and future directions
Findings from the present study suggest that whether a patient in long-term maintenance treatment is treated with an FGA or an SGA medication may have little impact on their subjective well-being, perhaps because individual factors play a large role in influencing their subjective quality of life. Considering the greater expense of SGA compared to FGA medication, as well as the adverse metabolic effects of SGA medication, it might be worth reconsidering the place of these newer more expensive drugs in the treatment of schizophrenia. It is possible that many patients in long-term maintenance therapy may be able to achieve satisfactory levels of subjective well-being even with FGA treatment.
The findings seem to suggest that antipsychotic monotherapy may be more beneficial for the patient’s subjective well-being than polypharmacy. Future studies with larger samples
193
are needed to determine to what extent monotherapy patients differ in SWN from polypharmacy patients. Additionally, there was tentative evidence that the combination of an
LAI SGA with oral olanzapine seemed to be particularly unfortunate compared to other treatment options. Research examining the impact of specific polypharmacy combinations from the patient’s perspective appear to be lacking and are therefore important considering the prevalence of polypharmacy.
The present study confirmed previous research findings that depression has a strong negative relationship with SWN. In fact, depression, seemed to have a stronger impact than anxiety or stress, and there may be considerable conceptual overlap between depression and
SWN. Research is needed to determine the nature of the causal relationship between depression and SWN, and to assess whether treatment of depression improves SWN. The findings of the present study also suggest that although side-effect severity has a negative impact on SWN, a number of other factors seem to have a more substantial impact. Selfassessed health and personality traits, particularly agreeableness, extraversion, and neuroticism, seem to have large effects on SWN. There is evidence that SWN tends to be fairly stable, and this stability could relate to the stability of personality traits. However, depression was also relatively stable in the present sample, and changes in SWN and in depression were strongly associated. Personality traits, particularly neuroticism, are associated with vulnerability to depression, therefore the stability of depression in the present sample may also have been related to stable personality traits. Therefore, treatment interventions aimed at improving SWN may therefore need to consider and possibly be tailored to the patient’s personality traits. Additionally, there was evidence that exercise had a beneficial impact on SWN. Therefore, exercise programs might be investigated as a treatment option for improving SWN.
194
Exploratory factor analysis suggested that the SWN scale was best represented by two correlated dimensions, one representing negative aspects of subjective well-being, the other representing positive aspects of subjective well-being. Negative SWN was more strongly associated with neuroticism, depression and to a lesser extent total side-effects, whereas positive SWN was more strongly associated with health, agreeableness, and extraversion.
Further research is needed to confirm whether this factor structure can be replicated. Perhaps this factor structure is applicable mainly to patients in long-term maintenance therapy and may or may not generalise to other patient groups. Furthermore, the five subscales developed by Naber (1995) did not appear to match the factor structure of the SWN, and most of the subscales had rather low internal consistency. This finding contrasts somewhat with that of de Haan et al. (2002), who found that most of the subscales (apart from self-control) had reasonably acceptable internal consistency (α ranging from .68 - .84). The sample study by de
Haan et al. was considerably younger (mean age 21 years) than the present sample. The subscales may be less reliable in older, chronically ill samples, such as in the present study.
The personality traits assessed in the present study are very broad personality characteristics that subsume narrower traits. For example, extraversion comprises facets of assertiveness, sociability and excitement seeking. Research could examine the relationship between these narrower traits and SWN. It is possible that sociability, for example, may be more important for SWN than assertiveness. Self-regulation is thought to underlie agreeableness (Laursen, Pulkkinen, & Adams, 2002), a robust predictor of SWN. Research could examine more directly the relationship between a person’s capacity for self-regulation of emotions and behaviour and their SWN. As noted previously the influence of personality on subjective well-being may be both direct and indirect. For example, agreeableness could influence SWN directly through the person’s capacity for self-regulation, and also indirectly through the impact of interpersonal behaviour on the person’s quality of relationships. Future
195
research could therefore examine both these direct and indirect influences on SWN. Research has found that aspects of cognitive function can be improved through training interventions
(Bender et al., 2004) and that this training was associated with improvements in SWN. The possibility that self-regulation could also be improved through training interventions should be explored. If improvements in self-regulation were associated with improvements in SWN, this would shed some light on the mechanisms that underlie subjective well-being in this population.
Both personality traits and depression are strongly associated with self-esteem. The present study did not assess participants’ self-esteem and therefore future studies could examine whether self-esteem has an influence on SWN that is independent of the influence of personality traits and of depression. Furthermore, the possibility that socially desirable responding may influence SWN scores needs to be examined as this would clarify how valid self-report measures are in assessing subjective aspects of quality of life.
Conclusion: Putting SWN in perspective
Subjective well-being as a treatment outcome appears to be important in its own right because subjective well-being is sensitive to patient distress, particularly depression and to some extent to adverse side-effects. Additionally, there is evidence that baseline subjective well-being and early improvements in subjective well-being can predict remission of psychiatric symptoms at discharge (Schennach-Wolff et al., 2010). However, the importance of subjective quality of life needs to be considered in relation to other treatment outcomes, such as psychosocial functioning and symptom reduction (Naber & Vita, 2004). A potential limitation of subjective well-being as an outcome measure is that patients who are not distressed by their symptoms, such as those with grandiose delusions, may perceive that they have adequate subjective well-being (Karow, Schäfer, Hirdes, Osterwald, & Naber, 2008).
196
Lambert et al. (2009) suggested that patients with manic symptoms may have elevated subjective well-being that reflects their euphoric state. In the present study, patients diagnosed with schizoaffective disorder had higher subjective well-being than those diagnosed with schizophrenia, which may have reflected the presence of manic symptoms.
Therefore, subjective well-being as an outcome measure may be of limited usefulness for certain patient groups.
Naber and Vita (2004) proposed that schizophrenia treatment should consider six overlapping yet distinct outcome domains, of which subjective well-being is one. These domains are symptoms, tolerability, everyday functioning, subjective well-being, family/caregiver burden, and treatment adherence. See Figure 5 (reproduced from Naber & Vita, 2004).
The present study primarily focused on subjective well-being and was not able to address some of these domains. Although a number of studies have examined how subjective
197
well-being relates to symptoms of disease, treatment adherence and tolerability of treatment, there does not appear to have been any research addressing relationships between everyday functioning and family/carer burden. Additionally, Naber and Vita (2004) argued that factors influencing each outcome are likely to include patient-related, disease-related, treatmentrelated, family-related, and health system-related variables. Research on SWN began by particularly focusing on treatment-related factors, especially the specific kind of antipsychotic treatment, although disease-related factors, that is, symptoms, have also been addressed. The present study has provided evidence that patient-related factors, that is, personality traits, appear to play an important role in influencing the domain of subjective well-being. Additionally, the personality trait of neuroticism in particular related to sideeffect severity, an aspect of the tolerability domain. Previous research has shown that personality traits also appear to be important in disease-related domains (Dinzeo & Docherty,
2007), in everyday functioning (Kentros, et al., 1997b), and perhaps in other domains as well.
There currently appears to be a lack of research on family-related and health system-related factors that could influence subjective well-being. Furthermore, apart from studies comparing differential effects of various antipsychotic drugs, there appear to have been few studies examining interventions that could potentially improve subjective well-being (Vothknecht et al. 2011). A study on computer-based cognitive training in patients with schizophrenia found that the training not only improved cognitive functioning, but SWN as well (Bender et al.,
2004). Non-pharmacological interventions to improve subjective well-being are therefore a potentially important area for future investigation.
198
References
Allison, D. B., Mackell, J. A., & McDonnell, D. D. (2003). The Impact of Weight Gain on
Quality of Life Among Persons With Schizophrenia. Psychiatr Serv, 54 (4), 565-567.
Bagby, R. M., Bindseil, K. D., Schuller, D. R., Rector, N. A., Young, L. T., Cooke, R. G., et al. (1997). Relationship between the five-factor model of personality and unipolar, bipolar and schizophrenic patients. Psychiatry Research, 70 (2), 83-94.
Balanza, V., Merino, T., Tatay, A., Lerma, J., Cepeda, S., Laguna, L., et al. (2008). Similar subjective response and adherence rates for long-acting risperidone and conventional depots. European Psychiatry, 23 (Supplement 2), S155-S155.
Balestrieri, M., Di Sciascio, G., Isola, M., Lomonaco, E., Maso, E., Merli, R., et al. (2009).
Drug attitude and subjective well-being in antipsychotic treatment monotherapy in real-world settings. Epidemiologia e Psichiatria Sociale, 18 , 114 - 118.
Baron, R. M., & Kenny, D. A. (1986). The Moderator-Mediator Variable Distinction in
Social Psychological Research: Conceptual, Strategic, and Statistical Considerations.
Journal of Personality and Social Psychology, 51 (6), 1173-1182.
Barrowclough, C., Tarrier, N., Humphreys, L., Ward, J., Gregg, L., & Andrews, B. (2003).
Self-Esteem in Schizophrenia: Relationships Between Self-Evaluation, Family
Attitudes, and Symptomatology. J Abnorm Psychol, 112 (1), 92 - 99.
Bell, M. D., Lysaker, P. H., Beam-Goulet, J. L., Milstein, R. M., & Lindenmayer, J.-P.
(1994). Five-component model of schizophrenia: Assessing the factorial invariance of the positive and negative syndrome scale. Psychiatry Research, 52 (3), 295-303.
Berenbaum, H., & Fujita, F. (1994). Schizophrenia and personality: Exploring the boundaries and connections between vulnerability and outcome. Journal of Abnormal
Psychology, 103 , 148 - 158.
Bhanji, N. H., Chouinard, G., & Margolese, H. C. (2004). A review of compliance, depot intramuscular antipsychotics and the new long-acting injectable atypical antipsychotic risperidone in schizophrenia. European Neuropsychopharmacology, 14 (2), 87-92.
Brown, T. A., Chorpita, B. F., Korotitsch, W., & Barlow, D. H. (1997). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples.
Behaviour Research and Therapy, 35 (1), 79-89.
Camisa, K. M., Bockbrader, M. A., Lysaker, P., Rae, L. L., Brenner, C. A., & O'Donnell, B.
F. (2005). Personality traits in schizophrenia and related personality disorders.
Psychiatry Research, 133 (1), 23-33.
Casey, D. E. (2004). Pathophysiology of Antipsychotic Drug–Induced Movement Disorders.
The Journal of Clinical Psychiatry, 65 (Supplement 9), 25-28.
Casey, D. E. (2006). Implications of the CATIE Trial on Treatment: Extrapyramidal
Symptoms. CNS Spectrums, 11 (7 Suppl 7), 25-31.
Cañas, F., & Möller, H.-J. (2010). Long-acting atypical injectable antipsychotics in the treatment of schizophrenia: safety and tolerability review. Expert Opinion on Drug
Safety, 9 (5), 683-697.
Chamorro-Premuzic, T., Furnham, A., & Ackerman, P. L. (2006). Ability and personality correlates of general knowledge. Personality and Individual Differences, 41 (3), 419-
429.
Charles, S. T., Gatz, M., Kato, K., & Pedersen, N. L. (2008). Physical Health 25 Years Later:
The Predictive Ability of Neuroticism. Health Psychology, 27 (3), 369-378.
199
Citrome, L., Jaffe, A., & Levine, J. (2010). Treatment of schizophrenia with depot preparations of fluphenazine, haloperidol, and risperidone among inpatients at stateoperated psychiatric facilities. Schizophrenia Research, 119 (1 – 3), 153 – 159.
Clark, L. A., & Watson, D. (1991). Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100 (3), 316 -
336.
Cohen, J. (1992). A power primer. Psychol Bull, 112 (1), 155 - 159.
Cooke, M., Peters, E., Fannon, D., Anilkumar, A. P. P., Aasen, I., Kuipers, E., et al. (2007).
Insight, distress and coping styles in schizophrenia. Schizophrenia Research, 94 (1-3),
12-22.
Cooke, M. A., Peters, E. R., Greenwood, K. E., Fisher, P. L., Kumari, V., & Kuipers, E.
(2007). Insight in psychosis: influence of cognitive ability and self-esteem. The
British Journal of Psychiatry, 191 (3), 234-237.
Correll, C. U., Leucht, S., & Kane, J. M. (2004). Lower Risk for Tardive Dyskinesia
Associated With Second-Generation Antipsychotics: A Systematic Review of 1-Year
Studies. Am J Psychiatry, 161 (3), 414-425.
Correll, C. U., Rummel-Kluge, C., Corves, C., Kane, J. M., & Leucht, S. (2009).
Antipsychotic Combinations vs Monotherapy in Schizophrenia: A Meta-analysis of
Randomized Controlled Trials. Schizophrenia Bulletin, 35 (2), 443-457.
Costa, P. T., & McCrae, R. R. (1980). Influence of extraversion and neuroticism on subjective well-being: Happy and unhappy people. Journal of Personality and Social
Psychology, 38 (4), 668-678.
Costa, P. T., & McCrae, R. R. (1992). Revised NEO Personality Inventory and NEO Five factor Inventory. Odessa Fl: Psychological Assessment Resources .
Cuesta, M. J., Peralta, V., & Zarzuela, A. (2001). Effects of olanzapine and other antipsychotics on cognitive function in chronic schizophrenia: a longitudinal study.
Schizophrenia Research, 48 (1), 17-28.
Czernecka, K., & Szymura, B. (2008). Alexithymia - Imagination - Creativity. Personality and Individual Differences, 45 (6), 445-450.
Davis, J. M., Chen, N., & Glick, I. D. (2003). A meta-analysis of the efficacy of secondgeneration antipsychotics. Arch Gen Psychiatry, 60 , 553 - 564.
Day, J. C., Wood, G., Dewey, M., & Bentall, R. P. (1995). A self-rating scale for measuring neuroleptic side-effects. Validation in a group of schizophrenic patients. The British
Journal of Psychiatry, 166 (5), 650-653.
Dawkins, K., Lieberman, J. A., Lebowitz, B. D., & Hsiao, J. K. (1999). Antipsychotics: Past and Future National Institute of Mental Health Division of Services and Intervention
Research Workshop, July 14, 1998. Schizophrenia Bulletin, 25 (2), 395-405. de Haan, L., Nimwegen, L., Amelsvoort, T., Dingemans, P., & Linszen, D. (2008).
Improvement of subjective well-being and enduring symptomatic remission, a 5-year follow-up of first episode schizophrenia. Pharmacopsychiatry, 41 (4), 125 - 128. de Haan, L., van Bruggen, M., Lavalaye, J., Booij, J., Dingemans, P. M. A. J., & Linszen, D.
(2003). Subjective Experience and D2 Receptor Occupancy in Patients With Recent-
Onset Schizophrenia Treated With Low-Dose Olanzapine or Haloperidol: A
Randomized, Double-Blind Study. Am J Psychiatry, 160 (2), 303-309. de Haan, L., Weisfelt, M., Dingemans, P. M., & Linszen, D. H. (2002). Psychometric properties of the Subjective Well-Being Under Neuroleptics scale and the Subjective
Deficit Syndrome ScaleWouters L. Psychopharmacology (Berl), 162 (1), 24 - 28.
DeNeve, K. M. (1999). Happy as an extraverted clam? The role of personality for subjective well-being. Current Directions in Psychological Science, 8 , 141 - 144.
200
DeNeve, K. M., & Cooper, H. (1998). The Happy Personality: A Meta-Analysis of 137
Personality Traits and Subjective Well-Being. Psychological Bulletin, 124 (2), 197-
229.
DeShon, R. P., & Alexander, R. A. (1996). Alternative Procedures for Testing Regression
Slope Homogeneity When Group Error Variances Are Unequal. Psychological methods, 1 (3), 261 - 277.
Diener, E. (1984). Subjective well-being. Psychological Bulletin, 95 (3), 542 - 575.
Diener, E., & Emmons, R. A. (1984). The independence of positive and negative affect.
Journal of Personality and Social Psychology, 47 , 1105 - 1117.
Diener, E., Suh, E. M., Lucas, R. E., & Smith, H. L. (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125 (2), 276-302.
Dinesen, H., Gram, L., Andersen, T., & Dam, M. (1984). Weight gain during treatment with valproate. Acta Neurologica Scandinavica, 70 , 65 - 69.
Dinzeo, T. J. P., & Docherty, N. M. P. (2007). Normal Personality Characteristics in
Schizophrenia: A Review of the Literature Involving the FFM. Journal of Nervous &
Mental Disease, 195 (5), 421-429.
Dubisar, B. M., Stoner, S. C., Reynolds, J., Khan, R., & Ramlatchman, L. (2004). Adverse effects of atypical antipsychotic agents and their effects on quality of life.
Pharmacotherapy, 24 (7), 843 - 847.
Erdle, S., Gosling, S. D., & Potter, J. (2009). Does self-esteem account for the higher-order factors of the Big Five? Journal of Research in Personality, 43 (5), 921-922.
Faries, D., Ascher-Svanum, H., Zhu, B., Correll, C., & Kane, J. (2005). Antipsychotic monotherapy and polypharmacy in the naturalistic treatment of schizophrenia with atypical antipsychotics. BMC Psychiatry, 5 (1), 26.
Franz, M., Lis, S., Pluddemann, K., & Gallhofer, B. (1997). Conventional Versus Atypical
Neuroleptics: Subjective Quality of Life in Schizophrenic Patients. British Journal of
Psychiatry, 170 (5), 422-425.
Furukawa, T., Hori, S., Yoshida, S. i., Tsuji, M., Nakanishi, M., & Hamanaka, T. (1998).
Premorbid personality traits of patients with organic (ICD-10 F0), schizophrenic (F2), mood (F3), and neurotic (F4) disorders according to the five-factor model of personality. Psychiatry Research, 78 (3), 179-187.
Gardos, G. (2005). Antipsychotic polypharmacy or monotherapy?
Neuropsychopharmacologia Hungarica, 7 (2), 72 - 77.
Gaughan, E. T., Miller, J., D., Pryor, L., R., & Lynam, D., R. (2009). Comparing Two
Alternative Measures of General Personality in the Assessment of Psychopathy: A
Test of the NEO PI-R and the MPQ. Journal of Personality, 77 (4), 965-996.
Geddes, J., Freemantle, N., Harrison, P., & Bebbington, P. (2000). Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis.
BMJ, 321 , 1371-1376.
Gharabawi, G. M., Bossie, C. A., Zhu, Y., Mao, L., & Lasser, R. A. (2005). An assessment of emergent tardive dyskinesia and existing dyskinesia in patients receiving long-acting, injectable risperidone: Results from a long-term study. Schizophrenia Research, 77 (2-
3), 129-139.
Glahn, D. C., Ragland, J. D., Abramoff, A., Barrett, J., Laird, A. R., Bearden, C. E., et al.
(2005). Beyond hypofrontality: A quantitative meta-analysis of functional neuroimaging studies of working memory in schizophrenia. Human Brain Mapping,
25 (1), 60-69.
201
Gold, J. M., Queern, C., Iannone, V. N., & Buchanan, R. W. (1999). Repeatable Battery for the Assessment of Neuropsychological Status as a Screening Test in Schizophrenia, I:
Sensitivity, Reliability, and Validity. Am J Psychiatry, 156 (12), 1944-1950.
Goldberg, J. O., & Schmidt, L. A. (2001). Shyness, sociability, and social dysfunction in schizophrenia. Schizophrenia Research, 48 (2-3), 343-349.
Goodwin, R. D., Fergusson, D. M., & Horwood, L. J. (2003). Neuroticism in adolescence and psychotic symptoms in adulthood. Psychological Medicine, 33 (06), 1089-1097.
Guadagnoli, E., & Velicer, W. F. (1988). Relation of Sample Size to the Stability of
Component Patterns. Psychological Bulletin, 103 (265 - 275).
Gurpegui, M., Álvarez, E., Bousoño, M., Ciudad, A., Carlos Gómez, J., & Olivares, J. M.
(2007). Effect of olanzapine or risperidone treatment on some cognitive functions in a one-year follow-up of schizophrenia outpatients with prominent negative symptoms.
European Neuropsychopharmacology, 17 (11), 725-734.
Gurrera, R. J., Nestor, P. G., O'Donnell, B. F., Rosenberg, V., & McCarley, R. W. (2005).
Personality Differences in Schizophrenia Are Related to Performance on
Neuropsychological Tasks. Journal of Nervous & Mental Disease, 193 (11), 714-721.
Gurrera, R. J. M. D., Nestor, P. G. P. D., & O'Donnell, B. F. P. D. (2000). Personality Traits in Schizophrenia: Comparison with a Community Sample. Journal of Nervous &
Mental Disease, 188 (1), 31-35.
Hamann, J., Kolbe, G., Cohen, R., Leucht, S., & Kissling, W. (2005). How do psychiatrists choose among different antipsychotics? European Journal of Clinical Pharmacology,
61 (11), 851-854.
Hamann, J., Langer, B., Leucht, S., Busch, R., & Kissling, W. (2004). Medical Decision
Making in Antipsychotic Drug Choice for Schizophrenia. Am J Psychiatry, 161 (7),
1301-1304.
Hansson, L. (2006). Determinants of quality of life in people with severe mental illness. Acta psychiatrica Scandinavica, 113 (s429), 46-50.
Harrow, M., Yonan, C. A., Sands, J. R., & Marengo, J. (1994). Depression in Schizophrenia:
Are Neuroleptics, Akinesia, or Anhedonia Involved? Schizophrenia Bulletin, 20 (2),
327-338.
Heinrichs, R. W. (2007). Cognitive Improvement in Response to Antipsychotic Drugs:
Neurocognitive Effects of Antipsychotic Medications in Patients With Chronic
Schizophrenia in the CATIE Trial. Arch Gen Psychiatry, 64 (6), 631-632.
Hertling, I., Philipp, M., Dvorak, A., Glaser, T., Mast, O., Beneke, M., et al. (2003).
Flupenthixol versus risperidone: Subjective quality of life as an important factor for compliance in chronic schizophrenic patients. Neuropsychobiology, 47 (1), 37-46.
Herzberg, P. Y., Glaesmer, H., & Hoyer, J. (2006). Separating Optimism and Pessimism: A
Robust Psychometric Analysis of the Revised Life Orientation Test (LOT-R).
Psychological Assessment, 18 (4), 433 - 438.
Heyscue, B. E., Levin, G. M., & Merrick, J. P. (1998). Compliance With Depot
Antipsychotic Medication by Patients Attending Outpatient Clinics. Psychiatr Serv,
49 (9), 1232-1234.
Hobart, M. P., Goldberg, R., Bartko, J. J., & Gold, J. M. (1999). Repeatable Battery for the
Assessment of Neuropsychological Status as a Screening Test in Schizophrenia, II:
Convergent/Discriminant Validity and Diagnostic Group Comparisons. Am J
Psychiatry, 156 (12), 1951-1957.
Hogan, T. P., Awad, A. G., & Eastwood, R. (1983). A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychological
Medicine, 13 (01), 177-183.
202
Horan, W. P., Blanchard, J. J., Clark, L. A., & Green, M. F. (2008). Affective Traits in
Schizophrenia and Schizotypy. Schizophr Bull , sbn083.
Huppert, J. D., Smith, T. E., & Apfeldorf, W. J. (2002). Use of Self-Report Measures of
Anxiety and Depression in Outpatients with Schizophrenia: Reliability and Validity.
Journal of Psychopathology and Behavioral Assessment, 24 (4), 275-283.
Jan-Erik, L., Sampo, P., Markku, V., Sointu, L., Annamari, T.-H., & Jouko, L. (2007).
Personality characteristics of research volunteers. European Journal of Personality,
21 (8), 1017-1030.
Jensen-Campbell, L. A., Rosselli, M., Workman, K. A., Santisi, M., Rios, J. D., & Bojan, D.
(2002). Agreeableness, conscientiousness, and effortful control processes. Journal of
Research in Personality, 36 (5), 476-489.
John, O. P., Donahue, E. M., & Kentle, R. L. (1991). The Big Five Inventory--Versions 4a and 5a . Berkeley, CA: University of California, Berkeley, Institute of Personality and
Social Research.
Jones, P. B., Barnes, T. R. E., Davies, L., Dunn, G., Lloyd, H., Hayhurst, K. P., et al. (2006).
Randomized Controlled Trial of the Effect on Quality of Life of Second- vs First-
Generation Antipsychotic Drugs in Schizophrenia: Cost Utility of the Latest
Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry,
63 (10), 1079-1087.
Kapur, S., Zipursky, R., Jones, C., Remington, G., & Houle, S. (2000). Relationship Between
Dopamine D2 Occupancy, Clinical Response, and Side Effects: A Double-Blind PET
Study of First-Episode Schizophrenia. Am J Psychiatry, 157 (4), 514-520.
Karow, A., Czekalla, J., Dittmann, R. W., Schacht, A., Wagner, T., Lambert, M., et al.
(2007). Association of subjective well-being, symptoms, and side effects with compliance after 12 months of treatment in schizophrenia. J Clin Psychiatry, 68 (1),
75 - 80.
Karow, A., Moritz, S., Lambert, M., Schoder, S., & Krausz, M. (2005). PANSS Syndromes and quality of life in schizophrenia. [Original Paper]. Psychopathology, 38 .
Karow, A., & Naber, D. (2002). Subjective well-being and quality of life under atypical antipsychotic treatment. Psychopharmacology, 162 (1), 3 - 10.
Karow, A., Schäfer, I., Hirdes, F., Osterwald, C., & Naber, D. (2008). Positivsymptome und
Lebensqualität aus der Sicht schizophrener Patienten.
Psychiat Prax, 35 (06), 286,293.
Kay, S., R., Opler, L., A., & Fiszbein, A. (1996). Positive and Negative Syndrome Scale
(PANSS) Rating Manual . Camperdown: Brain and Mind Research Institute.
Keefe, R. S. E., Bilder, R. M., Davis, S. M., Harvey, P. D., Palmer, B. W., Gold, J. M., et al.
(2007). Neurocognitive Effects of Antipsychotic Medications in Patients With
Chronic Schizophrenia in the CATIE Trial. Arch Gen Psychiatry, 64 (6), 633-647.
Keefe, R. S. E., Silva, S. G., Perkins, D. O., & Lieberman, J. A. (1999). The effects of atypical antipsychotic drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophrenia Bulletin, 25 (2), 201 - 222.
Keefe, R. S. E., Young, C. A., Rock, S. L., Purdon, S. E., Gold, J. M., & Breier, A. (2006).
One-year double-blind study of the neurocognitive efficacy of olanzapine, risperidone, and haloperidol in schizophrenia. Schizophrenia Research, 81 (1), 1-15.
Kendler, K. S., Gatz, M., Gardner, C. O., & Pedersen, N. L. (2006). Personality and Major
Depression: A Swedish Longitudinal, Population-Based Twin Study. Arch Gen
Psychiatry, 63 (10), 1113-1120.
Kendler, K. S., & Myers, J. (2010). The genetic and environmental relationship between major depression and the five-factor model of personality. Psychological Medicine,
40 (05), 801-806.
203
Kentros, M. D., Smith, T. E., Hull, J., McKee, M., Terkelsen, K., & Capalbo, C. (1997a).
Stability of Personality Traits in Schizophrenia and Schizoaffective Disorder: A Pilot
Project. Journal of Nervous & Mental Disease, 185 (9), 549-555.
Kentros, M. D., Terkelsen, K., Hull, J., Smith, T. E., & Goodman, M. (1997b). The relationship between personality and quality of life in persons with schizoaffective disorder and schizophrenia. Quality of Life Research, 6 , 118 - 122.
Kim, J. H., Ann, J. H., & Kim, J. H. (2011). Relationship between improvements of subjective well-being and depressive symptoms during acute treatment of schizophrenia with atypical antipsychotics. Journal of Clinical Pharmacy and
Therapeutics, 36 (2), 172 -178.
Kim, J. H., Ann, J. H., & Kim, M. J. (2010). The relationship between depressive symptoms and subjective well-being in newly admitted patients with schizophrenia.
Comprehensive Psychiatry, 51 (2), 165-170.
Kim, J. H., & Kim, M. J. (2009). Association of Adverse Drug Effects With Subjective Well-
Being in Patients With Schizophrenia Receiving Stable Doses of Risperidone.
Clinical Neuropharmacology, 32 (5), 250-253.
Kinnear, P. R., & Gray, C. D. (2009). SPSS 16 made simple . Hove [England]; New York:
Psychology Press.
Krabbendam, L., Janssen, I., Bak, M., Bijl, R. V., De, G., Ron, & van Os, J. (2002).
Neuroticism and low self-esteem as risk factors for psychosis. Social psychiatry and psychiatric epidemiology, 37 (1), 1-6.
Krakowski, M., Czobor, P., & Volavka, J. (1997). Effect of neuroleptic treatment on depressive symptoms in acute schizophrenic episodes. Psychiatry Research, 71 (1),
19-26.
Kubzansky, L. D., Kubzansky, P. E., & Maselko, J. (2004). Optimism and Pessimism in the
Context of Health: Bipolar Opposites or Separate Constructs? Personality and Social
Psychology Bulletin, 30 (8), 943-956.
Lambert, M., Naber, D., Karow, A., Huber, C. G., Köhler, J., Heymann, J., et al. (2009).
Subjective wellbeing under quetiapine treatment: Effect of diagnosis, mood state, and anxiety. Schizophrenia Research, 110 (1-3), 72-79.
Lambert, M., Schimmelmann, B. G., Naber, D., Schacht, A., Karow, A., Wagner, T., et al.
(2006). Prediction of remission as a combination of symptomatic and functional remission and adequate subjective well-being in 2960 patients with schizophrenia. J
Clin Psychiatry, 67 , 1690- 1697.
Lambert, M., Schimmelmann, B. G., Schacht, A., Karow, A., Wagner, T., Wehmeier, P. M., et al. (2009). Long-term patterns of subjective wellbeing in schizophrenia: Cluster, predictors of cluster affiliation, and their relation to recovery criteria in 2842 patients followed over 3 years. Schizophrenia Research, 107 (2-3), 165-172.
Lambert, M., Schimmelmann, B. G., Schacht, A., Suarez, D., Haro, J. M., Novick, D., et al.
(2010). Differential 3-year effects of first vs. Second-generation antipsychotics on subjective wellbeing in schizophrenia using marginal structural models (MSMS).
Schizophrenia Research, 117 (2-3), 284-284.
Lambert, T. (2011, 28/03/2011). Conversion software. from http://www.open4media.com/NCC2/NCC2.html
Lasser, R. A., Bossie, C. A., Gharabawi, G. M., & Turner, M. (2004). Patients with schizophrenia previously stabilized on conventional depot antipsychotics experience significant clinical improvements following treatment with long-acting risperidone.
European Psychiatry, 19 (4), 219-225.
204
Laursen, B., Pulkkinen, L., & Adams, R. (2002). The Antecedents and Correlates of
Agreeableness in Adulthood. Developmental Psychology, 38 (4), 591-603.
Leucht, S., Corves, C., Arbter, D., Engel, R. R., Li, C., & Davis, J. M. (2009). Secondgeneration versus first-generation antipsychotic drugs for schizophrenia: a metaanalysis. The Lancet, 373 (9657), 31-41.
Leucht, S., Pitschel-Walz, G., Abraham, D., & Kissling, W. (1999). Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo. A meta-analysis of randomized controlled trials. Schizophrenia Research, 35 , 51-68.
Leucht, S., Wahlbeck, K., Hamann, J., & Kissling, W. (2003). New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and metaanalysis. The Lancet, 361 (9369), 1581-1589.
Lewander, T. (1994). Neuroleptics and the neuroleptic-induced deficit syndrome. Acta psychiatrica Scandinavica, 89 , 8-13.
Libiger, J., Masopust, J., & Köhler, R. (2008). Patients on monotherapy differ in subjective well-being from those on combined antipsychotic medication. Schizophrenia
Research, 102 (1-3, Supplement 2), 28-28.
Liddle, P. F., Friston, K. J., Frith, C. D., Hirsch, S. R., Jones, T., & Frackowiak, R. S. (1992).
Patterns of cerebral blood flow in schizophrenia. The British Journal of Psychiatry,
160 (2), 179-186.
Liddle, P. F., & Morris, D. L. (1991). Schizophrenic syndromes and frontal lobe performance. The British Journal of Psychiatry, 158 (3), 340-345.
Lieberman, J. A., Stroup, T. S., McEvoy, J. P., Swartz, M. S., Rosenheck, R. A., Perkins, D.
O., et al. (2005). Effectiveness of Antipsychotic Drugs in Patients with Chronic
Schizophrenia. New England Journal of Medicine, 353 (12), 1209-1223.
Lysaker, P., & Davis, L. (2004). Social function in schizophrenia and schizoaffective disorder: Associations with personality, symptoms and neurocognition. Health and
Quality of Life Outcomes, 2 (1), 15.
Lysaker, P. H., Bell, M. D., Kaplan, E., Greig, T. C., & Bryson, G. J. (1999a). Personality and Psychopathology in Schizophrenia: The Association Between Personality Traits and Symptoms. Psychiatry, 62 , 36 - 48.
Lysaker, P. H., Campbell, K. M. P. H., & Johannesen, J. K. (2005). Hope, Awareness of
Illness, and Coping in Schizophrenia Spectrum Disorders: Evidence of an Interaction.
The Journal of Nervous and Mental Disease, 193 (5), 287 - 292.
Lysaker, P. H., Wilt, M. A., Plascak-Hallberg, C. D., Brenner, C. A., & Clements, C. A.
(2003). Personality dimensions in schizophrenia: Associations with symptoms and coping. The Journal of Nervous and Mental Disease, 191 (2), 80 - 86.
Lysaker, P. H., Wilt, M. A., Plascek-Hallberg, C. D., Brenner, C., & Clements, C. A. (2003a).
The association of personality with symptoms and coping in schizophrenia. J Nerv
Ment Dis, 191 , 80 - 86.
Lyubomirsky, S., Sheldon, K. M., & Schkade, D. (2005). Pursuing happiness: the architecture of sustainable change. Review of General Psychology, 9 (2), 111 - 131.
Lönnqvist, J.-E., Verkasalo, M., Haukka, J., Nyman, K., Tiihonen, J., Laaksonen, I., et al.
(2009). Premorbid Personality Factors in Schizophrenia and Bipolar Disorder: Results
From a Large Cohort Study of Male Conscripts. Journal of Abnormal Psychology,
118 (2), 418-423.
Marder, S. R. (2003). Evidence for Using Atypical Antipsychotics in Psychosis. Primary
Care Companion Journal of Clinical Psychiatry, 5 (Suppl 3), 22-26.
205
Marshall, G. N., Wortman, C. B., Kusulas, J. W., Hervig, L. K., & Vickers, R. R. J. (1992).
Distinguishing Optimism From Pessimism: Relations to Fundamental Dimensions of
Mood and Personality. Journal of Personality and Social Psychology, 62 , 1067 -
1074.
Masthoff, E. D., Trompenaars, F. J., Van Heck, G. L., Hodiamont, P. P., & De Vries, J.
(2007). The relationship between dimensional personality models and quality of life in psychiatric outpatients. Psychiatry Research, 149 (1-3), 81-88.
McCrae, R. R., & Costa, P. T. (1999). A five-factor theory of personality. In L. A. Pervin &
O. John (Eds.), Handbook of Personality: Theory and Research (2nd ed.). New York:
Guildford Press.
Meltzer, H. Y. (2004). What's atypical about atypical antipsychotic drugs? Current Opinion in Pharmacology, 4 (1), 53-57.
Miller, D. D., Caroff, S. N., Davis, S. M., Rosenheck, R. A., McEvoy, J. P., Saltz, B. L., et al.
(2008). Extrapyramidal side-effects of antipsychotics in a randomised trial. The
British Journal of Psychiatry, 193 (4), 279-288.
Moore, O., Cassidy, E., Carr, A., & O'Callaghan, E. (1999). Unawareness of illness and its relationship with depression and self-deception in schizophrenia. European
Psychiatry, 14 (5), 264-269.
Mortimer, A. M., & Dye, S. (1996). Clozapine and the neuropsychology of schizophrenia.
European Psychiatry, 11 (Supplement 4), 279s-279s.
Mortimer, A. M., & Dye, S. (1999). Clozapine and the neuropsychology of schizophrenia.
European Psychiatry, 11 (Supplement 4), 279s.
Mortimer, A. M., Tyson, P., & Dye, S. (1998). Cognitive improvements on clozapine: A two year follow-up study. Schizophrenia Research, 29 (1-2), 143-143.
Musek, J. (2007). A general factor of personality: Evidence for the Big One in the five-factor model. Journal of Research in Personality, 41 (6), 1213-1233.
Möller, H.-J. (2006). Long-acting risperidone: Focus on safety.
Clinical Therapeutics, 28 (5),
633-651.
Naber, D. (1995). A self-rating to measure subjective effects of neuroleptic drugs, relationships to objective psychopathology, quality of life, compliance and other clinical variables. Int Clin Psychopharmacol, 10 (Suppl 3), 133 - 138.
Naber, D. (1996). Rating of subjective effects of antipsychotic drugs, relationships to objective psychopathology and quality of life. European Psychiatry, 11 (Supplement
4), 164s-164s.
Naber, D. (2005). Subjective effects of antipsychotic treatment. Acta psychiatrica
Scandinavica, 111 (2), 81-83.
Naber, D., & Karow, A. (2001). Good tolerability equals good results: the patient's perspective. European Neuropsychopharmacology, 11 (Supplement 4), S391-S396.
Naber, D., & Lambert, M. (2009). The CATIE and CUtLASS Studies in Schizophrenia:
Results and Implications for Clinicians. CNS Drugs, 23 (8), 649-659.
Naber, D., Moritz, S., Lambert, M., Rajonk, F., Holzbach, R., Mass, R., et al. (2001).
Improvement of schizophrenic patients' subjective well-being under atypical antipsychotic drugs. Schizophrenia Research, 50 (1-2), 79-88.
Naber, D., Riedel, M., Klimke, A., Vorbach, E. U., Lambert, M., Kuhn, K. U., et al. (2005).
Randomized double blind comparison of olanzapine vs. clozapine on subjective wellbeing and clinical outcome in patients with schizophrenia. Acta Psychiatr Scand,
111 (2), 106 - 115.
Naber, D., & Vita, A. (2004). Tools for measuring clinical effectiveness. European
Neuropsychopharmacology, 14 (Supplement 4), S435-S444.
206
O'Connor, B. P. (2002). A Quantitative Review of the Comprehensiveness of the Five-Factor
Model in Relation to Popular Personality Inventories. Assessment, 9 , 188-203.
Ode, S., & Robinson, M. D. (2007). Agreeableness and the self-regulation of negative affect:
Findings involving the neuroticism/somatic distress relationship. Personality and
Individual Differences, 43 (8), 2137-2148.
Ode, S., Robinson, M. D., & Wilkowski, B. M. (2008). Can one's temper be cooled? A role for Agreeableness in moderating Neuroticism's influence on anger and aggression.
Journal of Research in Personality, 42 (2), 295-311.
Okun, M. A., & George, L. K. (1984). Physician- and self-ratings of health, neuroticism and subjective well-being among men and women. Personality and Individual
Differences, 5 (5), 533-539.
Okun, M. A., Stock, W. A., Haring, M. J., & Witter, R. A. (1984b). Health and subjective well-being: a meta-analysis. The International journal of aging & human development., 19 , 111 - 132.
Omori, I. M., & Wang, J. (2009). Sulpiride versus placebo for schizophrenia (Review).
[Review]. Cochrane Database of Systematic Reviews (2), 1 - 25.
Owens, T. J. (1993). Accentuate the positive - and the negative: Rethinking the use of selfesteem, self-deprecation, and self-confidence. Social Psychology Quarterly, 56 , 288 -
299.
Porsdal, V., Beal, C., Kleivenes, O., Martinsen, E., Lindstrom, E., Nilsson, H., et al. (2010).
The Scandinavian Solutions for Wellness study - a two-arm observational study on the effectiveness of lifestyle intervention on subjective well-being and weight among persons with psychiatric disorders. BMC Psychiatry, 10 (1), 42.
Pressman, S. D., & Cohen, S. (2005). Does positive affect influence health? Psychol Bull,
131 , 925 - 971.
Purdon, S. E., Jones, B. D. W., Stip, E., Labelle, A., Addington, D., David, S. R., et al.
(2000). Neuropsychological Change in Early Phase Schizophrenia During 12 Months of Treatment With Olanzapine, Risperidone, or Haloperidol. Arch Gen Psychiatry,
57 (3), 249-258.
Putzhammer, A., Perfahl, M., Pfeiff, L., & Hajak, G. (2005). Correlation of Subjective Wellbeing in Schizophrenic Patients with Gait Parameters, Expert-rated Motor
Disturbances, and Psychopathological Status. Pharmacopsychiatry, 38 (03), 132-138.
Quilty, L. C., Oakman, J. M., & Risko, E. (2006). Correlates of the Rosenberg Self-Esteem
Scale Method Effects. Structural Equation Modeling: A Multidisciplinary Journal,
13 , 99 - 117.
Rammstedt, B., & John, O. P. (2007). Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. Journal of Research in Personality, 41 (1), 203-212.
Ren, X. S., Kazis, L. E., Lee, A. F., Hamed, A., Huang, Y. H., Cunningham, F., et al. (2002).
Patient characteristics and prescription patterns of atypical antipsychotics among patients with schizophrenia. Journal of Clinical Pharmacy & Therapeutics, 27 (6),
441-451.
Ritsner, M., Farkas, H., & Gibel, A. (2003). Satisfaction With Quality of Life Varies With
Temperament Types of Patients With Schizophrenia. The Journal of Nervous and
Mental Disease, 191 (10), 668-674.
Ritsner, M., Gibel, A., Perelroyzen, G., Kurs, R., Jabarin, M., & Ratner, Y. (2004). Quality of
Life Outcomes of Risperidone, Olanzapine, and Typical Antipsychotics Among
People with schizophrenia Treated in Routine Clinical Practice: A naturalistic comparative study. Journal of Clinical psychopharmacology, 24 (6), 582-591.
207
Ritsner, M., Perelroyzen, G., Ilan, H., & Gibel, A. (2004). Subjective response to antipsychotics of people with schizophrenia treated in routine clinical practice: a naturalistic comparative study. Journal of Clinical Psychopharmacology, 24 (3), 245-
254.
Ritsner, M., Ponizovsky, A., Endicott, J., Nechamkin, Y., Rauchverger, B., Silver, H., et al.
(2002). The impact of side-effects of antipsychotic agents on life satisfaction of people with schizophrenia: a naturalistic study. Eur Neuropsychopharmacol, 12 (1), 31
- 38.
Robins, R. W., Tracy, J. L., Trzesniewski, K., Potter, J., & Gosling, S. D. (2001). Personality
Correlates of Self-Esteem. Journal of Research in Personality, 35 (4), 463-482.
Rosenheck, R., Perlick, D., Bingham, S., Liu-Mares, W., Collins, J., Warren, S., et al. (2003).
Effectiveness and Cost of Olanzapine and Haloperidol in the Treatment of
Schizophrenia: A Randomized Controlled Trial. JAMA, 290 (20), 2693-2702.
Rushton, J. P., & Erdle, S. (2010). No evidence that social desirability response set explains the general factor of personality and its affective correlates. Twin Research and
Human Genetics, 13 (2), 131 - 134.
Sands, J. R., & Harrow, M. (1999). Depression During the Longitudinal Course of
Schizophrenia. Schizophr Bull, 25 (1), 157-172.
Sanger, T. M., Lieberman, J. A., Tohen, M., Grundy, S., Beasley, C., Jr., & Tollefson, G. D.
(1999). Olanzapine Versus Haloperidol Treatment in First-Episode Psychosis. Am J
Psychiatry, 156 (1), 79-87.
Schennach-Wolff, R., Jäger, M., Seemüller, F., Obermeier, M., Messer, T., Laux, G., et al.
(2009). Attitude towards adherence in patients with schizophrenia at discharge.
Journal of Psychiatric Research, 43 (16), 1294-1301.
Schennach-Wolff, R., Seemüller, F., Obermeier, M., Messer, T., Laux, G., Pfeiffer, H., et al.
(2011). Response and remission of subjective well-being in patients suffering from schizophrenia spectrum disorders. European Psychiatry, 26 (5), 284-292.
Schimmelmann, B. G., Moritz, S., Karow, A., Schafer, I., Bussopulos, A., Golks, D., et al.
(2005). Correlates of subjective well-being in schizophrenic patients treated with atypical antipsychotics. International Journal of Psychiatry in Clinical Practice, 9 (2),
94-98.
Schmidt, P., Clouth, J., Haggenmuller, L., Naber, D., & Reitberger, U. (2006). Constructing an Index for the Subjective Well-being Under Neuroleptics scale (SWN), short form: applying structural equation modeling for testing reliability and validity of the index.
Qual Life Res, 15 (7), 1191 - 1202.
Segerstrom, S. C., Evans, D. R., & Eisenlohr-Moul, T. A. (2011). Optimism and pessimism dimensions in the Life Orientation Test-Revised: Method and meaning. Journal of
Research in Personality, 45 (1), 126 – 129.
Siamouli, M., Moutou, K., Pantoula, E., Magiria, S., Chatzivasileiou, I., Arapidis, K., et al.
(2009). Preliminary data concerning the reliability and psychometric properties of the
Greek translation of the 20-item Subjective Well-Being Under Neuroleptic Treatment
Scale (SWN-20). Annals of General Psychiatry, 8 (1), 3.
Soares, B., Fenton, M., & Chue, P. (1999). Sulpiride for schizophrenia. Cochrane Database of Systematic Reviews, (1). Retrieved from http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001162/frame.
html. doi:10.1002/14651858.CD001162
Staring, A. B. P., Van der Gaag, M., Van den Berge, M., Duivenvoorden, H. J., & Mulder, C.
L. (2009). Stigma moderates the associations of insight with depressed mood, low
208
self-esteem, and low quality of life in patients with schizophrenia spectrum disorders.
Schizophrenia Research, 115 (2-3), 363-369.
Steel, P., Schmidt, J., & Shultz, J. (2008). Refining the Relationship Between Personality and
Subjective Well-Being. Psychological Bulletin, 134 (1), 138-161.
Tabachnick, B. G., & Fidell, L. S. (2001). Using Multivariate Statistics (4th ed.). USA:
Pearson.
Tandon, R., & Jibson, M. D. (2003). Efficacy of newer generation antipsychotics in the treatment of schizophrenia. Psychoneuroendocrinology, 28 (Supplement 1), 9-26.
Theme-Filha, M. M., Szwarcwald, C. L., & Souza-Junior, P. R. B. d. (2005). Sociodemographic characteristics, treatment coverage, and self-rated health of individuals who reported six chronic diseases in Brazil, 2003.
Cadernos de Saúde Pública, 21
,
S43-S53.
Tien, A. Y., Costa, P. T., & Eaton, W. W. (1992). Covariance of personality, neurocognition, and schizophrenia spectrum traits in the community. Schizophrenia Research, 7 (2),
149-158.
Tollefson, G. D., Sanger, T. M., Lu, Y., & Thieme, M. E. (1998). Depressive Signs and
Symptoms in Schizophrenia: A Prospective Blinded Trial of Olanzapine and
Haloperidol. Arch Gen Psychiatry, 55 (3), 250-258. van 't Wout, M., Aleman, A., Bermond, B., & Kahn, R. S. (2007). No words for feelings: alexithymia in people with schizophrenia and first-degree relatives. Comprehensive
Psychiatry, 48 (1), 27-33. van Os, J., & Jones, P. B. (2001). Neuroticism as a risk factor for schizophrenia. Psychol
Med, 31 , 1129 - 1134.
Voruganti, L. N. P., & Awad, A. G. (2002). Personal evaluation of transitions in treatment
(PETiT):a scale to measure subjective aspects of antipsychotic drug therapy in schizophrenia. Schizophrenia Research, 56 (1-2), 37-46.
Vothknecht, S., Schoevers, R. A., & de Haan, L. (2011). Subjective well-being in schizophrenia as measured with the Subjective Well-Being under Neuroleptic
Treatment scale: a review. Australian and New Zealand Journal of Psychiatry, 45 (3),
182-192.
Walburn, J., Gray, R., Gournay, K., Quraishi, S., & David, A. S. (2001). Systematic review of patient and nurse attitudes to depot antipsychotic medication. The British Journal of Psychiatry, 179 (4), 300-307.
Wechsler, D. (1997). Manual for the Wechsler Adult Intelligence Scale, 3rd ed (WAIS-III).
San Antonio, TX: Psychological Corporation.
Wechsler, D. (2001). Wechsler Test of Adult Reading . San Antonio, TX: Psychological
Corporation.
Wehmeier, P. M., Kluge, M., Schacht, A., Helsberg, K., Schreiber, W., Schimmelmann, B.
G., et al. (2008). Patterns of physician and patient rated quality of life during antipsychotic treatment in outpatients with schizophrenia. Journal of Psychiatric
Research, 42 (8), 676-683.
Wehmeier, P. M., Kluge, M., Schneider, E., Schacht, A., Wagner, T., & Schreiber, W.
(2007). Quality of life and subjective well-being during treatment with antipsychotics in out-patients with schizophrenia. Progress in Neuro-Psychopharmacology and
Biological Psychiatry, 31 (3), 703-712.
Williams, P. G., O'Brien, C. D., & Colder, C. R. (2004). The effects of neuroticism and extraversion on self-assessed health and health-relevant cognition. Personality and
Individual Differences, 37 (1), 83-94.
209
Wolters, H. A., Knegtering, H., van den Bosch, R. J., & Wiersma, D. (2009). Effects and side effects of antipsychotic treatment in schizophrenia: Pros and cons of available selfrating scales. Schizophrenia Research, 112 (1-3), 114-118.
Wolters, H. A., Knegtering, R., Wiersma, D., & van den Bosch, R. J. (2006). Evaluation of the Subjects' Response to Antipsychotics Questionnaire. International Clinical
Psychopharmacology, 21 , 63 - 69.
Yamauchi, K., Hirofumi, A., Masahito, T., Jun-Ichi, I., Syusuke, N., Ikuyo, M., et al. (2008).
Predictors of subjective and objective quality of life in outpatients with schizophrenia.
Psychiatry and Clinical Neurosciences, 62 (4), 404-411.
210
List of Appendices
Appendix A: SWN Subscale items and BFI items ................................................................................. 213
Appendix B: PANSS Factor Items ......................................................................................................... 216
Appendix C: Missing Data ................................................................................................................... 217
Appendix D: Adjunctive Medications .................................................................................................. 218
Appendix E: Alternative Factor solutions ............................................................................................ 225
Appendix F: Correlation Tables ........................................................................................................... 229
Appendix G: Miscellaneous Group differences.................................................................................... 236
Appendix H: Initial ANCOVA/MANCOVA analyses .............................................................................. 238
Appendix I: ANCOVA/MANCOVA analyses using imputation of missing data .................................... 246
Appendix J: Follow up data ................................................................................................................. 251
211
Appendix A: SWN Subscale items and BFI items
Table A1. SWN subscale items (Naber, et al., 2001)
Subscale
Mental functioning
Self-control
Emotional regulation
Social integration
Physical functioning 2
5
9
16
4
10
18
20
6
1
15
12
19
8
13
14
Item # Content
3
7
11
17
I find it easy to think
I am imaginative and full of ideas
My thinking is difficult and slow (R)
My thoughts are flighty and undirected. I find it difficult to think clearly. (R)
I feel powerless and not in control of myself (R)
I find it easy to draw a line between myself and others
My feelings and behaviour are inappropriate to situations. I get upset over small things, important ones hardly affect me (R)
My feelings and behaviour are appropriate in the particular situation
I have no hope for the future (R)
My emotions and sensations are dull. Nothing matters to me. (R)
I am interested in what is happening around me, and it is important to me
I am full of confidence, everything will be alright
I am very shy about getting to know people (R)
My environment seems friendly and familiar to me
I find it easy to keep in touch with people around me
I perceive my environment as being changed, strange and threatening.
(R)
I feel very comfortable with my body.
My body feels familiar.
I feel weak and exhausted. (R)
My body is a burden to me. (R)
(R) indicates reverse scored items.
212
Table A2. BFI personality factor items (John, et al., 1991)
Note: all items complete the initial stem, “I am someone who...”
Personality factor
Extraversion
Item # Content
1 Is talkative
6R Is reserved
Agreeableness
Conscientiousness
3
8R
13
18R
23R
28
33
38
43R
36
2R
7
12R
17
22
11
16
21R
26
31R
27R
32
37R
42
Is full of energy
Generates a lot of enthusiasm
Tends to be quiet
Has an assertive personality
Is sometimes shy, inhibited
Is outgoing, sociable
Tends to find fault with others
Is helpful and unselfish with others
Starts quarrels with others
Has a forgiving nature
Is generally trusting
Can be cold and aloof
Is considerate and kind to almost everyone
Is sometimes rude to others
Likes to cooperate with others
Does a thorough job
Can be somewhat careless
Is a reliable worker
Tends to be disorganized
Tends to be lazy
Perseveres until the task is finished
Does things efficiently
Makes plans and follows through with them
Is easily distracted
213
Neuroticism
Openness to experience
R indicates reverse scored items.
5
10
15
20
25
30
35R
40
41R
44
4
9R
14
19
24R
29
34R
39
Is depressed, blue
Is relaxed, handles stress well
Can be tense
Worries a lot
Is emotionally stable, not easily upset
Can be moody
Remains calm in tense situations
Gets nervous easily
Is original, comes up with new ideas
Is curious about many different things
Is ingenious, a deep thinker
Has an active imagination
Is inventive
Values artistic, aesthetic experiences
Prefers work that is routine
Likes to reflect, play with ideas
Has few artistic interests
Is sophisticated in art, music, or literature
214
Appendix B: PANSS Factor Items
Factor items adapted from Bell, et al. (1994)
PANSS factor
Positive
Negative
Affective
Cognitive/disorganised
Hostile Excitement
G1
G2
G3
G6
G15
P2
N5
G5
G10
G11
G13
P4
P7
N7
G4
G8
G14
Item Code Item Title
P1 Delusions
P3
P5
P6
Hallucinatory behaviour
Grandiosity
Suspiciousness/persecution
G9
G12
N1
N2
Unusual thought content
Lack of judgment and insight
Blunted affect
Emotional withdrawal
N3
N4
N6
G7
G16
Poor rapport
Passive/apathetic social withdrawal
Lack of spontaneity and flow of conversation
Motor retardation
Active social avoidance
Somatic concern
Anxiety
Guilt
Depression
Preoccupation
Conceptual disorganisation
Difficulties with abstract thinking
Tension
Disorientation
Poor attention
Disturbance of volition
Excitement
Hostility
Stereotyped thinking
Tension
Uncooperativeness
Poor impulse control
215
Appendix C: Missing Data
Data was missing for the following variables.
Table C1
Variables with missing cases in each long acting injectable group
Variable
DASS
LUNSERS
PANSS
ITAQ
WTAR
Information
ROMI
Life difficulties
RBANS
4
3
3
4
1
3
1
4
FGA group SGA group Total
1 2 3
2
4
3
8
4
6
4
4
0
5
8
9
7
8
1
8
216
Appendix D: Adjunctive Medications
Table D1 Breakdown of five patients taking two oral antipsychotics
Long acting injectable First oral Second oral
FGA
SGA
Olanzapine
Zuclopenthixol
Risperidone
Risperidone
Olanzapine
Chlorpromazine
Chlorpromazine
Aripiprazole
Quetiapine
Risperidone
Table D2 Breakdowns of patients taking mood stabilisers
FGA long acting injectable
% of total
N sample
Mood stabiliser taken
None
Sodium valproate
Lithium carbonate
Carbamazepine
32
12
2
0
Lamotrigine
Subtotal
Any mood stabiliser
(41.5%)
(15.6%)
(2.6%)
(0%)
1 (1.3%)
15 (19.5%)
Total 47 (61%)
1
0
12
18
9
2
SGA long acting injectable
% of total
N sample
(23.4%)
(11.7%)
(2.6%)
(1.3%)
(0%)
(15.6%)
N
1
1
27
50
21
4
Total
30 (39%) 77 (100%)
Long acting injectable medication groups did not significantly differ in use of mood stabilisers, χ
2
(4) = 2.73, p = .60.
% of total sample
(64.9%)
(27.3%)
(5.2%)
(1.3%)
(1.3%)
(35.1%)
217
Table D3 Breakdowns of patients taking antidepressants
FGA
Antidepressant taken?
Total
None
Sertraline
Citalopram
Fluoxetine
Subtotal
Any antidepressant
43 (91.5%)
1 (2.1%)
2 (4.2%)
1 (2.1%)
4 (4.8%)
47 (100%)
FGA Total
28 (93.3%) 71 (92.2%)
1(3.3%) 2 (2.6%)
1 (3.3%)
0
2 (6.6%)
30 (100%)
3 (3.9%)
1 (1.3%)
6 (7.8%)
77 (100%)
Long acting injectable medication groups did not significantly differ in use of antidepressant medications, χ 2
(3) = .79, p = .85.
Table D4 Breakdown of patients taking antiparkinson medication
Total
FGA SGA
Antiparkinson medication
None
Benztropine
41
6
28
2
69
8
Total 47 30 77
Long acting injectable medication groups did not significantly differ in use of antiparkinson medication, χ
2
(1) = .73, p = .47.
Table D5 Breakdowns of patients taking benzodiazepines
Benzo None
Lorazepam
Total
Diazepam
Temazepam
Total benzo use
FGA
36
2
6
3
11
47
SGA
23
1
5
1
7
30
Total
59
3
11
4
18
77
Long acting injectable medication groups did not significantly differ in PRN benzodiazepine use, χ 2
(3) = .56, p = .91.
218
Table D6. Differences between antidepressant users and other patients on DASS, PANSS and side-effects scores
Scale t d Mean (Std. D.)
Antidepressant users Others p
Depression
Anxiety
Stress
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
Hostile excitement symptoms
PANSS total
Total side-effects
Neurological SE
Autonomic SE
Psychic side-effects
Sexual SE
21.33 (6.89)
20.00 (3.35)
22.00 (7.38)
2.44 (.93)
2.10 (.76)
2.93 (.47)
1.81 (.67)
1.53 (.36)
64.00 (12.52)
43.33 (14.67)
6.67 (2.58)
8.83 (4.17)
18.67 (4.93)
5.67 (3.72)
12.14 (11.03)
11.47 (9.45)
13.79 (10.88)
3.15 (1.01)
1.98 (.97)
2.19 (.79)
2.39 (.84)
2.04 (.82)
69.81 (15.43)
29.74 (18.80)
5.21 (4.77)
9.03 (8.84)
10.15 (6.43)
3.06 (3.03)
2.88
.89
-1.78
-1.22
.05
-3.16
-1.99
-2.00
-2.19
-1.81
1.63
-.30
-2.26
1.64
.38
.08
.26
.96
.002
.051
.049
.032
.08
.11
.77
.027
.11
.015
1.00
1.20
.88
.41
-.07
1.14
.40
.81
.22
.81
-.84
.01
1.49
.77
219
SWN Total scale
Negative SWN
Positive SWN
Mental functioning
Self control
Emotional regulation
Social integration
Physical functioning
Depression
Anxiety
Stress
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
Hostile excitement symptoms
PANSS total
Total side-effects
Neurological SE
Autonomic SE
Psychic side-effects
Sexual SE
Red herrings
Table D7. Comparisons of patients ever trialled on clozapine or planning to trial versus those who have never used with no use planned
Scale t p d Mean (Std. D.)
Clozapine used or planned n = 12
No clozapine ever n = 65
63.08 (14.09)
36.58 (9.34)
68.00 (18.63)
37.69 (10.47)
28.67 (10.40)
14.08 (3.15)
31.34 (11.40)
13.48 (4.88)
11.75 (4.99)
13.92 (4.78)
11.00 (4.71)
12.33 (3.11)
13.67 (10.44)
13.38 (4.11)
14.23 (4.32)
13.51 (4.58)
13.40 (4.65)
12.74 (11.19)
14.67 (9.77)
18.50 (10.89)
3.31 (1.47)
2.11 (0.86)
2.48 (0.98)
2.69 (0.87)
11.68 (9.32)
13.67 (10.74)
2.75 (1.06)
1.93 (0.83)
2.14 (0.88)
2.61 (0.94)
1.98 (1.01)
75.09 (14.15)
36.25 (24.72)
6.17 (5.54)
9.83 (7.32)
12.00 (7.86)
4.17 (4.13)
7.42 (6.79)
1.90 (0.96)
68.21 (15.26)
29.23 (17.60)
5.16 (4.48)
8.21 (7.21)
10.61 (6.51)
3.10 (2.92)
5.69 (5.04)
1.22
.23
1.74
.76
-.27
.87
.34
.76
-.41
-1.01
-1.42
-1.50
-.66
-1.16
-.26
-.25
-1.39
-1.18
.69
-.71
-.65
-1.08
-1.02
.23
.82
.09
.45
.79
.39
.73
.45
.68
.32
.16
.14
.51
.25
.79
.28
.05
.40
.18
-.06
.20
.08
.18
-.09
-.23
-.33
-.37
-.16
-.29
-.06
.81
.17
.24
.50
.48
.52
.28
.31
-.06
-.34
-.28
-.16
-.17
-.15
-.25
-.24
220
Table D8. Comparisons of patients with history of ECT versus those with no history of ECT
Scale
SWN Total scale
Mean (Std. D.)
History of ECT n = 10
62.00 (11.68)
No ECT ever n = 67
68.01 (18.71)
Negative SWN
Positive SWN
38.30 (6.83)
25.80 (7.24)
37.40 (10.71)
31.69 (11.55)
Mental functioning
Self control
Emotional regulation
Social integration
11.30 (4.11)
11.70 (2.98)
13.90 (3.38)
13.20 (3.36)
13.91 (4.64)
13.34 (4.40)
14.22 (4.51)
13.10 (4.84)
Physical functioning
Depression
Anxiety
Stress
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
11.90 (4.23)
17.40 (11.28)
13.00 (11.48)
17.2 (10.16)
2.52 (1.36)
2.31 (0.93)
2.43 (1.21)
2.70 (0.82)
13.43 (4.47)
12.19 (10.89)
12.03 (9.13)
14.03 (10.95)
2.90 (1.11)
1.90 (0.80)
2.15 (0.83)
2.61 (0.94)
Hostile excitement symptoms
PANSS total
Total side-effects
Neurological SE
Autonomic SE
Psychic side-effects
Sexual SE
Red herrings
1.98 (1.16)
74.10 (15.21)
31.70 (16.92)
6.30 (4.28)
7.80 (6.96)
11.50 (7.20)
2.80 (2.78)
5.10 (5.13)
1.90 (0.94)
68.49 (15.18)
30.16 (19.32)
5.17 (4.71)
8.58 (7.28)
10.73 (6.69)
3.34 (3.21)
6.11 (5.41) t p d
.99
-.26
1.56
1.68
1.14
.22
.06
.33 .23
.80 -.06
.12 .36
.10 .39
.26 .26
.83 .05
.95 .01
1.02 .31 .24
-1.40 .17 -.33
-.30
-.86
.76
.39
-.07
-.20
.96 .34 -.01
-1.47 .15 -.36
-.89
-.26
.38 -.22
.78 -.06
-.25 .81 -.06
-1.08 .28 -.27
.24 .81 .06
.71
.32
.48
.75
.17
.08
.85
.51
.55
.74
.61
.58
.20
.12
.14
221
Table D9. DASS scale scores for combined oral and LAI medication groupings.
1
9
2
16
3
11
4
7
5
5
6
16
7
5
N
M SD M SD M SD M SD M
10.44 8.99 14.88 10.58 15.09 13.72 11.14 11.99 6.40
SD
11.08
M SD
13.13 12.46
M
16.80
SD
9.23
Depression
9.33 7.071 12.75 7.99 12.36 9.70 12.85 11.82 6.40 10.03 12.00 10.58 18.40 7.92
Anxiety
12.44 9.98 15.37 9.02 15.45 12.23 14.57 14.50 8.00 8.36 14.25 13.04 18.00 7.61
Stress
Key: 1 = LAI FGA only; 2 = LAI FGA & olanzapine; 3 = LAI FGA & other SGA; 4 = LAI FGA & FGA oral; 5 = LAI SGA only; 6 = LAI SGA & risperidone; 7 = LAI
SGA & olanzapine
222
Table D10. ANOVA results for combined LAI and oral medication grouping regarding DASS scores
F p Partial η 2
Depression R 2 = .06 Adj. R 2 = .05
Total dosage converted into CPZE
Medication grouping
Anxiety
Total dosage converted into CPZE
Medication grouping
Stress
Total dosage converted into CPZE
Medication grouping
.02
.40
R 2 = .08
.12
.50
R 2 = .11
.37
.09
.89
.88
Adj. R 2 = .03
.73
.81
Adj. R 2 = .01
.90
.76
.00
.04
.00
.05
.04
.00
223
Appendix E: Alternative Factor solutions
Note: Negative items have been reverse coded.
Loadings greater than .40 are in bold. Loadings less than .01 are not shown.
Comment: All factor solutions shown here have at least two cross-loadings with values greater than .40. Factor 1 in all of the solutions shown here consists of at least nine of the negatively worded items. The five-factor solution contains a factor with only two items with loadings > .40. The six-factor solution contains a factor with only one item with a loading > .40. Factors with only one or two items are likely to be unreliable.
Varimax rotation was also applied with similar results. That is, factor 1 in all solutions consisted of at least 9 negatively worded items, all factor solutions with more than two factors had three cross-loadings > .40, and the five and six factor solutions contained factors with only two items. However, the two-factor varimax solution contained no cross-loadings (factor 2 consisted only of 9 items).
Powerless
Comfortable in body
Easy to think
No hope
Body feels familiar
Shy
Imaginative
Environment friendly
Exhausted
Nothing matters
Slow thinking
Inappropriate
Keep in touch
Strange environment
Draw a line
Burden
Flighty thoughts
Interested
Appropriate behaviour
Three factor solution
Structure matrix
1
.734
Component
2
.129
3
.050
.108 .546 -.331
.069 .736 -.221
.433 .198 -.339
.257 .315 .176
.520 .200 .251
-.078 .433 -.443
-.085 .176 -.776
.579 -.187 .126
.689 .043 -.021
.718 .013 -.197
.596 -.110 -.220
.145 .512 -.273
.433 -.195 -.564
-.086 .521 -.012
.689 .087 .030
.718 .071 -.013
-.011 .519 .144
.034 .784 .198
224
Full of confidence .129 .748 -.206
Powerless
Comfortable in body
Easy to think
No hope
Body feels familiar
Shy
Imaginative
Environment friendly
Exhausted
Nothing matters
Slow thinking
Inappropriate
Keep in touch
Strange environment
Draw a line
Burden
Flighty thoughts
Interested
Appropriate behaviour
Full of confidence
-.190
.740
.761
.053
.071
.123
.188
.219
-.152
.139
.693
.097
.431
.177
-.039
.022
.564
.052
-.152
.562
.625
.730
.504
.091
.260
.070
.465
.192
.538
.034
1
Four factor solution
Structure matrix
.695
2
.185
Component
3
-.074
4
.118
.039 .622 -.262 -.143
-.008
-.117
.190
.061
-.295
-.449
.310
.116
-.565
-.025
-.181
-.126
-.378
-.199
-.760
-.798
-.490
.160
.147
-.247
.083
-.142
.056
.691
-.013
-.021
.408
.717
.719
-.144
.105
.059
.310
.323
-.018
.262
-.177
-.191
-.141
-.042
-.262
225
Five factor solution
Powerless
Comfortable in body
Easy to think
No hope
Body feels familiar
Shy
Imaginative
Environment friendly
Exhausted
Nothing matters
Slow thinking
Inappropriate
Keep in touch
Strange environment
Draw a line
Burden
Flighty thoughts
Interested
Appropriate behaviour
Full of confidence
Structure matrix
1
.702
2
.216
Component
3
-.095
-.022
.087
.498
.004
.612
-.010
-.182
.604
.548
.693
.396
.054
.165
-.112
.674
.709
-.018
.122
.192
.494
.646
.182
.052
.274
.073
.241
-.032
.044
-.050
-.080
.473
.035
.773
-.122
-.095
.175
.664
.765
-.298
-.019
-.125
-.103
.200
.015
-.569
-.018
-.237
-.173
-.438
-.226
-.793
-.097
.036
-.002
.252
.324
-.003
4
.136
-.173
-.310
-.408
.156
.144
-.854
-.442
.210
.120
-.247
.066
-.163
.102
.315
-.234
-.231
-.258
-.080
-.237
5
.033
.261
.085
-.243
.868
-.094
.040
-.183
-.168
.271
.241
.192
.039
-.046
.221
.150
.470
.178
-.081
226
Powerless
Comfortable in body
Easy to think
No hope
Body feels familiar
Shy
Imaginative
Environment friendly
Exhausted
Nothing matters
Slow thinking
Inappropriate
Keep in touch
Strange environment
Draw a line
Burden
Flighty thoughts
Interested
Appropriate behaviour
Full of confidence
-.213
.736
.781
-.031
.091
.176
.212
.179
-.305
.152
.080
-.071
.319
-.137
.884
.287
.144
.003
.101
-.169
.517
.573
.739
.406
.046
.120
.162
.536
.065
.533
Six-factor solution
Structure matrix
1
.660
2
.087
Component
3
-.100
4
.283
.068 .803 -.134 -.068
-.153
-.721
-.104
-.115
-.145
-.398
-.343
-.846
.067
-.154
-.005
.106
-.634
-.224
.299
.111
-.144
.042
.063
.146
-.068
-.174
.013
.344
.471
.009
.118
-.172
.440
.645
-.153
.058
.076
-.041
.189
-.105
.550
-.186
-.183
-.098
.211
.143
.268
.199
.437
.118
.050
-.120
-.049
-.044
.343
-.065
6
.036
-.147
-.003
-.031
.811
-.166
-.197
-.236
-.161
.305
-.036
.277
.073
.121
5
.016
.258
-.310
-.050
.131
.096
.183
-.019
-.221
.105
.123
-.024
.905
.509
.260
227
Appendix F: Correlation Tables
Key: * p <.05; ** p <.01; *** p <.001
Table F1
SWN subscale intercorrelations
Self Control
.52** Mental
Functioning
Self Control
Emotional
Regulation
Physical
Functioning
Social
Integration
Emotional
Regulation
.69**
.67**
Physical
Functioning
.57**
.57**
.53**
Table F2 BFI intercorrelations
Agreeableness Conscientiousness Neuroticism
-.54**
-.46**
-.38**
Social
Integration
.49**
.53**
.60**
.42**
Openness to experience
.47**
.27*
.33**
-.31**
E
A
C
N
.30** .50**
.52**
Table F3 DASS intercorrelations
Anxiety
Depression .77***
Stress
.81***
Anxiety .83***
SWN Total
.89**
.81**
.87**
.77**
.76**
228
Table F4 SWN correlations with age, education, and time on medication
Mental
Functioning
Self
Control
Emotional
Regulation
Physical
Functioning
Social
Integration
Age .05 -.01 -.05 .01 .08
-.08 -.11 -.17 -.10 -.11 Years on any antipsychotic medication
Time on current LAI medication
Years of education
.00
.12
-.07
.10
-.10
.19
-.10
-.19
.15
.09
SWN
Total
.02
-.14
-.03
.07
Table F5 SWN correlations with premorbid IQ
WTAR estimated IQ
SWN Total
Mental Functioning
Self Control
Emotional Regulation
Social Integration
Physical Functioning
Negative factor
Positive factor
0.05
0.05
0.07
0.1
-0.19
0.17
-0.16
-0.06
Information estimated IQ Premorbid IQ (averaged from WTAR and
Information test)
0.01
0.04
0.05
0.06
-0.15
0.05
0.05
0.06
-0.09
-0.09
-0.01
-0.02
-0.2
-0.01
0.04
-0.09
229
Table F6 SWN correlations with neurocognitive status
RBANS Scale Language Attention Immediate memory
.24*
Visuospatial constructional
0.14 0.20 0.03
SWN Total
0.18 0.1 0.15 0.01
Mental Functioning
.28* 0.18 .24* 0.01
Self Control
.38** 0.09 0.2 0.07
Emotional Regulation
-0.11 -0.01 0.12 -0.17
Social Integration
.25* 0.22 0.1 0.22
Physical Functioning
-0.11 -0.1 0.09 -0.01
Negative factor
0.18 0.09 .27* -0.04
Positive factor
Table F7 SWN scales and substance use
Cigarettes per day
Mental
Functioning Self Control
Emotional
Regulation
-.20 -.25* -.29*
Physical
Functioning
-.09
Alcohol
Amphetamines
Cannabis
Cocaine
Opiates
Humber of hallucinogen trips ever
Ecstasy
-.07
-.02
-.01
-.03
-.11
-.04
.05
.04
.10
.14
.16
-.08
.05
.05
-.05
.04
.12
.08
-.06
.09
.06 .02
.00
.00
.01
.07
-.12
.02
-.05
-.02
.10
.00
-.14
-.02
Delayed memory
.24*
0.16
0.19
.30*
0.07
0.21
-0.17
0.17
Total score
0.22
0.14
.24*
.26*
-0.03
.27*
-0.08
0.15
Social
Integration SWN Total
-.22 -.26*
-.06 .03
-.03
.02
.09
.07
-.13
.02
230
Table F8 PANSS intercorrelations
Positive
Negative
Affective
Cognitive/ disorganised n = 69
Negative
-.21
Affective
.29*
-.05
Cognitive/ disorganised
.06
.30*
.22
Excitement
.37**
-.18
.34**
.41***
Table F9 BFI and PANSS correlations
Extraversion
Positive
.22
Negative
-.22
Affective
-.27*
Cognitive/ disorganised
.06
Agreeableness -.01
Conscientiousness -.01
Neuroticism
Openness to experience
-.13
.25*
-.14
-.10
-.03
-.27*
-.31**
-.36**
.44**
-.25*
Table F10 DASS correlations with PANSS Factors
Positive
Depression Anxiety
.11 .04
Stress
.03
-.28*
-.05
.16
-.14
Excitement
.21
.02
.13
-.05
.21
Negative
Affective
Cognitive/ disorganised
Excitement
.04
.53***
.21
.10
-.10
.47***
.10
.12
-.01
.50***
.11
.11
231
Table F11 Correlates of lifestyle factors
Health Exercise Life difficulties
.30** Exercise
Life difficulties
Loneliness
Mental problems
Depression
Anxiety
Stress
Total side-effects
Neurological side-effects
Autonomic side-effects
-.28*
-.30**
-.31**
-.40**
-.30**
-.31**
-.43**
-.40**
-.38**
-.23
-.21
-.12
-.19
-.21
-.14
-.27*
-.27*
-.23*
.29*
.43**
.36**
.26*
.34**
.26*
.19
.01
Psychic side-effects -.33** -.34** .35**
Sexual side-effects -.33** -.21 .09
Positive symptoms .00 -.14 .10
-.14 .00 -.15 Negative symptoms
Affective symptoms -.41** -.22 .23
.04 -.03 .03 Cognitive/disorganised symptoms
Excitement symptoms
PANSS total
.03
-.16
.13
-.09
.03
.08
Insight
Cigarettes per day
-.07
-.20
.07
-.05
.20
-.09
Loneliness Mental problems
.27*
.21
.28*
.27*
.20
.30**
.31** .42**
.36**
.45**
.34**
.30**
.19
.19 .31**
.08
.16
-.11
.15
.05
.16
.02
-.07
.33**
.22*
.03
.10
.05
-.04
.14
.21
.39***
.08
232
Table F12 ROMI Correlations with SWN, DASS, and side-effects scales
Adherence score Nonadherence score Total ROMI Score
SWN Total -.23 -.20 -.05
-.28* -.21 -.08
Negative SWN
Positive SWN
-.11 -.14 .00
-.14 -.21 .03
Mental Functioning
-.23 .06 -.20
Self Control
-.07 -.16 .04
Emotional Regulation
Social Integration
-.23
-.25*
-.23
-.23
-.03
-.04
Physical Functioning
Depression .22 .19 .05
Anxiety
Stress
Total side-effects
Neurological SE
Autonomic SE
Psychic side-effects
Sexual SE
.25*
.37*
.16
.25*
.04
.23
.00
.23
.04
.14
.03
.11
.21
.23
.16
.21
-.01
.05
-.11
.15
-.08
233
Table F13 Correlates of ITAQ insight
ROMI adherence
Insight
.51***
-.44*** ROMI non-adherence
ROMI Total .63***
-.32** Positive symptoms
Negative symptoms -.28*
-.15 Cognitive/disorganised symptoms
Affective symptoms -.09
Excitement symptoms
PANSS total
Depression
Anxiety
Stress
Extraversion
Agreeableness
.10
-.29*
.17
.27*
.35**
-.21
-.07
-.04 Conscientiousness
Neuroticism
Openness to experience
Neurological side-effects
Autonomic side-effects
Psychic side-effects
Sexual side-effects
Total side-effects
.25*
.01
.13
.21
.29*
.07
.21
234
Appendix G: Miscellaneous Group differences
Table G1. Gender differences in premorbid IQ and substance use
Cannabis use
Amphetamines
Information test
Mean
Males
1.91
.85
100.35
SD
1.79
1.37
17.44
Females
Mean SD t p
0.72
.31
1.03
.81
-3.26
-2.17
002
.033
90.89 16.95 -2.26 .027
Cohen’s d
.81
.48
.55
Table G2. Differences between diagnostic groups
Negative symptoms
Sexual side-effects
WTAR IQ estimate
Attention
Schizophrenia
Mean SD
2.11
3.78
97.17
75.08
.96
3.26
9.19
17.14
Schizoaffective
Mean SD t p
1.62 .84 1.96 .056
1.90 2.36 2.35 .021
87.11 12.56 3.63 .001
61.95 16.51 2.87 .005
Cohen’s d
.54
.46
.89
.78
Table G3. Significant LAI group differences in substance use
Cigarettes per day
Cannabis
Amphetamines
FGA LAI
Mean SD
17.54
1.74
.96
19.32
1.82
1.40
SGA LAI
Mean SD t p
11.53 17.54 2.04 .045
.97 1.20 2.07 .042
.13 .51 3.10 .003
Cohen’s d
-.52
-.50
-.79
235
Table G4. LAI groups compared on SWN scales with language as a covariate
SWN total F p Effect size (partial η 2 )
Long acting injectable type .02 .88 .00
Oral antipsychotic type
Language
Total dosage converted into CPZE
1.23 .30
.617 .44
.03
.01
.433 .51
.01 .93
.01
.00 Interaction between long acting injectable and language
R
2
= .08 Adj. R
2
= .01
Positive SWN
Long acting injectable type
F
.56 p Effect size (partial η
.46 .01
2
)
Oral antipsychotic type
Language
.47 .62
2.70 .11
.01
.04
Total dosage converted into CPZE .35
.69
.56
.41
.01
.01 Interaction between long acting injectable and language
R 2 = .11 Adj. R 2 = .04
Self-control
Long acting injectable type
Oral antipsychotic type
F
.00 p
.99
1.60 .21
Effect size (partial η
.00
.04
2
)
Language
Total dosage converted into CPZE
1.90 .17
.18 .67
.01 .94
.03
.00
.00 Interaction between long acting injectable and language
R
2
= .11 Adj. R
2
= .03
236
Agreeableness
Neuroticism
Depression
Exercise
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
Affective symptoms
Neurological side-effects
Autonomic side-effects
Psychic side-effects
Sexual side-effects
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
Oral antipsychotic type
Interaction between LAI and oral type
Appendix H: Initial ANCOVA/MANCOVA analyses
Table H1. Initial model comparing LAI groups on total SWN with all covariates including side-effect subscales
Extraversion
Analysis with imputation of missing values (n
= 77)
R 2 = .80 Adj. R 2 = .70
F p
Partial η 2
7.338** .009 .133
Analysis with deletion of cases with missing data (n = 69)
R 2 = .83 Adj. R 2 = .73
F p
Partial η 2
6.550* .014 .138
9.440**
.174
5.272*
2.881
5.778*
.311
.821
1.033
5.375
.003
.678
.026
.096
.020
.580
.370
.315
.025
.164
.004
.099
.057
.107
.006
.017
.021
.101
7.762*
.118
4.963*
1.716
6.313*
.216
.516
1.615
5.947*
.008
.733
.031
.197
.016
.645
.476
.211
.019
.020
.171
.036
.131
2.030
2.405
.559
.960
.002
.269
1.012
.182
.887
.681
.850
.719
.161
.128
.458
.390
.969
.606
.371
.671
.000
.004
.001
.003
.041
.048
.012
.038
.000
.006
.040
.004
.090
.029
.004
.133
2.016
2.364
.225
1.598
.132
1.114
1.061
.014
.765
.865
.947
.717
.163
.132
.638
.215
.718
.297
.356
.907
.072
.003
.026
.049
.000
.159
.003
.108
.040
.133
.005
.012
.038
.127
.002
.001
.000
.003
.047
.055
.005
237
Table H2. Initial model comparing LAI groups on total SWN with all covariates including total side-effects
Extraversion
R
Analysis with imputation of missing
2 = .78 values (n = 77)
Adj. R 2 = .70
F p Partial η 2
4.658* .035 .079
Analysis with deletion of cases with
R 2 = .82 missing data (n = 69)
Adj. R 2 = .74
F p Partial η 2
6.982* .011 .137
Agreeableness
Neuroticism
8.824**
.003
.004
.956
.140
.000
7.757**
.041
.008
.841
.150
.001
Depression
Exercise
Health
Life difficulties
6.751*
3.604
8.173**
.514
.012
.063
.006
.476
.111
.063
.131
.009
5.972*
2.190
7.468**
.144
.019
.146
.009
.706
.120
.047
.145
.003
1.554
1.907
4.733*
.218
.173
.034
.028
.034
.081
.443
1.832
5.789*
.509
.183
.020
.010
.040
.116
Loneliness
Mental problems
Cognitive/disorganised symptoms
Affective symptoms
Total side-effects
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
Oral antipsychotic type
Interaction between
LAI and oral type
.119
.646
1.571
.023
1.538
.000
.000
1.137
.553
.731
.425
.215
.881
.224
.990
1.000
.328
.460
.002
.012
.028
.000
.054
.000
.000
.040
.010
.000
1.654
2.286
.003
1.939
.178
.807
1.299
.033
.995
.205
.138
.958
.156
.675
.374
.283
.858
.000
.036
.049
.000
.081
.004
.018
.056
.001
238
Table H3. Initial multivariate model comparing LAI groups on SWN factors with all covariates including sideeffect subscales
Analysis with imputation of Analysis with deletion of cases missing values (n = 77)
Wilks’ λ F with missing data p Partial η 2 Wilks’ λ F
(n = 69) p Partial η 2
Extraversion .877 3.29* .046 .123 .883 2.657 .083 .117
Agreeableness
Neuroticism
Depression
Exercise
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
Affective symptoms
Neurological sideeffects
Autonomic sideeffects
Psychic side-effects
Sexual side-effects
Red herrings
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
Oral antipsychotic type
.855
.980
.975
.946
.936
.801
.996
.840
.951
1.000
.974
.986
.942
.961
.999
.960
.990
.913
.987
.989
.891
5.82** .006
.090 .914
4.48* .017
1.224 .303
3.97* .025
.468 .629
.597 .555
1.331 .274
1.609 .211
.011 .989
.624 .540
.339 .714
1.439 .247
.966 .388
.015 .985
.989 .380
.245 .784
1.088 .367
.307 .737
.258 .774
1.396 .241
.145
.020
.025
.054
.064
.199
.004
.160
.049
.000
.026
.014
.058
.039
.001
.040
.010
.044
.013
.011
.056
.835
.974
.986
.935
.918
.812
.987
.818
.967
1.000
.987
.981
.955
.961
.982
.961
.995
.891
.972
.975
.918
4.63* .016
.255 .776
4.44* .018
.679 .513
3.94* .027
.541 .586
.285 .754
1.385 .262
1.793 .180
.006 .994
.263 .770
.382 .685
.942 .398
.821 .447
.358 .702
.809 .453
.095 .910
1.190 .322
.586 .561
.522 .598
.870 .486
.045
.039
.018
.039
.005
.056
.028
.025
.042
.165
.026
.014
.065
.082
.188
.013
.182
.033
.000
.013
.019
239
Table H4. Initial multivariate model comparing LAI groups on SWN factors with all covariates including total side-effects
Analysis with imputation of Analysis with deletion of cases missing values (n = 77)
Wilks’ λ F with missing data p Partial η 2 Wilks’ λ F
(n = 69) p Partial η 2
Extraversion .905 2.819 .068 .095 .873 3.190 .051 .127
Agreeableness
Neuroticism
Depression
Exercise
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
Affective symptoms
Total side-effects
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
Oral antipsychotic type
.994
.956
.970
.972
.921
.965
.998
.904
.825
.947
.965
.944
.951
.822
.989
.801
.946
5.851** .005
.288 .751
6.710** .002
1.552 .221
5.732** .006
1.502 .232
.982 .381
1.590 .213
1.379 .261
.169 .845
1.237 .298
.830 .442
.001 .972
1.139 .342
.978 .383
.064 .938
1.396 .240
.006
.044
.030
.001
.040
.035
.002
.049
.175
.053
.035
.056
.049
.178
.011
.199
.054
.999
.916
.952
.997
.889
.934
.978
.917
.826
.954
.990
.930
.912
.815
.989
.800
.949
5.000* .016
.234 .792
5.489** .007
1.189 .314
4.634** .015
1.072 .351
.216 .806
1.66 .201
2.120 .132
.024 .976
2.030 .144
1.104 .341
.061 .941
.001
.084
.048
.003
.174
.046
.010
.070
.088
.188
.011
.200
.051
1.336 .263 .057
1.546 .934 1.546
a
.505 .607 .022
.974 .426 .042
240
Table H5. Predictors of Negative SWN factor (side-effects subscales included)
Negative SWN
Extraversion
Analysis with imputation of missing values (n = 77)
R 2 = .70 Adj. R 2 = .55
F
1.312 p
.258
Partial η 2
.027
Analysis with deletion of cases with missing data (n = 69)
R 2 = .74 Adj. R 2 = .59
F
2.247 p
.142
Partial η 2
.052
Agreeableness
Neuroticism
Depression
Exercise
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
Affective symptoms
Neurological sideeffects
Autonomic sideeffects
Psychic side-effects
Sexual side-effects
Red herrings
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
Oral antipsychotic type
.519
.054
8.676**
1.600
.208
.897
1.053
1.021
1.021
1.021
1.021
1.021
1.021
1.021
.028
1.487
.012
1.849
.513
.009
.406
.651
.348
.310
.317
.317
.475
.817
.005
.212
.317
.317
.317
.168
.477
.923
.668
.317
.317
.869
.229
.914
.004
.018
.021
.021
.021
.011
.001
.153
.032
.021
.021
.021
.072
.011
.000
.017
.021
.021
.001
.030
.000
.082
.070
8.694**
.796
.258
1.030
.255
2.486
1.981
.013
.430
.655
1.893
1.034
.306
1.041
.192
1.505
1.044
.004
.196
.614
.316
.616
.123
.167
.775
.793
.005
.378
.910
.515
.423
.234
.313
.949
.823
.176
.315
.583
.314
.664
.068
.025
.000
.009
.044
.025
.007
.025
.005
.006
.025
.006
.057
.046
.002
.002
.175
.019
.000
.010
.016
241
Table H6. Predictors of Positive SWN factor (side-effects subscales included)
Positive SWN
Extraversion
Analysis with imputation of missing values (n = 77)
R 2 = .70 Adj. R 2 = .55
F
4.851* p
.032
Partial η 2
.092
Analysis with deletion of cases with missing data (n = 69)
R 2 = .83 Adj. R 2 = .73
F
2.329 p
.135
Partial η 2
.054
Agreeableness
Neuroticism
Depression
Exercise
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
Affective symptoms
10.793**
.146
.159
.670
7.578**
.112
.093
.006
1.528
.016
1.174 Neurological sideeffects
Autonomic sideeffects
Psychic side-effects
Sexual side-effects
Red herrings
.314
.419
.759
.001
.367
.468
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
.330
.165
.498
2.677 Oral antipsychotic type
.008
.740
.762
.937
.222
.002
.704
.692
.417
.901
.284
.578
.721
.687
.484
.079
.521
.388
.971
.547
.497
.136
.002
.002
.000
.031
.184
.003
.003
.014
.000
.024
.007
.014
.003
.010
.100
.009
.016
.000
.008
.010
8.897**
.500
.024
.384
7.179*
.194
.236
.112
1.123
.000
.185
.051
.644
.308
1.059
1.768
.171
.401
.310
.375
.001
.011
.662
.630
.740
.295
.005
.484
.878
.539
.987
.669
.823
.530
.582
.309
.183
.681
.530
.581
.544
.978
.000
.004
.001
.030
.007
.025
.079
.004
.010
.008
.009
.000
.149
.005
.006
.003
.027
.178
.012
.001
.009
242
Table H7. Predictors of Negative SWN factor (total side-effects included)
Negative SWN
Extraversion
Analysis with imputation of missing values (n = 77)
R 2 = .67 Adj. R 2 = .55
F
.157 p
.693
Partial η 2
.003
Analysis with deletion of cases with missing data (n = 69)
R 2 = .82 Adj. R 2 = .74
F
3.279 p
.077
Partial η 2
.068
Agreeableness
Neuroticism
Depression
Exercise
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
.439
.071
13.528**
1.209
.162
2.735
1.630
2.912
.956
Affective symptoms
Total side-effects
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
.243
2.432
1.608
.057
1.472
1.359
.018
.229 Oral antipsychotic type
.238
.249
.893
.796
.624
.125
.210
.813
.689
.104
.207
.094
.332
.510
.791
.001
.276
.051
.024
.000
.008
.004
.042
.028
.001
.003
.047
.029
.050
.017
.008
.001
.197
.022
.029
.022
10.76**
1.506
.230
1.813
.153
3.110
2.479
.010
4.151*
1.661
.026
1.796
2.730
.047
.036
.178
.105
.830
.965
.921
.048
.204
.873
.634
.185
.698
.085
.122
.865
.882
.002
.226
.074
.057
.001
.002
.000
.084
.036
.001
.005
.039
.003
.065
.052
.001
.000
.193
.032
243
Table H8. Predictors of Positive SWN factor (total side-effects included)
Positive SWN
Extraversion
Analysis with imputation of missing values (n = 77)
R 2 = .69 Adj. R 2 = .57
F
5.327* p
.025
Partial η 2
.088
Analysis with deletion of cases with missing data (n = 69)
R 2 = .70 Adj. R 2 = .57
F
2.345 p
.133
Partial η 2
.050
Agreeableness
Neuroticism
Depression
Exercise
10.881**
.470
.000
1.621
Health
Life difficulties
Loneliness
Mental problems
Cognitive/disorganised symptoms
11.099**
.550
.222
.150
1.562
Affective symptoms
Total side-effects
ROMI adherence
Combined antipsychotic dosage
Mood stabiliser use
Diagnosis
LAI type
Oral antipsychotic type
.069
.211
.023
.000
.673
.836
.121
2.708
.514
.364
.729
.076
.793
.648
.880
.982
.002
.461
.640
.700
.217
.002
.496
.986
.208
.024
.015
.002
.090
.001
.004
.000
.000
.168
.010
.004
.003
.028
.165
.008
.000
.029
9.849**
.476
.048
.611
8.671**
.637
.229
.087
1.276
.661
.778
.909
2.008
.033
.081
.343
.111
.521
.383
.345
.146
.856
.777
.561
.741
.005
.429
.634
.770
.265
.003
.494
.827
.438
.029
.017
.020
.082
.001
.002
.008
.002
.162
.014
.005
.002
.028
.180
.010
.001
.013
244
Appendix I: ANCOVA/MANCOVA analyses using imputation of missing data
Table I1 SWN as a function of medication groupings, personality, depression, health and cognitive/disorganised symptoms
SWN total F p -value Effect size (partial η 2 )
Extraversion 9.78** .003 .14
Agreeableness
Depression
Health
Cognitive/disorganised symptoms
Long acting injectable type
Oral antipsychotic type
9.09**
21.03***
15.42***
5.93*
1.16
1.35
Interaction between long acting injectable and oral type
R 2 = .77 Adj. R 2 = .73
Table I2 Multivariate predictors of SWN factors
Extraversion
.00
Analysis with imputation of missing
Wilks’ λ values (n = 77)
F p Partial η 2
.88 4.43* .016 .12
.96
Agreeableness
Depression
Health
Total side-effects
LAI type
Oral antipsychotic type
.78
.72
.79
.95
1.00
.89
9.50*** <.001
13.04*** <.001
9.11*** <.001
1.94
.13
1.96
.15
.88
.10
.22
.28
.21
.06
.00
.06
.004
<.001
<.001
.018
.29
.27
.02
.04
.00
.13
.26
.21
.09
245
Table I3 Predictors of Negative and Positive SWN factor scales
Negative SWN
Extraversion
Analysis with imputation of
R 2 = .70
F
.02 missing values
Adj. R 2 = .55 p
.90
Partial η 2
.00
Agreeableness
Depression
Health
Total side-effects
LAI type
Oral antipsychotic type
Positive SWN
Extraversion
.00
26.32***
1.07
3.86
.05
1.19
.98
<.001
.30
.053
.83
.31
Agreeableness
Depression
Health
Total side-effects
LAI type
Oral antipsychotic type
R 2 = .70
F
8.98**
19.28***
.25
17.42***
.07
.21
2.81
Adj. R 2 = .55 p
.004
Partial η 2
.01
<.001
.62
<.001
.78
.22
.00
.20
.00
.65
.07
.00
.08
.00
.28
.02
.05
.00
.03
246
Table I4 Multivariate predictors of SWN subscales
Wilks’ λ
Extraversion .89
Agreeableness .83
Neuroticism
Health
.86
.81
Exercise
Insight
Depression
Cognitive/disorganised symptoms
Negative symptoms
ROMI adherence
LAI group
Oral group
.89
.81
.75
.92
.94
.87
.91
.89
Table I5 Predictors of mental functioning
Extraversion
Agreeableness
Neuroticism
Health
Exercise
Insight
Cognitive/disorganised symptoms
Negative symptoms
Depression
ROMI adherence
LAI group
Oral group
R 2 = .60 Adj. R 2 = .52
F
.03
.32
1.73
19.42***
.76
.17
.07
.63
6.55*
.00
.00
1.45 p
.88
.57
.19
<.001
.39
.69
.79
.43
.013
.95
.98
.24
F
1.51
2.46*
2.00
4.13**
1.59
2.69*
3.90**
1.08
.73
1.79
1.13
.73
.18
.029
.004
.38 p
.20
.043
.09
.003
.60
.13
.36
.70
Partial η 2
.11
.17
.15
.26
.12
.19
.25
.08
.06
.13
.09
.06
Partial η 2
.00
.01
.03
.24
.01
.00
.00
.01
.09
.00
.00
.04
247
Table I6 Predictors of self-control
F
Extraversion
Agreeableness
Neuroticism
Health
Exercise
Insight
Cognitive/disorganised symptoms
Negative symptoms
Depression
ROMI adherence
.06
5.43*
.04
LAI group
Oral group
R 2 = .60
.02
1.23
Adj. R 2 = .52
Table I7 Predictors of emotional regulation
Extraversion
Agreeableness
Neuroticism
Health
Exercise
Insight
Cognitive/disorganised symptoms
Negative symptoms
F
6.62*
9.03**
.08
6.85*
3.41
.77
.87
Depression
ROMI adherence
LAI group
Oral group
R 2 = .68 Adj. R 2 = .61
1.63
4.76*
1.62
1.32
.52
2.51
5.31*
2.46
10.79**
.02
.17
.20 p
.21
.033
.21
.26
.48
.12
.024
.80
.023
.85
.90
.30
.12
.002
.88
.68
.82 p
.012
.004
.79
.011
.07
.38
.36
Partial η 2
.10
.13
.00
.10
.05
.01
.01
.04
.15
.00
.00
.00
Partial η 2
.03
.07
.03
.02
.01
.04
.08
.00
.08
.00
.00
.04
248
Table I8 Predictors of social integration
Extraversion
Agreeableness
Neuroticism
Health
Exercise
Insight
Cognitive/disorganised symptoms
Negative symptoms
F
.82
3.43
.16
.10
6.76*
.04
.27
Depression
ROMI adherence
LAI group
Oral group
R 2 = .48 Adj. R 2 = .37
.13
9.81**
1.35
.26
.36
Table I9 Predictors of physical functioning
Extraversion
Agreeableness
F
1.13
3.23
Neuroticism
Health
Exercise
Insight
1.15
7.32**
.48
3.22
Cognitive/disorganised symptoms
Negative symptoms
Depression
ROMI adherence
LAI group
Oral group
R 2 = .42 Adj. R 2 = .30
1.22
.41
1.80
5.58*
4.20*
2.23
.73
.003
.25
.61
.70 p
.37
.07
.69
.76
.012
.85
.61
.27
.52
.19
.021 p
.29
.08
.29
.009
.49
.08
.045
.12
Partial η 2
.01
.05
.00
.00
.10
.00
.00
.00
.14
.02
.00
.01
Partial η 2
.02
.05
.02
.10
.01
.05
.02
.01
.03
.08
.06
.07
249
Appendix J: Follow up data
Table J1 Breakdowns of oral antipsychotic and other adjunctive medications by LAI group
Oral antipsychotic taken
None
FGA oral
Haloperidol
Zuclopenthixol
Total
SGA oral
Risperidone
Paliperidone
Olanzapine
Quetiapine
Total
Total any oral medication
Mood stabiliser
None
Sodium valproate
Lithium carbonate
Antidepressant users
Benzodiazepine users
Benztropine users
FGA depot SGA depot
1
3
4
4
1
0
0
3
4
8
8
3
1
3
3
1
0
1
2
1
0
2
3
0
5
6
6
1
1
0
1
0
No depot
0
0
1
1
0
0
0
1
0
0
1
0
0
1
1
0
Table J2 Daily chlorpromazine equivalent (CPZE) dosages for each long acting injectable group.
Mean (Standard Deviation)
Dosage converted to daily
CPZE
FGA group SGA group t p
4
5
1
15
15
4
2
Total
1
4
6
5
2
2
3
3
10
Long acting injectable dosage 310.00 (211.58) 333.64 (112.80) -.29 .78
Oral dosage
Combined dosage
215.18 (147.60)
473.36 (173.58)
159.38 (183.19)
505.64 (287.28)
.74
.31
.47
.76
Cohen’s d
250
Table J3 Changes in oral medication from baseline
Oral medication at follow up
None FGA Baseline oral medication
None 3
H Z R O
FGA
Haloperidol
Zuclopenthixol
Total FGA
SGA
Risperidone
Olanzapine
Quetiapine
Clozapine
Total SGA
Follow up totals
2
2
7
1
1
1
2
3
3
3
2
2
SGA
Q
1
2
3
P
1
1
2
Total
4
Key: H = haloperidol; Z = zuclopenthixol; R = risperidone; O = olanzapine; Q = quetiapine; P = paliperidone
Table J4 Differences between follow up participants and drop-out participants
SWN total
Negative SWN
Positive SWN
Mental functioning
Self-control
Follow up status
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
N
56
21
56
21
56
21
56
21
56
Mean
69.32
61.67
38.13
35.90
32.21
27.48
14.07
12.24
13.73
Std.
Deviation
17.57
18.39
9.94
11.15
11.19
10.83
4.65
4.46
4.07 t p
1.68 .097
Cohen’s d
.39
.84 .40 .19
1.67
1.56
.10
.12
2.07 .042
.38
.36
.48
251
1
15
21
6
2
6
1
2
1
Emotional regulation
Social integration
Physical functioning
Extraversion
Agreeableness
Conscientiousness
Neuroticism
Openness to experience
Depression
Anxiety
Stress
Total side-effects
Neurological SE
Autonomic SE
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Successful 53
56
21
56
21
Not followed
21
Successful 53
Not followed
21
Successful 53
56
21
56
21
21
56
21
21
56
21
56
21
56
Not followed
Successful
21
21
53 Not followed
Successful
Not followed
Successful
21
53
Not followed
21
53
2.74
2.89
3.50
3.12
11.77
15.71
12.62
3.24
2.80
3.81
3.69
3.75
3.42
11.52
14.64
12.95
13.41
12.33
13.46
11.36
14.19
13.59
16.67
34.38
28.77
6.43
4.89
9.48
8.08
.81
.90
.86
.76
10.95
10.90
4.41
.942
.66
.762
.67
.86
.67
4.47
4.36
4.20
4.71
4.53
4.47
1.53 .13
.90 .37
.74 .46
9.08
10.10
-1.17 .25 -.27
10.75 -1.11 .27 -.26
11.00
21.75 -1.15
17.63
5.68
4.14
.25 -.27
-1.30 .20 -.30
7.45
7.13
-.75 .45 .17
.35
.21
.17
1.94 .06
.62 .54
1.59 .12
-.70 .49 -.16
1.79 .08 .41
-1.40 .17 -.32
.14
.37
.45
252
Psychic side-effects
Sexual SE
Positive
Negative
Cognitive/disorganised
Affective
Hostile excitement
PANSS total
Premorbid IQ
WTAR IQ estimate
Information IQ estimate
Immediate memory
Visuospatial constructional
Language
Attention
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
Not followed
Successful
2.38
2.20
1.98
2.00
2.18
1.90
2.63
2.21
72.00
68.13
11.81
10.45
3.43
3.21
2.85
3.19
75.71
83.54
79.10
85.23
69.38
90.43
94.40
91.33
95.67
89.52
98.98
53.67
63.98
21
48
21
48
21
48
21
48
21
48
21
53
21
53
21
48
21
48
21
48
21
21
49
21
48
21
49
21
46
.70 -1.15
1.03
.69 -1.98
.88
.78 -.85
.79
.75 .091
.84
13.22 -.974
15.98
7.45
6.43
3.12
3.18
1.02 1.29
1.01
-.78 .44
-.271 .79
.20
10.60 .915
18.57
9.41 1.493
11.69
15.72 2.14
17.47
12.21 2.46
17.36
.40
.93
.25
.052
-.03
.036
.016
.33
.36
.14 -.41
.26
-.26
.49
.57
.30
.27
.18
.06
.46
.23
15.52 1.70
18.40
15.53 1.42
16.84
15.67 .64
.09 .39
.16
.53
-.38
-.17
253
Not followed
Successful
48
21
72.38
58.86
18.82
17.56 2.27 .027 .52
Delayed memory
Not followed
Successful
48
21
69.27
60.14
17.57
11.93 2.32 .023 .54
RBANS total
Not followed
Successful
48
20
68.67
11.00
14.84
7.51 -.84 .40 .22
Insight
Not followed
Successful
49 9.30 7.64
ROMI adherence
21 1.81 .45 -.78 .44
Not followed
Successful
48
21
1.72
1.30
.43
. 40 .25 .80
ROMI nonadherence
Not followed
Successful
48 1.32 .33
ROMI total score
21 .51 .64 -.73 .47
Not followed
48 .40 .57
Table J5 Correlations between SWN scales at follow up and other variables also at follow up
Mental
Functioning
Self
Control
Emotional
Regulation
Physical
Functioning
Social
Integration
Health .564* .388 .606* .377 .542*
.20
-.05
.18
SWN
Total
.737**
Exercise
Life Difficulties
.275
-.272
-.120
.082
.115
-.284
.100
-.231
-.004
-.399
.109
-.341
Loneliness Last Month
Mental Problems
Total side-effects
Red Herrings
Neurological side-effects
(EPS)
Autonomic side-effects
Sexual side-effects
Depression
-.491
-.349
-.476*
-.394
-.359
-.504*
-.277
-.273
-.509*
.042
.134
-.103
-.365
-.318
.085
-.088
-.474*
-.410
-.356
-.226
-.369
-.306
-.427
-.184
-.378
-.395
-.753**
-.043
-.007
-.303
-.117
-.263
-.242
-.225
-.037
-.432
-.303
-.251
-.343
-.272
-.449*
-.077
-.497*
-.353
-.730**
-.360
-.226
-.408
-.364
-.458*
-.241
-.374
-.380
-.718**
254
Anxiety
Stress
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
Excitement symptoms
PANSS total
-.466*
-.651**
-.190
-.205
-.413
-.210
-.055
-.528*
-.395
-.632**
-.059
-.247
-.345
-.091
-.289
-.396
-.593**
-.735**
-.386
-.370
-.536*
-.026
-.074
-.709**
-.320
-.556**
-.357
.012
-.393
-.163
-.198
-.473*
-.610**
-.601**
-.507*
-.437
-.382
.131
.049
-.582**
Table J6 Correlations of negative and positive SWN with other variables from follow up assessment
Depression
Negative SWN
-.551**
Positive SWN
-.694**
Anxiety -.525* -.516*
Stress
Neurological side-effects (EPS)
Autonomic side-effects
Psychic side-effects
-.770**
-.317
-.287
-.487*
-.616**
-.463*
-.157
-.221
Sexual side-effects
Red Herrings
Total side-effects
Positive symptoms
Negative symptoms
-.117
-.190
-.417
-.416
-.139
-.522*
-.410
-.317
-.239
-.443
Affective symptoms
Cognitive/disorganised symptoms
Excitement symptoms
PANSS total
Health
Exercise
Life Difficulties
-.647**
-.196
-.223
-.66**
.746**
.020
-.672**
-.272
.050
.036
-.54*
.496
.152
-.049
-.602**
-.801**
-.384
-.313
-.525*
-.091
-.141
-.682**
255
Loneliness Last Month
Mental Problems
-.749**
-.448
-.031
-.053
Table J7 Correlations of follow up SWN scores with baseline variables
Mental
Functioning
Self
Control
Emotional
Regulation
Physical
Functioning
Social
Integration
Extraversion .266 .152 .308 .150 .214
Agreeableness
Conscientiousness
.308
-.134
.515*
.104
.728**
-.022
.264
-.196
.652**
.096
Neuroticism
Openness to experience
Health
Exercise
-.163
.484*
.677**
.210
-.238
.067
.398
.040
-.541*
.236
.396
.253
-.047
.360
.438*
.075
-.486*
-.017
.134
.176
Life Difficulties
Loneliness Last Month
Mental Problems
Total side-effects
Red Herrings
Neurological side-effects
(EPS)
Autonomic side-effects
Psychic side-effects
Sexual side-effects
Depression
Anxiety
Stress
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
-.049
-.432
-.094
-.115
-.067
-.189
-.199
-.008
.026
-.203
-.193
.014
.15
-.14
-.40**
-.09
-.054
-.090
-.186
-.254
-.233
-.327
-.285
.020
-.361
-.376
-.314
-.232
-.01
-.13
-.48**
-.33**
-.169
-.411
-.337
-.377
-.321
-.380
-.370
-.250
-.186
-.505*
-.431
-.274
.05
-.31**
-.49**
-.23*
-.071
-.417
-.064
-.197
-.137
-.153
-.217
-.045
-.155
-.252
-.267
.047
-.21
-.06
-.35**
-.22
-.075
-.382
-.299
-.376
-.267
-.318
-.319
-.264
-.248
-.469*
-.484*
-.426
-.03
-.12
-.36**
-.21
SWN
Total
.277
.620**
-.044
-.371
.292
.518*
.193
-.107
-.444*
-.246
-.332
-.257
-.343
-.350
-.140
-.228
-.454*
-.426
-.215
-.01
-.19
-.52**
-.26*
256
Excitement symptoms
PANSS total
.08
-.18
-.01
-.31**
-.00
-.35**
Table J8 Correlations of follow up SWN factors with baseline variables
Negative SWN Positive SWN
Extraversion .428 .125
Agreeableness
Conscientiousness
.489*
.151
.598**
.020
Neuroticism
Openness to experience
Depression
Anxiety
-.534*
.218
-.404
-.403
-.204
.289
-.351
-.306
Stress
Neurological side-effects (EPS)
Autonomic side-effects
Psychic side-effects
Sexual side-effects
Red Herrings
Total side-effects
Positive symptoms
Negative symptoms
Affective symptoms
Cognitive/disorganised symptoms
Excitement symptoms
PANSS total
Health
Exercise
Life Difficulties
Loneliness Last Month
-.340
-.511*
-.402
-.255
-.192
-.255
-.450*
.105
.218
-.346
-.155
.045
-.006
.566**
.355
-.170
-.555**
-.113
.328
.025
-.021
-.249
-.120
-.141
.154
-.197
-.193
.041
-.043
-.094
-.204
-.006
-.135
-.176
-.05
-.33**
.07
-.25*
.03
-.36**
257
Mental Problems -.432 -.043
Table J9 Means for side-effects scales, effect size compares FGA and SGA long acting injectable groups
Total side-effects
Neurological sideeffects (EPS)
Autonomic sideeffects
Red Herrings
Total
FGA
SGA
Total
Sexual side-effects FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
N Mean
12 38.25
8 26.63
21 8.81
12
8
21
12
8
6.75
4.50
6.00
14.33
8.25
Std.
Deviation
23.79
17.22
6.86
5.67 1.02
3.16 t
1.19
4.79
14.02 1.12
21 12.23
12 12.67
8 10.75
21 12.48
3.75 12
8
21
12
8
21
2.63
3.24
9.67
7.75
8.81
7.42
11.77
6.61 .55
9.07
7.79
3.60 .75
2.72
3.18
7.38
6.78
6.86
.59 p
.25
.32
.28
.59
.46
.56 .27
.24
.35
Cohen’s d
.56
.49
.54
258
Table J10 PANSS Factor scores for each long acting injectable group.
Positive factor
Negative factor
Cognitive/disorganised FGA
SGA
Affective factor
Total
FGA
SGA
Excitement factor
PANSS Total
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
FGA
SGA
Total
2.33
.74
.80
-.03 t
.78
.11
2.47
1.71
2.19
1.79
1.59
1.69
66.27
60.71
64.74
1.98
1.94
2.51
2.45
2.46
Mean
3.02
Std.
Deviation
1.18
2.59
2.98
1.92
.98
1.19
.82
.84
.58
.80
.51
.58
.52
14.12
14.83
14.10
.49
.68
.66
.74
.66
.37
.38
.09
1.05
Cohen’s d
.40
-.09
.47
.44
.98
.034
.91 p
.45
259
Table J11 Changes in RBANS indexes in each long acting injectable group
Immediate memory
LAI
FGA
SGA
N
11
7
11
Mean
4.45
5.29
.55
Std.
Deviatio n
13.78
12.32
20.18 t
-.13 p
.90
.11 .92
Cohen’s d
-.06
.05 Visuospatial constructional
FGA
SGA 7 -.43 16.79
Language FGA
SGA
11
7
5.27
6.86
9.00
16.36
-.12
Attention
Delayed memory
FGA
SGA
FGA
SGA
11
7
11
7
2.82
-1.29
-.73
7.42
13.34
7.06
6.90
20.07
-.27 .79
.75 .47
-1.26 .23
.14
-.54
RBANS
Total
FGA
SGA
11
7
3.09
3.57
5.36
7.93
-.15 .80 -.07
Table J12 Mean changes in insight and ROMI scales. Correlations between baseline and follow up scores are shown
Change in insight score
N
20
Minimum Maximum
-11.00 13.00
Mean
.85
Std. Deviation
5.53 r (Correlation between baseline and follow up scores)
.70**
20 -.86 .86 -.04 .43 .42 ROMI adherence change
ROMI nonadherence change
ROMI total change
20
20
-.77
-.86
.54
1.05
-.03
-.01
.31
.54
.65**
.57**
260
Table J13 Correlations of changes in insight and ROMI scores changes in SWN scale scores
SWN scale Insight ROMI ROMI ROMI total change adherence nonadherence
SWN total .02 -.26 -.09 -.16
-.22 .21 .24 -.03 Negative
SWN
Positive
SWN
Mental functioning
Self-control
Emotional regulation
Social integration
Physical functioning
-.13
.19
-.15
.30
-.17
-.05
-.15
-.24
.08
-.16
-.04
-.32
.35
.25
.53*
.04
-.17
-.30
-.27
-.04
-.25
-.15
.07
-.09
261