Document
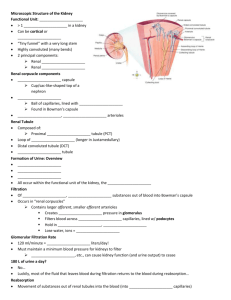
advertisement

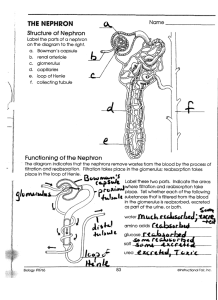
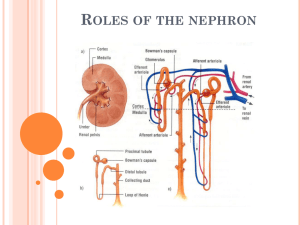
10.1 – Overview of the Excretory System (Taken from Biology 12, MHR, 2011) - The excretory system (urinary system) produces urine and conducts it to outside the body. Functions of the Excretory System 1) Excretion of Metabolic Wastes - The kidneys excrete metabolic waste (mainly nitrogen-containing waste). - Nitrogenous wastes include ammonia, urea, and uric acid. 2) Maintenance of Water-Salt Balance - By regulating salts in the blood, the kidneys are involving in regulating blood pressure. - The kidneys also maintain appropriate levels of potassium (K+), bicarbonate (HCO3-), and calcium (Ca2+) in the blood. 3) Maintenance of Acid-Base Balance The kidneys monitor and help keep the blood pH at about 7.4 by excreting hydrogen ions (H+) and reabsorbing the bicarbonate ions (HCO3-) when needed. 4) Secretion of Hormones The kidneys secrete two hormones: calcitriol and erythropoietin. Calcitriol (active form of vitamin D) promotes absorption of calcium (Ca2+) from the digestive system. Erythropoietin stimulates the production of red blood cells and is released in response to increase oxygen demand. The kidneys also secrete renin which leads to the secretion of aldosterone from the adrenal cortex. Organs of the Excretory System - See Figure 10.2, pg 445 Kidneys are supplied “junk” blood by renal arteries. Renal veins return “clean” blood to the heart so it can be circulated back around the body. At any given time, up to 25% of the body’s blood is held by the kidneys. The waste that filters out of the blood collects in the ducts of the kidneys and is moved into the bladder via the ureters. At the base of the bladder is a sphincter muscle that acts as a valve, permitting the storage of urine. As the bladder fills, first to 200mL, then 400mL, it activates stretch receptors and sends a message to the brain to urinate. If this is ignored and the bladder fills up to 600mL, the sphincter loses control, and the urine enters the urethra. The Kidneys - The kidneys are bean shaped and reddish in colour. Figure 10.3, pg 446 illustrates a cross-section of the kidney the outer layer, the renal cortex, encircles the kidney the inner layer, the renal medulla, is found beneath the cortex a hollow chamber, the renal pelvis, joins the kidney with the ureter The Nephron Nephrons are functional units of the kidney. They are embedded within the renal cortex and extend into the renal medulla. The nephrons are responsible for filtering various substances from blood, transforming it into urine. Each nephron is organized into three main regions: a filter, a tubule, and a collecting duct. See Figure 10.4, pg 447 Filter Tubule - Each nephron is supplied with blood by the afferent arterioles, which branch into a capillary bed, called the glomerulus a cluster of arterioles enclosed in a capsule is called Bowman’s capsule. The glomerulus act as a filtration device. They are impermeable to proteins, large molecules, and red blood cells therefore they remain in the blood. Water, small molecules, ions, and urea are filtered from the blood. This filtered fluid that enters the Bowman’s capsule is referred to as filtrate and will eventually become urine. Blood leaves the glomerulus through other arterioles, the efferent arterioles. The tubule has three sections: the proximal tubule, the loop of Henle, and the distal tubule. This tubule absorbs substances that are needed by the body (glucose and variety of ions) from the filtrate. The tubules also secrete substances into the tissues surrounding it. Collecting Duct The collecting duct is a large pipe-like channel that functions as a waterconservation device, reabsorbing water from the filtrate so that little water is lost from the body. The remaining filtrate is now called urine. Summary of Nephron Structure and Description Structure afferent arteriole glomerulus efferent arteriole peritubular capillary bed venule - HOMEWORK: Description -carries blood to the glomerulus -a high-pressure capillary bed enclosed by the Bowman’s capsule -carries arteriolar blood away from the glomerulus -capillaries that network around the nephron -reabsorbs solute from the nephron into the blood and secretes solute from the blood into the nephron -carries filtered blood back to the heart pg 448 #1-10 10.2 – Urine Formation in the Nephron - There are 4 processes that result in the formation of urine: glomerular filtration, tubular reabsorption, tubular secretion, and water reabsorption. 1) - Glomerular Filtration The movement of water and solutes from the blood into the Bowman’s capsule (nephron) is called filtration. This fluid is called the filtrate. Each nephron of the kidney has an independent blood supply, and blood moves through the afferent arteriole into the glomerulus, a high pressure filter. The pressure in the Bowman’s capsule is about 4x as much as in normal capillary beds. Plasma proteins, blood cells, and platelets are too large to move through the walls of the glomerulus. Smaller molecules pass through the walls and enter the nephron. According to Table 10.1, pg 451, the filtrate is identical to blood plasma – minus proteins and blood cells. 2) - Tubular Reabsorption Tubule reabsorption removes useful substances (sodium) from the filtrate and returns them into the blood for reuse by body systems. About 65% of the filtrate that passes through the proximal tubule and loop of Henle is reabsorbed and returned to the body. If none of the filtrate were reabsorbed, you would form 120mL of urine each minute, and would be requiring 1L of fluids every 10 minutes to maintain water balance. Both active and passive transport help reabsorb the fluids. See Figure 10.7, pg 451 Active Transport Nutrients (e.g., glucose, amino acids, Na+, K+) are actively reabsorbed. Carrier molecules move Na+ ions across the cell membranes of the cells that line the nephron. Reabsorption occurs until the threshold level of a substance is reached, excess NaCl remains in the nephron and is excreted with the urine. Other molecules are actively transported from the proximal tubule, such a glucose and amino acids, as they “hitch a ride” with specific carrier molecules that “shuttle” them out of the proximal tubule and back into the blood. Passive Transport Negative ions, such as Cl-, are passively reabsorbed by electrical attraction to Na+. Water is reabsorbed by osmosis. Focussing on the Loop of Henle in the Proximal Tubule 3) 4) - The function of the loop of Henle is to reabsorb water and ions from the glomerular filtrate. The descending limb of the loop of Henle is permeable to water and only slightly permeable to ions. As a result of the salty environment of the medulla and permeability of the descending limb, water diffuses from the filtrate to the capillaries by osmosis. See Figure 10.8A, pg 452 Near the bend in the loop of Henle (thin portion of the ascending limb), the tubule is impermeable to water and slightly permeable to solutes. Sodium ions diffuse from filtrate and pass into nearby blood vessels. See Figure 10.8B, pg 452 At the thick portion of the ascending limb, sodium ions are moved out of the filtrate by active transport. See Figure 10.C, pg 452 By now, about two thirds of the Na+ and water from the filtrate has been reabsorbed. Tubular Reabsorption and Secretion in the Distal Tubule The movement of additional wastes and excess substances from the blood back into the nephron (filtrate) is called secretion. Potassium (K+), excess H+ ions, and other minerals are balanced with secretion. Like reabsorption, tubular secretion occurs by active transport – unlike reabsorption, molecules are shuttled from the blood into the nephron. Reabsorption and secretion in the distal tubule are controlled by hormones. See Figure 10.9 Water Reabsorption from the Collecting Ducts Water reabsorption removes water from the filtrate and returns it to the blood for reuse by body systems. Because the collecting ducts extend into the medulla, the concentration of ions along its length increases. This causes the passive reabsorption of water from the filtrate in the collecting ducts by osmosis. If the blood plasma is too concentrated, the permeability to water in the distal tubule and the collecting duct is increased. The body wants to conserve water so more water is reabsorbed into the surrounding capillaries. Hormones also control reabsorption and secretion in the collecting ducts. A Summary of Nephron Functions (Figure 10.3, pg 454) Part of the Nephron Glomerulus Function Filtration Glomerular blood pressure forces some of the water and dissolved substances from the blood plasma through the pores of the glomerular walls Receives filtrate from glomerulus Reabsorption Active reabsorption of all nutrients, including glucose and amino acids Active reabsorption of positively charged ions such as sodium (Na+), potassium (K+), and calcium (Ca2+) Passive reabsorption of water by osmosis Passive reabsorption of negatively charged ions such as chloride (Cl-) and bicarbonate (HCO3-)by electrical attraction to positively charged ions Bowman’s capsule Proximal tubule Descending loop of Henle Ascending loop of Henle Distal tubule Secretion Active secretion of hydrogen ions (H+) Reabsorption Passive reabsorption of water by osmosis Reabsorption Active reabsorption of sodium ions (Na+) Passive reabsorption of chloride and potassium ions Reabsorption Active reabsorption of sodium ions (Na+) Passive reabsorption of water by osmosis Passive reabsorption of negatively charged ions such as chloride (Cl-) and bicarbonate (HCO3-) Secretion Active secretion of hydrogen ions (H+) Passive secretion of potassium ions (K+) by electrical attraction to chloride ions (Cl-) Reabsorption Passive reabsorption of water by osmosis Collecting duct Animation of the Kidney http://www.biologymad.com/resources/kidney.swf HOMEWORK: pg 455 #1 - 12 Urine Formation (Table 2, pg 351) Site Description of Process Substances Transported 1.glomerulus and Bowman’s capsule -Filtration of water and dissolved solutes occurs as blood is forced through walls of glomerulus into Bowman’s capsule by fluid pressure in capillaries. 2.proximal tubule -Selective reabsorption of nutrients from filtrate back into blood by active and passive transport. -Within proximal tubule, pH is controlled by secretion of hydrogen ions (H+) and reabsorption of bicarbonate ions (HCO3-). -Descending limb of loop of Henle is permeable to water, resulting in loss of water from filtrate by osmosis. -Salt (NaCl) becomes concentrated in filtrate as descending limb penetrates inner medulla of kidney. -Thin segment of ascending limb of loop of Henle is permeable to salt, resulting in diffusion of salt out of ascending limb. -Salt continues to pass from filtrate to interstitial fluid in thick segment of ascending limb. -Selective reabsorption of nutrients from blood into nephron by active transport. Distal tubule helps regulate potassium (K+) and salt (NaCl) concentration of body fluids. -As in proximal tubule, pH is controlled by tubular secretion of hydrogen ions (H+) and reabsorption of bicarbonate ions (HCO3-). -Urine formation. -sodium ions (Na+), chloride ions (Cl-), water (H2O), hydrogen ions (H+), glucose, amino acids, vitamins, minerals, urea, uric acid -bicarbonate ions (HCO3-), salt (NaCl), water (H2O), potassium ions (K+), hydrogen ions (H+), ammonia (NH3), glucose, amino acids, vitamins, urea 3.descending limb of loop of Henle 4.ascending limb of loop of Henle 5.distal tubule 6.collecting duct -water (H2O) -salt (NaCl) -salt (NaCl), potassium ion (K+), water (H2O), hydrogen ions (H+), bicarbonate ions (HCO3-), uric acid, ammonia (NH3) -water (H2O), salt (NaCl), urea, uric acid, minerals 10.3 – Other Functions and Disorders of the Excretory System - Basically, the body adjusts for increased water intake by increasing urine output, and it adjusts for low water levels in the blood by reducing urine output (more concentrated). In order for these adjustments to take place, 2 body systems must interact: nervous system and endocrine system. Regulating Water-Salt Balance Reabsorption of Water (Blood Volume) - The body produces a hormone called antidiuretic hormone (ADH) which helps regulate the osmotic pressure of body fluids by causing the kidneys to increase water reabsorption. When ADH is released, a more concentrated urine is produced conserving water. ADH is produced by specialized nerve cells in the hypothalamus. The pituitary gland stores and releases ADH into the blood. Changes in osmotic pressure in the blood are picked up by specialized nerve receptors in the brain called osmoreceptors. If your blood water level drops because of sweating, blood solutes become more concentrated, which increases the blood’s osmotic pressure – water moves out of cells and into the bloodstream. When the cells of the hypothalamus shrink, a nerve message is sent to the pituitary, signaling the release of ADH. The ADH is carried by blood to the kidneys, making the tubules more permeable to water, which allows more water to be reabsorbed into the blood more concentrated urine is produced. A greater amount of water in the blood causes its osmotic pressure to stop increasing and prevents body cells from losing water to the blood and become dehydrated. The shrinking of the hypothalamus cells also initiates a behavioural response – the sensation of thirst. As soon as the amount of water in the blood increases and the hypothalamus cells swell, the nerve messages signal the pituitary to stop, ADH is not released, and less water is reabsorbed from the nephrons. ADH and the Nephron - ADH makes the upper part of the distal tubule and collecting duct permeable to water. The water leaves the upper part of the distal tubule and enters the blood. This makes the blood more dilute while making the urine more concentrated. - See Figure 10.11, pg 457 - In a condition called diabetes insipidus, ADH activity is insufficient so the reabsorption of water cannot occur. A person with diabetes insipidus urinates excessively – as much as 4 L to 8 L per day. They may need to take synthetic ADH to restore the balance of water reabsorption. - Alcoholic beverages and Caffeine - Both alcohol beverages and caffeine are diuretics increase volume of urine. - Diuretics inhibit the release of ADH which decreases the permeability of the tubules and collecting ducts for water. As a result, less water is reabsorbed into the blood and more water stays in the urine. Reabsorption of Salts (Blood Pressure) - Kidneys play a role in regulating blood pressure by adjusting for blood volumes. A hormone called aldosterone (produced in the cortex of the adrenal gland) acts on the nephrons to increase Na+ reabsorption in the distal tubules and collecting ducts. As NaCl reabsorption increases, the osmotic gradient increases and more water moves out of the nephron by osmosis. Blood pressure receptors in the juxtaglomerular apparatus (found near the glomerulus) detect low blood pressure. Specialized cells within the structure release renin, an enzyme that converts angiotensinogen – a plasma protein – into angiotensin. Angiotensinogen has two important functions: 1) Causes constriction of blood vessels. Blood pressure increases when the diameter of blood vessels is reduced. 2) Stimulates the release of aldosterone from the adrenal gland. Aldosterone is then carried in the blood to the kidneys, where it acts on the cells of the distal tubule and collecting duct to increase Na+ transport. This causes the fluid level of the body to increase thus increasing blood pressure. - Since Na+ reabsorption is followed passively by chloride ions (Cl-) and water, aldosterone has the net effect of retaining both salt and water. As a result, blood volume and blood pressure increase. Juxtaglomerular Apparatus http://www.wisc-online.com/objects/ap2204/ap2204.swf Regulating Blood pH - The pH of the body remains relatively constant, between 7.3 and 7.5. In addition to regulating body fluid volumes and maintaining the composition of salts in the blood, the kidneys also maintain pH balance. There are three mechanisms that keep blood pH at about 7.4: acid-base buffer system, respiration, and the function of the kidneys. Acid-Base Buffer System - An acid-base balance is maintained by buffer systems that absorb excess H+ ions or ions that act as bases. - Excess H+ ions from metabolic processes are buffered by bicarbonate ions (HCO3-) in the blood. Carbonic acid (H2CO3) is produced in the process. - In turn, the carbonic acid breaks down to form carbon dioxide and water. Respiration - If H+ ion concentration in the blood increases, the medulla oblongata increases the breathing rate. - The carbon dioxide is then transported to the lungs where much of it is exhaled. - When carbon dioxide is exhaled, the number of hydrogen ions is reduced. The Kidneys - The kidneys excrete H+ and reabsorb HCO3- as needed to maintain normal blood pH. - If the blood is too acidic, H+ is excreted and HCO3- is reabsorbed. - If the blood is too basic, H+ is not excreted and HCO3- is not reabsorbed. - Ammonia (NH3) provides another means of buffering and removing the hydrogen ions in the urine. Remember, ammonia is produced by the breakdown of amino acids. - See Figure 10.12, pg 459 Releasing Hormones - The kidneys secrete renin which leads to the secretion of aldosterone from the adrenal cortex. The kidneys also secrete two hormones: calcitriol and erythropoietin. Calcitriol - If the level of Ca2+ in the blood falls below normal, parathyroid hormone (PTH) is released by the parathyroid gland. - PTH stimulates the release of calcitriol by the kidneys. - Calcitriol (active form of vitamin D) promotes absorption of calcium (Ca2+) from the digestive system. Erythropoietin Erythropoietin stimulates the production of red blood cells and is released in response to increase oxygen demand or when the oxygen-carrying capacity of blood decreases. Disorders of the Excretory System Urinary Tract Infection - If the bladder has a bacterial or viral infection, the disorder is called cystitis; if only the urethra is involved, the condition is called urethritis. - UTI’s are more common in women. - Symptoms of UTI’s include painful burning sensation during urination, need to urinate frequently, and bloody or brown urine. - Treatment is usually with antibiotics but in more serious cases surgery may be needed. Kidney Stones Most stones consist of calcium. Most kidney stones form due to excess calcium in the urine. Very painful. Many stones pass through the urinary tract on their own. Traditional treatment for kidney stones has been surgical removal followed by a period of rest. A new technique called extracorporeal shock-wave lithotripsy (ESWL) uses high-energy shock waves to break the kidney stones into small fragments. After a few days, tiny granules from the stone can be voided through the excretory system. Figure 10.13, pg 461 Diabetes Mellitus - Diabetes is caused by the inadequate secretion of insulin from the pancreas. - Insulin allows glucose to enter a cell (insulin allows the cell membrane to become permeable). - Because of the higher concentration of glucose in the kidneys, it opposes the osmotic pressure of other solutes that have left the nephron. - This results in water not being able to be reabsorbed therefore, water is lost in urine. - Individuals with Diabetes Mellitus are always thirsty. Diabetes Insipidus - This is the destruction of ADH producing cells in the hypothalamus or the destruction of the nerve tracts leading to the pituitary gland therefore, urine output increases. - In extreme cases, an individual can lose 20 L of dilute urine in one day. Bright’s Disease (Nephritis) - Invading microbes destroy the tiny blood vessels in the glomerulus, thereby altering the permeability of the nephron. - Proteins and other large molecules are able to pass into the nephron. - Proteins cannot be reabsorbed therefore, drawing water into the nephrons results in increased urine output. Treatment of Kidney Disease - Dialysis and transplants are currently the most common treatments for kidney disease. Dialysis: the exchange of substances across a semi-permeable membrane. Like a normally functioning kidney, a dialysis machine operates on the principles of diffusion and blood pressure. Unlike a kidney, a dialysis machine cannot perform active transport. There are two types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis - The machine is connected to the patient’s circulatory system by a vein. - Blood is pumped through a series of dialysis tubes that are submerged in a bath of various solutes. Glucose and a mixture of salts set up concentration gradients. - Urea will move from the blood into the dialysis fluid until equal concentrations are established. - By continually flushing expended dialysis solution and replacing it, urea and other waste solutes are continuously removed. - During hemodialysis, the body also receives the hormones the kidneys are unable to produce. - See Figure 10.14A, pg 462 Peritoneal Dialysis - 2 L of dialysis fluids is pumped into the abdominal cavity, and the membranes of the cavity selectively filter wastes from the blood. - Urea and other wastes diffuse from the plasma into the peritoneum and into the dialysis fluid. - Wastes accumulate in the dialysis fluids, which can be drained off and replaced several times a day. - Patient may continue with less strenuous activities. Peritoneal dialysis allows for greater independence because patients can perform the procedure on their own at home. - See Figure 10.14B, pg 462 Kidney Transplants - Individuals with 10% or less kidney function will eventually need new kidneys. - Organ donation rate in Canada is very low compared to other developed countries. - The success rate of organ transplantation is around 95-98%. - Surgical techniques, such as laparoscopic surgery are constantly being improved. - The main disadvantage with any transplant is the immune response of the recipient. - The donor kidney is often identified as a foreign invader and the recipient’s immune system acts in an attempt to destroy it. - New medicines to prevent rejection of the new organ are constantly being developed and improved. Evaluating Kidney Function - Physicians use urinalysis and blood tests to make reasoned inferences and hypotheses about a person’s health and kidney function. - See Table 10.4, pg 464 for normal values from common urine tests. - Blood tests can also reveal information about kidney function. - Blood can be tested to measure the amount of urea and creatinine it contains. High levels of urea or creatinine indicate that the kidneys are not working properly. HOMEWORK: pg 465 #1 - 10