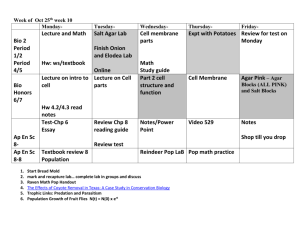
Class schedule of microbiology for the 3rd year students of English
advertisement

Class schedule of microbiology for the 3rd year students of English Division Academic Year 2013/2014 Groups I, II, III & IV: Tuesday 13.45 – 16.00 (class room) (total: 40 hours) Groups: V, VI, VII & VIII: Friday 7.30 – 9.45 (class room) Laboratory sessions of microbiology last 135 minutes and are held every two weeks in the student laboratory in the Department of Medical Microbiology ul. Chałubińskiego 4 GENERAL SCHEDULE OF CLASSES IN WINTER SEMESTER: WINTER SEMESTER 7 weeks x 3 hours = 21 hours Class 1. Bacterial morphology, staining and growing bacteria in culture Class 2. Gram-positive cocci: staphylococci and streptococci. Class 3. Gram-negative anaerobic, fermentative, intestinal and nonfermentative rods; Class 4. Gram-positive bacilli, corynebacteria, Actinomyces and Mycobacterium. Class 5. Spiral bacteria. Class test #1 Class 6. Antisepsis. Antimicrobials – part I Class 7. Antimicrobials – part II 30.IX – 04.X 2013 14.X – 18.X 2013 28.X – 1.XII 2013 11.XI – 15.XI 2013 25.XI – 29.XI 2013 09.XII – 13.XII 2013 13.I – 17.I 2014 Class 1. Tuesday 1.10.13; Friday 4.10.13. Bacterial morphology, staining and bacterial cultures Learning objectives: a) work organization and safety precautions at classes of microbiology; b) types of microscopes used during classes of microbiology: bright-filed, dark-field and fluorescent; c) bacterial cells morphology; d) staining techniques used in bacteriology: simple (Loffler), complex (Gram), negative staining, and negative-positive staining; e) growth requirements for in vitro culturing aerobic and anaerobic bacteria (temperature, pH, oxygen requirements, exogenous growth factors, selective/nonselective media) f) laboratory process of patient’s specimens: direct microscopy, bacterial cultures, identification procedures, antimicrobial susceptibility testing, serological assays and interpretation of the results; Practice: a) observation and description of bacterial colonies on culture media; b) smears preparation and staining (Gram staining technique;) microscopic examination of bacterial morphology c) ready-made microscope slides examination in dark-field and fluorescent microscope d) demonstration of liquid and agar media for culturing bacteria. Types of bacterial grow. 1 Class 2. Tuesday 15.10.13; Friday 18.10.13. Gram-positive cocci: staphylococci and streptococci. Learning objectives: a) culture, identification and pathogenicity of Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus saprophiticus and Micrococci; b) culture, identification and pathogenicity of Streptococcus pyogenes, Streptococcus pneumoniae, Viridans Streptococci and Enterococcus; Practice: a) observation and description of growth characteristics of gram-positive cocci on blood agar: colony morphology, hemolytic activity; b) microscopic examination of staphylococci and streptococci; c) identification tests for staphylococci (catalase activity, clumping factor (CF), sensitivity to noviobiocin and furazolidone, coagulase activity, ID 32 Staph); d) identification tests for streptococci (sensitivity to bacitracin and optochine, biochemical reactions for enterococci, tests detecting group antigens, API Strep). Class 3. Tuesday 29.10.13; Friday need to be established. Gram-negative anaerobic, fermentative, intestinal and non-fermentative rods; Learning objectives: a) culture, identification and pathogenicity of intestinal rods of Enterobacteriaceae family: Salmonella, Shigella, Yersinia, Escherichia, Proteus and Klebsiella; b) culture, identification and pathogenicity of non-fermentative rods of genera: Pseudomonas , Acinetobacter and Stenotrophomonas. c) culture, identification and pathogenicity of obligate anaerobic gram-negative rods (Prevotella, Porphyromonas, Bacteroides, Fusobacterium) Practice: a) observation and description of growth characteristics of fermentative and non-fermenative rods on selective media: Mac Conkey agar, SS agar, nutrient agar; b) microscopic examination of gram-negative rods; c) microbiological identification of gram-negative rods: ID 32 GN; oxidase activity and pigment production; d) microbiological identification of gram-negative obligate anaerobic rods: ID 32A test. Class 4. Tuesday 12.11.13; Friday 15.11.13. Gram-positive bacilli , corynebacteria, Actinomyces and Mycobacterium. Learning objectives: a) culture, identification and pathogenicity of bacilli: Bacillus anthracis, Clostridium tetani, Cl. botulinum, Cl. perfringens and Cl. difficile; b) culture, identification and pathogenicity of Corynebactrium diphtheriae; c) DTP vaccine; d) classification of mycobacteria e) culture, identification and pathogenicity of Mycobacterium tuberculosis and mycobacteria other than tuberculous (MOTT group) f) clinical presentation and significance of tuberculosis, diagnosis, BCG vaccine, tuberculin reaction g) Koch’s fenomen h) culture, identification and pathogenicity of Actinomyces and Nocardia Practice: a) demonstration of cultures: bacilli, corynebacteria, Actinomyces, Nocardia and mycobacteria; b) microscopic examination of the bacteria; 2 c) microbiological identification of Corynebacteria (API ANA, API Coryne); d) Elek assay. e) Susceptibility testing of Mycobacterium tuberculosis; Class 5. Tuesday26.11.13; Friday 29.11.13. Spiral bacteria: Treponema, Leptospira, Borrelia, Campylobacter, Helicobacter. Class test #1 Learning objectives: a) culture, identification and pathogenicity of spiral bacteria (epidemiology, vectors); Practice: a) Campylobacter and Helicobacter cultures demonstration; b) microscopic examination of a gram-stained slides from stomach biopsy of patient infected with H. pylori; c) demonstration of the slide with Treponema pallidum stained with sliver technique; d) demonstration of the wet mount slide with Leptospira spp. in a dark-filed microscopy; Class 6. Tuesday 10.12.13; Friday 13.12.13. Antisepsis. Antimicrobials – part I Learning objectives: a) control of microbial growth; antimicrobial activity of various physical and chemical agents. Techniques used in sterilization and disinfection. b) Agents used to treat bacterial infections: general mechanisms of action and antibacterial spectra of the major groups of antibiotics c) antimicrobials susceptibility testing of bacteria: - disc-diffusion technique; - serial dilution technique (MIC, MBC); - E-tests; - susceptibility testing of mycobacteria (demonstration). Practice: a) hygienic hand washing. b) performance of the disc-diffusion tests for: Staphylococcus aureus MRSA I MLSb (pus) Pseudomonas aeruginosa MBL (+) (pus ) Klebsiella pneumonia ESBL (+) (sputum) Class 7. Tuesday 14.01.14; Friday 17.01.14. Antimicrobials – part II. Learning objectives: a) mechanisms of bacterial resistance to antibiotics: MRS, MLSB, VISA, VRSA, VRE, GRE, MBL, HLAR, ESBL, KPC Practice: a) Hygienic hand washing – results reading. b) disc-diffusion tests result reading; c) ATB test reading; d) cefinase assay of Moraxella β-lactamases; e) demonstration of DDT (double disc test) for detection of ESBL-producing Klebsiella pneumoniae (positive and negative result) f) demonstration of MBL, KPC detection tests g) detection of the ESBL production with E-test. h) Nasal carriage of Staphylococcus aureus – antibiogram 3 Class schedule of microbiology for the 3rd year students of English Division Academic Year 2013/2014 summer semester Groups I, II and III: Tuesday 13.45 – 16.00 (class room) (total: 40 hours) Groups: IV, V and VI: Friday 7.30 – 9.45 (class room) Laboratory sessions of microbiology last 135 minutes and are held every two weeks in the student laboratory in the Department of Medical Microbiology ul. Chałubińskiego 4 GENERAL SCHEDULE OF CLASSES IN SUMMER SEMESTER: Summer semester: 5 weeks x 3 hours 2 weeks x 2 hours = 19h Class 8. 24.II – 28.II. 2014 Principles of diagnostic procedures in fungal infections. Class 9. Normal microbial flora of human body. Upper and lower respiratory tract infections. Class 10. Urinary tract infections (UTI) and gastrointestinal tract infections (GTI). Class 11. Wound and soft tissue infections and sexually transmitted diseases Class 12. Blood and central nervous system infections 10.III – 14.III 2014 24.III – 28.III 2014 07.IV – 11.IV 2014 2.V.2014 (gr. wtorkowa) 25.IV (gr. piątkowa) Class 13. Principles of diagnostic 12.V – 16.V 2014 procedures in viral infections. Class 14. Practical exam. 26.V – 30.V 2014 Credit of classes. Class 8. Tuesday 25.02.14; Friday 27.02.14. Principles of diagnostic procedures in fungal infections. Learning objectives: a) most common cases of local and disseminated fungal infections; b) common etiologic agents of fungal infections: Candida, Cryptococcus and Aspergillus; c) collection and transport of patient’s specimens to the laboratory. d) Agents used to treat fungal infections: general mechanisms of action and antifungal spectra of polieny, imidazole, triazole, 5-flucytozune, echinocandines. Practice: a) yeasts identification: colony morphology on Sabourand and Chromagar media; b) blastospores and arthrospores examination in a gram-staining slides; c) filaments assay; d) microscopic examination of structures characteristic of yeasts; e) yeasts identification tests: ID 32 C; f) molds identification: colony morphology of Aspergillus and Penicillium on Czapek medium; 4 g) examination of the lactophenol-stained slides prepared from molds cultures (Trichophyton, Epidermophyton, Microsporum); h) antimycogram (Fungi-test) demonstration Class 9. Tuesday 11.03.14; Friday 14.03.14. Normal microbial flora of human body. Upper and lower respiratory tract infections. Learning objectives: a) microflora of human body and endogenous infections. b) discussion of the etiologic agents of the upper and lower respiratory tract infections; c) diagnostic procedures; collection and transport of patients specimens Practice: a) examination of the pathogens cultures isolated from respiratory tract infections and discussion of the results; - patient № 1: pharyngeal swab (pharyngitis caused by Streptococcus pyogenes )- slide stained with Gram, identification tests (bacitracin disc, detection of microbial antigen); - patient № 2: sputum sample (community – acquired pneumonia caused by Streptococcus pneumonia)- slide stained with Gram, identification tests (optochin disc test), antimicrobial susceptibility testing; - patient № 3: bronchial secretions (hospital – acquired pneumonia caused by Acinetobacter baumannii ; patient of ICU) )- slide stained with Gram, identification tests (ID32GN), antimicrobial susceptibility testing; b) demonstration of the ready-made Plaut – Vincent pharyngitis slide stained with Gram and cultures of Corynebacterium diphtheriae and Staphylococcus aureus; Next class preparing: inoculation of the samples from patients with urinary tract infections and gastrointestinal tract infections: a) patient № 1 (UTI caused by Enterococcus faecalis): urine sample inoculation onto blood agar, Mac Conkey agar and Sabourand agar. b) patient № 2 (UTI caused by Escherichia coli): urine sample inoculation onto blood agar, Mac Conkey agar and Sabourand agar. a) patient № 3 (GTI; Salmonella spp. and E. coli): smear from rectum inoculation onto Mac Conkey agar, SS and selenine. Class 10. Tuesday 25.03.14; Friday 28.03.14. Urinary tract infections (UTI) and gastrointestinal tract infections (GTI): Learning objectives: a) discussion of the etiologic agents of the urinary tract infections and gastrointestinal tract infections b) diagnostic procedures; collection and transport of patients specimens Practice: a) examination of the cultures prepared during last class and discussion of the results; b) E. coli identification (ID 32GN), antimicrobial susceptibility testing; c) Enterococcus faecalis identification: gram-stained slide from the culture, differentiating biochemical test reading, antimicrobial susceptibility testing; d) Salmonella identification (ID 32GN), demonstration of slide agglutination test for Salmonella typing; Demonstrations: a) examination of a cultures of common intestinal pathogens: E. coli, Klebsiella spp., Proteus spp., Staphylococcus epidermidis, S. saprophiticus, Enterococcus spp., Candida albicans 5 b) examination of a cultures of common intestinal pathogens: Salmonella, Shigella, Escherichia coli, Yersinia enterocolitica, Campylobacter jejuni; c) positive and negative Gold test demonstration; d) demonstration of the contaminated urine sample (4 bacterial strains: lactose-positive and lactosenegative rods, Enterococcus and Staphylococcus spp.); e) examination of gram-stained slides presenting the pathogens f) Uriline and Uricult culture-transport media demonstration g) demonstration of the Rota-Adeno Kit for detection of Rotaviruses and Adenoviruses in patient’s specimens; h) Widal test demonstration and results interpretation. Next class preparing: inoculation of the samples from patients with wound and soft tissue infections: a) patient № 1 (subdiaphragm abscess with mixed flora: Bacteroides fragilis and Enterococcus spp.): pus from abscess inoculation onto blood agar, Schaedler agar and tioglycolan medium. b) patient № 2 (carbunculosis caused by Staphylococcus aureus): smear from carbunculosis inoculation onto blood agar, Mac Conkey agar, Schaedler agar and tioglycolan medium. c) patient № 3 (burned wound infected with Pseudomonas aeruginosa): smear from the wound inoculation onto blood agar, Mac Conkey agar and glucose broth. Class 11. Tuesday 08.04.14; Friday 11.04.14. Wound and soft tissue infections and sexually transmitted diseases (STD). Learning objectives: a) discussion of the etiologic agents of wound and soft tissue infections; b) discussion of the etiologic agents of sexually transmitted diseases; c) diagnostic procedures; collection and transport of patients specimens. Practice: a) examination of the cultures prepared during last class and discussion of the results; b) Bacteroides spp. (API 20A) identification tests reading; c) Escherichia coli identification tests reading (ID32GN) and smear from culture preparation; d) Staphylococcus aureus identification tests reading (ID 32 Staph; coagulase and catalase activity) and microscopic examination; e) Pseudomonas aeruginosa identyfication tests (oxidase activity, ID32 GN, susceptibility testing); f) demonstration of the cultures of the pathogens associated with soft tissue infections: E. coli, Pseudomonas aeruginosa, Staphylococcus aureus, Bacteroides fragilis; microscopic examination of the pathogens. g) Syphilis diagnosis: USR and TPHA tests for reading; FTA-ABS and ELISA assays; silver-stained slide presenting Treponema pallidum in brain tissue of the patients with tertiary syphilis; h) Gonorrhoea diagnosis: Neisseria gonorrhoeae culture on Roiron medium; oxidase test; Loffler-stained slide from gonorrhoeal pus; screening Microcult CG test; i) trichomoniasis diagnosis: Giemsa-stained slide from urethral discharge of patient with trichomoniasis; 6 j) Non-gonococcal urethritis (NGU) diagnosis: Mycoplasma hominis culture; Mycoplasma IST test reading and interpretation; Chlamydia trachomatis – picture of infected Mac Coy cell line; k) Sexually transmitted fungal infections (class 8 informations) Next class preparing: inoculation of the samples from patients with blood and central nervous system infections: a) patient № 1: patient with CNSI(Neisseria meningitidis) cerebrospinal fluid in Meningomedium transport medium after 24h incubation; aseptic inoculation onto TSA agar, Mac Conkey and Classman agar; cerebrospinal fluid in sterile tube; examination of gram-stained slides, latex agglutination test for bacterial antigen detection (demonstration) blood sample on transport medium after 24h incubation: inoculation onto TSA agar, Mac Conkey and Classman agar; b) patient № 2: (patient with endocarditis caused by Streptococcus salivarius): blood sample on transport medium after 24h incubation: inoculation onto blood agar and Mac Conkey agar; a) patient № 3: (patient with infected catheter; Staphylococcus epidermidis ): blood sample on transport medium after 24h incubation: inoculation onto blood agar and Mac Conkey agar. Class 12. Tuesday 2.05.14; Friday 25.04.14. Blood and central nervous system infections. Learning objectives: a) discussion of the etiologic agents of blood and cardiovascular infections. Etiologic agents of central nervous system infections. b) diagnostic procedures; collection and transport of patients specimens. Practice: a) examination of the cultures prepared during last class and discussion of the results; identification of Neisseria meningitidis: (microscopy, oxidase activity, API NH); identification of Streptococcus salivarius (microscopy, susceptibility to optochine, API 20 Strep, antimicrobial susceptibility testing); identification of Staphylococcus epidermidis (microscopy, ID32 Staph, antimicrobial susceptibility testing ) b) examination of the cultures of common CNSI and blood and cardiovascular infections pathogens: Neisseria meningitidis, Streptococcus agalactiae, Haemophilus influenzae, (ID tests: growth factors, API NH, ATB NH demonstration), Enterobacter cloacae, Staphylococcus epidermidis, Escherichia coli, Candida albicans; c) examination of gram-stained slides presenting the pathogens; d) demonstration of the transport media for cerebrospinal fluid collection and transport; e) demonstration of the Bactec Alert System for cerebrospinal fluid samples culture. Class 13. Tuesday 13.05.14; Friday 16.05.14. Principles of diagnostic procedures in viral infections. Learning objectives: a) diagnostic procedures; collection and transport of patients specimens. b) laboratory identification and culture of human virus pathogens c) serological diagnosis of viral infections demonstrations: a) virus infected cell line (cytopathic effects) b) bacteriophage culture 7 c) Hirst test -hemagglutination assay for quantifying viruses and Hirst-Salk hemagglutination d) ELISA test Class 14. Tuesday 27.05.14; Friday 30.05.14 . Practical exam. Credit of classes. Person in charge Dr hab. Beata Sobieszczańska, prof. nadzw. 8