Todo lo que hay que saber del Imiquimod - PIEL
advertisement
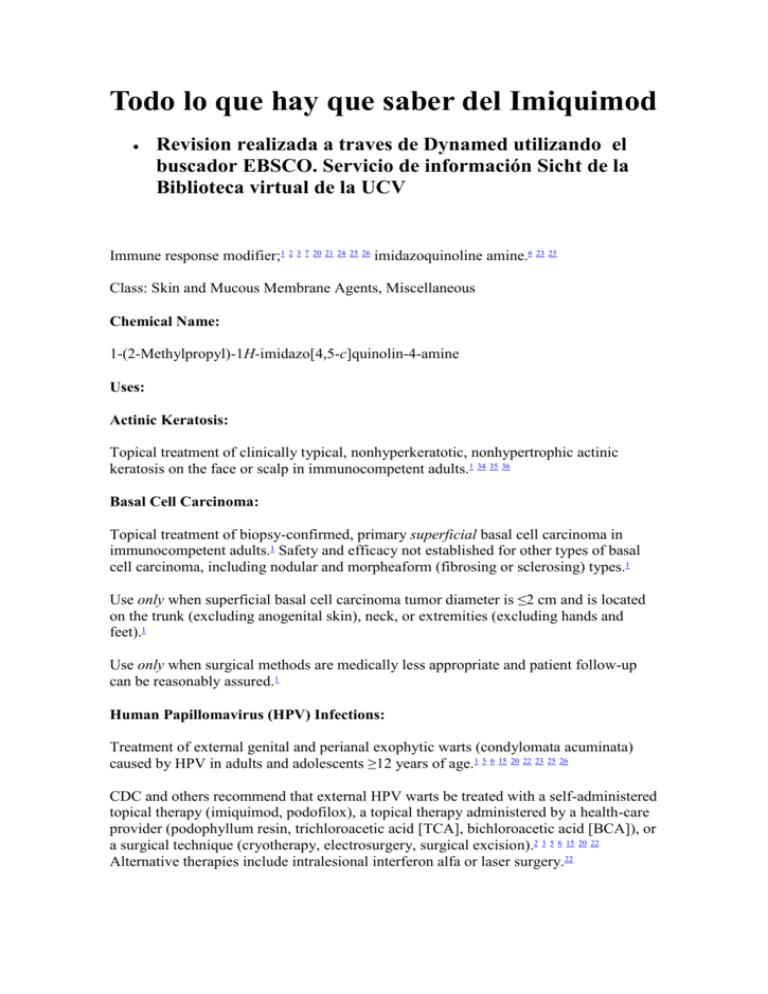
Todo lo que hay que saber del Imiquimod Revision realizada a traves de Dynamed utilizando el buscador EBSCO. Servicio de información Sicht de la Biblioteca virtual de la UCV Immune response modifier;1 2 3 7 20 21 24 25 26 imidazoquinoline amine.6 23 25 Class: Skin and Mucous Membrane Agents, Miscellaneous Chemical Name: 1-(2-Methylpropyl)-1H-imidazo[4,5-c]quinolin-4-amine Uses: Actinic Keratosis: Topical treatment of clinically typical, nonhyperkeratotic, nonhypertrophic actinic keratosis on the face or scalp in immunocompetent adults.1 34 35 36 Basal Cell Carcinoma: Topical treatment of biopsy-confirmed, primary superficial basal cell carcinoma in immunocompetent adults.1 Safety and efficacy not established for other types of basal cell carcinoma, including nodular and morpheaform (fibrosing or sclerosing) types.1 Use only when superficial basal cell carcinoma tumor diameter is ≤2 cm and is located on the trunk (excluding anogenital skin), neck, or extremities (excluding hands and feet).1 Use only when surgical methods are medically less appropriate and patient follow-up can be reasonably assured.1 Human Papillomavirus (HPV) Infections: Treatment of external genital and perianal exophytic warts (condylomata acuminata) caused by HPV in adults and adolescents ≥12 years of age.1 5 6 15 20 22 23 25 26 CDC and others recommend that external HPV warts be treated with a self-administered topical therapy (imiquimod, podofilox), a topical therapy administered by a health-care provider (podophyllum resin, trichloroacetic acid [TCA], bichloroacetic acid [BCA]), or a surgical technique (cryotherapy, electrosurgery, surgical excision).2 3 5 6 15 20 22 Alternative therapies include intralesional interferon alfa or laser surgery.22 A preferred treatment regimen for external genital HPV warts in HIV-infected† adults and adolescents;39 data are limited regarding the response rate in HIV-infected patients compared with those without HIV infection.39 An alternative treatment regimen for external HPV warts in HIV-infected children† ; topical therapies often are ineffective in such children and a surgical technique (cryotherapy, electrosurgery) usually is preferred.40 Primary goal is destruction or clearance of visible, symptomatic warts.2 4 5 22 27 No regimen has been shown to eradicate HPV or affect natural history of HPV infection;2 3 4 22 27 effect on transmission of HPV unknown.1 22 Should not be used to treat subclinical genital HPV infection (without exophytic warts).22 Safety and efficacy for treatment of urethral, intravaginal, cervical, rectal, or anal HPV warts not established.1 22 Some clinicians suggest use of topical imiquimod for treatment of distal meatal HPV warts† , but data are limited.22 Molluscum Contagiosum: Has been effective in a limited number of children, adolescents, and adults for the treatment of molluscum contagiosum† ,31 32 33 but safety and efficacy not established.1 Clinical studies in children 2–12 years of age with molluscum contagiosum indicate imiquimod is no more effective than placebo.1 Administration: Topical Administration: Apply topically to skin as a 5% cream.1 2 22 23 24 25 26 For external use only.1 Avoid contact with eyes, lips, and nostrils and do not administer orally, intravaginally, or intra-anally.1 12 Suitable for self-administration.1 Prior to initial use, patients should be instructed regarding proper techniques for application and removal of the drug.1 Wash hands before and after applying the cream.1 Prior to application, wash affected area with mild soap and water and allow to dry thoroughly (≥10 minutes).1 Apply the cream to entire treatment area and rub in until no longer visible.1 Apply the cream to affected area immediately prior to normal sleeping hours (bedtime) and rub in until no longer visible.1 Allow cream to remain on the skin for approximately 8 hours (6–10 hours) and remove the following morning by washing with mild soap and water.1 Delay use until skin has healed from any previous sunburn or any previous drug or surgical treatment.1 Do not use occlusive dressings or wrappings.1 Imiquimod cream is supplied in single-use packets (250 mg of cream; 12.5 mg imiquimod).1 Avoid use of excessive amounts.1 When treating actinic keratosis, no more than 1 packet of the cream should be applied to the contiguous treatment area.1 When treating external genital or perianal HPV warts, 1 packet of cream should be sufficient to cover a wart area ≤20 cm2.1 Partially used packets should be discarded and should not be reused.1 Dosage: Pediatric Patients: HPV Infections: External Genital and Perianal HPV Warts: Topical: Children ≥12 years of age: Apply thin layer of 5% cream to HPV wart area at bedtime 3 times weekly (e.g., Monday, Wednesday, Friday or Tuesday, Thursday, Saturday) until warts have cleared completely or for a maximum of 16 weeks.1 22 Remove drug in the morning (6–10 hours after application) by washing with soap and water.1 22 HIV-infected children† : Apply thin layer of 5% cream to wart area at bedtime 3 times weekly (nonconsecutive days) for ≤16 weeks.40 Remove drug in the morning by washing with soap and water.40 Follow-up examinations not generally required for patients self-administering imiquimod, but may be useful several weeks after initiation of therapy to determine response to treatment, to monitor and treat complications of therapy, and to provide additional patient education and counseling.22 A follow-up examination 3 months after completion of treatment may be beneficial since identification of external genital warts may be difficult.22 Adults: Actinic Keratosis: Topical: Apply thin layer of 5% cream to affected area of face or scalp at bedtime twice weekly (e.g., Monday and Thursday or Tuesday and Friday) for 16 weeks.1 Treatment area should be a single contiguous area approximately 25 cm2 (e.g., 5 cm long and 5 cm wide) occurring on the face (e.g., forehead or one cheek) or on the scalp; both areas should not be treated concurrently.1 Remove drug in the morning (6–10 hours after application) by washing with soap and water.1 Assess response to treatment after local skin reactions and/or application site reactions have resolved.1 Lesions that do not respond to treatment should be carefully reevaluated and management reconsidered.1 Safety and efficacy of repeat courses of imiquimod not established.1 Basal Cell Carcinoma: Biopsy-confirmed Superficial Basal Cell Carcinoma: Topical: Apply thin layer of 5% cream to affected area at bedtime 5 times weekly (e.g., Monday through Friday) for 6 weeks.1 Treatment area should include the target tumor and a 1cm margin of skin around the tumor.1 (See Table.) Remove drug in the morning (6–10 hours after application) by washing with soap and water.1 Assess response to treatment after local skin reactions and/or application site reactions have resolved and skin has regenerated (approximately 12 weeks after treatment ends).1 If there is clinical evidence of persistent tumor after treatment, a biopsy or other alternative intervention should be considered.1 Lesions that do not respond to treatment should be carefully reevaluated and management reconsidered.1 Safety and efficacy of repeat courses of imiquimod not established.1 Dosage for Treatment of Superficial Basal Cell Carcinoma Target Tumor Diameter (cm) Cream Droplet Diameter (mm) Approximate Dosage in Cream Droplet 0.5 to <1.0 4 10 mg 5 times weekly for 6 weeks ≥1.0 to <1.5 5 25 mg 5 times weekly for 6 weeks ≥1.5 to 2.0 7 40 mg 5 times weekly for 6 weeks HPV Infections: External Genital and Perianal HPV Warts: Topical: Apply thin layer of 5% cream to HPV wart area at bedtime 3 times weekly (e.g., Monday, Wednesday, Friday or Tuesday, Thursday, Saturday) until warts have cleared completely or for a maximum of 16 weeks.1 22 23 39 Remove drug in the morning (6–10 hours after application) by washing with soap and water.1 22 39 HIV-infected adults† : Apply thin layer of 5% cream to wart area at bedtime 3 times weekly (nonconsecutive days) for ≤16 weeks.39 Remove drug in the morning by washing with soap and water.40 Follow-up examinations not generally required for patients self-administering imiquimod, but may be useful several weeks after initiation of therapy to determine response to treatment, to monitor and treat complications of therapy, and to provide additional patient education and counseling.22 A follow-up examination 3 months after completion of treatment may be beneficial since identification of external genital warts may be difficult.22 Prescribing Limits: Pediatric Patients: HPV Infections: External Genital and Perianal HPV Warts: Topical: Children ≥12 years of age: Maximum of 16 weeks of treatment (3 times weekly).1 22 29 40 Adults: Actinic Keratosis: Topical: Maximum of 16 weeks of treatment (2 times weekly).1 Maximum treatment area is 25 cm2.1 Safety and efficacy of repeated use (i.e., multiple courses of treatment) in the same area of actinic keratosis not established.1 Superficial Basal Cell Carcinoma: Topical: Maximum of 6 weeks of treatment (5 times weekly).1 Safety and efficacy of repeat courses of imiquimod not established.1 HPV Infections: External Genital and Perianal HPV Warts: Topical: Maximum of 16 weeks of treatment (3 times weekly).1 22 29 39 Special Populations: No special population dosage recommendations.1 Contraindications: Manufacturer states there are no known contraindications to use of imiquimod.1 Warnings/Precautions: Warnings: Precautions Related to Treatment of Actinic Keratosis: Safety and efficacy for treatment of actinic keratosis in skin areas >25 cm2 not established.1 Degree of systemic exposure may depend on surface area of application rather than amount of applied dose.1 Safety and efficacy of repeat treatment of actinic keratosis (multiple treatment courses applied to the same 25-cm2 skin area) not established.1 Subclinical actinic keratosis lesions may become apparent in the treatment area and may subsequently resolve.1 Precautions Related to Treatment of Superficial Basal Cell Carcinoma: Confirm diagnosis of superficial basal cell carcinoma prior to initiating topical imiquimod therapy.1 Safety and efficacy for other types of basal cell carcinoma, including nodular and morpheaform (fibrosing or sclerosing) types not established.1 Safety and efficacy for treatment of basal cell carcinoma lesions on the face, head, or anogenital area not established.1 Safety and efficacy for treatment of basal cell nevus syndrome or xeroderma pigmentosum not established.1 Patients treated for superficial basal cell carcinoma should receive regular follow-up of the treatment site.1 A medical evaluation is indicated if any suspicious lesion arises in the treatment area at any time after initial clearance of superficial basal cell carcinoma.1 Precautions Related to Treatment of External Genital and Perianal HPV Warts: Safety and efficacy for treatment of urethral, intravaginal, cervical, rectal, or anal HPV warts not established.1 22 Follow-up visits are not required for patients self-administering imiquimod, but may be useful several weeks after initiation of therapy to determine response to treatment, to monitor and treat complications of therapy, and to provide additional patient education and counseling.22 Follow-up examinations not mandatory if visible genital and perianal warts have cleared after treatment, but may be beneficial 3 months after treatment is completed since identification of external genital warts may be difficult.22 Examination of sexual partners is not necessary for the management of genital HPV warts because data do not indicate that reinfection plays a role in recurrences and, in the absence of curative therapy, treatment to reduce transmission is not realistic.22 However, sexual partners of patients with genital HPV warts may benefit from examination to assess the presence of HPV warts or other sexually transmitted diseases and also may benefit from counseling about the implications of having a partner who has HPV warts.22 HIV-infected individuals† may not respond as well and may have more frequent recurrences of genital HPV warts after treatment compared with immunocompetent individuals.22 39 40 (See Immunocompromised Individuals under Cautions.) Women with genital HPV warts should be advised to undergo regular Papanicolaou (Pap) tests as recommended for women without genital HPV warts.22 Sensitivity Reactions: Local Inflammatory Reactions: Intense local inflammatory reactions (e.g., skin weeping, erosion) can occur after a few applications of imiquimod cream.1 2 9 10 23 24 25 26 These local inflammatory reactions may be accompanied or preceded by a flu-like syndrome with systemic manifestations (e.g., malaise, fever, nausea, myalgias, rigors).1 Consider temporary discontinuance of the drug if local reactions and/or systemic manifestations are severe; treatment interruptions lasting several days may be taken if required.1 (See Local and Dermatologic Effects under Cautions.) Photosensitivity: Possible increased susceptibility to sunburn.1 Avoid or minimize exposure to sunlight (including sunlamps) and use protective clothing (e.g., hat) during imiquimod treatment.1 Do not use in patients with sunburn until full recovery from sunburn has occurred.1 Use with caution in patients with considerable sunlight exposure (e.g., occupational) and in those sensitive to sunlight.1 General Precautions: Local and Dermatologic Effects: Local skin reactions (e.g., edema, erosion/ulceration, erythema, flaking/scaling/dryness, scabbing/crusting, vesicles, weeping/exudate) commonly occur following topical application of imiquimod.1 (See Local Inflammatory Reactions under Cautions.) Application site reactions (burning, pruritus) also may occur.1 Local skin reactions may extend beyond the application site onto the surrounding skin.1 Although usually mild to moderate, these reactions may be severe enough to require temporary discontinuance of the drug.1 If signs or symptom at the application site restrict or prohibit daily activity or make continued application of the cream difficult, the drug may be discontinued for several days.1 Local reactions generally decrease in intensity or resolve when the drug is discontinued; treatment can be resumed after the skin reaction subsides.1 Because of local reactions, the treatment area is likely to appear noticeably different from normal skin until such reactions have healed.1 Localized hypopigmentation or hyperpigmentation has been reported; these skin color changes may be permanent in some patients.1 If doses are missed or treatment is temporarily discontinued because of local reactions and/or systemic manifestations, the total duration of treatment should not be extended beyond the maximum recommended duration (i.e., 16 weeks for treatment of actinic keratosis, 6 weeks for treatment of superficial basal cell carcinoma, 16 weeks for treatment of genital and perianal HPV warts).1 Preexisting inflammatory skin conditions, including chronic graft versus host disease, may be exacerbated.1 Immunocompromised Individuals: Safety and efficacy in immunocompromised patients not established.1 30 If used for treatment of genital HPV warts in HIV-infected individuals† , consider that these patients may not respond as well and may have more frequent recurrences after treatment compared with immunocompetent individuals.22 39 40 Patients with Autoimmune Disorders: Use with caution in patients with preexisting autoimmune disorders.1 Specific Populations: Pregnancy: Category C.1 Lactation: Not known whether topical imiquimod is distributed into milk.1 Use caution.1 Pediatric Use: Safety and efficacy for treatment of actinic keratosis not established in children <18 years of age.1 This skin condition generally does not occur in children.1 Safety and efficacy for treatment of superficial basal cell carcinoma not established in children <18 years of age.1 This skin condition generally does not occur in children.1 Safety and efficacy for treatment of external genital and perianal HPV warts not established in children <12 years of age.1 Geriatric Use: Safety and efficacy in patients ≥65 years of age with actinic keratosis and superficial basal cell carcinoma appears to be similar to that in younger adults,1 but increased sensitivity in geriatric patients cannot be ruled out.1 Common Adverse Effects: Treatment of actinic keratosis: Local skin reactions (edema, erosion/ulceration, erythema, flaking/scaling/dryness, scabbing/crusting, weeping/exudate, vesicles), application site reactions (e.g., bleeding, burning, induration, irritation, pain, pruritus, stinging, tenderness), eczema, diarrhea, headache, squamous carcinoma, sinusitis, upper respiratory tract infection.1 Treatment of superficial basal cell carcinoma: Local skin reactions (edema, erosion, erythema, flaking/scaling, induration, scabbing/crusting, ulceration, vesicles), application site reactions (bleeding, burning, erythema, edema, induration, erosion, flaking/scaling, scabbing/crusting, pain, papule, pruritus), back pain, coughing, dyspepsia, fatigue, fever, headache, lymphadenopathy, rhinitis, sinusitis, upper respiratory tract infection.1 Treatment of external genital and perianal HPV warts: Local skin reactions (e.g., erythema, erosion, excoriation/flaking, edema, induration, scabbing, ulceration, vesicles), application site reactions (burning, fungal infections, pain, pruritus, soreness), headache, influenza-like symptoms.1 Actions: Mechanism of action in topical treatment of actinic keratosis or superficial basal cell carcinoma unknown.1 Topical application to superficial basal cell carcinoma may increase infiltration of lymphocytes, dendritic cells, and macrophages into the tumor lesion; clinical importance unknown.1 The exact mechanism(s) of action of imiquimod in the topical treatment of exophytic HPV warts has not been elucidated, but may be related to the immunomodulating effects of the drug.1 23 25 26 Imiquimod induces production of a variety of cytokines6 20 23 and apparently can enhance cell-mediated cytolytic antiviral activity.2 7 In vitro in cell culture, imiquimod has no direct antiviral activity against HPV.1 6 7 26 Imiquimod is a rapid6 and potent inducer of IFN-α,2 6 7 20 21 23 interleukin-1 alpha and beta (IL-1α and IL-1β),2 6 interleukin-6 (IL-6),2 6 interleukin-8 (IL-8),2 tumor necrosis factor alfa (TNF-α),2 6 23 granulocyte-macrophage colony-stimulating factor (GM-CSF),6 granulocyte colony-stimulating factor (G-CSF),6 and macrophage inflammatory protein-1α.6 Pharmacokinetics: Absorption: Bioavailability: Absorbed systemically following topical application to skin.1 Systemic exposure appears to be related to surface area of application site rather than total applied dose.1 Distribution: Not known whether crosses placenta following topical application.1 Not known whether distributed into milk following topical application.1 Elimination: Elimination Route: Following topical application to the skin in adults with actinic keratosis (75-mg doses 3 times weekly for 16 weeks), 0.08–0.15% of topical dose is eliminated in urine as unchanged drug and metabolites.1 Following topical application in patients with HPV warts, 0.11 or 2.41% of topical dose is eliminated in urine as unchanged drug and metabolites in men or women, respectively.1 Half-life: Apparent half-life following topical application is approximately 10 times greater than that reported following sub-Q administration (2 hours); this indicates prolonged retention in skin.1 Comparative Pricing: Advice to Patients: Importance of reading manufacturer’s patient information.1 Importance of not using the drug for any disorder other than that for which it was prescribed.1 12 Importance of applying to affected areas as directed and not administering orally, intravaginally, or intra-anally.1 12 Importance of avoiding contact with eyes, lips, and nostrils.1 Advise patients to immediately rinse with water if the cream gets into the mouth or eyes.1 Advise patients to apply the cream at bedtime, leave the cream on the skin for the prescribed period of time, and not bathe or get treatment area wet until the following morning (6–10 hours after application).12 Importance of not using occlusive dressings.1 Advise patients that cotton gauze dressing can be used, if needed; cotton underwear can be worn if the genital and perianal area is being treated.12 Advise patients that if a dose is missed, the dose should be applied as soon as it is remembered and the regular treatment schedule continued.1 Advise patients that they may experience local skin reactions during treatment (e.g., edema, erosion/ulceration, erythema, flaking/scaling/dryness, scabbing/crusting, vesicles, weeping/exudate) or application site reactions (e.g., burning, pruritus) that are mild to severe in intensity and may extend beyond the application site onto surrounding skin.1 Advise patients to contact their clinician if they experience any sign or symptom at the application site that restricts or prohibits their daily activity or makes continued application of the cream difficult.1 Advise patients that local skin reactions may be severe enough to require temporary discontinuance of the drug.1 Treatment can be resumed as directed by the clinician after the skin reaction has subsided.1 If doses are missed or treatment is temporarily discontinued because of local skin reactions, the total duration of treatment should not be extended beyond the maximum recommended duration (i.e., 16 weeks for treatment of actinic keratosis, 6 weeks for treatment of superficial basal cell carcinoma, 16 weeks for treatment of genital and perianal HPV warts).1 Importance of using sunscreen and avoiding or minimizing exposure to natural or artificial sunlight (e.g., tanning bed) during imiquimod treatment.1 Advise patients that localized hypopigmentation or hyperpigmentation has been reported and that these skin color changes may be permanent in some patients.1 Advise patients being treated for superficial basal cell carcinoma to contact their clinician if any suspicious lesion arises in the treatment area at any time after initial clinical clearance of superficial basal cell carcinoma.1 Advise patients being treated for genital HPV warts that imiquimod is not a cure for HPV infection and that the drug's effect on transmission of HPV is unknown.1 22 New HPV warts may develop during or after treatment.1 22 Importance of patient watching for recurrences of HPV warts, particularly during the first 3 months.22 Advise patients being treated for genital HPV warts that uncircumcised males should clean under the foreskin before treatment and once daily during treatment and that females should avoid intravaginal application and take special care when applying near vaginal opening since local reactions at this site may result in pain or swelling and difficult urination.12 Advise patients being treated for genital HPV warts to avoid sexual (genital, anal, oral) contact while imiquimod cream is on the skin and that the cream may weaken condoms and vaginal diaphragms.1 12 Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1 12 Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 12 Importance of informing patients of other important precautionary information.1 (See Cautions.) General references used: Unless otherwise stated, source material derived from AHFS Drug Information Essentials®. See Acknowledgements Section for full AHFS copyright statement. Used with permission. References for AHFS DI Essentials: 1. Graceway Pharmaceuticals. Aldara® (imiquimod) 5% cream prescribing information. Bristol, TN; 2007 Apr. 2. Beutner KR, Ferenczy A. Therapeutic approaches to genital warts. Am J Med. 1997; 102:28-37. [PubMed 9217660] 3. Apgar BS. Changes in strategies for human papillomavirus genital disease. Am Fam Physician. 1997; 55:1545-7. [PubMed 9105185] 4. Phelps WC, Alexander KA. Antiviral therapy for human papillomaviruses: rationale and prospects. Ann Intern Med. 1995; 123:368-382. [PubMed 7625626] 5. Drake LA, Ceilley RI, Cornelison RL et al. Guidelines of care for warts: human papillomavirus. J Am Acad Dermatol. 1995; 32:98-103. [PubMed 7822522] 6. Testerman TL, Gerster JF, Imbertson LM et al. Cytokine induction by the immunomodulators imiquimod and S-27609. J Leukoc Biol. 1995; 58:365-72. [PubMed 7665993] 7. Bernstein DI, Miller RL, Harrison CJ. Effects of therapy with an immunomodulator (imiquimod, R-837) alone and with acyclovir on genital HSV-2 infection in guinea-pigs when begun after lesion development. Antiviral Res. 1993; 20:45-55. [PubMed 8457147] 8. Oriel JD. Genital papilloma virus infections and their sequelae: natural history. Paper presented at 17th World Congress of Dermatology international symposium. Berlin, Germany: 1987 May. 9. Syrjanen KJ. Genital papilloma virus infections and their sequelae. Virology and pathogenesis. Paper presented at 17th World Congress of Dermatology international symposium. Berlin, Germany: 1987 May. 10. Welander CE, Homesley HD, Smiles KA et al. Intralesional interferon alfa2b for the treatment of genital warts. Am J Obstet Gynecol. 1990; 162:348-354. [PubMed 2155531] 11. Beutner KR. Bridging the gap. Arch Dermatol. 1990; 126:1432-34. [PubMed 2173496] 12. Graceway Pharmaceuticals. Aldara® (imiquimod) 5% cream patient information. Bristol, TN; 2007 Apr 13. Reference not available 14. Ferenczy A, Mitao M, Nagai N et al. Latent papillomavirus and recurring genital warts. N Engl J Med. 1985; 313:784-8. [PubMed 2993887] 15. Tyring SK, Cauda R, Baron S et al. Condyloma acuminatum: epidemiological, clinical and therapeutic aspects. Eur J Epidemiol. 1987; 3:20915. [PubMed 3308509] 16. Silva PD, Micha JP, Silva DG. Management of condyloma acuminatum. J Am Acad Dermatol. 1985; 13:457-63. [PubMed 2414346] 17. Syrjanen KJ. Epidemiology of human papillomavirus (HPV) infections and their associations with genital squamous cell cancer. APMIS. 1989; 97:957-70. [PubMed 2556164] 18. Raab-Traub N. The human DNA tumor viruses: human papilloma virus and Epstein-Barr virus. Cancer Treatment Res. 1989; 47:285-302. 19. Verdon ME. Issues in the management of human papillomavirus genital disease. Am Fam Physician. 1997; 55:1813-6. [PubMed 9105207] 20. Baker GE, Tyring SK. Therapeutic approaches to papillomavirus infections. Dermatol Clin. 1997; 15:331-40. [PubMed 9098642] 21. Bernstein DI, Harrison CJ. Effects of the immunomodulating agent R837 on acute and latent herpes simplex virus type 2 infections. Antimicrob Agents Chemother. 1989; 33:1511-15. [PubMed 2479335][Free Fulltext PMC] 22. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. MMWR Recomm Rep. 2006; 55(RR-11):1-94. [Fulltext MMWR] 23. Anon. Imiquimod for genital warts. Med Lett Drugs Ther. 1997; 39:118-9. [PubMed 9422045] 24. Beutner KR, Tyring SK, Trofatter KF et al. Imiquimod, a patient-applied immune-response modifier for treatment of external genital warts. Antimicrob Agents Chemother. 1998; 42:789-94. [PubMed 9559784][Free Fulltext PMC] 25. Edwards L, Ferenczy A, Eron L et al. Self-administered topical 5% imiquimod cream for external anogenital warts. Arch Dermatol. 1998; 134:2530. [PubMed 9449906] 26. Beutner KR, Spruance SL, Hougham AJ et al. Treatment of genital warts with an immune-response modifier (imiquimod). J Am Acad Dermatol. 1998; 38:230-9. [PubMed 9486679] 27. Stone KM. Human papillomavirus infection and genital warts: update on epidemiology and treatment. Clin Infect Dis. 1995; 20(Suppl 1):S91-7. [PubMed 7540876] 28. Reviewers’ comments (personal observations). 29. 3M Pharmaceuticals. St. Paul, MN: Personal communication. 30. 3M Pharmaceuticals. Final report of study 111-2-IMIQ-XX: double-blind, vehicle-controlled study evaluating the safety and of 5% topical imiquimod cream for the treatment of external genital and perianal warts in HIV-positive patients. 1 Feb. 31. Skinner RB. Treatment of molluscum contagiosum with imiquimod 5% cream. J Am Acad Dermatol. 2002; 47(Suppl 4):S221-4. [PubMed 12271282] 32. Barba AR, Kapoor S, Berman B. An open label safety study of topical imiquimod 5% cream in the treatment of Molluscum contagiosum in children. Dermatol Online J. 2001; 7:20. [PubMed 11328641] 33. Strauss RM, Doyle El, Mohsen AH et al. Successful treatment of molluscum contagiosum with topical imiquimod in a severely immunocompromised HIVpositive patient. In J STD AIDS. 2001; 12:264-6. 34. Stockfleth E, Meyer T, Benninghoff B et al. A randomized, double-blind, vehicle-controlled study to assess 5% imiquimod cream for the treatment of multiple actinic keratoses. Arch Dermatol. 2002; 138:1498-502. [PubMed 12437457] 35. Persaud AN, Shauelova E, Sherer D et al. Clinical effect of imiquimod 5% cream in the treatment of actinic keratosis. J Am Acad Dermatol. 2002; 47:5536. [PubMed 12271300] 36. Salasche SJ, Levine N, Morrison L. Cycle therapy of actinic keratoses of the face and scalp with 5% topical imiquimod cream: an open-label trial. J Am Acad Dermatol. 2002; 47:571-7. [PubMed 12271303] 37. Neff JM. Parapoxviruses, molluscum contagiosum, and tanapox viruses. In: Mandell GL, Bennett JE, and Dolin R, eds. Principles and practices of infections diseases. 5th ed. New York: Churchill Livingston; 2000:1556-7. 38. Lewis EJ, Lam M, Crutchfield CE. An update on molluscum contagiosum. Cutis. 1997; 60:29-34. [PubMed 9252731] 39. Centers for Disease Control and Prevention. Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. MMWR Recomm Rep. 2004; 53(RR-15):1-112. 40. Centers for Disease Control and Prevention. Treating opportunistic infections among HIV-exposed and infected children: recommendations from CDC, the National Institutes of Health, and the Infectious Diseases Society of America. MMWR Recomm Rep. 2004; 53(RR-14):1-92. †. Use is not currently included in the labeling approved by the US Food and Drug Administration.