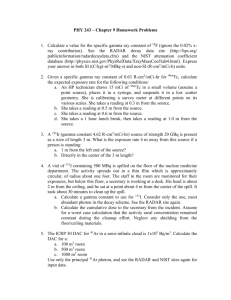
Pay particular attention to: Radionuclide decay (L4) Scintillation
advertisement

Pay particular attention to:
Radionuclide decay (L4)
Scintillation detection (L1)
Gamma camera (L1)
Radiation interactions relevant to medical imaging (L5) (L7) (L8)
Counting statistics (Bushberg)
Production of x-rays (L5)
CT scanner (L7)
Mammography (L6)
Operation of ultrasound transducers (L9)
Doppler flow (L10)
Basic principles of NMR and MRI (L12)
Spin-echo pulse sequences (L12)
Key: * on exam; # question; $ equation; (H) handwritten notes; (B) Bushberg; (V)
Valk; (I) Internet, (T) thought
Exam hints:
Read about the F-factor (L5 cont.3) [for prac?]
Work through examples in handout notes in chapter 5 (L6 cont, L6 cont.2)
Understand what filter does for backprojection (L7 cont.2)
Know the F-factor (L7 cont.3) [for prac?]
Know how to calculate dose (L7 cont.3) [for prac?]
L8:
Can be examined on any of chapters 24 & 25 of Bushberg.
Last year’s exam: two questions were short answer, worth 20 & 25 marks.
This year, not that way: 5-10 quantitative MCQ’s. Some short answer
questions not worth as much.
Study:
o Mammography
o CT
o Be in sections like this: question on image quality, spatial resolution,
contrast, how to compare, “What is CT, talk about generations”—don’t
talk about use. Won’t ask history.
o Will ask: why do CT instead of x-ray?
o Focus on clinician.
o Q’s at the end of this to give idea, so know typically what like to see.
o Won’t ask to regurgitate algorithm, but will give equation and ask e.g.
how does magnification effect image quality? 1/r^2 affect dose?
The questions are what should have been gotten out of these lectures (L8 cont.3)
Exam question: if 5MHz probe, four periods, what’s the minimum resolution to
resolve? (L9 cont.2)
L11:
Don’t plan on making things too difficult
Won’t have to revise everything.
L11 cont.5:
This year’s exam not going to be that different from last year’s
Ask basic definitions. Won’t ask things haven’t talked about.
Don’t worry about phase encoding.
Lecture 1: Scintillation detection and gamma cameras (Meikle)
Topics: scintillation detector*, scintillators, PMTs, processing, pulse height analysis,
gamma camera*, image quality.
Reference: Cherry, Sorensen and Phelps, Ch. 13
Scintillators
#{Does NaI(Tl) become more or less efficient with increasing gamma
energy? Exam Q!}
The scintillation detector is the basis of the gamma camera; it consists of
scintillation crystal, light guide, and photodetector which converts the light
into an electrical signal (PMT).
Scintillator converts ionising radiation into visible light.
o When ioninsing radiation is incident, it raises an electron’s energy state
in the scintillation crystal. This emits light rays as the electron falls
back down to the lower energy state.
Scintillation crystal is usually activated by impurities, such as NaI(Tl).
This means that the incoming radiation puts the electron in the forbidden
band; when this goes back to ground, it emits light of the desired
frequency.
o (H) Else, the light would be too UV and would take too long to happen.
o (H) Insulators have a large gap between valence and conduction band;
conductors have overlap. Crystals are semiconductors.
7 desirable properties:
o Transparent to its own emissions
o Short decay time; less important for pulsed operation.
o Durable and unaffected by moisture (non-hygroscopic) and low-cost
o Linear response over wide intensity range
o High conversion efficiency
This is associated with another plus, good energy resolution
(consistency in photon output)
Energy resolution is given by $ R=FWHM/h, where R is the
resolution and h is the peak height. Larger R values are bad.
o Index of refraction should be close to glass so it can be coupled to
PMT’s
o High attenuation for stopping x-rays and gamma rays.
Thicker crystals have greater stopping power but produce more
scatter.
Organic scintillators aren’t used in medical imaging because
they have too low attenuation
Specific scintillators:
o NaI(Tl) is slow and low density, but is cheap and has good light output.
It is used in most nuclear medicine applications, but it’s not as good for
PET. It’s fragile and hygroscopic, but has excellent energy conversion
(and thus high energy resolution) and is fairly cheap.
From a conversion ratio of 13% and from a single emitted
photon having about 3 eV (for a wavelength of 380 nm), you
get about 1 for every 20 eV of incident radiation (B).
o BGO is denser (Z=83) and tougher, but much less light. It’s fairly
slow, but fast enough for coincidence detection in PET scanners, which
is what it is mainly used for.
o LSO and GSO are new crystals with highly desirable properties for
PET. They have high attenuation and are fast, decreasing dead-time
and reducing random coincidences. They also have higher conversion
efficiencies.
o Calcium tungstate, CaWO4, is used to intensify film-screen images.
This and other film-screen scintillators aren’t fast, because they don’t
need to be.
o Cadmium tungstate, CdWO4, is used in many CT scanners because it
has high density, low afterglow, and reasonable conversion efficiency.
Photomultiplier tubes
A photon from the scintillation crystal passes through the glass and hits the
photocathode. Maximum efficiency is about 20%, meaning one electron is
released every 5 photons.
o (H) The material and thickness of the photocathode is very important.
If the photocathode is too thin, it won’t stop the incident electron and
hence will have low efficiency. If it’s too thick, the excited electrons
may be trapped and can’t come out to continue the chain.
This single electron is the accelerated by a potential difference to the first
dynode. When it interacts with the diode, it releases 2-5 further electrons.
From a further potential drop, these are accelerated to the next one,
multiplying as they go. All the electrons are then incident upon an anode,
which measures the current.
o For UV, conversion is limited by glass/silica. For IR, efficiency is
limited by the photocathode.
o After striking the dynode, up to 100 electrons are excited, but only a
handful have enough energy to be freed and continue on in the chain.
o Gain is on the order of 107. So for an input of V, output of volts.
o Amount of amplification is dependent on the voltage across the PMT.
Instead of PMTs, one can use photodiodes, where incident photons are
converted into an electrical current. These have no amplification.
Signal processing
Parts: preamplifier, amplifier, counter/analyser
o Preamplifier mostly just boosts the signal using an RC circuit.
o Amplifier amplifies. To the pulse it applies a differentiation filter
(eliminates low-frequency noise and shortens the pulse) and an
integration filter (eliminates high-frequency noise and makes peak
easier to read). The signal is now smoothed and amplified using RC
circuits.
The amount of filtering determines pulse height and width, but
Pout is always proportional to Pin. In other words, the circuit is
linear. So, H E, where H is the pulse height and E is the
gamma energy.
Pulse height analysis
(H) Used to discriminate between scattered and unscattered photons.
The operator defines upper and lower limits on the voltage. These only accept
pulses corresponding to within a certain energy.
Modes:
o Normal mode, only accepts pulses within a certain window, with the
upper and lower limits defined. This is also called single-channel
analysis. In window mode, the size of the window is determined by
one variable, and its position is determined by the other.
To make a spectrum using single channel analysis, choose a
small, fixed window. Start off with the position at zero energy.
Make a count, reset, increase the position of the energy, and
make another count, until the entire energy spectrum has been
histogrammed. This requires a lot of acquisition time!
o Integral mode, accepts everything above a set value.
o Multi-channel analysis uses an analogue-digital converter to determine
the height of the incoming peak; this is then routed to the channel
corresponding to the peak height, and that channel’s count increases by
one.
o Timing mode, produces start & stop pulses when the energy reaches,
then falls below, a certain value. This is dependent on peak energy,
but if split signal into two, delay one, attenuate the other, invert and
mix, find that the resulting signal zero point is independent of pulse
height. This has jitter unless constant fraction discrimination is used.
Counting Statistics
Three types of error: systematic (called bias, caused by things like poor
calibration), random (stochastic fluctuations), and blunder (writing down the
wrong number).
Radioactive decay, scintillation emission, and scatter all involve stochastic
processes. Hence counting statistics allows judgements on the validity of
these data.
Accuracy: close to the correct value. Precise: repeatable.
Can approximate the fractional error as 1/x1/2, where x is, for example, the
number of counts.
Rules for combining standard errors: multiplication and division is
straightforward; adding or subtracting is with the Pythagorean theorem;
raising to a power is the power times the fractional uncertainty.
Gamma camera
Consists of radiation source, collimator, scintillation crystal, light guide,
photomultiplier tubes, and electronics for pulse-height analysis and position
information.
o A thin crystal is desirable for limiting light spread; however, a thick
crystal is desirable for its greater stopping power.
Spatial resolution is obtained by comparing the response ot adjacent PMT’s.
Hence can get much better resolution than the diameter of the PMT’s (3-4cm);
max resolution is usually limited by the collimator, which has a maximum
resolution of its hole diameter
Collimators:
o Collimators only allow light traveling from a certain direction to
interact with the crystal.
Made of a sheet of thousands of parallel holes separated by lead
septa
o Resolution is given by $ D(L+H)/L, where D is the hole diameter, L is
the hole length, H is the distance to the patient. Hence max resolution
as H 0 is D.
Compromise between resolution and efficiency
o (H) Collimators block out >99% of the incident light.
o Collimators have umbra (light passes straight through) and penumbra
(light passes through at an angle)
o Cone beam or pinhole collimators can be used to magnify an image—
used in clinical applications for imaging small structures, such as
children.
Camera performance
o (H) Light guide is used to spread the signal across the detectors. This
reduces resolution (as expected, heh!) but increases uniformity. New
cameras have very thin light guides.
o Light can be localised using Anger positioning logic. This compares
the inputs from different PMTs, and works out where the incident light
on the crystal must have been
o Spatial resolution
The main (extrinsic) spatial resolution factor is the collimator.
But the crystal resolution (intrinsic) also limits it:
Randomness of electron output by PMTs. Higher
energy gamma rays produce larger number of electrons
and thus smaller random errors.
Scatter in the crystal. Crystal thickness also degrades
resolution, since more scatter occurs.
o Other important factors:
Uniformity
Spatial linearity
Sensitivity
o Hence, the main tradeoffs in gamma camera design are crystal and
collimator design:
Thick crystal: high efficiency; thin crystal: high resolution
Thick collimator: high resolution: thin collimator: high
efficiency.
Energy resolution
o Pulse-height analysis rejects photons of the wrong energy: this is
nuclear medicine’s only defense from scattered photons.
o Formula: $ ER(%)=100*FWHM/Epeak, where Epeak is the energy of the
peak (say, 140 keV) and FWHM is the width of the distribution at
Epeak/2.
o If photons of a single energy are incident on the crystal, some spread of
energy output will be observed. This limits the energy resolution.
Limited energy resolution in turn limits how narrow the limits
on an energy window are—thus, reject events that are OK and
accept events that have probably been scattered too much.
Even a 45 degree scatter only changes photon energy by about
8%.
Ideally, should have delta-spike from energy; this is what one
would get if no scattering.
(H) Count rate peformance: if the radiation levels are too high, the PMTs are
saturated and losses start to occur—nonlinear behaviour.
Also see nonuniformities and pulse pileup.
Phantoms are devices which are used for comparison or testing.
Lecture 2: Emission tomography SPECT (Bailey)
Topics: SPECT, sampling, reconstruction, projection slice theorem, filtered back
projection, filtering. Errors, attenuation and scatter, resolution.
SPECT basics
Uses gamma camera and tagged radiopharmaceuticals; attenuation is an
important concern
Time resolution is about 30 seconds; energy resolution is about ± 30%.
Uses projection theory to work out 2-3D structure from 1D projection.
Data are recorded in terms of a sinogram, which plots radial distance versus
camera angle.
Sampling
The number of angles that need to be sampled from depends linearly on the
object size and inverse-linearly on the spatial resolution, or $ N S/R, where
N is the number of angles, S is the object size, and R is the FWHM.
Spatial resolution can be defined in terms of the full-width at half maximum
(FWHM), which is what it says it is for a point source spread.
Reconstruction
Basic idea: an n dimensional system can be reconstructed by n-1 dimensional
projections from different directions (discovered by Radon).
Reconstruction can be done analytically (preferred method, using filtered
back-rojection), algebraically (possible, but computationally intensive), or
statistically (newer, occasionally used technique). (H) The advantage of the
statistical technique is that it can incorporate scatter and other complications.
Data is collected in the spatial domain; it can be transformed into the Fourier
domain (spatial frequency).
Filter out high spatial frequencies: this reduces noise at the cost of reduced
resolution.
(H) Responses that are narrow/steep in the spatial domain are broad in the
frequency domain, and vice versa. Hence, can cut out noise by rejecting high
frequencies.
Projection slice theorem
Each view is an integral of the activity through the patient. The Fourier
transform of this projection is the same as a slice through the Fourier
transform of the patient; the angle of this patient-Fourier-slice is given by the
angle of projection.
(V p.145) Also called the central slice theorem, the different angles of
projection sweep over all of frequency space so the fourier function F(vx,vy) is
known completely, from which the actual image f(x,y) can be trivially
reconstructed. In this process, the centre is oversampled if the edge is sampled
sufficiently.
Filtering
(H) Back projection produces a 1/r blurring effect and star artifacts. If no
filtering is done, each point acts like a star.
o (H) Ramp filter exactly corrects for 1/r attenuation effect, but amplifies
noise. Hence, use other filters.
Butterworth filtering cuts out high spatial frequencies: less resolution and
better SNR.
(H) The Nyquist frequency is the maximum spatial resolution that the system
can represent. It is equal to $ 1/(2*Sp), where Sp is the pixel size; in other
words, the maximum resolution is B-W-B-W etc. pixels, which have that
frequency.
(H) Iterative statistical approaches can account for attenuation and simulate
reconstruction. Iterative approach. Do by projecting virtual image to virtual
detector; convolve with noise and blurring, and see what gives the best match
to observation. Called forward projection. If this process is carried on for too
long, begin to start fitting noise.
Errors
Centre of rotation:
o Each system has an axis of rotation about which the gantry heads rotate.
If a source is placed on this line, a single point source at the middle of
the image should be observed from each projection.
o Offset can either be uniform for different angles (bad) or nonuniform
(really bad). In really bad cases, this produces doughnut artifacts. Else,
it just degrades spatial resolution.
o Nonalignment can be either mechanical or electronic.
Uniformity
o Nonuniformities produce ring artifacts centred at the image centre;
their importance decreases on 1/r; a nonuniformity right at the centre
produces a huge error in the final image.
o Uniformities are checked by using uniform high count studies
frequently (daily or weekly); they are updated (corrected for
electronically) every few months. These changes occur as a result of
changes in the crystal and the PMTs.
o Nonuniformities can be either spatial or intensity. Both can be
electronically corrected for.
Head tilt
o Occurs when the camera head normal is not exactly orthogonal to the
axis of rotation.
o Causes the greatest blurring at the edges of an image.
o Can test by placing a point-source on the axial direction, but near the
edge of transverse direction. Head tilt will show up as a change in the
axial position.
Patient motion produces blurring
Parameters
Minimum matrix size is given by $ M > S/R, where M is the matrix size, S is
the object size, and R is the resolution.
Angles obey $ Na > 2r/Sp, where r is the radius of the region of interest, Na
is the number of angles, and Sp is the pixel size.
180 degree acquisition is faster and uses less disk space, but can’t get
information on differential attenuation.
Want to maximise acquisition time
Attenuation and scatter
Scatter builds up as $ A- e-d; attenuation goes as e-d, where d is distance.
Easiest method of attenuation correction is the Chang method: simply assume
uniform attenuation and boost the signal accordingly.
More sophisticatedly, one can place a radioactive source behind the patient
and measure attenuation from different parts of the body—this is similar to xray CT.
Spatial esolution
Affected by:
o distance to detector (less is better)
o attenuation (less is better)
o nonuniformities (less is better)
Lecture 3: Emission tomography SPECT & PET (Bailey)
Topics: (Attenuation and scatter, scatter correction, quantification.) PET, cyclotrons,
gamma ray detection, spatial resolution, detectors, PET acquisition, (attenuation
correction).
PET
Typically high radiation doses, perhaps twice that of SPECT
Atomic physics:
o Five types of radioactive decay, but only two are used. The types are
alpha, beta, gamma, pair production, neutrons; only gamma and
positron are used for imaging; and of these, only gamma rays are
actually measured (H).
o Alpha emission (increases N/Z ratio, since an excess of N).
o Isomeric transitions (emission of gamma rays, such as [99m]Tc, where
m stands for metastable)
o ba X b1aY e (beta decay)
Neutron-rich sources can decay by emitting an electron and an
antineutrino (and a gamma ray); this is radioactive beta decay.
o e e 2 (pair production)
The positron and an electron form positronium, which is like
hydrogen, and then shortly annihilate, producing two opposite
gamma rays. Three photons can also be emitted but with low
probability.
a
o $ b X b 1a Y e (positron emission)
This is the main reaction by which PET isotopes decay. It
occurs for proton-rich nuclei such as produced in a cyclotron.
The radionuclide X decays into daughter compound Y which
has the same atomic mass but is a different element (one proton
has changed to a neutron). This process releases a positron and
an electron neutrino.
The gamma rays hence produced are observed in PET and have
a minimum energy of 511 keV each.
a
o b X b a1Y e (electron capture)
Electron capture, where the nucleus captures an electron and
converts a proton into a neutron, occurs in some elements; the
filling of the electron-shell vacancy results in characteristic
radiation
This process occurs when the compound does not have
sufficient energy to decay by positron emission.
o The fact that the positrons may travel some distance before
annihilation, and the fact that they can emit gamma rays at not quite
180 degrees, places a constraint on the accuracy on PET.
o Positron range varies depending on the decaying isotope; there is a
correlation between compound cross-section and positron distance. It
also depends on the tissue—localisation in the lungs is shit, for
instance.
o PET is based on principles of physiology—that is, the radiotracers will
be integrated into biochemical processes, allowing these processes to
be studied. Such processes include concentrations, receptor densities,
enzyme activity, etc.
o Emissions interact differently. Gamma rays are high-energy and hard
to stop; typically pass straight through tissue. Beta particles are easier
to stop; alpha is very easy to stop. Positrons travel several mm in
tissue.
Gamma ray detection
PET systems take advantage of the fact that two gamma rays are emitted,
using annihilation coincidence detection (ACD) circuits. PET, though a
tomographic technique, collects data for all projections simultaneously.
Several types of detection can occur:
o Single; this forms the basis of all other events. >90% of events remain
unpaired.
o True unscattered, where two events are registered and they lie on a line
with the point of annihilation.
o True scattered, where one gamma ray has been deflected, so the two
detectors and the point of annihilation do not lie on a single line. Due
to poor energy resolution, these events cannot always be rejected.
o Random, where the gamma rays from more than one nuclei are
simulataneously registered. This rate increases as the square of the
activity. It is stochastic whether or not these are from the same nucleus
or not.
o The rate of random activity can be improved by minimising the time
window, which depends on the crystal.
Energy discrimination is used to reject photons that have been scattered in the
patient; however, these also reject photons that have been scattered in the
crystal, which are fine.
Detectors and performance
Most common detector is a ring-type detector, but this is expensive since it
uses so many PMT’s and much crystal. Can also have partial ring and rotating
gamma camera setups.
Spatial resolution is about 5 mm; this is mostly limited by the detectors.
o Sources close to the edge of the system can emit photons which
interact with the crystals at a variety of depths; this causes a reduction
in resolution.
o Theoretical lower limit for spatial resolution is about 1.5 mm because
of the finite distance positrons travel.
PET acquisition
(H) Not a 1:1 correlation between the detectors and the PMTs; the crystal is
cut into blocks, and the size of the blocks determines the resolution.
3D PET is similar to 2D, except it’s more complicated, more efficient, has a
higher number of random coincidences and scatter.
o No collimation is used in 3D PET; this greatly increases sensitivity.
o Both 2D and 3D PET are used; one isn’t better than the other.
If the amount of activity is too high in 3D PET, most of what’s counted is
singles, which just wastes the system’s time. Thus the coincidence count rate
actually drops at high radionuclide concentration.
o This is because random coincidence rate increases as the square of the
count rates.
Attenuation correction is possible in PET since all photons pass through a
complete line-of-sight. Thus it can be accurately accounted for; however, high
levels of attenuation (e.g. 40) in the middle of the abdomen, for instance, mean
that the signal coming from there is going to be very noisy.
Can perform dual PET/CT acquisition. (SPECT and CT not popular, even
though practical, simply because SPECT machines are cheap.)
Lecture 4: Radiopharmaceutical chemistry in nuclear medicine (Kassiou)
Topics: Radiation decay*, radionuclide production, radiochemistry—general, baboons,
fluorine, FDG, fluoro-Dopa; animal models.
Radionuclide production
Radionuclides can either be produced in a cyclotron or a reactor.
o Cyclotrons
(I) Use a permanent magnet with a field pointing into the plane
of the magnets. Voltage is switched at the cyclotron frequency,
qB/m, and the particle is accelerated in ever-larger circles. The
cyclotron frequency remains constant, since the T=2*pi*r/v and
v=qBr/m, so =qB/m.
The cyclotron accelerates protons (or deuterons, etc.) into
stationary nuclei.
In a cyclotron, protons are accelerated at high speed and
rammed into a target; this produces proton-rich nuclei such as
[18]F and [15]O, which decay emitting a positron and a neutron,
producing such lovely entities as [15]N.
o In a reactor, a target is bombared with neutrons, producing a neutronrich nucleus such as [99m]Tc, which decays by emitting an electron, p
n, and a characteristic gamma ray.
o PET/SPECT radionuclide comparison:
Parameter
PET
SPECT
Production
Cyclotron
Reactor
Biological?
Yes
No
Price
Expensive
Cheap
Half-lives
Short
Long
Quantitativity Yes
No
Radiochemistry
Desirable quantities in a radiopharmaceutical:
o To reduce patient dose, as much as possible of its emission should be
in the form of clinically useful photons.
o It should have high target specificity to increase contrast.
o It should be as cheap as chips.
[11]C undergoes chemistry just like regular carbon—hence all the standard
reactions of methylation, esters, etc. are possible.
Example: benzodiazepine receptor
o Important in many diseases such as Alzheimer’s, cancer. Found
peripherally (e.g. heart, kidney etc.) and in brain (microglia)
o Can image by developing chemicals that bind very strongly to this
receptor. Also need to consider availability: i.e., must be able to cross
the blood-brain barrier.
o Also, must find a chemical that meets these requirements and can be
radiolabelled. In this case, use [11]C.
o It takes ~12 minutes to produce methyl iodide (CH3I), during which
time about 1/3rd of the carbon has decayed—time is of the essense!
o (H) Need high activity (so short production time) but also high purity
to avoid toxicity (but this takes time to test and filter). Total
production takes about 25 minutes.
When synthesising compounds with radionuclides, it is desirable to introduce
the radionuclide as late as possible. This is to minimise decay and operator
exposure.
Baboons
(H) New radiopharmaceuticals are tested on animals first. Baboons are
injected, and then you can PET the baboons.
These radiotracers can be used to study the effects of competitive inhibition.
In the presence of a competitive inhibitor, there may be very little/no uptake,
and then no signal is observed from the brain.
In general fluorine chemistry is complicated, since it exists in both F2 and Fforms. The latter form reacts nucleophillically, whereas the former interacts
electrophillically. F2 can be added across double bonds; F- can replace leaving
groups.
18
2-[ F]Fluoro-2-deoxy-D-glucose (FDG)
Most used radionuclide in nuclear medicine, especially in PET.
[18]F is produced from [18]O in a cyclotron.
Metabolism:
o Analogue of glucose; metabolised very similarly.
o However, after it is metabolised to FDG-6-phosphate, it gets stuck, and
can’t be metabolised.
Applications
o Since it is uptaken like glucose, it can be used to measure the amount
of metabolic activity in tissue. Since cancer is very metabolically
active, it shows up like a cold girl’s nipples on a PET scan.
o By contrast, mental disorders can be characterised by reduced uptake,
such as in Parkinson’s, Huntington’s, Pick’s, and multiple infarct
dementia.
o In addition to diagnosing disease, this can be used for staging. As
Alzheimer’s gets progressively worse, the uptake of FDG
progressively decreases, until the brain looks like a newborn’s. (I
know, doesn’t say much about newborns.)
o Targeting can be extremely specific: can target either the presynaptic
side (#{vesicles?}), postsynaptic side (receptors) or production
(dopamine).
Fluoro-dopa
Used to study Parkinson’s disease: reduced uptake since a loss of dopamine
receptors in the substantia nigra due to cell death.
Nicotinic receptors are downregulated in Alzheimer’s disease; this can also be
measured.
Drug development is a long, expensive, complex process. Medical imaging
can help with drug design by determining what is actually a problem in the
first place (e.g., dopamine receptor loss) and how effective treatments are (e.g.,
their binding properties).
Two phases are important for drugs. The pharmacokinetic phase is the phase
where the drug is being uptaken into the body and cleared from the blood;
PET studies can be done on this, but the drug itself needs to be radiolabelled.
The other phase is the pharmacodynamic phase, where the drug itself has its
action (e.g., binds to a receptor). In this case, through the radiolabelling of a
competitive inhibitor, information about the drug can be obtained indirectly.
If competitive inhibition occurs, the abolished uptake will be visible.
Good radioligands have:
o Can cross BBB
o High receptor affinity
o Quick to produce
o Low non-specific binding
o Subtype selectivity
o Metabolic stability
o Highly radioactive
o Optically pure
Animal models and random tidbits
99% of human genes have animal homologues. Thus, many diseases can be
studied in animals.
For PET, one of the main challenges is their size—2mm resolution is fine for a
human brain, but if it’s a rat, and the brain is, like, 3mm, that kind of like
really sucks. Hence, have developed special scanners.
In general, there is a tradeoff between the availability of an isotope and its
impact on the chemistry. For example, [11]C has no effect on the chemistry—
acts just like carbon. [18]F as a substitute for hydrogen has a minimal effect;
[123]I as a hydrogen substitute has a larger effect. Tc-99m has a substantial
effect, being a huh-wuh metal atom that is stuck to some poor little organic
compound.
Iodine-123 is the most useful iodine compound for imaging (H); it decays by
electron capture. Iodine-131 decays by gamma ray emission and has a much
longer half-life.
Of the four isotopes:
o I-123 has a short lifetime and is best for SPECT
o I-124 decays (sometimes) by positron and can be used in PET
o I-125 has a long half-life and is used in autoradiography
o I-131 has a long half-life and can be used for radiotherapy.
In a process taking about 2 hours, iodine can be used to label a nAChr ligand
for use in animal/human Alzheimer’s disease studies. This synthesis requires
a good leaving group of the original compound.
Tc-99m, which can be used in blood flow studies among others, has quite
simple chemistry compared to fluorine—you can just shake it up! (H)
Lecture 5: Radiological Imaging 1 (Hill)
Topics: X-ray tubes, production of x-rays*, factors affecting image, x-ray
interactions*, attenuation, units.
X-ray tubes
Consist of anode, cathode, vacuum tube, and rotator.
Basic principle: a huge voltage is applied across the system. The tungsten
cathode is heated, releasing electrons (thermionic emission). These electrons
are then accelerated, via the potential difference, to the cathode. Their kinetic
energy is then turned into x-rays.
Adjustable parameters are peak voltage (kVp), exposure time (s), and tube
current (mA). Shorter exposure times are used with larger tube currents.
Cathode:
o Consists of a tungsten filament (use tungsten because doesn’t melt)
heated to 2200 C. This emits electrons. Also use a focusing cup.
o In the absence of a voltage drop, these electrons will just form a spacecharge cloud around the filament. With a voltage drop, they will be
accelerated to the anode. However, if the voltage drop isn’t big
enough, the space-charge cloud will affect tube current.
The saturation voltage is the voltage at which further increases
in voltage have no effect on tube current. At lower voltages,
the process is limited by the space charge cloud; at higher
voltages, the process is limited by the filament current.
Increasing filament current increases tube current; increasing
tube voltage also increases tube current.
o Most machines have two filaments: big and small.
o Focal spot
The size/position of the focal stop is determined by the beam of
electrons, which in turn is determined by the filament size.
Focal spot size is also determined by the use of a focusing cup,
which focuses the electrons into a small spot. This can either
use the filament voltage or a different voltage, the bias voltage.
Bias voltages of hundreds of volts can focus the beam; of
thousands of volts can shut it off completely.
Anode:
o Made of tungsten on a copper electrode base for heat conduction.
Most electrons hitting the anode deposit the majority of their
energy as heat.
Tungsten is also used because its high atomic number means
that it is efficient at producing bremsstrahlung radiation.
o Rotates at high-speed, again for heat dissipation. High-speed rotation
is achieved using magnets and bearings (either ball-bearings, which
wear out, or liquid metal bearings, which are better and allow greater
heat conduction).
Portable and dental x-ray systems often just have a fixed anode.
The increased area for a rotating system is given by
$ A=W*r*(2pi), where A is the area, W is the width, and r is
the radius.
o Anode angle:
The angle of the anode affects the focal spot size given by
$ E=A*sin, where E is the effective focal spot size, A is the
actual focal spot size, and theta is the anode angle from vertical.
A smaller angle:
increases spatial resolution
decreases field coverage
o The size and shape of the focal spot depends on the position in the
image plane: closer to the anode, the spot is smaller.
Tube cooling:
o The maximum exposure time is usually determined by limitations on
the amount of heat that can be dissipated by the anode.
o As kVp is increased, both tube current and average electron energy is
increased, thus the energy dissipated goes as kVp2. Hence, there is a
decrease in maximum exposure time with increased kVp for a given
tube current.
o A heat unit is a joule of energy deposited. It can be calculated from
$ mA*kVp*s, where mA is the tube current, kVp is the tube voltage,
and s is the time. If rectification is used, then this is multiplied by a
factor of 1.35.
o Since so much of the energy is converted to heat compared to
bremsstrahlung, we can actually assume it’s close to 100%.
Heel effect:
o Portion of image towards the anode end gets less radiation than
towards the cathode end, because the radiation has to pass through a
greater thickness of anode to get to the patient. This can be used to the
radiologist’s advantage; the thick part of the patient can be put towards
the cathode end to get more irradiation. This is, however, a bit crude.
o Off-focus radiation is also a problem. This is caused by electrons
striking the anode outside the focal spot; it can be made better with a
collimator around the x-ray output window.
Production of x-rays
The wavelength (and of course energy etc.) of the x-rays is determined by the
kVp (H).
X-rays are produced continuously from 0 eV to slightly above the
characteristic energy; the low-energy ones are useless and just contribute to
patient dose. It is desirable to filter these bastards (H).
The two main types of x-ray production are bremsstrahlung and characteristic
x-ray production.
o Bremsstrahlung occurs when an electron traveling at high speed past a
nucleus is deccelerated; this releases a photon of energy from zero (for
a glancing blow) through to the maximum (where all the kinetic energy
of the electron is converted into the photon, if it “hits” the nucleus for
example).
An energy spectrum is thus produced, and the number of x-rays
at a given energy decreases linearly with that energy.
This spectrum is filtered for medical use, since low-energy xrays just increase patient dose.
Efficiency of bremsstrahlung (as compared to collisional loss)
is directly proportional to both x-ray energy and the atomic
number of the target.
o Characteristic x-ray production occurs when an incident electron
collides with one in the lowest energy state (“K-shell”) and ejects it
from the atom. Then an electron of a higher energy state falls into the
hole, and releases an x-ray as she goes. This produces an x-ray of a
certain wavelength depending on what the higher energy electron shell
was.
For electron shells, K=s, L=l, M=d, etc.
This only occurs if the incident electron energy exceeds the
electron binding energy in the target atom.
As the kVp increases, this increases the ratio of characteristic to
bremsstrahlung x-rays.
X-ray generators
An x-ray generator is the device that supplies the power (current at very high
voltage) to the x-ray tube. The parameters that can be varied are the kVp, mA,
and s.
Use transformers to step up (increase voltage, decrease current) or step down
(increase current, decrease voltage). Filaments need high currents and low
voltages; tubes need high voltages.
Since the input is AC, the response needs to be rectified. Full-wave
rectification is sufficient for pictures, but three-phase rectification is used for
CT scans (H).
The type of x-ray generator used affects the type of spectrum produced (H).
Factors affecting the image
Basic problem in radiological imaging: balancing image quality against patient
dose (H).
The operator selects the kVp, the mA, the s, and the focal spot size, but not all
independently.
“Exposure” is mA*s, or mAs. kVp is the peak kilovoltage which determines
the energy spectrum (H).
X-ray emission is affected by:
o Anode material (affects quality and efficiency of bremsstrahlung &
characteristic x-rays)
o Tube current (amount of x-rays produced; exposure >< mA)
o Exposure time (exposure >< s)
o kVp (quality of x-rays produced; exposure >< kVp2 because kVp
increases both the electron energy and the efficiency of
bremsstrahlung)
o Beam filtration (affects the hardness and number of x-rays)
The x-ray spectrum produced from the x-ray tube is filtered to reduce patient
dose. This is done primarily by removing low-energy x-rays which cannot be
used for imaging.
X-ray interactions
X-rays can interact in four ways:
o Rayleigh scattering
Elastic scattering of the photons off entire atoms in the material.
The scattering can be elastic since the mass of the electrons is
large compared to the momentum of the photons.
Proportional to E-4; not important in this context.
o Compton scattering
A gamma ray imparts some of its energy/momentum to an
outer valence shell electron, ioninsing it from the atom. The
amount of energy lost is proportional to the change in direction
of the gamma ray. It happens mostly with valence shell
electrons.
Compton scattering becomes more and more dominant with
increasing energy; at the energies used in x-ray radiography, it
is the dominant form of interaction.
Compton scattering increases with electron density; this is
linear with mass density except for hydrogen, which scatters
even more.
o Photoelectric effect
A gamma ray is completely absorbed by an electron in an atom
and ionises it completely from the nucleus. When this hole is
filled, it produces a characteristic x-ray.
$ Increases as Z3/E3.
o Pair production
Gamma ray turns into e+e- pair; this only occurs for very high
energy (minimum gamma ray energy 1.022MeV). Not used in
radioimaging.
The relative ratio of the different effects depends on both the energy of the
gamma ray and the effective Z of the material. For example, at 60 keV, most
interactions in water (Z=7.5) are from Compton; in NaI (Z>>8), they’re
photoelectric.
Attenuation
Caused by absorption (photoelectric effect) and scattering (Compton).
Important in radiotherapy as well as imaging.
Defined by a linear attenuation coefficient , where $ N=N0*e-x, for a
monoenergetic beam.
Two characteristic behaviours: narrow beam and broad beam; mass
attenuation coefficient or linear attenuation coefficient.
o Difference: linear attenuation coefficient is how much a certain
distance of material will attenuate. This depends on the density of the
material; for example, water and ice have different linear attenuation
coefficients.
o Mass attenuation coefficient is how much a certain mass-distance of
material will attenuate. For example, ice and water have the same
mass attenuation coefficent, since they have the same number of
electrons per gram.
o The two are related by $ linear/=mass.
In the nuclear medicine range of photon energies (~>100 keV), Compton
scatter is by far the dominant form of attenuation.
Units
The total linear attenuation is the sum of the linear attenuations from all four
scattering/absorption processes. At diagnostic energies, it’s mostly just
Compton though.
The half-value layer is another measure of attenuation, the distance by which
half of the radiation will have been blocked. The relation to is HVL =
ln(2). Formula is $ left=2(x/HVL), where x is the distance.
Because attenuation is inversely correlated with energy, more attenuation
tends to lead to beam hardening: x-ray spectrum becomes shifted towards
higher energies. The HVL also increases.
Fluence—the number of photons per area (time integral of flux)
Flux—the number of photons per area per time
Energy fluence —the energy per area (energy per photon * fluence)
Kerma—the energy released per mass, J/kg ( *tr.
o Calculated using the mass energy transfer coefficient, which is the
amount of energy released into charged particles as kinetic energy.
Dose—the energy deposited per mass, in grays, J/kg ( *. Also
measured in rads.
o If all energy is deposited locally, this is the same as the kerma.
o Calculated using the mass energy absorption coefficient, which is the
m.e.t.c. but taking into account bremsstrahlung and other methods of
energy lost to the small volume.
Exposure—the amount of ionisation per mass, C/kg or roentgens.
o Useful because can be directly measured.
Can be converted to air kerma using the conversion factor 1
C/kg = 33.67 J/kg.
o F-factor—the conversion factor from roentgens (ionisation in air) to
rads (absorbed dose), dependent on effective Z and type of radiation.
Equivalent dose—dose modified by a factor accounting for the different types
of radiation, measured in sieverts (=dose for x-ray photons). Also measured in
rem.
Effective dose—effective dose taking into consideration the sensitivity of
different tissue types to radiation (sum over whole body = 1; gonads most
sensitive)
Lecture 6: Radiological Imaging II (Hill)
Topics: Phosphors, x-ray film radiography, fluoroscopy, image intensifier, radiation
scattering, projection radiography, digital radiography, flat-panel detectors, digital
image processing, mammography*, x-ray tube design.
Phosphors and fluoroscopy
Fluorescence and phosphorescence are both types of luminescence; the only
difference is the emission time, <10-8 s for fluorescence and >10-8 s for
phosphorescence.
o Phosphorescence occurs as the result of a forbidden transition (T) and
is usually undesirable.
o Fluorescent intensifying screens are scintillators that can detect x-ray
radiation and convert the ionising radiation into visible or UV light.
o Different scintillator crystals have different output curves: CaWO4 is
towards the red, while BaFcl and CsI:Na are towards the ultraviolet.
The film itself is quite short-wavelength.
Definitions:
o The intrinsic efficiency of a luminescent screen is its efficiency at
converting ionising radiation energy into photon energy. This
decreases with Z.
o The screen efficiency is its transmittance of this released light.
o The quantum detection efficiency is the likelihood of an x-ray
interacting with the screen. This increases with screen thickness.
The intensifying factor of the screen (compared to using the film directly) is
given by $ (exposure without film)/(exposure with film). #{bit of detail on
“screen speed” I skipped}
Film is sandwiched between two screens and reflective layers to maximise
efficiency. The film helps amplify the signal, compared to the human eye.
The whole kaboodle is called the “cassette” and the cassette is opaque to
visible light, so only the visible light produced by x-ray/screen interactions can
expose the film.
X-ray film radiography
Luminescent screens are used since the film itself isn’t very sensitive; can get
get up to 5% direct darkening from ionising radiation, though.
Common screens: Gd2O2S and lanthanum-oxy-bromide. Cesium iodide is also
used for fluoroscopy and digital radiography.
In a silver halide film, silver and bromide ions coexist. When a photon hits a
bromide ion, it displaces the electron, which migrates to the “sensitivity
speck”. Since this is now negatively charged, the positively charged silver
ions migrate to it. This process of silver ion migration is what gives rise to the
image.
Use of a screen such as Gd2O2S increases film sensitivity by a factor of 50:
from 0.6% to 30%. This thereby reduces patient dose by a factor of 50. It
does degrade the resolution, however.
The photographic density of a film is given by $ log(I0/It), where I0 is the
incident light and It is the transmitted light.
Fluoroscopy
Fluoroscopy is the real-time viewing of x-ray images, at up to 30
frames/second.
Used for positioning catheters, images of the heart, etc.
Setup: have an x-ray tube to produce the radiation, filters to harden the beam,
collimation to make the rays parallel, the table and the patient to scan, an
image intensifier, a lens, and a video camera.
All of these are fairly normal except the image intensifier, also called a II for
some arcane reason.
o The image intensifier uses a phosphor, CsI, to convert the ionising
energy into photons, and then a photocathode to convert this into
electrons. This is the input screen.
o Electron lenses then focus these electrons.
Since the input screen is curved, this produces a pincushion
distortion in the final image.
o An output phosphor converts the freed, focused electrons into visible
light. The anode is very thin and carries away post-collisional
electrons.
o The electrons are accelerated by a factor of 1000—this is what
produces the gain; however, this comes at a cost of pincusion distortion.
Setup is called “pentode” because there is a photocathode, three
accelerating electrodes, and the anode.
o The anode is made of aluminium and removes the electrons.
o The transfer function of the image intensifier takes an input of
exposure rate (grays/second) and outputs an luminance (candelas/s)
o The gain is a product of the electronic gain (from the acceleration) and
the minification gain (taking a large area and projecting it onto a small
area). Increased magnification results in lower intensity/gain, which
can be compensated for by an increase in exposure.
o Quantum detection efficiency is limited by the film and the vacuum
window, which both absorb x-rays without converting them to photons.
o Due to the effect of the Earth’s magnetic field on the accelerated
electrons, some distortion is produced, as with a television.
o The output of the image intensifier is coupled to the video camera
using lenses, a partial mirror, and an aperture. This controls the
intensity of light passing through, giving automatic exposure control
(AEC).
Instead of using an image intensifier and video camera, can use a flat-panel
semiconductor detector. This gives a higher quantum detection efficiency
because there is no need to make a vacuum tube surrounded in aluminium.
Instead of continuous fluoroscopy (which gives a high dose), can use variableframe-rate fluoroscopy and frame averaging.
o Pulsed fluoroscopy provides the same exposure to the patient, but since
imaging is done over shorter periods of time, it reduces blur from
patient motion.
o Frame averaging reduces noise, but can cause unacceptable lag.
Can also freeze-frame (“roadmapping”) so, for example, the doctor can see
where he’s got the catheter up to.
Types of fluoroscopy suites:
o Gastrointestinal
o Angiographic
o Cardiology catheter
o Portable.
o They differ depending on what part of the anatomy needs to be
fluoroscoped.
Automatic brightness control is built-in feedback that reduces unnecessary
dose by maintaining constant image brightness.
An anti-scatter grid, effectively a 1-D collimator, is placed between the patient
and the image intensifier/flat-panel detector. This only lets primary
unscattered radiation through. However it attenuates the signal by an amount
Tp=Iin/Iout*100=D/(D+d)/*100. D refers to the hole width, d refers to the side
width, D+d is the spatial frequency of the thing.
o Grid improves contrast by blocking out scattered radiation, which
gives a haze to everything (H).
o It should also reduce patient dose.
o The bucky factor is the speed at which the bucky moves back and forth.
o The grid can be upside down, off-centre, misfocused, or crooked.
Scattered photons an also be reduced by reducing air gap, but this causes
increased skin dose and magnification and reduced field of view.
Projection radiography
Can be either transmission or emission imaging
$ From the inverse square law, I I0/d2, but can replace d with r*cos. Hence,
for an oblique image, I I0*cos3.
$ Depth-dependent magnification: M=d/z, where d is the distance from the
source to the screen and z is the distance from the source to the object. Source
magnificiation m is 1-M.
Transmissivity is given by the attenuation coefficient mu and the path length,
and maybe cos.
Blurring is dependent on source distance d and object distance z. More
blurring if the source is closer or if the object is further from the screen (H).
$ Contrast is the difference between signal and background: C=(Is/Ib-1). As Ib
Is, C 0.
$ SNR is the contrast times the square root of the number of photons.
Quantum efficiency is just the efficiency that a photon incident upon the
detector will be detected; “detective quantum efficiency” is the change in the
signal to noise ratio, $ (SNR1/SNR2)^2.
Compton scatter is greatest contributor to contrast loss. Equation: $ 1/(1+R),
where R is the ratio of scattered to primary photons.
Digital/computed radiography
Superior access and image manipulation
Increased start-up and running costs, lower dynamic range, problems with
security.
Not fully digital: image is still formed on screen, and is then converted to
digital from that.
Computed radiography is somewhat different; a phosphor screen image
intensifier (like Gd2O2S) is used to convert radiation into visible light; this is
then picked up by a CCD. Alternatively, a direct/fibre-optic connection or just
a lens can be used when high quality isn’t needed.
Flat panel detector systems only use a single screen—not a sandwich detector
system.
o Problems: some of the area of the CCD needs to be dedicated to
electronics
Mammography
Breast cancer detection; 1 in 8 women develop breast cancer.
Regular mammograms find tumours an average of >3 times smaller than
tumours found by accident.
The main challenge of mammography is that the total path attenuation is low
and the differences in attenuation are low (cancerous tissue has similar density
to normal). To help with this, low keV x-rays are used, as these are more
sensitive to density changes.
The difference between screening and diagnosis is that screening is used to
quickly and cheaply cover a large number of people. Diagnosis requires much
better image quality and is used to determine the amount, type, etc. of cancer
(T). Other techniques like ultrasound and MR are better for diagnosis, but are
too expensive/side effects to be used for screening.
Tube design requires a small focal spot and a low operating voltage. Low tube
currents because of low kVp and space charge effect.
Anode design:
o Don’t use tungsten since not that high energy; use rhodium or
molebdynum instead, since these have characteristic x-rays of the
desirable energy (15-25 keV).
o Need to filter to reduce dose. Use Be to avoid attenuating desirable xrays; then have both Mo and Rh targets and filters; can use all
combinations except a Mo filter with a Rh target, since this blocks out
the very characteristic x-rays we want to image.
o Slightly higher tube voltage (25 30) increases the number of
characteristic x-rays
o Tungsten really sucks—no characteristic x-rays and much
bremsstrahlung.
o Because smaller anode angles give better power loading (distribution
of energy on the anode), use a very small anode angle and then tilt the
tube to compensate.
o Place the thick part of the girl’s breast towards the cathode end of the
system; from the heel effect this will get more irradiation than the
nipple.
Other factors
o Focal spot needs to be very small to get good spatial resolution; its size
changes across the image (SID=source-to-image-distance)
o Beam hardness varies with tube age and kVp
Minimum and maximum half-value layers are regulated, since
these correspond to too soft (increasing exposure) and too hard
(reduced contrast) beams.
o Tube output depends on kVp, target material, filtration, location in the
field and distance from the source.
o The operator selects the kVp and the mA; the time is automatically
adjusted by the automatic exposure control, which has an ionisation
chamber, sensor, and voltage comparer, to see how things are going.
o Breast compression is necessary to uniformify attenuation. This
reduces scatter, reduces geometric effects, and hence lowers dose.
o Scatter reduction can be achieved by reducing breast thickness and
using an anti-scatter grid.
This is similar to a collimator. They can be designed to move
so lines from the septa are not visible.
The increase in dose required with the anti-scatter grid is called
the Bucky factor; typical values are 2-3.
o Magnification: placing the girl’s breast closer to the source improves
resolution and reduces scatter, but increases entrance dose, exposure
time, and geometric blurring.
Dose depends on $ exposure*badness, where badness is determined by breast
thickness and composition, kVp, anode material, and filtering.
In addition to total dose, entry dose is an important consideration.
MTF is the modulated transfer function, the Fourier equivalent of resolution.
Lecture 7: Radiological Imaging III (Hill)
Topics: applications—paediatric, dental, angiography; computed tomography*—basic
principles, history%, detectors, acquisition details, reconstruction, image display,
radiation dose*, image quality, resolution, noise.
Applications
General dose reduction:
o Mamography, the glandular dose is important
o Chest x-ray, the entrance exposure (not dose) is the most important
o Paediatric:
Change kVp/mAs
Reduce scatter
No mistakes/unnecessary scans
o Dental:
accurate timers,
consistent film,
restraint of patient movement, and
beam collimation.
o Angiographic:
Appropriate image intensifier,
keeping the patient-film distance to a minimum, and
increasing the SID.
Paediatric is similar in principle to other systems; just have to be extra weary
of dose.
Dental modes: Intraoral and bitewing are short exposure, high resolution;
maxillofacial and cephalometric are longer exposure, more dose, less
resolution.
Angiography and cardiography
o Temporal subtraction is a fluorscopic technique; digital subtraction
angiography compares an image with and without a contrast agent.
o Subtraction increases signal constast. Depending on what is subtracted,
either soft or hard tissue can be accentuated (H). This is accomplished
by imaging at different kVp’s.
o Dose to the clinician depends on the setup—overhead x-ray tubes
typically give off higher doses than underneath, in which case most
dose is from patient scatter.
o Important to use a cumulative timer to calculate total patient radiation
dose, since fluoroscopy doses are high.
Computed tomography
Geometric tomography is a cheap technique to get some idea of 3D
localisation.
o Works because all structures out of the focal plane become blurred out.
o While it can be used for a single slice, it has too high of a dose for
multiple slices.
History:
o Computed tomography based on Radon’s technique; first developed in
70’s.
o A single film only gives 2D information. A lateral view as well gives
some 3D information. A complete rotation gives sufficient
information for a full reconstruction.
o Multiple projections are combined into cross-sectional images; each
slice is of a uniform thickness.
Basic principles
o Each ray forms a line integral of the attenuation through the patient. A
fan/parallel beam of rays forms a projection. This is acquired at 1000
different angles; the patient is then moved in the z direction, and
another slice is acquired.
o The linear attenuation coefficient per ray is preprocessed and stored—
this is the information on which the image is based.
o Backprojection consists of finding out what 3D arrangement of
densities could produce the pattern observed.
History
o First generation translated across patient then rotated around—pencil
beam reduced scatter, but poor contrast and slow as dogshit.
o Second generation used a rotate/translate fan beam—this had greater
scatter but was 30 times faster than 1st generation.
o Third generation didn’t need to do any translation—just rotate/rotate.
Much faster (<5 seconds), but expensive since needed many more
detectors.
Bad detectors in this system lead to ring artifacts
o Fourth generation had a fixed ring of detectors instead of a moving
set—rotate/stationary. This was again more expensive, but this was
necessary since it prevented ring artifacts, since each detector acts as
its own control.
o Fifth generation doesn’t use a conventional x-ray tube: instead, an
electron gun produces electrons which are focused onto the target in
the appropriate place, but this wasn’t a big hit.
o Sixth generation used continuous table translation or helical motion of
the x-ray tube; this led to a further reduction in scan time.
o Seventh generation uses multiple scanners in the z-direction separated
by septa; this helps with heat capacity issues because more of the
signal is used.
Current detectors
o Xenon detectors are gaseous detectors for use with third generation
machines; since xenon isn’t the best at stopping, they needed to be
very thick; they have a very small acceptance angle.
o Solid-state detectors have a much larger acceptance angle. In these,
similar to digital radiography, the x-ray photon comes in, hits the
scintillator which releases photons; these hit the photodiode and
release electrons. There is a small gap between the detectors to
prevent signal from going from one into the other.
This is similar to digital radiography, but the resolution is much
poorer in an effort to increase contrast.
o These solid-state detectors are arranged in multiple detector arrays;
each detector is similar/larger in width to the collimated beam of the xrays.
Slice thickness
o Slice thickness is determined by the collimator, which also affects
patient dose. It is also affected by the width of the detectors and the
number of detectors binned together.
o Slice sensitivity is a Gaussian curve centred on the centre of the slice;
it drops away sharply as one moves away from the centre of the slice
towards the edges of the beam.
o A helical scan can over-determine the system (pitch is less than 1),
providing more patient dose and a slower scan but better SNR.
o $ Pitch = (table movement per 360 degrees)/(detector width)
o $ Collimator pitch = Pitch/(number of detectors)
Tomographic reconstruction
o The data are collected as a sinogram; the amount of data is given by
(rays/view)*views
o The number of rays determines the radial resolution; the number of
views determines the circumferential resolution (angular resolution).
If not enough views are collected, the sample is aliased: high
spatial frequencies are lost.
o After data is collected, it is preprocessed using known information
about the response of the detectors, electronics gain, and then the
logarithm is taken: $ It=I0*exp(-*t) *t=log(I0/It).
o Helical scanning gives a more complex reconstruction algorithm, but is
advantageous in that it has greater uniformity and can produce images
in any plane.
o Reconstruction technique isn’t interative nor algebraic (too much data);
instead, use backprojection.
o Simple backprojection causes 1/r blurring; hence, use filtered
backprojection, which corrects for this. Filtered backprojection is a
mathematical convolution of the signal with the convolution kernel (in
Fourier space). Convolution is: “the process of breaking the image
into pixels and blurring each point with a point-spread function”. (H)
This process is easy to do in Fourier space: just multiply!
A direct filter to correct for 1/r blurring greatly enhances noise;
hence, filters are used that either roll off at high frequency
(Shepp-Logan) or go back to zero (Hamming). Different filters
are better for different tissues: bone filters have less roll-off
than soft tissue filters, because bones have a better SNR.
o From the raw data and filtered back-projection, a CT number can be
assigned to a certain attenuation path, given by
$ CTnum=((x,y)-(w))/(w) where mu is the attenuation and
mu(w) is the attenuation in water.
CT number is characteristic of tissue type as it directly reflects
the electron density of the tissue. Hence bone has 3000, water
0, soft tissue -300.
The determinant of CT number is electron density (because this
has the largest impact on Compton scattering rates).
CT numbers are quantitatively useful—a single measurement
of something gives useful information.
o CT can be used as a fluoroscopic technique, with partially new images
6 times a second, a fully new image ever second
o Digital image display allows contrast to be varied independently of the
acquisition—something impossible/very difficult to do with film.
Leveling and windowing determine midpoint and amount of
contrast, respectively.
With sufficiently helical scans, or thin enough slices (to
increase resolution in the z direction), can get fully 3D images.
Dose
o Because of the nature of the technique, CT scans have a high dose-toslice ratio. Also, they have high dose in general—up to 40 times as
much as a chest radiograph.
o Primary form of dose is in Compton scattering; the scattered x-rays can
spread dose to a larger area than just that being imaged. Scattered dose
can be larger than primary dose.
o Multiple scan average dose (MSAD) and CT Dose index (CTDI) are
ways of measuring CT dose.
The MSAD is the average dose to a small tissue volume from
both direct and scattered radiation. It is measured using a…
…CTDI, which is a protocol using a 10cm ionisation
chamber—inaccurate if much radiation scatters outside the
chamber.
o Like always, dose scales linearly with mAs.
o High pitch affects dose just how you’d expect: $ dose=dose0*(1/pitch)
o In CT fluoroscopy, dose reduction is a major issue. Dose is given by
$ dose=CTDIdose*time*current/(mAs), or D=D0*R1*R2, where R1 is
the ratio of the times and R2 is the ratio of the currents.
Image quality
o Always a tradeoff between dose, spatial resolution, and contrast:
SNR 2
o D 3 , where D is the dose, SNR is the signal to noise ratio, delta
T
is the pixel size, and T is the slice thickness. #{why cubed?}
o Spatial resolution
Defined as the ability to distinguish two points
Spatial resolution is affected by
Focal spot size—smaller is better
Number of detectors/rays and angles—more is better
Source-image distance—less is better #?
Magnification—less is better
Field of view—less is better
Helicity—less is better
Filtering—lower roll-off filter is better
Patient motion—less is better
Can be characterised in terms of point spread, line spread, or
edge spread functions. This is where an arbitrarily small signal
is smeared over a finite area; the area is defined by the full
width at half maximum (FWHM).
A stationary system is one where the PSF is positionindependent.
Magnification can either increase or decrease the spatial
resolution, depending on the size of the focal spot. Large focal
spots will decrease resolution; small ones will increase it.
Because projecting from a point source and since the
patient is not right at the detector screen, get some
magnification—can’t get minification.
o
o
o
o
o
In the frequeny domain, spatial resolution is defined as 1/2S,
where S is the minimum discernable object size, e.g. a pair of
lines.
The modulation transfer function is exactly this: the spatial
resolution in the frequency domain, and it corresponds to the
Fourier transform of point spread function.
The modulation transfer function characterises how
amplitude (contrast) is varied depending on frequency.
If no degradation, Cin=Cout, where C is the contrast. For
complete degradation, C=0. For example, low spatial
frequency lines will appear black and white; very high
frequency lines will appear uniform grey.
Although MTF provides best measure of spatial
resolution, its calculation can be tricky compared to a
PSF/LSF; these are hence often used instead.
Contrast resolution is affected by
kVp—shows maximum
mAs—more is better
Attenuation differential—more is better
Slice thickness—more is better
Reconstruction filter—quicker roll-off is better
Patient size—less is better
Artifacts
Beam hardening: when x-rays pass through bone, the beam
hardens; this confuses the reconstruction algorithm
Partial volume effect: if more than one type of tissue in voxel,
the CT system will provide the average attenuation coefficient.
Image quality is subjective; obviously correlated to SNR, but
graininess and other factors come into play. The key point is the
usefulness of the image in making an accurate diagnosis.
Five types of contrast: detector, display, subject, digital image,
radiographic.
Subject contrast is the actual difference in attenuation
coefficients across the patient, given by $ C=1-e-mu*t, where t is
the patient thickness. Total thickness doesn’t change contrast,
but changes in thickness do.
Detector contrast is given by $ contrast=(ODa-ODb)/(logAlogB), where OD is the optical density of the beam and A and
B are the #? total photon flux in two paths through the material.
Display contrast is the computer’s display—it’s at the whim of
the operator. However, garbage in, garbage out.
Digital image contrast is the contrast-to-noise ratio of the image,
whereby a constant factor has been subtracted from all terms
(A-B)/A. Hence, this simplifies to (A-B)/(A-k).
Radiographic contrast is the base difference between optical
densities: ODa-ODb.
Noise
The standard deviation of the signal is N1/2, where N is the
number of counts. Hence the SNR is N/N1/2 = N1/2. Hence
increasing SNR can be done by increasing patient dose.
Noise mostly affects observing low-contrast structures. Rose’s
guess is that objects are visible when SNR > 5, may be visible
under other circumstances.
Averaging information typically increases SNR and decreases
the resolution/contrast
Detective quantum efficiency encapsulates overall SNR
Highest possible imaging resolution is the space between
detector elements #{really? what about in nuc med?}
Averaging information improves SNR
Lecture 8: Radiological Imaging IV (Hill)
Topics: Patient dose*, radiobiology*, dosimetry, revision questions.
Patient Dose
The amount of dose the patient receives is highly dependent on modality. For
example, fluoroscopic techniques and CT both have high dose rates.
The effects of radiation are stochastic—except in high doses, all that happens
is an increased likelihood of cancer etc.
There are also some deterministic effects of radiation, but these are not so
important.
Dose is measured in terms of J/kg (grays), but this does not take into
consideration radiation damagingness or tissue sensitivity. The factor that
does take these into account is effective dose, measured in sieverts (same units,
J/kg).
o Energy imparted is another good one: measured in grays*kg, or just
joules.
o Entrance skin exposure is another important factor. This can be
defined by dose area product, dose over relative size.
In case it hasn’t sunken in yet, dose depends linearly in mAs.
Dose depends, as always, with 1/r2 dependence.
Automatic brightness/exposure control dynamically varies the kVp; this is
used to reduce the dose.
Backscatter makes up an important contribution to patient dose, about 35%
To calculate the dose at a certain tissue depth, use a look-up table or software.
Radiobiology
In addition to stochastic and deterministic effects, also have direct and indirect.
Direct: radiation kaputs a DNA double strand. Indirect: free radical creation
causes damage.
Interaction is typically by excitation, ionisation, and thermal heating; all later
damage arises from chemical changes in the cells.
o Most common chemical change is the production of free radicals from
water.
In general, damage from radiation rises with increased linear energy transfer.
However, above a certain point, everything has been killed 2-3 times over, and
there is no longer an increase.
Main processes in radiobiology are DNA strand breaking/thymine dimer
production, strand peroxidation, and strand linkage.
Amount of cell death is characterised by the quasithreshold dose (the dose that
would kill no cells if the process were linear, which it’s not) and the
extrapolation number (extrapolating the linear death curve back to zero
radiation, find that some thousands of percent of cells are alive!)
Higher linear energy transfer greatly increases the damage to the cells. For a
given percentage of cells surviving, the number of grays of radiation for highLET radiation is several fold less.
If the radiation ceases, cell repair is visible—this is from sublethal doses of
radiation causing reparable cell damage.
Different tissues respond differently to ionising radiation. Bone marrow and
the gonads are the most sensitive; neutrophils and thrombocytes in bone
marrow can be used as markers for the intensity of radiation exposure.
o Cells are most sensitive when they are highly mitotic, longly mitotic,
and/or undifferentiated.
When exposed to radiation, there is a lag time and then a (temporary) increase
in the likelihood of cancer. The integral of the extra curve represents the
associated risk of dying from cancer over your lifetime.
Measurement Systems
Quality control and assurance is important and federally regulated, but not as
strict as imaging parameters.
Testing systems are usually phantoms or electronic devices.
Lecture 9: Ultrasonic imaging (Hughes)
Topics: sound propagation and generation*, transducers, signal properties, attenuation
and propagation, signal processing, scan types.
Basics and sound generation and propagation
Sound propagates as longitudinal waves
When the wave contacts material of a different density, an echo is reflected—
this is the basis of ultrasound.
Forward compression doesn’t cause problems, but rarefaction can cause
cavitation and damage—used to treat kidney stones
Basic equations:
o Movements are extremely small (nanometres!), but accelerations are
huge: 105 g!
o $ Z=c, where Z is the impedance, rho is the density, and c is the speed
of sound. Changes in impedance determine how much sound energy is
reflected.
o $ Z2=tissue density* bulk modulus, where the latter is the
compressibility of the material.
Reflection:
o If a wave is reflected, it comes back at the same frequency. It
compresses the crystal, which can be measured as a voltage change.
Hence crystal has a transmitting mode and a listening mode.
o For clarity, a 5 MHz ultrasonic pulse will be received by measuring an
AC potential of 5 MHz.
Refraction occurs, just like in light, when sound wave travels into denser body.
Can even form double-images of deep arteries
Transducers
A piezo-electric crystal is used. When the voltage across the crystal is
changed, the orientation of the crystal elements change, changing the shape of
the crystal. A high-speed AC voltage supply will thus produce a sinusoidal
crystal displacement, and hence a sinusoidal pressure wave.
Piezoelectric transducer consists of: connector, live & earthed terminals, tuner,
backing material, piezo-electric crystal, and matching layer.
o The damping block at the back is very attenutating—to stop it from
shaking to pieces.
o The matching layer provides a transition between the crystal and the
tissue; otherwise, most of the sound energy would simply be reflected
back at the interface and the transducer would piezoelectrify itself to
death.
Resonance transducers are designed to operate with a very short pulse (such as
a microsecond).
o This causes it to ring at its fundamental modes; the frequency depends
on the crystal thickness.
o $ The thickness required to produce a certain fundamental mode is
given by T=(1/2)*(c/f), where T is the thickness, c is the sound speed,
and f is the frequency.
Arrays can be either linear or phased:
o Linear arrays fire a subset of crystals at once. This steers the beam; the
area is swept out by progressively activating groups of transducers.
Time delays are used for focusing.
Linear arrays have a wide and rectangular field of view; they
typically have up to 512 transducers.
o Phased arrays fire all at once, but with a time offset which can be used
to steer the beam to sweep out the region of interest. Time delays are
also used for focusing. All elements also receive at once.
They are smaller, easier to position, and have up to about 128256 transducer elements.
Transducer operation:
o Dynamic aperture is where the number of receiving elements is
increased to offset the reduction in lateral resolution from deep
structures.
o Transmit focus is where the transducer elements with time delays so as
to focus the beam.
o Receive focus is where the transducer elements are electronically given
a time delay so that when the signal is recombined, it’s not distorted.
This is because there is a greater range of time delays for a near source
than a far source.
o Pulse-echo operation is a procedure whereby a very short pulse is
given to the transducer, it “rings”, these rings stop before the return
pulse arrives. When the return pulse arrives, it deforms the transducer
and produces a voltage. This process is repeated at a rate of about 2
kHz, which gives a maximum tissue depth of about 40 cm.
o The steps in the receiver process are:
Detection, whereby the signal is received by the piezoelectric
element.
Preamplification, where the faint electrical signals are
amplified.
Time gain compensation, whereby signals are boosted
depending on the time delay.
Logarithmic compression, whereby the dynamic range is
compressed from 80 dB to about 30 dB.
Envelope detection, where the amplitude information is
extracted from the wave forms.
Filtering, whereby small peaks are rejected.
o Display modes:
A-mode (amplitude mode) simply presents the echo at each
interface. The data are plotted in 2D, with one axis refering to
amplitude and the other to depth (=time delay).
B-mode, same thing, except brightness is plotted in lieu of
amplitude. This is a 1D display mode.
M-mode, a 2D display mode which is just B-mode displayed
over time. Hence the axes in M-mode are brightness (strength
of reflection), as well as depth and time.
o 2D image creation
Image is produced by sweeping an ultrasound beam over the
region of interest, and displaying the information in B-mode.
There is a trade-off between spatial resolution (lots of A-lines)
and time resolution, since each line takes a finite amount of
time to produce.
Field of view, spatial resolution, and temporal resolution are
interchangeable.
Signal properties
The field can be separated into near-field and far-field regions.
o Near field has a converging beam profile. Its length increases with
transducer frequency and radius squared. The signal intensity is not
uniform because of the complex pattern of destructive interference.
o Far field has a diverging beam profile and amplitude decreases with
distance.
o Curved transducers have yet further focusing than normal transducers.
Higher frequencies have higher resolution but are attenuated by a factor of 1/f,
where f is the frequency.
$ The energy reflected at an interface is given by
2
Z Z2
, where R is the reflected energy and Z are the impedances.
R 1
Z1 Z 2
Impedance matching is the insertion of a material of intermediate impedance
to aid energy transfer. For example, pure PZT to skin has a reflectance of
80%; the addition of a plastic with intermediate impedance can reduce this to
60%.
The distance to the structure the reflection is coming from is just $ d=c*t/2,
where d is the distance, c is the speed of sound, and t is the time. The factor of
2 because it has to go out and come back.
The maximum axial resolution is given by x=n*/2, where delta x is the
separation between two interfaces, n is the number of periods in the pulse, and
lambda is the pulse wavelength. Lateral resolution is about half as good.
o The reason that separation distance increases linearly with period
number is that the first pulse will already be reflected to the first
interface by the time the trail end of the last pulse hits that interface.
Thus just gives blur.
Sound propagation in terms of attenuation
Sound energy is dissipated in three ways. The first is through heating of the
material. Second, much of the energy is reflected at each interface (both on
the way in and on the way out!). Third, sound is scattered.
The coefficient of attenuation is =2, since the attenuation goes as the
amplitude, and the intensity depends on the amplitude squared.
Have $ =(1/x)*ln(I0/I), in decibels, have =(1/x)*10*log(I0/I).
Rule of thumb: attenuation is 1dB/cm/Mhz.
o Tradeoff: resolution increases with frequency, but penetration depth
decreases.
The velocity of sound varies as a function of tissue density, of course, but
another good rule of thumb is 1540 m/s. This is slightly greater than water.
#{Can’t get example on L9.4.5(23) to work}
When a sound spreads from a circular transducer, it first assumes a sinusoidal
pattern, then a slow exponential decay. The area under the curve is constant, it
just spreads out and becomes less intense.
Signals range in intensity over a factor of 108, but must be displayed on a
monitor over 103, so must be compressed by a factor of 105.
o This compression can either be simply logarithmic or can amplify the
signal depending on the time elapsed from crystal excitation. This
later will make the deep structures as visible as the near ones, which
otherwise would not be the case.
Lecture 10: Doppler imaging/3D ultrasound (Hughes)
Topics: Doppler theory*, types of Doppler, examples, tissue harmonic imaging,
nonlinear propagation. Transducer, setup, ellipsoid fitting, hairy golf ball, volume
rendering, surface rendering.
Doppler theory
Double Doppler shift when sound is reflected from a moving source, given by
$ =s=vT, where delta_lambda is the change in wavelength, s is the distance
the object has moved, v is its velocity, and T is the period.
Doppler shift is given by $ f = -2*f*v*cos/c, where f is the frequency, v is
the object’s velocity, and c is the speed of sound, factor of two from reflection,
theta is the angle between the direction of motion and the probe.
Continuous wave Doppler:
o Uses a transmitting element and a separate receiving element; the
overlap between the areas excited by the transmitter and the areas
listened to by the receiver represents the sensitive volume.
o The transducer produces a continous wave, unlike in normal ultrasound
imaging.
o The frequency sent to the transducer is sent to the demodulator, which
then subtracts this from the received signal. Hence, what’s left is the
Doppler shift.
o The signal is then amplified and made audible, since the frequency
shift for blood is usually in the audible range.
o Continuous Doppler gives only the blood velocity; it loses information
on range.
Pulsed Doppler systems:
o Use a pulse-echo sequence similar to imaging, but with a longer pulse
sequence (5-25 cycles instead of <4). This reduces axial resolution.
o The pulse cannot be simply used to determine the Doppler shift.
However, when sound waves are reflected off a stationary pulse, a
constant phase is observed. When they are reflected off a moving
pulse, a phase change is observed.
o Each pulse represents a single measure of the phase; to construct the
frequency shift, the pulses need to come twice as frequently as the
phase is changing, or fmax=PRF/2, where fmax is the maximum
measurable Doppler shift and PRF is the pulse repetition frequency.
o Aliasing occurs when a signal isn’t sampled at a high enough
frequency (below the Nyquist frequency, which is twice per cycle)
Colour flow imaging
o Uses phase autocorrelation detection to determine Doppler flow. Here,
two (or more) beams are sent along the same path with a small time
delay. The two beams are compared; if the object in the beam path is
moving, the beams will have a phase shift relative to each other.
o This technique has lower temporal resolution because the flow and
image data must be acquired separately. Other problems include
reduced spatial resolution and aliasing.
Power Doppler
o Power Doppler is based on the amplitude of the Doppler signals
coming back; it does not rely on phase information. Hence, it is more
sensitive than colour Doppler, but the direction of flow information is
lost.
#{Relationship between vmax, dmax and f}
Tissue harmonic imaging
THI is a nonlinear effect, like in optics, only appearing at high intensities,
when the amplitude of the oscillation becomes greater than 0.1% of the
wavelength.
o Alternatively, it can arise from the use of micrometer contrast agents.
o In this mode, the output frequency is the same (but may be less
damped), but the receiver receives at a different frequency. For this to
happen, the transducer must have a large bandwidth.
A problem with ultrasound is the production of side and grating lobes which
interfere with the original signal. These are the same frequency as the output,
but they are not strong enough to produce harmonics; hence, harmonics being
recorded are free of disturbance from the grating lobes.
o Also, second harmonics are not return echos from the original
transducer, and this also reduces the noise.
Because the harmonics are high frequency, they have better resolution. But,
since they are generated at tissue depth, penetration is not compromised. This
can be used to image fat people.
Because of the advantages of harmonics at depth, you can use the fundamental
frequency to image close tissue and harmonics to image deep tissue.
In summary, tissue harmonic imaging allows superior depth, resolution, and a
reduction in noise.
Given a sinusoidal input, the nonlinear can be re-expressed using the
trigonometric identity cos(2x)=cos2x-sin2x=2cos2x-1.
Lecture 11: Magnetic resonance imaging (Baldock)
Topics: history, basic principles—magnetism, Larmour precession, resonance, free
induction decay (T2), relaxation (T1); pulse sequences—spin echo*, T1 weighting,
T2 weighting, density weighting, inversion recovery, imaging—slice gradient, phase
gradient, 2D acquisition, Fourier-space transformation.
History
Like everything, made possible by Fourier
Also relied on nuclear measurements and the development of NMR in the 50’s
Damadian developed first machine, but he was an idiot
Mansfield and Lauterbur developed first working machine in the 80’s.
Excellent contrast for soft-tissue imaging because there are lots of protons in
soft tissue; by contrast, in bone there aren’t many visible protons (fixed in
place).
Basic Principles
Magnets always exist as dipoles. When an atom is placed in a magnetic field,
it can be either aligned or anti-aligned with the field, since the atom itself has a
magnetic moment. Before, the orientation of the atom is random.
To some extent, proton and neutron spins cancel each other out; hence, only
atoms which have an imbalance (e.g. H, 13C) can be imaged.
o Since hydrogen is by far the most abundant, this is what is imaged
(except in fMRI, which uses carbon-13). H also has the highest
gyromagnetic ratio.
Although all protons line up, only a tiny fraction—just above 10-6—are in
excess from the parallel to the antiparallel state. This difference is due to the
difference in energy states, which in turn is dependent on the magnetic field
strength.
o If the temperature were zero, all atoms would be in the parallel state.
o The random phase of the precession means that no magnetic field is
observed in the transverse direction, but there is a net magnetic field
along the axis of the applied magnetic field.
All protons precess around the magnetic field lines with a frequency given by
the Larmor frequency, $ =gB, where omega is the frequency, g is the
gyromagnetic ratio, and B is the magnetic field strength.
o The energy is proportional to the Larmor frequency, and higher
magnetic fields produce faster precessions.
The phase of the precession is random, and hence no magnetic field
perpendicular to the external field direction exists.
But if a pulse of radiofrequency EM radiation at (well, within 10-12) the
Larmor frequency is inputted, this will flip some of the spins from the low
energy state to the high energy state.
o This is because the Larmor frequency is proportional to the energy
difference between the parallel and antiparallel states.
o The time this pulse is on for determines what percentage of the protons
flip.
o In the rotating frame of reference, this is like the incident RF magnetic
field applying a torque to the precessional magnetic field and tipping it
into the transverse plane. This, similar to before, happens at $ =gBt,
where theta is the angle of tipping, and t is the time.
o In addition to being tipped, all the atoms are in phase. This is similar
to the up-down phase alignment that happens when an external
magnetic field is applied.
Free induction decay: T2
o After the pulse is applied, the spins start dephasing. This can be
measured by a receiving coil as a damped sine wave. Dephasing does
the damping; the rotation gives the sine wave.
o Time constant of this decay is T2; typical values are 10-400 ms. This
depends on the proton’s environment, how tightly bound the protons
are. More mobile tissues have longer T2’s. This time does not depend
on the magnetic field strength.
o Dephasing represents a release of energy.
This dephasing is caused by spin-spin interactions; these are
made possible by magnetic inhomogeneities. This changes the
precessional frequency for different atoms, and hence they
begin to dephase.
Dephasing is also caused by magnetic inhomogeneities. Hence,
it is very important to keep the field as uniform as possible.
The T2 taking these into account is known as T2*.
T2 is shortest for materials with large, fixed molecules; slowest
for small, freely mobile fluids.
Return to equillibrium: T1
o After the 90 degree pulse eliminates Mz, it gradually begins to regrow
o This occurs because of interactions and energy exchange between the
proton spin and the surrounding tissue lattice, returning the atoms to
their (initial) lower energy state.
o This is the change in the longitudinal, not transverse, component of the
magnetic field. For after the pulse, all the magnetic moments are
knocked over; this is a higher energy state, so over time they go back
to the vertical.
To measure, apply a second 90 degree pulse and measure the
amplitude of the free induction decay. Different delay times
give different points on the T1 regrowth curve.
o These interactions are favoured if the vibrational modes of the material
overlap with the Larmor frequency. This happens with proteins and
lipids, and these thus have the shortest T1 times. Water and solids
have longer T1 times.
o The time of T1 depends on the strength of the magnetic field: larger
magnetic fields reduce its time.
o The characteristic time for this to happen is T1, and takes between
100-4000 ms, or 10 times longer than T2.
o Hence, small molecules have long T1 and long T2, medium molecules
have short T1 and T2, and large bound molecules have short T2 and
long T1.
Pulse sequences #{I know this stuff pretty well, but I should come back to it}
The spin density, T1 and T2 are characteristic of the tissue type, and
measuring these values is what gives information for constructing an image.
There are three main types of pulse sequence: spin echo, inversion recovery,
and gradient recalled echo.
o Pulse sequences are, more specifically, the series and shapes of 90 and
180 degree pulses.
o This is used to get spin density, T1, and T2 weighted images.
Spin echo
o Used to extract T2 (wanted) from T2*.
o Apply a 90 degree pulse; all the magnetic moments are transverse and
in phase.
o From both intrinsic causes and from inhomogeneities, the moments
start to dephase.
o Next, apply a 180 degree pulse. The intrinsic dephasing will continue,
but the inhomogeneities will be in the opposite direction, and the pulse
will be ressurrected.
o Repeat this 180 degree pulse multiple times (with the echo time
interval, TE), and the curve on top of the peaks represents the actual
T2.
o After a certain delay (repetition time, TR), the whole procedure is
repeated. However, the second free induction decay will be less than
the first one because not all magnetic moments will have returned
before the 90 degree pulse is delivered.
The amount by which the second FID is less depends on how
saturated the tissue is—that is, how much of the magnetic field
hasn’t returned to Mz. The longer T1, the greater the saturation.
Weighting
o Weighting comes from the fact that the observed signal is
o S=*f*(1-e-TR/t)e-TE/t, where rho is the proton spin density, f is a factor
depending on flow, and t is the time. The nature of this is that T1 can
be increased/decreased by shortening/lengthening TR, while T2 can be
increased/decreased by lengthening/shortening TE. Hence:
o T1 weighting
Emphasises T1 over T2 and spin density.
Done by presenting the 90 degree pulses quickly together; this
maximises the differences in recovery.
Also, the 180 degree pulses are done quickly; this reduces the
T2.
This technique is best for showing fat.
o Spin density weighting
De-emphasise T1 by using a long TR; de-emphasise T2 by
using a short TE. What’s left is the spin density.
This technique shows water the most clearly, since water has a
high proton density (compared to fat).
o T2 weighting
T1 is de-emphasised by using a long TR
T2 is emphasised by using a long TE
Tissue contrast is similar to the reverse of T1 weighted images
Inversion recovery
o This emphasises T1 by extending it by a factor of two.
o Start with a 180 degree pulse, then a 90, then another 180. This
doubles the time for TR. The time between the 180 and 90 degree
pulses is called inversion time (TI).
o FLAIR and STIR are inversion recovery techniques that suppress
certain types of tissue. When the recovery is at zero, applying a 90
degree pulse will have no effect. Since tissues have different recovery
times, applying a pulse then will suppress tissues which have reached
zero recovery length.
This is called the “bounce point”.
o When the inversion time is short, the technique cancels out fat; when
the inversion time is long, it cancels out fluid. This is because fat has a
short recovery time and fluid has a long recovery time.
Gradient echo
o Instead of a 180 degree pulse to rephase, as in spin echo, gradient echo
uses a magnetic field gradient reversal to rephase spins. This
technique is mostly determined by T2*.
Magnetic resonance
Gradient coils are used to superimpose a magnetic field on the main magnetic
field; since electromagnets, the field strength can easily be varied.
o Key properties are the peak strength of the gradients, usually mT/m,
and the time required to achieve that peak strength.
Three gradients are applied: the slice select gradient, the frequency encode
gradient, and last but not least, the phase encode gradient.
o Magnetic fields can be converted to Hz by multiply by the
gyromagnetic ratio, which is 42.58 MHz/T for the proton. Hence,
gradients can be measured in terms of Hz/cm.
Slice select gradient
o The slice in the z direction is determined by the RF pulse and the
magnetic field gradient.
o The thickness of the slice is determined by the strength of the gradient
and the bandwidth of the RF pulse.
o A sinc-function RF pulse is used to excite the protons; a perfect sinc
function would produce a perfect rectangular pulse.
o A wider sinc function produces a narrower slice.
o A rephasing gradient has to be applied of opposite sign and ½ the area
of the original in order to rephase the spins.
Phase encode gradient
o Another gradient is applied in a transverse direction (say y). This
changes the precessional frequency. This gradient is then switched off,
and the protons return to the Larmor frequency, but each one has now
been phase-shifted.
o This is repeated once per pulse, or 256-512 times during each line of
image acquisition.
Frequency encode gradient
o Another gradient is applied in a direction orthogonal to the slice-select
gradient; for example, the x direction. This occurs after the pulse has
been applied, and during data recording.
o The precessional frequency of the protons is changed slightly as a
result of this gradient.
o The signal is demodulated by removing the Larmor frequency from all
the responses, leaving the gradient effect behind, which ranges from 0
at the centre of the system to ± f at the extremities.
o Position is then determined by Fourier transform.
Frequency encoding
o MR data is stored in the frequency domain or k-space, with phase
information in the y frequency direction and frequency-encode
information in the x frequency direction.
o An image can then be recovered by 2D Fourier transform
MR procedure:
o The patient is placed in the magnetic field.
o A slice select gradient is turned on.
o A 90 degree RF pulse is applied, turning the z magnetic moments into
transverse magnetic moments; only protons in the selected slice are
excited.
o During recovery, the phase encode gradient is applied.
o A 180 degree pulse is applied to start rephasing.
o During the signal readout, the frequency encode gradient is applied, so
each decay has its own x-dependent frequency.
o More 180 degree pulses are applied to measure the T2 time.
General notes
# Limiting factors in spatial resolution for all imaging modalities:
o Gamma camera: collimator
o PET: positron emission and detectors
o X-ray CT: focal spot size, detector size
o MR: magnetic field gradient
o Ultrasound: pulse length/frequency
Brendan’s questions
How does dose vary with mAs?
o Dose increases linearly with mAs because the number (but not the
quality) of the x-rays increases linearly with mAs.
How does dose vary with kV?
o If all other parameters are fixed, increasing kV increases both the tube
current and the x-ray energy. Hence dose goes roughly as kV2.5.
Which has greater spatial resolution, CT or general radiography, how
measured?
o General radiography has better spatial resolution, i.e. it can resolve
smaller structures. Typical digital radiography spatial frequency is 5
line pairs/mm compared to 1 line pair/mm for CT. Main difference is
from detectors: CT maximises signal to noise ratio, at the expense of
resolution.
o Measured using the point-spread or line-spread function, the Fourier
transform of which is the modulation transfer function.
For CT how does SNR change with dose?
o Assuming a perfect Poisson distribution, SNR increases as the square
root of dose.
How does spatial resolution change with slice width?
o Spatial resolution obviously becomes worse with increasing slice width.
Obviously it reduces resolution in the caudal-cranial axis, it will blur
all objects that do not run exactly perpendicular to the slice.
What does magnification do to dose and image quality for fluoroscopy and
general radiography?
o Magnification typically increases dose because the same intensity of
radiation is used for a longer exposure time. Skin exposure is also
greatly increased.
o The change in image quality depends on the size of the focal spot. For
general radiography, the resolution can either increase or decrease,
depending on the size of the focal spot. Very small focal spots
(detector-resolution limited), the resolution will actually increase.
Magnification in fluoroscopy is achieved by changing the voltage of
the electrodes, resulting in improved image quality (but less field of
view).
What are the factors contributing to noise in general radiography and do these
change with digital systems?
o The random nature of x-ray attenuation and scintillator crystal output
produce much of the noise in the image.
Past exam questions
Transmission based attenuation in PET
o Because both photons have to travel through the entire patient
thickness, one can make a transmission measurement of attenuation
through the patient by placing a source on one side and a detector on
the other. Even though attenuation can only be measured along the
total path length, this is all that’s required.
Ideal properties of a SPECT scintillator
o Quite similar, actually—but ideal density is lower.
Discuss how a dedicated mammography unit differs from a general
radiographic unit.
o Main issues: low attenuation differences and need high resolution.
Hence, use different anode and kVp; use mostly characteristic x-rays
not bremsstrahlung.
o Very small focal spots are used to maximise resolution.
o To reduce overlap and improve uniformity, vigorous compression of
the breast is used.
o AEC is located underneath the cassette, instead of on top.
o Use an antiscatter grid underneath breast.
MR signal to noise ratio
o Determined by:
Intrinsic signal, based on T1, T2, and spin density
Voxel size, larger is linearly better
RF pulse, narrower bandwidth provides square-root better SNR
Magnetic field strength, larger is linearly+ better
Reconstruction algorithm.
Describe and discuss:
o Q factor is the frequency/bandwidth of the signal. Higher-damped
signals have a lower Q factor. although low bandwidth is desirable, so
is a short signal, and so a tradeoff must be reached.
o Pulse length is wavelength*number of cycles.
o Duplex scanning is a combination of 2D B-mode ultrasound and
pulsed Doppler ultrasound. This is useful to get spatial orientation.
Axial and lateral resolution
o Axial resolution is primarily determined by pulse length, so R=PL/2.
The pulse length is determined by the frequency, speed of sound, and
the number of cycles.
o The lateral resolution is approximately half the axial resolution;
however, it varies with depth. It is best at the near/far field interface.
It is determined by acoustic focusing, the width of the excited detector
array, the frequency. Lateral frequency can be improved by using only
data collected from the in-focus part of the beam near the near/far
interface; this degrades temporal resolution however.
Contrast agents
o Use microbubbles because of their high change in impedance, and
hence very high reflectance. In addition to B-mode, harmonic
techniques can be used and the time delays from bubble annihilation
can be used to gather additional information.
Describe CW and pulsed operation.
o In continous wave operation, a transducer continously puts out a US
signal; by its side, a receiver continously picks it up. The overlapping
volume defines the volume being observed.
o This is a Doppler technique.
o A signal from the transducer is sent back to the receiver; this is used to
demodulate the signal, and from that the Doppler shift can be extracted.
o Phase information is lost.
o This technique is a 1D technique, it is not used for imaging.
o In pulsed mode, the same receiver is used for both, as in normal
ultrasound. However, the pulse length is longer. After each pulse, the
phase shift is measured; the combination of multiple phase shifts can
be used to determine the frequency shift.
o This method can determine whether blood flow is oncoming or
offcoming, although if aliasing occurs because the frequency shift is
higher than half the pulse repitition frequency, (PRF), the velocity sign
will be reversed.
Ultrasound questions
A phased array transducer operates by activating all its elements
simultaneously, but with a time delay. By Huygen’s principle, the time delay
produces an advancing wavefront of non-perpendicular direction, and
destructive interference focuses the beam. Thus the beam can be both focused
and directed by changing the time delays to each of the transducer elements.