Case study cover sheet - New Zealand Association of Hand Therapists
advertisement

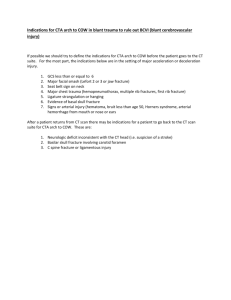
Case study cover sheet Name: Theresa Vaughan Please Note: This electronic version of the casestudy is not the complete hard copy that was sent in for marking as some appendices are missing. Details of problem Date of injury: 08/03/05 Date of surgery: 08/03/05 Admission: 08/03/05 Discharged: 11/03/05 (from Ward) This crush injury was sustained at work when the right little finger was caught in a pipe bending machine. Involved /damaged structures Right hand, little finger sustained a severe crush injury. The proximal phalanx fracture was comminuted and intra-articular at the PIP joint. The proximal interphalangeal joint was dislocated. The distal phalanx sustained a tuft fracture. The volar skin was split longitudinally from the tip of finger to just proximal to the metacarpophalangeal joint. Tendons and bone were exposed. The ulnar neurovascular bundle was considered stretched. Medical/Surgical intervention 08/03/05 -Surgery Open reduction and internal fixation of fracture dislocation. The distal intercondylar (intra-articular) fracture was fixed with a lag screw while the comminuted proximal phalanx shaft fracture was fixed with a circlage wire loop fixation. The volar plate of the proximal interphalangeal joint was repaired. The wound was explored and washed out. The radial neurovascular bundle was sighted and intact while the ulnar neurovascular bundle was noted to have been stretched. The viability of the skin of the fingertip was in question. Post operative management Post operatively the patient was sent back to the ward and instructions were to elevate the hand and intravenous antibiotics and analgesia was administered. It was requested that the dressings were down the following morning for the wound to be checked. He remained in hospital for 2 more days for wound observation. The patient was discharged with a hand based splint for the little finger of the right hand. The MCP joint was splinted in flexion and the IP joints in optimal extension. Bandages were bulky at this stage and it was not possible to achieve full extension due to this and the significant oedema, and soft tissue damage. Considering that the volar plate had been repaired, extension had to be addressed cautiously not to cause damage to this repair. Initial instruction was for passive motion of the MCP joint only with elevation and splinting full time. This instruction was changed by the consultant after the 1 patient had left the ward and a message was then left with a family member for the patient to only wear splint at night while actively mobilising during the day. (this was prior to formal hand therapy referral) Post discharge follow-up was a Hand Clinic review on 14/03/05. Oral antibiotics and pain medications were prescribed on discharge. Social and vocational history Mr. A is a 35 year old factory worker who is right dominant. He has a wife and 2 young children one of whom is in primary school. He has lived in New Zealand for the past 12 months and although he was a secondary teacher he is now employed as a factory worker. He was fluent in English and there appeared not to be any aspects of his culture that hindered treatment. He did tend to under report the level of pain experienced as he was keen to please, but this was easily discussed with him. His wife is home with their children and he is therefore the breadwinner. He enjoys sport and had played club cricket rugby and volley ball since he has been in NZ. He also assists with cooking family meals. His main aim was to regain function for return to work. The accident has however encouraged his thoughts to convert his teaching qualification to enable him to teach in New Zealand and he now plans to do this next year. He is a non smoker and does not drink alcohol. Biomechanical and wound healing implications Although this fracture was surgically fixed with a lag screw and interosseous wire, there was concern regarding the stability of the comminuted fracture and therefore differing opinions as to whether to mobilise early considering the extensive soft tissue damage. One opinion was to immobilise the finger until fracture stability had been achieved to avoid long-term problems of non-union. Others thought however that considering the extensive soft tissue damage that early mobilisation was essential. The intra-articular fracture was stable and adequately fixed and not of concern, but the comminuted fracture of the proximal phalanx shaft was showing signs of having shifted on x-ray at first follow up appointment in Hand Clinic. Significant soft tissue damage caused extensive oedema and blood supply was compromised. This contributed to a slow healing wound with extensive scar tissue forming, leading to poor glide of tissues. A superficial infection at one week after the surgery further slowed the healing and rehabilitation. Stitches were removed early due to the infection and the wound had to heal by secondary intention. Dressings were done by dressing clinic twice a week and a non-stick dressing was used. Functional and psycho-social implications Mr. A. remained well motivated to return to work and as he was involved in a manual labour job it was essential for him to regain optimal grip strength and range of motion to perform his job safely using all previously operated machines. Although greatly concerned about the injury and whether he in fact would loose his finger, he remained cooperative throughout rehabilitation. He showed good insight and understanding of his injury and the rehabilitation process. 2 Medical History: Mr. A. keeps good health. He had however sustained an injury to his little finger on his left hand when he was 6 years old and has no flexor digitorum profundus function in that little finger. Details of assessment 14.03.05 Subjective: The patient was seen on the first two occasions at the Hand Clinic with the surgeon. This and the first therapy session assessment will be included in this section. Wound - The right little finger had a longitudinal wound for the length of the finger extending 1 cm proximal to the metacarpophalangeal joint crease. The distal ulnar sided skin looked dull and black in colour and appeared vascularily compromised. The wound was superficially infected and sutures were removed early on this occasion. The wound was cleaned by dressing clinic nursing staff and redressed with a non stick dressing. It was not sufficiently healed to make formal range of motion assessment appropriate at this point. The patient remained on oral antibiotics. Fracture - X-Rays showed the distal intra-articular fracture of the proximal phalanx to be well reduced and stable. The more proximal comminuted fracture of the proximal phalanx was not adequately stable and there was concern that this needed to be given time to become stable prior to starting a mobilisation programme. He was instructed not to mobilise but remain in the hand based resting splint full time for 3 weeks post surgery to allow for wound and bone healing to take place. This was a change from initial instructions to mobilise. The distal phalanx tuft fracture did not present any concern and was immobilised in the same splint. Oedema - The finger was grossly swollen (about twice the size of the left little finger). No measurements were taken as the wound was open and infected. Joint range – the right little finger proximal interphalangeal joint (PIPJ) was resting in about 30 degrees flexion. This was due to the oedema. Bulky bandages required at this stage further prevented splinting to achieve an ideal position of extension and considering the volar plate repair full extension at this point would not be appropriate. Treatment - The patient was given instructions to continue elevation and active motion of the unaffected fingers to facilitate oedema reduction. A light coplus compression bandage was used to provide light compression as to not compromise wound healing. He was educated with regard to his injury. He was also instructed to continue to maintain ROM in unaffected fingers and thumb. The splint was checked and minor modifications were made in an attempt to achieve an improved position of the interphalangeal (IP) joints. It was noted that the unaffected fingers had good range of motion and minimal oedema despite the severe injury to the little finger. No further therapy was planned until Hand Clinic review in 2 weeks. 21.03.05 Hand clinic review with surgeon. The wound was observed to be improving with no further signs of infection or skin loss. Oedema appeared to be slowly reducing. Instructions by the surgeon were to start mobilising in one more week. A further review 3 by surgeons was planned for 2 weeks time and the patient was to continue dressing clinic appointments for wound care. No therapy intervention on this occasion. 30.03.05(first out patient therapy visit) Subjective: Sensory function - was not assessed formally due to wound but patient did report numbness of the ulnar aspect of the finger at this time. Wound/scar - the patient still required dressing changes at dressing clinic as the wound needed soaking and debridement of dead skin. The proximal end of the wound was healed proximal to the metacarpophalangeal joint. It was rigid red and raised (1mm). The distal wound required dressings. Pain - The patient did report discomfort over the fracture site with motion unless the fracture site was supported but it was not a major concern. He was not taking any pain medication at this point. Splinting – splint needed altering to improve fit due to oedema reduction. Objective: Range of motion MCP joint 0 – 65 PIP joint 30 – 50 DIP joint 0 – 25 Uninvolved fingers and thumb – he had full range of motion. Oedema – circumferential measurements Middle phalanx 86mm Proximal phalanx 95mm Oedema was predominantly located in the little finger and did not cause any limitation in function of the unaffected fingers and thumb. Scar – A modified Vancouver scale was used for scar assessment (see appendix 2) Pliability (P) – 4; Height (H) – 1; Vascularity (V) – 3. Treatment goals Long term goals: 1. To return to work performing the same tasks. (12 weeks) 2. To achieve optimal grip strength and hand function. (10 weeks) 3. To return to playing sport. (12 weeks) Short term goals: 1. To facilitate wound and fracture healing. (3 – 6 weeks ) 2. To decrease oedema of the right little finger. ( 2 weeks) 3. To increase joint range in all joints of the right little finger. (8 weeks) 4. To maintain joint range in all unaffected joints of the right hand. (1 – 2 weeks) 5. To decrease the development of severe scarring and facilitate prompt scar resolution. (3 – 12 weeks and longer as necessary) 6. To facilitate tendon and soft tissue glide. (4 – 8 weeks) 7. To provide education concerning limited sensory function. (2 weeks, ongoing input as functional use increases). 4 Intervention 30.03.04 Subjective& Objective: as per initial assessment Treatment: Wound/oedema - Wounds redressed by dressing clinic and coplus applied for oedema control. Continue elevating hand and actively mobilising unaffected fingers and thumb. Splinting - The hand based resting splint was remoulded for fit and was to be worn at night and between exercise sessions. Exercise - Active blocked flexion and extension exercise at both PIP joint and DIP joint starting with 5 repetitions and increasing this as pain and oedema allows. Active MCP joint flexion and extension exercise. The fracture was manually supported for all exercise. The patient was provided with education so as to enable him to judge when he was aggravating the oedema. He was to support fracture while doing exercise as he did still experience discomfort at the fracture site but the surgeon had requested mobilisation without splinting. Exercise was to be performed every 2 hours. Sensory function - The patient was provided with education and precautions as for avoiding injury to the ulnar aspect of his right little finger although the dressings and splint did provide protection at this time. Plan: Review at Hand Clinic on 04.04.05. Discuss with surgeon the use of a splint to support the fracture site circumferentially, immobilise the MCP joint in flexion and allow IP joint motion, as and alternative to the above mentioned hand based resting splint. This was considered as the fracture did not appear to be clinically stable considering patient discomfort with exercise. This would only be possible once the wound was adequately healed and minimal dressings were needed. 04.04.05 Subjective: Review at Hand Clinic, discussed possibly providing splint to support fracture site but this not thought to be necessary by Surgeons. The hand based resting splint was to be worn at night and between exercises. Instructions to continue mobilising as before were given. The proximal half of the wound was now healed and the distal half required only light dressings. No measurements were taken at Hand Clinic. Treatment: Splinting – Hand based resting splint to be worn during the day between exercises. For night wear a finger based volar gutter splint, with dorsal component over the proximal phalanx was made (Appendix 4). It included the MCP joint and was to place IP joints in optimal extension providing gentle pressure over the dorsal aspect of the proximal phalanx to facilitate progress into extension. It was now nearly 4 weeks post surgery and the volar plate was now considered to be adequately healed to tolerate more specific splinting into extension therefore the change of night splint. Exercise - Continue active MCP joint flexion and extension. Continue active blocked flexion and extension exercise of PIP and DIP joints. Hook fist exercise was started. The 5 fracture site was to be supported with the other hand while exercising. Passive DIP joint stretches were started during therapy sessions with middle phalanx well supported as to not stress the proximal phalanx fracture. The tuft fracture appeared clinically well healed and no discomfort was experienced related to this. Scar management/oedema management - Scar massage and the use of digi sleeves were started. For wear during the day and night. Oedema – digisleeves provided for day and night wear. Remove for exercise. Gentle retrograde massage avoiding wound damage was started. Plan: Hand Therapy appointment later this week. 07.04.05 (4 weeks) Subjective: The patient still reports significant pain over the fracture site which limits his ability to exercise. While the fracture is provided with manual support dorsally he is able to move pain free. This is however difficult to maintain. Objective: Oedema - Circumferential measurements Middle phalanx 81mm Proximal phalanx 95mm Range of Motion MCP joint 0 – 70 PIP joint 20 – 55 DIP joint 6 – 30 Wound /scar - Now small scab areas distally. No dressings needed. Scar raised red and rigid. (Vancouver scale – P- 4; H-1; V-3) Analysis: As the patient is still reporting significant pain when mobilising it was assumed that the fracture is not adequately stable to allow for bone healing. As the decision had been made by the surgeons to mobilise due to fear that the extensive soft tissue damage can no longer tolerate immobilisation it was decided to provide a splint to support the fracture site for exercise and to facilitate IP joint flexion and extension while immobilising the more mobile and uninjured MCP joint. Treatment: Splint - Continue night extension splint. Discontinue hand based resting splint during the day. A day splint was made to support the fracture while exercising and for light functional use. The splint immobilised the MCP joint in 20 degrees flexion and allowed full PIP joint flexion and extension. The splint was hand based and allowed PIP joint and DIP joint motion without discomfort as it provided circumferential support over the proximal phalanx. It also prevented hyperextension at the MCP joint of the little finger which allowed for improved tendon gliding at the IP joints. Oedema - Digi sleeves day and night. Remove for exercise and massage. Wound/scar - Use silpos sleeve for 3 one hour periods a day and gradually increase this as new scar tissue is able to tolerate this. Avoid skin breakdown. Wear digisleeves at all 6 other times. Use cica care gel on proximal end of scar in the distal palm area. Use day and night when possible. Massage scar 3 or more times a day to facilitate softening of scar. Exercise - Continue as before. Plan: Review next week. 11.04.05 Subjective: Patient still concerned about fracture site discomfort but this is only evident out of splint and he has therefore been maintaining the splint at all times. Objective: Oedema - circumferential Middle phalanx 76mm Proximal phalanx 92mm Range of Motion MCPJ 0-70 PIPJ 20-55 DIPJ 6-35plus Measured with proximal phalanx supported, therefore MCP joint immobilised and blocked when PIP joint and DIP joint motion is measured. Analysis: Small improvements in range of motion at the DIP joint and good improvement in oedema reduction were evident. Treatment: as before. Plan: Review later this week. 13.04.05 Subjective: Small areas of superficial breakdown over distal scar were present, caused by silpos sleeve. Objective: Oedema – circumferential measurements Middle phalanx 76mm Proximal phalanx 92mm Range of motion PIPJ 15-50 DIPJ 6-40 Wound/scar - Small area of breakdown was present on distal scar. The proximal scar is slowly flattening, but is still rigid and red. Vancouver scale – P-3; H-1; V-2. Analysis: Minimal improvements were evident over past week, but no concerns as there is no evidence of increased inflammation and pain. 7 Treatment: Exercise as before & start place and hold exercise of DIP joint in an attempt to improve FDP(flexor digitorum profundus) glide. Oedema - Modify digi sleeve to include the hand as both scarring and oedema over the volar aspect of the MCPJ is very rigid and has improved minimally so far. To wear this modified mitt only at night as it is difficult to remove regularly for exercise. Use digisleeve during the day. Wound/scar - Hypafix dressings were used on small open areas. Wear digi sleeve only till healed and then start silpos sleeve for short periods during the day. Discontinue silpos sleeve until wound healed. Splinting - As before. Plan: Review at Hand Clinic with surgeons on Monday. 18.04.05(6weeks) Subjective: (seen inHand Clinic)X-Ray not showing healing. Plan to continue therapy with splint to support fracture. Repeat X-Ray in 2 weeks prior to surgeons review. Objective: Wound /scar Healed and flat but still pink and rigid. Vancouver scale – P-3; H -0/1; V-1 Range of motion PIPJ 15-60 DIPJ 6-40 Treatment: Exercise - As above Wound /Scar/Oedema - Use silpos(as tolerated) and digi sleeve during the day and continue modified mitt at night with cica care on proximal scar. Plan: Review in 1 week. 27.04.05(7weeks) Subjective: Patient reports poor sensation on ulnar aspect of little finger not improving. Objective: Oedema – circumferential measurements Middle phalanx 72mm Proximal phalanx 87mm Range of motion PIPJ 25-55 DIPJ 15-45(65 passive) Sensation - Semmes Weinstein monofilament (SWM) assessment (see appendix 3) was performed. The patient could only respond positive for the T6.65 filament and therefore had no protective sensation on the ulnar aspect of the right little finger. 8 Treatment: Exercise - as above Oedema / scar management – as above. Splinting – day splint adjusted for fit as oedema is decreasing. Sensory function – education re potential injury due to limited sensation again discussed. Patient also educated as to how nerves heal, potential outcomes and time frames. Plan: Review at Hand Clinic. 02.05.05(8weeks) Subjective: X-Ray showed no significant change and surgeons were cautiously optimistic about bone healing. Requested small ring splint instead of hand based splint to support fracture for a further 2 weeks and then to use splint only for exercise but to allow functional tasks unsupported. The patient was to return to work on light duties with the support of the splint. This splint allowed some MCP joint motion and therefore improved function. Objective: (composite flexion and extension measurements taken by surgeon) Range of motion PIPJ 30-56 DIPJ 15-40 DPC (distal palmer crease) - 4.5cm Oedema – circumferential measurements Middle phalanx 72mm Proximal phalanx 94mm Treatment: Small ring splint made as requested by surgeon. This splint provided circumferential support for the length of the proximal phalanx allowing motion at both the PIP joint and the MCP joint. It had a lateral velcro closure on the ulnar aspect which made allowances for an increase or a decrease in oedema and allowed the patient to fit splint firmly. This allowed the patient to perform exercise and functional task pain free. All other treatment as above. Plan: Therapy appointment later this week. 10.5.05 Subjective: Patient reports to being able to touch his palm passively if he supports the fracture site. Objective: Range of motion PIP joint 22 -70 DIP joint 10-42(55 passive) DPC - 4.5 cm Discomfort stops the patient from further motion when not supported by splint. Oedema - Circumferential measurements Middle phalanx 74mm Proximal phalanx 89mm 9 Sensory function - SWM assessment, now able to detect Q5.88 over volar ulnar aspect of little finger (a small improvement). Scar - Scar in palm now mobile and soft. The scars over proximal phalanx are still rigid and pink, but flat. Vancouver scale – P-1/2; H-0; V-1. Analysis: Slow progress with range of motion and oedema reduction has been made. A greater passive compared to active range of motion is present in both the IP joints, due to poor tendon glide and shortening of the proximal phalanx causing poor tendon function. The fracture site remains uncomfortable with motion if unsupported even though the surgeon has suggested weaning from splint. Splint use has therefore continued. Treatment: Exercise - Range of motion exercise as before. Gentle passive motion of the PIP joint was started as patient found this possible without pain at fracture site while supported in the splint. Splinting - Night splint, gentle static progressive splint with support over fracture site as before. Day splint – small ring splint over the proximal phalanx only allowing limited MCP joint flexion and IP joint flexion and extension. Oedema – Digisleeve, mitt and massage. Scar – massage and silpos sleeve during the day, cica care and mepiform with modified lycra mitt to keep contact media in place at night. Plan: Review at Hand Clinic. 16.05.05 Subjective: (10 weeks post op) Reviewed by surgeon but no repeat X-Ray. Patient to return to full-time work but remain on light duties as fracture is not considered stable. Clinically only minimal motion at fracture site but still significant discomfort on motion if unsupported. Continue splint as required. Plan: Continue exercise and splinting as before and allow soft tissue oedema and scar to settle before considering further surgery to possibly bone graft the mobile fracture and consider neurolysis of the ulnar digital nerve. Review in Hand Clinic in 4 weeks. Review in Hand therapy next week. 25.05.05 Subjective: The patient continues wearing ring splint at work but has tried not to wear it at home. He is however not able to play sport or do any heavy tasks without causing discomfort and therefore avoids this. 10 Objective: Range of motion PIP joint 20 – 85 DIP joint 10 - 60 (90 Passive) Oedema Middle phalanx 72mm Proximal phalanx 92mm Sensory assessment: SWM assessment – now able to detect N5.07 to level of DIP joint crease. Scar - No significant change. Analysis: Slow improvements are being made in all areas but fracture healing does not show any clinical changes. Treatment: As before. Altered night splint to improve extension. Plan: Review in one week. 01.06.05 Subjective: Patient reports no subjective change in fracture site discomfort. The patient is coping well at work while using the splint. He is able to operate all smaller machines but has not been able to return to operating larger machines which require heavy lifting. Objective: Range of motion PIP joint DIP joint Oedema Middle phalanx Proximal phalanx 20(10 passive) -80 10 – 60 70mm 87mm Analysis: Good improvement in oedema but no significant change in range of motion. Treatment: Oedema /scar management - New digisleeves provided. Continue massage and contact media as before. Exercise - As before. Plan: Review next week. 08.06.05 Subjective: Nil change. Objective: Range of motion PIP joint DIP joint 25(20 passive) – 78 0 -56 11 Oedema Middle phalanx 66mm Proximal phalanx 80mm Scar - now pale in colour and starting to break up in proximal phalanx area. Linear scar along volar aspect of finger tends to be tight and rope like when silpos sleeve is removed for long periods. When maintained it is flat but blanches on full passive extension. Vancouver scale – P-1; H-0; V-0/1. Treatment: Reinforce tendon gliding exercises. Continue all other exercise. Continue oedema and scar management as before. Plan: Review at Hand Clinic and question fracture healing as this does not appear to be improving. 13.06.05 Hand Clinic review by surgeon today. Decision was made to continue therapy as before and to review for possible surgery in one month. 15.06.05 Subjective: No problems. Patient remains at work full time in area where he works with smaller machines where heavy lifting is not required. Scar - slowly improving. Objective: Range of motion PIP joint 25-75(90 passive) DIP joint 0-50(70 passive) Oedema – circumferential measurements Middle phalanx 71mm Proximal phalanx 85mm Sensory function- K4.56 filament sensation is now present to the level of the DIP joint crease. Treatment: Continue exercise and oedema/scar management as before. Splinting – continue day and night splinting as before. Analysis: Some increase in oedema possibly due to increased use of hand at work as patient is trying to increase level of function. Clicking at fracture site also more evident today and patient therefore needs to remain protective of fracture at work. Changes in management with splinting or exercise are not possible to date as fracture remains clinically unstable. Main aims of treatment continue to be, maintaining optimal joint range, scar management and oedema resolution. Plan: Review in 2 weeks. 12 4.07.05 Subjective: Nil change. Objective: Range of motion PIP joint 20-80 DIP joint 10-60(80 passive) Oedema – circumferential measurements Middle phalanx 71 Proximal phalanx 83 Scar- significant softening of scar during past 2 weeks. Vancouver scale – P-1; H-0; V-0 for all but linear scar along the volar aspect of the length of the finger over proximal and middle phalanx. This scar remains tight and blanches on full stretch and appears rope like when no contact media has been in place for some hours. Treatment: As before. Plan: Hand Clinic review in 1 week to discuss surgical options. Therapy intervention has now reached a plateau and minimal change has been seen in the past month. 12.07.05 Seen by surgeon at Hand Clinic. X-Rays and clinical assessment was considered and although the patient still reports pain, it was decided that there was now adequate healing to work towards not using a splint. No further surgery was to be considered at this point and a further review by the surgeon was planned in 2 months time. Therapy intervention was planned only to supervise splint weaning, monitor sensory improvements and to continue to monitor scar which still impacts on PIP joint range if not treated. 4.08.05 (final therapy session for the purpose of case study) Subjective: Patient has not used splint at all for past 2 weeks after slowly decreasing splint wear since seen by surgeon. Pain still a problem if using hand unrestricted and he has taken pain relief twice in past week. He has now permanently shifted to an area in the factory where less heavy lifting is required and will not return to previous job due to the restrictions placed on him by his pain. He still finds that PIP joint contracture increases during the day but with the use of the static progressive splint and gel sleeve at night, the extension range is maintained. Objective: Range of Motion PIP joint 15 - 65 (80 when fracture site is supported) DIP joint 25 (0 passive) – 70 Oedema – circumferential measurements Middle Phalanx 67 Proximal Phalanx 83 Scar - The scar is flat but on full extension a linear band along the length of the finger blanches. All scars are soft and pliable now and have assumed a near normal colour. 13 Vancouver scale - P-1; H-0; V-0. Sensory function - Semmes-Weinstein monofilament assessment – Mr. A now has the 4.31 filament present 1cm distal to the DIP joint crease. This implies that he now has diminished protective sensation present on the ulnar aspect of his right little finger except for the distal tip which scores at T4.56. Grip strength - Right hand – 49 kg (left unaffected non dominant hand – 49 kg). The little finger on the right hand was not fully engaged for this test due to discomfort. Grip strength had not previously been measured due to continued discomfort at fracture site. It was felt to be information that would be useful for next surgical review. Analysis: Mr. A has now reached a point in rehabilitation where he has adapted to the limitations of his injury. Sensory function, although poor, has changed to a level of some protective sensation and this should still improve over the coming months although it will remain limited. On discussion with the surgeon there is no indication to intervene surgically as there is minimal chance of improving sensory function. Grip strength is now near normal without full use of little finger but pain remains a factor when he uses his hand totally unrestricted including the little finger in tasks such as heavy lifting and power grip. He has however made adjustments in how he uses his hand to avoid continually causing pain. This does however remain an issue to be addressed on his next visit with the surgeon. He has stopped playing sport due to pain and discomfort and still wishes to be able to do this in the future but does not presently feel able as he remains fearful of further injury. At work he has moved permanently to an area where limited heavy lifting is required. Treatment: Continue use of mineral gel sleeve at night with splint to ensure maintenance of extension at PIP joint. Continue functional use and exercise to maintain joint range and strength. Plan: Monthly follow up for another 2 months to monitor scar management and maintenance of range of motion is planned. It is hoped that all night splinting and gel use could possibly be discontinued by then. Feedback to the surgeons at next clinic follow up as to the continued pain at fracture site with full hand use, will be given. It is also my opinion that there has been minimal change clinically in the discomfort experienced at the fracture site over the past 2 months although this well motivated patient has adapted well to remain functional at work. As therapy has now become very infrequent it has been decided to discontinue further discussion of sessions for this case study. 14 Treatment rationales Wound healing/skin/scar Mr. A sustained a severe crush injury and tissue damage was therefore extensive. The extent of the oedema, vascular and nerve damage significantly slowed the natural healing process. Wound healing is described by Davidson (1998) as a succession of events leading to restored tissue function and architecture. He continues to say that this continuous process can be divided into discrete sets of overlapping cellular and biochemical events. Traditionally it has been divided into 3 phases. 1. Inflammatory phase: (day 0 - 3) This phase commences upon injury and lasts for at least 3 days and can persist for days or weeks especially in complex injuries (Stewart Pettengill, 2002). The first event in tissue injury is disruption of blood vessels, followed by a brief period of vasoconstriction and platelet degranulation. The clotting cascade follows and a fibrin clot is formed. Vasodialation follows in response to chemical mediators from damaged tissue. Tissue becomes red and hot and pain sets in due to chemicals released from dying cells. Swelling may be immediate due to extensive bleeding or may take a few hours to develop. Increased capillary permeability in response to the chemicals released by damaged cells causes this swelling. Activated platelets produce many growth factors. These are chemotactic and mitogenic for inflammatory cells such as neutrofils and monocytes, the latter transforming into macrophages. The inflammatory cells eliminate bacteria and debris from the wound by phagocytosis. Macrophages first appear 48 hours after injury and remain until wound healing is complete. They are important in sustaining the wound healing process. 2. Proliferative (fibroblastic) phase: (starts at 3 to 4 days – 4 weeks) Macrophages secrete cytokines and growth factors which attract fibroblasts and new blood vessels. The composite of fibroblasts, macrophages and new capillaries is known as granulation tissue. Fibroblasts soon outnumber other cells in the wound and collagen is being synthesised at a rapid rate, but the tensile strength of the wound still remains low. By the end of the 3rd week the size and collagen content of the wound stabilises, but collagen production continues to be active for many months. All tissues are bound together as the scar develops. 3. Remodeling phase (scar maturation): This may take from 3 weeks to 6 months at its most active and then continue for many more months at a reduced rate, (Stewart Pettengill, 2002). The extra cellular matrix is reorganised during this phase. All scars as they mature have to reach equilibrium between collagen synthesis and collagenolysis. Type 3 collagen is gradually replaced by type 1 collagen which is highly cross-linked and reoriented in response to mechanical stress. Overall cell numbers are reduced and so is vascularity. Initially the collagen is disorganized and thin, but it thickens and increases in strength and ultimately reaches 80% of the strength of normal skin. Newly formed scar shrinks in all directions and managing this becomes an important part of rehabilitation. In the proximal phalanx scar tissue tends to involve all of the structures within the zone of the injury. The scar tends to produce adherence between the bone and the adjacent tendons, joint capsule and ligaments especially when tendons remain dormant during fracture healing, (Freeland, 15 Hardy, Singletary, 2003). Many authors have reported that controlled stress (compression or tension) and motion influence collagen formation and organisation, increasing strength of healing tissues and decreasing adherence between adjacent tissues, (Stewart Pettengill, 2002). The exact mechanism of this is not fully known. Optimal wound healing is facilitated by good blood supply, moist wound environment, no infection, minimal disturbance, healthy diet and no smoking. In Mr. A’s case compromise of the vascular system at the time of the initial injury and infection slowed the wound healing and therefore the rehabilitation process. Mr. A’s severe crush injury caused extensive tissue damage and oedema. The vascular and nerve supply was stretched on the ulnar aspect of the finger. Vascular compromise and infection caused some distal skin loss ulnarly. Due to infection the stitches were removed early which further delayed wound healing. Complete wound healing was delayed for up to the 6th week. The progress through the stages of healing was therefore slow and significant oedema then persisted beyond that time which further slowed the achievement of good tendon glide. These delays would have increased the amount of scar tissue formed and the scar maturation process was delayed. Cyr & Ross (1998) suggests that it is important for the therapist to understand the effects of immobilisation on injured tissues and the importance of early controlled motion to prevent negative effects of immobilisation. A thorough understanding of the biomechanical, biochemical and physiological changes that occur is important to ensure that tissues are stressed in a beneficial manner and do not create further complications, (Cyr & Ross, 1998). Because of this Mr. A’s fracture was only immobilised for 3 weeks which was possibly to short for the extent of the bone damage. To further immobilise his finger considering the extent of the soft tissue damage was felt to be a bigger risk in terms of final outcome and function than the risk of possible non-union. Time frames for passive range of motion and splinting to increase joint range was delayed though due to slow bone healing. Bone healing/fracture fixation As in soft tissue healing, bone healing passes through the 3 basic healing phases. Fracture healing can however take place either by primary or secondary healing stages to produce bone. The type of healing that occurs depends on the type of fixation used. Fixation methods that provide a compressive force across the fracture site and stability allows for primary healing to take place as it eliminates the interfragmentary gap. Direct regrowth of bone across the fracture site is made possible and is known as primary fracture healing. When motion is minimised, but not eliminated, healing must go through a fibrous callus repair phase that is converted to bone. This is known as secondary fracture healing. For final fracture healing the immature bone produced by either method needs to remodel to allow support and load transmission, (LaStayo, Winters, Hardy, 2003). Primary healing: This type of healing only occurs in a mechanically imposed stable environment because of motionless fixation. The implants used for the fracture fixation serve as a substitute for external callus. The heamatoma that bled into the fracture site is eliminated by the 16 apposition of the fracture ends during reduction. Cutting cones, that move across the fracture site forming new haversian canals, are formed by osteoclasts in the intact bone. These cutting cones contain blood vessels that revascularise bone fragments as they cross the fracture site. Osteoblasts follow to fill the canals with new osteons, the single basic unit of bone that bridges the fracture site. The fibrous stage of primary healing generates new bone directly that unites the fracture. This immature bone is weak, non-stressorientated bone and the strength of the fracture depends on the implant. Static and cyclic loading of bone stimulates remodeling. Faster union in primary healing does not mean faster tensile strength development, but allows for early mobilisation (LaStayo, Winters, Hardy, 2003). Primary healing for Mr. A took place at the condylar intra-articular fracture of the proximal phalanx where lag screw fixation was used and a well aligned stable reduction was achieved. Healing at this fracture site progressed uneventfully allowing for early protected motion at the PIP joint with the achievement of good range of motion considering other complicating factors such as extensive soft tissue damage and the slow healing comminuted proximal phalanx shaft fracture. Secondary bone healing: This takes place when the fracture is reduced (e.g. closed fracture reduction) or when semi rigid fixation such as K-wires, intermedullary pins and external fixators are used. Fractures are aligned but not compressed and some obligatory motion occurs. Mr. A’s comminuted shaft fracture of the proximal phalanx was wired in an attempt to achieve reasonable fracture alignment and stability to facilitate secondary healing. Some shortening and angulation of the phalanx was present and further shift in the fracture fragments were evident when X-Rays were repeated at first follow up one week post surgery. Throughout the rehabilitation process, the adequacy of this fixation remained in question and bone healing was very slow. Although surgeons are optimistic that fracture healing has now taken place, this has taken significantly longer than would normally be expected as it is now 6 months post injury and some fracture site discomfort is still present. Krop (2002) suggests that comminuted fractures have a higher rate of delayed union as the result of damage to the blood supply of the bone due to higher energy levels imported in open comminuted fractures. This would definitely have been a factor in the delayed union for Mr. A. Stages of bone healing: 1. Inflammation (3 – 10days) This starts immediately after the fracture, initiating a cellular and vascular response. A heamatoma is initially formed to bridge the fracture site. Macrophages and neutrophils are the first cells to arrive, then mast cells and fibroblasts. The heamatoma is replaced with granulation tissue, rapid capillary growth and young connective tissue cells. Reestablishing sufficient blood supply is essential to healing. As suggested by LaStayo et.al. (2003), it must be considered that internal fixation methods may interrupt periosteal or medullary blood supply by 60 to 70%. The degree of movement at the fracture site also influences this process and excessive motion may prevent capillary formation across the fracture site. Symptoms during this phase are swelling and pain. 17 2. Repair - Soft callus (3 – 6weeks) Callus is formed to stabilise the fracture and to initiate the restoration of rigid laminar bone. A soft callus is formed as the original heamatoma is replaced by granulation tissue. A clinical union is present in 2 to 3 weeks. Under the influence of growth factor and mechanical loading the healing continues and a collar of soft callus develops around the fracture and connects the 2 fragments. Within this soft callus the bone and connective tissue are poorly organised and not aligned in a manner to resist excessive force. The fracture stabilises clinically and pain is significantly reduced. - Hard callus (6 – 12weeks) The fracture is now adequately stabilised and hard callus begins to form through endochondral ossification. Woven bone is formed and clinical and radiographic healing is achieved and is visible on X-Ray within 12 to 16 weeks, (LaStayo, Winters, Hardy, 2003). This stage of healing has not truly been achieved in the case of Mr. A as X-Ray results are still not convincing although surgeons are optimistic that some signs of healing are starting to be visible. This is a very late stage for healing not to be complete and rehabilitation has been greatly slowed by this slow proximal phalanx fracture healing. 3. Remodeling (12 – 52weeks) This is the phase where woven bone is converted to laminar bone. The medullary canal is reconstructed in this phase. The original bone strength and structure are restored over months to years by replacement and reorganisation of the repair tissue. Middle and proximal phalanx fractures have been shown to be most common in 10 – 29 year olds, caused by sports injuries. Work injuries are a more common cause in older patients (Purdy and Wilson, 2002). This was the case with Mr. A. Initial injury severity is the most highly correlated determinant of hand fracture outcome (Freeland, Hardy & Singletary 2003). Other factors are the close proximity of the flexor tendon to the injury, complex wounding, intra-articular fracture involvement, comminution, bone loss, and multiple hand fractures. Proximal phalanx fractures are also indirectly influenced by the interossei, whose vectors flex the proximal fragment and extend the distal one. This results in a volar apex angulation. This will cause laxity of the extensor tendon which in turn causes a decrease in the proximal interphalangeal joint extension and then a secondary PIP joint contracture. For every 1mm of extensor tendon redundancy a 12 degree extensor lag is caused and any additional extensor adhesion will further increase the lag (Purdy and Wilson, 2002). Phalangeal shortening resulting from bone compression, bone loss or comminution may further accentuate this problem. Persistent volar angulation of greater than 25 degrees will also progressively limit finger flexion, (Freeland, Hardy, Singletary, 2003). In worst case a pseudo claw deformity develops and further joint contracture may follow. The flexor sheath and extensor apparatus have a very intimate proximity with the proximal phalanx and adhesions are easily formed with any disturbance of the normal balance through injury. For Mr. A. shortening as well as angulation of the phalanx were factors that influenced outcome and tendon glide on both the extensor and flexor surfaces were limited by the soft tissue damage and was evident by the fact that passive motion was greater than active motion. Any fracture that is intraarticular must be reduced to restore accurately the articular surface. When this is achieved the primary goal should be to restore joint motion, as stated by Shrikant and Bing, (2003). 18 Any repair needs to aim to achieve restoration of anatomy in such a way as to allow for active IP joint motion with tendon gliding during healing. Standard x-rays are usually sufficient for evaluation of phalangeal shaft fractures. Lateral and anterioposterior views are essential and additional oblique views may be required. For Mr. A lateral and anterioposterior views were taken. “The need for biomechanical stability must be balanced with the need to preserve biological integrity and blood supply, while minimizing the risk of scaring.”(Freeland, Hardy, Singletary, 2003) Fracture fixation. Splints that are used to support and protect hand fractures can be finger, hand or forearm based depending on the injury and the extent of the oedema. Unstable fractures may need to be supported in a static splint for the first 4 weeks prior to starting the mobilisation programme. If these splints are hand based the MCP joints should be positioned in 50 – 70 degrees of flexion while the IP joints are supported in 0 – 15 degrees of flexion to minimize contracture risk (Freeland, Hardy and Singletary, 2003). This position also facilitates relaxation of the intrinsic muscles and therefore facilitates balance at the fracture site. Although Mr. A was internally fixated he was initially treated as an unstable fracture as the wiring was considered inadequate as there was evidence of movement of the fracture fragments at first hand clinic review within the first week post surgery. The period of immobilisation was somewhat short considering the fracture mobility as most text suggest at least 4 weeks of immobilisation to reach adequate stability for active exercise. This decision was made by surgeons due to the significant soft tissue damage. Open fractures presents 2 problems. The wound and the fracture. Fractures must be dealt with as is closed fractures using the same principals. The wound must be cleaned and closed or covered. Simple wounds can be dealt with easily and fractures fixed at the time of initial surgery. Complex wounds may need review 48 – 72 hours after initial surgery and reconstruction may only be done then. Bone grafts may be needed and the wound incision may need to be extended. If and when open fracture reduction and internal fixation are required the repaired digits are capable of and require more accelerated and intense mobilisation to optimise functional recovery, (Freeland, Hardy, Singletary, 2003). Secure fixation and early motion may help to reduce the risk of joint contractures and tendon adhesions in severe injuries. For Mr. A. surgery was one procedure within the first 24 hour period. Unfortunately fixation of the comminuted fracture was not as stable as hoped and this presented the ongoing difficulty. Compromise between early mobilisation for the soft tissue and immobilising the fracture for long enough to achieve fracture healing, remained an ongoing issue. “The fundamental purpose of internal fixation is to stabilize bone fragments in their correct position and alignment so that soft tissue repair and rehabilitation can proceed at the optimal pace to obtain maximal functional benefit.”(Jabaley, Wegener, 2003). Fracture fixation and interfragmentry compression minimizes the movement and bone necrosis and permits the migration of osteons across the fracture site. This is considered primary bone healing, bone healing without callus. In the hand this is a very useful aspect to healing as the absence of callus is most useful because of the close constraints of the 19 hand and fingers. It is helpful in the retention of movement in the joints and tendons by minimising scarring and ligament shortening, (Jabaley, Wegener, 2003). Timing of fracture fixation must always be considered in the context of the wound in which they occur. If the tissue viability is uncertain it may be that the wound is initially debrided and dressed. Further fixation of fracture and delayed primary wound closure may follow in a few days, (Jabaley, Wegener, 2003). The degree of fracture fixation needs to be adequate to allow rehabilitation without fracture motion and deformation. Commonly used implants for fracture fixation are interosseous wires, pins, screws, plates or a combination of these. Kirschner wires are commonly used but are not compressive and may loosen in time. They are however quick to insert and cheap. Screw fixation is commonly used for fracture fixation. Screws may be self tapping or they may require a tap when inserted. Predrilling is required for all screws. The lag screw principal is frequently employed when a screw is passed across a fracture line in such a way that its tightening compresses the fragments. To lag a screw successfully the fracture must be oblique to the long axis and the fracture should be at least 2 times the diameter of the bone. Two screws are commonly used for one fracture to achieve stability. Bone fixed with screws should tolerate immediate active motion, (Jabaley, Wegener, 2003). Screw fixation was used for stabilising the inter-articular proximal phalanx fracture for Mr. A. and a stable well aligned joint surface was achieved which allowed for early motion although this was limited by the lack of stability at the proximal phalanx shaft fracture. Interosseous wire fixation can also be used to fix fractures. It is applicable in transverse and short oblique fractures and is also used for arthrodesis. The surgeon may also choose to use K-wires in conjunction with interosseous wires. Wires were used to stabilise the comminuted proximal phalanx fracture for Mr. A. No K-wires were used. Plate fixation is more commonly used in fixing fractures in the metacarpals and indications for their use become less as one proceeds distally into the fingers. Plates may be applied dorsally or laterally but is rarely used volarly. To secure the plate firmly two screws are needed on either side of the fracture, (Jabaley, Wegener, 2003). LaStayo et.al. (2003) states that: “The reality of fracture management is that it is clinically irrelevant whether the bones unite by primary healing or secondary callus. What is essential, however, is (1) whether or not the bone heals in a stable, well-aligned fashion, (2) how well the soft tissues glide, and (3) how the extremity functions after it is healed.” He also suggests that when multiple tissues are involved in the injury, the weakest tissue repair or method of fixation often dictates the treatment progression. This was so in Mr. A’s case as progress continued to be slowed by the inadequate wire fixation of the proximal phalanx shaft fracture. 20 Nerve healing If a nerve is contused, incompletely transected or not repaired under tension, little or no immobilisation is needed. If transected and repaired, the nerve should be protected from excessive stress for 3 weeks and splints usually immobilise the joint above and below the sight of the injury, (Stewart Pettengill, 2003). Protected early mobilisation of the contused nerve may help to restore nerve gliding and prevent constriction and traction by scar adhesions. In an end-to-end repair exact approximation is impossible and some function will be lost. The nerve will, after a 3 to 4 week latent period start growing 1 to 3mm per day, (Stewart Pettengill, 2003). In a crush injury the regeneration of the nerve is more rapid but still slow and dependent on how much scar tissue is interfering with the nerve function, and functional return may be unpredictable. Mr. A’s nerve recovery was very slow and to date it would seem that significant permanent damage was done at the time of the injury to the ulnar digital nerve of the little finger. According to Sunderland’s classification of nerve injuries he would have possibly had a type 3 injury where the epineurium is intact but significant fibrosis and scarring is present. When first tested using Semmes-Weinstein monofilament assessment he only registered the thickest filament and although there has been some change he now has only limited protective sensation 6 months after the injury. As Wheen (2003) suggests a patient should have at least diminished protective sensation present to commence sensory re-education. Sensory re-education was not part of his rehabilitation programme as he was already involved in full time work by the time he gained adequate sensory function to consider re-education. As he was coping well functionally there did not appear to be any reason to consider this now. No hypersensitivity was experienced by the patient and therefore only education concerning the nerve injury and the predisposition to injury was considered part of the treatment programme. Future management of this nerve injury may include a neurolysis if further surgery is required for problems at the fracture site. This is not presently being considered by the surgeon. Oedema When the capillaries and the lymphatics are injured as the result of trauma or surgery oedema is created, (Sorenson, 1989). Initially there is vasodilation in the area of injury, thrombosis of damaged vessels and contraction of the muscular vessels. In the immediate area of the wound protein rich fluid called exudate leaks out of the injured capillaries. This results in a fluid shift that renders the injured area oedematous and creates a condition of vascular insufficiency. The local lymphatic system is also occluded by fibrin plugs formed from escaping plasma proteins. Sorenson (1989) states that: “Although oedema is a pathological condition of tissue fluid it is a normal response to trauma.” Oedema is a protein-rich fluid that carries the chemical mediators of lysis and synthesis of new connective tissue. After an injury it is rich in fibrocytes, producing fibrous tissue which heals the connective tissue. This same fibrous tissue can also form adhesions that constrict and contract and therefore limits the full excursion of the capsule, ligaments and tendons. Oedema may cause irreversible stiffness if not treated and as in the case of this severe crush injury, the result of significant oedema is partially unavoidable. This was the 21 case for Mr. A as the crush injury was severe and the damage to all tissues including the vascular and lymphatic system was significant. Wound healing was initially of primary concern and initially extensive oedema was addressed by elevation and light compression as the wound allowed. Mobile loose skin on the dorsum of the hand and digits make it an ideal place for fluid to collect. Oedema draws tissues into predictable patterns of deformity. The position is one which allows for the most volume effusion and at the PIP joint this will posture the joint at 30 to 40 degrees of flexion, (Freeland et.al., 2003) In the case of Mr. A the oedema was primarily present in the injured digit and therefore the PIP joint which did posture in flexion. Due to the extensive wound and mobile fracture attempts to correct this was difficult with splinting and oedema control measures, as the wound remained the priority in the early weeks. Elevation was the primary treatment used. All anatomical structures in the digit were damaged by the severe crush injury and oedema therefore influenced the healing process significantly for Mr. A. Joints: Capsular and ligament fibrosis cause joint contracture. At the PIP joint flexion contracture is most common and is caused mainly by contracture of the volar plate, check rein ligament, collateral ligaments, and secondary capsule and adjacent connective tissue adhesions. Tendons: Motion may be limited by restricted tendon glide of the flexor or extensor tendons. Adhesions at the pulleys or bifurcation of the FDS, FDS adhesion to FDP, tendon adhesion to bone or adjacent connective tissue may all contribute to limited tendon function. Loss of tendon glide was evident for Mr. A as he has remained able to achieve better passive range of motion compared to active motion through most of his rehabilitation. Skin: Skin contractures caused by thick scarring caused by slow healing will limit motion. In this case the skin scar was primarily volar and for the full length of the digit and therefore contributed to the PIP joint flexion contracture. Some skin scarring dorsally over the proximal phalanx fracture site also caused limitations in the extensor tendon glide. Early oedema control is therefore essential in crush injuries to limit the extent of the stiffness caused by oedema if not resolved. Excessive oedema can be the prime cause of excessive scar tissue and adhesion formation. Elevation, compression, massage and active motion are the primary means of aiding the venous and lymphatic drainage. Elevation of the limb above the level of the heart allows for passive drainage of fluid from the injured hand in the early phase of relative immobility. Gentle compression using coplus and later lycra digisleeves assisted the lymphatic and venous systems by increasing hydrostatic pressure and therefore facilitating lymphatic and venous flow. It also provides the support needed to avoid gains in oedema reduction to be lost. Early active motion may initially only include the unaffected joints, as was the case for Mr. A, and when there is no contraindications, the injured joints are also involved, (Sorenson, 1989). Splinting the hand in the safe position where the joint, ligament and capsular structures are placed in a lengthened position as to limit contracture formation is also 22 essential. This provides the hand the rest needed between exercises to not lengthen the inflammatory process already present in the initial healing phase. The rest between exercises in a safe position was essential for Mr. A as oedema was present for many weeks and great caution was taken not to lengthen the inflammatory process. Regular assessment of oedema is important to measure changes in the amount of oedema present and therefore the effect of treatment. It can be measured by using the volumeter (measures water displacement) or by circumferential measurements of each digit with a flexible tape measure or a circumferential gauge, (Sorenson, 1989). Measurements need to be taken at the same place on the digit each time and preferably also by the same therapist. As Mr. A’s wound was present for some weeks we used circumferential measures throughout the rehabilitation. Splinting Hand therapists have to carefully manage soft tissue to control and diminish scar formation optimally. Many therapeutic modalities are used and may temporarily alter soft tissue length but splinting is the only available therapeutic modality that applies controlled gentle forces to soft tissues for a sufficient length of time to induce tissue remodeling without causing detrimental microscopic disruption of cellular structures, (Fess and McCollum, 1998). Static splinting: In fracture management static splints to protect fractures until stable are commonly used. Splints that totally immobilise the digit are indicated only for fractures that remain unstable, (Freeland et.al., 2003). During the inflammatory and early fibroblastic stages of healing splints are used to immobilise to promote healing or, in special circumstances to provide both protection and specific motion parameters for early passive or early active motion programmes, (Fess and McCollum, 1998). Depending on the injury some limited motion may be implemented to allow for appropriate soft tissue remodeling to minimise long-term limits in function due to scarring. During the first month of treatment Mr. A. was supported in a volar hand based resting splint which aimed to achieve the safe position. The splint also provided the wound and fracture with support that prevented motion of the injured part of the hand during the initial inflammatory phase and therefore facilitated healing. The safe position refers to the MCP joints being flexed to between 50 and 70 degrees (Freeland, et. al., 2003) to prevent the collateral ligaments from becoming shortened and therefore causing extension contractures at this joint. The IP joints were splinted in optimal extension to prevent/minimize flexion contractures at these joints. Initial gross oedema caused the extended position not to be achieved while in the resting splint. Bulky bandaging and the extensive soft tissue damage (vascularity was compromised) caused exact positioning to remain a challenge. Static splinting for support and protection remained the only splinting option during the first weeks after this injury as any other forms of splinting would have interfered with wound healing and vascular supply. It also provided the fracture time for healing in an attempt to avoid non-union. Splints can be used to facilitate the required movements to prevent contractures while protecting the fracture as in a functional position splint that block MCP joints in flexion 23 to facilitate PIP joint extension while providing the proximal phalanx fracture with protection. This splint also allows the extensor hood to move proximally with MCP joint flexion, providing circumferential compression to the proximal phalanx fracture. At the same time it prevents MCP joint hyperextension which then focuses the extensor tendon tension at the PIP joint. With the MCP joints in flexion the flexor tendons also rest further away from the fracture site in the proximal phalanx, (Freeland et.al., 2003). This type of splint was used for Mr. A as soon as his wound healing allowed. A static splint to support the proximal phalanx fracture by immobilising the MCP joint was made. The splint provided circumferential thermoplastic support at the level of the proximal phalanx while allowing free PIP and DIP joint motion. This facilitated both extension and flexion of the IP joints as it immobilised the unaffected MCP joint (it prevented hyperextension at the MCP joint) while providing the fracture site with adequate support to make motion pain free, while hoping to allow adequate immobilisation of the fracture to ensure continued bone healing. As fracture healing for Mr. A was slow a smaller circumferential ring splint was used on surgeons request to support the fracture site without immobilising the MCP joint or the IP joints. This provided enough support to enable the patient to increase his function while limiting pain, as the surgeons were of the opinion that the fracture was showing adequate signs of healing. This was used as a step towards coping with no splint as the patient had become dependant on the static splint that included the MCP joint as he still experienced pain when using his hand without the support of the splint. Static progressive splinting: Once the initial oedema had settled and was only present in the finger the hand based splint was exchanged for a static progressive night splint to improve the PIP joint flexion contracture. This was a splint which had a volar gutter extending the length of the finger and proximally supported the finger to a level just proximal to the MCP joint. A dorsal cap which was secured with a D-ring strap fitted over the dorsum of the proximal phalanx. (Appendix 4) The extent of the pressure provided by the dorsal component was controlled by the patient who was instructed to keep pressure gentle so stretch could be maintained over a long period to ensure influencing the scar tissue positively. Fess (1998) reports that low-load application of force through splinting is the key to positively influencing scar matrix turnover and remodeling. The splint was maintained at night for 6 hours or more as it was suggested in the study by Glasgow, Wilton and Tooth, (2003). Although many questions about the ideal daily total end range time (TERT) were raised in this study it indicated that contracture resolution was at a faster rate if the TERT was more than 6 hours per day over a 4 week splinting period. The volar component of Mr. A’s splint was molded straighter than the finger flexion contracture and therefore allowed the contracture to gradually be stretched more as the joint contracture improved. Again we were limited by the fact that the fracture did not heal as was hoped and pressure was cautiously applied over the dorsum of the proximal phalanx. Excessive force application was avoided as not to cause further inflammation, scarring or motion at the fracture site. 24 Scar management: Hypertrophic or keloidal scars may develop when an excessive accumulation of collagen occurs. Hypertrophic scars are limited to the confines of the initial injury while keloids extend beyond the original wound. Surgery is rarely indicated in the management of scars and all non surgical options such as pressure garments or contact media need to be tried before surgery is considered. Masson (2003) suggests that pressure is thought to decrease tissue metabolism and increases collagen breakdown by increasing the activity of collagenase. This enzyme is heat-sensitive and therefore the local warming produced by a pressure garment may have its effect partially by this mechanism. He also suggests that treatment should persist for a minimum of 6 months and could be for as long as 2 years. Silicon gel sheets, putty or mineral gel digital sleeves may also be used in addition to pressure, to reduce raised or thickened scar tissue. These products are mainly used at night as they limit motion but could be worn during the day depending on the therapy programme. The exact mechanism of the silicon products is not known but they are thought to have a water retention effect. The capillary demand is reduced and thus reduced capillary activity and deposition of fibrous tissue follows, (Davey, 1997). They are not to be used on open areas of fragile skin. The pressure garment or gels need to be used constantly for the best results but need to be balanced with other rehabilitation goals and the products used will be chosen to best suite the individual patients needs. To mobilise superficial scar by stretching adhesions to underlying tissues, deep friction massage, crossing the grain of the tightening connective tissue, can be used, (Stewart Pettengill, 2003). All the above mentioned scar management methods were used in Mr. A’s case as the change in wound healing and splinting as well as increased function changed the most appropriate choice at any particular time. Primarily an attempt was made to maintain the best scar management at any particular time without compromising other aspects of his rehabilitation. Massage Massage can be used to soften tissue and scar and also to reduce oedema. It also enhances proprioception. Retrograde massage, which is performed in a distal-to-proximal direction, aids the venous and lymphatic systems in reducing oedema, (Sorenson, 1989). Sorenson also suggests that massage should be firm but gentle and can be carried out by the patient at home (2003). Elevation of the arm during massage will further facilitate drainage. According to Prosser (2003) it should be done for 3-5 minutes, distal to proximal 4-6 times per day. The patients’ skin quality must be monitored to avoid damage to newly healed skin. Diligent scar massage done for short periods frequently during the day is clinically very effective in mobilising the skin and subcutaneous soft tissues. A study by Patino, Novick, Merlo and Benaim (1998) showed no improvement after 3 months of friction massage therapy in paediatric patients with hypertrophic scars but massage was 25 for a 10 minute per day period only and further research was suggested. It remains a commonly used modality with clinicians supporting it widely. In the case of Mr. A, massage had to be very slowly upgraded due to extensive soft tissue damage and initial skin loss distally. This was essential to ensure that newly healed tissue was not damaged and that the inflammatory phase was not perpetuated. Retrograde massage was initially used for oedema and later as the wounds healed scar massage was used in conjunction with other scar management treatments. Exercise Feehan, L. M. (2003) quotes Tubiana as describing early fracture mobilisation as follows: “it must be gentle, never rough or painful, progressive, supervised and engage the active cooperation of the patient.” Exercise may be active, passive or resisted. In this case exercise used was mainly active due to continued fracture instability and passive motion was only used when fracture site was supported to avoid motion of the fracture. As fracture healing was slow, formal strengthening was not implemented as part of the programme although general hand strength increased with increased functional use and work. This did however mostly exclude the little finger which was the injured digit during the first 8 – 10 weeks and even thereafter, as non-union remained a problem. Exercise was used to maintain joint mobility, reduce oedema and to facilitate tendon and soft tissue glide during the healing phase. Tendon gliding exercises which maximises the differential glide of the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP) was important to maintain as extensive scarring had a significant affect on tendon glide even though there was no tendon repair. An attempt was made to perform the 4 basic tendon gliding exercises as described by Sorenson (1989) although full fist and flat fist was only possible towards the latter part of rehabilitation due to having to provide the fracture site with splint support. Place and hold exercises were also used to maximise tendon function and to improve active motion where passive motion had been achieved. Freeland et.al. (2003) reports that 5mm of excursion in the digital extensor and flexor tendons or PIP joint motion of 0 to 40 degrees, in the initial 4 weeks of rehabilitation, minimises the risk of serious tendon adhesions and is a favourable prognostic sign. These tendon gliding exercises remain important throughout the rehabilitation. Both extensor and flexor tendon gliding exercises need to be included and when splints were removed synergistic wrist motion was included with digital flexion and extension. Freeland et.al. (2003) also notes that strengthening and conditioning exercises should be gradually introduced into the rehabilitation programme beginning at 6 weeks after the fracture depending on the adequacy of healing as judged by clinical and x-ray evaluation. Formal strengthening was not used during Mr. A’s rehabilitation programme as bone union was not achieved. Rigid fracture fixation allows for earlier unprotected motion but they do not accelerate the fracture repair process and therefore all fractures need to be protected form excessive stresses during the inflammatory and repair phases. Progressive loading during 26 the remolding phase assists in callus conversion to bone and strength development in primary bone healing. Patient education As each patient is an individual, the response to injury will vary greatly. The goal of all hand rehabilitation is a hand that is functional and esthetically acceptable, (Stewart Pettengill, 2002). Psychological issues of confronting the injury and reintegrating the hand into normal use must be addressed. The therapist therefore does not only have to have knowledge of the physical injury and its implications but must also be able to understand the patient’s ability and motivation to participate in the therapy programme. The patients’ goals remain very important in determining the overall therapy programme. Mr. A, although remaining motivated during rehabilitation, needed encouragement and reassurance as to progress. He also benefited from education concerning the implications of his injury and was therefore able to, with good insight, become involved in his rehabilitation. His continued involvement in the rehabilitation ensured a good outcome for a very severe injury. Reflective practice Internal fixation of Mr. A’s comminuted fracture appeared in the very early stages to be inadequate and decisions concerning when to mobilise were initially inconsistent. This was due to the fact that damage to this finger was severe and there was a real chance of losing this finger. This made the early phase of eventual immobilisation less than optimal as the patient had been given different instructions by different staff members involved. This lack of complete immobilisation during the first week and then the decision to mobilise at 3 to 4 weeks, (possibly too early, considering the instability of the fracture) possibly added to the causes of slow bone healing. The decisions of when to progress treatment was also not made by the same surgeon on every occasion and in this case of a complex injury, such consistency may have been more ideal as it was always a difficult balance between fracture stability and mobilisation. Changes in therapy would have been to splint the patient for support of the fracture from the first day of mobilisation. This was however not done on surgeons request but later initiated due to patients continued report of pain and discomfort. Providing good splint support, while mobilising was also initially difficult, as this may have compromised wound healing. A more regular assessment of the level of pain experienced may have been useful in terms of clinical assessment of fracture healing, but at the time seemed unnecessary as pain was never a factor that greatly affected this patients’ involvement in rehabilitation. 27 Reference list 1. Connolly, W.B. and Prosser, R. (2003). The stiff hand. In: Prosser, R. and Conolly W.B. (dds). Rehabilitation of the hand and upper limb, ButterworthHeinemann, 2J, 83-94. 2. Cyr, L.M. and Ross, R.G. (1998). How controlled stress affects healing tissues. Journal of Hand Therapy, April-June, 125-130. 3. Davey, R.B. (1997). The use of contact media for burn scar hypertrophy. Journal of Wound Care, 6(2), 80-82. 4. Davidson, J.M. (1998). Wound repair. Journal of Hand Therapy, April-June, 80-94. 5. Feehan, L.M. (2003). Early controlled mobilization of potentially unstable extra-articular hand fractures. Journal of Hand Therapy, April-June, 161-170. 6. Freeland, A.E., Hardy, M.A. and Singletary, S. (2003). Rehabilitation for proximal phalangeal fractures. Journal of Hand Therapy, April-June, 129-141. 7. Fess, E.E. (1998). The influence of splinting on healing tissues. Journal of Hand Therapy, April-June 1989; 11:157-61. 8. Glasgow, C., Wilton, J. and Tooth, L. (2003). Optimal daily total end range time for contracture: resolution in hand splinting. Journal of Hand Therapy, 16(3), 207-218. 9. Jabaley, M.E. and Wegener, E.E. (2003). Principals of internal fixation as applied to the hand and wrist. Journal of Hand Therapy, April-June, 95-104. 10. Krop, P.N. (2003). Fractures: General principles. In: Mackin, E.J., Callahan, A.D., Skriven, T.M., et al (dds). Rehabilitation of the Hand and Upper Extremity, 5th ed. St. Louis, Mo: C.V. Mosby, 371-381. 11. LaStayo, P.C., Winters, K.M. and Hardy, M. (2003). Fracture healing: bone healing, fracture management, and current concepts related to the hand. Journal of Hand Therapy, April-June, 81-92. 12. Masson, J.A. (2003). Wound and tissue healing. In: Prosser, R. and Conolly, W.B., (dds). Rehabilitation of the hand and upper limb, 1st ed. ButterworthHeinemann, 1A, 1-4. 28 13. Michlovitz, S.L. and Harris, B.A. (2004). Therapy interventions for improving joint range of motion: A systematic review. Journal of Hand Therapy, AprilJune, 118-131. 14. Nedelec, B., Shankowsky, H. and Tredget, E. (2000). Rating the resolving hypertrophic scar: Comparison of the Vancouver scar scale and scar volume. Journal of Burn Care and Rehabilitation, (21), 205 -212. 15. Patino, O., Novick, C., Merlo, A. and Benaim, F. (1999). Massage in hypertrophic scars. Journal of Burn Care & Rehabilitation, 20(3), 268-272. 16. Pettengill, K.M. (2002). Therapist’s management of the complex injury. In: Mackin, E.J., Callahan, A.D., Skriven, T.M., et al (dds). Rehabilitation of the Hand and Upper Extremity, 5th ed. St. Louis, Mo: C.V. Mosby, 2002:1411-26. 17. Prosser, R. (2003). Therapy principles and modalities. In: Prosser, R. and Conolly, W.B., (dds). Rehabilitation of the hand and upper limb, 1st ed. Butterworth-Heinemann, 1B, 5-10. 18. Purdy, B.A. and Wilson, R.L. (2002). Management of non-articular fractures of the hand. In: Mackin, E.J., Callahan, A.D., Skriven, T.M., et al (dds). Rehabilitation of the Hand and Upper Extremity, 5th ed. St.Louis, Mo: C.V. Mosby, 382-395. 19. Scougall, P. and Prosser, R. (2003). Metacarpal and phalangeal fractures. In: Prosser, R. and Conolly, W.B., (dds). Rehabilitation of the hand and upper limb, 1st ed. Butterworth-Heinemann, 2B, 28-39. 20. Shrikant, J.C. and Gan, B.S. (2003). Management of proximal interphalangeal joint fractures and dislocations. Journal of Hand Therapy, April-June, 117-128. 21. Sorenson, M.K. (1989). The oedematous hand. Physical Therapy, 69(12), 6772. 22. Sutton, G.S. and Bartel, M.R. (1994). Soft-tissue mobilization techniques for the hand therapist. Journal of Hand Therapy, July-September, 185-192. 23. Purdy, B.A. and Wilson, R.L. (2002). Management of non-articular fractures of the hand. In: Mackin, E.J., Callahan, A.D., Skirven, T.M., et al (dds). Rehabilitation of the hand and upper extremity, 5th ed. St. Louis, Mo: Mosby, 2002:382-95. 24. Wheen, D. (2003). Peripheral nerve injuries. In: Prosser, R. and Conolly, W.B. (dds). Rehabilitation of the Hand and Upper Limb, 1st ed. ButterworthHeinemann, 7A, 274-286. 29 Appendix 1 Objective measurements Range of motion – summary Date MCP joint PIP joint DIP joint 30/3 0-65 11/4 0-70 27/4 N/A 10/5 N/A 25/5 N/A 15/6 N/A 4/7 N/A 4/8 N/A 30-50 20-55 25-55 22-70 20-85 25-75(90) 20-80 0-25 6-35 15-55 10-42(55) 10-60(90) 0-50(70) 10-60(80) 15-80(65 if fracture unsupported) 25(0)-70 All joint range measurements were taken with fracture site supported and as indicated in last measurement the range is limited by pain if unsupported All measurements in brackets are passive ranges MCP joint measurements were not taker after the first month of treatment as near normal range had been achieved. Oedema – circumferential measurements taken at mid- phalangeal level(summary) Date 30/3 Middle 86mm phalanx Proximal 95mm phalanx 11/4 76mm 27/4 72mm 10/5 74mm 25/5 72mm 15/6 71mm 4/7 71mm 4/8 67mm 92mm 87mm 89mm 92mm 85mm 83mm 83mm 30 Appendix 2 Modified Vancouver Scale (Hutt Valley Health) 31 Appendix 3 Semmes-Weinstein Monofilament Assessment 32 Appendix 4 33