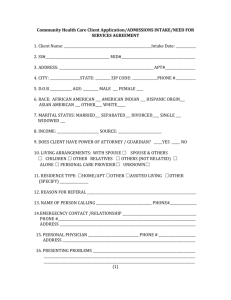
F4 CAP Functional Assessment Tip Sheet
advertisement

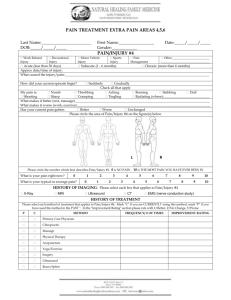
CAP FUNCTIONAL ASSESSMENT TIP SHEET ADL Self-Performance Scores 0 Independent: No help or caregiver oversight: OR caregiver oversight provided only 1 or 2 times during he last 7 days. (Evaluation tip: Does the client walk about at lib, performs bathing, dressing, toileting, eating without set-up or supervision and they are not incontinent. Or, they could need occasional prompts or assistance, if not more than once or twice during the last 7 days.)* 1 Supervision: Oversight, encouragement, or cueing provided 3 or more times during he last 7 days, OR supervision (3 or more times) plus assistance provided, but only 1 or 2 times during the last 7 days. (Evaluation tip: You would not trust them to walk on all home surfaces, such down steps without someone supervising, giving verbal instructions, standby assistance for safety, or reminders to use device. Do they need verbal cues, stand-by assistance or encouragement to complete bathing and dressing, feeding? Even if they required some physical assistance but not more than once or twice in the last 7 days, code as supervision (1))* 2 Limited assistance: Client highly involved in activity received physical helping guided maneuvering of limbs or other non-weight bearing assistance on 3 or more occasions. OR limited assistance (3 or more times) plus more weight-bearing support provided, but only 1 or 2 times during the last 7 days. (Evaluation tip: Minimal Assistance provided. Do they require hands on assistance for safety for the fear they would miss-step, or to correct loss of balance, or with weight bearing precaution? Do they need assistance with a portion of their bathing, dressing or feeding items? Do they need a helping hand?)* 3 Extensive Assistance: While client performed part of activity over the last 7 days, weight-bearing support or full caregiver of activity occurred 3 or more times during part (but not all) of last 7 days. (Evaluation tip: Do they require more consistent help to bear weight, or correcting balance? More intervention and effort is needed by caregivers to safely manage transfers. Caregivers perform much of the ADL for bathing, dressing, toileting, feeding. Substantial or consistent hands-on assistance with eating, toileting, bathing, dressing, personal hygiene, self-monitoring of meds and/or with weight bearing assistance is needed. The client needed weight bearing support 3 or more times. Or the caregiver totally performed the activity, without any assistance from the client, 3 or more times, but not all the activity, for the last 7 days.)* 4 Full dependence: Full caregiver performance of activity during the last 7 days. Evaluation tip: are unable participate, caregivers fully perform the ADL during the last 7 days 8 Activity did not occur. (Not performed by the client or for the client during the entire 7 day period.*) Support Provided Scores 0 No set-up or physical help needed. Evaluation Tip: The client can perform the entire activity on their own. )* 1 Set-up help only ( Evaluation Tip: If the client is provided with materials or the necessary device, they can perform the ADL independently)* 2 1 person physical assistance- (The ADL is accomplished with the assistance of one person) * 3 2 + persons assist and/or one person assist w/ assistive equipment (Two or more persons were required to assist the client perform the ADL)* 8 Activity did not occur (The activity did not occur in the prior 7 days by the client or someone to provide the ADL)* * Evaluation tips, not part of the program scoring instructions. ADL Support Provided Scores should correlate to ADL Self-Performance Scores Factors Affecting Performance ADL performance can be permanently or temporarily limited by the patient’s physical condition, mental, emotional or cognitive status, activities permitted medical restrictions and environmental barriers. Consider these limitations in accessing ADL performance. The home environment ( lighting, stairs, floor surfaces and pathways and door thresholds, availability of adaptive equipment, location and accessibility of bathrooms and closets) Physical function ( vision, ROM, strength, endurance, dexterity, balance, coordination, ability to chew and swallow) Medical restrictions (weight bearing precautions, hip precautions, orders for bed rest, aspiration precautions, dressings, splints or slings to be kept dry) Physical and clinical conditions (pain, paralysis, edema, impaired balance, strength and sensation, visual acuity, presence of wounds, lesions, feeding tubes, catheters) Cognitive/emotional/behavior state ( cognitive ability, alertness, judgment, ability to sequence tasks, fear of activity, fear of falling, attention span) ADL Item Ambulation, inside Ambulation, outside Bathing Bed mobility Dressing Eating Personal hygiene (grooming) Toilet use Transfer. Definition Measures how well the client ambulates in their home, and outside of their home. Additional Information Consider Factors Affecting Performance on page 1 including environmental barriers Measures how well the client takes full-body bath/shower or sponge bath (EXCLUDE washing of back and hair and TRANSFER). Includes how each part of body is bathed: arms, upper and lower legs, chest, abdomen, perineal area. Measures how well the client moves to and from lying position, turns side to side, and positions body while in bed. Consider Factors Affecting Performance, bathroom accessibility, and availability of assistive devices Measures how well the client dresses and undresses above and below the waist, including prostheses, orthotics, fasteners, pullovers, shoes, socks, belts. Measures how the client eats and drinks (regardless of skill), includes intake of nourishment by other means (e.g., tube feeding, total parenteral nutrition) Measures how well the client maintains personal hygiene, including combing hair, brushing teeth, shaving, applying makeup, washing/drying face and hands (excludes baths and showers) Measures how the client uses the toilet (or commode, bedpan, urinal) cleanses self after toilet use or incontinent episodes, changes pad, manages ostomy or catheter, adjust clothes ( EXCLUDE transfers to toilet). Measures how well the client moves between surfaces-to or from: bed, chair, wheelchair, standing position. Consider Factors Affecting Performance, do they have a hospital bed with rails to assist with bed mobility or a trapeze. This item contributes to RUG Calculation Consider Factors Affecting Performance Consider Factors Affecting Performance. Is the client fed by tub feedings or TPN? If so, what assistance to they need. This measure does not include food preparation which is an IADL. This item contributes to RUG Calculation Consider Factors Affecting Performance such as cognition, sequencing of tasks. Consider Factors Affecting Performance bathroom accessibility and accommodations including This item contributes to RUG Calculation Consider Factors Affecting Performance such as barriers in the bedroom. Does wheelchair have removable arms and legs; is the bed adjustable for ease of transfer? This item contributes to RUG Calculation