Cardiovascular System
advertisement
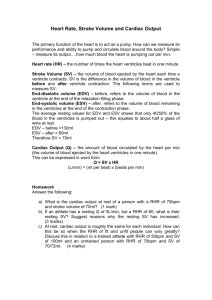
Cardiovascular System I. Cardiac function A. Cardiac cycle: four-phase cycle in which one complete heartbeat occurs We looked at the cardiac cycle with respect to the left side of the heart, so anything dealing with the cardiac cycle, unless otherwise noted, will be talking about the left side of the heart. 1. 2. Phases a. Phase one i. Early ventricular filling – blood passively flows into ventricles from atria ii. Late ventricular filling – blood actively flows into ventricles from atria via atrial contraction; only 20% of stroke volume (amount of blood circulated through the body from one ventricle per heartbeat) comes from late ventricular filling b. Phase two – isovolumetric contraction (ventricular contraction that occurs when mitral valve is closed and the volume in the left ventricle stays the same [isovolumetric]), which increases pressure required for ejection c. Phase three – ejection phase, in which pressure inside left ventricle exceeds pressure of aortic semilunar valve, causing blood to be ejected from left ventricle and into aorta d. Phase four i. Isovolumetric relaxation: ventricular relaxation that occurs when the aortic semilunar valve is closed and the volume in the left ventricle stays the same [isovolumetric] ii. Dicrotic notch: graphic representation of changes in pressure in the aorta after receiving blood from the left ventricle; represents aortic recoil, in which a decrease in pressure in aortic arch decreases (as the aortic semilunar valve closes) is followed by an increase in pressure in the aortic arch (as a result of blood continuing to flow through the aorta) Pressure differences between the ventricles a. Pressure in right ventricle is 25% of pressure in left ventricle; however, volume ejected by both ventricles is equal The right ventricle has to pump blood over a relatively short distance (from the heart to the lungs), whereas the left ventricle has to pump blood to the entire rest of the body. However, the blood that gets pumped to the lungs (from the right ventricle) is the blood that flows to the rest of the body (from the left ventricle). In order for the body to maximize efficiency, the amount of blood that gets oxygenated in the lungs should be equal to the amount of blood that flows to the rest of the body. b. 3. Pulmonary circuit has less resistance than systemic circuit This is another reason why the right ventricle doesn’t have to pump as hard (i.e. with as much pressure) as the left ventricle. Because there is so much resistance in the systemic circuit, due mainly to length (as length of blood vessels increases, resistance increases), the left ventricle has to pump much harder in order to overcome the resistance. Pressure-volume loop: shows relationships between pressure and volume in one side of the heart Again, most of the discussion focuses on the left ventricle, so unless otherwise noted, notes about the pressure-volume loop will be talking about the left ventricle. a. b. c. d. e. Inverse relationship between pressure and volume (i.e. as pressure increases, volume decreases) End systolic volume (ESV): the volume of blood remaining in a ventricle at the end of ventricular contraction (systole) End diastolic volume (EDV): the volume of blood in a ventricle at the end of ventricular filling (diastole) Work = pressure × volume Net work done by heart = work during systole – work during diastole During diastole, the heart does not do any actual work. During systole, the heart does work. However, when looking at a pressure-volume loop, the work done during both diastole and systole are present. In order to determine what work is actually done by the heart, the work done during systole must be subtracted from the work done during diastole. B. Factors affecting the work of the heart 1. Heart rate: rate at which the heart pumps blood; measured in beats per minute (bpm) 2. Preload: degree to which cardiomyocytes are stretched before they contract; increases contractility of cardiomyocytes Increasing the length of stretch in cardiac muscle optimizes the amount of actin-myosin overlap, creating greater contraction strength. 3. C. Afterload: pressure that must be exerted to eject blood from ventricles; pressure in ventricles must exceed pressure of semilunar valves for ejection to occur 4. Contractility: increase in contractile strength independent of muscle stretch (preload) and EDV (afterload); e.g. Ca2+ influx, which causes rapid depolarization Types of work performed by the heart 1. Pressure-volume work a. Work = pressure × Δ volume b. Ejection fraction: pressure needed to move a given volume of blood 2. Kinetic energy (KE) work a. KE = ½(mass)(velocity)2 b. Describes acceleration of blood flow provided by heart during contraction The amount of work being done by the heart, in terms of kinetic energy work, can be analyzed by looking at how much blood is being pumped (mass) and how fast that blood is moving (velocity), due to the pressure driving the movement. 3. Tension-time work a. Compares tension produced in ventricular wall and time that tension is held b. Work = k × tension × Δ time The amount of work done by the heart increases with both tension and time (i.e. if time or tension increases, the work done by the heart increases). D. 4. Total work = (pressure × Δ volume) + (½(mass)(velocity)2) + (k × tension × Δ time) LaPlace’s law: wall tension = wall stress ÷ wall thickness There is a direct relationship between the amount of tension on the ventricular walls and the amount of stress placed on them. Wall thickness remains constant, so if stress (i.e. pressure) increases, then tension increases. There is an inverse relationship between wall tension and wall thickness. If wall stress stays constant, then wall tension will decreases as wall thickness increases. 1. 2. E. Transmural pressure: pressure exerted on walls of ventricle due to filling (with blood) In response to transmural pressure, ventricular wall exerts inward tension to resist stretch; requires ATP 3. Increased stress on wall = increased preload = increased myocardial O 2 consumption (VO2) Cardiac output: volume of blood (generally liters) pumped by the heart per unit time (generally minutes) 1. Product of heart rate and stroke volume; Cardiac output = heart rate × stroke volume Q = HR × SV 2. Factors regulating cardiac output a. Heart rate i. Parasympathetic nervous system – decreases heart rate ii. Sympathetic nervous system – increases heart rate b. Stroke volume i. Mean arterial pressure (MAP) (average blood pressure) – increased MAP leads to decreased stroke volume (as long as cardiac output stays consistent) ii. Sympathetic nervous system – increases contraction strength, which increases stroke volume iii. Frank-Starling mechanism: degree of muscle stretch (preload) controls stroke volume Increased muscle stretch = increased contraction strength = increased stroke volume Increased EDV = increased muscle stretch = increased contraction strength = increased stroke volume Increased EDV means there is more blood in the ventricles before contraction. The ventricles will be more stretched, optimizing actin-myosin overlap, leading to greater contraction strength, which leads to increased stroke volume. iv. 3. 4. F. HR – inverse relationship between HR and SV (i.e. if Q stays consistent, then SV will decrease as HR increases) v. Afterload – decreased afterload = increased SV Cardiac output is a function of the work task, not the person performing the task Cardiac output is proportional to absolute VO2, not max VO2 Cardiac output is proportional to available O2, not the maximum O2 levels of the body. Heart rate 1. Ventricular filling occurs during diastolic phase 2. As HR increases, time for diastolic filling decreases Decreasing the time for diastolic filling allows the ventricles to pump more frequently, supplying the body with more blood. G. 3. Direct relationship to work rate up to a maximum HR 4. Maximum HR = 220 – age 5. Maximum HR does not increase with physical training EDV and preload are affected by venous return (flow of blood back to the heart via the veins) 1. Venoconstriction: constriction in diameter of veins; reduces amount of blood returned to the heart, ultimately resulting in decreased EDV 2. Skeletal muscle pump: rhythmic skeletal muscle contractions that force blood in the extremities to move toward the heart; one-way valves in veins prevent backflow of blood 3. Respiratory pump: use of differential pressure created by breathing to cause blood to move back towards the heart a. Pressure gradient exists between thorax and abdomen b. Decrease in thoracic pressure relative to external environment during inspiration (breathing in) allows air to flow into lungs At rest, the lungs do not take in air because the pressure inside the lungs is equal to atmospheric pressure. Decreasing thoracic pressure allows the lungs to take in air during breathing. c. Decreased thoracic pressure causes increased pressure in abdomen Because there is a pressure gradient between the thorax and the abdomen, the pressure in both locations will change if the pressure in one location changes. d. H. To alleviate pressure differences, blood flows from area of higher pressure (abdomen) to area of lower pressure (thorax, specifically inferior vena cava of heart) Ventricular contractility 1. Mediated by sympathetic nervous system 2. Increasing SV a. Circulating epinephrine and norepinephrine – cause sympathetic innervation b. Direct sympathetic stimulation of heart c. Increased Ca2+ permeability in myocardium – faster depolarization i. Increased local permeability to Ca2+ ii. Increased sensitivity of sarcoplasmic reticulum to extracellular Ca 2+ In cardiac muscle, extracellular Ca2+ triggers release of intracellular Ca2+ from sarcoplasmic reticulum, ultimately resulting in increased strength of contractions. iii. d. e. Enhanced Ca2+ reuptake by sarcoplasmic reticulum, increasing available Ca 2+ stores iv. Increased Ca2+ conductance, increasing Ca2+ available for storage in sarcoplasmic reticulum Increased ejection fraction Decreased residual volume (here, amount of blood left in heart after contraction) – decreased residual volume = increased SV 3. SV = EDV – ESV a. Frank-Starling mechanism affects SV by increasing EDV Increasing the amount of stretch on the ventricles (by increasing EDV) results in stronger contractions, which result in higher SV. It is important to note that the Frank-Starling mechanism does not act to increase SV, but to maintain it. b. 4. 5. Contractility affects SV by decreasing ESV Decreasing the amount of blood left in the ventricles after contraction (decreasing ESV) implies higher SV. Because increasing EDV requires ATP (see LaPlace’s law), the body chooses to increase contractility (by decreasing ESV) to maintain SV. Sympathetic nervous system innervation a. Norepinephrine initiates cAMP system, which opens Ca2+ channels in plasma membrane b. Increased extracellular Ca2+ increased intracellular Ca2+ increased depolarization High afterload decreased stroke volume If there is a high amount of pressure required to force blood out of the ventricles (i.e. high afterload), then the amount of blood pumped out of the heart will be lower (i.e. decreased stroke volume). However, it is important to note that afterload is relatively constant and normally does not affect SV. I. J. 6. Maximum SV affected by reduced diastolic filling time and chamber volume Factors affecting arterial blood pressure 1. Factors that increase arterial blood pressure (BP) a. Increased blood volume b. Increased HR c. Increased SV d. Increased blood viscosity e. Increased peripheral resistance (i.e. afterload) 2. Expressed in terms of systolic and diastolic pressures a. Expressed as systolic pressure (pressure created during systole) over diastolic pressure (pressure created during diastole) b. Normal BP: 120/70 mmHg c. High BP: > 140/90 mmHg 3. Pulse pressure: difference between systolic and diastolic pressures Pulse pressure = systolic pressure – diastolic pressure 4. Calculating MAP a. MAP = diastolic pressure + 1/3 (pulse pressure) b. MAP = Q × afterload O2 delivery during exercise 1. O2 demand much higher during exercise than at rest This occurs due to the need to produce more ATP. 2. Ways to increase O2 delivery a. Increased Q b. Redistribution of blood flow to skeletal muscle i. Tissues may need more O2 (and therefore more blood), but Q cannot increase that much flow must be redistributed among tissues ii. Muscle blood flow to working muscles increases iii. Splanchnic blood flow (blood flow to liver, kidneys, and GI tract) decreases c. Increased extraction of O2 by skeletal muscle d. Autoregulation e. Increase local vasodilation – LOCAL VASODILATION OVERRIDES SYSTEMIC VASOCONSTRICTION K. L. Fick principle: used to measure volume of O 2 used by the body volume of O2 used = cardiac output × (arterial O2 concentration – venous O2 concentration) VO2 = Q × (CaO2 – CvO2) MAP is relatively constant – increase in systolic pressure is almost offset by decrease in diastolic pressure, so there is only a small change in MAP as work rate increases In order to maintain homeostasis in blood pressure, increases in systolic pressure can be balanced with decreases in diastolic blood pressure so that overall blood pressure remains relatively constant. M. N. O. P. Q. R. Total peripheral resistance (TPR): total resistance of the arteries in the body 1. Pressure = flow × resistance 2. If MAP (pressure) stays constant and cardiac output (flow) increases, then TPR (resistance) decreases 3. Because MAP is relatively constant, decrease in TPR causes increased cardiac output Cardiac limitations to performance 1. Cardiac performance can be analyzed using Fick principle - VO2 = Q × (CaO2 – CvO2) 2. VO2 = Q × (CaO2 – CvO2) = HR × SV × (CaO2 – CvO2) 3. Maximum HR = 200 bpm 4. Maximum CaO2 = 20 ml O2/dL 5. Minimum CvO2 = 2 ml O2/dL 6. SV is only variable with relatively large limits SV determines limitations for cardiac performance Cardiovascular control during exercise 1. Initial signal to “drive” CV system comes from higher brain centers 2. Feedback from chemoreceptors, mechanoreceptors, and baroreceptors modify CV control 3. CV adjustments to exercise a. Increase blood flow to skeletal muscles i. Increased skeletal muscle activity metabolic vasodilation in muscles ii. Sympathetic vasoconstriction in viscera b. Increase cardiac output i. Deeper breathing improved venous return increased stroke volume ii. Skeletal muscle activity improved venous return increased stroke volume iii. Adrenal gland stimulation increased heart rate and increased stroke volume Factors regulating cardiac output 1. Stressors 2. Blood pressure 3. Blood volume 4. Chemicals in body CV control 1. Blood pressure acts as the parameter necessary to initiate negative feedback control on heart 2. Factors that control HR and SV ultimately have control over cardiac output CV response to hemorrhage 1. Regulated by sympathetic nervous system 2. Processes a. Decreased activity in high-pressure baroreceptors = enhanced sympathetic activation If high pressure decreases in the body, then the body is not pumping enough blood. Therefore, the sympathetic nervous system will increase cardiac output, by increasing HR and SV. b. Decreased activity in low-pressure volume receptors = decreased glomerular filtration rate (rate at which kidneys filter blood) and increased ADH secretion If the volume receptors have decreased rates of activity, then the fluid levels in the body are low. Therefore, the body will reduce glomerular filtration rate and increase ADH secretion in order to maintain blood fluid levels. S. c. Decreased peripheral chemoreceptor activity d. Increased central chemoreceptor activity If a hemorrhage occurs, the body needs to focus more on the hemorrhage rather than other activities. If a hemorrhage occurs, the body needs to focus more on the hemorrhage rather than other activities. Cardiac insufficiency (see slide 50) 1. Sympathetic compensation for cardiac insufficiency (see slide 51) 2. Renal compensation for cardiac insufficiency (see slide 52) Sympathetic compensation aims to increase cardiac activity in order to make up for all of the cardiac insufficiencies present in the heart. Renal compensation aims to maintain blood fluid levels and ion concentrations in order to make up for all of the cardiac insufficiencies present in the heart.